Blind/Low Vision pg 16
Spotlight pg 22
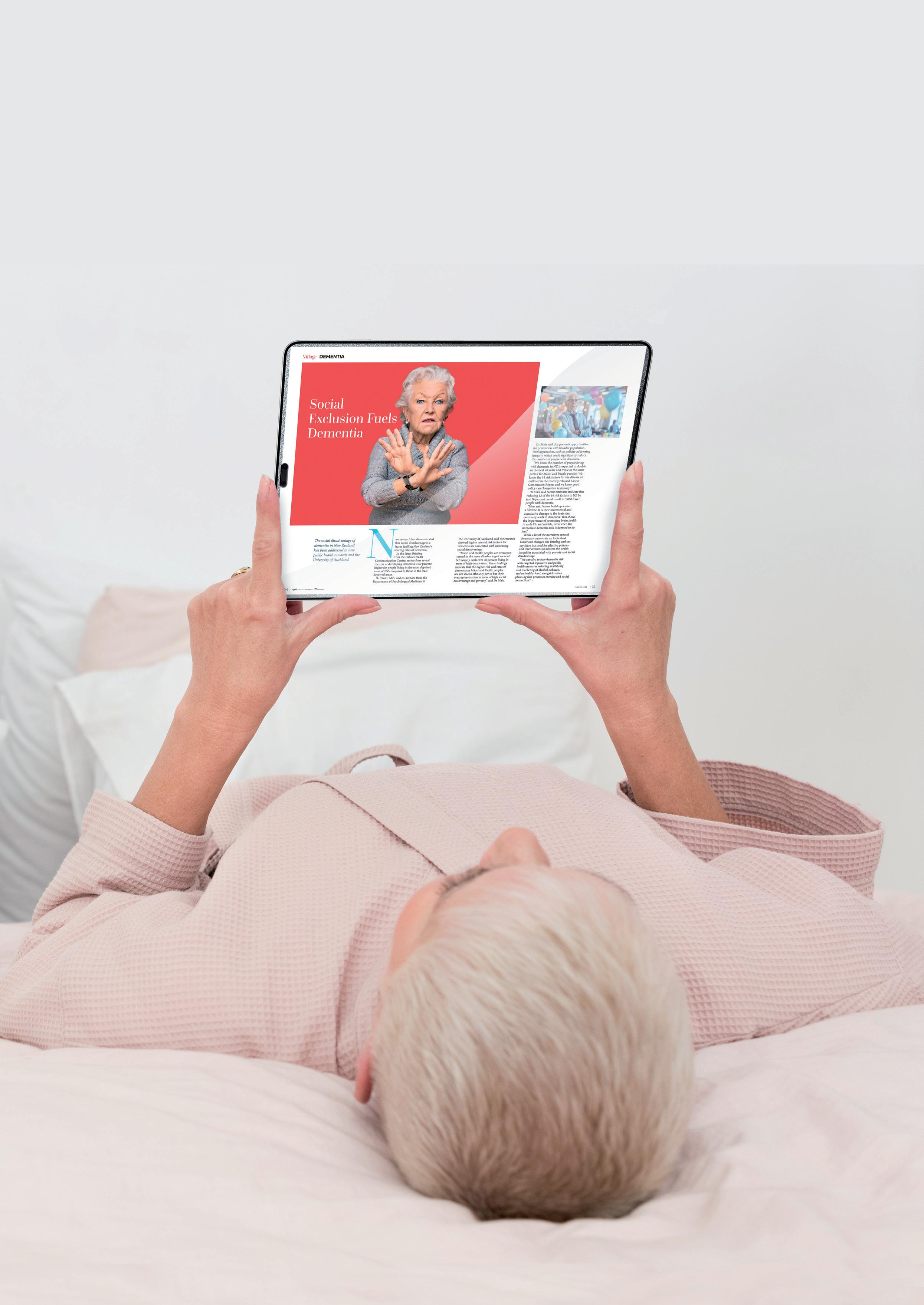
Dementia pg 30






Blind/Low Vision pg 16
Spotlight pg 22
Dementia pg 30





s we live longer, one quiet change that often slips under the radar is how our eyesight shifts with age. For many older New Zealanders, low vision becomes part of daily life, affecting not just how we see but how we move, connect, and feel confident in our surroundings.
Conditions such as macular degeneration, glaucoma, cataracts, and diabetic eye disease are now common, and while modern treatment can slow their progress, many people still find their world growing dimmer. It’s not just about reading or driving; it’s about staying independent, social, and safe.
The good news is that support has grown significantly. Low Vision NZ and the Blind Low Vision Foundation are doing important work, helping people adapt through home visits, mobility training, and assistive technology. Simple tools like better lighting, large-print books, and digital magnifiers can make a real difference. Even everyday tech,
such as phones and tablets with voice controls and screen readers, is opening up new ways for older adults to stay connected.
We’re also seeing thoughtful design in aged-care facilities and retirement villages, with improved signage, stronger contrast, and brighter shared spaces that make life easier for those with reduced sight. These small touches have a big impact.
The real key, though, is awareness. Many eye conditions develop slowly, and early checks can protect vision and maintain independence for years to come. As we continue to focus on ageing well, supporting good sight should be part of that bigger picture. Tania Walters, Publisher tania@reviewmags.com
PUBLISHER: Tania Walters
GENERAL MANAGER: Kieran Mitchell
EDITORIAL DIRECTOR: Sarah Mitchell
EDITOR-IN-CHIEF: Caitlan Mitchell
EDITORIAL ASSOCIATES: Sam Francks, Jenelle Sequeira
ADVERTISING SALES: Caroline Boe
SENIOR DESIGNER: Raymund Sarmiento
GRAPHIC DESIGNER: Raymund Santos
Retail 6, Heards Bldg, 2 Ruskin St, Parnell, Auckland New Zealand P: +64 3040142 Email: edit@reviewmags.com

