

INSIDE:
AI scribes on trial in BC British Columbia is running a multi-site trial of six different AIpowered scribes. Whereas a recent test in Ontario involved family doctors, the BC project has enlisted a wide range of clinicians.
Page 4
Springboard for innovation
The National Healthcare Innovation Council was launched in Newfoundland and Labrador late last year. It will help promote Canadian healthcare innovators across the country.
Page 6
AI scribes and more Markham, Ont.-family physician
Dr. Paul Forman has created an integrated system called Alifor for doctors’ offices. The platform combines AI scribes, clinical decision support and workflow to ease the burden on GPs and other clinicians.
Page 14

New health innovation council announced in NL
The National Healthcare Innovation Council was launched at the Newfoundland and Labrador Health Services’ Health Innovation Summit in St. John’s last November. The new group intends to break down policy, procurement and structural barriers and build commercialization pathways across Canada. Pictured at the summit are members of the NLHS board of trustees: (left to right) David Thornhill, Edward Goudie, Lloyd Walters (vice-chair), Sharon Forsey, Robert B. Andrews (chairperson), Dr. David Sutherland. SEE STORY ON PAGE 6.
Ontario Shores wins second HIMSS Davies Award
BY JERRY ZEIDENBERG
WHITBY, ONT. – At Ontario Shores Centre for Mental Health Sciences (Ontario Shores), information technology has become a key enabler of clinical innovation and continuous improvement.
“We use real-time data to drive clinical decision-making and to do the right thing,” noted Sanaz Riahi, executive vice-president, transformation, clinical services and chief nursing executive.
That kind of thinking, and the improvements in clinical care to which it has led, resulted in Ontario Shores winning the 2025 HIMSS Davies Award.
It’s the second time Ontario Shores has received the prestigious award. That makes it the first mental health hospital worldwide to achieve this distinction twice and the second Canadian organization to do so since the award’s inception in 1994.
“We use technology to solve clinical issues and problems,” said Riahi. “We don’t make any decisions without data,” she asserted.
Some examples that impressed HIMSS include:
• Reducing incidents of aggression on inpatient units to keep patients and staff safe.
• Giving patients digital tools and im-
Ontario Shores is the first mental health hospital worldwide to win the award twice.
proved portals to make care more accessible and reduce missed appointments.
• Limiting restraint and seclusion to uphold dignity and support recovery.
What kind of corporate culture does Ontario Shores have when it comes to IT?
First, the organization ensures that information technology is always in the service of
improving care and enhancing the safety of patients and staff.
For this reason, its professional practice, clinical informatics, data analytics and IT teams works closely together.
The partnership ensures there is an integrated approach to developing new initiatives. Together, they also work out what needs to be measured, to give management the information they require to track performance and quality.
Riahi said Ontario Shores became a public hospital in 2006 and realized at the time that IT could help support decision-making and patient care through the acquisition of an EHR. That’s when it purchased its MEDITECH system.
“The EHR was our first major IT investment,” she said. “It’s served us well by helping to reduce variability in care and embedding quality standards in our processes.”
Since then, the top leadership team at the
Ontario Shores Centre for Mental Health Sciences wins second HIMSS Davies Award
hospital has been a strong supporter of innovation and continuous improvement using technology – another important factor that’s needed for success.
On a related tech front, Ontario Shores has become the first hospital in Canada to deploy the pharmacogenomics module in MEDITECH. This has enabled its clinicians to make more informed prescribing decisions by aligning medications with a patient’s genomic profile.
This helps clinicians decide on the right medication and the best dose.
Riahi said the rollout of the genomic module has been successful for its eligible inpatient population. Ontario Shores has since expanded it to select outpatients with a diagnosis of major depressive disorder.
And finally, on the corporate culture front, she said the organization isn’t afraid to fail. In order to advance, it needs to try different solutions – and it learns even when things don’t work out.
Riahi explained that overall, in the technology marketplace, there’s less of a focus on mental health. For that reason, the or-
ganization has been creating its own solutions – either in-house or in partnership with the private sector.
Because many of these solutions are first of their kind, there’s more to be learned along the path of development.
“Less technology is custom-made for mental health,” said Riahi. “We need to test our solutions through trial and error.”
That testing and refinement has resulted in numerous solutions that have enhanced patient care and improved safety for both patients and staff.
For example, when it comes to inpatient aggression, it’s known that using a structured way to assess and de-escalate the situation supplements the skills of nurses and staff, leading to better outcomes for everyone.
The hospital built and embedded evidence-based tools into its digital system to help staff assess patients and spot when someone might be at higher risk of aggression.
These tools give clinicians helpful strategies to prevent incidents and support patients during difficult moments, and they’ve led to very positive results.

It also invested in staff education, so nurses could identify unsafe situations and respond to them quickly and effectively.
Clinical practice leaders, clinicians and IT staff developed a nursing-driven approach that ensured the daily completion of the Dynamic Appraisal of Situational Aggression (DASA), followed by the activation of the Aggression Prevention Protocol (APP) for high-risk patients.
To streamline the process, the prompts to complete APP assessments were embedded within the existing workflow,
minimizing the documentation burden.
As well, automated real-time monitoring reports were developed, refreshing hourly to track compliance and highlight patients needing follow-up.
And an email notification system alerted leadership when required interventions were missing.
These enhancements fostered a proactive response to aggression risk, improving patient safety and reinforcing accountability among clinical teams.
The hospital notes in its report on patient aggression, “As a result of these datadriven improvements, the average MOAS (Modified Overt Aggression Scale), reflected a significant reduction in incidents of patient aggression, demonstrating the effectiveness of structured assessments and timely interventions.”
On another front, Ontario Shores has improved its patient portal as a way of engaging patients in their own therapy and providing clinicians with more information about their patients.
The organization was able to identify patients who weren’t yet enrolled in its portal and reached out them with redesigned methods and easier ways of joining.
Issue DateFeature ReportFocus Report
March Artificial IntelligenceInteroperability
April Mobile SolutionsHospital at Home
May EHR / EMR TrendsPrecision Medicine
June/July IT Resource GuidePoint-of-Care Systems
September Community CareStart-ups
October Virtual CareSurgical Technologies
Nov/Dec AI/AnalyticsCardiology
Coming up in 2026 www.canhealth.com
For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com

Address all correspondence to Canadian Healthcare Technology, P.O. Box 907, 183 Promenade Circle, Thornhill ON L4J 8G7 Canada. Telephone: (905) 709-2330. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2026. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others: $67.80 per year ($60 + $7.80 HST). Registration number 899059430 RT. ©2026 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited. Send all requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, P.O. Box 907, 183 Promenade Circle, Thornhill ON L4J 8G7. E-mail: jerryz@canhealth.com. ISSN 1486-7133 CANADA’S MAGAZINE FOR MANAGERS AND USERS OF INFORMATION TECHNOLOGY IN HEALTHCARE Volume 31, Number 1 February 2026
Canada
Publisher & Editor
Jerry Zeidenberg jerryz@canhealth.com
Office Manager Neil Zeidenberg neilz@canhealth.com
The portal could then send reminders about appointments to patients, greatly lowering the rate of missed appointments. Patients were given access to educational resources and to their own data, including their electronic health record, building their sense of agency and self-management.
What’s more, they could fill out questionnaires about their own conditions, which are directly entered their online record, enabling clinicians to see how they were doing in real-time – something that helps with timely decision-making.
Ontario Shores’ patients became more engaged in tracking their own progress and felt they had a more substantial role in managing their care. This also helped lower the rate of missed appointments and contributed to better compliance with individual care programs.
On a related note, when it comes to encounters between patients and clinicians, Ontario Shores is a big believer in using technology to make things easier. The use of virtual care exploded during the COVID-19 pandemic, when many facilities were in lock-down, but subsided greatly afterwards at most hospitals.
For its part, Ontario Shores is still a major user of video visits for outpatients.
In fact, notes Riahi, a high degree of ambulatory patients are using virtual care for appointments. “We’ve left it to the patients to decide whether they’d like to use virtual appointments,” she said. “We try to make it easier for them.”
Contributing Editors
Dianne Daniel dianne.l.daniel@gmail.com Will Falk will@wfalk.ca Dr. Sunny Malhotra Twitter: @drsunnymalhotra Norm Tollinsky tollinskyn@gmail.com
Art Director
Walter Caniparoli art@canhealth.com
Digital Media Specialist
Rebecca Downer rebecca@canhealth.com
Sanaz Riahi, executive vice-president
The world’s first singlesource photon-counting CT










siemens-healthineers.ca/naeotom-alpha-prime












Part of the NAEOTOM Alpha class family, NAEOTOM Alpha.Prime is the fastest, highest-resolution single-source CT in our portfolio and is now available in Canada. It expands access to Quantum Technology while preserving the image quality and diagnostic confidence that define the NAEOTOM Alpha class. NAEOTOM Alpha. Prime delivers ultra-high resolution imaging and spectral information in every scan, making photon-counting CT more accessible than ever.
Want to learn more in-person?
















Scan for more event information


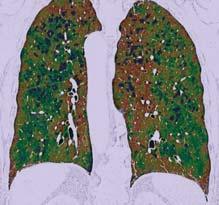
Visit us at the Canadian Association of Radiologists (CAR) Annual Scientific Meeting April 16-19, 2026 | Montreal, Quebec





Courtesy of Diagnostikum Graz, Austria The products/features (mentioned herein) are not commercially available in all countries.
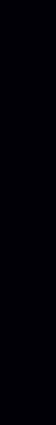
BC conducts large-scale trial of six different AI scribes for care providers
BY DR. ANGEL ARNAOUT, DR. MAXIMILLIAN BESWORTH AND NAOMI BROOKS
As generative artificial intelligence tools become more widely available, healthcare organizations across Canada are confronting a new operational reality: clinicians are increasingly adopting AI tools on their own initiative. This trend – often described as Bring Your Own AI (BYOAI) – reflects both unmet clinical needs and growing familiarity with consumer AI platforms (e.g. ChatGPT) that support summarization, drafting, and information synthesis.
While such tools can improve efficiency, their unregulated use in clinical contexts introduces significant risk to health authorities and organizations. Patient privacy, clinical data security, regulatory compliance, and professional liability remain unresolved when consumer-grade AI is used outside institutional controls. Guidance from the Canadian Medical Protective Association (CMPA) has reinforced that clinicians remain accountable for AIassisted care, even as legal and regulatory frameworks continue to evolve.
Attempts to ban BYOAI have largely proven ineffective. Research from the MIT Center for Information Systems Research suggests that prohibitions tend to push AI use underground, increasing organizational exposure to privacy and security risks rather than reducing them. The reality is that AI is already embedded in clinical practice, whether health systems formally acknowledge it or not.
In British Columbia, that shift has led to the BC Scribe Trial – a coordinated, multi-site evaluation of ambient AI scribe

