






The first major step towards achieving this goal was announced last month – WA’s first ever preventative health strategy.
Preventative health has long been a buzzword in the sector –we’ve all heard the saying ‘prevention is better than a cure’.
This year, the state government is aiming to put that into action.
A new approach to health was ushered in after last year’s state election, with the aim of making WA the healthiest state in the nation.
In a first, five ministers were appointed to work across the health portfolios. Preventative Health Minister Sabine Winton has the goal of improving the wellbeing of West Australians and reducing demand on public hospitals over the long-term.
The first major step towards achieving this was announced last month – WA’s first ever preventative health strategy.
While the strategy is yet to be written – it will be informed by key health stakeholders and medical professionals – it’s a clear acknowledgement from the government that the health system cannot continue under the pressure it faced last winter.
As always in the health sector, the proof will be in the pudding. Announcements like this are always met with enthusiasm and endorsement, but headlines mean nothing if outcomes are not delivered.
Perhaps this is the first key test to determine whether the state government’s new shared approach to health is working. We will wait and see.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




Our competitions are back for 2026, kicking us off with another WA wine giveaway.
We have a dozen of Woody Nook wines for one lucky reader to enjoy. Described as “well worth a visit” by or Master of Wine, the winery offers Cabernet Sauvignon, Shiraz, Merlot, Cabernet Franc, Chenin Blanc, Chardonnay, Sauvignon Blanc and more.
Read our Master of Wine’s review of the Margaret River winery on page 55.
PUBLISHERS
Alice Miles – Director
Fonda Grapsas – Director
Tony Jones – Director
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Studio Scotts hello@studioscotts.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Advertising Account Manager and Clinical Services Directory
Rita Murphy 08 9203 5222 rita@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
















A drug used to treat patients with a severe and rare condition has been approved for use in the United States based on the results of a WA study.

The Food and Drug Administration (FDA) approval of plozasiran marks the first time an siRNA (small interfering RNA) drug to treat adult patients with familial chylomicronemia syndrome (FCS), a condition that leads to extremely high level of blood fats, has been approved in the US.
Plozasiran, now marketed under the brand name Redemplo, was approved based on the results of a Phase 3 study, published in the New England Journal of Medicine The lead author was Winthrop Professor Gerald Watts (pictured above) from UWA’s medical school.
“Extremely high blood levels of triglycerides in the blood, known as
The Pharmaceutical Benefits Advisory Committee has recommended that semaglutide be subsidised through the Pharmaceutical Benefits Scheme for adults with established cardiovascular disease (eCVD) with obesity. The recommendation covers patients who have already experienced a cardiovascular event such as a heart attack, stroke, or have symptomatic peripheral arterial disease.
The PBAC considered three potential patient populations based on different Body Mass Index cut-offs: ≥ 27kg/m2, ≥ 35kg/m2 and ≥ 40kg/m2.
However, the committee recommended limiting PBS access to people with a BMI of 35kg/m2 or higher, or 32.5kg/m2 or higher
chylomicronemia, are caused by a rare genetic defect known as FCS that impairs their clearance from the circulation after a fat-containing meal,” Professor Watts said.
“It can have serious consequences, including acute and potentially fatal pancreatitis, chronic abdominal pain, skin eruptions called xanthomata, diabetes, fatty liver and cognitive issues.
“Before this drug was approved there were limited therapeutic options to adequately treat this condition.”
Plozasiran is a chemically modified small interfering ribonucleic acid that selectively inhibits the messenger-RNA and hepatic
for people of Asian, Aboriginal, or Torres Strait Islander ethnicity. By limiting access to the drug, the committee hopes to minimise the financial burden on the PBS and target potentially higher risk individuals.
Health practitioners who have a tribunal finding of professional misconduct with a basis of sexual misconduct will have this information permanently added to the public register from April. Ahpra published new guidance on adding information about sexual misconduct to the register of practitioners late last year in preparation for the requirements. It follows changes to national law following a decision by
production of apoC-III, a protein that raises triglycerides, by slowing the breakdown by an enzyme called lipoprotein lipase and the clearance of their smaller remnant particles by receptors in the liver.
Professor Watts has been caring for patients with severe hypertriglyceridemia for 40 years. He said to have a drug that provides a much-improved quality of life was a great achievement for the patients who could access it.
The drug is available in Australia on a special access scheme for those with FCS-like characteristics, persistent chylomicronemia, and recurrent pancreatitis.
health ministers in 2024 that sexual misconduct findings should be publicly available via adding it to the register.
A statement issued by Ahpra and the National Boards said the measure would provide the public with information they need and expect when choosing a health practitioner.
The change will be retrospective and comes into effect in April 2026.
National Boards are responsible for deciding if a tribunal finding of professional misconduct included a basis of sexual misconduct.
The Guidance notes that sexual misconduct represents “a serious violation of professional and ethical standards and constitutes a significant betrayal of trust placed in practitioners by patients/clients, colleagues, and the community”.
More than 100 players took to the hockey pitch in December to take part in the Western Hockey Master’s Gala Day.
The event was proudly sponsored by Medical Forum for the fifth consecutive year.
The gala promotes sport for players who have faced medical problems including hip and knee replacements, cancer, heart conditions and other concerns.
It aims to show sport is still for everyone, no matter the challenges they have faced.
“We try to highlight that medicine is helping people to move on with their lives and play sport after what would have been a major challenge to their
OBE Challenge Cup – men over 80 Golden Masters (2) White Knights (1)
Laurie Packham Challenge Cup – women over 70 Trailblazers (0)
Vintage Vixens (3)
PUC Survivors Cup Women
Nice n Kneesy (3) Breast Friends (1)
PUC Survivors Cup Men Cancer (1) Hearts (2)
AOA Bionic Cup Hips (1) Knees (2)
The federal government will invest $14.5 million to support an additional 306 fully funded places on the Australian GP Training (AGPT) Program in 2026.
Some 200 training places were due to be delivered in 2026 but an announcement last month saw the federal government add an additional 106 places to that tally.
The investment will take the total number of doctors commencing GP training to around 2,100, a 14% increase on the 1,840

health,” said Western Hockey Master President Tony Jones.
Other sponsors include Western Cardiology, Panchos Villa Mexican Restaurant and Hockey WA, with support from the Heart Foundation, Cancer Council WA, Scott Print and a team of volunteers to make the day possible.
Perth Urology Clinic sponsors two of the cups – one for women

with knee or hip replacements versus those who have had cancer or heart conditions, the other for men in the same category.
The Bionic Cup, the gala’s longest running competition, is sponsored by the Australian Orthopaedics Association. It is played by men who have had hip replacements versus men who have knee replacements.

achieved in 2025, according to Health Minister Mark Butler.
The RACGP welcomed the announcement as a win for access to primary care.
President Dr Michael Wright said: “The Government is delivering on its commitment to train more specialist GPs.
“A record number of doctors took up Commonwealthfunded specialist GP training with the RACGP in 2025, with all places filled for the first time in a number of years.
“The RACGP trains 90% of GPs across Australia, in our cities and our rural and remote communities – and as we have said, more funding and support means we can train more specialist GPs.
The boost in training places comes as the number of doctor registrations nationally increased more than 30% in 2024-25 compared to 2021-22.
The RACGP is expected to announce further details about its 2026 AGPT Program cohort soon.
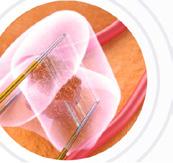
Aortic stenosis symptoms can often be overlooked as normal signs of ageing, but GPs should reach for their stethoscope to avoid underdiagnosis of Australia’s most common heart valve disease.

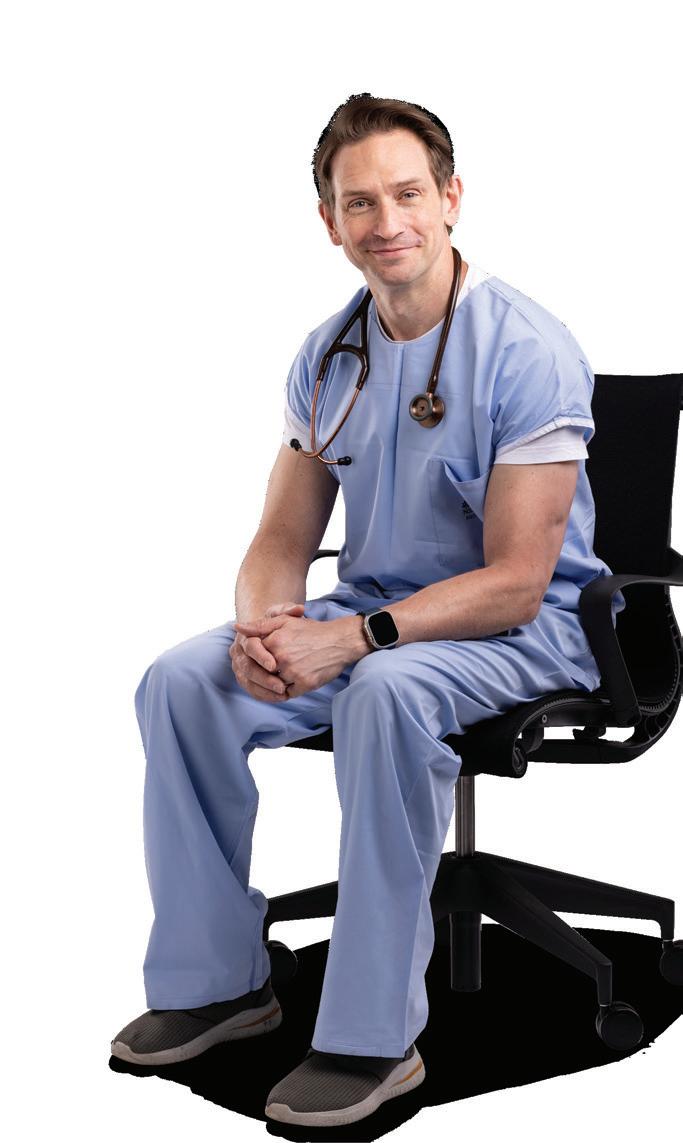
Early aortic stenosis often goes undiagnosed and without valve replacement prognosis can be abysmal, according to interventional and structural heart cardiologist Dr Gerald Yong.
Dr Yong is the head of the Valve Intervention Program at Fiona Stanley Hospital and operates privately at The Mount, Hollywood and Murdoch hospitals.
Much of his time in the theatre is spent completing transcatheter valve replacement and repair
procedures that provide patients a chance of a healthier future.
So, what should GPs know about aortic stenosis?
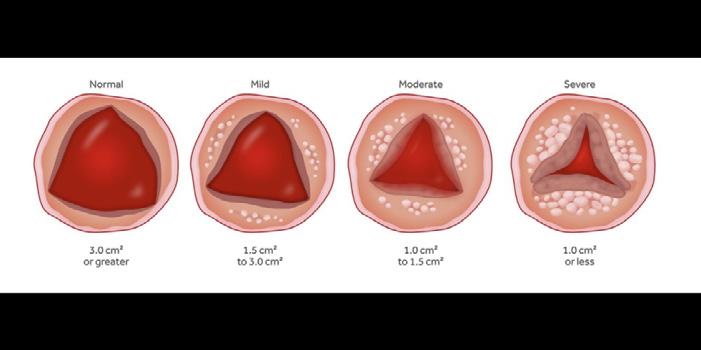
Aortic stenosis is Australia’s most common heart valve disease. It affects one in eight patients over the age of 75, with age being one of the main risk factors.
Dr Yong said: “Essentially over 10% of elderly populations could have severe early stenosis or other serious heart valve disease.”
Are your patients over 65 and feeling short of breath, lightheaded or weary?
These could be the signs of a common underlying heart valve disease, such as aortic stenosis. On Tuesday February 17 between 9am and 5pm, Hollywood Private Hospital will be hosting Free Heart Checks for patients over 65 experiencing these symptoms.

Bookings can be made via the Hearts for Hearts website or here

It occurs when the aortic valve hardens, reducing blood flow and placing strain on the heart. If left untreated, it can lead to heart failure.
And here is why it is not always picked up.
The main presentation is exertional symptoms such as exertional shortness of breath or chest pain, which are also typical symptoms that are associated with ageing.
Even before patients see their GPs, many will have spent time dismissing symptoms such as breathlessness, fatigue, or dizziness as normal ageing, which inevitably delays diagnosis and treatment.
Not only is aortic stenosis often put down to age, but it is sometimes mistaken for asthma.
Dr Yong said shortness of breath, chest discomfort, syncope, and reduced exercise tolerance should all prompt further investigation.
That’s why if he gets a chance to speak with GPs Dr Yong always reminds them of the importance of getting out a stethoscope.
“When you get these patients in, at least listen to their heart for a murmur,” he said.
“When you hear a murmur, investigate that by doing an echocardiogram. If you do that you are less likely to under diagnose the condition.”
Early intervention is key
As with most things in medicine, early referral to an interventional cardiologist was a key step to successful patient management.
“Early engagement with cardiology teams can significantly improve outcomes,” Dr Yong said.
“Once you’ve developed a severe aortic stenosis with symptoms, it is a clear-cut indication that you need valve replacement. Without it, your prognosis is abysmal.
“We’re talking about one to two years mortality at 50%, which is actually worse than cancer, and the only way to reverse that is a valve replacement.”
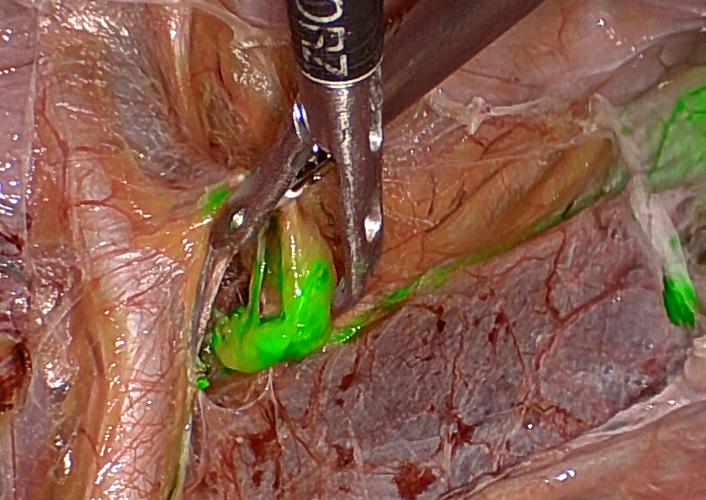
Dr Yong started the Transcatheter Aortic Valve Replacement (TAVR) program in Western Australia some 15 years ago.
“Prior to that, the only way to treat aortic stenosis was open heart surgery to replace the valve,” Dr Yong explained.
“More and more now we are doing transcatheter valve replacement.”
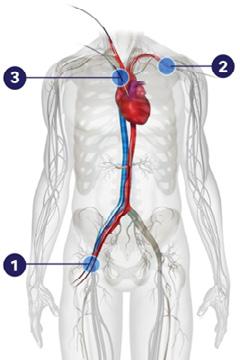
The procedure sees a new valve made of animal tissue guided into
place through keyhole surgery and expanded, pushing the old valve aside.
“We can replace the valve through the TAVI procedure, where we essentially push the valve through a small puncture in the femoral artery all the way to inside the native aortic valve,” he said.
“We then expand the transcatheter valve and it pushes away the native valve.”
Dr Yong said this procedure offers far less trauma and recovery time than open heart surgery.
In fact, the majority of procedures are undertaken while the patient is awake under local anaesthesia, rather than general anaesthetic.
Ensuring patients are fit for procedure
Structural heart nurse Cecilia Wong is an integral member of Dr Yong’s multidisciplinary structural heart team, which provides comprehensive assessment and care for patients being considered for TAVI.
Patient evaluation is thorough and collaborative, commonly involving interventional cardiologists, cardiac surgeons, cardiac imaging specialists, and geriatricians. The assessment process includes advanced investigations such as CT imaging and coronary angiography, alongside functional and frailty assessments, to ensure patients are optimally selected and prepared for the procedure.
Care is delivered within a structured multidisciplinary framework,
GPs can encourage patients to maintain heart health through:
• Blood pressure and cholesterol management
• Regular physical activity
• Smoking cessation
incorporating formal heart team discussions, coordinated periprocedural management, and postprocedural rehabilitation supported by allied health professionals. Ongoing follow-up includes clinical review and echocardiographic surveillance to ensure optimal longterm outcomes.
The European Society of Cardiology has recently updated its guidelines to recommend TAVI for patients aged 70 years and older, expanding access to this minimally invasive treatment for a broader patient population.
Dr Yong’s private practice is iSave Heart Clinic, located at Suite 52, Wexford Medical Centre, 3 Barry Marshall Parade, Murdoch WA.

