In the eight years from 2016, the number of people giving birth at home rose a staggering 435%. It’s another clear indication of a changing narrative in maternity care and the need to cater for all parents.
YOU ASKED, WE DELIVERED: WE ARE NOW CPD VERIFIED


Complete the self-reflection and claim your CPD time, please scan here
A lot can change in a year. It’s something I thought about a lot in sitting down to pen this editorial after being at the helm of Medical Forum since January.
This time last year we ran a feature on WA’s slow progress to update its assisted reproductive and surrogacy laws. It explored the pressing need for reform, and we concluded the state government would need to gain traction on this issue in 2025.
It did gain traction and the Assisted Reproductive Technology and Surrogacy Bill 2025 is currently going through Parliament.
As WA plays catch up on surrogacy laws it has long lagged behind other states on, the way people want to give birth has also shifted.
In this edition we look at the rise in popularity of home births and how to best support parents who want to give birth at home.
In the eight years from 2016, the number of people giving birth at home rose a staggering 435%. It’s another clear indication of a changing narrative in maternity care and the need to cater for all parents.
The state is also facing a maternity system under strain, with several private maternity closures or cutbacks over the last couple of years.
Which brings me to the main theme of 2025 – more investment in the sector is needed.
Investing in maternity services across the board would help ensure the best possible experience for parents both in hospital and at home. The same is of course true of other parts of the health system.
Let’s see what 2026 has to offer, but I’m sure the need for investment will be coming up again.
From all of us here at Medical Forum we wish you a very relaxing holiday season and Happy New Year. We look forward to bringing you more content and new opportunities in 2026.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




The more things change, the more they stay the same
58 Surfing the wave of good mental health
From scrubs to squats
History and innovation at Sandalford Wines – Dr Craig Drummond MW
Our round of competitions this month includes movies tickets, a book giveaway and more wine. We have two copies of The 1% Good Club to give away to lucky readers.
We also have five double passes to see French comedy film My Brother’s Band in cinemas on Boxing Day.
Or we have 12 double passes to see The Choral in cinemas from January 1 and 12 double passes to see Anaconda, in cinemas Boxing Day.
And we’ve got another round of WA wine for one lucky reader, this month from Sandalford Wines in the Swan Valley. Read our Master of Wine’s review on page 63.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director
Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Advertising Account Manager
Rita Murphy 08 9203 5222 rita@mforum.com.au
Clinical Services Directory
Rita Murphy 08 9203 5222 rita@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au


















Up until recently Dr Paul Stobie’s bike was only ever dusted off for a ride about once a year, but that all changed when a group of friends convinced him to cycle 700kms in less than five days.
The Perth cardiologist is taking part in the 2026 Hawaiian Ride for Youth. The event sees teams of cyclists ride from Albany to Perth to raise funds for Youth Focus, which provides free mental health services to young people in WA.
Heading into its 24th year, the event has raised more than $34million and this year organisers are aiming to add another $2million to that total.
Dr Stobie is hoping his background in endurance running will help him complete the four-and-a-half days of cycling. His bike is now being taken out three times a week for training.
“Crawling out of bed at a quarter past four has been a new experience, but it’s actually been very rewarding so far,” he told Medical Forum
“Work can get so busy, sometimes you become so busy that your own requirements are put to the side a lot. But this forces you to do the exercise that we keep on reminding people they should be doing.
“Part of it was to get literally back on the bike, get back to regular exercise and then also to participate in an event that has such a great cause.”
Corporate sponsors cover the costs of supporting teams to participate in the Ride for Youth and Dr Stobie is part of the Hawaiian team, captained by John Slade, property asset and infrastructure consultant at Youth Focus.
Notifications to Australia’s health practitioner regulatory body have surged by 19% in the last year.
Ahpra’s annual report for 2024/25 revealed the regulator received 13,327 more notifications – 19% higher – than the previous year.
A total of 22,658 notifications about 16,209 practitioners were received.
Of these notifications, 12,744 (56%) were medical practitioners – a significant rise from the 11,000 recorded last financial year.
Of those medical practitioners, some 1,082 were from WA.
Overall, the number of notifications received about WA practitioners across all fields increased from 1,717 in 2023/24 to 1,887 in 2024/25. While notifications were up

Youth Focus chief executive Derry Simpson said riders sharing their stories and experiences was a powerful way to show young people that they are not alone.
“The need for mental health support in Western Australia has never been greater, especially in regional and remote areas,” she said.
The 2026 Ride for Youth will take place from March 24-28.
Travelling over four-and-a-half days, riders are separated into three different pelotons, and visit 18 towns across three different routes; Coastal, Inland and Wheatbelt. Throughout the ride, participants stop to visit and speak with high school students about mental health.
Dr Stobie has raised more than $50,000 so far but is hoping to raise more. You can donate at: rideforyouth.com.au/2026/riders/paul-stobie
nationally, not all were completed. The regulator closed 12,086 notifications in 2024/25, 8.3% more than the previous year and higher than any previous year, the report stated.
However, it was still struggling to keep pace with the number of notifications. As at June 30 there were 5,627 open notifications –some 26% more than the previous year.
The most frequent reasons for a complaint being lodged against a medical practitioner remained issues related to clinical care and communication.
The annual report also showed the medical practitioner workforce not only grew but adopted significant regulatory reforms and addressed emerging clinical and ethical challenges.
There were a total of 148,185 registered medical practitioners in Australia in 2024/25, up 3.9% from the previous year. Of those, 15,810 were registered in WA.
Medical practitioners made up 15.4% of all registered health practitioners for this period, of which there were nearly one million.
Ahpra chief executive Justin Untersteiner said while reaching nearly one million practitioners was a significant milestone, the regulator acknowledged that “growth isn’t just about numbers”. “We’re working hard to make registration easier while keeping safety front and centre,” he said.
A number of Western Australian GPs were recognised for their outstanding contributions to their communities at the RACGP’s annual conference last month.
Among the GPs, GP supervisors, GP registrars and practices celebrated at the event was Adjunct Associate Professor Frank Jones who was awarded the most prestigious honour the RACGP affords, the Rose Hunt award.
RACGP President Dr Michael Wright said Prof Jones had made “immense contributions to general practice” over his nearly 45-year career.
Originally from Wales in the United Kingdom, Professor Jones moved to Australia in 1981 and became a College member in 1985.
Prof Jones has worked with the Royal Flying Doctor Service, as a procedural GP obstetrician, and spent the past 40 years working at Murray Medical Centre in Mandurah.
Within the RACGP, he has been an active member of several boards and committees and has been a stalwart of the RACGP WA Council since 2004.
Prof Jones has held the positions of WA Faculty Deputy Chair, Chair and Provost, served as an RACGP Board member from 2010-2016 in his capacity as WA Chair, before moving to the role of Vice President and eventually becoming President in 2014.
A dedicated examiner, supervisor and senior clinical lecturer at the UWA Medical School, he has made substantial contributions to education and training of medical students, registrars and peers over a long and dedicated career.
Other West Australians recognised at the awards were Dr Rajeshwary ‘Raji’ Krishnan who was named General Practitioner of the Year and Dr Joanne Wong who was awarded the Prof Charlotte Hespe research award.


Medical student Keisha Calyun took out the Rising Strong Medical Student Award.
It’s been a big year for Dr Raji Krishnan, who also won the AMA’s
President’s award at the AMA25 conference.
RACGP vice president and WA chair Dr Ramya Raman said: “Dr Krishnan is a true generalist, providing comprehensive primary health care and an unwavering service to Australia’s vulnerable communities and First Nations Peoples.”
In her nomination, Dr Krishnan was described as selfless in the service and care she provides in palliative care and through Street Doctor, a mobile clinic for culturally and linguistically diverse patients.
Her contribution to research on rheumatic heart disease and hepatitis B and C was also recognised.

Infectious syphilis cases are increasing across the country and Australia’s Chief Medical Officer recently declared syphilis to be a communicable disease incident of national significance.
Infectious syphilis case numbers in Western Australia have surged by almost 300% over the past 10 years, from 162 in 2015 to 606 in 2024. All of WA is now a declared outbreak area.
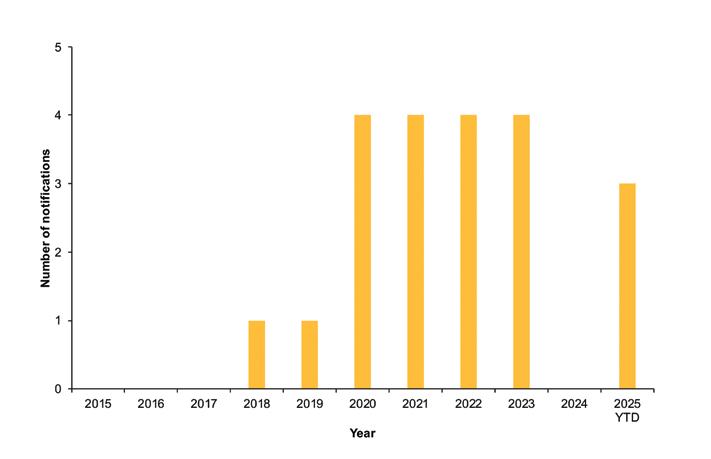
Sadly, this is also reflected in increasing cases of congenital syphilis – a preventable cause of stillbirth and neonatal and lifelong complications (see Figure 1).
Of concern, there have been three cases of congenital syphilis notified in Western Australia so far this year, which reflects ongoing high levels of infectious syphilis in the community.
Syphilis can present in many ways and often has no or minimal symptoms. Recent syphilis cases in Western Australia have been identified by a wide range of specialists, including GPs, dermatologists, dentists, ophthalmologists, rheumatologists,
emergency physicians and obstetricians – it is the great masquerader.
Given the rise in cases across all population groups, if we are not testing for syphilis, then cases will be missed. Most people with syphilis do not know they are at risk, and most will not have symptoms.
Early identification of syphilis in pregnancy enables treatment that can positively change the life course of both the pregnant mother and baby. Treatment in pregnancy is safe and effective.
Western Australian and national pregnancy care guidelines recommend that everyone has routine syphilis testing at three key points during every pregnancy:
1. At diagnosis of pregnancy
2. At 24 weeks – time of routine 2428-week blood tests
3. At 36 weeks – time of routine 36week blood tests.
Additional testing in pregnancy is
also recommended:
• Routinely at time of any premature birth
• Opportunistically, when an STI or risk for an STI is identified
• Whenever a patient requests testing
• Opportunistically, when routine antenatal care schedule is disrupted, consider socioeconomic issues and social risk factors such as housing, substance use and mental health issues that affect access to care.
Implement the five Ts to tackle syphilis in your daily practice:
1. Talk about syphilis with your patients
2. Think of syphilis when considering diagnosis
3. Test for syphilis – PCR swab of mucosal lesions and serology
4. Treat syphilis promptly
5. Trace contacts with support from local public health unit.
Consider practice audit and quality improvement activities.



Audit:
• Is syphilis serology included in antenatal blood request forms at the first visit, 28 and 36 weeks? If not, consider programming them into your practice software
• Is syphilis serology included in routine STI test requests? Think STI = think syphilis
• Is syphilis PCR requested when investigating mucosal ulcers/ lesions
• Is a pregnancy considered whenever a female of reproductive age undergoes syphilis testing, and if infectious syphilis is diagnosed, is pregnancy status determined within one working day in accordance with the national guideline for public health management of syphilis?
Consider doing a practice education session on syphilis with your colleagues.
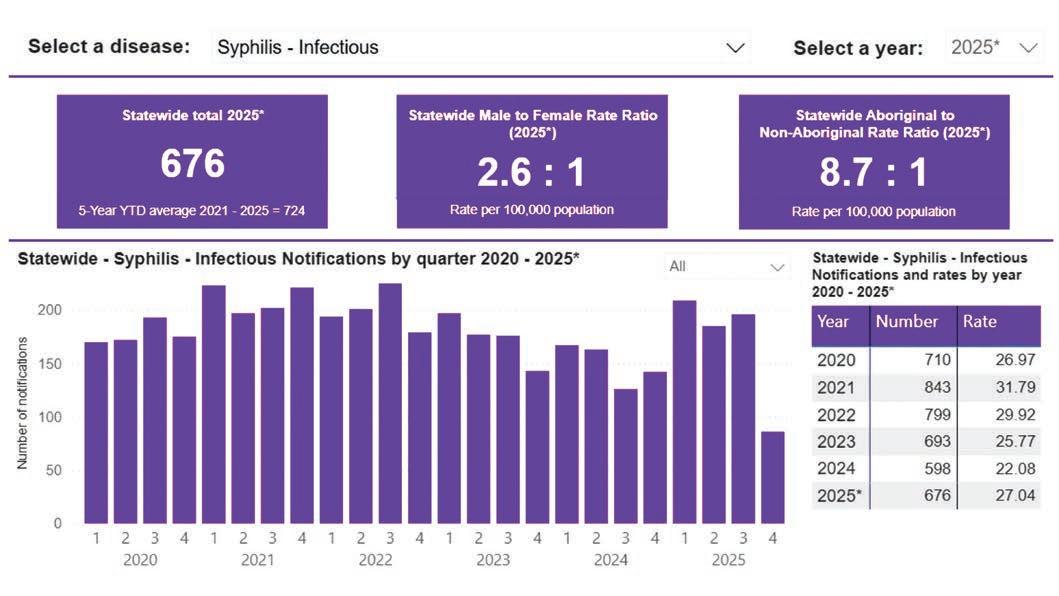
The WA Notifiable Infectious disease dashboard contains realtime information about syphilis notifications broken down by sex, age-group, region and Aboriginal status, and is a great resource to help
discussions with patients & colleagues about syphilis (see Figure 2).
Display posters and patient education materials in your waiting room – you can find out how to order resources from the ‘ordering resources’ page on the WA STI and BBV guidelines page. Together, we can all make a difference with small changes that will help prevent congenital syphilis and stop the spread of syphilis in WA. Think of syphilis and make a difference today.
Figure 2: WA notifiable infectious disease dashboard
Available at www.health.wa.gov.au/Articles/N_R/Notifiable-infectious-disease-dashboard
Figure 1: Number of congenital syphilis notifications in WA, 2015 to 2025 YTD
Want to learn more?
Visit: www.health.wa.gov.au/WA-STIand-BBV-guidelines/Infections/Syphilis www.health.wa.gov.au/Articles/U_Z/ WA-Syphilis-outbreak-response www.ashm.org.au/education/syphilisoutbreak-training-website www.health.wa.gov.au/Articles/N_R/ Notifiable-infectious-diseasedashboard
Email: shbbvp@health.wa.gov.au
The WA State Government is set to purchase St John of God Mt Lawley Hospital in an effort to add new beds to the public hospital system and relieve some of the pressure the system has been facing.
To fund the purchase the government has scrapped the $1.6 billion Perth Convention and Exhibition Centre redevelopment to create a $1.5 billion Building Hospitals Fund.
Negotiations around the sale of the 197-bed facility are understood to be in the advanced stages. It will add up to 100 beds to the public system, with a portion of the beds at the hospital already contracted to WA Health.
It will also provide eight additional operating theatres to the public system.
The move follows increasing pressure on the public health system this year, which has seen record rates of ambulance ramping due to a lack of available beds, and the postponement of elective surgeries at some hospitals.

It is not known how much the government plans to spend on the purchase of the hospital. The Building Hospitals Fund is comprised of $500 million announced in September and an additional injection of $1 billion announced on November 6.
Health Infrastructure Minister John Carey said: “Bringing St John of God Mt Lawley Hospital into public hands will add new beds to the public system quicker than we can build them.

“Rescoped projects at both hospitals will deliver new facilities that will serve the public health system for decades to come, while limiting disruption during construction.”
AMA (WA) President Dr Kyle Hoath welcomed the announcement: “It has been a long and difficult winter, and we’ve been saying we can’t have another winter like this.
“We’re talking about significantly reducing waiting times for people to get in the front door of our health system which is bursting at the seams. It will be an immediate benefit; people will notice that the waiting period will be improved.”
The private hospital is expected to begin operating as a public hospital in 2026.
St John of God Health Care Group chief executive Bryan Pyne said staff would be supported through the process.
“We’ve seen a reduction in demand for private hospital services in the Mt Lawley area, which is already well served by St John of God Health Care and other private hospitals, while at the same time there is growing demand for private care at our Subiaco, Murdoch and Midland hospitals,” he said.
“A significant number of caregivers will be provided the opportunity to take up positions at the new Midland Private Hospital once it opens in 2026.”

