The problem is that healthcare is becoming financially unviable for many patients too.
YOU ASKED, WE DELIVERED: WE ARE NOW CPD VERIFIED


Complete the self-reflection and claim your CPD time, please scan here
Andrea Downey | Managing Editor
We recently asked readers if they would be implementing the government’s bulk billing incentives coming into play this month.
We had an idea of the answer, but it was a resounding no from most GPs who responded.
It’s not because GPs don’t want to bulk bill or make access to primary care easier for patients, it’s because it is just not financially viable.
The problem is that healthcare is becoming financially unviable for many patients too. The 2025 Ipsos Health Service Report found for 41% of Australians the cost of accessing treatment was their biggest concern with the healthcare system.
The government’s goal of delivering 18 million more bulk billed appointments every year isn’t a bad one, but the way it hopes to achieve this looks unlikely to work.
GPs have been calling for better Medicare rebates for longer consults for years – as well as increased rebates across the board – to help cover the cost of running a practice.
This month GPs told us, in no uncertain terms, that the system isn’t working.
As a patient, I agree. I had the NHS at my door for a decade (not without its faults, I know) and the reality of having to pay for healthcare and prescriptions again hit hard.
Perhaps a better solution is a new model altogether? Read our full story on the bulk billing incentives program on page 14.
Let me know your thoughts at editor@mforum.com.au
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




Our round of competitions this month includes movie tickets, another book giveaway and more wine. The British Film Festival returns from November 5 to December 7. We have five double passes to giveaway.
We also have five copies of Hot Ground up for grabs.
And we’ve got another round of WA wine for one lucky reader, this month from Olive Farm Wines in the Swan Valley. Read our Master of Wine’s review on page 55. See our lifestyle section for this month’s wine review and more details on our competitions.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Advertising Account Manager
Rita Murphy 08 9203 5222 rita@mforum.com.au
Clinical Services Directory
Rita Murphy 08 9203 5222 rita@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au



















West Australian GPs stepped out of the clinic and onto the steps of Parliament this month to outline the measures they want taken to ease strain on the state’s hospital system.
The GPs offered politicians health checks for both themselves and the state’s healthcare system, while providing solutions to its challenges.
They called for four key measures including incentivising a GP consult within a week of hospital discharge, additional funding for GPs to provide afterhours consults, expanded access to free immunisations, and the appointment of a Chief GP Advisor to improve collaboration between primary and secondary care.
RACGP Vice President and WA Chair Dr Ramya Raman said: “Our message is that GPs can reduce pressure on the rest of the system.
“Up to one in seven hospital discharges results in an unplanned readmission within 28 days. Imagine how much extra hospital capacity we would have if we reduced readmissions by giving more people access to follow-up care from a GP who knows them.”
“There were 350,000 potentially avoidable presentations to emergency departments for issues that could have been managed by GPs last year, and 60% of people have accessed after-hours care in the last five years,” she said.
Meanwhile, nationally the RACGP has outlined the biggest issues facing GPs in its 2025 Health of the Nation report.
This year’s report was informed by a survey of more than 2400 GPs.
More than 400 GPs have applied to take part in training to allow them to diagnose and prescribe for ADHD.
The initial 65 GPs to undergo the first-of-its-kind training program developed by the RACGP have now been chosen.
Dr Sean Stevens, chair of the RACGP WA ADHD working group, told Medical Forum: “I think it shows a level of interest and concern that GPs have for their patients in this area.”
Once trained, GPs will be able to assess ADHD in patients aged 10 and older and, under recent changes to WA’s prescribing regulations, prescribe stimulant medications.

RACGP President Dr Michael Wright highlighted that increasing complexity of care was the “number one challenge identified by GPs”.
More than two thirds of GPs surveyed raised complexity of consultations as an issue.
It also found the average GP consultation now lasts 19.7 minutes, one minute longer than GPs reported in 2024 and an 11% increase from 2022.
“Rates of chronic disease and mental health presentations are on the rise, our population is ageing, and 68% of GPs pinpointed the increasing complexity of patient presentations as the greatest challenge facing the profession,” he said.
“It also highlighted a significant missed opportunity when it comes to preventive care; 84% of GPs want to provide more preventive care, but only one in three have the time to provide it to their patients.”
It is hoped this will ease pressure on paediatricians and psychiatrists, helping more people access early diagnosis and treatment.
Participating GPs have been split into three cohorts, with the first of those groups to begin six months of training by the end of October. The second cohort would begin training in February and the third sometime after that in 2026.
Dr Stevens said GPs in rural and remote areas and those servicing lower socio-economic areas had been prioritised.
“It’s important to note that the GPs are not able to diagnose and initiate stimulant medication on their own for ADHD until the end of the training program.
“They have to complete the full six months of training before they can
do that and are still expected to practise within their scope.”
The WA government was the first Australian jurisdiction to announce a comprehensive program for ADHD diagnosis and management by specialist GPs, with other states following suit in recent months.
The Therapeutic Goods Administration (TGA) has issued a safety advisory regarding imported unregistered melatonin products. While doctors may choose to prescribe melatonin to their patients ‘off-label’ the TGA is warning of serious safety concerns after lab testing indicated significant discrepancies in the levels of melatonin in products compared to the labelled amounts.
The results of testing of 11 melatonin products, which can be purchased online from other countries, found three had less melatonin than labelled, including one which had none.
Eight of the products tested had more, with one containing more than 400% of the labelled content.
The TGA has warned this variability raises serious safety concerns for consumers, including the risk of hospitalisation and accidental overdose, especially in children.
While the administration does not regulate clinical practice for off-label use, it reminded health professionals that while off-label use was allowed it should be assessed on a case-bycase basis.
Rural health leaders have welcomed the formal recognition of rural generalism as a specialist medical field, saying it gives long-overdue visibility and validation to doctors in this area.
While a National Rural Generalist Pathway was established in 2018 to attract, retain and support rural generalists, it had not been formally recognised as a specialty until now.
The change means GPs with an approved Fellowship of the RACGP or ACRRM will be able to apply for specialist registration as a rural generalist under a protected title and their skills and qualifications can be incorporated into the National Law that governs registered health professions.
Rural Health West chief executive Professor Catherine Elliott said:
“For medical students, this creates a clear and exciting career pathway at a time when general practice training numbers are under pressure, but interest in rural medicine is on the rise.
“This recognition gives longoverdue visibility and validation, which is critical to keeping doctors in our communities.”
RACGP President Dr Michael Wright said recognition was a positive step forward in ensuring that rural generalists are appropriately remunerated for the work they do in rural and remote communities.
“Rural generalists add to the broad and substantial GP skill set with

The first phase of construction has begun on Perth’s new Women and Babies Hospital.
The hospital, at the Fiona Stanley Hospital precinct, will replace the centuryold King Edward Memorial Hospital.
The state government said the 12-storey design was centred on supporting the many dimensions of women’s health and wellbeing.
“It aims to create a space that delivers high-quality clinical care, encourages family connection, and provides spaces for quiet reflection,” it said in a statement.
The 274-bed hospital will include inpatient facilities for gynaecology and maternity patients; a neonatology unit for newborns needing specialised care; operating theatres; a family birth centre; and outpatient clinics.
In addition the project, budgeted to cost $1.8billion, includes two new multi-deck car parks delivering 2500 bays within the Fiona Stanley Hospital precinct, a major expansion of Osborne Park Hospital, and an expansion of neonatal services at Perth Children’s Hospital.
However, the location of the hospital has been widely questioned within the medical community.
Health Minister Meredith Hammat said the project would deliver modern, purpose-built facilities to meet the needs of the community.
“This hospital will support complex and efficient clinical operations, but it’s also been designed with holistic healthcare in mind,” she said.
training in key disciplines that rural areas and hospitals need, so they are highly valued by their communities,” he said.
“The range of additional rural skills training available also offers junior doctors an appealing choice of disciplines, and we can see
these add to medical students’ interest in general practice, which will help address rural workforce challenges.”

In October of 2020, consultant cardiothoracic surgeon Dr Pragnesh Joshi performed the first cardiac surgery at Perth’s Hollywood Private Hospital.
While much of the world was locked down in response to the COVID-19 pandemic, the lack of community spread of the virus and the WA ‘bubble’ meant the new cardiothoracic unit at Hollywood had one of the highest caseloads of such services in the world.
Cardiothoracic services at Hollywood have continued to go from strength to strength since, and the team of cardiac surgeons, anaesthetists, perfusionists, nurses, physiotherapists, dietitians, and allied health professionals behind the service have recently celebrated its five-year anniversary.
While Hollywood has been delivering cardiovascular care to the community for more than 25 years, the launch of surgical services rapidly expanded heart and lung care capability for WA.
Dr Joshi has been involved with the service since its planning stages.
“Normally, you walk into the hospital, and everything is there for you to do the operation. Most of the hospitals were designed a few decades ago and when you work in a particular hospital, you identify that more could be done as you learn more over time,” he said.

“The advantage of the Hollywood was that we were able to consider everything from our past experiences to come up with a hospital that has everything included. This matters as the patient's expectations and journey are more meaningful.”
The hospital offers four cardiac catheter labs featuring some of the most advanced medical imaging technologies in Australia, with construction of two additional labs underway – bringing the total to six, the most of any hospital in Western Australia.
Hollywood also boasts a 24/7 emergency department, interventional cardiology services, around-the-clock referral to cardiothoracic surgeons, a 24-hour acute chest pain service, and onsite coronary care and intensive care units.
Management has invested heavily, resulting in the hospital becoming a leading, comprehensive heart health facility.
It is one of the only centres in the

Asia-Pacific region for training of advanced atrial fibrillation ablation surgeries and is a leader in the hybrid convergent procedure for atrial fibrillation – a complex, collaborative technique combining surgical and electrophysiological expertise.
The service has established itself as a leader in minimally invasive cardiac and thoracic surgery.
It has adopted minimally invasive extracorporeal circulation technology and, in 2023, the launch of the robotic thoracic surgery program opened a new chapter for the hospital, enhancing precision and recovery outcomes for thoracic patients.
Recently, the hospital has advanced into more complex cardiac procedures, including structural heart interventions such as transcatheter aortic valve implantation.
It was the first hospital in WA to provide endoscopic vein harvesting for coronary artery bypass grafting which is aimed at elimination of 2030cm long incisions in legs.
Education and outreach have remained central to the team’s mission, with education evenings and multidisciplinary education and recovery programs reinforcing Hollywood’s commitment to shared learning and community health.
Dr Joshi said monthly multidisciplinary meetings allowed clinicians to learn from complicated and complex patient cases.
“Those who have not been exposed to some new treatments, they also get to learn and be inspired by other clinicians,” he said.
Hollywood Hospital’s Head of Cardiology, Clinical Professor Rukshen Weerasooriya has enjoyed seeing Hollywood Private Hospital through from a concept to the patient-centred service it is now.
“What is unique about working at Hollywood, having worked at many hospitals around the state and around the world, is that it's a family atmosphere here.

“Everyone knows everyone, we work collaboratively across different wards and across different areas like cath lab and theatre, and everyone has really taken cardiothoracic surgery and open heart surgery at Hollywood as a point of pride.
“They go the extra mile to look after patients, to look after the doctors, to help us to do a really good job. It's been a really positive experience.
“I want to thank all of the staff in every ward area – theatre, intensive care, our step-down ward, our cardiology ward, our coronary care unit, our cath lab staff – they've all come along on the journey. They've all been extremely supportive, and without them, we couldn't do it.
“I also want to thank all of the patients who have entrusted their care with us. It's a big step to trust someone with your heart, that's a huge leap of faith.”
Since the hospital’s inception the team of cardiothoracic surgeons has expanded to include Dr Karim Slimani, Dr Sanjay Sharma, Dr Lucas Sanders, Dr Deepak Mehrotra and Dr Kaushal Rathore.
Almost 1500 cardiac surgeries have now been completed at Hollywood and with each procedure, patient journey is prioritised.
The hospital provides a wraparound service involving pre-admission interviews and comprehensive care during and after hospitalisation,
with a unique cardiac rehab service on-site integrating dietitians, clinical nurse specialists, exercise physiologists, physiotherapists, and psychologists.
Plans are well underway for Hollywood’s Cardiology Day event in February, which will see around 200 GPs take part in interactive sessions with cardiologists and cardiothoracic surgeons.


There has been an upward trend in surgical deaths in WA since 2020 with non-technical skills playing a part, according to a new report.
The Western Australian Audit of Surgical Mortality (WAASM) released in October found many issues relating to surgical mortalities in the state last year were due to non-technical skills such as communication and leadership, rather than the surgical procedures themselves.
A total of 695 deaths were recorded in WA where a patient died having been under the care of a surgeon, regardless of whether an operation was performed. Or they had been under the care of a physician and subsequently underwent a surgical procedure.
That number has steadily increased each year from 2020, when 534 deaths were recorded.
WAASM Clinical Director Dr James Aitken told Medical Forum the rise had been driven by deaths in general surgery, which accounted for about 40% of deaths.
“The rise is probably indirectly related to COVID, people presenting later, not having their routine medical checks,” he said.

As with previous reports, many of the clinical management issues identified in the latest audit were unrelated to the technical aspects of surgery but instead related to nonsurgical issues such as communication or leadership.

Dr Aitken said these results mirrored data from two papers recently published by the Australian and New Zealand Audit of Surgical Mortality
problems are not related to surgeons – if a patient comes into ED and isn’t appropriately supervised and that patient then dies because the surgery is delayed, the skill failure wasn't in the surgical community, it was in the ED community,” he added.
“We can give lots of examples where the patient may die under the surgeon, but the cause of the problem isn't the surgeon, it's some other part of the health system.”
“It’s been said for years, one of the consequences of COVID will be that people don't have screening procedures, they don't have their colonoscopies, they're not screening for diabetes, they don't have their cardiac studies, and this is the result.”
The audit aims to continuously improve surgical care by providing an independent, external clinical review of all patients who die under the care of a surgeon, regardless of whether there was an operation.
Dr Aitken said the message for the surgical community was clear: “If people have had COVID in the past, you just need to be aware that they're probably slightly higher risk and, again, there's good evidence to support that.”
"The focus of people when they look at a surgery if things don't go right is that they assume it's a technical error related to some aspect of the operation itself, but the data that we've got shows a far greater problem is what would be known as the non-technical errors,” he told Medical Forum
“Things like, was the consultant supervision appropriate? Was there a delay in managing the patient because of poor communication? Or was it because a test wasn't done?”
He said there was a definite need for more training around these soft aspects of care.
“The question is, is that led by the College or is it led by the health department? Many of these
A spokesperson for WA Health said the report continued to provide valuable insights that support improvement in clinical practice and patient outcomes.
“To strengthen system-wide capability, the Department of Health has introduced the Safety and Quality Workforce Capability Framework, which outlines six domains central to clinical excellence, including effective clinical communication,” they said.
“In addition, statewide e-learning modules launched in November 2024 are helping build capability across WA Health, supported by a broader program aimed at embedding quality improvement and patient safety principles into everyday practice.”
As time marches on since the release of a parliamentary report into diabetes, experts want action to improve access to technology that keeps patients safe.
More than 12 months have passed since a parliamentary inquiry into diabetes recommended fairer access to diabetes devices, but many Australians and their GPs are still waiting.
The State of Diabetes Mellitus in Australia in 2024, which was tabled in Federal Parliament in July last year, supported making access to technology and devices more equitable, instead of the current ‘diabetes lotto’ based on which type of the condition a person has.
Recommendations included better access to continuous glucose monitors (CGMs) for people with type 2 and other forms of diabetes who require intensive insulin therapy, as well as funded insulin pumps for those with type 1.
There have also been calls to allow GPs to initiate insulin treatment instead of having to refer to specialised diabetes services.
While Federal Health Minister Mark Butler’s office says it is still considering the inquiry's report, experts are calling on

By Cathy O’Leary
the government to act, arguing that some people with type 2 or gestational diabetes are having to choose between good health and putting food on the table.
They risk complications including amputation, cardiovascular issues, kidney failure and even death.
While CGM sensors are subsidised for people with type 1 diabetes, they
are not funded for those with type 2 diabetes who make up 85% of diabetes cases – or nearly 1.3 million people – according to the National Diabetes Services Scheme.
A CGM sensor can cost $3,000$5,000 a year, rising to $8,000 if the person needs an insulin pump.
For many diabetics, the process of checking blood glucose levels (BGL) continues to involve pricking a fingertip with a needle, then blotting a drop of blood on a tiny paper-like object plugged into a small electrical device.
But CGMs use a sensor to measure BGLs constantly, allowing for more convenient, less painful access to essential information.
Many doctors argue that at the very least all insulin-dependent diabetics – whether they are type 1 or 2 – should have access to lowcost CGMs, while some experts believe the net should be wider to include anyone with diabetes.
Diabetes experts believe CGMs can change the way people understand their condition, because they can see what is happening to their blood sugars across a whole day in real-time, and this can influence their behaviour.
Local demand
Deborah Schofield , General Manager Health Services with Diabetes WA, said there were at least 200,000 West Australians with type 2 diabetes, with about 29,000 needing insulin who could not access subsidies.

