

INSIDE:
EWS for mental health
Waypoint has created an AIpowered early warning system to anticipate when patients are at risk of mental health deterioration. The project has now been successfully piloted.
Page 4
Knowledge translation
Hamilton Health Sciences has launched a knowledge centre to communicate research findings from its labs and think-tanks to physicians at the bedside, where patients can benefit from new ideas.
Page 6
SEED for doctors
Kitchener, Ontario family doctor
Rebecca Lubitz is pioneering a system she calls SEED to make physician offices more efficient.
SEED is short for Stop, Eliminate, Educate and Delegate, the four steps to a more effective practice.
Page 8

Kingston shows leadership in surgical robotics
Kingston Health Sciences Centre has acquired a new robot to assist with surgeries. The latest system, from Da Vinci, is said to offer advanced technologies and will be of great benefit to patients as it enables surgeons to move around the chest and abdomen with far greater precision. KHSC has become a national leader in robot-assisted surgeries in the area of liver and pancreatic cancer. SEE STORY ON PAGE 12.
Sunnybrook Health Sciences acquires Oracle EHR
BY JERRY ZEIDENBERG
TORONTO – Sunnybrook Health Sciences made waves in the electronic health records sector a few months back with its choice of the Oracle Health system to update and upgrade its current solution. It seems that of late, many of Canada’s top academic hospitals have been opting for Epic, and that Sunnybrook was going against the grain.
But in a rigorous and objective review at the hospital, Oracle Health was the clear winner.
“It was the choice of our clinicians,” said VP and CIO Rob Lee. “In 2022, we issued an RFP that had over 7,000 clinical requirements. And it was all Sunnybrook specific.”
He noted the review at the hospital involved 768 clinicians and front-line staff. Decisively, their choice of EHR was Oracle Health.
Lee observed that the Oracle Health solution was particularly good at addressing the specific needs of Sunnybrook, which is a provincial and national leader in many areas of care delivery.
The new digital system will be used not only by physicians, but by nurses and other clinicians.
For example, it has the largest trauma centre in Canada, a major burn centre, and a leading cancer care facility – the Odette
Cancer Care Centre. It’s also a top surgery provider, has some of the most advanced imaging equipment in the country, and is a major innovation creator, especially with its INOVAIT program for image guided surgery and the wide-ranging Sunnybrook Research Institute.
Locally, it tends to work closely with regional partners like North York General Hospital and Michael Garron Hospital, which also use the Oracle solution.
Of course, it collaborates with the downtown Toronto hospitals, like the University Health Network and Mount Sinai Hospital.
But Lee stresses that with Sunnybrook’s advanced areas of healthcare delivery, patients are coming from afar, as well. “The
Sunnybrook acquires Oracle EHR, plans leading-edge deployment
whole province is our catchment area,” he observed.
Lee agreed that interoperability of patient records is increasingly important, as clinicians need to know the history of patients, especially their recent medical encounters, imaging histories and medication profiles to provide the best diagnoses and treatments – and the safest care.
He said, however, that interoperability of EHRs – in Ontario – has never been better, thanks to the Health Information Exchanges (HIEs) that make it possible to see data from other hospitals directly in the electronic chart, regardless of the vendor.
These repositories are even enabling the back-and-forth transmission of records with nursing homes, most of which use the PointClickCare system in Ontario.
The plan for Sunnybrook is to deploy the Oracle Health solution in 2027. It will be a “big-bang” implementation, with many areas going-live all at once.
Lee explained that most hospitals do it this way now, instead of using a gradual rollout. “If you don’t, and you drag it out,
people tend to get fatigued,” by an overly long series of meetings and training sessions. Best to concentrate it all in a given period, he said, and to go live all at once.
A fascinating aspect of Sunnybrook’s Oracle Health deployment is that it will affect a wider range of clinicians than ever before.
In fact, previous iterations of EHRs at Sunnybrook were really physician-centric.
Now, nurses will have electronic solutions, including electronic notes and documentation. “Currently, our nurses are still primarily paper-based,” said Lee. “This will be a monumental step for us. We’re excited for all our health professions to be going on to one system.”
As well, clinicians and allied professionals throughout the enterprise will be part of the digital system. That includes pharmacists, lab and imaging professionals.
Lee noted that occupational therapists and physiotherapists, dieticians, speech language therapists, and others will be accessing and using the system, too.
“They won’t be chasing paper charts anymore, trying to find out who has the chart,” said Lee. “Everyone will be able view and edit the records.”


Just as it has become one of the top acute-care hospitals in Canada and worldwide, Sunnybrook aims to become a leading-edge site for the Oracle Health EHR system – a super-user, so to speak.
“We intend to become a Canadian reference model. We’re going to deploy Oracle’s ‘best build’ at Sunnybrook. And in turn, our goal is that Sunnybrook will contribute to the ongoing creation of Oracle’s new solutions,” said Lee.
“We’ll be involved in co-designing the system with Oracle, developing applications, but all balanced with patient safety. We never forget that we’re taking care of some of the sickest patients.”
Within those parameters, however, the hospital intends to become a powerhouse user and developer of the electronic health record. “Our ambition is to become a global reference site.”
These applications include artificial intelligence, which Lee agrees holds amazing potential for the future.
“We’re buying all of the AI tools, not just for doctors, but for nurses, too,” he said. Lee pointed out that Oracle has been investing in AI for nurses, something that’s sometimes overlooked in the AI excitement over the gains that have recently been made in ambient listening systems for doctors.
Lee said the hospital will certainly be investing in ambient listening systems and AI scribes for its physicians but wants to go beyond these systems with solutions for other clinicians, as well.
The plan is that AI will be deployed to solve many problems, and in doing so, to significantly improve patient care.
For example, one application can identify oncology patients who may qualify for clinical trials, and at the same time, can collate trials and match the patients with them.
Currently, this is often done manually; automating it and widening its scope with artificial intelligence could potentially save lives while helping to develop treatments.
Issue DateFeature ReportFocus Report
February Medical ImagingPhysician IT
March Artificial IntelligenceInteroperability
April Mobile SolutionsHospital at Home
May EHR / EMR TrendsPrecision Medicine
June/July IT Resource GuidePoint-of-Care Systems
September Community CareStart-ups
October Virtual CareSurgical Technologies
For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
Coming up in 2026 www.canhealth.com

Publisher & Editor
Lee also sees great potential in AI for summarizing notes and giving clinicians a better picture of how the patient is progressing or declining.
In the end, Lee sees AI as a great enabling device. “Treatment isn’t driven by computers, but computers can effectively distill information and support our clinicians.”
“Oracle Health’s new AI-powered solution changes the EHR from an administrative burden into a clinical asset. It will enable Sunnybrook doctors to use voice commands to plan their day, gather relevant information about a patient’s prior history or medications, and even request summaries of recent research to inform care decisions,” said Erin O’Halloran, vice president and Canada market leader, Oracle Health.
“Equally important, it nearly eliminates menus and clicks, so doctors can spend less time looking at screens and more time focused on patients. We built this new EHR from the ground up to leverage the power of the latest advances in cloud and AI technology. It is a massive step forward for the industry, and it will keep Sunnybrook at the forefront of Canadian healthcare for years to come.”
She added, “Sunnybrook is consistently ranked among the world’s best hospitals and is a hub for groundbreaking medical research and treatment, and we look forward to supporting them in their vision to invent the future of healthcare.”
Art Director
Jerry Zeidenberg jerryz@canhealth.com
Office Manager
Neil Zeidenberg neilz@canhealth.com
Contributing Editors Dianne Daniel dianne.l.daniel@gmail.com Will Falk will@wfalk.ca
Dr. Sunny Malhotra Twitter: @drsunnymalhotra Norm Tollinsky tollinskyn@gmail.com Funded by
Address all correspondence to Canadian Healthcare Technology, P.O. Box 907, 183 Promenade Circle, Thornhill ON L4J 8G7 Canada. Telephone: (905) 709-2330. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2025. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others: $67.80 per year ($60 + $7.80 HST). Registration number 899059430 RT. ©2025 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited. Send all requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, P.O. Box 907, 183 Promenade Circle, Thornhill ON L4J 8G7. E-mail: jerryz@canhealth.com. ISSN 1486-7133 CANADA’S MAGAZINE FOR MANAGERS AND USERS OF INFORMATION TECHNOLOGY IN HEALTHCARE Volume 30, Number 8 Nov/Dec 2025
Walter Caniparoli art@canhealth.com
Digital Media Specialist
Rebecca Downer rebecca@canhealth.com
Rob Lee Erin O’Halloran

ELEVATING INTERVENTIONAL PROCEDURES
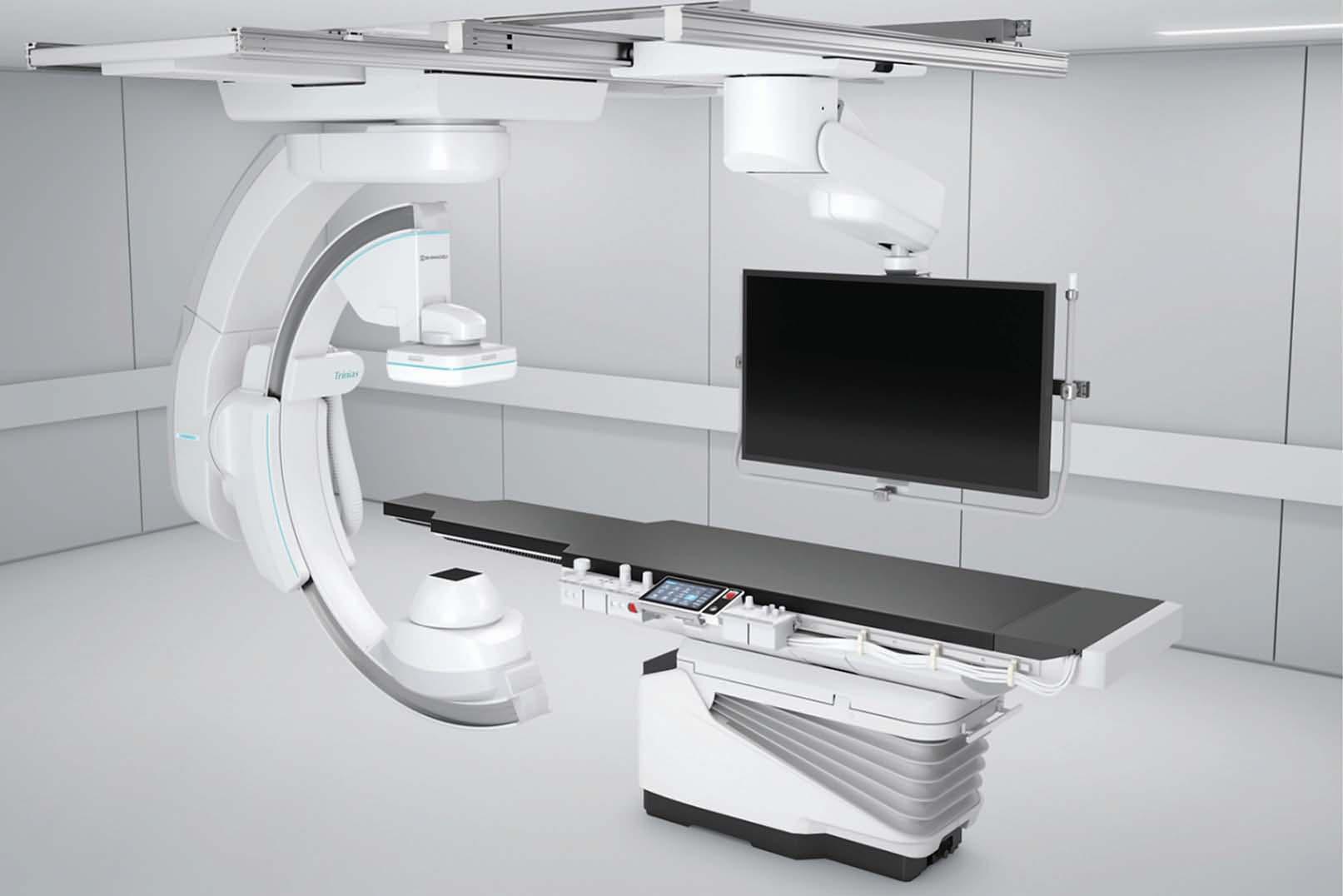
Trinias with SCORE Opera
Crossover Angiography System
The new Shimadzu Trinias with SCORE Opera represents a significant step forward for clinicians seeking to optimize outcomes, reduce procedure times, and streamline workflows.
SMART Voice function improves examination efficiency, and reduces the burden on physicians and healthcare personnel.











Waypoint develops AI-powered early warning system for mental health
BY NORM TOLLINSKY
Waypoint Centre for Mental Health Care and its research institute have developed an AI-powered early warning system to anticipate when patients are at risk of mental health deterioration.
Led by Dr. Andrea Waddell, Waypoint’s medical director for clinical informatics and quality, the solution leverages integrated patient data from the organization’s MEDITECH Expanse electronic health record (EHR) to calculate risks. The project has been successfully piloted in four 20-bed units at the Penetanguishene, Ontario, hospital.
“Psychiatric admissions are associated with more incidents of preventable harm than other hospital admissions,” said Dr. Waddell, who is also associate director of adult psychiatry and health systems at the University of Toronto’s Temerty Faculty of Medicine and Ontario Health Central Region’s clinical lead for mental health and addictions.
“Mental health deterioration,” she said, “can result in suicidal ideation, self-harm and violence against hospital staff and other patients, so if we can identify patients who are worsening, we can intervene and prevent these kinds of events.”
Waypoint’s high-secure provincial forensics program cares for some of the most severely ill patients in the province. They include those who come in contact with the legal system and are referred to mental health care by the Ontario Review Board if found to be not criminally responsible or unfit to stand trial.
The hospital also offers mental health inpatient services for the Central Region and a forensic assessment program for patients admitted from the courts, correctional facilities and regional psychiatric hospitals.
Waypoint also consulted with St.
Michael’s Hospital in Toronto to understand the principles they used to build and deploy their ChartWatch tool. “ChartWatch looks at patients on medical units and identifies if they’re deteriorating to avoid adverse outcomes and admission to the ICU,” she noted.
The AI early warning application, developed with the assistance of Dr. Christo El Morr and Dr. Elham Dolatabadi of York University. After approval from the hospital’s Research Ethics Board, the model was trained on four years of deidentified data from thousands of Waypoint patients to learn what risk factors are associated with adverse outcomes.
“There are what we call static risk factors and dynamic risk factors,” explained Dr. Waddell. “Static risk factors are things that happened to a person in the past and are predictive, but don’t change over time.
“So, if someone has been violent in the past, they’re much more likely to be violent in the future. If someone has had a suicide attempt in the past, they’re at much higher risk of a future suicide attempt.” Other static risk factors include co-morbidities, chronic pain and substance abuse.
Dynamic risk factors include changes in medication, refusing medication, changes in eating and sleeping patterns, as well as nursing assessments of a patient’s mental status and any signs of agitation or anxiety.
All of the data used by the model is routinely collected by clinical staff and displayed in Waypoint’s MEDITECH EHR system, so there’s no additional workload for staff.
During a pilot over the preceding five to six months, said Dr. Waddell, the model was approximately 98 percent accurate in identifying patients at low risk of
Waypoint’s Dr. Andrea Waddell
mental health deterioration: “It was very effective as a screening tool to be able to identify patients who are proceeding along their expected trajectory.”
For people who were identified as highrisk, approximately one-third of them actually do go on to have an adverse event in the subsequent 24 hours.
“So, it’s not perfect,” she said. “Everyone flagged as high-risk doesn’t necessarily go on to have an event, but physicians found that rate acceptable because it does screen out the other patients” and it’s not unduly onerous to check up on those few identified as high-risk.
Physicians use the early warning system as a decision support tool and will typically review the patient’s care plan. They may increase a patient’s access to pleasurable activities, adjust their medication or increase engagement with nursing staff.

