

NEW ACTION ON PLACEMENT POVERTY
Optometry students having to make choices between food and other expenses


NEW ACTION ON PLACEMENT POVERTY
Optometry students having to make choices between food and other expenses
At Specsavers, partnership means more than just running a store — it’s about shaping a business, leading a team, and making a real impact in your community. With the right support, structure, and shared purpose, you’re empowered to grow something that’s truly yours. Because when you lead with passion, success follows.
Find out more about a Specsavers partnership today at www.spectrum-anz.com /partnership


Ms Jessie Woodward started her fourth year as an optometry study at UNSW with nothing in the bank.
In order to do the numerous mandatory clinical placements in that year, optometry students must buy their own clinical equipment, which costs around $7000. To do that, Woodward used all of her savings. She then had to make choices around food and other necessities to fund her regional placement, a flight to Coffs Harbour, a 50km daily commute by car and extra petrol costs.
All without pay and financial support for those placements.
“It’s essentially full-time work,” she said speaking to Optometry Australia (OA), “Monday to Friday, 9 to 5, often with long commute times.
"There’s no room to take on other paid work unless you give up your
weekends or your wellbeing.”
Woodward’s is just one of many stories spurring new calls for an immediate expansion of the Commonwealth Prac Payment (CPP) and the inclusion of all allied health professions in the program, including training optometrists.
The allied health sector, supported by Optometry Australia (OA) and the UNSW School of Optometry and Vision Science, has urged Education Minister Mr Jason Clare and the Federal Government to make that happen.
The CPP, announced in the 2024–25 Federal Budget, started on 1 July this year for nursing, midwifery, teaching and social work students.
The payment of $331.65 per week for eligible students on placement recognises the significant unpaid workload of clinical placements and

the gap between theoretical knowledge and practical skills is through placements.
Image: Med Studio/shutterstock.com
the disproportionate impact that can have on many students.
But according to the Allied Health Professions Australia (AHPA), the program excludes most allied health disciplines, including optometry, leaving students to take on mandatory placements – often lengthy and in rural or remote locations – without financial support.
AHPA, of which OA is a member,
Australia generated £863.3 million for the global Specsavers business in 2024-25 – an increase of 8.1% year-on-year before foreign exchange rate adjustments – and is contributing 20% of the group’s annual revenue as its second largest market.
In the year to February 2025, revenue across all 10 countries Specsavers operates in reached £4.18 billion, growing 7.5% year-on-year.
Now with 395 optical stores and 321 locations offering audiology, Australia continues to be a key market for the group 17 years after its arrival. The UK, where the Guernsey-based company was founded in 1984, remains its largest contributor with £2.32 billion in 2025-25.
Revenue in New Zealand reached £104.1 million, generated from 61 optical practices and 49 audiology locations.
“I am incredibly proud of our scorecard. But this isn’t a sporting tournament. There’s no finish line, no final round, no match point,” CEO and chief sustainability officer Mr John Perkins said.
“Our purpose to ‘change lives through better sight and hearing’ isn’t measured by a scoreboard, and it’s not assessed by comparison to our competitors.
"Instead, our cause is an unrelenting, unending crusade to continually improve what and how we do things. It’s the pursuit of a goal that’s always just out of reach.”
One of the biggest achievements from the ANZ business was the launch
of seven new stores across the region, providing 10,000 additional sight tests throughout the year. Plus, there were more than 160 refits ensuring Specsavers locations had the latest visual technology, including digital screens and illuminated frame displays.
The company also marked the 60-millionth customer order from Melbourne Glazing Services, based out of its Port Melbourne support office, 15 years after it was established.
“Our Australia and New Zealand stores have been busier than ever,” the company said. “Improved customer communications, through multi-channel recall, new recall intervals, and an enhanced
8
said that allied health students completed between 500 and 1,000 hours of mandatory unpaid placements, with some courses and professions requiring up to 56 weeks of unpaid placement hours.
Evidence showed that financial barriers during those placements “impact completion rates, decisions about which placements to undertake, and ability to focus on learning”.
AHPA chair Ms Samantha Hunter said: “The decision to limit Commonwealth Prac Payments to a narrow set of disciplines fails to reflect the significant workforce shortages in many allied health professions, their vital role in Australia’s health, mental health, disability, education, and aged care systems, or the high volume

Partridge has been prescribing ACUVUE Abiliti 1-Day for more than 18 months – a head start over her Australian counterparts who have only recently gained access to the latest soft contact lens for myopia control.
Know when to take a closer look
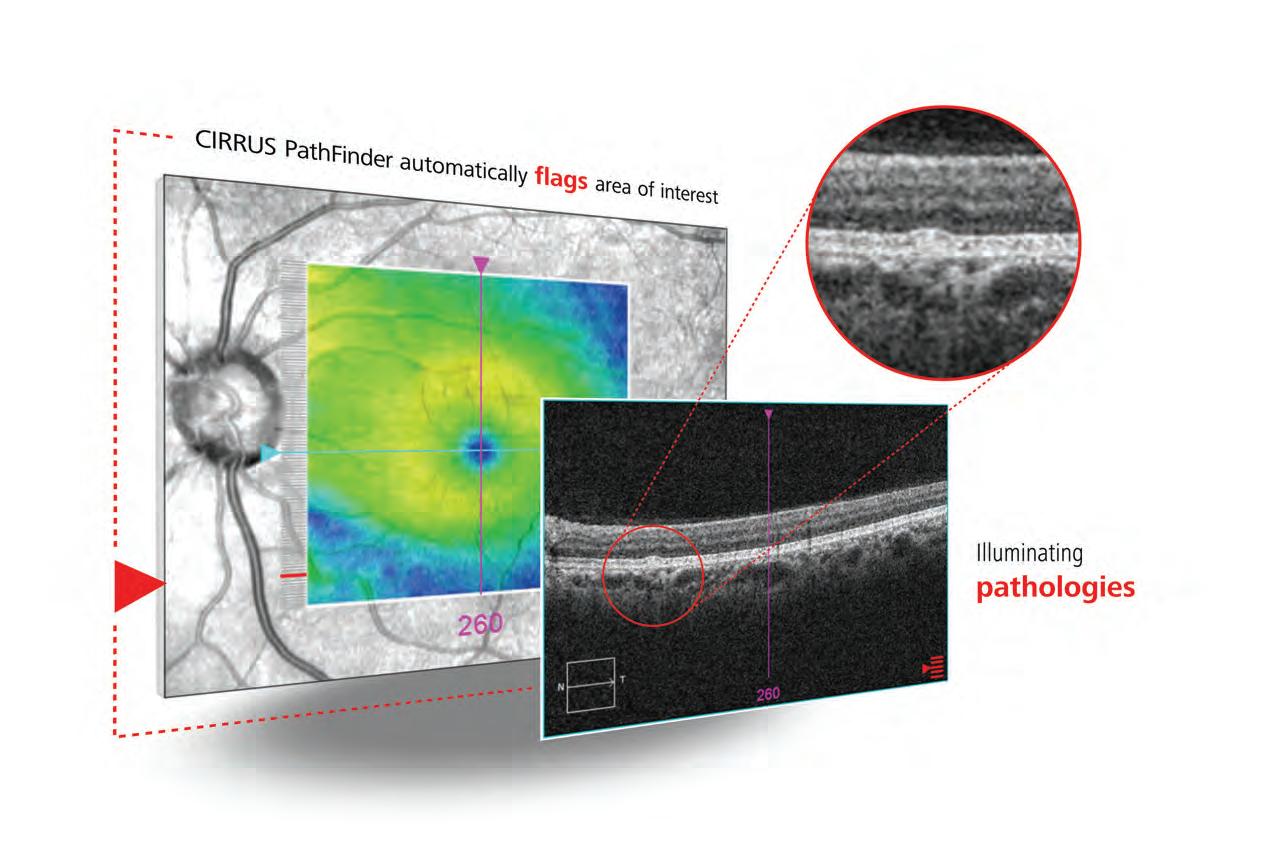
CIRRUS ® PathFinder™ from ZEISS is an innovative clinical support tool that enables more confident decision-making and accelerates your workflow with OCT interpretation assistance. ZEISS CIRRUS PathFinder* uses proprietary deep learning algorithms to automatically identify abnormal macular OCT B-scans that can aid in early disease detection and encourage further evaluation.
*PathFinder is available on ZEISS CIRRUS 500/5000/6000 devices
ZEISS
AU: 1300 365 470
NZ: 0800 334 353 med.au@zeiss.com
For information about ZEISS CIRRUS 6000, visit www.zeiss.com/cirrus6000
13 Root causes
The ASO has a number of concerns about the Grattan report into ophthalmology.

The ODMAFair25 tick Eyes Right Optical came away with a number of awards from the industry event.

30 Smart choice
HOYA reveals eight years’ worth of data on its MiYOSMART lenses.
When compiling the first myopia report of 2025 Insight’s April edition, one thing stood out for its absurdity: some schools in China are installing high-intensity lighting to mimic sunlight.

It’s an impressive technical solution that has produced small but significant reductions in new myopia. But it’s equally disturbing. Have we really designed childhood so tightly around indoor life that we now need to engineer daylight into classrooms?
It’s an indictment on how far lifestyles have drifted from the simple act of sending kids outside to play – an act that comes with many benefits, including a first-line of defence against myopia.
As a myopic father to two children under three, this topic feels deeply personal. Every day, I catch myself doing mental arithmetic: Have they been outside enough? Did I reach for the screen too quickly today? Like many parents, I’m navigating trade-offs between convenience and what’s best for their health.

How Vision Australia is making a big difference in the lives of its clients and the country.
That’s why this edition’s special report resonated with me (page 26). We asked Australian optometrists to step out from behind the slit lamp and share how they combat myopia in their most prized patients – their own children.
Mr Jason Teh, for example, made outdoor time a daily non-negotiable, breaking a generational cycle of myopia in his family. Others, like Dr Susan Ang, intervened early with Stellest plano lenses when the hyperopic reserve of her son’s eyes began to erode. I always love hearing from people who have skin in the game.
Of course, not every child will dodge myopia, but as our experts remind us, the high-tech treatments we now have are often the second step.
The first? It’s still outside, digging up worms, kicking a ball. It’s simple advice that sometimes requires no-nonsense, straight talking, as optometrist Mr David Neilson does in his Toowoomba practice (page 34).
As myopia management becomes mainstream, shifting families beyond “just glasses” to altered behaviours and early intervention is changing futures. Your role in guiding parents like me has never been more crucial.
MYLES HUME Editor

Just as Insight went to print, ALCON announced an agreement to acquire STAAR Surgical Company, the manufacturer of the implantable collamer lens (ICL). The AU$2.3 billion acquisition would include the EVO family of lenses for vision correction for patients with moderate to high myopia, with or without astigmatism. IN OTHER NEWS, Specsavers is turbocharging its presence in Canada by opening 111 new locations inside selected Loblaw-owned grocery stores across
Neuro and materials scientists have developed infrared contact lenses that allow people to see in the dark, even with their eyes closed. The lens enables wearers to perceive multiple infrared wavelengths. Because they’re transparent, users can see both infrared and visible light simultaneously, though infrared vision was enhanced when participants had their eyes closed. “Our research opens up the potential for non-invasive wearable devices to give people super-vision,” the authors reported in Cell
A new Centre for Eye Research Australia (CERA) study has looked at the genes associated with different types of cataracts in a first step towards new, targeted therapies. The researchers collected tiny samples of lens cells from 89 patients undergoing routine cataract surgery at several Melbourne hospitals, which were sent for sequencing. It was the first project that directly compared gene activity across the four types of cataracts in humans.
the country. The optometry provider – which entered Canada in 2021 – will offer eyecare in Loblaws, Real Canadian Superstore and Zehrs stores, marking the phase-out of Loblaw’s existing optical banner, Theodore & Pringle. Loblaw is Canada's food and pharmacy leader, and the nation's largest retailer. There are now more than 2,700 Specsavers healthcare businesses globally. FINALLY, macular disease patients in Europe may only need to have up to two anti-VEGF injections per year after a label extension was granted in the European Union (EU) for Eylea 8 mg (aflibercept 8 mg) for
those with neovascular age-related macular degeneration (nAMD) and diabetic macular edema (DME). The drug is now the only treatment of its kind in the bloc with treatment intervals of up to six months for the two diseases. The higher dose of aflibercept was approved in Australia and added to the Pharmaceutical Benefits Scheme from 1 October 2024. Currently in Australia, the recommended dosing schedule involves three initial monthly injections for both nAMD and DME, followed by extended dosing intervals of eight to 16 weeks based on visual and or anatomic outcomes.

The number of ophthalmologists in Australia has increased by 19% during the past decade. Page 12
THIS MONTH
A bizarre case report from July 2025 describes a patient presenting with an unusual symptom – unilateral Roth spots (retinal hemorrhages with a white centre) – that was ultimately linked to a benign uterine tumour. This head-scratcher case shows how “Roth spots can be a sign for serious underlying systemic conditions and can be reversible if the underlying cause is diagnosed and treated early”, the authors noted.
SCC 2025
13 – 14 September
Also open to non-Specsavers optometrists, the event is returning in-person, with a hybrid format live in Melbourne and streamed across ANZ. specsaversclinicalconference.com.au
Complete calendar page 64
NEXT MONTH
OSO 2025
10 – 12 October
The Orthokeratology Society of Oceania event is taking place at RACV Royal Pines in Queensland, with speakers including Dr Noel Brennan and A/Prof Daddi Fadel. oso.net.au
Published by:
379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766
www.primecreative.com.au
Chief Executive Officer
Christine Clancy christine.clancy@primecreative.com.au
Publisher
Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Assitant Editor
Rob Mitchell
rob.mitchell@primecreative.com.au
Commissioning Editor, Healthcare Education
Jeff Megahan
Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Karyssa Arendt karyssa.arendt@primecreative.com.au
Head of Design
Blake Storey
Art Director
Bea Barthelson
Subscriptions T: 03 9690 8766
subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright –No part of this publication can be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
continued from page 3
of placement hours required to complete the training.
“Every part of the health workforce is critical, and every student should be supported to complete their education without facing financial crisis.”
AHPA said many allied health students reported significant hardship while on placement, including loss of income, housing insecurity, food insecurity, and increased mental distress – a growing problem dubbed “placement poverty”.
These challenges disproportionately affected students from low-income, regional, or diverse backgrounds, said the AHPA, threatening Australia’s diversity and the ability to build a future health workforce.
“As a sector, we are working closely with governments, universities, clinical educators, and placement providers to identify barriers and issues underpinning current workforce shortages across health, aged care, disability, and mental health,” said Hunter.
“There is clear evidence that students are dropping out, deferring or swapping to part-time study because they can’t afford to complete unpaid placement requirements. If the federal government is serious about addressing ongoing workforce shortages in the allied health sector, this is a policy blind spot that must be addressed.”
OA agreed.
CEO Ms Skye Cappuccio, also the AHPA deputy chair, said Woodward and other optometry students had shared experiences of “food stress, mental exhaustion and housing instability while on placement”.
“These are not isolated cases and they reflect a systemic problem – the lack of support is impacting optometry student wellbeing,” she said.
“Optometry students undertake extensive, full-time unpaid placements, often away from home and over long periods, and experience significant financial pressure as a result.”

She said placements, including those to regional, rural and remote areas, were crucial to developing a strong, well-distributed eyecare workforce for the future, but placement poverty had to be tackled.
“Optometry Australia believes extending the support offered by the CPP to optometry students will help ease placement-related financial pressures.”
As well as supporting the co-ordinated campaign to Canberra, OA was “participating in broader allied health advocacy efforts, contributing to cross-sector submissions and engaging directly with government decision-makers”, said Cappuccio.
“Through our Student Advocacy Placement program, we are also helping build future leaders who understand how policy and advocacy intersect to impact issues relevant to the profession, including funding and workforce design.”
“THE
DECISION TO LIMIT COMMONWEALTH PRAC PAYMENTS TO A NARROW SET OF DISCIPLINES FAILS TO REFLECT THE SIGNIFICANT WORKFORCE SHORTAGES IN MANY ALLIED HEALTH PROFESSIONS.”
Professor Lisa Keay, head of the UNSW School of Optometry and Vision Science, said a 2023 survey of the school’s students had confirmed that financial hardship was common, affecting more than half of its students.
She said the industry was supportive, often providing a student discount for equipment purchases.
“Further, there is often support and hospitality from our clinical placement hosts, particularly those in rural areas, which is much appreciated.”
Also, the school had received educational grants from Alcon and some donations from Young Optometrists, topped up by UNSW funds.
“However, these measures are limited and not sustainable,” she said. “Government support is a preferred, longer-term solution.”
The school said its own workforce projections indicated that optometry was not currently experiencing a shortage, but extending the support to optometry students would help ease those placement-related financial pressures.
Beyond widening the scope of the CPP, that support could include reducing the cost of public transport for students struggling with lengthy commutes to campus and clinical placements.
Like Cappuccio and others, Prof Keay had brought the issue to the attention of Clare’s office and provided data to support their advocacy work.
booking system, made it even easier for our customers to interact with us.”
Specsavers also shed more light on its plan to roll out new services for dry eye disease in Australia. It has piloted low-level-light treatment and intense pulsed light treatment, with its optometrists reporting “great professional satisfaction in being able to provide effective and long-term solutions”.
“The technology will become available across our Australia and New Zealand clinics to support even more patients,” the report stated.
In other updates, Specsavers was ranked the sixth Best Workplace in Australia, rising from its previous position at number eight, and it has strengthened its partnerships with universities across Australia and New Zealand.
“Nearly 500 clinical placements were hosted across our ANZ store network, and 52% of final-year students from our eight affiliated optometry schools chose Specsavers as their graduate employer,” the company said.
After launching its audiology business in Australia in 2017, 3.5 million people have now had their hearing screened, and a further 500,000 in New Zealand.
Last year, Specsavers celebrated its 300th Australian store to offer audiology, and the fifth anniversary of its first audiology offering in New Zealand.
“Australia continued its ongoing double-digit growth [in audiology], with orders up 16% year-on-year,” the company said. “Service measures in the region remain strong, with net promoter scores of customers fitted with hearing aids measuring at 88.01 in Australia

On the corporate responsibility front, Specsavers Australia and New Zealand donated AU$2.4 million to charities and good causes.
After 16 years of partnership with The Fred Hollows Foundation, it also surpassed AU$10 million in donations.
The Royal Victorian Eye and Ear Hospital (Eye and Ear) has become the first public hospital in the country to integrate iCare Oculo as part of its patient management system.
In a media release, Eye and Ear said it was breaking new ground to connect public patients to the benefits of Oculo’s e-referrals, including clinical images.
The e-referral system uses the VicKey platform that supports inter-service referrals across several public health services in Victoria.
As part of the partnership, iCare has updated Oculo’s interoperable, secure clinical communications platform to adhere to the Victorian State Referral Guidelines, including adding new functionalities for Aboriginal, non-English speaking and patients with disabilities.
“We are delighted that this initiative, the first public hospital integration with Oculo in Australia, enhances our commitment to inclusive and accessible care,” Mr Brendon Gardner, CEO at the Eye and Ear, said.
“iCare has further developed Oculo so that referrers can note if patients identify as Aboriginal and/or Torres Strait Islander and if patients have accessibility requirements. Connection to community-based optometrists and ophthalmologists is a critical part of our commitment to a patient-centred care.”
Ms Leanne Turner, executive director operations and chief nursing officer at the Eye and Ear added: “We have already had feedback from our triage team that the increased quality of diagnostic imaging from the Oculo’s platform e-referrals results in more accurate triage.
“In addition, fewer referrals are rejected due to incomplete clinical information needed for efficient and accurate decision-making, including poor quality imaging. Already in the first month, 74% of our referrals are coming through Oculo –516 referrals in total.”
Ms Kate Taylor, who co-founded Oculo with Professor Jonathan Crowston in 2015, said: “We built Oculo to support secure exchange of quality clinical

Using Oculo has already led to fewer referrals rejected due to incomplete clinical information. Image: iCare.
information to improve patient triage, access to care and collaborative care.
“Linking into our national networks of over 5,000 optometrists and ophthalmologists, the Eye and Ear is bringing the benefits of digitally connected eyecare to public patients. It’s an overdue step for greater equity in quality care for all Australians and improved care for indigenous Australians.
“Oculo is a standards-based platform with all the benefits of interoperability for patient care, notably better continuity of care and promoting collaborative care between optometry and ophthalmology.
“Oculo also provides the ability to connect patients into important support programs like KeepSight’s national diabetic eye disease register and patient support programmes by Glaucoma Australia and the Macular Disease Foundation Australia.”
Editor’s note: Insight would like to acknowledge Mr Peter Larsen as a founder of Oculo.
Improved for the Australian climate - performs in the heat, stays darker, reacts faster and available in the world’s thinnest 1.76 lens




RANZCO and Australia’s other specialist medical colleges will speak with one unified voice on healthcare policy under major governance reforms designed to accelerate responses to workforce shortages and access barriers. As the peak body for Australia’s specialist medical colleges, the Council of Presidents of Medical Colleges (CPMC) said the transformation comes at a critical time for Australian healthcare. “We are building a voice for specialist doctors, including GPs, that is responsive, accessible and can respond to challenges in real time. This unanimous decision shows we are united and ready to help shape urgent healthcare reform with a clear, strong voice,” said Associate Professor Sanjay Jeganathan, president of the council and chair of the board.
Eco-friendly eyewear brand Project Green has released two bold eyewear models ‘Ayla’ and ‘Alani’, expanding its sustainable collection with striking designs in time for the spring season. Both models are crafted from premium bio-acetate and packaged in fully biodegradable materials. Ayla is described as an “unapologetically bold frame with wide temples and a squared off finish, designed to make a statement from every angle”, supplier Eyes Right Optical said. It’s available in high-impact colours including forest green, purple fade, black and crystal blue. Alani offers a soft yet bold silhouette with a chunky oversized look that is complemented by wide temples. Available in hues like purple fade, black, crystal blue and a brown stripe, Alani “balances everyday wearability with a standout attitude”.
CR Labs has launched its complete Satin+ coatings suite, along with the release of a Satin+ catalogue to support independent practices with detailed product guidance and prescribing confidence. The Australian lens manufacturer said following the success of the Satin+ Premium AR coating introduced in 2024, it had expanded the range into a full coatings suite developed to meet the diverse visual demands of today’s patients. The newly launched Satin+ coatings include specialised options such as Satin+ Night for enhanced low-light performance and Satin+ Blue for digital comfort – all made and applied in Australia. Plus, CR Labs has released an updated Satin+ catalogue, featuring simplified coating comparisons, visual tools, and prescribing information to help practices easily integrate the Satin+ range into their dispensing. “Our vision for Satin+ was to create a truly local, premium coating offering that evolves with patient needs,” said Mr Todd Spencer, chief commercial officer at CR Labs. “This catalogue brings that vision to life by giving practices the clarity and tools they need to confidently recommend the best coating for every lifestyle.”

Angel Eyecare has won the grant to improve indigenous eye health. Image: Sawoon/stock.adobe. com
Melbourne-based optical wholesaler Good Optical Services has been sold to Mr Aaron McColl, founder of Aaron’s Eyewear.
Good Optical Services founders Mr Rick and Ms Marissa Good will remain actively involved during a 12-month transition period, before they enter retirement. The company is a popular supplier to optometrists, opticians, ophthalmologists, hospitals, and universities across Australia and New Zealand, offering therapeutic products and optical supplies.
Good Optical Services will now join Aaron’s Eyewear as companies of The McColl Group. McColl runs the business with wife Heidi and is widely respected for a customer-first ethos.
McColl describes the acquisition as “a meeting of kindred spirits”. He noted Rick and Marissa’s “unwavering” commitment to their customers, with a continued focus on service, trust, and supporting the evolving needs of Australia’s optical professionals.
“Rick and Marissa have built something truly exceptional,” McColl said. “And I’m both proud and excited to work alongside them over the next 12 months learning from the very best. I feel incredibly fortunate to have their guidance during this time.”
During the transition, Rick and Marissa

will work alongside McColl to share their extensive knowledge and relationships built over 43 years.
Good Optical Services was founded after Rick originally arrived in Australia from the US in April 1980 on an expert’s visa working for a leading American ophthalmic pharmaceutical company. Two years later he started Good Optical Services, commencing business operations in 1982.
“Good Optical Services has been our life’s work, it’s more than a business; it’s about the people we’ve helped and the community we’ve built along the way,” Rick said.
“Turning 70 this year is a good time for Marissa and I to do some extended travelling and I’m looking forward to reacquainting myself with my seven iron.”
A national initiative to deliver cutting-edge eyecare to remote indigenous communities using next-generation chip-based imaging technology has been awarded a half-a-million-dollar government grant.
Angel Eyecare announced it will receive $499,483 through the Critical Technologies Challenge Program: Round 2 – Stage 1, to lead Project GINAN.
The project brings together a consortium of research and technology partners including CSIRO, Siloton, and the Lions Eye Institute.
It’s aiming to transform bulky and expensive eye imaging machines into compact, chip-based retinal imaging devices that are portable, affordable, and capable of detecting sight-threatening diseases.
“It is a deep and sacred honour – for me, my family, and my ancestors – to lead this work,” said Mr Shane Brookman, founder of Angel Eyecare and proud Gundungurra man.
Angel Eyecare is an Indigenous-led eye health provider working to close the gap in vision care for First Nations Australians.
“This project isn’t just about technology. It’s about equity, access, and restoring dignity. With Project GINAN, we’re removing the barriers to care and delivering world-class imaging to every corner of Australia.”
Designed in partnership with First Nations communities, the handheld devices will be tested in real-world conditions, ensuring they are not only medically effective but also culturally safe and appropriate for remote use.
“As a clinician, I’ve seen the heartbreak of preventable blindness in remote communities. As an Australian, I believe we can do better,” said Brookman.
“This grant allows us to turn cutting-edge research into practical tools, and lead the world in health equity through innovation."
Pilot testing and co-design phases will commence in 2025.

