












ementia continues to shape the reality of aged care in New Zealand. Recently, the terminology used to describe dementia has shifted. Internationally, the condition is now often referred to under the broader term “cognitive impairment syndrome.” This change reflects an effort to reduce stigma and provide a more clinical, descriptive label. While “dementia” remains widely used and understood, the new name is gaining traction in medical circles, particularly as research reveals the diverse causes and manifestations of cognitive decline.
For those working in aged care, the renaming is more than a semantic shift. It highlights the growing understanding that cognitive disorders in older adults are complex, not always fitting into a single definition. Conditions such as Alzheimer’s disease, vascular dementia, and Lewy body dementia all fall under the broader umbrella of major neurocognitive disorders, reinforcing that no two cases are the same. This recognition is influencing how care plans are developed, ensuring greater emphasis on individual needs, abilities, and progression patterns.
One of the significant challenges linked with dementia is incontinence. As cognitive function deteriorates, residents are often less able to recognise or communicate toileting needs, leading to accidents that can cause distress for both the individual and their caregivers. Incontinence in this context is not simply a physical condition but also a behavioural and emotional one, requiring careful management and understanding.
The intersection of dementia and incontinence underscores the need for integrated care approaches. Successful strategies are multidisciplinary, involving medical professionals, nurses, carers, and families. Tailored routines, adaptive equipment, and discreet products can all reduce the impact, but just as important is the emphasis on dignity. The stigma surrounding both dementia and incontinence can be as damaging as the conditions themselves, reinforcing the importance of open discussion and proactive planning.
Advances in continence care products have provided new options for residents and caregivers alike. Discreet pads, wearable protection, and even sensor-based technologies allow for more personalised and effective management. Training for staff now stresses not just clinical response but empathetic care, recognising that incontinence linked with dementia is a sensitive issue that can deeply affect quality of life.
As aged care providers look ahead, the key message is clear: addressing dementia and incontinence together, with the right language, tools, and compassion, is essential. By doing so, the sector can provide care that preserves both health and emotional wellbeing in an ageing population.
Tania Walters, Publisher tania@reviewmags.com
PUBLISHER: Tania Walters
GENERAL MANAGER: Kieran Mitchell
EDITORIAL DIRECTOR: Sarah Mitchell
EDITOR-IN-CHIEF: Caitlan Mitchell
EDITORIAL ASSOCIATES: Sam Francks, Jenelle Sequeira
ADVERTISING SALES: Caroline Boe
SENIOR DESIGNER: Raymund Sarmiento
GRAPHIC DESIGNER: Raymund Santos
Retail 6, Heards Bldg, 2 Ruskin St, Parnell, Auckland New Zealand P: +64 3040142 Email: edit@reviewmags.com

9 Proud to be a Chef 2026 Australia’s leading culinary mentorship program is back: Proud to be a Chef.
10 Old, Not Weak: Strength-based Falls Prevention in Aged Care
Falls are the leading cause of injuryrelated hospitalisations for older New Zealanders.
12 Building on a Remarkable Legacy
The incredible legacy of one of New Zealand’s finest military leaders and strategists, Sir Keith Park, was heralded with a fantastic Warbirds flyover above the Ryman Healthcare village named after him.
New research carried out by care homes meal provider Apetito has revealed that over half of care homes in the UK find it difficult to provide specialist catering to residents living with dysphagia with adequate nutrition, a challenge still unresolved across the sector two years on.
Suitable training has helped SouthAustralian care home Resthaven Marion increase its kitchen efficiency and improve nutrition to better serve residents.
Daily consumption of two serves of ordinary skim milk (ORD) or A1 protein-free skim milk (A1PF) over three months was beneficial to a broad range of cognitive measures.




22 Combatting Nutritious Food & Loneliness
Michele Buxton moved into the aged care sector after looking into aged care homes for her mother.
24 Removing the Stigma
New research from Chinese Studies PhD student, Zihan He, has resulted in a new Chinese-language term for the word ‘dementia’, one that reduces stigma and shame for Chinese speakers. 26 Skilled Care at the Heart of Aged Care
Every day across New Zealand, thousands of healthcare assistants and nurses quietly carry out some of the most skilled, demanding, and compassionate work in our health system.


28 Pushing for Public Awareness
Over 7.2 million Australians are affected each year by incontinence, impacting their daily lives, emotional well-being and social participation.
30 The realities of retirement Village Economics
Independent analysis challenges perceptions of quick profits in the sector
32 An Environmental Focus
In a first for a New Zealand agedcare facility, Pacific Coast Village in Pāpāmoa is trialling an innovative way to reduce the amount of incontinence products it sends to landfill.
34 Dealing with the Issue
Many older people with complex health conditions experience incontinence and other bladder and bowel symptoms.
STIG has reported strong financial results, enabling a seven percent per annum distribution to investors, while entering into a new loan facility.
Senior Trust Retirement Village Income Generator Limited (STIG) has released its Annual Report for the year ended 31 March 2025, reporting a profit of NZD 12.7 million. This enabled gross distributions of NZD 12.57 million to investors, representing a seven per cent pre-tax annual return.
The company’s audited results also report all bank debt repaid during the year, NZD 11 million held in cash reserves at balance date, and equity increasing to NZD 198 million. Read more online
Aged care charities from around the UK have signed a joint statement encouraging more input from seniors in research that directly affects older generations.
NIHR has signed a joint statement alongside other major UK research-funders, committing to greater inclusion of older adults in health and care research. This builds on its announcement in November 2024 that inclusion needs to be considered in all applications for its funding. Read more online

Bupa New Zealand is rolling out a digital tool to help aged care employees consistently identify and respond to early signs of health deterioration in residents.
The tool is based on the Deterioration Early Warning System (DEWS), which was trialled at Bupa’s Northhaven Care Home during a feasibility study conducted in partnership with the Te Tāhū Hauora Health Quality & Safety Commission and the University of Auckland. Read more online




A new social housing development has opened in Northcote, specifically designed to meet the need for affordable housing for seniors.
Auckland’s shortage of quality, affordable rental housing for older people has received a significant boost today with the opening of Haumaru Housing’s new Greenslade Court apartment complex in Northcote, a purpose-built development offering warm, dry homes for seniors in the heart of a revitalised community. Read more online