Dr. Waddell cited the example of one patient who was flagged as a high-risk for mental health deterioration the same day they were scheduled for discharge. “That was a fairly dramatic example of the tool’s value. The physician cancelled the patient’s discharge, avoiding a potentially adverse outcome and making a big difference in the patient’s recovery.”
The machine learning model uses data from MEDITECH, but the results identifying patients at risk are currently external to the EHR and communicated to physicians via email.
Manual distribution of the results is feasible with the limited deployment of the tool in the context of a pilot, but far from ideal once it’s rolled out hospital-wide to 25 physicians, so Waypoint is working with MEDITECH on an Application Programming Interface (API) that will distribute the results through the EHR.
“That will be much more seamless for the physicians as they’ll see the alerts with the names of the patients when they log in to MEDITECH every morning,” said Dr. Waddell.
“We are pleased to be a part of Waypoint’s effort to improve patient safety and workflow efficiency through integration with the Early Warning System,” said MEDITECH director of Canadian market and product strategy Bob Molloy. “By designing a cloud-native EHR that adheres to the latest FHIR standards, we provide our customers with a platform that is interoperable and scalable. This approach supports innovation now and, in the future, to ensure that organizations like Waypoint are able to continue to advance healthcare.”
A prototype of the API is currently in development. A clinical trial will then be conducted to determine if the alerts improve patient outcomes. The early warning system is expected to be deployed hospital-wide by the end of this year or early spring 2026.
FluidAI creates early warning system for sepsis, post-op complications
KITCHENER, ONT. – As calls grow for a Canadian action plan to address sepsis – a life-threatening emergency caused by infection and a leading cause of death worldwide – an innovative Kitchener-based medtech company is on a mission to transform the way patients recover after surgery, reducing their chance of life-threatening infection, speeding recovery and ultimately, saving lives.
FluidAI Medical has launched a groundbreaking intelligent risk analysis platform that can flag early on a broad range of post-operative complications, including sepsis, deep vein thrombosis, respiratory failure, bleeding, pulmonary embolism, pneumonia and more.
Called Stream Care, the platform incorporates data from patient records, continuous vital sign monitors, wearable sensors and other medical devices to provide advanced risk assessments following colorectal surgery, bariatric
surgery and surgery to treat benign and malignant diseases of the liver, pancreas, gallbladder and bile duct.
It includes a digital companion app for patients so they can learn more about their surgical procedure, report symptoms while recovering on a hospital ward or at home, and track medication compliance or dietary issues that may impact their recovery.
The technology also integrates with electronic health record systems to give clinicians a unified view of all relative patient information, highlighting critical values.
“We’re ushering in a new era of intelligent recovery, where post-operative patient care becomes proactive rather than reactive,” said Dr. Mustafa Obeidat, medical advisor at FluidAI.
Stream Care builds on FluidAI’s flagship product, Origin, originally launched in 2022. Origin is a first-of-its-kind patient monitoring system for early detection of anastomotic leaks in surgical
drains, indicating a surgical connection hasn’t healed properly, which can lead to life-threatening infection.
The device connects between the tubing and the drain reservoir, using nanosensors and AI analytics to monitor the surgical drainage for changes in acidity (pH) and conductivity, both of which

alert to a leak long before a patient would experience symptoms like fever, rapid heartbeat or vomiting, meaning clinicians can intervene before a more severe complication results.
On average, eight percent of patients who undergo a gastrointestinal procedure
will experience a leak, and the mortality rate for those who do is one in six.
By expanding focus from hardware to software with the company’s new intelligent platform, Dr. Obeidat explained that “instead of just catching leaks, we want to catch everything else that can go wrong.” He explained that care teams can use Stream Care as a companion to Origin or standalone, with the ability to monitor more than 50 validated risk scores as well as their own custom risk scores.
Founded by three students – two from the University of Waterloo and one from Toronto Metropolitan University – FluidAI currently numbering 80 employees.
The company owes its success in good part to Mitacs, a leading innovation organization that connects businesses and researchers to drive collaboration, deploy skilled talent, and build innovation capacity to strengthen Canada’s productivity and global competitiveness.


More than an image. The big picture.

Work connected. Work confident. Work in balance.
AGFA HealthCare’s Enterprise Imaging Platform brings everything together — blazing-fast streaming, smart orchestration, embedded AI, deep clinical integrations, and flexible deployment in the cloud or on-premises.
Built for precision, personalization, and simplicity, it creates a connected ecosystem where radiologists stay focused, IT teams cut complexity, and care teams collaborate with clarity.
Whether reading on-site or remotely, managing growing imaging volumes, or expanding across specialties, Enterprise Imaging adapts to your environment — and evolves with you.

Discover what imaging looks like when everything just works at RSNA. agfahealthcare.com/rsna
HHS Knowledge Centre aims to channel research to benefit patients
BY LISE DIEBEL
Hamilton Health Sciences (HHS) has launched the HHS Knowledge Centre to promote knowledge synthesis, knowledge mobilization, and quality of care. Broadly speaking, it will work to communicate research findings to healthcare professionals, policy makers and the public so that patients receive the latest and most advanced care.
“While leading-edge research is happening at HHS, our researchers aren’t always aware of each other’s work and findings because we’re such a large organization,” said Dr. Marc Jeschke, who since joining HHS two years ago has focused on improving collaboration among the research community at HHS, McMaster University and beyond. “The greatest impact happens when we work together and share our findings, and the new Knowledge Centre will foster collaborations across many clinical and research areas.”
Knowledge synthesis focuses on gathering and organizing studies, reports and other findings to determine which treatments work best and creating guidelines for physicians to follow. Knowledge mobilization is about ensuring that recommendations for best practice find their way to the bedside; and quality improvement focuses on improving patient outcomes, enhancing the patient experience, and making sure the hospital works as efficiently as possible.
The HHS Knowledge Centre began operating in July. It is led by three co-directors who are HHS physicians: interventional cardiologist Dr. J.D. Schwalm; intensive care physician Dr. Bram Rochwerg; and anesthesiologist Dr. Ekta Khemani. All three are also researchers and experts in knowledge synthesis, knowledge mobilization and quality improvement.

R“The new centre will make us much stronger as we approach projects, because we can cover the full spectrum of knowledge translation from start to finish,” said Dr. Schwalm, whose area of expertise is implementation science. This involves figuring out how to introduce researchbacked methods into everyday practice and making them stick.
In 2018 Dr. Schwalm became director of the Centre for Evidence-Based Implementation (CEBI) to advance health care at HHS through research and education. CEBI has now been folded into the new HHS Knowledge Centre.
“We’re morphing into something bigger
and broader with greater reach,” said Dr. Schwalm, whose work as CEBI’s director had a strong focus on improving the delivery of cardiovascular care.
The new centre will include other HHS pillars such as trauma and critical care, oncology, children’s health, women’s health, rehabilitation medicine and aging. The centre’s involvement could range from small projects, like consultations, to leading large projects from start to finish. All projects will directly benefit HHS patients.
“The exciting part, and the challenge, will be uniting forces across specialties through the new centre,” said Dr. Rochw-
erg, whose specialty is knowledge synthesis with a focus on the intensive care unit.
“HHS is a world leader in producing evidence-based guidelines in areas including critical care, hematology, cardiology and thrombosis,” said Dr. Rochwerg. “Worldwide, it’s hard to find a guideline from these areas published in the last decade that doesn’t include at least one HHS investigator.”
Dr. Khemani brings leadership in teaching quality improvement strategies to physicians and other healthcare providers who work directly with patients, such as nurses, occupational therapists and physiotherapists.
“Our healthcare providers really want to improve the system, but they don’t necessarily have the quality improvement background or tools to do so,” said Khemani, whose support includes helping healthcare providers build the skills and knowledge needed to improve workflows, create a culture of continuous improvement, and even develop their own quality improvement projects.
The three co-directors credit HHS president and CEO Tracey MacArthur and vice president of Research Dr. Marc Jeschke for recognizing the need for a Knowledge Centre and supporting its formation. HHS is a top Canadian research hospital, but with so many physicians and staff involved in research projects, it can be easy to stay in silos.
Dr. Khemani noted, “This has been a great opportunity to combine what we’ve been working on, and advance knowledge translation work across the organization. We all share the same goals of building capacity and supporting HHS as a research powerhouse.”
Lise Diebel is Communications Advisor at Hamilton Health Sciences.
Royal Victoria Hospital accelerates cardiac care with Hypercare
oyal Victoria Regional Health Centre (RVH) in Barrie, Ontario, is no stranger to the pressures facing acute care hospitals. It serves one of the fastest-growing regions in the province, providing a vast array of subspecialty care. RVH has seen rising demand for emergency cardiac care as the population ages. For patients experiencing ST-Elevation Myocardial Infarction (STEMI), every minute between arrival at the emergency department and treatment in the catheterization lab, known as the “door-to-balloon” time, has a direct impact on survival and recovery.
RVH’s system for activating the cardiac response team relied on outdated tools. Pagers and call lists meant that a single STEMI team activation could involve multiple phone calls, voicemail delays, and misdirected pages if schedules weren’t up to date. The hospital knew that a faster, more reliable solution was needed.
RVH turned to Hypercare – a secure clinical communication and coordination platform – for a better and more ef-
ficient approach. The goal was to streamline the STEMI team activation process and give clinicians the tools to coordinate seamlessly when every second matters. Instead of relying on manual call-outs, a single activation now notifies the entire on-call response team simultaneously through secure messaging, overriding silent or “Do Not Disturb” settings.
If the first message is not acknowledged, the system can automatically escalate to a phone call or SMS message until confirmation is received, ensuring no team members are missed.
Equally important, Hypercare directly maintains RVH’s on-call schedules. Clinicians no longer worry about calling the wrong person or tracking down who is covering a shift. The system draws on live, centrally managed schedules so that only the correct on-call staff are alerted. This automation not only reduces administrative burden but also removes one of the most common points of error in manual processes.
The platform has also improved col-
laboration with paramedics and referral hospitals. When first responders capture an ECG in the field on Zoll ECG monitors, it can be sent directly to the interventional cardiologist on call, enabling rapid diagnosis and allowing teams to prepare before the patient arrives.
Referral hospitals and paramedic services, meanwhile, can bypass traditional
If the first message is not acknowledged, the system can automatically escalate to a phone call or SMS message.
switchboard delays and connect immediately with specialists at RVH through a dedicated phone number. This dedicated number connects directly to switchboard, where clerks immediately transfer the call to Interventional Cardiology, preventing callers from being stuck in the regular caller queue.
“Activating a STEMI is now seamless,”
said Dr. Mark Kotowycz, interventional cardiologist and medical director at RVH. “We no longer wait for pages to be returned, the entire team is alerted instantly. The faster we mobilize, the sooner we can open the artery, directly improving patient outcomes.”
The results have been striking. RVH has reduced activation delays and improved decision making by ensuring that the right clinicians have the right information at the right time. Staff have reported less frustration and wasted effort, as they no longer need to spend critical minutes chasing down colleagues by phone. And most importantly, patients are getting faster access to life-saving treatment.
RVH’s experience also reflects a broader shift underway across Canadian healthcare. Hospitals are increasingly recognizing that traditional paging systems and phone trees are not designed for the speed and complexity of modern acute care. Secure, digital platforms are
The new Hamilton Health Sciences (HHS) Knowledge Centre is led by three co-directors who are all HHS physicians: Dr. Bram Rochwerg, Dr. Ekta Khemani and Dr. J.D. Schwalm. They each bring expertise in knowledge synthesis, knowledge mobilization and quality improvement.

Accomplish more by delegating in the medical office: SEED initiative
BY JERRY ZEIDENBERG
Despite the arrival of AI scribes in their offices, many doctors find they still have too much to do – they’re swamped by a never-ending stream of results to review and an overabundance of paperwork. AI scribes are assisting with some of the load, as these computerized systems can automate a lot of documentation during patient encounters.
Still, there are many other tasks to be done, and one person can only accomplish so much.
To the rescue, with a strategy for reducing the load, is Kitchener family doctor Rebecca Lubitz. She is championing a system called SEED – short for Stop, Eliminate, Educate and Delegate.
It’s a framework for reducing a physician’s workload by eliminating redundant and unnecessary reports and tasks. Moreover, it also trains office staff to take care of low-risk tasks that were traditionally done by a doctor.
Dr. Lubitz gave a fast-paced presentation at the OntarioMD conference in September where she summarized SEED.
“I’m going to go through how to stop and eliminate certain types of data that you don’t need. Some of the data doesn’t need to be in your EMR, and that’s what we’re going to help you eliminate,” she said.
She added, “Education and delegation is a much bigger piece that I’m really passionate about, and I’m going to help you leverage some tech tools to improve.”
Dr. Lubitz mentioned that there is a substantial body of literature about cognitive overload and having too much to do. Much of it originated in the aviation sector. It was found that when pilots have too many tasks and alarms in the cockpit, it actually makes it harder to fly the plane.
On a personal note, she said she prided herself as a medical resident on being thorough; however, she eventually realized –on the advice of colleagues – that by being too detail-oriented, she was sometimes missing the forest for the trees.
By better managing data, she could perform more effectively and also find more time for family and friends.
She cited studies which found that 40 percent of the administrative burden in a
Hypercare partnership
CONTINUED FROM PAGE 6
helping providers close the communication gaps that once delayed patient care. For critical conditions like STEMI and stroke, where delays can cost lives, these tools are indispensable.
For RVH, the move to Hypercare has been more than a technological upgrade, it has been a cultural shift toward faster, safer, and more reliable collaboration. What began with STEMI activations has since expanded to include Code Blue, Code Pink, Code OB, Code Stroke, and specialized Code Transfusion alerts, including Pediatrics. RVH has also built a unique Life &