technologies designed to provide a managed, enterprise-approved alternative to unmanaged BYOAI use.
A first-of-its-kind evaluation at scale:
The BC Scribe Trial is believed to be Canada’s first multi-vendor, multi-site randomized evaluation of third-party non-enterprise integrated AI scribes within a publicly funded healthcare system. Led through the Provincial Health Services Authority (PHSA) in collaboration with partner health authorities, the program spans multiple electronic medical record (EMR) platforms and clinical environments.
The B.C. initiative builds on recent work by OntarioMD, which evaluated AI scribes primarily within family medicine and determined that these tools helped physicians’ daily work in reducing documentation burden and cognitive overload.
B.C.’s approach differs in scope. Rather than focusing solely on individual clinician experience, the BC Scribe Trial exam-
ines whether third party individual AI scribe solutions can be governed, supported, and scaled responsibly across a complex public healthcare system. The trial was designed to support and evaluate AI scribe use across approximately 8,000 providers, making it one of the largest coordinated AI initiatives undertaken in Canadian healthcare to date.
There was no traditional RFP by design. Instead of endorsing a single vendor, the program deliberately brought six AI scribe tools already in widespread, unregulated use into a structured, health authoritycompliant environment. The focus was system readiness, not product selection: determining whether commonly used tools could meet public-sector requirements for privacy, security, data stewardship, and clinical governance.
Participating clinicians rotate across solutions, enabling direct comparison of performance, usability, workflow impact,
and support requirements. This approach allows system leaders to assess how different tools function across specialties, encounter types, and care settings, while reducing vendor-specific bias.
The evaluation is guided by Canada Health Infoway’s Technology Evaluation Framework, ensuring that assessment extends beyond usability to include privacy, security, interoperability, clinical safety, and implementation readiness. Quantitative data, including usage metrics and surveys, are combined with qualitative feedback from clinicians to assess documentation quality, trust, and integration into real-world workflows.
From evaluation to provincial deployment: A distinguishing feature of the BC Scribe Trial is that it was designed from the outset with post-trial deployment in mind. Rather than concluding with a traditional pilot report, the program established pathways to enable broader access to approved tools across British Columbia.
Following the free-access trial, clinicians transitioned to a discounted self-pay model supported by a provincial master agreement. Participating vendors are offered the opportunity to enter negotiated, health authority–compliant contracts that meet standardized requirements for privacy, security, data handling, and clinical governance.
This structure enables deployment beyond early adopters, including expansion to the remaining B.C. health authorities, while preserving clinician choice and ensuring alignment with institutional standards – without requiring immediate centralized funding. By pre-negotiating contracts and standardizing requirements, PHSA has reduced one of the most com-
Be more proactive and use ‘sprints’ to solve problems, expert says
TORONTO – Dr. Tejash Shah told the crowd at the HIMSS Eastern Canada conference last October that we’ve got the technologies needed to solve the problems dogging the healthcare system – such as physician burnout and a lack of interoperability.
It’s just that most health professionals aren’t using them. Or they’re not using them very effectively.
Instead, everyone is pretty much doing things the way they did 30 years ago.
“I think that we’re running a marathon [today] using a playbook from the 1990s,” he asserted.
When he was starting out as a doctor 30 years ago, he dealt with stacks of paper records; today doctors are shuffling through stacks of PDFs and electronic records.
Instead, technologies like generative AI could be used to retrieve the right records and make summaries for doctors and nurses – all within seconds.
What’s required, he said, is a concerted push by all organizations to set goals and to figure out which technologies are available to reach them.
He mentioned interoperability as a persistent problem.
“If your lab systems, your e-referrals, your med lists are not fully integrated today, start 90-day sprints right now so that you have a plan and you’re moving towards that interoperability.”
But the sprints must be done in a thoughtful way.
They must address real problems; they have to reinvent the workflows so that things are done effectively; and staff re-training is a must. Not much will happen, he asserted, unless people are trained to work in a different way and to use the new systems.
Dr. Shah described a hospital that was testing a new AI system to reduce the administrative work of nurses on the floor. But when he asked whether they had trained the nurses to use it, the answer was: “Well, we haven’t done that part yet.”
He said the hospital was thinking of shutting down the whole project because they couldn’t afford the extra cost of training.
“So, when I talk about the operational challenges of generative AI, that’s what I mean. The technology is not enough.”
Dr Shah is a former ER doctor who is managing director at Accenture and serves as the global lead for care reinvention within Accenture’s Global Healthcare practice, helping to improve how hospitals function around the world.
He said many nursing practices are also stuck in the 1990s.
“Why aren’t we exploring, investigating, deploying the technologies to improve [nursing] experiences, get them away from doing the administrative
Embrace change: “We can’t just do things the way we’ve always done them before,” said Dr. Tejash Shah.
work, from doing the documentation tasks, from doing the things that take them away from patient care,” he asked.
And he continued, “why are we not helping them redeploy that work, so they could actually be with their patients, to hold the hands of those patients, to guide them, to coach them, to help them feel better, to reintroduce the
humanity into healthcare?”
He said AI could be used by nurses to create end-of-shift summaries, discharge summaries, literature reviews and more.
Dr. Shah mentioned a Georgia facility that was getting millions of faxes and electronic documents of lab results and DI tests each year.
Clinicians were looking at each one of them and putting them into individual patient records.
As a solution, the facility used intelligent optical character recognition to read the documents and automatically put them into the patient charts.
“They were able to take those millions of incoming documents and reduce the amount of time that clinicians were spending by thousands of hours.”
To spur even more activity, organizations should publicize their wins, showing how they’ve improved processes. “Start tracking it, start reporting it, and start delivering on it.” This will galvanize others to start their own projects.
Finally, he said healthcare organizations must embrace change. “We can’t just do things the way we’ve always done them before.”



















just the beginning. furthering the interoperability network’s impact transforms fragmented data meaningful and actionable insights.

Innovation council aims to break down barriers for home-grown tech
BY NORM TOLLINSKY
ST. JOHN’S, NL – The official launch of a new, pan-Canadian organization dedicated to accelerating the adoption of innovative, home-grown healthcare solutions was announced at Newfoundland and Labrador Health Services’ (NL Health) 2025 Health Innovation Summit, held in St. John’s last November.
Spearheaded by HealthPro Canada, a national group purchasing organization consisting of more than 2,000 hospitals, health authorities and other healthcare services, the new National Healthcare Innovation Council will champion innovations with scalable impact, mobilize adoption across jurisdictions, break down policy, procurement and structural barriers and build commercialization pathways.
“Canada has no shortage of exceptional healthcare innovations,” said Christine Donaldson, president and CEO of HealthPro Canada. “Through the council, we’re creating a clear path to scale by connecting leaders across provinces, sectors and disciplines to drive real system change.”
The goal of the organization, said Ron Johnson, inaugural chair of the council and NL Health’s vice president of digital health, innovation and research, “is to take innovations from one jurisdiction and move them into others without the necessity of a time-consuming evaluation and procurement process.”
The council expects to have regular meetings through the year, some in person and others held virtually.
Johnson cited the example of one Newfoundland-based company, PolyUnity
Tech Inc., that could benefit from the council’s work. Based in St. John’s, the company designs and produces parts and products for healthcare organizations using 3D printing technology.
One of its products, a 3D-printed facial mould, is used in Newfoundland to accurately target radiation therapy for patients with head and neck cancers. The 3D printed moulds are personalized by scanning the patient’s face and replace a more time-consuming manual process.
“We helped to incubate PolyUnity and have a contract with them, but it’s very difficult for a company in startup mode to take an innovation in one jurisdiction and move it to another because they have to go through a time-consuming procurement process every time. A day in the life of a startup is very different from a multinational because they don’t have the money to burn, so what we’re trying to do with this national innovation council is shorten that runway from one jurisdiction to the next.”
Using the same technology, PolyUnity also won an award at the summit for developing a perfectly fitting breast prosthesis for a patient who had undergone a double breast mastectomy.
CAN Health Network, a federally funded organization with a similar mandate, is also a member of the National Health Innovation Council. Working together, said Johnson, the two organizations will strive to further streamline the procurement process by listing an innovative product or solution on the HealthPro site once it has been procured in one jurisdiction, thereby reducing the need for repeated pilots.
NL Health’s sixth annual innovation
summit attracted more than one thousand attendees and 66 speakers from across Canada and beyond.
Newfoundland and Labrador Health Services relies on partnerships to develop, acquire and disseminate innovative healthcare products and solutions.
“A number of years ago, we realized that the problems in the healthcare system were

getting such that the normal ways of solving problems weren’t working as well,” said Johnson. “The challenges in the system are so great that the traditional reliance on quality improvement wasn’t sufficient, so we had to come up with a new way to solve our problems.”
NL Health’s new strategy for solving problems in the healthcare system is to collaborate and partner with local as well as national companies. Every year, the health authority publishes a public request for proposals inviting companies to join its roster of strategic innovation partners. The health authority asks frontline staff
across the province’s healthcare settings to identify opportunities for innovation and invites one or more of its strategic innovation partners to come up with a solution.
There are currently 20 strategic innovation partners, including five new ones who were announced at the November summit.
Johnson cites the example of an alternate level of care (ALC) problem that was successfully addressed through partnerships with Seafair Capital of St. John’s and Mobia Health Innovations of Dartmouth, Nova Scotia.
“In Newfoundland, on any given day, we have hundreds of hospital beds taken up by patients who no longer require acute care,” said Johnson. “So, we issued a challenge and partnered with Seafair Capital to create a software solution called Discharge Hub, which has taken three days off our discharge process for ALC patients.”
Discharging ALC patients from hospital is only possible when the supports such as beds, walkers, oxygen and home care are arranged for them. Discharge Hub identifies the supports required and expedites the process.
The solution was tested for six months at Newfoundland’s Health Sciences Centre and St. Clare’s Mercy Hospital in St. John’s and was subsequently introduced at hospitals across Newfoundland and Labrador. NL Health is now working with HealthPro Canada and others to make Discharge Hub available to other jurisdictions.
The development and testing of Discharge Hub is an example of NL Health’s characterization of the province’s healthcare system as a “living laboratory where public and private partnerships are actively forged to improve patient care.”
New tool improves health management for childhood cancer survivors
BY LAUREN ETTIN
For over two decades, the Pediatric Oncology Group of Ontario, POGO, has been at the forefront of using data to manage the care of survivors. Continuing the trend, POGO now is implementing Passport for Care in Ontario in collaboration with ACCESS and other national partners. It’s transitioning from a paperbased, manually updated system to a web-based tool with real-time linkage to provincial and national registries with personal health information (PHI).
In doing this, POGO is empowering childhood cancer survivors with secure, personalized, user-friendly access to their treatment summaries, for life.
The problem – Survivorship in the shadows: Two of every three childhood cancer survivors in Ontario face the startling reality of experiencing serious late effects from their treatment, including heart disease and secondary cancers.
Some also face cognitive challenges and fertility issues. Yet, many lack access to personalized care plans that could help detect and manage these risks early. With over 20,000 childhood cancer
survivors in Ontario alone and more than 5,000 actively followed in POGO AfterCare Clinics (province-wide health monitoring and screening clinics), the need for timely, individualized health information is urgent.
The current survivor care software, in place since 2015, is outdated and inconsistent across regions, leaving survivors, especially those in marginalized communities, without the guidance they need to thrive. POGO’s plan will revolutionize how survivors and clinicians access their health information and manage late effects.
Dr. Paul Nathan is an important partner on the POGO Passport for Care implementation team. He is head of the Solid Tumour Section and director of the POGO AfterCare Program in the Division of Hematology/Oncology at The Hospital for Sick Children.
“Passport for Care will provide all survivors, regardless of where they live or receive medical care, with an invaluable tool that consolidates their treatment exposures, long-term risks, and recommended surveillance in one easyto-access place,” said Dr. Nathan. “It will empower survivors to communicate ef-
fectively with their healthcare providers and to obtain the tests and follow-up care they need to optimize their longterm health and quality of life.”

The solution – Linking Passport for Care to real-time data: Developed by Baylor College of Medicine and Texas Children’s Cancer Center, Passport for Care is a clinical decision support tool that generates personalized, evidenceinformed Survivorship Care Plans based on the Children’s Oncology Group (COG) Guidelines. In regions across North America where Passport for Care has been implemented, it’s already made a significant impact with over 29,409 survivors accessing their care plans online. Despite this implementation, reliance on manual data entry remains a significant challenge.
The partnership between POGO and ACCESS, a national research network, is groundbreaking. Launched in 2025, the
Ontario pilot aims to link Passport for Care with POGO’s childhood cancer registry (POGONIS) and the national Cancer in Young People in Canada (CYP-C) registry to automate care plan generation. This will reduce clinician workload and ensure survivors receive real-time recommendations to manage their health. Unmatched in the world, POGONIS contains nearly 40 years of population-based standardized and comprehensive data on demographic, diagnosis, treatment and outcomes of children with cancer in Ontario.
The pilot is more than a provincial initiative. While two children’s hospitals in Canada have adopted Passport for Care with manual data entry, the Ontario provincial linkage to cancer registry data will lay the ground for all provinces to streamline their survivorship care and close longstanding gaps.
Equity at the heart of Passport for Care: POGO’s leadership is evident in every phase of the Passport for Care rollout – from securing funding and developing privacy-compliant data-sharing protocols, to piloting the system in select clinics and planning province-wide
Lauren Ettin
Ron Johnson, inaugural chair of the council.















Our health projects speak for us.











At Pomerleau, the quality of our work and the collaborative way we undertake our health projects are some of our best endorsements.
From early planning to final handover, we work as a trusted partner to health authorities, design teams, Indigenous communities, and local stakeholders, to build more sustainable hospitals, labs, research centres and more.
Whatever you need for health projects in Canada, from coast to coast we can build it.



