Biologically based materials that leave no scar Bionic devices like cochlear implants and bionic eyes are currently made using relatively stiff metals that the body recognises as foreign, which limits the effectiveness of these devices when they are implanted. We spoke to Dr Rylie Green about the work of the Living Bionics project in developing new, softer materials that can be integrated into the body more effectively. The vast majority of bionic devices like cochlear implants, pacemakers and bionic eyes currently include metallic electrodes, with a non-conductive polymer as the insulating component. These types of devices are not naturally compatible with the tissue with which they interface when they are introduced into the body, as Dr Rylie Green explains. “When these devices are introduced, the body recognises them as foreign. It responds by essentially putting up a wall of scar tissue over time, to stop what it sees as a threat from causing damage to the rest of the body,” she outlines. This leads to the formation of a scar tissue capsule, which impedes communication between a bionic device and the rest of the body. “Where you want to be communicating very efficiently with the nerve cells within a system, instead you’re communicating through a big wall of scar tissue, to try and stimulate cells - or record from cells - that have moved further away from the interface,” says Dr Green.
Image credit: Dr Aaron Gilmour, postdoctoral researcher.
Living bionics project An alternative option is to use biologically based materials in a bionic device that the body will respond to in a more natural way, a topic central to the work of the Living Bionics project, an ERC-backed initiative based at Imperial College in London. As the project’s Principal Investigator, Dr Green is working to develop biomaterials that can be integrated with tissue without the formation of scar tissue. “We are trying to make biosynthetic materials that can essentially trick the body into thinking that they are natural,” she explains. This can be done in a variety of different ways; one of the simplest is to make something that is softer than the metals currently used. “Nervous tissue is very soft, somewhere in the region of very low kilopascals down to pascals in terms of stiffness. Whereas the metals usually used in electrodes are over the gigapascal range,” says Dr Green. “So there’s a huge difference in stiffness between the metals that are used conventionally, and the actual tissue in which they implant devices.”
10
The Bionic Man. © Control Publishing
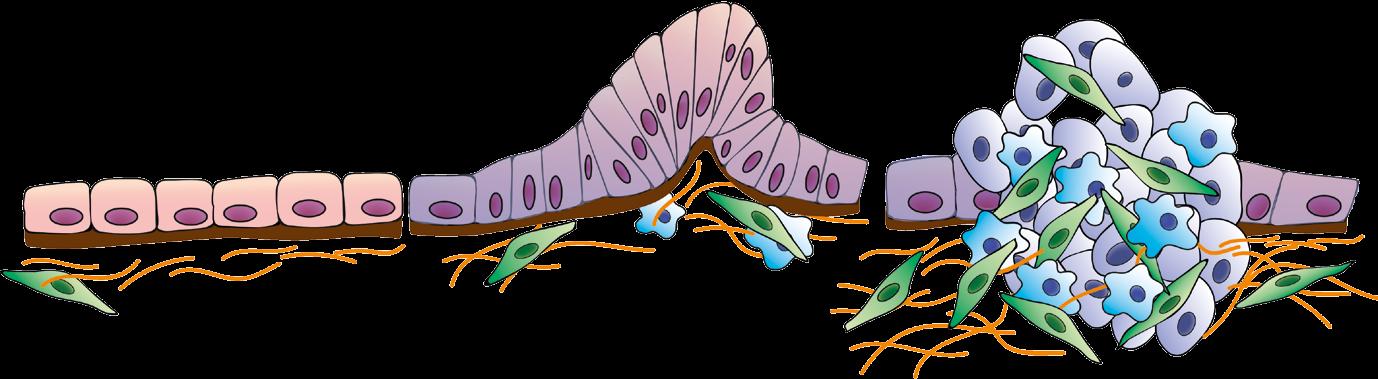
Image credit: Dr Ulises Aregueta-Robles.
A lot of energy in research has been devoted to essentially softening up that interface by using materials that are also in the kilopascals range, so that the neighbouring cells feel something soft when a device is introduced. While the body still recognises that a device has been
made with synthetic materials, the mechanical properties do not cause physical damage. “There is a better response at the interface,” stresses Dr Green. Biological elements that are normally present in the environment around the cells, such as protein-type components, can also be added to these materials, making them ‘biosynthetic’. “The body then starts to interact with these components, and we see some positive interactions,” says Dr Green. “However, when we implant these softer, more biological devices, the body can still recognise that they’re foreign in some respects. Critically, there is still implant damage when you actually introduce the device. In Living Bionics, we see this as a window of opportunity to create a better connection between the device and the surrounding tissue.” The aim here is to add in some stem cells or progenitor cells that will grow out from the device to interact with the tissue. By essentially pushing the stem cells down a particular developmental line, Dr Green hopes to ensure that they develop into neural cell networks that are more compatible with the local environment. “We provide, within the device, the ingredients the stem cells need to become neural cells that will then target the tissue that we’re looking to interface with,” she explains. However, stem cells do not always differentiate into neural cell networks, which is one of the major challenges facing the project. “No matter what cues you provide stem cells with, you never get 100 percent of one particular cell type. We’re working to develop not just one cell type, but a ratio of different cells that are present within the brain, to make functional neural tissue,” continues Dr Green. “We don’t just want nerve cells on their own, that’s not sufficient. We need to also think about their supporting cells.”
Cell networks Researchers have developed a method that enables the introduction of cells that have already been differentiated, called astrocytes. These act as support cells to the nerve cells, and form part of a wider network. “Nerve cells don’t contact each other and create a conduit on their own, they need these other
EU Research