February 2026

Way in Higher Retention, Elevated Care
February 2026







Chief Editor
Tani Johnson tj@carehomemagazine.co.uk
Publication Manager
James Davies james@carehomemagazine.co.uk Tel: 01795 509 112
Credit Facilities Manager
Gwen Lee creditcontrol@cimltd.co.uk Tel: 01795 509 103
Design and Production
James Taylor james@cimltd.co.uk
Grant Waters grant@cimltd.co.uk
Marketing Manager
Lucas Payne lucas@cimltd.co.uk
Head of Digital
Xhulio Bishtaja press@carehomemagazine.co.uk
Social Media Manager
Lily Lawson press@carehomemagazine.co.uk
Director
Tom Woollin tom@cimltd.co.uk
Managing Director
John Denning
If there is one conversation that never really leaves the care sector, it is staffing. But this month, rather than circling the familiar challenges, we look at what genuinely makes a difference: not in theory, but in practice.
Our feature on staff training begins with quality of care, not compliance. It explores what happens when learning is shaped around people and outcomes, rather than inspection frameworks. When staff understand the why behind their work, confidence grows, care improves, and compliance follows as a natural consequence rather than a primary driver.

That focus on people continues in our recruitment and retention feature, which takes a long view of the sector through the eyes of a Home Manager with 50 years’ experience in care. These insights are honest and grounded: how to keep good staff, how to recruit with integrity, and how the sector can do more to present itself as a career worth choosing. We also place a strong emphasis on students, placements and collaboration with universities, highlighting how partnerships can help build the next generation of care professionals.
Our cover story, from CPD, ties these themes together, making the case for training as an ongoing, confidence-building process rather than a tickbox exercise.
Additionally, the issue reflects the richness of everyday life in care. We visit KYN Bickley as our Care Home of the Month, where culture and workforce investment go hand in hand. Dishing Up celebrates the simple, heartwarming comfort of spaghetti meatballs, while Editor’s Day Out takes us to Herne Bay Manor, offering a reminder that good care is often found in thoughtful details.
The February issue emphasises that addressing the sector’s workforce issues requires more than just compliance or recruitment efforts. True advancement depends on investing in people, fostering future talent, and prioritizing quality care in daily decisions.
As ever, I hope you find this issue both informative and thoughtprovoking.

An inside look at KYN Bickley, Care Home of the Month for February, where ample staffing, careful design, and a commitment to joyful aging influence all aspects of the home.
This feature explores the shift from tick-box compliance to training rooted in lived experience, inclusion and person-centred care.
CPD explains why embedding high-quality training into everyday practice is key to retaining staff, strengthening teams and improving care outcomes.
This month, we are exploring how tabletop games can be reimagined to provide residents with an engaging, ever-changing activity that boosts connections and social opportunities.
A home manager with 50 years’ experience shares the leadership behaviours that build loyalty, confidence and quality in care teams
Executive Chef Tyler Horton presents a beloved classic, Spaghetti Meatballs, carefully modified to promote choice, nutrition, and inclusivity in care environments.




A couple of months after Aston Manor’s opening, Harrington Care Home’s flagship location, Care Home Magazine spoke with Rishi Dhamecha, the Managing Director, to review the progress since our October visit. Read on to discover more about the Aston Manor opening and its early achievements.
Aston Manor is proving to be more than just a place of residence: it’s become a vibrant, community-driven environment where residents thrive, and family members feel truly at home. While much of the attention tends to fall on the founders or key figures, Rishi emphasised that the real success story lies in the collective efforts of the entire team, from those providing care to the support staff, all working together to achieve the vision of a better, more fulfilling care environment.
One of Aston Manor’s standout features is its community hub, which has far exceeded expectations. At the time of our interview, the home had just 10 residents, but the hub’s facilities, such as the hair salon, cinema room, and private dining area, have already made a significant impact. The hair salon is used daily, and the cinema room, with its daily film schedule, has quickly become a favourite among families, who enjoy bringing their children to the home. The piano room is another unique touch, offering opportunities for social activities such as gin-andtonic evenings.
Ellie and Justyn, the Wellbeing Coordinators at Aston Manor, have played a key role in organising events for the residents and their families. For example, the home’s Christmas celebration, complete with decorations, Santa’s grotto, and gingerbread making, was

