

INSIDE:
Palliative care
Hospital and community palliative care providers have teamed up to connect information through Epic, improving the delivery of palliative care in the region.
Page 6
Addiction assessments
HiBoop, a new platform for addiction treatment assessment, has shown great success, moving beyond tracking only relapse rates to more comprehensive outcome measurement.
Page 8
Agentic AI
The next few years will undoubtedly be dominated by AI agents, or “agentic AI”. These impartial collections of code are capable of exhibiting empathy and kindness to patients. They offer tireless support and never take sick days.
Page 12

UHN spinoff HALO monitors patients Canada-wide
HALO Tele-Monitoring, a remote patient observation company that was spawned at the University Health Network, in Toronto, has grown to serve 24 hospitals and six long-term care facilities across Canada. The organization is committed to expanding further; with many healthcare sites hard-pressed to find staff to monitor at-risk patients, HALO is proving to be a useful and cost-effective solution SEE STORY ON PAGE 4.
Virtual medical services are keeping many EDs open
BY NORM TOLLINSKY
growing number of rural and remote hospitals across Canada are using virtual ER physician services to cope with physician shortages and avoid ER closures, but not everyone is sold on the idea, fearing it normalizes rural inequity.
That’s not the case in Newfoundland and Labrador, where the provincial health authority contracts with Teladoc Health Canada to help staff 11 rural and remote ERs.
Newfoundland and Labrador Health Services began considering the use of virtual ER services in 2022, said Joanne Pelley, vicepresident and provincial chief nursing officer. “We were at the tail end of the global pandemic, and a number of our rural and
For many rural and remote communities, virtual ED services have provided a lifeline.
remote ER departments were experiencing staffing shortages that led to closures for hours or even days. The decision at the time was that we would look at virtual ER care as a complement to our current service delivery model to help support access across communities and more stability for our sites. We’ve had great success with virtual ER service, and our closures have gone almost to zero.”
Teladoc Health Canada is a subsidiary of New York City-based Teladoc Health, a global leader in telemedicine services.
Founded in 2002, the U.S.-based company operates in more that 130 countries. In Canada, it operates virtual ER services in 14 hospitals, including sites in New Brunswick and British Columbia.
A Canadian competitor, Maple, provides virtual ER services in 12 rural hospitals in Prince Edward Island, Nova Scotia and New Brunswick. Elsewhere across the country, Alberta Health Services is operating a virtual ER pilot in four rural and remote communities and even in Toronto, a growing number of hospitals, including University Health Network, Sunnybrook Hospital and Michael Garron Hospital, offer virtual emergency services. Virtual ER services can either supplement care to reduce wait times in hospitals with in-
Virtual medical services are keeping many rural and remote EDs open
sufficient in-person ER physicians or provide care in rural and remote hospitals that would otherwise be forced to close when local physicians and locums are unavailable.
Teladoc began providing virtual ER service in Canada in 2023 and claims to have prevented more than 30,000 hours of emergency department closures in the communities it serves.
“Doctors are able to examine and treat patients working collaboratively with inperson nurses,” said Joby McKenzie, managing director, Teladoc Health Canada. “The nurse triages the patient and the doctor – through our technology – has eyes and ears on the patient as if they were there in person.”
The doctor controls the high-definition camera and can zoom in as required. Teladoc also supplies stethoscopes and otoscopes that allow the doctor to remotely listen to the patient’s breathing and examine their ears.
“All of our physicians are emergency medicine doctors located in Canada and licenced in the province where they’re prac-
tising,” said McKenzie, who claims that more than 97 percent of patients have their issue resolved as a result of the virtual ER encounter and that more than 95 percent of patients are satisfied with the service.
“That leaves approximately 3 percent of cases requiring transport to a better equipped hospital for emergency care.
Maple began offering a six-month virtual ER pilot program at Western Hospital in Alberton, PEI in 2018. That program, said Amii Stephenson, Maple’s vice-president of sales, is still in operation.
In 2022, the company contracted with Nova Scotia Health on a virtual ER pilot at the Colchester East Hants Health Centre in Truro, and that too has since been expanded to other communities.
“The goal,” she said, “is to strengthen clinical capacity, reduce patient transfers and preserve access to care in rural communities.”
Maple uses a network ER specialists and family doctors with emergency medicine experience, who connect with patients over the Internet using two-way audio and video communication technology, including stethoscopes and otoscopes.
“The vast majority of encounters in our
Coming up in CHT
Issue DateFeature ReportFocus Report
Nov/Dec AI/AnalyticsCardiology
February 2026 Medical ImagingSurgical Technologies
March 2026 Hospital at HomeInteroperability
April 2026 Mobile SolutionsArtificial Intelligence
May 2026 EHR/EMR TrendsPrecision Medicine
For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
www.canhealth.com

virtual ER programs are managed onsite,” said Stephenson. In higher acuity situations, virtual ER docs stabilize patients with the assistance of in-person nurses and paramedics, and coordinate transportation as required.
Depending on how an individual program is structured, ER docs will often follow-up with patients after an encounter in the ER.
“If a patient leaves the hospital and

MAGAZINE FOR MANAGERS AND USERS OF INFORMATION TECHNOLOGY IN HEALTHCARE Volume 30, Number 7 October 2025
Address all correspondence to Canadian Healthcare Technology, P.O. Box 907, 183 Promenade Circle, Thornhill ON L4J 8G7 Canada. Telephone: (905) 709-2330. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2025. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others: $67.80 per year ($60 + $7.80 HST). Registration number 899059430 RT. ©2025 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited. Send all requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, P.O. Box 907, 183 Promenade Circle, Thornhill ON L4J 8G7. E-mail: jerryz@canhealth.com. ISSN 1486-7133
Publisher & Editor
Jerry Zeidenberg jerryz@canhealth.com
Office Manager
Neil Zeidenberg neilz@canhealth.com
there are still outstanding results, we absolutely follow-up,” said McKenzie. “Because we operate virtually, we don’t have the same constraints of a physical environment, so our patients are often pleasantly surprised when they hear from us at home beyond just the hours you would expect.”
Virtual ER care provides an important service for patients in rural and remote communities who might otherwise have to drive long distances to larger hospitals when their local ER is closed.
“As a parent, you may not know if your child has an acute medical condition, so when you drive up to the door of your local hospital, you need it to be open,” said McKenzie. “These emergency departments are a lifeline for the 20 percent of Canadians living in rural and remote communities.”
She added, “They pay taxes like the rest of us and deserve to have their healthcare needs supported.”
At the same time, she asserted, it’s also important that we do it in a way that’s fiscally responsible, noting that virtual ER docs can cover multiple ERs, especially during overnight shifts when volumes are low. In addition to providing an important service for patients, virtual ER services provide lifestyle balance for overworked family doctors in rural and remote communities who are usually responsible for ER coverage.
“Virtual ER services give family doctors in these communities more control over how and when they work,” said Stephenson. “It’s essential for their well-being and retention.”
In one community Teladoc serves, a local physician was able to spend her first Christmas with her family in over five years, said McKenzie. “That means she’ll be able to stay in the community because the full burden of providing healthcare doesn’t sit on her shoulders.”
The North Shore Health Network, which serves Blind River, Thessalon and
Contributing Editors Dianne Daniel dianne.l.daniel@gmail.com Will Falk will@wfalk.ca
Dr. Sunny Malhotra Twitter: @drsunnymalhotra Norm Tollinsky tollinskyn@gmail.com
Art Director
Walter Caniparoli art@canhealth.com
Digital Media Specialist
Rebecca Downer rebecca@canhealth.com
Remote physicians can
high-definition cameras and medical devices to examine patients at a distance.






