We’re excited to introduce the Complete Pair program, powered by our trusted brands and high-quality lenses.
Always have the styles your patients love.
Showcase Ray-Ban and Oakley best-sellers, always in stock with our EssilorLuxottica Complete Pair program. When a patient places an order, we provide a brand-new frame paired with advanced Essilor lenses, tailor-made to their prescription, and send it all in one delivery and invoice covering both the frame and lenses.
No need to hold frame inventory – keeping your display looking great and your patients happy.

Iconic designs from the Aviator to the Wayfarer QUALITY CRAFTSMANSHIP
Durable and comfortable for everyday wear
Perfect for athletes and outdoor enthusiasts
SPORT-SPECIFIC
Trusted by cyclists, runners, and skiers
Trusted innovation, tailored vision, and the power to grow your practice with premium lens technology.
Deliver clear, comfortable vision with lenses your patients can trust.
Activate our EssilorLuxottica Complete Pair program and provide your patients with the ideal combination of iconic eyewear and trusted lenses.
For more information, please contact our friendly customer care team today: 1300 655 612 (Australia) or 0800 441 066 (New Zealand), or email us at OpticalCC@au.luxottica.com





The Australian Society of Ophthalmologists has welcomed a Grattan Institute report into specialist care but warns it paints a one-sided picture of the challenges posed to ophthalmology in Australia.
The Grattan Institute, Australia's independent policy think tank, has turned its spotlight on Australian specialist medical fees and in the process worked to grapple with some of the biggest problems facing ophthalmology.
But not everyone agrees that it tells a full and fair story.
In its June 2025 report Special Treatment: Improving Australians’ Access to Specialist Care, the institute outlines what it sees as systemic flaws in the current ophthalmology landscape, from limited training capacity to high patient fees and poor public access.
It drew the conclusion that patients who need to see an ophthalmologist often face “a painful dilemma” – pay privately out-of-pocket, sometimes double or triple the Medicare schedule fee, or join the queue for an appointment in the public sector.
While the report attempts to confront long-standing issues in the
sector, the Australian Society of Ophthalmologists (ASO) says it misses some key points, potentially obscuring more fundamental problems within Australia’s healthcare system.
“The Grattan report is a good piece of work, but it draws many wrong conclusions,” says ASO president Dr Peter Sumich. “When I see smart people making flawed assessments, I start to wonder whether it was massaged to support an ulterior motive.”
Ophthalmology was one of four specialities the report identified as critically under-supplied, alongside obstetrics and gynaecology, psychiatry and dermatology. The number of ophthalmologists in Australia has increased by 19% over the past decade, well below the average growth seen across other medical specialities.
A persistent mismatch between training capacity and community need is central to the report’s diagnosis.
“The issues start in the training system,” Ms Elizabeth Baldwin, senior associate in Grattan’s Health Program, tells Insight. “Decisions on what type of specialists to train, and where, are made without an overall plan or assessment of the community’s health needs.
“Specialties such as ophthalmology have been growing slower than average, despite being identified as under-supplied by the Department of Health.”
The report also pointed to a bottleneck in specialist training. Though demand for ophthalmology training positions is high, places are limited – influenced by hospital workforce needs and specialist colleges, the Grattan report says.
However, Dr Sumich says this framing doesn’t strike at the root of the problem.
“Firstly, we have to clear up this urban myth about the colleges not training enough specialists. Specialists are trained in public hospitals, not inside a college,” he says. “If public hospitals are not doing enough surgery or outpatient clinics, then we can’t train more specialists. Simple maths.”
Dr Sumich argues that the Grattan report fails to grasp the underlying issue: the deteriorating performance of the public hospital system.
He points to figures showing the ratio of eye surgeons to Australians is roughly one to every 24,181 set of eyes. Yet, only an estimated one in 10 positions is in the public sector.
“If the public hospital system was operating in a reasonable manner, then people would not need private specialists in the numbers they do,” he says. “The government is outsourcing by proxy into a highly inflationary private environment and then complaining about the outcome.
“If medical services were cheap to provide, the government would not have trouble funding them.”
As an indication of Australia’s eroding public eye health service, the Grattan Institute confirmed the well-documented statistic that the vast majority of ophthalmology services occur in private clinics.
In fact, it found 80% of ophthalmology appointments happen privately. But access is patchy: some communities receive far fewer appointments than others, and public clinics aren’t filling the gap. In areas with the least private ophthalmology care, there are 25 fewer appointments per 1,000 people than average – and just six more via the public system.
The cost of private care, meanwhile, varies. While the median out-of-pocket cost for an initial ophthalmology consultation in 2023 was around $100 (placing it 17th out of 34 specialties), 6% of initial
consultations were charged at more than triple the Medicare schedule fee. Around 7% of ophthalmologists were said to charge “extreme fees”, averaging $215 per consultation.
Still, the report acknowledges those charging extreme ophthalmology fees remain significantly lower than other specialties like psychiatry (over $650) and cardiology ($350).
The authors recommend introducing measures to reduce what they describe as excessive charging. One proposal is particularly contentious: to strip Medicare funding from specialists who charge excessively, and name them publicly.
This, Dr Sumich warns, would be both ineffective and potentially inflammatory. He points out that the Medicare rebate itself is fundamentally broken.
Granted, the Grattan report does call for a review of the Medicare schedule fees to ensure they reflect the cost of care. But Dr Sumich questions why it is being used as a benchmark in the first place when “the Medicare patient rebate is uncalibrated, and unrepresentative and unindexed”, meaning it then serves “as no useful metric for specialist services”.
“The Medicare rebate is out of date. It has no meaning in the commercial world,” he says. “It’s been frozen, cut, and has never kept up with inflation or average wages. Therefore, as a metric of a medical service, it is unreferenced and meaningless.”
This is on top of another proposal for the federal government to direct the Australian Competition and Consumer Commission to study how specialists set prices, including how closely their prices reflect the costs of providing care.
Dr Sumich stresses that specialist fees reflect real-world costs –wages, insurance, rent, medical technology, and more.
He also rejects “the implied threat” to remove patient rebates.
“The Medicare rebate belongs to the patient, not the doctor. If it is withdrawn by the government, then specialists would go the way of dentists and charge their own fees regardless,” he warns.
“Most patients would be furious if the rebate was withdrawn.”
For ophthalmology specifically, the report recommends targeted investments in low-access regions through new public clinics ($500 million a year across the medical sector), expanded virtual care, and support for existing clinics to serve more patients. It also urges state governments to develop strategies to reduce hospitals’ reliance on registrars for service delivery.
The report authors want governments to set up a workforce planning body to ensure Australia is training enough ophthalmologists and other doctors, where they are needed.
“Governments should also increase the funding available for training. The federal government should double the funding available for flexible training approaches (an extra $9 million a year), led by colleges, that

“Specialists
are trained in public hospitals, not inside a college. If public hospitals are not doing enough surgery or outpatient clinics, then we can’t train more specialists. Simple maths.”
Dr Peter Sumich Australian Society of Ophthalmologists
Finding: Ophthalmology is a persistently under-supplied specialty in Australia.
ASO fact: The ratio of eye surgeons to Australians is roughly one to every 24,181 set of eyes. Yet, only an estimated one in 10 positions is in the public sector.
ASO question: Why is more public health funding not directed to ophthalmology when nine in 10 Australians reported ‘sight’ as their most valued sense in the 2017-18 Australian Census?
Finding: There are far more applicants for ophthalmology training than there are training places.
ASO fact: Ophthalmology is one of the smaller craft groups with an estimated 1,100 registered practitioners in Australia. Naturally, this makes it a competitive specialty, especially with only 30-35 government-funded training positions available per clinical year. A total of 154 applied for the 2024 RANZCO Vocational Training Program.
ASO question: Why won’t our governments across the country invest in more ophthalmology training positions in our public hospitals – the training ground for the next generation of eye surgeons? There is local demand for surgical training in ophthalmology, why is government not addressing this as a solution to workforce needs?
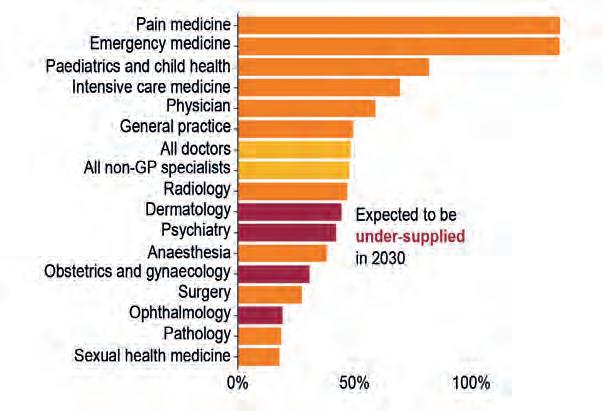
ABOVE: Ophthalmology was one of four specialities the report identified as critically under-supplied.
expand the number of training positions available,” Baldwin says.
“Training standards should be more consistent and transparent. Some work is under way to do this, and the effects of these changes should be reviewed in three years to ensure they have made training more consistent and responsive to community needs.”
Some things the report recommends are already under way, such as making it simpler for overseas-trained specialists to work in Australia – although this new fast-tracking initiative has received criticism from RANZCO and the ASO around safety and quality.
For Dr Sumich and the ASO, the core message is clear: any real reform must start with fixing public hospital capacity.
“The most egregious aspect of this coordinated media blitz is the smokescreen it provides for the woeful failure of public hospitals,” he says. “Inadequate surgical volumes, reduced medical outputs, inefficiencies and bureaucratic wastage feature squarely.”











Succession planning can be a daunting process for practice owners. But ProVision business services manager MARK CORDUFF says it needn’t be. And often the solution is right under your nose.
Transitions and succession planning are not one-way streets. For every business owner thinking and fretting over retirement, the challenge of finding a buyer and the potential end of their legacy, they can rest assured that, more often than not, there is another person pondering how to advance their own career and grab that opportunity of ownership.
If only there was someone who could bring the two together . . .
Dr Michael Kimber was an optometry practice owner nearing the end of his career and pondering that next step for himself and his business, Kimber Optical in the southern Sydney suburb of Hurstville.

Dr Howie Yin was an ambitious practitioner, relatively fresh out of university but keen to make his mark and establish his own practice along strong clinical guidelines.
The one would eventually find the other, at a crossroads on very different career journeys.
But that union would need a matchmaker, and as we all know, the path of true love never did run smooth. Even in business. There would be twists and turns along the way.
Taking on an established practice was not high on the list for Dr Yin, who was just a year out of university and eager for opportunities.
“I’ve always been quite a clinical optometrist,” he says. “I wanted to eventually have my own practice – that's always been my dream – not really for the money but more so that I could look after patients the way I wanted to.”
His first thought was a greenfield practice, probably in a local shopping mall.
“I thought I could build it from the ground up. I'm a bit of a niche practitioner. I do orthokeratology and advanced lenses – that's what my interest is – these sort of more complicated situations, and I wanted to be able to serve the community in a more clinical environment.”
Luckily, he sought the guidance of professionals that specialise in the commercial side of optometry to provide advice and support around leases, ownership options and other complicated business activities.
Dr Yin had joined optometry network ProVision in 2023 as an associate. And although he wasn’t a practice owner yet, that put him in touch with

“That's always the first question I ask: Is there anyone in your practice that's the perfect succession plan, or is there someone in our network or something like that?”
Mark Corduff ProVision
They worked with Dr Yin on the numbers behind his plan.
“I looked into the rent, into the fit-out costs, then into how the cashflow would look for the first 18 to 36 months,” he says.
“The greenfield was just too expensive and I could not fund a reasonable amount of it by myself.”
Bartholomeusz, a ProVision NSW business coach, and Corduff, the network’s business services manager, also helped with insights into the competitive Sydney market.
“Sydney is just super-saturated, so finding a new location, a new spot where people haven't gone in and taken all of the market share as well is impossible unless you go an hour and a half away from the CBD,” says Dr Yin.
“It just wasn’t going to work out.”
That news might have been a considerable setback for others in their mid-20s, but Dr Yin at least felt some relief that he wasn’t making a poor business decision.
And it wasn’t long before his mentors presented him with another opportunity, one he had not explored before.
Bartholomeusz and Corduff knew they had a young optometrist with strong clinical interests keen to set up a practice in Sydney. They also knew they had an experienced practitioner considering retirement and pondering the next step in his succession planning.
“They put me in contact with Michael,” says Dr Yin.
He wanted to know if this would be a good fit clinically; Dr Kimber had to be sure that this young man would be a good addition to the practice over the next three years, as they worked together on the transition to his departure and Dr Yin’s handover.
First impressions sorted, “there was just a couple of months where me and Michael chatted, sort of worked out what kind of deal we wanted to do and, and after that, it was away we go”.
Dr Yin says ProVision was the matchmaker – “like Cupid” – the winged infant’s bow and arrow replaced with business calculators, contracts and plenty of helpful advice.
Corduff chuckles at that comparison.
“Often it's about connecting the retiring optometrist and the younger one who's ambitious, then bringing them together and helping with that fit,” he says. “This is a big part of how we assist both parties at ProVision

and is extremely rewarding for all involved.”
He says those arrows hit the mark with Drs Yin and Kimber.
“I think they will be a great fit those two, they got along like a house on fire. Then it was just about them going through all the steps to execute it.”
That execution is not always easy for practitioners considering succession planning and the sale of a long-held business.
“It's because it’s the first time and last time most people do it,” says Corduff.
“So when you're considering your plan, we always recommend looking three to five years out, because, number one, you’ve got to make sure your practice is profitable and ticks all the boxes to launch to the market.”
That’s when Cupid sometimes needs to administer a little tough love.
“Profitability that can be clearly demonstrated is king,” says Corduff.
“Often in longer term succession plans, we find some opportunities to increase profitability.
"As you would appreciate, these take time to embed, so identifying these things can make the practice more profitable as well as more appealing to a larger pool of buyers.”
Appraising the value of a business can be difficult for both buyer and seller.
Corduff says he and his team can help with that. ProVision is also working on a tool to help all parties better understand the value of the business transaction they are considering.
For the most part, he prefers to steer people away from greenfield projects and sometimes complex and costly shopping mall leases.
He believes the best union is often a partnership between professionals like Drs Yin and Kimber in an established practice.
“That's always the first question I ask: Is there anyone in your practice that's the perfect succession plan or is there someone in our



network worth reaching out to? Because if you're going in cold, it can be a longer process.
“If you've got a bigger practice with a few optometrists in there, it's about finding the right time, having the conversation, just explaining, ‘hey, look, I might be nearing retirement. You're a great optometrist and an asset to the business. Would you be interested in potentially buying in or buying me out in the not-too-distant future?’.”
ProVision can then facilitate and support that transition, for both buyer and seller.
Corduff says that helps to keep independent optometry thriving, which is ProVision’s "north star".
“If we assist in selling a practice that doesn't remain within ProVision but remains independent, that's still a huge win,” he says, “just to make sure that the industry continues to thrive.”
Dr Yin represents that future.
He’s 27, has taken on a business himself but is learning from an experienced practitioner and supported by a strong optometry network.
And he’s loving it.
He’s a one-man show as he talks with Insight; someone has rung in sick so he has to jump up a couple of times during the interview to answer the phone.
As well as his optometry duties, he’s taken on more of the management role, which means looking after pricing, HR, accounting and payrolls.
“A lot of little knick-knacks that you don't normally expect to do as an optometrist.”
Far from daunted, with the support of Dr Kimber and his mentors, Dr Yin is enjoying his deep dive into business.
“I could not be any happier.
“The barrier to entering a practice was inconceivable, and ProVision really broke down those walls.”




Go to: rodenstock.com/bigvisionforall























*A clinical study shows that Blink® Intensive Tears Eye Drops significantly provides more improved visual sharpness, and is more comfortable, soothing, and less blurring than another leading brand.1
Soothing relief for dry, irritated & uncomfortable eyes
Contains Sodium Hyaluronate 0.2%
Safe to use with contact lenses
Also available in preservative-free single dose units


Proven to deliver superior efficacy and customer preference*


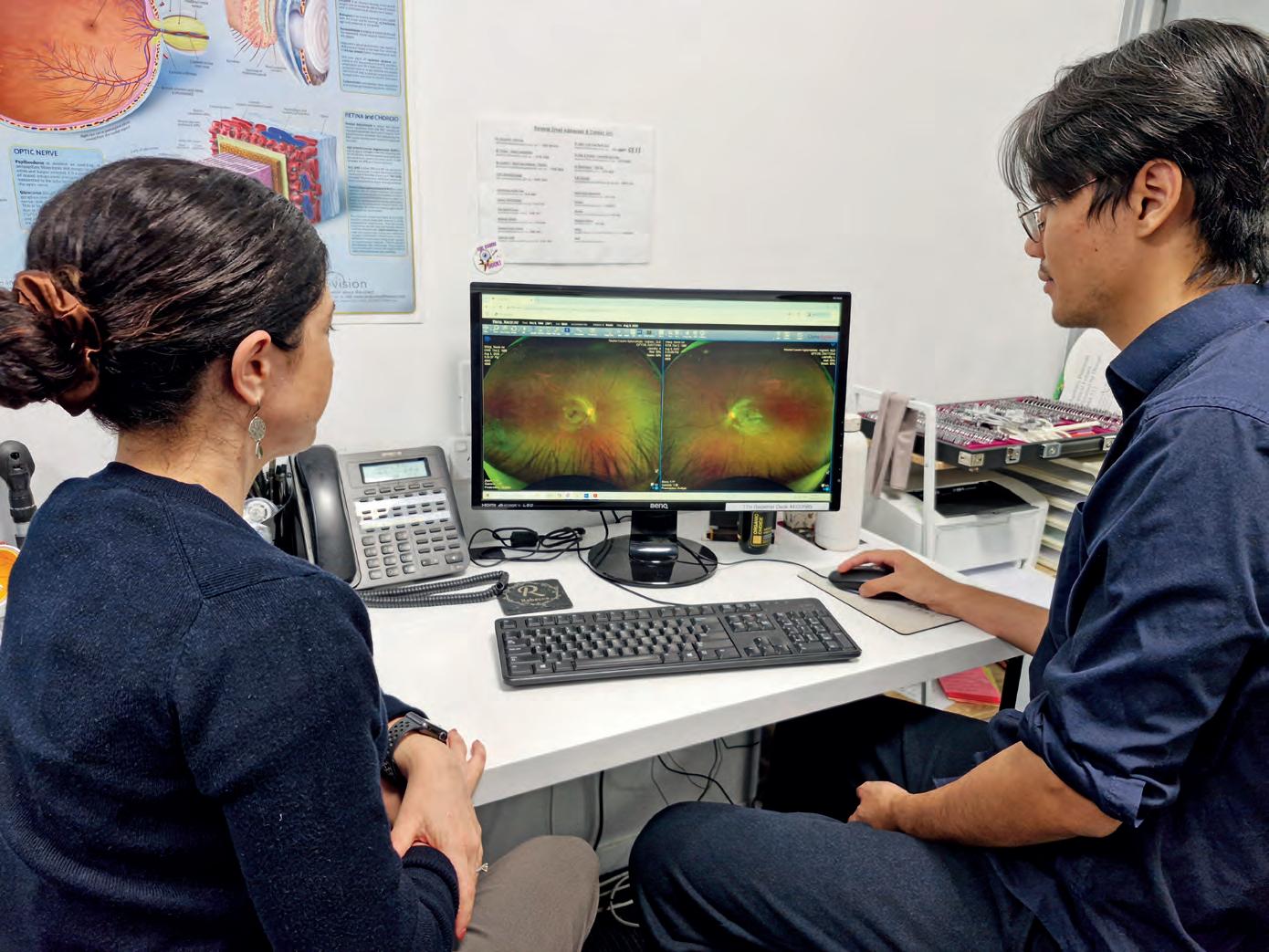
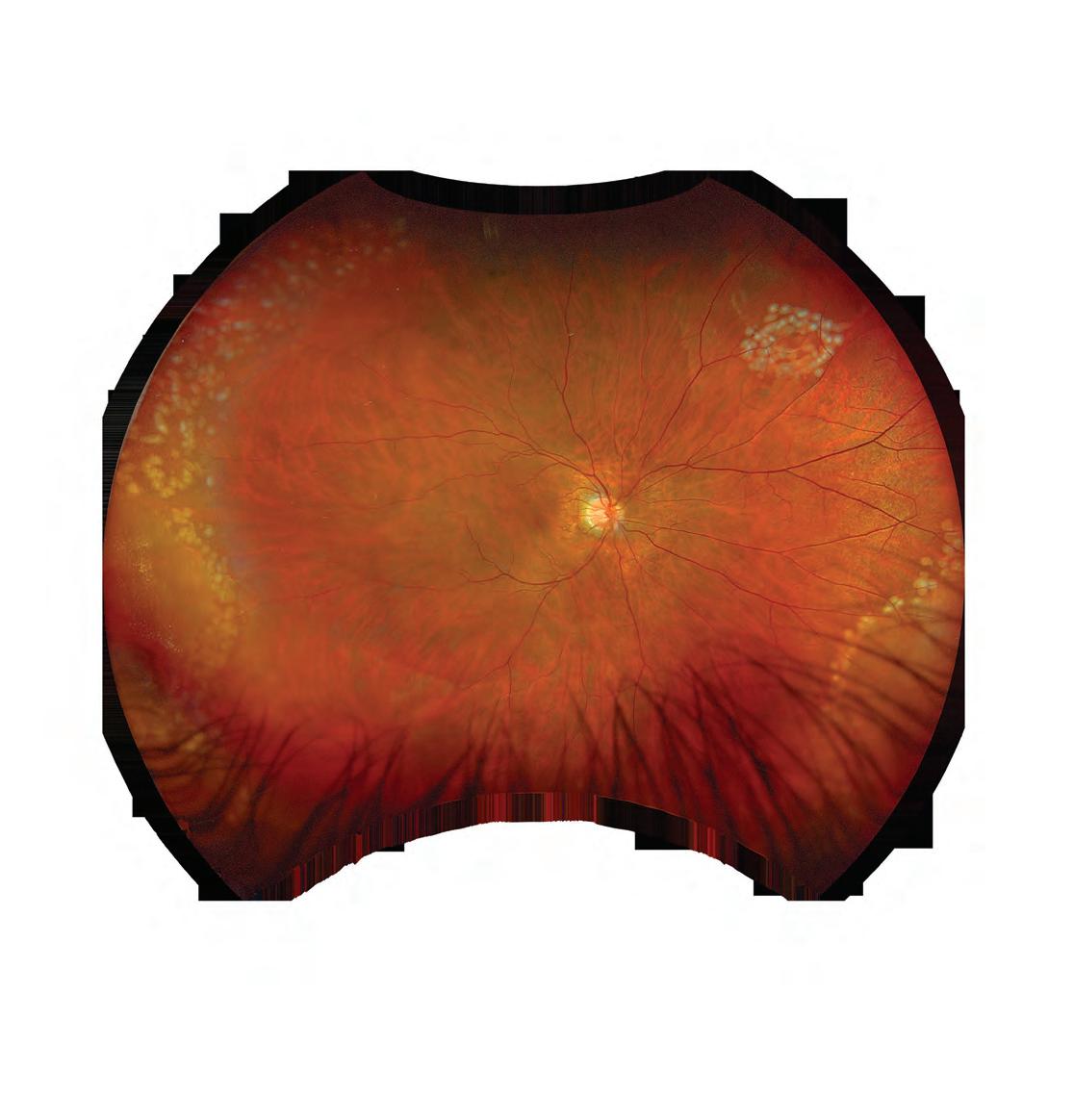
Ultra-widefield retinal imaging has transformed care at Rachel Cauchi Optometrists, where every patient is now screened on the device. For this regional practice, it’s delivering one of the most valuable outcomes in eyecare: trust between the clinician, patient and ophthalmologist.
For patients living in and around Ingham, a regional town in North Queensland, accessing specialist eyecare often means travelling more than 100 kilometres to Townsville – a trip that can be time-consuming, costly, and difficult to arrange at short notice.
It means that every referral carries significant weight – not only in terms of the patient’s time and resources, but also for the region’s hard-working ophthalmologists juggling full appointment books.
It’s one of the reasons why ultra-widefield retinal imaging has become such a vital part of the patient workflow at Rachel Cauchi Optometrists.
With the ability to capture a high-resolution 200-degree view of the retina in a single image, the Optos Daytona system provides an elevated level of clinical confidence for the practice’s three optometrists.
Offering several imaging modalities, including autofluorescence, it helps them to detect conditions they might not have otherwise, especially out in the peripheral retina, while minimising unnecessary referrals. Ultimately, it galvanises relationships with patients and local ophthalmologists.
“We wouldn’t have a practice without our Optos system,” says Mr Travis Cauchi, who co-owns the practice with wife Ms Rachel Cauchi, the principal optometrist. “Every patient receives an optomap image in the pre-test phase – it’s that essential to how we work.”
As the only optometry provider in the Hinchinbrook Shire, the practice serves a large catchment, including parts of neighbouring Cardwell Shire. That kind of reach brings its own set of challenges: the nearest ophthalmology services are an hour and 10 minutes away, which is more than an inconvenience, especially with elderly patients.
“We work closely with the public eye clinic at Townsville Hospital and the local ophthalmologists down there. They’re booked out most of the time,