medical practice could be reduced through elimination and delegation.
For example, a couple years ago she received an echocardiogram result four times in her inbox. “Every time you get the result again you think, is this new? Is there an addendum? And after reviewing it four times, I just started to cry and I called OntarioMD. They explained to me that I could just shut off duplicates!”
That helped germinate the idea for SEED.
As a first step, Dr. Lubitz said doctors must learn what to stop receiving or reviewing. “We’re going to stop items of low clinical value from being sent to you.”
She said physicians should eliminate data that has almost zero clinical value if it’s in the chart in another format, and they don’t need a second, third or fourth version.
As well, “things you can eliminate are things that don’t actually need to be in the EMR because they’re not actionable for the patient – what I would call virtually zero risk.”
She gave the example of urgent results.
“You may get 300 urgent results a week, but there’s only a few that actually need to be dealt with in a very timely manner.”
She said an audit of her own practice found that in the past two years, she once received 500 urgent results in a week, but only five of them really needed urgent attention.
“Five to five hundred, right? Something has to be done,” she asserted.
Limb/Vascular activation, designed to mobilize vascular surgeons and surgical/recovery nurses immediately in emergency situations. Previously, this process required multiple phone calls and often led to delays in reaching the care team. With Hypercare, the Life & Limb pathway now notifies the vascular team instantly, saving precious time and ensuring patients receive rapid, life- and limb-saving interventions. As hospitals across Canada look for ways to modernize emergency workflows, RVH’s journey offers a glimpse of how digital coordination not only accelerates cardiac care but also transforms a broad spectrum of emergency response codes, helping clinicians deliver better outcomes when every second counts.
Another example of duplicates, at least in the province of Ontario, comes in the form of Hospital Report Manager (HRM). Referring physicians often receive multiple copies, and the reports can be exceedingly long.
Family physicians may also receive the patient’s lab report, which is also contained in the HRM report.
So, it’s important to filter out multiple copies of Hospital Report Manager, if
When aviation pilots have too many tasks and alarms in the cockpit, it actually makes it harder to fly the plane.
they’re coming into the office. And separate lab reports may not be needed, either.
Dr. Lubitz said these are examples of things that can be stopped or eliminated. The next step is to stop looking at documents that someone else in the practice can review.
“What you might want to consider are things that are not actionable for you as a practitioner for the patient, where there is no follow up or communication needed for the chart.”
Examples in her own practice include items such as massage notes and physiotherapy notes, and requests for orthotics. “Staff intercept them, and staff does not send me a message about it,” she said.
Consult requests and referral redirects are also handled by staff – in cases where the specialist responds that they can’t see the patient quickly enough and to refer elsewhere.
“I was being my own secretary for many years and copying and pasting that referral, reattaching all of the things and sending it on to another specialist only to have it declined again,” said Dr. Lubitz.
Finally, she decided to create a protocol for staff to intercept and handle those declined referrals. They’re routed to her if they’re urgent or semi-urgent, but otherwise, staff take care of them.
She said that items which staff can safely handle have protocols. They’re tied to buttons in the EMR, which lead to eforms and templates for the staff.
“Many of you order MRIs, and the creatinine is out of date and you get a fax
from the hospital saying please update the creatinine. I’m never going to say no to that, and it needs to get done, but I don’t need to see it. So, we’ve developed a protocol for it,” said Dr. Lubitz. “It never goes through me.”
She asserted that once you’ve looked at how many things are coming in that do not require a physician’s attention, and that can be done by the receptionist or another member of the office, you can develop protocols that are tied to helpers like buttons, templates and stamps.
The next step is to review a higher level of data that could potentially be handled by staff. In this case, you go on to create an educational program to train staff members.
“Education is huge for everybody, because it just makes the environment so much more interesting. It empowers your staff. You can delegate more, and it makes the culture better,” she said.
That in turn reduces staff turnover, as people become more interested in their jobs.
However, educating staff is not easy; it’s time consuming. “I found I was running into problems educating my staff because they were working when I was working. So, I redid all their workflows to allow them to have some protected time, when I’m not seeing patients.”
Dr. Lubitz can then meet with staff for training. “That has changed my life,” she said, “and it’s changed our clinic dramatically.” Staff are so much more engaged, and Dr. Lubitz spends far less time on paperwork.
How do you train staff? The best place to start, she said, is to educate people about the difference between common results and urgent results.
She said that lab orders are often pretty much the same, and educating staff about results is not difficult.
“Any hemoglobin less than 100, I want to know about it. Any creatinine less than 45. A white count over 13.
“Last night, I had 75 things in my inbox,” she said. “My nurse went through it all and all I had to deal with was one issue. So, I didn’t have to spend three hours mining all of that.”
A nurse in Dr. Lubitz’s office has also learned to read consult notes that come back to the office from specialists, and to annotate the patient charts. At first, Dr. Lubitz would read the charts to make sure the annotations were done properly.
“As she got really good at annotating things, I stopped opening the PDF for most consults,” said Dr. Lubitz.
“When the allergist sends a three-page consult note and what I need to know is whether the patient was allergic to anything on testing, whether there is an anaphylactic issue I need to know about, and if so, I need the problem list detailed – such as a peanut allergy. So, she learned all that.”
Dr. Lubitz said there’s a lot of information available on how to delegate and how to do it safely. A major factor is to ensure a lot of documentation is readily available to the person performing various tasks, so they can review it when needed.
But the bottom line is that if physicians don’t delegate, and try to do everything themselves, it creates an inefficient or unsafe environment.
Dr Rebecca Lubitz, left, and Katie Peter of OntarioMD, presented on SEED at the September conference.
Fostering connection in long-term care with the help of AI-enabled social robots
VANCOUVER – As Canada’s aging population continues to grow, so does the demand for innovative solutions to enhance the care and quality of life for older adults. At the forefront of this technological shift is Vancouver Coastal Health Research Institute researcher Dr. Lillian Hung, whose new study explored the potential of social robots to support well-being among residents of long-term care homes.
Published in the Journal of Rehabilitation and Assistive Technologies Engineering, findings from this research reveal powerful insights into how technology can create new pathways for emotional engagement and social interaction, particularly for people with dementia.
While visiting Japan for another research study, Hung encountered LOVOTs: accessible, easy-to-use artificial intelligence (AI)-enabled companions. “These robots were very popular,” said Hung. “People bought them outfits, made them jewelry and treated them like pets. I became curious about how my own patients would interact with this kind of technology.”
Equipped with wheels, cameras and microphones, LOVOTs can see and hear their surroundings to enable interactive behaviours, such as tracking movements, recognizing faces and reacting to sounds. The robots also respond to gentle petting or hugs, enhancing the sense of physical and emotional connection. Using machine learning algorithms, they learn to adjust their actions to better suit the user’s needs and desires based on previous interactions.
“I have seen firsthand how dementia can leave people isolated,” noted Hung. “I was interested in uncovering how social robots like LOVOTs can offer not just companionship but real, tangible emotional support.”

For her study, Hung brought two LOVOTs to Canada, named Mango and Kiwi, to investigate how they could impact the emotional and social lives of long-term care residents. Over a year, Hung and her research team visited various care homes, community centres and public libraries. In one of the care homes, 36 participants, including family members and staff provided valuable feedback about the residents’ emotional responses to the robots.
Following discussions with participants about their experiences with the robots, researchers identified three key ways in which LOVOTs supported the psychosocial needs of older adults: joy, creativity and acceptance.
The researchers found that the presence
of LOVOTs brought a sense of novelty and excitement to everyday routines, breaking up the monotony of long-term care settings. Whether playing with the robots or watching them dance, participants were often seen smiling and laughing during their interactions.
The robots also inspired self-expression among participants. “Since the robots do not speak human language, participants had to use their imaginations to interact,” said Hung. “Some people came up with their own languages for them, and some created fun stories about the robots based on their own memories, which sparked further conversations among staff and residents of the care homes.”
Another critical finding was how the
robots provided a consistent and reassuring presence. This was particularly meaningful for those who struggled with verbal communication or who experienced confusion due to dementia.
For example, Hung recalls a participant with dementia who was considered to be ‘aggressive’. “People would warn us to use caution around this particular resident because he could be unpredictable and combative. However, when he was playing with the robots, all the aggression evaporated. It left everyone in awe, because they had never seen his affectionate side before.”
While social robots are not a replacement for other forms of companionship, such as that of a pet, family member or friend, they do offer some unique benefits. Unlike cats or dogs, social robots do not require food, water or medical care, making them an ideal option for individuals with mobility issues or dementia.
“Robots like LOVOTs are specifically programmed to seek out affection and respond to emotional cues,” Hung explains. “For people in long-term care, this technology provides a source of companionship without the physical or cognitive demands of caring for a pet.”
In the future, Hung envisions broader applications for LOVOTs and other emerging forms of social robots, such as in critical care and rehabilitation centres, where patients often experience pain, isolation or emotional distress. They may also play an important role in mental health care, helping those experiencing depression, anxiety or social isolation to feel loved.
“There is something fundamentally comforting about having a companion, even one that is robotic,” said Hung. “For people struggling with their mental health, the emotional connection a robot offers can be a vital part of the healing process.”
CUBEC: Empowering the next generation of biomedical engineers
BY GAAYATHRI GANESH
In an era of rapid medical innovation, the Canadian Undergraduate Biomedical Engineering Council (CUBEC) is helping shape the next generation of biomedical engineers. This student-led, not-for-profit organization empowers students by promoting awareness, education, and inclusion in the field of biomedical engineering. Whether it’s inspiring curious high schoolers or equipping undergraduates with mentorship and career-building tools, CUBEC is fostering a nationwide support network and leadership hub.
“CUBEC plays a vital role in bridging the gap between academia and industry by helping students navigate complex career paths and uncover opportunities that often remain hidden or inaccessible,” said Mark Tchinov, the organization’s president. “By fostering meaningful connections between students, their academic institutions, and a diverse range of professional pathways including emerging and specialized fields, CUBEC
opens doors and broadens horizons for aspiring biomedical engineers.”
From annual conferences and editorial features to podcasts, outreach campaigns, and leadership summits, CUBEC empowers students to take ownership of their futures by exploring new ideas, driving innovation, and shaping the future of biomedical engineering in Canada and beyond.
At the heart of its mission lies the CUBEC National Conference, the flagship annual event. The first in-person conference was held in January, with simultaneous events in Toronto, Calgary, and Montreal. The events were organized in partnership with university clubs such as UTBIOME, BUSS, and BMESS. With generous support from sponsors like Medtronic, Stryker Breast Care, Providence Therapeutics, AbCellera, and Circle Cardiovascular Imaging, it has become the largest BME gathering for undergraduates in Canada.
More than 700 students from over a dozen universities met for a day of connection and inspiration. Startup
founders, professors, clinicians, and industry professionals shared their journeys and insights. For many attendees, it wasn’t just a conference, it was a launching pad.
“The CUBEC conference offers students to learn about diverse careers in the biotech and medtech sectors through interesting talks, networking, and establishing relationships,” said Amanda
More than 700 students from over a dozen universities met for a day of connection and inspiration.
Spilkin, an aerospace and biotechnology researcher. “I highly recommend this conference for all undergraduate students looking forward to building their career paths and personal development.”
Looking ahead to the next conference on January 31st, 2026, CUBEC is preparing an expanded lineup of speakers, workshops, and collaborative forums to make
the event more impactful than before!
While the conference is the heartbeat of the organization, the editorial and media team keeps the energy flowing year-round. Biweekly LinkedIn articles spotlight innovators, companies, and emerging technologies transforming healthcare. Topics range from clinical needs and design processes to regulatory tensions and the social impact of biomedical engineering.
Recent features include a profile of Dr. Amir Hooshiar and McGill’s medical robotics SuPER Lab, a deep dive into AIdriven drug discovery startup Conscience, and an opinion piece on how shifting U.S. healthcare policy under President Trump’s second term, might affect Canadian research collaborations.
“When I first went into BME, I had no clue how big the field actually was until I joined editorial with CUBEC,” said Aric Quan, former co-VP of editorial. “Through this, I was able to build many meaningful connections and truly learn what it means to be a biomedical engineer.”
Dr. Lillian Hung is an associate professor with the University of British Columbia (UBC) School of Nursing and a clinical nurse specialist at Vancouver Coastal Health. Hung is the founder and lead of the Innovation in DEmentia and Aging (IDEA) Lab.]
Leveraging AI to optimize efficiency, improve patient access to care
BY MAISIE CHEUNG
As artificial intelligence (AI) becomes increasingly embedded into our daily lives, a growing number of hospitals and healthcare partners are turning to Medtronic Canada to find ways to leverage the power of the emerging technology to improve patient care and optimize their operations.
For nearly a decade, Medtronic’s Integrated Health Solutions (IHS) team has been helping health care organizations cut through complex challenges that limit efficiency, drain already strained resources and create barriers to timely access to patient care.
But the rapid evolution of AI and machine learning over the past couple of years has been a game changer for the IHS team as it supports healthcare providers to optimize care pathways and improve operational efficiency.
Medtronic recently launched a suite of innovative solutions and services called CarePathIQ that combines the IHS team’s traditional consulting expertise with a portfolio of digital and AI-powered tools –including predictive analytics, remote monitoring, and patient engagement technologies – tailored to meet the unique needs of each healthcare environment.
The initiative is central to Medtronic’s vision of intelligent, data-driven patient pathways that reduce wait times, shorten the time from diagnosis to therapy by addressing systemic challenges in Canadian healthcare. The end goal is to get patients timely access to the right care, without in-