INTRODUCING THE VOLARA SYSTEM

HELP MORE PATIENTS BREATHE EASIER 1
The Volara System promotes accurate, consistent therapy in acute and chronic care settings, and uses Oscillation and Lung Expansion (OLE) technology which has shown improvement in clinical outcomes.1-7



– 3-in-1 therapy: Combines Continuous Positive Expiratory Pressure (CPEP), Continuous High Frequency Oscillation (CHFO) and Nebulizer
– By combining three therapies into one treatment using the Volara System, therapy times can be reduced down to 10 minutes1


– Wide therapeutic pressure range: Allows you to treat a broad range of patients
– Programmable therapy presets: Facilitates standardization of therapy across patient groups
Contact your Baxter representative to learn more at 1-800-267-2337.
References
1. Data on File at Baxter International Inc.


For the safe and proper use of the devices referenced within, refer to intended use, warnings, precautions, and complete instructions for use or the appropriate manual.
2. Huynh TT, Liesching TN, Cereda M, Lei Y, Frazer MJ, Nahouraii MR, Diette GB, Efficacy of Oscillation and Lung Expansion in Reducing Postoperative Pulmonary Complication, JACS (2019).


3. Chasteen,B. C. Becker, M. Wanjala; Respiratory Care, Oscillation Lung Expansion Therapy (OLE) with The MetaNeb System Is Associated with Decreased Hospitalizations for Acute Reactive Airway Disease Exacerbations Compared to Standard Small Volume Nebulizers. OU Health, Oklahoma City, OK, United States, Medical Affairs, Hillrom Inc., Saint Paul, MN, United States.
4. B. C. Becker, K. Piston, Medical Affairs, Evaluation Of Work Of Breathing And Health Care Utilization In Patients Prescribed Daily Oscillation And Lung Expansion (OLE) Therapy At Home. Hillrom, St. Paul, MN, United States, Medical Affairs, Hillrom, Skaneateles Falls, NY, United States.
5. Neil Mushlin, Mwanamisi Wanjala, Carlos Urrea, Kimberly Koloms, Brian Becker (2021, October 17-20) Evaluation of Trends in Patient Reported Outcomes Following Initiation of Oscillation and Lung Expansion Therapy with The Volara System (Poster Presentation). Virtual Meeting, American College of Chest Physicians Annual Meeting. DOI: https://doi.org/10.1016/j.chest.2021.07.1670.
Baxter and Volara are trademarks of Baxter International Inc. or its subsidiaries. CA-FLC188-250002



6. Anwar Hassan, Maree Milross, William Lai, Deepa Shetty, Jennifer Alison, Stephen Huang, Feasibility and safety of intrapulmonary percussive ventilation in spontaneously breathing non-ventilated patients in critical care: A retrospective pilot study. 2021, Vol. 22(2) 111–119.
7. Nyland B, Spilman S, Halub M, et al. A preventative respiratory protocol to identify trauma subjects at risk for respiratory compromise on a general in-patient ward. Respiratory Care. 2016;61(12):1580-1587. Baxter.com



Nurse’s insight sparks Canadian patient safety innovation with HALO
TORONTO – What began from a single moment of inspiration in the pre-lung transplant ward at University Health Network (UHN) has blossomed into a nation-wide healthcare innovation. H.A.L.O Tele-Monitoring Inc. (“HALO”), a remote patient observation technology, has grown to serve 24 hospitals and six long-term care facilities across Canada, with the company committed to expanding further within its home country of Canada.
The inception of HALO dates back to 2015 when Marijana Zubrinic, a nurse practitioner at UHN’s Toronto General Hospital, encountered a difficult challenge while caring for an at-risk patient. The patient was exhibiting behaviors that were putting their safety at serious risk.
Traditional interventions weren’t effective and securing a constant care observer was not possible at that moment.
Recognizing the pressing need for a practical solution, Marijana led the development of an audio-visual monitoring device in collaboration with UHN’s Techna engineering team and subsequently piloted its use in patient’s room.
The device streamed a live feed to a central location, enabling trained technicians to monitor the patient around the clock.
This successful experiment marked the foundational step toward creating HALO, a novel approach to remote patient observation that has since grown into a fully operational spin-out company incubated at UHN.
“We call him Patient #1 and he continues to inspire us every single day at HALO,” reflects Marijana, who now serves as HALO’s chief operating officer and chief nursing executive. “From that very first moment, Patient #1 believed in the concept. He said hospitals might argue they can’t afford such technology, but patients will love it, and nurses will recognize its value. He encouraged me to make a

promise – that I wouldn’t stop until every hospital in Canada had access to the solution. It’s a promise I’ve carried with me since 2016, and I haven’t stopped working on HALO telemonitoring since.”
Fast forward to today and HALO is changing the patient observation landscape in Canada. The HALO device, stationed at the patient’s bedside, securely streams a live audio-video feed of a patient to HALO’s observation centre.
There, a trained patient observation technician continuously monitors up to 12 patients at once which enables HALO to offer hospitals a more cost-effective method to observe at-risk patients without compromising quality of care or patient safety.
From its headquarters in downtown Toronto, HALO directly employs 27 patient observation technicians who provide its telemonitoring service on a 24/7/365 basis.
Each technician is trained by practicing clinicians to intervene in real-time to prevent adverse events. This type of proactive support complements on-site care teams and enables them to focus on their core clinical duties.
Nationwide impact and proven value: HALO has been deployed across UHN, including 50 inpatient units, where it has supported more efficient patient monitoring and reduced reliance on costly, temporary staffing solutions. In 2022 alone, UHN reduced its staffing agency spend by $2.5 million by using HALO.
Beyond cost savings, HALO directly addresses workforce challenges by easing the burden on nurses and clinical teams. In units using HALO, staff report greater confidence knowing their patients are under continuous observation by trained technicians.
Do More With One Device
Optimize workflows and empower care teams with a Zebra Mobile Computer.

As it relates to patient safety, at one hospital in Western Canada, HALO contributed to a 75 percent reduction in highrisk patient falls within the first year of use – demonstrating the meaningful impact virtual observation can have on patient outcomes.
HALO continues to scale as hospitals and health systems across Canada seek innovative strategies to support their teams. The platform’s centralized observation model frees up bedside staff to focus on direct, high-value care, advancing key system priorities such as digital transformation, patient safety, and sustainable staffing.
A recent milestone includes HALO’s province-wide rollout across Newfoundland and Labrador, where it now supports 11 hospitals and six long-term care homes.
HALO’s deployment has proven particularly valuable in rural and remote communities, such as those in Newfoundland and Labrador, where staffing geographic and resource challenges can make continuous in person observation more complex. In these settings, HALO complements onsite care teams by enhancing patient safety and enabling more flexible use of existing staff resources.
Designed for the Canadian healthcare system: The mentorship between Dr. Shaf Keshavjee, a world-renowned lung transplant surgeon and chief of innovation at UHN, and Marijana, a nurse practitioner, played a critical role in HALO’s creation.
“Dr. Keshavjee encouraged me to pursue HALO when it was still just an idea and supported its evolution every step of the way,” says Marijana. “That clinician-toclinician mentorship shaped not just the technology – but how we built it, how we validated it, and who we built it for.”
During early development, the HALO team reviewed several U.S.-based technologies for virtual observation. However, they found that most solutions were poorly suited to the Canadian environment – designed for different staffing models, incompatible cost structures, and often reliant on the hospital to hire and manage their own observation staff.
Recognizing this gap, HALO was purpose-built for Canada’s single provincial payor healthcare system.
“HALO was thoughtfully designed by clinicians to be, first and foremost, easy to use. The setup is simple, clinicians using the device require minimal training, and it integrates seamlessly into established clinical workflows and protocols,” said Dr. Keshavjee, co-founder and chief medical officer at HALO.
“At HALO, every decision we make places safety and the patient at the centre of our work. Our unwavering commitment is to deliver exceptional care to the patients we monitor.”
The leadership team at HALO is composed of experienced clinicians and medtech professionals, including Marijana Zubrinic and Dr. Keshavjee, alongside Sumeet Thind (president), Rick Mangat (executive director), and Thomas Wellner (chairman of the board).
HALO operates its state-of-the-art, 24/7/365 remote patient observation centre from the MaRS Discovery District in Toronto.
Dr. Shaf Keshavjee encouraged UHN nurse practitioner Marijana Zubrinic to develop and launch HALO.






























































































































