“It’s about being able to deliver the kind of care that patients deserve, without them having to travel unnecessarily or wait longer than they should.”
“Six months later, he got an Optos system for himself.”
Using the same imaging platform provides a level of familiarity and continuity between primary and tertiary eyecare. It also means

ophthalmologists can assess optomap images remotely and provide feedback quickly.
“We’ve had specialists ask us to email the scan so they can check it on their phone. Thanks to the resolution of the image, they’ll have a look and call back straight away with advice,” he says. “That speed of assessment has been a real advantage.”
Rachel Cauchi Optometrists’ journey with retinal imaging began back in 2007, when the practice purchased its first fundus camera, one of its first eye health instruments.
“It was a 45-degree camera, and that in itself felt like a big step at the time,” Travis recalls.
The motivation came from a Canadian optometrist working at the practice, who had experience using pre-test lanes and more advanced technology in his own clinic overseas. It was a turning point for Rachel and Travis, who decided to modernise their workflow despite some early pushback.
“Pre-testing was a foreign concept back then, especially in regional practices. Some of the staff really struggled with the idea. But we knew we had to start moving beyond how optometry had been done for the past 20 years,” Travis says.
Going from refraction-based optometry to a more eye health-focused model was gradual, but not without hurdles. Introducing a $40 imaging fee was a major shift for patients who had never paid for such services before. But looking back, Travis says it was an important move.
“I’m glad we went through that journey early. It set the foundation for everything we do now.”
Today, that retinal imaging is performed with the Optos Daytona. It’s the second Optos device the practice has owned, after switching to the manufacturer in 2016.
The practice became aware of Optos’ imaging capability after a locum ventured up from Brisbane, where she’d seen the technology in action. Later, she went to a trade show and returned with Optos brochures. Understanding the power of an outside voice, especially for an isolated regional practice, Travis and Rachel “made the leap” not knowing how transformative it would be.
“The first time our optometrists saw a widefield image like that, they were
blown away. They were used to trying to view the periphery manually with an ophthalmoscope, but seeing it captured so clearly in one image was a completely different experience,” Travis says.
The system quickly began picking up pathology that might otherwise have been missed, particularly in the far periphery. Retinal tears, for example, became far easier to detect and manage early.
“It really did change how we assess eye health,” Travis says. “We went from a narrow field to seeing so much more – and doing more for our patients as a result.”
Initially the practice was going to acquire optomap scans judiciously, but the locum optometrist intervened again.
“She'd done her MBA, and said, ‘look here’s a working model for you. It's amazing technology, you should do it on everyone, and make it that little bit more affordable’,” Travis says.
“At the end of the day, you can’t make that kind of investment and only use it occasionally. We did the numbers and realised using it consistently made the most sense – financially and for better patient care.”
It was integrated into the pre-test lane. The 200-degree widefield view can be captured without dilation. While Rachel Cauchi Optometrists doesn’t dilate during routine eye examination, it does for diabetic patients, and on indication.
With three full-time optometrists seeing patients in 30-minute slots, the device runs continuously throughout the day.
“Every optometrist is worried about having a piece of equipment that turns out to be a white elephant, but this just goes and goes. It’s a very reliable machine, which is important when your closest service support is a flight away in Brisbane.”
And support from the Optos team has also been a strong point. “They’ve been great to deal with. That matters in a regional setting.”
After using Optos ultra-widefield for nine years, it has become more than just a diagnostic tool. It’s offering a long-term record of each patient’s retinal health.
“After using it for that long, we now have what I call a ‘picture book’ of our patients’ eyes,” Travis says. “Especially for our older patients, we can scroll through and see how their retina has changed over time, and now we’re starting to gather images of their kids and grandchildren too.”
That capability is invaluable for monitoring progressive conditions.
“It gives us the ability to keep an eye on things accurately. If someone’s waiting to see a specialist, we can do a review and know if anything’s changed since their last image,” he says.
The images also form part of the practice’s communication with local GPs, particularly for diabetic patients.
“We automatically send optomap scans with our GP reports. It helps them understand how well a patient’s diabetes is being managed and whether it’s affecting their vision. GPs appreciate having that certainty, and it really builds the professional relationship.”
As regional practices continue to hold significant weight in the broader healthcare landscape, tools like Optos Daytona provide a level of confidence and trust between the optometrist, ophthalmologist and patient.
“For us, it’s not just about keeping up with technology,” Travis says. “It’s about being able to deliver the kind of care that patients deserve, without them having to travel unnecessarily or wait longer than they should.”
And when asked what things would look like without Optos, Travis doesn’t hesitate.
“We just wouldn’t. That’s the truth. From the clinical point of view, it’s a must-have.”





Optical lenses make up a sizeable portion of any practice’s revenue but samples are often consigned to a drawer. Rodenstock is looking to change that mindset with a dynamic system that helps customers better understand the power of the lens and the science behind it.
“The ultimate tool.”
That’s high praise for what appears to be a simple mechanism for helping optometry patients better understand what they are purchasing – and for practices to upgrade on those purchases.
But Ms Sonya Broadhead is so impressed and passionate about this particular item that when she’s asked if she would recommend it to other practices, her reply is emphatic:
“Not in the Illawarra – no!”
It’s not just that Broadhead, the owner of Seeside Optical in Thirroul, a southern Sydney coastal suburb, is protective of her patch. It’s also that she understands how this item and the products it promotes helps her business stand out in a competitive marketplace.
The object that she is so enthusiastic about? Rodenstock’s new B.I.G. Vision Lens Experience system.
The system is a physical hub within the practice that serves as a conversation-starter, an education point, and a decision-making tool all in one.
Patients can explore their vision needs in a hands-on way, seeing and understanding for themselves how the latest biometric lens technology can transform their vision.
For practice owners like Broadhead, the B.I.G. Vision Lens Experience system is more than a display. It’s a bridge between cutting-edge lens technology and the human experience of vision turning science into something patients can touch and see.
The display – which comes in three different sizes depending on a practice’s space needs and specialisation – features magnetic modules covering different topics, including physical features of the lens, thinness, how fast it reacts to light and dark, and the scratch resistance of its coating,
which can be easily upgraded and switched for launches of new products or maybe a focus on specific visual issues.
There are also other interactive tools, including touch screens and a torch to help demonstrate how a lens changes in different light.
But to Broadhead, the display is so much more than a clever tool to help upsell lenses and grow awareness of Rodenstock products.
Like the monolith that was a key marker of human evolution in the movie 2001: A Space Odyssey, she believes this modern totem is a sign pointing to the future of optometry and optical dispensing.
“I think as independents, we need to start looking at the most important thing and becoming more medical,” she says.
“We're trying to differentiate ourselves and be more in the health or medical fields, rather than in fashion and the two-for-one sales. That's where we're trying to align ourselves.
“And the way to do that is behind lenses and showing the technology that is there,” she says.
Lenses make up a significant portion of a practice’s revenue, about 50% according to Rodenstock Australia marketing manager Ms Rozalb Naqshbandi.
But they are largely invisible in most stores.
“Frames have so much advertising and I guess it's advertising for lenses which is really lacking,” says Broadhead.
“This [Rodenstock’s display system] is what you should have in place of over half the stock on your shelf, because this is what's going to increase your average selling price.”
She has witnessed that for herself since installing the B.I.G. Vision Lens Experience system over six months ago.

“We're trying to differentiate ourselves and be more in the health or medical fields, rather than in fashion and the two-for-one sales. And the way to do that is behind lenses and showing the technology that is there.”
Many customers were visiting the practice, their minds set on simple single vision lenses for reading.
But after talking to Broadhead’s staff and using the interactive information on the display, they understood the advantages of using the Rodenstock Office Lens instead and were happy to pay more for the premium product.
“We do a lot more of what we call digital office lenses rather than readers now.”
She says the display is the “ultimate tool” for her optical dispensing team.
“Everybody looks at the frame, and there's so much branding and fashion around the frame, but at the end of the day, what you're selling is vision,” she says.
“From a customer's point of view, we're selling something they can't see. They're going off our word as to what we're going to give them. And when you put a wall in there that they can physically touch, then they can see something that they're going to purchase.
“It's going to give customers more confidence in what they're receiving
It takes most people an average of five years to seek support once they start to lose their vision.
At Vision Australia, we have made it our mission to ensure nobody faces the confusion, frustration and loneliness of vision loss on their own. Our low vision experts are here to support your patients to make the most of their remaining vision and maintain their independence.
Refer your patients to Vision Australia today through Oculo or by scanning this QR code.
from you and more confidence in what they're purchasing as well. And even when trying to explain things to a customer, this makes it just so much easier –they can physically see and touch the items.”
Naqshbandi agrees that frames are an essential product for an optometry business.
But she feels lenses are due their day in the sun.
“The B.I.G. Vision Lens Experience system helps to make lenses more visible in the practice,” she says.
“Traditionally, you would have some samples, which most of the time live in a draw somewhere in a practice. You will have an iPad or another form box device; you might have some tools and other things.
“It's basically all over the place. This concept brings everything together, all the physical aspects of the lens that are bread and butter for the practice.”
The displays are designed to be easy to mount on a wall, and practices can choose to have systems with three, six or nine removable modules.
Also, those modules can be updated easily if a new coating or lens is launched, or if a practice is keen to focus on a specific aspect of eyecare.
Training to use the system is minimal, especially for practice staff familiar with Rodenstock products, and language used is patient-centric.
“It's designed to help patients understand and grasp the concepts,” says Naqshbandi.
“It's not very technical, it's not optometry slogan, just language and tools they can engage with.”
Feedback from practices using the displays has been positive.
Many of those had started with the smaller versions and then decided to order the bigger displays, she says.
Broadhead recommends that practices use the displays as part of their work to stand out from other businesses.
Just not in Illawarra, perhaps.



Eyes Right Optical emerged as a dominant force in the independent optical scene’s most coveted awards program in 2025. The wins reinforce a reputation that’s built on eyewear design excellence and a service practices trust.
As the independent optical community gathered to hear the winners of the Optical Distributors and Manufacturers Association (ODMA)’s revamped awards program in 2025, one company name just kept cropping up.
Whether it was the best product, people or service, three words – Eyes Right Optical – featured prominently as ODMA’s CEO Ms Amanda Trotman recognised those making the biggest impact on the independent scene right now, as voted by 2,100 industry professionals in the lead-up to ODMAFair25 in Sydney.
But while awards often make the headlines, they rarely tell the full story.
For Eyes Right Optical managing director Mr Mark Wymond, the real victory isn’t the accolades – it’s what they represent. The relentless pursuit of high-quality product backed by exceptional customer service. Delivered day in, and day out.
“It was one of those moments where you take stock to appreciate the brands we’re fortunate to represent in the Australian market, and the work of our team,” he reflects.
“At the end of the day, all we want to do is make our customers – independent optometry practices – look good. That’s not only the frames on the shelf, but the customer service behind that too.”
Eyes Right Optical’s impressive haul at ODMAFair25 started in the Versatile Frame of the Year category, where the company reigned supreme. Best seller Face à Face’s Didot 1 topped the category. But impressively, all three finalists were frames distributed by Eyes Right Optical. The other two designs were Face à Face Offset 1 and Prodesign Denmark Glow 5.
In the Sales Representative of the Year Award, Ms Kristy Gierisch was announced the joint-winner. She’s the company’s sales rep for west Victoria, South Australia and Tasmania, and just edged out colleague Ms Belinda Bishop, also a finalist, who works as another of Eyes Right Optical’s reps in the southern states.
The company also stood tall in the Supplier of the Year category, ultimately won by HOYA. But Eyes Right Optical was the only frame wholesaler in a field dominated by lens companies, most of them multinationals.
It’s an extension of a long and consistent winning legacy for Eyes Right Optical, and other Wymond-owned eyewear supply businesses Modstyle, Morel Australasia and Sunglass Collective – especially in the frames category,
with victories in 2011, 2013, 2015, 2023, 2024, and now 2025.
“During that time, we've continued to be the front runner in the frame category, but it’s also pleasing to do so across various brands,” Wymond says.
“Whether it’s ProDesign, Morel, Avanti, Face à Face, Project Green or Kaleos, we've been fortunate to distribute a host of brands that resonate with the Australian market. They’re continually trying new things, evolving in the shapes, techniques and colorways that keep them ahead of the curve. They're the brands we like to distribute: avant-garde, at the top of their game, and creating design-driven product.”
This year’s award-winning frame, the Face à Face Didot 1, isn’t something Eyes Right Optical would normally submit for an ODMA award that usually recognises boundary pushing pieces that might not necessarily be a best-seller but are magnificent examples of design-focused eyewear.
Wymond and his team were mindful to stick to the ‘versatile’ brief, which they interpreted as best-seller designs.
“Face à Face Didot is a frame that’s selling extremely well,” he says. “It hits that sweet spot – appealing to the conservative customer who wants just a hint of colour and still wants outstanding quality.”
The Face à Face brand itself is no stranger to awards and acclaim. Designed and created by Design Eyewear Group, and distributed exclusively in Australia through Eyes Right Optical, its bold acetate cuts, vibrant colourways and expressive design language have made it one of the most recognisable luxury eyewear brands in the country.
“Design Eyewear Group have nailed the formula,” Wymond explains. “They strike this balance between saleability and avant-garde design. Just when you think all avenues have been explored, they come out with another beautiful new shape and acetate cut that’s fresh and exciting.”
The independent optical community also appreciates colour in another way: colourful characters, like Gierisch. Despite being five years into the role, Wymond was thrilled, yet wasn’t surprised, she won the Sales Representative of the Year Award, given her extensive optical knowledge and character.
After many years as a respected optical dispenser-practice manager at Wills Street Eyecare in Bendigo, Victoria, and Holdfastbay Optometry in Adelaide, Gierisch joined Eyes Right Optical as a sales representative in 2020.

“Her optical acumen, her friendly nature – it just resonates with practices,” says Wymond, who’s known Gierisch for more than 20 years through her previous roles.
Gierisch carries ProDesign, Project Green, and Vera Wang, for Eyes Right Optical and Kaleos, Serengeti and Bollé for Sunglass Collective and is a popular visitor to practices across west Victoria, South Australia, Tasmania.
“She’s not just someone selling you a frame; she comes with sound optical knowledge and advice – she enters the practice and brightens your day.”
With Bishop also recognised as a finalist in the same awards category, Wymond says it’s a testament to the calibre of talent the company identifies and attracts.
“Belinda has extensive industry experience and represents Morel and Face à Face and WOOW for our southern states and with her kind and friendly nature, is a favourite for many practices,” Wymond says. “To have two finalists in that category shows the strength of the team we’ve got out on the road.”
One of the more quietly significant accolades at ODMAFair 25 came in the Supplier of the Year category, where Eyes Right Optical was the only frame wholesaler listed among finalists – the others being major lens players like ZEISS, Rodenstock, EssilorLuxottica and HOYA, which took out the top honour.
“We were flanked by huge multinational companies,” Wymond says.
“We're just a small family business in a lot of ways. To be mixing it with those companies, to be there or thereabouts in customer service and product offering, that’s a powerful win in itself.
“We’re not a multinational, but our relationships, our reliability, and our brands have got us to this point.”
Underpinning all of this is a service ethos that’s as much about relationships as it is about sales and data.
“We pride ourselves on being a partner in the practice’s dispensing area,” Wymond says. “We don’t do the short term, hard sell. We want to grow together, with the practice for the long term.”
That support extends to “old-school” touches on the service side. If practices call about a frame, an Eyes Right Optical customer service representative will pick it off the warehouse shelf, and ship it that day.
“We’ve got the tech to automate a lot of that, but we choose to do it this way. There’s a real reliability in that approach.”
That reputation also paid dividends at ODMAFair25 where the each of the four Wymond-owned eyewear companies nailed their most important objective – doing business.
“It was pleasing to open a number of new accounts and secure more shelf space in existing ones,” Wymond says.
“Face à Face always draws attention, but ProDesign and Avanti from Modstyle also had great reactions. And Project Green’s latest collection really turned heads. I saw people stop and come back for a closer look with some new bolder designs.
“We’re fortunate with the number of beautiful, high-quality brands we have that hold significant shelf space and weight in the industry. It’s taken some time, but we’ve reached a point where we can significantly benefit any practice’s frames range, and really could become a one-stop-shop for their frames supply.”


Myopia is sweeping the world and beginning to have an impact in Australia. But there may be a way to identify it and stop it in its tracks. Insight takes a closer look and finds two eyecare professionals who have successfully prevented myopia in their own families.

Mr Jason Teh has broken the cycle.
Before the arrival of his own children, family gatherings were a sea of bobbing spectacles, a vibrant froth of frame styles, colours and lens thicknesses.
He’s seeing a few of those now as he speaks with Insight, during a visit to Vietnam with family to celebrate his father’s 80th birthday.
“In my family there’s me, my brother, my sister and our parents – all five of us are myopic,” says the Victorian optometrist , who has a special interest in myopia and dry eye disease in his In2Eyes practice in Melbourne’s Surrey Hills.
“My wife and her family circle are also highly myopic.”
Rather than stand by while two more young pairs of eyes were lost to the wave of myopia beginning to hit Australia, Teh decided prevention had to be better than management. That dealing with the possibility of pre-myopia was preferable to trying to control the eye disease after it had begun to undermine his children’s sight.
So Teh set upon a preventative path also trodden by a number of other professionals, including Sydney optometrist Dr Susan Ang, who had the same concerns for her children.
It’s a path with important waypoints, including initial work to detect the risk of pre-myopia in children, and then use of strategies to ensure the final destination is not myopia and vision loss. A path they encourage other ophthalmic colleagues to follow.
“When I had my two kids – they are 16 and 18 now – I was super focused on prevention,” says Teh.
He drew on all his experience from 24 years in independent practice, including the early years of myopia management, and the use of contact lenses and atropine.
He was swayed by growing evidence of the influence of environmental factors, and especially the promotion of outdoor time and reduced screen time, including research presented at the recent Global Orthokeratology and Myopia Control Conference in Singapore.
“There was a presenter who extrapolated all the researched data about outdoor time.
"He basically came up with a statement that in the first 10 years of your
child's age, if they got three hours of outdoor time a day, the risk of developing myopia is under 10%.”
That evidence backed up what he did with his own children, including encouraging them to put down their screens, head outside and pursue a sport.
Partly because of that, his 18-year-old son is a handy basketballer with “really good eyesight”, while his 16-year-old daughter remains a work in progress.
“She had a little bit more of an axial length risk. And then she started becoming ever so slightly myopic, so I got into the MiYOSMART D.I.M.S. [Defocus Incorporated Multiple Segments] lenses very early in the piece.
“Today, she still has a bit of astigmatism, which we’re managing, but her myopia remains extremely low and hasn’t progressed beyond -0.50D.”
Dr Ang has been similarly proactive to keep myopia at bay for her young son.
She is an optometrist with a special interest in paediatrics and special needs children, and sees patients aged between zero and 24 years old in her Sydney practice, Eyestore.
“The risk of changes in eyes usually stops about 24 and I feel that once they finish university and they've started work, their eyes generally stabilise and we can graduate them out of my care,” she says.
Dr Ang’s own son is far from graduating age, but at eight years old he was at risk of joining the growing global myopia alumni.
“I noticed last year that his eyes were growing a little bit, quite fast for that age group, so in July last year, I decided that although he was +1.00 D, I would put him in a pair of Essilor Plano Stellest glasses.
“He wears them during school time, homework, screen and device time, and I've just noticed a nice steady plateau of his eye length.”
That screen time is limited; the iPad use is only for school work and a little bit of social time at the weekend.
Dr Ang acknowledges that the lenses can be a pricy intervention for some parents, even before they face the challenge of enforcing sometimes unpopular rules around screen time and outdoor activities.
Also, this can often follow results of eye tests showing their child’s vision is good at this point.
But she insists that such actions are sometimes needed if there is a risk that
eyesight might not stay that way. “We need to educate parents that seeing well is sometimes not good enough.”
That education is needed for practitioners as well.
One of the problems about heading down this particular path of pre-myopia is that it is still fresh, and the few signs along the way are vague and potentially misleading.
The path of myopia control and management is itself relatively new but at least well-trodden and understood.
Whereas, not a great deal is known about pre-myopia, how to detect its risk and the guidelines for ensuring it does not become its debilitating older brother.
That means optometrists and other eyecare professionals can find themselves on shaky ground.
The International Myopia Institute (IMI) has a little guidance on evaluation of pre-myopia.
It defines the condition as “a refractive state of an eye of ≤+0.75 D and >−0.50 D in children where a combination of baseline refraction, age and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions.
“It is likely that the other quantifiable risk factors include hereditary/genetic influences and lifestyle,” it says.
Using that definition, a recent study of almost 24,000 children in Taiwan aged five to six years found that the prevalence of pre-myopia could be 52%.
Another study, in Shanghai, put the number at 21.9%.
Beyond this definition, there is little else to help eyecare professionals reach definitive conclusions on which they can build a case for clinical intervention, including potentially expensive glasses and significant behavioural change that might not actually be needed.
A child with a refractive result of ≤+0.75 D and >−0.50 D will not necessarily become myopic.
What that means in Australia is that practitioners like Teh and Dr Ang must go beyond simply measuring that refractive range and the axial length of a young child’s eye to determine if they are pre-myopic and at risk of myopia.
For Teh, “if you're at age six and your cycloplegic refraction is around ± 0.50 D then that's a risk factor.
“And then the axial length, anything over 23.5 millimetres, is definitely a risk factor.”
For him, other factors include whether one or both parents are myopic, whether the child spends less than 90 minutes outdoors each day, and how much near work the child does.
Ethnic background is another consideration for both practitioners.
Myopia is particularly prevalent in Asian cultures.
“When I first opened the practice, I didn't realise that I was going to get such a following of Malaysians and Singaporeans and people from Hong Kong, so definitely about 80% of my client base is Asian or of Asian origin.”
That means he sees plenty of myopia.
“Growing up, we were always indoors and education is a huge thing,” he says.

