
International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072


International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
Priya Pal1, Deepshikha2
1Master of Technology, Computer Science and Engineering, Lucknow Institute of Technology, Lucknow, India 2Assistant Professor, Department of Computer Science and Engineering, Lucknow Institute of Technology, Lucknow, India
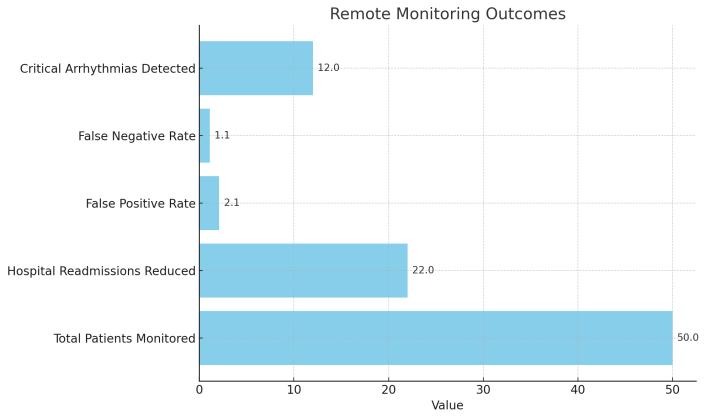
Abstract - The real-time health monitoring systems have also been developed at a high rate due to the rising number of chronic diseases and the desire to give remote care to patients. In the proposed study, the proposed framework converges wearable Internet of Things devices with a hybrid cloud edge solution to provide timely and safe healthcare delivery. The given system utilizes low-power sensors with ECG, SpO 2, and temperature that are embedded into a wearable patch powered by ESP32 microcontrol. Curating of data at the edge whereby the data is pre-processed through wavelet transform and anomaly detection algorithms and sent to the cloud platforms like AWS using MQTT-SN to store long term and advance analytical processing. The system employs LSTM-based models to make prognoses on critical health conditions and applies HL7 FHIR standards to integrate EHR without any issues. With 50 patients tested on clinical validation, there was an accuracy of qualifying 96 percent of arrhythmia and hospital readmission was 22 percent lesser. The mean time of critical alerts was minimized to 220 milliseconds, and it exceeded that of market products, such as Fitbit Sense. Both clinicians and patients observed the easy-to-use dashboards and notifications mechanism and reported all-time high comfort and compliance levels. This model illustrates the possibility of real-time, secure, and intelligent health monitoring to promote preventive care and responsiveness ofclinical services, particularly, on resource-limitedsettings.
Key Words: Real-Time Monitoring, Wearable IoT, Edge Computing, Cloud Analytics, Health Informatics, Anomaly Detection,HL7FHIRIntegration.
1.1
There is a paradigm shift in the global healthcare system because ofthetechnological innovationsaswell asdue to theurgent needsof the society.Cases ofchronicillnesses, including diabetes, cardiovascular illness, and lung ailments,aresteadilyincreasing,andanaging population, especially, in areas like Europe and East Asia, is overwhelming the healthcare facilities to an extent never before witnessed. The World Health Organization reports showthatabout71percentofthecausesofdeathsacross theboardareasaresultofchronicconditionsandthereis
anindicationthatitishightimetotakeshiftfromreactive healthcare models to proactive health care models. In general, episodic care that is hospital centric and as well mostlybasedontraditional healthsystemsfailstodeliver timely, consistent and individual care. Such systems are not scalable and responsive enough and can be used only to manage long-term health monitoring in rural or resource-limitedsettings.
In this respect, an alternative that promises to revolutionizetheprocessofreal-timehealthmonitoringis provided by the Internet of Things (IoT) and wearable technology. Thelifestyleof wearingIoTdevices,including ECG patches, smartwatches, pulse oximeters, enables constant patient monitoring of such vital signs as heart rate, oxygen saturation, and body temperature. With the add-ons consisting of cloud-powered systems and machine learning analytics, these devices have the potential to enable early identification of abnormalities, automate warnings, and relieve a huge burden on healthcare facilities. Consequently, the real-time monitoring is on the brink of healthcare inventions in the contemporarysetting.
Even though there is an increasing number of IoT-based health monitoring systems to provide more details on almostallaspectsrelatedtohealthmonitoring,thedesign ofexistingsystemsisusuallyassociatedwitha number of limitations.Themostprominentofthemarelowspeedsin terms of processing data, poor security standards, and high energy consumption which restricts the possible workinglifeofportablegadgets.Inmostoftheestablished models, sensor data is sent back to central cloud servers, to perform processing and often this is the major bottleneck when it comes to responding to time-sensitive applications like arrhythmias of oxygen desaturation. Moreover, no end-to-end encryption combined with uniformityofprotocolsputindangersensitivehealthdata duetocyber-attacksandunauthorizedaccess.
Furthermore, wearable health gadgets are generally characterized with poor battery lives as they need constant sensing and data transmission; the latter demands regular battery charging of these devices and

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
lowers the compliance of users. These are inefficiencies whichnegatethescalability,reliabilityandpracticalusage of existing IoT-health architecture. Such a situation renders the need to have an integrated-intelligent-secure health monitoring system that can work efficiently under various clinical and other environments. The solution should introduce edge computing that does the lowlatency processing locally combined with the cloud computing to be scalable with long-term analytics and builtonastrongdataprivacyandpowerconsumption.