Canberra politicians and the Australian College of Nurse Practitioners will strengthen the aged care workforce and careers.
The Australian Government is backing its dedicated aged care workforce across Australia, investing AUD 21.5 million in scholarships to help aged care workers and nurses progress in their careers.
Workers in aged care deliver the very best care for loved ones. The government said it wants those working in the sector to have long, fulfilling careers providing the love and care that older Australians deserve. Read more online

A review of New Zealand's aged care system has been welcomed by Alzheimer's NZ CEO Catherine Hall.
Alzheimer's NZ has welcomed the update from Health NZ on what it described as the long overdue review of Aotearoa New Zealand’s aged care system, as well as two related industryfocused reports.
Chief Executive Catherine Hall said the reports have reinforced the size and scale of the challenges currently facing the health sector as a result of our rapidly growing ageing population. Read more online
Australia’s leading culinary mentorship program is back: Proud to be a Chef. Applications for the 2026 program opened on 4th August 2025, offering 32 apprentice and trainee chefs a once-in-a-lifetime opportunity to step up to the plate and learn from the industry’s best and brightest stars. This year, applicants from Aotearoa, New Zealand, are invited to join in the fun for the first time in a decade.
Proud to be a Chef isn’t an experience that up-andcoming chefs usually get to have in the early stages of their career. Selected finalists from Australia and Aotearoa will fly all expenses paid to Melbourne, spending four days immersing themselves in masterclasses with world-class mentors, and getting key opportunities to network within their chosen industry. The final day is an adrenaline-packed cookoff, culminating in a chance to win a coveted $10,000 International Culinary Scholarship.
Alongside Resident Mentor, Mark Normoyle, 2026 mentors Sarah Todd and Gareth Whitton are chomping at the bit to meet the 32 lucky finalists.
“Proud to be a Chef has positively impacted hundreds of young chefs around Australia over its 25-year history and it’s exciting to be able to open the program to New Zealand entrants again,” said Vic Landells, Foodservice Director at Fonterra Oceania.
“Now in its 26th year, the program continues to shape future industry leaders by connecting emerging talent with world-class chefs and life-
changing opportunities, providing them with the guidance they need to succeed.”
Proud to be a Chef Resident Mentor and Fonterra Oceania’s Executive Chef, Mark Normoyle, is looking forward to returning for his seventh year.
“This program isn’t just about cooking, it’s about character, curiosity and community. We’re looking for chefs who soak up knowledge, ask smart questions and lift others around them.”
Renown chefs from around Aotearoa have already come out in support, urging apprentice and trainee chefs to apply for the 2026 program to sharpen their skills.
Applications are open until 19 October 2025, giving Australian and Kiwi rising culinary stars plenty of time to perfect their applications. For more information and to apply, visit www.proudtobeachef.com

Summerset Retirement Villages has partnered with Mode Technology to introduce the largest fleet of commercial cleaning robots in the Asia-Pacific sector.
Mode Technology said it was incredibly proud to have developed a strong working relationship with Summerset Retirement Villages that has resulted in the successful deployment of the largest fleet of commercial cleaning robots into retirement villages across the Asia-Pacific region.
In New Zealand, Mode Technology successfully secured the contract and managed the full nationwide deployment of autonomous cleaning robots within the retirement living sector, marking the largest robotic

fleet implementation of its kind in the country’s history.
These robots use advanced sensors and artificial intelligence to navigate complex spaces with precision, setting a new benchmark for hygiene, safety, and efficiency while relieving staff of labour-intensive floor cleaning tasks.
"We are proud to have secured this contract and to have managed the full deployment, with SIMPPLE acting as the distributor to get the robots from the manufacturer to us,” said Dallas Vincent, Director at Mode Technology.
“This rollout clearly demonstrates how cleaning robots are transforming retirement living environments, supporting staff with labour-intensive cleaning, improving hygiene, and enhancing the experience for residents.”
Jessica Haines, General Manager at Mode Technology and Project Director/Client Lead on the initiative, said that leading this project from initial planning through to full nationwide deployment has been incredibly rewarding.
“The collaboration with Summerset and our team’s ability to deliver a seamless implementation demonstrates the impact of robotics in transforming everyday operations for retirement communities.”
Falls are the leading cause of injury-related hospitalisations for older New Zealanders. But for Mairead Woods (NZRP), preventing falls is about more than safety. It’s about preserving independence, confidence, and quality of life.

airead and the team at Physiotherapy Works provide innovative, evidencebased physiotherapy services in residential care facilities and in the community. She works onsite at an Auckland aged care facility where she uses HUR exercise equipment as part of her physiotherapy programme. She holds a Bachelor of Health Science from AUT and is passionate about the importance of exercise in managing and preventing health conditions.
“Falls can be life changing for older adults,” says Mairead. “We know they’re the leading cause of injuryrelated hospitalisations in NZ and unfortunately the sequela of health issues can lead to a loss of independence, confidence, function, and even mortality.”
It affects care staff too. “There is added emotional strain due to a sense of responsibility for their
residents, and a disruption to routines due to increased falls prevention requirements.”
That’s why her approach is proactive and strength based. “It is not just about safety. It’s about preserving dignity, independence, and quality of life.”
Muscle strength, especially in the fast-twitch type IIb fibres (muscle fibres that contract and relax quickly), plays a vital role in balance and fall recovery. “We require our fast twitch muscle fibres to work well for sufficiently fast and powerful reactions when we lose our balance,” Mairead explains. “Muscle strength also contributes to faster gait and postural control.”
At her facility, residents who engage in regular strength and balance training see clear improvements. “They’re able to perform their activities of daily living
with more independence and are more likely to be safer when out in the community or visiting family and friends,” she says. “We measure changes in gait speed, lower limb muscle strength, and reaction time. I’ve seen impressive results for clients well into their nineties.”
The facility uses HUR resistance training equipment, developed with seniors in mind. The HUR equipment is purpose-built for older adults, making it easier and safer to prescribe resistance training at every stage of ageing and recovery. For Mairead, the benefit is both physical and psychological.
“The equipment is comfortable and doesn’t look too intimidating. This can be helpful for a client who, at least initially, doesn’t have much confidence or control over their movement.”
She adds that the pneumatic system allows for fine-tuned control. “Using compressed air and very fine-tuned loading increments, we can manage their strength work with excellent control and gentle progression. The movement is not harsh or jerky, which is great for joint-related pain.”
For residents, seeing their own improvement during a session is often a strong motivator.
“Clients love seeing their personalised programme on the screen and tracking their progress through their
session,” says Mairead. “I can also take them through their progress with reports on usage, loading, strength gains, and areas for improvement. It’s a great tool for linking their rehabilitation to their goals.”
Some residents have made life-changing gains.
“There are a number of clients who have experienced rapid carryover to improved function, even sufficiently for them to return to living independently when this was in question upon discharge from hospital.”
“Any facility that invests in maintaining or improving their residents’ strength and balance will see a return in resident satisfaction and function.”
“We work by the mantra ‘old not weak’. Improving strength and balance has extensive benefits for older adults’ health, far beyond the physical domain. Physiotherapy expertise is important in managing complex health conditions in a rehabilitation context, however there are very few reasons not to attempt resistance training.”
“I see a huge sense of satisfaction and self-efficacy improvements from my clients when they see their strength and balance improve”, she says. “Having the right equipment, expert input, and a safe setup is the perfect environment to achieve this. Your loved ones will be happier, feel capable and live better.”