“Pre-myopia is a natural extension of myopia management, so I think that in order to reduce the overall impact of myopia, naturally it's important to also focus on pre-myopia.”
Jeanne Saw Myopia Profile

That includes plenty of near-work and intense study on languages, music and other subjects, which raises the risk of myopia.
Dr Ang also likes to test a child’s hyperopic reserve, which is another recent focus for the IMI and an indication of how effective the child’s distance vision is.
“Hyperopic reserve can be eroded through too much device use,” she says.
“As a six-year-old, my expectation is that your child should have a hyperopic reserve or a plus figure that sits about +1.50 to +1.00 D. And then I'll do my testing and say, ‘Look, your child sits at +0.50 D, and it's a little bit low for this age group’.”
That intense education and a growing reliance on laptops and tablets in schools may be myopia risk factors for some, but Dr Rohan Hughes believes more education about pre-myopia may actually help to provide one path to preventing it in the first place.
The Postdoctoral Research Fellow in the Queensland University of Technology (QUT) Centre for Vision and Eye Research has secured significant overseas funding to investigate the early warning signs of myopia in Australian children.
The research, funded through the American Academy of Optometry Foundation, will be the first of its kind in Australia to investigate pre-myopia.
Dr Hughes knows myopia well. He sees plenty of it in the QUT Myopia Control Clinic, where he works as one of the supervising optometrists.
“It's the kids that are pre-myopic that have always interested me because we know that they're already on the pathway to myopia, so the logical question is always whether we can try and stop the process.”
It’s already too late for Dr Hughes.
“I'm myopic, but I find it interesting because I grew up in North Queensland and you tend to spend a fair bit of time outdoors,” he says.
“But I was also a pretty avid reader, and I feel like I had the two most well-established risk factors sort of working against each other, but I've still ended up being myopic.
"So that has certainly piqued my interest in research.”
He too believes that preventing myopia in the first place would be better than having to rely on various ways of managing it.
“We know that if we can delay or prevent myopia progression, then we have

“Diet and sleep have been loosely linked with myopia in the past, but there's not a lot of solid evidence behind either of them,” says Dr Hughes.
That’s one of the challenges of approaching pre-myopia.
Many eyecare professionals like Dr Ang and Teh are doing good work, but pre-myopia and its treatment is understudied.
However, research is rapidly emerging, says Dr Hughes.
“The definition for pre-myopia was only established in 2019 from the original IMI white papers,” he says.
“Until now, most people have identified that myopia is a problem and that we should try to slow progression, and clinicians have certainly been offering advice regarding lifestyle modifications with the hope of preventing myopia development or delaying onset.
“But now, with this definition, I think the focus has shifted in the last couple of years to trying to identify what we can actively do to prevent or at least delay myopia from developing using our current myopia control treatments.”
The sector was already grappling with the building wave of myopia.

better outcomes long term with respect to the ultimate level of myopia and the risk of myopia-related eye disease.
“If we can actually stop them from becoming myopic in the first place, if we're able to identify factors that can predict the kids that will become myopic, it gives us the opportunity, clinically, to intervene a bit earlier with myopia control treatments that might actually prevent or at least delay the onset.”
As part of the study, Dr Hughes and colleagues Dr Emily WoodmanPieterse, Professor Steve Vincent and Professor Scott Read, intend to first conduct vision screenings of more than 1,000 children at schools across Brisbane, to identify the prevalence of myopia, pre-myopia and other refractive errors in Australian school children.
The second part of the project will be a 12-month longitudinal study of those children identified as pre-myopic.
“We'll be measuring eye growth and refractive error, and capturing images of a range of eye structures, and seeing if there's anything that we can measure in a clinical setting that might predict a kid who's going to progress towards myopia development.”
The researchers will also look at a range of environmental factors, from the oft-mentioned near-work and outdoor time to different variables such as diet and sleep.
“The added concept of pre-myopia may be adding complexity to clinical myopia management, but pre-myopia and myopia are essentially part of the same process, so we can always be doing work to understand and manage both aspects.”
Ms Jeanne Saw, manager of professional affairs and relationships at Myopia Profile, doesn’t believe that a focus on myopia management should come at the expense of work to prevent the eye disease in the first place.
“Pre-myopia is a natural extension of myopia management, so I think that in order to reduce the overall impact of myopia, naturally it's important to also focus on pre-myopia.”
Myopia Profile, founded by Brisbane optometrists Dr Kate Gifford and Dr Paul Gifford almost a decade ago, is now one of the world’s premier sources of support and assistance for eyecare professionals, practices and parents.
It has some pre-myopia guides and resources on its online platforms.
“Our Managing Myopia Guidelines Infographics, which are freely available on the Myopia Profile website, has a section for risk factors on the practitioner chairside reference side. This details all of the different risk factors to look out for,” says Saw. “And it also details what to discuss with patients and parents on the parent-facing side.”
She agrees that while it may be ideal to focus on prevention and not just management, research on pre-myopia is currently sparse and limited, and there are plenty of knowledge gaps for eyecare professionals, parents and young patients.
Dr Hughes and his team plan to publish their findings in about two years.
He hopes that these will reveal scientifically backed predictive factors that have direct clinical applications for practices and patients.
“If we find something significant that you could actually measure clinically that then indicated, or ideally predicted, that a particular child was about to undergo a really rapid rate of eye growth and then most likely go on to develop myopia, it would allow us to identify and intervene with those children and start applying myopia control treatments to either prevent, delay or slow it.”
Dr Ang and Teh will be keen to see those results and the tools that flow from them.
But they are not hanging around.
Research and data might be limited, but all agree that environmental factors such as outdoor time, near-work and screen use, among others, are helping to fuel the rise of myopia and are possibly key to preventing it in the first place.
“I just said to a young parent, ‘If you're going to a dentist appointment or optometrist appointment, bring your child a toy, a water bottle, fidget toys, and let them go for it,” says Dr Ang.
“You don't need to hand them the phone at three years old – that’s the social norm because it's a whole social anxiety about how their kids have to be online, catching up with their social life through Tik Tok and what have you.
“We've engineered myopia into our lives.”
Now it’s time to find the tools to prevent it.

BY UP TO 60% WITH ATROPINE 0.01% EYE DROPS AT 2 YEARS COMPARED TO PLACEBO *1 -3
*P-value not available (ATOM 1 & 2 studies, placebo was a historical control from ATOM 1). ATOM 2 study data available for 5 years with 1 year washout after 24 months.3

EIKANCE 0.01% eye drops (atropine sulfate monohydrate 0.01%) is indicated as a treatment to slow the progression of myopia in children aged from 4 to 14 years. Atropine treatment may be initiated in children when myopia progresses ≥ –1.0 diopter (D) per year.1
PBS Information: This product is not listed on the PBS.

Before prescribing, please review full Product Information available by scanning the QR Code, or call 1300 659 646
This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at https://www.tga.gov.au/reporting-problems.
Optometrists can prescribe MiYOSMART with even more confidence with HOYA revealing new eight-year data. No other clinical study on myopia management spectacle lenses has tracked outcomes over such an extended period.
“First mover advantage.” It’s a term referring to the competitive edge a company gains by introducing a product ahead of its competitors. For HOYA in myopia management, this early entry hasn’t just built brand recognition and customer loyalty — it’s enabled the company to consistently raise industry standards.
The lens manufacturer’s MiYOSMART product first launched in Australia and New Zealand in 2020, and during those five years, the ophthalmic landscape has seen a wave of other myopia spectacle lens options.
But while companies have been working to bring their own products to market, HOYA has forged ahead with its product development, making MiYOSMART available in clear, polarised, and photochromic options, and increasing the power range.
Most importantly, it has been building an evidence base that reinforces the long-term effectiveness of the lens, as well as its performance in key areas including combination treatment with atropine, across various ethnicities and age groups, and in pre-myopes.
Many of these key updates were presented at the company’s scientific program, ‘Exploring new frontiers in myopia management with MiYOSMART’, at the Association for Research in Vision and Ophthalmology (ARVO) 2025 Annual Meeting in Salt Lake City, Utah, in May 2025.
One of the headline read-outs was the eight-year data on MiYOSMART, which incorporates Defocus Incorporated Multiple Segments (DIMS) technology, stemming from the widely accepted peripheral hyperopic defocus theory. This makes it the world’s longest-running clinical study on myopia management spectacle lenses.
It showed that continuous DIMS spectacle lens wear significantly reduced myopia progression (-1.00 D ± 0.41 D, p=0.017) and axial elongation (0.42 ± 0.18 mm, p=0.019) consistently over the full eight years (n=11) of follow-up.¹
The results – from Lam CSY et al – are an extension of the important two-year randomised clinical trial showing that daily use of MiYOSMART slowed myopia progression on average by 60% compared to wearing standard single vision spectacle lenses.²
The latest eight-year evidence demonstrates that wearing MiYOSMART spectacle lenses continuously and long-term may improve myopia management outcomes, the company says.
Dr Natalia Vlasak, global head of medical and scientific affairs at HOYA Vision Care, says:
“This landmark study, featuring the longest follow-up to date for myopia management spectacle lenses, reveals that long-term MiYOSMART use continues to significantly slow myopia progression so that children can enjoy their lives to the fullest.
“These findings emphasise the life-changing value of long-term adherence, providing crucial information and guidance for eyecare professionals and parents committed to protecting children’s vision health for the future.”
Meanwhile, the first 12-month data read-out from the ASPECT randomised controlled trial demonstrated that combining low-dose 0.025% atropine eye drops with DIMS spectacle lenses stopped myopia progression in around
The researchers also explored vision-related quality of life (VR-QoL), indicating a trend towards improvement in general vision (p=0.049) and competence (p=0.031) in children using low-dose atropine and DIMS spectacle lens combination treatment. 4
“Our findings suggest that combining MiYOSMART spectacle lenses with atropine can unlock even greater outcomes for children with myopia progression, marking a positive step towards more personalised, powerful treatment strategies in myopia management that suit the unique needs of each child,” says Dr Vlasak.
As optometrists place more emphasis on preventing myopia in the first place, at ARVO HOYA also released outcomes from a first-of-its-kind pilot study evaluating DIMS spectacle lenses for pre-myopia management in five- and six-year-old children.
This indicates DIMS technology may offer a protective effect against the development of myopia in this population, says HOYA.
Over nine months, the average cycloplegic spherical equivalent refraction (SER) remained stable with a yearly change of +0.06 D compared with -0.15 D in a control group.


While axial length increased slightly (22.48 mm to 22.64 mm, p<0.01), the choroidal thickness remained stable.
The company says these promising initial findings suggest MiYOSMART spectacle lenses may help to prevent myopia development and postpone onset in pre-myopic preschoolers, laying the groundwork for future research. 5
“We want eyecare professionals to feel confident in our MiYOSMART solutions when managing childhood myopia in their everyday practice,” says Mr Ulli Hentschel, HOYA Lens Australia's training and development manager.
“That’s why we have generated a robust and wide spectrum of evidence, with the aim of empowering eyecare professionals to meet the diverse needs of patients.”
And there’s more data to back that up — perhaps the most compelling of it all: to date, more than 12 million MiYOSMART spectacle lenses have been sold worldwide in over 40 countries.
NOTE: References will appear in the online version of this article and are available upon request.





Kiwi optometrist GINA PARTRIDGE discusses instances when the new Abiliti 1-Day soft contact lens has made the difference in some worrisome cases of myopia.
New Zealand optometrist Ms Gina Partridge has been prescribing ACUVUE Abiliti 1-Day for more than 18 months – a head start, it would seem, over her Australian counterparts who have only recently gained access to the latest soft contact lens for myopia control.
But in many ways, Australian optometrists are in a unique position to hit the ground running, drawing on insights from their Kiwi colleagues who’ve been diligently figuring how out how to integrate the new lens into their management strategies.
In Partridge's Auckland Myopia Clinic, soft contact lenses are a cornerstone of myopia management, used in 60% of cases. She often prescribes them for low myopes, typically under -1.50 D or -2.00 D or those not yet ready for orthokeratology. Soft lenses are also ideal for anisometropia when one eye has good vision and the child might resist glasses.
In the case of Abiliti 1-Day, she has observed several key advantages since becoming one of New Zealand’s early adopters of the Johnson & Johnson (J&J) Vision lens in late 2023.
Firstly, the smaller size and lens properties make it easier to fit, especially in very young children with smaller eyes. The high oxygen permeability provides significant peace of mind given their potentially long lifetime of contact lens wear, and the concentrated high plus in the centre is beneficial, especially in patients with smaller pupils and low or no astigmatism.
On average, Abiliti 1-Day has been shown to slow axial elongation by 0.25 mm over a two-year period,1 with almost 65% showing no clinically meaningful myopia progression (less than 0.25 D).
But Partridge has also seen the lens have remarkable effect in some more extreme and unique cases.
One of those patients is a four-year-old boy already -8.00 D and diagnosed with genetically-influenced high myopia. Previous attempts with atropine caused an eye turn, myopia control spectacles weren’t effective enough, and an earlier trial with soft contact lenses was also unsuccessful due to dry eye issues and lens dislodgement. Furthermore, his eyelid anatomy made insertion of larger lenses challenging. The smaller Abiliti 1-Day lens addressed these issues directly, while also providing a bandage effect against his inward turning eyelashes which were causing corneal staining and discomfort.
"With Abiliti, he could learn to put it on and take it off completely by himself," Partridge explains.
“We fitted him with the lens in July-August 2024, and for the last year his spectacle and contact lens prescription hasn't changed. His axial length is still progressing, but instead of being ~0.6-0.7 mm per year, it’s reduced to ~0.2-0.3 mm a year.”
With the patient having a smaller pupil, Partridge can’t say for sure but suspects the high treatment zone in the centre of the lens contributed to this success story, plus his better visual acuity promoted greater compliance.
In another instance, a child presented with a unique scenario where one eye was progressing at a much faster rate than the other (R 0.22 vs L 0.12mm) over 10 months.
Abiliti 1-Day was fitted to the progressing eye, creating a direct comparative study within a single patient.
“After 15 months, the right eye fitted with Abiliti progressed at a much slower rate (~0.07mm) while the other progressed at a rate similar to the year before (~0.15mm). So, the Abiliti lens did seem to have more of an effect in this child.”
Teenage patients present their own set of challenges, particularly concerning compliance with prolonged lens wear.
Another of Partridge’s patients is a 17-year-old high myope who dropped out of orthok wear due to poor vision and allergies. He was still experiencing significant discomfort and redness from his previous myopia control soft contact lenses due to extended wear hours – often from 7am to midnight due to educational demands. He resorted to changing his lenses twice a day, using lubricating and anti-allergy eye drops in order to remedy this.
While not endorsing excessive wear, Partridge had some comfort knowing he was in a silicone hydrogel lens when switching over to Abiliti 1-Day, which is made from senofilcon A, the same material as ACUVUE OASYS 1-Day, known for its comfort and breathability.
“This allowed him to wear a single lens for the majority of the day, significantly improving his comfort and proving more cost-effective for his family,” Partridge adds.
It’s these sorts of patients – those with “high or tricky scripts” – where Partridge’s Auckland Myopia Clinic does its most powerful work. Being able to offer Abiliti 1-Day in her myopia management repertoire is a
privilege for Partridge, who – as a high myope herself with subsequent yet mild retinopathy – is personally motivated to ensure progressing myopes aren’t resigned to a similar fate.
She has worn contact lenses since the age of 11 and understands the practical and emotional journey many of her young patients embark on. This lived experience, coupled with her unexpected foray into paediatric optometry, serendipitously drew her into the world of myopia management.
Her practice, co-founded with two other colleagues, was originally a central CBD practice providing general optometry services, but it pivoted dramatically post-COVID lockdowns to become myopia-focused.
This was driven by the volume of children who were presenting with progressive myopia.
“It was also a chance to make a difference in an area of optometry that we were so passionate about," she adds.
That passion for myopia management continues to grow, driven not only by emerging research and clinical insights but also by innovations like Abiliti 1-Day.
For Partridge and her optometry colleagues, much of the fascination lies in its unique design that includes a smaller diameter and base curve suited to a child’s eye.
But at its core, Abiliti 1-Day has two critical elements: a +10D Central Boost zone and a +7 D RingBoost design. 2
Dr Emma Gillies, J&J Vision’s professional education and development lead, says the +7 D RingBoost provides a substantially greater amount of plus to be incorporated into the treatment zones.
The ring is focused off the line of sight, creating a treatment effect that maintains visual quality, while the +10 D boost is designed to increase the overall efficacy of the design.
She references the BLINK study3 demonstrating the more plus power that can be incorporated into a design, the greater the efficacy in myopia management. But, there' s a limit to the amount of plus that can be built into the design without significantly impacting the quality of vision through the lens.
“This has historically been a limitation in most soft contact lens designs used for myopia management,” Dr Gillies says. "The breakthrough technology of Abiliti 1-Day breaks that nexus."
The principle of non co-axial optics – which doesn’t feature in competing designs – is the secret sauce in Abiliti 1-Day.
“The non co-axial design allows the light from the treatment zones to be focused in a ring around the line of sight. This is what allows us to introduce significantly more plus into the design without significantly impacting the visual quality for the patient,” Gillies says.
For other practitioners looking to prescribe Abiliti 1-Day, Partridge believes it stands out in first-time wearers with smaller apertures and higher corneal curvatures.
She encourages careful and precise fitting in the presence of astigmatism (the clinical study inclusion criteria limited astigmatism less than 1.00D cyl), or when the child has a dilated pupil from atropine. She encourages a longer trial period of approximately two to three weeks to allow for adaptation.
“I find teaching children much easier than adults with contact lens wear. They are so much more adaptable, more fearless and quick to learn,” Partridge says. “Soft contact lenses make a huge difference to a lot of children and families who want to avoid the stigma of wearing glasses or being short-sighted, plus it allows them to more confidently pursue the activities and hobbies they love.”
NOTE: References can be found in the online version of this story.
Insight’s new website keeps you updated on the latest industry news and information. With a world-class responsive design, Insight is now accessible seamlessly on any device, 24/7.
Sign-up FREE to our eNewsletters and industry reports delivered weekly straight to your inbox.

One Queensland optometrist is helping his patients deal with short-sightedness while he considers his own longer-term prospects. Luckily, he has a prominent support network to lean on for help.
The saying goes that you can’t teach an old dog new tricks. But in Toowoomba, Queensland, one seasoned optometrist has turned that on its head and is teaching timeless tricks to a new generation of families.
Optometrist Mr David Neilson may be near retirement, but until he moves into that new chapter later this year, there’s still plenty of well-travelled wisdom to impart for young parents and their potentially myopic children.
Now part of the George & Matilda Eyecare network, Neilson Eyecare balances the freedom of local care with the support of a national backbone.
Neilson is part optometrist, part teacher, part counsellor in the regional practice he has either worked in or owned for the past two decades.
Neilson Eyecare has been an optometry practice in Toowoomba under one name or another since the 1940s.
The two and half optometrists and five support staff (at time of writing they were looking for number six) work out of a beautiful 110-year-old house; they’ve still got some decades-old cards featuring pounds and notes in fountain pen.
The irony is that such things might be considered out-dated, museum pieces made redundant by newer technology, but it is the parental advice of a bygone era that people are now turning to to help preserve their children’s vision.
Neilson sees a broad spectrum of people in his business – from young families and their kids to patients in their 90s who have a strong connection with the 80-year-old practice.
But it’s the former that he is seeing a lot more of, and the risk of myopia is often why they are there.
“Traditionally we did better, myopia wasn’t as prevalent as other areas, because we've got backyards here, we've got farm kids,” he says, touching on the known benefits of two to three hours of minimum outdoor activity in preventing the onset or slowing the progression of myopia.
“But what I've noticed within the last couple of years is that there's more screens in primary schools, so you've got more kids on the edge of it [myopia].”
That’s where Neilson comes in. He’s built a strong paediatric practice by working hard to keep kids from falling over that edge, which has to start early and involves plenty of pushing, prodding and counselling younger parents often reluctant to place rules on their children’s screen and outdoor time.
Many years of talking to parents, explaining how eyes work in an easy-to-un derstand way, has helped create a strong local following.
“It’s about preparing the parents,” he says, outlining his approach that relies just as much on sound technology as it does on straight talking.
“You can see there's a predisposition to myopia in terms of visual inefficiency there, and certainly with family history.
“You look at mum and say, well you're short-sighted and we want to try and prevent that happening, so you have the conversation early, so it's on the parents’ radar.”
The difficulty is often that he is explaining a problem that has not really
happened yet. “We are looking to change the mindset to prevention, rather than just waiting for the wheels to fall off.”
Convincing those parents that changes might be needed at home to keep myopia at bay can be a challenge.
For Neilson, the OCULUS Myopia Master and other equipment in his practice can help demonstrate the risk to parents and patients through axial length measurements, analysis software and easy-to-understand reports for parents. But it’s old-school parenting, common sense and the highlighting of consequences that really hammer it home.
“When you've got a parent who’s short-sighted, you explain, well you didn't start off short-sighted. And then you start to talk about them about their journey. “They’ll say, ’When I was at uni, I couldn't see the lecture boards’. And you question, ‘was it lecture boards that caused the problem?’. And they sit and start to think.
“Now I've got cause and effect in their minds,” he says, “and they haven't actually talked about prevention or averting something, so you're changing that mindset of the parent early on.”
His younger patients get the benefit of that advice as well.
“I’ll say it's like fast food; some of it's OK, but what if you ate hamburgers every day, what would happen?"
Neilson will then encourage his modern, young parents to consider advice of those from the past: stop watching that screen and find something to do outside.
“I’ll say to the parents, well, you know, we didn't grow up with computers compared to what these kids are going to do now.”
If there’s an element of old-fashioned ‘tough love’ there, many parents appear to appreciate it. “Sometimes I feel like a broken record, but I think parents appreciate the fact that it's not just in and out, bang, there you go. We're here to be your optometrist, if not for life, then at least in the longer term.”