The federal government’s ban on social media for under 16s is set to come into play this month in the hope it will improve the wellbeing of young Australians.
There are concerns that restricting access to social media platforms may also pose mental health risks for certain groups of young people, including those who are LGBTIQA+ and neurodivergent.
Under the newly created social media minimum age laws effective as of December 10, some platforms must take “reasonable steps” to prevent those under 16 years of age from holding accounts.
The 10 platforms that will be subject to the new laws are Facebook, Instagram, Snapchat, TikTok, YouTube, X, Threads, Reddit, Twitch and Kick. They could be subject to fines of up to $49.5 million if they do not adhere.
Minister for Communications Anika Wells said the measures would give kids a reprieve from the “persuasive and pervasive pull” of social media.
But Children and Young People with Disability Australia (CYDA) and WAAC, an organisation that provides sexual health and support services in WA, have concerns about the impact that reduced access to online platforms may have.
CYDA chief executive Skye Kakoschke-Moore said: “Social media offers young people with disability one of few accessible ways to bond with peers, express their identities, participate in advocacy,
By Aleisha Orr
and access important information and news.”
A report by the e-Safety Commissioner found that 70% of young people with disability said it was easier to be themselves online compared to 59% of their nondisabled peers, and one in four uses it weekly to make friends.
“Restricting access for under-16s carries real mental health risks, worsening social isolation by barring them from the platforms they use for connection, community participation, and self-expression,” Ms Kakoschke-Moore said.
“Age-assurance technologies, including ID checks or AI-based facial recognition, can discriminate against people with disability if they are not thoughtfully and deliberately designed and tested to be inclusive.
“We’re concerned that young people over 16 with physical, cognitive, or sensory disability could be incorrectly flagged and prevented from accessing social media.”
Chief executive officer at WAAC Dr Daniel Vujcich also holds concerns about the ban. While the intent was to provide protection from the harms of online spaces, it would result in it being harder to reach young LGBTQIA+ people who need support.
He said WAAC relied heavily on these platforms to communicate their work and services to young people.
“Social media has been shown to play a key role in identity development, peer connection, and mental health for LGBTIQA+ young people,” he said.
“For those in regional areas, or in homes or schools where they cannot be open, online spaces are often the only place they can find others who understand them.
“Of course, online environments are not always kind, homophobia and transphobia happen there. But this ban does not address the source of the harm.
“We still see public figures using LGBTIQA+ young people as targets in culture wars. That climate makes it even more important that young people can find affirming support when they need it.”
He said now the organisation faced the task of finding new ways to reach young people who were already isolated.
For a GPs perspective on the social media bad, read our guest column by Dr Andrew Leech on page 32

Australia has achieved remarkable progress in HIV prevention and management through effective antiretroviral treatments, the introduction of pre-exposure prophylaxis (PrEP), and robust community-led initiatives.
In 2018, the Australian Government declared that “we are now living in an era where HIV is no longer a death
sentence, and we can dare to hope for its elimination”.
These advances have been reflected across the country, including in Western Australia, where overall HIV notifications have significantly declined.
However, as total case numbers have decreased, late- and advancedstage HIV diagnoses have remained
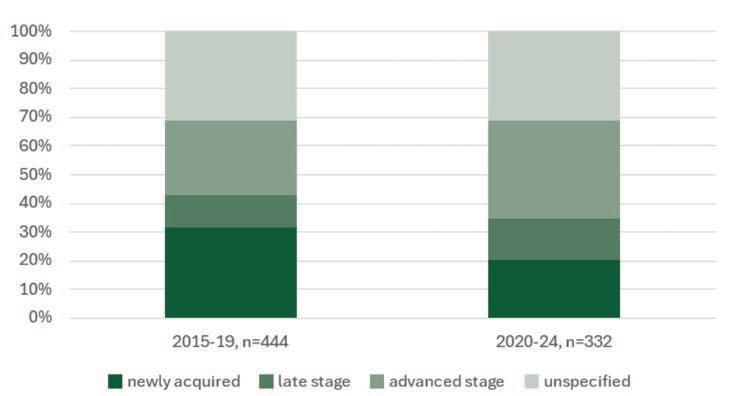
relatively stable, meaning they now represent a larger proportion of new diagnoses (see Figure 1).
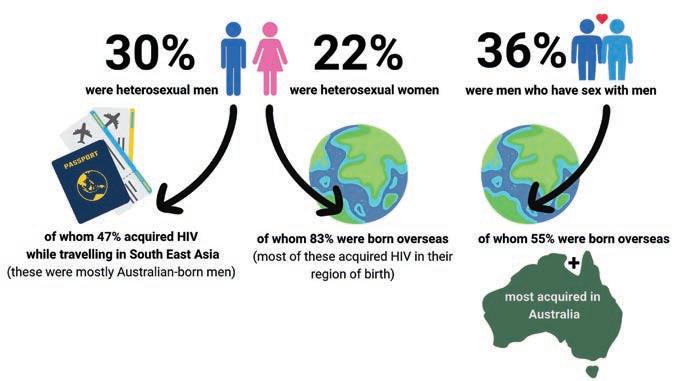
This emerging pattern is particularly notable among people who identify as heterosexual and acquired their infection overseas, highlighting the next key challenge in HIV elimination efforts (see Figure 2).
People who are diagnosed late with HIV are at risk of worse morbidity and mortality outcomes, including:
• AIDS-related illnesses
• Higher risk of death soon after diagnosis
• High rates of hospitalisation
• Sub-optimal antiretroviral therapy outcomes
Of the West Australians diagnosed with late- or advanced-stage HIV during the 2015-2019 period, five subsequently died of AIDS-related illnesses.
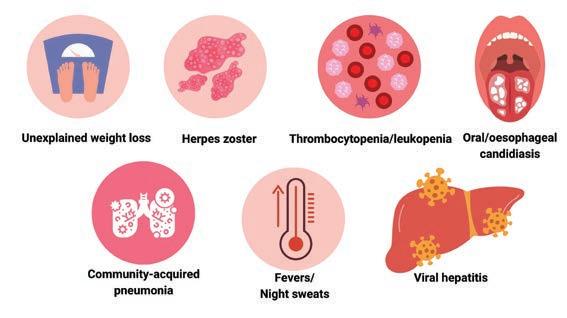
A retrospective cohort study of 80 patients with late-stage presentation of HIV in a Melbourne healthcare network found that 55% had at least one HIV indicator condition (see Figure 3) which ought to have triggered HIV testing. Of these, almost half were diagnosed with the


indicator condition at least one year prior to HIV diagnosis.
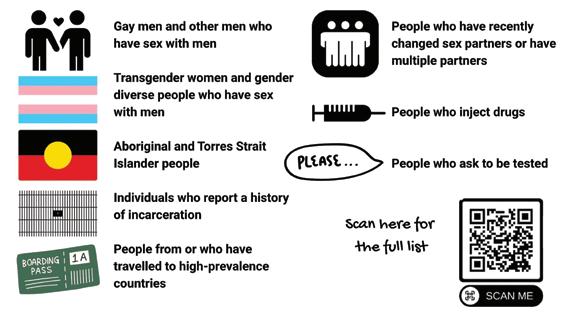
Reduce the number and proportion of people diagnosed with late- or advanced HIV by offering HIV testing more often and to more people, especially those with behavioural, epidemiological, and clinical characteristics specified in the HIV National Testing Policy (see Figure 4).
Consider using these questions to offer opportunistic STI and HIV testing:
“We are offering sexually transmissible infection testing to all sexually active people under 40. Would you like to have a test now or find out more about STIs, including HIV?”
“Since you are here today for/ to discuss contraception/cervical screening, could we also talk about some other aspects of sexual health, such as an STI check-up?”
“As you mentioned that you have a new partner/have recently returned from an overseas trip/have recently come out from prison, would you like to have a STI and HIV check-up now?”
Both daily and on-demand HIV PrEP are highly effective HIV prevention strategies for men who have sex with men (MSM), heterosexual men and women, transgender people, and people who inject drugs who are atrisk of HIV acquisition.
GPs and authorised nurse practitioners can prescribe PrEP which is PBS-funded.

Condoms are safe, cheap and effective at preventing HIV transmission. Encourage people going overseas to pack condoms and water-based lubricant.
While Australia's HIV prevention successes are undeniable, the persistence of late-stage diagnoses represents a critical gap that demands immediate clinical attention.
The tragic reality that five West Australians died of AIDS-related illnesses between 2015-2019 after late diagnosis, combined with evidence that over half of patients with latestage HIV had previous healthcare encounters where indicator conditions should have prompted testing, underscores both the human cost and preventable nature of these missed opportunities.
With HIV now a highly manageable chronic condition when diagnosed early, clinicians hold the key to eliminating late-stage diagnoses by normalising HIV-testing conversations, maintaining high clinical suspicion for HIV-indicator conditions and promoting condom use and HIV PrEP.
Want to learn more?
Visit: www1.racgp.org.au/newsgp/ clinical/no-longer-a-death-sentenceaustralia-making-progre
www.nejm.org/doi/10.1056/ NEJMoa1506816
https://academic.oup.com/qjmed/ article/112/1/17/5116105
Email: shbbvp@health.wa.gov.au
An increase in demand for home births in Western Australia means parents need to register their interest early in their pregnancy to be able to do so under the public system.

By Aleisha Orr
So, what is driving the interest in home birthing and what needs to be considered when it comes to planning for a home birth? Medical Forum spoke to two WA obstetricians and a midwife who has delivered thousands of babies to gain insight into the increasingly popular birthing option.
Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) WA councillor Dr Anna Clare described WA’s Community Midwifery Program (CMP) – the program people must register with to birth at home – as “quite oversubscribed”.
“People can self-refer or be referred by their GP, but you need to get in really early because it does book out with the capacity of the midwives,” she said.
While the percentage of home births in WA may make up less than 2% of all births in the state, the percentage of women having home births has more than tripled in less than a decade.

Just 89 women had a home birth in WA in 2016, according to Australian Institute of Health and Welfare data, however that number rose to 477 in 2024 – a 435% increase in eight years.
Just 89 women had a home birth in WA in 2016, according to Australian Institute of Health and Welfare data, however that number rose to 477 in 2024 – a 435% increase in eight years.
Dr Clare is also the head of obstetrics at King Edward Memorial Hospital and part of her work includes the antenatal clinic where she sees women who are part of the public home birth program.
She said there was a move towards home birth during the pandemic due to the restrictions in hospitals during that time, including limitations on visitors.
Dr Clare said women who had previously birthed a child in a hospital were among those looking for an alternative.
“For women who have experienced things not going as well as they had hoped, or were traumatised by a previous birth in hospital, sometimes home birth helps them feel more in control and they often prefer the continuity of care model you get with a home birth,” she said.
Under the CMP, which supports a limited number of women in WA each year to give birth in their home, parents are supported by the same midwife, or a familiar team of midwives, throughout their pregnancy and during their birth. This is not the case for the majority of people giving birth as public patients in WA.
Dr Lesley Kuliukas , a former vice chair of the WA executive committee for the College of Midwives, a practising midwife for 42 years, said midwife-led continuity of care often gave women a sense of safety and security that helped them through the birthing experience.
people around, where there aren't loud noises and clangs and clashes, strange people coming in and out and things feel good, our bodies will labour really efficiently.”
However, given home birth programs like WA’s only allow select women to birth at home, comparing outcomes between births that take place in familiar settings and those that take place in hospitals is not realistic.
“It's not a fair comparison, likefor-like, because women having their babies at home generally, everything's straightforward for them,” Dr Kuliukas said.
The 2023 RANZCOG guidelines on homebirths noted women with low-risk pregnancies who had homebirths were more likely to have an unassisted vaginal birth, with reduced likelihood of severe perineal trauma, caesarean section birth or instrumental birth and that there was little or no difference in stillbirth for planned home birth or hospital birth.
While Dr Clare was uncertain as to what proportion of pregnant women would be deemed eligible for a home birth in WA, she said the proportion of women meeting the criteria to be eligible was likely reducing.
“It’s probably getting a bit lower because of women delaying pregnancies – many are older and being older in itself is a bit of a risk, but also you are more likely to have picked up another medical problem as you get older,” she said.

“As a country we are also getting a bit more overweight, so that is also a risk factor for complications in pregnancy, and it also increases the risk of diabetes and high blood pressure in pregnancy.
“There are quite clear guidelines to rule people in and rule people out and when you start pushing those guidelines you are more likely to have bad outcomes.”
Among the recommendations within the RANZCOG clinical guidance is that publicly funded home birth programs include protocols that cover not only eligibility criteria but also referral processes and planning for transfer/escalation of care.
Dr Clare said about one third of first-time mothers who choose to homebirth will end up having to be transferred to a hospital.
“For women who are low risk, who are fit and well it's a very safe option.
“If it’s your first baby, then there is a risk of having to transfer in the labour and that’s maybe 30%.
“It’s not usually as an emergency, it tends to be they are requesting an epidural as its more intense, or because there has been slow progress in labour and maybe that’s an indication for another assessment or interventions you can only do in hospital.”
Dr Clare stressed it was important to differentiate between homebirths and freebirths. Freebirth is birthing at home without a medically qualified person available, such as a midwife or obstetrician.
Dr Clare said sometimes a doula was present, but while a doula is able to provide social support, they were not a medically qualified person.
“There has been a lot of media coverage recently about bad outcomes with freebirth,” she said.
“If you think of an animal going into labour, it finds itself a warm, dark, secure, familiar place, and labours very efficiently. If that labour is stopped in any way by a predator or a loud noise, physiologically the labour stops, and it doesn't restart until they find themselves in that secure place,” she said.
“We're animals too, so the same is true for us. If we're able to be somewhere where there are familiar
“Overall women are becoming a bit more complex in their pregnancy journey.”
She said one of her concerns about women considering a home birth is that they take the data and evidence for low risk women and then apply it to themselves.
“Although it is safe for a lot of women, that doesn’t mean it is safe for everyone.”
“There is a huge difference between a planned home birth with a suitably selected group of women who are experienced and who have pathways into the hospital if it is needed, and then women who are birthing at home without clinical attendance.”
In the wake of several recent deaths linked to freebirth, RANZCOG and the Australian College of Midwives have called on Commonwealth, state and territory governments
Dr Jaimini Raniga GP, Integrative Medicine

Trying to decide on an indemnity insurance provider? Here’s some of the reasons our 55,000 members choose to make it MIPS:
• Comprehensive indemnity insurance cover of up to $20 million
• 24/7 access to support and advice
• Accredited risk management and education resources including webinars, available on-demand Visit www.mips.com.au for a quote today. T&Cs apply.
continued from Page 13
to enact legislation restricting the practise.
Dr Clare said there was not a lot of data around freebirth but based on case reports there is an increased risk associated with it.
She said freebirth was being encouraged on social media platforms by people sharing idealised versions of natural birth.
“There are a lot of people on social media who have an agenda around that and are not open and honest about the risks associated with it, so I think women are not really as informed about the risks.”
Dr Clare said it was important for GPs to encourage pregnant patients to engage with care.
National Association of Specialist Obstetricians and Gynaecologists WA representative Dr Hannah Sylvester said while social media influencers may talk about how women have historically birthed in their homes without the need for hospitals, there were some harsh realities about the risks of childbirth in the past.
“If you want to go back to how we birthed centuries ago then you have to accept that our perinatal morbidity and mortality rates are going to increase back to that level. That’s not really acceptable, and it's not acceptable for a baby to be avoidably damaged in childbirth,” she told Medical Forum
“Up until about 100 years ago you had about a one in six chance of dying in childbirth. The interventions that have reduced the maternal and neonatal morbidity and mortality are analgesia, assisted vaginal delivery – forceps and vacuum – caesarean section, antibiotics, and medical and surgical intervention for obstetric haemorrhage.
“In the same way that the homebirth doula movement is picking up with people saying ‘I don’t want that in-hospital vaginal birth that I had last time’, I’m also seeing people who say ‘I don’t want that in-hospital vaginal birth that I had last time - I would like an

elective caesarean with a private obstetrician’.
“Or they would at least like continuity of care, or doctor-led care.”
She believes rather than there being a need for more alternative birth options, it points to wider problems in the maternity system that need addressing.
“What we're doing is saying some people can have a homebirth and some people need midwifery continuity of care. You just need to provide an adequately funded and staffed service to a capacity that can cope with the women that we have,” Dr Sylvester said.
We know the number of births in WA is rising, we know that the public sector is over capacity and private maternity units are closing, so there is no way that the service can be as good as we want it to be working to those numbers.
“Rather than try to find an alternative, just invest in the system that we have and make medicalised in-hospital birth, whether that’s vaginal or caesarean, an appropriate service so that women want to do that.”
While Australia’s public home birth programs may provide many positive experiences and outcomes
for the women who are lucky enough to be low risk, Dr Sylvester said such programs only took funds from the general maternity system.
“They are taking all of this public funding and you are channelling it into a tiny percentage of well women and putting in stop gaps to filter out the few that are slightly high risk.
“You are taking all the public funds away from the sickest people, the people who don’t have the luxury of having a low risk birth and taking it away from the basic standard of care for the majority of women, which at the moment is not being provided to the capacity we need.”
The WA Department of Health did not respond to questions about the cost of its homebirth program supported by the CMP, or about numbers of homebirths in the state.
It also did not provide comment on what efforts were going into improving the experience of women giving birth in WA hospitals under the public system.
By Ara Jansen