The cost of CGM therapy was $250 to $400 per month.
She said the recommendation was for blood glucose levels to be at least 70% time in range (3.9 -10mmol/L). Time in range (TIR) provided a more granular insight into glucose fluctuation than traditional blood tests like HbA1c, but TIR could only be measured by using CGM.
“One of the hot topics is access for people with type 2 diabetes to subsidised continuous glucose monitoring, and we hear about this quite often on our WA diabetes helpline,” she told Medical Forum
“For type 2, none of the 29,000 on insulin would currently be able to access subsidised CGM. So how about we start there, with that group at least, to get that time in range and avoid hypos. We would also like to see subsidies for women with gestational diabetes.”
Insulin pumps were also cost prohibitive, she said. There were more than 14,000 people with type 1 diabetes in WA, and while 74% were using CGM, only 36% were on insulin pump therapy, and Diabetes WA believed this was largely driven by cost.
Ms Schofield said their insulin pump consumables were subsidised by the National Diabetes Service Scheme but not the purchase of a pump in the first instance, which could cost about $10,000.
“If you're under 21, you can get something from the insulin pump program, and most likely you'd be under Perth Children’s Hospital which would be assisting, but beyond that you have to either selffund or have very top tier private health insurance,” she said.
“We would like to see insulin pumps be extended, because it can improve outcomes. And we know that the people on insulin pumps can link their CGM to their pump and have a hybrid closed loop, so they are getting closer to having an artificial pancreas.
“That can reduce the burden on people to manage their diabetes and keep that time in range.
“With type 2, you cannot know your time in range without CGM, otherwise you’d be pricking your finger all the time. With CGM you can link that with how you administer your insulin as well, and then you’ve got a powerful diabetes management tool in your hands.”
She said the technology had been around for some time and Australians should have access to it.
“If you have diabetes, an insulin pump is essential for your life, and we want people with diabetes to avoid long-term complications of constantly being out of range with their blood glucose. We want to give them every chance to get that right,” she said.
But access to technology is only half the story, according to Dr Gary Deed, Chair of the RACGP Specific Interests Diabetes Group.
He told Medical Forum that GPs needed to remain up to date and knowledgeable so their advice on the clinical use of technology was contemporary, individualised and appropriate for the patient.
“The field is expanding quickly so for GPs the area of clinical utility in type 2 diabetes is something each GP needs to become better educated about,” he said.
“The main concern is that technology is most effective when aligned with quality education for the user and health provider team to allow for enhanced changes in therapeutic management.
“Also, there are increasing imports of devices available but the standards on quality across each device needs to be developed.”
Dr Deed said the need for technology was small in people with stable type 2 using
oral medications other than sulphonylurea and insulin. But once management included these agents, hypoglycaemia could occur if there was poor monitoring and awareness by the person.
“Technology can help a person develop 'safety netting' to manage symptoms or even detect symptoms before impairment. Some technology now has 'alarms' that activate at set levels of high or low glucose.
“These are educational but can lead to anxiety and disempowerment if they occur in sleep or social situations without adequate education and planning for management.”
Dr Deed said that not every person with diabetes needed CGM, such as those stable on medications which did not give rise to hypoglycaemia. Other options included a meter that used sensor strips that could be used on an 'as needs basis’ such as sick days or when the person was unwell.
While intermittent CGM – where a device is used for a period such as 10-14 days – could capture data to provide insight into the effects of illness, diet or lifestyle, or medication changes.
These approaches could reduce costs and provide a more structured educational platform to promote self-management.
Dr Deed said it was concerning that GPs remained hamstrung by not being able to sign off on type 1 diabetes CGM needs.
“This is a hindrance to people living in not only metropolitan but especially regional and rural or remote areas where access to health team members may be restricted or done by telehealth,” he said.
“The additional costs in terms of time or financial to see a health team member to get such a form signed off is a red flag for bureaucracy being more important than the person.”
Diabetes Australia says the diabetes epidemic is now at crisis point, estimating the disease costs the health system $9.1 billion a year. Its chief medical officer, endocrinologist Professor David
continued on Page 13

Learn about the new Support at Home aged care program, referral pathways, services available, and how to support your patients to receive in home care.
Speakers: Head of Policy and Advocacy Dr Ronelle Hutchinson, GP Liaisons Dr Leena Patel and Dr Erin O’Donnell-Taylor and Director of Nursing and Safety Chris Snepvangers.
Date: November 12, 6.30-8.00pm Where: Online
Diverticulitis
Demystified
Modern management and meaningful outcomes.
Speaker:
Dr Haroon Rasheed
General surgery
Date: November 18, 6.30pm
Where: Online
RSVP: November 18
Session 1
GSM – Genitourinary syndrome of menopause, premature ovarian insufficiency, highlights from the AMS Congress.
Session 2
A patient journey in mitral TEER, TAVI and the dangers of unmitigated valve insufficiency and appropriate patient selection.
Speakers:
Dr Philip Currie – Cardiology Dr Gerald Yong – Cardiology
Dr Wen-Loong Yeow - Cardiology
Date: November 26, 6.30pm
Where: Tucci Restaurant 58 Duncraig Rd - Applecross WA 6153
RSVP: November 23
Urogynaecology, threatened miscarriage and early pregnancy problems, fertility updates and fertility after gynaecological cancers.
Session 3
Bleeding issues from amenorrhoea to HMB, PCOS, endometriosis, cervical screening update, contraception.
Speakers: Dr Bernadette McElhinney, Dr Jenni Pontre, Dr Lucy Williams, Dr Pippa Robertson, Dr Shital Julania, Dr Anna Clare, Dr Jenny Beale, Dr Todd Ladunchuk, Dr Louise Hobson, Dr Roger Hart, Dr Raj Mohan.
Date: November 29, 8.30am Where: UWA Uniclub Ballroom, Hackett Drive, Crawley RSVP: November 27
Clinician Assist WA is a secure website providing GPs and other health professionals with guidance for assessing, managing and referring patients across WA. It has replaced HealthPathways WA.
Date: November 18, 12.30-1.15pm Where: Online
The virtual training is suitable for GPs, enrolled and registered nurses, dietitians, diabetes educators, pharmacists, exercise physiologists and other allied health professionals.
Date: November 25, 9am-4.30pm
Where: The Boulevard Centre, Floreat
Delivering RACGP accredited education delivered by your local WA specialists – have your say on the topics and speakers you’d most like to see on the program.
Scan the QR code to help design your perfect masterclass

continued from Page 11
Simmons, said increasing access to insulin pumps could keep blood glucose levels stable and reduce the risk of long-term health complications, saving huge costs for the health system.
He told Medical Forum diabetes technologies were both lifechanging and lifesaving.
“Australians with all types of diabetes should have equitable access to the technology they need to live well, but right now they don’t and this needs to change,” he said.
“Access to diabetes technology isn’t fair and equitable. Some people have technology like CGM devices and insulin pumps, while others can’t afford it and go without.”
Prof Simmons said the government needed to expand subsidies for insulin pumps so that more people living with type 1 diabetes could access them.
With a CGM device, a person was half-way to having an automated insulin delivery system.
“But what they also need is an insulin pump. When you have both pieces of tech, you can connect them and have your CGM working alongside your insulin pump and automate the process of blood glucose management.
“That leads to more normal blood glucose levels and less chance of coma due to a low glucose and longterm complications such as kidney failure and blindness.”
Additionally, while CGM devices were subsidised for people with type 1 diabetes, they were not funded for people with type 2 diabetes.
Diabetes Australia has been advocating for expanded subsidies, initially for key vulnerable groups, including insulin pumps for people with type 1 diabetes under the age of 21, those with a health care card, and Aboriginal and Torres Strait Islander people.
Its economic modelling shows that a $200 million investment would support tens of thousands of Australians to have access to diabetes technologies.
Prof Simmons said there was clear evidence that access to diabetes
GPs can encourage their patients to call the Diabetes Helpline if they have questions about their diabetes management or if they want to add their voice to advocacy for increased technology access.
They can call 1300 001 880 during office hours to speak with the on-duty diabetes educator or email their query to info@diabeteswa.com.au
Last year the RACGP released its updated diabetes handbook, bringing together the latest evidence and guidance for GPs in managing type 2 diabetes.
The Management of type 2 diabetes: A handbook for general practice is the first revision since 2020 and the result of collaboration between the RACGP and Diabetes Australia.
There are more educational resources on CGM for GPs at: www.nadc.net.au/cgm-gp/

technologies reduced overall healthcare costs for both the individual and the healthcare system.
“Worryingly, Australia is falling behind many other comparable countries when it comes to access to diabetes technology,” Prof Simmons said.
“Countries like Canada, New Zealand and the UK fund insulin pumps through their public health system, and France, Germany and Japan have already seen the economic and health benefits of subsidising diabetes technologies.”
He said there were serious health outcomes for people living with diabetes that arise when blood glucose levels were not well managed and fell outside their target ranges.
If blood glucose levels fell too low then this could lead to hypoglycaemia which, if not treated, could cause loss of consciousness and seizures.
Conversely, blood glucose levels could be too high – hyperglycaemia – and in the short-term, this could
lead to dehydration and infections.
In type 2 diabetes, if blood glucose levels continued to be too high this could lead to a worsening of diabetes, which might require more medications or more frequent insulin injections.
In pregnancy, if blood glucose levels are high this can lead to more congenital malformations, stillbirths and the baby being more likely to end up in neonatal intensive care with breathing problems or a low blood glucose.
“CGMs and insulin pumps have been a game changer when it comes to helping people with diabetes monitor and manage their blood glucose levels and ultimately improve their quality of life, while reducing the cost to the health system,” Prof Simmons said.
“But for 61% of people living with diabetes, the cost of diabetes medicines and technologies is their greatest challenge.
“Nobody should have to decide between good health and putting food on the table.”
New incentives for GPs to bulk bill all of their appointments have come into play – but the likelihood of nine in 10 GPs signing up remains to be seen. Medical Forum asked WA GPs what they think of the program.
By Aleisha Orr

It has been promoted by the government as the “single largest investment in Medicare since its inception”, and it begins this month.
The Bulk Billing Incentive Program has been funded to the tune of $7.9 billion to expand access to bulk billed GP appointments beyond children and concession card holders to all Australians.
Designed by the government with the aim of encouraging 90% of GP clinics to fully bulk bill all consultations by 2030, it is an opt-in program for GPs and practice managers.
When the incentive was announced there were about 1600 GP clinics across the country that bulk billed all patients – this number would have to triple to reach the government’s goal.
On the table for those that sign up is a 12.5% incentive payment. For a clinic to benefit from the new incentives, all GPs at that clinic must take part.
The government is counting on clinics signing up to receive incentive payments for a wider variety of patients, but GPs have had to consider whether the incentive payments will boost their income or not.
In most cases, for clinics that already bulk bill all patients, it is likely a simple decision as revenue looks set to increase through the additional payments.
But this program was designed to increase patient access to bulk billing, so how many clinics that do not already offer 100% bulk billing will be convinced to make that change?
Speaking to RACGP Vice President and WA Chair Dr Ramya Raman in the lead up to implementation, she said the College was unsure and had not collated numbers on this.
A small-scale survey of West Australian GPs carried out by Medical Forum showed just two of 29 who responded said their clinics were signing up to be part of the program.
In the practice one of those doctors works in, all patients were already bulk billed and in the other 90% of patients were already bulk billed –so it’s not a big change to the way they already work.
All the GPs who would not be signing up to the program said it was not financially viable. One respondent said they currently bulk bill 80% of their patients and it would “cost me too much to change”.
Another said: “It is not financially viable for my practice. It is also not stated whether the government will increase the Medicare rebates according to inflation and whether there could therefore be another Medicare ‘freeze’ once the GP practices are locked into the bulk billing system.
“All other costs are increasing significantly but will the bulk billed rebates keep pace with inflation and cost of living?”
Given GPs see a different mix of patients and may or may not already be charging a gap fee on top of their bulk billed appointments, the equation is not the same for all GPs and clinics.
Health program director at the Gratton Institute Peter Breadon said it depended on the level of fees a clinic had been charging as to whether taking up the incentive would be of financial benefit or not.
better off under the new incentive program.
Incentives are scaled by remoteness via the Modified Monash Model, which sees practices in more remote and rural areas receiving higher incentive values.
“The program is a major injection of new funding into the system and the increases outside cities will be even bigger, so if there’s going to be an increase in bulk billing, you’d expect it to be even greater in those areas.”
Mixed billing practices may decide to remain mixed billing, accepting that only services to certain patients will receive the old incentives, or they may convert entirely to bulk billing for all eligible services and receive the 12.5% loading.
But a number of comments provided by GPs to Medical Forum ’s survey expressed concern the MBS rebates did not reflect the costs of providing care.
GPs have for some time spoken about the overheads of running a practice being too high to support fully bulk billing, as care continues to get more expensive for patients.
One GP said their clinic had not entertained the idea of signing up to the program as the payment would be less than the current fees they charged.
“We would be struggling to pay the fixed costs of business, like rent and staff costs,” they said.