As well as the advice, Neilson outlines a plan for monitoring the development
“You look at mum and say, well you're short-sighted and we want to try and prevent that happening, so you have the conversation early, so it's on the parents’ radar.”
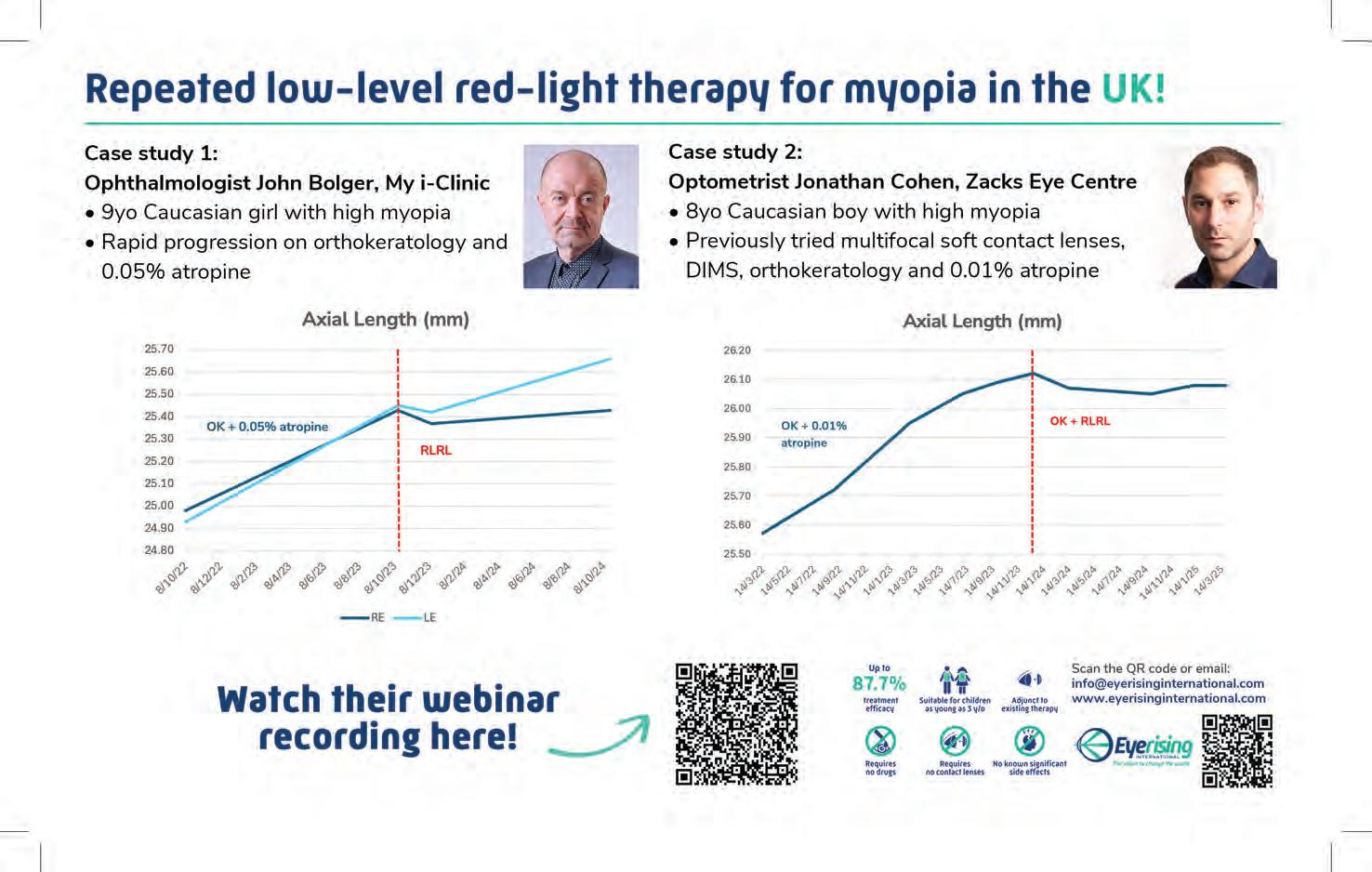
“The Myopia Master really helps with this,” he says. “It produces several graphs which we use to explain the child’s progress to the parents.
“We use a series of strategies – lifestyle factors, looking closely at binocular vision problems and prescribing accordingly, and the early use of atropine drops. We then have the range of DIMS lenses, myopia control soft contact lenses and ortho K.
“We have been doing this for quite a while. I even have a handful of patients who are still using their old Executive bifocal lenses [Myopialux]. They have had good success and are keen to keep things as is.”
That extra advice and time spent taking a parent through their own journey to help them understand the path their child might be on can create a bond between practice and parent, practitioner and patient.
It’s extra time that other optometrists might not be able to spare.
But Neilson says it’s something that many are prepared to pay a little extra for. They see it as an investment.
“We don't bulk-bill,” he says. “It would be very tough to do all of that on the bulk billing. That's the reality.
“People are happy to pay, but the responsibility is that you give a higher level of care and service to people.”
Neilson’s relationship with George & Matilda supports that philosophy. His practice became part of the network last year, following the company’s acquisition of National Optical Care, a group that had already shared many of the same values around independent practice and clinical autonomy.
The move has brought even greater support behind the scenes, allowing Neilson and his team to focus more fully on patients while planning for the future.
He believes George & Matilda has improved its professional services and supports the network’s clinical work.
It holds regular conferences and there’s a chat group that brings
practitioners together to support their clinical work and patient care.
And George & Matilda is now helping Neilson prepare for his own next chapter – retirement, of sorts, and a move to the coast with this wife.
When he announced that it was time to move on, he agreed to stay on for two years to support the transition for his team.
“The two-year handover has helped me deal with the staff, get the optometrist up to speed and in a good position where they can carry on practising the way we do.”
The partnership with George & Matilda happened during that transition and Neilson says the company has been a great support.
“G&M took the weight of management off our shoulders, so we could focus on patient care,” he says. “We've got a HR department we can call on and there’s purchasing and stock management.”
Mr Anthony Sargeant, national professional services manager at George & Matilda, says the goal is to make succession feel seamless, not surgical.
“We don’t take away what made a practice special. We back it," he says.
"Succession should preserve trust, protect clinical independence, and make sure the team and patients are thriving long after the owner steps back.”
Retirement and succession planning can be scary subjects.
Neilson has had plenty of patients in his practice approaching that chapter and keen to talk about things other than their eyesight.
“Being a rural practice here, I get people off the farms, and the husband is scared to death of retiring and dying, and the wives have had enough for the farm. They just want to get off.”
He appreciates having George & Matilda to help with the tricky process.
“I remember this guy saying that getting into business is hard, but getting out of business is harder. We're all going, 'have I got enough super? How long do I work for?'. So I think the George & Matilda model, this business plan of buying these practices, this is a great exit strategy for a lot of people.”
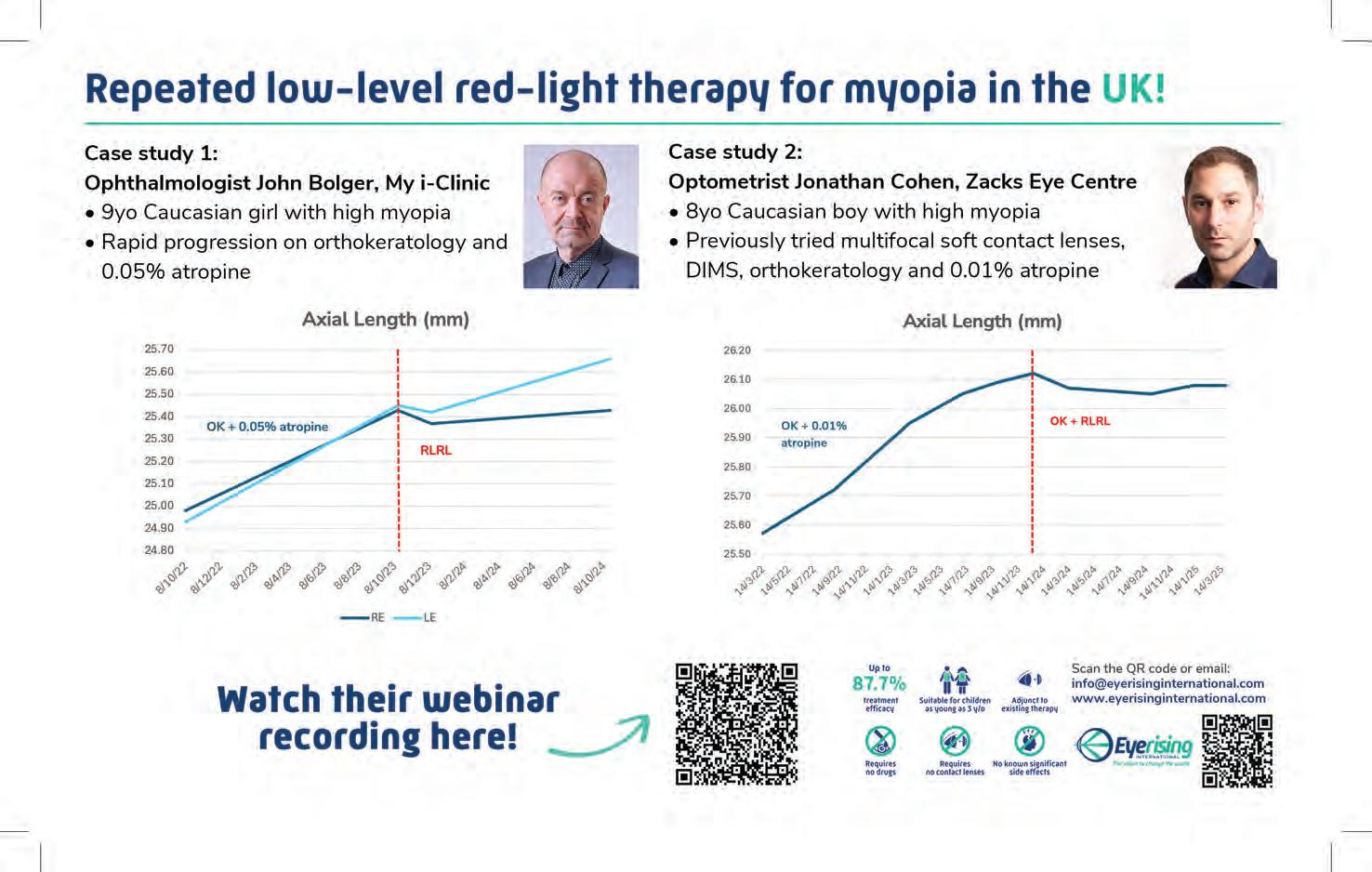
Tokai Optical unveiled its MYOGEN myopia lenses at ODMAFair25. Other companies have similar products in the market, but the Japanese lens manufacturer says that sometimes, good things come to those who wait.

Tokai Optical recognises it has arrived a little later than others in the Australian market for myopia management spectacle lenses. But as the company’s Australia general manager, Mr Justin Chiang, points out: practitioners may have tried the rest, but have they experienced what he considers the best?
One advantage of entering a little later than competitors is the chance to get a good gauge on what works and what doesn’t, and find ways to refine your own offering.
Chiang says the principles behind Tokai’s MYOGEN Advanced Myopia Control Lens are similar to those in other products – peripheral light is redirected to induce myopic defocus, a clinically validated approach shown to reduce axial elongation, the structural hallmark of progressive myopia. That defocus function, where the point of focus is in front of the retina, rather than behind, is available in other designs.
But the MYOGEN lenses, which were registered and approved by the Therapeutic Goods Administration (TGA) in April 2025 and officially unveiled to an eager ophthalmic audience at ODMAFair25 in June, advance on that technology with Tokai’s unique, proprietary “honeycomb structure”, improved contrast and clarity, and what the company describes as its superior scratch-resistance qualities.
That makes them ideal for young myopic patients with active lifestyles, says Chiang.
“I think one of the advantages for Tokai being compared to some others, and a bit late into this market, is that we have seen what is out there and improved on that existing product,” he says.
And he has some numbers to back that up, but more on that later.

At the core of MYOGEN is its innovative honeycomb microstructure, featuring hexagonal lens segments approximately 600 μm in size.
These elements are distributed with a 300 μm spacing between adjacent hexagons.
These precisely positioned segments are key to the success of the lens in encouraging children to wear their myopia-management glasses for sometimes long periods, says Chiang.
Conventional lenses provide a central focus point around the circle in the middle of the eye, between 9-10 millimetres, and then the peripheral defocusing spreads out over the remainder of the lens.
Tokai’s MYOGEN lens operates on a similar principle, but its denser honeycomb microstructure, with tightly spaced hexagonal segments, helps minimise visual “jump”, blur, and discomfort beyond the central optical zone, delivering a smoother and more comfortable visual experience for the wearer, the company says.
“So imagine you’ve got a lot of links but more spread out, and when the image goes through those links that will cause a certain jumping in the image, jumping between the microstructures, which can be a cause of discomfort and blurred vision,” he says.
“But in Tokai’s MYOGEN lens, in the same area we can fit more micro lenses and because they are smaller and it's more dense, the gap is less, so the transition is more smooth.”
He says because that makes the visual experience better, young myopic patients may be more likely to wear the glasses longer and comply with their treatment.
“A lot of kids actually drop out because they don't want to wear them, so it defeats the purpose of needing to wear the glasses for certain hours to control the myopia progression,” he says.
“And being able to improve that part [visual comfort] will encourage them to wear what they need to wear for more than eight hours a day.

“Imagine you have a pair of lenses and there's this scratch or you don't see very well or they're very thick and heavy. You probably wouldn't want to wear them for too long. And they don't feel comfortable wearing them.”
Justin Chiang

“So I think that's one of the key improvements in myopia control lenses.”
Helping to increase that compliance, especially for sometimes very young patients, is the thinness of the Tokai lenses, which makes them light and more comfortable.
Tokai is able to provide 1.7 index lenses, even in a higher refractive prescription.
And its renowned scratch-resistant coating options make it ideal for younger children needing to wear their myopia-management glasses for long periods in their active lifestyles.

The company’s Super Power Shield coating is standard with the lenses, providing exceptional scratch resistance, durability, and ease of cleaning.
Blue Cut Coating is also available as an option to filter high-energy blue light for children who frequently use digital devices.
“Tokai is quite specialised in coatings – we have a special division doing the thin film and industrial coating,” says Chiang.
This, along with the greater visual comfort of the honeycomb structure and the lightness and comfort of the thin lenses, further encourages children to keep their glasses on and get the most benefit from the myopia-control treatment.
“Because imagine you have a pair of lenses and there's this scratch or you don't see very well or they're very thick and heavy,” he says.
“You probably wouldn't want to wear them for too long. And they don't feel comfortable wearing them.”
Another advantage of turning up later has been Tokai’s ability to conduct plenty of analysis and comparisons between more established myopia-control lenses.
Chiang says it has data showing that, compared with other lenses, Tokai’s MYOGEN offers better contrast and visual acuity.
Also, its higher ABBE values of 42 (for 1.60 index lenses) and 36 (1.70) mean greater optical quality and less chromatic aberration compared with other products on the market with lower values.
The ABBE value is a measure of how much a lens material disperses light. A higher value means less dispersion and better image quality, while a lower value indicates more dispersion and potential colour fringing.
All of which made Tokai’s official launch of the MYOGEN lens a popular part of ODMAFair25 in Sydney.
“There was a lot of interest,” he says. “The biggest interest was for the higher refractory index, like 1.7, and we've received quite a few orders.”

“Eyecare Plus has truly empowered my practice to grow and thrive.”
Shaina
Zheng, Optometrist Eyecare Plus Mermaid Beach

EssilorLuxottica has marked 45 years of research and innovation in myopia management with a big presence at APSPOS 2025, reflecting decades of dedication to managing this global condition through science, technology, and collaboration.
EssilorLuxottica has most bases covered with myopia management in Australia and New Zealand. One of the industry’s most powerful lens-based interventions, backed with high quality monitoring tools like the REVO FC OCT and Myopia Expert 700, are compelling options for optometrists now offering the standard of care for this condition.
But the company isn’t done there. It believes the solution lies not only in innovative products, but in collaboration – where optometrists, ophthalmologists, orthoptists, and vision scientists work in step to protect children’s eye health.
This was the driving message behind EssilorLuxottica’s presence of the 3rd Congress of the Asia-Pacific Strabismus and Paediatric Ophthalmology Society (APSPOS), held in Brisbane from 29 June to 1 July 2025. The company was the premier partner at the region’s most significant event for paediatric eye health, co-hosted with the Australian and New Zealand Strabismus Society (ANZSS) and the Australian and New Zealand Paediatric Ophthalmology and Strabismus Society (ANZPOS).
Themed ‘Inspiring Collaboration’, the meeting welcomed more than 560 delegates from 37 countries and offered a platform for professionals to converge around the big priorities in paediatric eye health.
“This APSPOS partnership was incredibly important to us because it reflects our commitment to collaborative care and advancing clinical knowledge in caring for paediatric and strabismic patients,” says optometrist Ms Amy Pillay, professional affairs manager for EssilorLuxottica ANZ.
“By being at the forefront of this event, we’re able to engage directly with ophthalmologists, orthoptists, and optometrists – sharing evidence-based insights and innovations like Essilor Stellest lenses. It’s also an opportunity to reinforce our shared goal: slowing myopia progression and improving visual outcomes for children.
“Our role extends beyond product innovation – it's about building awareness, supporting early detection of pre-myopia, and equipping practitioners with evidence-based solutions.”
Essilor Stellest lenses have emerged as one of those solutions. After
launching in ANZ in 2022, the myopia progression control spectacle lens has become a key addition to the optometrist’s toolkit, supported by robust long-term clinical evidence.
Highlighting the strength of this data was a major focus of the EssilorLuxottica contingent at APSPOS that included Pillay alongside ANZ eyecare and medical & professional affairs director Ms Sephora Miao, and ANZ senior vice-president of operations Mr Carl James.
Joining them were Australian myopia authorities Dr Loren Rose and Dr Kate Gifford who featured in the EssilorLuxottica-hosted breakfast symposium to discuss a collaborative approach to curbing the myopia epidemic along with Pillay and Miao.
Dr Rose, discussing best practices in ophthalmology, also presented the latest six-year clinical data on Essilor Stellest lenses. The results showed the lenses slowed myopia progression by 1.95 D (57%) and axial elongation by 0.81 mm (52%) compared to an extrapolated single-vision lens control group. Importantly, these effects were sustained up to 19 years of age, underscoring the product’s long-term efficacy.1
“We have robust data to explain to our patients and their families about the use of myopia control spectacles to reduce myopia progression over the long term and in older patients,” Dr Rose says.
“I am asked when to treat with these glasses. I would say the earlier, the better and single vision glasses only correct vision, while these interventions correct vision and help control the growth of the eye.”
Dr Gifford, a leading voice in optometric myopia management, highlighted the importance of early pre-myopic intervention, including risk factor identification and published research on proactive treatment strategies, in addition to increasing time spent outdoors and managing near work time. She discussed new clinical evidence supporting the use of Essilor Stellest lenses (plano pair) in children at risk of developing myopia.
This proactive mindset, now being increasingly embraced by eyecare professionals, comes as the Essilor Stellest lens was evaluated recently in three studies for its potential to delay myopia onset in non-myopic children.2,3,4

In one of the first published studies exploring optical interventions for children with low hyperopic reserves, pre-myopic children aged six to 10 years who wore Essilor Stellest lenses (plano pair) for more than 30 hours per week demonstrated a slowing in axial elongation compared to children using standard single vision lenses.2
A separate retrospective study in China further supported these findings, the company said, showing slower axial growth in 88% of at-risk children after one year of wear, with axial growth rates even lower than those of emmetropic peers.3,5
At APSPOS 2025, the EssilorLuxottica booth served as a learning hub for delegates, many of whom sought out deeper clinical insights after the symposium, helping to also broaden awareness of Essilor Stellest lenses beyond the optometry scope.
“Slowing myopia progression with spectacle solutions are gaining recognition in ophthalmology, especially through collaborative platforms such as APSPOS,” Pillay says.
On the booth, a large-format wall display of the Essilor Stellest six-year data was complemented by a comprehensive information pack featuring 17 published studies and a new Essilor Stellest lens prescription pad with plus and minus cylinder formats and conveniently featuring the full lens range.
Delegates also engaged with diagnostic technologies on display, including the REVO FC OCT available with the myopia forecast module, Myopia Expert 700 for axial length measurement, and the ICON paediatric retinal camera – tools available through OptiMed that support best-practice care for paediatric patients.
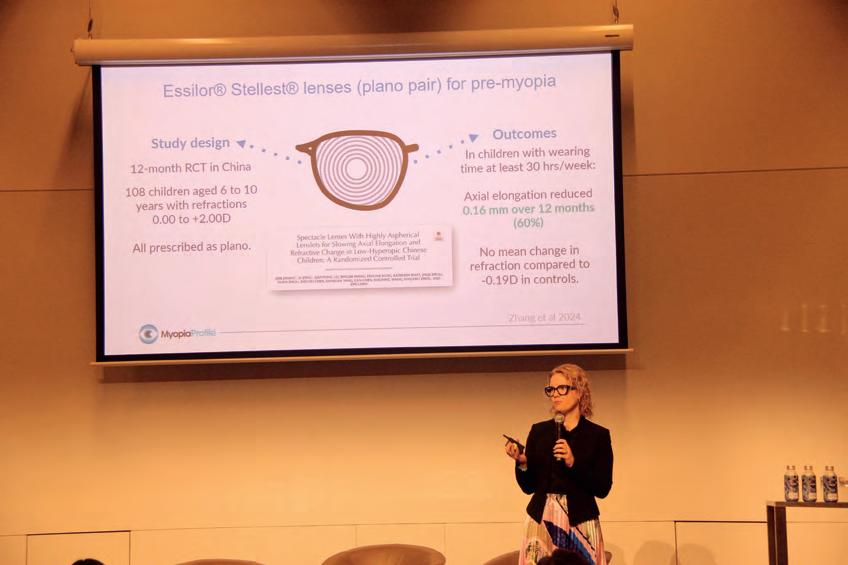
As EssilorLuxottica deepens its role across the eye health ecosystem, its message at APSPOS 2025 was clear.
“It’s clear that long-term clinical evidence remains essential in validating the effectiveness of the available myopia management solutions," Pillay says.
"The event also reinforced the importance of collaborative care between optometrists and ophthalmologists, as well as the benefits of combination

“By working alongside optometrists, orthoptists, ophthalmologists, and universities, we are shaping a future where we are curbing the myopia epidemic and slowing myopia progression,” Pillay says.
NOTE: References will appear in the online version of this article and are

Ortho-k success starts where most large-cone topographers fall short—at the periphery. While others guess, the smallcone Medmont Meridia™ gives you real corneal data where large lenses land. Get the edge, win the first-fit.
Stop relying on extrapolated data. Book a demo to see what you’re missing: email jason@medmont.com

The Medmont Meridia™ Pro supports myopia management and ocular surface analysis in one seamless workflow. It’s everything you need to expand your care and your practice—in one compact instrument.
Scan to download your free feature guide and learn how the Meridia Pro can work for you >>

60% Slower Myopia Progression: The results of a 2 year randomised clinical trial showed that daily use of MiYOSMART spectacle lenses slowed down myopia progression on average by 60% compared to wearing standard single vision spectacle lenses.*
Backed by 8 Year Data: The extensive eight year follow up study on MiYOSMART spectacle lenses highlights their safety and long-term effectiveness in controlling myopia.**

60% slow down of myopia progression*
Myopia control effect sustained over 8 years**

With childhood myopia on the rise, timely communication about progression and treatment is essential. THOMAS JOHN NADUVIALATH, information science manager at Brien Holden Vision Institute, explains how the organisation’s free, evidence-based tool can help optometrists support early intervention and guide informed discussions with parents and patients