creasing the health human resource burden or financial budget.
CarePathIQ is built on a partnership model, where Medtronic’s IHS team works with hospitals and health systems to codevelop and implement solutions that address their specific operational challenges.
By integrating real-time data, automating administrative tasks, and supporting multidisciplinary teams, CarePathIQ allows providers to deliver timely, appropriate, and coordinated care. This collaborative approach enhances patient compliance, streamlines recovery protocols, and fosters innovation in clinical practice.
AI is increasingly being incorporated into this suite of solutions to progress a smart healthcare system. From AI-powered diagnostic support to intelligent clinical decision support systems, AI can enable smart hospital operations, which in turn improves the
patient experience. By optimizing resource allocation, patient flow, and operational efficiency, clinicians can dedicate more time to patient care, reduce burnout, and establish a much more efficient care pathway for all.
In addition to increasing operational excellence, Medtronic is using AI as a tool to help hospitals decrease health risks for patients.
Imagine using AI to find potentially dangerous heart problems which may have otherwise gone undetected until patients arrive at the emergency department experiencing a cardiac episode. For one customer, we used a custom-written algorithm to scan hundreds of thousands of echocardiogram records to identify patients who may have underlying aortic stenosis that may have been overlooked during regular diagnostic testing.
These patients are flagged for further
investigation by a cardiologist who can then confirm the finding and determine an appropriate course of treatment. Identifying these at-risk patients with the help of AI helps better protect them against possible health problems in the future and helps them get medical support earlier.
AI capabilities are also being added into more of our growing line-up of innovative medical devices, such as robotic-assisted surgery platforms, colonoscopy and endoscopy systems, cardiac monitoring, and insulin pumps.
For example, our GI Genius intelligent endoscopy module relies on AI and a deep-learning algorithm to act as a second set of eyes for physicians during colonoscopies. It scans every visual frame of the procedure in real-time and alerts physicians to the presence of lesions – including small, flat polyps that can easily go undetected by the human eye. Earlier detection, powered by AI, helps hospitals increase colon cancer prevention.
As AI applications for healthcare continue to advance at lightning speed, Medtronic is determined to keep ahead of the curve and identify the right AI tools for our customers. Our AI strategy is focused on deeper integration of predictive analytics, workflow automation, and personalized care tools. Our sights are set on continuing to empower providers and patients, set new standards for operational excellence, and drive continuous improvement in healthcare delivery across Canada.
Maisie Cheung is senior director of marketing at Medtronic Canada.
AI analyzes headaches, and new methods relieve them, company says
BY KEREN GOLAN
When Idan Health deployed an AI system that connected chronic headaches in women with endometriosis, EDS, fibromyalgia, and MS, it revealed something profound: we’ve been treating symptoms while ignoring the underlying biochemical architecture. For clinicians who pride themselves on thinking beyond the obvious, this discovery offers a compelling new approach to chronic migraine treatment.
Understanding the migraine challenge: Chronic headaches and migraines affect millions of people worldwide. The suffering extends far beyond the immediate pain. For many sufferers, migraines are a debilitating condition that persists for years or even decades. It’s a resistant condition: although there are plenty of drugs to alleviate the symptoms, the underlying condition persists after these treatments, and the migraines return.
Traditional migraine management typically focuses on pain relief and prevention through medications, lifestyle changes, and trigger avoidance. However, for many patients, these approaches provide only temporary relief, leaving them trapped in cycles of recur-
ring pain and medication dependency.
The hidden connections – What AI revealed: Idan Health’s breakthrough in migraine treatment emerged from an unexpected discovery made through artificial intelligence pattern recognition.
While analyzing medical data from thousands of patients, our algorithm identified a previously unrecognized connection between chronic headaches and specific underlying chemical imbalances.
The AI system identified a striking pattern among women suffering from various conditions including:
•Endometriosis
•Ehlers-Danlos Syndrome (EDS)
•Fibromyalgia
•Multiple Sclerosis
What connected these seemingly disparate conditions was a shared symptom: chronic headaches accompanied by specific blood chemistry patterns that had never been correlated before.
Unlike traditional approaches that focus on managing pain after it occurs, this discovery pointed toward addressing the root chemical cause of chronic headaches. The research suggested that certain chemical imbalances in the body were creating the conditions for chronic headache patterns to develop and persist.
The AI’s pattern recognition revealed
something crucial: these diverse conditions shared not just chronic headaches, but specific, measurable chemical imbalances. This discovery suggested that rather than treating headaches as isolated symptoms, there might be an opportunity to address the underlying biochemical disruptions causing them.
This insight led Idan Health’s research team to ask a different question: What if we could correct these chemical imbalances directly? Instead of managing pain
Instead of focusing on managing the pain, the discovery pointed to addressing the causes.
after it occurs, could they prevent headaches by restoring optimal biochemical balance?
The brain recalibration protocol: Building on the AI discovery, Idan Health developed a treatment approach based on a revolutionary concept: training the brain to maintain the chemical balance that prevents headaches from occurring in the first place.
The treatment leverages the brain’s natural ability to recalibrate – similar to
how the body adjusts to maintain a new weight after diet changes. By providing specific nutritional supplements for a defined period, the brain learns to maintain a chemical balance that eliminates the conditions causing chronic headaches.
Treatment evolution and refinement: The development of this groundbreaking treatment unfolded through several phases of research and refinement, each building upon previous discoveries to create increasingly effective protocols.
The initial protocol, launched in 2021, involved an intensive three-month supplementation regimen tested on a small but significant group of 16 women, including the founder herself.
This pioneering phase achieved remarkable results, with participants experiencing complete elimination of their chronic headaches. Most importantly, these results proved durable, with participants remaining headache-free for over 3.5 years without requiring any ongoing treatment.
Building on this early success, the research team expanded their study in 2022 to include 47 individuals, comprising 45 women and two men. This second phase yielded an unexpected but encouraging discovery: participants


















360° Cardiovascular Care





















1
Scan to watch the video




Syngo Carbon Cardiology powered by syngo Dynamics










Evolved syngo Dynamics is a unified cardiovascular imaging and information solution designed to enable enterprise-wide reading and smart structured reporting, anywhere, anytime.





Access anywhere, anytime¹








































































systems
systemsHemodynamics





Remote Workplace Forviewing,post-processing, and creating reports in low-bandwidth environments. Workplace Fordailyclinical operations,along with diagnostic andinterventionalequipment.
Multi-modality image review and evidence-based reporting system

• Adult& pediatricecho
• Vascular ultrasound
• Maternalfetalmedicine
• Cardiaccatheterization
• Angiography
• Nuclear medicine
• CardiacCT & MR 1
syngo Dynamics seamlessly consolidates multi-modality images and data for a holistic patient view.

The


is
to view images and reports from a smartphoneortablet.
Vendor-agnostic measurements are automatically populated into the syngo Dynamics worksheet. Based on clinical guidelines, reference and normality values are applied to produce evidence-based reports.
Structured reporting enables storage of all clinical and operational information in a single database. Key indicators can be analyzed to improve efficiencies and in clinical research.
AI-assisted breast screening helps radiologists detect cancer earlier
BY KRISTEN TAM
When Linda went for her routine mammogram at North York General (NYG), she expected it to be just another screening appointment to check off her list. Her images were reviewed by a radiologist, and at first glance, nothing seemed out of the ordinary.
But behind the scenes, NYG was piloting a new artificial intelligence (AI) tool called Genius AI Detection. The technology, developed to act as a second set of eyes for radiologists, flagged a 3mm lesion that had previously gone undetected.
Because of that second look, Linda’s care team was able to act quickly, arranging further imaging, a biopsy, and treatment. She underwent cryoablation, a minimally invasive procedure that freezes and destroys cancer cells, which successfully treated the cancer.
Linda’s story is anonymized to protect her privacy, but the lesson it illustrates is powerful. Thanks to the generosity of our donors and support from the North York General Foundation, artificial intelligence is already changing lives at NYG, and Linda’s story demonstrates the real-world potential of AI to improve patient outcomes.
“By giving radiologists another set of highly advanced eyes, Genius AI Detection solution is helping us detect potential cancers earlier,” said Dr. Ryan Margau, NYG chief radiologist and medical director of the Department of Medical Imaging. “That has a direct impact on survivorship because the earlier we find it, the better the chances for our patients.”
North York General is setting a new standard in breast cancer care. NYG is the first and one of the very few sites in Ontario to offer tomosynthesis (3D mammography) as the standard screening method for every patient and the first site in Canada to integrate Genius AI Detec-

tion technology into its breast screening program. In addition, it is the only hospital in Ontario providing cryoablation as a treatment option for breast cancer.
NYG is proud to be the only breast cancer centre in Canada to be internationally accredited by the National Accreditation Program for Breast Centers (NAPBC), which recognizes our commitment to the highest standards of quality and patient care. Together, these innovations are redefining what early detection and breast cancer treatment can look like, improving outcomes and recovery experiences.
Genius AI Detection solution is powered by deep learning and integrated into Hologic Dimensions Mammography Systems. Its algorithm combs through every slice of breast tomosynthesis or 3D image sets, looking for subtle patterns that could suggest abnormalities like cancer. It is trained to identify three main categories of concern: calcifications, masses, and tissue distortions, or any combination of these.
When something suspicious is detected, the system highlights the area for the radiologist to evaluate. It also generates caselevel metrics, flagging higher-risk cases for immediate review. In doing so, Genius AI Detection technology enhances the expertise of radiologists, providing an added layer of safety so that no detail is missed.
With the Genius AI Detection solution, radiologists can prioritize their workloads more effectively and focus their expertise where it is needed most. For patients, this translates into early detection and potentially faster access to treatment, which can make all the difference.
“Genius AI Detection technology was created to give radiologists greater confidence in their interpretations while helping patients get answers sooner,” said Jay Malayny, Hologic vice president & general manager, Canada & LATAM. “Seeing North York General lead the way by integrating our technology into routine screening is inspiring. They are setting a
new standard for how AI can elevate breast cancer care from the outset.”
At North York General, adopting AI tools is not about chasing the newest technology, but about enhancing the delivery of care. The hospital’s approach to AI adoption has always been thoughtful and deliberate with a clear focus on solving practical challenges for both clinicians and patients while safeguarding privacy and security. Whether supporting clinicians or improving patient experiences, NYG remains committed to a transparent and ethical approach to AI that is firmly aligned with our values.
“By integrating AI into our clinical workflows, we’re able to reduce the administrative burden on providers, support better clinical decision-making, and ultimately enhance the quality of care for our patients,” said Dr. Phil Shin, NYG chief medical information officer.
As one of the first hospitals in Canada to bring AI into everyday clinical practice, NYG is shaping what the future of digital health looks like. From pioneering Canada’s first cloud-based electronic health record to leading the way in AI adoption, North York General has built a reputation for turning innovation into impact. Genius AI Detection solution is the latest example of how NYG is translating digital transformation into meaningful outcomes at the bedside.
“Digital initiatives like AI are key enablers to our new 10-year Strategic Plan,” said Duska Kennedy, NYG vice president strategy, digital health and chief digital officer. “They allow us to deliver the best possible care by excelling in specialized areas, responding to the diverse needs of our community, and equipping our teams with the very best technology available. That combination is what will truly set us apart for our patients and families.”
Kristen Tam is a Senior Communications Specialist at NYG.
KHSC expands surgical robotics program, adds second surgical robot
Kingston Health Sciences Centre (KHSC) is strengthening its position as a national leader in robotic surgery with the addition of a second surgical robot. The new system, made possible through the generosity of donors, will allow KHSC to effectively double the number of robotic-assisted procedures performed in Kingston and expand access to more patients across the region.
KHSC launched its A. Britton Smith Q.C. Robotics Program in 2018, and since its first year has grown from performing about 130 robotic-assisted surgeries to more than 400 each year. The program, initially focused on urology, now includes colorectal, gynecology, and thoracic surgery and KHSC is now recognized as Canada’s leader in robotic-assisted colorectal cancer surgery.
“This expansion means even more patients will benefit from minimally invasive surgery, shorter hospital stays, and
faster recoveries. For some patients with complex liver or pancreatic cancers, this means avoiding a major open surgery altogether thanks to the growth of our program,” said surgeon Dr. Sunil Patel, KHSC’s robotic surgery lead.
The new robot, a Da Vinci XI surgical system, represents a major leap forward in technology compared to KHSC’s first robot that was purchased in 2018.
“It’s like upgrading your phone from an iPhone 10 to an iPhone 16 – the difference is profound,” said Dr. Patel. “We can now move around the chest and abdomen with far greater precision, take on more complex cases, and complete more surgeries in the same amount of time.”
For patients, the benefits are clear: robotic-assisted surgery reduces the need for large incisions, lowers the risk of complications, lessens the use of the intensive care unit, and shortens recovery times.
“This expansion represents an important step forward in our ability to deliver
world-class, specialized care here in Kingston,” said Dr. David Pichora, KHSC president and CEO. “We are incredibly grateful to our community, whose generous support has made it possible for us to provide patients across southeastern Ontario with greater access to this advanced surgical technology.”
“It’s like upgrading your phone from an iPhone 10 to an iPhone 16 – the difference is profound.”
The purchase of the second surgical robot was made possible through the generosity of community donors and pledges via the University Hospitals Kingston Foundation (UHKF). As technology in surgical care continues to advance, ongoing community support will be essential to ensure the robotic surgery
program at KHSC remains at the leading edge of care and innovation.
“This achievement is a shining example of how community generosity drives innovation in healthcare,” said Tom Zsolnay, president and CEO of UHKF. Jason Hann, KHSC’s executive vice president of patient care and chief nursing executive, said the expansion reinforces KHSC’s reputation as a destination for specialized care and teaching.
“Few hospitals in Canada have more than one robotic surgical system. By investing in this technology, KHSC is ensuring that patients and medical trainees in our region have access to the same leading-edge technology found in the country’s top academic centres.”
The second surgical robot is now in active use at KHSC with operating room teams beginning to perform procedures earlier this month. It is running now in parallel to KHSC’s first robot which also remains in operation.

Canadian Healthcare Technology magazine
Canadian Healthcare Technology offers the country's leading healthcare I.T. publications. And they're free to healthcare providers. Get your complimentary subscriptions now!
Canadian Healthcare Technology breaks the news about important projects, programs and technologies, and provides hospital executives and senior managers with an excellent source of information for improving the delivery of healthcare. It’s sent to over 3,900 readers in print format and to over 7,300 opt-in subscribers of the digital edition.

White Papers
eMessenger newsletter
Canadian Healthcare Technology’s e-Messenger contains breaking news about important deals, installations and developments. Four blasts are sent each month, via e-mail, to over 7,100 senior managers and executives in hospitals, clinics and health regions.
Canadian Healthcare Technology’s White Papers are sent out once a month, via e-mail, to over 5,500 senior managers and executives in Canadian hospitals and health regions. The monthly blast contains summaries and links to White Papers issued by various organizations, providing cutting-edge information about topics of interest to healthcare decision-makers.

For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
Digital workflow solutions speed up imaging bookings at Royal Victoria
BY JERRY ZEIDENBERG
BARRIE, ONT. – Last year, the Royal Victoria Regional Health Centre, in Barrie, Ont., received 175,000 requisitions for diagnostic exams – a substantial number, and one that’s expected to surge in the quickly growing community just north of Toronto.
Problem is, scheduling those exams requires a lot of people working together, and it will be difficult in an era of budget constraints and personnel shortages to hire more staff to handle the expected growth.
Add to that a second challenge: the process of scheduling DI exams currently revolves around paper. Most of the requisitions were coming in as faxes and paper forms, and even when digital, the routing in the hospital is by paper documents.
It can take days for the right people to receive and process the requisitions and send them on to the next person.
As well, all the paper has to be filed. It requires manual labour to put it all away, and of course, it’s difficult to find again, when needed.
Luckily, PACS manager Damian Hitchins has been monitoring digital referral and workflow solutions, including those assisted by artificial intelligence and other sophisticated technologies. He felt that in the past, the systems weren’t ready for real-world use, but lately, they’ve made incredible progress. He and his colleagues at RVH felt it was time to deploy them.
Earlier this year, they started testing a system developed by Toronto-based GoAutomate. Its founders come from the

banking tech world and understand the use of AI and smart agents. They’re now taking that expertise and applying it to the healthcare sector.
The solution that’s being deployed at RVH includes the ability to scan and read paper documents with great accuracy – using intelligent optical character recognition – and to automatically route them to the right people.
In tests that have been conducted, so far, referral processes that have normally taken five to seven days – from receiving the requisition to getting the patient on the imaging table – have been reduced to two or three. That’s better than a 50 percent improvement.
Hitchins explained that DI requisitions have many steps, and it helps to convert them to a digital process.
For example, in the current way of doing things, a fax requisition may come in, and a clerk will review it to make sure it
contains the right information. If not, the referring physician must be contacted and the missing information is added. Right away, that can cause a delay.
The form then goes on to a technologist who applies the right protocols to the exam.
If the technologist has an issue with the right protocol or procedure, it goes on to the radiologist to decide. At that point, the MRI, CT, or other exam can actually be scheduled.
All of this requires physically walking the paper around to the right people. In the process, it can get lost or may get stuck in someone’s in-basket.
But with the GoAutomate solution, the forms are sent on electronically with alerts. They can’t be lost, and routing is instantaneous.
There are also impressive service improvements. For instance, Hitchins notes that “physicians will sometimes call in and ask if we received their requisition for a certain patient. Before, we couldn’t always