“Fees are totally unregulated. People can charge what they like and if they are charging patients more than the increase in the incentive, then it won't make financial sense for them,” he said.
As bulk billing incentives also differ depending on where a GP is practising, this factor also plays a part in whether doctors will be
The RACGP ran a number of webinars to help clinics and individual doctors understand the program and how it would operate.
Dr Raman said the College had been providing information so that practices and GPs can make informed decisions.
"We are not looking over any shoulders or telling them how they should be doing things, instead we are offering them support to make that informed decision,” she said.
“From the College’s point of view, we're committed to supporting our members and our membership teams in the best way that we can,
“It is not financially viable for my practice. It is also not stated whether the government will increase the Medicare rebates according to inflation.”
no matter what they choose to do.”
Department of Health figures made public in the months leading up to the launch of the program suggested 23% of GP clinics were unlikely to take part in the incentive program based on financial incentives.
The split of the 12.5% incentive payment between the practice and individual GPs has also been controversial.
Following consultation, the government announced doctors and their clinics would share the payment equally, with 6.25% being given to individual GPs and the other half being paid to the practice.
Two thirds (22 of the 29) of GPs who responded to Medical Forum ’s survey did not agree with the decision to split the payment in this manner.
Dr Raman said the College wanted to see the whole payment go to GPs.
"I think there's a clear majority view here, we surveyed our members and nine out of 10 of those surveyed told us that it shouldn't be 50-50 and it should go directly to the GP,” she said.
She added there were multiple reasons she would support the entire payment going to GPs as in the end it was the GPs reviewing patients and providing quality services to their patients.
"All of the GPs within the practice need to agree to bulk billing for that to be applied as well, so there's just multiple touch points.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
continued from Page 15
"From a College point of view, we have made it clear that in order for the program to succeed and to make it more attractive that the majority, if not all, should go to the GP,” she said.
Another issue raised in Medical Forum ’s survey was concern that the bulk billing incentives program could decrease the quality of care being provided.
One labelled it “great for six-minute junk consultations” adding that it would “do nothing to improve quality consultations”.
Just three of the 29 doctors who provided input said they thought the incentive program would work.
On expressed concern that “bulking billing results in a lower standard of care”.
Another said they were “pessimistic that private billing general practice will survive”.
Others agreed that funding should be focused on increasing Medicare rebates, particularly for longer consultations, something the RACGP continues to advocate for as a way to improve access to primary care.
One GP responded: “I think that increased rebates should be given for longer consultations and mental health work, as these are important areas where mental health and chronic disease management can be addressed.”
Another said the structure of Medicare rebates was causing some GPs to leave the profession entirely.
“The deck chairs are being rearranged on the deck of the Titanic. So many resources are being pulled into avoiding giving adequate Medicare rebates to make GPs stay in a financially viable business providing complex care in longer appointments,” they said.
“Good quality thoughtful holistic medicine is not being rewarded.”
Mr Breadon said the government had work to do to get GPs on board with any policy changes and needed to communicate better.
"If you look back at the last attempt at trying a new funding format that wasn't just tipping money into the current model, it was the Healthcare Homes Funding Reform. One of the findings to come out of that was the communication with GPs and patients wasn't great,” he said.
“It wasn't clear enough what the benefit of this program was, why we were doing it, what we were hoping to achieve, how it would benefit GPs and patients.
“I think that's a clear lesson from implementation of new policy in general, and certainly in the most recent attempts at general practice funding. Communication and engagement with this sector is really crucial, so I think that is essential for success.”
The Health Consumers’ Council WA said it broadly welcomed any initiative that encouraged more GPs to bulk bill.
Executive director Clare Mullen said the council was hopeful that GPs would see the benefits of bulk billing for both their patients and their businesses.
“If enough practices take up the incentives, the market could start to shift – practices who do not offer bulk billing may find themselves losing patients to those who do,” she said.
patient is poorer, this patient has more conditions’ and therefore we should have a bigger budget for caring for that patient,” Mr Breadon said.
As health policy experts, health practitioner associations, advocacy groups, and patients alike wait to see what impact bulk billing incentives will have on access to primary care, the government continues to express confidence in its program.
Health Minister Mark Butler said: “We know this investment will work, because it has already worked for the patients the incentive already applies to - pensioners, concession cardholders, and families with kids.
“Already GP practices around the country have said they will move to a fully bulk billing practice. Doctors and practices are making the shift because they know it is good for patients, and it is good for their bottom line.”

There will no doubt be strong focus on the number of clinics that have switched to be fully bulk billing as of November, once those figures come out. What comes over the next four years will determine whether the government’s ‘nine out of 10’ promise becomes a reality.
Ms Mullen highlighted the need for the government to assess the program as it went.
Mr Breadon said no matter how great or small the increase in bulk billing from this move, Australia badly needed a change in the way healthcare was funded.
He said deeper reform of GP funding was needed, as the current fee for service model forces clinicians to churn through appointments as fast as possible.
He supports a flexible funding model linked to patient needs, which he said would allow doctors to focus on prevention, deploy a multidisciplinary team, and ensure continuity with patients.
“The best way to do it is to say ‘Okay this patient is older, this
“If the incentives don’t see large enough numbers of GPs switching to bulk billing, then it’s important the government remains open to improving what is being offered, by engaging with GPs and WA health consumers.”

A doctor with a feminist clothing apparel brand, Dr Raffi Waltman is changing what it means to be in medicine.
By Ara Jansen
Dr Raffi Waltman has a lot of things to do. At 31 she defines herself not only as a doctor but, among other things, an entrepreneur, a feminist, supporter of equal domestic duties and a dog lover.
She might have even been good enough to play soccer for Australia at one point.
Raffi is part of the younger cohort of doctors who no longer believe that those two letters are exclusively defining. Being more than one thing only enriches their lives and skills as doctors and makes them no less dedicated.
“One of the most important things I have learnt so far is to think about patients as whole people and treat them as such. Every person is different and their understanding of the world is different.”
Her route to medicine wasn’t straight though, spending almost a decade in and out of university, while taking gap and life years in between. She has a diploma in Chinese, took a study tour to China and hopes to keep honing her language skills.
Raffi and her younger sister Laura (who is manager of the family business) also spent six months travelling in Europe and playing in a soccer tournament.
Born in Perth, Raffi grew up in the Hills and graduated from medicine at UWA in 2020. She did her third year with the Rural Clinical School in Narrogin and an intern year at Royal Perth Hospital.
Interested in lots of things at school, Raffi thought maybe she could be a vet or perhaps a career as a soccer player beckoned. Then her thought to study history and Chinese turned into pharmacology and human biology.
She got a job as a pharmacy assistant to see if she’d like it and instead received a good basic grounding in the health space.
Conversations turned to whether medicine would suit Raffi in terms of being able to have greater connection with patients and potentially being able to see them through to the closure of an issue.
Passionate about social issues, she thought medicine could be a place
for her to make an impact. Keen to learn about lots of things, Raffi enjoyed her rotations throughout different specialties, whether it was surgery or at the GP practice in Narrogin.
She’s currently a registrar with the mental health service at Sir Charles Gairdner and hopes to one day pursue psychiatry training.
“One of the most important things I have learnt so far is to think about patients as whole people and treat them as such,” says Raffi. “Every person is different and their understanding of the world is different.
“I’m excited about psychiatry because it feels like you can make such a difference to people’s lives. You listen to people’s stories, take your time and learn about them and build that relationship over time. It will be challenging – and I’m looking forward to it.”

The pair have been playing all their lives and Raffi is thrilled women’s soccer is finally getting its due in terms of exposure and opportunities.
“I’m so excited that young girls now have real pathways in the sport.”
She’s keen to get back playing in the local leagues, but also acknowledges that in a busy life, some things have to give.
“My parents migrated from South Africa. My dad ended up being successful. I always appreciated their sacrifices and felt lucky to be born here. I’ve always felt really grateful for that,” she says.
“They really encouraged us and I wanted to give that back to other people who were less fortunate.”
It’s part of what led Raffi to volunteer with the Salvos to help with homeless outreach during university.
“It’s always stuck in the back of my mind how lucky I am and I wanted to do something with that. Even at school I took every opportunity to try everything – I can’t dance and I signed up for the dance production. I’m grateful and lucky and every day I feel privileged to do the job I do.”
When Raffi decided to start a feminist apparel brand, she turned to one person who knows plenty about business – her dad. He’s had a successful plumbing supply company for as long as Raffi can remember and instilled a strong work ethic in his children.
She called it The F Word (no, not that F word), hoping it serves as a catalyst for change and a way to channel her passion for equal rights. Some 10% of sales from the online store and market stalls go to groups ending gender violence, such as Full Stop Australia.
continued

Partner with Australia’s largest independent practitioner network and experience freedom over your billings, appointment types, and clinic care.
Explore our WA GP vacancies

continued from Page 19
“It was very busy and I didn’t really know what I was getting myself into, but once I was there, I loved it. I’m grateful to younger me going through all the hard steps to get the business running.”
As to the origins of the name of her range, Raffi says it wasn’t something specific which sparked the choice, but she suspects a lifetime’s worth of growing up as a girl and a woman in a patriarchal society.
As a young sport-playing tomboy she didn’t care much for gender issues, assuming everyone was doing what she was. But at a certain point you can’t play with the boys anymore and things change.
“I wanted to be a footy player but I ended up playing soccer because there was no pathway for me. More recently the AFLW has done a really good job, as has soccer, and it continues to grow. At some point I hope to be part of it again, in some way.”
With shirts emblazoned with lines like ‘Would You Say That to a Man?’, ‘Cinnamon Scrolls Not Gender Roles’, and ‘Girls Just Wanna Walk Home Safely’, Raffi says the goal is to bring awareness with a sense of humour.
It’s more effective than being rude and confrontational face-to-face. She also wanted to draw attention to the subtle ways inequality remains pervasive.
“I wanted to go about it in a creative way. Growing up at family events, there was always someone making insensitive comments, women congregated in the kitchen, and with my male cousins, there was no expectation they would clean up. But if I said something about it, I was being rude and disrespectful.
“There are lots of subtle things, like I would never go running at night alone, but my partner can. I once lived with someone and we were both working but I was still doing everything at home and then we got a puppy, which I also looked after. He would empty the dishwasher once and think he had done enough.

“I grew up with it being rare there was an equal division of labour. In a work context you are often confronted by more serious issues – such as domestic and family violence. Together all of these things have made me passionate on the issue. How can you challenge it and make the discussion productive and interesting.”
More people wearing The F Word t-shirts and apparel will hopefully spark more everyday conversations about gender inequality.
For her mental and physical health, Raffi keeps in shape by making sure she’s active. She loves to hike, recently did her first half marathon and plans to do another.
Active travel is high on the list and she takes every opportunity to use her scuba ticket, most recently during a dive trip off Cairns. Raffi has also spent some time learning to free dive and says it’s like meditation and a way to learn breath control.
When she does slow, Raffi loves books and to read. Her home has a lot of bookshelves. They’re mostly non-fiction because she enjoys learning about the world.
Archer, a little black Maltese and toy poodle cross dog, brings great joy to her life. The ‘Unhinged Dog Mum’ caps say it all.
“There was a time in medicine where being a doctor was your only identity and your whole life. That’s changed for the better. People are more well-rounded and I believe this makes for better doctors.
“Being able to pursue other interests and not being married to the job is important. Not that there is anything wrong with that either –but it’s just not for me, and I believe most young doctors feel similarly.
“Having external interests or running businesses outside medicine doesn’t have to jeopardise our commitment to medicine or the quality of care we provide.”

With
details arriving late in the mail, GPs are quickly having to come up to speed with changes to how they manage and charge patients with chronic diseases.
By Cathy O’Leary
There were high levels of frustration in the corridors of general practice earlier this year, as doctors waited on the details of incoming reforms to chronic disease management which were earmarked to begin from July 1.
The intention to simplify and streamline the processes for CDM was not new – first mooted in the May 2023 Federal budget – but details of the new item numbers and remuneration remained scant only weeks out from the start date.
With the changes originally scheduled to begin in November last year, the start date had been pushed back to the middle of this year, but doctors and their practice managers were still in the dark in late May.
By the time the Federal Government revealed the new MBS fees, transition arrangements and referral pathways for CDM, GPs had little time to digest the changes before launch day.
Key changes include the removal of multiple plans and the need to collaborate with members of the patient’s multidisciplinary team in the development of a plan.
The need for a referral form for allied health services has also been removed, allowing standard referral letters in the same way that a GP refers a patient to a non-GP specialist.
At the time the details were finally announced, the RACGP had vented its frustration that vital information had been kept from GPs, which was significant given chronic disease management is a core part of business, with almost eight million patients accessing the CDM items each year.
President Dr Michael Wright argued the new item numbers were crucial for the care of patients and the viability of practices, and a lack of clarity had left many of its members feeling jittery.
A College survey last year found that almost 70% of members believed that if chronic disease funding was not increased, they would have to start charging a fee rather than bulk billing patients.
But despite frustrations over the delay in getting the details, the RACGP has since welcomed the changes as an important step in the ongoing job of reducing red tape and unnecessary processes for doctors and patients alike.
There have been reports of teething problems, including issues related to MyMedicare registration which have resulted in some claims being rejected.
If a patient is registered in MyMedicare they must receive the plan and review services from the practice at which they are registered.
While only time will tell how the funding side of CDM plays out, the RACGP says the initial signs have been encouraging, with more changes planned from July 2027.
According to the Department of Health, Disability and Ageing, this is the first major change to the framework in almost 20 years. It follows other trends over that time in the burden of chronic disease, patient expectations and technology.
Many industry groups argue the reforms are especially timely, given the rising multi-morbidity trend among Australians and growing demand for Medicaresubsidised CDM services for people with chronic and complex health conditions.
An Australian Institute of Health and Welfare report published midyear found that in 2022-23, 16% of the Australian population – or more than 4.1 million people – accessed
co-ordinated care through a GP chronic disease management plan.
About 38% of people have two or more chronic conditions, with anxiety and depression the most common co-occurring conditions, affecting almost one in 10 of the population.
Anxiety and back problems are the second most commonly cooccurring conditions among all age groups, followed by back problems and depression.
Conditions such as attention deficit hyperactive disorder and autism feature more heavily in younger age groups, while the presence of back problems, osteoarthritis and hearing loss increase with age.
In an effort to explain the revised CDM reforms to doctors, the RACGP held a webinar in June covering the impact on practices, including software systems. Among the key speakers was RACGP Vice President and WA Chair Dr Ramya Raman
Speaking to Medical Forum shortly after the changes had come in, she said from the point of view of practising GPs, the rolling out period had been quite short.
designed to simplify, streamline and modernise the process, and promote the continuity of care with chronic disease management services.
“For someone who is in practice –and I was using the GPCCMP for some of my patients only yesterday – I have found that the process itself has become a lot more simplified and it definitely reduces the red tape and the paperwork that’s affiliated with it,” she said.
“There were a lot of things we were previously doing with the team care arrangements around having to communicate with the providers that we were referring for, and if the patient wanted to change the provider, they had to get in touch with the GP again, so there was a lot of double handling.