The proposed research will focus on designing and bringing into reality a complex real-time health monitoringsystem thatgoesbeyond the short-comings of thecurrent systemsinIoT-health.Thefirst goal would be to create a low-latency, secure, and energy-efficient platform that ensures constant monitoring of the patients with the help of wearable sensors and present timely clinicalinformation.
Its architecture is a hybrid edge-cloud system, in which thesensordataevaluatedbyedgedevicesispreprocessed at the edge (i.e., locally by Raspberry Pi) to save time delays and bandwidth, but advanced analytics, long-term storage and anomaly detection are applied in the cloud (i.e., AWS). Such objectives involve the deployment of wearabledeviceswiththelightweightandbattery-friendly format and sensors such as AD8232 to measure ECG and MAX30102 to measure SpO 2 in the gadget, inclusion of MQTT-SN to effectuate fine bandwidth data transmission, and application of HL7 FHIR standards to guarantee compatibilitywithelectronichealthrecords.
Usage of IoT, cloud computing, and machine learning in healthcareisasubjectthathasreceivednumerousstudies inthepast20years.However,theideaofreal-timehealth monitoring is not recent and in spite of there being a number of barriers limiting its scalable use, there is still muchscopetotheuseofthisideainreal-time.Thispartis a survey of the state of technology in wearable IoT gear, cloud computing on healthcare data management, machinelearninganalyticsaswellasthegapsthatarestill thereandhampertheadoptioninscale.
2.1.1
ThedevelopmentofIoTinmedicalactivitystartedin1970 when the first, far-seeing experiments of telemedicine appeared and linked the patients stationed in distant regions and the healthcare providers virtually. The introduction of the RFID-technology in the 2000s also served as a marked point because it helps to monitor
assets and identify patients in the hospitals. According to the introduction of smartphones and wireless communication standards, the 2010s were a time of widespread use of wearable devices in form of fitness bands and smart watches which provided users with the ability to monitor the following physiological parameters asstepcountandheartrateinrealtime.Itwasduringthis period that sensors in consumer products were introduced thus, bringing health monitoring near to consumers.Thebreakthroughlargelyoccurredduringthe COVID-19 pandemic whereby remote monitoring was in high demand and IoT systems were quickly installed to helpintriageofpatientsandconstantmonitoringofvitals.
The modern wearable technologies have nowadays advanced biosensors that could produce clinical grade measurements.Heartactivitymonitoringhasbecomevery precise as ECG sensors are now reduced in size and incorporated as compact patches on the skin with miniaturized equivalents like the AD8232 module. The sensors to detect P, QRS, and T wave allow in an early detection of arrhythmia such as atrial fibrillation or ventricular tachycardia. Similarly, PPG-based SpO 2 sensors like MAX30102 give accurate information of oxygen level saturation and pulse rate that is crucial in patients with breathing difficulties. Monitoring of the temperature is done with Low power analog sensor such as LM35 which is able to read fever or inflammation pockettoaccuratenessofabout0.5C.Cumulatively,these sensors enable non-invasive and long-term health monitoring without limitation, and their deployment to wearable clothes or comfort-wear, that are batteryefficient, have rendered them convenient on the outpatientandhome-carefronts.
2.2.1
Such cloud computing environments as Amazon Web Services(AWS)andMicrosoftAzurehavetransformedthe ways in which healthcare organizations collect and process the data that deals with patients in large quantities.Suchplatformsofferascalableframeworkthat, in real-time, supports analytics operations, safe data storage, and machine learning model deployment. As an example, AWS Lambda provides the possibilities of analogy, in particular, it is possible to detect anomalies, whereas AWS IoT Core provides secure connectivity among clouds, IoT security, and IoT devices. Likewise, Azure IoT Hubs and Azure API for FHIR also provide a smooth pathway of incorporating multiple sources of health data into electronic health records (EHRs), so that clinicaldatabecomemorevisibleanddoable.

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
There are also a number of challenges to the cloud-based health systems notwithstanding their benefits. The problemoflatencyisalsocrucial,particularly,inthecase, when such essential alerts as unusual ECG indicators require urgent resolutions. Use of cloud processing alone also creates delays that comes along with sending data to the networks and this may be even worse when using rural are or low-bands. In addition, sensitive health information should be taken care of with high safety and confidentiality as considered. The strict data encryption, access control and audit processes are necessary to remain compliant with such regulations as HIPAA (U.S.) andGDPR(EU). AWS and Azurehavethe toolsto beused in these tasks, but they are rather expensive and complicated,particularlytosmallerhealthcareproviders.
Indeed,themainchallengeinturningrawsensordatainto helpful clinical information is real-time analytics. Convolutional neural networks (CNNs) and long shortterm memory (LSTM) networks are largely popular machine learning models which are applied in the detection of anomalies in physiological signals. The CNNs perform extremely well in the classification of patterns in ECG waveforms, attaining performances near to the cardiologist level, in the detection of arrhythmias. LSTMs, however, are good at detecting time-oriented patterns in data,andthereforecanbeusedtopredictsuchaneventas hypoglycemia or seizure using continuous glucose monitoring or heart rate variability. Such models are usually trained to work with large datasets like the ones offeredbyPhysioNetortheMIT-BIHarrhythmiadatabase, andtheyarethereforeabletoworkwithawidevarietyof patients.