A new system for delivering home care services to older people, focusing on restorative care, is set to begin in the South Island. 12 Effective
A study by the University of New South Wales has highlighted the effectiveness of the Short-Term Restorative Care Programme. 14 A Person-Centered
For seniors with vision impairment, there is a fear that it may cause them to lose their independence or have to relinquish hobbies such as reading or crafts. Low vision aids allow seniors to make the most of their sight, and devices such as magnifiers enable seniors to see better, even when their vision begins to decline.
By 2035, the retired population is expected to be twice of what it is presently and will account for nearly one in every four New Zealanders.
Blind Low Vision NZ said new figures reveal inequities facing more than 183,000 New Zealanders affected by vision impairment.
Voice technology has become an effective way for care providers globally to ease pressure on staff and combat loneliness.
Retirement Commissioner Jane Wrightson will conclude her second term early and not seek reappointment to the role she’s held since 2020.






22 Persistence pays offDiversional Therapy learner gains confidence and makes a difference
They say third time’s a charm and for Sue Moxom, this is particularly true as she nears completion of her Diversional Therapy Apprenticeship on her third try.
25 Supergrowth or Fiscal Downfall?
Treasury has revealed that fiscal pressures will accelerate in the coming decades, with the cost of superannuation and healthcare expected to rise significantly.
As the healthcare sector continues to adopt new technologies, research front the University of Auckland has suggested artificial intelligence may be the key to unlocking future potential.
32 Fearful of the Future
Alarming new research shows dementia is now affecting three New Zealanders every hour, around 500 people every week, according to Alzheimers NZ.
As an Event Coordinator, Eileen Verona said a highlight of her role is being able to bring connection, joy and unforgettable moments to life, one event at a time.
Pāpāmoa Beach Village, a Metlifecare village situated in Tauranga, has been announced as a finalist in the Gilmours Excellence in Food Service Award at the EBOS | ACA Excellence in Care Awards in October 2025.
North Auckland's Settlers Lifestyle Village has been named as one of the country's best at the 2025 New Zealand's Best Awards.
Settlers Lifestyle Village on Auckland’s North Shore, a property of Premier Lifestyle Villages Group, has been recognised across categories in the New Zealand’s Best Awards, which recognise the best Aged Care, Retirement, and Lifestyle Villages across the country.
The 2025 awards given
to Settlers Lifestyle Village demonstrate the Auckland Retirement Village’s excellence as a leader across multiple years within the competitive retirement village sector.
These awards have been held since 2015 and are highly credible because they are based on independent reviews and ratings from residents, their families and visitors.
Along with accolades for this year, Settlers Lifestyle Villages has

won an Enduring Excellence Trophy 2025 for Consistently High Resident Recognition for five years. As only the sixth such award presented in the last
Summerset Group has reported 420 sales for the quarter ending
30 September 2025, comprising 244 new sales and 176 resales.

More diagnostic tests will be available through Health New Zealand, as the Government commits to faster answers for Kiwis.
Health New Zealand will deliver an additional 75,000 diagnostic procedures this year through its NZD 65
million Diagnostic Improvement Plan, aimed at reducing wait times for critical diagnostic procedures such as MRI scans, colonoscopies, and colposcopies, Health Minister Simeon Brown said.
“It is estimated that approximately 40,000 New Zealanders are waiting longer than they should for the tests they need. Long waits
Summerset Group CEO Scott Scoullar said the company is pleased to continue its first half sales momentum with another record quarter.
“We’ve worked hard throughout the business to bring new residents into our villages, it’s pleasing to achieve our highest ever sales quarter in this difficult market,” said Scoullar.
“We have continued
10 years, Enduring Excellence Awards recognise facilities that have shown consistent award excellence over a period of at least five years. Read more online
to sell new Care Occupation Rights Agreements (ORA) and convert our care rooms to ORA as we seek to improve our care profitability. In Q3, 29 percent of sales were Care ORAs (38 percent of new sales and 16 percent of resales). New and current residents have warmly welcomed this offering as an alternative to paying daily premium charges.”
Read more online

not only cause stress and anxiety for patients and their families, they also delay the start
of treatment and put extra pressure on our hospitals.”
Read more online







Scam victim numbers are down, but losses are up. The Banking Ombudsman said the drop in scam cases has reflected bank action. The Banking Ombudsman Scheme helped more than 5,800 bank customers and facilitated compensation or refunds totalling more than NZD 2 million, according to its latest annual report. The most common complaints were about personal transaction accounts, property lending and credit cards.
disputes were up four percent and seven percent, respectively. Despite this, the scheme exceeded its timeliness targets and maintained high satisfaction among users (more than 80 percent).
Financial hardship complaints rose 55 percent, according to the report. Most involved vehicle and home loans and KiwiSaver withdrawals. Servicerelated complaints rose 11 percent. Poor communication was a recurring issue in many of these complaints.
Scam-related complaints fell 17 percent to 694 cases, but the average reported loss increased 10 percent to NZD
88,000 this year, up from NZD 80,000 in 2023-24.
Banking Ombudsman Nicola Sladden said the drop in scam cases reflected recent initiatives by banks to tackle scams. However, she cautioned against any suggestion that scammers were on the ropes.
"Scams remain a serious concern, especially given their increasing sophistication and impact," said Sladden.
"We are pleased to be part of the new AntiScam Alliance, and we continue to push for stronger industry codes and coordinated action to protect consumers." Read more online