“Now that a lot of that paperwork has been taken out, the timeframe of doing these plans seems a lot more efficient, which also makes it easier for the patient.”
Dr Raman said the second component was that when doctors made a referral within the GPCCMP to see an allied health provider, the patient could now choose who they go to see.
One of the most important changes had been to item numbers for the preparation and review of plans, changing from 721 and 723 to 965 and 967 respectively, with the remuneration also changing.
“The webinar had a couple of components – what the plan is and how it operates, and from my perspective I was also there as a GP to talk about how it impacts me,” Dr Raman said.
“We also talked about the software component because there is a significant amount of software that has needed to be integrated. Operationally it’s all about workflow and keeping patients informed in the process.
“We’re in a timeframe where reform in primary care is something we’ve been calling for and we’re starting to see, so we need to acknowledge that these changes are part of that process.”
Dr Raman said that with the new Medicare GP CC management plan (GPCCMP), the changes were
“It’s not that previously they couldn’t choose, but if for whatever reason the allied health provider was no longer working there or their books were full, the patient would have to go back to their doctor, so that sort of doubles up,” she said.
“From an efficiency point of view there is significant change, and that’s good for a practising GP, but from the remuneration point of view I think we need to wait a bit longer to see how that plays out.
“But we’ve been calling for reform, and when change does happen, we need to look at it from a patient outcome point of view – and this is good for them because they find it a lot easier – and it’s also easier for the GP.”
Dr Raman said the College would continue to work with the government to ensure funding in general practice was supporting
Home to the Mandurah region’s only Dual Source CT machine

ChestRad are specialists in Cardiac CT, Chest CT and Lung Cancer Screening
Cardiologists – Dr Edmund Brice, A/Prof Abdul Ihdayhid, A/Prof Chris Judkins, Dr Sam Tayeb, Dr Justin Teng and Dr Tashi Zhaxiduojie
Cardiothoracic radiologists – Dr Conor Murray and Dr Shriv Srigandan
ChestRad's rooms are at the Mandurah Specialist Centre on Minilya Parkway, Greenfields (near the Peel Health Campus) All Medicare rebated services in Mandurah BULK BILLED!

www.chestrad.com.au
continued from Page 23
the care GPs provided to their patients.
“I think we can agree that improvements can be made to streamline and modernise it, and this is probably an important step forward in that,” she said.
“Change is a bit tricky, but most GPs I’ve spoken to have commented that the workflow and the operation of these GPCCMPs are a bit easier now because before there was a lot of paperwork and a lot of things to filter through to the allied health staff.”
Dr Raman told Medical Forum that chronic disease management remained a core function of general practice, particularly with the ageing population and issues
such as cancer survivorship, where patients might get a second cancer diagnosis but still had complex health issues because of previous treatment.
“With cancer treatment for example, someone who’s gone through chemotherapy or radiotherapy and surgery, just the chemotherapy side effects can be quite tremendous and affect multiple organ systems in the body including the skin, the gut, the eyes and the nervous system,” she said.
“And all of those need to be managed so the patient can come back to their normal life and be able to function, so they don’t feel like they’re unwell all the time.
“Sometimes people can develop auto-immune conditions, or they develop an intolerance to food
Under the CDM changes, existing items for the preparation of GP management plans, team care arrangements and reviews were replaced with a new GP chronic condition management plan.
The Medicare items have been simplified to a single item for plan preparation and second item for plan review.
The MBS fee for the preparation or review of a plan is $156.55 for GPs and $125.30 for prescribed medical practitioners.
Previously, the rebate for preparation of a GP management plan was $164.35, preparation of a team care arrangement was $130.25, and a review was $82.10.
Under the new arrangements, the GP chronic condition management plan is available to patients with at least one medical condition that has been, or is likely to be, present for at least six months, or is terminal.
Patients registered through MyMedicare must access the plan and review items through the practice where they registered, while other patients can access the items through their usual GP.
Where multidisciplinary care is required, patients can access the same services previously available through GP management plans and team care arrangements.
Practice nurses, Aboriginal and Torres Strait Islander health practitioners and Aboriginal health workers can assist GPs or prescribed medical practitioners to prepare or review the plans.
because so much of the gut has been disrupted by the treatment.
“There is also the psychological component, so we can’t forget the mental health services side of things.”
Dr Raman said that for now, the CDM reform process was still a work in progress.
“Overall, these recent changes have been well-received, but it is important to say we’re continuing to work with the government on the CDM funding to ensure it aligns well with general practice, and it’s still early days.”
This was part of our October CPD catalogue. Scan here to claim your time

Patients who had a GP management plan and/or team care arrangement in place before July 1 can continue to access services that are consistent with those plans under transition arrangements.
Any plans put in place since July 1 must meet the requirements of the new GP chronic condition management plan, and any new referrals for allied health services must meet the new referral requirements.
Patients would need to have their GP chronic condition management plan prepared or reviewed in the previous 18 months to continue to access allied health services.
From July 2027, a GP chronic condition management plan will be needed for ongoing access to allied health services and to access domiciliary medication management reviews.
GPs and prescribed medical practitioners can refer patients with a GP chronic condition management plan to allied health services in the same way as other referrals.
But the requirement to consult with at least two collaborating providers has been removed and the referral form for allied health services is no longer needed.

Stress is an essential consideration when approaching glucose management.
Not only does chronic stress impact the biological pathways that regulate glucose metabolism, but it also affects our ability to make positive lifestyle choices, such as having a consistent sleep routine, eating a healthy dietary pattern and exercising regularly.
As such, stress management and mental health support should be a cornerstone of our diabetes care plans.
While stress is a natural response to difficult situations, the prolonged production of glucocorticoids (GC) and catecholamines due to chronic stress can lead to longterm health issues. These include the development of diabetes and difficulty managing blood glucose levels in people living with diabetes.
GCs cause blood glucose levels to increase through a variety of mechanisms. Firstly, GCs increase gluconeogenesis and deplete glycogen, meaning there is increased glucose available to the body.
At the same time, GCs inhibit muscle and white adipose tissue from being able to take up glucose by inhibiting GLUT-4 transportation to the muscle cell surface and by interfering with insulin signalling in white adipose cells.
Stress can have a profound impact on the body and when it comes to diabetes it can even exacerbate symptoms, writes Dr Charlotte Rowley.
While that’s happening, corticosteroids also reduce the ability of the pancreas to produce and stimulate insulin. Increased catecholamines suppress glycogenesis, while increased levels of adrenaline and noradrenaline promote insulin resistance.
There’s a lot going on, even without considering the many other metabolic pathways that stress can impact upon.
Stress can also have a huge impact on our ability to engage with healthy lifestyle behaviours. When we are stressed, our brains have a reduced capacity to make positive choices.
When overwhelmed, the brain opts for the path of least resistance. If healthy eating and exercising is a new habit, there is more resistance to engaging with those choices.
This means it is harder to keep these habits going, and we fall back into old patterns, which might be less healthy food and sitting on the couch instead of going for a walk.
We also need to consider that stress triggers unhealthy coping strategies, which we may not even be aware of. One common coping strategy we see in clinic is emotional eating.
People may eat larger portions, or might seek out comfort foods, such as chocolate or ice cream. Even
when we are aware of healthier coping strategies, it’s harder to reason with ourselves to use them when the brain is already overwhelmed.
So, if stress and mental health management is so important in your diabetes care, what does this mean in practice?
What the doctor ordered
Part of being human is having negative experiences – chronic stress from work, family or home stressors, financial difficulties, the list goes on.
As practitioners, we aren’t able to remove these from the lives of our patients, but we can support them to develop beneficial coping strategies so they have healthy ways to deal with stressful situations.
If you aren’t already doing so, asking your clients about their stress levels is a simple place to start. Not everyone is open about their stress levels, either because of stigma and shame, or because they may not realise how stressed they are.
Sometimes these discussions take a while to eventuate, so don’t completely dismiss stress as a factor in care just because patients say they aren’t stressed.
Once we understand the stressful factors of a patient’s life, we can support them to access appropriate
Stress can also have a huge impact on our ability to engage with healthy lifestyle behaviours. When we are stressed, our brains have a reduced capacity to make positive choices.

services. Sometimes just the diagnosis of diabetes is a stressor, and a diabetes educator might be a great person to support them.
Diabetes distress must be considered, characterised by avoidance of diabetes management, frustration and overwhelm.
Sometimes our clients need to learn healthier coping strategies instead of emotional eating, in which case an appropriately trained dietitian can help.
Often, they will benefit from some form of mental health support or education, in which case a
counsellor or psychologist will be a beneficial addition to the care team. However, not everyone needs, or wants, intensive support, and may simply benefit from some low-level coping skills coaching. This is where the LISTEN program can be helpful. LISTEN, which stands for Low Intensity mental health Support via Telehealth Enabled Network is a new evidence-based program developed by The Australian Centre for Behavioural Research in Diabetes.
This telehealth service delivered by specifically trained allied health professionals, which will soon


be free to all West Australians, is designed to promote skills development and self-help in adults living with diabetes and cardiovascular disease and needing mental health support.
ED: Dr Rowley is a Diabetes Educator at Diabetes WA.
Diabetes WA will be offering the LISTEN program to West Australians living with diabetes.
Introducing the River and Garden Home Collection at Burswood Point. These elegant green-titled homes offer peaceful foreshore views, and effortless access to Perth’s CBD and major healthcare precincts.


Western Australia was one of the first jurisdictions in the world to regulate assisted reproductive technology (ART) and IVF back in 1991, but that legislation is now over 30 years old. It is outdated and no longer fit for purpose.
It has long been recognised that the previous legislation was discriminatory and based on a restrictive ‘command and control’ model of regulation.
To address this, legislative reforms were first proposed over eight years ago and a Bill to update the legislation was introduced in Parliament in 2019.
However, with the strong and divergent opinions that surround ART, this attempt was halted by a 22-hour filibuster speech, leading to six years of further reviews and delays.
Since then, there has been extensive community consultation, and a ministerial expert panel to guide the development of a new Act.
In August this year the Assisted Reproductive Technology and Surrogacy Bill 2025 was introduced in the Western Australian Parliament to replace the existing legislation.
This long overdue reform aims to modernise the regulation of ART in WA and align it more closely with other Australian states and territories.
The state’s assisted reproductive technology laws are no longer fit for purpose, but new legislation aims to change that, writes Dr Sebastian Leathersich.
The new Act will permit surrogacy for all West Australians, including same-sex couples, single men and gender-diverse people, improving equity in healthcare access.
The new Act will streamline assisted reproduction and surrogacy while expanding access to all in the state regardless of sex, gender identity, sexual orientation, relationship status, disability, race or religion.
Current laws restrict who is allowed to use ART, with IVF being available only to people who are diagnosed as ‘medically infertile’. This sometimes creates a need to ‘prove’ infertility before offering IVF as a treatment option.
In practice, this means single women and same-sex couples may be required to try several rounds of insemination before being allowed to access IVF, limiting their ability to choose the treatment that would be most appropriate for their situation.
The updated legislation will allow any person to access ART procedures if a medical practitioner certifies that the treatment is appropriate when taking into
account a person’s current and future circumstances.
The process for accessing preimplantation genetic testing will also be simplified. There will be a list of approved monogenic conditions maintained by a newly appointed advisory board, reducing red tape and potential delays to treatment.
The proposed Act also creates a pathway for the posthumous use of reproductive material (eggs, sperm or embryos) for the reproductive use of a surviving partner in cases when the deceased has provided explicit consent to that use.
Regarding donor conception, the new legislation will continue to keep the wellbeing of any child born from ART procedures at the centre of all decision-making.
Donor-conceived people will maintain the right to access identifying information about their gamete or embryo donors once they reach 16 years of age, ensuring
that they can obtain information about their genetic background.
The global five family limit, which places a limit on the number of families an individual donor can contribute to, will also remain in place, with clinics required to ensure adherence to this.
When it comes to surrogacy, there are several significant changes proposed. The biggest change is with respect to access.
Previously, only heterosexual couples or single females were eligible for surrogacy arrangements, a situation that has widely been considered discriminatory.
The new Act will permit surrogacy for all West Australians, including same-sex couples, single men and gender-diverse people, improving equity in healthcare access.
People seeking surrogacy arrangements will also be able to use donor sperm, eggs and embryos from de-identified donors, provided that the donor gave consent.
This will facilitate access to surrogacy for those that require donor conception, which was previously limited by the requirement for the donor – and their partner if applicable – to be part of the counselling process and legal agreements.
Administrative barriers will also be reduced under new laws, with surrogacy arrangements no longer requiring approval by the Reproductive Technology Council.
Although individual approval of each arrangement will not be required, people entering into a surrogacy arrangement will still need to obtain independent legal advice and attend counselling sessions to be eligible, as well as complying with all other regulatory requirements.
While there are likely to be substantial changes in the access to surrogacy and the processes surrounding it, protection of potential surrogates and the wellbeing of any child born from a surrogacy arrangement will remain paramount.
This includes prohibition of commercial surrogacy, or surrogacy arrangements that are ‘for reward’.
Donor-conceived people will maintain the right to access identifying information about their gamete or embryo donors once they reach 16 years of age, ensuring that they can obtain information about their genetic background.

The new Act also seeks to expand the reach of this requirement, making it an offence to enter into commercial surrogacy arrangements overseas.
While all arrangements must be altruistic, the new law will permit clinics to recruit potential surrogates, creating a means of introducing them to prospective intended parents and facilitating surrogacy arrangements.
Finally, the legislation would also allow parental recognition for those who have already had a child through an overseas surrogacy arrangement that could not be approved under previous legislation, and who have therefore been unable to become their child’s legal parent(s).
The proposed legislation passed the lower house in September, and it may not be long before we see these reforms introduced.
We, as clinics and clinicians, are prepared for these changes, which reflect contemporary societal values and would align WA with the rest of the country.
However, while these reforms will improve access to ART and surrogacy, the reality is that the sector is still governed by a patchwork of over 40 pieces of legislation across the country.
Recent adverse events have led to increasing scrutiny and calls for national regulatory harmonisation and the development of countrywide donor and surrogate registries, which would support improved safety and oversight and ensure that all Australians can access the same care, regardless of where they live.
ED: The Act is still making its way through Parliament so may be subject to change.
Dr Leathersich is the Medical Director of Concept Fertility.

