















































































Cotton swabs (Q-Tips) are still commonly used by many people to try to remove wax inside their ears, and to remove moisture from ears after bathing or swimming. But this routine can be dangerous and is also counter-productive. While you may see some residue on the cotton swab, inserting swabs can actually cause debris and ear wax to go further into the ear canal. Swabbing in your ears may affect your sense of hearing if the ear wax gets pushed further toward the eardrums.

Ear wax is a natural part of the body’s defenses – it is a protective lining that traps dirt and bacteria, helps prevent infection, and creates a protective coating on the delicate skin of the ear canal. Removing it using cotton swabs can stop the wax from doing its important job. Too much earwax can sometimes cause problems, but a healthcare provider can safely remove ear wax blockages if and when necessary.
In the fall and winter months, skin tends to lose moisture due to the colder, drier air and indoor heating, etc. This can lead to dryness, flakiness, and potential skin irritation. It’s important to adapt your skincare routine to manage these changes and protect your skin barrier.
Recommended steps include switching to richer moisturizers, using a more gentle cleanser, and running an air humidifier to alleviate the impacts of dry indoor air.

Cold weather can also trigger flare-ups of certain skin conditions, including:
•Eczema: If you are affected by eczema, the fall and winter months can be challenging. Keep your skin well moisturized and use fragrance-free, soothing products to minimize irritation. Consider applying an emollient-rich cream or ointment daily that forms a protective skin barrier.

•Rosacea: The colder air, coupled with rapid changes in temperature (moving between indoor heating and outdoor cold), can trigger rosacea flare-ups. Choose gentle, hydrating skincare products and avoid products with alcohol, which can irritate sensitive skin.
•Psoriasis: Dry, cold air and reduced sunlight can lead to increased skin irritation and potential flare-ups. Limit hot showers/baths, and protect your exposed skin outdoors by wearing a warm hat, scarf, and gloves.
Our subscriber base is growing and we have moved to a digital landscape for our subscribers. Please ensure you have provided an email and resubscribed to the magazine to keep receiving a digital copy going forward. You can do this on our website by scanning this QR code or by following this link: magazine/get-the-magazine.
Thank you for all the love you’ve shown this magazine over the last 15 years, and we are excited to continue sharing more stories with you through Canadian Skin


Fall/Winter 2025 • Volume 16 • Issue 1

ISSN 1923-0729
Publisher: Craig Kelman & Associates www.kelman.ca
All rights reserved. ©2025 Contents may not be reproduced.

Canadian Skin Patient Alliance: M72-851 Industrial Avenue, Ottawa, ON K1G 4L3 Toll Free: 1-877-505-CSPA (2772) • Email: info@canadianskin.ca
Canadian Publication Mail Sales Product Agreement No 40065546. Printed in Canada.

To subscribe to this complimentary magazine, visit: https://canadianskin.ca/magazine/get-the-magazine

By Dr. Raed Alhusayen and Dr. Dimitra Bednar
AQWhat are varicose veins? Can they be treated?
You may notice some visible or bumpy veins on your legs at any time of year. Varicose veins are due to poor blood return to the heart. Risk factors include genetics, age, hormones, pregnancy, prolonged standing, and obesity. To prevent their development or worsening, maintain a healthy active lifestyle and consider doing calf raises if you stand for prolonged periods. Compression stockings facilitate blood return and may improve leg swelling and varicosities. Low-pressure stockings (10–20 mmHg) may be purchased over the counter, but higher-pressure stockings require a prescription and particular measurements of your foot and leg. Visit your primary care provider to learn more. Before wearing stockings, you may need imaging to test blood flow in the legs. Further intervention is considered if there is significant pain, heaviness, or cramping with activity. Those additional procedures are cosmetic and not covered by provincial health insurance. Options include sclerotherapy (careful injection of a destructive substance into the vein), surgical removal, or laser destruction. These procedures are performed by dermatologists, plastic or vascular surgeons, and some primary care providers. Request a referral to review your case and discuss treatments including procedure logistics, expected benefits, and risks.


AQIs there such a thing as a “healthy tan”?

Among certain cultures since the beginning of civilization, bronzed skin was considered “healthy.” Unfortunately, we were misled. Repeated intermittent or chronic sun exposure increases the risk of skin cancers including melanoma, basal cell carcinoma, squamous cell carcinoma, and accelerated skin aging. There is no such thing as a “healthy tan” – unless you have a medical condition that responds to light or are diagnosed with a rare sun sensitivity. Select patients with conditions such as eczema, psoriasis, or polymorphous light eruption may benefit from medically supervised light therapy. Otherwise, consider sun-tanning (either outdoors or in a tanning booth) unsafe. Self-tanners applied to the skin are available over the counter and can help achieve a bronzed glow without the skin damage. They contain chemicals that tint skin without sun exposure. Practice caution: self-tanners do not provide sun protection and can be irritating. Always read the label and test a small area of skin first.
Have a question? Send it to info@canadianskin.ca.
Dr. Raed Alhusayen is a consultant dermatologist at Sunnybrook Health Sciences Centre in Toronto, Ontario. Dr. Dimitra Bednar is a dermatology resident at the University of Toronto in Ontario.



By Bianca Te and Valerie C. Doyon
Introduction
Atopic dermatitis (AD), psoriasis, and hidradenitis suppurativa (HS) are chronic inflammatory skin disorders, each well-known for their hallmark features – AD by persistent itch (AAAAI/ACAAI, 2024), psoriasis by raised pink plaques with silvery scale (Griffiths et al., 2021), and HS by painful nodules or abscesses in skin folds. Much deeper than meets the eye, the impact of these skin conditions extends far beyond the skin, as each condition is associated with several comorbidities spanning both physical and mental health (Kovitwanichkanont et al., 2020; Silverberg et al., 2018). Recognizing these associations is crucial for individuals to receive optimal care of the skin as well as their global health, including proactive screening and comprehensive management.
Atopic comorbidities
“Atopy” refers to a genetic tendency to develop allergic conditions.

In addition to AD, other atopic conditions include food allergies, asthma, allergic rhinitis, and eosinophilic oesophagitis (Choi et al., 2025; Tang & Li, 2024). AD is often the first clinical manifestation of what is known as the “atopic march,” a sequential progression whereby AD is followed by the development of food allergies, asthma, then allergic rhinitis (Choi et al., 2025; Tang & Li, 2024). The atopic march might begin with AD because the impaired skin barrier exposes the skin’s immune cells to allergens, leading to sensitization (Tang & Li, 2024). Consequently, emerging evidence suggests that more intensive treatment of AD in its early stages (infants) – with topical corticosteroids or systemic therapy –may reduce the risk of developing other atopic conditions (Geba et al., 2023; Yamamoto-Hanada et al., 2024).
Although the atopic march is sometimes observed, not all patients with AD progress to develop other atopic conditions, and not all patients with food allergy, asthma, or allergic rhinitis, and eosinophilic oesophagitis have a preceding

diagnosis of AD. Nevertheless, it is still valuable to proactively monitor for the development of other atopic conditions in patients with AD, especially in children and those with a family history of atopy (Choi et al., 2025;). For instance, caregivers of children with AD can keep watch for immediate food reactions (e.g., hives, lip swelling) or signs of asthma (e.g., coughing, wheezing).
Several other skin conditions are also seen in patients with AD. The skin barrier dysfunction characteristic of AD is thought to stem from genetic mutations affecting a key structural skin protein (Fenner & Silverberg, 2018). Ichthyosis vulgaris – an inherited condition that causes dry, scaly skin –and keratosis pilaris – a condition that presents like small red goosebumps –are both associated with abnormalities in this same protein (Fenner & Silverberg, 2018). As a result, these conditions often co-occur with AD.
Beyond an impaired skin barrier, mechanical trauma from scratching


in AD also results in an increased risk for secondary skin infections (AAAAI/ACAAI, 2024; Roh et al., 2022; Thyssen et al., 2023). These infections are often bacterial, leading to impetigo, or viral infections such as eczema herpeticum (Roh et al., 2022).
Lastly, AD is associated with immune system dysregulation, which is thought to contribute to its link with certain autoimmune skin conditions. These include alopecia areata, characterized by patchy hair loss due to immunemediated attacks on hair follicles, and vitiligo, which presents as depigmented patches resulting from autoimmune destruction of pigment-producing cells (Fenner & Silverberg, 2018; Roh et al., 2022; Thyssen et al., 2023).
There are several well-established psychosocial comorbidities with AD. Notably, the risk of depression and anxiety is up to three times higher in adults with AD, and 1.5 times higher in children and adolescents (LeBovidge & Schneider, 2025; Thyssen et al., 2023). As early as age four, patients with AD

are more likely to develop internalizing symptoms such as excessive worrying, low mood, or poor self-confidence (LeBovidge & Schneider, 2025).
Moreover, both children and adults with AD have an increased risk of suicidal ideation (LeBovidge & Schneider, 2025; Thyssen et al., 2023).