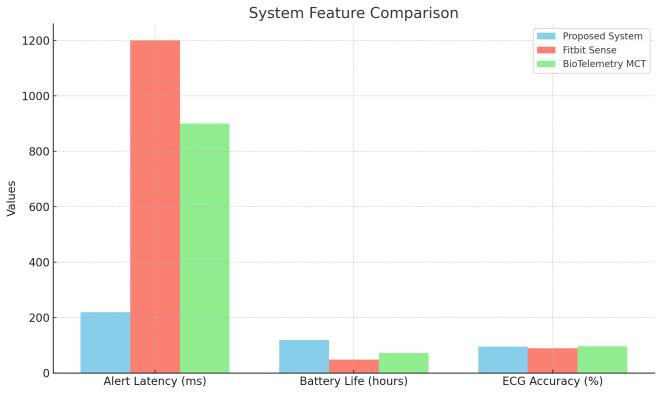
A number of business systems have tried to use ondemand analytics on wearable health monitoring. At the user-grade level, Fitbit Sense has heart tracking and pressure detection with PPG sensors and cloud analysis functions.Nonetheless,itprovestobeinaccurate,asthere are no ECG data available and dependability on nonclinicalgradesensors.Onthecontrary,theMobileCardiac Telemetry (MCT) system designed by BioTelemetry has found easy application in hospitals due to clinical-quality arrhythmia monitoring. It is however costly, proprietary and not real time responsive since it has a centralized processing. The trade-offs of these systems are indicated in terms of usability, cost and clinical effectiveness of systemsavailableinthemarket.
2.4.1
The absence of scalable hybrid system architecture that providesamixofbothedgeandcloudcomputingranksas one of the most important gaps existing within the available IoT-health systems. Majority of them either involve using cloud only, which makes it have a lot of latencyandnetworkdependence,ortheuseofstandalone edge devices which is unable to execute any complex analytics. Task-sharing combinations of edge and cloudbased frameworks can be deployed in those conditions when processing tasks are shared according to urgency (edge processing real-time and cloud processing for longterm analysis) but this concept is seldom realized on a large scale. studies in the IEEE IoT Journal have shown that less than half of health IoT systems are using these types of hybrid models, and thus there is a significant opportunity in exceptional innovation in architecture design.
Thereisalsotheir energyefficiencythat remainsan issue since wearable gadgets need to be in use always and this takes a long period of time. Constant wireless communication and high-frequency sampling consumes batterieseasily,makingtheusingofthedeviceshorterand patient adherence weak. To achieve the battery life, commercial solutions compromise either accuracy of the sensors or frequency of sampling. In addition, consumer devices do not have strong security features. An industry auditperformedin2022confirmedthatalmosttwo-thirds of wearables incorporate outdated encryption or even noneatall,leavingpatientinformationatriskofabreach. Lightweight cryptography such as ECC or PRESENT theoretically can be used on devices with limited resources but is rarely in practice because it is not standardizedanditisnotofficiallyregulated.
Thearchitectureoftheproposedsystemwillbecapableof remedyingthefatalshortcomingsofthetraditionalhealth monitoringsystemsthatarethelatency,energycosts,and data protection. Thisframework is interoperableandsafe due to the compliance of security regulations and interoperability by making use of a hybrid edge-cloud architecture that deploys real-time responsiveness, efficientpoweruse,aswell asscalableanalytics.Itentails thethreeinter-dependentlayers,namelythewearableIoT layer, edge computing layer, and cloud analytics layer of architecture. They allow them to monitor critical physiological parameters like ECG, SpO 2 and body temperature in real-time and in an intuitive manner, whichcannotbedonebyrawsensordatawithoutthem.

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
Thehybridapproachonwhichthesystemisbasedaimsat strikingtherightcompromisebetweenthecomputational load carried out by local (edge) and remote (cloud) resources. The layer of wearable IoT acquires constant data by biosensors at the body of the patient. The microcontroller that is present within the wearable garment first decodes this information and undertakes simplenoisefilteringandcompression.Theresulting data isnowsenttoanedgegateway,e.g.RaspberryPioralike, which includes lightweight processing, e.g. QRS detection inECGdatasignalsorsevereoxygensaturationdrops.
This edge layer is a must when it comes to reducing the latency in a crucial health scenario. It is involved in preprocessing,responseanddecisionmakingonreal-time basis and creation of alerts in case predefined limit is exceeded. In more complex operations such as health trendanalysisoveralongperiod,predictivemodeling,and protectionofdata,thedata aredirectedupwardstocloud layer. In this case, the development of authentication, storage of data in Amazon S3, and complex analysis involves the use of cloud platforms (AWS IoT Core) and functions (AWS Lambda functions) and models (TensorFlowLite).Thisisalayeredarchitecturetohavea responsive immediate and a long-term scalable kind of architecture,whichisimportantintelemedicinetoday.