A pilot program of advance care planning in general practice showed clear benefits for doctors and patients, writes Dr Kanwal Singh who took part in the pilot.
Embedding advance care planning (ACP) in general practice facilitates the integration of proactive ACP discussions. In turn this enables earlier, values-based conversations, improves alignment of care with patient goals and reduces family stress during acute episodes.
Supported by WA Primary Health Alliance, we took part in the Palliative Care Champions initiative, which has greatly improved staff skills and confidence in ACP and early palliative care through education and mentoring. It is now standard practice at our surgery, with staff and patients feeling better supported than before.
We nominated our Practice Manager Shikha Panag as our Palliative Care Champion and initiated regular practice meetings led by doctors to identify how best to embed ACP and bring the whole team on the journey.
Twelve months on, witnessing the tangible benefits for both staff and patients has been transformative. Overall, the project has strengthened our practice’s capacity to provide timely, coordinated, and patient-centred palliative care.
By integrating ACP discussions into routine appointments, health assessments (75+ and Indigenous Health Assessments) and chronic condition management plans, we now provide more personalised care.
We are trialling the Supportive Care model developed by WAPHA, involving consistent use of Primary Sense reports and two palliative care assessment tools.
There were several notable benefits delivered by the pilot, including:

We reviewed Primary Sense reports to identify our patients with complex needs and who may be at risk of dying within 12 months, and then adopted two palliative care evidence-based tools – the Australian Karnofsky Performance Scale (AKPS) and the Symptom Assessment Score (SAS) – as part of our assessment process.
These tools allowed us to proactively manage care in the setting of expected deterioration and trigger referrals to appropriate community and specialist services. The aim is to reduce crisis presentations to the emergency department and support choice for patients to remain at home for as long as possible, or to die there if that is their preference.
Our nurses are now actively involved in ACP delivery, conducting SAS/AKPS assessments, and developing GPMPs, enhancing team capacity and coordination of care.
Ongoing education has improved staff confidence and capability in recognising palliative needs and managing complex symptoms. Post-project analysis showed a significant uplift in skills.
Clinical flags such as frailty, frequent admissions and advanced chronic disease enable proactive identification and follow-up of high-risk patients. Regular contact and early interventions have helped more patients to remain at home and reduced avoidable hospital presentations.
The project has meaningfully improved coordination of care within our clinic and across services. It enhanced our team’s awareness and understanding of advanced health directives, which strengthened communication between clinicians, patients and external providers.
The practice integrated ACP into
routine workflows, leading to earlier and more frequent ACP discussions. High-complexity patients are now proactively identified and prioritised, ensuring timely care and allowing many to remain at home in line with their preferences.
The project also enhanced the practice’s quality improvement culture, with better documentation, data tracking and increased staff engagement.
The after-death audit involved a multidisciplinary review of all patient deaths over the past 6-12 months, focusing on the presence of ACP, place of death, involvement of palliative services and whether preferences were honoured.
Reflective meetings allowed us to analyse findings and identify areas for improvement, revealing that early ACP discussions increased the likelihood of patients dying in their preferred setting.
As a result, we embedded ACP prompts into chronic disease management, and regular after-
death reviews have become a standard part of our practice’s quality improvement efforts.
This has had many benefits, including CPD for Educational Activity, Reflective Practice and Measuring Outcomes.
A patient with advanced COPD took part in an ACP discussion with their GP and the clinic’s Palliative Care Champion, clearly expressing their wish to remain at home and avoid hospital admission at the end of life.
When their health declined, the ACP documentation enabled all providers to respect these wishes. The community palliative care team supported the patient to stay at home, where they died peacefully with family present.
This case study demonstrates how early ACP conversations and coordinated care can honour patient preferences and support their families.
Initially, we encountered hesitancy due to a lack of confidence among
our staff about initiating end-of-life conversations.
We overcame this through regular training, open dialogue and a collaborative approach involving all team members who have wholeheartedly embraced this new way of working and are seeing the tangible benefits for our patients and their families.
The practice now maintains ACP as a routine component of care, supported by ongoing team education, mentoring and systematic after-death audits to continually refine end-of-life practices.
ED: Dr Singh is a GP at Burslem Medical Centre, Maddington
Primary Sense is a clinical decision support tool for general practices in WA that share their de-identified, full population health data set.

This was part of our October CPD catalogue. Scan here to claim your time




The Play That Goes Wrong
7TH – 16TH NOV
Where everything that can go wrong… does!
James Morrison with Big Band Liechtenstein SUN 23RD NOV
A big band experience like no other, bringing to life the timeless classics.



Vegas The Show
21ST NOV All the glitz and glamour of Vegas!
Level Up
30TH NOV
Get ready as the award-winning WA Wind Symphony brings iconic video game soundtracks to life.


22ND NOV A Night of Music and Memories. The Wizard of Oz – A Traditional Christmas Pantomime
12TH – 24TH DEC
Click your heels together and get ready for a whirlwind adventure!



















We
often talk to patients about worklife balance, but do we practise what we preach?
In theory, time moves at a constant rate, but in the real world we’re always wondering where time is disappearing to.
Time seems to go faster when you are busy, and there doesn’t seem to be anyone in the health sector who is not busy.
Some years ago, at a presentation on managing and reducing stress, a point was made that time is our only finite resource – we each only get a limited number of minutes on this planet.
The recent passing of a doctor I went through medical school with brought it home.
The old adage that nobody on their deathbed regretted not spending more time at the office (or the surgery) still holds today. Headstones will typically describe the deceased as a husband/wife/son/daughter, rather than list their employment history or papers published.
Does that make our professional lives unimportant? Of course not. What it does say is that family and friendship ties are what endure.
More broadly as the year comes towards a close and we are all a year older, it is timely to reflect on how we spend our time. We often talk to patients about work-life balance, but do we practise what we preach?
What would we do if we knew we only had a month or a year to live? Would we act differently?
There is no right answer other than the one which is right for the individual. The key, in my opinion, is to actually ask ourselves the question: What really matters in my life and is this my focus? Complete your CPD with Medical Forum

Sign up to our Wednesday clinical newsletter to get the latest updates from your local specialists.
Scan the QR code to subscribe
By Dr Jens Carsten Ritter, Vascular & Endovascular Surgeon, Murdoch
The diabetic foot remains a challenge sitting at the intersection of neuropathy, ischaemia, and infection – a pathological triad that, if not managed promptly and effectively, culminates in tissue loss and amputation.
Despite advances in revascularisation techniques and diabetic care, diabetic foot disease remains a global health burden. Its consequences are devastating: a limb worldwide is lost every 20 seconds due to diabetic complications.
Up to 85% of these amputations are preceded by a foot ulcer and many are preventable with timely intervention.
Unfortunately, patients are often referred too late after having reached advanced stages where reconstructive options are limited.
Understanding the diabetic foot
There are three key pathological components to diabetic foot disease. They are:
Peripheral neuropathy: Loss of sensation and proprioception makes the foot vulnerable to repetitive trauma, pressure, and injury. Motor neuropathy leads to muscle imbalance and drives contracture deformities like claw toes.
Autonomic neuropathy reduces sweating, leading to dry, cracked skin and entry points for infection. All together they can drive the typical Charcot foot deformity characterised by collapse of the mid foot skeleton.
Peripheral arterial disease (PAD): Diabetes accelerates atherosclerosis and preferentially affects the small vessels – particularly below the knee with destruction of the foot arch. This pattern often makes surgical bypass challenging and endovascular solutions technically demanding.
Infection: Hyperglycaemia impairs immune function, allowing infection to spread rapidly through deep


tissue planes. Infected ulcers can rapidly progress to cellulitis, abscess, osteomyelitis, or even necrotising fasciitis.
These three components frequently co-exist and, in surgical practice, this overlap complicates management. Isolated strategies are bound for failure, making effective management of all components essential for successful outcomes.
Clinical presentation and diagnostic approach
The primary focus lies on identifying ischaemic versus neuropathic ulcers, signs of critical limb-threatening ischaemia (CLTI), extent and depth of infection and responsible microorganism and viability of tissue for healing post-revascularisation.
Key clinical signs include nonhealing or worsening ulcers at lasting longer that 4-6 weeks, rest pain, skin changes such as pallor, cyanosis, absence of palpable pulses and tissue necrosis, or foul-smelling discharge/gangrene.
• Plain X-rays to assess for gas in soft tissues or osteomyelitis
• Laboratory markers – WCC, CRP, ESR, HbA1c, renal function, and culture data guide systemic and local infection management
• ABI, toe pressures, tissue oxygen saturation
• Duplex ultrasonography – first line for assessing arterial status
• CT angiography or MR
angiography – for detailed vascular mapping/operative planning
• Digital subtraction angiography (DSA) – mostly with concurrent endovascular revascularisation
Revascularisation is the cornerstone of limb salvage. The options are:
Endovascular approaches: For example, angioplasty with or without stenting, atherectomy, drug-coated balloons.
Open surgical approaches: Endarterectomies and bypasses preferably using autologous vein as conduit. The choice depends on lesion characteristics (for example TASC classification), availability of suitable conduit, and patient comorbidities.
In diabetic patients, distal revascularisations even including the foot arch may be necessary, highlighting the technical challenges. Surgical debridement is often required to remove necrotic tissue, drain abscesses, or perform minor amputations. Where feasible, this is done in conjunction with revascularisation to optimise healing potential. Adequate anti-microbial cover is essential.
When the tissue loss is beyond salvage, revascularisation is not possible, or everything has failed, major amputation becomes necessary. The aim is to perform the
Diabetic foot disease is a common and serious complication of diabetes mellitus which can lead to limb-threatening infections, gangrene, and major amputations
Timely recognition of a threatened foot, diagnosis of peripheral arterial disease (PAD), and prompt revascularisation are crucial to limb salvage
A proactive and integrated approach remains key in preventing the devastating consequences of diabetic foot complications.
lowest-level amputation possible that allows for wound healing and eventual rehabilitation (below-knee over above-knee).
Major amputations carry high morbidity and mortality – up to 50% mortality at two years postamputation. Thus, every effort is made to avoid them.
Late referrals: Many patients are referred too late, by which time
tissue salvage may be already unrealistic.
Comorbidities: Poor cardiac, renal, and glycaemic control complicate surgery and recovery.
Patient compliance: Ongoing smoking, poor glucose control, and missed appointments lead to recurrence or failure of limb salvage.
The success of surgical intervention is heavily dependent on coordinated care. No single specialty can manage diabetic foot in isolation.
An effective core multidisciplinary team (MDT) includes endocrinologists, podiatrists, infectious disease specialists and vascular surgeons. It may be supported by orthopaedics/plastics, wound care nurses, rehabilitation specialists, GPs and community care providers/liaisons.
Early identification of high-risk feet, routine surveillance, pressure offloading, glycaemic control, and patient education are all nonsurgical yet crucial pillars that support surgical outcomes.
From a vascular surgeon’s

perspective, prevention is the most powerful tool in diabetic foot management. The surgical suite should be the last resort, not the entry point into care.
Key preventive strategies include regular foot screening and risk stratification, prompt treatment of minor lesions, smoking cessation and risk factor optimisation, education on foot hygiene, footwear, and daily inspection and early referrals
Vascular surgeons provide an essential part of care, however without multidisciplinary collaboration outcomes will be suboptimal.
The diabetic foot is not merely a surgical issue; it is a systemic and preventable problem that requires integrated care across all levels of the health system.
Patient education, prevention and early multidisciplinary intervention are key.
Author competing interests – nil





By Dr Nick Lan & A/Prof Abdul Rahman Ihdayhid , Cardiologists, Harry Perkins Institute of Medical Research
A 42-year-old male attends for a cardiovascular risk assessment. His older brother recently experienced a myocardial infarction at the age of 44 years despite being ‘fit and healthy’.
The patient has no other traditional cardiovascular risk factors, takes no regular medications, and physical examination is normal, including blood pressure, body mass index and waist circumference.
Investigations show a low-density lipoprotein cholesterol of 3.9 mmol/L, fasting glucose of 4.5 mmol/L and normal renal and liver function. The Australian CVD Risk Calculator estimates his five-year absolute risk at only 1%.
He asks you whether additional tests can be performed to better assess his cardiovascular risk.
A family history of premature coronary artery disease (CAD) captures the interplay between shared genetic, environmental and lifestyle factors within families.
A parental history of premature CAD is associated with an approximately 1.5-to-2-fold increase in risk, independent of other risk factors.
A sibling history may confer an even greater risk than parental history. The magnitude of risk can be influenced by the number of affected relatives, their degree of relatedness, and the age of disease onset. This highlights the importance of obtaining a detailed family history.
It is also important to consider inherited conditions such as familial hypercholesterolaemia or elevated lipoprotein(a).
Despite its predictive value, family history of premature CAD is inconsistently defined and variably recorded in medical records. Most

risk calculators, including the Australian CVD Risk Calculator exclude it from baseline risk estimates.
Instead, it is applied as a binary ‘risk reclassification factor’, defined as myocardial infarction or stroke in a first-degree female relative under 65 or male under 55.
This approach may underestimate lifetime risk, especially in younger adults where age is the dominant driver of calculated risk.
Although common genetic variants contribute to CAD risk, routine genetic testing is not currently recommended for clinical risk assessment. Polygenic risk scores for CAD remain largely research tools, not integrated into standard practice.
Family history identifies highrisk families, but not which individual will develop disease. Non-invasive imaging with cardiac CT has emerged as a method to personalise the risk assessment. It can also guide preventive strategies and potentially improve adherence to therapies.
Coronary artery calcium (CAC) scoring, obtained by non-contrast CT, quantifies subclinical calcified plaque and has strong predictive value for future events, but is not MBS rebated.
International guidelines recommend that CAC scoring can be considered in select asymptomatic individuals aged over 40 years who
A premature coronary event in a first-degree relative increases lifetime risk, but this is often under-recognised by standard risk calculators in younger people
Cardiac imaging personalises risk assessment: CAC scoring can detect subclinical coronary plaque (calcified only) and refine risk stratification, guiding preventive pharmacotherapies and potentially motivating lifestyle change and adherence
The CASCADE-MI trial will evaluate whether adding CT coronary angiography into routine risk assessment improves the preventive strategy for individuals with a family history of premature CAD.
are at low calculated risk but have a family history of premature CAD.
However, CAC does not detect non-calcified plaque, which may be present in younger individuals.
The CASCADE-MI trial
CT coronary angiography (CTCA) provides more information on plaque presence, burden, and morphology, including non-calcified and potentially high-risk features.
While current guidelines do not recommend CTCA for populationlevel screening of asymptomatic individuals, studies show that individuals with a family history
of premature CAD have a higher prevalence of both calcified and non-calcified plaque.
Medicare reimbursement for CTCA is only available via specialist referral when symptoms are present and coronary ischaemia is suspected.
We are conducting the CASCADEMI trial, a randomised study aiming to enrol 300 individuals aged between 30-55 with a first-degree relative with myocardial infarction before age 55.
Participants will be randomised to (1) routine risk assessment including the Australian CVD Risk Calculator, or
(2) routine risk assessment plus CT coronary angiography.
All CT imaging will be performed using state-of-the-art photoncounting CT, which provides highresolution plaque characterisation with low radiation exposure (Figure 1).
The primary endpoint is reduction in LDL-cholesterol at one year. Secondary outcomes include plaque detection – both calcified and non-calcified – initiation of proven preventive therapies such as statins, adoption of heart-healthy lifestyle modifications, and health economic analyses.
If successful, CASCADE-MI could redefine how inherited risk of CAD is managed, shifting clinical practice from population-based calculators towards personalised imaging-guided strategies for risk stratification and prevention.
Author competing interests – the authors are involved in the trial.
ED: The research team are looking for trial participants. If you have patients, or know anyone who may be eligible, please consider referring them to the CASCADE-MI trial run through the Harry Perkins Institute of Medical Research. More information is available at www. cascade-mi.org