One woman having a baby doesn’t just change her family, it can affect a whole community. Likewise, a woman not being able to have a child can have a negative outward effect too.
Gynaecologist, reproductive endocrinologist and fertility specialist Dr Sebastian Leathersich believes having a child – or being unable to – creates a much wider ripple effect than we often consider, extending beyond the immediate family.
This interest in public health is part of the reason Sebastian has worked hard to balance both clinical and research work in his field. He’s passionate about both and can’t see a world where he ever gives one up for the other.
“Fortunately, in my work I'm able to spend time on both clinical practice and research,” Sebastian says. “For me they go hand in hand, especially since advances can move really fast sometimes. My driver is curiosity mixed with academic interest. In the field of reproductive medicine there is so much scope for research, as well as for collegiate and collaborative work.”
“It’s such a young field – it’s 47 years since the first IVF procedure. It took over 300 egg collections to get that baby. The rate of change is phenomenal. It’s an academically exciting field to be in and there’s such a drive to improve. There is so much we still have to learn, but with each new discovery we can improve outcomes for patients.”
“To help or have some influence over a woman being able to conceive and deliver safely, it’s an area where research and innovation can make a huge difference. That not only changes the life of a woman and her family, but of her community too.
“People are waiting longer to have babies while families and parents look different. That creates so many different combinations of how fertility works and the identity of a family. It’s socially and ethically complex, even without reproductive difficulties.
“The path to a successful pregnancy can be long and challenging for some people, and any improvements we can make to clinical outcomes and the patient experience can have a big impact.”
Unsure of what he wanted to do after graduating high school in Perth, Sebastian moved to Germany as an exchange student and began work experience at an architecture firm. He did plenty of travelling and as chance would have it, met a lot of people who were in medical school. It was his first exposure and those people he met were loving it.
Enthused by what they shared, Sebastian returned to Perth and started a medical degree at UWA. He knew he was in the right place when he started enjoying the preclinical science and all the learning.
Wanting to go travelling again, Sebastian took a year off to do a Bachelor of Medical Science in Montreal where he earned first class honours at McGill University Health Centre. He then returned to Perth to complete the final two clinical years of his medical training. First class honours from UWA followed.
During that time he also completed a maternal and perinatal health internship with the World Health Organisation in Geneva. He later earnt dual master’s degrees in public health and health management.
Sebastian then competed specialist training in obstetrics and gynaecology at King Edward Memorial Hospital, where he received the highest fellowship exam score in Australia and New Zealand.
He’s also received numerous awards including: the Camille Michener Award for Registrar of the Year, the David Liu and Tony McCartney Prizes for Research, Best Early Career Researcher and Mentor of the Year. He’s also earnt the Certification in Reproductive Endocrinology and Infertility (CREI) subspecialist qualification, the

highest level of fertility training in Australia, held by only two other practising specialists in WA.
Returning from Spain earlier this year, Sebastian has completed an advanced clinical fellowship at the Dexeus Fertility Institute in Barcelona. From Perth he’s finishing his PhD at the University of Barcelona on the management of diminished ovarian reserve, supported by the Jean Murray Jones Scholarship.
The 35-year-old was recently appointed Medical Director at Concept Fertility & Day Hospital. He is also a director of Menopause Alliance Australia, a member of the WA Reproductive Technology Council, representative for the Doctors’ Health Advisory Service of WA and an associate editor of The Australian and New Zealand Journal of Obstetrics and Gynaecology
“From a clinical perspective I was particularly interested in obstetrics because it was about building relationships and helping people feel safe and supported,” he says. “Working with a multidisciplinary team was also a powerful motivator for me.
“Fertility is also one of the medical areas where people are not necessarily coming to you with a specific disease. They are often generally healthy but might need assistance achieving a pregnancy, and when that’s successful it’s something incredibly positive and life changing. I feel very privileged to be able to help people navigate that journey.
“That relationship building is also important and it’s rewarding being able to build those relationships, over an extended period of time – sometimes over several pregnancies.”
The road can be long. As Sebastian points out, someone can start seeing him this month and it might be a year or more until a birth happens.
“When you do that ultrasound and you see the heartbeat with the parents for the first time it’s incredible to share that together. Then when they bring the baby back to meet you or send a card with a photo and you see how this family has grown, and having

Recognise early signs of valvular disease and heart failure, interpret ECG and rhythm changes relevant to atrial fibrillation, determine when to order and how to interpret echocardiography reports, apply cardiometabolic risk management strategies and navigate collaborative care pathways.
Speakers:
Professor Rukshen Weerasooriya, Dr Gerald Yong, Dr Sekaran Gana, Dr Thato Mabote, Dr Yuli Ten, Mr Eric Karim Slimani, Mr Pragnesh Joshi, Dr Keng (Siang) Ung, Dr Philip Currie, A/Prof Kushwin Rajamani, Dr Pasko Dedic - Cardiology.
Date: February 7, 8:00am Where: UWA Uniclub Ballroom, Hackett Drive, Crawley RSVP: February 6
Women’s health GP education with a difference. A focus on common conditions that present differently in women and gender-specific management options. Learn more about peripheral vascular disease, complex conditions of menopause, rare women’s cancers and pain presentations.
Speakers:
Dr Robert Tewksbury, Dr Wasing Taggu, Dr Rajiv Menon, Dr Mike Kamara, Dr Navin David Palayoor.
Date: February 21, 8.30am
Where: Grand Ballroom, Rendezvous Scarborough Hotel, Scarborough
RSVP: February 13
will be introducing live GP Masterclasses in 2026

Delivering RACGP accredited education by your local WA specialists – have your say on the topics and speakers you’d most like to see on the program.
Scan the QR code to help design your perfect masterclass

continued from Page 17
been able to help them, it’s truly incredible.”
Fertility and reproduction remain challenging – both for parents and doctors. Sadly, not everyone will get the outcome they want. It’s part of the double-edged sword of being able to help a lot of people, though not all of them.
“Sometimes, we also have to give bad news and be with our patients in those moments to help them through it. We have to ensure that all of our patients feel supported, regardless of the outcome. Every time a patient gets a negative result it’s difficult. You feel it every time. The day you stop feeling it, is the day you should stop practising.
“I think it’s important to remember that no one wants to have to ask for help conceiving. It’s a difficult journey, particularly for people who go down the path of IVF, and can be emotionally, mentally, physically and financially challenging. As a clinician, it’s important not to become desensitised to that. While we may see this every day, for our patients it is often unfamiliar and uncharted territory.
“We have to be focussed on clinical outcomes but we also have to meet people where they are and be there for them. That’s why building relationships is so important.

Sebastian spent 18 months working and studying in Barcelona and returned to Perth a couple of months ago. His adventure was preceded by four weeks of intense language study. His research was done in English, but his clinical work and meetings were mostly in Catalan or Spanish, and he enjoyed the challenge of learning a new language and working in a multinational team.
Now Sebastian splits his time between Concept and Perth Children’s Hospital. Next year he will start working at King Edward too. He tries to split his time between clinical and research work but says he doesn’t always achieve that.
“I enjoy working across both private and public health systems, where I get to work with different teams, in

different models of care, and with different health focuses, from IVF to early menopause to the Gender Diversity Service at PCH.
“Working with a group like Menopause Alliance Australia gives me an opportunity to contribute to greater workplace acceptance and understanding of menopause, creating safer and more supportive workplaces through education and advocacy. Being part of groups like this, I believe we can make a difference.”
Sebastian is also passionate about providing care to individuals and couples in the LGBTQIA+ community. Especially in light of this year’s landmark legislative reforms with the Assisted Reproductive Technology and Surrogacy Bill 2025 which will expand access to fertility treatment, enhance donor-conceived rights and have more inclusive surrogacy laws. This includes making surrogacy more accessible to a wider range of people, including same-sex male couples and transgender individuals.
Sebastian enjoys his work but he’s also conscious of working too much and has to be strict with himself to have downtime. Strict enough to train to do the Rotto Swim solo
a few years ago and a Busselton Ironman. He’s making another trip to Busselton this month and will be signing up for the full Ironman again next year. He would love to compete at Kona – the world stage of ironman competitions in Hawaii. If he’s not cycling, running or swimming, Sebastian likes to travel as much as possible. He also takes every opportunity to go diving, whether it’s Exmouth or the Galapagos.
In his quieter moments and as a nod to his mental health, he makes pottery, plays the violin and enjoys the beach. They help ground him. He’s a member of a 24-hour pottery club which allows him to throw a piece whenever he feels like it. He loves the arts, especially the opera and the symphony, and loves movies and reading. Once again, he likes the variety and having different outlets, depending on what is calling his attention at the time.
Sebastian describes himself as very driven and his achievements to date would confirm it. Curiosity is a nagging factor in his drive and where he has ended up. He calls it one of the most fun parts of medicine.

It’s been just over a year since some overseas doctors were permitted to register in Australia through an expedited pathway without first being assessed by the Royal Colleges. Medical Forum looks at whether the pathway is delivering what it set out to.
By Suzanne Harrison
In October last year a fast-tracked route to working in Australia was launched for doctors with the aim of boosting our medical workforce. It was met with caution from leading medical bodies but warmly welcomed overseas.
While it has proved to be popular and applications are rising, it seems the Expediated Specialist Pathway (ESP) for overseas doctors still has a few teething problems.
The pathway was introduced after a review held in 2023 by retired public servant Robyn Kruk, who urged the government to fast-track the accreditation process.
Doctors from the United Kingdom, Ireland and New Zealand were able to apply to work in Australia through the pathway.
It enables eligible internationally qualified medical specialists (SIMGs) with specific international qualifications to apply directly to the Medical Board of Australia and the Australian Health Practitioner Regulation Agency (Ahpra), rather than be assessed individually by a specialist college.
It opened in the final quarter of 2024 for general practice, with anaesthetics and psychiatry added in December, and obstetrics and gynaecology in March this year.
One year since its launch 67 specialists have registered to practise in WA. Nationally, 536 specialists have applied through the pathway, with 343 now
registered to practise – 305 of which were GPs.
Between October 2024 and August 2025, 49 GPs registered to work in WA.
But while the numbers look promising, it is still early days and there are concerns.
As a rural GP and RACGP WA Deputy Chair Dr Damien Zilm is well-placed to experience first-hand how the new pathway has influenced rural doctors.
Dr Zilm’s initial response is that it’s too early to determine if the pathway has met its goals. However, he believes the pathway is going to be “part of the solution” and that it is addressing the shortfall of doctors the state is facing.
international specialists, such as Clinician Assist provided through the WA Primary Health Alliance and the Health Professionals Network provided by Rural Health West.
He said support systems around any international medical graduate were crucial.

“There's a lot of nuances to training in the Australian system that make it hard for our overseas colleagues because of the differences within patient care and the standards of care, but also, probably more importantly, the local care pathways.
“It takes time to learn those and to be able to implement them safely and to provide the best level of care.”
The issue for practitioners such as Dr Zilm is that around 80% of doctors coming through the program are reportedly working in MMM1 (major city) areas instead of the intended more remote areas (MMM2-7).
“Only about 20% are actually going to rural or remote areas, which is insufficient to address workforce needs.
“Increasing the workforce in smaller, rural communities remains a priority.
“But there are two key needs. One is getting more doctors into rural areas, the other is providing robust support to ensure they can work safely.”
Dr Zilm said some systems were already in place to help support
The total specialists registered to work in Australia during the pathways first year included 305 GPs, 12 psychiatrists, three obstetrician-gynaecologists, 22 psychiatrists and 11 anaesthetists.
Most – some 86% – of applicants were qualified in the United Kingdom.
“Numbers are changing all the time as new specialists are registered through the pathway and starting work in locations around Australia,” a spokesperson for the Medical Board of Australia told Medical Forum
They added that the pathway had streamlined the registration processes while maintaining high standards. It allows highly qualified
medical specialists from similar health systems to be registered faster so they can start seeing patients in Australia sooner.
Ahpra chief executive Justin Untersteiner said the pathway was one of several workforce initiatives where the regulator had an important role to play.
“We're using a range of regulatory strategies to safely boost Australia's health practitioner workforce to help patients get the care they need, when they need it,” Mr Untersteiner said.
The Board said that getting doctors to work in rural and remote communities in Australia is an ongoing challenge facing governments and employers, which are responsible for workforce distribution.
Governments require specialist international medical graduates to practise where there are identified workforce shortages, controlling workforce distribution through access to Medicare.
A detailed report on pathway outcomes for the six months from October 2024 to April 2025, shines a light on where these specialists are registered to practise.
It shows how the new specialists have been approved to practise where they are needed – 86% in identified areas of workforce shortage such as fast-growing outer metropolitan areas, and 20% specifically in regional, rural or remote areas where it is traditionally harder to recruit.
By the end of September 2025, international specialists had been registered to practise in all states and territories.
The numbers of specialists in all states and territories: By the end of September 2025 nationally, 536 specialists had applied through the pathway, with 343 now registered to practice – 305 of which were GPs.
Obstetrician and gynaecologist Jared Watts has completed three assignments with Médecins Sans Frontières/Doctors Without Borders (MSF) in Nigeria, Syria, and Sierra Leone.

Not only was the work rewarding, but it helped him develop skills to manage challenging cases in remote Western Australia. Why did you want to work with MFS?
When I started working in the Kimberley, I had a contract that allowed me to work overseas with MSF. I was instantly attracted to their principles of impartiality, neutrality and independence.
For me, it is an organisation that always aims to provide the best care possible, irrespective of where or who the patient is. I saw these principles in action and have never looked back.
What experience did you have that prepared you for working with MSF?
Before MSF, I worked for two years in rural parts of WA, which is the best pre-departure experience someone can have. I also undertook a post-grad qualification in tropical medicine and global health, which helped me understand the health issues in the areas MSF works.
MSF also has a support network of international staff. Before my
first assignment I spoke to an experienced doctor about my concerns, which was a huge help.
What is a memorable moment for you on assignment?
In Syria, I worked to rebuild a service in a hospital that had previously been occupied by Islamic State. The team was made up of professionals from engineers to nurse managers, orthopaedic surgeons, obstetricians, midwives and translators.
It grew so quickly because of the high demand for medical care. I remember walking into the birth suite one day at 8am and walking out at 8:04am having seen five babies born.
The passion, hard work and dedication of all the staff was incredible. To see a service start and grow so quickly was something I will never forget.
What did you learn from working overseas?
Right from my first assignment, I learnt so much about providing care in remote emergency settings.
When I was in Nigeria, I worked with local doctors who taught me

a lot about operating on difficult and complicated cases with limited resources. In Australia, we aim for complicated cases or births to occur in tertiary hospitals, with all their available equipment and expertise, but we know unexpected births and emergencies can still occur anywhere.
Since being back in Australia, I have taught the skills I learnt on assignment to many rural doctors, helping improve the emergency obstetric care we provide across rural and remote areas.
What advice would you give to someone considering working with MSF?
Do it. It can seem a little scary to start with, but the support MSF gives you is incredible. You learn a lot and often don’t want to leave.
MSF is recruiting obstetriciangynaecologists, surgeons, anaesthetists and paediatricians to work on humanitarian projects.

continued from Page 21
She added that general physicians, general paediatrics and diagnostic radiology were the next tranche of specialities to be added to the pathway.
The view from the West
According to Rural Health West deputy chief executive Kelli Porter, the pathway has had a small impact in regional WA.
Specialists were destined for a range of locations and work settings, including hospitals and metropolitan regions.
AMA National President Dr Danielle McMullen said that IMGs were a critical part of Australia’s healthcare system, particularly in regional, rural, and remote communities.
“But their pathway to being able to practise remains unnecessarily convoluted, costly, and opaque,” Dr McMullen said.

“Rural Health West has worked with seven medical practitioners using the pathway to gain registration in Australia; one has commenced practise in Newman, one has been approved and is in transit, and five have accepted placements and are in the process of obtaining registration,” Ms Porter said.
These doctors are destined for locations including Port and South Hedland, Kalbarri, and Geraldton, where they will work as general practitioners.
“When the pathway was introduced, eligible candidates already progressing through the RACGP Practice Experience Program Specialist were offered the opportunity to transition across.
“One is now practising at Puntukurnu Aboriginal Medical Service (PAMS) in Newman, and one who will commence in the Wheatbelt in December are examples of practitioners who transitioned their applications to the expedited pathway.”
But as the overseas-trained workforce grows, there are concerns about the level of support they are receiving.
The AMA wants to see more done to ensure international medical graduates in Australia can thrive.
IMGs now make up 53% of Australia’s rural medical workforce and account for more than 50% of all general practitioners nationwide.
However, the Medical Board disputes this, pointing to recent data that shows the Board granted registration less than six weeks after applications were completed for most international specialists through the pathway.
Previously, under usual pathways where assessment is controlled by the medical colleges, it could take between two to eight years before a doctor was granted specialist registration.
Dr McMullen called for reforms to better support all of Australia’s international medical graduates.
She said IMGs play a vital role in delivering healthcare yet outdated red tape and bureaucratic inefficiencies were hindering them and undermining the nation’s ability to meet growing healthcare needs.
“Despite their significant contribution being widely acknowledged, the current system fails to provide IMGs and their families with the support, transparency, and co-ordination they deserve.
“Many report feeling trapped in a complex and confusing registration process, often having to work outside of medicine while awaiting registration.
“Qualified doctors are left feeling stuck, navigating a maze of duplicate documentation, inconsistent requirements, and vague job descriptions – at a time when Australia faces widespread medical workforce shortages that are only expected to worsen.”
Ms Porter said the pathway had gone some way to addressing this, particularly through its streamlined registration process.
“By simplifying registration, the pathway saves valuable time and
resources, enabling practitioners to begin working in Australia more efficiently,” she told Medical Forum
The RACGP recently launched a new fellowship to support doctors who have navigated the expedited pathway to work in Australia.
While the College initially expressed concern about the pathway’s simple paper-based assessments substituting the medical colleges’ evaluations of suitability, the fellowship represents a turning point on its stance.
RACGP Vice President and WA Chair Dr Ramya Raman said the fellowship would deliver clear benefits to patients and the profession.
“These doctors are already working safely in our communities. By offering them fellowship, we can reduce professional isolation, strengthen their connection to Australian standards, and ensure they have access to ongoing education, mentorship, and resources,” she said.
“We’ll continue to monitor the expedited pathway and consult with the Medical Board and government to ensure evaluation remains rigorous and upholds Australian standards, and if issues arise, they are promptly addressed.”
What the future holds
Ms Porter added that while the pathway is delivering on its intended outcomes, some challenges remain.
“Delays can occur due to visa processing, individual circumstances, or red tape in the application process. Rural Health West continues to monitor and support candidates through these steps.
“However, overall, the expedited pathway is starting to show signs of filling critical regional placements and attracting skilled practitioners, helping to address shortages and improve healthcare access for communities across WA.”