The incredible legacy of one of New Zealand’s finest military leaders and strategists, Sir Keith Park, was heralded with a fantastic Warbirds flyover above the Ryman Healthcare village named after him.



early 250 residents and guests gathered outside the village centre to watch the flyover, consisting of three vintage Harvards, which kicked off celebrations to mark the official opening of the Hobsonville village.
As well as marking the incredible milestone of the village’s development, it was a chance to recognise three significant anniversaries of Sir Keith Park’s life: 2025 marked 50 years since his passing in 1975, 80 years since the end of WWII, and 85 years since the Battle of Britain, in which he played a significant part.
A hero of both World Wars, Sir Keith Park was best known for his leadership during the Royal Air Force’s air defence of London
and south-east England, prompting the head of the RAF, Lord Tedder, to comment after the war.
“If ever any one man won the Battle of Britain, he did. I don’t believe it is realised how much that one man, with his leadership, his calm judgement and his skill, did to save not only this country, but the world,” said Lord Tedder.
Joining the many residents with Air Force connections to the former RNZAF base Hobsonville and neighbouring Whenuapai were members of the Park family, including Sir Keith’s great nephews Brian and Stephen Park. Along with them, there was the CEO of the Sir Keith Park Airfield Trust in Thames, Geoff Furkert, and RNZAF Flight Sergeant Nathan Hodges, whose Continued on page 14.

Continued from page 13.
mother, Jenny, also ex-RNZAF, resides at the village.
Proving how interconnected the community is, village resident and former RNZAF Sergeant Neil Harris shared an incredible direct link to history, having been one of the six pallbearers who carried Sir Keith Park at his funeral 50 years ago.
Ryman’s Chief Operating Officer, Marsha Cadman, said Sir Keith Park’s legacy was truly inspiring.
“In order for us to leave a legacy as enduring as Sir Keith’s, we want to ensure that our purpose of enhancing the freedom, connection and wellbeing for people as we grow older remains our true focus and at the heart of every decision we make,” said Cadman.
“This beautiful village is a testament to the enormous amount of work and commitment put in by Ryman team

members and our partner organisations and to our residents who have created such a fantastic community.”
Keith Park Village Manager Kim Dawson spoke of the pride she felt to be leading the team in her home suburb of Hobsonville, having visualised herself in the role when the development was first announced.
With her parents, Brian and Zoelien, now residents in the village too, it made Ryman’s philosophy one that literally rang true.
“It meant I could genuinely say, hand on heart, that what we do is good enough for mum and dad. Because it truly is,” she said.
Massey University lecturer Dr Adam Claasen described the village as ‘a monument’ and ‘a living, breathing entity that would celebrate Sir Keith Park’s legacy for the next 100 years’. He gave a gripping and powerful telling of Sir Keith’s story that left many feeling emotional.
“I put it to you, ladies and gentlemen, gathered here today in this fantastic facility named after Saint Park, that no single New Zealander, in uniform, had more of an impact on the course of the Second World War and of the 20th century in Europe than, of course, the New Zealander Keith Park,” he said with a joking reference to Kim’s accidental description of Sir Park as Saint Park.
Brian Park described his first impressions as a 12-year-old of his great uncle, that of a very tall, distinguished man with white hair and a moustache who allowed him to win any bout of one-upmanship with his friends.
“Well, I had them all beat! My uncle was Air Chief Marshall!” he said.
“His achievements as a soldier, an aviator, a wartime fighter pilot and a commander of distinction, and a man who in civilian life contributed significantly to the community, the city of Auckland, business to charitable organisations, particularly those with special needs, his Anglican faith and a very keen yachtsman. These days, Keith Park is rightfully rated as one of the top 10 New Zealanders.”
Brian Park also acknowledged the financial contribution Ryman has made each year to entities that reflect the values and interests of Keith Park, namely aviation and those with special needs. These include MOTAT, Sir Keith Park School in Māngere, and Sir Keith Park Airfield Trust.
Construction of the village on Scott Road in Hobsonville began in 2019, with five of the nine apartment buildings and the main


village centre completed so far.
The care centre, consisting of rest home, hospital and dementia care options, was one of the fastest-filling in Ryman’s history, with amazing views from the higher levels. Since moving into the communal spaces last year, residents now enjoy a range of amenities including an indoor swimming pool, spa, gymnasium, hair and beauty salons, cafe, movie theatre, library, bar and billiards room.
now locally available from our NZ Warehouse

Sterri-Matt® PPE Stations & Dispensers are the ultimate IPC solution with over a 100 versatile combinations to enhance your infection control programs

we also offer a wide range of Quad Glove Dispensers for added convenience & accessibility are also now available!