Research suggests that the link between atopic dermatitis (AD) and mental health is shaped by the interplay of poorly controlled symptoms, sleep disturbance, and psychosocial stressors (LeBovidge & Schneider, 2025). Chronic itch can significantly impair quality of life and heighten stress. Conversely, acute stress has been shown to increase spontaneous scratching in patients with AD, which can contribute to AD exacerbations (Mochizuki et al., 2019). Sleep disturbance due to persistent itch affects the majority of patients with AD, which can further impair mood and behaviour. Additionally, patients may withdraw from school, work, social events, or recreational activities – not only during flares, but also due to stigma and reduced self-esteem.

AD is also associated with behavioral psychiatric conditions, including attention deficit hyperactivity disorder and autism spectrum disorder (Cheung et al., 2024). Although the exact nature of this relationship remains unclear, research suggests it may be driven by shared genetic factors and underlying inflammatory pathways.
In addition to the previously discussed comorbidities, atopic dermatitis (AD) has been linked to a broad range of other conditions. For example, eye problems, such as allergic conjunctivitis, are common and can lead to chronic rubbing around the eyes (Thyssen et al., 2023).
AD is also associated with systemic autoimmune diseases, such as celiac disease, lupus, and inflammatory bowel disease (Thyssen et al., 2023). These associations further emphasize the importance of monitoring for comorbidities and reinforce the benefits of interdisciplinary care in managing severe AD.

Psoriatic arthritis





Psoriatic arthritis (PsA) is the most common comorbidity of psoriasis, affecting 10–40% of patients (Griffiths et al., 2021). Psoriasis precedes PsA in 85% of patients, with the onset of PsA developing approximately 7–10 years after the onset of psoriasis (Elman et al., 2025; Griffiths et al., 2021). PsA presents as swollen, red, painful joints. It affects most often the finger joints, elbows/knees, or the back. Contrary to regular “wear and tear” arthritis, PsA also presents with extended periods of joint stiffness in the morning or after inactivity. PsA can also manifest itself as episodes of a finger swelling up like a sausage (also known as dactylitis) or as inflammation of tendons such as in the Achilles (Elman et al., 2025; Griffiths et al., 2021). Regularly screening for these symptoms is valuable as the outcomes are better the sooner it is diagnosed and treated (Elman et al., 2025). Management of PsA is often interdisciplinary, involving both dermatology and rheumatology (Elman et al., 2025).



Individuals with psoriasis are up to 50% more likely to develop cardiovascular disease (CVD) compared to those without psoriasis (Garshick et al., 2021). This risk of developing CVD is higher in those with more severe psoriasis and in patients who also have PsA (Garshick et al., 2021; Hu & Lan, 2017). The underlying mechanism is thought to be in part due to common inflammatory pathways between psoriasis and CVD (Hu & Lan, 2017). The immune cells that are up-regulated in patients with psoriasis are linked to both vascular inflammation and atherosclerosis













“ Regular follow-up visits and a proactive approach to screening can help detect comorbidities early, allowing for timely interventions and more personalized care strategies that optimize long-term health outcomes.”


development (Garshick et al., 2021). As a result, patients with psoriasis are at an increased risk for serious vascular events such as heart attack and stroke (Hu & Lan, 2017). For this reason, it is important for these patients to adopt lifestyle behaviours to mitigate their risk, such as exercising regularly, eating healthy, and refraining from smoking (Egeberg & Skov, 2016).

Psoriasis is also associated with several risk factors for developing CVD, including high blood pressure, high cholesterol, diabetes and obesity (Hu & Lan, 2017). Interestingly, studies suggest the relationship may go both ways, as having high blood pressure or high cholesterol may also increase someone’s risk of later developing psoriasis (Hu & Lan, 2017). Together, these conditions make up what is known as metabolic syndrome, which is more prevalent in individuals with psoriasis – especially those with more severe skin involvement. Metabolic syndrome significantly increases an individual’s risk for cardiovascular events (Hu & Lan, 2017). Adequate systemic (oral/injectable) treatment of moderate to severe psoriasis has been shown to decrease the risk of CVD. For example, studies show that systemic treatments for psoriasis such as methotrexate can lower an individual’s risk for subsequent cardiovascular events (Hu & Lan, 2017). Conversely, adequate treatment of metabolic comorbidities may also improve psoriasis. For example, in diabetic patients, optimal control of blood sugar levels with diabetes medications has been shown to improve skin psoriasis (Hu & Lan, 2017).









in their lives (Hedemann et al., 2022). Effective management of psoriasis symptoms may improve mood, as studies show that distressing symptoms like itch can worsen depression (Hedemann et al., 2022). Anxiety is another commonly reported mental health comorbidity, affecting up to half of patients (Hedemann et al., 2022). Moreover, other psychiatric conditions such as schizophrenia and thoughts of suicide are seen more frequently in those with psoriasis than in the general population (Hedemann et al., 2022).



In addition to physical comorbidities, psoriasis is associated with several psychiatric comorbidities. Individuals with psoriasis are 1.5 times more likely to develop symptoms of depression, with up to 36% of patients having experienced depression at some point



The relationship between psoriasis and these psychiatric comorbidities may be driven by both physiological and psychosocial factors. Research suggests that psoriasis shares inflammatory pathways with both depression and anxiety, which may explain their association (Hedemann et al., 2022; Mrowietz et al., 2023). However, the mental health burden of living with a visible and socially stigmatized skin condition likely also contributes to the development or worsening of mental health (Hedemann et al., 2022).

Beyond what is described above, psoriasis is also associated with gastrointestinal immune-mediated conditions including Crohn’s disease, ulcerative colitis, and celiac disease (Kovitwanichkanont et al., 2020). Moreover, research suggests that patients with moderate to severe psoriasis may also be at increased risk for developing non-alcoholic fatty liver disease and chronic kidney disease (Kovitwanichkanont et al., 2020). Although several comorbidities have been linked with psoriasis, it’s important to remember that not all patients will develop these diseases. Regular follow-up visits and a proactive approach to screening can help detect comorbidities early, allowing for timely interventions and more personalized care strategies that optimize long-term health outcomes.



















PART 3: Comorbidities of hidradenitis suppurativa
Cardiovascular disease and risk factors
Individuals who have HS are at an increased risk of developing cardiovascular disease (CVD), when compared to patients without HS (Tzellos & Zouboulis, 2022; Rohan et al., 2025). Research has shown that patients with HS may be twice as likely to experience serious cardiovascular events, such as heart attack and stroke (Krajewski et al., 2024; Rohan et al., 2025). Interestingly, this risk is higher than in patients with psoriasis, when comparing those of similar age, weight, and overall health (Rohan et al., 2025).
syndrome, encompassing pyoderma gangrenosum, which often presents as ulcers on the lower leg, acne, and HS (Maronese et al., 2024). Other examples are PAPASH syndrome, which further includes pyogenic arthritis, and PsAPASH syndrome, which further includes psoriatic arthritis (Maronese et al., 2024).












In addition to cardiovascular disease itself, patients with HS are also more likely to have risk factors for cardiovascular disease, such as high blood pressure, high cholesterol, diabetes and obesity (Krajewski et al., 2024). Among these, there is a strong link between obesity and HS, with research suggesting there is a two-way relationship between the two – patients with HS are more likely to be overweight, and having higher body weight can make HS symptoms worse (Wang et al., 2025). This relationship was not observed between HS and other components of metabolic syndrome, such as high blood pressure or high cholesterol, which emphasizes the importance of weight control in managing HS (Wang et al., 2025).

Dermatologic comorbidities

Psychosocial comorbidities
Patients with HS are about twice as likely to have mental health challenges, compared to those without HS (Folkmann et al., 2025). In particular, depression is more common, and tends to occur more often in those with more severe HS (Folkmann et al., 2025). Other associated mental health conditions include anxiety and bipolar disorder (Folkmann et al., 2025).