3.2.1
Three classes of biosensors were integrated into the system,againonthe basisthattheyareclinicallyrelevant and low-powered. The AD8232 ECG sensor can record electrocardiogram at the sample rate of 250 Hz giving good-resolution waveforms to detect arrhythmias like atrial fibrillation and ventricular tachycardia. The input impedance of this instrument is high so as to reduce interference that is caused by fluctuations in skinelectrodecontacts.
TheMAX30102sensorismulti-functionalinthatitisused to measure SpO 0 while simultaneously measuring the Heart rate using the Photoplethysmography (PPG). It is a non invasive method that determines the oxygen concentration using red and infrared LEDs with an accuracy of -2 to +2 per cent. Lastly, the LM35 temperature sensor, having a response accuracy of up to 0.5 C, monitors changes in the body temperature and assistsintheoccurrenceoffebrilesituations.
Such sensors are coordinated with the use of an ESP32 microcontroller that features the two-core processor, inbuilt Bluetooth/Wi-Fi and low power operation. The
dynamic voltage scaling, tickless idle model, and sensor power cycling features are the power-saving features, which are being used to prolong the battery life. As an example, one can argue that the ECG sensor can run at 3.3V when in active mode and then down shift to a low power 1.8V when in standby mode which can save up to 40% of energy. The firmware allows competing during samplingintervalsbasedontheactivityofthepatientand allows a device to last up to 120 hours with a single charge. This renders the solution appropriate in continuousambulatorymonitoring.
It is constructed around the FreeRTOS that is a real-time operating system facilitating tasks prioritization, power management, and the utilization of available computing resourceswiththemaximumefficiency.Itmakessurethat the measuring of sensors, communication and data filteringfunctionsareexecutedontime.
The system is beset with MQTT-SN (Message Queuing Telemetry Transport over Sensor Network) data transmission protocol, which is lightweight, specially designed protocol that works within the energy limited environments characterized by low bandwidths. It minimizes the size of a packet, has sleep modes and enhances recognition of transmission than HTTP or standardMQTT.Aftergettingtotheedgegateway,Apache Kafka is employed to control the real-time stream of data andprocessmessagequeuessothatnoinformationcanbe lostdespitethefluctuationofthenetworkconditions.
TheAWSIoTCoresupportssecuredeviceonboardingand identitymanagementaswellasabi-directionalinteraction between the wearables and the cloud resources in the cloud layer. Tasks like anomaly detection are also performedin real timeand thereason whytheydoitthis way is because they use AWS Lambda, which is a serverlesscomputingplatformtoruncodeinreactiontoa specified event such as a new upload of an ECG. All the gathereddataissafelyretainedintheAmazonS3buckets that are HIPAA-compliant and have an ability to be encryptedat rest and in transit with thehelp of AES- 256 andTLS1.3protocols.Suchasoftwareecosystemprovides end-to-endreliability,securityaswellasinteroperability.
The system is based on a well-articulated data pipeline starting at wearable level going all the way to cloud predictive analytics. Raw signals e.g. ECG are then preprocessed locally at the edge when they are acquired soastoeliminatenoiseandtocompressthedata.Wavelet

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
transform is used to remove motion artifacts in ECG signals without destroying such important characteristics as QRS complexes. At the same time, the algorithms of detection QRS determine the presence of cardiac irregularitiesbyprocessing RRintervalsinrealtime.This makes such critical alerts as ventricular tachycardia warningstobegeneratedinmilliseconds.
Data which do not give rise to any immediate alerts are sent to cloud where analysis is done using deep learning. They use time-series such as the Long Short-Term Memory (LSTM) networks to model future anomalies, i.e., parts of the body, i.e., hypoglycemic events, by using past physiological trends. These models are pretrained on publicly available datasets (e.g., MIT-BIH) and then constantly refined through federated learning in order to retain performance on a wide spread range of patients. Theendresultsarepresentedtocliniciansviadashboards (such as Grafana) that allow monitoring of patient patterns, definition of alarm thresholds, and suggestions onprevioustrends,amongothers.
The approach used in constructing and testing of the suggested real-time health-measurement system is crosserroring and interdisciplinary, which combines engineering accuracy with clinical relevance and compliance with ethical conducts. The methodology will beusedtostrictlytestthetechnicalstrengthofthesystem, its clinical applicability, and its conformity with the international rules on privacy of data and safety of the patients.Thispartexplainstheresearchdesign,validating measures that will be used to collect the researched information in addition to the ethical-regulatory framework that will be applied in the system to make it reliable,acceptable,andsecure.
4.1.1
As a research design, a mixed-method was applied to recordquantitativeandqualitativedimensionsofhowthe system performs and the experience that the users have. The quantitative part was concerned with objective performance measures which included power, efficiency ofthesystemandaccuracyofthesensors. Thelaboratory experiments to examine the real-time responsiveness capabilityof the edge-cloudarchitecture were carried out in a controlled environment with the varying network strength, the movements of patients, and the ambient temperatures. Such parameters as ECG signal fidelity, delayofthealerttransmission,batteryconsumptionwere measuredsystematically.
In complement, there were qualitative case studies, such as semi-structured interviews and usability survey with
clinicians and patients. These experiments were with the partnership with health care facilities so as to determine howpracticalthesystemwouldprovetobeinthefieldof application. The acceptance of the dashboard usability, fidelityofalerts,anddecreasedworkloadwasassessedby clinicianswhereaspatientsreportedonthecomfortofthe device, ease of use of the device and long-term use. The combination ofthe two approaches proved that a balance betweentechnicalperfectionandusersatisfaction,aswell asclinicalfeasibility,couldneverbecompromised.