New research carried out by care homes meal provider Apetito has revealed that over half of care homes in the UK find it difficult to provide specialist catering to residents living with dysphagia with adequate nutrition, a challenge still unresolved across the sector two years on.
uilding on the insights from the ‘Nourishing Lives: A New Era of Care Home Dining’ Report released by the partners in early 2024, this new study has aimed to examine how the sector’s key challenges have evolved over the past two years and to identify how the market has changed and any emerging trends.
“It is clear from this data on specialist catering in care homes that there are still grave concerns and challenges across the sector, two years on. We understand the complexities involved in meeting individual resident needs with texture-modified meals that are both safe and nutritious, whilst simultaneously providing a full regular menu
for others. And this is only exacerbated by the increasing economic pressures on labour and services,” said Richard Woodward, General Manager at apetito and Wiltshire Farm Foods Professional.
“However, the consequences of getting this wrong are severe. Rising numbers of care homes are struggling to meet IDDSI guidelines when preparing meals, and with a high proportion finding it difficult to provide appropriate nutrition, the findings signal a concerning trend in the world of care catering. Our message to homes is that Wiltshire Farm Foods Professional service can support you by providing an easy-tocook, nutritious and safe solution that works in harmony with kitchen teams cooking from scratch. Our extensive range of pre-prepared options is all made in line with IDDSI guidance and with expert Dietetic input, providing peace of mind for staff, residents and their families.”
Professor Martin Green OBE, Chief Executive of Care England, also added a comment on the research findings.
“This important research, which has been done by Care England and apetito, underlines the importance of good nutrition for people living with complex health conditions in care homes. This report clearly identifies the challenges but also offers some clear and tangible ways in which care providers can get specialist advice, and through working with apetito, can ensure that people receive the nutrition that they need for a good life”.

Suitable training has helped South-Australian care home Resthaven Marion increase its kitchen efficiency and improve nutrition to better serve residents.
elly Parini oversees food services at Resthaven Marion, a 159-bed aged care home in Adelaide.
She started working in aged care after caring for her father, who is now a resident.
"The best thing about working in aged care is being able to improve the environment people live in. Interacting with residents is important. It’s one of the things I love about my job," Parini said.
The department has partnered with the Maggie Beer Foundation to deliver free training to aged care staff. The foundation’s Trainer Mentor Program includes a menu appraisal and coaching from a qualified chef trainer to improve residents’ food experience. Staff also have access to the online learning modules to stay up to date on aged care nutrition and dining best practice.
"We thought it would be a good idea because we’re always looking to learn, develop and improve. It’s good for residents and staff," Parini said.
Going into the training, Parini was confident that the food was of a high standard.
"We weren’t perfect, but I think we were moving in the right direction. There are always improvements to make. You always need to be pushing and developing," Parini said.
The Trainer Mentor Program approach is tailored to each home’s kitchen operations, food quality and residents’ dining
experience. An initial assessment informs where the trainer should focus to achieve the greatest improvement.
To start, the trainer focused on making kitchen workflow more efficient and collaborative.
"We’ve looked at staff shifts and how they work in the kitchen. We moved shifts so the chef and assistant cook work together more, collaborate and get more cooking done," Parini said.
Resthaven will be incorporating learning from the program across all 12 of their residential sites. Aged care providers will need to meet a new dedicated food and nutrition Quality Standard from 1 November 2025 under the new Aged Care Act.
"The training has helped us move forward with a more natural approach to protein and nutrition fortification, which will help us meet the new standard," Parini said.
"We have incorporated the Maggie Beer mashed potato recipe, as well as their gravies and some soup recipes into our

menus. We are fortifying with protein using skim milk powder and lentils."
Under the new Quality Standard, providers need to work with older people to find out what they like to eat and drink. Resthaven Marion has existing processes to seek residents’ feedback.
All residents are encouraged to fill out menu feedback cards and share their thoughts when they see staff.
"We also ask for feedback about the food in the resident meetings every second month. And we have meal committee meetings with residents when our seasonal menus are renewed," Parini said.
"Staff and management buy lunches from the kitchen every day, so we eat the food alongside the residents."
Parini understands the importance of social interaction and how the dining experience can help with that. This is an area she wants to continue to improve.
"Going into the dining room and enjoying lunch or dinner can be a big part of every
The training has helped us move forward with a more natural approach to protein and nutrition fortification, which will help us meet the new standard,
individual’s day. It’s an opportunity for them to socialise," Parini said.
Currently, most residents enjoy breakfast in their rooms, but Parini is considering options to create a social morning dining experience.
"We’re going to trial a big buffet-style breakfast in the dining room. Over time, we’re hoping to get a majority of residents eating breakfast in the dining room."