ASKmeGOC supports communication about patients’ goals of care
Three intensive care physicians in Barrie, Ont., Dr. Chris Martin, Dr. Doug Austgarden and Dr. Giulio DiDiodato have developed a digital tool that brings much-needed clarity to families forced to make sudden, high-stress decisions around a loved one’s preferences for resuscitation and other invasive ICU interventions. These decisions are made using a goals of care (GOC) process which brings a chronically ill patient’s wishes to the forefront of urgent care.
Their ASKmeGOC software, created at the Royal Victoria Regional Health Centre (RVH), empowers health teams to navigate complex care discussions in a safe, confident and patient-centred way.
The innovation leverages investment from the “Health Care Unburdened Grant” provided by the Canadian Medical Association (CMA), MD Financial Management (MD) and Scotiabank, who share a commitment in supporting the medical profession and advancing health in Canada. As a demonstration of this commitment and in collaboration with the CMA and MD, Scotiabank is investing $115 million over 10 years to support physicians and the communities they serve across the country.
“Most patients have not shared their resuscitation preferences with loved ones before developing a critical illness, leaving them unable to communicate their wishes,” said Dr. Doug Austgarden, co-creator of ASKmeGOC and critical care physician at RVH. Evidence shows in fact that 75 percent of these patients lack decision-making capacity at the time of ICU admission.
“Family members are often placed in the very difficult and stressful situation of making life-and-death decisions urgently without knowing the patient’s values and preferences.”
Despite how critical these conversations are, there is no standardized practice for

clinicians to follow – until now. The evidence-based ASKmeGOC tool is the first of its kind in Canada, bringing structure and consistency to how providers can approach care plans proactively with patients, before an acute health event occurs.
Dr. Chris Martin, co-creator of ASKmeGOC and RVH chief of critical care, said patients often feel relieved after they’ve gone through this process. During the pilot study – Canada’s largest randomized clinical trial conducted in a community hospital – patients reported feeling that the tool gave them the right amount of information to make an informed choice around resuscitation and other invasive ICU interventions.
“ASKmeGOC gives us a way to bring
clarity, compassion and structure to those moments, so patients feel seen, heard and supported,” Dr. Martin said. “It’s not just about planning care, but about building trust and ensuring that what matters most to the patient is always at the centre of the discussion.”
To evaluate the new solution, RVH clinical researchers enrolled more than 1,900 patients over the age of 80 for one year, ending October 2024. They found that 62 percent of patients who used the tool changed their status – and in nearly every case, it was a “de-escalation of care.”
Stemming from these preferences, the study highlighted tangible results when comparing the ASKmeGOC group to a control group. They include:
•Nearly 30 percent fewer days spent in the ICU
•Nearly 60 percent fewer days spent on ventilator
•Total direct patient care costs dropped by $80,000
The solution is also designed to alleviate burden on physicians, a goal that the Health Care Unburdened Grants are meant to inspire.
It provides a reliable foundation for non-physician providers to step in and have systematic conversations with patients who are at higher risk of adverse events – and record their preferences for resuscitation in advance. Dr. Austgarden said this shared team approach enables physicians to reallocate time to direct patient care. At RVH, this service is now delivered by a dedicated team of ICU nurses that is trained in best practices.
Since RVH implemented ASKmeGOC, feedback has been overwhelmingly positive. Patients and family members who have heard about the tool are asking to take part in their own goals-of-care discussions, and physicians and staff who have seen its impact are requesting it for their patients. There have also been many requests to expand into outpatient settings, leading the team to adapt the tool accordingly.
“I think this reflects the fact that patients want the opportunity to express their wishes and participate in developing their individualized care plan,” said Dr. Austgarden.
While the tool is now rolled out across the hospital, the Healthcare Unburdened Grant allows RVH to spread and scale ASKmeGOC far beyond its borders. They are now partnering with nine additional sites, including acute care hospitals, community clinics and assisted living facilities – bringing this important service into a broad range of clinical settings.
Cardio software shared among four hospitals ensures region-wide access
BY NORM TOLLINSKY
The Simcoe Muskoka Regional Heart Program at the Royal Victoria Regional Health Centre, in Barrie, Ont., is one of 20 cardiac care centres in the province and a recognized leader in embracing its regional mandate.
Ontarians experiencing cardiac events and requiring emergency care in smaller communities within a range of 125 kilometres of Barrie either call 911 for immediate transportation by ambulance to RVH or show up at Muskoka Algonquin Healthcare sites in Huntsville and Bracebridge, Georgian Bay General Hospital in Midland, or Collingwood General and Marine Hospital.
Several years ago, Muskoka Algonquin Healthcare integrated with RVH’s instance of Philips Cardiovascular Workspace software (previously IntelliSpace Cardiovascular, also known as ISCV). In 2024, Georgian Bay General Hospital integrated with RVH’s instance of Philips
Cardiovascular Workspace software and IntelliSpace ECG (ISECG), while Collingwood General and Marine Hospital adopted only the Cardiovascular Workspace software. This strategic collaboration marked a significant milestone in advancing cardiac care across the Simcoe Muskoka region.
Before integration, many processes –such as scanning ECG results or transferring rhythm strips – were manual, creating delays and opportunities for errors. This integration delivers significant benefits, including streamlined access to cardiac data across sites, faster diagnostic workflows, improved collaboration among clinicians, and improved patient care.
Having access at RVH to a patient’s historical ECGs, echocardiograms, stress test and Holter test results in the Cardiovasular Workspace software can also be helpful if the patient does at some point have a cardiac event. “Previously, we had no visibility into whether an ECG or echocardiogram had been completed be-
cause the information wasn’t shared,” said Amy Bellisle, RVH’s regional manager of clinical informatics.
“What RVH is doing to embrace its regional mandate is something that other regions in Ontario are only limping towards,” remarked Andrew McClure, a Philips cardiology specialist. Some regional cardiac care centres have
Streamlined access to cardiac data across sites has resulted in improved collaboration among clinicians.
made a similar commitment to integration and interoperability, but others have been slow to extend their cardiac care software to smaller hospitals in the region they serve.
By sharing RVH’s instance of Philips software, the participating hospitals were able to acquire Philips ISCV and ISECG with significant cost efficiencies com-
pared to purchasing them individually. In addition, leveraging RVH’s dedicated cardiac informatics team – a highly skilled group of four specialists – enabled hospitals to achieve economies of scale.
“By leveraging a shared instance and RVH’s cardiac informatics expertise, we’ve enabled participating hospitals to achieve cost efficiencies and operational savings that would not be possible through individual procurement. This model demonstrates how regional partnerships can optimize resources, enhance interoperability, and deliver sustainable value for both clinicians and patients,” said Sarabjit (Sunny) Singh, RVH’s regional chief nursing informatics officer.
“Usually, hospital informatics teams are responsible for a much broader portfolio,” said McClure. “At RVH, the informatics team has a deep knowledge of cardiology and a lot of experience with the Philips software. This level of dedicated focus on cardiology informatics is rare across Canada, and it truly sets
From left to right: Dr. Giulio Didiodato, Dr. Christopher Martin, and Dr. Doug Austgarden.







MobileDaRt Evolution MX9 now available in Canada
Building on proven performance, the MX9 elevates mobile imaging with smart innovation. Featuring a 3D camera for confident positioning, in-bucky charging, and an innovative tubehead touchscreen, paired with FUJIFILM D-EVO III glassless detectors for unmatched durability and reliability where it matters most.












University of Toronto students demonstrate AI’s reach at showcase
BY MATT HINTSA
As part of the University of Toronto’s distinctive Master of Science in Applied Computing (MScAC) program, students embark on eight-month applied research internships with companies, hospitals and other organizations.
More than 100 student-led projects were on display at the annual U of T Department of Computer Science’s annual Applied Research in Action (ARIA) Showcase at the Metro Toronto Convention Centre.
One such project explored how AI could make skin health insights more accessible and transparent. Working with ModiFace, MScAC student An Cao developed Digital Dermatologist, an explainable AI system that analyzes selfies to identify visible facial skin concerns and explains its observations through an interactive, conversational interface.
The system links its responses directly to visual evidence in the image, demonstrating how explainable AI could support more understandable, user-friendly health assessments, while addressing common concerns around trust and transparency in AI-driven tools.
AI is also being applied to the biological foundations of disease, where earlier detection with less invasive techniques can have a meaningful impact on outcomes.
In collaboration with the Princess Margaret Cancer Centre at University Health Network, MScAC student Ashka Shah explored a non-invasive approach to lymphoma detection using blood-based signals.
Rather than relying solely on genetic mutations, the project analyzed epigenetic patterns – chemical modifications to DNA that differ between healthy and cancerous

cells – found in fragments of DNA circulating in the bloodstream. The results showed that AI-driven analysis of these patterns could distinguish patients with lymphoma from healthy controls with promising accuracy, supporting a proofof-concept of the potential role of liquid biopsies as a complement to traditional imaging-based monitoring.
Beyond detection, AI is increasingly being used earlier in the therapeutic pipeline to support drug and vaccine development.
Working with Sanofi, MScAC student Ofek Gross applied AI techniques to the design of mRNA sequences used in vaccines and other therapies. While many different genetic sequences can encode the same target protein, they vary in properties such as stability and half-life.
Gross’s project used AI models trained
on millions of known mRNA sequences to generate and evaluate new designs that balance these objectives, illustrating how AI can help researchers navigate complex design spaces and accelerate early-stage therapeutic research.
Personalized treatment is another recurring theme in AI-enabled healthcare, particularly involving the brain.
MScAC student Alex Kappen, working with the Temerty Centre for Therapeutic Brain Intervention at the Centre for Addiction and Mental Health, examined how machine learning could help tailor transcranial magnetic stimulation (TMS) treatments for psychiatric disorders.
By analyzing electrical brain activity recorded during TMS sessions, the project aimed to identify cognitive and emotional states that could inform treatment adjust-
ments in real-time. The findings suggest that AI-based interpretation of complex brain signals could support more adaptive and individualized approaches to brain stimulation therapy in the future.
That focus on early detection and timely intervention also extends to acute care settings. In collaboration with The Hospital for Sick Children, MScAC student Po-Yu (Daniel) Chen explored how AI could help identify early warning signs of deterioration in the ICU.
By analyzing continuously collected physiological data such as heart rate, blood pressure and oxygen saturation, the project estimates risk in real-time, learning patterns directly from longitudinal data rather than relying heavily on manually labelled events. The work highlights how AIdriven risk estimation could support clinicians in fast-paced critical care environments, where subtle changes can precede serious clinical events.
MScAC student Bailey Ng, working with the Centre for Addiction and Mental Health, analyzed large-scale brain imaging and demographic data to explore how patterns of brain connectivity relate to cognitive performance.
Using data from tens of thousands of participants, the project evaluated multiple machine learning approaches to assess which brain features contribute most to predictive accuracy. Although prediction remains challenging, the findings help clarify where current techniques show promise and where further research is needed, laying the groundwork for future studies of cognition, aging and brain health.
Matt Hintsa is a senior media relations & communications officer, Department of Computer Science, University of Toronto.
Connected Care grant-winners are solving problems at the front lines
BY DR. RASHAAD BHYAT
The most impactful transformations in healthcare rarely begin with country-wide rollouts. Rather, they start at the grassroots, where dedicated clinical leaders, patient partners, and health system champions identify local problems and develop practical solutions.
This philosophy drives Canada Health Infoway’s Centre for Innovation in Digital Health (CIDH), an ambitious Centre that supports Infoway’s ongoing national efforts to advance interoperability and Connected Care.
At the heart of the CIDH’s work is its Connected Care Innovation Grant Program, which supports clinical leaders advancing digital health solutions that improve patient care and promote standards-based interoperability.
This year’s Connected Care Innovation Grant cohort demonstrates the impact of this support.
The 2025 grant cycle funded 18 projects across five provinces, focusing on three critical areas: reducing administra-
tive burden, improving health equity, and enhancing data interoperability.
These projects reflect the growing sophistication of Canada’s digital health ecosystem, highlighting strategic applications of artificial intelligence (AI) and a strong emphasis on Indigenous-led initiatives. They also illustrate how local innovations can generate insights and practices with relevance across the health system.
Among the 2025 Grant winners, AI has emerged as a particularly valuable tool for supporting primary care sustainability. The unprecedented pressures facing primary care providers demand solutions that enhance efficiency and reduce cognitive burden.
Many grant recipients are implementing AI-driven documentation tools to streamline workflows and allow clinicians to spend more time with patients.
For example, Dr. Daniel Pepe and Dr. Cassandra Lin-Pepe in London, Ontario, are integrating AI scribes for continuous analysis and structured documentation, while the Pharmacy Association of Nova Scotia is using AI scribe technology to generate standardized patient sum-
maries, supporting pharmacists in collaborative, team-based care.
Meanwhile, the Edmonton North Primary Care Network is leveraging AI to triage, document, and summarize nonurgent requests for specialist advice from primary care providers.