HS is a part of what is known as the “follicular occlusion tetrad.” The other conditions in this group include acne conglobata, a severe form of deep and painful acne; dissecting cellulitis of the scalp, which are scarring nodules on the scalp; and pilonidal sinus, which are deep hair-filled cysts commonly near the tailbone (Jastrząb et al., 2023). All of these conditions result from blocked hair follicles and inflammation, leading to the formation of deep, interconnecting fluid-filled pockets (Jastrząb et al., 2023).
The Canadian Skin Patient Alliance (CSPA) is constantly striving to make a meaningful impact on the lives of those we serve. By becoming a monthly donor, you will be joining a special group of dedicated individuals who provide us with the consistent support we need to plan and execute our programs effectively. Your monthly contribution, no matter the size, will enable us to maintain and expand our initiatives, ensuring that our community continues to benefit from the vital services we offer.
Why should you consider becoming a monthly donor?
• Sustained impact: Monthly donations provide us with a predictable source of income, allowing us to focus more on our mission and less on fundraising efforts.
• Efficiency: Your recurring donation minimizes administrative costs, ensuring that the majority of your contribution goes directly into our programs.
• Exclusive updates: As a monthly donor, you will receive regular updates on the impact of your contribution, allowing you to witness firsthand the change you are making.

HS can have a profound impact on quality of life. In addition to the uncomfortable symptoms of HS, many patients also struggle with lower selfesteem due to the appearance of the skin and social stigma that can come with it (Nguyen et al., 2021). HS can also contribute to sleep disturbance and sexual difficulties (Montero-Vilchez et al., 2021; Nguyen et al., 2021). Lastly, HS can affect one’s career, with studies showing that HS can impact work productivity and needing to take time off work (Tzellos & Zouboulis, 2022).
Other comorbidities


HS can also present as a component in an autoinflammatory syndrome. For example, there is PASH





Research suggests that HS is also associated with several other conditions. For example, female patients with HS are twice as likely to develop polycystic ovarian syndrome (PCOS), a hormonal disorder characterized by irregular periods, higher male hormones such as testosterone, and cysts on the ovaries (Garg et al., 2018). Hormonal treatments, such as birth control pills, can simultaneously manage symptoms




Become a monthly donor today, at https://canadianskin.ca/getinvolved/donate.


of PCOS and HS, showing the role of hormones in the development of HS (Alikhan et al., 2018).
HS is also associated with inflammatory bowel disease (IBD), particularly Crohn’s disease (Deckers et al., 2017). In fact, research suggests that IBD is about 4 to 8 times more common in people with HS, compared to those without it (Deckers et al., 2017). This association highlights the role of inflammation in the development of each of these conditions.
Conclusion
In summary, AD, psoriasis, and HS are linked with a broad spectrum of conditions that extend far beyond the skin. Decades of research have led to the discovery of the inflammatory pathways that underlies these three skin conditions, which contributes to their systemic effects on inner organs. Understanding the common comorbidities for each of these conditions empowers both patients and physicians to take a more proactive and holistic approach to care. By recognizing and addressing associated conditions, we can not only improve the skin condition, but the individual’s health as a whole.
Canadian Hidradenitis Suppurativa Foundations: Part II: Topical, intralesional, and systemic medical management. Journal of the American Academy of Dermatology, 81(1), 91–101. https://doi. org/10.1016/j.jaad.2019.02.068
3. Cheng, Y., Lu, J. W., Wang, J. H., Loh, C. H., & Chen, T. L. (2024). Associations of Atopic Dermatitis with Attention Deficit/ Hyperactivity Disorder and Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Dermatology (Basel, Switzerland), 240(1), 13–25. https://doi.org/10.1159/000533366
4. Choi, U. E., Deng, J., Parthasarathy, V., Liao, V., D’Amiano, A., Taylor, M., Bordeaux, Z. A., Kambala, A., Cornman, H. L., Canner, J. K., Drucker, A. M., & Kwatra, S. G. (2025). Risk factors and temporal associations of progression of the atopic march in children with early-onset atopic dermatitis. Journal of the American Academy of Dermatology 92(4), 732–740. https://doi. org/10.1016/j.jaad.2024.10.107
5. Deckers, I. E., Benhadou, F., Koldijk, M. J., Del Marmol, V., Horváth, B., Boer, J., van der Zee, H. H., & Prens, E. P. (2017). Inflammatory bowel disease is associated with hidradenitis suppurativa: Results from a multicenter cross-sectional study. Journal of the American Academy of Dermatology 76(1), 49–53. https://doi.org/10.1016/j.jaad.2016.08.031
6. Egeberg, A., & Skov, L. (2016). Management of cardiovascular disease in patients with psoriasis. Expert opinion on pharmacotherapy, 17(11), 1509–1516. https://doi.org/10.1080/146 56566.2016.1190336
7. Elman, S. A., Perez-Chada, L. M., Armstrong, A., Gottlieb, A. B., & Merola, J. F. (2025). Psoriatic arthritis: A comprehensive review for the dermatologist-Part II: Screening and management. Journal of the American Academy of Dermatology 92(5), 985–998. https:// doi.org/10.1016/j.jaad.2024.03.059
8. Fenner, J., & Silverberg, N. B. (2018). Skin diseases associated with atopic dermatitis. Clinics in dermatology 36(5), 631–640. https:// doi.org/10.1016/j.clindermatol.2018.05.004
9. Folkmann, C. L., Pinborg, E. H., Iversen, M., Rønnstad, A. T. M., Holgersen, N., Nielsen, M. L., Egeberg, A., Thyssen, J. P., Thomsen, S. F., & Christensen, M. O. (2025). The Association of Hidradenitis Suppurativa and Psychiatric Disease: A Systematic Review and Meta-analysis. The British journal of dermatology, ljaf151. Advance online publication. https://doi.org/10.1093/bjd/ljaf151
10. Garg, A., Neuren, E., & Strunk, A. (2018). Hidradenitis Suppurativa Is Associated with Polycystic Ovary Syndrome: A PopulationBased Analysis in the United States. The Journal of investigative dermatology, 138(6), 1288–1292. https://doi.org/10.1016/j. jid.2018.01.009
11. Garshick, M. S., Ward, N. L., Krueger, J. G., & Berger, J. S. (2021). Cardiovascular Risk in Patients With Psoriasis: JACC Review Topic of the Week. Journal of the American College of Cardiology 77(13), 1670–1680. https://doi.org/10.1016/j.jacc.2021.02.009

12. Geba, G. P., Li, D., Xu, M., Mohammadi, K., Attre, R., Ardeleanu, M., & Musser, B. (2023). Attenuating the atopic march: Meta-analysis of the dupilumab atopic dermatitis database for incident allergic events. The Journal of allergy and clinical immunology, 151(3), 756–766. https://doi.org/10.1016/j.jaci.2022.08.026





References


20. Maronese, C. A., Moltrasio, C., & Marzano, A. V. (2024). Hidradenitis Suppurativa-Related Autoinflammatory Syndromes: An Updated Review on the Clinics, Genetics, and Treatment of Pyoderma gangrenosum, Acne and Suppurative Hidradenitis (PASH), Pyogenic Arthritis, Pyoderma gangrenosum, Acne and Suppurative Hidradenitis (PAPASH), Synovitis, Acne, Pustulosis, Hyperostosis and Osteitis (SAPHO), and Rarer Forms. Dermatologic clinics, 42(2), 247–265. https://doi.org/10.1016/j.det.2023.12.004
21. Mochizuki H, Lavery MJ, Nattkemper LA, et al. Impact of acute stress on itch sensation and scratching behaviour in patients with atopic dermatitis and healthy controls. Br J Dermatol 2019;180(4):821-827. doi:10.1111/bjd.16921
22. Montero-Vilchez, T., Diaz-Calvillo, P., Rodriguez-Pozo, J. A., Cuenca-Barrales, C., Martinez-Lopez, A., Arias-Santiago, S., & Molina-Leyva, A. (2021). The Burden of Hidradenitis Suppurativa Signs and Symptoms in Quality of Life: Systematic Review and Meta-Analysis. International journal of environmental research and public health 18(13), 6709. https://doi.org/10.3390/ijerph18136709
23. Mrowietz, U., Sümbül, M., & Gerdes, S. (2023). Depression, a major comorbidity of psoriatic disease, is caused by metabolic inflammation. Journal of the European Academy of Dermatology and Venereology : JEADV 37(9), 1731–1738. https://doi. org/10.1111/jdv.19192
24. Nguyen, T. V., Damiani, G., Orenstein, L. A. V., Hamzavi, I., & Jemec, G. B. (2021). Hidradenitis suppurativa: an update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. Journal of the European Academy of Dermatology and Venereology : JEADV 35(1), 50–61. https://doi.org/10.1111/jdv.16677
25. Roh, Y. S., Huang, A. H., Sutaria, N., Choi, U., Wongvibulsin, S., Choi, J., Bordeaux, Z. A., Parthasarathy, V., Deng, J., Patel, D. P., Canner, J. K., Grossberg, A. L., & Kwatra, S. G. (2022). Real-world comorbidities of atopic dermatitis in the US adult ambulatory population. Journal of the American Academy of Dermatology, 86(4), 835–845. https://doi.org/10.1016/j.jaad.2021.11.014