A multi-centre, double-blinded, randomised controlled clinical study has found that daily consumption of two serves of ordinary skim milk (ORD) or A1 proteinfree skim milk (A1PF) over three months was beneficial to a broad range of cognitive measures in 88 milk-tolerant Chinese adults, aged 65 to 75 years with mild cognitive impairment (MCI).
Further, participants who consumed A1 protein-free milk showed a greater improvement in a range of cognitive measures and in their reported quality of life. Further research is warranted to confirm these benefits to other population demographics.
Building on previous research, the primary study objectives sought to examine whether ordinary milk containing the A1 protein, compared to A1 protein-free milk, could improve aspects of cognition measured by way of the Subtle Cognitive Impairment Test (SCIT), and investigate potential linkages with changes in serum levels of the antioxidant glutathione (GSH). Secondary objectives included additional cognitive function assessments, self-reported quality of life measures, muscle strength using the hand grip scale, inflammatory and immune markers, and vitamin D levels. Additional cognitive assessment was conducted by two widely accepted clinical tools, the Montreal Cognitive Assessment (MoCA) and the Audio Verbal Learning Test (AVLT).
A1 protein-free milk differs from
ordinary cows’ milk. Beta-casein makes up approximately 30 percent of the protein in cows’ milk. These beta-casein proteins can be grouped into two types, A1 and A2. Ordinary milk contains both A1 and A2type proteins, whereas A1 protein-free milk naturally only contains A2-type proteins. Though the A1 and A2-types are classified by reference to only a single amino acid in the sequence of 209 amino acids that make up the protein, this subtle difference has a material impact on its breakdown during digestion, as milk free from A1 protein may be easier on digestion for some people. Both milk groups demonstrated significant improvements across all three cognitive tests. However, no significant changes were observed in serum GSH levels or inflammatory markers, suggesting alternative mechanisms underpinning these benefits. Both groups had severe vitamin D deficiency at baseline, which is common in older people living in China. The authors speculated that enhanced vitamin D absorption may be involved, as both groups showed a significant increase in serum vitamin D levels from baseline. However, participants still had vitamin D levels below
recommended levels at the end of the study.
The research reported a 23 percent reduction in total error rate for the A1 protein-free group on the SCIT test, a significant finding and similar to the outcome for the ordinary milk group. However, the research reported earlier improvement amongst the A1 protein-free group for this measure.
Whilst both milk groups demonstrated improvements in all cognitive test scores, study participants in the A1 protein-free group achieved significantly better scores in secondary cognitive measures, the MoCA and AVLT cognitive tests. These tests measure cognitive domains such as executive function, memory, and attention. These findings underscore the potential of milk choice in shaping cognitive outcomes in vulnerable older adults with MCI. Other studies investigating the relationship between beta-casein type and cognitive outcomes reported stronger outcomes on aspects of cognition for A1 protein-free groups in milk-intolerant preschool children and adult populations. These studies hypothesised different mechanisms of action, so further research is needed to confirm the results and mechanisms.
With an ageing population, there is an increased need to embrace lifestyle changes that support cognitive health and quality of life.
In Australia, it is estimated that around 840,000 seniors, approximately 20 percent of those aged older than 65 years, may be living with MCI, a condition characterised by subtle changes to cognitive health that can affect quality of life. Cognitive health refers to the brain’s capacity to think, learn, remember, and perform everyday tasks that are essential for communication, decision-making, and social engagement. While symptoms are mild, MCI can influence quality of life, and for some people, it can progress to degenerative conditions such as Alzheimer's disease; however, progression is not inevitable. Lifestyle changes can influence the progression of MCI, including
adopting a balanced and nutritious diet.
Professor Stephen Robinson, researcher at RMIT University and corresponding author of the clinical study, said that the new data represent a promising step forward in understanding how nutrition can play a role in supporting and preserving cognition as we age.
“The most important finding from this study was that milk in general has benefits when consumed regularly by healthy older adults. While the group that received the A1PF milk showed a stronger effect in comparison to ordinary milk, we saw important overall effects of dairy milk on aspects of cognitive performance, reported quality of life and vitamin D levels,” said Professor Robinson.
“We hope that through further research into the regular consumption of dairy milk, which can be an easy addition to our daily diets, we will be able to better understand the longer-term health benefits.”
Dr Emma Beckett, food and nutrition scientist at FOODiQ, said A1PF milk, as part of a balanced diet, can play a valuable role in improving the nutrition of older adults.
“This is an exciting study because it shows that a small dietary change, adding A1PF milk, may be effective for those experiencing cognitive changes. As Australia’s population continues to age, A1PF milk may offer an accessible way to support overall health and wellbeing, particularly in adults living with MCI,” said Dr Beckett.
Dr Andrew Clarke, Chief Scientific Advisor at The a2 Milk Company, said that the latest research reflects that A1PF has the potential to benefit all life stages and could be a superior option to ordinary milk in some contexts.

“The outcome of this research is consistent with the hypothesis that A1PF milk may enhance the benefits contained in milk, notably with respect to cognitive function. Importantly, the study highlights the potential for improving aspects of health and quality of life for the elderly through nutritional as opposed to pharmaceutical solutions,” said Dr Clarke.

Michele Buxton moved into the aged care sector after looking into aged care homes for her mother.
uxton, the residential manager at BaptistCare Orana, said she just loves working in aged care.
“It’s so fulfilling and beautiful to be part of the residents’ lives every day.”
A long-term Maggie Beer fan and keen cook herself, Buxton didn’t think twice about signing BaptistCare Orana up to the Maggie Beer Foundation’s Trainer Mentor Program. The program pairs staff with a qualified chef trainer to improve residents’ food, nutrition and dining experience. The training also helps aged care homes prepare to meet a
new dedicated food and nutrition Aged Care Quality Standard under the new Aged Care Act.
“I had faith that the things she can teach our staff will be really valuable. It’s about providing our staff with the tools and knowledge to serve our residents,” said Buxton.
Buxton knows the difference food makes for quality of life and enjoyment. BaptistCare Orana has a diverse resident group with different preferences and needs.
‘We cater for all kinds of people. People with varying levels of ability. People with varying cognitive abilities. We have

Michele Buxton Residential Manager
BaptistCare Orana
veterans, First Nations residents, people from varying ethnic backgrounds, people living with dementia. We try and cater for all their needs,’ said Buxton.
“It is absolutely the residents’ home and we’re there for their benefit.”
Before applying for the training, Buxton was confident that they served delicious food. But nutritional fortification, presentation and the dining experience were things they wanted to improve on.
“Our focus is just to make the whole experience better. So, I was looking at food presentation because you can make food that’s absolutely tasty, but you eat with your eyes first, right?”
She said there has been training on how to present things, how to serve the meals.
“You don’t leave the main meal plates splayed on the table while the residents are having dessert. It’s just those niceties like that. Some of the things that we’d already started to introduce were really reinforced in the training.”
The training has also helped BaptistCare Orana maximise the nutrition of every meal.
‘There’s a lot of work about your protein needs, making sure we have enough protein in each meal. Making sure it’s really healthy for residents,’ said Buxton.