Dr. Rashaad Bhyat
Dr. Neil Naik’s clinic group, working with Amplify Care in Waterloo, is integrating AI-powered virtual receptionists with EMRs to manage patient calls more efficiently. Collectively, these innovations are not only improving clinical workflows but creating adaptable models that can inform practices across settings and teams.
When speaking with the Grant winners directly, we’re already seeing the practical benefits of these solutions on the front lines.
As Nazila Afghani, director of care at
long-term care facility, Isabel & Arthur Meighen Manor, shared, “The Connected Care Innovation Grant allows us to bring modern digital solutions directly into daily practice. For our nursing and care teams, this means faster, more standardized documentation that improves both continuity of care and communication across disciplines. Ultimately, this project will strengthen resident safety and quality outcomes.”
Her experience illustrates how tailored, AI-powered digital tools can produce meaningful improvements for patients and care teams alike.
Equity and cultural safety are equally central to the CIDH’s mission. Six of this year’s projects specifically support Indigenous communities, reflecting a commitment to addressing community-specific needs while respecting Indigenous data sovereignty.
In Ontario, Alderville First Nation and Walpole Island First Nation are adopting modern community-based EMRs like Mustimuhw, enabling integrated mental, physical, and social health

AI-driven ultrasound at point-of-care enables more accurate diagnosis
From the heart of London, Ontario, ICU physician Rob Arntfield recognized a need for change in the status quo of respiratory image diagnostics. What began as a medical AI interest research group evolved into what is now Deep Breathe, a medical technology company specializing in lung ultrasound diagnostics. Their deep learning-enabled, lung ultrasound diagnostic platform, ATLAS, supports rapid and accurate assessment of respiratory conditions at the point-of-care, in any setting.
Let’s use the example of pneumothorax (a collapsed lung). Imagine you’re a patient in the hospital with concern for this commonly investigated condition. Typically evaluated using a chest X-ray (CXR), and patients and staff alike presume this is the most efficient and accurate approach.
However, with turnaround times of 60120 minutes and accuracy as low as 46 percent for this life-threatening condition, it turns out we have lost track of the opportunities afforded by portable, non-ionizing and hyper-accurate ultrasound of the lung.
Deep Breathe was built to bring the best technology to the patients and providers who deserve better.
Deep Breathe changes the plot line of this story as their technology brings diagnostic imaging directly to the point-of-care, with no CXR wait times and expert processing required.
It also offers 94 percent accuracy (according to published articles, including “Computers in Biology and Medicine” and “Chest”) for the detection of pneumothorax and instant results, so that patients can learn what comes next in their care without delay.

The company’s mission has always been clear: to identify the key barriers to adopting point-of-care ultrasound (POCUS) across hospital and pre-hospital environments (like EMS and the military) and to bring the highest standard of diagnostic care directly to the patient.
It’s a mission shaped by real clinical challenges where time, expertise, and access make all the difference.
“In critical care, minutes matter. Delayed diagnosis can mean the difference between stabilization and decline. Deep Breathe’s technology gives physicians like me the access to instant, accurate bedside answers, transforming how quickly and confidently we can respond to respiratory emergen-
cies,” said Dr. Ross Prager, Deep Breathe’s clinical lead and an ICU physician.
Through built-in guidance tools and AI-powered detection, the platform can identify conditions that would typically require physicians with more than five years of specialized training.
By adopting a solution that not only streamlines workflow but also improves diagnostic accuracy, physicians can save time, reduce costs, and conserve resources, all while enhancing patient outcomes. These capabilities reflect the work of a team deeply rooted in POCUS, software development, and machine learning.
This past October 2025, the company achieved a significant milestone – its first
U.S. FDA 510(k) approval of a foundational diagnostic model within their platform. This validation highlights that its vision is backed by deep competence in science, research and organization.
Companies like Deep Breathe rely on the support of strong partnerships with leading clinicians, hospital networks, and accelerator and incubator programs.
They’ve played a crucial role in validating the technology, shaping workflow integration, and supporting adoption along the way.
Such programs as the U.S. Army’s xtech International competition, where Deep Breathe placed first among 150 international companies, highlighted its capacity to impact frontline care in any setting.
Across Canada, this work is gaining recognition and support through involvement in national incubator and accelerator programs, including Deep Breathe’s recent selection for the government of Canada’s Innovative Solutions Canada (ISC) Testing Stream and the NATO Defence Innovation Accelerator for the North Atlantic (DIANA) 2026 Challenge Programme.
Step by step, these achievements and partnerships are helping move instant, accurate diagnostics toward real-world clinical and field practice.
“My obsession as an ICU physician has always been to assure the best technology can reach the sickest patients. I founded Deep Breathe to strap nitro boosters to this vision, allowing rapid and portable diagnostics for life altering conditions to be delivered by virtually anybody in any environment,” said Dr. Rob Arntfield, CEO and founder of Deep Breathe, and director of ICU at the London Health Sciences Centre.
Artificial intelligence is now the backbone of the DI department
BY JEFF VACHON
CHICAGO – Another remarkable RSNA 2025 wrapped up last December, and one message was impossible to miss: artificial intelligence has officially moved from the periphery of radiology IT to the very centre of the ecosystem.
Walking the AI Showcase and vendor halls, the story was no longer about how many AI tools exist, but how deeply AI is now embedded across every layer of the radiology workflow. From image acquisition and triage to advanced analytics, reporting, and enterprise governance, AI has become a foundational element of modern radiology infrastructure.
AI has moved from bolt-on to builtin: One of the most striking trends at RSNA 2025 was how vendors are embedding AI directly into RIS/PACS, workflow orchestration, and reporting systems. AI is no longer positioned as an optional add-on or a standalone application. Instead, it is becoming foundational to how radiology informatics applications are designed and deployed.
This architectural shift is critical. When AI lives inside the core systems ra-
diologists already use, it becomes part of the natural diagnostic workflow rather than an extra step. The result is smoother adoption, greater consistency, and a far more meaningful clinical impact.
Radiology IT is evolving into an intelligent, AI-native ecosystem rather than a collection of loosely connected tools.
Moreover, algorithms now span detection, quantification, triage, workflow optimization, reporting, and predictive analytics. What began as isolated, singlepurpose applications has grown into an unprecedented breadth of innovation.
Nevertheless, RSNA 2025 also highlighted a necessary next step: consolidation. Health systems are increasingly moving away from fragmented point solutions toward large, integrated multi-algorithm platforms. These platforms are designed to support entire diagnostic pathways rather than isolated tasks.
This shift represents a major maturation of the AI landscape. Enterprise-scale platforms enable standardized integration, consistent user experiences, centralized governance, and reliable performance across sites. In short, they make AI scalable and sustainable in real-world radiology environments.
AI is reshaping radiology reporting: At RSNA this year, it was clear that AI is moving beyond simple assistance to become a powerful driver of augmented structured reporting.
AI systems are now capable of generating measurements, identifying findings, and producing guideline-aligned content before the radiologist even begins dictation. Radiologists can then review, validate, and refine AI-generated content rather than starting from a blank page.

The impact is significant: faster reporting, greater consistency, improved adherence to standards, and higher overall report quality.
Rather than replacing the radiologist, AI is emerging as a true co-pilot – handling repetitive and structured elements while allowing radiologists to focus on complex interpretation and clinical judgment.
Workflow automation is accelerating: Workflow automation was everywhere at RSNA 2025. Smart worklists, intelligent triage, context-aware prioritization, and automated clinical pathways are rapidly becoming the norm.
The objective is clear: reduce friction, improve throughput, and give radiologists the time and cognitive space to focus on the most challenging diagnostic tasks. As imaging volumes continue to rise and staffing pressures persist, AI-driven workflow orchestration is no longer a luxury, it is an operational necessity.
Quality and benchmarking: Organizations are increasingly focused on quality, consistency, and benchmarking. They want to understand how algorithms perform across sites, use cases, and patient populations. changes over time. This is precisely where the Bialogics AIQ Quality Framework plays a critical role. By enabling transparent, continuous performance monitoring across algorithms and clinical settings, AIQ provides the objective analytics needed to build trust, support governance, and ensure AI delivers real clinical value.
Jeff Vachon is the president of Bialogics.
Jeff Vachon


More than an image. The big picture.

Work connected. Work confident. Work in balance.
AGFA HealthCare’s Enterprise Imaging Platform brings everything together — blazing-fast streaming, smart orchestration, embedded AI, deep clinical integrations, and flexible deployment in the cloud or on-premises.
Built for precision, personalization, and simplicity, it creates a connected ecosystem where radiologists stay focused, IT teams cut complexity, and care teams collaborate with clarity.
Whether reading on-site or remotely, managing growing imaging volumes, or expanding across specialties, Enterprise Imaging adapts to your environment — and evolves with you.

Discover what imaging looks like when everything just works at HIMSS. agfahealthcare.com/himss
That’s life in flow.
AI-driven platform combines scribes, decision support and workflow
MARKHAM, ONT. – Family physician Dr. Paul Forman has developed an AI-powered platform that transforms the way primary-care physicians document and reason through patient care – improving medical office productivity, reducing stress on doctors, and improving patient care.
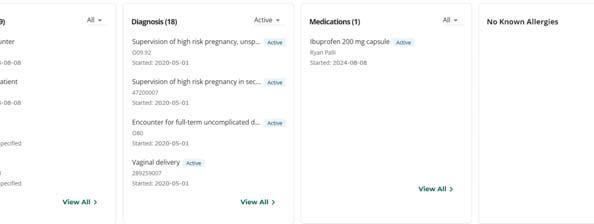
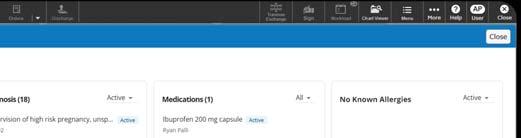
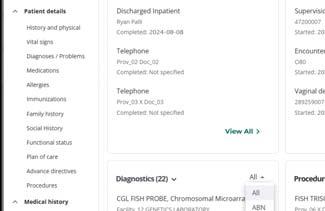
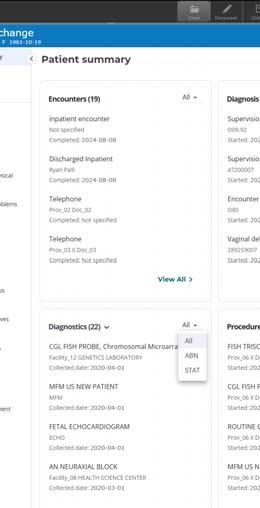
Called Alifor Clinical Decision Support, the system acts as both a digital medical scribe and a real-time clinical assistant –automatically capturing encounters, generating a complete SOAP note and Cumulative Patient Profile (CPP), and cross-referencing them against verified Canadian medical guidelines, journal evidence, and regulatory standards in seconds.
“It’s like having a specialist in the room with you,” said Dr. Forman.
Developed in collaboration with an AI programmer experienced in OpenAI’s technology, Alifor was refined in Dr. Forman’s own busy Markham, Ont. family practice, where he and his wife, Dr. Leandra Forman, work alongside two registered nurses.
The system mirrors the workflow he honed over 30 years in South Africa and across Saskatchewan, Alberta, and Ontario. It gives doctors an instantly familiar interface that complements real-world primary-care demands.
Beyond decision support, Alifor automates the administrative side of practice.
Tasks that previously took 20 minutes – such as composing a credible SOAP note and CPP – are now completed in under a minute.
“Since using Alifor, I leave on time every day and never work at night,” said Dr. Forman. “I can comfortably see 30 patients a day, and everything is done in-clinic.”
Beyond a scribe – Cognitive decision support: While many AI scribes simply record encounters, Alifor goes further. It reasons the way clinicians do – cross-referencing Canadian guidelines from Hypertension Canada, Diabetes Canada, the Canadian Task Force on Preventive Health Care and other sources – and suggests relevant questions, therapies, and follow-ups during the encounter.
“It’s really designed to duplicate the way a doctor thinks,” explained Dr. Forman. “Instead of creating more doctors, you expand the cognitive capacity of every doctor and reduce burnout. It’s about restoring the joy back to Family Medicine, which is what we have achieved.”
The result: fewer unnecessary referrals and stronger in-house care, as physicians have the Canadian guidelines at their fingertips.
Dr. Forman notes that even a modest reduction in unnecessary referrals – for example, from 10 to seven per day per clinic – could yield significant provincial savings and faster access for patients who truly need specialists.
Enhancing team-based care: Alifor also strengthens Family Health Teams, identifying how nurses, dietitians, physiotherapists, and other allied professionals can contribute to the patient’s plan. Nurses now capture the Subjective portion of the SOAP note, charting reasons for visit and symptoms, a workflow that makes their role more engaging and clinically aligned.
“My nurses find the work far more interesting than simply taking vitals,” he said. “It builds team morale and shared ownership.”
Measuring the Quintuple Aim: The system quickly provides feedback to the doctor on whether these goals have been met in the encounter – helping ensure care stays aligned
with the principles of the Quintuple Aim: improving patient experience, supporting provider well-being, advancing population health, lowering per-capita costs, and promoting health equity.
A smart assistant, not a replacement: While capable of analyzing thousands of data points in moments, Dr. Forman stresses that Alifor enhances rather than replaces physician judgment.