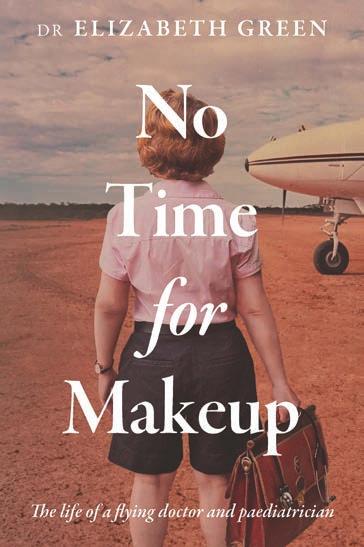
It’s a calling many doctors will be familiar with – the one to make a difference. It was that calling that inspired Dr Elizabeth Green to follow a career in medicine.
Dr Green’s desire to help others saw her travel from remote North Western Australia where she grew up in Kununurra to study medicine at the University of Melbourne.
After an application for a GP position got lost, a spur of the moment decision in 1988 saw Dr Green apply for a job at the Royal Flying Doctor Service (RFDS) Eastern Goldfields base in Kalgoorlie.
A number of experiences pinpoint Dr Green’s journey into medicine. One was seeing her dad treated in hospital for hepatitis as a young girl.
“That’s the first time I realised people get sick and I started thinking about that,” Dr Green told Medical Forum
“Then when I was eight, I was in a plane with my dad – it was a Bible Society plane and we were travelling
to an outback station – and a call comes from the RFDS to ask if we can divert to pick up a man who has fallen in a fire and was badly burned.
“I just remember the tone in the aircraft changed. There was this feeling that something bad was happening.
“I remember this man getting into the plane, he was badly burned, he was wrapped in a wet blanket and he was shivering. My dad was air sick and I helped him with a bucket while looking at this man trying to be reassuring.
“I thought ‘Maybe I could be a doctor’… and I think somewhere there must have been an interest, that feeling that you can make a difference.”
Stories like this, and many others
of her time as a RFDS doctor and paediatrician in Perth, are detailed in her memoir No Time for Makeup: The life of a flying doctor and paediatrician
She looks back on her time in Kalgoorlie as a time when she worked to the full scope of her practice, wearing many hats to deliver care to the people in the town.
She recalls doing a ward round at the hospital when she first arrived, where she often looked after patients, and asking the surgeon who the paediatrician was. He replied: “You are”.
“At that stage Kalgoorlie didn’t have an obstetrician, a paediatrician… so I was suddenly realising that I was it,” she said.
“That was the scariest part I suppose, when you got a call in the middle of the night and it was a distress call to a child who was ill. You’d get into the aircraft and you’d be in the pitch black of night flying on dead reckoning with no GPS.
“You didn’t know what medical condition the child would be in when you landed, and you just had to think ‘Have I got everything here to cope with this situation’. That was the most challenging thing.
“But you knew you made a difference. Without the remote nurse and the RFDS, that child would have died. Sometimes that kid might be an hour or two from death and you know that RFDS plane is their lifeline.”
One story that would send shivers down anyone’s spine is that of a rescue of a miner trapped underground at the Lady Bountiful mine outside of Menzies after a rockfall.
Dr Green had to venture

everything about it was. The physicality of the mine was very close, it was damp, it was hot”
Dr Green told Medical Forum
“It was also surreal. I’d never been down a mine and here I was, inappropriately attired as it turned out, and I got to this man who was trapped.
the rumble of the mine – it was an unstable mine. When I got to this man I must have looked terrified and I’m trying to put on my doctor hat, asking all those questions you ask as a doctor, and then hearing these rocks falling like a thunderous roar.
“This wonderful man said to me ‘Don’t worry, that’s from one or two levels above us, but if it gets closer


Do your patients need some extra support over the holidays?
Free mental health and emotional support are on hand at Medicare Mental Health Centres in Armadale and Midland throughout the festive season, including all public holidays. Walk-in support is available, or patients can book an appointment for counselling.
Open 10am – 8pm daily
No Medicare card or referral needed.
Medicare Mental Health

continued from Page 25
Among the nerve-wracking stories are more humorous ones. Like the time Dr Green and the RFDS went to pick someone up from Eucla who had a snake bite, but it turned out they’d just had a few too many, fallen down a sand dune and had a spear of spinifex bite them on the leg.
Reflecting back on her time as a paediatrician, including a traumatic stint at King Edward Memorial Hospital that still makes her feel emotional, Dr Green worries for the future of the specialty as the waitlist expands and cases become more complex.
“There are about 10,000 kids on the waiting list in Western Australia now and when I finished my private practice in 2022 there were about 6000. I knew things were going to get worse because I was seeing 1500 to 2000 kids a year on my books and they had to go somewhere,” she said.
“A lot of my colleagues are also
winding down in private practice for different reasons, so I think that the child waiting times, and the workforce issue is an ongoing, critical problem.
“I don’t really know how that is going to be resolved other than spreading resources and diluting paediatrics, so people won’t get to see a paediatrician very often.”
She hopes the “heart and soul” she put into her career in medicine and the importance of trust between a patient and their doctor comes across in her memoir.
She also wants it to be a timely reminder to those in positions of power – like politicians – that medicine is a challenging profession, one that is becoming harder in the face of more complex care needs and high patient demand and needs proper investment and resource.
No Time for Makeup: The life of a flying doctor and paediatrician, is available online and in bookshops.

“It
shows us how newer cancer treatments are evolving. The whole treatment paradigm is changing and, hopefully in the future, immunotherapy or targeted therapies and other emerging treatments are the way to go forwards. It could completely evolve the way we look at and treat cancers.”
By Aleisha Orr
Doctors at Sir Charles Gairdner Hospital (SCGH) have been able to cure cancer in two patients thanks to the use of a new medication.
Oncologist Dr Rajiv Shinde told Medical Forum the recent use of Dostarlimab as an immunotherapy drug for young patients with rectal cancer was part of what he sees as a change in the treatment paradigm.
The team at SCGH, where Dr Shinde works, was able to access this medication for free from the manufacturer as part of a compassionate access scheme.
Dostarlimab is a type of monoclonal antibody that works by attaching to a protein called PD-1 on the surface of cancer cells. This helps stimulate the immune system to recognise and attack the cancer.
It has been approved by the Therapeutic Goods Administration (TGA) for certain cases of endometrial cancer and was included on the Pharmaceutical Benefits Scheme (PBS) for this use in 2024.
However, it is not subsidised for other cancers. Accessing the medication for rectal cancer patients could cost tens of thousands of dollars.
“Dostarlimab has been used in trials internationally, which has shown some really amazing responses,” Dr Shinde said.
“We would have to wait many years for these approvals to come through, but sometimes we can request companies who make these products to allow earlier access on a compassionate basis for our patients.”
Dr Shinde said while data around the use of Dostarlimab for rectal cancer was “still evolving” it had been promising enough to trial for two patients with locally advanced cancer.
“Usually, the standard of care would be having chemotherapy, having radiotherapy, and looking at surgery, which has its own potential complications,” Dr Shinde said.
“We’ve been able to replace those traditional treatments by giving immunotherapy.”

Administered as an injection every three weeks, which took about an hour each time, the drug was given across nine cycles.
“Both patients had remarkable responses, even after two or three rounds of treatment. Their
whole treatment paradigm is changing and, hopefully in the future, immunotherapy or targeted therapies and other emerging treatments are the way to go forwards. It could completely evolve the way we look at and treat cancers.”
Dr Shinde said it was amazing to be part of the team who helped cure these patients of cancer, adding that immunotherapy treatments could play a greater role in cancer responses in the future.
While these two cases will add to the overall evidence around the use of Dostarlimab, they are not part of a specific trial.
Dr Shinde said he was hopeful that increased data coming from trials of the medication would identify the patients who could benefit most and lead to it being added to the PBS for certain rectal cancers.
symptoms disappeared, bleeding and the pain that is caused by the cancer goes away and the scans showed a complete response,”
Dr Shinde said.
“It shows us how newer cancer treatments are evolving. The
300 hours of AMC accredited training

Designed for registered medical and dental practitioners
Includes needle and low-level laser acupuncture techniques
Integrates evidence-based medicine with Traditional Chinese Medicine principles
Builds clinical skills for safe, effective management of pain and chronic conditions
Develops understanding of neurophysiology, diagnosis, and treatment planning
Meets Medicare and AHPRA requirements for medical acupuncture practice

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Western Australia’s Chief Health Officer is set to retire next year after more than two decades at the forefront of public health in the state.
Dr Andy Robertson helped guide the state’s health policy through the unprecedented COVID-19 pandemic.
He became a familiar face outside of heath circles during that time, often relaying critical health information to the public during live press conferences beside then Premier Mark McGowan.
But his career, including 22 years within the Department of Health, spanned a wider range of work.
Before joining the Health Department, he spent 19 years with the Royal Australian Navy where his specialist medical qualifications in public health medicine and medical administration, and his sub-specialty training in underwater medicine, disaster medicine, and chemical, biological and radiological defence were put to use.
He completed three tours to Iraq as a biological weapons chief inspector with the United Nations Special Commission as well as a number of sea postings.
“I’ve been fortunate that through my career, while I initially started out training in general practice within a military setting, I then had opportunities to further go on and train in public health medicine,” Dr Roberston said.

Dr Robertson joined the WA Department of Health in 2003 as the Director of Disaster Preparedness and established a career focused on public health emergency management.
He led health sector responses to events such as the 2004 Indian Ocean tsunami, the 2005 Bali bombings, and undertook emergency deployments after regional earthquakes and the Fukushima nuclear incident.
“Since entering the Department of Health, some of the high points have been working in the disaster response phase, leading the medical team into the Maldives after the 2004 Asian Tsunami,” he said.

“Leading a medical team to Yogyakarta after the earthquake there, working as the radiation health advisor in Japan after the Fukushima reactor disaster – that was interesting.
“And being part of the forward team to Nepal after the 2015 Nepal earthquake.”
During the pandemic he was a key part of the Australian Health Protection Principal Committee, established to lead national health responses to the pandemic.
Dr Robertson looked back on that period as an eventful time.
“I think we did well. We learnt a lot. I think we’re far better prepared for any future outbreaks or pandemics,” he said.
As well as serving as CHO, Dr Robertson has held roles as the Deputy Director General, Public and Aboriginal Health in the Department of Health, and chaired the Radiological Council of WA among other duties.
Dr Robertson will continue in the roles of Chief Health Officer and Deputy Director General, Public and Aboriginal Health until February.
Premier Roger Cook extended his thanks to Dr Robertson, whose contribution to the state’s public health he described as “exceptional”.
“As Health Minister at the time, I want to personally thank Andy for his leadership, advice, and steadfast intellectual discipline in a globally exemplary response to the pandemic,” he said.
“His leadership was pivotal during the COVID-19 pandemic – arguably the most significant public health crisis in a century – where he guided the state’s response with expertise and resolve.”

From December the Australian Government’s under-16 social media restrictions are set to take effect.
Platforms will carry much more responsibility for preventing access by children under 16 and will likely require age verification for new and existing accounts, using methods such as Face ID and official identification.
For some families this will feel like a helpful reset on screen time, especially those who haven’t started phones in their children yet. But for teens who've grown up socialising online, it may feel sudden and unsettling.
Our role is not to police, but to prepare families for a transition that protects safety while preserving connections.
We should bring this into routine care now. I add a ‘digital’ domain to HEEADSSS, and I treat social media the way we treat sleep or substances and as part of every adolescent review.
It’s worth asking which platforms a young person uses, what the feed is doing for them (connection, distraction, coping), when they are using it – is it impacting sleep or other things like exercise, eating with the family, meeting up with friends – whether accounts are public or private, and what might change if access is limited.
The government’s social media ban for under 16s could go beyond the screen to impact their health and GPs need to be prepared, writes Dr Andrew Leech.
With teenagers, I keep it straightforward and nonjudgemental. We have never gone through such drastic changes like this before and so we are all in this together and learning about how to manage it.
This is a systems change, and it’s normal for them to feel frustrated or anxious about losing a familiar routine. We talk about alternatives before any lockout occurs.
Most teens will still have access to messaging via SMS/iMessage, WhatsApp or Messenger, and these can be used to keep small friendship groups connected.
They should consider exchanging important numbers now, setting up group chats, and as the ban was intended to do – encouraging them to build more offline contact through sport, hobbies, walks, birthdays, and school activities.
I've spoken to parents about this as well and to try to be impartial, keep their calm and understand that this is a new era in which they need to do their best to navigate and not overreact.
Families could co-create a ‘digital transition plan’ that states what stays (core messaging), what pauses in the family (infinite scrolling), and what replaces it (scheduled in-person time, a family dinner or structured online contact).
I encourage parents to model the same habits, such as not scrolling at dinner, phone-free bedrooms, and to make expectations fair and predictable.
What are the risks?
There will be an adjustment period. Some young people may show a withdrawal-like pattern – irritability, disrupted sleep or low mood – as routines change.
Others may lose access to communities that have been protective. We should watch for impulsive efforts to regain access, including sharing ID images, engaging with unknown ‘verification’ contacts, or moving to high-risk platforms.
It’s also possible that a sudden reduction in scrolling exposes underlying issues that were being masked or that teens were escaping from via their smartphone.
Issues like loneliness, bullying, or family stress which may briefly become more visible. I’ve seen teens end up self-harming or suicidal from sudden bans on their phone use at home.
It sounds extreme but just be mindful of those teens you might see who do have a history of mental health challenges or who might be less supported.
Who is most at risk?
Some teens rely on their online space to feel part of a community.
Groups such as LGBTQIA+ young people; neurodivergent teens may use structured online communities as safe, predictable social channels; teens in rural and remote areas; Aboriginal and Torres Strait Islander youth using group chats to maintain kinship ties.
Ask directly whose contact would be lost if access changes, which communities feel safe, and what alternative pathways we can set up now.
For teens with existing mentalhealth challenges, or those in higher-risk groups, I develop a brief safety plan that lives in the record and with the family.
We document early warning signs, agreed coping strategies, names of trusted adults, and where to present for urgent help. I provide crisis contacts and remind families that a GP review is available quickly if things deteriorate.
For ongoing support, I offer psychology referrals – via a mental health care plan if appropriate – and offer to write a letter to their school wellbeing teams.
Useful digital supports eHeadspace offers online chat style counselling and phone support. MOST is a newer app that can be self-referred to and has been useful for some teens seeking connection when isolated.
Red flags for closer monitoring include marked withdrawal, escalating school refusal, sleep reversal, self-harm thoughts or behaviour (including covering up injuries), and high-risk attempts to regain access.
If a family simply senses something isn’t right, I book a shorter review within one to two weeks. It can sometimes help just having a telehealth ‘check in’ or arranging a consultation with their parents to help them feel heard and validated as well.
When I speak to young people, I reassure them about confidentiality and tell them my focus is on safety and connection, not judging how they’ve used social media.
With parents, I emphasise that they don't have to be perfect: hold firm on the boundaries that keep kids
safe, avoid punishment-framed responses, and keep open lines of communication and checking in.
For current guidance, the most reliable source to watch is the eSafety Commissioner’s Social Media Age Restrictions Hub, which also includes printable clinic resources.
As this change rolls out, health professionals also have a responsibility to remain updated on the changes, to be checking in and educating teenagers and their families about what is going on just as we do with other issues they might confront.
ED: Dr Leech is the Director of Garden Family Medical Clinic
To access eHeadspace support: www.headspace.org.au/online-andphone-support/connect-with-us/
Warmest wishes from all of us at Perth Radiological Clinic, for a joyful and safe holiday season. We sincerely appreciate your continued support and valued partnership. Together, we’ve helped improve patient care and outcomes, and we look forward to continuing that work in 2026.
With appreciation, The team at Perth Radiological Clinic
Anxiety among new parents is increasing and GPs play an important role in reassuring, writes Dr Leon Levitt.
Anxiety among new parents has been increasing dramatically in recent years, even among GPs.
In early parenting anxiety can create long-term negative patterns for families.
What has changed? Babies are not crying more, there are no new infant diseases, breast feeding is no more difficult.
There are five possible reasons why parents are more stressed:
1. Extremely high and unreasonable expectations
2. Lower levels of family support
3. Little training, fewer teachers/ examples in the community
4. Both parents are now actively parenting, either possibly anxious
5. Ready access to information on our devices, but no training in using them
Reducing anxiety
GPs may be working with anxious patients or be anxious parents themselves.
So how can they reduce that anxiety in their patients and in themselves as parents?
With respect to these five reasons, there are several steps that can be taken.
Help to lower expectations: Inform parents of what is normal and real, share stories of struggle and challenge their misunderstandings. Babies cry frequently and the majority of the time there is no pain or distress. Most babies in the first months cry in response to an empty tummy, a full tummy, a full rectum, a gurgling tummy, passing a stool – it is going to be very frustrating if we try to fix what is not broken
Encourage them to find support: Call in family and friends, cultural supports, ask a friend to be a friend. Use the village or actively create one.
Connect them to reliable sources of information: Connect them with


good health advisors. If the anxiety is overwhelming and persistently present, then anti-anxiolytics and psychological therapy are both very successful.
Involve both parents in the education and the support.
With access to information readily available, it’s important to teach parents how to use ‘Dr Google’.
Parents ask Google or ChatGPT: “My seven-week-old baby is vomiting, what could be wrong?”
Dr Google will answer with all possibilities, including bowel obstruction, or brain cancer. The question is the problem here.
Parents need to be taught to ask “My seven-week-old baby is
vomiting. Is that normal for this age?”
Then they will be reassured and be given red flags to watch out for to escalate the concern.
GPs must have the same perspective. The question is not “What is wrong here?” but rather “Is this normal for the age? And are there any red flags?”.
To get to this assumption both doctor and parent must first ask if the baby is healthy or sick.
If sick – pale, lethargic, poorly feeding, not gaining weight – and the unwell baby is rarely crying and vigorous, then investigate immediately and refer to the Children’s Hospital.
If healthy – good colour, vigorous, gaining weight, crying – then ask the second question “Is the behaviour of concern, normal for the age or not?”
These two questions for parents and GPs will prevent unnecessary anxiety, tests, treatments and expense, and leave the whole family calmer and able to enjoy parenting more.
GPs need to learn what normal babies do, despite there being no specific training in normal, healthy parenting issues.
We look for the problem to fix and eliminate serious conditions not to be missed, or seek conditions to treat.
This attitude encourages us to look for illness in each presentation, despite the majority of early parental concerns being related to developmentally appropriate behaviours.
We must manage these like a headache in adult medicine. Some headache patterns raise red flags requiring active intervention or escalation, but don’t chase brain cancer with every headache just in case.
Rather, use clinical judgement and your educated perspective of normal and unwell infants.
Principles of responding to anxious parents
• Is the child healthy or sick? If healthy, is the concerning behaviour normal for the age? Jump to the conclusion that it is normal first
• Listen, record, summarise and show parents that they have been heard and understood
• Make a diagnosis and treat or explain the normal range – give parents your educated perspective
• Actively treat perinatal anxiety
• They need time – review in a week, build trust as a reliable, caring advisor.
All doctors will be anxious at some point, depending upon their own personality
It is when anxiety becomes overwhelming, intrusively preventing you from being present for your patients or at home for your family, that you should seek help, just as your patients should.
Anxiety is widespread. We should not think that we are immune. And treatments are effective if we seek that help.
So, find yourself a GP for yourself and then take their advice.
Take holidays regularly, schedule periods of pressure release, take that walk along the beach, think of activities that have made you feel good in the past and reintroduce them.
The path to a less anxious life is adding one nourishing activity a week into your schedule at a time.
ED: Dr Leon Levitt is a GP Obstetrician and author of ‘What do I do Now? The basics of parenting babies without stress’.