A big issue in aged care can be loneliness. Food plays an important part in providing residents with more lifestyle opportunities.
“I’ve been at Orana for two years now. When I first got there, I was really surprised about the number of residents who stay in their rooms, by choice. What we’ve focused the team on, for a couple of years now, was trying to look at that whole dining experience to encourage residents to come out of their room.”
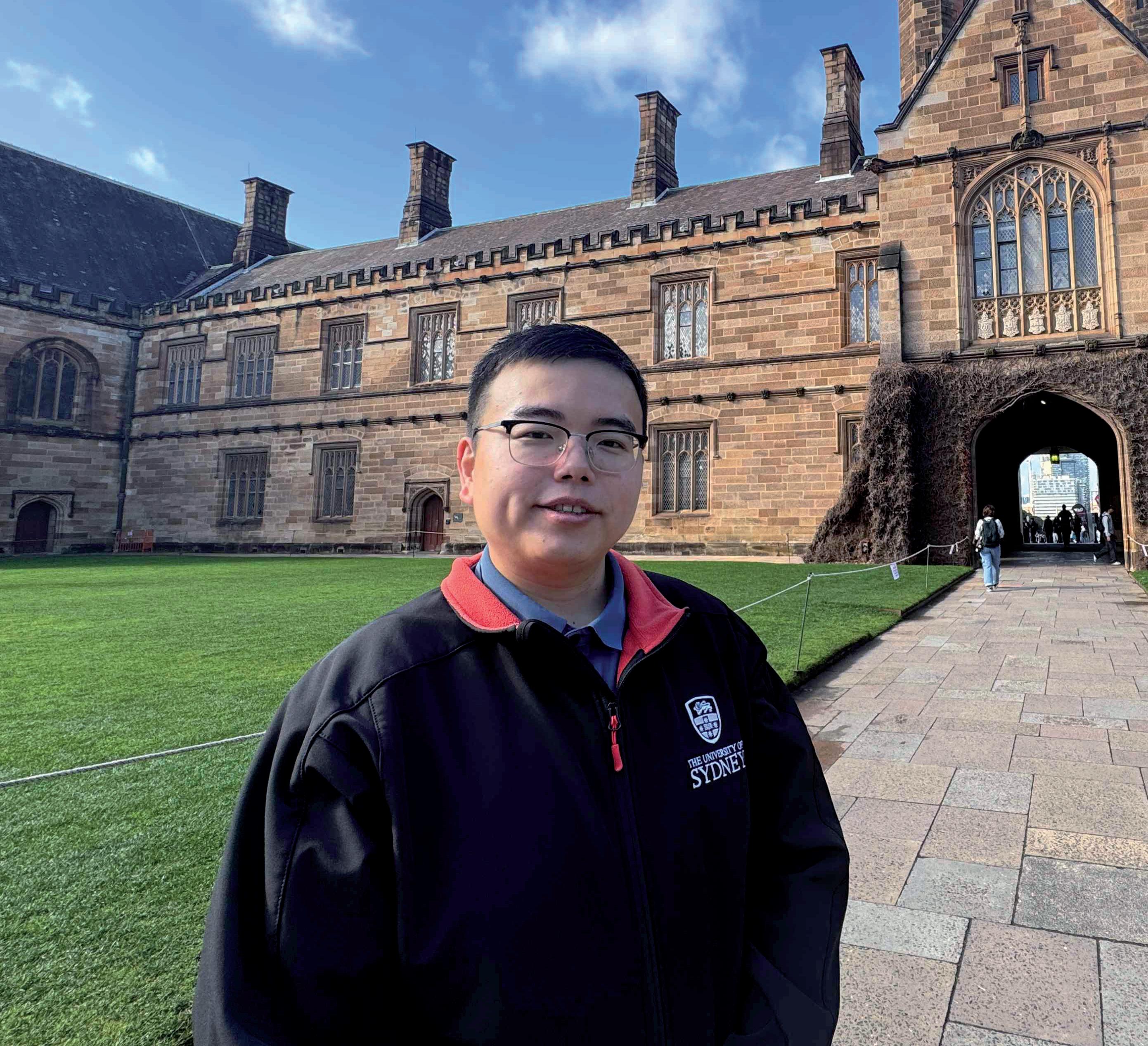
New research from Chinese Studies PhD student, Zihan He, has resulted in a new Chinese-language term for the word ‘dementia’, one that reduces stigma and shame for Chinese speakers.
he new term for dementia, “cognitive impairment syndrome” (认知障碍症), is hoped to be internationally recognised by speakers around the world.
The updated term replaces the outdated and stigmatising term “dummy disease” (痴呆症), which literally translates as “idiocy” or “stupidity”. It also replaces the medically inaccurate term “brain degeneration syndrome” (脑退化症), which covers a wider range of health conditions than dementia.
The new term “cognitive impairment

syndrome” (认知障碍症) offers a more neutral, scientifically accurate alternative that is expected to be adopted internationally.
“The term for dementia in Chinese translates to ‘stupidity,’ which is incredibly hurtful,” Zihan explained.
“Some Chinese families refuse to seek medical help because the terminology is so stigmatising. I hope the new term really makes a difference.”
Zihan, 28, is an international student from Mainland China. His motivation for the research is personal. A close relative showed signs of dementia but didn’t get
the treatment they needed due to the stigma around the language. Zihan wants to make a difference for other families.
“The stigma around dementia has been present in Chinese culture for a long time,” Zihan said.
“While Chinese Australians have access to Chinese dementia-related educational material, a lot of its language has literal translations,” he said.
“I’ve witnessed many Chinese-speaking people in Australia delay their first appointment with doctors because they did not want to face their health situations. I hope that the new translations can help destigmatise diseases in the community.”
Dementia Australia Executive Director Services, Advocacy & Research, Dr Kaele Stokes, said the decision is an important step in better connecting with and supporting Australia’s Chinese communities. There are 980,555 speakers of Mandarin and Cantonese in Australia, or four percent of the population.
“Adopting this preferred term is a reflection of our commitment to ensuring our services are culturally informed, respectful and responsive to the communities we support,” Dr Stokes said.
“We are listening to and learning from multicultural communities, and reviewing our services and resources to ensure our approach will be culturally aware and attuned to the nuances that matter most to them. We are also working to assess specific needs of Chinese communities so that our support, information and advocacy are as relevant, accessible and effective as possible.”
Every day across New Zealand, thousands of healthcare assistants and nurses quietly carry out some of the most skilled, demanding, and compassionate work in our health system: caring for older New Zealanders. Much of this care takes place in aged residential care (ARC) facilities, where more than 39,000 residents live - many with complex physical, cognitive, and mental health needs.