a major success, drawing 115 attendees despite having only 10 residents. This sense of community and warmth is at the heart of what makes Aston Manor truly special.
Another major highlight of the home is its approach to personalised care. The team at Aston Manor goes above and beyond to cater to the needs and preferences of each individual. The home rolls out the red carpet for each new resident, ensuring they feel welcomed and supported from day one. They are committed to maintaining this high standard of care as the home fills, with plans in place to ensure growth doesn’t affect the quality of the experience.
The home’s success is also reflected in heartwarming stories from the residents and their families. One resident, who had been unable to bathe for months due to hospitalisations, was finally able to bathe upon
arrival at Aston Manor. Another man, who had been unable to walk for six months after a stroke, regained his ability to walk after just two weeks of physiotherapy and rehabilitation. These stories highlight the transformative effect of personalised care at Aston Manor. Residents’ feedback has been wonderful, and it’s fantastic to see them sharing their positive experiences with friends and family. Looking ahead, the team at Harrington Care Homes is excited to continue expanding and enhancing the services they provide. The addition of more residents, the use of outdoor garden spaces in the summer, and the continued community-driven atmosphere are all part of their vision for the future. As the home grows, the team remains committed to keeping the care experience warm, personal, and focused on the wellbeing of every individual.

Amidst widespread workforce shortages, rising complexity, and greater family expectations in the care sector, KYN Bickley stands out with their clear philosophy and assured execution of what care should look like. Situated in South East London, the home exemplifies a care model centred on excellent staffing, continuity, and a firm belief that later life should be engaging, fulfilling, and joyful.
Daisy Slavkova, Bickley’s Home Manager, highlights that what sets KYN Bickley apart is its focus on people. The home boasts unmatched staffing levels, allowing staff to spend quality, unhurried time with residents. The goal is for care and nursing to be provided solely by the in-house team, without relying on agency staff. Daisy emphasises that this is crucial for maintaining consistent care and fostering a cohesive, positive culture. Staff members understand what it means to be part of KYN, recognise the unique ways care is delivered, and take pride in their roles.
Clinical excellence remains fundamental; KYN Bickley provides exceptional nursing and care for residents with complex conditions such as dementia, multiple sclerosis, and Parkinson’s disease. This is driven by Caroline Naidoo, KYN’s nurse-trained, hands-on CEO, who ensures that high clinical standards are established and actively upheld within the home. Nonetheless, Daisy emphasises that wellbeing goes well beyond just clinical results.
KYN Bickley has been thoughtfully designed to support the whole person. The residence brings together leaders from various disciplines to foster an environment residents can genuinely enjoy. Interiors are
Sponsored By

A
Life enrichment at KYN Bickley is intentionally resident-led.
designed by Nina Campbell, gardens by Randle Siddeley, and cuisine by Tristan Welch, under the supervision of clinical nutritionist Eva Humphries MSc. Libraries are curated by Heywood Hill, and the art collection is assembled by Adam Ellis. The outcome is a setting that exudes elegance, comfort, and cultural vibrancy. Residents wake up in a space that promotes curiosity, social engagement, and pride, complemented by a cultural and wellbeing programme that encourages participation without feeling obligatory.
At the heart of this experience is the team. KYN Bickley prioritizes training and development that go beyond basic compliance, focusing on personal growth and making residents and their families feel truly recognised and understood. The business model fosters staff flourishing, and this sense of fulfilment positively influences
residents’ daily lives. Families often praise the team’s kindness and competence, considering it one of the home’s key strengths.
The organisation demonstrates its commitment to staff through transparent opportunities for advancement. With expansion plans for Kensington and Highgate set for 2028 and additional projects in progress, employees trust in a consistent flow of growth possibilities. KYN emphasises internal promotion and retention, choosing team members not just for their skills but also for their compassion, integrity, and dedication to care and service. Recruitment prioritises attitudes and values, supported by customised training that develops talent and upholds a culture of excellence.
Life enrichment at KYN Bickley is intentionally resident-led. While the home has a solid framework,
programming is often initiated by residents themselves. This is supported by Head of Life Enrichment & Wellbeing, Jessica Shiel, who has extensive experience in designing creative programmes across arts and health. Working closely with clinical teams and dementia specialists, she ensures activities are diverse and tailored to individual needs. The programme includes salons and events with archaeologists, astronomers, mathematicians, economics professors, royal photographers, and theatrical performers, providing intellectual stimulation alongside enjoyment and social connection. Community reaches well beyond the home’s walls. KYN Bickley actively supports national charities such as the Alzheimer’s Society, Parkinson’s UK, and Age UK, demonstrating that care extends beyond the front door. Recently, residents started a monthly gathering for local peers focused on engaging conversation, friendly company, and afternoon tea. This is a strong example of residents not only shaping their own community but also contributing to the broader neighbourhood.
Families and friends play a vital role in daily life at KYN Bickley. They are included in all events, stay updated via a private newsletter, and receive personal invitations for