At the completion of this article, the reader should be able to ...
• Effectively communicate predicted myopia progression and treatment benefits using visual aids from the BHVI calculator.
• Integrate International Myopia Institute (IMI) recommendations into clinical practice through measurement and management strategies.
• Promote early intervention and prevention in childhood myopia to reduce long-term visual impairment risks.
ommunicating with parents and patients about the risk of myopia onset in children and the risk of myopia progression up to adulthood is a challenging part of an optometry consultation. It is important to communicate the long-term sight-threatening risks associated with progressive myopia. This would pave the way to discussions about myopia management and current myopia control treatment strategies.
To aid in communication, online resources such as Vision Simulator 1 and myopia infographics2,3 are freely available to explain myopia, the effect of the visual environment on myopia and the classification of myopia control options. In this space, Brien Holden Vision Institute (BHVI) was the first to introduce the online myopia calculator as a communication tool to assist eyecare practitioners to communicate with parents and patients the
extent of myopia progression expected with standard correction and compare it to what could be expected with several myopia control treatment options.
The updated myopia calculator is a tool developed through BHVI’s collaboration with researchers from Shanghai Eye Disease Prevention and Treatment Centre in China, Ulster University in Northern Ireland, and Linnaeus University in Sweden. The estimates shown in the calculator are derived from evidence-based models 4,5 that were built using population and clinical studies and from meta-analysis of randomised clinical trials of myopia control options.
The online Myopia Calculator (https://bhvi.org/ myopia-calculator-resources) includes three tools: 1. A myopia progression calculator
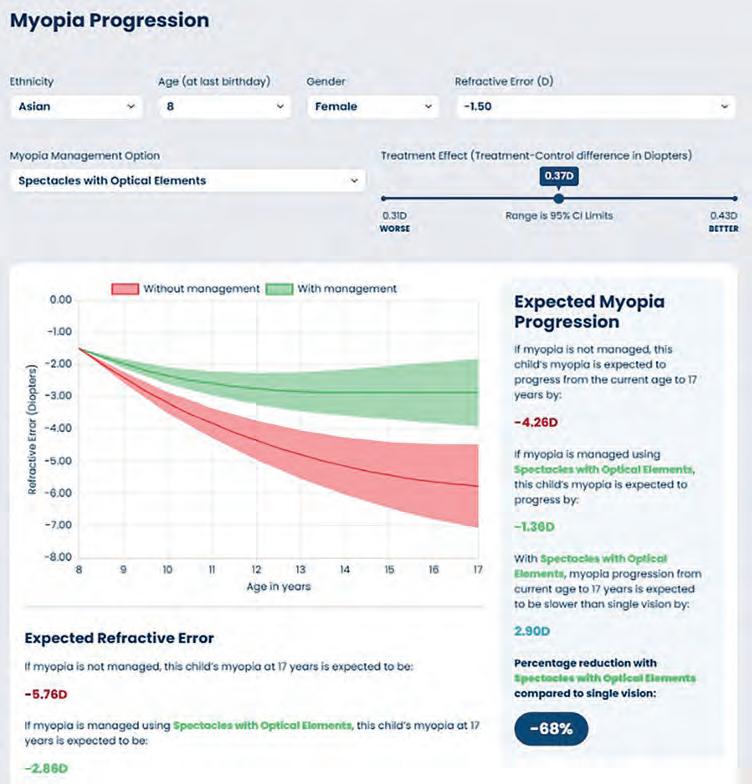
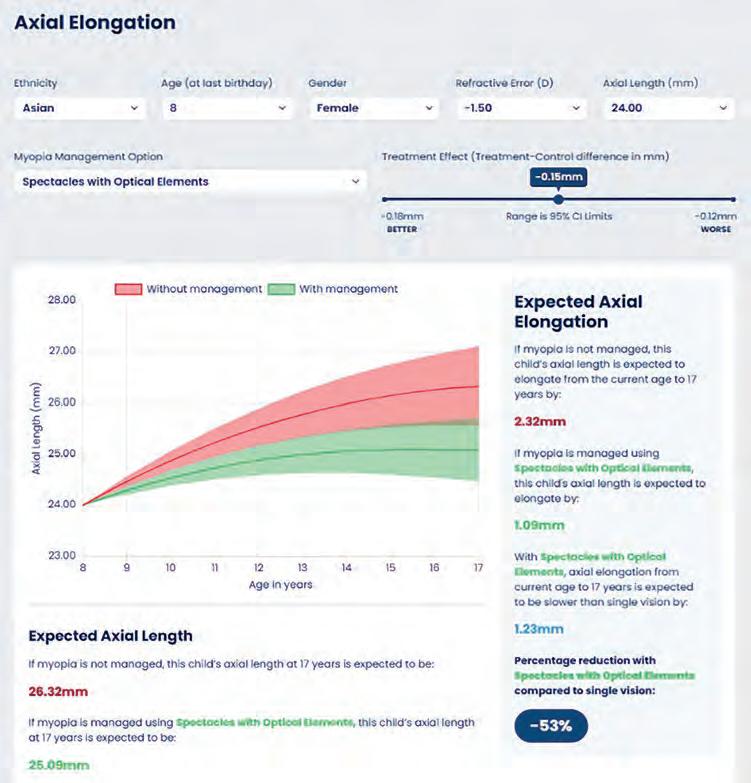
2. An axial elongation calculator
3. A risk of myopia calculator
Each tool is available by selecting its corresponding tile on the webpage. Their practical use is demonstrated in the following three case cenarios.
SCENARIO 1: Myopia progression calculator
Consider a scenario where an optometric consultation takes place with an eight-year-old female of Asian descent presenting with symptoms of blurred vision. Following subjective refraction, the optometrist diagnosed -1.50 D of myopia in the right eye and -1.25 D in the left. The parent wants the child’s myopia corrected with standard single vision spectacles, but the optometrist wants to introduce the concept of myopia control to the parent, rather than just myopia correction. Here, the myopia calculator is a useful tool to aid in this communication.
Open the Myopia Calculator web page and inform the parent that this a tool developed using data on myopic children to explain expected myopia progression in children wearing standard single vision spectacles compared to expected
progression with myopia control options. Select the appropriate options from the drop-down lists based on the child’s demography (ethnic descent, gender and age and the child’s prescription in the more myopic eye). Based on the selected options, a graph is generated as shown in Figure 1.
The red line on the graph – important to be explained first – represents the expected average progression of myopia in dioptres based on selected risk factors if single vison correction is provided to the child. The shaded area around the red line represents the range of uncertainty around the population average provided.
The interpretation of the red line can be communicated in multiple ways to the parent and patient, such as:
1. G iven the child’s Asian background, current age of eight years and current refractive error of -1.50 D, the child’s myopia is typically expected to increase by 4.26 dioptres between the ages of eight and 17 years if the child uses single vision spectacles/contact lenses.
2. G iven the child’s Asian background, current age of eight years and current refractive error of -1.50 D, the child’s myopia is predicted on
average to be -5.76 dioptres at 17 years.
3. The child’s current myopia of -1.50 D, which is classified as low myopia6 is predicted to increase to -5.8 D at the age of 17 years. The average predicted myopia at 17 years being in the -3.0 D to -6.0 D category, is associated with a significantly greater risk of uncorrectable visual impairment in adulthood.7 This risk exponentially increases if high myopia levels (≤-6.0 D) are reached.7
The optometrist can then communicate how to reduce this risk using myopia control treatment options, which are provided as a drop-down list in the calculator. The treatment options reflect generic treatment strategies, not specific brands, for example spectacles with optical elements include spectacles with highly aspherical lenslets (HAL)/defocus incorporated multiple segments (DIMS)/cylindrical annular refractive elements (CARE).
Given the child’s risk of becoming highly myopic in adulthood, let’s consider the scenario where the optometrist would like to discuss spectacles with optical elements as a treatment option. Once the specific treatment option is chosen from the treatment drop-down list, the green line on the graph is updated. For each myopia control treatment, the average efficacy in dioptres is obtained from meta-analysis of randomised clinical trials. Treatment efficacy is set at an average level. The slider beside the treatment option can be moved to the left for a worse-case scenario and right for a best-case scenario. The range of the slider reflects the 95% confidence limits of the treatment efficacy.
The green line on the graph represents the expected average progression of myopia in dioptres for the given child if spectacles with optical elements is used for managing myopia.
The interpretation of the green line can be communicated in multiple ways to the parent and patient, such as:
1. If spectacles with optical elements are chosen for myopia management, then the child’s myopia is typically expected to increase by 1.36 D between the ages of eight and 17 years as opposed to 4.26 D with single vision lenses.
2. If spectacles with optical elements are chosen for myopia management, then myopia progression is expected to slow down by 2.90 D between eight and 17 years and as a percentage this amounts to 68% reduction in progression. Research shows that reducing myopia progression by just one dioptre during childhood can lower the risk of uncorrectable visual impairment by 40%. 8
3. If spectacles with optical elements are chosen for myopia management, then the child’s myopia is typically expected to be -2.86 D at 17 years
compared to -5.76 D with single vision lenes. With myopia control, the predicted average myopia at 17 years, which is between -0.5 D and -3.0 D, is associated with less risk of uncorrectable visual impairment in adulthood than it is with single vision lenses.7
The updated BHVI calculator includes an axial elongation calculator in line with the International Myopia Institute (IMI) recommendations to use both spherical equivalent and axial length measures in the management of myopia in children. 9
Axial length measures are used to monitor myopia progression and risk of long-term complications. In terms of absolute numbers, myopia seems to commence at an axial length of 23.85 mm10 and further stabilises to 25.2-25.5 mm at 16.2-16.5 years in myopic children,11 while axial length of >=26 mm is associated with a significantly greater risk of uncorrectable visual impairment in older ages.7 Axial elongation, the preferred endpoint for assessing myopia progression in clinical research,12 is now gaining momentum in clinical use. Evaluating both axial elongation and myopia progression is helpful when evaluating myopia management options.
The use of the axial elongation calculator is similar to the use of the myopia progression calculator. The current measured axial length in mm is an additional input in the axial elongation calculator.
Consider the previous scenario of an optometric consultation involving a parent and a myopic child, who is an eight-year-old female of Asian descent with -1.50 D in the more myopic eye and a measured axial length of 24 mm. When these values are input, the axial length graph is updated as shown in Figure 2.
Similar to myopia progression, the red line on the graph represents the expected average elongation of axial length in mm based on selected risk factors, and this can be communicated as follows:
1. G iven the child’s Asian background, current age of eight years, current refractive error of -1.50 D and axial length of 24 mm, the child’s eye length is typically expected to increase by 2.32 mm between the ages of eight and 17 years. Though axial elongation is not constant across ages, a rough calculation of 2.32/(17-8) indicates a risk of fast myopic progression (>=0.22 mm/yr).13
2. G iven the child’s Asian background, current age of eight years, current refractive error of -1.50 D and axial length of 24 mm, the child’s a xial length is typically expected to be 26.32 mm at 17 years. Axial length >=26 mm is associated with a significantly greater risk of uncorrectable visual impairment in adulthood.7 Like with the myopia progression calculator, the
optometrist would like to introduce spectacles with optical elements to the parent, given the high risk of complications. The green line on the axial elongation graph represents the expected average elongation of eye length in mm for the given child if spectacles with optical elements is used for managing myopia. This can be communicated in multiple ways including:
1. If spectacles with optical elements are chosen for myopia management, then the child’s axial length is typically expected to increase by 1.09 mm between the ages of eight and 17 years as opposed to 2.32 mm with single vision lenses.
2. If spectacles with optical elements are chosen for myopia management, then elongation of eye length is expected to slow down by 1.23 mm between eight and 17 years and as a percentage this amounts to 53% reduction in elongation. Both myopia progression and axial elongation show a consistent percentage reduction of >50%.
3. If spectacles with optical elements are chosen for myopia management, then the child’s axial length is typically expected to be 25.09 mm at 17 years compared to 26.32 mm with single vision lenses. With myopia management, the predicted average axial length at 17 years, which is <26 mm, is associated with less risk of uncorrectable visual impairment in adulthood.7
The risk of myopia calculator helps to communicate the importance of the preventing or delaying the onset of myopia in children who are not yet myopic. Each year of myopia prevention is more effective than three years of myopia control therapy in lowering the level of myopia that the child reaches in adulthood.14 Identifying children at risk of developing myopia allows for the early introduction of prevention measures and, where appropriate, early intervention strategies. The risk assessment tool is developed using population-based data of non-myopic children followed over time.
Consider a scenario where an optometric consultation takes place with a child, who is a seven-year-old male of Asian descent of non-myopic parents. Subjective refraction revealed 0.25 D in the right eye and 0.25 D in the left. The parent is glad that the child requires no vision correction, but the optometrist realises that the child is at risk of becoming myopic and would therefore like to introduce strategies for myopia prevention and/or early intervention.
Using the risk of myopia calculator, the optometrist can select the appropriate options from the drop-down lists based on the child’s demography (ethnic descent, gender, age, parental myopia and child’s prescription). Based on the selected options, a risk gauge is generated as shown in Figure 3.

Based on the input risk factors, the calculator estimates the probability of becoming myopic within one year as 11% and within two years as 27%. The two-year probability of becoming myopic for this child is presented as a risk value categorised as low, slightly high, moderately high and significantly high. In this situation, the child’s risk of becoming myopic in the next two years is moderately high.
If the scenario is extended to the next year (age=eight years) where the child's refractive error may progress to 0.0 D, then the child’s risk level increases from moderately high at seven years to significantly high at eight years.
The risk gauge can be used to increase awareness of myopia, discuss preventive strategies and early intervention to delay onset.
Of course, these tools were not developed to replace the optometrist’s clinical judgment –they were developed to enhance it. By offering clear, visual projections, the myopia calculator can encourage discussions with parents and reinforce management recommendations. As myopia becomes more common, tools like this can be a valuable addition to the clinician's toolkit, helping eyecare professionals to offer treatments strategies and preventive measures with greater clarity and confidence.
NOTE: References can be found in the online version of this story and are available upon request.

Marking nearly 15 years in Australia, Astellas is a world leader in the development of innovative new medicines, employing more than 17,500 people globally. With a strong foundation in Oncology, Urology, and Transplant, we are now broadening our horizons to include new therapeutic areas such as Ophthalmology.
By combining our expertise in eye biology with cutting-edge technologies, we’re pioneering new approaches including novel cell- and gene-based therapies.
We’re looking forward to meeting with the ophthalmic community and engaging in the latest scientific discussions, as we believe that together we can deliver meaningful value to patients who are urgently waiting.
Contact your local MSL to learn more.

Alex Abalos NSW, ACT
MBBS B.Sc (med) Ophthalmology t. 0439 605 923 e. alex.abalos@astellas.com

Natalie Buckman QLD, WA, NT
MOptom MPH BVisSci GCBus FBCLA AFHEA t. 0401 192 393 e. natalie.buckman@astellas.com

Michelle Waugh VIC, SA, TAS
BOptom, MPhil, PhD, MBA t. 0413 139 151 e. michelle.waugh@astellas.com

From a clearly defined patient journey and same-day visual field testing, to mastering the three-way handover, NICK GIDAS details five soft skills giving practices an edge to their customer service.
n today’s evolving healthcare landscape, staying across the latest developments in clinical care is essential, but it’s often our ‘soft skills’ that are most effective in influencing the health outcomes of our patients. Skills like communication, empathy, adaptability, teamwork and professionalism truly elevate our impact. These skills not only shape how we interact with our patients and colleagues but influence how we grow as individuals within our professions.
As the largest provider of eyecare services in Australia and New Zealand, Specsavers sees the encouraging results of these skills every day, which were recently reinforced as part of a tour of both nations delivering the ‘Trusted Experts’ series.
Here, I’ll share key takeaways from the series, highlighting the often-overlooked skills that can make the difference between good service and truly exceptional care. I will outline learnings from different experiences in the field, focusing on the soft skills that support professional growth, strengthen team dynamics, and enhance the overall patient experience.
Whether you’re an optometrist in the testing room or a dispenser on the shop floor, these insights can help you grow with confidence, purpose and professionalism and most importantly elevate your impact beyond the clinic, leading to improved patient health outcomes.
The reason we all turn up to work every day is to provide a crucial service to our patients – we protect and care for their eye health.
For patients to feel supported, we need to respect their time and attention and provide a clear experience of care that is easily understood. Eye health is personal and can sometimes be anxiety-inducing or stressful for patients. A smooth, thoughtful journey can help the patient feel comfortable, confident, and cared for.
In the Trusted Experts series, we work-shopped opportunities to use our soft skills to make patients feel cared for at different parts of the patient journey. Examples discussed were considering cultural safety and unconscious bias, acknowledging patients as soon as they walk into the store and knowing their name. Taking the time to explain the different
aspects of the eye test – and why each is important – was also identified, along with consideration of any special requirements, for example speaking clearly if a patient has hearing loss.
A key takeaway specific to optometrists was the importance of effectively understanding the lifestyle needs of each patient.
When a prescription is required, it is important the optometrist asks the right questions to ensure an optimal vision solution to meet that patient’s needs.
We invited optometrists to start with an open question to encourage the customer to explain their needs in their own words. After that, it is natural to follow up with more specific questions, which could be a combination of open and closed.
Optometrists could consider ‘The 4 Cs’: clarity, consistency, comfort and convenience to drive these questions.
These are built around a trust framework and prompt the optometrist to explore vision beyond just clarity, making the solutions and benefits relatable to patients.
Finally, as a result from patient feedback data, it was shared that optometrists should refrain from ‘leading’ questions as they may make a customer feel pressured and uncomfortable, as though we are trying to sell them something rather than provide a personalised solution to their vision and lifestyle needs.
In a single appointment, patients are often cared for by multiple professionals. During this, their trust and care is being passed from person-to-person and if this isn’t smooth, patients can feel uncared for, forgotten or like they must repeat themselves.
At Specsavers, an optometrist most commonly receives a patient from a pre-tester and then after the eye test is complete, hands them over to a dispenser who assists them with any visual solutions.
The handover between the optometrist and the dispenser at the end of the eye test has been named the ‘three way handover’ because it requires

"Taking a moment to explain what is being tested – and how important each test is for the optometrist –frames the process and reassures the patient they’re in expert hands."
equal input from the optometrist, dispenser and patient.
The Trusted Experts series showed that an effective three-way handover occurs while still in the testing room and consists of the optometrist introducing the patient to the dispenser, followed by explaining the patient’s management plan and lifestyle requirements. This ensures that vital information from the eye test is being passed over to the dispenser and, as a result, the patient should feel confident in the handover.
To enable this with every patient, effective clinic coordination is vital. Next, depending on the store set up, a process should be agreed upon where dispensers are supported to enter the testing room at the right moment to enable the three-way handover. This could include implementing a buzzer system where optometrists notify a dispenser to come into their room as they’re finishing an eye test. It could also include assigning dispensers to optometrists so everyone outside the testing room is clear on responsibilities.
Immediately after the three-way handover has taken place, the series taught us that it’s important for the dispenser to repeat and affirm the recommendations of the optometrist and highlight the lifestyle benefits discussed earlier as they complete the lens/frame dispense. This, again, makes the patient feel confident in the personalisation of their recommended solution. At Specsavers, we provide regular training sessions on the lens options and products in store so all team members are up-to-date and feel confident in their recommendations.
In the series, we work-shopped the impact of clear communication on patient experience and looked at examples of language that makes patients feel supported and confident.
An example shared was the difference a clear and informed pre-tester can make in setting the tone for the appointment.
Our top three tips for pre-testers were: introduce yourself and know the patient’s name, signpost the different moments throughout the pre-test, clearly explaining what to expect and why each test occurs, and to avoid jargon.
A pre-tester's goal is to capture the scans and information required for the optometrist while also ensuring the patient is as comfortable as possible. Taking a moment to explain what is being tested – and how important each test is for the optometrist – frames the process and reassures the patient they’re in expert hands.
Another example was the importance of clear communication during a glasses collection.
Here, dispensers could start by confirming the type of spectacles and their intended use. When handing over the glasses, it is effective to communicate that the frame fit will be assessed and personalised
before checking vision. This helps manage expectations and prevents unnecessary worry or disappointment if their vision isn’t perfect straight away. We recommended dispensers talk to their customers professionally about what they’re doing while adjusting glasses, explaining what each change will have on their glasses and comfort.
Patients trust us with their time and out of respect we need to do all we can to eliminate wait periods and unnecessary return visits. This can be managed through effective clinic coordination and flexibility.
A common culprit for unnecessary wait times and return visits is when a visual field test is clinically indicated.
Many professionals may feel like it is easier to have the patient return at another time.
However, we have found performing a visual field test straight away in the same appointment helps to optimise the patient’s time in store, while obtaining all relevant clinical information the optometrist requires.
Further to this, we know that a third of patients who require a visual field do not return to have it if the test is not completed the same day. By failing to complete this test, we are not prioritising our patient’s eye health and risk missing early signs of eye conditions or potential vision loss.
Effective store coordination will improve patient experiences as well as create a happier work environment for your team. Specsavers uses a system which allows us to visualise the customer journey using live data. This allows the implementation of clinic changes, ensuring we are running a smooth clinic flow.
As Australia’s most trusted eyecare organisation,1 Specsavers has spent a lot of time strengthening and empowering our professionals to lead with integrity and deliver service that goes beyond expectations, no matter where they sit in the patient journey.
While they may seem simple, we hope these takeaways are a helpful reminder of what should be implemented everyday in your profession. By investing time and energy into practising these essential soft skills, we don’t just enhance performance, we contribute to a culture of care, consistency, and excellence.
REFERENCE: 1. S pecsavers ANZ crowned ‘most trusted’ optometry brand for six years running, 4 June 2025: https://www.insightnews.com.au/specsavers-anz-crowned-most-trusted-optometry-brand-forsix-years-running/ ABOUT THE AUTHOR: Nick Gidas is a qualified optometrist and head of clinical performance at Specsavers ANZ where he leads a team of clinical performance consultants supporting stores across Australia and New Zealand.
Alcon Vision Suite represents Alcon’s seamless ecosystem designed to power the eye care surgeon’s practice by bringing together the industry’s most comprehensive operating room suite with clinical diagnostics, digital solutions, plus our first-class training and services.1
Complete product offering
Seamlessly Connected from clinic to OR By your side to deliver excellent Care

ARGOS® Biometer
Biometry and surgical planning integrated with your health record for empowered decisions and confident surgery2
Digital Marker M
Image guidance overlays working with most microscope brands for surgical precision3
LuxOR® Revalia™
Advanced microscope displaying image guidance overlays and phaco parameters4
Contact your Alcon representative today to discuss your ophthalmic equipment needs.
*Based on bench testing when compared with Constellation® and Centurion® Vision Systems.
NGENUITY® 3D Visualisation System
Enables true 3D digital visualisation working with most common microscope brands5
VCS
Superior efficiency for Vitreoretinal and Cataract Surgery*6-9 designed for current and future integration with Alcon’s ecosystem of products, digital innovations and services10,11
References: 1. Market Scope. 2020 Ophthalmic Diagnostic Equipment Report: A Global Analysis for 2019 to 2025. 2. ARGOS® Biometer Operator’s Manual, 2019. 3. VERION® Digital Marker M Operator’s Manual. 2020. 4. LuxOR® Revalia™ (LX3 LED) Ophthalmic Microscope Operator’s Manual, 2019. 5. NGENUITY® 3D Visualization System Operator’s Manual 2021 (Version 1.4). 6. Alcon Data on File, 2024; [REF-24644]. 7. Alcon Data on File, 2024; [REF-24615]. 8. Alcon Data on File, 2024; [REF-24576]. 9. Alcon Data on File, 2024; [REF-24379]. 10. UNITY™ VCS and CS user Manual, 2024. 11. UNITY™ Phaco Handpiece. Directions for Use. Please refer to relevant product direction for use for list of indications, contraindications and warnings. For healthcare professionals only.
Scan QR code to register for the latest Alcon news and communications.
At Specsavers, your future looks bright. Whether you’re fresh out of uni or ready to take your next step we’re here to to help you grow with mentorship, clinical development, and career pathways. Ready to take the next step? Your future starts here. Take your next step at spectrum-anz.com/ careers-at-specsavers



Wide-angle non-contact visualisation changed the game for vitreoretinal surgeons globally. Two surgeons discuss how two manufacturer-agnostic innovations from OCULUS have set new standards in their highly complex work.
Knowing what he knows now, Dr Kazuhito Yoneda reflects in quiet amazement on how retinal surgeries were performed early in his career. A prism or indirect viewing contact lenses – held steady by hand – provided the portal into the delicate, high-stakes world of his vitreoretinal procedures.
At the time, this was the norm. But even then, the limitations were obvious.
“When I started out using prism lenses, this was a very narrow viewing system. We then moved to other contact lens systems, which offered an improved field of view but because it needed to be held steady by hand, it was challenging when I needed to operate bimanually with both hands,” he says.
“If I wasn’t holding it myself, I had to depend on an assistant to hold it steady, however that wasn’t always reliable and it was difficult to achieve consistent visualisation.”
Stereopsis reduction, fogging and smudging are other issues that could cause interruptions for Dr Yoneda. Eventually, other visualisation technology came but fell out of favour due to its bulkiness, obstructed surgical view, or low image quality.
It was the complexity of vitreoretinal surgery that first attracted Dr Yoneda to the subspecialty more than 25 years ago. But ironically, it wasn’t until he encountered technology from German ophthalmic device manufacturer OCULUS that he fully realised just how limiting his earlier tools had been –particularly in tackling challenging cases like giant retinal tears, proliferative diabetic retinopathy (PDR), and proliferative vitreoretinopathy (PVR).
That realisation occurred 10 years ago, and still rings true today.
The OCULUS’ BIOM 5 wide-angle non-contact viewing system, used in conjunction with the company’s WiFi (wide-field) HD lens, is the linchpin in his vitreoretinal surgery setup at Sakura Eye Clinic group and Subarukai Eye Center.
It’s all seamlessly integrated with his Leica Proveo 8 microscope, including its inverter to correctly orientate the surgeon’s view, with the surgery then displayed on his Alcon NGENUITY 3D heads-up system. Three components from three manufacturers working harmoniously. When it arrived in 1985, OCULUS says its BIOM technology altered the vitreoretinal landscape, reshaping fundus viewing by continuously incorporating the principle of indirect ophthalmoscopy in the operating microscope. It allowed more surgeons to branch out into the field. Crucially, the BIOM 5 is aligned coaxially with the operating microscope, and during extraocular phases of surgery it is swung out of the observation beam while the inverting action of the OCULUS SDI inverter is neutralised. Surgeons can then pair the BIOM 5 with various lens types, with the most popular being the WiFi HD lens – also known as the gold lens – offering high resolution and a wide field of view across 60-130 degrees.
Combined, the system has been developed for precisely the type of cases Dr Yoneda manages. He describes its integration with the Leica Proveo 8 microscope as “streamlined and intuitive”, enabling synchronised
Together, the BIOM 5 and WiFi HD lens are a powerful visualisation tool for vitreoretinal surgeons.

focusing via the microscope’s native foot pedal – a feature he now considers indispensable.
“During extraocular phases of surgery the built-in inverter of the Proveo 8 integrates seamlessly with the BIOM 5,” he says.
“The swing-out function operates smoothly and naturally, and the synchronised focusing system operated by the native foot pedal allows effortless focus adjustment, enhancing surgical flow without disrupting the procedure.”
Dr Yoneda also highlights the physical improvements the system has brought to his work. Performing five to 10 retinal surgeries during each operating session can leave him physically strained, but the efficiencies brought about by BIOM 5 paired with the NGENUITY 3D display system has significantly improved ergonomics in the operating theatre.
“This has helped reduce fatigue and improved my concentration,” he says.
But the core value, he says, lies in the image quality and field of view.
Using the WiFi HD lens on the BIOM 5, the system offers a wide viewing angle allowing him to visualise both the macula and far periphery without the need to switch lens types.
“I can use the WiFi HD lens in every case,” says Dr Yoneda, who opts for the disposable version of this lens with advantages in sterility, reduced contamination risk, and consistent optical clarity – even though the reusable WiFi HD lens is the most commonly selected option among surgeons.
“It gives me the confidence to tackle complex conditions without interruption. Retinal detachments, PDR and PVR can have peripheral and posterior elements to address at the same time. But when I use the WiFi HD lens, we can see a very clear peripheral view and, at the same time, very clear macular view.”
In PDR cases, this is where fellow Japanese surgeon Dr Shunsuke Osawa agrees the BIOM 5 and WiFi HD lens stand out.
He uses an identical setup to Dr Yoneda, the only difference being the use of a contact lens to protect the cornea and maintain a smooth corneal surface (this lens is not for magnification). For macular work, with the WiFi


HD and BIOM 5 system, he uses the zoom function of the microscope to achieve a 60-degree macular view without the need to switch to a separate 60-degree lens. He recommends a 60-edegree lens when a more stereoscopic view is required.
“In PDR, it allows me to perform a posterior vitreous detachment as far out as the equator, and then accurately visualise and dissect proliferative membranes near the vascular arcades using the 60D lens under excellent stereopsis,” he says, performing surgeries at MIE Eye Clinic.
“In cases of giant retinal tears, retinal slippage during reattachment is a major concern. The seamless operability of the BIOM 5 allows for smooth surgical manoeuvres, while the excellent clarity provided by the WiFi HD lens ensures precise subretinal fluid drainage, helping to prevent retinal slippage.”
In many ways, OCULUS’ contributions helped open up the field of vitreoretinal surgery.
That’s according to regional director for Asia, Mr Richard White, who
says the company’s journey into the subspecialty began when Mr Rainer Kirchhübel – CEO of the OCULUS family enterprise since 1981 – began working with surgeons to develop the SDI inverter.
“In the beginning, very few surgeons in any country were doing vitreoretinal surgery,” he explains. “It was difficult – hand-eye coordination was hard, and it was tough to truly visualise the posterior segment.”
The original SDI inverter system helped orientate the surgeon’s hand movements with what they would expect to see. In other words, when their hand goes up, it also goes up through their oculars.
“Innovations like this helped to increase the number of retinal surgeons 10-15 fold,” White says.
“And with more great surgeons being able to see and understand the problems at a deeper level, they wanted to start exploring more surgical capabilities. They asked, ‘right now we're only concentrating on 30 degrees with a contact lens, but what about if we can start doing surgery more in the peripheral areas of the eye?’.”
Working closely with German surgeon Prof Manfred Spitznas, OCULUS developed the BIOM system.
“It really revolutionised the retinal subspecialty,” White says. “The SDI let more people get involved. The BIOM helped them do more surgeries and treat more patients.”
Asked what continues to keep OCULUS at the forefront of this field, White says all roads lead to the company’s rich heritage in optics. The multi-lens trial frame – which overcame complicated wavefront issues and distortions brought about by stacking of lenses – is an example of its grounding in optics.
White also believes OCULUS’s smaller size enables a nimble, collaborative approach to innovation. “We’re just over 500 people globally. If a surgeon has an idea, it can reach our CEO in a day, depending on the strength of the idea. That direct connection with the field helps us stay aligned with what surgeons really need.”
The WiFi HD lens is a case in point, overcoming the need to switch out lenses during retina surgery.
“It allows the surgeon to see from 60 to 130 degrees – and everything in between, which all comes into focus with just the foot pedal,” White explains.
“That’s unique to us – all other lens options are set-degree. Around 95% of our retinal lens orders are for this lens.”
Compatibility and workflow flexibility are also key. The BIOM system can be adapted to fit virtually any microscope on the market, partnering with at least eight of the biggest names in ophthalmic manufacturing.
Plus, with growing interest in disposable products, OCULUS offers single-use options for emergency use or infection control, particularly valuable when sterilisation delays are impractical or when there’s a blood pathogen concern like HIV.
“With really solid IP, coupled with a grassroots connection to the industry,” White adds, “we're able to keep on top of what the industry wants and needs and set the future direction in this space.”
Reflecting on how those needs have evolved, Dr Yoneda sees the BIOM 5 and WiFi HD lens not only as an upgrade, but a shift in how he approaches retinal surgery.
“It’s changed how I work. I’m faster, more comfortable, and more confident. Most importantly, I can perform some of the most difficult cases in ophthalmology and give my patients the best treatment and the best chance of recovery,” he says.
For Dr Osawa, the most impressive features of the BIOM 5 system are its high image resolution – even during fluid-air exchange – widefield angle view, compatibility with the Proveo 8 microscope, and integration with his Alcon NGENUITY 3D heads-up display.
“Above all, the BIOM 5 enables high-resolution, panoramic visualisation of the entire globe, which contributes to safer and more efficient surgeries across all cases,” he says, “especially those that are complex or delicate.”