1. AAAAI/ACAAI JTF Atopic Dermatitis Guideline Panel, Chu, D. K., Schneider, L., Asiniwasis, R. N., Boguniewicz, M., De Benedetto, A., Ellison, K., Frazier, W. T., Greenhawt, M., Huynh, J., Kim, E., LeBovidge, J., Lind, M. L., Lio, P., Martin, S. A., O’Brien, M., Ong, P. Y., Silverberg, J. I., Spergel, J. M., Wang, J., … Chu, D. K. (2024). Atopic dermatitis (eczema) guidelines: 2023 American Academy of Allergy, Asthma and Immunology/American College of Allergy, Asthma and Immunology Joint Task Force on Practice Parameters GRADE - and Institute of Medicine-based recommendations. Annals of allergy, asthma & immunology : o cial publication of the American College of Allergy, Asthma, & Immunology 132(3), 274–312. https://doi.org/10.1016/j.anai.2023.11.009


2. Alikhan, A., Sayed, C., Alavi, A., Alhusayen, R., Brassard, A., Burkhart, C., Crowell, K., Eisen, D. B., Gottlieb, A. B., Hamzavi, I., Hazen, P. G., Jaleel, T., Kimball, A. B., Kirby, J., Lowes, M. A., Micheletti, R., Miller, A., Naik, H. B., Orgill, D., & Poulin, Y. (2019). North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and


13. Gri ths, C. E. M., Armstrong, A. W., Gudjonsson, J. E., & Barker, J. N. W. N. (2021). Psoriasis. Lancet (London, England) 397(10281), 1301–1315. https://doi.org/10.1016/S0140-6736(20)32549-6
14. Hedemann, T. L., Liu, X., Kang, C. N., & Husain, M. I. (2022). Associations between psoriasis and mental illness: an update for clinicians. General hospital psychiatry, 75, 30–37. https://doi. org/10.1016/j.genhosppsych.2022.01.006
15. Hu, S. C., & Lan, C. E. (2017). Psoriasis and Cardiovascular Comorbidities: Focusing on Severe Vascular Events, Cardiovascular Risk Factors and Implications for Treatment. International journal of molecular sciences 18(10), 2211. https:// doi.org/10.3390/ijms18102211
26. Rohan, T. Z., Hafer, R., Duong, T., Dasgupta, R., & Yang, S. (2025). Hidradenitis Suppurativa Is Associated with an Increased Risk of Adverse Cardiac Events and All-Cause Mortality. Journal of clinical medicine, 14(4), 1110. https://doi.org/10.3390/jcm14041110
27. Silverberg, J. I., Gelfand, J. M., Margolis, D. J., Boguniewicz, M., Fonacier, L., Grayson, M. H., Simpson, E. L., Ong, P. Y., & Chiesa Fuxench, Z. C. (2018). Patient burden and quality of life in atopic dermatitis in US adults: A population-based cross-sectional study. Annals of allergy, asthma & immunology : o cial publication of the American College of Allergy, Asthma, & Immunology, 121(3), 340–347. https://doi.org/10.1016/j.anai.2018.07.006

28. Tang, X., & Li, M. (2024). The role of the skin in the atopic march. International immunology, 36(11), 567–577. https://doi. org/10.1093/intimm/dxae053
29. Thyssen, J. P., Halling, A. S., Schmid-Grendelmeier, P., GuttmanYassky, E., & Silverberg, J. I. (2023). Comorbidities of atopic dermatitis-what does the evidence say? The Journal of allergy and clinical immunology 151(5), 1155–1162. https://doi. org/10.1016/j.jaci.2022.12.002
30. Tzellos, T., & Zouboulis, C. C. (2022). Which hidradenitis suppurativa comorbidities should I take into account? Experimental dermatology 31, 29-32.

16. Jastrząb, B., Szepietowski, J. C., & Matusiak, Ł. (2023). Hidradenitis suppurativa and follicular occlusion syndrome: Where is the pathogenetic link?. Clinics in dermatology, 41(5), 576–583. https://doi.org/10.1016/j.clindermatol.2023.08.021
17. Kovitwanichkanont, T., Chong, A. H., & Foley, P. (2020). Beyond skin deep: addressing comorbidities in psoriasis. The Medical journal of Australia 212(11), 528–534. https://doi.org/10.5694/mja2.50591


18. Krajewski, P. K., Matusiak, Ł., Ständer, S., Thaçi, D., Szepietowski, J. C., & Zirpel, H. (2024). Risk of cardiovascular disorders in hidradenitis suppurativa patients: A large-scale, propensitymatched global retrospective cohort study. International journal of dermatology 63(6), 799–805. https://doi.org/10.1111/ijd.17186

31. Wang, H., Wu, B., Luo, M., Han, Y., Chen, J., Liu, J., Lin, L., & Xiao, X. (2025). Association of hidradenitis suppurativa (HS) with waist circumference: A bidirectional two-sample Mendelian randomization study of HS with metabolic syndrome. The Journal of dermatology, 52(1), 155–158. https://doi.org/10.1111/1346-8138.17436
19. LeBovidge, J. S., & Schneider, L. C. (2025). Depression and anxiety in patients with atopic dermatitis: Recognizing and addressing mental health burden. Annals of allergy, asthma & immunology: o cial publication of the American College of Allergy, Asthma, & Immunology, S1081-1206(25)00094-8. Advance online publication. https://doi.org/10.1016/j.anai.2025.02.017







32. Yamamoto-Hanada, K., Kobayashi, T., Mikami, M., Williams, H. C., Saito, H., Saito-Abe, M., Sato, M., Irahara, M., Miyaji, Y., Ishikawa, F., Tsuchiya, K., Tamagawa-Mineoka, R., Takaoka, Y., Takemura, Y., Sato, S., Wakiguchi, H., Hoshi, M., Natsume, O., Yamaide, F., Seike, M., … PACI Study Collaborators (2023). Enhanced early skin treatment for atopic dermatitis in infants reduces food allergy. The Journal of allergy and clinical immunology 152(1), 126–135. https://doi.org/10.1016/j.jaci.2023.03.008
Bianca Te, BSc, is a medical student at the University of British Columbia in Vancouver.


Valerie C. Doyon, BSc, MD, is a dermatology resident at the Université de Montréal.







BY SIMAL QURESHI (PGY1)
What is urticaria?
Urticaria, commonly known as ‘hives,’ is an inflammatory skin condition that affects up to one in every five people at some stage in their life.1 It presents with weals – a superficial swelling of the skin that may be skin-coloured or red in appearance.6 Weals are often itchy and may range in size between one millimetre to several centimetres.1 Urticaria may also occur concurrently with angioedema – a deeper swelling of the skin or mucous membrane, often seen in allergic reactions.1,6 Both children and adults can experience urticaria, although certain forms, such as chronic urticaria, are more common in adults.6
Are there different kinds of urticaria?
Urticaria is generally divided into two categories: acute and chronic. Acute urticaria involves symptoms lasting less than six weeks, usually resolving within hours to days. Chronic urticaria involves symptoms that persist longer than six weeks, with frequent or daily weals2. Acute urticaria may be due to infections, medications, foods, or inhaled allergens.2 Chronic urticaria, on the other hand, may be spontaneous or inducible, and not necessarily due to any specific cause (also known as idiopathic).2 Some inducible forms of urticaria can be triggered by specific factors like heat, cold, vibration, and contact with liquids, to name a few.
A close-up look at Chronic Spontaneous Urticaria
Chronic Spontaneous Urticaria (CSU) is one of the forms of chronic urticaria, next to Inducible Urticaria. It more commonly affects women, especially those between 30 to 50 years-old.4 As mentioned earlier, the exact cause of CSU is unknown, but research suggests it may be autoimmune. In over half of CSU cases, the immune system produces IgE or IgG antibodies that activate mast cells – the same cells