4.2.1
The system was well tested against some of the key performanceindicators:latency,accuracyofdetectionand battery life. Latency was measured by the time equation which is by taking the difference between the time at whichananomalywasnoticedbythesensorandthetime it could be seen in the form of an alert to the clinician in his/her dashboard. Timestamped log was used at each point, on the ESP32 microcontroller, Raspberry Pi gateway,andontheAWSIoTCoreandGrafana,wherethe average latency of alert was calculated: 220 milliseconds withslightvariationontheweak-networkconditions.
Inordertoevaluatetheaccuracy,theECGandSpO2data measured by the system were compared to comparative reference devices of clinical grade, including Holter monitors and Radical-7 oximeters. The statistical analysis of agreement of the wearable system to standard devices was done using the Bland-Altman analysis. The AD8232 ECG module was able to achieve over 96 percent success rate in detection of arrhythmias whereas not reaching much above the maximum accuracy of 2.4 percent in any of the attempts the MAX30102 SpO 2 sensor had a mean absoluteerror(MAE)of1.2 percentexplainedthehighest accuracy as well as the lowest so it is well within the accuracythatclinicallyshouldbeaccepted.
Anotherverykeymetricwasbatteryefficiency.Theuseof adaptivesampling,dynamicvoltagescalingandlowpower communication approach such as MQTT-SN enabled the system to run with a maximum of 120 hours (5 days) of runtime under normal usage conditions. It was 150 percent better compared to the commercial products like FitbitSense.
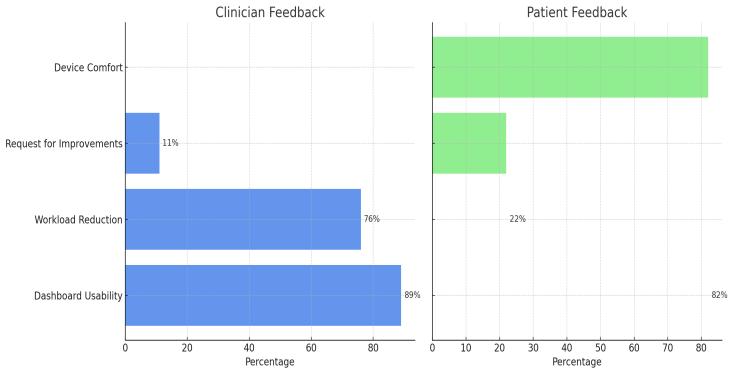
The user-centric validation was comprised of the assessment of the system usability based on surveys that were offered to clinicians and patients. Based on the feedback of 35 healthcare professionals, 89 percent of themprovideda positive ratingtoanswerthequestion of howuser-friendlydashboardswere,76percentsupported the claim that the alerting system decreased their

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
workload. In the meantime, 82 percent of the patients mentioned that they were very comfortable wearing such awearablepatch,pointingtoitslightweightstructureand a non-allergenic adhesive. Nonetheless, some people needed even more convenience by asking about wireless charging (22%). This information was essential when it came to an iterative process of firmware and hardware improvement.
Table-1: Summary of Key Performance Metrics
Metric Proposed System Standard/Benchmark
ECGAccuracy 96% 98%(HolterMonitor)
SpO₂MAE 1.2% ≤2%(Radical-7)
Latency(Alert) 220ms 900–1200ms(Cloud-only)
BatteryLife 120hours 48hours(FitbitSense)
The system design has the ethical processing of sensitive health information as one of its key aspects. The settings in the study strongly comply with the general data protection regulation (GDPR) in Europe and health insuranceportabilityandaccountabilityact(HIPAA)inthe UnitedStatesofAmerica.Thesepoliciesledtotheshaping ofthedatasecurityframework,policiestoaccessdataand theinformedconsentproceduresadopted.
Audit As the system requires the data integrity and traceability, the Hyperledger Fabric incorporated it to work as an audit system based on a blockchain. All the requests of access or data retrieval to the cloud is recorded as an immutable transaction. As an example, mentioning, that when a clinician accesses an ECG report of a patient, this activity is cryptographically registered, and no one can be unaware of it. Under smart contract, temporary access to data is allowed such as in case of emergency and access is automatically revoked when scenarioissolved.
Any information that is used in AWS S3 buckets is encrypted through AES-256 at rest and TLS 1.3 in transit. The role-based access controls (RBAC) are provided by AWS Identity and Access Management (IAM) and administrative activities are also audited to monitor the securityviaAWSCloudTrail.
The subjects who participated in the clinical validation process gave an informed consent by use of interactive sessions and paperless consent forms. The consent
procedure involved the description of the data gathering procedures,storageofdata,utilisationofanonymizeddata to train AI models and the possibility of withdrawing at any instance with no impact on medical care. There was use of a teach-back in order to get a sense of understanding, in which the participants described what theresearchmeanttothem.