Pharmac savings have been pleasing to see, according to the ministers responsible, especially enabling broader medicine access.
Associate Health Minister
with responsibility for Pharmac, David Seymour, and Health Minister Simeon Brown said they were are pleased to see Pharmac negotiating savings to increase medicines access.
"For many New Zealanders, funding for pharmaceuticals is life or death, or the difference between a life of pain and suffering or living freely,” Seymour said.
“Pharmac has announced its proposal to


fund five new treatments for conditions including multiple sclerosis, breast cancer, eye conditions, and lung cancer. We are focussed on fixing what matters. Pharmac estimates that over 1,700 New Zealanders could benefit from the proposal in the first year of funding, rising to 4,000 by year five.”
Seymour said the impact of this proposal was huge, and the new subcutaneous injections are significantly quicker to administer than current IV treatments. If approved, it would save an estimated 7,500 hospital infusion hours in year one, and 12,800 by year five. This frees up health professionals to deliver other treatments. Read more online

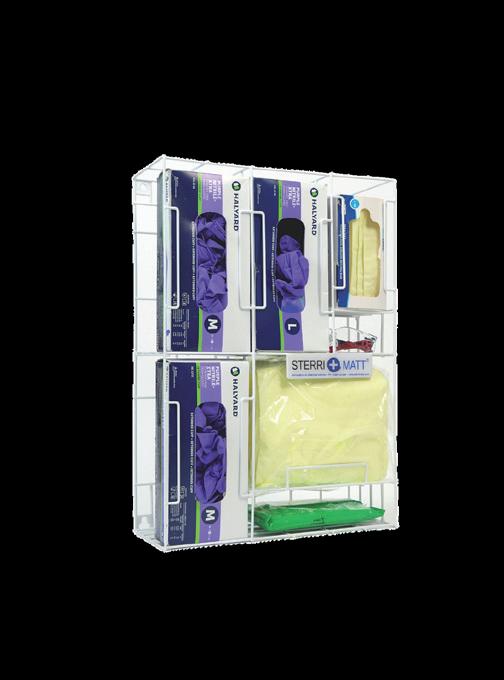
Sterri-Matt® PPE Stations & Dispensers are the ultimate IPC solution with over a 100 versatile combinations to enhance your infection control programs

we also offer a wide range of Quad Glove Dispensers for







A new system for delivering home care services to older people, focusing on restorative care, is set to begin in the South Island.

Casey Costello Associate Health Minister
ssociate Health Minister Casey Costello said this was one of a series of improvements being made to the current aged care system, backed by a significant increase in funding, to support improved care and the aged care sector.
The aged residential care (ARC) sector has received a four percent funding uplift and will see a total increase of NZD 96 million this year, and funding for home and community support services (HCSS) will increase by NZD 44 million.
The total funding increase of NZD 140 million this year is in addition to an annual increase of NZD 129 million last year, meaning that government spending on aged care now exceeds NZD 2.5 billion.
“The funding increases are aimed at relieving pressure on the sector and improving care services for older New Zealanders while we work towards the longer-term reform needed to better help
people age well,” said Costello.
“The reality is the current aged care model is out of date, so we are making improvements in the short term as well as considering system-level change.”
These changes in home care funding and provision introduce a new ‘case mix’ framework and funding model across the South Island to support those who receive care at home.
“Four providers have been contracted to provide the new model, which is designed to move away from “task-based” care plans where providers are paid by the hour for specific tasks to more flexible care which is responsive to what people need. The new service model will provide better care with a focus on keeping people as independent as long as possible.”
The case mix framework and funding model will be introduced across the other three Health NZ regions to provide national consistency.
The Minister stated that Health NZ was also collaborating with the aged care sector to update the current contract for aged care and to develop a more effective system for categorising care needs.
“The sector has said, and I’ve seen, that people entering residential aged care have higher health needs than before, and some older people need greater care from home services as well as more specialised services, such as bariatric and even palliative care in ARC facilities. I want this process to better categorise this need, and the care people require, which will support the development of an appropriate funding model.”

A study by the University of New South Wales has highlighted the effectiveness of the Short-Term Restorative Care Programme.

estorative care for seniors has largely centred around independence and has aimed to maximise their ability to perform daily tasks. It has often been credited as a flexible approach that can follow rehabilitation and is focused on a personalised plan of care that encourages active participation with the goal of delaying or reducing the need for ongoing long-term support services.
The study analysed data from 484 clients who participated in the programme and focused on their functional improvements and ability to remain in their own homes post-intervention.
The Short-Term Restorative Care Programme was a governmentfunded, eight-week, multidisciplinary intervention designed to help older adults regain independence and avoid the need for more intensive aged care services and premature entry into residential care.
As part of the new Support at Home program, it was replaced by the Restorative Care Pathway earlier in the year, offering allied health support over 12 weeks.
The study, led by researchers from the Centre for Positive Ageing at HammondCare and the School of Population Health at UNSW Sydney, identified that the Australian Government’s ShortTerm Restorative Care Programme significantly improved health outcomes for older adults experiencing functional decline.
The research also found that participants, with an average age of 81.5 years, showed statistically significant improvements in physical function, mental health, and goal attainment.
Lead author Dr Lindsey Brett said the findings demonstrate the value of restorative care in supporting older Australians to maintain independence.
“Our study shows that STRC can lead to meaningful improvements in daily functioning and wellbeing, particularly when care is tailored to individual goals,” she said.
This study contributed valuable evidence to the growing field of restorative care and supports the continued investment in community-based services that prioritise independence and quality of life for older adults. This included insights into various clinical and outcome measures used, identifying those that work well with this population and those that require further consideration.