By Tara Stevens, Credentialled Diabetes Educator, Diabetes WA
In Australia, one in seven pregnancies are complicated by gestational diabetes mellitus (GDM). Factors affecting the rates of GDM diagnosis are complex and can in part be attributed to changing diagnostic criteria, increased maternal age and increased maternal BMI.
In June 2025, the Australian Diabetes in Pregnancy Society (ADIPS) released their new consensus recommendations for screening and diagnosis of GDM, which will again impact rates of GDM.
Having gestational diabetes puts women at increased risk of developing Type 2 diabetes (T2DM). In Australia it is reported that between 30-50% of women with GDM will go on to develop T2DM within 10 years.
Aboriginal women who have had GDM have a cumulative prevalence of T2DM of 22% at 2.5 years postpartum. This shows that our Aboriginal mums are at even higher risk of going on to develop T2DM than their non-Aboriginal counterparts.
It is not just our GDM women we need to worry about in terms of progression to increased risk of T2DM. Offspring born to mothers who have had GDM have been shown to have higher BMI, increased risk of T2DM and adverse cardiometabolic health that go beyond birth, childhood, adolescence and even adulthood.
Post partum Glucose Tolerance Test (GTT) uptake to screen for T2DM is limited due to both systematic and personal barriers that women face. It is understandably a difficult time for women to do this as they are new mums who are often experiencing poor quality sleep, may be breastfeeding and are required to fast for this test.
The NDSS National Diabetes GDM Register provides women with follow-up reminders by SMS/


email with the aim to increase postpartum screening.
Regular screening is important in picking up T2DM early. It is also imperative to actively work with our women to maintain a healthy weight, eat quality foods and stay physically active.
Women in Australia who have had GDM are able to register for the NDSS ‘Baby Steps’ program, which aims to help women make lifestyle changes to improve their health and wellness and reduce their risk of T2DM.
It uses online motivational tools
in the format of video’s, learning sessions and interactive activities exploring topics around food, exercise and stress.
It also allows women to set achievable goals, link with monitoring tools such as activity trackers and gives women a place to log their HbA1c, weight and other biometric data. To use the Baby Steps program women must have a reliable internet connection, so access needs to be considered for women living in remote areas. Baby Steps was developed and researched by the Leicester
The optimal time for women to participate in the Baby Steps program is around 12 months postpartum. By this time, women have settled into being a mum and generally have more time to focus on looking after themselves
Baby Steps has been shown to decrease participants weight on average by around 1kg, increase their likelihood to participate in physical activity and make healthy food choices, and improves overall wellbeing
The chat function in the program allows participants to link with other women who have had GDM. This has been shown to boost engagement and women feel supported by their peers.
Diabetes Centre for the NHS and adapted for Australian women.
An Australian pilot evaluation demonstrated a significant decrease in weight of 0.98kg and significant increases in total fruit and vegetable intake, physical activity and overall wellbeing.
Importantly, 38% of the pilot cohort included women born outside of Australia in non-English speaking countries and 16% spoke a language other than English at home.
Studies of user experience for the Baby Steps program highlights that the private chat forum helped to boost engagement.
The main barrier to using the app currently is a lack of awareness in both women and their healthcare professionals.
A CSIRO survey of Australian women with previous GDM found that only 15% had heard of the Baby Steps app. Similarly, only 17% of healthcare professionals surveyed had heard of app.
Women have also indicated a preference of timing to hear about the Baby Steps app, with 12 months preferred over six weeks postpartum. At a recent GDM symposium held in Perth, attending
GPs suggested that vaccination schedules may provide a unique opportunity for primary care to engage with women with GDM and encourage them to participate in the Baby Steps program.
Author competing interests – nil

By Dr Michael Hancock , Endocrinologist, & Anneika Curtois, Diabetes Educator
Investigating and managing both type 1 diabetes (T1D) and type 2 diabetes (T2D) is rapidly evolving with the increasing uptake of advanced diabetes technologies.
Continuous glucose monitoring (CGM) and insulin pump therapy, particularly hybrid closed-loop (HCL) systems, are now central to best-practice care in T1D, while CGM technology is playing a growing role in T2D management.
For many GPs, these technologies may feel unfamiliar and outside of traditional care models, and their rapid evolution and integration into care may be overwhelming.
However, GPs remain crucial in providing ongoing diabetes management and coordinating multidisciplinary care. Gaining confidence in these tools can improve clinical outcomes and strengthen relationships with patients navigating an increasingly digital health landscape.
T1D is a complex, demanding condition. People living with T1D make over 180 additional healthrelated decisions each day compared to those without diabetes, ranging from insulin dosing and carbohydrate counting to exercise planning in unpredictable real-life contexts.
This constant decision-making burden can significantly affect quality of life and mental health.
As clinicians with lived experience of T1D, we recognise both the weight of this burden and the capacity of technology to ease it. Devices like CGMs and HCL systems help reduce the daily decision-making burden, minimise glucose variability, and provide reassurance through realtime feedback.
CGM technology is now fully subsidised through the National Diabetes Services Scheme (NDSS) for all people with T1D in Australia.
CGMs offer real-time glucose



readings and trend data, allowing clinicians and patients to detect patterns not visible through traditional HbA1c or snapshot fingerprick tests.
Key advantages of CGM include: Behavioural insight: Patients can see how diet, physical activity, stress, and medications affect their glucose levels.
Improved safety: Customisable alerts for hypo- and hyperglycaemia, supporting timely intervention. Shared data: Family members, carers, and clinicians can monitor remotely.
CGM interpretation can be done easily in general practice using data from patients’ smartphones or cloud-based platforms. Reviewing key metrics such as time-in-range and glycaemic variability (Figure 1), can guide therapy adjustments more effectively than HbA1c alone.
These tools are just as applicable for T2D patients, particularly those with sub-optimal control, using insulin or complex regimens.
In people with T2D, CGM use remains unsubsidised but is gaining traction. CGM has been shown to improve glycaemic outcomes and encourage patient behaviour change, particularly around food choices, exercise habits, and medication adherence.
Insulin pump therapy has evolved considerably over the past decade. Evolving from simple syringe drivers, modern HCL systems integrate CGM and pump technology to automate insulin delivery via algorithms which can adjust basal rates and give automated correction boluses if required, with minimal input from the user (Figure 2).
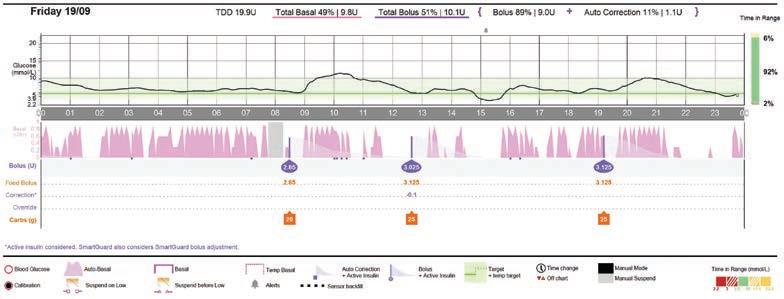
2: A HCL pump report, displaying auto-adjusted basal rates and correction boluses, with target glucose 5.5 mmol/L
There are a number of HCL systems currently available in Australia. These systems have been shown to improve time-in-range, reduce hypoglycaemia, and lower diabetes distress, even in complex groups such as adolescents and young adults.
However, access is limited to those with private health insurance or those able to self-fund, as no public subsidy currently exists.
GPs play a critical role in supporting and maximising the benefits of these tools, and GP confidence
in reviewing and discussing these devices can significantly enhance patient care.
For all patients:
Ask about diabetes technology use in routine reviews. Many patients are willing to demonstrate their CGM or pump interfaces.
This presents an opportunity to explore patients’ use of diabetes technologies, or lack of, and their relationship and engagement with their broader multidisciplinary specialist team.
Initiate and review CGM data via phone apps or printouts to guide
conversations about glucose patterns, lifestyle impacts, and therapeutic adjustments.
For patients with T1D:
Encourage all patients to access NDSS-subsidised CGM.
Where clinically appropriate, initiate discussions about the potential benefits of insulin pump and HCL therapy and refer to specialist diabetes services for further assessment and management.
Approach insulin pump discussions with curiosity. Many patients may know more than yourself, and their insights can lead to valuable, patientled conversations regarding their management and health.
For patients with T2D:
Consider recommending CGM in patients on insulin or with suboptimal control.
Use glucose trend data to guide decisions around initiating or adjusting insulin and to reinforce the impact of lifestyle changes such as diet and exercise on blood glucose, and help motivate change.
Author competing interests – nil
Mr Saud Hamza
Specialising in:
Oncoplastic Breast Surgery including breast reconstruction and rotation flaps
Breast reduction and mastopexy (nipple lifting)

Removal of breast implants and mastopexy Thyroid Surgery.
Practicing Location: Mandurah & Murdoch
Operating Locations:
St John of God Murdoch, Murdoch Peel Health Campus, Mandurah Hollywood Private Hospital, Nedlands
The Mount Hospital, Perth
Email: info@saudhamza.com.au
Healthlink EDI: mrhamzas

Dr Wei Ling Ooi
Specialising in:
Oncoplastic Breast Surgery including breast reconstruction and rotation flaps
Breast reduction and mastopexy (nipple lifting)

Removal of breast implants and mastopexy.
Practicing Location: Murdoch
Operating Locations:
St John of God Subiaco, Subiaco
Email: secretarydrooi@gmail.com
Healthlink EDI: wlingooi
Dr Kai Hellberg
Specialising in:
Gallbladder Surgery Hernia Surgery
Endoscopic Services with Gastroscopy & Colonoscopy Haemorrhoid treatments and other benign procto-rectal conditions
Ingrown Nail Surgery

All Skin and Soft Tissue Procedures.
Practicing Location: Mandurah & Murdoch
Operating Locations:
St John of God Murdoch, Murdoch Peel Health Campus, Mandurah
Email: murdochrooms44@gmail.com
Healthlink EDI: hellberg
Postal Address | Suite 44, Level 2, Murdoch Clinic, 100 Murdoch Drive, Murdoch WA 6150
Appointment Bookings | Phone: (08) 6148 0540 Fax: 9332 9425
www.perthsurgeons.com.au
BSc(Med), MBBS(UNSW), FRACS (Vascular), FRACGP, FARGP
Vascular and endovascular surgeon

What is your area of practice?
MA: I am a Vascular and Endovascular Surgeon with 20 years of surgical experience. I am also the first vascular surgeon in Australia and New Zealand to hold three fellowships – FRACS (Vascular Surgery), FRACGP (General Practice) and FARGP (Rural Generalist –Surgery/Emergency).
My work covers the complete spectrum of vascular and endovascular care from minimally invasive vein treatments to complex arterial and aortic reconstruction, delivered across both metropolitan and regional WA.
Where did you train and where do you practise?
MA: I completed my Bachelor of Science (Medicine) and Bachelor of Medicine and Bachelor of Surgery degrees at the University of New South Wales, Sydney.
My career has spanned metropolitan, rural, remote and Indigenous health settings across Australia. After years in regional Queensland, I moved to Western Australia serving with WA Health and the WA Country Health Service.
I currently practise in Geraldton, Bunbury, Albany, Mandurah and Perth, with admitting rights at St John of God Subiaco, Bunbury and Geraldton, Hollywood Private Hospital and Albany Day Hospital.
I founded Australian Vascular to bring specialist vascular care closer to home for regional West Australians.
My philosophy is
What procedural services do you offer?
MA: My practice includes a broad range of vascular and endovascular procedures, including: Aneurysm repair, aortic stenting and bypass surgery
Peripheral angioplasty and stenting
Varicose vein treatments – Radiofrequency Ablation (RFA), VenaSeal Closure System (Glue), and Liquid and Foam Micro-Sclerotherapy
Carotid and renal access surgery
Management of leg ulcers, superficial vein thrombosis, diabetic foot complications and hyperhidrosis.


Left: Endovascular repair of complex aortic and iliac aneurysms
Right: VenaSeal services are offered at Dr Al-Najjar's practice.
What sets you apart?
MA: My mission is different – I am building a state-wide network of regional vascular access and expertise.
By combining specialist vascular skills with dual fellowships in general practice and rural generalist medicine, I provide an integrated, holistic approach that few surgeons can offer.
This enables me to bridge the gap between tertiarylevel vascular care and the realities of rural health, ensuring rural patients receive the same standard of advanced endovascular and open surgery available in Perth.
My philosophy is simple: deliver cutting-edge vascular surgery without postcode disadvantage
I also invest heavily in education and collaborate with local clinicians. As a Clinical Senior Lecturer with the Rural Clinical School of WA, a member of both the RACS WA State Committee and the RACS WA State Trauma Subcommittee, a Co-opted member of the RACS Rural Surgery Section Committee (WA – Vascular Surgery), I’m committed to strengthening rural surgical capability and trauma readiness across the state.
www.australianvascular.com.au

By Dr Siva Sundararajan , General & Bariatric Surgeon,
Obesity is a major health burden linked to chronic disease, premature death, and rising healthcare costs. In Australia, 70% of adults are overweight or obese. Effective interventions are critical – not only to achieve meaningful weight loss but also to improve metabolic health and reduce comorbidities. For years, bariatric surgery was the only reliable option, but recently glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as a powerful medical alternative.
GLP-1 agonists were a medical breakthrough. GLP-1 is an incretin hormone that boosts insulin, suppresses glucagon, slows gastric emptying, and increases satiety.
Drugs like liraglutide, semaglutide, and newer dual-acting agents such as tirzepatide mimic these effects, leading to 10-21% total body weight loss in clinical trials, improved blood sugar control and insulin sensitivity, and reduced cardiovascular events and kidney benefits.
They have a good safety profile. Most side effects are gastrointestinal and transient. Rare risks include pancreatitis and gallbladder disease.
Long-term treatment is required; stopping usually results in weight regain. Patients stop treatment due to ongoing costs, side effects or lesser than expected results.
Bariatric surgery: still the gold standard
Bariatric (metabolic) surgery – most commonly sleeve gastrectomy and gastric bypass – works through restriction, malabsorption, and powerful hormonal shifts such as reduced ghrelin, increased GLP-1. Key outcomes include 2535% sustained weight loss, high rates of remission for diabetes, hypertension, sleep apnoea, and dyslipidaemia and reduced cardiovascular events, cancer incidence, and mortality.
While risks include bleeding, infection, and long-term nutritional