A first of its kind preventative health strategy is set to be launched in WA with the aim of keeping people healthier and out of the state’s hospital system.

Six roundtable events will inform WA’s first preventative health strategy, with the first held on January 21.
Around 150 senior representatives across government, nongovernment organisations, community groups, universities and research institutes will take part in the discussions.
Key health stakeholders including the Public Health Association of Australia (PHAA), AMA, The Kids Research Institute Australia, and Cancer Council WA will be involved.
PHAA acting chief executive Malcolm Baalman told Medical Forum the association hoped the evidence gathered during these sessions would prompt increased financial commitment towards preventative health.
“We hope it feeds into actions the government needs to take to make good on its promise to dedicate 5% of its health budget on prevention by July 2029,” he said. This goal was outlined in the Sustainable Health Review.
“Properly resourcing prevention programs mean fewer people get sick, that means a better quality of life for everyone, and eases pressure on our hospitals and ambulance services,” he added.
Executive director of The Kids Professor Jonathan Carapetis commended the government for taking a long-term strategic approach to identifying and actioning priorities that will shift the focus from treatment to prevention.
“The evidence is compelling that investment in preventative health saves lives and reduces the burden on our health system,” he said.
Preventative Health Minister
Sabine Winton said insights from the roundtables would ensure the strategy was grounded in realworld experience and focused on practical ways to make the biggest difference in people’s lives.
“Prevention is the most powerful tool we have to improve health outcomes, and the WA Preventative Health Strategy is about making sure Western Australians can live healthier lives,” she said.
“By investing in prevention now, we are building a stronger, more sustainable health system for generations to come,” she said.
Ms Winton will host the roundtables in collaboration with WA Health, the Mental Health Commission, and Healthway.
Areas of focus will include mental health and wellbeing in the early years, health promotion, immunisations, cancer screenings, sexual health, targeted population strategies, and cross-government initiatives.
How to promote healthy eating and active living, injury prevention, and a public health approach to the prevention of tobacco, e-cigarettes and vaping will be considered, as well as ways to boost screening and vaccination rates.
Feedback from the strategy roundtables will inform the next stages of work, with a public consultation process set to open in the coming months via the Department of Health to encourage members of the public to provide input.
The National Lung Cancer Screening Program has screened more than 45,000 people since it was launched last July.


Figures from mid-December 2025 show 49,473 people had enrolled in the screening program through the National Cancer Screening Register.
The National Lung Cancer Screening Program (NLCSP) offers low-dose CT scans to people aged 50-70 who smoke or have a history of smoking and who don’t have the symptoms or signs of lung cancer.
It targets people considered at high risk for lung cancer in the hope of catching the disease and intervening early. So far, more than 45,000 low-dose CT scans have been completed with around 5,000 people requiring more frequent

follow-up screening and about 560 people requiring immediate further investigation.
Professor Fraser Brims , a Consultant Respiratory Physician at Sir Charles Gairdner Hospital and Director of Early Years Clinical Skills at Curtin University, said the program had surpassed initial expectations.
Professor Brims said it would take time for national data to emerge regarding the impact of the program, but clinicians were already seeing anecdotal impacts.
“We have all begun to see individuals who have been positively impacted, be it the identification of early lung cancer at a time when it can be cured, improved awareness of lung health, or empowering and
encouraging others to overcome their nicotine addiction,” he said.
“Further, we have seen initial success in rural WA with the mobile Heart of Australia CT scanners working with local communities and already finding early lung cancer.
“It is hugely exciting to see the early impact of the NLCSP on individuals and local communities.”
Professor Dorothy Keefe, chief executive of Cancer Australia, said with lung cancer being the most common cause of cancer death in Australia early intervention was vital.
“This program represents a major milestone in Australia’s efforts to improve cancer outcomes,” she said.
“As one of the first countries in the world to implement a national lung cancer screening program, we are detecting lung cancer early and improving survival through culturally safe, accessible screening services.”
The federal government has invested more than $260 million in the program, which is expected to save hundreds of lives a year.
Of that funding, $13 million has gone towards the It’s Good to Know campaign to inform Australians about the program. The program may also prove to be a reminder to focus on overall health. Among those who have been screened was 60-year-old Eleesa who had smoked since she was 14.
Her scan was lung cancer-free, but it did pick up early onset emphysema, which Eleesa said was a “wake-up call” to prompt her to quit smoking.
With Australia mid-way through another summer sports season with its omnipresent gambling advertising, doctors are warning it’s a sure bet that the health of thousands of families is at risk.
By Cathy O’Leary

The head of one of Australia’s peak medical groups admits many people are baffled at why doctors would have any role in problem gambling.
But being a GP in her day job, AMA National President Dr Danielle McMullen sees first-hand the health, financial and social havoc that gambling can wreak on her patients and their families. She finds it sobering and sad.
“People often say why does the AMA care so much about gambling, but it’s because we do see it as a health issue, it’s an addiction just like an addiction to a substance or another behaviour,” she told Medical Forum
“And when people have a severe problem with gambling it can have direct and indirect health harms, and that’s where we come in.

“People neglect other aspects of their life and health because they’re so caught up in their gambling behaviour or financial distress that they’re not eating, sleeping or looking after themselves.
“Then there’s the consequences when people have got themselves into severe financial distress thanks to their gambling, so for themselves and their families their livelihoods are at risk, and that means housing and food security.”
Dr McMullen admits gambling issues can be an uncomfortable conversation, but doctors do and should step up, because it’s an addiction that is getting worse, fuelled by a powerful gambling industry and government inaction.

Australians are among the world’s biggest losers, forking out an estimated $32 billion a year in bets – the highest per capita losses in the world and more than what households spend on electricity and gas.
These losses now eclipse what governments spend on aged care, and rival NDIS expenditure.
Gambling is woven into the fabric of Australian society, from a casual flutter on the Melbourne Cup to the lure of pokies at the local club. While about 70% of Australians buy a lotto ticket or place a bet each year, most follow the mantra and ‘gamble responsibly’.
But the prevalence of problem gambling and its associated harms continues to rise, representing a significant public health issue.
However, all bets are off that national law reforms – which many gambling researchers argue are desperately needed –will be in place anytime soon.
The Federal Government has been accused of sitting on its hands, failing to respond in any meaningful way to an inquiry that handed down a compelling report and list of recommendations in 2023 to address the problematic gambling running rife in Australia.
A parliamentary inquiry headed by the late MP Peta Murphy sounded a loud warning that gambling risks were accelerating and reforms were urgently needed to protect the community, particularly from the pervasive online risks.
The inquiry’s cross-party committee unanimously endorsed 31 recommendations in its report You Win Some, You Lose More, aimed at reducing gambling harm, including a phased-in ban on advertising for online gambling.
But two and a half years later, the Murphy report sits on a website that comes up blank: ‘This inquiry currently has no government response documents.’
Some media reports had suggested the Government was considering a watereddown version of the reforms, such as a partial ban to remove gambling ads from social media.
However, there are now deepening concerns from crossbenchers and gambling harm advocates that even that recommendation might have been bumped off the agenda by the Government’s recent under-16s social media ban, which it could argue addresses concerns about children seeing gambling ads online.
Dr McMullen is among those highly critical of the delays in implementing recommendations from the review, despite gambling causing severe mental health disorders, substance abuse, family breakdown and financial devastation.
“There’s been nothing hugely visible happening which means another summer sporting season with what we would see as an unacceptable amount of online and other advertising of gambling platforms,” she said.
“Gambling affects all parts of Australian society, although it is an area where groups who are already at disadvantage are
particularly at risk of gambling harm – so that’s young adult men, people with English as a second language, or socio-economically disadvantaged people.
“The target of much of the gambling advertising is men aged 18 to 35, and that’s where we’re seeing the largest uptake, but gambling doesn’t discriminate and there may be people where it is surprising to find they have a gambling problem.
“It’s important as doctors we keep an open mind about who might be struggling and be ready to support to them, no matter what it looks like.”
Dr McMullen said the other cohort that doctors were particularly worried about was children. Not concerns about them acting on it now but fears they were seeing so much advertising from a young age.
“Particularly with sports betting and online gambling, and social media, with bright lights and lots of noises and the pokies scrolling around in the background, it all looks fun and exciting. It’s sending the wrong message to children and really underestimating the harms that gambling can cause,” she said.
Dr McMullen said she was often shocked by gambling content on social media and from Instagram influencers, with some trying to make gambling a sport in itself.
More broadly, online gambling had taken risks to a whole new level.
“Gambling is a health harm and it’s an addiction and in situations where you don’t have to leave your home, or you can do things in secret, it’s harder to escape that addiction and manage the risk,” she said.
“Prior to online gambling, people had to leave home or at least make a phone call or plan ahead for their gambling, whereas now it’s far too easy with mobile devices at any time of day or night to take your money and amplify your losses.”
But while national gambling reforms have stalled, there is a small light at the end of the tunnel in Western Australia, with a separate push to bring in gambling reforms here.
Continued on page 13

Providing a holistic approach to patients needs with focus on prostate cancer, Nanoknife IRE, urinary continence, prostate health, sexual function, wellness
Associate Professor Tom Shannon Consultant Urologist
A/Prof Shannon is a graduate of the University of WA. He completed his Fellowship in Urology in 1999 and completed post-fellowship training in the UK and the US focusing on minimally invasive surgery and prostate brachytherapy. He was a pioneer of minimally invasive urological surgery in WA and is a leader in the development of prostate MRI. He is a strong advocate for men's health and has been a board member of the Prostate Cancer Foundation of Australia (WA) for over 10 years.
Perth’s Prostate Cancer and BPH Centre
Research shows that : Continued from page 11
Question: “In the past 12 months, have you had an issue with gambling?”
This screening question is validated as having a 92% detection rate for identifying gambling harm in patients in a primary care and medical setting.
Know the comorbidities
Gambling harm is a complex issue that often co-occurs alongside mental ill-health, use of tobacco and AOD, family and relationship conflict, or various forms of trauma (such as interpersonal, multi-generational or acquired).
39% of people who experience problem gambling have a diagnosed mental health condition, such as depression, anxiety, alcohol use disorder or post-traumatic stress disorder (Kessler Psychological Distress Scale)
39% of people who experience problem gambling are in a state of high distress, compared with 5% of the general population
there is a correlation between risky gambling behaviour and heavy alcohol and tobacco use.
Source: Gambling Factsheet for GPs, from the RACGP and the Victorian Responsible Gambling Foundation
Submissions recently closed on a government review of the state’s outdated gambling laws – some of which date back more than 70 years.
A Department of Local Government, Industry Regulation and Safety consultation paper canvassed several options that would restrict gambling advertising, including a total advertising ban consistent with the Murphy review. If this was enacted, WA would potentially lead the country in gambling reform.
The review has piqued the involvement of the AMA (WA), which sought feedback from its members late last year ahead of making its own submission before the December 12 deadline, but is yet to respond further.
self-reported satisfaction with life drops as risky gambling behaviour increases (Australian Unity Wellbeing Index) Educational
Dr McMullen urged doctors to be receptive to signals of gambling problems in their patients. Patients who had a regular GP
often found those conversations easier, because there was some rapport and understanding of the family context.
“It’s well within the skills set of general practice, it’s certainly taught, although we can always do with more resources about services to which we can refer people,” she said.
“There is a whole lot of shame and fear associated with addictions of all sorts. I’m a GP in my day job and I know that often once you’ve seen someone for other health conditions, they will disclose a gambling problem.
“This is a good reminder to GPs and other doctors about gently raising the question with patients, even if they don’t respond in that moment. It’s planting the seed that patients can feel safe and comfortable to be able to talk to you if there’s something they’re worried about.
“We’re skilled in things like nicotine cessation with patients who
smoke. We know that the first time we have a conversation with them they might not be ready for help yet, but planting that seed and building that relationship, you just never know if that’s the conversation that saves someone.
“Two and a half years on from the Murphy report, we remain disappointed that there hasn’t been more action on it but in the meantime doctors do have a role in helping patients identify and get support for their gambling problems, by just starting that conversation.”
0.5 0.5 hours

Medical Forum is now an approved RACGP CPD provider for general practitioners, offering EA, RP and MO modules

Look for the RACGP CPD logo on Medical Forum content to complete your annual CPD hours.
Scan the QR code in the magazine or follow the links on our website to complete the activity requirements.
Your hours will be automatically added to your RACGP CPD home seven days after completion.