do it, because we couldn’t physically tell where the file was in the process, or whether we even got the requisition.”
Now, however, it’s easy to look in the electronic record system to see whether it was received and where it is in the entire booking and scheduling process.
GoAutomate CEO Jag Basrai observed that the system contains artificial intelligence – not ChatGPT, but a fine-tuned Large Language Model trained in-house, specifically for healthcare and specifically for each hospital network. It can read a wide variety of forms, including faxes, paper documents or emails with astonishing accuracy.
“It doesn’t matter if it’s a 10-year-old requisition form used by a doctor’s office or a new form from another institution that looks very different, our system will read it,” said Basrai.
Once a document is scanned or a digital message is read, GoAutomate Agentic AI can determine which fields to put the patient information into, and it can figure out if data is missing. If so, it can alert the clerk to obtain it or approve for the next step, so very little is missed.
Sometimes, clinics will send in a requisition for the same patient several times, or send supplemental information later; Basrai says this is not a problem, as Agentic AI can detect whether duplicates or additional documents have been received.
The GoAutomate system can be set up to alert the referring physician when the patient has an appointment, so the doctor can let the patient know. In future, Hitchins said, it could also alert the patient.
Impressively, to help technologists and radiologists and to speed up the whole booking process, GoAutomate’s AI capabilities are being used to do protocolling of standard exams.
Hitchins explained that in many cases, such as MRIs of the knee, many of the exams are of the same type. “If it’s a case of an ACL tear, we can automatically schedule a 15-minute exam. But the doctor will have a chance to review and may say he’d like a 30-minute exam if he’d like to see more images.”
Hitchins added, “The system can do a lot of the protocolling, because of machine learning. It’s a matter of, we’ve seen this many times before and 90 percent of the time it requires a certain protocol.” So that can be scheduled, and most of the time it will be fine. Of course, the radiologists will be reviewing and can easily change the protocols.
But in cases where it’s straightforward, it’s saving the technologists and the radiologists a lot of time and keystrokes. That reduces some of the pressure on these imaging professionals who have been suffering from burnout.
Hitchins said the hospital has already integrated the GoAutomate system with its PACS, which is an Optum solution. It’s also integrating GoAutomate with its MEDITECH electronic health record.
He said that once the GoAutomate system is fully operational in the diagnostic imaging department, the plan is to take it into other departments. He noted, it’s a whole platform for automating and improving processes in the hospital.
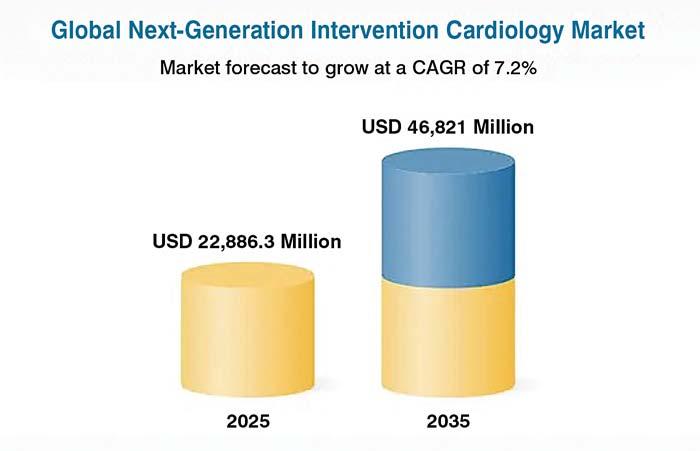
Robotic surgery, AI set to impact cardiology the next five years: study
DUBLIN – The global next-generation interventional cardiology market is expected to witness significant expansion, projected to reach $46.82 billion (US) by 2035, driven by the escalating burden of cardiovascular diseases – including coronary artery disease, structural heart defects and valvular disorders – that demand safer, more precise alternatives to open-heart surgery, according to a new study from Research & Markets.
This market is anchored in minimally invasive, catheter-based solutions that integrate advanced robotics, and AI-guided imaging to deliver superior procedural accuracy, faster recovery, and expanded patient access, says the study, titled The Next Generation Intervention Cardiology Market: A Global and Regional Analysis.
Next-generation intervention cardiology represents a paradigm shift, combining automation, data-driven precision, and operator ergonomics to improve outcomes while reducing occupational hazards.
Key milestones, such as the commercial launch and adoption of robotic-assisted Percutaneous Coronary Intervention systems like Robocath’s R-One – currently the only commercially available R-PCI platform – have validated these disruptive approaches and the CE Mark for transcatheter mitral valve replacement
(TMVR) platforms, have underscored the shift toward standardization and scalability of catheter-based therapies.
Market expansion is further bolstered by supportive reimbursement and regulatory pathways in the U.S., EU, and Japan, alongside investments by public and private sectors in cath lab modernization, operator training, and digital integration. Countries across North America, Europe, and Asia-
Pacific are scaling infrastructure and fostering innovation hubs, with emerging economies such as India and Brazil offering significant untapped potential for nextgeneration intervention cardiology market.
Technological convergence is accelerating growth, with innovations such as AI-enabled OCT/IVUS imaging, remote robotic PCI platforms, and bioresorbable scaffolds enhancing both pro-
cedural quality and long-term outcomes.
Leading players such as Abbott, Medtronic, Boston Scientific Corporation, and Terumo Corporation are shaping the competitive landscape, advancing first-in-class devices, expanding portfolios, and investing in clinical validation and commercialization to strengthen their foothold in next-generation interventional cardiology.
As healthcare increasingly prioritizes precision medicine, patient-centric care, and minimally invasive solutions, nextgeneration intervention cardiology stands at the forefront of cardiovascular innovation, poised to redefine care paradigms and improve outcomes for diverse patient populations worldwide.
The field of cardiac care is increasingly shifting toward minimally invasive, catheter-based interventions that offer shorter recovery times, reduced procedural risks, and lower healthcare costs –particularly beneficial for elderly and high-risk patients. Techniques such as Transcatheter Aortic Valve Replacement (TAVR), Left Atrial Appendage Closure (LAAC), MitraClip, and robotic Percutaneous Coronary Intervention (PCI) are progressively replacing traditional openheart surgeries, establishing themselves as standard-of-care treatments for various cardiac conditions.
Elevating interventional cardiology: Shimadzu Trinias with SCORE Opera
Christie Innomed is proud to bring to the Canadian market the new Shimadzu Trinias with SCORE Opera, which represents a significant step forward for clinicians seeking to optimize outcomes, reduce procedure times, and streamline workflows.
In interventional cardiology, precision, efficiency, and patient safety are paramount. Shimadzu redesigned the workflow of the Trinias angiography systems to offer improved solutions for the challenges currently facing medical treatment centers and to address the challenges that they will face in the future.
Building on years of trusted performance and feedback from interventional radiologists and cardiologists worldwide, this latest generation of Trinias is designed to deliver an experience that feels as intuitive as it is innovative, the company said.
For many medical professionals, Shimadzu is already a familiar and trusted name in radiology systems.
Over the years, it has built a reputation for combining image quality with dose reduction and system reliability. With the latest iteration, Shimadzu has pushed the boundaries of what is possible, refining not just the hardware, but also the software intelligence that supports clinical decision-making.
A new benchmark in image processing: At the heart of this generation is SCORE Opera, Shimadzu’s latest imaging engine. Designed with the end-user in mind, SCORE Opera integrates ad-
vanced image-processing algorithms that allow for exceptional clarity while maintaining low radiation dose.
Clinicians will notice sharper visualization of vessels, improved contrast resolution, and reduced background noise – essential for complex interventional cardiology procedures.
Real-time image processing ensures that even challenging cases – such as those involving patients with calcifications or overlapping vessels – can be visualized with confidence.
SCORE Opera also facilitates smoother navigation through complex anatomies, enabling faster, more precise interventions.
Dr. Brian Brown, interventional cardiologist at Cardiology Consultants in Spartanburg, S.C., said, “This [SCORE RSM] is my favorite feature…and the main reason I bought the product [Trinias]. It provides the ability to show a detailed DSA like image ‘real time smooth masking’ with motion.”
Smart Voice: An intuitive leap forward: Among the most innovative additions to this generation is Smart Voice, a voice-recognition feature that allows clinicians to control key system functions hands-free.
Including SMART Voice function improves examination efficiency and reduces the burden on physicians and healthcare personnel.
During lengthy and delicate procedures, Smart Voice enables operators to adjust imaging parameters, store images, or change display settings without break-
ing sterility or interrupting workflow. This not only enhances procedural efficiency but also supports a more ergonomic working environment, reducing the need for repetitive manual inputs.
Optimizing workflows for cardiology: Efficiency is central to this new platform. From quicker system boot times to customizable user interfaces, the Trinias with SCORE Opera is designed to fit seamlessly into busy cath lab schedules. Its enhanced motion control delivers smooth C-arm movement and faster positioning, reducing procedure time and minimizing patient discomfort.
In cardiology, where every second counts, these workflow improvements can make a tangible difference. For example, reduced preparation time and in-

tuitive controls help teams move swiftly from diagnostic imaging to therapeutic intervention, supporting faster decisionmaking and treatment initiation.
Radiation dose management: Safety without compromise: Radiation safety remains a priority for both patients and
clinicians. SCORE Opera employs sophisticated dose-reduction technologies, including pulse rate optimization and advanced noise-reduction algorithms, to keep radiation exposure as low as reasonably achievable (ALARA). Dose tracking and reporting tools provide transparent data for continuous quality improvement and compliance with regulatory requirements.
Seamless integration and connectivity: The new Trinias is designed to integrate effortlessly with existing hospital IT infrastructure, RIS, and PACS systems. Its compatibility with multimodality imaging and data sharing ensures that cardiology teams can access comprehensive patient information at the point of care, supporting collaborative and informed decision-making.
Shimadzu’s focus on scalability ensures that the system can evolve with the changing needs of healthcare facilities. Modular upgrades and software enhancements make it possible to stay current without requiring full system replacement, protecting the investment for years to come.
Developed with direct input from cardiologists and technologists, the new Trinias with SCORE Opera offers superior imaging, intuitive workflow, and intelligent automation. At a time when cardiology teams face growing demand for faster diagnoses and better outcomes, this system helps them focus on what matters most: patient care.
It’s not just an upgrade, it’s a leap forward in angiography technology.
St. Joseph’s Healthcare Hamilton develops new systems in forensic psychiatry
VR has proven to be effective for training, while Cloud-based eHARM helps measure and manage risk.
BY DIANA MARGINEAN RN, BScN, MSc AND DR. GARY CHAIMOWITZ
St. Joseph’s Healthcare Hamilton has recently implemented several innovations in forensic psychiatry, most notably using virtual reality (VR) in staff training and the launch of a cloud-based violence risk management tool.
Staff training in healthcare has long been difficult to deliver effectively, largely due to shift work, high costs, and limited engagement. Traditionally, education for doctors, nurses, and other clinical staff has been delivered synchronously, and has taken place in classroom settings through lectures or seminars, sometimes supplemented with live reenactments of health events using actors or mannequins.
Over the past six years, Dr. Gary Chaimowitz, head of service, and myself, Diana Marginean, knowledge translation specialist, both of us with the Forensic Psychiatry Program, have worked with an Ottawa-based simulation company to develop multiple VR staff training scenarios. The Forensic Psychiatry Program has been using VR as an adjunct to traditional education, enabling healthcare workers to navigate challenging situations safely and ethically. The setup is simple, requiring only a VR headset and a laptop, with an instructor guiding learners through each simulation.
During training, staff don VR headsets and use handheld controllers to feel present physically in a scenario and interact with simulated patients and colleagues, providing realistic and immersive experiences.
Simulations include responding to a code white (a violent patient), code blue (a medical emergency), and some forensic psychiatry – specific scenarios, such as a courtroom walkabout or expert witness testimony experience. Unlike passive learning methods such as listening to lectures, immersive learning places the learner directly in a realistic environment where they must make clinical decisions that have an immediate impact on patient care and safety.
The benefits extend beyond technical skills. These sessions also strengthen soft skills like communication and empathy – really understanding the patient’s perspective and how to interact with them.
Since skills are acquired more rapidly, there is a cost savings by reducing the time staff spend in training and minimizing the need to backfill shifts for education.
Staff have the ability to learn at their own pace and within their comfort levels. There is an ethical and safety element to this form of training. Staff can experience any anxiety and stress in an environment where no one is at risk, and their exposure can graduate as their skill and comfort increases.
Early feedback from the pilot has been very positive. One participant described VR as “a great tool to aid staff with getting a feel of intense situations before going hands on in the workforce. The ability to practice in a safe and controlled environment without the risk is appealing.”
Looking ahead, the virtual reality training program hopes to expand and embrace new technology, such as incorporating artificial intelligence into scenarios to create dynamic, interactive scenarios that more closely resemble real life experiences. With continuous advancements in headsets, immersive virtual environments, and large language models, the Forensic Psychiatry Program is committed to re-


maining at the forefront of this technological evolution.
eHARM: The assessment and management of risk has been a major area of concern and focus in mental health settings. Although there are several tools that assess risk over time, they are time-consuming, require additional training and expertise, and only predict long-term risk. What has been missing is a tool to assess and manage short-term risk in order to assist clinical staff in their day-to-day tasks.
In addition, notwithstanding the concern about violence in mental health units, there has been no easy way to measure violence, and hence there is a problem in managing something you cannot measure. It is into this space that the Aggressive Incident Scale (AIS) and eHARM landed.
Driven by advancements in health information technologies, the development of a cloud-based risk
eHARM takes only a few minutes to complete, is done by the team as a group and collects hundreds of data points each time.
assessment tool represents a significant opportunity to elevate clinical practice and patient care in psychiatry. Violence risk assessment and management are important aspects of forensic psychiatry clinical practice. Forensic patients are often detained within the hospital and one of the primary goals of the clinical team is to help them reintegrate back into the community safely. Community patients also require nimble assessment and management of their risk.
Drs. Gary Chaimowitz, head of Service, and Mini Mamak, senior psychologist with the Forensic Psychiatry Program, co-developed the Hamilton Anatomy of Risk Management (HARM), a structured professional judgment tool, to enhance the short-term risk assessment and risk management process, guide treatment planning, and foster team-based risk assessment.
What began as a paper-based assessment, moved to an Excel based version and now has transformed into a modern, cloud-based platform.
Each month, the clinical team reviews patient

progress and collaborates within the online tool, which can be accessed seamlessly across devices and locations. The eHARM system is further strengthened through its integration with the nine-point measure of aggression, the Aggressive Incident Scale – widely recognized as a gold-standard measure of aggression.
eHARM takes only a few minutes to complete, is done by the team as a group and collects hundreds of data points each time.
The functionality is impressive, with the ability to graph multiple factors, predict risk and manage risk and predict elopement.
Moreover, it serves as a source of readily available data that allows for research and quality improvement for groups of patients and organizations.
The data collected has allowed for machine learning and the use of big data to predict and manage risk. Staff work well as teams, speak on point with respect to research-validated risk criteria and make their decisions based on evidence, truly transforming the way we assess and manage risk.
The cloud-based eHARM system:
•streamlines the collection and analysis of risk and management data;
•facilitates more individualized risk assessment and management;
•enhances patient care by providing deeper insights through improved functionality and analytic capabilities;
•increases accessibility and adoption of risk assessment, including for services in remote, community, or underserviced areas;
•allows for the use of big data in predicting and managing risk;
•shows clinicians a patient’s progress on risk factors over time, and
•exports data and creates reports to answer specific questions.
Diana Marginean RN, BScN, MSc is project lead and knowledge translation specialist, Forensic Psychiatry Program, at St. Joseph’s Healthcare Hamilton. Dr. Gary Chaimowitz is a forensic psychiatrist and Head of Service with the Forensic Psychiatry Program at St. Joseph’s Healthcare Hamilton.
Dr. Gary Chaimowitz Diana Marginean
Mini Mamak
50 years of contributing to Canada’s evolving digital health knowledge
BY SHELAGH MALONEY
For half a century, Digital Health Canada has been a trusted convener of ideas, expertise, and shared learning. Since its founding in 1975, the association has brought members together to compare notes and share lessons learned as they work to advance digital health across Canada. What began as a small network of like-minded professionals has grown into a national association whose collective output reflects the evolution of Canadian health and healthcare innovation.
A tradition of knowledge sharing: From its earliest days, Digital Health Canada supported members in navigating emerging technologies and complex policy environments through networking, conferences, and peer-to-peer collaboration. These meetings made clear that, as a collective, Digital Health Canada members possess a wealth of knowledge and realworld experience that could benefit people outside the circle of membership.