activities matching their interests. The home is lively, with frequent visits, seasonal parties, and spontaneous celebrations, fostering a welcoming and communal atmosphere.
At KYN Bickley, technology is thoughtfully integrated to enhance dignity and foster human connection. Advanced AI supports caregiving without replacing personal interactions, enabling

staff to focus on meaningful engagement. PainChek’s AI assesses pain using facial microexpressions and behavioural cues, making it especially useful for residents with variable communication abilities. Ally’s Resident Monitor, operating overnight, utilises discreet sensors to learn individual movement and sound patterns, alerting staff to signs of restlessness or discomfort while safeguarding privacy and uninterrupted sleep. Infrared systems reduce fall risks, and integrated care planning promptly flags dietary needs and allergens.
For Daisy, the strongest signs of quality are observed when residents thrive. Even those facing tough circumstances, such as severe dementia or nearing end-of-life, often regain confidence, appetite, sociability, and happiness. Families, who previously believed their loved ones were declining or withdrawn, experience renewed purpose and well-being. These results highlight a care model that sees later life as an opportunity to live fully. KYN Bickley isn’t just providing excellent care; it is transforming expectations for residents, families, and professionals alike.
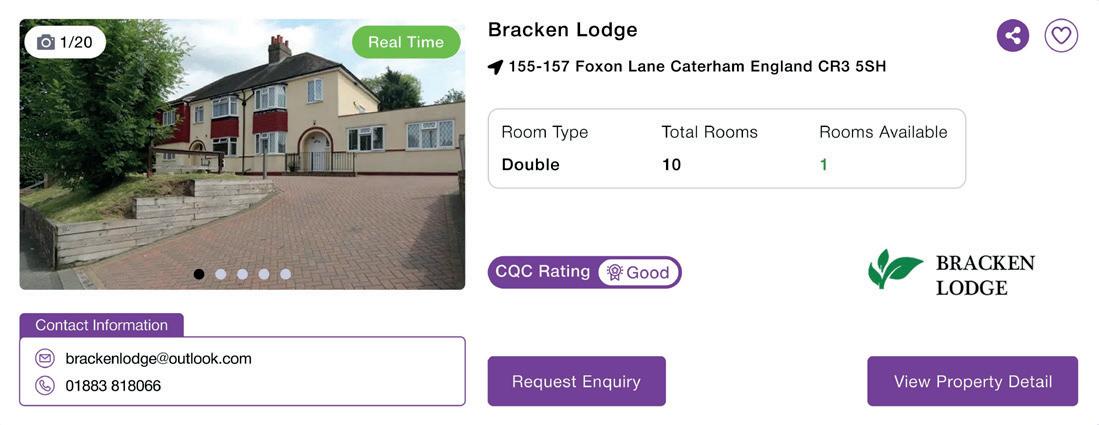
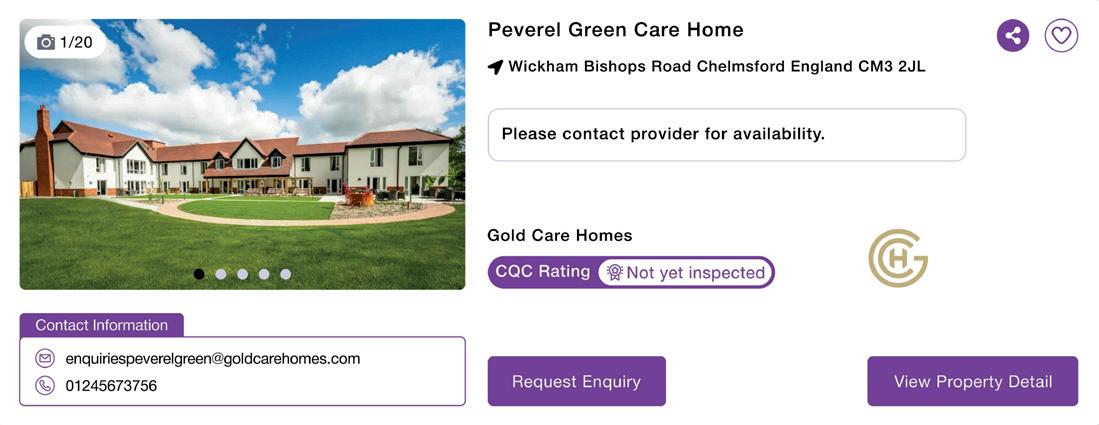
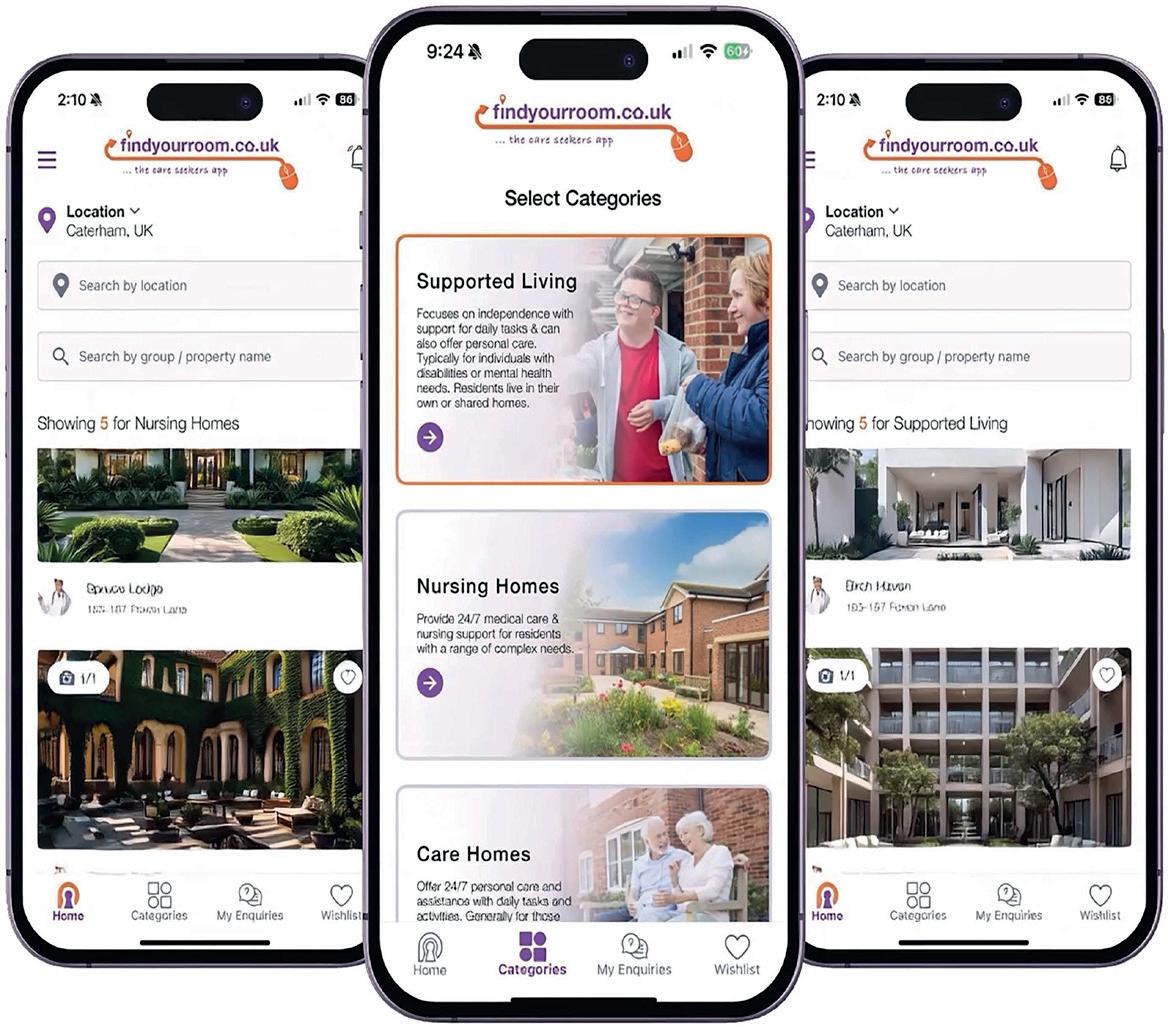
Explore how Find Your Room can help boost occupancy across UK care homes.
Find Your Room is a digital platform available online and on the iOS and Android app stores that allows families of prospective residents to search for available rooms across various UK care providers. Utilising real-time search capabilities, it helps families quickly and reliably find vacant rooms that meet the specific needs of the prospective resident.
The team at Find Your Room has over thirty years of experience in the care sector, giving them a profound understanding of the challenges faced by individuals, families, placement teams, and care providers when seeking a suitable care environment to meet all needs. This understanding inspired the creation of Find Your Room, making the process of finding care simpler than ever before for both providers and clients.
Find Your Room is the most affordable care home directory in the UK, priced at £24 per property per month. By utilising the service, care homes are able to increase occupancy rates through the real-time room availability feature, increasing visibility to potential clients who are looking for care within the area.
By giving browsers clear, realtime visibility of room availability, Find Your Room is helping care providers connect with enquiries more efficiently while reducing administrative burden.