Meet MAMMOMAT B.brilliant, a whole new mammography system that brings you the next generation of 3D mammography. Experience:
U nique 50° Wide Angle Tomosynthesis

PlatinumTomo


Excellent depth resolution and in-plane resolution
Scanning in under 5 seconds
PlatinumComfort
For both technologists and patients








Scan to learn more or visit: siemens-healthineers.ca/ mammomat-bbrilliant
Baxter’s Volara OLE system improves CF and bronchiectasis patient care
BY NORM TOLLINSKY
Clearing the airways of cystic fibrosis (CF) and bronchiectasis patients struggling to breathe can be a real challenge for clinicians using conventional therapies.
However, the Foothills Medical Centre in Calgary has been delivering dramatic results using Baxter Canada’s Volara Oscillation and Lung Expansion (OLE) system, says Dr. Christina Thornton, an adult respirologist and assistant professor at the University of Calgary’s Cumming School of Medicine.
Bronchiectasis is the third most common airway disease after COPD and asthma, said Dr. Thornton. “In fact, CF, which is much better known, is actually a type of bronchiectasis. Both are characterized by shortness of breath, copious amounts of very thick mucus that is hard to clear and, over time, repeated cycles of infection, causing exacerbations or flareups resulting in more mucus, more coughing and more shortness of breath.”
Traditional treatments include aerobic activity for very mild cases, chest physiotherapy including manual percussion, postural drainage, and the use of a nebulizer to deliver saline or pulmozyne to break down mucus and make it easier to expel.
The Volara system is a relatively new method of treating CF and bronchiectasis patients that provides alternating cycles of continuous positive expiratory pressure (CPEP) and continuous high frequency oscillation (CHFO), along with aerosol delivery of saline or medication via an integrated nebulizer to help maximize treatment effectiveness.
The positive pressure expands and keeps the airways open, while the oscillation, a pneumatic form of chest therapy, loosens and mobilizes secretions.
“Where we have seen really good efficacy is with patients who have really thick, tenacious mucus that we are unable to clear using manual percussion,” said Dr.

Thornton. “These patients tend to be frail and co-morbid without a lot of other options after traditional approaches have failed to clear their mucus.”
Dr. Thornton cites the example of one patient who was receiving extremely high levels of oxygen on a specialized Airvo high-flow system for a week. “We used the Volara and within a few days, we went from needing the maximum oxygen you can give someone to a magnitude of less oxygen.”
While the hospital has no hard data on how the Volara system affects patient length of stay, anecdotal examples indicate speedier discharge of patients in some circumstances, she said.
In the United States, where the Volara system was introduced in 2020, Baxter has data indicating a 1.6-day reduction in hospital length of stay, a two-day reduction in
*Source: Reference from Volara brochure - Huynh TT, Liesching TN, Cereda M, Lei Y, Frazer MJ, Nahouraii MR, et al. Efficacy of Oscillation and Lung Expansion in Reducing Postoperative Pulmonary Complication, JACS (2019).
ICU length of stay and a 68 percent reduction in time on ventilator.*
Foothills Medical Centre received its first Volara system in 2022 and began using it primarily for CF and bronchiectasis patients in worst case scenarios, said Dr. Thornton.
“But because it was working so well, we asked ourselves, ‘Why are we only using it in these extreme cases?’ So now we’re using it on patients with mucus plugging who aren’t necessarily so sick.”
She added, “We’ve also broadened its use for other patients with thick mucus plugging who might benefit from it, including patients with lung cancer and allergic bronchial pulmonary aspergillosis.”
After acquiring two additional units, the hospital started using the Volara system post-op on thoracic patients who are in a lot of pain and therefore unable to tolerate manual percussion.
“Good mucus clearance is important for post-op thoracic patients,” noted Dr. Thornton, “because we don’t want to run into any problems that interfere with their recovery.”
Burn unit patients with skin grafts on
their chest may also benefit from use of the Volara system as they, too, wouldn’t be candidates for manual percussion, she acknowledged.
Another benefit of using the Volara system is that it takes only 10 to 15 minutes to complete a treatment. That compares with 40 to 45 minutes that it would otherwise take to administer manual percussion, promoting more efficient use of hospital resources and faster relief for patients.
The device sits on a stand that can be wheeled from patient to patient and features a digital touchscreen that allows the clinician to change the pressure, time and frequency, and program presets for standardization of therapy across patient groups.
“It’s very user-friendly and patients like it, too, because they can see when the Volara is about to switch from positive pressure to oscillation and to prepare for it,” said Dr. Thornton.
The Volara system was officially introduced to Canada in 2024 but is already well known in Calgary because of its earlier acquisition by the University of Calgary’s Adult CF Clinic and Foothills Medical Centre.
“Everyone in our respiratory division at Foothills Medical Centre uses it and thinks about it when they see patients,” said Dr. Thornton. “Because of the rounds we do at the other three hospitals in Calgary, respirologists there are also aware of it, and many of them have procured the Volara system because they also want their patients to have access to it.”
Baxter is now focused on replicating Calgary’s successful adoption of the Volara system across Canada’s healthcare landscape.
Disclaimer: This interview was sponsored by Baxter Canada; however, the opinions expressed by the healthcare provider are solely her own. This represents one healthcare provider's perspective, and individual outcomes may vary.
Scarborough partnership delivers solution to fragmented palliative care
TORONTO – Scarborough Health Network (SHN) and Scarborough Centre for Healthy Communities (SCHC), along with their partners in Scarborough Palliative Care (SPC), have developed a unique solution to delivering more integrated services for the hundreds of patients across the community who receive palliative care.
By connecting the SPC partners through SHN’s Epic clinical information system for documentation and managing digital health records, the organizations are now able to make more expedited referrals, communicate more collaboratively, and care for and transfer patients between each other more seamlessly.
Sharing one health record helps to avoid preventable Emergency Department visits, support patients to die in their location of preference, and improve the overall patient/family experience. In
fact, this marks the first time in Ontario that a hospital network has fully integrated a community organization into its Epic system to improve the delivery of palliative care.
“This is a great example of how we can use digital solutions to improve patient care and what’s possible in local health system integration,” said Michele James, executive vice president, people and transformation, at SHN. “I am so proud of the collaborative effort put forward by all our partners, which truly benefits our patients and families who need palliative care services in Scarborough.”
Connecting the dots for better patient care: SHN, SCHC, and their partners Yee Hong Peter K. Kwok Hospice, Scarborough Academic Family Health Team, Ontario Health atHome, and Shepherd Village – who are all affiliated with the Scarborough Ontario Health Team (SOHT) – have a long history of
working together to provide palliative care services in the Scarborough area.
This reflects the nature of a palliative diagnosis, which often necessitates the patient moving between different care settings and resources provided by different organizations.
However, because the partners
The network has integrated community organizations into an Epic system for improved palliative care.
worked from different IT systems and processes that did not ‘talk’ to one another, transferring patients between organizations often meant added delays and redundancies in their healthcare journey. For example, patients may have been required to provide all their
information repeated times, which could lead to missed information or inaccuracies.
“As partner organizations, we wanted to be more in sync to better support these transitions, which was the drive behind launching SPC. Our aim was to address the fragmentation of patient records that can disrupt continuity of care and find a new way to offer the best possible healthcare experience,” said Sari Greenwood, director, mental health & addictions, oncology & palliative care. Through SPC, each partner has been connected to SHN’s Epic clinical information system. This allows them to view and work from the same record, no matter what services patients receive.
Going a step further to be the province’s first: In addition to bringing all six organizations together to view records, there was also the opportunity

Canadian Healthcare Technology magazine
Canadian Healthcare Technology offers the country's leading healthcare I.T. publications. And they're free to healthcare providers. Get your complimentary subscriptions now!
Canadian Healthcare Technology breaks the news about important projects, programs and technologies, and provides hospital executives and senior managers with an excellent source of information for improving the delivery of healthcare. It’s sent to over 3,900 readers in print format and to over 7,300 opt-in subscribers of the digital edition.