responsible for allergic reactions. Weals may be aggravated by viral or bacterial infections, heat, tight clothing, stress, or certain medications.6 CSU has also been associated with connective tissue disorders, such as systemic lupus erythematosus, as well as other conditions including pregnancy and hyperthyroidism.5 People with CSU may feel a variety of symptoms beyond skin changes including joint pain, headache, fatigue, flushing, gastrointestinal symptoms, and shortness of breath.5 CSU can persist for years or even decades, significantly impacting patients’ quality of life.3 This condition can cause physical, mental, and social distress, potentially resulting in patients missing school, work, or having to experience frequent healthcare visits.3
How can we diagnose and treat urticaria?
There is no single diagnostic test to diagnose urticaria. It is generally diagnosed based on clinical history and presentation, particularly when weals last less than 24 hours, occurring with or without angioedema.6 Physicians will perform a thorough physical exam and take a detailed history, asking about medication or family history to identify any potential triggers.6 For instances of acute urticaria, skin prick testing may take place if a food or drug allergy is suspected.6 For individuals in which CSU is suspected, Complete
Blood Count (CBC) or C-reactive Protein (CRP) investigations may be ordered to investigate inflammatory conditions.6 The first-line treatment for both adults and children experiencing urticaria is a non-sedating, second-generation antihistamine, such as cetirizine or loratadine.2 For CSU patients, they may take up to 40 mg of Certirizine daily for four weeks, under guidance of a physician.6 For patients that are antihistamine-resistant, there is strong evidence supporting the use of omalizumab, a humanized monoclonal anti-IgE antibody, or cyclosporine, an immunosuppressive agent.3 In such persistent cases of urticaria, patients should also be referred to a dermatologist or allergist to help guide further treatment options.6
References
1. Deacock, S. J. (2008). An approach to the patient with urticaria. Clinical & Experimental Immunology 153(2), 151-161.
2. Kolkhir, P., Giménez-Arnau, A. M., Kulthanan, K., Peter, J., Metz, M., & Maurer, M. (2022). Urticaria. Nature Reviews Disease Primers 8(1), 61.
3. Wedi, B., Wieczorek, D., Raap, U., & Kapp, A. (2014). Urticaria. JDDG: Journal der Deutschen Dermatologischen Gesellschaft 12(11), 997-1009.
4. Kolkhir, P., Bonnekoh, H., Metz, M., & Maurer, M. (2024). Chronic spontaneous urticaria: A review. Jama
5. Allergy UK. (2024, July). Acute, chronic and physical urticaria: A brief guide for healthcare professionals. Allergy UK. Retrieved from https://www.allergyuk.org/wp-content/uploads/2024/07/ HCP-CSUeBook2024.pdf
6. Oakley, A. (Ed.). (2021, April). Urticaria – An overview. DermNet NZ. From https://www.dermnetnz.org/topics/urticaria-an-overview/
Simal Qureshi is a medical student in the Class of 2025 at Memorial University.




The






Canadian Skin Patient Alliance (CSPA)
is proud to recognize Dr. Julien Ringuet as our 2024 Dermatologist of the Year!
Dr. Ringuet is a passionate clinician, educator, and researcher whose work has already left a meaningful imprint on the field of dermatology. Based at the Centre de Recherche Dermatologique de Québec and actively involved in teaching at McGill University’s MUHC, Dr. Ringuet balances research innovation with a profoundly human approach to care. For him, the heart of medicine lies in listening to patients and involving them in every step of their therapeutic journey.
“Words are never sufficient to express appreciation for these kinds of nominations,” says Dr. Ringuet. “Being acknowledged by peers and colleagues is always an honour, but when it comes from patients, it means everything. It means we listened. It means we helped them feel seen and heard. That’s the real reward.”
His path to dermatology was paved by an appreciation for the field’s complexity and diversity –from intricate internal medicine and cutting-edge therapeutic



algorithms to surgical precision. It’s this dynamic mix that continues to fuel his enthusiasm. “What an avenue!” he remarks with genuine excitement. “The advancements in inflammatory disease treatments over the past 20 years have been incredible, and I’m so energized by what lies ahead.”
Dr. Ringuet’s clinical and research focus includes vitiligo, atopic dermatitis, prurigo nodularis, alopecia areata, and psoriasis; conditions that have historically posed enormous challenges for both patients and clinicians. With the advent of new therapies, from innovative topicals to biologics and targeted molecules, he’s witnessed firsthand the transformational impact of modern medicine.
“The highlight for me,” he shares, “is that culminating moment when a patient, once burdened by a disease we struggled to control, now walks into the clinic smiling, confident, and thriving. It’s the sum of years of development, collaboration, and trust.”
Looking ahead, Dr. Ringuet and his team remain at the forefront of dermatological research in Quebec, determined to bring even more effective, accessible treatments to patients across the province. At the same time, he continues to invest in the next generation of dermatologists, helping shape their clinical expertise while reinforcing the importance of empathy and shared decision-making.



The CSPA has been truly fortunate to collaborate with Dr. Ringuet on the Canadian Skin magazine and other educational resources and deeply values his commitment to patient-centered care, his leadership in clinical research, and his contributions to improving skin health in Canada. His compassion, innovation, and tireless advocacy are a testament to the very best in dermatological care.
Thank you, Dr. Ringuet, for your outstanding work, your unwavering commitment, and the lasting impact you’ve made, and continue to make, on the lives of so many.













By Mahan Maazi and Dr. Khalad Maliyar


What is it?
Seborrheic dermatitis (SD) causes redness, greasy scaling, flaking, and itchiness, typically in oil-rich areas like the scalp, sides of the nose, eyebrows, ears, chest, back, and genitals. In infants, it’s known as “cradle cap” and usually resolves within the first year. In adults, however, SD often lingers with unpredictable flare-ups that can last for years.¹
While not dangerous, its visibility can feel overwhelming. Flakes on clothing, red patches on the face, and persistent itch are hard to ignore, especially in social or professional situations. For many, SD is more than a skin issue –it’s a daily challenge that impacts confidence and well-being.²
What causes it?
Our understanding of SD has come a long way. Experts now recognize it as primarily an inflammatory condition, triggered by multiple factors.
At its core is a yeast called Malassezia, which normally lives on healthy skin. In SD, this yeast overgrows in oily areas, breaking down skin oils and releasing irritating by-products like free fatty acids. These trigger an immune
response, leading to inflammation and the familiar redness, scaling, and itch.
But Malassezia isn’t the only factor. Genetics, cold and dry weather, stress, and certain health conditions – such as Parkinson’s disease, HIV, and mood disorders – can also make the skin more reactive and prone to flare-ups.³
Understanding this inflammatory cycle is crucial. It shows why treatment needs to go beyond controlling yeast to also calming the immune response and easing symptoms like redness, scaling, and itch.
How common is it?
SD is more common than many realize. It affects approximately 5% of the global population. Meanwhile, the milder, noninflammatory form – familiar to many as everyday dandruff – can affect up to 50% of people worldwide.⁴
Risk factors
• Age (first three months of life, and fourth decade of life)
• Parkinson’s Disease
• Cerebrovascular accidents
• HIV
• Spina bifida
• Mood disorders
• Stress
• Immunodeficiency
• Low humidity and temperature
Because SD is driven by both yeast overgrowth and inflammation, effective treatment strategies target both.⁵
Anti-yeast treatments reduce Malassezia levels on the skin:
• Ketoconazole 2% shampoo or cream
• Ciclopirox olamine 1.5% shampoo
• Clotrimazole cream
• Zinc pyrithione shampoo
• Selenium sulfide 2.5% shampoo
• Salicylic acid shampoo (helps with scaling)
• Tar shampoos (helps with scaling and inflammation)
However, antifungal treatments alone are often not enough, especially during flare-ups with significant redness and itching. That’s why anti-inflammatory treatments are essential.
Topical corticosteroids, like hydrocortisone 1% cream or desonide 0.05% cream, can quickly calm inflammation during active flare-ups, especially helping with redness and scaling in visible areas like the face and scalp.