By 2035, the retired population is expected to be twice of what it is presently and will account for nearly one in every four New Zealanders.

nabling and fostering restorative care practices will help seniors maintain their independence and will help to sustain the health system. Providing seniors with equitable access to timely, high quality health care will help them to achieve their maximum potential for good health and wellbeing.
Introducing a restorative care approach will work directly to achieve these goals. Many providers in New Zealand, especially within the South Island, have already reported the noticeable benefits of restorative care within their villages.
Restorative care is a flexible approach to health care that respects the individual, and will help them to maintain the highest level of function and independence for longer, actively participating in decisions about their care.
Implementing restorative care into village operations relies on decisive factors that determine the best programme for each resident.
Older people are assessed through a comprehensive multidimensional assessment (interRAI). Care planning is goal-oriented and reflects the individual’s needs and desires. Targeted, evidencebased interventions are used to optimise daily living functions. Interventions are delivered safely and balanced against potential risks. They are also culturally appropriate and responsive to the changing needs of the individual. If evidence-based
research is not available, interventions based on best practice are used.
Care is provided by a multi-disciplinary team, which often includes general practice, registered nursing, physiotherapy, occupational therapy, dietetics, speech language therapy, pharmacy, social work, and appropriate cultural support. Teams meet regularly to review challenging or resource-intensive cases and facilitate the input of other community organisations that could provide support.
Education is encouraged for all older people, their carers, and professional staff. For example, chronic disease selfmanagement, healthy ageing, continence, nutrition management, use of medication, illness or accident prevention strategies, and improvement or maintenance of skin integrity.
Older people, their families and whānau, and their carers are encouraged to participate fully in all care decisions, promoting their sense of autonomy and reducing the need for ongoing in-person supervision. Active engagement in a range of daily living activities is promoted, and task analysis, work simplification, and assistive technology and telemedicine are used where appropriate. Strength, balance, and endurance programmes are used to improve or maintain mobility.
In time, it is hoped that each older person will have a single care plan, which provides a complete view of their care and is shared by all providers.

Blind Low Vision NZ said new figures reveal inequities facing more than 183,000 New Zealanders affected by vision impairment.

Bernadette Murphy Head of Fundraising
Blind Low Vision New Zealand
s cost-of-living pressures dominate headlines, data from Blind Low Vision NZ revealed how blind, deafblind, and low vision New Zealanders are disproportionately affected, facing not only higher costs but also the emotional strain of barriers most Kiwis never encounter.
According to the Stats NZ Household Disability Survey, 58 percent of disabled New Zealanders earn NZD 30,000 or less annually, compared with 33 percent of non-disabled people. For those who are blind, deafblind, or low vision, these financial pressures are compounded by hidden expenses, from taxis that cost more than public transport, to adaptive technology priced in the thousands, to medical services that remain inaccessible.
Blind Low Vision NZ clients report skipping GP appointments because travel is unaffordable, and delaying treatment
because forms and health information aren’t available in formats they can read.
The inequities extend into the workplace. While one in six New Zealanders identify as disabled, 60 percent are unemployed or underemployed. For Blind Low Vision NZ clients, 51 percent of working-age members are without a job, and 74 percent of youth clients have never had a part-time or summer job.
These figures reflect systemic barriers such as bias, inaccessible recruitment systems, and persistent myths about cost or productivity, despite the fact that 75 percent of working-age disabled New Zealanders require no additional support or equipment from their employer to do their job.
Beyond the financial pressure, the hidden costs are emotional. Relying on strangers to read personal mail or medical forms compromises privacy. Inaccessible transport and unsafe streets reduce independence. Social connection is lost when daily participation feels overwhelming or impossible.
The impact is growing. Census data shows the number of people reporting no or limited sight that affects daily activities has risen by about eight percent since 2018, from just over 169,000 to nearly 183,000 in 2023. As prevalence rises, so too does demand for services and support.
Blind Low Vision NZ client Ethan said orientation and mobility training, Braille and being matched with his guide dog Jack have been “life-changing”, however despite the support from Blind Low Vision, his whānau and guide dog, Ethan still faces barriers.
These include inaccessible websites, confusing systems, verbal abuse and stray dogs running up to guide dog Jack. However, he doesn’t let these setbacks stop him, saying “No matter what happens, I’m still going to get out of the house. Don’t hide from the hard stuff- what some people see as a massive inconvenience, I see as opportunity”.
Blind Low Vision NZ currently supports more than 15,000 clients. In 2025 alone, over 64,000 books were borrowed from their accessible library, nearly 1,000 people
took part in its adaptive technology webinars, and 1,400 volunteers contributed more than one million hours, the equivalent of 500 full-time staff. Services include guide dog training, mobility support, skills for independence, emotional wellbeing programmes, youth employment readiness, deafblind services, and tailored support for Māori and Pasifika clients. Referrals are rising, with a 46 percent increase in specialist referrals in 2024 alone showing that demand for these services has never been greater.
This year, Blind Low Vision NZ has also introduced a White Cane Initiative, allowing eligible members to apply for one fully funded cane and up to two tips annually, an essential lifeline for safe mobility that many previously had to purchase at personal cost.
“With 80 percent of our income coming from donations, community support is critical,” said Bernadette Murphy, Head of Fundraising, Blind Low Vision NZ.
“The cost-of-living crisis is hard for everyone, but when you add inaccessible services, higher transport costs, and the price of adaptive technology, New Zealanders who are blind, deafblind, or have low vision are unfairly disadvantaged. Donations help us reduce those inequities and ensure people can live with dignity, equity, and independence.”
Blind Low Vision NZ is calling on New Zealanders to support its Blind Low Vision Month appeal this October, aiming to raise NZD 500,000 to fund essential services for people who are blind, deafblind, or have low vision.