White Papers
eMessenger newsletter
Canadian Healthcare Technology’s e-Messenger contains breaking news about important deals, installations and developments. Four blasts are sent each month, via e-mail, to over 7,100 senior managers and executives in hospitals, clinics and health regions.
Canadian Healthcare Technology’s White Papers are sent out once a month, via e-mail, to over 5,500 senior managers and executives in Canadian hospitals and health regions. The monthly blast contains summaries and links to White Papers issued by various organizations, providing cutting-edge information about topics of interest to healthcare decision-makers.


For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
Addiction centres successfully implement HiBoop’s assessment platform
BY SHANNON POTTS
Canadian Addiction Treatment Centres (CATC) has successfully implemented HiBoop’s digital assessment platform at three inpatient facilities. Full staff adoption was achieved within weeks rather than the months typically expected for healthcare technology deployments.
The implementation, which began as a pilot program in fall 2024, resulted in nearuniversal assessment completion rates and the CATC’s first comprehensive outcome data spanning six months of treatment programs.
The Victoria-based mental health technology company’s platform provides access to a growing library of over 40 validated assessment scales, enabling CATC to move beyond traditional relapse-rate metrics to comprehensive outcome measurement.
“We’ve moved from measuring success purely through relapse rates to capturing a complete picture of client recovery, including quality of life metrics and overall wellbeing,” said Melanie Matthews, director of clinical programs at CATC. “The platform has given us the ability to demonstrate program effectiveness with concrete data rather than anecdotal evidence.”
CATC, which operates virtual and outpatient clinics across Canada and inpatient treatment facilities in Ontario, has so far introduced HiBoop within its inpatient programs.
Leadership budgeted several weeks for staff training and system implementation. However, the intuitive design enabled immediate adoption by clinical staff. “Our team was using the system productively within days,” said Stacey Ferland, vice president of clinical operations. “In my 25 years in mental health, I’ve never seen technology adoption happen this quickly or this smoothly.”
The platform’s automated scoring eliminates the 15-20 minutes previously required for manual calculation during clinical sessions. Without specialized psychometrists on staff and only two psychologists serving

the entire network, the democratization of assessment tools has proven particularly valuable.
During initial deployment, the platform identified previously undetected mood disorder symptoms in a client undergoing addiction treatment.
The automated screening enabled immediate psychiatric referral, potentially preventing weeks of delayed diagnosis.
“The early detection capabilities have proven invaluable,” Matthews noted. “Having automated flagging of clinical concerns ensures nothing is missed during busy intake periods.”
Previously, when paper was used, fewer than half of clients finished their assessments, with many abandoning them partway or refusing altogether.
Since introducing HiBoop, nearly every client now completes intake, midpoint, and discharge assessments, giving clinicians consistent, reliable data across the entire course of treatment.
An unexpected development emerged in how clients interact with the assessments. Rather than completing forms on their own as anticipated, clients are choosing to work through questions with their addiction
counsellors, transforming administrative tasks into therapeutic opportunities.
“We expected clients would want privacy when completing assessments,” Ferland explained. “Instead, they’re using it as a rapport-building exercise with their counselors.”
The visual progress tracking has particularly resonated with clients. When presented with graphs showing decreasing severity scores over time, clients can see tangible evidence of their improvement. “Change can be so gradual that clients don’t notice it,” Matthews said. “But when they see their scores, they recognize they’re making real progress. It’s deeply motivating.”
HiBoop was founded in 2024 by technology entrepreneur Jason Morehouse following his own mental health diagnosis journey. Morehouse, who previously built Checkfront into a global tourism booking platform processing $1.5 billion in reservations annually, launched HiBoop after spending $80,000 on comprehensive mental health assessments that revealed previously undiagnosed ADHD, complex PTSD, and anxiety disorders.
“Not many people have 80 grand to figure out where their brain is at,” Morehouse
said. “Our ultimate goal is making comprehensive assessment accessible to everyone who needs it.”
Matthews describes the vendor relationship as uniquely collaborative. “Every suggestion we’ve made has been implemented. It’s a true partnership model.” CATC’s input on gambling and shopping addiction assessments is already shaping upcoming features in the product roadmap.
The implementation comes as Canadian mental health providers face increasing pressure to demonstrate treatment efficacy through measurement-based care. CATC’s experience demonstrates that digital platforms can significantly reduce documentation time while improving outcome tracking capabilities.
For addiction treatment specifically, the shift from binary relapse metrics to comprehensive outcome measurement represents a fundamental change in how success is defined and demonstrated. CATC can now provide funders and stakeholders with data showing improvements across multiple dimensions of recovery, not just substance use cessation.
“Technology will play an increasingly important role in mental healthcare delivery,” Ferland said. “The key is ensuring it enhances rather than replaces the human element of care.”
Looking ahead, both organizations see the partnership as a model for digital transformation in mental healthcare. With six months of positive outcome data and 94 percent provider satisfaction rates, CATC plans to expand the platform’s use across additional programs while HiBoop prepares for its broader market launch.
The rapid implementation success challenges common assumptions about healthcare technology adoption timelines, demonstrating that with the right design and partnership approach, digital transformation can happen in weeks rather than months or years.
For more information about CATC, please visit https://canatc.ca. For more information about HiBoop, please visit https://hiboop.com
Scarborough partnership delivers solution to fragmented palliative care
for a full integration between SHN and SCHC within Epic.
SHN’s Rowntree Palliative Care Centre has a particularly close, relationship with SCHC that includes a number of joint initiatives, sharing physicians across both organizations, and providing complementary services that see a lot of the same patients.
This tight connection opened the possibility of exploring uncharted territory – which truly captures SPC’s pioneering vision.
“I’m incredibly proud of my team’s role and the collaborative spirit displayed by all our partners, This initiative is not just about improving patient care today; it’s about creating a blueprint for the fu-
ture of healthcare that other regions and sectors can look to as an example,” remarked Jeanie Argiropoulos, CEO, SCHC.
After the feasibility assessment came months of highly technical programming work by the SHN team, followed by many hours of training by SCHC staff. The result is a first for Ontario – a community partner organization plugged directly into a health network’s Epic clinical information system.
“SCHC is now able to see health records for patients receiving palliative services during a stay in an SHN hospital – and conversely, when a patient arrives to the hospital, the team there has instant access to everything that has happened in the community,” said Dr. Raymond Berry, SHN division head for palliative care. “This means we are pro-
viding coordinated care that removes the problems inherent in having disparate systems that don’t talk to each other.”
A game-changer for patient information sharing: One of the benefits of the new solution is that it allows for better
Hospital professionals and community palliative care workers are able to see each other’s patient records.
data collection and analysis, which can help identify gaps, trends, and opportunities for improvement in palliative care.
For example, the partners can track how long it takes for patients to receive palliative care after a referral, how often
patients are transferred between settings, and more. The partners can then use this data to inform their planning, decision-making, and quality improvement initiatives.
The integration also supports the use of mobile tools, like tablets and smartphones, enabling healthcare providers to bring health records with them to patients who need to receive treatment in their homes. The providers can then make updates right there on-the-spot instead of taking notes that must be transcribed into the system later.
The feedback from these cross-organization care interactions has been very positive, with a clear sense that use over time will open up further enhancements, as SPC and palliative services in Scarborough continue to lead and innovate.
Patients gain control over their health data via the patient summary
BY DAREK SZADKOWSKI
Across Canada, healthcare is undergoing a significant transformation. There is growing recognition that patients should have direct access to their personal health information and the ability to decide how and when it is shared. This shift in mindset is helping to reshape the way care is delivered and experienced.
At Canada Health Infoway, we have been leading the development and adoption of the Pan-Canadian Patient Summary Specification, also known as PS-CA. This specification provides a standardized way to capture and share a patient’s most essential health information.
It is designed to support sharing by either providers or patients, ensuring that Canadians can view and share personal health records when needed.