The platform’s real-time availability tool allows homes to showcase room types and live capacity at any given moment, supported by a simple weekly notification sent to providers who have enabled the feature. Where homes are fully occupied, no action is required, and availability automatically defaults to zero, ensuring accuracy without unnecessary updates. Providers can also choose to disable the feature, in which case profiles display a “Please contact provider for availability” message.
To maintain genuine real-time data, registered managers receive a weekly email prompting them to confirm or amend availability with a single click. If no response is received, availability is reset to zero, saving teams operating at full capacity valuable time. Should a vacancy arise mid-week, providers can log in and update availability instantly, ensuring opportunities are never missed.
Find Your Room is tailored to support everyone involved in care placements, including local authority teams, social services, and families making care decisions. The platform uniquely features a dedicated mobile app that allows users to quickly check the real-time availability of care homes, nursing homes, and supported living services.
Users can filter and compare options by location and care type, contact providers directly through the platform, and manage all enquiries on a single, easy-to-use dashboard. The service is entirely free on both the website and mobile app, helping to accelerate placements and ease system-wide pressure.
findyourroom.co.uk



In this Q&A, Jamie Lee, Mobility Solutions Specialist at Subsidium, discusses how the company supports care homes with digital devices as rapid technological change reshapes resident care.
bring to the table for care providers?
Drawing on a history of supporting over 250 care providers and 50,000 devices, Subsidium focuses on removing friction from everyday care. Devices “just work,” allowing teams to focus on residents over technology. Everything from security policies to application lifecycles is managed behind the scenes. Subsidium ensures tech is fit for purpose, productive, and secure right out of the box. If problems occur, specialists are on hand to restore operations. Service extends beyond shipping; every stage of the device’s life is covered.
Where are care homes currently hitting a wall with their IT?
The biggest problem isn’t the software; it’s the unmanaged hardware it runs on. Devices are locked because a staff member left without sharing a passcode, tablets that haven’t updated in months, and systems that fail to communicate. This is frustrating, wastes time, and pushes staff to burnout. If technology feels like a failure, it won’t be embraced, leading to wasted investment and a significant barrier to providing care.
does managed support help keep things running?
In care, an IT issue isn’t just an inconvenience; it can stop medication records, handovers,
and safety checks in their tracks. The strategy focuses on preventing issues before they happen. Updates and fixes are deployed quietly in the background, often overnight. Hardware health is closely monitored to spot problems early, and industry-leading resolution times ensure staff aren’t left staring at a frozen screen while delivering care.
What should operators do right now to protect data without making life harder for staff?
Security must be automatic and invisible. If it slows people down, they will find workarounds, which is where breaches happen. Enforcing secure logins, kiosk modes to lock down the devices, update management, banning unmanaged social media, and preventing accidental settings changes are all essential.
Can tech reduce admin, or does it just add more screens?
When done properly, tech makes life easier. No one enters the care profession for paperwork; it is a necessary evil. A well-managed digital system automatically builds an audit trail. Reports that once took hours can be pulled in seconds, getting managers out of the office and back on the floor. Minimising the time and cost of administration allows more resources to be reinvested into frontline care.