For seniors with vision impairment, there is a fear that it may cause them to lose their independence or have to relinquish hobbies such as reading or crafts. Low vision aids allow seniors to make the most of their sight, and devices such as magnifiers enable seniors to see better, even when their vision begins to decline.

ow vision aids and other assistive technologies aim to enhance seniors’ remaining vision and provide aid or compensation, for impaired vision, making daily living activities easier to perform. They utilise the angular magnification effect by increasing the relative size and relative distance. Low vision aids are useful in clinical conditions like retinitis pigmentosa, glaucoma, macular degeneration, albinism, aniridia, retinal detachment, diabetic retinopathy, optic atrophy, and chorioretinitis.
As technology continues to advance, assistive technologies for vision play a significant role in the lives of seniors, especially those with disabilities, supporting their engagement in daily activities and participation in their communities. Magnification aids, such as optical devices or electronic magnifiers, are commonly used to meet low vision people’s needs.
There are various types of low vision aids in different forms and strengths that can make
day-to-day living easier for seniors.
Hand magnifiers allow the user to adjust the height of the magnifier until their vision is focused. They are typically illuminated with an inbuilt light source, portable, easy to use and have flexible working distances.
Non-illuminated stand magnifiers rest on the page without needing to be focused. They are often designed for higher magnification, don’t require good hand control as they rest on the page, and ensure the object is always in focus.
Alternatively, illuminated stand magnifiers can be powered through batteries or plugged in, and often use LED globes for visual clarity. For many, the concept of illumination is extremely important. The light source is kept near to the eye, and moving the light source closer will provide higher illumination. A higher level of illumination is required in patients with retinal pathologies like loss of cone function (age-related macular degeneration), glaucoma, diabetic retinopathy, retinitis pigmentosa, and chorioretinitis.
It is important for carers to discuss with seniors about which lens is best for them. It should depend on individual needs and preferences, affordability and ease of use.
Common varieties include plano-convex lenses, which are an ideal choice for people who need to magnify small text or images, such as books, newspapers and magazines, or biconvex lenses, which could be better suited for people wanting to magnify larger objects like maps, menus and signs.
Low vision aids are crucial for seniors wanting to maintain their independence and build their confidence. As a practical solution for everyday tasks, low vision aids provide a better quality of life and allow seniors to remain engaged in the community.


Voice technology has become an effective way for care providers globally to ease pressure on staff and combat loneliness.
rom rising demand and limited resources to workforce challenges and growing expectations, providers are constantly seeking new ways to deliver high-quality, person-centred care. In this context, technology is no longer a nice-to-have but an essential part of modern service delivery. One area showing particular promise is voice technology.
Devices like Amazon Alexa, when deployed in a managed and secure way, are helping care teams support residents with greater efficiency, while also enhancing daily life for those receiving care.
Voice technology is increasingly recognised for its ability to support people of all ages and abilities. In care and supported living, its impact is especially profound. Whether used off-theshelf by individuals or through a managed service, voice technology offers a wide range of functions that support wellbeing, routine, and independence.

Seniors using voice technology are able to set reminders for medication, meals or appointments, hear the weather or local news, listen to the radio, podcasts or play music, play voice games or quizzes, or call friends and family.
All of this is done by voice, without needing to use a phone, app, or screen. For people with mobility or memory challenges, this creates a low-effort, accessible way to stay informed, stimulated, and connected.
Voice technology is also helping to combat loneliness, which is increasingly recognised as a serious public health issue. Research has shown that loneliness increases the risk of depression by up to 64 percent, and that lonely individuals experience a 20 percent faster rate of cognitive decline. In 2023, the World Health Organisation declared loneliness a significant global health threat, linking its mortality impact to smoking 15 cigarettes a day.
Voice technology provides a gentle, alwaysavailable presence. For many people, having something to interact with during quiet moments creates emotional comfort. It brings a sense of companionship, structure, and even joy, especially when used for music, humour, and connection.
The benefits to staff are just as important. In busy care environments, time is precious. Fleetmanaged systems help by automating routine prompts, reducing unnecessary checks and visits, sharing messages and updates without disturbing residents, and supporting digital engagement without requiring residents to use screens or apps.
Voice technology also reduces the need for multiple systems to manage basic communication. Staff can broadcast messages across devices, manage reminders for whole schemes, and track device engagement through a single dashboard.
Retirement Commissioner Jane Wrightson will conclude her second term early and not seek reappointment to the role she’s held since 2020.
rightson has led the Retirement Commission for nearly six years, overseeing research, policy advice on retirement incomes and villages, and public education to support New Zealanders’ financial wellbeing.
Throughout her time as Retirement Commissioner, she has successfully advocated for key policy changes which will see more New Zealanders enjoy a better retirement as a result.
Key achievements of hers included the first substantive review of the Retirement Villages Act 2003 with a decision expected on legislative changes by the end of 2025.
Wrightson recommended employer and employee KiwiSaver contributions increase to four percent and for 16 to 17-year-olds to be included, confirmed in Budget 2025, and she championed the compulsory inclusion of financial education in schools, announced in April 2025.
She also rallied a diverse financial services sector around supporting the National Strategy for Financial Capability with three-year action plans, and ensured that Sorted keeps growing as a popular and appealing upskilling resource for the more than two million New Zealanders who use it each year.
Minister of Commerce and Consumer Affairs Scott Simpson acknowledged the work of the Retirement Commissioner.
“I would like to thank Jane Wrightson for her leadership and for the way she’s advocated for better financial capability and retirement

outcomes for New Zealanders. I wish her all the very best for the future,” Simpson said.
He said recruitment for the next Retirement Commissioner will begin shortly.
As Retirement Commissioner, Wrightson said she was proud of what’s been achieved during her time in the role.
“I can’t do anything without a great team, and while we might be small, over the years have achieved some big wins,” she said.
“Our work on the National Strategy for Financial Capability actively encourages different parts of the sector, from the big end of town to NGOs, to pull together on projects that make a difference.”
Wrightson added that high-quality research and analysis provided evidence for considered policy change, and that the Commission would ensure it’s public so that people can rely on it to inform themselves and their ideas.
“Years of championing for a stronger focus on financial education in schools has been heard, and it will be a game-changer for the next generation’s financial wellbeing,” she added.
“It’s been a privilege to hold this position, and I’d like to thank my team, the Ministers I’ve worked with, and our sector partners and stakeholders who help us to improve the financial futures of New Zealanders so a better retirement can be enjoyed by all.”