For sensitive areas or longer-term use, non-steroidal immunomodulators –such as pimecrolimus 1% cream and tacrolimus 0.1% ointment – are good options, helping to control inflammation safely over time.
Excitingly, one of the newest treatments is roflumilast 0.3% foam, recently approved in Canada, and indicated for topical treatment of seborrheic dermatitis in patients 9 years of age and older. Roflumilast is a phosphodiesterase-4 (PDE4) inhibitor that targets enzymes involved in skin inflammation. By calming this pathway, it effectively reduces redness, scaling, and itch, even in sensitive areas like the face.
For many patients, combining antifungal and anti-inflammatory treatments provides the best relief.
Sarah: A patient’s story
Sarah, a 38-year-old teacher, has been managing SD since her late twenties. What began as mild dandruff gradually spread to her face, causing redness and flakes around her eyebrows, nose, and ears.
“At first, I thought it would clear up with regular shampooing, but instead, it started showing up in more visible places,” Sarah recalls. “My skin became itchy, red, and flaky, which made me extremely self-conscious.”
Sarah’s experience shows how SD affects daily life. She constantly checked her appearance, avoided social situations, and felt anxious about flare-ups.
With guidance from her dermatologist, she started using ketoconazole shampoo and hydrocortisone cream.
“Once I started using the treatments regularly, I noticed a huge improvement.
“For anyone living with SD, remember –you’re not alone. With proper care and guidance from a healthcare provider, it’s possible to manage the condition and improve daily life.”
The itchiness subsided, and my skin became clearer,” she says.
Though flare-ups still occur, especially in colder months or stressful times, Sarah feels empowered knowing how to manage her condition. Her story underscores the value of early diagnosis, effective treatment, and ongoing self-care.
“Living with SD has taught me patience and self-care. It’s more than just skin deep – it affects how you feel about yourself.”
Common myths
1. Myth: Poor hygiene causes SD. Reality: SD is not related to cleanliness. Even those with excellent hygiene can develop it.
2. Myth: SD is contagious. Reality: It cannot be spread from person to person.
3. Myth: Dandruff shampoos will permanently cure SD. Reality: Shampoos help manage symptoms, but SD often requires ongoing management.
4. Myth: Diet alone can control SD. Reality: While healthy choices are beneficial, diet alone rarely controls SD completely.
5. Myth: Stress directly causes SD. Reality: Stress does not cause SD, but it can trigger or worsen flare-ups.
Looking ahead:
Hope with new treatments
With new insights into its causes and treatments like roflumilast, patients have more options than ever. Early diagnosis and the right treatment plan can ease
symptoms, improve comfort, and boost confidence.
For anyone living with SD, remember –you’re not alone. With proper care and guidance from a healthcare provider, it’s possible to manage the condition and improve daily life.
References
1. Heath CR, Usatine RP. Seborrheic dermatitis. J Fam Pract 2021;70(9):E3-E4. doi:10.12788/jfp.0315
2. Sampogna F, Linder D, Piaserico S, et al. Quality of life assessment of patients with scalp dermatitis using the Italian version of the Scalpdex. Acta Derm Venereol 2014;94(4):411-414. doi:10.2340/00015555-1731
3. Lin Q, Panchamukhi A, Li P, et al. Malassezia and Staphylococcus dominate scalp microbiome for seborrheic dermatitis. Bioprocess Biosyst Eng. 2021;44(5):965-975. doi:10.1007/s00449-020-02333-5
4. Tao R, Li R, Wang R. Skin microbiome alterations in seborrheic dermatitis and dandru : A systematic review. Exp Dermatol 2021;30(10):1546-1553. doi:10.1111/exd.14450
5. Borda LJ, Perper M, Keri JE. Treatment of seborrheic dermatitis: a comprehensive review. J Dermatolog Treat. 2019;30(2):158-169. doi:10.1080/09546634.2018.1473554
Mahan Maazi is a third-year medical student at the University of British Columbia.
Dr. Khalad Maliyar is a Dermatology resident at the University of Toronto.



















By Valerie C. Doyon

Sun protection is the most important aspect of skincare. Ultraviolet rays damage the skin and can lead not only to skin aging but can also exacerbate many skin conditions such as lupus. Thirty-nine percent of women wear makeup daily1 and many find it challenging to reapply sunscreen without ruining their makeup. Below are strategies for reapplication.
Build an ultra-protective base with sunscreen & makeup2
• Adequate initial sunscreen: Apply a thick layer of broadspectrum sunscreen as the final step of your skincare routine – at least a half teaspoon for your face and neck. Let it absorb for 2–3 minutes so it creates a uniform barrier under makeup.
• SPF-infused cosmetics: Seek cosmetics like primers, foundations, concealers, bronzers, powders, and lipsticks with built-in SPF. Multiple brands offer various types of SPF-containing cosmetics.
Sunscreen reapplication options over makeup
• Sunscreen mists and sprays: Hold your breath, close your eyes, and spray in multiple passes from about 15 cm away. Avoid inhaling the mist.
• SPF powders: Available as brushes or loose/pressed compacts. They’re portable and easy to use, though brush-on versions often under-deliver product and can appear chalky on darker skin tones.
• Liquid sunscreen top-up: The most reliable way to apply enough product to achieve the SPF number on the label: use a damp beauty

blender or cushion puff to press (not rub) the formula into your skin, on top of makeup. Expect slight smudging of blush or bronzer. Simply reapply color and/or setting powder afterwards. 2
Maximize sun protection beyond sunscreen
• Physical barriers: Wear a wide-brim hat, UV-blocking sunglasses, or even carry a portable sun umbrella or face shield. Choose light, breathable garments labeled UPF 40+ whenever you can.
• Oral adjuncts: Polypodium leucotomos supplements3 won’t replace sunscreen, but they help neutralize free radicals and reduce DNA damage from any missed spots.
• Multiple layers of defense: No single strategy is perfect. Stacking sunscreen, protective clothing,
supplements, and shade gives you the strongest shield. Wanting to protect your skin doesn’t mean you have to give up makeup. Combining methods and being consistent offers the best defense. It may take some trial and error, but these tips should make it easier to stay sun safe.
References
1. CivicScience. (2019, September 9). Makeup is losing its luster https://civicscience.com/makeup_is_losing_its_luster/
2. Kim, M. A., Jung, Y. C., Bae, J., Ha, J., & Kim, E. (2021). Layering sunscreen with facial makeup enhances its sun protection factor under real-use conditions. Skin Research and Technology, 27(5), 751–757. https://doi.org/10.1111/srt.13010
3. McDonald, K. A., Lytvyn, Y., Mufti, A., Chan, A. W., & Rosen, C. F. (2023). Review on photoprotection: A clinician’s guide to the ingredients, characteristics, adverse e ects, and disease-specific benefits of chemical and physical sunscreen compounds. Archives of Dermatological Research, 315(4), 735–749. https://doi.org/10.1007/s00403-022-02483-4
Dr. Valerie C. Doyon is a dermatology resident at the Université de Montréal.



By Kimia Ameri
The development of permanent, autologous skin substitutes represents a major advancement in burn treatment. At the forefront of this innovation is the LOEX (Laboratoire d’Organogénèse Expérimentale) research centre at Université Laval in Quebec City, led by

Dr. Lucie Germain, which celebrates its 40th anniversary this year. Over four decades, LOEX has pioneered new approaches in tissue engineering, culminating in the creation of the Self-Assembled Skin Substitute (SASS): a fully autologous, bilayer skin graft
To date, LOEX has cultured cells from patients of all ages, including neonates and individuals up to 93 years old.

designed for long-term regeneration and functional recovery.
LOEX’s legacy began in 1986, when its researchers performed Canada’s first graft using cultured epidermis autografts. This breakthrough marked the beginning of a shift away from traditional split-thickness skin grafts toward laboratory-grown alternatives for severely burned patients. In 1998, LOEX introduced the self-assembly approach, which allowed for the fabrication of skin substitutes that
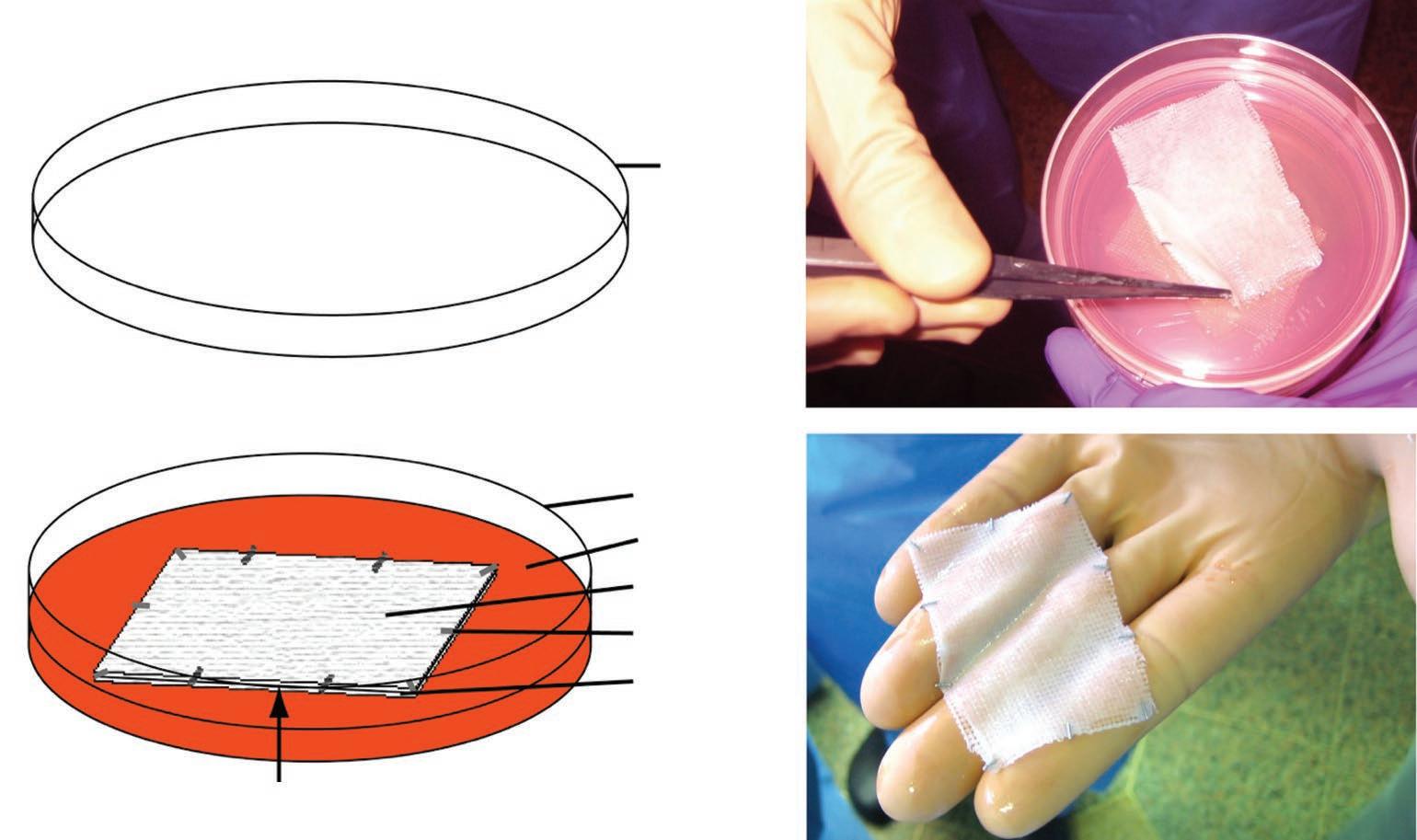