DR MAREK GARBOWSKI

Complete four hours of CPD, including MO, with our Pelvic Venous Congestion podcast. Learn when to consider the diagnosis and how to manage it.
The state’s public hospitals rely on a maintenance system that is underdeveloped, constrained and too reactive, a new report has found.
The audit undertaken by former Under Treasurer Michael Barnes and Dr Neale Fong, made public last month, lays bare the condition of WA’s health maintenance.
The review was commissioned in August after numerous media reports highlighted ageing hospital facilities and an underpressure health system.
It came at a time the state was facing record flu cases and ambulance ramping. Sustained pressure on the system saw some elective surgeries postponed as emergency departments struggled to keep pace with demand.
The audit handed down 24 findings and eight recommendations, including that WA Health had limited data to benchmark performance, no systemwide targets for maintenance spend or maintenance planning, and poor procurement processes.
It found major metropolitan hospitals lack master plans, constraining longterm service alignment.
It also found around 75% of maintenance at North Metropolitan Health Service and 77% at East Metropolitan Health Service was reactive, compared to other jurisdictions like Queensland’s health services where there is a target of 65% planned maintenance.
The state government has accepted the findings and recommendations in full.
A $50 million investment fund was also announced to support maintenance completion at Sir Charles Gairdner Hospital, Royal Perth Hospital, and Armadale Health Service.

AMA (WA) President Dr Kyle Hoath, who has repeatedly warned of a public health emergency in the state, said it was an “I told you so moment”.
“These problems in our health system are there; it’s not a world-class health system. We deliver world-class care thanks to our frontline workers and our tireless hospital staff, but our facilities are languishing – they need upkeep and they need this maintenance program,” he said.
“To see the government at least own up to that, and to see the report demonstrate that fairly clearly, is a good thing.”
Health Infrastructure Minister John Carey said he was determined to take action on the concerns raised by clinicians.
“We recognise the need for maintenance to be delivered effectively – ensuring the best possible care for patients, a safe environment for staff and value for taxpayers,” he said.
The state government has promised to:
• reduce red tape for lower value maintenance projects
• develop a health-specific trades and services panel to make it easier to procure work
• establish key performance indicators for maintenance activities across health providers
• provide further transparency of maintenance expenditure

REACT+ is a high-level CPD emergency course that goes beyond the basics, preparing participants for the complex, high-stakes realities of rural and remote emergency care. It’s a fast-paced, immersive course where experienced doctors are challenged to perform under pressure in realistic, high-fidelity simulations.
Eligibility: REACT+ participants are expected to have foundational knowledge in basic and advanced airway management, Basic Life Support (BLS) and Advanced Life Support (ALS) protocols, and the structured A-E assessment of critically unwell patients. Familiarity with emergency and simulation environments is also recommended.
Date: February 21-22 Where: Perth
Interesting cardiology case – real world cases with practical insights for GPs
Speakers: Professor Rukshen Weerasooriya, Dr Gerald Yong, Dr Sekaran Gana, Dr Thato Mabote, Dr Yuli Ten, Mr Eric Karim Slimani, Mr Pragnesh Joshi, Dr Keng (Siang) Ung, Dr Philip Currie, A/Prof Kushwin Rajamani, Dr Pasko Dedic - Cardiology.
Date: February 7, 8am
Where: UWA Uniclub Ballroom, Hackett Drive, Crawley
RSVP: February 6
Speakers: Dr Chloe Nettlefold, Dr Paul Maggiore, Dr Kevin Chung
Topics: Cardiometabolic risk, Arrhythmia management, Valvular heart disease
Date: March 11, 6.30pm
Where: UWA Uniclub

Women’s Health – Spot the Difference
Speakers: Dr Robert Tewksbury, Dr Wasing Taggu, Dr Rajiv Menon, Dr Mike Kamara, Dr Navin David Palayoor.
Date: February 21, 8.30am
Where: Grand Ballroom, Rendezvous Scarborough Hotel, Scarborough RSVP: February 13
A 12-month program that combines educational content and practical experiences to maximise impact and professional growth. The program blends hands-on experience with structured learning to ensure healthcare professionals are well-prepared to manage the complexities of Parkinson’s care. Register your interest email Yasmin Naglazas: yasminnaglazas @parkinsonswa.org.au
Medical Forum will be introducing live GP Masterclasses in 2026
Delivering RACGP accredited education by your local WA specialists – have your say on the topics and speakers you’d most like to see on the program.
Scan the QR code to help design your perfect masterclass
A new facility dedicated to the entire journey of children who become burns patients is set to be delivered at Perth Children’s Hospital.
The WA Comprehensive Centre for Childhood Burns has been backed by a $27 million commitment over 10 years to the Fiona Wood Foundation from the Stan Perron Charitable Foundation.
The centre aims to accelerate research-driven innovation, deliver excellence in clinical care, and enhance community education to improve outcomes for children and families across the state and beyond.
Founder of the Fiona Wood Foundation Professor Fiona Wood is well known for developing a spray-on skin solution which was used to treat patients from the 2002 Bali bombings.
The foundation hopes to drive the next generation of regenerative and scarless healing solutions through this centre.
The centre’s vision is a future where no child is defined by a burn injury, with holistic healing and lifelong health preserved through regenerative science, innovation, and care.
Its goal is to achieve healing without scarring, minimising trauma

and reducing long-term physical and psychological impacts.
The facility will deliver child and family-centred care focused on early intervention, pain reduction, personalised treatment, and improved long-term outcomes.
It aims to advance pioneering diagnostics, therapies, and technologies to drive scarless healing and better mental health outcomes, with clinical trials embedded into routine care while strengthening skills and awareness across health professionals, families, schools, and first responders.
Professor Wood said investment from the Stan Perron Charitable

Foundation would strengthen the organisation’s commitment to delivering the best care for children and their families.
“It enables us to build a truly comprehensive paediatric burns research pipeline, from discovery through to treatment, where clinical trials are embedded into routine practice to ensure every innovation is tested, translated and delivered where it is needed most,” she said.
“Our patients and their families remain central to everything we do; their lived experience shapes the questions we ask and the solutions we pursue.
“Together, we can create a future where children not only survive their injuries but thrive, with care, research and innovation working hand in hand to transform lives.”
Elizabeth Perron, chair of the Stan Perron Charitable Foundation, said she was proud to help enable a centre to drive world-leading research and care right in WA.
“We believe this work will profoundly improve the lives of young people who have experienced burn trauma, both now and into the future,” she said.
It’s not unusual to see Dr Raji Krishnan doing a blood pressure check or dressing a wound in a park. For decades, the award-winning doctor has always gone to where her patients are most comfortable or able to see her.

By Ara Jansen
When most people are thinking about retirement – or have already hung up their stethoscope – Dr Rajeshwary Krishnan is full of beans and joy, genuinely excited to be working.
Known to her patients as Dr Raji, the GP is in her 70s and carries a patient load doctors decades her junior might find hard to keep up with. She has dedicated her career to Aboriginal health care, perfecting the art of listening, which she considers an essential part of treatment.
Born in the Indian city of Jaipur, Raji came from a middle-class family. While education was important, her brother became an engineer but there wasn’t money for the girls in the family to go to university.
Once he got a job, that brother paid for Raji to go to medical school. Determined not to disappoint him or waste his investment, she was a diligent student.
“That first year was not easy at all,” remembers Raji. “There were lots of things going on – living away from home, new friends, studying.
“When I started off, I had one good friend and we came to school with similar backgrounds. When I was feeling low, she would come and say ‘we have to do this!’.
“She was a great friend and we supported each other through those years. We focussed on our education and nothing else, passing our exams and getting to the next year. We could not afford to do badly.”
That friend and several senior mentors got her through and she eventually became a hospital registrar, training in obstetrics and gynaecology. Soon after, she met her husband as part of an arranged marriage and left India.
Raji migrated to Perth in 1977 to join her husband, Arun Krishnan, a specialist in Japanese economics. After doing the requisite conversions of her skills – a repeat of years five and six and having to go to Melbourne to sit the exams – Raji started working as a doctor.
A year later, their daughter, now Dr Priya Krishnan, was born.
“I joined the Aboriginal Medical Service (now Derbarl Yerrigan Health Service) in 1980. After that I don’t think I had time to think about anything. I got into that world and started practising.”
What came next has driven the way she subsequently chose to practise medicine in Western Australia for a career which is now in its sixth decade. Working with disadvantaged and majority Aboriginal patients, she recognised the parallels faced by locals which she saw in India as a younger doctor.
“My drive comes from the trust my patients place in me and the fortitude they exhibit in every facet of their lives. These are people who have gone through unimaginable trauma and adverse life circumstances, but still they welcome me into their lives and the lives of their extended families for generations. I always believe I learn more from my patients than they do from me.”
Raji sometime muses that the hand of destiny guided the course of her medical career. Her introduction to the Aboriginal Medical Service came from a neighbour who at the time was a GP with the group.
“She told me about where she was working and I kept thinking about how similar things were to work in India. There I did a lot of acute medicine and people were very sick by the time they presented.
“That also taught me about the concept of preventative health care and taking that to people, rather than waiting for them to come to the clinic.”
Raji has worked in many different areas of general practice, starting with the Aboriginal Medical Service, where she stayed for more than 20 years.
She then branched out into mainstream general practices in Kelmscott, Willetton and Maddington, also working for Silver Chain Palliative Care Services for 10 years, aged care and the Street Doctor 360 Health mobile community medical services, which she continues to be part of.
Alongside her daughter Dr Priya Krishnan, Raji created Pramana

Medical Centre (PMC) in September 2021. The practice has doctors and nurses as well as a stable of allied health professionals and specialists, spanning social work, mental health and addiction specialists, to paediatrics, optometry and sleep therapy. They are a team ready to support the full spectrum of family medicine from birth.
While the practice is located in Gosnells, Raji spends a lot of time visiting her patients all over Perth and outer metro areas – in their homes or places they are comfortable to meet, such as a local park.
“There are many social determinants of health – one of the main ones is poverty –and there are often multiple competing issues in a person’s life, not just health concerns.
“I’ve tried to work according to the priority of the patient and now some of those relationships go back to the 1980s. I feel proud that people trust me and I have known some of those people for 30 years or more. They keep coming to see me, following me from practice to practice.
“I’m not interested in 10-minute medicine. I work according to the patient’s needs. That has always been very obvious to me – now it’s part of my DNA.”
For her service and care for vulnerable communities last year Raji received the RACGP WA Faculty’s GP of the Year and was awarded National GP of the Year at GP25.
In August, the AMA bestowed the President’s Award on her,
which acknowledges Raji’s tireless service to First Nations communities, pioneering of traumainformed and culturally safe care and leadership in shaping more equitable models of healthcare.
“These awards are so humbling and not something I ever expected to be granted in this lifetime,” she says. “For me it means a recognition of work over many long years, but moreover a recognition of the amazing team work I get to participate in with our wonderful group at PMC.
“Together we are able to address so many areas of unmet need and I am constantly learning in this process.
“Looking back over more than four decades in practice, the most significant shift I’ve witnessed hasn’t been in the conditions people present with, but in our understanding of what truly drives health in Aboriginal communities.
“When I started, mainstream general practice was – and largely still is – dominated by a biomedical model. It’s a model that serves some people well, but it simply doesn’t account for the social determinants of health that shape almost every aspect of Aboriginal wellbeing: intergenerational trauma, cultural dislocation, unstable housing and the harsh daily realities that make managing chronic conditions extraordinarily difficult.
“Mainstream general practice has been slow to meaningfully integrate these realities into routine care.
Continued on page 21



“Over the years, I realised that if we kept trying to treat medical problems in isolation from social ones, we were setting ourselves and our patients up to fail.
“The turning point for me was accepting that true healthcare – the kind that actually shifts outcomes – must bring medical and social support together under one roof. That insight pushed me to pioneer a more inclusive, interdisciplinary model of care, co-designed with our community and delivered as a unified team rather than a series of disconnected services.
“Australia’s health system has made world-class advances in primary and secondary care, but these advances have not translated into equivalent gains for Aboriginal people. What has made our model at PMC so effective is that we have always remained uncompromisingly patient-led.
“Every change we made began with listening to an individual’s story, identifying the barriers in front of them and updating our service to remove those barriers. Over time, these individual solutions have reshaped our entire practice, attempting to close local gaps one structural change at a time.”
When it came to setting up in private practice, Raji said she initially had great trepidation. Friends and colleagues had approached her over the years to join them and she had always declined.
But now, five years on and surrounded by a multi-disciplinary team who work enthusiastically under her guidance, she says for the first time in her career, she feels genuine optimism.
“We are finally seeing health system reforms – particularly in funding models – which begin to acknowledge the reality that primary care must operate differently if we are to close the gap. Just as importantly, I am seeing unprecedented collaboration: specialists and tertiary services working alongside us within general practice, rather than at arm’s length. This integration has transformed both outcomes and efficiency. I believe it represents

the most sustainable path to meaningful, long-term change.
“After 45 years, the lesson is simple but profound: when care is culturally grounded, patientled and delivered by a truly integrated team, the community not only engages – it thrives.”
This month, Raji will become a patient for a while after she has a knee replacement but looks forward to being back on her feet and seeing patients as soon as possible.
She has been training the team in her approach to continue during her recovery. Currently accompanied by a nurse practitioner and sometimes also a social worker, she has been seeing patients weekly in a nearby park and does home visits and drops in to a local women’s refuge.
“When you visit someone at home, there’s so many things you learn about their circumstances. They come and see you in clinic and they are sick and can’t relax, but when you visit their home you realise the water or sewage is not running properly, or there’s 10 people living in a house built for three.
“This might explain why they are sick, but they wouldn’t tell you
that sitting in the clinic. I think this is an integral part of medicine. People tell me it’s expensive, but I consider it too important.
While she has a very busy schedule, Raji makes time to indulge in her love for art, particularly Indian dance, and keeps closely connected to her cultural heritage and Hinduism. She’s vegetarian and loves to cook and experiment in the kitchen.
Raji hasn’t watched television in years but has discovered the marvels of YouTube and still argues there are not enough hours in the day.
“I’m a simple human being. But I also feel that God has given us each special things to do for humanity – and I have to do this. I love what I do. Every day is a new day and has challenges for us. I feel quite blessed to be able to contribute in this way.”
Such is Raji’s dedication that her daughter constantly reminds her (with good humour) that when her first grandchild was born, Raji was multitasking, standing outside the delivery room taking a phone call from an anxious patient – always recognising the urgency for that patient in the moment. Continued from page 19