What’s the five-year outlook? What should owners be planning for now?
Care will be a fully connected model, linking homes directly with the NHS, GPs, and pharmacies. Devices are clinical infrastructure, not just gadgets. Without a managed setup and a strong digital foundation, providers will hit a “tech ceiling,” where outdated hardware prevents the use of the tools that will define the next generation of care. This is where we come in.









A successful induction and ongoing training program not only embeds role expectations, values, and skills but also fosters a culture of consistency, engagement, and continuous improvement. By actively involving managers and tailoring training to real-world feedback, care homes can ensure staff are well-prepared to deliver exceptional care and maintain high standards across all shifts.
A successful induction program should consistently embed role expectations, behaviours, and core values over time. This thorough approach helps new staff fully understand their responsibilities, align with the care home’s culture, and foster strong relationships with colleagues. Reinforcing these principles regularly ensures staff are well-prepared to deliver high-quality care and make meaningful contributions to the home.
Staff training yields the best results when line managers actively participate in the learning process. They reinforce essential concepts and provide follow-up during supervision and daily leadership interactions. By understanding the training material and consistently supporting staff in implementing new skills, managers help translate learning into improved practice. This continuous engagement fosters accountability, boosts staff confidence, and promotes a culture of ongoing improvement, ultimately benefiting both staff and those in care.
Training should be provided consistently across all shifts and roles, including night staff, part-time workers, and agency personnel, to avoid disparities in care practices. Such uniformity minimises errors, promotes teamwork, and upholds high standards of care, ensuring everyone in the care setting receives optimal support at all times.
Training records should be seen as a flexible management resource rather than merely a compliance checklist. Regular review enables managers to spot skills gaps, design focused development programs, and enhance workforce planning. This proactive method ensures staff possess the required competencies to meet care standards and adapt to changing demands. Using training data like this promotes ongoing improvement and supports more strategic, efficient workforce management.
5 4 3 2 1
Reviewing training by using staff feedback and real-world experience is essential for promoting engagement and retention. Actively gathering staff input allows organisations to pinpoint parts of the training that may be overwhelming or ineffective, enabling them to make necessary adjustments. This strategy ensures training does not add extra stress, creating a positive, supportive work environment. As a result, staff satisfaction improves, burnout decreases, and overall care outcomes are enhanced.


How Could Smarter Catering Support Your Catering Team and Boost your Bottom Line?

Catering Procurement Plus from White Oaks, empowers your in-house catering team to to deliver nutritious, homestyle meals while cutting costs and streamlining daily operations. With Catering Procurement Plus, you get:
Specialist support from catering & operations specialists Resident engagement support