include both dermal and epidermal layers, using only cells from the patient. This scaffold-free method involves culturing fibroblasts to produce their own extracellular matrix, which forms a dermis capable of supporting a stratified epidermis formed by seeded keratinocytes. The result is a biocompatible, bilayer skin graft with regenerative potential. By 2005, the first clinical application of this bilayer substitute was completed in Montreal.
The current SASS production process begins with a biopsy roughly the size of a two-dollar coin. This sample is processed at LOEX laboratory in the CHU de Québec -Université Laval Hospital, where cells are expanded and cultured over 52 to 65 days to form the final skin substitute. One of the most important innovations in this process is the ability to isolate and preserve epithelial stem cells, which remain active after grafting. These cells contribute to the long-term regeneration of the skin, including its ability to repair after subsequent injury. To date, LOEX has cultured cells from patients of all ages, including neonates and individuals up to 93 years old.

A pivotal 2018 case series highlighted the clinical success of SASS. Fourteen patients with severe burns, covering up to 92% of their total body surface area (TBSA), were treated with SASS under Health Canada’s Special Access Program.1 The grafts demonstrated a mean take rate of 98%, with longterm epithelial survival, high elasticity, and minimal hypertrophic scarring. In pediatric patients, the grafts expanded naturally with the child’s growth, eliminating the need for contracture release surgeries that are often necessary with conventional grafts. Today, LOEX’s technology is being used in a multicenter clinical trial involving burn centers in cities across Canada, including Quebec City, Montreal, Toronto, Winnipeg, Calgary, Edmonton, and Vancouver. Surgeons at these centers identify eligible patients, and send small biopsies to LOEX, where skin substitutes are cultured

Because it is entirely autologous, there is no risk of immune rejection.
and returned for surgical application. This model centralizes production while ensuring timely access to personalized, regenerative grafts.
SASS offers several key advantages over conventional autografts and synthetic substitutes. Because it is entirely autologous, there is no risk of immune rejection. Also, the absence of synthetic components reduces the risk of infection, and supports integration with the patient’s tissue. The substitute also has the capacity to regenerate, grow, and heal over time, and does not produce the meshed appearance or excessive scarring often seen with traditional methods.
Despite these benefits, some limitations remain. Pigmentation is often inconsistent post-grafting, with many patients initially presenting with hypopigmented skin that may develop patchy repigmentation over time. This is likely due to the slower replication of melanocytes compared
to keratinocytes during culture. Addressing this limitation and reducing production time are key areas of ongoing research.
The work at LOEX represents a convergence of biomedical science and patient-centered innovation. The ability to engineer permanent, self-renewing skin not only improves survival for patients with extensive burns but also enhances their long-term quality of life. In recognition of her leadership and groundbreaking contributions, Dr. Germain was awarded the King Charles III Coronation Medal in February 2025.
Reference
1. Germain, L., Larouche, D., Nedelec, B., Perreault, I., Duranceau, L., Bortoluzzi, P., ... & Dumas, A. (2018). Autologous bilayered self-assembled skin substitutes (SASSs) as permanent grafts: A case series of 14 severely burned patients indicating clinical e ectiveness. Eur Cell Mater, 36, 128-141. DOI: 10.22203/eCM. v036a10
Kimia Ameri is a first-year medical student at the University of British Columbia.
By Victoria Young
X-linked ichthyosis (XLI) is a genetic disorder of keratinization characterized by the development of large, dark brown or light grey, polygonal scales that primarily affect the trunk, neck, and extensor surfaces of the limbs.1 It usually spares the face, palms, soles, and flexural areas. After ichthyosis vulgaris, XLI is the second most prevalent kind of ichthyosis.
The Xp22.3 chromosome contains the STS (steroid sulfatase) gene, which can be mutated or deleted to cause XLI.1 Due to the consequent decrease in steroid sulfatase enzyme activity, cholesterol sulphate builds up in the stratum corneum, interfering with normal desquamation and causing the distinctive scaling. 2



Photo(s) sourced from https://dermnetnz.org/topics/recessive-x-linked-ichthyosis.

XLI is an X-linked recessive disorder that primarily affects males, with an estimated prevalence of 1 in 1,500 live male births; however, it is diagnosed in only approximately 1 in 6,000 males.1 Although there have been isolated reports of minor scaling, female carriers are mostly asymptomatic.
Usually, the first few weeks to months of life are when symptoms appear. Asymptomatic corneal opacities, cryptorchidism, and in certain situations, mild neurodevelopmental or behavioural problems like attention-deficit/ hyperactivity disorder (ADHD) are examples of extracutaneous symptoms in addition to skin findings.1 It is believed that contiguous gene deletions in the Xp22.3 region are responsible for these relationships.1
Although the diagnosis is mostly clinical, it can be verified by leukocyte or fibroblast enzyme assay or STS gene testing. 2 Although it is rarely required, a skin biopsy may reveal a normal granular layer and compact hyperkeratosis. 2 Regular application of emollients, keratolytics like lactic acid or urea, and infrequent application of topical retinoids are all part of the symptomatic management. 2 Affected families should have access to genetic counselling to talk about reproductive options and inheritance patterns. 2
References
1. Wren, G. H., & Davies, W. (2022). X-linked ichthyosis: New insights into a multi-system disorder. Skin Health and Disease, 2(4). doi:10.1002/ski2.179
2. Recessive X-linked ichthyosis. (2024). Retrieved from https:// dermnetnz.org/topics/recessive-x-linked-ichthyosis
Victoria Young is a third-year medical student at the University of Toronto.

By Valerie C. Doyon, BSc, MD and Anne-Sophie Groleau, MD Division of Dermatology, Centre Hospitalier Universitaire de Montréal (CHUM), Department of Medicine, Université de Montréal

Itch is often described as more distressing than pain, and significantly impacts quality of life. In dermatology, itch is a common and persistent symptom across a range of skin conditions. This article explores the approach to itch management in four common chronic conditions: atopic dermatitis, prurigo nodularis, seborrheic dermatitis, and psoriasis. Atopic dermatitis (AD) and seborrheic dermatitis typically present with itchy plaques in skin folds and oily areas of the upper body, respectively. While psoriasis is not classically itchy, many patients experience itchy plaques. Prurigo nodularis, however, arises from chronic skin scratching and is both a symptom and a self-perpetuating consequence of severe itch.
The foundation of itch therapy is lifestyle measures. All patients are encouraged to frequently moisturize with fragrance-free emollients2, to take lukewarm showers, and to use gentle cleansers.2 Covering itchy plaques with bandages and keeping nails short are other physical measures that can help. It is also important for patients to understand the chronic nature of their condition, commit to maintenance treatments, and avoid known triggers to prevent flare-ups.