We wish our colleagues in the WA medical community a happy and safe festive season.
Thank you for your continued support throughout the year.
Warmest wishes from our staff and all the best for 2026.
AndrewTome,
Renaud Mazy and Steve Cohen-Jones, Ramsay Health Care WA CEOs


Parkinson’s nurse specialists play an important role in keeping GPs informed and supported in the ongoing care of their patient, writes Sheree Ambrosini, Clinical Lead Parkinson’s WA.
Parkinson’s disease and related conditions such as Multiple System Atrophy (MSA), Progressive Supranuclear Palsy (PSP), and Cortico Basal Degeneration (CBD) can significantly affect individuals and their families.
While neurologists play a central role in diagnosis and treatment, community-based support is essential to improve quality of life and care outcomes.
Parkinson’s nurse specialists provide a range of services to support patients.
These include:
• Home visits (or aged care facilities)
• Initial nursing assessment
• Ongoing assessment and monitoring
• Review of environment
• Education for a newly diagnosed person with Parkinson’s and their families
• Nursing management of symptoms
• Identification and nursing management of medication and side effects
• Monitoring responses to medications
• Education around device assisted therapies
• Referrals to other health professionals
• Advocacy
• Assistance with navigating the health, aged care and NDIS systems
When to refer
Follow up contacts with Parkinson’s nurses are based on the requirements of the person and the professional assessment of the nurse.
There is no predetermined frequency of visits, as each person using the service is an individual and everyone's needs vary.


GPs are encouraged to refer patients as early as possible following a confirmed diagnosis.
Early intervention by a Parkinson’s nurse specialist can help support patients and families in understanding the condition, improve self-management and symptom control and assist with navigating services and care planning.
It can also reduce avoidable hospital presentations and delays in accessing allied health.
In addition to newly diagnosed patients, referrals are also appropriate for individuals experiencing a progression or change in symptoms, needing support with medication management or side effects, facing psychosocial challenges or carer stress, or transitioning to aged care or requiring palliative support.
Who can refer?
Parkinson’s WA operates under an open referral system. Referrals can be made by GPs, neurologists and other medical specialists, allied health professionals and patients or their carers under self-referral services.
The only requirement is a formal medical diagnosis of Parkinson’s disease or a related condition. Referrals are simple and can be made online or over the phone.
Parkinson’s WA provides a unique, nurse-led service that complements the work of GPs and specialists. Our Parkinson’s Nurse Specialist Service offers expert clinical care, education, and coordination from diagnosis through to advanced stages and palliative care.
Our team covers the Perth Metropolitan area and the South West, offering home visits and support tailored to individual needs.
Once referred, our Parkinson’s nurse specialists work collaboratively with the patient’s healthcare team, keeping GPs informed and supported in the ongoing care of their patient.
ED: To refer online visit www.parkinsonswa.org.au/referrals or over the phone call (08) 6457 7373. More information at www.parkinsonswa.org.au
A single, well-timed preventive consultation represent one of the most powerful, cost-effective forces in healthcare, writes Dr Ramya Raman.

When we talk about healthcare, the spotlight often falls on hospitals, their waiting lists, bed shortages, or emergency department pressures. Yet, beneath the surface lies the quieter, steadier engine of our health system: general practice. Much of its most vital work happens invisibly in prevention, early diagnosis, complex clinical reasoning, and the lifelong relationships that help people stay well and out of hospital.
What defines primary care?
The conference convened by the World Health Organization at Alma Ata in 1978 used 100 words to describe primary care; they included essential, practical, scientifically sound, socially acceptable, universally acceptable, affordable cost and first-level contact amongst many others.
Three decades ago, Professor Barbara Starfield and colleagues asked a deceptively simple question in The Lancet : Is primary care essential? The answer, then and now, is yes.
Her analysis of health systems across countries found that nations with strong, well-resourced primary care achieved better health outcomes, greater equity, lower mortality, and lower overall costs than those that invested disproportionately in hospital and specialist services.
These findings have since been replicated worldwide. The conclusion is consistent: investing in general practice is the most efficient, equitable, and best way to deliver care. In Australia, where general practice provides over 90% of all patient contacts, this is particularly relevant.
Prevention better than a cure
Preventive care is the most invisible, yet most powerful, aspect of general practice. Each GP consultation offers an opportunity to identify risk early, support behaviour change, and prevent disease progression.
Take John, a 52-year-old truck driver who came in for what he thought was just a routine blood pressure check.
During the consultation, I noticed he hadn’t had recent bloods done and suggested a cardiovascular risk review. The results showed elevated cholesterol and borderline diabetes.
Over the following months, I worked with him on gradual dietary changes, smoking cessation, and blood pressure control. John lost weight, quit smoking, and normalised his HbA1c, all without a single hospital admission.
That 20-minute consultation over a few months, backed by continuity, trust, and follow-up likely prevented a heart attack or stroke within the next decade. It also saved the health system tens of thousands of dollars in potential hospital costs.
A single, well-timed preventive consultation like John’s will never make the news, but multiplied across the population, these quiet interventions represent one of the most powerful, cost-effective forces in healthcare.
Now, take Mary, a 58-year-old casual cleaner who hadn’t seen a GP for years. She dismissed her increasing fatigue and swelling ankles as ‘just getting old’.
By the time she presented to an emergency department with shortness of breath, she was found to have advanced heart failure and poorly controlled diabetes.
Her condition required a prolonged hospital admission, multiple specialist appointments, and lifelong medication. Perhaps, this could have been prevented?
The data speak for themselves. In Western Australia, avoidable hospital admissions for chronic conditions like diabetes, heart failure, and COPD account for tens of thousands of bed days each year, each costing around $2000 per day.
By contrast, a routine GP consultation attracts a Medicare rebate of around $42.
Every day that a patient avoids a hospital admission through proactive GP management represents both a personal and a public win: fewer complications, less time away from work and family, and less pressure on an already strained hospital system.
Australia’s health system has long benefited from a strong general practice foundation. The OECD’s Health at a Glance report shows that countries with higher continuity of care, like Australia, have lower hospitalisation rates for chronic disease and higher patient satisfaction.
Studies have shown that patients who see the same GP over time
have significantly lower mortality and fewer emergency visits.
What makes general practice indispensable isn’t only its efficiency, it is its humanity. Patients share their most private fears, their family stories, and their lived context with their GP. Over time, this trust becomes therapeutic in itself.
As Western Australia and the nation grapple with hospital strain and rising health costs, it’s worth recalling Barbara Starfield’s conclusion: strong primary care systems not only make people healthier, they make health systems fairer and more efficient.
In Western Australia especially, with large remote regions the invisible preventive work of GPs is the foundation to keeping public hospitals from being overwhelmed.
Enhancing that capacity is one of the most cost-effective health policies in our reach.
ED: Dr Raman is the RACGP Vice President and WA Chair.
MANDOONESTATE.COM.AU
Wild Swan is our contemporary fine dining restaurant, overlooking the manicured gardens and the Llawn at Mandoon Estate. Executive Chef Michael Hartnell and Wild Swan Head Chef Anthony Power have created modern and innovative a la carte and tasting menus that combine classic techniques with the finest local and seasonal produce. Their modern Australian menu has been carefully designed to match with our award winning wines and craft beers.







Make Medical Forum your go-to place to complete your CPD.
From next year we will be a RACGP CPD provider, offering EA, RP and MO content developed by WA specialists for you. Every module you complete will be added straight to your RACGP CPD home and put towards your yearly requirements.

Medical Forum
will be introducing live GP Masterclasses in 2026
Delivering RACGP accredited education by your local WA specialists – have your say on the topics and speakers you’d most like to see on the program.
Scan the QR code to help design your perfect masterclass


This is where cutting ribbons is the easy part. Running operations is less glamorous and does not lend itself to photo opportunities.
Politicians love openings and big announcements. They create photo opportunities and give the impression that something is being done.
As reported by Medical Forum, the state government is in advanced negotiations to purchase St John of God Mt Lawley Hospital.
I have a personal interest in this facility having been born there last century when it was St Anne's.
Health Infrastructure Minister John Carey said: “Bringing St John of God Mt Lawley Hospital into public hands will add new beds to the public system quicker than we can build them.”
The purchase, assuming it goes through (and given the announcement one would be stunned if it didn’t), will add 100 beds to the public system.
What is not clear is where additional doctors will be found to staff the hospital.
One assumes that current nursing, allied health and other staff will be offered positions by the new owner. However, not everyone wants to work for the government, some may choose to retire, take a sabbatical, or ponder other options.
This is where cutting ribbons is the easy part. Running operations is less glamorous and does not lend itself to photo opportunities.
Call me a cynic but let’s see what happens in six months before the backslapping goes too far.
It has been a challenging year for all with a slowing economy and increasing inflation, and the health sector has not been immune. As the year draws to a close our public heath system has faced one of its worst on record, with calls for action to ease pressure on hospitals.
Only time will tell whether this move from the state government will deliver.


I would like to thank all contributors and readers for their support in 2025 and wish you all a Merry Christmas and a happy, healthy and prosperous 2026. Complete your CPD with Medical Forum
Sign up to our Wednesday clinical newsletter to get the latest updates from your local specialists.
Scan the QR code to subscribe
Home to the Mandurah region’s only Dual Source CT machine

ChestRad are specialists in Cardiac CT, Chest CT and Lung Cancer Screening
Cardiologists – Dr Edmund Brice, A/Prof Abdul Ihdayhid, A/Prof Chris Judkins, Dr Sam Tayeb, Dr Justin Teng and Dr Tashi Zhaxiduojie
Cardiothoracic radiologists – Dr Conor Murray and Dr Shriv Srigandan
ChestRad's rooms are at the Mandurah Specialist Centre on Minilya Parkway, Greenfields (near the Peel Health Campus)

All Medicare rebated services in Mandurah BULK BILLED!
www.chestrad.com.au
By Matt Tilley, Curtin University & Clinical Psychologist, West Leederville
Performance anxiety is central to our understanding of sexual dysfunctions and disorders, like erectile dysfunction (ED), premature ejaculation (PE), and even male hypoactive sexual desire disorder (MHSDD).
Of course, there are other factors to consider, and a thorough assessment is warranted, especially in the case of ED which can be a symptom of more serious health conditions needing treatment, such as cardiovascular disease, diabetes or metabolic syndrome.
Men’s sexuality is heavily impacted by myths and stereotypes. For example; he is always horny, he would prefer sex over relationships, he can only self-regulate emotion through sex, he only thinks of his own pleasure and not his partner's.
Although there may be some truth in these for some men, how do they impact the men that don’t fit them, let alone the partners of these men?
In order not to alienate, misdiagnose, or pathologise the men we see, we need to remember that despite the myths, men’s sexuality is complex. Men will likely have varied sexual experiences throughout their lives, and these will contribute to their sexuality. These experiences may vary further depending on their sexual orientation and even gender identity.
The societal pressures that men can feel are key to understanding their experiences.
Men don’t typically ask for the role society ascribes to them, and they can have disastrous consequences; creating expectations that become internalised and can be felt like ‘givens’ in the man’s life. Although these roles can afford men privileges, they also come with expectations which create pressure and can contribute to the difficulties.
Men’s sexuality is a complex interplay of biological, psychological, and sociocultural factors
Performance anxiety is central to our understanding of sexual dysfunctions and disorders
Creating an ‘intimate team’ which is playful, erotic, pleasurable, and sexually satisfying is the antidote to sexual performance anxiety.
Broadly performance anxiety refers to the fear or stress of performing in front of others, underpinned by the fear of negative appraisal and evaluation. It can affect anyone.
The symptoms can be both cognitive and physical – worry, a fear of failure, nausea, a racing heart, shaking/trembling etc.
In a sexual context, these experiences likely cause a negative cycle of worry about a man's sexual performance, disrupting his ability to be present and attend to his pleasure.
If this becomes a feature for him, it may lead to sexual difficulties like ED or PE, fuelling more anxiety.
When he is over attending to his performance, and not the experiences of pleasure, he is likely to be engaging in something called "spectatoring", which we can think of as self-monitoring.
Doing so further shifts his attention away from the erotic cues and connection with his partner, disrupting and reducing his arousal and therefore the couple's sexual satisfaction.
This type of pattern is likely to lead to a pervasive loss of interest in sexual behaviours, a reduction in relationship satisfaction, and have a negative impact on his

overall quality of life as well as his partner’s.
Using the biopsychosocial framework for the assessment and treatment of sexual difficulties is vital.
It is also important that we consider the 4P framework – predisposing, precipitating, perpetuating, and protective factors – as doing so allows us to identify the interaction of complex factors which contribute to his experience and the most efficacious treatment plan.
In most cases, options like pharmacotherapy and counselling/ psychotherapy should be considered.
The antidote to sexual performance anxiety
Instead of thinking of sexual experiences as performative and something ‘to be done’, we assist our patients to view sexual experiences as playful, erotic, and pleasurable.
The experience of intimate time together replaces the focus on performance and outcome, thus increasing their overall sense of sexual satisfaction.
This then becomes a sustainable protective factor against performance anxiety, and hence any experiences of sexual difficulties.
As sexual performance anxiety is maintained by being overly concerned with how well one is ‘doing’ sexually, this reframe to a sexually playful, erotic, and pleasurable time together, with open communication and a mindful focus on enjoyment, typically generates an ‘intimate team’ which is key to the antidote.


By Dr Rashida Hakeem , Gynaecologist, & Dr Johannah Scaffidi , Senior Registrar in Obstetrics & Gynaecology, Joondalup
Existing fertility testing primarily serves as screening tests, aiming to identify women more likely to have a poor response to assisted reproductive technology (ART) and thus lower likelihood of achieving a pregnancy with treatment rather than the likelihood of spontaneous conception.
Anti-mullerian hormone (AMH) has become the mainstay of testing infertility patients, replacing the traditionally used day three FSH, oestrogen levels and antral follicle count.
It is related to the size of the primordial follicle pool and represents a marker of ovarian reserve. Importantly, it shows little variation between and within cycles, however newer studies have shown levels can be artificially decreased with the use of oral contraceptives, the Mirena and GnRH antagonists.
Ongoing oocyte atresia, a natural process during reproductive years, contributes to the age-related decline in normal AMH levels, accelerating after the age of 37.
Lower AMH levels are associated with poor response to ovarian stimulation, but the test is not sensitive or specific enough for predicting pregnancy rates.
Crucially, AMH levels do not correlate with the likelihood of spontaneous conception or the time to pregnancy, and they do not predict the age of menopause.
Furthermore, AMH levels do not provide information about the reproductive quality of the available oocytes. Age, therefore, is a much stronger predictor of reproductive success than AMH alone.
Who should have AMH testing?
The best overall strategy for AMH testing is to limit it to those who
Key messages
AMH levels don’t predict the chance of natural conception or the timing of menopause
AMH levels do not reflect the quality of a patient’s oocytes
A low AMH can create unnecessary anxiety, while a high AMH may give false reassurance about fertility.
are at an increased risk for having diminished ovarian reserve or infertility, who would benefit from ART and fertility preservation. Those women who would benefit
most from fertility screening include those >35 years, single women or same sex couples, those with unexplained infertility and family history of early menopause who would likely need ART.
Additionally, women who have had previous oocyte damage (ovarian surgery, torsion, chemotherapy/ radiotherapy, smokers) and those with known endometriosis also benefit from testing. Importantly however, AMH testing is not Medicare funded.
How low is low AMH?
Low levels of AMH predict a suboptimal response to treatment and low egg yield in an infertile
patient. It reflects quantitative decline but there is no consensus on the level which defines a depleted ovarian reserve. Pregnancy can still occur at undetected levels especially in young women.
Women with AMH <1ng/ml have similar cumulative pregnancy rates compared to women with normal level (EAGER study) and women with low AMH (<0.7ng/ml) or raised FSH have similar cumulative
pregnancy rates after 6-12 cycles of attempting pregnancy versus normal levels (Time to conceive study).
A low AMH can falsely create anxiety in a woman who hasn’t tested her fertility.
Similarly, a high AMH may falsely reassure a woman when not assessed in totality, hence pre and post-test counselling is important when recommending AMH levels.
Located at the Hollywood Consulting Centre in Nedlands, PBCI is a comprehensive Breast Cancer Centre dedicated to providing streamlined, evidence-based care Our team includes specialist breast surgeons, medical oncologists, experienced breast physicians, and a genetic counsellor who work together to support women and men through every stage of their breast cancer journey
T | 08 6500 5501 W | www.bcrc-wa.com.au
Fertility preservation options now widely available include oocyte cryopreservation and embryo cryopreservation.
An important consideration is that it is not medically funded unless undergoing treatment for cancer.
While assessment of fertility is multifactorial, below is an agerelated guide to ART for oocyte cryopreservation.
Women <30yo may consider oocyte cryopreservation in specific medical situations like low AMH, family history of early menopause, BRCA carriers or when there are barriers to natural conception like tubal factors, deep endometriosis and ovarian surgery.
Though AMH is a part of the puzzle of fertility, there are other important variables like female age, medical and gynaecological history, family history, relationship goals and family aspirations that come into play when considering oocyte cryopreservation.
Author competing interests – nil
Patients have access to same-day consultation with an experienced Breast Physician, breast imaging, and diagnostic biopsy, with ongoing surveillance available for those at familial high risk
Our model of care includes the support of specialised Breast Care Nurses and clinical psychologists, ensuring comprehensive care throughout their breast cancer journey