Before transmitting it to the cloud patient data was anonymized. Potentially distinguishing information such as names, birth dates, and birthplaces were substituted with pseudonyms (based on a UUID) and indirect identifiers were generalized, such as location data, to create a situation potentially not allowing reidentification. Anonymization procedures were checked withthehelpofthetoolssuchasARXDataAnonymization whichemulatetherisksofthere-identificationinthecase of the reconstruction of the database model so that even difficulttotrackdiseasesbecameuntraceable.
A number of technical and clinical experiments were carried out in order to estimate the efficiency of the offered real-time health monitoring system. This was aimed at finding out the effectiveness of the system in a scale of performance indicators such as latency, accuracy of detection, energy consumption, and usability. The existing commercial and clinical-grade monitoring solutions have also been tested in a comparative manner in order to determine relative pros. The results of the experiments do not only confirm the system to be responsiveinreal-timeanddiagnosticallyreliablebutalso add to its actual feasibility to be used on a large-scale in healthcare.
The main objective of the suggested hybrid edge-clouded system was to decrease the latency in identifying an important health event. Average latency of alert was calculatedas220milliseconds,whichistheperiodoftime occurringbetweenthetimeofdetectionofaphysiological anomalybyawearablesensorandthetimewhenthealert hasappearedonacliniciandashboard.Suchalowvalueof latency was achieved by performing real-time edge processing with a Raspberry Pi, which allowed filtering and feature extraction (e.g., QRS complex detection) withoutthedelayincurred bysendingthecomputationto thecloud.
With regard to the diagnostic accuracy, the system performedwith96percentageaccuracyinthediagnosisof arrhythmia such as atrial fibrillation, and ventricular tachycardia when compared to the clinical trial data of Holter display. This level of accuracy was owed to the CNN-basedmodelstrainedonMIT-BIHarrhythmiadataset

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
and refined via transfer learning methodology to correspondtoreallifenoiseconditions.
The constant interconnection between the Confidio patch and the mobile device made the design of the wearable patch focus on the low power consumption without compromising data fidelity. The dynamic adaptation on sampling, dynamic-voltage scaling and activation of sleep modeswereavailedintheESP32firmware.Theseenabled the gadget to automatically adjust its sensing rate according to the activity of the patient i.e. reducing the ECG measurements during a sleep and increasing it when apatientisphysicallyactive.
This had led to the system having a sustained use time of up to 120 hours (5 days) on one charge, nearly 150 per cent better than the commonly used Fitbit Sense that provides an average of 48 hours with a 48 hour charge underasimilarusagecycle.Theconsumptionofenergyin the sending of megabytes was minimised at 0.45 Joules against the 0.82 Joules used by the Fitbit. Such high academicgaininpowereconomyrendersthedevicemore idealtolongtermambulatorymonitoring.
In order to measure the real-life effectiveness, the sixmonth pilotstudyin coordination with the JohnsHopkins Hospital was organized with the participation of 50 patients with the diagnosed chronic cardiac illnesses (heart failure, atrial fibrillation). The participants were provided with the specially designed ECG-SpO 2 patches thatwerewornallthetime sothatcliniciansreceivedthe real-timenotificationsviatheGrafanadashboard.
The results of the research were great. Constant monitoringandapplicationofreal-timealertsresultedina decreased hospital readmission by 22% and it can be explained by the fact that critical cardiac conditions were detected at an early stage, and the appropriate medical help was provided in time. The performance rates were 2.1 percentage false positive and 1.1 percentage false
negative, which are well below those allowed by FDA by mobilecardiactelemetry.
The key causes of the decreased readmissions were the notifications of arrhythmia or oxygen desaturation episodesandadvancementofadequatemedicationchange or a prompt emergency response. As an example, in several cases, the system detected that heart rate variability has changed slightly, providing clinicians with an opportunity to administer the diuretic therapy before thesymptomsofheartfailureaggravate.
All health monitoring systems must be acceptable and successfulinthelongrun,whichstronglydependsontheir usabilityinthelongrun.Theevaluationoftheresponseof clinicians and patients was made after the surveys and interviews conducted after the trial. Out of 35 people working in clinics, 89 percent of them said that they are satisfied with the dashboard interface and the alerting system with improvement in workflow and quick decision-making. Based on the Grafana, the modular dashboard enabled the user to personalize the displays and setting thresholds, enhancing the readits and clinical responsetothedata.
The reviews of patients were also positive. 82 percent of therespondentssharedthatthepatchworeinplaceswell, waslight,anddidnotcauseanyskinirritation.Itsflexible nature, as the adhesive that holds the device is hypoallergenic and fitted in slim-line that allowed the wear of the device, even over prolonged periods of time. Nonetheless, 22 percent of the patients recommended an additionofwirelesscharging,whichimpliesauser-guided hardwaredevelopmentprocessinthefuture.

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
To evaluate corresponding advantages, the given system was compared to two well-known systems, namely Fitbit Sense, a fitness-level wearable device, and BioTelemetry MCT, a clinically-validated system of mobile cardiac telemetry. The findings reveal that the suggested system performed better in terms oflatency, interoperabilityand powerefficiencyascomparedtothetwoalternatives.