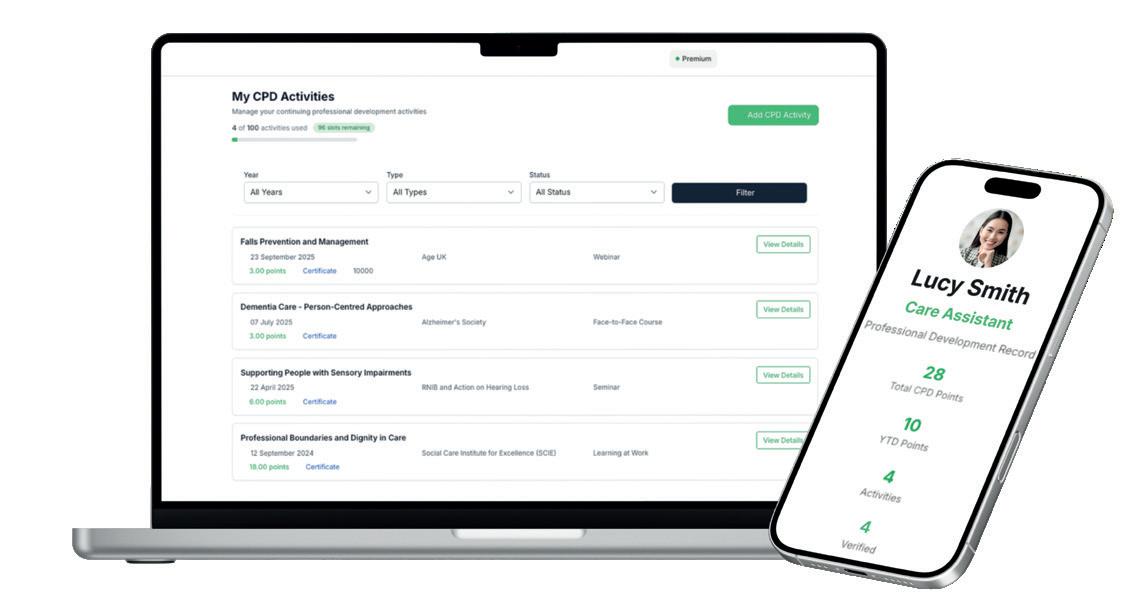
Investing in Continuous Professional Development (CPD) is one of the most effective ways care homes can strengthen their teams, improve care, and meet regulatory standards. In a sector facing rising complexity, workforce shortages, and increasing expectations, CPD is no longer a tick-box exercise but an essential tool for building confident, capable, and motivated staff.
The care sector continues to evolve rapidly. Regulatory expectations are shifting, technology is advancing, and residents’ needs are becoming increasingly complex.
CPD creates confident teams, consistent care, and professional pride that shows in every interaction with residents. When staff understand the “why” behind their practice, not just the “what”, they become advocates for quality care rather than simply taskcompleters.
While investing in CPD is essential, it’s important to recognise that not all external training is of the same quality. The sector has seen a rise in quick, low-cost courses that meet compliance requirements but lack genuine learning value.
To combat this, care homes should look for clear quality

markers. Does the training come from a reputable, accredited provider? Is content up to date with current best practice? Are the trainers experienced practitioners who understand the realities of care work? Quality CPD should challenge and develop staff, not just provide certificates. Read on to discover how to identify and implement high-quality, accredited CPD that truly makes a difference.
Training is often delivered as isolated events with little continuity or follow-up. For CPD to
have real influence, it must become routine and embedded in everyday work. Care homes can make learning part of daily life through micro-learning sessions during handovers, reflective supervision, weekly team discussions, on-thefloor coaching, and peer mentoring. By integrating CPD into daily routines, learning becomes part of “how we do things here”: a living culture rather than a calendar entry. This approach ensures that training translates into practice and that knowledge is continuously refreshed and applied.
A strong organisational culture is built through connection, confidence, and a shared commitment to excellent care.

CPD contributes directly to each of these elements in meaningful ways.
Staff feel valued and motivated. When care homes invest in development opportunities, they send a clear message that their employees matter. This boosts morale, engagement, and job satisfaction, creating a positive working environment where staff feel supported.
Teams communicate more effectively. Shared learning experiences reduce misunderstandings, promote consistency in care approaches, and support open dialogue during complex situations. When everyone speaks the same professional language, collaboration becomes smoother and more effective.
Confidence leads to higherquality care. Skilled, confident staff respond calmly to challenging situations, work accurately and efficiently, and create a positive experience for residents and their families. They’re better equipped to make sound decisions, advocate for residents, and deliver care that truly makes a difference.
Retention is one of the biggest pressures facing care homes today. High turnover disrupts continuity of care, increases recruitment and training costs, and places additional pressure on remaining staff. The Adult Social Care Workforce Survey found that 37% of staff considering leaving cited “lack of career opportunities or progression” and 23% cited “lack of learning and development” as key factors.
Care workers are more likely to stay when they see opportunities to progress. Offering clear learning pathways provides purpose, signals that employees matter, and strengthens overall team capability. Investing in people reduces turnover, ultimately protecting continuity of care for residents.
Ultimately, CPD exists to improve the lives of the people in care.