Through clinical trials, we provide patients with the benefit of access to international drug treatment trials and patient-focused research Our research informs and underpins the treatment we provide to our patients
By Dr Cameron Britton, Endocrinologist, Osborne Park
Gestational Diabetes Mellitus (GDM) is an increasingly common metabolic disease of pregnancy, potentially leading to adverse outcomes for mother and baby. These may occur in pregnancy itself (e.g. preeclampsia, macrosomia, complications from delivery) or in the long-term (subsequent increased risk of type 2 diabetes in mother and infant).
The importance of early detection and treatment of hyperglycaemia is increasingly supported by evidence and has contributed to updates in the diagnosis of GDM and overt diabetes in pregnancy made in the recently published Australian Diabetes in Pregnancy Society (ADIPS) guidelines.
The first ADIPS guidelines were published in 1991 in response to a lack of uniformity in the diagnostic methods and thresholds for the diagnosis of GDM.
These guidelines remained in use until updated in 2014, largely driven


by data from the Hyperglycaemia and Adverse Pregnancy Outcomes (HAPO) study.
HAPO was a large observational trial designed to assess if maternal hyperglycaemia in pregnancy not meeting criteria for type 2 diabetes carried an increased risk of adverse pregnancy outcomes.
It found a continuous association of maternal hyperglycaemia with
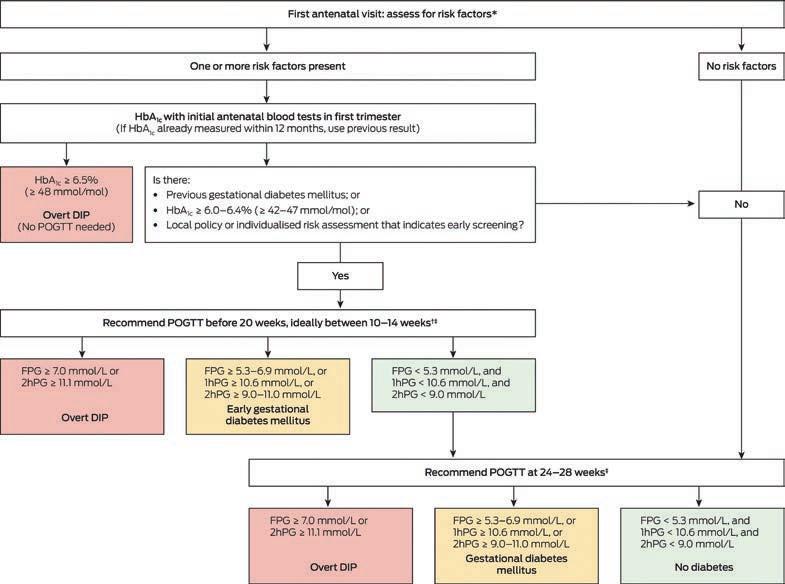
adverse pregnancy outcomes, particularly increased birth weight, without a clear inflection point.
The ADIPS 2014 guidelines recommended screening all women for GDM by Oral Glucose Tolerance Test (OGTT) between 24-28 weeks' gestation.
Higher-risk women would continue to be tested earlier in pregnancy. Diagnostic thresholds were derived from an odds ratio of 1.75 for adverse pregnancy outcomes in HAPO, which reduced the fasting cut-off value from 5.5mmol/L in previous guidelines to 5.0mmol/L.
ADIPS has drawn on two key publications to inform change from the 2014 guidelines. The Gestational Diabetes Mellitus Study of Diagnostic Thresholds (GEMS) study group published a New Zealand-based study in 2022 comparing ADIPS 2014 diagnostic criteria with higher OGTT cut-off values (5.5mmol/L fasting and 9mmol/L at two-hours).
This found no significant difference in the primary outcome of largefor-gestational-age infants >90th percentile.
However, a separately published subgroup analysis of the women with OGTT results between the two cut-offs found a significant improvement in the primary outcome for treated women.
There are new guidelines regarding early GDM testing in high-risk women
Thresholds for the diagnosis of GDM on OGTT have increased
Women meeting criteria for T2DM diagnosis in pregnancy are now diagnosed as ‘Overt Diabetes in Pregnancy’.
The Treatment of Booking Gestational Diabetes Mellitus (TOBOGM) group published data in 2023 from 802 women in New South Wales diagnosed with GDM. This demonstrated a significant improvement in the composite neonatal outcome for women who commenced early treatment of GDM prior to 20 weeks, particularly for those who underwent OGTT prior to 14 weeks gestation, or who demonstrated higher-range glycaemic levels.
These two studies led to a focus on early diagnosis and management of GDM and a reconsideration of OGTT cut-off values.
Early GDM screening for women at increased risk
Early assessment of GDM risk has now been clarified. All women with a risk factor for GDM should have HbA1c assessed at the first antenatal visit.
HbA1c ≥ 6.5% is diagnostic of overt diabetes in pregnancy (DIP), which will be discussed below. HbA1c 6.06.5% carries a recommendation of OGTT before 20 weeks' gestation (ideally 10-14 weeks).
If the woman has a history of GDM, then any HbA1c <6.5% also carries a recommendation of OGTT prior to 20 weeks.
Amended diagnostic thresholds
The diagnostic cut-offs for the diagnosis of GDM on OGTT have been amended to reflect an odds ratio of 2.0 for adverse outcomes in the HAPO study (adjusted from the previous ratio of 1.75).
GDM is now diagnosed at fasting plasma glucose ≥ 5.3-6.9mmol/L, one hour ≥10.6mmol/L and two hours ≥ 9.0-11.0mmol/L.
Women meeting diagnostic criteria for the diagnosis of T2DM in pregnancy on either HbA1c or OGTT are now diagnosed as overt diabetes in pregnancy.
The purpose of this diagnosis is to identify a more severe subset of hyperglycaemia, more likely to have pre-existing disease.
Women diagnosed with overt DIP can potentially avoid OGTT and be identified early for treatment and close monitoring.
It appears likely that these changes to OGTT diagnostic thresholds will result in a lower incidence of GDM. There is a focus on early diagnosis and management of the most needful of patients with hyperglycaemia in pregnancy.
To inform future guidelines the subset of patients who would have previously been diagnosed with GDM – but no longer meet diagnostic criteria – warrant prospective monitoring for associated outcomes.
Author competing interests – nil


Our warmest Christmas greetings, best wishes of health, happiness & work life balance for 2026 to all our referring doctors, allied health professionals, colleagues and their families. Thank you for entrusting us to be part of the health and wellbeing of our mutual patients.
Best of true health
Marek Garbowski & Perth Vascular Clinic Team
Perth Vascular Clinic is WA’s leading vascular solutions centre. With state of the art management & treatment of conditions affecting vascular health, we also offer practice-based, minimally invasive investigations and treatment.
Dr Marek Garbowski | Vascular & Endovascular Surgeon All enquiries & appointments bookings Phone: 6116 4955 | Email: reception@perthvascularclinic.com.au
Visit our comprehensive website www.perthvascularclinic.com.au
By Dr Sebastian Leathersich , Fertility Specialist, Subiaco
Obesity affects one third of Australian women of reproductive age, and over half are overweight.
A growing number are turning to incretin-based treatments such as GLP-1 receptor agonists (RAs) and dual GLP-1/GIP RAs, with prescriptions among women aged 18-44 increasing seven-fold since 2011.
This aligns with international guidelines recommending pharmacotherapy as an adjunct to lifestyle interventions in adults who are obese or overweight with obesity-related comorbidities.
In a recent study of Australian women of reproductive age prescribed GLP-1 RAs, only one in five were using effective contraception when treatment was started, and 2% reported a pregnancy within six months of starting treatment.
The safety of these medications during pregnancy has not been established and effective contraception is advised during treatment for all women at risk of pregnancy.
For many, this can be achieved with standard contraceptive options (considering the usual risk factors and contraindications), and there is no evidence that typical GLP1 RAs reduce the efficacy of oral contraceptives.
However, limited data raise concerns that the dual GLP-1/GIP RA tirzepatide might reduce oral contraceptive efficacy due to its greater effect on gastric emptying. It is therefore recommended that users of oral contraceptives employ an additional form of contraception for four weeks after starting tirzepatide, and for four weeks after any dose increase.
Non-oral contraceptive methods including IUDs and implants remain effective in women taking any of these medications.


For patients desiring emergency contraception during GLP-1 RA treatment it is uncertain whether oral options are effective. The copper IUD is the most effective method of emergency contraception and is also reliable in patients with obesity.
Whilst the term “Ozempic babies” has emerged to describe reports of increased fecundability when using GLP-1 RAs, the exact impact of these treatments on fertility is unknown.
For women with PCOS who are overweight and have anovulatory infertility, weight loss of 5-10% is associated with an increase in ovulatory cycles and live births. There is emerging evidence that treatment with GLP-1 RAs in this
population also improves menstrual regularity and natural conception rates by up to 70% compared to controls.
Whether GLP-1 RAs may have a role in obese patients planning to undergo IVF remains uncertain. A pilot study of metformin with or without liraglutide for three months prior to commencing IVF (with a one-month washout period) reported a significantly increased pregnancy rate in the liraglutide group despite similar degrees of weight loss in both groups. Further research is required in this area.
The improved metabolic and reproductive function occurring with GLP-1 RA treatment has resulted in pregnancies during treatment in
The weight loss and metabolic effects of GLP-1 RAs may increase natural and assisted conception rates
Reproductive age women using GLP-1 agonists should avoid pregnancy and be counselled regarding effective contraception
Although animal studies show toxicity of GLP-1 RA use during pregnancy, limited observational data in humans is generally reassuring regarding safety of inadvertent exposure.
both clinical trials and routine clinical practice, despite recommendations to avoid conception when using these medications.
This is a concern due to the lack of safety data regarding periconceptional GLP-1 RA exposure.
Animal studies in rats, rabbits and monkeys have demonstrated toxicity in pregnancy, with an increased risk of congenital anomalies, foetal growth restriction and early pregnancy loss.
These abnormalities are generally associated with substantial maternal weight loss and reduced food intake, and it is uncertain how they translate to humans.
The limited safety data in humans relies largely on registry-based population databases.
The largest, a Danish cohort of 756,643 pregnancies, identified 543 pregnancies with periconceptual GLP-1 RA exposure and reported a higher risk of pre-term birth in the exposed group but similar rates of other obstetric complications.
Furthermore, the available data in humans do not demonstrate a consistent pattern of congenital anomalies in pregnancies with inadvertent GLP-1 RA exposure, and rates do not seem to be significantly increased when compared to appropriately matched controls (i.e. with obesity or type 2 diabetes).
Given the paucity of safety data in humans and the evidence of harm in animal studies, GLP-1 RA use is contraindicated in pregnancy, and manufacturers recommend ceasing tirzepatide one month prior to conception, with a longer
Advanced Oncoplastic Breast Surgery Thyroid Surgery Cutting-Edge Breast Cancer Surgery Minimally Invasive Hernia Repair
Mr Saud Hamza
Specialising in:
Oncoplastic Breast Surgery including breast reconstruction and rotation flaps
Breast reduction and mastopexy (nipple lifting)

Removal of breast implants and mastopexy Thyroid Surgery.
Practicing Location: Mandurah & Murdoch
Operating Locations:
St John of God Murdoch, Murdoch Peel Health Campus, Mandurah Hollywood Private Hospital, Nedlands
The Mount Hospital, Perth
Email: info@saudhamza.com.au
Healthlink EDI: mrhamzas

Dr Wei Ling Ooi
Specialising in:
Oncoplastic Breast Surgery including breast reconstruction and rotation flaps
Breast reduction and mastopexy (nipple lifting)

Removal of breast implants and mastopexy.
Practicing Location: Murdoch
Operating Locations: St John of God Subiaco, Subiaco
Email: secretarydrooi@gmail.com
Healthlink EDI: wlingooi
washout period of two months for semaglutide.
If pregnancy occurs whilst using a GLP-1 RA, patients should contact the prescribing clinician, and the treatment should usually be ceased if safe to do so.
GLP-1 RAs may have a role in prepregnancy weight optimisation, but informing patients of the risks of increased fecundability and periconceptual exposure is an essential part of informed consent.
For women who do conceive after pre-conceptual treatment with GLP-1 RAs, support to manage gestational weight gain is essential, along with referral to an appropriate multidisciplinary team for ongoing management.
Author competing interests – nil
Dr Kai Hellberg
Specialising in:
Gallbladder Surgery
Hernia Surgery
Endoscopic Services with Gastroscopy & Colonoscopy Haemorrhoid treatments and other benign procto-rectal conditions
Ingrown Nail Surgery

All Skin and Soft Tissue Procedures.
Practicing Location: Mandurah & Murdoch
Operating Locations:
St John of God Murdoch, Murdoch Peel Health Campus, Mandurah
Email: murdochrooms44@gmail.com
Healthlink EDI: hellberg
Postal Address | Suite 44, Level 2, Murdoch Clinic, 100 Murdoch Drive, Murdoch WA 6150 Appointment Bookings | Phone: (08) 6148 0540 Fax: 9332 9425
www.perthsurgeons.com.au
By Dr Arpita Ghosh , Gynaecologist & Fertility Specialist, Hollywood
The updated Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) clinical guidelines on Miscarriage, Recurrent Miscarriage and Ectopic Pregnancy aims to improve clinical outcomes, enhance patient experience, and promote empathetic, culturally safe care.
Miscarriage, the involuntary loss of a pregnancy, is classified as a stillbirth after 20 weeks in Australia and New Zealand,
Incomplete miscarriage, occurring before 20 weeks, involves partial pregnancy tissue loss, moderate to severe vaginal bleeding, and pain.
Complete miscarriage involves expulsion of all pregnancy tissue, characterised by vaginal bleeding, pelvic pain, and passage of tissue.
A missed miscarriage occurs when the embryo or foetus dies, but pregnancy tissue remains in the uterus. It may be asymptomatic or present with vaginal bleeding or pain.
Threatened miscarriage is vaginal bleeding and uterine cramping before 20 weeks’ gestation.
Recurrent miscarriage is two or more miscarriages in pregnancies up to 20 weeks’ gestation, regardless of whether a gestational sac is present, or the miscarriages are consecutive.
An ectopic pregnancy happens when a fertilised egg implants and grows outside the uterus, mostly (97%) in the fallopian tubes.
from the guidelines
About 80% of all pregnancy losses occur in the first 14 weeks. Progesterone supplementation is not recommended for women with threatened miscarriage (having had no more than one miscarriage), as there’s no significant difference in live birth, stillbirth, or preterm birth rates.
In recurrent miscarriage, screening tests should be recommended when supported by evidence, including their limitations, alongside
Options for Missed or Incomplete Miscarriage
Management For: Clinically stable women with no heavy bleeding or infection.
Allows for natural resolution with follow-up (ultrasound/hCG monitoring) to confirm completion.
Medical Management
– Missed Miscarriage For: Women choosing a non-surgical approach. Process: A two-drug regimen. 1. Mifepristone: 200 mg orally.
2. Misoprostol: 24-48