Unleash your full potential with OPSM. With our unwavering support and experience, you have the freedom to pursue an area of expertise and practice full-scope optometry. Choose the field you love and thrive with OPSM.
ACCELERATE YOUR CAREER ASPIRATIONS WITH OPSM. Visit opsm.com.au/careers today.


The event was a record-setting four days of colour, conga lines and sometimes comedy. But beyond the costumes there was some serious learning going on. Insight offers a flavour of this often crazy conference.
AUSCRS 2025 began with an ending.
But in the four days that followed, there was enough evidence that not only did the event have an exciting future as Australia’s premier gathering for cataract and refractive surgeons, the sector itself was ready for an exciting future of innovation in technique and technology – much of which was on display in the trade exhibits surrounding the main stage and arena.
That ending was the announcement that Australian Society of Cataract and Refractive Surgeons (AUSCRS) co-president Professor Gerard Sutton would be stepping down after three years at the helm with Dr Jacqueline Beltz.
After entertainment from Gamilaraay man Mitch Tambo and his wife LeLe, and a video promoting host city Darwin and the Northern Territory, Prof Sutton and Dr Beltz entered the opening evening dressed as fair-dinkum Aussie tour guides.
Driving a battered 4WD to the main stage.
Crikey. Strewth. AUSCRS was up and running in typical style.
Three years ago, the pair took over the co-presidency roles from Professor Graham Barrett and Dr Rick Wolfe, who founded AUSCRS in the mid-1990s. Dr Beltz will now be the society’s president, with Dr Andrea Ang, a consultant ophthalmologist at Lions Eye Institute in Western Australia, named as vice-president.
“It's been an absolute ride,” Dr Beltz told the audience of nearly 220 eye surgeons, advanced trainees and support staff about her time with Prof Sutton.
“We've shared so many memorable moments up here on stage, but it's behind the scenes, plotting, planning, laughing that I treasure the most.
“We're going to say thank you a few times throughout this meeting, but I want to take every chance I can to say it again now.
"So Gerard, it's been a blast. Thank you very much.”
That ending suitably acknowledged, the event, famous in global ophthalmology circles for its relaxed staging, themes and costumes, kicked off with the Barrett/Wolfe lecture delivered by Professor Michael Knorz, medical director of the FreeVis LASIK Center Mannheim and internationally recognised as one of the leading experts in the field of refractive and cataract surgery.
He talked about the past and present of presbyopia-correcting intraocular lenses. But it was his views about the future that would have gained most attention.
Prof Knorz has been involved in trials and analysis of a number of IOLs and told those assembled that he was particularly impressed at the technology and rise of extended depth of focus (EDOF) IOLs.
“Patients can expect excellent distance vision and quick intermediate vision,” he said.
“They can expect few side effects at night.”
Although, he conceded that it was more likely that patients would need glasses for reading or other near-focus tasks.
Mulifocals also allowed for good distance and intermediate vision, with patients less likely to need glasses at all.
“But optical side effects [glare, halos, especially at night] are much lower, much less in EDOF IOLs,” he said, “whereas multifocal IOLs have significant side effects.”
He liked to take his time with patients, explaining the compromises they would have with different IOLs.
“Patients will make this choice, and it's really important to let them know that there is a price, but undersell and over-deliver.”
He highlighted the rise of new technology to help eye surgeons do that, including an Austrian simulator that let ophthalmologists and patients

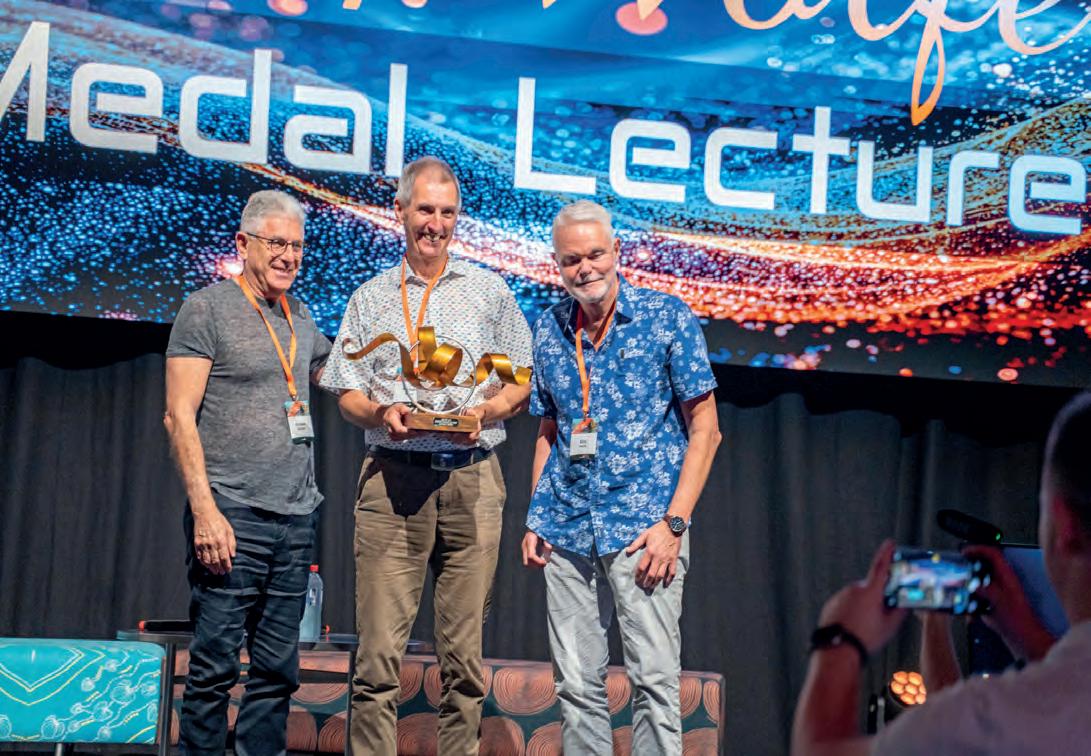

ABOVE, L to R: Prof Michael Knorz (centre) delivered the Barrett/Wolfe lecture. He’s thanked by Prof Graham Barrett (left) and Dr Rick Wolfe; Part cos-play, part conference, presenters dressed up in various costumes during the event; Presenters were often questioned by members of the audience about techniques and technology used during surgery or treatment.
experience what their vision would be like using various lenses.
Prof Knorz believes that EDOFs will become the standard of care in surgery, certainly in comparison with monofocals.
“Their benefits far outweigh the small side effects.”
The future, he says, is about “adjustability”, whether that is development of the light adjustable lens that could be altered post-surgery or accommodating lenses that worked more with the eye’s muscles.
Another innovation to watch was a lens that relied on contraction of the ciliary muscle to alter the shape of the lens for “absolute accommodation”.
“I believe that the future will be some accommodating design.”
The future was very much on the minds of other presenters at AUSCRS.
Whether they wore mediaeval costumes for a Game of Thrones-themed exploration of challenging cases, or donned hoverboards for the Back to the Future-foray into cataract surgical outcomes, the discussion was always forward focused.
Leading ophthalmic experts, including Dr David Lockington, consultant ophthalmologist at Tennent Institute of Ophthalmology, in Glasgow, and Dr Matthew Rauen, a board-certified and fellowship-trained cornea and refractive surgery specialist in the US, talked about some of their most difficult and stressful surgical cases, including sometimes confronting videos.
They then faced up to often challenging discussion and inquiry about what they might have done or considered if they had the chance again.
It was not quite the Red Wedding (a pivotal and shocking massacre in the Game of Thrones), but upcoming presenters would have been aware that Winter was coming and the White Walkers were not going to take any prisoners.
It was the same as Dr Rauen again stood up, this time dressed as Dr Emmett Brown from Back to the Future, white hair suitably shocked and upstanding for the electrically charged topic of interoperative intraocular pressures in cataract surgery.
He promoted the use of lower pressures during surgery to help keep the surgical environment more stable.
Using video and other resources, he demonstrated that introducing

a phaco probe with an infusion pressure of 65 mmHg could make the patient uncomfortable and the eye unnecessarily tense and hyperinflated. “But watch when we drop the infusion pressure to 28 mmHg – we see relaxation of the intraocular tissues and a return to a more natural anatomic state.
“It just shows us when we operate at higher infusion pressures, we are distorting the ocular anatomy,” he told the audience. “There are many groups throughout the world looking at this.”
There is also less leakage from incisions when surgery is performed using lower infusion pressures. This leads to less unnecessary fluid travelling through the eye during routine cases.
“So the question is, with modern technology and advanced fluidic systems, why would we use such high infusion pressures?” Dr Rauen asked.
“When it comes to corneal endothelial cell loss and intraoperative patient comfort, there is a growing body of evidence showing benefits of lower infusion pressures.”
“Where we are going . . . we don’t need a high pressure.”
But it was not just the speakers putting out those questions over the three days of presentations for surgeons and their support staff. There


were plenty in return that pushed many to the edge of their comfort zones and often beyond.
That was evident in numerous other sessions, including those looking at head-to-head comparisons of different IOLs, the future of lenses and cataract and refractive surgery, the use of AI in surgical education, and Controversy Corner, the “masked debate” on “hard calls and hot takes” in ophthalmology.
That sometimes uncomfortable challenge to push and improve, albeit delivered by a person possibly in plastic chain mail and holding a fake sword, is what makes AUSCRS the premier industry event in Asia-Pacific, says Prof Sutton.
“AUSCRS 2025 was another successful conference,” he says.
“Apart from the usual local ophthalmologists contributing with knowledge and passion, I think the international speakers were particularly strong this year.
"In particular, I enjoyed the lectures from Dr Cathleen McCabe and Dr Sri Ganesh.”
He believes he is leaving the role of co-president with AUSCRS in a healthy position. He will remain on its committee.
“It was always going to be a tough task taking over from Graham Barett and Rick Wolfe after 25 years.”
COVID had been challenging and put financial pressure on AUSCRS.
“We were determined to ensure that that was addressed and AUSCRS is now in its strongest financial position ever for further growth and we have increased the number of sponsors.”
The 2025 event featured a record six gold and 20 silver sponsors, on top of five platinum sponsors.
There were 150 company representatives as well in the many exhibits and booths that ringed the main stage and arena.
And far from being put off by the sometimes challenging debate and discussion, there was a “continual stream of the best international experts in ophthalmology pleading to be invited each year”, says Prof Sutton.
He thanked Dr Beltz, executive officer Ms Jenny Boden and others at AUSCRS for their support, as well as former co-president Prof Barrett and Associate Professor Michael Lawless, “who will always be my role model of the professional surgeon”.
Dr Beltz said feedback had been “overwhelmingly positive, with many calling it the best AUSCRS meeting they’ve ever attended, even while recovering from middle-of-the-night flights home from Darwin”.
She said the opening ceremony featuring Tambo and his wife LeLe, who performed You're the Voice in both Gamilaraay and English, was “an unforgettable, emotional moment that left me with tears in my eyes, even during rehearsal”.
The drive into the arena took her back to her youth, “the 4WD reminiscent of the one I learned to drive in during the ‘90s”.
But it was thoughts of the future that had her most excited.
AUSCRS 2025 had featured “engaging, thought-provoking discussions throughout the program, from topics like When is a cataract not a cataract? to forward-thinking sessions on IOL choices, education strategies, and laser technologies”.
There was record support from sponsors, and strong, ongoing engagement from delegates, “showing the continued momentum and relevance of AUSCRS”.
“As Gerard steps down and Andrea Ang steps into a leadership role, I’m incredibly excited about the future of AUSCRS and the growing AUSCRS family,” Dr Beltz said. “Some people are already trying to book their accommodation for Sunshine Coast 2026!”
Get ready for the extra plus in your O.R.

Experience fundus viewing at its best! As the name suggests, the new BIOM® ready+ offers quite a few plus points:
• Adjustable lens retainer To optimally centre the fundus image
• Newly designed pivot joint For even greater mechanical stability
• Ideal for 3D Heads-up systems
Its optic never shows the slightest trace of use

In an upcoming Sydney boot camp, the national network will be able to celebrate its 25th anniversary of silver service, and plan for the next quarter of a century and beyond.
This September, Eyecare Plus members from across Australia will come together in Sydney for their biennial Boot Camp – to sharpen their business and clinical processes, and to celebrate the major milestone of 25 years of Eyecare Plus.
What began as a bold idea in the late ’90s, and was brought to life in the year 2000 by founders Mr Tony and Ms Vicki Hanks, with founding directors Mr Nick Hansen and Mr Ray Fortescue, has grown into Australia’s largest branded group of independent optometrists.
More than a buying group, Eyecare Plus has become a trusted name, a collegiate community, and for many, a professional family.
The founding mission was to create a stronger platform for independent optometrists at a time when the industry was changing and bigger players were creating greater competition.
Chain stores and retail-driven models were on their way from overseas.
Eyecare Plus gave independents the opportunity to refocus on clinical care and greater patient service.
“We could see the writing on the wall,” recalls Hansen, a founding director and partner at Hansen’s Eyecare Plus in Orange, NSW.
“We knew that if independents didn’t find a way to work together, we’d be picked off one by one. The vision was to create a group where optometrists could maintain their independence, their values, and still compete with the growing corporate giants.”
That vision proved not only right but well ahead of its time.
Today, Eyecare Plus includes many of the most respected and successful independent practices in Australia.
Its model offers the best of both worlds: local ownership and clinical autonomy, supported by a national brand, marketing resources, business
systems, and a peer network built on trust and shared purpose.
For Mr Martin Gregory, chairman of Eyecare Plus and partner in a large regional practice in Wagga Wagga, NSW, that business foundation is a critical part of the story.
“This isn’t just a feel-good story,” Gregory says. “It’s a great business story. We’ve helped practices grow and thrive against corporate competition, largely by bringing the best practices together to share trade secrets and strategise.”
Gregory, an optical dispenser by trade with an MBA and deep experience in practice management, says what makes Eyecare Plus unique is its commitment to supporting practices without ever controlling them.
“We’re not a franchise,” he says. “We don’t take a cut of profit, and we don’t tell members what to stock or how to treat their patients. We provide opportunities to share knowledge, systems, training, marketing, and a framework for success – but the decisions stay with the practice owner.
“That’s the power of independence.”
That spirit of autonomy within community is a key reason Eyecare Plus has grown such a loyal following among established practices, and also among the next generation of leaders.
Ms Lara Foster, owner of Eyecare Plus Moss Vale and a current board director, represents that next generation.
She joined the network in 2010 and says the impact on her practice and her professional life has been significant.
“Eyecare Plus and my fellow members have been critical to my development as a practice owner,” Foster says.
“The vision was to create a group where optometrists could maintain their independence, their values, and still compete with the growing corporate giants.”
ensures members aren’t competing with each other, which encourages open, honest discussion and problem-solving across the group.
It’s a model that has stood the test of time, and now, 25 years in, the results speak for themselves.
Eyecare Plus Boot Camp in Sydney this September will be more than a workshop and training session. It will be a celebration of everything the group has built – together.
Founders, as well as current and now retired members, will return for the occasion. There will be practical workshops, strategic planning sessions, and, as always, plenty of social opportunities and shared stories.
“You’re not just getting access to marketing or buying power, you’re getting mentorship, friendships, and a support network that feels like family.

Nick Hansen Eyecare
"It’s an environment where you can grow without losing who you are.” Foster says that for young optometrists considering their career path, independent practice within a group like Eyecare Plus offers a powerful alternative to the salaried, target-driven world of corporate optometry.
“You get the freedom to practise the way you believe is right,” she says. “And you get to build something that’s yours. That’s incredibly rewarding.”
That message resonates now more than ever, as recent industry research has highlighted growing dissatisfaction among young optometrists, many of whom report feeling disillusioned with high-pressure sales environments and limited clinical autonomy.
At Eyecare Plus, the culture is different. There’s a strong emphasis on peer-to-peer knowledge sharing, professional development, and collegiate collaboration. The network’s model of territory protection
“Some people think independence means going it alone,” says Hansen. “But the truth is, we’re stronger together. That was true 25 years ago when we started, and it’s even more true today.”
Gregory agrees: “We’ve created something rare – a national brand that respects local identity. A support system that enables growth without compromising values. That’s not easy to build, and it’s even harder to sustain. But we’ve done it and we’re proud of it.”
Looking ahead, Eyecare Plus is committed to remaining at the forefront of independent optometry, by bringing leading optometrists together through new initiatives like the Entrepreneurs Club, expanding education and training, and welcoming the next generation of practice owners into the fold.
As Foster puts it: “It’s about legacy and opportunity. Honouring where we’ve come from and making sure we’re ready for where we’re going next.”
And for all those who will gather in Sydney to celebrate, the message is clear: Eyecare Plus was never just about resisting change. It was about creating something better.

Much of the work done by Vision Australia’s staff involves helping others gain what might seem like minor wins in their lives, but it all contributes to an often profound impact on those people and a bigger victory for the country.
The question is a simple one: What does a typical day look like for you?
A simple question but Ms Marg Harvey’s answer gives a valuable insight into not only her role and contribution as an orientation and mobility (O&M) specialist at Vision Australia, but also the vital role the organisation plays in their clients’ lives and their contributions to the country and economy.

Harvey is a former teacher who now works with people aged practically from zero to 100 who are blind or have low vision.
As an O&M specialist she not only helps them with all aspects of their mobility, from walking around in the community to catching public transport and getting prepared for dog mobility and other aids, she also does assessments of environments at schools and other public facilities, workplaces, and advocates around accessibility improvements such as installation of traffic lights, road crossings and other infrastructure.
But what does a typical day look like?
“I've been to see a student at a school,” she says. “He’s transitioning to high school next year. And he's also a recent arrival in Australia, from Afghanistan. So complex vision loss, very complex health issues.
“He was getting around really well at school, has mapped it out despite his really low vision. So my plan there is for him to learn to use a long cane as an aid that will support his low vision, be a bit safer and also help the community understand something about him.
“This afternoon I'm seeing a very independent person who is blind. He works hard to be independent, but he needs training to navigate a massive road crossing so he can walk to the hairdressers to get his hair cut.
“But the funniest one is . . . I work with this little lad who's two, and he is totally blind as well. It was raining here in Dandenong [Victoria] but when I got there, he was already outside, fully dressed in his little waterproof pants and his raincoat, and we spent the whole session out in the rain.
“So I just put my raincoat on and we just spent the whole time floating things down the gutters, tapping the water to see how deep it was

“You want people to have the same opportunities as every other person. That's how I feel about it. That's how we should be.”
Marg Harvey Vision Australia
and really allowing him to develop his skills and understanding of his environment.”
You can take the woman out of teaching but . . .
If Harvey’s role gives blind and low vision people practical skills and knowledge to help navigate their sometimes new and challenging world, colleague Ms Debbie Loke and her team play an important role in building confidence and a safe bridge to that sometimes scary new land.
Loke, a trained orthoptist, is Vision Australia’s national social support and wellbeing lead.
The organisation deals with people at every stage of their journey of vision loss, says Loke.
“In Australia, it takes adults an average of five years to seek support for vision loss,” she says. “Sometimes this can be a fear of confronting a vision condition; in many cases it’s simply not knowing who to turn to or when.”
The social support and wellbeing team help to ease that transition.
There are a number of programs, groups and funded pathways to help blind and low-vision people connect not only with others facing similar challenges but also groups to help them regain confidence, and colleagues like Harvey who can assist with navigating daily life.
“We have a well-being check-in and chat program that’s targeted to our clients who are 65 plus and above. It’s a one-on-one Telehealth program that supports older clients and their families in adjusting to vision loss.
“There's another team that runs our quality living group program, a forum and safe space for clients in a similar age or stage, where they can get together and talk about their story, learn strategies and tips and help each other out.”
Other groups in recreational programs get together around certain activities, such as craft and woodwork.
Loke believes her former ophthalmic colleagues can also play an important role by continuing to refer people to the services available at Vision Australia.
“Vision Australia has the services and the supports in place that can provide that wraparound service to that client who might be going through a particular stage of their vision-loss diagnosis,” she says.
For Harvey, the reason for doing that is simple.
“You want people to have the same opportunities as every other person. That's how I feel about it.
“That's how we should be.”




























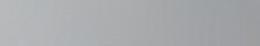






Much of the world is coming to terms with the rise of myopia and the many new products and therapies to help control it, but in some less-developed nations, such things are seemingly out of reach.
magine this: You’re five years old, just starting school, eager to learn and excited to play but you can’t make out the words on the board and you’re having to rely on your classmates for help.
Your confidence fades and you begin to withdraw.
But education equals opportunity and opportunity starts with vision.
In Australia and New Zealand, access to eyecare is something many of us take for granted. A simple eye exam and a pair of glasses can drastically improve quality-of-life, especially for those with low myopia.
With the global rise in myopia, there is an increasing focus on myopia-control strategies, including specially designed lenses aimed at slowing progression.
WAVING TO THEIR FRIENDS AND FEELING TRANSFORMED."
Meanwhile, in developing countries, the need is far more basic: millions still live with uncorrected myopia. There, it’s not about advanced solutions, it’s about having any solution at all.