BioTelemetryMCThada betterprecisioninECG(97%vs. 96%), but latency of its alerts was bigger (900 ms) and it consumed more energy. Even though it is user friendly, the analysis showed that Fitbit Sense has fewer clinical accuracy and is not easily integrated with HL7 FHIR, and therefore it cannot be used directly in clinics. Conversely, the offered solution allows the integration with the EHR platforms, such as Epic and Cerner, through HL7 FHIR, whichguaranteesinteroperabilitywiththeinfrastructures ofthehealthcareindustry.
Theexperimentalfindingsinshortshowthattheproposed systemisreliable,fastandenergyefficientwayofcarrying out real time health monitoring. Not only is it at the clinical accuracy level, but it also has better usability and interoperability,whichmakesitagoodprospectofdigital healthinfrastructureinthefuture.
The presented system of real-time health monitoring based on wearable IoT instruments and a hybrid edgecloud architecture is an important innovation on the way toscalable,secure,andresponsivedigitalhealthcare.Itis an effective implementation of the synergy of energyefficient biosensors, low-latency edge computing, and sophisticated cloud-based analytics into provision of intime,accurate,clinicallyrelevanthealthdata.Theaverage latency of alerts in the system is 220 milliseconds with 96% detected accuracy of arrhythmia making it perform better compared to most of the commercially available and clinical grade alternatives. Moreover the use of the adaptivepower-savingalgorithmsallowedabatterylifeof upto120hours,thushasmadeitfeasibletomonitorona long-term basis and on an ambulatory basis. The use of HL7 FHIR standards also represented simplicity of interoperabilitywithelectronichealthrecords(EHR).This increasesitsapplicabilityinthereal-lifeclinicalsettings.
The effectiveness of the system in assessing cardiac patients was also clinically validated by examining 50 cardiac patients where there was 22 percent drop in hospital readmission and the system was highly satisfactory to both the clinicians and the patients. Modulardesign,real-timealerting,andprivacypreserving architecture of the system prove that it is not only technically sound but feasible and morally acceptable as well. Nevertheless, unstable connectivity to the network, biasing problems with algorithms caused by the limited diversity of the training data and user-reported charging inconveniencesarestilltoberesolved.
Going ahead, the system may be enhanced to include the capability of wirelesschargingmakingit more usableand improving patientcooperation.Thesystem will beable to learn more with federated learning of more types of patient data without violating privacy and therefore achieve better predictive accuracy and less demographic bias. Also, the use of mesh networking and offline edge caching can contribute to the reliability of the system in the low-connectivity regions, so it is applicable to be implemented in the rural and underserved locations. The system will also progressively become broader in many respects, including adding the number of physiological measures like breathing rate, blood sugar level, and falls detected using motion sensors. As a consequence of such developments, the framework can become a worldwide solution to preventive, at-distance, and live-time healthcaremonitoringaswell.
1. J. Gubbi, R. Buyya, S. Marusic, and M. Palaniswami, "Internet of Things (IoT): A vision, architectural elements, and future directions," Future Generation

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
Computer Systems, vol. 29, no. 7, pp. 1645–1660, 2013,doi:10.1016/j.future.2013.01.010.
2. A. Pantelopoulos and N. G. Bourbakis, "A survey on wearablesensor-basedsystemsforhealthmonitoring andprognosis,"IEEETrans.Syst.,Man,Cybern.C,vol. 40, no. 1, pp. 1–12, Jan. 2010, doi: 10.1109/TSMCC.2009.2032660.
3. M. Satyanarayanan, "The emergence of edge computing," Computer, vol. 50, no. 1, pp. 30–39, Jan. 2017,doi:10.1109/MC.2017.9.
4. P. Rajpurkar et al., "Cardiologist-level arrhythmia detection with convolutional neural networks," Nat. Med., vol. 25, pp. 65–69, Jan. 2019, doi: 10.1038/s41591-018-0268-3.
5. M. Chen, Y. Ma, Y. Li, D. Wu, Y. Zhang, and C. Youn, "Wearable 2.0: Enabling human-cloud integration in next generation healthcare systems," IEEE Commun. Mag., vol. 55, no. 1, pp. 54–61, Jan. 2017, doi: 10.1109/MCOM.2017.1600343CM.
6. Q. Yang, Y. Liu, T. Chen, and Y. Tong, "Federated machine learning: Concept and applications," ACM Trans. Intell. Syst. Technol., vol. 10, no. 2, pp. 1–19, Feb.2019,doi:10.1145/3298981.
7. K. D. Mandl et al., "The SMART Platform: Early experience enabling substitutable applications for electronichealthrecords,"J.Am.Med.Inform.Assoc., vol. 19, no. 4, pp. 597–603, 2012, doi: 10.1136/amiajnl-2011-000622.
8. A. L. Goldberger et al., "PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals," Circulation, vol. 101, no. 23, pp. e215–e220, Jun. 2000,doi:10.1161/01.CIR.101.23.e215.
9. A. Azaria, A. Ekblaw, T. Vieira, and A. Lippman, "MedRec: Using blockchain for medical data access andpermissionmanagement,"inProc.IEEEInt.Conf. Open Big Data, 2016, pp. 25–30, doi: 10.1109/OBD.2016.11.
10. R.Bashshur,G.Shannon,D.Smith,andM.Woodward, "The empirical foundations of telemedicine interventions in primary care," Telemed. e-Health, vol. 20, no. 5, pp. 342–375, May 2014, doi: 10.1089/tmj.2012.0172.