This vision is already becoming a reality for patients today. In New Brunswick, provincial leaders have partnered with health organizations, vendors, clinicians, and patients to enable access to patient summaries through the MyHealthNB patient portal. This initiative allows individuals to generate their own patient summary based on the PS-CA standard. It includes up-todate information such as medications, immunizations, and recent test results.
Patients can view their summary, download it, and share it with healthcare providers, caregivers, or family members.
Now, instead of repeating their story at every appointment, patients can carry an accurate, up-to-date summary of their health information with them.
Early insights show that patients have avoided duplicate tests and feel better prepared for emergencies, knowing they do not have to worry about missing critical details during a crisis.
Not only does this transform how patients engage with their care, but clinicians benefit from having more complete and reliable data at the point-of-care, leading to faster, more-informed decisions. The broader system also gains from reduced duplication, fewer administrative burdens, and stronger foundations for coordinated, team-based care.
This approach is beginning to show broader promise as patients travel and seek care in different settings. We’ve already heard from clinicians in other regions who have cared for patients presenting with their own summaries, highlighting the value of having that information readily available at the point-of-care.
These real-world examples underscore the benefit of giving individuals the ability to generate and share their own health records when needed. That’s the power of the Patient Summary when able to be generated by patients: it puts trusted, essential information in their hands and supports continuity of care wherever their journey takes them.
The work in New Brunswick demon-
strates what is possible when governments, health organizations, vendors, clinicians and patients come together around a shared goal.
By aligning on the national PS-CA standard and delivering a real-world solution, they have shown that patient-mediated access is not only feasible, but transformative. At Infoway, we are continuing to support the advancement of PS-CA across Canada. Whether implemented through clinician-directed workflows or patient-mediated access, the goal is the same. We want to make health information more accessible, more portable, and more meaningful to those who need it most.
Darek Szadkowski is Vice President, Strategy, Programs, and Partnerships, Canada Health Infoway.


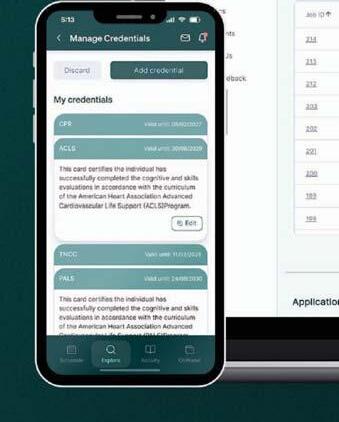
Cut Costs. Hire Smarter.
Healthcare recruitment is broken: expensive, inefficient, and risky.
Oli fixes it with one secure, affordable platform that connects you directly to qualified clinicians and steamlines every step of hiring.





High, Unpredictable Costs
Per-per-click fees, agency placement fees, and enterprise suites drain budgets.
Poor Targeting
Generic platforms flood you with unqualified applicants.
Fragmented Workflow
Juggling job boards, emails, and thirdparty contracts slows everything down


Stop wasting your budget. Start building your dream team.
Scan to see your savings in 60 seconds.

Predictable, Fixed Pricing

Subscription tiers provide budget certainty.
Targeted Healthcare Marketplace
Oli’s AI connects you with qualified professionals
All-in-One Platform
Post jobs, video interview, sync calendars, and manage contracts seamlessly.


Darek Szadkowski
Untangling the taxonomy of AI in clinical decision support (AI CDS)
How to understand the differences in purpose, data and regulation among various solutions.
BY WILL FALK (WITH AI ASSISTANCE)
Clinical decision support (CDS) for both clinicians and patients is changing quickly. This reflects societywide changes on Internet usage but is particularly dramatic in healthcare. The Economist reported recently that global health Internet search volumes are down by 30 percent since June of 2024. AI replaces search for clinicians too.
Most resident physicians now use some type of AI tool instead of either Internet search or the online textbooks that their institutions purchase on their behalf. Med students and attendings are following suit, and AI CDS will be the norm in some form in the next few years for clinicians, as it is for patients.
Hospital administrators and policymakers are faced with a huge shift in usage that they have little control over, despite paying large amounts for formal programs which may or may not survive the shift caused by generative AI. Let’s unpack this.
The label “AI CDS” hides real differences in purpose, data, and regulation among the tools. In this article I attempt to build the language and taxonomy by outlining two dimensions.
I identify four tool types (a 2 × 2) in use today and then three added dimensions that modify these tool types. I suggest using an orchestrator layer to integrate them, which would accommodate new data and agents over time.
Dimension 1: Best practice vs. past practice: Best practice systems rely on published, normative knowledge. Examples: OpenEvidence and Doximity Pathway (formerly Pathway Medical), and specialty “RAG” (retrieval-augmented generative AI) tools like Perlis (bipolar depression) and HandRAG (hand surgery).
They answer: “What does the literature recommend?” These are typically PHI-free and often function as complements, not substitutes, for clinical judgment.
General vs. Specialty (Best Practice):
•General (OpenEvidence, Doximity Pathway): Apply broad, citation-backed materials within guardrails. These systems are being adopted quickly by millions of clinicians as a better alternative to base
Virtual medical services
CONTINUED FROM PAGE 2
Richard’s Landing on the north shore of Lake Huron in Northern Ontario, is a good example of how physician shortages in rural and remote regions of Canada affect ER staffing. Although funded for 16.5 family physicians across the three communities, the North Shore Health Network is short eight family doctors, said president and CEO Tim Vine.
“It’s constant work to keep our ERs open,” he confided in an August interview. “Today, we’re supposed to be closed in Thessalon, but I received a text from a doctor at 7 am this morning to say they’d take the shift. We’ll be closed tomorrow because we haven’t been able to find a locum and we’ll probably be closed on Monday, but we won’t make that call until tomorrow. Currently,
AI platforms (Gemini/ChatGPT) without medical knowledge tuning.
It is worth noting that the base platforms also have millions of users as MDs move from Internet to AI search (“peeking at the Gemini answer” to quote one MD).
They can include services like drug checkers and other tools and can be locally tuned (see deterministic/local tools below). Enterprise adoption will depend on solving problems like data sharing/process agreement availability, PHI handling, and governance of advertising.
•Specialty RAG: Tuned to a domain, disease, or specialty (e.g., Perlis; HandRAG). These enable best-practice personalization by specialty, department, or training program.
Imagine a medical resident coming on service being able to review and RAG into an AI all their supervisors’ past publications and/or a curated list of relevant articles and guidelines. Early days, but you can see the potential.