While some parts of the world focus on controlling the future of myopia, others are still struggling to meet the most fundamental vision needs.
In July 2025, Optical Dispensers Australia (ODA) spent five days visiting primary schools and villages in Fiji as part of their annual ODA Fiji Outreach Project. I was fortunate to be one of the volunteers on a team made up of two optometrists and 12 optical dispensers.
We arrived equipped with vision screening tools and hundreds of donated pre-made spectacles to provide eye tests and dispense glasses to those in need.
Many of the children we examined in Fiji required basic correction just to see the classroom board. Sadly, some had previously been labelled as having learning disabilities or behavioural problems due to their inability to read from the board. The possibility of a refractive error was not even considered by teachers or families.
We saw many shy children walk in, avoiding eye contact. After being fitted with glasses, they would walk out grinning, waving to their friends and feeling transformed by the ability to see clearly.
The spectacles revealed a world of opportunity. For some, this simple intervention reshaped their entire future. Here is just one story of many that stood
out that we were honoured to witness: A 13-year-old boy who had realised his vision was poor compared to that of his friends came straight from school when he heard ODA was in the village.
After his screening, we gave him a pair of -2.00D spectacles. He sat quietly, looking around in awe as he took in the birds, the leaves, the other children. He had never seen the world in such clarity.
With limited resources in Fiji, something as basic as a pair of prescription glasses becomes a powerful first step toward a brighter, more confident life.
In contrast, Australia and New Zealand offer a wide range of advanced myopia management options. These include contact lenses, myopia control lenses, atropine eye drops, ortho-k and even red-light therapy.
The opportunities to manage this condition are extensive. Dispensing to a myopic child isn’t just part of your job, it’s a responsibility. Each child is different, and recommendations should be tailored to their needs, lifestyle, and age.
It’s a privilege to be able to provide the right tools and guidance.
Among the most common options available today are advanced myopia control lenses, such as HOYA’s MiYOSMART. These lenses use special
technology that corrects central vision while a surrounding honeycomb-like treatment zone slows the eye’s growth.
Clinical studies show that children wearing MiYOSMART lenses experience up to 60% less myopia progression compared to those wearing standard single vision lenses.
For these lenses to be effective, accuracy in dispensing is crucial. Optical dispensers must carefully select frames and ensure precise measurements for proper function and comfortable wear.
In addition to providing solutions, we also need to raise awareness. Eyecare professionals must educate families about the signs of myopia, which include:
• Squinting
• Sitting close to the TV
• Holding books closely
• Trouble seeing distant objects
• Frequent headaches
• Excessive eye rubbing or blinking. Early intervention is key. The sooner myopia is detected and managed, the better the outcomes for the child.
Every young eye presents a chance to change a life.

Vision assessments for stroke survivors need to go beyond standard checks and involve neuro-orthoptists, says Dr MICHELLE COURTNEY-HARRIS.

COURTNEY-HARRIS
"NEUROORTHOPTISTS APPLY THEIR SPECIALISED EXPERTISE TO ASSESS AND DIAGNOSE COMPLEX VISUAL DISTURBANCES IN PATIENTS WITH ACQUIRED BRAIN INJURIES, SUCH AS STROKE.
Vision impairment can be a debilitating consequence of stroke.1-3 If you couple that with pre-existing ocular conditions with pathological changes contributing to vision impairment, then standard rehabilitation programs need modifications to ensure optimum patient responses and outcomes without hinderance.
During the acute inpatient phase of the stroke journey an inclusive vision assessment by an eyecare practitioner, such as an orthoptist, is key for information dissemination among the stroke care team.
Research indicates that many stroke survivors do not receive timely or adequate assessment of their visual function following stroke, resulting in vision impairments that are often unrecognised, untreated or managed too late. 3,4
Comprehensive vision assessment in stroke survivors should extend beyond functional deficits such as visual field (VF) loss or neglect. It must also include evaluation of visual acuity, refractive error, and pre-existing ocular conditions to inform clinical decisions regarding overall visual status, the need for ongoing treatment and the urgency for referral.
Furthermore, communication and mobility challenges common among stroke survivors can complicate the examination process, necessitating a modified and patient-centred approach to visual assessment.
Neuro-orthoptists apply their specialised expertise to assess and diagnose complex visual disturbances in patients with acquired brain injuries, such as stroke.
In non-verbal patients, objective measures of visual acuity can be obtained using resolution or grating tests in conjunction with matching plates. Careful observation of head posture, eye movements, and integration of other sensory pathways provide insight into functional impact of ocular motility abnormalities.
Notably, patients may not report diplopia, particularly if their vision is poor, if the double images are widely
separated, or if they fall within a visual field defect.
Comprehensive assessment of both central and peripheral vison is essential to determine the extent and distribution of preserved visual function.
Additionally, the use of an ophthalmoscope to assess red reflexes can assist in identification of refractive errors, certain types of cataracts, and signs of severe retinal atrophy.
A bedside assessment can limit the tools at the examiner’s disposal. Orthoptists undertaking this role are often required to modify their methods to gain results.
KEY TESTING TIPS:

ABOVE: Motion, action and recognition pathways linked to vision are complex and include frontal, partial and temporal lobes and the brainstem.
• Q uestion the patient about pre-existing and previously treated eye conditions.
Vision Assessment
• For non-verbal or cognitive impaired patients, use resolution or grating tests (e.g. LEA paddles, Teller, Cardiff or OKN drum).
• U se a 3m chart when possible, with or without matching board. Sheridan Gardiner single letters are a suitable option.
• Test vision with known glasses; patients over 45 may require near correction even if they don’t wear distance glasses.
• U se colour vision tests and Amsler chart for central function.
• Performing confrontation visual field (VF) is a useful initial screen but ensure proper technique.
• For peripheral function, use manual quantitative tests like Bjerrum or Goldmann where possible. Bjerrum’s VF also helps educate patients and families on spatial impact of field loss.
• With computerised perimetry, slower response settings may be needed and include one test that explores greater than 30 degrees of VF.
• An ophthalmoscope (even without dilation) can help detect refractive error, cataract and retinal disease - best performed in a darkened room and requires skill.
• O bserve eye alignment and use light reflex to detect abnormalities.
• If an abnormal head posture (AHP) is present, test with and without it and note any change to the eye pattern and or presence of diplopia. If the patient has already compensated for ocular motility issues this should be acknowledged and supported during rehabilitation.
• Engage the vestibular-ocular pathway to assess and potentially enhance eye movement range for rehabilitation.
• Remember, motion, action and recognition pathways linked to vision are complex and include frontal, parietal and temporal lobes and the brainstem.
NOTE: References can be found in the online version of this story.
ABOUT THE AUTHOR: Dr Michelle Courtney-Harris is a clinical orthoptist and early career researcher at UTS, whose work spans neurological visual deficits, ocular pathology, and interdisciplinary reflective practice, with a strong focus on patient-centred care and contributions to the Australian Stroke Foundation’s Living Guidelines. Acknowledging the contribution of Ms Kate Thompson, a senior clinical orthoptist with special interests in stroke, brain injury and neuro-orthoptics.
ORTHOPTICS AUSTRALIA is the national peak body representing orthoptists in Australia. OA’s Vision is to support orthoptists to provide excellence and equity in eye health care. Visit: orthoptics.org.au
Independent optometry practices can now leverage new ODMA-developed resources, helping to drive patient acquisition and improve operational efficiency.

INDEPENDENT OPTOMETRY.”
ractising independent optometry in 2025 is a highly rewarding pursuit, but it doesn’t come without its challenges. With increasing clinical demands, rising patient expectations, and intensified corporate competition, differentiation and efficiency are ideals that can be difficult to live up to amid the daily practice hustle.
Fortunately, there are practical tools developed by trusted industry bodies to support independent optometry.
Two recent innovations from the Optical Distributors and Manufacturers’ (ODMA)
Eyetalk business – LocalEyez and the Eyetalk Subscription Portal – illustrate how purpose-built digital resources can streamline operations, enhance practice visibility to patients, and support more effective clinical care.
Boosting visibility
In an increasingly corporatised market, it can be difficult for independent practices to compete with the digital marketing power of large retail chains. LocalEyez (localeyez.lookbookau.com.au) is an online directory specifically developed to promote Australian independent optometry practices to consumers. It provides independents a critical digital presence in a trusted, optometry-specific environment – with no advanced marketing expertise required.
LocalEyez integrates with LookBook, Eyetalk’s consumer education platform, allowing prospective patients to search for practices while also engaging with content on the latest eyewear trends and eye health advice. This connection is vital because whether someone is seeking fashionable frames or advice on managing dry eye, LookBook acts as a gateway that funnels interested, informed consumers toward independent care providers.
The platform also helps reinforce the distinct value of independent optometry.
For ODMA and Eyetalk, ‘independent’ refers to practices that retain control over the eyecare they offer – from consultation time and prescribed lenses to the frame collections they stock. These practices are often practitioner-owned and operated, with a strong vested interest in long-term patient relationships and clinical outcomes. Supporting them means supporting patient choice, supplier diversity, and high

standards of care.
Crucially, while many independents engage in grassroots marketing or community sponsorships, sector-wide promotion is harder to coordinate. LocalEyez helps fill that gap by giving the whole independent channel a stronger, unified digital voice – one that helps to compete collectively with the louder marketing engines of larger players.
Operational efficiency is another pressure point for independent practices – especially when it comes to managing supplier data and product updates. The new Eyetalk Subscription Portal aims to make this easier by offering subscribers on-demand access to the Eyetalk quarterly publication, product Reference Guide data, and a range of subscription options.
Most significantly, practices can now download up-to-date data files for integration into their practice management systems (PMS). Previously, users had to visit separate platforms or even request files manually. Now, whether a practice needs digital access to product specs, dispensing data, or simply manage its Eyetalk subscription, it’s all centralised in one place.
The portal caters to different needs, offering subscription tiers from a printed Reference Guide to full digital access. This flexibility acknowledges the spectrum of digital readiness across practices: many still value the tactile Reference Guide, but increasingly want the efficiency and convenience that comes with digital integration.
Having current, verified product information directly in the PMS helps minimise errors in ordering and dispensing, improves stock control, and provides staff

ABOVE: ODMA has created new resources to help independents improve their business operations (Eyetalk Subscription Portal) and promote practices to consumers (LocalEyez).
with a reliable training resource. It’s a shift that reflects best practice in digital health: bringing consistent, trusted data into everyday clinical workflows to reduce admin load and enhance accuracy.
The portal is also a step forward for Eyetalk’s own systems, moving from a high-touch, manually managed subscription process to a scalable digital platform. This change benefits both subscribers and Eyetalk, enabling more innovation and responsiveness in the future.
Both LocalEyez and the Eyetalk Subscription Portal are practical examples of how independent optometry practices can use industry-specific digital tools to meet today’s challenges. Unlike generic platforms, these resources are developed by an organisation that understands the intricacies of the Australian optical industry, and are designed with the realities of independent practice in mind.
As patient behaviours shift and operational demands grow, using the right resources can help practices gain an edge. These tools not only make practices more visible and efficient, but also reinforce the strengths that define independent optometry: personal service, clinical integrity, and deep community ties.
ABOUT THE AUTHOR: Laura Moore is managing director of IGN Media, which helps specialised industries grow through tailored marketing and media strategies, delivering innovative solutions that connect niche businesses with their ideal audiences and unique market needs. IGN Media currently manage all ODMA Eyetalk publications.
BY ADAM SPENCER
Imagine a future without having to send an ophthalmologist on a multi-day tour across the vast Australian landscape to examine regional and remote patients. Instead, a nurse or teacher downloads an app, patients stare into a smartphone camera for 20 seconds, and within minutes, AI flags those needing follow-up care. Those few are referred efficiently, accurately, and affordably. Huge gains are made, not only with time, but in terms of eye health outcomes.
It's just one example of how AI is going to transform the work of eyecare and other health professionals. It’s only around the corner and something to be excited about.
Now, before you picture humanoid robots replacing eyecare professionals, let’s zoom in on how AI is already quietly reshaping your world.
In small healthcare businesses – like independent optometry practices and private ophthalmology clinics – AI is already lending a hand. Tools are helping practitioners summarise patient notes, draft referral letters, write emails, and even provide clinical insights from the latest research. If you’re using something to transcribe or summarise a consultation, you’re already in the AI game.
On the marketing side, I’ve heard of practices using AI to mine insights from shopping centre data to tailor offers based on foot traffic demographics. Promotions for Gucci glasses one night, affordable family packages the next – all guided by trends AI can pick up in large datasets.
But if you’re an independent practice owner reading this, thinking, “I don’t know where to start”, you’re not alone –and you’re not behind.
There’s no need to become an AI aficionado overnight or invest in a costly subscription upfront. You just need to experiment. Start small. Sign up for a free trial of a platform that interests you –image generation, transcription, writing assistance. Dip a toe in. You might be surprised how intuitive these tools are. If you’ve got a 20-something-year-old optical dispenser, ask them what they’re using. They probably know more than you think.

decades of career ahead. AI isn’t a trend to "wait out". It’s something to grow with.
One concern is that AI will “depersonalise” patient care. But used well, it does the opposite. One financial advisor I spoke to has an AI scribe that listens in on client calls and drafts the advice afterwards. That saves him about an hour per client. He can either see more clients or spend more time understanding each client’s story. That’s the point: AI doesn’t remove the human element. It lets us be more human, by minimising the administrative overheads of practice life. Surely that’s music to the ears of often more time-intensive independent optometry practice.
Further on the time horizon things get even more interesting.
Imagine if a body like RANZCO developed its own large language model – its own bespoke GPT. It’s trained not on the entire internet, but on peer-reviewed research, expert consensus, and local clinical guidelines. A regional optometrist could query it mid-appointment, or a patient could get preliminary advice online before even setting foot in the practice. Individual practitioners wouldn’t have the resources to build such a system on their own AI, but you’d subscribe to one built by the best minds in your profession – for a fraction of the cost of hiring another staff member. All of this leads to a future of truly personalised care. Your patient walks in,
the vehicle in an AI-reliant world. We're already close to real-time language translation via smart glasses. Put in a clinical context, an elderly Greek patient walks into your practice, you greet them in English, but your glasses instantly translate their reply played through speakers embedded in your frames. I believe eyewear will be one of the most exciting technology platforms of the next two decades. We're headed toward a world without language barriers – and for an industry that puts devices on faces, that’s a big deal.
So, if you take one thing from this: the genie’s out of the bottle. You don’t need to master AI overnight. But it’s time to start. Start small, stay curious, and surround yourself with people who get it. Because the future isn’t just coming – in eyecare, some would argue it’s already looking you straight in the eye.
NOTE: Adam Spencer was a keynote speaker at ODMAFair25 where he presented on AI in business and eyecare. His newsletter can be subscribed via: https://landing.mailerlite.com/ webforms/landing/u0z4s4
ABOUT THE AUTHOR:
Name: Adam Spencer
Qualifications: Dr Spencer (honoris causa)
Job title: AI educator and maths nerd
Location: Sydney
EYEWEAR MAY SERVE AS THE VEHICLE IN AN AI-RELIANT WORLD. WE'RE ALREADY CLOSE TO REAL-TIME LANGUAGE TRANSLATION VIA SMART GLASSES.

2025
EUROPEAN SOCIETY OF CATARACT AND REFRACTIVE SURGEON (ESCRS) MEETING
Copenhagen, Denmark 12 – 16 September congress.escrs.org
EYECARE PLUS BOOTCAMP 2025
Sydney, Australia 12 – 14 September eyecareplus.com.au
SPECSAVERS CLINICAL CONFERENCE 2025
Melbourne, Australia
13 – 14 September specsaversclinicalconference.com.au
TASMANIA'S LIFESTYLE CONGRESS
Hobart, Australia
20 – 21 September tlc.optometry.org.au
SILMO PARIS
Paris, France
26 – 29 September silmoparis.com/en
ORTHOKERATOLOGY SOCIETY OF OCEANIA MEETING Benowa, Australia 10 – 12 October oso.net.au

After a record 2024 turnout in Barcelona, EUSCRS will take place at the Bella Center Copenhagen in Denmark this September.
AMERICAN ACADEMY OF OPHTHALMOLOGY MEETING AND EXPO
Orlando, US 18 – 20 October aao.org/annual-meeting
RANZCO CONGRESS
Melbourne, Australia 14 – 17 November ranzco2025.com
MIDO Milan, Italy 31 January – 2 February mido.com

Current position:
WHY DID YOU PURSUE AN OPTOMETRY CAREER?
I’ve always had a strong interest in healthcare – there’s something fulfilling about helping people in a tangible way. At the same time, I was conscious of wanting a career that offered a healthy work-life balance. Optometry struck the perfect chord: it allowed me to work in a clinical setting, make a meaningful difference in people’s lives, and still have time for personal pursuits.
My journey began as an optical dispenser, which gave me a firsthand look at how vision care impacts people’s day-to-day lives. That experience cemented my decision to pursue optometry more seriously. After completing my university degree, the transition into becoming a practising optometrist felt natural.
Interestingly, Specsavers wasn’t initially on my radar. It was a friend who suggested looking it, and I’m so glad they did. I was working as the sole optometrist in a metro location, which was a great starting point as a graduate. It gave me the chance to build confidence, develop my clinical skills, and understand the day-to-day realities of running a practice. But I found myself wanting more –more variety, more challenges, and more opportunities to make a broader impact. That’s when regional and remote work started to appeal to me. The idea of combining travel with meaningful healthcare delivery was attractive, and Specsavers offered a pathway to do just that. It felt like the right move, both professionally and personally.
WHAT WAS YOUR FIRST ROLE WITHIN
Supporting the Port Pirie store in regional Adelaide. It didn’t have a full-time optometrist, and they needed someone who could step in and provide consistent care.
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Optometrist employment enquiries: Specsavers Recruitment Services –anz.srsdepartment@specsavers.com
Locum employment enquiries: ANZ.locumteam@specsavers.com
Graduate employment enquiries: apac.graduateteam@specsavers.com
That opportunity introduced me to mobile optometry. I quickly realised how significant the gap in eyecare access c an be in regional and remote areas. People were waiting longer for appointments, and many hadn’t had their eyes tested in years. Being able to bring optometric services to these communities wasn’t just about prescribing glasses, it was about identifying serious eye health issues early and making sure people received the care they needed.
Fast forward to today, and I’m now in a mentoring role at Port Pirie – the very store where my mobile optometry journey began. It’s a proud, full-circle moment. Working in remote locations, you see a spectrum of conditions, learn to adapt quickly, think critically, and build strong rapport with patients who may not have regular access to healthcare. Now, I get to pass that knowledge on to graduates. Many are stepping into regional practice for the first time and my role is to help them find their footing, just as others helped me. It’s rewarding to watch them grow in confidence and capability.
It might sound cliché, but helping people truly is the heart of what I do. Every day brings a new opportunity to improve someone’s quality-of-life. There’s a real sense of purpose in knowing that your work has a direct impact on someone’s wellbeing. No two days are the same, especially in mobile optometry. You meet people from all walks of life, hear their stories, and become a trusted part of their healthcare journey. That connection, that trust –it’s what keeps me motivated and passionate about the wo rk I do.
Optometrist Joint Venture Partnership Opportunity –Tauranga & Tauranga Crossing, NZ
Specsavers has a unique opportunity for an experienced Optometrist to join as a Joint Venture Partner across two well-established stores in Tauranga. Situated in the stunning Bay of Plenty region, Tauranga boasts a vibrant coastal lifestyle with beautiful beaches, excellent dining options, and a loyal customer base. Enjoy a supportive team, modern technology including OCT and a guaranteed salary plus a share in dividends.
Eyes on Leadership? Part-Time Senior Optometrist Role in Ellenbrook, WA! We’re seeking a passionate Optometrist to join our Ellenbrook team in a permanent part-time role (3–4 days/week). You’ll work alongside 6 experienced Optometrists, mentor new graduates, and manage 20-minute rolling clinics in a diverse community setting. Enjoy a strong work-life balance with a flexible roster (Mon, Tues, Thurs, Sat), a supportive team, and exposure to dry-eye management with a new IPL machine arriving soon.
Package includes: Up to $125K base salary (pro-rata) + super + performance bonuses. Take the next step in your optometry career today!
Optometrist opportunity – Specsavers Porirua, NZ
Specsavers Porirua is looking for an Optometrist to join the team in early 2026! With a flexible roster that supports work-life balance and a competitive salary package on offer, this is a fantastic opportunity to work in a newly refurbished store in Wellington, known for its diverse pathology and supportive team environment.
Thinking about getting out of the city? Specsavers have a number of exciting opportunities throughout regional Australia and New Zealand. Specsavers continue to be the largest employer of Graduate Optometrists across Australia and New Zealand with our industry leading two-year Graduate Program. To discuss these opportunities, or find out more about our graduate program, please contact your Graduate Recruitment Consultant or email anz.graduateoptometry@specsavers.com

Given Stephanie Bahler’s success as Alcon's surgical glaucoma specialist for Western Australia, her role has been expanded to now cover South Australia and Northern Territory. Her ophthalmic and optical experience of 20 years includes clinical, management and business commercial roles across several ophthalmic medical device companies. She also currently holds the leadership position as president of Optometry WA. “Originally trained as an optometrist, Stephanie’s industry experience, coupled with her passion for community eye health, will ensure she can deliver adaptable and effective support for the Hydrus Microstent technology across WA, SA and NT,” Alcon said.

Eyecare Plus has welcomed its new business development manager (BDM) Ms Lily Wegrzynowski to its national office team. She is an optometrist with more than 30 years' experience in clinical and business management roles and has worked with independent and corporate practices across Australia. Most recently she was responsible for HR and optometry at the EyeQ Optometrists group. "Her background also includes serving on various industry boards, including three years as president of Optometry WA. She has also been a member of the Deakin University Optometry Advisory Board since 2012," Eyecare Plus said, noting she’ll work alongside Mr Ethan Nguyen in the BDM role.

The Royal Victorian Eye and Ear Hospital (Eye and Ear) has elevated Dr Nathan Vos into the role of director of medical services. He has been supporting the hospital as its medical administration fellow since the beginning of 2025. He has experience in medical administration at public and private hospitals, is a fellow of the Royal Australasian College of Medical Administrators and has studied a dual Master’s in Public Health and Health Leadership and Management. “We look forward to Nathan’s leadership as we continue to deliver world leading eye, ear, nose and throat care,” the Eye and Ear said.

Ms Sai Kandibanda is an optometrist with more than six years’ experience and a Doctor of Optometry degree from the University of Melbourne. As the new professional services manager at CR Labs, she is involved in delivering engaging training and expert product education on specialised lens technologies, helping independent optometry practices across Australia achieve exceptional patient outcomes, the company said.

Mr Anthony Stella has been appointed as Opticare’s business development manager for Victoria and Tasmania. He joins the company with a career spanning retail, wholesale, training, and leadership roles. He’s a qualified ophthalmic lens mechanic and dispenser and has managed both chain and independent optometry practices, including launching a greenfield practice. Plus, Stella has served as an operations manager of an optical laboratory for 11 years and an account manager for 13 years. “His appointment is a significant and positive step forward in our growth strategy, ensuring even stronger relationships and tailored support for our Victorian and Tasmanian customers,” Opticare said.

Ms Juliana Yan is excited to have stepped into the role of professional services manager of NSW/ACT for EssilorLuxottica. “I had a rewarding experience serving as an area eyecare manager previously, working closely with our optometrists and retail teams to support clinical excellence and growth,” she said. “In this new role, I’ll be focusing on driving professional development, enhancing patient care through eyecare innovation, and supporting our network across the region.”
B.App.Sci (Optom)

Like most 18 year olds, Charmaine was not sure which career path to pursue. But as fate would have it, she attended her grandmother’s eye test and was impressed by the optometrist who shared how they helped others and how the profession allowed them balance to raise a family.
Charmaine graduated from QUT and then went to practise in Tasmania before returning to Brisbane, where she settled in Gympie. “I love Gympie because it offers wonderful city living but is very community based. I’ve loved treating generations of families over the last 23 years… patients who were children and are now all grown up, still come to our practice”.
I’ve fallen back in love again with being an optom as I can focus on delivering the best patient care. That has been a key reason why I joined George & Matilda. They also believe in being patient first.
Charmaine and her amazing team have worked hard to build a successful practice. They joined George & Matilda Eyecare in 2016. “It’s difficult to do it all on your own. I’ve had great support while being able to maintain independence in where I want to specialise and how I treat patients, providing longer consults. I now have more time, so I am mentoring Deakin University students. I feel it’s important to help mould the next generation of optometrists”.
Let’s Connect
Contact Cassie Gersbach, General Manager of Partnerships at cassie.gersbach@georgeandmatilda.com.au