Doctors over the age of 70 will not be required to undergo mandatory health checks to continue practising – a proposal that had attracted widespread criticism.
In a move labelled “commonsense” by the RACGP the Medical Board of Australia announced late last year that it would abandon its plans to introduce mandatory health checks for older doctors.
Instead, it said it would support older practitioners to continue working through ‘profession-led support’.
The Board had sought feedback in late 2024 on its plan to introduce mandatory health checks every three years for doctors aged over 70 and then every year from the age of 80 in a bid to reduce the number of notifications received about older practitioners.
It was widely criticised by the medical community including the RACGP and AMA.
The consultation was in response to a spike in patient complaints about older practitioners, with the rate of health-impairment related notifications for doctors aged over 70 more than three times higher than younger colleagues at the time.
New analysis from Ahpra shows regulatory action is taken on late career doctors at 1.6 times the rate of doctors aged under 70, with communication,
clinical care and medication concerns topping the list.
However, after collating responses to the consultation, the Board found no evidence that health checks would definitively reduce notifications.
Feedback showed general acceptance there was increased risk to patients from unsafe practice and unmanaged health issues among late career doctors, but disquiet about mandated health checks.
Board chair Dr Susan O’Dwyer said there were still clear issues in the practice of some doctors aged over 70 that health checks alone won’t address.
“We are keen to collaborate with the profession on supporting this group of doctors to keep their practice safe and their knowledge and skills up to date,” Dr O’Dwyer said.
The RACGP, which had argued that the focus should be on supporting doctors’ wellbeing rather than adding to the regulatory environment, welcomed the news.
President Dr Michael Wright said: “Mandatory health checks don’t reduce patient harms
or notifications. Instead, they risk increasing administrative burdens for GPs and worsening workforce shortages.
“Having worked with GPs in their 70s and 80s, including my father, I know the invaluable care our highly experienced senior GPs can offer.
“The most important message here is that no matter your age, everyone should have a regular GP, and that includes doctors themselves. What we need to do is reduce barriers that prevent clinicians from seeking this care and continue growing the GP workforce.”
AMA National President Dr Danielle McMullen said every doctor should have regular check-ups with a GP, but not as a regulatory requirement.
“Doctors who continue to practise beyond the age of 70, in most circumstances, do so with sound skill and judgment, adapting their scope of practice, workload, and procedures to mitigate risks and ensure patient safety,” she said.
“It is crucial to recognise their autonomy and the value of their extensive experience, while also safeguarding patient wellbeing.”

First of its kind research has found that general practice staff are commonly subjected to verbal violence and abuse, as well as physical violence and threats. We take a look at the steps you can take to prevent issues in your clinic.
By Aleisha Orr
The results of global research that found violence and abuse towards general practice staff was widespread did not come as a surprise to Dr Cameron Loy.
The research found that despite such behaviours having an impact on both individuals and service delivery, interventions were under researched.
Dr Loy is a former RACGP Chair, has been a GP for 25 years and now educates his colleagues on managing violent and aggressive patients. He told Medical Forum that he had experienced “the full spectrum” of violence and aggression.

That included a patient getting in his face and yelling aggressively, another knocking him on the head with their bag, one patient’s partner king hit him and another agitated patient returned to the clinic with a knife after their appointment.
Dr Loy believed such behaviour was not often talked about. The nature of the new research would suggest that has been the case.

The University of Nottingham research is among the first of its kind. In the past, when researchers had looked at violence and abuse towards healthcare staff by patients, it had tended to focus on secondary care facilities such as hospitals rather than general practice settings.
This research, published in the British Journal of General Practice, analysed 50 studies from 24 countries.
It showed that rates of violence and abuse by patients and the public towards general practice staff ranged from 13.8% to 90.3%, and career-long estimates were from 18.3% to 91.0%.
Verbal violence and abuse was most commonly reported, alongside physical violence, and threats. Less commonly reported were defamation, slander and vexatious complaints.
Unsurprisingly, it found the abuse and violence had an impact on staff mental health, turnover intention, and service capacity.
It identified long wait times and unmet patient demands as the most common factors influencing a patient’s behaviour.
GP ’s unique role
“General practice is in a unique position in that we get to enter some of the most private places of people’s lives – their health and their homes and their relationships,” Dr Loy said.
“We meet people often at the most vulnerable parts of their life and there are some people that just don’t know how to deal with that, and the way they deal with it is threats and punching.”
Dr Loy said while most patients were not a cause for concern, violent and aggressive behaviour at work could have a big impact on a GP.
He said the offenders were not always the people you might expect to be violent or aggressive, and that such behaviour often took GPs by surprise.
“We’re not in a job where we expect violence. If you’re in some jobs, a police officer for example, it’s understood you will likely be on the receiving end of some sort of violence during your working life because that’s the nature of policing,” he said.
“We’re not used to it and we don’t expect it, so when it comes out of the blue and when we start to feel and experience it, it’s very confronting for healthcare professionals and GPs.
“Some people are just angry, they are they are looking for something and they think that the way they’re going to get it is intimidation, threats, and violence. That is probably how they traverse their entire lives.
“But some people are unwell so sometimes, particularly with psychiatric disease, you’ll
have people who aren’t in their normal headspace.”
While there was little data to show whether GPs were dealing with increased levels of violence, Dr Loy said he could see there were certain factors contributing to violence and aggression.
He said he believed the increased cost of living and people’s financial stress was sometimes playing a role in poor behaviour.
“We’ve got a society that is really suffering from cost of living,” he said.
“We’ve got a government that in pursuing its objectives can paint general practices as being a problem, which feeds into it.
“For example, in clinics that haven’t signed up to the Medicare Bulk Billing Practice Incentive Program, it’s not infrequent for patients to come in and get upset that they’re paying a bill because the government told them it was going to be free.”
There was also a growing distrust of experts.
“The trust that we are acting in our patients’ best interests – that we’ve done 15 years of education and 25 years of work and ongoing education in medicine – that community understanding is getting broken down hard and fast,” Dr Loy said.
Dr Loy has taken a special interest in the factors around patient aggression towards GPs and spent time talking to other doctors about their experiences.
He himself has been caught off guard by a patient’s violence in the past.
Continued on page 27
“We meet people often at the most vulnerable parts of their life and there are some people that just don’t know how to deal with that”
Medicare Mental Health Centres offer free and confidential mental health support in communities across Perth for people aged 18 and over.
Walk-in support is available, or patients can book an appointment for counselling.
No Medicare card or referral needed.

| Midland | Mirrabooka | Gosnells
Medicare Mental Health 1800 595 212

Continued from page 25
“The most significant assault I experienced was when somebody caught me by surprise. They split my upper eyelid, knocked me out and broke some ribs when I was on the ground.
“And in that circumstance, I actually had other people in the room with me.”
Dr Loy said GPs should trust their instincts: “It’s that gut feeling which is often right on the money. If you feel at threat, you’re under threat, and at that point their only job is managing that threat.”
There are many interventions that can be used to prevent these issues occurring, such
If you believe you are not in immediate danger, try to de-escalate the situation by:
appearing calm and remaining respectful, controlled and confident
using reflective questioning – demonstrate that you are listening by confirming the message is right
being clear and direct in your language, and clearly and simply explaining your intentions
monitoring your body language and avoiding acts like crossing your arms and intense eye contact
assuring the patient your actions are in their best interest
engaging the patient by asking questions that are likely to elicit a ‘yes’. The most effective way is to briefly summarise the patient’s perceptions and views as you understand them, with questions at the end such as ‘Have I got that right?’ or ‘Is that what you mean?’


Complete four hours of CPD, including MO, with our Pelvic Venous Congestion podcast. Learn when to consider the diagnosis and how to manage it.
as posters discouraging bad behaviour, a no tolerance approach and duress alarms.
Dr Loy said while duress alarms may increase response times when a violent threat occurred, he had not seen evidence that their presence prevented violence in GP clinics.
He encouraged individual clinics to have their own approach to dealing with violent and aggressive patients and have processes in place to ensure such behaviour is documented.
He pointed to WorkSafe training in de-escalation tactics, as well as resources including physical posters to hang in waiting rooms reminding patients there should be zero aggression in the clinic.
“The important thing is having an absolute zero tolerance and following through with that,” he said.
“We need to make it absolutely clear within clinics that anything that is aggressive, threatening or violent, that’s it, you no longer come to the clinic.
“When you let a little bit get through, there’s always going to be a group that will push that boundary.
“Someone yelling and screaming could go on to a serious assault, that distance is shorter than nothing to a serious assault.”
Resources for managing patient violence and aggression are available on the RACGP website.
0.5 0.5 3
All eyes are on drugs of dependence as regulators increase scrutiny on who is prescribing and being prescribed these drugs, writes Kate Reynolds, Barrister, Francis Burt Chambers.
Across all Australian jurisdictions, there has been a purposeful and deliberate leap towards tighter regulation and stricter monitoring of Schedule 8 and reportable Schedule 4 medications.
Here, in Western Australia, the Medicines and Poisons Act 2014 (the Act), the Medicines and Poisons Regulations 2016 (the Regulations), together with the Department of Health’s Monitored Medicines Prescribing Code authorise what is monitored and how this is managed.
It is now compulsory for practitioners to register with ScriptCheckWA prior to prescribing, dispensing, or supplying a monitored medicine as per 22A of the Regulations. However, it is not yet mandatory to use the system prior to prescribing. It is likely that WA will follow suit with other states and territories, where use of script monitoring systems has been mandatory in some jurisdictions since 2020.
While WA has had a prescription monitoring program for over 20 years, ScriptCheckWA now offers a real time prescription monitoring system allowing prescribers and pharmacists access to upto-date information as to what has been prescribed, dispensed and supplied to patients.
The purpose being to alert practitioners to patients who are drug dependent, those who may be at risk of over-supply, and those who engage in doctor shopping.
All practitioners must be individually registered and login data allows transparency for prescribers, dispensers and regulators as to whom has accessed the system on each occasion.
Only those patients with whom a prescriber has a treating relationship should


be accessed. You should assume that unauthorised access will be monitored.
Be under no illusion, attention is being paid. Authorised Department of Health officers access ScriptCheckWA as part of their regulatory role and the data obtained forms part of the State’s Drugs of Addiction Record.
A recent spike in regulatory action targeting Australian health practitioners suggests that regulators are intensifying their scrutiny of real time prescription system compliance.
The chief executive officer of the Department of Health may take action against a practitioner whose conduct is in contravention of the Act. This includes imposing conditions, suspending or cancelling the practitioner’s professional authority.
If a practitioner in their professional capacity forms an opinion that a patient is drug dependent, then a mandatory report must be made within 48 hours of forming such an opinion. Failure to do so may incur a fine of $5,000.
Authority of the chief executive is required when prescribing a drug of
dependence to a drug-dependent patient. This is in addition to the requirement for PBS authority.
A practitioner who, without authority, prescribes a drug of addiction for a person whose name is included on the Drugs of Addiction Record as a drugdependent person, commits an offence. A fine of up to $30,000 could be imposed.
Prescribing drugs of dependence
From a Medical Board perspective, part four of the Good medical practice: a code of conduct for doctors in Australia sets out how medical practitioners should work to develop good doctorpatient relationships, and this includes effective communication as to any prescriptions or other medications prescribed.
Further, part eight details risk management strategies to improve patient safety including participation in systems for surveillance and monitoring of adverse events and near misses, which would encompass effective use of resources such as ScriptCheckWA.
"It
Per part 4.15 of the Code, medical practitioners must not – amongst other things – prescribe Schedule 8 or drugs of dependence to anyone with whom they have a close personal relationship. Selfprescribing of a drug of addiction is an offence under the Act.
According to the Ahpra regulatory guide, conduct involving inappropriate prescribing of scheduled medicines may prompt the Board to take immediate action to protect the public from serious risk.
Such interim measures may include conditions on a practitioner’s registration or suspension. Prescribing may also be a causal factor in the Board requesting a practitioner undergo a
Hear from WA specialists on common presentations in General Practice including:
Management
discussing HRT considerations
performance assessment or attend a professional standards panel in order to determine whether a practitioner’s practise of the profession is unsatisfactory or not.
A reasonable belief of professional misconduct will result in a referral to the tribunal. Penalties applied vary depending on circumstances.
0.5 0.5


When it comes to the experience of poor mental health, particularly with eating disorders, practitioners are often reluctant to seek help, writes Clinical Psychologist Pheobe Ho.
As medical and health practitioners, we preach proactive self-care for the physical and mental wellbeing of our patients.
However, many of us may not heed our own advice: rates of depression, anxiety, suicide and overall psychological distress are significantly higher among medical practitioners compared to the general population.
This is not surprising, given practitioners can experience work-related stress, burnout and even vicarious trauma.
One area warranting special attention is eating disorders. It is estimated 24-47% of eating disorder practitioners have their own past or current eating disorder, contrasting with the 2-8% lifetime prevalence rates in the general population.
Eating disorders bring unique challenges. They are psychiatric illnesses with one of the highest mortality rates, entailing significant medical and psychological impacts.
There is also a lack of available services compared to other areas of mental health.
Finally, a unique consideration is how patients can perceive practitioners’ bodies and appearance in treatment – which can be further complicated if a practitioner is currently experiencing an eating disorder.
The challenges faced
If you had a heart attack, you would see a cardiologist, even if you were a cardiologist yourself.
However, when it comes to experiences of mental health, including eating disorders, practitioners are often reluctant to seek support.
Stigma, shame and fears of professional repercussions may
prevent practitioners from seeking help. They may fear loss of their Ahpra registration or how their professional reputation is impacted.
Practitioners with lived experience may grapple with deciding whether to disclose to their workplace. While disclosure can lead to increased workplace supports, uncertainty around how line managers, supervisors or colleagues may respond precludes disclosure.
Eating disorders can involve a focus on body weight and appearance. If colleagues are aware of a practitioner’s eating disorder history, changes in their appearance can lead colleagues to question the practitioner’s wellness, even if they are well.
This knowledge may also affect how colleagues perceive the practitioner’s professionalism or performance. Eating disorder practitioners with lived experience warrant special considerations.