Tracey Martin Chief Executive Aged Care Association
hile often described simply as “care,” the reality is far more specialised. Staff in residential care facilities provide a combination of clinical support, personal care, and emotional reassurance. They monitor vital signs, administer medication, support safe mobility, prevent falls, maintain nutrition and hydration, and document every intervention to meet rigorous clinical standards. But for those working in dementia and psychogeriatric units, the demands rise even higher.
Dementia care requires patience,
adaptability, and a deep understanding of human behaviour. Residents may experience memory loss, confusion, or sudden changes in mood. Skilled caregivers learn to communicate in ways that reduce anxiety; through tone of voice, body language, and careful choice of words. They create structured routines to provide comfort, redirect agitation with calm reassurance, and use non-verbal cues to preserve dignity.
This is work that requires training and practice, but also empathy and emotional resilience. A single shift might involve helping a resident recognise their own reflection in the mirror, gently guiding someone back to their room when they feel lost, or supporting a family through the difficult process of seeing a loved one change. Each moment is both technically skilled and profoundly human.
Psychogeriatric care takes that complexity further. Residents often live with advanced dementia combined with mental health conditions, such as severe depression, anxiety, or psychosis. Here, care workers and nurses must manage not only memory loss and confusion, but also behaviours that can be unpredictable or challenging.
De-escalation techniques are critical. Staff are trained to anticipate triggers, defuse conflict before it escalates, and maintain safety for residents and others. They must make rapid assessments, balance compassion with firm boundaries, and draw on specialised strategies to calm

distress. In doing so, they protect both the resident’s wellbeing and the wider care community.
Caregiving has too often been minimised as “women’s work.” In reality, this is highly skilled professional practice that blends clinical precision, advanced communication, and deep emotional intelligence. It requires a workforce that is resilient, well-trained, and appropriately valued.
Healthcare assistants and nurses in dementia and psychogeriatric units are not just providing comfort - they are specialists managing some of the most complex conditions in our health system. Their work allows thousands of older New Zealanders to live with dignity and security, even in the most difficult stages of ageing.
With New Zealand’s ageing population, the demand for dementia and psychogeriatric care will only grow.
Ensuring that staff are recognised for their skill and supported in their roles is essential not just for workforce stability, but also for the wellbeing of every older person who depends on them.
When we talk about aged care, we must move beyond stereotypes of “basic” support. This is specialised healthcare delivered in people’s homes, which just happen to be a residential care facility, day after day, by professionals who balance compassion with competence. The skill involved deserves recognition equal to its value.
At the heart of it is a simple truth: caring for people with dementia and complex conditions is among the most challenging and important work in our health system. If we want to ensure dignity and quality of life for older New Zealanders, we must ensure that the people who provide that care are valued as the highly skilled professionals they are.
Over 7.2 million Australians are affected each year by incontinence, impacting their daily lives, emotional well-being and social participation, according to a nationwide survey commissioned by Continence Health Australia.
ocused on the health and social impact of incontinence across Australia, the survey revealed key issues for patients and carers.
Despite one in four people being affected by incontinence issues, 70 percent of the public lack basic awareness about incontinence issues. Females (69 percent) continue to be more than twice as likely as males (39 percent) to report incontinence-related issues, and one in three people experiencing incontinence has had it for over five years.
Fifty-seven percent of respondents said having incontinence limits their desire to socialise with others outside their house.
Jim Cooper, CEO of Continence Health Australia, said this data has underscored the urgent need for action.
“While the Commonwealth Government has been a trusted partner of Continence Health Australia for 38 years, there is still much work to be done to address incontinence in Australia,” said Cooper.
“Our 2025 survey highlights the scale of this silent epidemic of incontinence. It’s a challenge that requires strong, unified leadership.”
Incontinence-related issues currently cost the health system over AUD 100 billion annually in health and wellbeing impact, and Australia’s population is set to grow larger.
Dr. Jane Pittman, a registrar in obstetrics
and gynaecology, highlighted her personal experience and the importance of addressing the issue at the highest levels.
“We need to start talking openly about incontinence to encourage more people to seek help,” said Dr Pittman.
“Addressing incontinence requires comprehensive, national action, not just across health services, but through public awareness as well.”
Continence Health Australia has called for action on six key priority points it believes will transform incontinence care. These are to advocate for multidisciplinary clinics for holistic, person-centred care; drive better outcomes for NDIS participants; create a national dataset to understand the true impact of incontinence; normalise conversations about bowel and bladder health; upgrade public facilities, such as toilets, to be more accessible and inclusive; and host the inaugural summit on continence health in 2026.
"By working together, policymakers, healthcare providers, and communities, we can improve lives and significantly reduce the societal and economic burden of this condition," added Cooper.
One in three women and one in six men are impacted by incontinence issues. The majority of people affected by incontinence issues can be treated, but it is essential to educate staff and residents about incontinence awareness.


Independent analysis challenges perceptions of quick profits in the sector

Michelle Palmer Executive Director, RVA

he belief that retirement villages deliver large surpluses within just a few years is a persistent one, but new independent research shows the reality is far more complex and long-term.
Grant Thornton’s report, The Path to Profitability, examined 25 years of data from two very different operations: a rural Canterbury village and a high-density Auckland apartment complex. In both cases, it took more than two decades for the villages to break even and begin generating a return on the initial capital investment.
“This confirms what operators have long understood,” says Michelle Palmer, executive director of the Retirement Villages Association (RVA).
“Retirement villages require significant upfront capital, long timeframes, and a commitment to providing quality housing and services for older New Zealanders.”
The analysis tracks every stage of village development, from land acquisition and
construction through to achieving target occupancy and sustaining service delivery.
It also highlights the critical factors influencing long-term viability: unit pricing, build costs, resale cycles, and operating expenditure.
Pam Newlove, Retirement Village Services Lead at Grant Thornton, says that many external perceptions overlook the reality of ongoing costs.
“Weekly fees typically cover operational expenses, which are rising faster than fees can be adjusted.
“While initial sales provide an early injection of cash, inflows plateau after seven to ten years, while costs for maintenance, staffing, and refurbishments continue to climb.”
The findings have direct implications for the pending reforms to the Retirement Villages Act.
The RVA supports regulatory change that delivers clarity for residents and certainty for operators but is warning against measures that could unintentionally undermine the sector’s ability to develop and reinvest.
One example is mandatory buyback timeframes, says Palmer.
“In a slow housing market, prescribed repayment periods could hit smaller or regional operators hard, delay new developments, particularly those including hospital-level care, and increase costs for residents.
• Approximately 70 per cent of villages have already adopted best-practice measures, including:
• Ending weekly fees once a unit is vacated
• Re-licensing vacant units as quickly as possible
• Enhancing disclosure on transitions to care
• Supporting interest payments on outstanding capital after an agreed period
• Clarifying chattels, repairs, and maintenance responsibilities
“While financial sustainability is critical, the sector’s core focus remains on meeting the needs of the 53,000 older Kiwis living in retirement villages.
“Retirement villages remain a trusted and popular choice. The challenge, and the opportunity, is to keep delivering excellent resident experiences while maintaining the capacity to invest in future supply.”
The full Grant Thornton report is available at: www.grantthornton.co.nz/insights/the-pathto-profitability