Dimension 2: Past practice systems answer: “What has worked (here) for this kind of patient?” They rely on large, curated datasets – often EHRbased, but increasingly including images, voice, and device signals.
Specialty repositories (e.g., for cardiac care, oncology, dermatology,) may integrate condition-specific data such as omics, imaging, or sensors. These systems promise to find patterns missed by normative evidence.
They are either based on legacy datasets collected for another purpose or face high costs for cleaning and structuring unstructured data often using new natural language processing tools that are also AIbased.
PHI/PII must be carefully controlled in these models and leakage is of concern. Equity is also of concern because past practice systems reflect past practice!
Our health system’s past does not reflect equity values currently held and does reflect past standard
we have 18 uncovered shifts between all three emergency departments from today and the end of the month.”
Vine hasn’t considered virtual ER service as a possible solution and believes Ontario requires an in-person emergency medicine doctor for an emergency department to be considered open. “It would also be confusing to patients not knowing whether to come here for this, but not for that,” he worries.
In Newfoundland, it doesn’t matter if you’re having a heart attack or a case of the flu in a community served by a virtual ER service. People show up no matter what their concern is.
“We’ve managed heart attacks and multiple traumas successfully,” said Pelley. “Patients would be seen by the on-site care staff – a nurse or an advanced care paramedic. They would then have an assessment with the virtual provider and be stabilized and transported to the nearest hospital able to care for them.”
operating procedures. These values are implicit in the data sets and hard to address.
General vs. Specialty (Past Practice):
•General-purpose data oceans: Promise many-tomany mapping, population queries, and CDS nudges. In the news over the past few weeks have been Epic’s CoMET. CoMET pulls from Epic Cosmos (~300M de-identified patients) to support analytics and queries. Canadian initiatives include GEMINI (35+ hospitals, 2.4M+ admissions, now linked with ICES and expanding to other provinces), plus efforts at Hamilton Health Sciences and BC PHSA.
These projects are important and will change the world, but near-term individual CDS impact may be limited. Population CDS insights and discoveries are a very different use case than bedside or ambulatory care CDS. It’s a shame we can’t find different names for the two types of decision support.
•Specialty systems: Proliferating across conditions; many integrate population features and peer benchmarking. They often require condition-specific data (omics, images, sensors, SDOH, et c.), custom structure, and pre-resolved consent.
These may be advantages over “one big lake.” Fahrner et al. (2025) did a great job of listing dozens of these efforts. Sometimes they use pre-existing repositories of data, images, and disease staging. Prognosis is booming at the specialty level. AutoPrognosis 2.0 (van der Schaar Lab in the UK) provides modular risk modeling tailored to specialties and boasts dozens of projects and webinars on many conditions. Every specialty will have five to 10 of these before consolidation begins. This will be exciting but also a bit dizzying.
Additional dimensions: A neat 2×2 (Best vs. Past × General vs. Specialty) helps start our taxonomy, but there are more dimensions. Unfortunately, these other dimensions orthogonal to the first two; that means that there is messy overlap.
In some they may be end up being dependent upon them – which will mean that the taxonomy won’t break out cleanly. Honestly, I am still unsure and would welcome comment on this. Policymakers and hospital administrators will see that these dimensions may be critical for implementation plans
Here are Three additional dimensions that matter and modify the above:
1. Seek vs. Nudge (aka Pull vs. Push)
•Seek (pull): A licensed professional asks the question; they stay within their scope of practice. This is lower risk for administrators as a result as the clinician is taking responsibility for using and interpreting the tool.
Seek is the migration from Internet search to AI search and will follow many of the same rules. This is clear for best practice systems. For past practice systems, the same way that you can search an intranet instead of globally, you can AI search past practice at your institution as well as best practice.
•Nudge/alert (push): The system recommends or interrupts. Higher complexity and alert-fatigue risk; governance and liability multiply. Because past practice systems are geared to population health currently, they tend to do more nudges – but this may not be the case in the future.
One can imagine a best practice AI “watching” a visit and providing comments. Indeed, such functionality was described back in pre-GenAI era companies (Babylon anyone?). I haven’t seen it yet but a mid-visit SOAP note, scrubbed to remove PHI and
Will Falk
dropped into a normative or empirical CDS, could generate a question list or a “likely differential” percentage.
There appear to be several companies in Ontario working on this functionality either in a scribe or an EMR context.
2. With/Without Deterministic/Local Overlay
SOPs, formularies, local pathways, and insurer rules are rules engines. They are not generative AI, but they shape what models see and can be consumed by them. There are also some excellent history collection and differential systems available (a Canadian one is FirstHx). Global bestpractice tools can be localized; past-practice datasets already reflect these constraints, raising equity/traceability issues.
Deterministic overlays should be explicit, auditable, and separable where possible. Unfortunately, these same rules can end up being implicit in past practice databases. Inequities, bias, dumb insurance rules, and even poor practice can all be hiding in past practice; it will take time to sift through this.
And for some patients the most important data may not be in the health record; (gen)omics, social, environmental data just don’t exist or are buried in free text.
3. Complement vs. Substitute
•Complement: Enhances clinician judgment (textbooks, search, AI copilots).
•Substitute: Replaces judgment for a period (e.g., automated ICU ECG reads). Heavier regulation. Context matters: a specialty tool may complement the subspecialist but act as a substitute for others.
This dimension is almost more of a characteristic or output; the use case and scope of practice determine where a tool lands – and influence regulation/licensing.
This point is key for companies seeking to have their products adopted. A tool that has no PHI and fits cleanly within a clinician’s existing scope of practice will move quickly into production and may fit within existing regulations.
Scribes have shown this. When a tool overrides a clinician, they substitute and become a diagnostic tool; this will be highly regulated. As I have discussed previously, I believe that regulation should be competency-based (rather than drug or device). However we regulate, we need to set clear boundaries for CDS AI as we have for scribes. The use of these systems by patients will, of course happen. That will be a topic for another article!
The Orchestrator Model: By 2030, Internet search will have been replaced by AI and we may not be faced with a choice of only one among these available CDS models.
A “model of models” is likely to emerge in which expert systems are orchestrated with human guidance. This is not science fiction but was described, built and tested by a Microsoft team this summer. Nori et al. (2025) describe MAI-DxO (Model-Agnostic Diagnostic Orchestrator), which coordinates multiple specialized agents and significantly improves diagnostic accuracy on sequential benchmark (NEJM-CPC) cases compared to single models.
A practical clinical metaphor for healthcare leaders might be as follows: imagine a team of (AI) medical residents supervised by a Chief Resident Orchestrator (also an AI). The Orchestrator is not the Attending. That’s your job! The “Chief” aggregates inputs from multiple “Residents” (best-evidence, past-practice, specialty-specific as
well as general, formulary/SOP, etc.), reports disagreements/alternatives, and supports auditability. Teams are modular by specialty (psychiatry, orthopedics) and could be multi-disciplinary as well. For example, we could include:
•SDOH/equity agent to find housing and supports
•Finance/formulary agent to match insurance
•Local SOP/pathway agent (helping to schedule labs and diagnostics)
•Formulary expert to pick up on drug interactions and recommend generic substitutions
•A lawyer (no wait, that’s a bad idea)
We can rotate in residents and other team members based on the type of patient if desired. The accountability sits at the Chief Resident level to report to the At-
tending. Where we have arguments about the recommendation, we can surface the causes of the disagreement.
Will Falk is a retired management consulting partner who spends his time with start-ups and as a public policy fellow at four institutions. He is a contributing editor at Canadian Healthcare Technology magazine.


Accelerating Connected Care at the 2025 Infoway Partnership Conference
Connect with some of the brightest minds in digital health and learn how innovation is driving progress in healthcare.
Nov. 17-18, 2025
AI agents can lighten the burden on swamped healthcare professionals
AI agents are particularly adept at administrative work and they operate tirelessly, 24/7.
BY JENNIFER MACGREGOR
The spotlight in healthcare AI is shifting dramatically. While AI scribes have dominated the narrative for the past few years, touted as the “silver bullet” for the clinical documentation burden and deeply integrated into electronic medical records, a new, more profound trend is emerging: agentic AI.
These scribe technologies, rapidly evolving into commodities regardless of vendor, now compete primarily on price and ease of integration. With low switching costs, more entrants and further price differentiation will undoubtedly occur over the coming years until market consolidation takes hold.
Yet, the broader landscape of administrative burden has already been revolutionized by readily available GPT solutions like ChatGPT, Co-Pilot, Gemini, and Claude. These tools are not only hype; they’re delivering tangible results, with some claiming to reduce administrative time by 6-12 hours weekly.
As a healthcare executive and technology professional, I can personally attest to the reality of these figures; I’ve achieved a 40 percent increase in productivity with these tools and now consider them indispensable.
The next few years will undoubtedly be dominated by AI agents, or “agentic AI,” as the industry has termed them. These impartial agents, capable of exhibiting empathy and kindness, offer tireless support – working without time limits, vacations, or sick days.
Such resources can profoundly impact healthcare by closing care gaps, performing thousands of outreach calls, improving medication compliance, decreasing no-shows, and ultimately enhancing outcomes for both high-risk patients and familiar faces.
Our healthcare systems desperately need this infusion of AI-powered helpers, schedulers, extenders, augmenters, and assistants.
That raises important questions: Can these technologies provide an answer to our human healthcare resource crisis? Can they reduce admissions and alleviate congestion in high-cost care settings? Bolster chronic disease management? Could they even be de-
Our healthcare systems desperately need this infusion of AI-powered helpers, schedulers, extenders, augmenters and assistants.
ployed during emergency responses to mitigate the negative impacts of floods, fires, and extreme heat?
The potential use cases are limitless, and the application of these models could be vast and impactful. The question is no longer “Can they work?” but “Are we ready?”
For me, that readiness came into sharp focus in August 2023. Listening to an AI agent perform an outreach call was a seismic moment, fundamentally shifting my perspective and allaying my skepticism.
For weeks, I was consumed by thoughts of the myriad use cases and wicked problems this technology could address. Obvious questions quickly followed: What would be the engagement and completion rates? Could we integrate additional interaction modalities to boost adoption? How do
we build trust? And the overarching concern: How do we safely deploy these digital experiences?
In healthcare, this necessitates crucial requirements: defining guardrails, safety engines, empathy constructs, cultural intelligence and impartiality to ensure equity in every interaction.
We need clear, warm handoffs, escalation pathways, and robust supervision models – both human and machine – along with understanding how the system would learn and evolve.
Intake AI agents capture patient histories by automating intake, surveys and follow-ups releasing time to care for clinicians. The AI tailors the interactions depending on the patient’s co-morbidities, creating a personalized experience.