Dr. Paul Forman
“I built the system around deliberately conservative principles: The AI can reason, but it does not act. It supports clinical judgment; it never replaces it. It makes thinking more explicit and auditable, not faster at the expense of safety. The clinician remains visible, accountable, and in control.”
He added, “It’s a cognitive assistant that helps every healthcare provider practice at the top of their game.”
The Alifor app is being offered to Canadian physicians at an accessible subscription rate, available for Mac iOS and Android devices. It delivers a secure, guideline-anchored system that unites documentation, decision support, and care coordination in one tool.
To learn more about Alifor and its Canadian primarycare vision, visit: alifor.ca.
OntarioMD helps prepare digital-ready teams and patients
BY DR. CHANDI CHANDRASENA, SIMON LING, REZA TALEBI
AND DR. ABBAS ZAVAR
Across Canada, primary care clinics are feeling the strains of administrative burden, fragmented workflows, and limited interoperability.
A 2024 survey by OntarioMD (OMD) to gauge technological burnout among more than 1,500 physicians confirmed what many already knew: documentation tasks, varying processes and siloed data are impacting clinician capacity, continuity and morale.
To address this issue, OMD proposes a pragmatic vision for the modern, digitally optimized medical practice, built upon four pillars: Empowered, Connected, Streamlined, and Supported. This vision outlines the characteristics of a high performing and digitally enabled team, drawing from our collaboration with community clinics, insights from clinician surveys and expertise with change management and digital solutions via our Peer Leaders and OMD Advisory Staff.
Rather than chase one-off tools, the vision offers clinics a path toward dismantling silos and building bridges, aligning with provincial and pan-Canadian interoperability efforts while staying grounded in the realities of daily patient care.
This four-part editorial series will delve into each vision pillar, beginning with Empowered clinics (the human founda-
tion for any serious digital or AI agenda), and followed by Connected (interoperability), Streamlined (workflow design and automation) and Supported (managed digital services and infrastructure). Together, they provide a scalable and sustainable blueprint for vendors, policymakers, and health system leaders in collaborating with clinics on tangible solutions.
“Empowered” comes first: The definition of a digitally optimized clinic is not how many tools it has, but whether its people can use them confidently, consistently and safely. The culmination of OMD’s research points to gaps in digital and EMR skills, heavy workloads, role ambiguity and limited capacity to change workflows as the biggest barriers to adoption – even with available and fully funded technologies.
Digital tools alone will not improve a clinic. There is also no “one-size-fits-all” solution that can be applied to all clinics. Quite simply, a team is what is needed for a clinic to be truly empowered and digitally optimized, and many clinics do not yet function as one. Success starts by working together to outline and redefine roles and responsibilities related to staff, clinicians, and the clinic, using technology as a support to strengthen collaboration and make workflows more efficient.
In this context, “Empowered” clinics are those that deliberately build capability, clarity, and confidence across their workforce and patient community, where: •Roles and responsibilities for staff,
clinicians, and the clinic are re-evaluated to enable a shared goal.
•Digital literacy is embedded within these roles.
•Role-specific training and micro-credentialing are available for clinicians, medical office assistants (MOAs), and other staff.
•Patients receive targeted support to learn about and navigate digital tools.
This is not easy work. Insights from OMD surveys show that ease of usability correlates with less burnout and higher perceived value of digital tools – a sign
A digitally optimized clinic is not defined by how many tools it has, but by whether its staff can use them well.
that investing in skills, design, and support is itself, a burden reduction strategy.
Building a digitally ready workforce: For many clinics, structured, role-based training serves as the starting point. Within the Empowered pillar, clinicians and staff are encouraged to systematically use EMRs and digital tools to support decision making and enhance quality improvement. Achieving these goals requires multi-pronged empowerment strategies to address these areas: •Digital literacy and EMR proficiency: core skills in documentation, ordering, task management and data use, tailored
by individual roles and practice models.
•Micro-credentialing and modular training: short, focused learning units for physicians, nurses, staff, and MOAs that can be stacked over time and tailored to each clinic’s strategic goals.
•Human resources planning: hiring, onboarding, and performance expectations that incorporate digital competence as a primary focus in a team-based environment.
To facilitate the building of a digitally ready workforce, OMD can assess a clinic’s readiness and identify capabilities on which to build and expand, using digital health maturity concepts.
Through the OMD Educates program (omdeducates.com), we offer a range of educational opportunities including webinars, hands-on workshops, eCoaching modules, communities of practice, and project-based learning tailored to the diverse roles within the circle of care. These offerings are designed to meet the digital health learning needs of clinic staff, nurses, and physicians, supporting them in building confidence and competence in their day-to-day practice.
An Empowered workforce also benefits vendors and system partners as they can roll out more sophisticated solutions with a trained team on the ground to safely adopt them.
Patients as digital care partners: Empowerment is not limited to staff. In a digitally optimized clinic, patients are
BC conducts large-scale trial of six different AI scribes for care providers
mon barriers to scale: the need for individual clinicians or departments to independently assess vendor compliance and risk. Enterprise support and shared accountability with vendors: Scaling AI scribes across thousands of providers requires operational support beyond the technology itself. The BC Scribe Program leverages existing enterprise support structures, including health information management teams and education specialists who traditionally support front-end speech recognition and clinical dictation tools.
These teams provide onboarding, training, and workflow optimization, ensuring that third party AI scribe solutions are implemented consistently and safely. Vendors are assigned clearly defined roles and responsibilities, including technical support and issue resolution, with formal escalation paths between enterprise support and vendor customer support. This shared accountability model for technology support helps mitigate organizational risk in unmanaged BYOAI environments.
Enabling responsible market entry through a new private public partnership model: Beyond clinical evaluation, the BC Scribe Trial is also testing a new public–private partnership model for AI adoption in healthcare. AI companies have historically faced significant barriers to entering Canada’s publicly funded healthcare market. Through PHSA and the BC Scribe Program, B.C. has established a structured entry pathway that enables vendors to test, refine, and scale solutions within a controlled public-sector framework.
For vendors, the model provides access to clinical scale and diversity – across thousands of providers, multiple specialties, and
Cancer survivors
CONTINUED FROM PAGE 6
expansion. The initiative aligns with Ontario’s Childhood Cancer Care Plan: A Roadmap for Ontario 2024-2029, which prioritizes optimizing survivor well-being through improved access to treatment histories and continuity of care.
Looking ahead: POGO is proud to bring Passport for Care to Ontario, where it will ultimately be integrated into the seven POGO AfterCare Clinics, and to help facilitate adoption Canada-wide. By working closely with ACCESS and our clinical partners, POGO is empowering childhood cancer survivors to have the information and tools they need to make informed decisions about their health.
As the Ontario pilot moves forward, stakeholders are focused on sustainability, evaluation, and scale-up. With support from the Ontario Ministry of Health, ACCESS, and survivor communities, Passport for Care is poised to become a cornerstone of survivorship care in Canada.
For survivors, it means no longer navigating the future alone. For clinicians, it means better tools and less manual work. And for Canada, it means a bold step toward equitable, modern, and compassionate care for every child who has faced cancer.
Lauren Ettin is CEO, Pediatric Oncology Group of Ontario (POGO).
several EMR environments – while aligning product development with public-sector requirements. The trial has become a “living lab” for vendors to test different communication, marketing, product design interventions, all while learning from each other in a competitive environment.
From BYOAI Risk to Opportunity: As generative AI continues to evolve, healthcare organizations face increasing pressure to
distinguish between unmanaged consumer tools and institutionally supported AI solutions. The BC Scribe Trial offers a practical, governance-led response. By combining large-scale evaluation guided by a national framework, standardized contracts, enterprise support, and clear accountability structures, the program reframes BYOAI from a compliance risk into an opportunity for responsible system-wide adoption.
Dr. Angel Arnaout is a surgical oncologist, professor of surgery, scientist and chief medical informatics officer at Provincial Health Service Agency in BC. Dr. Maximillian Besworth (PhD) is an adjunct professor at the University of British Columbia and PHSA senior director of medical informatics. Naomi Brooks is the senior executive director for Lower Mainland Health Information.
MIIT 2026
Friday, April 24, 2026 8am 5pm
Liuna Station
360 James St. N. Hamilton, Ontario
Register now
Early bird pricing until April 1 $100 individual / $80 per person for groups (5+)
Breakfast + lunch + coffee/snacks included
Learn more & register: www.miit.ca

Canada’s Medical Imaging Informatics Conference.
Local. Practical. Connected.
Learn what’s next in imaging informatics – right here in Canada. Join us for a full day of practical insight, emerging tech, and realworld problem solving – built for imaging leaders, informatics teams, IT, and clinicians.
FEATURED KEYNOTE
Dr. Woojin Kim (Chief Strategy Officer & CMIO, HOPPR; CMO, ACR DSI)
“The Promise and the Pitfalls: Navigating Generative and Agentic AI in Medical Imaging”
ON THE AGENDA
• Agentic AI & foundation models in radiology
• Imaging informatics best practices & career planning
• PanCanadian updates, cybersecurity, and more
• Vendor talks + networking (with prize draw)
• Interoperability standards that actually work
NETWORK + LEARN IN A WELCOMING COMMUNITY
Meet – and learn from – leaders, faculty, and peers in an inclusive, welcoming environment. Stay after the meeting for the networking event and keep the conversation going.
Can AI clinical co-pilots break open Canada’s EMR ecosystem?
AI co-pilots offer a credible chance to reset competitive dynamics and reduce clinician burden.
BY WILL FALK AND KELDON BESTER
now has a credible path to disrupt Canada’s electronic medical record (EMR) markets. Not through wholesale replacement, but by working above and beside existing systems. Ambient scribes and second-screen clinical decision support (CDS) tools are already changing the lived experience of care without ripping out core infrastructure.
Ambient scribes are used by more than 25 percent of Canadian primary care physicians and adoption is accelerating in both ambulatory and hospital settings. Several hospitals are deploying rapidly by relying on OntarioMD and Infoway procurement agreements as safe harbours.
About 20 vendors have been vetted for security, privacy, liability coverage, and enterprise readiness. Major international players not on those lists, including Microsoft Dragon and Heidi, have entered anyway.
Concurrently, best-in-class CDS tools have arrived through a different route. Products like OpenEvidence and Doximity operate without personal health information, live on a second screen, and don’t integrate with EMRs.
That no-PHI, no-EMR design choice has enabled fast adoption. Doximity’s acquisition of Montrealbased Pathway.MD for US $63 million shows that Canadian technology is part of this story. Vendors claim that more than 40 percent of U.S. physicians are regular users.
Canadian usage data are unavailable; anecdotally they are already widespread. They are a safer and more reliable substitutes for foundation AI models or the Internet.
Late 2025 moved quickly. First, the mainstream EMR vendors validated the model. Epic and Oracle Health (formerly Cerner) announced that their nextgeneration platforms will include ambient documentation and advanced CDS (by 2026).
Wolters Kluwer announced partnerships for UpToDate to move beyond static reference. Second, scribes and CDS converged. Doximity already had a scribe and a dialer, when they acquired Pathway. OpenEvidence added a scribe and a dialer. Canadian vendors such as Tali.ai and Microsoft Dragon have
announced functional expansions. The result is the emergence of a “clinician co-pilot”. These systems combine ambient documentation, second-screen CDS, and a growing list of functions.
They can prepare patient summaries before visits, support patient communication, coach clinicians during encounters, provide translation services, draft notes, referrals, prescriptions, and sick notes, and verify clinical decisions against current evidence.
Crucially, they do this without needing to replace