- Diversional
gains confidence and makes a difference
They say third time’s a charm and for Sue Moxom, this is particularly true as she nears completion of her Diversional Therapy Apprenticeship on her third try.

n the past, I just felt so overwhelmed, and it was too much for me. Now that I’m 62, I just thought it’s now or never,” she said.
Moxom works at Metlifecare’s
The Orchards aged care home in Auckland as an Activities Coordinator and is close to completing her Apprenticeship in Diversional Therapy through Careerforce. Careerforce is a work-based training provider for the health and wellbeing
sectors and supports learners to achieve NZQA qualifications fully on-the-job.
Every Careerforce apprentice is supported by an Apprenticeship Advisor and Moxom’s Advisor Nicky Liles commented, “Sue shared her initial worries and doubts and asked lots of questions which made space for reassurance and encouragement, and together we made a plan for success”.
Moxom is now well on her way to completing her apprenticeship and is feeling more confident, “I’m over halfway, and I know I can achieve it,” she said.
Careerforce also offers Study Hubs which are a chance for learners to drop in, ask questions, meet with other ākonga (learners) and receive help with achieving their unit standards. She is finding these sessions beneficial and enjoyed connecting with other ākonga. “There are a lot of other older people studying too and it is reassuring to know that everyone in their second part of life can achieve these things which you didn’t think you could have achieved before”.
She has seen huge changes in herself throughout the programme and said, “I think it’s made me a better person because I feel more confident in myself, and I know that I’m more capable of doing things than I was beforehand”.
Liles added “I’m so proud of Sue and her confidence on the apprenticeship journey has just gone from strength to strength”.
A few years ago, Moxom watched a programme called ‘Old People’s Home for 4 Year Olds’ which brought together a group of ten elderly care home residents with ten preschoolers. The two groups took part in daily activities together and the researchers monitored the physical and mental health of the older participants. Moxom said, “I watched this, and I thought ‘oh my goodness, I’ve got to do this for my oldies’, it’s just so meaningful”.
Reaching out to local primary school Beach Haven, She now has two groups of children that come in once a week. The children and the residents complete activities together such as colouring, dancing and sharing what the children have been up to, and the resident’s stories
Continued on page 24.

about their travels and lives. “It’s more than just a chitchat. They form special relationships, and a lot of the kids even call them grandma and grandpa”.
Moxom also sees huge benefits for her residents, “We had one lady who said, ‘It’s so nice to see the young kids, it keeps me young. It’s something to look forward to and breaks down the isolation’”. Another resident previously spent most of his time in his room, but came out to see the children and enjoyed showing them his badges that he had collected from around the world. “It’s really special. I think every care home should have kids coming in, it just gives meaning and purpose,” she said.
Not one to sit still, Sue has already started planning her next steps for after she has completed her Apprenticeship. “My goal, way in the future when I retire, is to go around and help the other Diversional Therapists and help give them ideas; to get speakers in, pet therapy, set up intergenerational programmes and give them a different
approach to the normal activities”.
As for whether she would recommend the Careerforce apprenticeship programme to other Diversional Therapists – “Absolutely, it’s not always easy, but you must work hard for anything worthwhile. If you have the determination and you’re willing to put in the extra work and time, it’s so rewarding”.
To help ease the burden of training costs across the Aged Care sector, Careerforce is offering 50% off its Advanced Care and Support Apprenticeship and Diversional Therapy Apprenticeship enrolments from 1 October until 30 November 2025. Enrolments are priced at just $1,000 (incl. GST), a saving of $1,000 (incl. GST), subject to eligibility.
For more information about Careerforce apprenticeships, visit www.careerforce. org.nz. Workplaces may also qualify for Apprenticeship Boost funding and receive $500/month for the first 12 months of each apprenticeship.

Save $1,000 on Aged Care
We’re offering 50% off selected apprenticeships from 1 October until 30 November 2025
Enrolments are now priced at just $1,000 (incl. GST)*, a saving of $1,000 for the following programmes:
NZ Apprenticeship in Diversional Therapy
NZ Apprenticeship in Advanced Care and Support
Also, apply for Apprenticeship Boost and access $500/month (excl. GST) for your eligible first-year apprentices.
*subject to eligibility – refer to website for details
Careerforce.org.nz/aged-care-promotion2025
Treasury has revealed that fiscal pressures will accelerate in the coming decades, with the cost of superannuation and healthcare expected to rise significantly.
he Treasury has published He Tirohanga Mokopuna, its latest Long-term Fiscal Statement, which highlighted the growing pressures on New Zealand’s public finances, especially the cost of superannuation and healthcare, and called for a proactive, balanced response to ensure long-term fiscal sustainability.
“Over the past two decades, the Treasury has consistently warned that population ageing is placing increasing strain on the Government’s fiscal position. Despite some positive developments, New Zealand has been running a structural operating deficit since 2019/20, underscoring the need for sustained fiscal adjustment,” said Iain Rennie.
“This means that even without future pressures from population ageing, climate change, or infrastructure needs, we must adjust our fiscal settings to bring revenue and expenditure back into balance.”
As per earlier Statements, He Tirohanga Mokopuna found that population ageing remains a significant long-term fiscal challenge with New Zealand Superannuation (NZS) and publicly-funded healthcare expected to rise substantially.
In 1965, there were seven working-age New Zealanders for every person over 65. Today, that ratio is four to one, and by 2065, it is projected to be just two to one.

Most New Zealanders over 65 receive a pension funded from general taxation. As the age structure of our population shifts, the cost of maintaining NZS in its current form will rise significantly. Similarly, health expenditure could increase from 7.1 percent of GDP today to around 10 percent by 2065 if policies remain unchanged.
The Statement also noted that climate change, defence, and infrastructure investment will add further fiscal pressures in the decades ahead.
The Treasury’s analysis showed that early action would reduce the overall cost of reform, make changes less disruptive, and result in higher per capita incomes and lower long-term tax rates.
“We don’t need to tackle 40 years of pressures in one fell swoop,” added Rennie.
“Starting earlier provides more opportunities to share transition costs across generations and avoid more disruptive change later. It allows us to signal changes well in advance, helping New Zealanders plan and adjust. Returning to surplus is an important first step.”
The Statement outlined a range of policy options, including adjustments to NZS eligibility and indexation, changes to tax settings, and improvements in public asset management. It emphasises that no single tool will be sufficient and Governments will need a portfolio of responses over time.