Embedded with therapeutic techniques to handle even the toughest conversations and trained on millions of recorded communications, these solutions do not aim to replace irreplaceable humans. Instead, they offer a vital expansion of services, providing interactions and support that are simply beyond our current capacity.
The signs are clear: the future of healthcare support includes empathetic, intelligent agents working alongside us. Elewana Advisory stands ready to empower your efforts in digitally transforming the healthcare experience through Agentic AI. Contact us at ElewanaAdvisory.com to accelerate your transformation.
Creating patient-centered healthcare with digital technologies
BY KASSAUNDRA McKNIGHT-YOUNG
Modern healthcare stands at a pivotal crossroads, where the convergence of technology and human expertise is redefining what’s possible for patients, clinicians, and healthcare organizations. As a nurse leader and informatics specialist, I’ve witnessed firsthand how digital health technologies are opening new doors for care delivery and the entire patient journey from the bedside to the home.
The most profound benefit of digital healthcare technologies is the ability to increase access to care for people who might otherwise be left behind. Virtual care platforms, telehealth, and remote monitoring have emerged as essential tools, especially as our health systems respond to workforce shortages and an aging population with complex needs.
Through remote monitoring devices and connected frontline solutions, clinicians can track vital signs, medication adherence, and recovery in real-time, intervening proactively when issues arise.
This helps keep patients safer and allows them to heal in familiar surroundings, which research shows can reduce anxiety, lower readmission rates, and enhance overall satisfaction.
One of the most significant advances has been the rise of “virtual sitters” and remote nursing mentorships. As experienced nurses retire and healthcare organizations strive to onboard new talent, virtual mentorship bridges the knowledge gap.
Veteran nurses can guide their less-experienced colleagues through complex procedures in real-time, preserving institutional wisdom and reducing burnout. For clinicians, this
level of support is invaluable; for patients, it means consistent, highquality care no matter who is at the bedside or behind the screen.
tal or out in the community.

Healthcare is a human endeavor, and safety must always be at the center. Unfortunately, violence against healthcare workers is on the rise. According to Nurses United, an alarming 8 in 10 nurses face violence at work.
Digital health solutions can help protect both patients and clinicians. Features like duress buttons, real-time location tracking, and secure communication can assist with getting help quickly inside the hospi-
As we look ahead, the integration of connected frontline solutions, intelligent automation, and asset visibility will continue to drive progress. Connected solutions will unlock new opportunities for innovation, business growth, and, most importantly, better outcomes for patients and providers alike.
To realize this vision, healthcare organizations must prioritize flexible, interoperable, and clinician-centered platforms.
It’s not about a single device or application; it’s about a robust ecosystem that supports real-time insight, connected collaboration, and optimized workflows across the continuum of care.
Kassaundra McKnight-Young is CNIO, Healthcare Industry Principal, Zebra Technologies.
Jennifer MacGregor is Managing Director and Founder, Elewana Advisory.
Ms. McKnight-Young
Next Big Thing in healthtech might be the person sitting next to you
BY SHELAGH MALONEY
I’ve heard it said that your network is your net worth. This feels truer to me now than it did decades ago when I first joined Digital Health Canada as a member. Over the course of my career, my involvement with Digital Health Canada – as a member, on committees, and as Board President and Digital Health Canada Fellow – has played an important role in helping me build and expand my professional networks.
I was able to create and deepen relationships, learn new skills, and connect with mentors, all thanks to my membership in the association.
Now, I’m approaching the six-month mark in my role as CEO of Digital Health Canada, and two questions I’m asked most often are: “How do you like the new role?” and “What have you learned so far?”

To the first, my answer is simple. I enjoy the interactions and the opportunities for connection that come with a position like this one.
The second question makes me reflect on the many conversations I’ve had with digital health professionals and colleagues across the country over these past six months.
I’ve had the good fortune to participate in Digital Health Canada regional conferences across the country, to represent the association at partner and member events, attend board and committee meetings, and interact with members in multiple settings.
The one thing I’ve learned so far is that the importance of networking endures. As we celebrate the association’s 50th anniversary, it’s worth remembering that networking and relationship-building have always been a core benefit of membership, and remain the key to our collective success.
As Bill Nye aptly said, “Everyone you’ll ever meet knows something you don’t.”
I’ve heard that you should build your network before you need it. Strong networks can help with career advancement, provide personal and professional support, and help us gain knowledge and grow. At Digital Health Canada, we recognize the power of networking and have expanded and enhanced our service offerings to provide more (and more varied) networking opportunities to our members across Canada.
We built a Community Hub where members can log in for virtual connection and mentorship through MentorLink, scheduled mentorship sessions that foster connections between a selected mentor and a small group of up to seven Digital Health Canada Student Members. Each session focuses on a specific topic and offers a supportive space for open discussion, shared experiences, and practical advice and guidance.
We’ve increased the frequency of our regional events and expanded into areas where members asked for connection and learning opportunities.
Over the next six months, we will bring
the power of networking to members in Winnipeg, Montreal, Nova Scotia and the wider Atlantic region, Regina, Vancouver, Calgary, and Toronto.
We are investing in the next generation of digital health leaders with Driving the Future of Digital Health, a one-day virtual

event focused on empowering emerging professionals by providing them with knowledge, mentorship, and networking opportunities.
Academic and author Brene Brown says, “Courage starts with showing up and letting ourselves be seen”.








To succeed, we all need the benefits that networking brings: to be exposed to new ideas and perspectives, and to be inspired by our peers.
Shelagh Maloney is CEO of Digital Health Canada.
