It is crucial to seek supervision and your own supports, through personal or workplace channels. It can also be helpful to ask yourself the following questions:
• What symptoms of an eating disorder am I experiencing, and are these impacting my work with patients?
• What strategies am I using, personal and professional, for my wellbeing?
• When should I seek supervision from a colleague or manager to determine that my clinical judgment is not adversely impacted by my symptoms?
• What supports do I need at work? Should I continue practising if I have an eating disorder currently?
• Should I let a line manager or supervisor know? How much do I let them know, and what reasons are there to tell them?

"When it comes to experiences of mental health including eating disorders, practitioners are often reluctant to seek support . "
• What is the best way for me to address a dual relationship if I am receiving treatment at a service my own patients also attend?
Supporting colleagues
As a colleague, you may consider the following:
• What should I say to a colleague if I think they are unwell with an eating disorder and are concerned that it may be impacting on their patient care?
• Does my knowledge of a colleague having an eating disorder affect how I interact with them or think about them?
If you are a manager or supervisor, you may consider the following:
• What processes could be implemented for new and existing employees who inform they have a current or past eating disorder?

• What supports should be put into place at work for practitioners with current or past lived experience, to ensure safe and ethical practice?
• What supports can be provided at work for employees during leave related to their mental health? How can a return-towork plan be jointly developed?
• What are the best ways to manage a dual relationship when an employee informs that they are working alongside a past or current practitioner for their own treatment?
• What do I understand about the obligations for mandatory reporting to Ahpra, clinical impairment, and fitness to practice requirements?
Leading by example
Building a mentally healthy workforce involves eating disorder
practitioners coming together to have supportive conversations. This is key for workforce sustainability and retention.
Supporting practitioner wellbeing will enhance the quality of care provided for patients, thereby improving their outcomes.
We owe it to our patients to put into place the advice we give.
Research conducted at Curtin University aims to better understand and support eating disorder practitioners with lived experience. With support from several Australian peak eating disorder bodies, it is hoped that results from a recent nationwide survey will inform future development of guidelines.
These guidelines will help eating disorder organisations worldwide support practitioners with lived experience and provide an exemplar for other fields of health and mental health.
ED: Pheobe Ho is a PhD Candidate specialising in eating disorders. She is involved in the research at Curtin University.
Medical Forum is now an approved RACGP CPD provider for general practitioners, offering EA, RP and MO modules

Look for the RACGP CPD logo on Medical Forum content to complete your annual CPD hours.
Scan the QR code in the magazine or follow the links on our website to complete the activity requirements.
Your hours will be automatically added to your RACGP CPD home seven days after completion.

DR MAREK GARBOWSKI

Complete four hours of CPD, including MO, with our Pelvic Venous Congestion podcast. Learn when to consider the diagnosis and how to manage it.

Adverse medical outcomes from individual doctors are typically examined with a view to change and improvement. Public health should be no different.
There is a wonderful quote from economist Milton Friedman: “One of the great mistakes is to judge policies and programs by their intentions rather than their results.”
In health we can be guilty of this. It was evident in the latest health and wellbeing of adults survey run by WA Health, which found most aspects of the population’s health was declining.
The survey of 13,780 people revealed the number of people rating their health as very good or excellent fell 10% in the last decade and was now under 50%.
Smoking rates increased by 1% from 2023 to 13.5%. Use of illicit drugs and harmful use of alcohol also increased 1%.
Consumption of fast food has also increased over the decade. On the plus side obesity was down 1% on 2023, but still up 10% from 2014.
What are we to make of this? If we are honest, we would question current policy settings. They are well intended but clearly not having the intended results.
There is a growing view that tobacco taxation has reached a point of being counterproductive, with people going to the black market where the cost is about a quarter of that bought legally.
Is the quit message losing effect? Smoking rates suggest so.
Are current dietary guidelines, as adopted in the early 1980s working? Obesity rates suggest not.
More of the same cannot be the answer. Adverse medical outcomes from individual doctors are typically examined with a view to change and improvement. Public health should be no different.





By Dr Stuart Salfinger, Gynae-Oncologist, Subiaco
Endometrial cancer is the most common gynaecological malignancy in the first world, with incidence rising in parallel with obesity, metabolic disease, and population ageing.
General practitioners play a pivotal role in early recognition, investigation and referral as prognosis is strongly linked to stage at diagnosis. The majority of endometrial cancers are cured, usually by surgery alone.
Epidemiology and risk factors
Endometrial cancer primarily affects postmenopausal women, with a median age at diagnosis of approximately 60 years. However, up to 10% of cases occur in premenopausal women, including a small proportion under the age of 40.
The dominant risk factor is unopposed oestrogen exposure. This may be endogenous (e.g. obesity, polycystic ovary syndrome) or exogenous (e.g. oestrogen-only hormone replacement therapy). Additional risk factors include:
• Obesity and metabolic syndrome
• Type 2 diabetes mellitus
• Nulliparity and infertility
• Early menarche and late menopause
• Tamoxifen use
• Lynch syndrome (hereditary non-polyposis colorectal cancer)
Conversely, combined oral contraceptive use and progesterone-containing intrauterine devices are protective.
Clinical presentation
Abnormal uterine bleeding (AUB) is the hallmark symptom and should always prompt consideration of endometrial cancer, particularly in postmenopausal women.

Key presentations include:
• Postmenopausal bleeding (PMB) – endometrial cancer (or atypical hyperplasia which is preinvasive change) is diagnosed in approximately 10-20% of women presenting with PMB
• Intermenstrual or irregular bleeding in perimenopausal women
• Heavy or prolonged menstrual bleeding in younger women with risk factors
• Less commonly, pelvic pain, abnormal vaginal discharge, or systemic symptoms in advanced disease.
Importantly, even a single episode of postmenopausal bleeding warrants investigation, regardless of bleeding volume or duration.
Initial assessment
The GP’s role is to identify atrisk patients and initiate timely investigation and referral.
Assessment should include a full menstrual and bleeding history, menopausal status,
medication review (including HRT and tamoxifen), relevant risk factors (BMI, diabetes, family history) and pelvic examination where appropriate to assess for alternative causes of bleeding. Cervical screening status should be reviewed, but a normal smear does not exclude endometrial pathology. Postmenopausal bleeding should be referred urgently, for example through a suspected cancer pathway.
Transvaginal ultrasound (TVUS) is usually the first-line investigation. An endometrial thickness <4mm in a woman with PMB is associated with a very low risk of malignancy.
Thickness >4mm, persistent bleeding, or inadequate imaging necessitates further assessment.
Definitive diagnosis requires endometrial sampling, which may be performed in secondary care via pipelle biopsy –blind sampling of the endometrium – or hysteroscopy with directed biopsy, considered the gold standard for investigation of PMB.
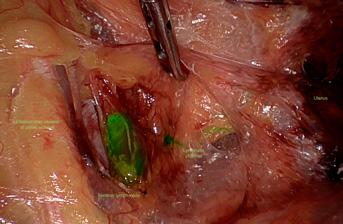
Premenopausal women with persistent abnormal bleeding and significant risk factors should also be considered for referral, particularly if symptoms are refractory to medical management.
Pathophysiology and classification
Endometrial cancers are broadly classified into two types.
Type I (endometrioid): oestrogen-dependent, more common, often low grade, and associated with better prognosis.
Type II (non-endometrioid): includes serous and clear cell carcinomas, typically
oestrogen-independent, higher grade, and more aggressive.
Understanding this distinction is useful when counselling patients, though management decisions are specialist-led.
Management and follow up
Primary treatment is usually surgical, consisting of total hysterectomy with bilateral salpingo-oophorectomy. Complete pelvic lymph node dissection in selected patients has now been replaced with sentinel lymph node biopsy, which should be considered standard of care.
Adjuvant radiotherapy or chemotherapy may be required for higher-risk disease.
Selected patients with early-stage disease who wish to preserve fertility may be candidates for conservative hormonal management under specialist care.
Prognosis is generally favourable when diagnosed early. Five-year survival exceeds 90% for stage I disease but falls significantly with advanced stages. The outcomes are so good for most patients with
low-risk disease they do not require gynaecologic oncology follow up.
GPs play an important role in survivorship care, including monitoring for recurrence symptoms, managing long-term treatment effects (e.g. menopausal symptoms, lymphoedema) and supporting psychological wellbeing While specialist advice should be sought, most of these patients can be safely prescribed oestrogen replacement therapy if required. Maintaining a low threshold for investigation and referral is central to improving outcomes for women with endometrial cancer.
Author competing interests – nil


By Dr Qurrat van den Blink, Radiation Oncologist, Joondalup/Wembley
Osteoarthritis (OA) is one of the most common and disabling conditions seen in general practice. Many patients fall into a difficult therapeutic gap: too symptomatic for conservative care alone, yet not severe enough for joint replacement.
Low-dose radiotherapy (RT), long used in Europe, is now reemerging as a potential option for selected patients with persistent pain and moderate disease.
Traditional management of OA centres on exercise, weight loss, analgesia and intra-articular injections. However, non-steroidal anti-inflammatory drugs carry gastrointestinal, renal and cardiovascular risks, and steroid injections may accelerate cartilage thinning with repeated use.
The Kellgren-Lawrence grading system classifies OA severity based on radiological appearances (Grade 0-4) and is used to evaluate progression of OA.
Large numbers of patients can remain symptomatic for years. Many struggle to participate in physiotherapy programs, poorly tolerate or are contraindicated for standard analgesics.
Low-dose RT may offer an option to improve pain sufficiently to allow patients to resume exercise-based therapy.
OA has traditionally been considered a mechanical “wear-and-tear” condition. This model explains part of the disease process – some patients demonstrate severe structural damage with little pain, while others with modest changes experience significant symptoms.
Current evidence supports a more complex inflammatory and immune-mediated pathway. Synovitis is recognised as a central driver of pain and progression.
Activated macrophages and fibroblasts release proinflammatory cytokines that
accelerate cartilage breakdown and alter subchondral bone.
Low-dose radiotherapy (typically delivered in six treatments) has anti-inflammatory and immunomodulatory effects. It down-regulates pro-inflammatory cytokines, reduces macrophage activity and may slow the inflammatory cascade that contributes to joint degeneration.
While not a cure for osteoarthritis, evidence suggest that low-dose radiotherapy may become an important adjunct in managing this increasingly common condition.

response at four months compared to 40% in the sham treatment arm.
Improvements were seen in pain, function and patient-reported quality of life with no significant toxicity. Most patients included had moderate OA (KL grade 2-3).
Other studies report improved physical function, lowering pain scores and reduction in rates of joint replacement.
Overall, when applied to selected patients, low-dose RT appears to reduce pain, improve function and, in some cases, delay progression.
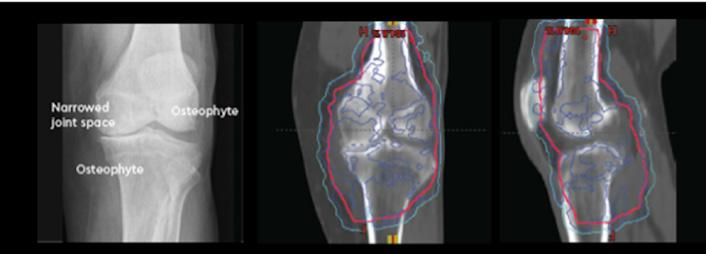
European experience spans decades, with multiple randomised and prospective studies reporting meaningful pain improvement in hands, knees, feet and shoulders.
Typical response rates range from 60–70% at 3–12 months, depending on site and study design.
Earlier small Dutch trials reported no benefit compared with sham treatment, generating debate; however, these studies included high proportions of severe (KLgrade 4) OA, single-course treatment only, and inconsistent control of concomitant analgesia.
More recent larger studies are changing the narrative. A randomised Korean study (2025) involving 114 patients receiving low dose versus sham radiotherapy demonstrated a 70% clinical
GPs play a central role in identifying patients who may be suitable for low-dose RT. These include:
• Patients over 50 years
• Kellgren–Lawrence grades 1–3 (mild–moderate OA)
• OA involving upper and lower limbs
• Persistent pain despite structured conservative management
• Intolerance to or failed NSAIDs or steroid injections
• Patients limited in physiotherapy participation due to pain.
Low-dose RT may not be helpful in severe OA or for those seeking a rapid resolution of symptoms without addressing underlying biomechanics.
The spine is less commonly treated due to a much higher bone marrow exposure to radiation and theoretical risk of leukaemia.
Key messages
• Low-dose radiotherapy provides meaningful pain relief for 6070% of patients with moderate osteoarthritis who have failed conservative management
• Treatment is best suited for mildmoderate OA (Kellgren- Lawrence G1-3) and is safe, well tolerated and does not preclude future joint replacement
• Low-dose radiotherapy aims to reduce pain enough to resume physiotherapy and delay potential surgery, bridging a therapeutic gap.
Low-dose RT involves <5% of radiation required to treat cancers, giving very low toxicity. There are no acute effects and extremely low risks of secondary cancers (skin cancer estimated at 0.2% and rarely soft-tissue sarcomas).
Pain responses are typically noted within 6-12 weeks and if maintained at three months, they may persist to a year or longer. Most patients require only one course but 20-30%
Grade 0 No radiographic evidence of OA
Grade 1 No joint space narrowing (JSN) but possible osteophytic lipping
Grade 2
Definite JSN and definite osteophytes
Grade 3 Moderate and multiple osteophytes, definite JSN, sclerosis, possible bony deformity
may opt for a second course if they obtain a partial response.
Importantly, low-dose RT does not impair future joint replacement surgery, based on available long-term data.
A useful work-up prior to referral for low-dose RT includes plain X-ray with request for Kellgren–Lawrence grading, documentation of pain severity (VAS 0–10), summary of prior management attempts (analgesia, physiotherapy, injections), assessment of functional impact and mobility limitation, and counselling that RT aims to reduce pain, not regenerate cartilage.
Grade 4 Large osteophytes, marked JSN, severe sclerosis and definite bony deformity If you are looking to redefine women’s health, join our new Shenton Park team.