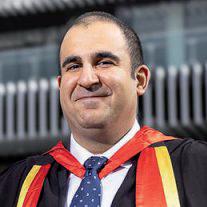
As the healthcare sector continues to adopt new technologies, research front the University of Auckland has suggested artificial intelligence may be the key to unlocking future potential.
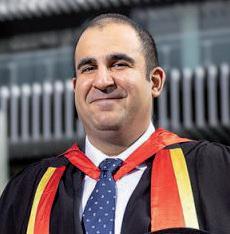
Dr Abtin Maghsoodi Associate Director & Lead Data Scientist, KPMG
r Abtin Maghsoodi is at the forefront of using artificial intelligence to solve complex problems in healthcare, and further afield.
Dr Maghsoodi, who crossed the stage to receive his PhD from the University of Auckland Business School in September, is at the forefront of utilising artificial intelligence to solve complex problems in the healthcare industry, and further afield.
The inspiration for his thesis, which he started in 2021, was very personal. At the time, Abtin’s late grandmother was living with Alzheimer’s, and he saw how challenging it was for her to navigate the healthcare system.
“That experience stayed with me and made me want to work on something that could improve care for older patients,” said Maghsoodi.
Older people often face complex health
issues such as multiple chronic conditions, which make their time in hospital particularly challenging, added Maghsoodi, who created an intelligent tool called REACH (Recognising Episodes of Acute Complexity in Health).
REACH uses machine learning to help hospitals identify complex patients in real-time and prioritise their care. It’s being considered for rollout across the Midlands region (Te Manawa Taki) of Health New Zealand.
Maghsoodi’s second programme, REACH 2.0, is also now being considered for wider implementation.
“This next version doesn’t just classify patients into complex and non-complex; it incorporates early supported discharge, aged residential care placement, and even mortality risk into the prioritisation process,” he said.
“Imagine a busy hospital ward where staff know in advance which older patients need more attention, and which can safely follow a standard pathway. That’s what my models do: they classify patients into complex and non-complex groups and predict who might be at risk of coming back to the hospital soon after discharge.”
He said this would mean hospitals can prioritise care, reduce delays, and prevent unnecessary readmissions.
In his second year of PhD studies, Abtin stepped into the role of lead data scientist at Health New Zealand, Te Whatu Ora. He says balancing doctoral studies with a leadership role in the health sector was intense, but it gave him a unique perspective on how research can directly influence real-world outcomes.
Maghsoodi said that the future of AI, not just specifically in Healthcare, will require clear governance, ethical frameworks and transparency.
He said that his PhD has taught him how to approach complex problems that are innovative and practical, and that this experience has given him a unique edge in his current role as an associate director and lead data scientist at KPMG, where he has continued to work on state-of-the-art AI projects across a range of industries.
“Imagine a network of AI agents managing hospital operations, supply chains, and customer service simultaneously, while learning and adapting in real time.”
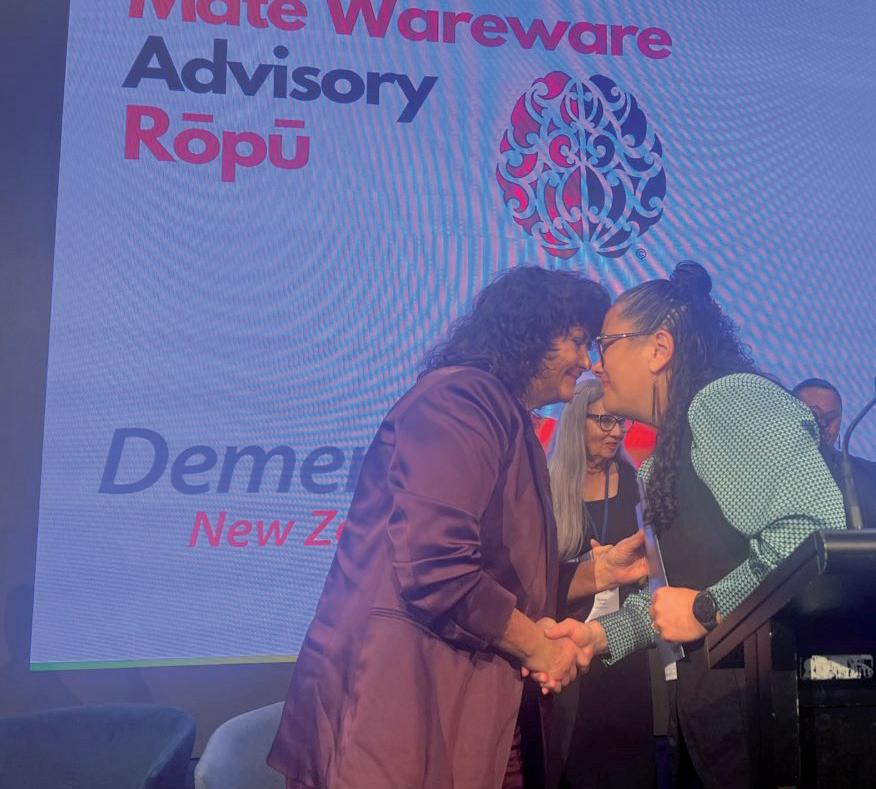
Alarming new research shows dementia is now affecting three New Zealanders every hour, around 500 people every week, according to Alzheimers NZ.
he University of Auckland data, commissioned by Alzheimers NZ, was released to mark World Alzheimer’s Month. Alzheimers NZ Chief Executive Catherine Hall said it has painted a stark picture.
It found that one in four New Zealanders will die with dementia, and that nearly 170,000 New Zealanders will live with dementia by 2050. The study also predicted that the annual costs of dementia care willl top NZD 10 billion, which is double of what it is today. Rates will climb the fastest among Māori, Pacific and Asian communities.
“Dementia is not a problem for the future. It’s one of the greatest health challenges