Select member groups began volunteering on working groups and committees to formalize the contributions they made at conferences and networking events into reports, frameworks, courses, and toolkits that could be more widely shared. The creation of an online resource library in the 2000s marked a turning point. For the first time, member-produced reports and guidance documents were collected in a central, publicly accessible repository. While the library itself does not extend back to the 1970s, it represents the continuation of a 50-year tradition: members coming together to capture insights and translate them into practical resources for the entire community.
Anchored in real resources: Today, the Digital Health Canada Resource Library showcases the breadth and depth of digital health expertise of our members from across Canada.
Early publications (2013-2015) anticipated the importance of patient data safety and set out to establish guidelines for esafety and the protection of health information. These best-practice resources acted as valuable tools for helping healthcare providers and other health informatics professionals enhance patient safety around eHealth solutions and provided a foundational model for establishing, implementing, operating, reviewing, maintaining and improving an eSafety management program.
Members also worked together in ad hoc groups to drill down on a single subject and produce white papers with findings always supported by the real-world examples available to those working in digital health. Examples include:
•The Digitally Empowered Patient. The Working Group behind this paper engaged patients, healthcare providers, system leaders and vendors across Canada to gain diverse perspectives on the barriers to wide-
spread access and adoption of digital health tools and services.
•Patients in Tech. To create this paper, thirteen subject matter experts from across Canada were interviewed and provided their insights, perspectives, and lessons learned on the topic of patient and family
partnership programs and their viability in the digital health space.
•Technology Adoption in Care Transitions. This paper offers an overview of Canadian home and community care technology used in care coordination and integrated patient transitions.
•Canada and Shared Information Governance: Expanding on Governance Standards – Steps Enabling Canada’s Digital Health EcoSystem. This timely update on earlier governance standards includes case studies that demonstrate the willingness of


Shelagh Maloney
AI technology will likely shore up the weak spots in care delivery
BY JERRY ZEIDENBERG
TORONTO – At the recent OntarioMD conference in September, keynote speaker Dr. Muhammad Mamdani, VP of data science and advanced analytics at Unity Health Toronto, asked the audience of physicians whether they’re seeing AI in their clinics. Many hands went up.
No doubt it’s because of the rapid uptake of ambient AI, with smart systems taking notes for the doctors. Many are eager to see the solutions start charting, too, and sending referral notes to specialists. These applications are already in the works and are not too far away from real usage.
As breathtaking as these solutions seem, there are many AI apps on the way that are even more mindboggling. Dr. Mamdani outlined some of them, giving doctors a heads-up about what’s in the pipeline.
Pointing out several areas in which the medical profession has been underperforming, he showed how AI-powered computers could be incredible helpers for physicians and other clinicians.
Dr. Mamdani zeroed in on some nagging medical problems, such as misdiagnosis.
“There is a study from the University of Toronto that looks at Parkinson’s disease. If you look at the literature, 20 to 30 percent of patients initially diagnosed with Parkinson’s disease have been misdiagnosed,” he said.
He noted, similarly, that 50 percent of patients diagnosed with schizophrenia have been shown to not have schizophrenia. And in a Canadian study, 600 patients diagnosed with asthma were later shown not to have asthma.
Could AI assist physicians in these areas? The implication is, of course it could, while acting as a highly intelligent clinical support system.
“Do you really need [AI] for the things that you do, from diagnosis to prognosis, to treatment to communication?” he asked. “Some would argue that you don’t. But many would argue that you do, if you actually step back and say, honestly, how good am I at this?”
With physicians being so stressed and experiencing cognitive overload, computers could be their salvation as decision support systems, or intelligent helpers.
Dr. Mamdani noted the average medical decision involves hundreds of parameters – from “signs and symptoms to medical imaging results, social histories, labs, vitals, diet, exercise, family history, sleep, let alone the plethora of evidence that’s out there in the published literature.”
“That’s a lot to go through your head.”
It can lead to serious repercussions when it comes to patient care. The overload sometimes leads to oversights.
Dr. Mamdani observed that one in four patients
How often were the doctors right?
Only 29 percent of the time.
It’s situations like this that led St. Michael’s Hospital to create its own AI-powered solution to monitor patients and to predict when they need additional care – especially when they’re going to crash.
The early-warning algorithm, called CHARTwatch, runs each hour and considers between 150 to 170 parameters, such as vitals, labs, and demographics. “And it predicts if someone is going to die,” said Dr. Mamdani.
If the algorithm reaches a certain threshold, it contacts the patient-care team. At that point, a medical team has to come see the patient within one hour.
Empathy for patients is another troublesome area for doctors, and one where machines actually performed better. Dr. Mamdani cited a study in which patients rated the empathy of ChatGPT as 10 times better than their GPs.
Dr. Mamdani said there are reasons for this, such as the stressful working lives of many doctors. Physicians often have time only for short answers, and must move on to the next patient, while ChatGPT has all the time in the world.
For this reason, ChatGPT and other AI solutions are particularly good at mental health applications. Indeed, in this area, patients often say that AI is as good as a human therapist.
“You’re going to see more of these sorts of solutions – such as AI for kids’ health lines. They’re working, for example, on launching a chatbot for youth in crisis.”
who are hospitalized experienced harm, and one in eight were harmed so significantly that it resulted in a longer length of stay or permanent harm that required life-saving intervention.
Another problem spot that Dr. Mamdani focused on was patient prognosis – forecasting outcomes for patients.
“So, let’s say you’ve made the right diagnosis. Now you’re on to prognosis. How good are we at this? Study after study shows how terrible we are.”
Ouch!
Dr. Mamdani said his own group did a study of the accuracy of doctors when it comes to judging which of their patients will live and which will die. To do it, they collected over 3,000 clinician predictions about their patients. It was done with clinicians working on hospital floors.
“It’s been running for four years, and it is showing a 26 percent reduction in patient mortality,” he said. The system has now been expanded to St. Mike’s sister hospital, St. Joseph’s.
It’s not that the computer is better than humans, said Dr. Mamdani. It’s that physicians are dealing with a huge cognitive load and need some help.
“It’s helping you focus, because you don’t have time to really do a good job in terms of understanding who the high-risk patients are. You have too many demands.”
On a different front, Dr. Mamdani mentioned a project in India where physicians have gone much further with AI scribes than what we’re seeing in North America; not only is the AI scribe in India taking notes, it’s embedded in the EMR, and it’s bringing DI and lab test results – and more – to the attention of the doctor. By clicking on a bubble, the computer system announces, “I see you’ve diagnosed a urinary tract infection, here are the three antibiotics that are recommended by national guidelines.”
The system is also integrated with a pharmacy in the same building, so the doctor can send the prescription to the pharmacy and the patient can pick it up on the way out.
While Dr. Mamdani observed that countries such as China and India are ahead of Canada in the application of AI to medical care, a member of the audience asked whether this is because of stricter ethical guidelines in Canada and the U.S. Dr. Mamdani asserted that in the case of India, it’s most likely due to that exact situation. “I asked the doctor in India whether he had obtained patient consent for this, and the answer was no, of course not, why would I?” The audience found this amusing but instructive about the national differences in AI development.
Dr. Mamdani averred that for better or worse, the markets where the regulatory environment for AI are weaker will move ahead faster than in North America.
“I do think where the markets are not as regulated, they’re going to be way ahead, for good or bad reasons. And this is the balance between how much do we regulate versus how progressive can we be and how innovative can we be? It’s gonna be a tough balance.”
Dr. Muhammad Mamdani contends that Canada’s healthcare system is troubled by misdiagnosis and that AI could help clinicians make improvements.
Nelson PULSE centre will combine AI and data for better outcomes
CALGARY – The Nelson Precision Medicine and Learning Health System (PULSE) Centre for Innovation at the University of Calgary’s Cumming School of Medicine (CSM) will establish a first-of-its-kind, provincewide data platform – one that links complex datasets to answer questions that help improve treatment and health outcomes specific to each patient.
The Nelson PULSE Centre will securely link anonymized diagnostic tests, such as imaging and electrocardiogram tracings, with laboratory, medication and lifestyle data including how people access care.
Assisted by AI technologies, this will allow researchers and physicians to identify patterns and insights that can help them answer questions about how best to detect diseases sooner and select the most effective treatments for each patient.
UCalgary alumna Susan Nelson’s $12 million gift will build on the CSM’s leadership and success connecting datasets to improve heart health outcomes through the Libin Cardiovascular Institute’s Precision Medicine Initiative.
“Knowing a donation to accelerate this work would create added value and benefit patients, caregivers, doctors and researchers, gave us a great feeling of happiness,” said donor Susan Nelson.
Nelson’s commitment will allow the current program to expand into other key areas, such as stroke, critical care, women’s health and more.
Susan Nelson is a Calgary entrepreneur, developer and community leader dedicated to building forward-thinking, technologyfocused businesses.
She has successfully launched and grown numerous companies while consistently driving positive social impact. She is a UCalgary alumni.
Her community service includes directorships with Habitat for Humanity Canada and the Leighton Art Centre, among others, reflecting her commitment to culture, housing and social betterment.
Her generosity will also enable researchers to foster province-wide collaboration and further catalyzes innovation to improve healthcare for all Albertans, said Dr. Ed McCauley, UCalgary’s president and vice-chancellor.
“Susan Nelson’s gift is a remarkable example of how philanthropy can accelerate innovation and improve lives. Susan is a very generous alumna and longtime UCalgary supporter who is helping us turn research into real-world solutions and position UCalgary to be a global leader in precision medicine – we’re deeply grateful,” said McCauley.
Right now, disconnected sets of health information exist across the province. The Nelson PULSE Centre has already established infrastructure that will securely link them in an anonymized way to protect patient privacy.
Artificial intelligence and other tools allow researchers, health administrators, doctors and nurses to provide personalized treatment and care for individuals and subsets of patients, or model how they might respond to a treatment.
“It’s an ambitious goal to bridge health data resources from an entire province and
bring them together for innovation,” said Dr. James White, director of the Nelson PULSE Centre “We want to make sure that all faculties and institutions, including post-secondary schools, gain access to this information to maximize its impact.”
Dean of the Cumming School of Medi-
cine, Dr. Todd Anderson, applauds Nelson’s generosity and foresight, noting that her donation “will allow Alberta researchers to make cutting-edge advancements in personalized medicine, with healthcare decision-making faster and more customized for everyone.”
Dr. Anderson adds he’s thrilled the Cumming School of Medicine’s precision medicine research leadership and its vision to advance equitable, personalized healthcare through data, AI and machine learning have attracted Susan Nelson’s investment.

Stop flying blind: Canada’s AI future risks failure on incomplete, stale data
BY MICHAEL MILLAR
Imagine the screen on a CMIO’s desk– Clinician Request: Pull all patients aged 65+ who have [Condition X] and [Condition Y], who are at risk of [Complication Z], with a family history of [A], who live in high-risk neighbourhood [B].
Every health system leader knows the punchline: Asking for a vital list of at-risk patients doesn’t yield a click; it requires launching a multi-week data excavation with no guarantee of success.
The fundamental crisis facing Canadian healthcare leaders is not just the strain on Health Human Resources; it is the systemic failure of disconnected digital systems that collectively remain unable to seamlessly connect data and reduce pressure where it matters most. Chronic issues like ED overflows and provider burnout are key symptoms of the underlying disease: ineffective, reactive population health management.
For years, the elusive “holy grail” has been the ability to easily pull accurate, reliable lists of high-risk citizens and apply stratification models to target interventions. Yet, most providers must rely on multiple, manual steps and tools to achieve this – if they can achieve it at all.
The unstructured data trap – why 80 percent of intelligence is invisible: The uncomfortable truth is that despite two decades and billions of dollars in EHR implementations, a core clinical data complexity remains unsolved. We are manag-
ing Canada’s most critical, multi-billiondollar system without much operational and clinical intelligence.
A wealth of critical clinical context –from a clinician’s analysis to critical social determinants of health – is trapped between the digital pages of a chart. This context exists primarily in uncoded, unstructured data formats (e.g., free-text notes, PDFs, faxes, dictations).
As a direct result, approximately 80 percent of all health data is contained in this unstructured format, making it virtually unusable to typical digital and AI solutions, which demand structured, standardized data, and slowing down advances in health innovation and AI sovereignty. This data blindness leads to compounding crises: •Financial paralysis: Digital investments are struggling for returns. The data’s complexity consumes high-cost operational budgets, forcing large teams into lengthy, manual data preparation of clinical text. This process traps valuable digital capital in administrative tasks, delaying critical time-to-insight by months.
•Provider burden and clinical risk: Unstructured data drives administrative overload, forcing clinicians to divert crucial patient-facing time to manual re-coding. This burden accelerates provider burnout and, more critically, creates dangerous blind spots where vital patient context is missed, increasing the risk of suboptimal care.
•The scribe paradox: AI scribes successfully reduce manual note-taking; however, by generating detailed, unclassified narra-
tives at a massive scale, these tools may inadvertently accelerate the growth of unusable data, heightening the system-wide challenge of trapped clinical contextual intelligence.
Ultimately, this inaccessible 80 percent means critical decisions on care and operations suffer data lags when timely action is most needed.