Referred patients will undergo further assessment, discussion of risks and benefits, and education on expectations and follow-up.
Author competing interests – nil
0.5 0.5 hours

“My period pain is totally normal.”

By Dr Amit Saha, Paediatric Gastroenterologist, Hollywood
Feeding-related symptoms in infancy account for a substantial proportion of general practice consultations, with gastrooesophageal reflux, gastrooesophageal reflux disease (GORD), and cow’s milk protein allergy (CMPA) frequently considered in the differential diagnosis.
They each have overlapping clinical features such as regurgitation, irritability and feeding difficulty.
This conceptual overlap can contribute to significant overtreatment, particularly through unnecessary use of acid suppression therapy and dietary elimination.
A structured clinical framework that clearly distinguishes the two is essential.
Physiological gastro-oesophageal reflux (GOR) is a normal developmental phenomenon in infancy, resulting from immaturity of oesophageal motility, transient lower oesophageal sphincter relaxations, a predominantly liquid diet, and supine positioning.
Regurgitation is common, occurring in up to two-thirds of infants, peaking at three to four months of age and generally resolves spontaneously by 12 months.
It is not associated with pain, tissue injury, or impaired growth; affected infants are typically well, settled between feeds, and thriving, reflecting a benign functional process rather than disease.
GORD, by contrast, is defined not by the presence of reflux alone, but by reflux that results in troublesome symptoms or complications.
In infancy, true GORD is uncommon. It may manifest as persistent feeding refusal, significant distress temporally related to feeds, faltering growth, or complications such as oesophagitis.


Critically, most infants who regurgitate do not have GORD, and the distinction between physiological reflux and disease rests on clinical impact rather than frequency or volume of vomiting. Further complexity arises from the distinction between acid and non-acid reflux.
In early infancy, gastric contents are frequently non-acidic due to buffering by milk feeds and relatively immature gastric acid secretion. Consequently, the majority of reflux events in young infants are non-acidic.
This physiological reality explains why symptoms such as regurgitation and irritability often persist despite acid suppression therapy. Proton pump inhibitors reduce gastric acidity but do not reduce the frequency of reflux events, nor do they improve symptoms in infants without acid-mediated mucosal injury.
This physiological reality underpins the consistent lack of efficacy of acid suppression and explains the disconnect between symptom burden and therapeutic response.
Cow’s milk protein allergy CMPA is an immune-mediated disorder affecting a minority of infants, with non-IgE-mediated disease predominating in early life. Gastrointestinal manifestations may include vomiting, diarrhoea, rectal bleeding, and feeding aversion, but these symptoms rarely occur in isolation.
It is more likely when gastrointestinal symptoms coexist with extra-intestinal features such as eczema, faltering growth, or a family history of atopy.
Importantly, CMPA does not cause reflux per se; rather, allergic inflammation may increase gut sensitivity and alter motility, producing symptoms that mimic or exacerbate reflux. Clinical assessment remains central to differentiation. Isolated regurgitation in a thriving infant strongly favours physiological GOR. Persistent distress, feeding refusal, or growth impairment suggest pathological processes such as GORD or CMPA, with multisystem involvement favouring the latter.
A key clinical principle is that reflux alone (acid or non-acid) rarely accounts for significant growth faltering or sustained distress. When these features are present, alternative diagnoses should be actively considered.
Follow a stepwise, phenotypedriven approach. In physiological GOR, parental education and reassurance are paramount. Explaining the natural history of reflux and normalising symptoms can significantly reduce parental anxiety and unnecessary intervention. Feeding review, avoidance of over-feeding, and consideration of feed thickening may reduce visible regurgitation, although effects on irritability are limited.
Avoid acid suppression in the absence of clear evidence of GORD, given its lack of efficacy for non-acid reflux (vast majority of these babies).
When CMPA is clinically suspected, a structured diagnostic elimination trial is appropriate. Formula-fed infants should be commenced on an extensively hydrolysed formula, while breastfed infants may require maternal cow’s milk protein exclusion.
Symptom improvement is typically observed within two to four weeks if CMPA is the underlying cause.
However, improvement alone does not confirm diagnosis. Planned rechallenge is essential to establish causality and prevent unnecessary long-term dietary restriction, which remains a major contributor to overdiagnosis and subsequent long-term feeding challenges.
Overtreatment
Despite this evidence, infant reflux has become one of the most medicalised and over-treated conditions in early life, with escalating use of acid suppression and specialised formulas, often initiated within weeks of birth.
Highly visible symptoms, parental anxiety, time-pressured consultations, and overlapping clinical phenotypes all contribute to overtreatment.
The absence of visible improvement within a few days, rather than the expected few months, can be seen as diagnostic failure, prompting escalation rather than reflection.
Prescribing medication or changing formula can feel more tangible than reassurance, even when evidence is limited. When reassurance fails, reflux becomes GORD; when medication fails, allergy is assumed – each step legitimising further escalation, even though the underlying symptoms remain unchanged.
Fear of missing pathology further biases clinicians toward intervention, despite increasing recognition that unnecessary treatment carries its own risks; with growing evidence linking longterm acid suppression to infection risk and microbiome alteration.
The greatest risk to infants with reflux is not under-treatment but over-treatment, stemming from diagnostic uncertainty.
Reframing reflux as a developmental process rather than a disease state, and defining pathology by impact rather than symptom presence, are critical steps toward rational care – reserving interventions for infants who fail to thrive or exhibit multisystem involvement, thereby reducing harm while maintaining vigilance.
In an increasingly medicalised healthcare landscape, reclaiming the normality of infancy with rational, developmentally informed care may be one of the most effective interventions available to primary care clinicians.
Author competing interests – nil
0.5 0.5


By Jeff Butterfield, Clinical Nurse Specialist, Alcohol and other Drug Assessment, Referral and Recovery
Alcohol misuse remains pervasive and frequently under-recognised in Australian primary care. Patients often present with disease, injury, or reduced quality of life linked to alcohol, yet may not identify their drinking as problematic.
Shame, embarrassment, or fear of judgement can limit disclosure, meaning alcohol-related harm is often hidden behind presentations that appear unrelated.
General practitioners are uniquely positioned to identify early risk and intervene before harm escalates. By noticing subtle cues and exploring them respectfully and safely, primary care can alter trajectories and support timely change.
Alcohol is the most widely used drug in Australia. Around 77% of adults consume alcohol, with approximately one-third drinking at levels increasing the risk of injury or disease.
While consumption among younger adults is declining, alcohol still contributes to more than 150,000 hospital admissions and around 6,000 deaths each year.
In Western Australia more than 20,000 hospitalisations in 2019 were alcohol related. These figures highlight the central role of general practice in early detection and prevention.
Alcohol-related harm often presents indirectly. Common cues include sleep disturbance or fatigue, anxiety or low mood, gastrointestinal complaints, recurrent injuries or sick-leave requests, and hypertension in younger or otherwise low-risk patients.
These presentations create opportunities to explore whether alcohol may be contributing. Simple, curious questions can open the conversation:
“Do you drink alcohol at the moment?”
“How often are you using alcohol across the week?”
“How many alcohol-free days do you usually have each week?”
“Do you feel in control of your drinking?”
Questions framed with curiosity rather than judgement reduce stigma and invite more honest responses.
Validated screening tools support clinical impressions and help patients visualise risk. The Alcohol Use Disorders Identification Test (AUDIT) is the most widely used tool in Western Australia and is promoted by the Mental Health Commission of Western Australia. When time is limited, the AUDIT-C offers a brief threequestion alternative.
Results can be discussed simply by categorising risk as low, risky, or high risk.

For very brief screening, the CAGE questionnaire can assist by asking whether a patient feels the need to Cut down, becomes Annoyed by criticism, feels Guilty, uses alcohol as an Eye-opener.
Though the CAGE questionnaire is less sensitive for earlystage misuse. Other tools (e.g. ASSIST, MAST, and SADQ-C ) can be more time-consuming
Brief GP interventions of just two to five minutes have been shown to significantly reduce risky drinking. Structured approaches such as FRAMES and FLAGS provide practical, evidencebased frameworks that fit well within routine consultations.
The FRAMES model highlights the therapeutic ingredients of effective brief intervention:
• Feedback provides individualised information about risk
• Responsibility emphasises that change is the patient’s choice
• Advice offers clear clinical recommendations

• Menu involves offering a range of practical options
• Empathy reduces shame and defensiveness.
• Self-efficacy reinforces the patient’s strengths and capacity for change.
The FLAGS model also provides a similar approach.
Both frameworks are enhanced when delivered using a motivational Interviewing style.
Helpful prompts include:
“What concerns you about your current pattern?”
“How is alcohol affecting your lifestyle?”
“What small change feels achievable this week?”
These conversations plant the seed for change rather than attempting to resolve the problem in a single visit.
Escalation should be considered when there are no alcoholfree days, morning drinking or withdrawal symptoms, relationship or work disruption, or persistent hypertension or liver function abnormalities.
These indicators suggest unassisted reduction may be unsafe.
Patients with heavy or prolonged alcohol use are at risk of thiamine deficiency, which can lead to Wernicke’s encephalopathy and progression to Korsakoff’s syndrome.
Initiating oral thiamine supplementation, commonly 100mg tds reduces neurological risk and can be commenced immediately while further assessment and referrals are arranged.
Primary care remains central, but shared care improves safety and outcomes.
Referral options include Community Alcohol and Other Drug Services in metropolitan areas, private alcohol and other drug clinicians for rapid access and relapse-prevention support and peer support programs.
GPs can also access free specialist guidance through the Drug and Alcohol Clinical Advisory Service (DACAS) on (08) 6553 0520.
DACAS provides advice on pharmacotherapy, withdrawal risk assessment, suitability for ambulatory withdrawal, and when inpatient withdrawal is indicated. Alcohol harm often hides behind routine consultations. By noticing subtle cues, asking about alcoholfree days, screening proactively, offering brief intervention, and involving specialist supports early, general practice can act as a powerful safeguard against alcoholrelated illness and hospitalisation. A short, curious question today may change the trajectory of a patient’s life.
Author competing interests - nil


- Ground, T6 of 718sqm*: Comprises a cold shell with high ceilings, lighting, kitchenette and disabled toilet.
- Suitable for medical, consulting or office users.
- Full ground level





By Dr Mahmoud Al-Najjar, Vascular & Endovascular Surgeon
Superficial vein thrombosis (SVT) is frequently encountered in general practice, often presenting as a painful, erythematous, cord-like swelling along a superficial vein. Traditionally considered benign, SVT is now recognised as part of the venous thromboembolism (VTE) spectrum, alongside deep vein thrombosis (DVT) and pulmonary embolism (PE).
Up to 20-25% of patients with SVT have a concurrent DVT or PE at diagnosis, including asymptomatic events. Risk is greatest when thrombus is extensive, recurrent, or close to deep venous junctions.
For general practitioners, identifying higher-risk SVT and applying a structured, risk-based approach is critical to prevent progression while avoiding unnecessary anticoagulation in low-risk cases.
Patients typically present with localised pain, erythema, warmth, and tenderness along a superficial vein, often with a palpable cord. The great saphenous vein and small saphenous vein are most commonly involved.
Significant limb swelling, proximal symptoms, or pain out of proportion should prompt urgent exclusion of DVT.
SVT may mimic cellulitis or lymphangitis, particularly early. Upper-limb SVT is often related to intravenous cannulation and is usually localised and self-limiting.
First-episode SVT in patients over 40 years without obvious provoking factors, or recurrent or migratory SVT, should prompt consideration of malignancy or thrombophilia.
SVT shares many risk factors with DVT, including varicose veins, immobility, obesity, recent surgery or trauma, intravenous cannulation, hormonal therapy, pregnancy (especially postpartum), active malignancy, inherited thrombophilia, smoking, increasing age, and previous VTE.
Superficial veins drain into the deep system via the saphenofemoral and saphenopopliteal junctions. Thrombus within 3cm of these junctions carries a high risk of extension into the deep veins and pulmonary embolism.
Perforator veins allow propagation from superficial to deep veins, particularly in the presence of venous reflux or varicosities.
Duplex ultrasound is the investigation of choice. It confirms SVT, defines thrombus length and location, assesses proximity to deep venous junctions, and excludes associated DVT.
Ultrasound is recommended in most patients, particularly if SVT is proximal, extensive, recurrent, atypical, or associated with VTE risk factors.
Isolated, short SVT confined to varicose veins in low-risk patients may be diagnosed clinically with ultrasound. Request thrombus length, distance from the saphenofemoral or

saphenopopliteal junction, and whether DVT is present. D-dimer testing has no role.
SVT is stratified according to thrombus characteristics and patient risk:
Low risk: Thrombus ≥ 3cm and less than 5cm in length from deep venous junctions, no additional risk factors. Anticoagulation is not required. Management includes NSAIDs for 7-14 days, mobilisation, limb elevation, warm or cool compresses, and graduated compression stockings (if no contraindications). Patient education is essential.
Intermediate risk: Thrombus ≥ 5cm in length or within 3cm of deep venous junctions. Prophylactic-dose anticoagulation is recommended for 45 days. Options include Fondaparinux (2.5mg subcut OD), Enoxaparin (40-80mg subcut OD), Rivaroxaban (10mg daily) or Apixaban (2.5mg bd). Follow-up is required to ensure symptom resolution and exclude thrombus progression.