Bariatric surgery remains the gold standard for durable and substantial weight loss, with proven metabolic and survival benefits
GLP-1 receptor agonists have transformed pharmacotherapy, offering a non-surgical alternative with meaningful weight loss and cardiovascular protection
The future lies in personalised care, where surgery and medications are viewed as complementary, not competing, options.
deficiencies, modern surgical outcomes are comparable in risk to common operations such as hysterectomy or joint replacement.
Accessibility remains an issue: in 2024, more than 94% of bariatric surgeries in Australia were performed in the private sector.
In terms of efficacy, GLP-1 RAs show strong results in trials, but real-world effectiveness is lower due to high discontinuation rates –50% stop within one year and more than 70% by two years.
Bariatric surgery consistently achieves greater, long-lasting weight loss, up to five times more than GLP-1s in recent ASMBS data.
In respect of metabolic benefits, both improve cardiovascular and

metabolic outcomes. Surgery achieves higher diabetes remission rates (69% of insulin users discontinued therapy at one year). GLP-1 RAs reduce cardiovascular risk, particularly in high-risk patients.
Looking at safety and quality of life, GLP-1s avoid surgical risks and are less invasive. Surgery improves mobility, self-esteem, and longterm health-related quality of life.
From a cost perspective, surgery has a higher upfront cost but becomes cost-effective within 9-12 months compared to GLP1 RAs which must be continued indefinitely.
Obesity management is shifting toward personalised, combined approaches. GLP-1s may benefit patients with lower BMI (30–32 kg/m²) or serve as pre-operative therapy in very high BMI (>50–60 kg/m²).
Combination therapy, using drugs after surgery especially in cases of weight regain, shows promise. New incretin-based drugs and minimally invasive procedures will expand treatment choices.
Bariatric surgery and GLP-1 receptor agonists represent the two strongest pillars of obesity management today. Surgery remains unmatched for durable weight loss and metabolic improvement, while GLP-1 RAs have revolutionised medical therapy with impressive, though less durable, results.
These treatments should not be viewed as rivals but as complementary tools. The best approach is one tailored to the individual, balancing efficacy, safety, cost, and patient preference, delivered through shared decisionmaking and multidisciplinary care.
Author competing interests – nil
By A/Prof Ming Khoon Yew, Endocrine, Oncoplastic Breast & General Surgeon, Subiaco
Adrenal lesions are a frequent incidental finding on cross sectional imaging.
Adrenal incidentalomas (lesions >1cm) are found in approximately 4% of abdominal CT scans. The two key aspects of evaluation are hormonal function (biochemical status) and malignant potential (imaging characteristics).
Hormonal assessment
The three common hormonal systems that require assessment are:
Aldosterone/Renin Ratio-Primary hyperaldosteronism (Conn’s Syndrome): An underdiagnosed entity causing hypertension. Hallmarks include refractory hypertension and hypokalaemia. The typical Conn’s adenoma is a 1-2cm, CT imaging benign adenoma.
Plasma Metanephrines: Patients with Phaeochromocytoma are often asymptomatic. Paroxysmal symptoms indicate the typical intermittent catecholamine release by the tumour.
These include palpitations, flushing, sweating, headache,


tremor, and anxiety. The typical phaeochromocytoma is a lesion >2cm with a high Hounsfield unit on CT scan.
Cushing’s Syndrome - 1mg Dexamethasone suppression test: Patients with Cushing’s Syndrome may be asymptomatic. Classical features include moon faces, acne, obesity, striae, easy bruising, osteoporosis, hypertension and
Cushing’s syndrome or subclinical Cushing’s syndrome
poor wound-healing. The patient takes 1mg of Dexamethasone at 11pm the night before the morning serum cortisol is sampled.
Cushing’s adenoma is typically >3cm with benign imaging characteristics.
Malignant potential
The imaging characteristics are key to the triaging of adrenal masses.
May be asymptomatic
Moon face, acne, buffalo hump, supraclavicular fat-pads, central obesity, striae, easy bruising, poor wound-healing, emotional and cognitive changes Hypertension
Conn’s syndrome Mostly asymptomatic
Muscle cramps, periodic paralysis, headaches, palpitations
Polydipsia, polyuria
Phaeochromocytoma
Adrenocortical carcinoma
Metastasis
May be asymptomatic
Palpitations, flushing, sweating, headache, tremor, anxiety
Mass effect
Palpitations, flushing, sweating, headache, tremor, anxiety, hirsuitism, gynaecomastia, amenorrhoea, infertility
Mass effect
Usually non-functional
Hyperglycaemia
Hyperlipidaemia
Osteoporosis
Hypokaleamia
(<3.5 mmol/L)
Severe hypertension
Weight loss
Severe hypertension
Weight loss
Malignant disease elsewhere
If hypertensive, plasma aldosterone to plasma renin activity ratio
Plasma Metanephrines
Plasma metanephrines and serum androstenedione, testosterone, DHEAS
Usually non-functional
Plasma metanephrines, Renin/ Aldosterone ratio, 1mg Dex suppression test
A patient with adrenal incidentaloma requires assessment of hormonal function and risk of malignancy
Findings to suggest referral include abnormal biochemistry and adrenal lesion >3cm
Surgery may be laparoscopic or open.
Most adrenal incidentalomas are benign non-functional adrenal adenomas. The incidence of benign non-functional adrenal adenoma increases with age.
The following features are typical of benign adrenal adenomas:
• A 1-3 cm uniform/ homogenous lesion
• A CT non-contrast Hounsfield unit (<10)
• High contrast washout and rounded, well demarcated margins.
CT features that raise concern for malignancy are size >3cm, irregular margins, heterogeneity and
invasion of adjacent structures. Malignant adrenal neoplasms are either primary or secondary. Primary adrenal malignancies are carcinoma, sarcoma, or lymphoma. They are usually large masses (5-20cm).
These are rare but highly aggressive requiring early referral to a specialist adrenal surgeon.
Secondary adrenal malignancy may arise from many solid tumours as the adrenal gland is a common site of metastasis. Necessarily a history of malignancy is suggestive.
Most benign tumours – functional or non-functional – and most metastatic lesions of the adrenal gland can be safely and successfully excised via a minimally invasive approach.
Laparoscopic adrenalectomy requires dissection of viscera overlying the adrenal gland (e.g. liver; pancreas; spleen).
Prone Retroperitoneoscopic Adrenalectomy has become popular because this approach provides more direct access to
the adrenal gland, requiring less dissection, resulting in quicker patient recovery.
Open resection is reserved for large benign adrenal neoplasms (>7cm) and primary adrenal malignancies. Adrenocortical carcinoma is a rare and highly aggressive malignancy.
Open resection without breach of tumour margin is critical to minimise the risk of recurrence. This may involve en-bloc nephrectomy if there is invasion of the kidney.
After unilateral adrenalectomy, the remaining adrenal is sufficient to maintain normal hormonal homeostasis.
Author competing interests – Dr Ming Yew is the first WA provider of Prone Retroperitoneoscopic Adrenalectomy surgery.

Delivered in collaboration with Western Cardiology, our Acute Cardiac Service provides a direct referral pathway for privately insured patients presenting with acute cardiac conditions, including:
• Chest pain
• Cardiac arrhythmia (such as bradycardia)
• Presyncope/syncope
• Suspected heart failure
• Pacemaker/cardiac device issues
Eligible patients who meet admission criteria are admitted directly to our CCU.
By referring suitable patients to the service, you can ensure they receive efficient, comprehensive cardiac care in the comfort of a private environment.

By Dr Prue Gregory, Advanced Trainee in Renal Medicine, & Dr Aron Chakera , Nephrologist, North Metropolitan Health Service
Diabetic kidney disease is now the leading cause of progressive chronic kidney disease (CKD) and kidney failure in Australia and other developed countries.
CKD is itself a major risk factor for cardiovascular disease and the cardiovascular-kidney-metabolic (CKM) syndrome is now being recognised by authorities to highlight the link between heart disease, kidney disease, diabetes and obesity as a driver of poor health outcomes.
Recent randomised-trial evidence has expanded the role of glucagonlike peptide-1 receptor agonists (GLP-1 RAs) from diabetic and metabolic drugs to a CKM therapy, adding a fourth pillar to the current guideline-based management of diabetic kidney disease.
This includes renin-angiotensin system inhibitors (RASi), sodium glucose co-transporter 2 inhibitors (SGLT2i) and the non-steroidal mineralocorticoid antagonist (nsMRA) finerenone.
GLP-1 RA and diabetic kidney disease.
Semaglutide is a GLP-1 RAs which mimics the natural hormone

resulting in increased insulin secretion and decreased glucagon release, resulting in lower blood glucose levels.
Other actions include delayed gastric emptying, appetite reduction and increased satiety. There have been several GLP-1 RAs cardiovascular studies completed which demonstrated a reduction in cardiovascular risk and all-cause mortality, with secondary endpoints demonstrating a reduction in


proteinuria and slowing of diabetic kidney disease progression.
On the background of this data, the FLOW trial was designed to primarily look at the kidneyprotective effects of GLP-1 RA in diabetic kidney disease cohort.
FLOW was a large, international, double blinded, randomised control trial conducted in more than 25 countries. It recruited over 3500 adults with type 2 diabetes mellitus (T2DM) at high risk of CKD on maximal tolerated RASi. The intervention was Semaglutide 1mg weekly vs a placebo.
The trial was stopped early for efficacy after a median of ~3.4 years follow-up because semaglutide significantly reduced the primary composite endpoint – kidney failure events, persistent substantial eGFR decline, or renal/ cardiovascular death – by ~24% versus placebo.
The benefits were seen across the range of baseline CKD severity and were accompanied by reductions in major cardiovascular events and all-cause mortality. FLOW has confirmed the reno-protective effect of GLP-1 RA in diabetic kidney disease and adds another

Semaglutide significantly reduced adverse kidney and cardiovascular outcomes in people with T2DM and CKD
Use the four-pillar framework (RAS blockade, SGLT2 inhibitor, nsMRA and GLP-1 RAs) to optimise the management of diabetic kidney disease
Counsel patients about expected benefits (kidney, cardiovascular, metabolic) and common side effects (GI) and titrate slowly.
important layer to the management of diabetic kidney disease going forward.
In July 2025, the manufacturer of semaglutide advised that its supply has significantly improved, allowing the Therapeutic Goods Administration (TGA) to lift the

FLOW trial and included a second indication that semaglutide is “indicated as an adjunct to standard of care therapy to reduce the risk of sustained decline in kidney function and to reduce the risk of cardiovascular death in adults with type 2 diabetes and chronic kidney disease”.
While this change is yet to extend to the Pharmaceutical Benefits Scheme (PBS) it is a positive step forward in expanding our management of diabetic kidney disease.
In summary, diabetic kidney disease is the leading cause of end-stage kidney disease in Australia and costs the country $2.68 billion each year.
Early detection and implementation of multi-modal medical therapy can dramatically slow progression and improve outcomes of individuals with diabetic kidney disease.
Guidelines now recommend a stepwise approach to care commencing with lifestyle modification followed by introduction of medications using the four-pillar framework for
residual risk factor optimisation. The management of diabetic kidney disease has evolved substantially over the last 10 years and outcomes have improved as a result.
However, challenges remain to ensure equitable access to these life-changing therapies within the Australian health system and supporting patients to maintain adherence in the face of polypharmacy, cost pressures, and treatment complexity.
Author competing interests – nil
Surgery vs GLP-1 agonists
Reducing T2D after gestational diabetes
Predicting inherited coronary artery disease
Managing diabetic foot disease
Assessing and managing adrenal lesions
Diabetes technology in general practice
Semaglutide and diabetic chronic kidney disease
The have and have-nots of diabetes care
Stress and diabetes
WA’s proposed new reproductive laws
Is it pelvic venous congestion?

Children with cystic fibrosis will be included in the next phase of a clinical trial of a WA-pioneered treatment aimed at boosting their immune responses.
Developed by researchers at The Kids Research Institute Australia and Perth Children’s Hospital the treatment, known as RSP1502, uses an antibiotic booster to improve the effectiveness of treatment for Pseudomonas aeruginosa infections in people with cystic fibrosis.
Respirion Chief Scientific Officer
Professor Barry Clements said a Phase 1b study of the trial had been successful, allowing researchers to proceed to a Phase 2 study involving children aged 12 years and older.
“With limited antibiotic options to address rising bacterial resistance, new options are urgently needed for people with cystic fibrosis and RSP-1502 represents a longawaited breakthrough for this vulnerable population,” he said.
The Phase 1b study was conducted under US FDA oversight and tested ascending doses of the RSP-1502 combination in cystic fibrosis
patients, with the highest dose proceeding to be tested in a Phase 2a study in children and adults.
The follow-on Phase 2a study will test the efficacy of RSP-1502 in reducing bacterial infections and improving lung function, as well as examine how the combination reduces biomarkers of inflammation in the lung.
The Phase 2a study will involve PCH and eight other sites in Australia, as well as additional sites in the USA, and will enrol 40 children and adults with cystic fibrosis.
“We are very excited by the potential for RSP-1502 to solve the challenge of chronic lung infections in children and adults,” Prof Clements added.
An early WA-based pilot study of chronically infected cystic fibrosis patients demonstrated an average 16% improvement in lung function, compared to 5% for patients using a standard of care antibiotic treatment.
The Phase 2a study will bring the new drug closer to receiving international regulatory approval, providing people with cystic fibrosis access to a more effective treatment which, if started early in childhood, could slow disease progression.
The treatment also has broader potential in other chronic lung conditions where new and effective antibiotics are needed.
Recruitment for the Phase 2a study is currently underway. Visit clinicaltrials.gov/ search?intr=RSP-1502 for more information
By Dr Aleena Ali , Australian Centre for
Diabetes Innovations, & Prof Grant Morahan , Harry Perkins Institute for Medical Research Foundation
Two million Australians have diabetes and a third of people with diabetes develop serious complications that have a significant impact on quality of life and a high economic toll.
One of the complications of diabetes is diabetic kidney disease (DKD), the leading cause of kidney failure in developed countries. Treating DKD costs Australia $2.68 billion annually.
Diabetes management
Management of diabetes currently focuses on glycaemic control to keep levels of glycosylated haemoglobin (HbA1c) below 7.5% (57 mmol/L).
Treatment strategies combine exercise, diet, and medications. Options for pharmacotherapy depend on the type of diabetes and may include oral hypoglycaemic agents, injectable medications and insulin.
Novel treatments approved for treatment of type 2 diabetes like SGLT2-inhibitors or GLP-1/GIP agonists not only help glucose control but have additional benefits that can reduce complications of diabetes.
SLGT2-inhibitors target sodiumglucose co-transporter 2 channels in proximal renal tubules. These agents offer modest improvements in glycaemia, blood pressure and weight.
The meaningful benefit, however, is achieved in cardiovascular morbidity, preventing progression of DKD and reduction in all-cause mortality.
GLP-1/GIP agonists target glucagonlike peptide +/- glucose-dependent insulinotropic polypeptide. These agents have potent glucose-lowering and weight-reduction effects and offer additional cardiovascular benefits including reduction in atherosclerotic disease, stroke and heart failure in people with obesity. They have also been shown to prevent decline in renal function,
reduce steatosis in metabolic liver disease and provide reduction in all-cause mortality in people with established cardiovascular disease.
Expensive treatment may be unnecessary for the approximately 70% of people who will not develop complications. However, it has not yet been possible to identify at the time of diabetes diagnosis who will develop complications.
For example, routine blood and urine tests can monitor kidney function but cannot predict future DKD outcomes, only any impairment detectable at the time of the test.
Optimal intervention requires a test that can be performed at the time of diabetes diagnosis and before the appearance of clinical signs.
This means that most people living with diabetes receive the same advice about glycaemic control even though most will not develop complications.
In collaboration with the Australian Centre for Accelerating Diabetes Innovations (ACADI) we reasoned that a genetic test could predict DKD risk years before onset of clinical signs – before the disease process is significantly underway.
Previously, we developed methods to produce a genetic risk test to identify people at higher risk of heart failure.
Applying these methods to data from the UK GOKIND study and Australian adults attending the Diabetes Clinic at the Austin Hospital in Melbourne, we generated a preliminary genetic test for risk of DKD.
More than 3600 people with diabetes were sorted into two groups: one having had a diagnosis of diabetes for at least 10 years, but without DKD, and the other with evidence of kidney failure (DKD).
Data included people with type 1 or type 2 diabetes, with or without


a diagnosis of DKD. The test was validated with patients’ data from other diabetes clinics across Australia.
Evaluation of medical tests and the strength of associations commonly use the Odds Ratio (OR) statistic. This compares the odds of an event occurring in one group to the odds of it occurring in another.
For context, most genetic studies of diabetes complications report an OR around 1.2 – so higher risk people have a 20% increase in their odds of DKD.
The OR of our DKD Risk test was 29.1 for the high-risk group. People at high genetic risk developed DKD more quickly than those at low genetic risk.
Examination of their medical records also found people in the high genetic risk group were more likely to have other complications, including retinopathy, neuropathy, cardiovascular disease and stroke.
There were no statistically significant differences in HbA1c, body mass index or duration of diabetes between those with and those without DKD, in either risk group.
Significantly, hyperglycaemia only increased odds of DKD in the low genetic risk group. These results suggest that genetic factors more strongly influence DKD than other clinical or modifiable risk factors.
Prediction of a person’s risk status at the time of diabetes diagnosis offers the opportunity to provide earlier and more targeted management to someone with high genetic risk, delaying or even preventing complications.
In contrast a person with low genetic risk could be advised to promote healthy lifestyle factors to avoid complications of diabetes.
Author competing interests – the authors were involved in the research.
Lisa Ellery’s second crime thriller strikes gold in Kalgoorlie, where a missing prospector exposes a vein of mystery running deep beneath the red dirt.