New Zealand faces now,” said Hall.
“If we don’t act urgently, it risks overwhelming our health and aged care systems, and the impact on families, communities, and the economy will be enormous.”
To confront the crisis, the kaitiaki group (Alzheimers NZ, Dementia NZ, NZ Dementia Foundation and Te Mate Wareware Advisory Rōpū), released the refreshed Dementia Mate Wareware Action Plan 2026-2031.
Presented to Minister of Seniors and Associate Health Minister Casey Costello, the refreshed Dementia Mate Wareware Action Plan set out five immediate priority areas in order to address the extreme
Dementia is not a problem for the future. It’s one of the greatest health challenges New Zealand faces now.
challenges that dementia presents over the coming years.
It outlined that taking action to promote brain health in a bid to reduce dementia prevalence was a key focus, as well as ensuring timely and accurate diagnosis and comprehensive management planning for people living with dementia.
Improving community dementia support services, better supporting both the formal and informal dementia workforces, and providing more effective governance for and within the dementia sectors were the report’s other areas of priority.
The first Dementia Mate Wareware Action Plan, published in 2020, was designed as a Government blueprint for action. The then Labour Government endorsed the Plan and provided some limited funding in 2022 to support pilot projects, but no further action or funding has followed. The work of the first Plan is not complete, so this refreshed Action Plan continues the work.
Alzheimers NZ has also called on the Government to fairly fund the country’s 17 chronically under-funded dementia services, and create a national older persons’ health and aged care strategy, which it said should be built on an integrated continuum of care.
“New Zealand faces a massive demographic shift in the next 20 years, and with it will come a huge number of new dementia cases, potentially overwhelming the health system and creating a major fiscal burden, unless we act now,” said Hall.
“Decisive action is needed, and the Government must step up with funding and policies to support Kiwis living with dementia.”

As an Event Coordinator, Eileen Verona said a highlight of her role is being able to bring connection, joy and unforgettable moments to life, one event at a time.

Eileen Verona Event Coordinator
er role is to plan and run events, activities and social moments that bring the community at Greenwich Gardens Village in North Auckland.
Whether it’s organising guest speakers, themed dinners, discussion groups, or exercise classes like Zumba, Verona’s goal is always the same; to give residents something to look forward to and an opportunity to create meaningful connections.
“One re sident once told me, ‘Without your events, my weeks would blur together’. That stuck with me,” she said.

One resident once told me, ‘Without your events, my weeks would blur together’. That stuck with me.
Some stand-out moments have included the French-themed dinner during the Tour de France, which was one of her first big events. The event included live accordion music, a French buffet, and decorations everywhere.
“I was nervous, but by the end, everyone was up, cheering and singing. It was a dressup night, and one resident wore a string of onions around their neck. I was confused, then realised, he’s a French onion soup!”
“Afterwards, I received a handwritten card saying it felt just like the old times before COVID. So much fun and laughter, thank you for bringing it back. That meant everything.”
Residents inspire the events. Verona said their suggestions and their passions write the script for her to work with. She said that was how Zumba started, and it has now become a weekly highlight.
Verona also launched a support group for those feeling isolated, and even paired
residents together as phone buddies, and now many visit each other regularly.
She said the team at Greenwich Gardens Village are incredible, and described them as her second family.
“We look out for each other, always ready to lend a hand, and there’s a genuine sense of care. That support gives me the confidence to try new ideas, knowing my team have my back.”
Her secret trick is to listen from the heart. She said she genuinely listen to residents, then mix in some creativity and organisation, which results in magical events.
If she had a superpower, Verona said she would clone herself in order to be everywhere at once on market days or big events.
With newarly 400 residents at Greenwich Gardens, Verona said there is always someone to talk to, and that is her favourite part.

Pāpāmoa Beach Village, a Metlifecare village situated in Tauranga, has been announced as a finalist in the Gilmours Excellence in Food Service Award at the EBOS | ACA Excellence in Care Awards in October 2025.

Stephen Barry Food Service Manager, Pāpāmoa Beach Village Metlifecare, Tauranga
etlifecare said this recognition reflects the incredible work of its talented kitchen team, led by Food Service Manager Stephen Barry, who has an illustrious wealth of over 40 years of experience crafting seasonally inspired, culturally inclusive, and nutritionally balanced meals for residents.
From five-week rotating menus and texturemodified options for residents with specific needs to Māori and Pasifika dishes and a focus on minimising food waste, the Pāpāmoa Beach Village Kitchen team ensures dining is a highlight of village life.
“We believe Pāpāmoa Beach Village sets the standard in food service in aged care, backed by MPI certification, regular audits, and positive

resident feedback.”
Barry said there is a real sense of community spirit within the village.
“It is like working at a holiday resort, with something different happening daily. From special events and dinners to cooking classes and happy hours.”
Barry said he considers the customer the most essential person in the kitchen.
“They all have different wants and needs, whether you’re in fast food, fine dining or aged care. As a chef, you are there to ensure the food is cooked correctly, presented well, and your customer is happy and enjoys their experience.”
Throughout his career, Barry has won several accolades for his work. He became a New


Zealand Beef + Lamb Platinum Ambassador and the national winner of the Monteith’s Beer and Wild Food Challenge. Barry mentioned that entering various cooking competitions challenges chefs to be creative and gives customers a chance to be adventurous with food.
When it comes to beginners in the current industry, he said that they need to have the passion to last. He noted that many young chefs have a dramatised idea of the industry from what they see on television and in movies, and although a demanding role, he wouldn’t change it for the world. The thrill and adrenaline rush during service and how work colleagues become a second family make it all worthwhile.