the EMR. They intermediate information flow, reduce documentation burden, and offload cognitive work. The EMR remains the system of record. The co-pilot becomes the system of work.
In Ontario, several hospitals have now stated explicitly that any scribe on the OntarioMD list may be used immediately in hospital settings without further local approvals.
That effectively allows co-pilots to operate across both acute and ambulatory EMRs. For the first time, a single clinical layer can span systems that have historically been kept apart.
This is disruptive given Canada’s EMR market structure. Both acute and ambulatory markets are three firm oligopolies. In acute care, Epic, Oracle Health, and Meditech dominate hospital implementations.
In ambulatory care, TELUS Health, WELL, and Accuro (owned by Shoppers Drug Mart/Loblaw) dominate. The result looks familiar to anyone with a Canadian cellphone plan: three firms, roughly 80
OpenAI makes major foray into healthcare sector
OpenAI is making a bigger push into healthcare with the announcement of OpenAI for Healthcare, a set of products designed to help healthcare organizations deliver more consistent, high-quality care for patients.
The products are aimed at both healthcare providers and consumers. OpenAI says physicians’ use of AI nearly doubled in a year. Yet many clinicians rely on their own tools because their organizations aren’t adopting AI fast enough, often due to the constraints of regulated environments.
OpenAI for Healthcare helps close that gap by giving organizations a secure, enterprise-grade foundation for AI – so teams can use the same tools to deliver better, more reliable care, while supporting HIPAA compliance.
Some of the features include:
•Models built for healthcare workflows: Highquality responses for clinical, research, and operational work – powered by GPT5 models built for healthcare and evaluated through physician-led testing across benchmarks and real workflows.
•Evidence retrieval with transparent citations: Answers grounded in relevant medical sources –drawing from millions of peer-reviewed research studies, public health guidance, and clinical guidelines – with clear citations including titles, journals, and publication dates to support quick source-checking.
OpenAI also released a set of tools for consumers, enabling them ask medical questions in a more secure environment. They can even connect their medical records to ChatGPT for Health and ask questions about their lab results and other tests.
percent market share, high switching costs, and limited competition.
The Competition Bureau’s 2022 digital health market study documented structural barriers to competition. These include restricted data access that functions as de facto data blocking, procurement frameworks that entrench incumbents, and high switching costs.
Health Canada and its agencies have raised similar concerns. Bill C-72 attempted to address these issues but died on the order paper. More recently, the Competition Bureau obtained a court order to compel records in its investigation of WELL Health’s acquisition of HEALWELL and Orion Health.
The Bureau’s 2024 Competition in the AI Era summit signaled that generative AI changes the competitive calculus across sectors.
The durability of EMR oligopolies has rested on friction. Workflow integration has been framed as synonymous with EMR integration. One vendor, one system, one tightly controlled environment.
Third-party innovation was tolerated at the margins and constrained through contractual, technical, and commercial barriers.
Many startup executives have complained privately about anti-competitive behaviour. A few have spoken publicly. Most stay quiet, fearing retaliation. A clinician co-pilot breaks that logic. If a physician can move from a clinic running Accuro to their inpatient site on Cerner and rely on the same co-pilot in both settings, a new competitive layer emerges. The co-pilot follows the clinician, not the institution. The EMRs’ moat begins to drain.
That shift has several implications. First, it reframes workflow integration. Integration isn’t just embedding everything in the EMR.
Second, it lowers entry barriers for third-party innovation. A co-pilot can compete on usability, intelligence, and trust without displacing the underlying system.
Third, it destabilizes the neat separation between acute and ambulatory markets. Vendors may be able to compete across settings.
Incumbents will respond. When threatened, EMR vendors historically restrict access. With AI co-pilots, this may appear as limits on data read-write permissions unless formal commercial relationships are in place.
Patient safety rhetoric will be deployed selectively to justify blocking data flows that would otherwise benefit patients. Acquisition and suppression of competitors will remain an attractive strategy.
Regulators should anticipate this behaviour and act early, using data portability requirements, interoperability enforcement, and merger review powers to protect nascent competition. New AI features should be loosely coupled.
There is reason for optimism, but only if regulators intervene quickly and deliberately. AI co-pilots offer a credible chance to reset competitive dynamics, reduce clinician burden, and improve patient care.
Will Falk is a retired management consulting partner who spends his time with start-ups and as a public policy fellow at four institutions. He is a contributing editor at Canadian Healthcare Technology magazine. Keldon Bester is Executive Director of the Canadian Anti Monopoly Project (CAMP).
Will Falk Keldon Bester
With partnerships, we can leverage health data to strengthen Canada
BY SHELAGH MALONEY
Canada is at a pivotal moment in its history, facing geopolitical tensions, economic uncertainty, rapid technological innovation, and veiled threats to national sovereignty. Many Canadians, recognizing that we can no longer depend on external partners for goods and technologies, are embracing a feisty independence (‘elbows up’) and a renewed sense of patriotism.
In 2025, the federal government launched an ad campaign to support their ‘Build Canada Strong’ budget that tapped into this groundswell of patriotism and highlighted the government’s plan to build a resilient economic future using Canadian resources and Canadian workers.
What does ‘Build Canada Strong’ mean to digital health? While Canada has the technology to collect, connect, analyze and share health data, our health systems and health data continue to exist in silos. Data governance is fragmented at best, and we have a risk-averse culture and a shortage of the trust required to make significant change.

The problem is not technology – it is culture, governance, and ambition. We simply do not have the financial or human resources to spend our way out of this situation; fundamental change is required. Can we, as a country, find the strength to build a collaborative, connected, Canadian health data system?
The case for ‘yes, we can’ was made by Dr. Anderson Chuck, president and CEO of CIHI, and Dr. Fahad Razak, co-founder of GEMINI and Canada research chair in health care data and analytics at the University of Toronto on the Digital Health Canada podcast episode, Transforming Health Data, Transforming Canada. These leaders articulated a compelling and optimistic vision of what is possible if Canada unlocks the full potential of its health data.
Canadian data is a valuable natural resource: Dr. Chuck argues that Canadian health data – like lumber or minerals –should be classified as an important natural resource. Rather than seeing it only through the lens of proprietary risk, health data should be treated as a shared national asset.
We are all too familiar with the issues around timely access to care, regional disparities, and system inefficiencies. Without a shift away from risk aversion and institutional silos and toward a shared system, no platform or technology can deliver transformation. With that shift, however, the benefits for patients, providers, and the country are enormous.
Dr. Razak shared how Denmark, often cited as a global leader in this domain, thinks about health data. In Denmark, health data is treated as part of national industrial policy. Governance involves not just the health ministry, but also ministries responsible for higher education, economic development, finance, and foreign affairs. Health data is positioned as a
strategic national asset and a cornerstone of the country’s global brand.
Dr. Razak suggests that Canada has a unique advantage and a very strong foundation from which to build this resource.
Specifically:
•Diversity: Canada has one of the most
diverse populations in the world, meaning that Canadian data can be used to develop AI tools and analytics that are globally applicable.
•Single-payer system: Canada has a single-payer system, enabling comprehensive population-level data capture.
•Talent: Canada has world-class scien-
•Scale: Canada’s larger population (42 million) provides the scale needed to develop, test, and grow healthcare solutions more effectively than in smaller countries like Denmark (6 million).
Shelagh Maloney
Diagnostic imaging departments and clinics are steadily moving their PACS to the cloud
By outsourcing, they no longer face astronomical costs to invest in hardware and software.
BY DIANNE DANIEL
Steady growth is predicted for the Canadian Picture Archiving and Communication Systems (PACS) market as healthcare providers across the country increasingly adopt digital imaging technologies and look to create more efficient workflow to deal with skyrocketing imaging demands.
One offshoot is a rise in the number of facilities deciding to move PACS to the cloud, a shift that is opening the door to future possibilities, such as seamless imaging exchange and advanced artificial intelligence (AI) tools, say industry observers. Vendors including AGFA HealthCare, Philips, and Sectra are responding by expanding cloud-based enterprise offerings for diagnostic imaging across the Canadian healthcare sector.
“We went from curiosity around the cloud to commitment,” said Sectra Canada president Nader Soltani, noting that the decision is no longer a choice between on-premise PACS versus cloud, but rather how quickly can healthcare providers move to the cloud and at what scale.
“The cloud is not the destination. The cloud is to enable us all to level up to a platform we can build from,” he added. “It’s not just about getting to the cloud, but it’s everything you’ll be able to do after that’s going to be interesting because otherwise, we’re just going to stagnate.”
Sectra Canada is one of a handful of vendors seeing rapid acceleration in Canada’s cloud imaging market. Early adopters of the Sectra One Cloud enterprise imaging solution include the province of Québec, where all public hospitals are transitioning to the cloud, amounting to roughly 12 million examinations per year; and, the 13 member hospitals making up Ontario’s Enabling Healthcare Across Networks for Central East (ENHANCE) where imaging will be consolidated in the cloud across 13 hospital sites to support collaboration within their radiology, breast imaging and orthopaedic workflows.
More recently, Southlake Health (Southlake) announced its transition to a fully managed Sectra cloud solution, starting with radiology and breast imaging. Southlake vice president, digital health and diagnostics, Amir Soheili, said it made sense to start with cloud-based PACS because the technology has reached a level of ‘digital system’ maturity that other systems like digital pathology have yet to reach.
A leading community teaching hospital in Ontario, Southlake performs roughly 200,000 diagnostic scans per year just in medical imaging. Transitioning to a cloud model alleviates the burden of purchasing and maintaining on-premise hardware –ensuring that patches are done, security is relentless and upgrades are up to speed – as diagnostic loads continue to grow.
At the same time, it provides one unified system for end-users, making it easier to access and share images.
“At the end of the day, when I speak with my users, what’s important to them is: do I get my cases quickly, do I have the functionality that I need to
ware like DVDs and players is replaced with a predictable monthly cost, and the service is there when you need it.
“I think most institutions or health authorities are realizing they don’t want to be in data centre management,” said Tysick, noting that deployment of a cloud-based PACS is typically three times faster, compared to scaling up on-premise solutions.
“You can have a baseline system built in a week and then your deployment time becomes a standard informatics deployment,” he said, adding that speed of deployment was a priority for Schroeder, which went from business consulting to start of a project in less than 60 days and ready for go-live within threeand-a-half months.