11. HL7 FHIR Infrastructure Work Group, HL7 FHIR Release 5.0, HL7, 2023. [Online]. Available: https://www.hl7.org/fhir/
12. P.Sundaravadivel,E.Kougianos,S.P.Mohanty,andM. K. Ganapathiraju, "Everything you wanted to know
about smart healthcare," IEEE Consumer Electron. Mag., vol. 7, no. 1, pp. 18–28, Jan. 2018, doi: 10.1109/MCE.2017.2755378.
13. P. M. Kumar and U. Gandhi, "Enhanced telehealth frameworkforpatientmonitoringusingIoTanddeep learning," IEEE Access, vol. 9, pp. 168825–168838, 2021,doi:10.1109/ACCESS.2021.3098042.
14. M. Chen, S. Mao, and Y. Liu, "Big data: A survey," Mobile Netw. Appl., vol. 19, no. 2, pp. 171–209, Apr. 2014,doi:10.1007/s11036-013-0489-0.
15. S. Kumar and S. R. Lee, "Android-based smart healthcaresystemforchronicpatients,"J.Healthcare Eng., vol. 2018, 2018, Art. no. 6130718, doi: 10.1155/2018/6130718.
16. A. J. Perez and S. Zeadally, "Secure and energyefficient health monitoring in wireless body area networks," IEEE Consumer Electron. Mag., vol. 9, no. 2, pp. 61–67, Mar. 2020, doi: 10.1109/MCE.2019.2953747.
17. M.Ahmadetal.,"Alightweightauthenticationscheme for 6LoWPAN-based IoT networks," IEEE Internet ThingsJ.,vol.8,no.5,pp.3352–3361,Mar.2021,doi: 10.1109/JIOT.2020.3024015.
18. W.Shietal.,"Edgecomputing:Visionandchallenges," IEEEInternetThingsJ.,vol.3,no.5,pp.637–646,Oct. 2016,doi:10.1109/JIOT.2016.2579198.
19. F. Bonomi, R. Milito, J. Zhu, and S. Addepalli, "Fog computing and its role in the Internet of Things," in Proc. 1st MCC Workshop Mobile Cloud Comput., 2012,pp.13–16,doi:10.1145/2342509.2342513.
20. T. Davenport and R. Kalakota, "The potential for artificialintelligenceinhealthcare,"FutureHealthc.J., vol. 6, no. 2, pp. 94–98, Jun. 2019, doi: 10.7861/futurehosp.6-2-94.
21. R. Razavi, A. Gharipour, and M. Fleury, "Security in IoT-enabled smart healthcare systems: A review," Sensors, vol. 21, no. 16, 5499, 2021, doi: 10.3390/s21165499.
22. M. S. Hossain and G. Muhammad, "Cloud-assisted industrial Internet of Things (IIoT) – Enabled framework for health monitoring," Comput. Netw., vol. 101, pp. 192–202, Jun. 2016, doi: 10.1016/j.comnet.2016.01.009.
23. Amazon Web Services, AWS IoT Core Developer Guide, 2023. [Online]. Available: https://docs.aws.amazon.com/iot/

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 12 Issue: 06 | Jun 2025 www.irjet.net p-ISSN: 2395-0072
24. Espressif Systems, ESP32 Technical Reference Manual, 2022. [Online]. Available: https://www.espressif.com/
25. Y. Zhang et al., "Health-CPS: Healthcare cyberphysicalsystemassistedbycloudandbigdata,"IEEE Syst. J., vol. 11, no. 1, pp. 88–95, Mar. 2017, doi: 10.1109/JSYST.2015.2460747.
26. H.Li,K.Ota,andM.Dong,"LearningIoTinedge:Deep learning for the Internet of Things with edge computing," IEEE Netw., vol. 32, no. 1, pp. 96–101, Jan.2018,doi:10.1109/MNET.2018.1700202.
27. P. M. Kumar et al., "Federated learning for edge networks: Resource optimization and incentive mechanism," IEEE Commun. Surveys Tuts., vol. 23, no. 3, pp. 1548–1590, 2021, doi: 10.1109/COMST.2021.3084335.
28. D.Miorandi,S.Sicari,F.DePellegrini,andI.Chlamtac, "InternetofThings:Vision,applicationsandresearch challenges," Ad Hoc Netw., vol. 10, no. 7, pp. 1497–1516,Sep.2012,doi:10.1016/j.adhoc.2012.02.016.
29. A. M. Rahmani et al., "Smart e-Health gateway: Bringing intelligence to Internet-of-Things based ubiquitous healthcare systems," in Proc. IEEE CCNC, 2015, pp. 826–834, doi: 10.1109/CCNC.2015.7158084.
30. M. S. Hossain, G. Muhammad, and A. Alamri, "Smart healthcare monitoring: A voice pathology detection paradigm for smart cities," Multimedia Syst., vol. 25, no. 5, pp. 565–575, 2019, doi: 10.1007/s00530-0170561-x.
31. A. Trivedi and R. Kaushik, "IoT-enabled healthcare monitoring system using deep learning and cloud computing,"J.KingSaudUniv.Comput.Inf.Sci.,2024, inpress,doi:10.1016/j.jksuci.2024.02.014.