Key messages
• Superficial vein thrombosis is part of the venous thromboembolism spectrum and may progress to DVT or PE
• Duplex ultrasound is central to diagnosis, risk stratification, and management decisions
• Anticoagulation dose and duration should be guided by thrombus length, location, and patient risk factors.
High risk: Thrombus ≤ 3 cm from deep venous junctions, propagation, recurrent SVT, thrombophilia, or malignancy. Treat as DVT with therapeutic anticoagulation for three months. Options are Enoxaparin (subcut 1mg/kg bd or 1.5mg/kg OD), Rivaroxaban (15mg bd for 21 days then 20mg OD) or Apixaban (10mg bd for seven days then 5mg bd). Early referral to vascular surgery or haematology is recommended.
Special populations
Pregnancy: Direct oral anticoagulants are contraindicated. Use low-molecular-weight heparin with specialist input for extensive disease.
Renal impairment: Avoid Rivaroxaban if eGFR <30 mL/min. Dose-adjusted Enoxaparin may be required.
Malignancy: Anticoagulation is recommended for at least 45 days and often longer, depending on ongoing risk.
All patients should be counselled on symptoms of DVT and PE, including worsening leg swelling, chest pain, and dyspnoea.
Repeat duplex ultrasound within 7-10 days is advised for intermediate and high-risk cases or if symptoms worsen. Addressing modifiable risk factors and considering definitive varicose vein treatment may reduce recurrence.
SVT is a clinically significant thrombotic condition rather than a benign complaint. A structured,
risk-based approach using duplex ultrasound and appropriate anticoagulation allows GPs to manage SVT safely and effectively, preventing progression while avoiding overtreatment.
Author competing interests – nil



What is your area of practice?
I am a consultant radiation oncologist in full-time private practice in Perth, seeing patients at GenesisCare Joondalup, Wembley and Murdoch.
My clinical practice focuses on lung cancer, head and neck malignancies, breast and skin cancers, and the management of oligometastatic disease. Alongside malignant conditions, I also treat selected benign diseases where there is emerging evidence for the use of radiotherapy, including inflammatory and degenerative conditions such as osteoarthritis.
I have a strong interest in technically complex radiotherapy and the application of advanced techniques to improve treatment precision, safety and patient outcomes.
Where did you train?
I completed my medical degree at the University of Liverpool in the United Kingdom in 2003, followed by physician training and specialist training in Clinical Oncology at The Christie Hospital in Manchester and Lancashire Teaching Hospitals.
In 2013, I undertook an international fellowship at the Princess Margaret Cancer Centre in Toronto, with a focus on advanced and stereotactic radiotherapy techniques. After relocating to Australia in 2020, I completed fellowships at Sir Charles Gairdner Hospital in Perth and Princess Alexandra Hospital in Brisbane and was awarded Fellowship of the Royal Australian and New Zealand College of Radiologists (RANZCR) in 2022.

What procedural services do you offer?
I specialise in modern external beam radiotherapy, including intensity-modulated radiotherapy (IMRT) and stereotactic body radiotherapy (SABR), particularly for lung cancers and oligometastatic disease.
I also have extensive experience in the management of head and neck cancers and in delivering technically complex treatments where accurate target definition, motion management and image guidance are critical to safe and effective radiotherapy.
How is your service different?
My practice is holistic and combines high-level technical expertise with a strong emphasis on collaboration and continuity of care. I am actively involved in lung and head and neck specialist groups, contributing to protocol development, quality assurance and multidisciplinary care pathways.
A key focus of my work is raising awareness of the evolving role of radiotherapy as a modern, effective treatment option across a range of cancers and disease stages. I am involved with Targeting Cancer, an initiative aimed at improving understanding of radiation therapy among patients, clinicians and the wider health community. Through education and professional engagement, I aim to support informed referral pathways and ensure radiotherapy is appropriately considered within multidisciplinary cancer care.
I place particular importance on clear communication, thoughtful treatment planning and close collaboration with referring doctors, ensuring care is well coordinated from diagnosis through treatment.
My practice is holistic and combines high-level technical expertise with a strong emphasis on collaboration and continuity of care.
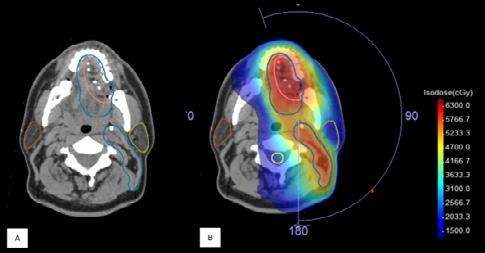
Radiotherapy contours (blue/pink) for a post-operative oral cavity head and neck cancer.
B: Radiotherapy plan delivering high dose to planned volume with lower and avoidance areas including parotid glands (brown and yellow contours).

By Tania Norman, Stomal Therapy Nurse, Mt Lawley
An ostomate is a person who has had surgery that results in the diversion of urine or faeces onto the abdomen via an opening referred to as a stoma or ostomy.
The two main faecal stomas are colostomy and ileostomy, and the urinary system opening is known as a urostomy.
The diverted urine or faeces is collected into a bag which is attached to the skin around the stoma. Ostomates in WA receive their bags and accessories from the Western Australian Ostomy Association (WAOA).
There are over 4,000 ostomates in WA, and approximately 50,000 nationally. Not all ostomates have their stomas permanently: in WA there are approximately 80 new ostomates every month and around 500 are reversed annually.
Stomal Therapy Nurses (STN) play an important role in preparing patients pre-operatively and supporting and educating them to manage their stoma post-operatively. Following discharge, ostomates are usually followed up by their STN in outpatient clinics, although not all hospitals offer this service. Support available
While being the only distributor in WA of the bags and accessories that ostomates require, WAOA also has a STN clinic to address the gap in out-patient clinics, both at its headquarters in Mt Lawley and around the state.
In addition to the STN service, WAOA provides much needed emotional support which includes the management of 12 face-toface support groups and online.
Living with an ostomy shouldn’t stop ostomates doing anything they wish to do. However many have difficulty coming to terms with and adapting to their new normal.
There are often complications which can also compound the effect on mental health.
The benefits of an individual peer support contact, particularly for potential ostomates,
cannot be overstated and is well understood to:
• Reduce anxiety
• Enhance confidence
• Reduce isolation, giving a sense of connectedness and a safe space for sharing
• Facilitate adjustment to life with a stoma and self-efficacy.
Until recently, there has been little research into the benefits of peer support specific to ostomates. Dr Julia Kittcha, an STN from NSW, has recently published the results of her thesis which researched this.
This year a Peer Support Service has been launched by WAOA that connects those who need extra support or advice with a Peer Support Volunteer (PSV).
The PSV is an ostomate with lived experience who has undergone specific training conducted by the STN at WAOA headquarters. It is highly recommended that those who are facing or considering ostomy surgery are offered the option of speaking to a PSV as soon as possible so a lot of the misconceptions and concerns related to having a stoma can be addressed.
Referral process
Anyone can refer to the service using the appropriate forms available on the WAOA website, which should then be emailed to the STN.
The STN will match the patient with a PSV of a similar age, gender, disease process, stoma type, and activity level and interests.
In the first instance the potential ostomate will be contacted by our PSV by telephone and, if felt beneficial, a meeting can be arranged.
Doctors should offer the service as soon as possible and call WAOA with any questions.
Don’t refer anyone who would pose a risk to others or without their consent.
There are other useful resources for patients, including a variety


of Facebook groups such as WA Ostomy – open and closed groups, Bowel and Stoma Health for rural ostomates, Bumps to Bubs for those with an ostomy expecting or trying for a baby, and Perth Young Ostomates. Useful websites include WA Ostomy (www.waostomy.org.au), Australia Council of Stoma Associations (www.australianstoma.com. au), and Australian Association of Stomal Therapy Nurses (www.stomaltherapy.au).
For further information call (08) 9272 1833 or email stn@waostomy.org.au
Author competing interests – nil
• WA has over 4000 ostomates
• Peer support can be very valuable to people with an ostomy
• A new peer support service has been launched in WA
0.5

By Dr Philip Finch, Pain Specialist
Complex Regional Pain Syndrome (CRPS) can start after a minor injury to a limb such as a fracture, a soft tissue injury or minor elective surgery including a peripheral nerve decompression.
Often the pain spreads and until recently this was thought to be a psychiatric problem.
It is hard for patients and their treating professionals to deal with, as the condition has no clear background pathophysiology and consequently no clear treatment paradigm.
CRPS symptoms usually include significant pain and skin sensory disturbances, initially confined to the affected limb. The condition can be associated with weakness, cramps and tremor. Frequently, swelling and vascular disturbances are present (see Figure 1).
Increased expression of alpha-1 adrenoceptors on nociceptor nerves may be involved in the initial peripheral trigger for this condition. We have seen upregulation of alpha -1 adrenoceptors in skin samples taken from patients with CRPS. Pain often spreads away from the injured site, but what drives this is unclear.
About 20 years ago, my colleague and co-researcher Professor Peter Drummond and I noted that CRPS patients often had hemisensory changes on careful physical examination.
We also noted that they often had asymmetric cranial nerve function. We were aware that Rommel et al. had reported this in 2001. Rommel concluded that hemisensory impairment in patients with CRPS is probably related to functional disturbances in processing of noxious events in the thalamus and may be a clinical correlate of subcortical brain plasticity in chronic pain.
With CRPS, the affected limb becomes extremely sensitive to light touch and minor changes in the environment including temperature movement and even to loud noise.
Sound sensitivity was described by Silas Wier Mitchel, a neurologist, in soldiers injured by musket balls and developing this condition during the American Civil War.
We have found that sensitivity to noise and bright lights is greater on the side of the affected limb in CRPS patients. We have also found that there is heightened sensitivity to thermal and mechanical stimuli on the side of the body ipsilateral to the affected limb.
Hemisensory changes suggest a failure to regulate sensations on the affected side. We are currently studying the locus coeruleus (LC) with 3 Tesla MRI with a grant from
the Australian and New Zealand College of Anaesthetists (ANZCA).
The LC is a small bilateral cluster of noradrenergic neurons in the upper pons and lateral to the fourth ventricle. It is an adrenergic ‘waystation’ in the brainstem. It may act as a ‘volume control’ for ascending neuronal traffic.
Recently, we studied the spread of CRPS symptoms away from the site of injury. Changes in the LC might explain sensory asymmetries and may occur over time, providing an explanation for the spatial progression of CRPS.
There are several possible causes for the spread of CRPS symptoms which may include the spread of pathology in the affected limb, intertwined nociceptor and adrenergic fibre types, a systemic disturbance including the presence of autoantibodies

• CRPS is often triggered by a trivial injury in a limb and is associated with painful skin sensory changes which can spread proximally
• The pathophysiology of CRPS is unclear but may involve a peripheral trigger in a limb and aberrant central neuronal processing, possibly in brain stem nuclei
• No clear treatment paradigm exists as the pathophysiology of CRPS is not well understood.
such as alpha-1 adrenoceptor autoantibodies, altered spinal processing of nociceptor signals and lastly, functional changes in subcortical or cortical pain processing centres such as the LC.
We postulate that as the understanding of the function of the LC improves, so will the understanding of the pathophysiology of CRPS. We would argue that CRPS is a condition with a peripheral trigger causing an upregulation of A1 adrenoreceptors.
Coupled with this is an alteration of control of ascending and descending traffic in the dorsal horn of the spinal cord and the brainstem.
CRPS can be a devastating condition for patients with little current effective treatment. Hopefully, a better understanding of the neurophysiology of CRPS through research will lead to more effective forms of treatment.
Author competing interests – the author is involved in some of the research described.






Dr Thomas Shannon, Urologist
Irreversible Electroporation (IRE)
NanoKnife focal therapy is now available in Perth after being pioneered in Sydney over the last 10 years.
Focal therapy is not a new concept, with around 20% of prostate cancers potentially curable by treating the cancer rather than the whole prostate. However, IRE NanoKnife is different to previous treatments. Irreversible electroporation (IRE) affects cell membranes only, effectively killing cancer cells while causing little damage to vessels and nerves.
Previous focal treatments relied on radiation or thermal effects, with more damage to surrounding tissue and less reliable cellular effects. This limited use to lowrisk lesions, away from critical structures. Most MRI detected lesions will be moderate to moderate high risk, by comparison. Unlike thermal modalities such as cryotherapy or highintensity focused ultrasound (HIFU), IRE preserves the extracellular matrix, blood vessels, and neural structures. This characteristic is particularly advantageous in prostate cancer treatment, given the close anatomical relationship between malignant tissue and critical structures including the urethra, external urinary sphincter, neurovascular bundles, and rectum.
As IRE NanoKnife has less effect on vessels, it is a possible treatment after failed radiation treatment.
Treatment is delivered as a day case procedure and a catheter left for a few days only. Pain is minimal and patients can return to full activity quickly.
Follow up imaging is simple and reliable. In our first 20 plus cases all patients have achieved MRI assessed complete response.
Patients undergo biopsy confirmation at six months and so
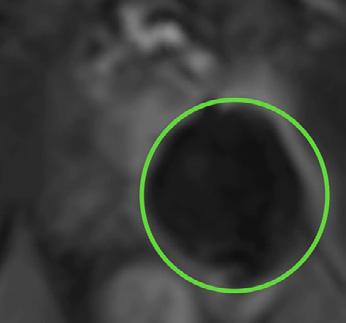
far, no residual cancers have been found in our group. This mirrors Australian 10 year experience from Prof Phillip Stricker in Sydney who has shown a 97% success rate over 10 years, with minimal impact on erections and no incontinence.
Careful patient selection is essential to the success of NanoKnife
IRE. The ideal patient has:
• Localised disease visible on MRI and biopsy
• Ideally low/moderate and moderate high risk cancer - GG 1/2/3
• Absence of other cancer foci on PSMA PET
• A desire to minimise the functional side effects associated with whole-gland therapies
• Acceptance of need for follow up MRI and biopsy.
For this reason, NanoKnife IRE is not recommended for patients with aggressive or high-risk prostate cancer. In these cases, radical prostatectomy, radiotherapy, or multimodal oncological treatment remains the standard of care to ensure adequate disease control.
There is a documented 20% chance of developing a new cancer elsewhere in the prostate over 10 years, making it less desirable in younger men with higher risk disease.


One of the key advantages of NanoKnife IRE is the preservation of urinary continence.
As the external urinary sphincter and urethra are largely spared from injury due to the non-thermal nature of the treatment, rates of post-procedural incontinence are significantly lower than those associated with radical prostatectomy or radiotherapy.
Most patients maintain baseline continence following treatment, allowing rapid recovery and minimal disruption to daily activities.
Erectile dysfunction is a major concern for men undergoing prostate cancer treatment. Damage to the neurovascular bundles during whole-gland therapy is a leading cause of long-term sexual dysfunction.
NanoKnife IRE selectively ablates malignant tissue while preserving neural architecture, reducing the risk of erectile dysfunction.
This is particularly beneficial when lesions are unilateral or located away from the neurovascular bundles, allowing many patients to retain erectile function post-treatment.
NanoKnife IRE is performed under general anaesthesia using transperineal electrode placement guided by ultrasound and MRI fusion imaging. The procedure is typically completed as a day case.
Post-procedure symptoms are generally mild and may include transient perineal discomfort, lower urinary tract symptoms, or short-term catheterisation. Most patients return to normal activities within several days.
Ongoing surveillance following NanoKnife IRE remains critical. Follow-up protocols typically include:
• Serial PSA monitoring
• Interval multiparametric MRI
• Targeted biopsy when clinically indicated.
This structured approach ensures early detection of residual or new disease. Importantly, focal IRE does not preclude future treatment options, and patients may still undergo radical therapy if disease progression occurs.