have, and does the system function without any glitches,” said Soheili.
Moving PACS to the cloud is a way of ensuring that end-users have the reliability, speed and features that they need.
“If you have an opportunity to go to the cloud, it’s the critical path for success in my mind because the level of effort for on-premise infrastructure management disappears,” he said.
“Philips Canada has delivered PACS as a managed service at both provincial and hospital scale for decades, so for us the move to a cloud SaaS model is a natural evolution, not a leap,” added Nathan Bluvol, head of healthcare informatics at Philips Canada. “With AWS, we supported more than 34 million patient exams exclusively in the cloud over the last 12 months and securely managed more than 134 petabytes of data, including nearly 11 billion medical images and patient records. That experience is helping Canadian facilities move quickly and confidently.”
An August 2025 report by strategic consultant 6Wresearch points to cost, interoperability issues, and data, security and privacy concerns as leading challenges in the Canadian PACS market, along with the constant need to update and upgrade systems as technology evolves. Moving to the cloud alleviates that IT burden, freeing up internal IT resources to focus their efforts elsewhere, such as modernizing their imaging systems by integrating advanced AI and machine learning capabilities.
“There was a time when hospitals were building Fort Knox data centres and putting in all of the bells and whistles and resources required to operate large data centres, but when we think about the cost and effort associated with that, it really is no longer feasible,” said Soheili.
“So, the question becomes, how do you create that balance…where the footprint of the on-premise could be as small as it can possibly be and then you can leverage some of the cloud services that are available,” he added.
Philips Canada is another vendor seeing an increase in PACS cloud adoption in Canada, including a recent implementation at Schroeder Ambulatory Centre, a state-of-the-art, non-profit health centre in Ontario, which was expected to go live in January. The company’s HealthSuite Imaging leverages AWS to provide cloud-based archiving, imaging sharing, diagnostic reading and reporting.
Philips enterprise informatics sales specialist and solutions architect Colin Tysick compares the transition to cloud-based PACS to the decision by consumers to adopt television streaming services –- the constant cycle of upgrading and managing hard-
“AI has the greatest impact when it’s seamlessly integrated into the flow of work, not layered on top of it,” said Omar Sunna, president, North America, AGFA HealthCare. “A cloud-based, fully managed platform creates the foundation for AI to support clinical decision-making and efficiency as imaging demands continue to grow.”
Industry observers note that cloud adoption is rarely a single, uniform step. Supporting healthcare organizations in transitioning at their own pace starting where cloud delivers the most immediate value for their clinical, operational, or financial priorities, and expanding over time has become an important consideration as imaging environments continue to evolve.
“It’s about creating a single enterprise platform that can evolve with each organization,” said
Sunna. “When delivered as a managed SaaS model, it can help reduce infrastructure complexity while supporting security, resilience, and continuous updates. That allows IT teams to focus on higher-value initiatives, while clinicians benefit from a consistent, enterprisewide imaging environment.”
Of note, this approach is already in use, including in the Province of Manitoba which is live on AGFA’s SaaS cloud for its VNA and Universal Viewer, while multisite private providers such as EFW Radiology are also moving imaging workloads to the cloud as part of broader modernization strategies.
EFW Radiology, based in Calgary, recently selected AGFA HealthCare’s Enterprise Imaging Cloud software-as-a-service (SaaS) offering to modernize its imaging infrastructure. Director of IT Eldhose Yoyakki said agility and flexibility were driving factors in the decision to move to the cloud.
“With our current PACS system that is on premise we see hardware dependencies, and the ability for us to scale up is very much limited without capital investment, whereas cloud is a predictable operating expense,” said Yoyakki. “We know this is the cost per study and we don’t need to worry about anything else.”
Users aren’t expected to see any difference as all EFW Radiology imaging modalities move to the cloud, he added, and the IT team can now shift focus from managing security patches and router connections to activities that add value.
“It’s opening the door for other tool sets and functionality we can do in the cloud,” said Yoyakki, adding that the roadmap includes incorporating AI. “That was all in the thought process when we decided to go to the cloud.”
Southlake’s strategy, said Soheili, is to develop AI solutions in partnership with large vendors like Sectra or Meditech, based on appropriate use cases such as helping to triage cases in a busy emergency department so that higher priority needs are brought to the top of the list. Another common use case might be to focus a radiologist’s attention on regions of interest when reporting on an image to speed decision making and improve accuracy.
“It doesn’t matter how much experience you have, we see cases where little things are missed,” said Soheili. “AI can potentially prevent that.”
At Sectra Canada, Soltani believes leveraging AI is necessary to help alleviate the enormous demand on healthcare as imaging demands increase in relation to Canada’s aging population.
The more that AI algorithms are approved for simple use cases, the more they can be applied to relieve pressure and decrease wait times in a busy emergency department, for example.
“We’re going to see an increased load on our care providers and a reduced number of care providers to handle that load,” he said. “AI won’t replace radiologists, but I do believe our healthcare system needs it to help radiologists scale their services to meet the demands.”
Building on the TV streaming analogy, Soltani underscores how cloud solution providers are providing a service that in-
cludes reliable storage, access and performance – just as users expect when they log into Netflix to watch a movie. Nevertheless, hospitals and clinics will still require PACS administrators to take care of data quality and ensure departmental needs are met.
“We’re managing that system in the cloud to make sure you have what you need when you need it, but how you use it
remains the ownership of each hospital,” he said. “You don’t have an IT person managing servers anymore, but they are transitioning to higher-level tasks– they can do different work focused on integrating healthcare solutions into your workflow.”
At Southlake, Soheili anticipates using the Sectra platform as a unified place where all the hospital’s different ‘ologies’ can ac-
cumulate images, including cardiology and digital pathology. Right now, a cardiologist who wants to read both an echocardiograph and a cardiac CT would have to log into different systems, he explained.
“This is where you get into a discussion around best of breed versus unified platforms, and I think yes, best of breed has advantages but a unified platform always wins that argument,” he said.
Despite a snowstorm and flight cancellations, the RSNA show must go on
The 2025 show floor included advances in AI, image-guided therapies, MR, CT, enterprise software and more.
CHICAGO – A snowstorm hit Chicago just before the start of RSNA 2025, resulting in more than 1,400 cancelled flights to the city’s O’Hare and Midway airports. Nevertheless, attendees found a way to North America’s biggest medical conference, hopping onto next-day flights or even driving. Few wanted to miss one of the premier sources of new information about diagnostic imaging trends and technology. Here’s a look at some of the new products and technologies announced at the show – some are still in the approval process with Health Canada and/or the FDA, while others may be works-in-progress.
Siemens
Siemens Healthineers announced what a company spokesperson called “a huge re-launch of the ARTIS lineup, all of them AI-powered.” That group of digital interventional angiography systems now includes eight machines organized into three different families, the Artis genio, Artis icono.explore and Artis icono.vision/Artis pheno.vision.
At the same time, the company released what it calls Optiq AI, which enhances the performance of each new Artis system by improving the image quality through noise reduction. IR is facing more complex challenges, and precision in early-stage treatments of small anatomies is on the rise.
Siemens Healthineers also launched a new set of artificial intelligence (AI)-enabled services to help healthcare providers address a range of challenges, from hands-on image interpretation to complex scenario planning for entire healthcare environments through the use of a ‘Digital Twin’.
To reduce the burden on radiology teams while helping them work more efficiently, a new, vendorneutral services suite has been designed to support radiologists by taking over some of the more mundane processes. In this way, it can mitigate the effects of staff shortages and reduce radiologist burnout. Pilot projects have shown that by using the new AI-enabled solution, radiologists were able to annotate chest CT images up to 25 percent faster and experienced noticeably less cognitive load. The clinical accuracy of the results remained at the same high level, the company said.
As well, Siemens Healthineers is expanding its advisory offering to include the use of AI. The ActExcell Operational Twin combines predictive simulation with expert guidance to help customers improve operational performance. Based on customer-specific data, Siemens Healthineers’ in-house supercomputer simulates future scenarios, and uncovers the most effective improvements and the path to getting there.
Through ActExcell Operational Twin, the company’s advisors can suggest data-informed improvements, explain why certain strategies are preferable, and provide a robust simulation environment before measures are adopted in real-world settings.
Siemens Healthineers also introduced new capabilities for its Mammomat B.brilliant mammography system, advancing contrast-enhanced mammography and biopsy functionality. In addition to generating high-resolution 3D breast images via wide-angle tomosynthesis in only five seconds, the Mammomat B.bril-
liant will now be equipped with a newly developed image reconstruction technique for contrast-enhanced examinations.
If a biopsy is required following a contrast-enhanced finding, the procedure is typically performed using contrast as well, ensuring continuity in diagnostic precision. ClearCEM provides a contrast localizer image for tomosynthesis-guided biopsy, which enables targeting accuracy within ±1 mm, potentially reducing time-to-diagnosis. The combination of ClearCEM-powered scout imaging and tomosynthesis-based targeting within the same compression is designed to strengthen confidence and eases the biopsy procedure.
GE HealthCare
GE HealthCare said that since 2022, it has invested more than $3 billion in research and development, fueling a wave of innovation across equipment, radiopharmaceuticals and cloud and AI-enabled solutions.
Siemens demonstrated ‘Digital Twin’ technology, using a supercomputer to simulate customer sites and to model the effects of proposed changes.
At the recent RSNA, some of the solutions it highlighted included a new photon counting CT (PCCT) system with advanced AI algorithms, called Photonova Spectra, which it calls a major milestone in the company’s CT innovation. (It is U.S. approval pending.)
Built on GE HealthCare’s proprietary Deep Silicon detector technology, Photonova Spectra is designed to deliver remarkable spectral and spatial res-
olution for ultra-high-definition (UHD) imaging with wide coverage, enabling fast acquisition speeds, precise visualization of anatomical structures and enhanced material separation.
According to GE HealthCare, this system is designed to maximize the vast amounts of data provided, harnessing up to 50 times more data than a conventional CT to enable advanced reconstruction techniques and precise outputs with the aim of supporting enhanced clinical decision-making and smooth workflows.
The company also announced its next-generation SIGNA MRI technology, also pending approval at the U.S FDA. A group of systems includes:
•SIGNA Bolt, which will be the company’s most advanced high-field, clinical wide bore 3.0T MRI system. It will combine ultra-high gradient performance, intelligent digital RF architecture, and sustainable design to deliver precision imaging, fast workflows, and clinical-to-research flexibility, all with low energy consumption and operational costs.
•SIGNA Sprint with Freelium aims to broaden access to sustainable and equitable MRI technology. With less than 1 percent helium usage compared to conventional magnets, Freelium is designed to provide effortless sustainability without compromising clinical and operational efficiency.
Both are powered by SIGNA One, an AI-powered workflow platform designed to improve the imaging experience by combining precision with simplicity.
On the mammography front, GE HealthCare showcased the Pristina Recon DL. This solution is GE HealthCare’s advanced 3D mammography reconstruction technology – which it calls the first to combine deep learning with iterative reconstruction to provide outstanding digital breast tomosynthesis (DBT) image quality at a low patient radiation dose. It also demoed the Vivid Pioneer: GE HealthCare’s most advanced and adaptive cardiovascular ultrasound platform. With one-click optimization, AI au-

tomation tools, simplified user interface and a lighter, compact, battery supported system, Vivid Pioneer is designed for extraordinary imaging, workflow, and comfort.
GE HealthCare showed several collaborative projects with AI-chip leader NVIDIA. The company is leveraging NVIDIA’s offerings and expertise in areas of physical AI, high performance computing, and simulation, which has the potential to reduce manual tasks, increase patient comfort, and alleviate radiologist burnout through AI-powered assistance.
Agfa HealthCare
Agfa HealthCare demonstrated advances in a number of systems, including MUSICA Xpert, its next-generation image processing software that offers enhanced contrast, gridless imaging, and selectable image preferences. Its radiologist-centric design was developed with radiologist feedback to reduce retakes and improve diagnostic confidence.
It also showed MUSICA Workstation enhancements that deliver improved cropping and color-coded exam trees, streamlined workflow and enhanced visual clarity. SmartPositioning QA provides preand post-exposure guidance, while cybersecurity has been upgraded with the migration to Windows 11, delivering stronger protection and performance.
In the area of digital radiography, it announced the new SmartGrip system for DR 600 – it enhances fine positioning with smoother motion control and auto-positioning transitions for greater precision and ease of use, the company said.
Canon
Canon Medical gained the attention of attendees with its display of a multi-position CT scanner, a joint-venture with Keio University in Japan. It’s the world’s first CT able to support scanning in the standing, sitting and supine positions.
It has already been launched in Japan, where it has generated significant clinical excitement. As part of a global deployment strategy, Canon is now introducing it to other markets.
The system is great for claustrophobic patients and for assessing musculoskeletal issues in more natural position, like standing and sitting. This may enable better diagnosis of conditions such as knee osteoarthritis and disc herniation – which cause pain when the patient is standing or sitting but not necessarily when lying down, as in a standard CT scanner.
For the first time, Canon exhibited its Photon Counting CT (PCCT), another work-in-progress. PCCT is an advanced diagnostic imaging system using a nextgeneration photon counting detector that captures the energy of individual X-ray photons. Unlike conventional CT, it enables multi-material differentiation and improved quantitative imaging, enhancing diagnostic accuracy.
Its higher resolution also improves lesion detectability at lower radiation doses. Canon said its approach to PCCT is aimed at overcoming the trade-offs and complexity of current-generation PCCT technologies.
The detectors that will equip Canon’s PCCT scanners will be made in Canada by Redlen Technologies, a company based in British Columbia.