What will it take for you to see and use your data? Flexibility in our data – the ability to connect social determinants of health with acute, community, and primary care data –will be our greatest strength in delivering population health improvements within today’s fragmented digital ecosystem. This flexibility means we must solve the core problem: turning clinical stories into useful data. This isn’t just one data problem; it’s three major hurdles rolled into one:
1. Extraction: How to extract data from all healthcare data sources, including unstructured data.
2. Normalization: How to standardize and harmonize clinical concepts from different sources.
3. Concept clustering: How to group and cluster data into relevant categories for risk stratification.
Innovative Canadian solutions are now delivering this necessary layer of
More than hype: AI is driving practical
BY SIMON LING
Primary care clinicians face many challenges in Canada, including mounting administrative workloads, fragmented flows of information, and increased complexities in patient care. The promise of artificial intelligence may provide some relief by restoring a sense of balance and efficiency in healthcare systems. Yet without careful curation, integration, and governance, AI can create as many problems as it solves.
Collaborative, clinician-centred approach to AI adoption: As a provincial leader in digital health, OntarioMD (OMD) is transforming AI’s potential into tangible clinical benefits for family doctors in Ontario – securely, ethically, and at scale.
By applying a collaborative, cliniciancentred approach to AI adoption and engaging directly with key stakeholders across clinical, regional, and provincial levels, OMD ensures that AI solutions are evaluated for technical performance, usability, workflow integration, patient safety, and privacy compliance.
This includes involvement from patients (to help secure their trust in the use of AI), technology vendors (to ensure products align with healthcare needs), research institutions (to lead in-
novation in response to the user experience), and policymakers and regulators (to create the frameworks needed for safe and ethical deployment).
Clinicians, however, play a unique role in integrating AI into healthcare settings. As the primary users of AI in clinical practice and the frontline providers of care, clinicians have invaluable insights into the technology’s impact on their patients, workflows, processes, and overall decision-making.
To that end, OMD is focusing on clinicians, specifically their views and usage of AI, to facilitate its deployment in healthcare via three key initiatives.
The Ontario AI Scribe Program: In 2024, OMD led an evaluation study of AI scribes in partnership with Amplify Care and the Women’s College Institute for Health System Solutions and Virtual Care (WIHV) to address physician burnout caused by documentation overload.
The study found that participants spent 70 percent to 90 percent less time on paperwork and saved nearly four hours a week on administrative tasks. It also noted 76 percent of participants reported a reduction in information overload during patient visits.
Based on the study’s results, the Ontario Ministry of Health and Ontario Health partnered with Supply Ontario
clinical narrative intelligence. Tools such as VERTO Connect use AI-powered technology to rapidly unlock and transform trapped clinical information, converting free-text context into structured, FHIR-conformant data for clinical operations and analytics – while maintaining provenance.
Crucially, creating this foundation does not need to come with the burden of multi-month, high-cost mapping exercises.
Overcrowded EDs are the symptom, insufficient population health management is the disease
For decades, digital health solutions have been largely focused on automating the treatment of the symptoms, not curing the disease. We have optimized reactive, informational technologies – better billing, faster charting, smoother patient portals – all of which deal primarily with the crisis after it has occurred. While necessary, this focus has drawn investment away from proactive, preventative technologies that could truly bend the cost curve and improve health outcomes.
The most profound opportunity to reduce cost and improve population health lies in systems that stop a crisis before it starts, and that requires moving beyond basic data capture to true clinical intelligence – the ability to understand and act on the complete, holistic story of every person.
Michael Millar is the founder and CEO of Verto Health.
solutions for better care
and OMD to launch the Ontario AI Scribe Program to scale AI scribe use to more clinicians. The program offers a vendor of record (VOR) list that vetted solution vendors and their products against three main categories:
• Clinical and business – ensuring that solutions provide high-quality service which can integrate effectively with existing clinical workflows.

• Legal and privacy – establishing that data is used, collected, and disclosed appropriately and remains compliant with relevant privacy laws.
• Security – verifying that vendors maintain best practices in cybersecurity and protect sensitive health information to help minimize clinicians’ exposure to risk.
For clinicians, the VOR list removes the guesswork in choosing the most suitable scribe for their needs, saving them time and money. Clinicians receive change management support from OMD, at no cost to them, to facilitate the adoption of AI scribes into their practices.
AI-generated summary pages in
Health Report Manager: Technology is a double-edged sword, with significant promise and resulting challenges. Health Report Manager (HRM®) is a case in point. Created to seamlessly deliver hospital reports directly into clinicians’ electronic medical record (EMR) systems, HRM does so brilliantly, with over 4 million reports sent to communitybased clinicians each month.
However, the successful adoption of HRM also increases administrative burden, with clinicians having to review lengthy PDF reports (which are not searchable by EMR systems) and often, multiple versions of the same report.
To counter these issues, OMD is trialing a series of changes to HRM, starting with duplicate reports and the handling of highly formatted reports (i.e., PDFs).
A limited number of users will see reports clearly labelled as duplicates and will receive PDF reports that are enhanced with an AI-generated summary.
AI-powered clinical decision support partnerships: With clinicians rapidly adopting AI solutions to manage administrative tasks and enhance efficiency, there is now an opportunity to leverage this emerging technology to enhance quality of care and patient outcomes.
Simon Ling is Executive Director, Partnerships and Stakeholders, at OntarioMD.
Simon Ling
Michael Millar
Canada’s sovereignty could be threatened by AI and digital healthcare
BY WILL FALK (WITH AI ASSISTANCE)
Canada’s federal National AI Strategy Task Force was appointed on September 26, 2025, by Ministers Evan Solomon and Mélanie Joly to update the country’s approach to artificial intelligence. The panel will run a 30-day sprint through October to consult and deliver actionable recommendations aimed at restoring Canada’s position in global innovation.
Solomon asserted: “Advancing the safe adoption and accelerated development of AI in Canada – while strengthening our digital sovereignty – is essential to building the strongest economy in the G7.”
The Task Force’s report is expected in November 2025. What are the likely implications? What specific healthcare questions need to be answered?
The easy predictions: Bill C-27 (Artificial Intelligence and Data Act, AIDA) and Bill C-72 (Connected Care for Canadians Act, CC4C) both died on the order paper in the last Parliament. Those bills will likely serve as inputs to the Task Force’s review. They will be refreshed in the context of the new digital nationalism and advanced AI.
The Pan-Canadian AI for Healthcare Guiding Principles (AI4H), finalized earlier this year, will also inform the healthcare portion. Together, AIDA, CC4C, and AI4H provide a solid legislative and regulatory foundation to build upon.
Many of these updates are long overdue and have now become urgent. Canada’s privacy framework, PIPEDA (2000), is a generation old and predates social media and cloud computing. We need coherent rules for responsible AI and interoperable digital health systems.
While the EU advances under GDPR and the U.S. expands frameworks under the 21st Century Cures Act, Canada risks lagging behind. Competitiveness, data sovereignty, and trust now depend on modern rules at the intersection of AI, health, and privacy.
As Trevor Jamieson and I argued in our earlier C.D. Howe Institute paper, “A National Digital Health Architecture Is Long Overdue,” stronger federal coordination and clear standards are essential for safe, interoperable adoption. The Task Force will now need to deliver those structural reforms through an AI and digital-sovereignty lens.
The commission will almost certainly be urged to recommend five priorities:
•Patient data rights, comparable to GDPR and the Cures Act.
•Mandated interoperability and antiblocking standards akin to Bill C-72.
•Harmonized, enforceable privacy protections across provinces.
•Secure digital sovereignty, ensuring Canadians’ data remains under Canadian legal control.
•An end to fax-based communication by mandating digital exchange.
That’s the easy part, thanks to years of groundwork by clinicians, health IT professionals, and officials. The system is ready. Now Parliament must be.
The hard questions: The difficult work lies in adapting to new market realities shaped by digital sovereignty and AI nationalism. Borders are hardening due to new concerns about trade and national security
that may create opportunities for national economic development and the creation of non-tariff barriers that could encourage national innovators. Some questions:
•Will Canada allow healthcare data to be stored abroad and outside the reach of Canadian courts? If not, who will host it here, and at what cost?
•U.S. vendors Epic, Oracle, and MEDITECH dominate inpatient EMRs. Will that continue under stricter sovereignty rules?
•Will AI clinical decision support and AI scribe tools be bundled with these platforms and trained on U.S. data? If Canadian training data are used, will they remain resident in Canada?
•Can we ring-fence legacy EMRs as systems of record while building modern AI layers nationally?
•Both Oracle and Epic have shown an ability to open windows or APIs to U.S. scribes (for example, Abridge) and clinical decision support integrations (announced but not yet implemented). Can Canadian companies plug into this modular design?
•Will provinces finally agree to federalprovincial health data sharing? Quebec and Alberta have resisted pan-Canadian frameworks for decades. If stalemate con-
Young
tinues, should Ottawa proceed with a “Rest of Canada” strategy?
•Should health data, like defense, banking, or currency, be recognized as a national responsibility rather than a provincial asset? The fact that an industry is delivered provincially does not mean its data must be housed provincially.

• Cohere has announced its broad agentic AI platform North (as in “we the…”) and TELUS opened Canada’s first “fully sovereign” AI factory. What role will new nationalistic offerings play in healthcare?
•Are we prepared to produce and host Canadian training datasets for AI? Today, innovators often rely on imported data because domestic sources are scarce and fragmented.
•Where we rely on U.S. or global datasets, how will we ensure that they do not reproduce poor past practices from those jurisdictions? How will we update them to reflect Canada’s population?
Looking forward to November: Answers will come. The foundation remains AIDA, CC4C, and AI4H – an AI-positive framework that embraces Canadian diversity while guaranteeing strong individual data rights and enforced interoperability. These are not universally popular principles. Some fear surveillance and oppose electronic data rights. Others seek to monopolize data and resist portability. Still others distrust private-sector participation in health innovation. We need clear decisions to unlock our strong AI and healthcare capabilities.
As Solomon said when announcing the Task Force, this is an exercise in nationbuilding. Healthcare is one of our largest and most important industries – it deserves a modern national AI infrastructure. It’s time to move beyond the pre-AI debates on digital health and build a cohesive, sovereign, and interoperable AI strategy for the health of Canadians. I am looking forward to Solomon’s decisions.
Will Falk is a retired management consulting partner who spends his time with start-ups and as a public policy fellow at four institutions. He is a contributing editor at Canadian Healthcare Technology magazine.
Canadians are transforming healthcare with tech
BY PATRICK CALLAN
Two young Canadian innovators are using technology and their personal experiences to address health equity challenges. By improving health literacy and developing holistic cancer support systems, Tami Vasanthakumaran and Chengetai Nyamande are demonstrating how digital solutions can meaningfully connect with Canadians and improve their health in innovative ways.
Through the Eureka Fellowship for Youth Changemakers in Canada – a joint initiative of AstraZeneca Canada and Plan International Canada that supports young sustainability leaders who are helping create a healthier, more equitable future – Tami and Chengetai will receive mentorship, funding, and resources to expand their tech-enabled healthcare solutions.
From personal moments to Meducine: For Tami, her innovation journey included three formative moments: a tsunami, a bus ride, and a pen. As a child, the Markham, Ont. native raised funds to support victims of the 2004 Indian Ocean tsunami. During her medical training in India, she treated an elderly man who had traveled all day by bus, only to learn that his cancer was too advanced for treatment. Years later, in Toronto, when a patient borrowed her pen, the woman spoke to Tami in Tamil about the medical doubts she had been unable to voice to her doctor because of a language barrier.
“Those moments showed me that positive health outcomes are shaped not just by doctors or hospitals,” she says. “They depend on whether people under-
stand, feel included, and have the tools to take charge of their health. That realization led to the creation of Meducine.”
Meducine is an interactive, mobile app that delivers accessible health information across cultures and education levels, offering content in more than 150 languages. Supported by more than 100 medical professionals from 35 countries, the AI-driven platform features adjustable learning levels, gamified progress tracking, and peer forums. It also connects users with trusted organizations

and local support groups, ensuring that education translates directly into action.
A survivor’s vision for cancer care: While Tami is using technology for education, Chengetai is using it to support patients navigating cancer. Her own journey began in Zimbabwe, where she was diagnosed with nasopharyngeal carcinoma at age 16. With limited treatment options locally, her family traveled to South Africa to access medical care. After immigrating to Canada, she faced a second diagnosis in 2024, spindle cell squamous cell carcinoma, which led to multiple surgeries – including a 10-hour procedure – followed by months of recovery
and ongoing, life-altering side effects.
“Through my own experience, I learned that cancer impacts far more than just the body,” says Chengetai, now based in Hamilton, Ont. “It affects finances, mental health, and the wellbeing of the whole family. It takes a toll on loved ones as much as it does on the individual. I founded Rise Above Cancer so no one has to face cancer alone.”
Scaling impact through the Eureka Fellowship: Tami and Chengetai are two of 10 young Canadian leaders selected for the 2025-26 Eureka Fellowship for Youth Changemakers in Canada. The 18-month program provides leadership training, mentorship, $10,000 in funding to advance their sustainability initiatives, and participation in an in-person summit to support each Fellow’s growth and development.
“We are incredibly proud to support the next generation of youth changemakers through the Eureka Fellowship,” says Gaby Bourbara, president of AstraZeneca Canada. “Leaders like Tami and Chengetai are demonstrating the impact young people can have on improving health equity by using technology to connect, educate, and support communities.”
The Eureka Fellowship also highlights the diversity of solutions young Canadian leaders are developing.
“We are proud to support youth who are harnessing digital tools to drive meaningful change,” adds Lindsay Glassco, president and CEO of Plan International Canada.
To learn more, visit https://www.astrazeneca.ca/en/sustainability/eureka-fellowship.html
Tami Vasanthakumaran
Will Falk
Closing the AI gap in continuing care: Why the time to act is now
BY STEVE KOVACIC
In a healthcare landscape increasingly shaped by artificial intelligence (AI), continuing care is being left behind. While acute care benefits from over $81 billion in annual investments and rapid AI adoption, continuing care remains underfunded, underdigitized, and largely absent from national health data systems. Even basic metrics, such as national spending on continuing care, are hard to track. This invisibility has real consequences.
As Canada’s population ages and demand for seniors care grows, AI must become a strategic priority in continuing care, not an afterthought. The technology holds immense promise: enhancing safety, improving efficiency, and easing workforce pressures. But its adoption must be thoughtful, ethical, and aligned with sector values.
AI implementation is a team sport, not just an IT conversation. As a certified futurist specializing in AI, I’ve seen how AI reflects the data it’s trained on, data often shaped by those with better digital access. This risks reinforcing existing inequities and excluding marginalized voices. One Canadian example is highlighted in The State of FemTech in Canada, which found that a lack of diverse data has led to gender-biased tools in women’s health technologies. These blind spots must be recognized before deploying AI in sensitive environments like continuing care.
Despite the risks, the opportunities are significant. Clinically, AI can support fall prediction, early detection of health issues, and personalized care planning. For example, AI-powered systems can monitor resi-
dent gait patterns and flag subtle changes that may indicate increased fall risk, allowing caregivers to intervene earlier and improve quality of life. Administratively, AI can streamline scheduling, documentation, and reporting, freeing staff to focus on direct care.
Yet most continuing care environments are not currently equipped, culturally, technically, or operationally, to take full advantage of these tools. And this is not just a lack-of-AI problem. It’s a lack-of-infrastructure problem. Many facilities lack reliable Wi-Fi, integrated electronic medical records (EMRs), or the secure digital ecosystems that AI tools require. Before AI can scale, this foundational groundwork must be laid.
To move forward, sector leaders must prepare the landscape. Here are five essential principles to guide responsible AI adoption in continuing care:
• Leadership accountability and strategic readiness: Boards and executives must lead AI adoption with clarity and intent. Inaction is no longer neutral, delays risk deepening the sector’s marginalization.
AI should be treated as a strategic enabler: embedded in plans, guided by ethical governance, and aligned with care values. Leaders must ask: What are the risks of standing still? Are we preparing responsibly?
A clear roadmap is essential. Without it, AI efforts become fragmented and reactive. A strategic plan aligns priorities, identifies gaps, and sets timelines, ensuring AI is integrated, not improvised. No roadmap, no results.
Productivity gains from AI must be reinvested with purpose, supporting resident engagement, staff development, and
innovation. At the same time, organizations must bolster cybersecurity to counter AI-driven threats.
• Education and digital literacy: AI should be viewed as a decision-support tool, not a definitive source of truth. As one educator put it, “AI is like a naïve intern”: insightful, but lacking context and empathy.
Staff need more than system training. They need critical digital literacy to evaluate AI outputs thoughtfully: Where did this recommendation come from? Does it align with our values? What’s missing?