counselling of patients about the benefits and harms of knowing the outcome of testing.
Thrombophilia screening: antiphospholipid antibodies (lupus anticoagulant and anticardiolipin antibodies) are routinely recommended.
Imaging and genetic testing: 3D ultrasound is routinely recommended, while parental karyotyping is considered case-bycase.
Thyroid screening: TSH, TPO antibodies, and thyroid function is routinely recommended, while other tests like HLA, cytokine, NK cell, and inherited thrombophilia tests are not routinely recommended.
Cytogenetic analysis of pregnancy tissue after miscarriage is not routinely recommended, as genetic abnormalities are unlikely to change clinical management.
Women with antiphospholipid syndrome and a history of recurrent
– Incomplete Miscarriage For: Women choosing a non-surgical approach.
Process: A single-drug regimen.
Surgical Management
For: Heavy bleeding, infection, patient preference, or failed expectant/medical management.
Process: A clinical procedure.
Preferred Method: Suction aspiration (includes manual aspiration).
Key Risk: Dilatation and sharp curettage increases the risk of intrauterine adhesions (risk rises with subsequent procedures).
Antibiotics: Prophylaxis is recommended. Doxycycline (± metronidazole) is common. Ideally given 2 hours pre-procedure.
Conservative (Expectant or Medical)
Clinically stable, no foetal heart activity, adnexal mass < 35 mm, willing/able for follow-up.
Surgical
Hemodynamically unstable, signs of rupture, hCG > 5,000 IU/L, adnexal mass > 35 mm, or contraindications to conservative management.
By hCG Level:
hCG < 1,500 IU/L: Expectant, Medical, or Surgical management.
hCG ≥1,500 & <5,000 IU/L (no significant pain): Medical or Surgical management.
Methotrexate (MTX) Regimen: Dose- 50 mg/m² administered intramuscularly.
Single Dose: hCG < 3,000 IU/L or mass < 20 mm.
Two Doses: hCG 3,000-5,000 IU/L or mass 20-35 mm (doses 4-7 days apart).
Procedures:
Salpingectomy (Recommended): Higher success rate, single procedure.
Salpingostomy (Consider if): Patient prefers fertility preservation without IVF. Carries a higher risk of treatment failure and need for further treatment (MTX or salpingectomy).
miscarriage should be offered low-dose aspirin (75 to 150mg daily) starting either before pregnancy or after a positive pregnancy test, in combination with low-molecular weight heparin (dose as per local protocols) from a positive pregnancy test until at least 34 weeks. Treatment should be stopped before birth.
In recurrent miscarriage and balanced translocations, options include natural conception or IVF with preimplantation genetic testing for structural rearrangements (PGT-SR), considering the specific translocation’s significance.
IVF does not improve recurrent miscarriage outcomes without known genetic conditions. Preimplantation genetic testing for aneuploidy (PGT-A) is an option when IVF is done for other reasons.
Genetic counselling is recommended for individuals with abnormal parental karyotypes and those with foetal or pregnancy tissue chromosome anomalies.
In recurrent miscarriage in women with uterine anatomical factors, septum resection is not recommended for uterine septum, regardless of pregnancy loss history.
Surgical management of congenital uterine malformations should be considered on a case-by-case basis, weighing benefits and harms, as there is no evidence to recommend it over expectant management.
Caesarean section niche resection is not recommended for women with or without recurrent miscarriage due
to insufficient evidence of improved live birth rates.
Hysteroscopic adhesiolysis for women with or without recurrent miscarriage should be considered on the merits of each case.
Polypectomy and myomectomy/ resection of submucosal fibroids are not recommended for women with recurrent miscarriage due to lack of evidence. Cases can be considered individually weighing benefit and harm.
In recurrent miscarriage, levothyroxine should be offered to those with overt hypothyroidism but not mild subclinical hypothyroidism (TSH > 2.5mlU/L) nor with a TSH ≤ 2.5mlU/L and positive thyroid autoantibodies (TPOAb+).
In women with recurrent miscarriage planning pregnancy taking levothyroxine, targets should be based on local pregnancy-specific reference intervals.
For women with subclinical hypothyroidism and/or thyroid autoantibodies not treated with levothyroxine, TSH should be checked in early pregnancy (7-9 weeks) with further monitoring as needed.
Pregnant women with two or more miscarriages and early pregnancy bleeding should be recommended progesterone.
It likely increases live birth rates and has no association with congenital abnormalities or severe adverse events.
Treatment should continue until 16 weeks’ gestation, with a daily dose of 400mg micronised progesterone vaginally.
In women with two or more miscarriages without early pregnancy bleeding there is no evidence that first trimester progesterone increases live birth rates.
An ultrasound can diagnose ectopic pregnancy by showing an adnexal mass with a gestational sac, an empty gestational sac, or specific signs like the ‘blob sign’.
An empty uterus or uterine fluid could suggest an ectopic pregnancy or an unknown persistent pregnancy. Other ultrasound features, symptoms, and hCG levels should be considered. Repeat ultrasound if initial findings are unclear.
Medical management can be methotrexate (MTX). Post-medical management includes close hCG level monitoring and potential for additional methotrexate doses.
Inform patients about temporary risks including nausea, diarrhoea, mucositis, abdominal pain, and mildly abnormal lab results.
Advise waiting three months before trying to conceive again and to discuss contraception options.
Insufficient evidence exists to recommend routine RhD testing and anti-D immunoglobulin for nonsensitised RhD negative women who miscarry before 10 weeks.
Anti-D immunoglobulin is recommended for surgically managed ectopic pregnancy and considered after discussion for medically or expectantly managed ectopic pregnancy.
The dosage is 250 IU for singleton pregnancies up to 12 weeks and 625 IU beyond 12 weeks.
Finally, women with early pregnancy loss must receive information about pregnancy tissue management options, recognising its importance for many, including the option to return the tissue to the woman and her family.
By David Roberts, Paediatrician, Woodvale
Most Australian states are changing stimulant medicines prescribing rules to enable GPs to independently diagnose and manage Attention Deficit Hyperactivity Disorder (ADHD) in response to increasing demand for assessment.
In WA, GP’s will be able to diagnose and treat adults and children over 10 years of age. This article relates to ADHD in children only. The existing stimulant co-prescribing arrangements remain in place.
The growth in the demand for assessment accompanies a growth in prevalence of ADHD, which many believe is caused principally by overdiagnosis.
The key to good management is correct diagnosis. In WA, the intended model of care is GP-led diagnosis and management in community-based family practices. As is the normal practice, difficult cases need to be referred on to specialists.
However, the six-month WA GP Training Program has only 65 places and has been greatly oversubscribed, meaning most applicants will be turned away.
So few being credentialled runs the risk of GP-staffed ADHD clinics springing up, which will exacerbate the overdiagnosis problem.
Stimulants are the first line treatment of ADHD. GPs are very familiar with prescribing Schedule 8 medicines – drugs of misuse, abuse and dependence.
Compared to other Schedule 8 drugs, these stimulants are not high-risk. The introduction of ScriptCheckWA adds another layer of safety.
The changes in prescribing restrictions is a movable feast and may well change in WA. By far the greatest risk in the new arrangements is not abuse of stimulants, it is of misdiagnosis.
The WA training program mandates
completion of two ADHD modules presented by the RACGP on its CPD platform, which have been written by Australasian ADHD Professionals Associations (AADPA).
These include The Identification and Management of ADHD, based upon AADPA’s Australian Evidence-Based Clinical Practice Guidelines (Guidelines), and The Pharmacological Management of ADHD based upon AADPA’s ADHD Prescribing Guide for Australian Healthcare Professionals.
The training also includes 10 hours of mentoring such as case conferencing and small group learning by an experienced ADHD clinician.
The modules claim ADHD “is still under recognised and undertreated” and that “heightened awareness, improved understanding, evolving diagnostic criteria and improved access to
diagnosis” explain the several-fold increase in prevalence in children observed world-wide over the past 20 years.
After much time, effort and money searching for a biomarker, no gold standard test has emerged for ADHD. The diagnosis is based upon subjective behavioural criteria, the core symptoms of inattention, impulsivity and hyperactivity – The Big Three of ADHD.
Further, population studies do not show a bimodal distribution of these core symptoms; rather they fall on a bell curve skewed to the right.
There is much evidence suggesting the rise in prevalence is due to a lowering of the diagnostic threshold for The Big Three; the emergence of a milder behavioural phenotype. The modules’ assertion that the rise in prevalence is due to ADHD now
being better recognised, rather than threshold for diagnosis being lower, is a controversial claim.
Further, one crucial diagnostic criterion is only mentioned in passing in the modules. The core symptoms must “interfere with or reduce the quality of social, academic or occupational functioning”. This relationship between The Big Three and functional deficit must be causal –mere association is not sufficient.
Finally, The Big Three of ADHD are normal in children. The modules are silent on how the diagnostician is to distinguish between normality and ADHD.
The RACGP modules are worthwhile, and I recommend GPs wanting to upskill in the management of ADHD should look at them. But they are not sufficient to provide a broad and insightful understanding of the condition necessary to diagnose and manage the patient competently.
Other more balanced perspectives should also be sought.
Author competing interests – Roberts is a CPD approved provider of ADHD training
More than 400 GPs have applied to take part in training to allow them to diagnose and prescribe for ADHD, despite only 65 places being available.
Participating GPs have been split into three cohorts, with the first of those groups beginning training at the end of October.
The second cohort are set to begin training in February and the third later in 2026.
Upon completing the training GPs will be able to assess ADHD in patients aged 10 and older. Under recent changes to WA’s prescribing regulations they will also be able to prescribe stimulant medications.
It is hoped the program would ease pressure on specialists such as paediatricians and psychiatrists by helping more people access early diagnosis and treatment.
The first of its kind training is being delivered by the RACGP.
The program will be supported by specialist mentorship from paediatricians and psychiatrists and delivered with oversight from WA Health.
The WA government was the first Australian jurisdiction to announce a comprehensive program for ADHD diagnosis and management by specialist GPs, with other states following suit in recent months.




By Dr Amy FitzGerald, Gynaecologist, Dr Ruth McCuaig, Gynaecologist, & Melinda Olive, Registered Nurse, Subiaco
Abortion care is health care. Ensuring safe equitable access to abortion care reduces maternal morbidity and mortality and is an essential component of the provision of reproductive health care.
It is not only essential healthcare but a fundamental human right, central to gender equality and bodily autonomy and is recognised globally as a priority under the United Nations Sustainable Development Goals.
Provision of safe abortion care empowers women, girls, and pregnant people to make informed decisions about their health and futures.
The Western Australian Abortion Care Clinical Guideline published in March 2025 provides best practice guidance for healthcare professionals delivering abortion care throughout WA aiming to improve access, equity, and safety in abortion services.
The guideline was initially developed by the Women and Newborn Health Service (WNHS) and North Metropolitan Health Service (NMHS) in response to the Abortion Legislation Reform Act 2023 coming into effect.
It was adapted from the widely respected Queensland Clinical Guideline: Termination of Pregnancy for a West Australian context. The Department of Health (DoH) and WNHS worked in collaboration with clinical experts and consumers, engaged key stakeholders and developed cultural consideration statements for Aboriginal people and those from culturally and linguistically diverse (CALD) backgrounds to further inform the guideline.
The guideline is easy to access online and encompasses not just the provision of surgical and medical abortion but provides guidance and explanation around key legislation changes, models of

care, cultural safety, consent, care for young persons, contraception, safe access zones, obligations of conscientious objectors, clinical and psychological assessments, care for Aboriginal persons and persons from CALD backgrounds and a family and domestic violence specific pathway.
Performing an abortion in WA has been decriminalised. Abortion on request is now permitted up to 23+0 weeks gestation, raised from the previous 20-week limit. A Ministerial Panel is no longer required for abortions above 20 weeks' gestation.
Mandated counselling prior to informed consent has been removed. Historically a person requesting an abortion needed to see two medical practitioners, one to provide information and obtain informed consent and a second to perform the abortion.
Now only one health practitioner is required to obtain informed consent in line with existing standards for abortions up to and including 23+0 weeks.
No additional training is required
to provide medical abortions (MS2 Step) up to 63 days gestation, although practitioners may wish to undertake this training.
Nurse Practitioners and Endorsed Midwives can prescribe early medical abortion drugs (e.g. MS-2 Step), under Schedule 4 medicine regulations in line with their scope of practice.
For abortions after 23 weeks, a primary medical practitioner must assess appropriateness based on medical, psychological, and social factors, and consult with another medical practitioner who agrees the abortion is appropriate in all circumstances.
Surgical abortion is currently available in WA up to 20 weeks' gestation in the public and private sector. Medical abortion is available at all gestations, but the patient must be an inpatient after 63 days. Feticide is recommended for abortions performed after 22 weeks.
Health practitioners may conscientiously object to performing abortions but must refer patients without delay to a provider or service that can perform an abortion or provide information approved by the
Chief Health Officer on accessing abortion services.
Conscientious objection does not absolve a registered health practitioner of any duty to perform, assist with, make a decision about, or advise a patient about a termination of pregnancy in an emergency (e.g. a life-threatening situation).
Further considerations
While these changes may seem significant, they simply bring Western Australia's abortion laws and clinical practices in line with other Australian states.
A request for abortion care should be met with respect for the person’s autonomy and their innate rights.
It further provides an opportunity to promote other aspects of healthcare including cervical cancer screening, breast cancer screening, STI screening, FDV screening and is an opportunity to discuss and provide contraception.
Often the road to an abortion requires multiple medical practitioner visits, pathology tests
Useful resources
1800 4 CHOICE helpline and website 4choice.org.au
Free helpline for people with unintended pregnancy and health care practitioners providing unbiased confidential advice from a qualified health practitioner

The website has an interactive map showing available services including pathology, imaging and abortion providers.
Phone line is open 9:30am-4:30pm Monday to Friday.
and imaging. There are significant costs and barriers to be overcome particularly for rural and remote persons, those experiencing FDV and Aboriginal and CALD persons.
For complex cases, the Pregnancy Choices Abortion Care Service at WNHS offers comprehensive, multidisciplinary support – bringing together medical, nursing, social work, psychological, and pastoral care professionals to provide patient-centred abortion care.
The 1800 4 CHOICE helpline is a valuable resource for both patients and practitioners, offering guidance and access to abortion services
across WA. The accompanying website provides region-specific service information to support informed decision-making.
While reproductive rights are continually challenged, these legislative reforms and clinical guidelines represent a meaningful step forward in protecting and advancing the right to safe, accessible abortion care and healthcare equity in West Australia.
Author competing interests - nil


By Dr Matt Clifford & Dr Will Ormiston , Interventional Radiologists, Nedlands
Varicoceles are the most common surgically correctable cause of male infertility, affecting up to 20% of adult men and 40% of those with primary infertility.
Despite this, optimal management has long been debated, with guideline recommendations varying. Recent evidence – both from a 2023 systematic review and a new 15-year retrospective series – has helped to clarify the picture, reinforcing varicocele treatment as a safe, effective and durable option that can meaningfully improve fertility outcomes in appropriately selected men.
A varicocele is a dilatation of the pampiniform venous plexus caused by valvular incompetence and retrograde venous flow.
This leads to scrotal venous congestion, increased scrotal temperature, oxidative stress and impaired spermatogenesis. Most cases are left-sided, but bilateral involvement occurs in up to 10%.
Clinically, varicoceles can be graded as small (palpable only on Valsalva), medium (palpable) or large (visible). Diagnosis is clinical, supplemented by ultrasound for confirmation or subclinical cases.
Treatment options include conservative management, surgical ligation (open, laparoscopic or microsurgical) and percutaneous embolisation – a minimally invasive radiological approach that occludes the refluxing gonadal vein using coils and/or sclerosant.
Who should be treated?
Not all varicoceles require intervention. Treatment is recommended in men with painful varicoceles, abnormal semen parameters or elevated sperm DNA fragmentation, and otherwise unexplained infertility in a couple seeking conception and in couples who have failed assisted reproductive technology (ART), recurrent pregnancy loss (RPT) or poor embryo development.



Asymptomatic or subclinical varicoceles with normal semen parameters and normal fertility are unlikely to benefit from treatment.
Evidence base
A 2023 meta-analysis published in European Urology Focus pooled 12 prospective studies (10 randomised) involving over 1300 men. Varicocele treatment – via either surgery or embolisation –significantly improved spontaneous or assisted pregnancy rates compared to observation (OR 1.29, 95% CI 1.00–1.65, p = 0.048).
Sperm concentration increased by an average of 12 million/mL, with notable within-group improvements in motility and morphology.
These benefits were confined to men with abnormal baseline semen parameters. Men with normal semen saw no fertility advantage. Taken together, these findings support active treatment for men with both clinical varicocele and
demonstrable spermatogenic impairment.
Complementing the metaanalytic data, a 2025 CVIR Endovascular study from Galway and Dublin reviewed 225 varicocele embolisations performed over 15 years.
The technical success rate was 96%, with clinical success (symptom or fertility improvement) in 93.8%.
Among men treated for subfertility, 51% achieved successful conception following embolisation. The confirmed ultrasound recurrence rate was remarkably low – just 6.3% over a mean follow-up of eight years, though ultrasound follow-up was inconsistent.
Complications were rare (1.8%), limited to minor oversedation, small groin haematoma, or transient pain. No major adverse events occurred. Outcomes were consistent across embolic agents; coils alone, coils
Varicocele repair improves pregnancy rates and sperm concentration in men with abnormal semen parameters
Embolisation achieves >90% clinical success with a very low recurrence rate and rapid recovery with efficacy and safety of embolisation comparable or superior to surgery
Close cooperation between urologists, fertility specialists and interventional radiologists optimises patient outcomes.
plus sclerosant and occlusion devices.
Importantly, embolisation remained highly effective even in patients with prior failed surgical ligation, all of whom were successfully treated radiologically.
Percutaneous embolisation is

high anatomic precision and low radiation exposure.
Compared with surgery, embolisation carries fewer complications (RR 0.63 vs. surgery), no risk of testicular arterial injury, and faster recovery – most men resume normal activity within 48 hours
Recurrence is usually related to missed collateral veins or incomplete occlusion and can often be managed with repeat embolisation.
Beyond improving spontaneous conception rates, varicocele repair enhances outcomes in assisted reproduction (IVF/ICSI) and reduces sperm DNA fragmentation.
Symptomatic relief for men with scrotal pain is common, with embolisation offering a durable solution and minimal downtime.
Guidelines published in the Medical Journal of Australia recommend that treatment of varicoceles be considered in clinically significant cases.
in most major Australian centres with interventional radiology expertise, but awareness remains limited.
Collaboration between urologists, reproductive specialists, and interventional radiologists ensures that men are appropriately selected and counselled on all management options.
As data continue to accumulate, embolisation is emerging not only as a minimally invasive alternative to surgery but as a first-line treatment in its own right for suitable candidates.
Varicocele treatment has finally moved beyond controversy. With consistent evidence from both randomised trials and long-term real-world data, embolisation now stands as a durable, minimally invasive, and fertility-enhancing option for men with clinically significant varicoceles.
Author competing interests – nil
Varicocele embolisation is available Complete
Performance anxiety and sexual dissatisfaction
GP management of ADHD
Varicocele treatment and fertility
Obesity medications and pregnancy
WA’s abortion care clinical guidelines
Miscarriage and ectopic pregnancy guidelines
Anti-mullerian hormone in fertility
Gestational diabetes guidelines
Home births
Social media ban –what to expect
Opportunistic HIV testing
Syphilis and affected babies
Digital first
Investigating anxiety in children
Respiratory and palliative care
From pro surfer to mental health advocate, Cooper Chapman says it only takes 1% of your day to truly make a difference.

By Ara Jansen
When it comes to being good, humans aren’t always great at keeping their word, particularly when it comes to things like sugar, exercise, social media engagement, keeping in touch and our mental health.
But what if you gave just 1% of your day every day to doing better for yourself and your mental health?
Cooper Chapman, founder of The Good Human Factory, says just 14 minutes a day will make all the difference. In his new book The 1% Good Club the Gold Coast-based mental health advocate is showing Aussies across the country how.
Over the last couple of years Cooper’s focus has turned to helping other people with their mental health. Using everything he learnt as a former top 100 pro surfer and the tips he’s gained from other high-performance people and coaches, he’s written The 1% Good Club
Starting as a Facebook group, it has morphed into a highly successful movement and now a book.