By Ara Jansen
You recognise an author really knows the city they are writing about when their wry comments are spot on.
In Lisa Ellery’s new book Hot Ground, the lawyer and author reminds us that Kalgoorlie people don’t care how early Perth people had to get up to catch a flight into town.
She also reminds us of the first rule of travel in WA: you must “confess in advance if there was someone who ought to know you’re in town, otherwise you’d be guaranteed to run into them in the street”.
It’s these quirky and astute daily life observations which pepper Lisa’s latest crime story, set in Kalgoorlie, a city where she has lived for more than two decades.
You might even go so far as to say it’s a bit of a love letter to one of the state’s largest regional cities.
While Lisa’s first book Private Prosecution was set in Perth, the author felt it was time to write about her own backyard.

“I love Kalgoorlie,” Lisa says. “I love the environment and I love the people here, the community, the sense of excitement and opportunity. There’s an ongoing gold boom; people are continuing to travel from all over the world to build their careers here.
“This book is a crime story and it has the added element of being located regionally. While it’s not ocker, I haven’t shied away from the things which make the story very West Australian and specifically very Kalgoorlie. We are very different here. It’s a different life.

“I feel like Kalgoorlie has all the benefits of a larger centre, while at the same time the benefits of a country town. Everyone has your back and if you don’t know people, you know of them. It was important in writing this book that I didn’t want to use all the cliches, like the skimpies, but show the place as it really is.”
In Hot Ground Detective Jessy Parkin, from Private Prosecution, takes centre stage after being sent to policing purgatory in Kalgoorlie. Her first big case is to find a missing prospector, a mystery built on the shifting sands of much coveted gold.
Lisa says she didn’t gel well with her character Jessy in the first book, but a conversation with a young police officer revealed that as an anxious person, when she put on the uniform, she became the person she wanted to be.
This gave the author an idea as to where she could take Jessy and she grew into the main character in Hot Ground

We’re continuing our bumper round of competitions this month with movies tickets, another book giveaway and more wine.
The British Film Festival returns from November 5 to December 7, with new releases, documentaries and retrospectives. Leading the festival is The Choral, a wartime drama led by Ralph Fiennes and directed by Nicholas Hytner.
We have five double passes to giveaway.
We also have five copies of Hot Ground up for grabs.
And we’ve got another round of WA wine for one lucky reader, this month from Sandalford Wines in the Swan Valley. Read our Master of Wine’s review on page 55.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
“I got to know her really well through this book and like her a lot. When I first wrote the story, I wasn’t happy with the policing side of it because it didn’t have enough accurate detail about how cops might conduct an investigation on a day-to-day basis, and that also impacted the character development.
“I wound up speaking to a police consultant who helped me turn Jessy into who I wanted her to be.”
In the four years between books, Lisa sold her law practice and considers herself semi-retired while working for a small select group of clients.
“I’m really happy about how it has turned out. The fact that I have been able to get a publishing contract for two books is just such an opportunity. I wanted to put my heart and soul into writing and it seems I’m good at it. Book three is already well on the way.”
Alongside writing, this has also allowed her to commit more time to her other passion – running. While
it might seem crazy to be a runner in a region as hot as the Goldfields, Lisa says it’s a glorious sport for the area. You just have to get up a little earlier.
“It’s a great place to run – the bush is beautiful here. You can head out on a bush track and by 8.30am be sitting at your desk ready for your workday. In summer we run at 5.30am.
“I’ve probably been running for 20 years. I get a high from it. I love running with friends and tend not to run on my own anymore. The social side of it is important. With running you meet new friends all the time, which I love.
“I run for a lot of reasons, and one is mental health, including social connection, even if you’re too puffed to speak. I also like being in nature – there’s something about the Goldfields bush in the morning sunlight.”

An early years album made in Fitzroy Crossing is not only preserving and sharing language but also supporting wellbeing.
While plenty of people consider music to have healing powers, in a Kimberley community it has also become a way to share and preserve Indigenous language, support language development and add to children’s wellbeing.
Buga Yanu Junba has been a multi-year project resulting in a joyful 22-track album of songs for young children and an illustrated companion songbook.
Sung in the languages of Bunuba, Gooniyandi, Walmajarri, Kimberley Kriol and English, the album celebrates language and culture as well as being a practical tool for early years learning.
Many of the songs were created
By Ara Jansen
through a research project, where songwriting in local languages was trialled to support children’s wellbeing and language development.
The original collection was written and recorded by Fitzroy Valley educators from the Marninwarntikura Women’s Resource Centre and the Baya Gawiy Children and Family Centre as part of Tura’s Sound FX program – an award-winning intercultural initiative exploring music, storytelling, cultural knowledge and language through long-term collaborations in the Kimberley. The songs cover a variety of topics such as sustainability of the land,
the return of the brolgas at each hot season and family gatherings, not overfishing and the different types of fish in the Fitzroy River.
Research undertaken during the project has shown that singing these new songs supports wellbeing. Educators observed enhanced feelings of calm, safety, connection and engagement among children when the songs were sung – outcomes that speak directly to the links between music and mental health.
Project lead Dr Gillian Howell says because of the length of the project, the early years educators were able to share the songs with the children as they went along to

see how they were reacting. They also tried them out on the local radio station to get feedback.
The musician and researcher says Buga Yanu Junba has also been a wonderful opportunity for generations to connect through song and music, as well as numerous singers finding their voices for the first time.
“One woman also used the project as an opportunity to become fluent in her language and connect better
with her Elders, which she hadn’t been able to do.
“Making music is something very human and it’s something we have always done. The sense that you are not good enough can strangle your breath. People also carry a lot of emotion around music, similar to how they carry emotion around language.”
The project has been a collaboration between educators, families, Elders, musicians,
language custodians, researchers and cultural advisors.
Gillian says embedding language with care for each other is something that can carry through generations and the more people become familiar with language carries everyone along.
These songs are more than just music – they are sources of cultural knowledge, central to the care and nurturing of Baya Gawiy’s children and their families.
Published by the Indigenous Literacy Foundation, the companion illustrated songbook extends the songs’ reach with lyrics, chords and notation, in-depth translations and introductions from each songwriter.
There are even karaoke versions of each song, a valuable tool for educators or families singing along at home.
Stream the Buga Yanu Junba album for free at tura.com.au and buy the songbook from bookstores.
Wild Swan is our contemporary fine dining restaurant, overlooking the manicured gardens and the Llawn at Mandoon Estate. Executive Chef Michael Hartnell and Wild Swan Head Chef Anthony Power have created modern and innovative a la carte and tasting menus that combine classic techniques with the finest local and seasonal produce. Their modern Australian menu has been carefully designed to match with our award winning wines and craft beers.








Our podcasts bring you the latest updates and key insights into new treatment options available.
Join our clinical editor Dr Joe Kosterich in conversation with WA specialists to learn more about developments to improve patient outcomes. Our podcasts are now CPD verified. Look for the CPD logo to complete your self-reflection and claim your time.
Learn more about:
Is it pelvic venous congestion? With Dr Marek Garbowski
Aortic stenosis: managing low-risk patients with Dr Gerald Yong
Rethinking radiation oncology with A/Prof Yvonne Zissiadis & Celia Byatt
Lung Cancer Screening with Prof Fraser Brims
How to approach acute and chronic knee pain with Dr Jean Louis Papineau
Listen on your favourite podcast platform – scan the QR code to follow us!
Located in the heart of the Swan Valley, Olive Farm Wines is steeped in history with the vineyard originally established by Botanist Thomas Waters in 1829.
This makes it the oldest vineyard site in WA and the second oldest in Australia. In 1933 Ivan Yurisich migrated from Yugoslavia and bought Olive Farm. starting a WA family wine dynasty. Then came second generation Vince, who by 1964 had added a new level to their winemaking, including making WA’s first traditional method sparkling wine.
By 1981, Vince’s son Ivan was at the helm and, being the first of the family with formal winemaking qualifications, he took the family business to a new level. A big change occurred in 2006 with a new purpose-built winery and a move within the Swan Valley.
Fourth generation Anthony Yurisich became the winemaker in 2008 and is still in charge today. He has been innovative, adding new varieties and wine styles. With 22 hectares under vine on site with the winery, he produces 40 wines from 25 grape varieties. Many styles are made – sparkling, whites, reds, rose, dry, sweet and fortified.
Some old vine Grenache is outsourced within the Valley but most wines are Estate grown. I reviewed six of Olive Farm’s wines and they certainly demonstrate the quality of our Swan Valley.


Olive Farm 2025 Swan Valley Verdelho RRP $29
Aromas are fruity with tropical notes of pineapple. The mid-palate fruit weight is typical of the Valley and the textural mouthfeel is balanced by the mineral backbone. Lemon rind and citrus flavours abound. A great seafood wine now with a six to eight year future.
Olive Farm Museum Release 2019 Swan Valley Chenin Blanc RRP $40
A wine that demonstrates very nicely what this variety from the Swan Valley can do with bottle age. The nose is wonderfully complex with ripe stone fruits. Palate is also complex with great fruit weight. Shows lanolin, lemon curd and a touch of toast. Its acidity holds it together and is central to its longevity. Drinking perfectly now and will reward for a few more years as it gains more honeysuckle and toasty characters.
Olive Farm 2025 Swan Valley Alicante Rose RRP $29
Made from the Alicante Bouchet grape variety, the unique feature of this grape is that it is redfleshed and lends itself to the rose style. The iridescent pink/red colour of this wine is striking. I see this as a fun wine for early consumption and great on warm summer days. It is sweet fruited, with overt red berry flavours, confectioned, fruit pastels but finishes dry.
Olive Farm 2021 Swan Valley Petit Verdot RRP $33
A Bordeaux variety usually used sparingly in blends, but with a few varietal examples now produced. It suits warm climates like the Swan Valley as it ripens late. Youthful for its age, the nose shows cedary oak, bramble bush, and menthol. Palate is full bodied showing earthy characters, mulberry, dark plum and cardamon. Currently drinking very well.
Olive Farm 2018 Swan valley Reserve Cabernet Sauvignon RRP $42
Another big wine. Displays a deep garnet colour with a slightly browning meniscus reflecting its seven years age. Herbaceous aromas with some aniseed and coffee ground. Palate is medium to full bodied showing power with some delicacy. Flavours of blueberry, blackberry and a touch of liquorice. Has good length and finish, will reward for another five to seven years.
Olive Farm 2018 Swan Valley Reserve Shiraz RRP $42
Wow! This is my top choice of this tasting – big, bold and beautiful. The Reserve label implies careful fruit selection and quality production and oak. The aromas are big with cracked black pepper, Indian Ink, and cigar box oak. Palate is vibrant aniseed, mushroom and black olive. The massive 15.4% alcohol is in balance, as is the oak. Flavours are long with a great finish. This wine has another 10 years in it yet.
This page intentionally left blank


CONTACT
VR GP POSITION
Full/Part-time or Weekend
• Brand-new
• Private Billing
• Supportive Team
• Modern Private Practice
For clinic details please visit jsmnorthbridgedoctors.com.au
For enquiry please email us at: admin@jsmn.com.au
Scan QR code for more details

CONTACT
GP OPPORTUNIITY
Who want to make a difference
In Aboriginal Health
• Competitive salary
• Mon/Fri (Thurs eve) Bunbury
• No weekends or on-call works
• Should be flexible for outreach clinics
• All travel done during work hours
Human Resources Dept : 9797 8111 during normal business hours
E: HR@swams.com.au
Scan QR code for more details

BURSWOOD
CONTACT
Dr Ang:
P: 08 9472 9306
E: info@thewalkingp.com.au
Scan QR code for more details
• 75% of gross billings
• Accredited mixed-billing clinic
• Perfect for new VR GP’s
• Full/Part-time options.

CHURCHLANDS
CONTACT
Practice Manager:
Seeking a GP who can work regular full time or part time hours
• No after hours consulting
• Remuneration is negotiable.
• Well equipped treatment room.
• Pathology adjacent.
• Privately owned/Mixed billing.
• Friendly registered nurses and experienced administration support.
E: practicemanager@herdsmanmedical.com.au
Scan QR code for more details

CONTACT
Jasmine Brierty:
P: 0457 905 538

CONTACT
Practice Manager: P: 08 6165 2444
E: reception@comogp.com.au
Scan QR code for to email

CONTACT
Practice Manager Folu:
P: 0435 800 320
Opening for VR GP - F/time or P/time Full Private List Available
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
• FRACGP essential
• Up to 70% private billings
• Enjoy working for a doctor-owned, non-corporate, well support, and accredited practice.
• Busy mixed billing general
• Well established patient base
• Flexible working hours
• Nursing support
• Positive team environment
E: pmanager@parkwoodmc.com.au
Scan QR code for more details

Jindalee Medical Centre Full or Part-time GP
• Flexible arrangement to suit lifestyle
• Private billing Mon-Fri practice
• On site pathology
• DPA approved location
• 12 consult rooms, treatment & procedure rooms.
E: Jasmine.Brierty@ipn.com.au
Scan QR code for more details


The ECU Health Service is seeking expressions of interest from vocationally registered general practitioners
15% service fee
Mixed billing
Free, reserved parking
Full time registered nurse support
Exceptional administrative support team
Best Practice Premier (Spectra)
Flexibility of four to six sessions per week.
Monday to Friday, 8.30am – 4.30pm. No weekends or after-hours.
Located within the Wellbeing Precinct on the ECU Joondalup Campus, our AGPAL accredited, purpose-built general practice is on the same floor as the free student psychological services, the Living Room (a peer led support and guidance service), with a coffee shop and free reserved GP parking close by.



at 162 Cambridge St West Leederville (directly opposite SJOG Subiaco).
2 large fully fitted consults rooms (including sink and treatment bed) available and seperate treatment room available.
Each consult room $250 per half day session (includes use of waiting room and kitchen area). Reception/Admin support available for an additional fee.
For further information regarding availability or to arrange inspection please contact: reception@oswa.com.au/ (08) 9332 0066
The ECU Health Service assists students, staff and the university community with their health care needs. The primary function of the service is to provide our students with accessible and affordable health care for the duration of their studies.
Students are charged the rebate fee or bulk billed, and staff and other patients are charged private commercial rates.
Applications are now open from candidates who have either Permanent Residency or Australian citizenship, unrestricted Medical Board of Australia registration and no Provider Number restrictions.
Please contact Laura Harnett – Practice Manager on telephone 0479 188 513 / 08 6304 5618 or email practicemanager@ecu.edu.au.




Fully fitted including sink
Includes use of waiting area, staffroom/kitchen
$250 per half day session
Reception/patient check-in support available for additional fee.
For further information or to