Shelagh Maloney
Remote regions continue to benefit from expansion of telehealth teams
Clinicians in Nunavut now collaborate with colleagues in Ottawa to stabilize critical care patients.
BY DIANNE DANIEL
The Ottawa Hospital’s (TOH’s) Virtual Critical Care Program (VCCP) recently expanded to give healthcare providers in the Qikiqtaaluk region of Nunavut real-time access to critical care specialists.
The service connects frontline physicians at the Qikiqtani General Hospital in Iqaluit to TOH critical care specialists, helping to manage and stabilize critically ill patients, including patients in shock, patients who are deteriorating, complex cases requiring a second opinion, or patients who require a ventilator.
The VCCP relies on telephone or video call connections to bring teams together for consultation, with one dedicated ICU physician and one dedicated ICU nurse available in Ottawa around the clock to receive calls as they come in.
The program started in 2023 as a tool to support patients in eastern Ontario regional hospitals during the pandemic and is now available at 13 sites, including the latest connection to Nunavut.
Hospitals using the Epic electronic health system securely connect to the Ottawa-based team through a video link provided within the Epic platform, simply by clicking on a button.
“Imagine a two-screen setup where on one screen you have a video going, talking to a physician or nurse, and on the other screen you have the patient’s chart open in all of its richness, with all of the blood tests, radiology reports and past history,” explained VCCP director Dr. Scott Millington. “Everything is there at your fingertips. It makes for a wonderful experience.”
To connect with Qikiqtani General, the program is piggybacking on existing telehealth infrastructure, already in place at the hospital to support other virtual care initiatives such as Ontario’s telestroke program.
“The program is more about people than it is about technology per se,” explained Dr. Millington. “We try to do video consults so that we can see each other’s faces and get that richness –including interacting with patients and their families. All of that is very helpful but we also sometimes just help over the telephone.”
antibiotics to administer, to whether to use a vasopressor (to constrict blood vessels), to how to adjust ventilator settings.
Another case involved a patient in one of the 12 remote communities supported by Qikiqtani General who was experiencing a critically low hemoglobin after a GI bleed.
“We were able to review the treatment we had given so far and make sure we had covered all of the appropriate bases,” said Dr. Patterson. “It also helped to facilitate transfer to the ICU once we got the patient out of the remote setting. It was much easier to say, ‘Okay. They’re here now and we’re waiting for the jet’ and then it went from there.”
The program is not limited to patients requiring transfer. In some cases, the consultation is used to stabilize critically ill patients who choose to remain in Iqaluit for treatment.
Qikiqtani General is the only hospital in the region and none of the communities are connected by road, meaning any time someone needs to be transferred out for medical treatment it involves a flight. “If they have a patient they’re at all wor-
“From a critical care perspective, it would be wonderful if every citizen of Ontario – and every Canadian citizen – could eventually be covered under a virtual critical care umbrella,” he said. “Many jurisdictions have virtual or remote programs for emergencies such as stroke or heart attack. I would love to see a third spoke of critical care added to that list.”
Neurosurgeon Dr. Ivar Mendez dedicated his career to understanding the complex interface between computer systems and the human brain, working to advance deep brain stimulation techniques to help rewire neural pathways in people suffering from issues like movement and sensory disorders, Parkinson’s disease or depression.
Now, as director of the Saskatchewan Virtual Health Hub (VHH), he’s on a mission to bring the power of technology to an even wider cohort of patients, starting with the most marginalized populations of Canada.
“It became clear to me that technology could be a real tool to decrease inequity in healthcare delivery, not only in our country, but globally,” said Dr. Mendez, who is leading the Indigenous-led healthcare hub as it builds out the major systemic processes required to scale virtual care to remote and rural areas across the province.

ried about, they can get a quick second opinion,” said Dr. Millington, adding that patient transfers occur faster when required and at the same time, can be avoided when unnecessary.
Moving forward the aim is to layer on emerging technologies like robotic ultrasound, which would require a more robust telecommunications connection between Ottawa and Nunavut, but for now it’s the live consultation between people that’s making the difference.
Qikiqtani General chief of emergency Dr. Mike Patterson has used the service a few times since its launch in April 2025. On one occasion he was intubating a critically ill patient before airlifting them to Ottawa and held a video group chat involving the respiratory therapist, ICU doctor and nurse coordinator at the receiving end.
The consult made sure everyone was on the same page, he said, as they discussed everything from what
“We’re not looking to transfer more patients or transfer less patients. We’re just looking to make sure that whoever we get called about gets what they need,” he said.
Telehealth services have been in place at Qikiqtani General for four years, for telestroke and to provide on-call support to remote communities. The VCCP builds on that connection and Dr. Patterson sees potential to continue to expand virtual care, particularly if bandwidth improves.
“I think programs like this could go a long way to improving equity in healthcare, but before we get there, we have to tackle the bandwidth and communication issues,” said Dr. Patterson.
Speaking personally, Dr. Millington is a big advocate for virtual care and hopes to see programs like VCCP continue to expand across Canada.
“When I envision the future –maybe beyond 10, 20 or 30 years – the frontier of healthcare is going to be at home,” he added.
The hub’s virtual care model, fully funded by the federal and provincial governments, is a partnership between the Whitecap Dakota First Nation, the Saskatchewan Indian Institute of Technologies (SIIT) and the Remote Presence Robotics program at University of Saskatchewan where Dr. Mendez is emeritus professor.
Based on more than a decade’s work to co-develop culturally appropriate virtual care interventions with Indigenous communities, the hub includes a specialized facility expected to open in 2027 in Whitecap. In addition to remote presence robots, artificial intelligence (AI), 5G telecommunications, and intelligent peripherals and sensors for remote patient assessment and monitoring, the hub will also offer training spaces, gathering spaces and culturally sensitive spaces such as a centrally located Elder’s room on the main floor.
Through their work to advance virtual care services in rural and remote areas, the VHH team has demonstrated that roughly 70 percent of medical cases can be successfully treated remotely when the tools are readily available, and people know how to use them.
They’ve also found that when clinicians and caregivers in small rural areas are supported by reliable connections to specialists in larger urban centres, there is a higher recruitment and retention rate.
“We can’t be doing what we’ve been doing over the past two to three decades. We need to make sig-
nificant change for the future and one of the models that will improve that care is virtual care, using technologies like advanced AI robotic systems,” said Dr. Mendez. “This is what the virtual health hub is all about. We are building, not the technology itself because technology changes and improves, but we are tackling the systemic issues.”
Those issues include considerations such as how to implement virtual care in a sustainable manner that supports diverse regional workflows; how to train clinicians; how to use a team approach to provide care to somebody, regardless of their location; and, how to ensure clinical gaps are filled in ways that are culturally appropriate. Two pillars at the core of the hub’s strategy are relationship building and capacity building.
Another key component is education and training. Under the VHH model, community members learn how to use the advanced technologies through accredited programs coordinated by SIIT. When they return to their communities, they serve the role of virtual care assistants, helping to facilitate virtual interventions.
To date, 24 individuals from 24 communities across northern Saskatchewan have received training and are working as integral members of the VHH team, said Dr. Mendez. One area already showing vast improvement in patient outcome is the use of robotic ultrasound technology to care for pregnant Indigenous women.
“You can help from the outside, but real transformation comes within,” he said, referring to newly trained virtual care assistants as the clinical workers of the future. “When they go back to their communities, they are seen as trusted individuals.”
Another patient group expected to benefit from the virtual model of care delivery are people diagnosed with diabetes who are prone to two complications: lower limb amputation and/or diabetic retinopathy, a leading cause of blindness affecting more than one million Canadians.
Both conditions are preventable with proper screening, explained Dr. Mendez, yet Saskatchewan has one of the highest rates of diabetes-related amputations in the country. To enhance care delivery, the hub has created a sustainable clinical pathway to deliver patient screening virtually.
For example, diabetic patients living in remote communities can now be referred to a local clinic where a trained assistant uses a handheld camera to capture a standard set of retinal images. The camera alerts the assistant when the positioning is perfect to ensure high-quality images are obtained. The images are then sent to a computer for analysis by an AI algorithm that automatically generates a report and, if the retina is abnormal, the data is sent to an ophthalmologist for review.
“The site assistant will use the sophisticated camera and on the other side, we have the ophthalmologist who will follow up with the patient,” explained Dr. Mendez. The model works because people are more comfortable dealing with their own community members in their own language, he added.
The technology may be cool, but the important aspect is the establishment of the clinical pathway. “We know the journey of the patient, when it starts, who takes the
picture, who does the assessment and follow up, who provides the report and how the patient is treated,” he said.
To combat the high prevalence of lower limb amputation, the VHH team has developed a clinical pathway to enhance diabetic wound care. When a patient arrives at a clinic, the local virtual assistant uses a cutting-edge telepresence system with augment reality to transmit
images of a wound to a vascular specialist miles away.
By creating a digital twin, the specialist sees what the assistant is seeing simultaneously, and the assistant sees the specialist in a small screen at eye level as they are guided on how to properly debride the wound.
If the virtual specialist deems that the patient needs to be seen in person, the patient is sent to Saskatoon for a consultation
before returning to their local community where their case is further monitored and managed at the virtual clinic until the wound heals.
As the hub continues to ramp up virtual services in the province, Dr. Mendez is hopeful the model can be replicated elsewhere. “It’s not the silver bullet that will fix everything, but it is going to be a pathway for the future of healthcare delivery,” he said.