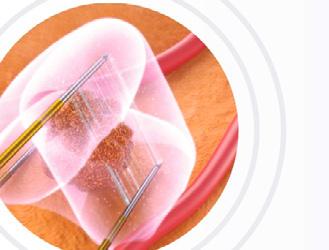
NanoKnife IRE represents a valuable focal treatment option for carefully selected men with localised prostate cancer.
By prioritising preservation of urinary continence and erectile function while delivering targeted oncological treatment, IRE offers an important alternative between active surveillance and radical whole-gland therapy.
While not appropriate for patients with aggressive disease, NanoKnife IRE continues to play an expanding role in personalised prostate cancer management,
As GPs, you often see patients living with chronic osteoarthritis pain who are no longer experiencing pain relief from conservative therapy, but for whom surgery is not yet indicated.1 Low-dose radiotherapy (LDRT) has emerged as a non-invasive alternative for pain relief and functional improvement, particularly in patients unresponsive to conservative measures.1
LDRT uses carefully controlled, low doses of radiation to help reduce inflammation in affected joints. It has been used in Europe for decades and is now emerging as a treatment option in Australia for selected patients with osteoarthritis.1
What can your patients expect?
• Symptom relief: Some patients may experience a reduction in pain and improved mobility following treatment.2-4
• Side-effects: LDRT has been shown to have very minimal acute side effects1-4
Albany Tel: (08) 6819 7900
Bunbury Tel: (08) 9726 6400
Hollywood Tel: (08) 9286 8800
particularly for men seeking effective treatment with reduced functional impact and without the need for androgen deprivation.
0.5


Patient suitability
• Early to moderate OA Age ≥50 years
• Confirmed diagnosis of osteoarthritis (Kellgren-Laurence (KL) scores 1-3)
• Upper and lower limbs (no axial spine)
• Failure of conservative therapy >3/12
• Contraindications; pregnancy, rheumatoid arthritis, active connective tissue disease
Treatment
A treatment course is typically six sessions over 2-3 weeks. Depending on outcomes, patients may require a second or third course of treatment.
Osteoarthritis affects around 8.3% of the Australian population5 (2022 data)
Mandurah Tel: (08) 9559 2900
Murdoch Tel: (08) 9366 1500
Available from: https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoarthritis (accessed October 2025).

Shenton House Tel: (08) 9400 6213
Dr Qurrat van den Blink MBBS, FRANZCR Radiation Oncologist
Wembley Tel: (08) 6318 2868
After a year away, Sculpture by the Sea returns to Cottesloe next month, with almost 70 artworks ready to steal your affections.
By Ara Jansen

If Sculpture by the Sea has a superpower, perhaps it’s that each year visitors often fall in love with a piece or two – and that’s what keeps them coming back for more.
Artistic director and founding chief executive David Handley is not immune to having a handsdown favourite amongst the large-scale beachside pieces of art every year. With Sculpture by the Sea at Cottesloe turning 21 this year, the event – and that choice – feels just that little bit more special.

“What motivates me each year is the sense of wonderment I see in the faces of young children as they wander through the exhibition,” says David.
“To have an idea that captures the imagination of artists around the world, who in turn create artworks
that excite and inspire such a large percentage of the people of Perth and south west WA to visit each year, is a humbling privilege.”
After a one-year hiatus, the muchloved exhibition is back thanks to federal funding. This year expect a mix of local artists, from stalwarts of the WA sculpture world Ron Gomboc, Tony Davis, Jen Cochrane and Tony Jones through to early mid-career artists like Jina Lee, Jarrod Taylor, Karla Hart and Britt Mikkelsen, as well as emerging artists such as Stephanie de Biasi.
This year’s Tourism WA Invited International Artist is Indian artist Subodh Kerkar who is creating special performance artworks with volunteers as integral parts of the artwork.
Attracting more than 250,000 local, interstate and international visitors annually, this year features 68 artworks, 70% of which have not been exhibited before.
The artists hail from seven countries, including 11 from Japan and four from Denmark who will be alongside more than 30 West Australians.
The free public event is open to all and allows visitors to walk between the works. David quips there aren’t many art galleries on a beach with a pub, restaurants and fish and chips across the road.
“Somehow the space immediately relaxes people as they wander in on the lawn among the trees and down to the sand,” he says.
“To transform that space into an international sculpture exhibition is a joy and a privilege.
“It is such a special feeling each year to see the connection between people and the sculptures by artists from across Australia and around the world.”
The artistic director has two favourite times of the day to visit the exhibition. He loves the day as

sunset approaches when thousands of people are wandering the beach among the sculptures. He also loves to wander through the sculptures and into the water for an early morning swim and look back to the exhibition from the Indian Ocean.
“The Cottesloe exhibition site is so special due to the unique
amphitheatre created by the sea wall and the sand curving round to Indiana’s. To be able to look down on the sculptures and to then wander among them allows you to experience the artworks from a distance and up close.
If turning 21 signifies the coming of age, then David loves that tens of

thousands of children have been introduced to sculpture through the open-air exhibition and it has become part of their lives.
“Sculpture as an art form is no longer hidden. For my part it feels like the exhibition has been part of the cultural evolution of Australia. When I was growing up you could only get a burger and a milkshake at the beach. Now we have world class restaurants on the beach and sculptures on the beach next to sunbathers, swimmers and surfers.”
Sculpture by the Sea is at Cottesloe Beach from March 6-23.
MANDOONESTATE.COM.AU
Wild Swan is our contemporary fine dining restaurant, overlooking the manicured gardens and the Llawn at Mandoon Estate.
Executive Chef Michael Hartnell and Wild Swan Head Chef Anthony Power have created modern and innovative a la carte and tasting menus that combine classic techniques with the finest local and seasonal produce. Their modern Australian menu has been carefully designed to match with our award winning wines and craft beers.






Writer Cam Jeffreys has released a quirky crime novel set in Perth which will have readers chuckling at the unique and recognisable parts of our city.
By Ara Jansen
Can poetry save a life? In Royce Leville’s version of Perth, unravelling mysterious lines of poetry are what’s going to solve the crime in his new book titled Botany Royce Leville is a pen name for writer Cam Jeffreys, who originally hails from Perth, but has been based in Hamburg, Germany for several decades.
As well as working as a commercial writer, he runs Rippple Media, the home for his creative work, which over the years has included books, films, TV, content, branding,
travel, music and workshops. His first screenplay has received development funding from the Hamburg Film Commission, has two established production companies on board and is currently in pre-production there.
Botany is Cam’s seventh book and the start of a series starring Quintus Huntley, a washed-up university poet trying to find his next lines but instead finds himself trying to solve a crime before it gets pinned on him.
Poetry is involved and understanding the clues in the stanzas will get Quintus and a rag-taggle team to the finish line.
One of the fun aspects of the book is that it’s set in Perth and features a lot of places you’ll recognise. There are also plenty of the types of characters you’ll recognise, which will sometimes make you laugh out loud because they are just so Perth.
“For Perth people reading the book, there will be things which don’t require much description,” says Cam. “By saying someone grew up at Trigg Beach, it tells you some things.
“Perth is a pretty unique place and when you live here or stay here for a while you don’t get a sense of how truly isolated it is.
“I knew I wanted to write a book about Perth but also where the landscape and place felt like an integral character in the story. Aspect like the wind and the flies, which everyone recognises.
“I also wanted it to be fun. The first drafts were a lot more violent and hardcore, but I felt it needed the element of fun – despite the crime, the sun still shines. The characters in the book are trying to do the right thing and you probably would have a drink with them if you met them in the pub.”
Cam grew up in Williams and then in the Perth Hills before
moving to Europe. He represented Australia at the world triathlon championships in 2013 and 2017.
A guy he met playing an Aussie Rules game in Frankfurt got Cam his first copywriting job and that kicked off his career more than two decades ago. Since then, he’s written copy for some of the world’s biggest brands, alongside satisfying his own creativity with different writing projects through Rippple – the three P’s standing for producer to public publishing.
While he’s lived overseas for a long time, Cam visits Perth regularly to see family and friends. These trips have continuously reminded him of aspects of life which are very typically Perth and provided plenty of fodder for Botany Fiercely independent, Cam says he’s always thought of his books in terms of legacy.
“What I care about is producing a book I love and am proud of and that readers find and enjoy. If I write a good book, people will find it. I do this because I love it. I believe in creating things that are going to stay around.”





Our competitions are back for 2026, kicking us off with another WA wine giveaway.
We have a dozen of Woody Nook wines for one lucky reader to enjoy.
Read our Master of Wine’s review of the Margaret River winery on page 55.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.




Hits Of The ‘60s and ‘70s By The 60 Four
SAT 7TH FEB
The 60 Four celebrate the sounds of Elvis, The Beach Boys and The Beatles.
Bluey’s Big Play The Stage Show
18 FEB 1 MAR
Join the Heelers in their first live theatre show made just for you, featuring brilliantly created puppets, this is Bluey as you’ve never seen it before, brought to real life.



A Winters Journey
FRI 13 FEB
Join Musica Viva Australia to hear one of the world’s finest artists in a hauntingly beautiful meld of art and music.
The Peoples Economist MON 2 MAR
Gary Stevenson, former Citibank trader turned best-selling author of the The Trading Game and global voice on inequality, comes to Australia for the very first time.

The 70s80s90s Show
SAT 14 FEB
The Ultimate TimeTravelling Party –Three Decades of Hits, One Electrifying Show!
Seventh Wonder
SAT 7 MAR
This world-class performance, brings together a star- studded band and a 16-piece string symphony orchestra to create an unparalleled tribute to Fleetwood Mac’s music.

Our podcasts bring you the latest updates and key insights into new treatment options available.
Join our clinical editor Dr Joe Kosterich in conversation with WA specialists to learn more about developments to improve patient outcomes. Our podcasts are now CPD verified. Look for the CPD logo to complete your self-reflection and claim your time.
Learn more about:
Is it pelvic venous congestion? With Dr Marek Garbowski
Aortic stenosis: managing low-risk patients with Dr Gerald Yong
Rethinking radiation oncology with A/Prof Yvonne Zissiadis & Celia Byatt
Lung Cancer Screening with Prof Fraser Brims
How to approach acute and chronic knee pain with Dr Jean Louis Papineau
Listen on your favourite podcast platform – scan the QR code to follow us!
Woody Nook vineyard and winery are located at Wilyabrup in the heart of the Margaret River Region.
The property was purchased by Jeff and Wynn Gallagher in 1978 with the first vines planted in 1982, and first vintage in 1987 taking place in their recently completed winery.
In 2000, the property was purchased by Peter and Jane Bailey with the Gallagher’s son Neil remaining a shareholder. He stayed on as winemaker and viticulturist until 2020.
Since then, winemaking and viticulture has been in the experienced hands of Digby Leddlin with sales and marketing manager Courtney Dunkerton assisting.
The vineyard grew to 17 hectares in 2007 when a further eight hectares were added. Cabernet Sauvignon, Shiraz, Merlot, Cabernet Franc, Chenin Blanc, Chardonnay, Sauvignon Blanc and Semillon plantings were increased and two native Spanish varieties – Tempranillo and Graciano – were added.
All wines are produced from estate grown fruit and with an annual crush of around 100 tonnes Woody Nook certainly qualifies as a boutique operation.
When in Margaret River, Woody Nook is well worth a visit.

Woody Nook 2025 Chenin Blanc, RRP $27
A nice easy drinking wine, good as an aperitif or accompanying seafood. Drinks well now but will reward over several more years. Aromas of tropical fruits which follow onto the palate. Pineapple, nashi pear, a touch of quince. Simple pristine clear flavours with a firm acid backbone and a clean finish.
Woody Nook Limited Release 2024 Rose, RRP $ 32
A nice summer drink. Fresh, light, bright and fruity. Described as a “field blend” it is made from Tempranillo and Shiraz with a small addition of puncheon-fermented Sauvignon Blanc. Displays an attractive salmon pink colour. Nose is confectioned, palate refreshingly alive with cranberry and boysenberry. A drink now wine.
Woody Nook Limited Release 2024 Fume Blanc, RRP $ 32
This wine is a superb example of the style. From experience in my own winery it is so difficult to get the right balance so the oak is not obtuse and the wine has complexity with delicacy –this wine has achieved that.

Shows complex developed secondary fruit on the nose, herbaceous with some slight pungency. Palate has lanolin and quince characters, fruit weight enhanced by bâttonage. Firm acidity holds it all together. Great current drinking and will evolve fascinating complex flavours over the next few years.
Woody Nook 2025
Tempranillo, RRP $27
Tempranillo with addition of 5% Graciano. Interesting ruby red/violet colour with aromas of Turkish Delight and spices. A medium bodied wine
Palate shows black cherries, spices and sarsaparilla. Oak evident
but not central to the style. Back palate displays a slight milkiness that I associate with Tempranillo wines of Rioja. A wine for short to medium term consumption.
Woody Nook 2023 Cabernet Sauvignon Merlot Cabernet Franc, RRP $ 42
A blend of Cab Sav 90%, Merlot 7% and Cab Franc 3% this ‘Bordeaux blend’ works so well for wines from this region. Garnet in colour with inviting aromas of blackberry, all spice and cloves.
Palate is full of flavour with blackcurrant, dark plum, Spanish black olive. Nice grippy tannins, lingering flavours. A very complete wine with a good future. Available at cellar door.
Woody Nook Gallagher ’s Choice 2018 Cabernet Sauvignon, RRP $67
A massive blockbuster of a wine from that exemplary 2018 vintage, now at six years.
In my opinion drinking optimally, but I would give it another 10 to 12 years yet. I recommend decanting this wine prior to drinking.
Still deep brick red in colour but meniscus showing slight browning. The nose is majestic, complex, rich, ethereal and loaded with blackcurrant and eucalyptus. Opulent concentrated flavours of blackcurrant and dark fruits. Tannins supple, oak integrated. Carries its 15.5% alcohol very well. A wine of contemplation.
Reviewer’s Pick