Education must build a culture of informed skepticism. As AI becomes more integrated into workflows, it’s the “thinking” skills, not just the “doing” skills, that will shape a future-ready workforce.
• Privacy and consent: AI tools must be implemented with robust privacy protections. The use of consumer-grade platforms, such as ChatGPT, introduces risks, these systems may store inputs or lack sufficient controls.
To mitigate this, organizations must prioritize enterprise-grade AI solutions with strong safeguards: encryption, audit trails, and transparent consent protocols. Even anonymized data, if mishandled, can violate privacy laws and ethical norms.
Privacy isn’t just a technical issue, it’s a moral imperative rooted in dignity and trust. That’s why digital literacy must include clear “do’s and don’ts” for AI use in healthcare.
• Bias and inclusion: AI mirrors the data it learns from. Without input from continuing care and marginalized communities, AI systems risk perpetuating harmful biases, in hiring, care planning, and resident engagement. While most providers can’t control how commercial models are trained, they can control how they’re used. Operators must recognize AI’s limitations and ensure decision-making includes human judgment, especially where equity is essential. Raising awareness of AI’s blind spots and fostering diverse input in procurement, testing, and evaluation are key to maintaining fairness and trust.
• Emotional intelligence and human connection: Concerns that AI will replace caregivers are understandable but misplaced. No algorithm can replicate human empathy, presence, or cultural awareness. AI will offload repetitive tasks, allowing staff to do what they do best: connect with, and care for residents. As roles evolve, emotional intelligence, compassion, and moral reasoning will grow in value.
Operators should invest in human-centered skills. Staff need the capacity to recognize when AI-generated outputs lack nuance, context, or relevance to a resident’s lived experience. In this way, AI won’t diminish humanity, it will amplify its importance.
A national call to action: Continuing care must not be left out of Canada’s digital transformation. Its invisibility in national health data systems reflects longstanding neglect. That must change.
Steve Kovacic is a Futurist, Vice President and Chief Innovation Officer with the Good Samaritan Society, Edmonton.
SE Health strives to deploy AI effectively through collaborative framework
BY ANOOSHA MUSSADDEQ AND KIRA MATSKOFSKI
Innovation does not happen in isolation”, says Farah Ismail, seniorvice president and chief legal, privacy, and compliance officer at SE Health, a non-profit social enterprise with a Legal, Privacy and Compliance department that is devoted to helping good people do good things.
Earlier this year, SE Health joined the leagues of technological innovation by launching its first cross-functional approach to the integration of AI.
While AI is often leveraged to accomplish specific goals within a tailored sphere, SE Health has been working dynamically to integrate AI-based technology ethically across the organization. With a holistic focus on improving the delivery of healthcare by streamlining operations, SE Health is integrating AI in a new way that protects the sensitivity of Personal Health Information (PHI) while building towards a smarter, more intentional future for Canadian healthcare.
As Farah Ismail explains, “At SE Health, we see AI as the driver for bridging the gap between provider efficiency
and patient experience.” This sentiment reflects SE Health’s approach to integrating AI as a cross-functional tool to accomplish the organizational mission of bringing hope and happiness to the populations we serve.
SE Health has expanded its AI-powered Co-Pilot initiative across departments, enhancing efficiency while maintaining secure, ethical standards. Now fully deployed, the project supports rapid improvements through intelligent tools like automated meeting transcription and AI-assisted candidate screening in HR. Additionally, upgrades to Contract Lifecycle Management systems are streamlining compliance, boosting collaboration, and reducing costs – marking a significant step toward smarter, more agile healthcare operations.
SE Health is proactively exploring how AI can support its mission to transform care, encourage positive health outcomes, and address the needs of changing demographics. Its Clinical AI Workstream is tasked with identifying the ways in which AI-driven tools can support care providers and patients by streamlining documentation efforts, improving wound assessments, guiding care plans,
and supporting clinical coaching. This approach to AI in human services is rooted in person-centered design – engaging both staff and clients to ensure technology serves real needs. While this workstream is in early testing using simulated patients, the team is committed to amplifying client voices in future development. By promoting critical thinking, creativity, and equitable out-
“At SE Health, we see AI as the driver for bridging the gap between provider efficiency and patient experience.”
comes, SE Health aims to raise the standard of care and stay true to its mission.
SE Health is leading with intention –transforming its guardrails to proactively address known risks such as bias, privacy violations, consent challenges, and data inaccuracies. At the core of this effort is a unique, cross-disciplinary partnership that brings together SE Health’s Innovation, Legal, Privacy, Compliance, and Digital, IT teams.
This collaborative framework ensures
that every new AI system is adopted with rigorous oversight and ethical clarity. While the Innovation team drives forward-thinking solutions, the Legal, Privacy, and Compliance teams ensure alignment with Canadian privacy laws and regulatory standards. The Digital, IT team focuses on implementing robust security and operational controls to safeguard sensitive data.
Together, these teams conduct comprehensive Privacy Impact Assessments and Threat and Risk Assessments – critical checkpoints that evaluate what data is collected, how it will be used, and what risks may emerge. This process serves as SE Health’s internal compass, guiding the transition from conceptual innovation to responsible deployment.
What sets SE Health apart is its commitment to technological responsibility, a principle informs every decision, ensuring that innovation is not only effective but also ethical, inclusive, and human-centered. By embedding accountability into every layer of its innovation strategy, SE Health is shaping a future where AI enhances care without compromising trust.
SE Health employees have been provided with training. Additionally, employ-
Steve Kovacic
Digital Health Canada
stakeholders at the regional and provincial level to address and develop models for successful governance in sharing information broadly; an e-poster that highlights an ongoing research investigation on information sharing in health sector; and a bibliography of publicly available documents for those with an appetite to continue reading on this subject area.
Each of these publications has been developed by members drawing on their lived experience in healthcare organizations, technology firms, and policy settings. They reflect not abstract theory, but the actual challenges and opportunities faced by anyone interacting with Canada’s health system.
A living library: The resource library is not static. It evolves as new issues emerge, ensuring members and stakeholders have access to current, relevant, and actionable insights. Topics span cybersecurity, privacy, interoperability, patient experience, workforce development, and leadership.
More than a catalogue, the Digital Health Canada Resource Library represents the collective efforts of hundreds of professionals who believe that sharing knowledge accelerates progress. By pooling insights, members reduce duplication of effort, shorten learning curves, and raise the baseline of expertise across the digital health sector.
CHIEF Executive Forum Resources –Leadership today and tomorrow: That tradition of knowledge sharing is alive and well in Digital Health Canada members today, particularly those engaged with the CHIEF Executive Forum (CHIEF). CHIEF brings together senior leaders from healthcare delivery, policy, and industry who understand that progress depends on collective insight. Two recent CHIEF resources illustrate how this model continues to pro-
ees are invited to complete surveys, share their concerns, and offer feedback to ensure that the deployment of AI is responsive to the needs of both care teams and patients. The data collected from these validated measure tools are then integrated within the AI product. “Our goal from the start has been to listen as much as we lead,” says Ismail, reflecting on the importance of employee involvement and course correction in developing and shaping the future of AI at SE Health.
With patient care being a top priority of SE Health, employee education remains a core tenet of this technological mission. The organization has leveraged existing tools such as an internal education series that keeps all members of the staff informed about evolving AI-related guardrails, data protection standards, and required practices.
These guardrails explicitly outline the use only of authorized AI tools, pathways to seek approval for new AI tools through the maintained AI Governance Council, and expectation of professional responsibility.
SE Health encourages participants to remember that there is no tool that can replace the human element of good work. While AI may aid in the completion of tasks, the individual is paramount to the final product.
duce forward-looking, practical guidance.
•Setting the Winning Conditions for AIpowered Healthcare in Canada. This member-driven report explores what it takes to responsibly scale AI in Canadian healthcare. Drawing directly from innovators already using AI, it distills lessons into practical insights for leaders charting their own AI journeys. From governance and ethics to integration and impact measurement, the resource offers a roadmap for creating the right conditions for AI to thrive in patient-centred, evidence-based ways. It reminds us that technology alone is not enough – leadership, policy alignment, and careful implementation are equally essential.
•AI in Action: Transforming Clinical Care across Canada. Building on Setting the Winning Conditions, the AI in Action Working Group recently completed Stage 1 of its mandate: Canada’s first environmental scan of artificial intelligence–driven clinical initiatives. This scan identified 152 initiatives across the country, with Ontario, Quebec, and British Columbia leading activity. It revealed that hospitals and acute care dominate adoption, while primary care, long-term care, and Indige-
nous/remote settings remain underrepresented. Most projects are still in pilot stage, underscoring the need for workflow integration, equity in adoption, and stronger evidence of outcomes.
Beyond the numbers, the scan is significant because it creates a baseline for monitoring Canada’s AI journey. It highlights where innovation is happening, where opportunities exist, and where gaps remain.
Primary care teams should be connected with community and social services, working together to support patients.
Just as importantly, it is designed as a living resource – inviting healthcare providers and organizations to contribute updates so the dataset remains timely and relevant.
Together, these two recent resources demonstrate how Digital Health Canada continues to evolve with the times. Just as earlier toolkits helped members tackle cybersecurity or interoperability, today’s CHIEF outputs provide practical guidance
for navigating the complexities of artificial intelligence.
Looking back, looking ahead: As we celebrate 50 years of Digital Health Canada, it is worth pausing to reflect on the body of work produced by our members and what makes it unique. Not the number of reports published, but the enduring process: professionals coming together voluntarily to share their expertise, challenge each other’s ideas, and co-create resources that potentially lead to better healthcare for all. This spirit of collaboration among our members is what makes the association stay relevant through decades of technological and policy changes.
It’s never been just about knowledge. It’s about trust. When a CIO downloads a cybersecurity toolkit, or when a clinician references an interoperability framework, they know it reflects the lived experience of peers across the country. That credibility is what makes the Digital Health Canada Resource Library an asset to Canada’s digital health ecosystem.
Shelagh Maloney is CEO of Digital Health Canada.
AI analyzes headaches, and new methods relieve them
CONTINUED FROM PAGE 10
showed significant improvement after just one month of treatment, suggesting that the intensive three-month protocol might be unnecessarily long. Even more remarkably, when the treatment duration was shortened, headaches did not return, indicating that the brain’s recalibration could be achieved more efficiently than initially thought.
As the research program continued to evolve, the team made increasingly sophisticated discoveries about the nature of
Employees have been provided with published articles exploring AI applications in healthcare to foster an environment of learning. SE Health is committed to maintaining an integrated model that allows for real-time policy articulation and risk mitigation education that supports participation without compromising trust. “It’s not enough to just say we are being careful. We have put real structures in place to ensure that AI is used safely and ethically through education and understanding” said Ismail.
“We at SE deem AI as a catalyst for the strategic growth of healthcare’s capabilities, not only from a clinical perspective, but as part of a broader digital transformation,” said Ismail.
SE Health continues to focus on its evolution of intentional AI technologies and encourages its members to leverage the permission process to become dynamic users. The cross-functional approach has ensured that this work is not siloed but deeply aligned with the overall organizational mission to continue to deliver care to patients in efficient and dynamic ways while improving operational efficiencies.
Anoosha Mussaddeq is Associate Legal Counsel at SE Health. Kira Matskofski is a Paralegal at SE Health.
chronic headaches themselves. Through careful analysis of patient responses and outcomes, they identified five distinct types of chronic headaches, each with its own underlying biochemical signature.
This breakthrough led to the development of specific supplement combinations tailored to each headache type, allowing for truly personalized treatment protocols. The refinement process also revealed that treatment duration could be optimized even further, with some protocols proving effective in as little as two weeks, while others required longer periods depending on the specific headache type and individual patient factors.
Clinical results and validation: The treatment’s effectiveness has been demonstrated across multiple patient groups:
•3,000+ patients have completed the various protocols by the end of 2022
•100 percent success rate reported for headache elimination
•No ongoing medication required after treatment completion
•Long-term durability with no reported recurrence over years of follow-up
FDA approval and safety: The supplement-based treatment has received FDA approval, indicating it meets safety and efficacy standards for patient use. The specific formulations and exact supplement combinations remain proprietary to Idan Health, developed through their AI-driven research and clinical validation process.
Understanding the five headache types: Idan Health’s research identified five distinct categories of chronic headaches, each requiring tailored supplement protocols:
1. Chemical Imbalance Type: Headaches caused by specific nutrient deficiencies
2. Inflammatory Response Type: Related to chronic inflammatory processes
3. Hormonal Fluctuation Type: Connected to hormonal imbalances
4. Vascular Pattern Type: Associated with blood flow irregularities
5. Neurochemical Type: Linked to neurotransmitter imbalances
Each type requires a specific combina-
tion of supplements and treatment duration, ranging from two weeks to several months depending on the underlying pattern. The precise formulations for each headache type have been developed through Idan Health’s proprietary research process and remain confidential to ensure treatment efficacy and safety.
Rather than masking symptoms, this approach addresses the fundamental chemical imbalances that create headache conditions. By correcting these imbalances, the treatment eliminates the source of pain rather than just managing its effects.
The treatment essentially “teaches” the brain to maintain optimal chemical balance independently. Once this new balance is established and reinforced through the
The treatment essentially teaches the brain to maintain optimal chemical balance independently.
supplementation period, the brain continues to maintain it naturally, eliminating the need for ongoing treatment.
By identifying specific headache types and tailoring treatment accordingly, the protocol represents a personalized medicine approach that addresses individual biochemical patterns rather than applying one-size-fits-all solutions.
For chronic headache sufferers, this treatment represents more than pain relief – it offers complete liberation from a condition that may have controlled their lives for years or decades.
Patients report:
•Complete elimination of chronic headaches
•Ability to function normally without pain management strategies
•Freedom from medication dependency
Keren Golan is the founder and CEO of Idan Health. The international company has an office in Toronto. www.idan.health



Medtronic CarePathIQ™
Healthcare delivery, reimagined.






































Patient and Care Teamcentric solutions



































consulting designed to help make healthcare work better.





