The book makes a case that for 1% of your day – or 14 minutes – you can help, improve and elevate your mental health.
In it, the 31-year-old shares his own journey around mental health and is honest about his own ups and downs. He shares practical tips for what he does daily to help himself.
He shows you his full potential habits charts, which he ticks off every day (and no, he’s not perfect), he talks about sleep (Cooper goes to bed at 8.30pm and gets up at 6.30am) and nutrition, regulating emotions and ways to build gratitude and calm. Things we know, but don’t always give to ourselves.

He also leverages his podcast to share insights from his guests, all of whom are listed in the back in case you want to take a deeper dive.
“I lost an uncle to suicide when I was six and during my teens saw my dad go through some hard times,” says Cooper. “Because of that I was always aware that my mental health was something I should be careful about.
“In my 20s I went through my own struggles with my surfing career and learnt some valuable lessons both from experience and the coaches I worked with.”
Cooper started on the journey to establishing his company The Good Human Factory when his sister told him about a boy at her school who had died by suicide.
Cooper wanted to do something and to help young men in particular, so he asked a friend at the school if he could talk to the students about their mental health, sharing with them what he had already learnt as an athlete.

We have two copies of The 1% Good Club to give away to lucky Medical Forum readers.
We also have five double passes to see French comedy film My Brother’s Band in cinemas on Boxing Day. The film follows two siblings separated by fate and reunited by music. It’s a feel-good trip to the cinema this summer.
If that doesn’t take your fancy, we have more movie tickets to giveaway. Win one of 12 double passes to see The Choral in cinemas from January 1. As the war rages on the Western Front and conscription papers start to arrive, one community discovers the best response to the chaos laying waste to their lives is to make music together.
Or take home one of 12 double passes to see Anaconda, in cinemas Boxing Day. When a midlife crisis pushes best friends to head to the Amazon to recreate the iconic Anaconda film, things turn chaotic when they encounter a real anaconda.
We also have more wine to give away. See our review of Sandalford Wines on page 63 for more info.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
A few years on, he has spoken to more than 50,000 students and his podcast has received one million downloads.
“In the back of my head, I think I knew that being a professional athlete wasn’t a forever career, but I did know that I would always be a surfer, I would always travel, and I would always be curious about the world, different cultures and be interested in different perspectives.
“I never guessed this is what I would be doing. It allows me to follow my own life philosophy that I started to realise when I was surfing. I read a lot about service and generosity and decided I wanted to direct my time and energy in service to others.”
Echoing that first chat he had with those high school students, Cooper now spends much of his time doing workshops and speaking engagements. He works with
adults and young people, hoping to spread the message of looking after your mental health.
“The world is changing so quickly with expanding technologies and our ability to regulate ourselves is diminishing. We have to look after and invest in our wellbeing and our mental health in the face of that.
“I talk about having 10 health habits for every day. You might not get through them all, but you want to aim for over half. That helps me build a life by design.”
The 1% Good Club is out now through Wiley RRP $34.95 from all good bookstores.
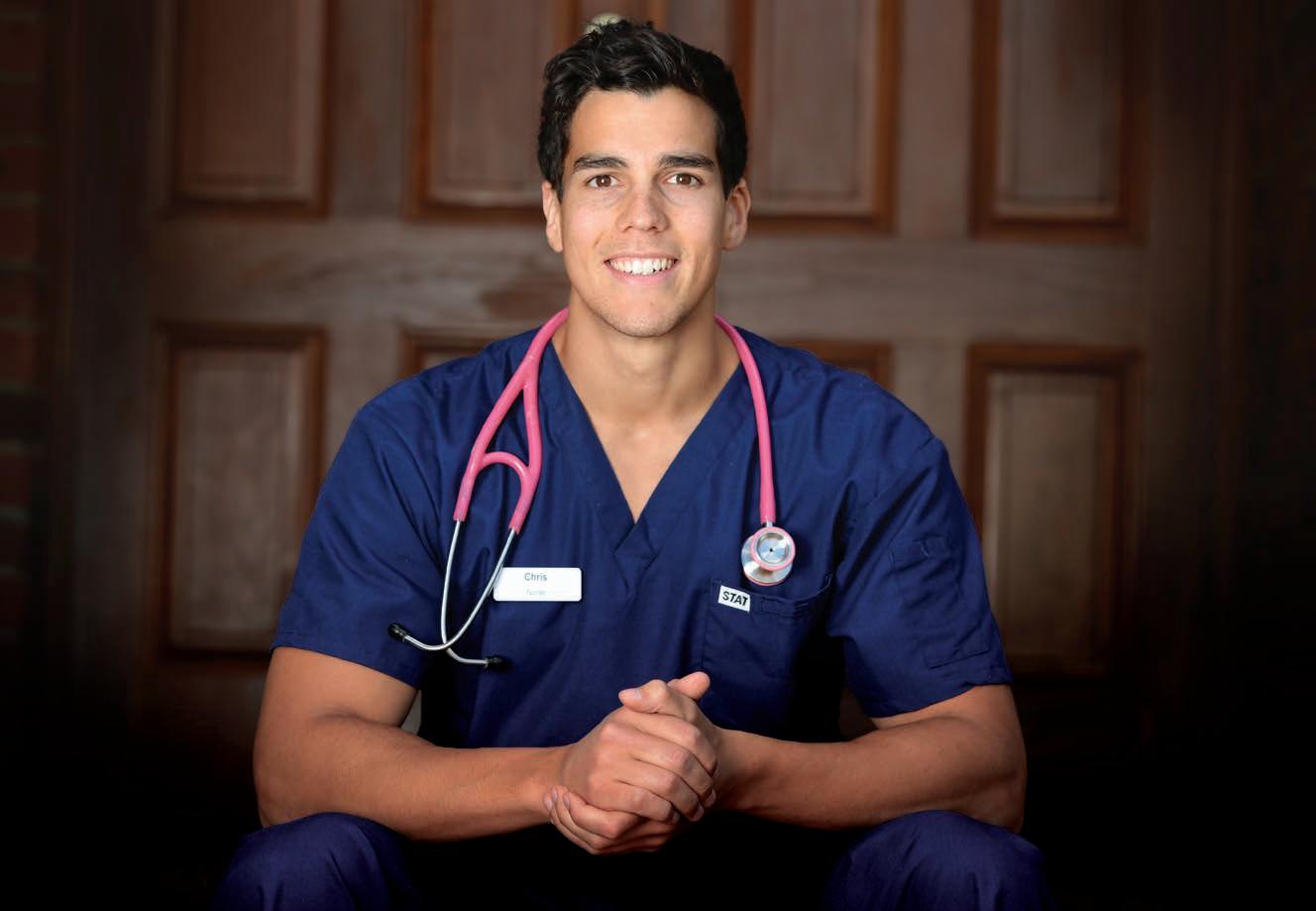
Now a health and fitness expert, former registered care nurse Chris Nayna looks after people during a different part of their life journey.
Being a former registered nurse might well be the secret to Chris Nayna’s success – and the key to his unique approach.
While studying nursing he fell in love with cardiology and went on to become a critical care nurse specialising in cardiology. It taught him to understand people holistically and meet them where they are at.
Interested in his own health and fitness following a pre-diabetic diagnosis as a teenager, Chris made time to train daily. He began to enjoy the process, progress and the sense of community – all of which quickly became the best part of his day.
Eventually Chris formalised his knowledge, delving deeper into human biology, exercise physiology and behaviour change
By Ara Jansen
and completed a degree in applied science, a certificate in personal training and strength and conditioning coaching.
“I was working fulltime as a nurse and doing post-graduate studies when enquires about personal training services escalated,” says Chris. “That’s when I knew it was time to get qualified and open a gym in my garage.
“I loved that I could still care for people, only this time in a more proactive and preventative way. It also allowed me to run my own business and provided me with the freedom to pursue other interests.
“The knowledge I gained from nursing has been invaluable. It taught me clinical insight and empathy, and it’s become a major point of difference.
“I love being part of the preventative side of healthcare, educating, building relationships and helping clients understand the significant positive flow-on effect that looking after their health and fitness has – more energy for family, greater focus at work and an ability to thrive in every area of life.”
Almost two decades later, Chris has become one of Australia’s most respected and sought after health and fitness experts thanks to this holistic approach which combines clinical nursing experience with strength and conditioning coaching. The dad of three considers himself a lifelong learner and multidisciplinary coach. He likes to be involved in different but allied projects, which explains why he has written for Men’s Health, coached CEOs and executives, been a Ninja Warrior

on television, is head of fitness at members club Lawson Flats and was handpicked to design the fitness offering at Melbourne’s Saint Haven, Australia’s first private wellness club.
Most recently, he launched Adapt Health Club in Claremont – a boutique health and fitness club.
Chris – who has lived in Perth for the last two years – considers health and wellness not a sprint, but a marathon which requires ongoing attention and creating systems to help you perform at your best.
“Medical professionals understand the demands of healthcare.
Long hours, emotional load and shift work make selfcare nonnegotiable. If you don’t have the energy or emotional bandwidth to give to others, your ability to care effectively diminishes.
“For me training isn’t just about aesthetics, it’s about changing your physiology to generate more energy, clarity and capacity to give more to life. The physical and psychological health benefits are significant when you invest in your own wellbeing.”
With the holidays looming, it’s a time when people can often be
less strict with their health and fitness. Chris suggests during the festive season and summer, start by remembering the basics – sleep, nutrition, hydration and movement.
“When travelling, I always pack a set of resistance bands, they’re lightweight and super versatile. If you’re out of your normal rhythm, walking, running, swimming, cycling or playing social sports like a game of backyard cricket are great alternatives. Movement is medicine and even better when it’s social,” he says.
“Keep your habits simple on holidays. No need for a gym with all the bells and whistles. Find a local park, use an outdoor gym or go for a run. Doing it with the people you’re on holiday with is a good way to connect and look after each other’s physical and mental health.
“Once you’re back to your routine, you can rebuild momentum quickly. Take it as an opportunity to recalibrate and get a different perspective. You might even find a new activity you like.”


The Wizard of Oz – A Traditional Christmas Pantomime
12TH – 24TH DEC
Click your heels together and get ready for a whirlwind adventure!
Taylor: A Tribute to the Eras Of Taylor Swift
SAT 17TH JAN
Swifties unite for the ultimate unofficial tribute show to every Taylor Swift era.


Stewart Copeland
SUN 11TH JAN
Legendary drummer Stewart Copeland embarks on his first spoken word tour.
Where Is The Green Sheep?
TUE 20TH JAN
An immersive theatre experience inspired by the beloved book Where is the Green Sheep?
Andy and the Odd Socks
MON 12TH JAN
Andy Day and the Band deliver a hilarious, uplifting, high-energy live kids show.
Hits Of The ‘60s and ‘70s By The 60 Four
SAT 7TH FEB
The 60 Four celebrate the sounds of Elvis, The Beach Boys and The Beatles.

Our podcasts bring you the latest updates and key insights into new treatment options available.
Join our clinical editor Dr Joe Kosterich in conversation with WA specialists to learn more about developments to improve patient outcomes. Our podcasts are now CPD verified. Look for the CPD logo to complete your self-reflection and claim your time.
Learn more about:
Aortic stenosis: managing low-risk patients with Dr Gerald Yong
Is it pelvic venous congestion? With Dr Marek Garbowski
Rethinking radiation oncology with A/Prof Yvonne Zissiadis & Celia Byatt
Lung Cancer Screening with Prof Fraser Brims
How to approach acute and chronic knee pain with Dr Jean Louis Papineau
Listen on your favourite podcast platform – scan the QR code to follow us!

Sandalford Swan Valley vineyard is one of WA’s oldest, established in 1840 by John Septimus Roe, the first surveyor-general of the Colony.
He was granted 4000 acres on the Swan River and, amongst his many agricultural endeavours, he pursued vines brought from South Africa. Once planted they heralded the dawn of the Swan Valley wine industry. He named it Sandalford after his English home.
Future generations of the Roe family continued on the property. In 1970 a large property was purchased in Wilyabrup, Margaret River, vines were planted and they became one of the pioneers of that region too.
Today this is where much of the premium fruit comes from. The combined vineyards now total over 100 hectares.
A quantum change occurred in 1990 when Sandalford Wines was purchased by Perth businessman Peter Prendiville. The Prendiville’s came with considerable experience in hospitality and tourism, and a significant injection of capital has seen a revamping of both properties and the creation of a state-of-the-art winery.
Wines today are released under six different labels, the pinnacle being the ultra-premium Prendiville Reserve range.
Sandalford 1840 Swan Valley 2025
Rose, RRP $35
The 1840 range of wines are made to showcase old Swan Valley vines. A refreshing wine for drinking slightly chilled this summer as an aperitif or accompanying salads and seafoods. Displays a lively pink colour, fresh and fruity aromas, rose petal. Light bodied, delicate, some texture added from lees contact, raspberry flavours with a crisp and dry finish.
Sandalford 1840 Swan Valley 2025 Chenin Blanc, RRP $35
A young wine drinking nicely now and with a big future. A fruit driven wine with aromas of guava, ripe banana, and a touch of spice. On the palate Granny Smith apple, citrus, a central core of acidity, and a minerally edge. Will take five-to-eight years to develop complex secondary fruit characters of quince, lanolin and honeysuckle, if you have the patience to wait that long.
Sandalford 1840 Swan Valley 2023
Grenache, RRP $40
Typical Swan Valley varietally expressive Grenache with its bright beetroot red colour, confectioned aroma with scented red fruits. Medium bodied with red currant and cherry kernel flavours. The 14.5% alcohol gives warmth to the palate. Tannins are gravelly. A rustic style to drink slightly pre-chilled this summer. May reward with three-to-four years cellaring.

Sandalford Margaret River 2023 Wilyabrup Cabernet Merlot, RRP $29
From the Margaret River range, their intentions being value for money wines. An easy drinking medium bodied wine. Combines the characteristic Margaret River Cabernet cassis with the mellow velvety suppleness of Merlot. The result is a harmonious balanced wine, enjoyable now and will develop over another few years. Certainly lives up to the value for money intention.
Sandalford Margaret River 2020 Estate Reserve Shiraz, RRP $59
The Estate Range are Wilyabrup wines made from selected fruit and given quality winemaking. This wine is still youthful with a five-to-eight-year future. Nose is spicy with nutmeg and blackberry. Palate shows fruit concentration with generous flavours of blackcurrant and mulberry. Savoury and spicy integrated with quality fine grained French oak. A very pleasing wine.
Sandalford Sandalera Rare Liqueur Verdelho, RRP $130 (500mls)
Words that immediately come to mind are sensational, captivating and delicious. This is what our Swan Valley was famous for – wonderful fortified wines. After the 1960s, drinkers transgressed to European-style table wines and fortified wine went into decline. Tasting this wine, one wonders why? The Verdelho grapes are left on vine to ripen fully. Fermentation is arrested with a neutral grape spirit retaining sweetness. Matured in old oak and cross blended over 30 years. The oldest component in this wine is from 1957. The result a luscious, unctuous wine, mahogany in colour, the aromas complex with raisins, walnut and roasted coffee. Flavours of toffee and caramel, with a nutty rancio. Palate length is amazing. If you have never experienced it, then it is well worth the price.
This page intentionally left blank

CONTACT
P: 1300 420 272
E: work@dyhs.org.au
Scan QR code for more details
Derbarl Yerrigan Health Service
General Practitioners
(Healthcare & Medical)
• Full Time
• $238k pa (pro rata) + Super & Medicare Incentive
• 12 days of personal leave per year
• Personalized professional development opportunities
• NAIDOC Day holiday

CONTACT
P: 1300 420 272
E: work@dyhs.org.au
Scan QR code for more details

BURSWOOD
CONTACT
Dr Ang:
P: 08 9472 9306
E: info@thewalkingp.com.au
Scan QR code for more details

CONTACT
Practice Manager:
Derbarl Yerrigan Health Service
Aboriginal Corporation
Chief Medical Officer
• Full Time
• Management (Healthcare & Medical)
• $330,000 to $350,000 pa (pro-rata) + Super

CONTACT
Practice Manager:
P: 08 6165 2444
E: reception@comogp.com.au
Scan QR code for to email

Opening for VR GP - F/time or P/time Full Private List Available
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
• FRACGP essential
• Up to 70% private billings
• Enjoy working for a doctor-owned, non-corporate, well support, and accredited practice.
• Billing Independence
• Immediate patient base
• Modern facilities
• Reputable practice
• Allied health onsite
• 75% of gross billings
• Accredited mixed-billing clinic
• Perfect for new VR GP’s
• Full/Part-time options.
Seeking a GP who can work regular full time or part time hours
• No after hours consulting
• Remuneration is negotiable.
• Well equipped treatment room.
• Pathology adjacent.
• Privately owned/Mixed billing.
• Friendly registered nurses and experienced administration support.
E: practicemanager@herdsmanmedical.com.au
Scan QR code for more details

• Mentor, supervise and support GPs, Registrars and medical staff CANNING VALE
GP to join our established mixed billing clinic in Canning Vale
• Established mixed billing clinic
• Guaranteed minimum of $200 per hour OR
• 65% of earnings whichever is greater
• Rostered on with 5 other GP’s
CONTACT
Odette Butler Practice Manager:
P: 0410 842 471
Email CV to: ahgpcvale@gmail.com
Scan QR code for more details
If you’re looking to join a professional, patient-centred team in a thriving practice, we’d love to hear from you.
CONTACT
Jasmine Brierty for more information:
P: 0457 905 538
E: Jasmine.Brierty@ipn.com.au
Scan QR code for more details





at 162 Cambridge St West Leederville (directly opposite SJOG Subiaco).
2 large fully fitted consults rooms (including sink and treatment bed) available and seperate treatment room available.
Each consult room $250 per half day session (includes use of waiting room and kitchen area). Reception/Admin support available for an additional fee.
For further information regarding availability or to arrange inspection please contact: reception@oswa.com.au/ (08) 9332 0066
































Fully fitted including sink Includes use of waiting area, staffroom/kitchen $250 per half day session
Reception/patient check-in support available for additional fee.
For further information or to arrange inspection please contact: admin@wocwexford.com.au