Yet another Canon innovation: it continues to combine high-performance angiography with CT.
This advanced multi-modality solution is designed for the future of interventional radiology, combining the Alphenix Sky + angiography system with the award-winning Aquilion ONE / INSIGHT Edition CT scanner (pending Health Canada approval). It enables diagnosis, planning, treatment, and verification in one room, all but eliminating the need for patient transfer between departments.
In addition to improving safety and patient care, the Alphenix Sky + provides the world’s only high-definition flat panel detector with its unique 76 µm pixel technology. The Aquilion ONE / INSIGHT Edition features a 16 cm wide-area detector and includes Canon’s Precise IQ Engine (PIQE) Deep Learning Reconstruction, and AI-assisted workflow experience.
This combination delivers cross-sectional imaging with an ultra-fast 0.24 second rotation speed and wide-area detector, enabling full organ coverage in a single rotation.
For X-ray, Canon introduced new mobile system, Mobirex i9 / Smart Edition. This latest addition to the lineup is equipped with a monitor on the tube head for more efficient radiography workflow. The addition of the Camera Application and Laser Marker options enable Laser Navigation to enhance positioning accuracy. These advanced imaging support functions create an environment that allows the operator to focus more fully on patient care.
In the ultrasound sphere, Canon Medical Systems announced its Aplio i-series / Prism Edition diagnostic ultrasound systems with Innovation 2026. This new release upgrade to be Health Canada approved mid 2026, introduces advanced imaging technologies designed to help clinicians achieve high-quality diagnostic images with greater efficiency.
Canon Medical continues its legacy of leadership in Healthcare IT. They are continuing their innovation in areas like AI and automation, cloud computing, cybersecurity enhancements and enterprise imaging. Their Automation Platform is an AI-based, zero-click solution that uses deep learning for automated CT and MR stroke as well as Chest Pain packages. Vitrea continues to evolve with automated applications designed to streamline workflow using Just-In-Time (JIT) processing.
Christie Innomed
Christie Innomed is the Canadian distributor of DI equipment from Shimadzu Medical Systems, including mobile X-ray carts. The latest iteration, the MobileDaRt Evolution MX9, is a mobile X-ray system designed for use in various hospital settings, including patient rooms, emergency rooms. operating rooms and others. Shimadzu’s mobile X-ray system is known for providing intuitive maneuverability and excellent forward visibility during travel, in this way reducing stress and strain on the operator.
Shimadzu noted there has been an increase in demand for streamlined operations that deliver simplified workflow and reduce the frequency of retakes. Responding to the needs of the clinical environment, Shimadzu offers Vision Support, an imaging function utilizing camera applications. For quality and efficiency, a camera looks for the angulation of the patient in
Philips unveiled the BlueSeal Horizon, calling it the world’s first 3T MRI scanner that operates without helium.
the bed and calculates the geometry for the best image.
Also, the new MX9 includes a tubemounted monitor. This provides a secondary workspace, making it possible to enhance workflow efficiency and provide essential information for dose management.
The MobileDaRt Evolution MX9 Version enhances workflow efficiency with a secondary monitor that conveniently displays patient information, live camera images, and protocol selections right at the operator’s fingertips.
Shimadzu also showed its Radiography system – RADspeed Pro SR5 for radiology suites.
The video image from a camera built into the collimator is displayed on the Xray tube support control panel and highvoltage generator control panel monitors. The optical camera application provides an environment where medical personnel can focus on patient care.
Live View Display supports accurate positioning by showing overlay of detector area, irradiation field and AEC pickup fields, which are difficult to check directly. To reduce repeat exposures, patient body movement can be confirmed from the point that body movement detection mode is activated.
Philips For its part, Philips unveiled a number of innovations, including BlueSeal Horizon, said to be an entirely new MRI that includes the world’s first helium-free 3T magnet. Not only is the scanner more environmentally friendly, as it doesn’t require the limited resource of helium, but it also doesn’t need the vent pipes that traditional MRIs require, meaning it can be sited more easily in hospitals.
Philips said it has led the development of helium-free MRI since 2018, with more than 2,000 of its 1.5T BlueSeal MRI systems installed worldwide, saving more than 6 million liters of liquid helium to date. It’s now bringing these benefits to the more powerful 3T scanner.
The company also announced the launch of Verida, called the world’s first detector-based spectral CT fully powered by AI. Philips said AI optimizes the entire imaging chain – lowering system noise, elevating image quality, and accelerating clinical workflow.
Spectral CT measures how tissues absorb different X-ray energy levels, enabling differentiation of materials that appear identical on conventional CT. Philips has pioneered detector-based spectral CT, delivering multiple spectral results from a single scan with no trade-offs in performance or scan time, the company said.
Now, by integrating AI across the imaging chain, from acquisition to reconstruction, Philips Verida generates better spectral image quality with minimal noise, in addition to high-definition conventional images. With its AI capabilities, it can achieve significant dose reduction without affecting image quality and reduces energy consumption by up to 45 percent.
On the enterprise software front, the company demoed its new Philips Advanced Visualization Workspace (AVW) 16, a vendor-neutral, multi-modality platform designed to help radiologists move ‘from images to answers’ with greater speed and confidence. It includes a new Cardiovascular Suite, which enables clinicians to conduct cardiac CT, MR, and vascular imaging and planning within a unified environment, supporting efficient workflows and customizable reporting.
With the AI-driven workflows and expanded multi-modality clinical portfolio in AVW 16, radiologists are supported in their interpretation of complex studies with speed, precision, and confidence, improving care delivery across cardiac, oncology, neuro, and vascular imaging studies.
According to Philips, by integrating automated workflows, quantitative analysis, and multi-modality view, AVW 16 turns complex imaging data into clear, actionable insights – reducing reading times by up to 44 percent in key applications like longitudinal brain analysis.
Philips also showed its Advanced Visualization Workspace on Philips HealthSuite, powered by Amazon Web Services (AWS). This Software-as-a-Service (SaaS) offering enables care teams to move seamlessly from image to diagnosis, enhancing efficiency and supporting decision-making. By extending advanced visualization capabilities to the cloud, the solution enables healthcare organizations to scale access to advanced tools, reduce IT complexity, and provide secure, anytime, anywhere access to studies.
With Siemens' ActExcell Operational Twin, the company’s advisors can suggest data-informed improvements.

Canadian Healthcare Technology magazine
Canadian Healthcare Technology offers the country's leading healthcare I.T. publications. And they're free to healthcare providers. Get your complimentary subscriptions now!
Canadian Healthcare Technology breaks the news about important projects, programs and technologies, and provides hospital executives and senior managers with an excellent source of information for improving the delivery of healthcare. It’s sent to over 3,900 readers in print format and to over 7,300 opt-in subscribers of the digital edition.

White Papers
eMessenger newsletter
Canadian Healthcare Technology’s e-Messenger contains breaking news about important deals, installations and developments. Four blasts are sent each month, via e-mail, to over 7,100 senior managers and executives in hospitals, clinics and health regions.
Canadian Healthcare Technology’s White Papers are sent out once a month, via e-mail, to over 5,500 senior managers and executives in Canadian hospitals and health regions. The monthly blast contains summaries and links to White Papers issued by various organizations, providing cutting-edge information about topics of interest to healthcare decision-makers.


For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
With partnerships, we can leverage health data to strengthen Canada
tists, with Nobel and Turing prize winners, as well as a deep bench of clinician and healthcare delivery specialists.
No other high-income country has this unique combination. Yet without national data governance and linkage, these advantages cannot be fully realized.
So, what will it take to get us there?
How do we build a modern, pan-Canadian health data ecosystem that connects infrastructure across jurisdictions, enables responsible data linkage, and supports discovery and innovation at a national scale while maintaining public trust and strong governance?
Partnerships, a unified, national approach and a paradigm shift are good starts.
Partnership is critical as no single organization can achieve this alone. Federal and provincial governments, clinicians, researchers, and technology companies, all have critical roles to play. A unified, ‘Build Canada Strong’ approach and effort is the only way to build a digital health ecosys-
Cardio software
CONTINUED FROM PAGE 8
RVH apart as a leader in regional cardiac care,” said both Singh and McClure.
The ISCV software features a dashboard with a cardiology timeline, a graphical, panoramic, and chronological overview of a patient’s cardiovascular care continuum. The timeline functions as a patient-centric, comprehensive repository of cardiovascular information.
It allows cardiologists to view multimodality images and reports in the same workspace, streamlining clinical workflow, improving operational performance and enhancing patient care.
“Having everything in one place is far more convenient,” asserted McClure. “You log in once and you can see everything. If you had to sign in to three separate accounts, it would be unnecessarily timeconsuming.”
Cardiologists seeing evidence of atrial fibrillation in an ECG will want to have a
Ontario MD helps
CONTINUED FROM PAGE 14
treated as partners, not passive recipients. In this respect, the Empowered pillar calls for:
•Patient literacy programs to address inequities in accessing and understanding digital tools, portals and virtual care, including language, accessibility and connectivity barriers.
•Access to external learning resources from trusted provincial and national organizations that reinforce what patients hear in clinic, making it easier to self manage between visits.
•Patient-facing processes with clear clinic goals and boundaries to ensure patients and staff know what to expect from digital channels and information management.
Empowerment as the foundation for AI: The question, “Are we ready for AI?”,
tem that will respond to today’s pressures and allow us to address future crises and opportunities.
We have seen some good examples of partnerships and pan-Canadian collabora-
Partnerships are critical, as no single organization can build the national, health data ecosystem alone.
tion recently. For example, Digital Health Canada was one of 30 health organizations that jointly responded to Innovation, Science and Economic Development Canada (ISED) Consultation on the Next Chapter of Canada’s AI Leadership.
A unified, national approach could reduce fragmented, duplicative investments that dilute impact and prevent Canada from achieving the scale required for global competitiveness. In a rapidly evolving AI and data landscape, speed is important; a ‘build once, serve all’ mindset will allow us
look at the patient’s echocardiogram, and if they see a pacemaker wire in the echo, they’ll want to go into the cath lab management software, XperIM, for further information.
So with ISCV, everything is easily accessible.
Philips’ XperIM software is only located at the Royal Victoria Regional Health Centre, the site of the region’s only cath lab.
However, the extension of the Philips software allows access to cardiac tests in one workspace regardless of where the tests were performed.
“The integration of these systems has transformed our cardiac workflows at RVH,” said Lori Vajda, operations director, Simcoe Muskoka Regional Heart Program. “They have streamlined documentation, reduced redundant data transfer, and enabled faster, more informed clinical decision making.”
She added that, “The ability to access patient data from anywhere has improved collaboration across our teams and ultimately enhanced patient care.”
is top of mind for clinicians and policymakers. The answer is to begin with Empowerment.
The use of AI tools, such as AI scribes, does not guarantee reduced burden or full accuracy. It is also unlikely that AI tools will be trusted if users are exhausted, unclear on roles, lack skills, and are unsupported when things go wrong.
In an Empowered clinic:
•Teams have baseline digital fluency, so AI tools are introduced as an evolution of existing workflows rather than a foreign imposition.
•There is clarity on responsibilities –for example, who verifies AI-generated content and resolves exceptions, how risks are escalated, etc. – rooted in the clinic’s mission and governance.
•Staff and patients are confident in identifying problems early, providing feedback, and participating in frequent calls for improvement.
A call to action: Empowered clinics
to move faster. Continuous improvement, close collaboration between innovators and policymakers, and a willingness to adapt are critical.
Invest in health system sustainability: Health spending is growing at roughly 4 percent annually – an expenditure that only allows us to maintain the status quo. Strategic investment in digital infrastructure, even at significant scale, would pay for itself many times over if it slowed cost growth even marginally. Furthermore, decisive action on health data will:
•Improve health equity, by using digital tools and better data to serve marginalized and underserved communities.
•Grow the economy by creating highquality jobs and generate economic value.
•Maintain data sovereignty, which may be at risk if Canada cedes control of its health data to foreign platforms and jurisdictions.
•Open up access to innovation. Countries that move faster on data will gain earlier access to new therapies and technologies.
As a national member-driven association, Digital Health Canada is committed to advancing Canada as a confident, global contributor. We will continue to work with existing partners, forge new partnerships, and advocate for decisive action in support of a paradigm-shift in thinking about health data. Build Canada Strong is good for Canada and is good for healthcare.
Shelagh Maloney is CEO of Digital Health Canada.
Connected Care grant-winners at front lines
records that improve coordination across programs.
In British Columbia, the Squamish Nation’s Detox and Treatment Navigator is streamlining referrals for addiction treatment, and Dilico Anishinabek Family Care in Fort William is expanding the use of remote Televu smart glasses to enable realtime specialist input, overcoming geographical barriers for chronic disease and
UHN is applying LLMs to extract social determinants of health from clinical notes, enabling more support.
wound care management, lowering the risk of amputations.
As Jessica Pace, Knowledge Program Manager at Indigenous Diabetes Health Circle, explained, “This grant will allow IDHC to facilitate sharing circles within communities to better understand the needs and concerns of our clientele in relation to the Electronic Medical Record (EMR) use. The knowledge share in the circles will help IDHC to create accessible
are not a happy accident, but the result of a deliberate investment in a team (clinicians, staff, and patients) and a support system (tools, playbooks, and partnerships). As the quote from the movie Field of Dreams goes, “Build it and they will come.” In this case, build technologies, services, and funding programs that provide training, literacy,
The question, ‘Are we ready for artificial intelligence?’ is top of mind for clinicians and policy makers.
governance, and patient support as core features (not optional add-ons), and the rest will fall into place.
As clinics invest in empowering their teams and patients, the question emerges: “How do we ensure this effort has an impact beyond the walls of a single clinic?”
resources that enhance clients’ understanding of EMRs, empowering community to confidently access, comprehend, and share their health information within their healthcare team.”
This program, in addition to the many others, reinforce that clinician and community-driven approaches ensure digital health solutions are both effective and trusted.
Finally, and in addition to local solutions, some of our 2025 Grant winners are also tackling systemic challenges, particularly around data fragmentation. EssentialMD’s “Master Chart” project uses AI to convert disparate scanned medical records into standardized digital formats, ensuring complete patient histories are accessible at the point-of-care.
In a tertiary care setting, the University Health Network is applying large language models to extract Social Determinants of Health from clinical notes, enabling personalized support and informed discharge planning.
Importantly, these projects show that innovation developed locally can also inform best practices system-wide.
Dr. Rashaad Bhyat is senior clinical leader, Canada Health Infoway.
Skills, literacy, and shared purpose are essential, but can only go so far if information across hospitals, labs, and community clinicians remains fragmented and digital tools do not communicate with one another. The value of an empowered clinic can only be unlocked when people and processes are supported by reliable, standards-based data that flows with patients across points of care.
In the next article of our four-part series, we will examine the second pillar, Connected, and how interoperability, data governance, and smarter integration can transform empowered teams into networked clinics, with system-wide impacts.
Dr. Chandi Chandrasena is OntarioMD’s chief medical officer; Simon Ling is executive director, partnerships and stakeholders; Reza Talebi is director, knowledge translation and education, client services & engagement; Dr. Abbas Zavar is the organization’s digital health research lead.