In a first for a New Zealand aged-care facility, Pacific Coast Village in Pāpāmoa is trialling an innovative way to reduce the amount of incontinence products it sends to landfill.
acific Coast Village has replaced some of these products with reusable incontinence underwear for residents. The impact of disposable nappies on the environment is widely understood, but an even greater problem in New Zealand is the amount of disposable incontinence products ending up in its landfills.
Incontinence pads account for 34 percent of all waste Pacific Coast Village sends to landfill, more than 4000kg a year. A recent Australian study predicts adult incontinence waste will be four to 10 times greater than baby nappies by 2030,
due to an ageing population.
“We wanted to find a dignified solution to a delicate problem. Incontinence affects many people and can be accompanied by embarrassment and social isolation, so any solution to incontinence product waste has to put people’s physical and emotional welfare first,” said Erika Rans, Pacific Coast Village Operations Manager.
A number of residents are taking part, trialling a New Zealand-designed reusable underwear product, made from organic cotton, and designed to outperform disposable products in comfort and ease of use.
After the first month of the trial,
participants said they were highly satisfied with the product.
“Initial feedback from the trial has been very positive, and we're now exploring how this approach could be expanded across the wider Generus Living group,” said Rans.
“The outcomes and learnings from this case study will also help inform the broader aged care sector, which is following the trial with strong interest.”
The trial has been made possible by the support of Tauranga City Council’s Resource Wise Community Fund, which supports local organisations and businesses that have innovative solutions for reducing the amount of waste ending up in local landfills.
Tauranga City Council’s Sustainability and Waste Manager, Dan Smith, said the trial is a great example of the type of local initiative the Resource Wise Community Fund is designed to support.
“Pacific Coast’s project has the potential to have a huge impact on waste reduction,
not only in our city, but importantly nationwide,” Smith said.
Alongside the reusable incontinence underwear trial, Pacific Coast Village is implementing a broader waste reduction programme. This includes educational workshops and ongoing communication to encourage environmentally responsible practices among residents and staff, as well as a comprehensive review of waste systems within the care facility, with several new initiatives introduced as part of the project.
The fund is intended to remove monetary barriers for organisations and businesses keen to reduce waste and promote waste reduction in Tauranga. The Resource Wise Community Fund (NZD 100,000 annually for distribution) is sourced from the Waste Levy, provided to councils by the Ministry for the Environment for waste minimisation education, and does not impose additional costs on general rates.

EBOS is proud to offer the Attends range in continence care. Attends offers a trusted range of products designed to support consumers, caregivers, and healthcare professionals. Their portfolio includes solutions for all levels and types of incontinence, ensuring individuals can find products tailored to their specific needs and lifestyle. Talk to us now about how we can help you.





Many older people with complex health conditions experience incontinence and other bladder and bowel symptoms.

he burden of disease associated with bladder and bowel symptoms is high and likely to rise in our ageing population. The prevalence of bladder and bowel symptoms such as urinary incontinence, faecal incontinence, nocturia, constipation and an overactive bladder is high in older people, particularly in older people with complex care needs. This has important implications for aged care providers in terms of interventions and strategies to optimise the health and well-being of older people who access their services.
The National Aging Research Institute in Australia (NARI) has reviewed collected evidence for the Australian Commission on Safety and Quality in Health Care to inform a clinical care standard about continence care for older Australians accessing
aged care services in the community and in residential aged care homes. The researchers explored the question of what constitutes ‘best practice continence care’ and produced a set of recommendations for safe, quality continence care for older Australians with complex care needs.
Data from New Zealand indicates that 17.3 percent of home care consumers have faecal incontinence. This contrasts with up to 42.8 percent (range 10.5-78 percent) in residential aged care homes.
The recent Royal Commission into Aged Care Quality and Safety reported 274,409 instances of substandard care over five years, many of which they termed ‘compromises to an older person’s dignity’. Whilst the Commissioners did not define ‘dignity’, multiple transcripts point to continence care that does not match community expectations.
The report recommended that it was important to identify, document and communicate the senior’s incontinence care needs, values and preferences through a supported shared decision-making process. It is essential to consider the needs of care partners in planning future incontinence care, and to adopt evidence-informed clinical pathways, guidelines and models of care to guide incontinence care.
Ensuring village staff have the necessary skills to care for incontinence will help to manage individual cases properly and with dignity. Accessing advanced and specialist support avenues in order to provide quality and safety was also recommended where needed.
Implementing lifestyle interventions, such as therapy or increased medical assistance, can also have a profound impact in helping seniors manage the turn of events. Ensure that seniors also have the support of friends and family as well should that be needed.
The review also identified several gaps in evidence, particularly in relation to the prevalence, risks, impact and management of bladder and bowel conditions among older Australians receiving in-home aged care services. It also identified a lack of measures to evaluate the quality of continence care for people who receive aged care services in Australia. NARI suggested further consideration be given to the design and systematic use of quality indicators that are informed by older people and carers expectations, preferences and values.
Although rates of incontinence and other bladder and bowel symptoms are high in residential aged care homes, the vast majority of people with these problems live in the community, with or without support.