Atopic Dermatitis:
With ongoing research, new therapies have recently been marketed. In terms of topicals, a topical Janus Kinase (JAK) inhibitor known as Ruxolitinib is approved for light to moderate AD in patients 12 years and older.2 Advanced sytemic treatments, including biologics (dupilumab, lébrikizumab and tralokinumab) as well as oral JAK inhibitors (Upadacitinib and Abrocitinib) have recently come to market, and can improve symptoms with varying speed.2
Prurigo Nodularis:
In prurigo nodularis, treatments are heavily focused on breaking the “itchscratch” cycle. In addition to most treatments used in AD, corticosteroid injections directly into the nodules can be attempted.3 Dupilumab, a common biologic prescribed in AD, was recently approved for prurigo nodularis.
A promising approach is to modify the central nervous system’s response to itch through medications typically used to treat anxiety or chronic pain, such as pregabalin, amitriptyline, and paroxetine.3 Since prurigo nodularis has many underlying causes, tailored treatments are needed.
Seborrheic Dermatitis:


In addition to anti-dandruff shampoos, antifungals, and corticosteroid creams, Roflumilast is a new medicated foam that can be used all over the body and scalp.1
Psoriasis:
Achieving psoriasis control typically helps to alleviate itch. A new medication, Tapinarof cream, complements an abundance of effective psoriasis therapies. Additionally, another oral JAK inhibitor called Deucravacitinib, has recently been approved.4



Itch-directed symptomatic therapies For symptomatic treatment, topical over-the-counter creams that contain menthol, capsaicin, and pramoxine can be helpful.2 Although they may irritate the skin (i.e., capsaicin), they block nerves from transmitting the itch sensation. Applying a cold damp washcloth can similarly appease itch. If the skin is very itchy and disrupts sleep, oral sedating antihistamines or other medications may be considered temporarily.2
Conclusion
Itch remains one of the most debilitating symptoms in dermatologic conditions, often driving patients to seek care. While lifestyle modifications and symptomatic treatments form the foundation of itch relief, newer targeted therapies offer hope for more sustained control. As our understanding of itch mechanisms
deepens, the therapeutic landscape continues to expand with innovative medications addressing both peripheral and central pathways of itch signals. For patients living with chronic skin disease, this progress brings meaningful relief within reach.
References
1. Blauvelt A, Draelos ZD, Gold LS, Alonso-Llamazares J, Bhatia N, DuBois J, et al. Roflumilast foam 0.3% for adolescent and adult patients with seborrheic dermatitis: A randomized, double-blinded, vehicle-controlled, phase 3 trial. Journal of the American Academy of Dermatology. 2024 Jan 21;90(5):986–93. Available from: https://doi.org/10.1016/j. jaad.2023.12.065
2. Bolognia, J. L., Scha er, J. V., Cerroni, L. (2024-04-18). Dermatology, 5th Edition. [Elsevier eBooks+ 10.2.1].
3. Brooks SG, Yosipovitch G. Prurigo nodularis in 2025: Current and emerging treatments. Clinics in Dermatology. 2025 Mar 1; Available from: https://doi.org/10.1016/j. clindermatol.2025.03.013
4. Carmona-Rocha E, Rusiñol L, Puig L. New and Emerging Oral/Topical Small-Molecule Treatments for Psoriasis. Pharmaceutics. 2024 Feb 6;16(2):239. Available from: https:// doi.org/10.3390/pharmaceutics16020239
5. Geng RSQ, Sibbald RG. Atopic dermatitis: clinical aspects and treatments. Advances in Skin & Wound Care. 2024 Jun 20;37(7):346–52. Available from: https://doi.org/10.1097/ asw.0000000000000161
A spotlight on our latest activities, events and other information of importance to skin patients in Canada
It’s hard to believe, but Canadian Skin magazine is turning 15!
Since our very first issue in Spring 2010, our goal has always been simple: to support, inform, and connect people living with skin, hair, and nail conditions across Canada. What started as a small publication has now grown into more than 50 issues filled with expert advice, personal stories, and evidenceinformed information you can trust.
This magazine is truly a team effort. So many of the articles you’ve read over the years have been written by volunteers: people living with the same conditions, caregivers, advocates, and healthcare professionals who believe in the power of shared experience. Every issue is also medically reviewed by dermatologists from across the country, to ensure what we publish is not only relatable, but reliable.

















We’re incredibly grateful to you, our readers, for being part of this journey. Whether you’ve been with us from the beginning or just picked up your first issue, thank you for trusting us to be part of your story.
titled “Skin diseases as a global public health priority” at the 78th World Health Assembly. This historic step recognizes the significant global burden of skin conditions and calls for stronger efforts in prevention, early detection, treatment, and long-term care. The resolution also aims to better integrate skin health into overall health systems and mandates the development of a Global Action Plan. As this work unfolds, CSPA is committed to being actively involved in the months and years ahead, ensuring that the voices and needs of patients in Canada are part of this global movement.
Here’s to continuing to learn, grow, and support one another for many more years to come.

We’re also excited to share important global news that will shape the future of skin health.


On May 24, 2025, the World Health Organization (WHO) adopted a resolution
SPONSORS OF CANADIAN SKIN MAGAZINE





Dana Gies Executive Director Canadian Skin Patient Alliance


is the Founding Sponsor of the Canadian Skin magazine and an ongoing supporter of CSPA's publications





These sponsors are not providing editorial support for the magazine. CSPA is responsible for the final content featured in Canadian Skin
CANADIAN SKIN MEDICAL ADVISORS + BOARD MEMBERS + VOLUNTEERS
Thank you to the medical advisors, board members, and volunteers who support the work of CSPA. For an updated list of names, visit canadianskin.ca/about-us.
The Canadian Psoriasis Patient Charter is a new initiative by PSO TOGETHER, a committee of expert patients, healthcare professionals, and patient group representatives, brought together with support from J&J Innovative Medicines, who aim to improve psoriasis patient care and experience in Canada.
The Charter’s goal is to understand and promote more equitable, inclusive care – and to strive for everyone in Canada living with psoriasis to receive appropriate, respectful, and effective support and treatment.
There’s no cure for psoriasis yet and ongoing access to high-quality, safe, and affordable care, treatment, and support remains critical. However, inequities in diagnosis, access to treatment, and care outcomes persist across Canada; for example:
• A recent survey finds that people with darker skin tones are five times more likely to receive a misdiagnosis, and it can take twice as long to be correctly diagnosed.
• Treatment concerns of individuals who are pregnant or of child-bearing age are not always addressed.
• One’s cultural background may shape how they experience psoriasis and navigate care, but these factors are often overlooked in treatment planning.
The Charter aims to:

















Living with psoriasis also impacts mental health, financial stability, and personal relationships and many people lack access to information needed to fully participate in care and treatment decisions.
“The launch of the first Canadian Psoriasis Patient Charter is a milestone in ensuring every person with psoriasis in Canada receives the care they deserve. Access to care is more than availability – it means removing barriers to equitable treatment.
As a dermatologist in an underserviced, often ruralized area of the Canadian midwest, I see patients’ challenges firsthand and was able to bring their concerns into this charter.
Psoriasis is more than ‘just a skin condition.’ It has major physical, mental, and psychosocial impacts, along with systemic associations such as psoriatic arthritis and cardiovascular disease. With ongoing medical advances, safe and effective therapies are increasingly available, bringing long-term disease modification and the hope of a cure closer.
This initiative unites patients, healthcare professionals, and community voices nationwide. By raising awareness and fostering collaboration, we can ensure all patients receive the understanding, support, and treatments they need. Together, we are shaping a future where every patient gets the care they deserve.”
– Dr. Rachel Asiniwasis, Dermatologist, Regina, Saskatchewan
Psoriasis Canada was pleased to join with people with diverse lived experience of psoriasis and healthcare professionals across the country to explore these issues together.
“Living with palmoplantar psoriasis (PPP) has shown me how gaps in care can leave those living with psoriatic diseases feeling unseen and unheard. The Charter gives us a voice and a framework to ensure that no matter who you are, where you live, or what your background is, you can count on receiving better care and support.”
– Christian Boisvert-Huneault, Vice-Chair & Acting Chair, Psoriasis Canada
• Value the diverse identities of patients and healthcare providers across race, religion, sexual orientation, gender identity, and ability to ensure all voices are heard, respected, and included.
• Expand the standard of psoriasis care to include all the diverse aspects of overall well-being.
• Educate patients on psoriasis and its treatment and raise awareness of available resources.
• Help patients to participate in decision-making by providing information.
• Help promote a high quality of care and sets standards for healthcare providers.
• Encourage open communication and trust between patients and healthcare providers.
It reminds us that there is hope for a future where care is equitable, informed by diverse lived experience, and supported by collaboration across patients, providers, and organizations.