Staff who are up to date with best practice in dementia communication, safeguarding, medication management, palliative care, and person-centred planning provide more compassionate, confident, and responsive support.
Residents benefit from more personalised, dignified care, reduced incidents through better risk awareness, a calmer environment, and staff who feel empowered rather than overwhelmed.
One of the biggest challenges is keeping CPD accurate, meaningful, and verifiable, as training records can easily become incomplete or outdated. The CPD Group has partnered with the CPD Passport to provide a secure, cloud-based platform for logging training, uploading certificates, and sharing verified records.
When seeking external CPD, care homes should prioritise training accredited by bodies such as The CPD Group to ensure learning is high-quality, practical, and recognised. Accredited courses meet verified professional standards, can be logged in the CPD Passport, and create a consistent knowledge base across teams.
Beyond individual training
accreditation, care homes can achieve recognition as a “Committed to CPD” employer through The CPD Group’s Employer Accreditation scheme, demonstrating to staff, regulators, and families that your organisation genuinely values professional development.
To achieve this recognition, care homes must meet The CPD Group’s A.C.C.R.E.D.I.T.E.D Employer Framework, which assesses ten key areas of CPD practice. The free employer accreditation helps attract and retain quality staff, builds trust, and provides external validation of your commitment to excellence.
Care homes that embed CPD into daily practice create stronger, more confident teams, higher retention rates, and better outcomes for residents. The care homes that will thrive in 2026 are those that recognise CPD not as an administrative burden but as a strategic investment in their most valuable asset: their people.
thecpd.group
Training remains one of the most powerful levers for improving care quality, yet it is too often shaped by inspection frameworks rather than resident outcomes. As providers and learning partners reflect on what genuinely drives quality, a quieter shift is taking place: away from reactive, inspection-led training and towards learning rooted in people, purpose and everyday practice.

In the care sector, compliance is unavoidable. Frameworks, standards and inspections exist for good reason, and no responsible provider would argue otherwise. Yet across the sector, training is frequently organised around what needs to be evidenced rather than what needs to change. The result can be a cycle of last-minute courses, refreshed certificates and completed workbooks that satisfy regulatory expectations, while leaving the deeper question unanswered: has life improved for the people receiving care?
Leah-Marie Smith, Co-Owner and Chief People Officer at Berkley Care
Group, describes this tension as one of anxiety rather than intention. She argues that when training is motivated by fear of inspection, the learning process may become overly procedural. Boxes are ticked, but the opportunity to meaningfully improve residents’ experiences is diminished. At Berkley, the decision has been to take a different route, grounding training not in inspection timetables but in everyday interactions between colleagues and residents.
That grounding begins with listening. Across Berkley’s twelve homes, feedback from residents and families is actively gathered and analysed to identify recurring
themes. These insights are not filed away; they directly shape training priorities. Real stories are woven into learning so that training reflects daily life rather than abstract policy. Initiatives such as B: In Your Shoes, where senior and central colleagues spend time in frontline roles, translate understanding into practical learning and reinforce the realities of care delivery.
This emphasis on lived experience also underpins Berkley’s neurodiversity strategy. Differences in communication, thinking and experience are recognised as strengths, influencing both training and recruitment. Feedback from colleagues revealed that traditional

approaches did not work for everyone, prompting changes such as sharing interview questions in advance, offering multiple application methods and training managers to make reasonable adjustments. Training, in this context, supports inclusion as well as care quality.
From the perspective of a training provider, Eyad Hanash, Assistant Operations Director at Embark Learning, reinforces the importance of intentional design. Mandatory training does not improve care by default; it does so when it is planned, contextualised, and delivered in partnership with employers. Embark works closely with providers to map annual training cycles, identify gaps and evaluate not just whether learning has taken place, but whether it has made a tangible difference on the ground.
Person-centred care sits at the core of Embark’s curriculum. While certification remains essential, the focus is on face-to-face, handson learning that builds practical capability and confidence. Skills Labs replicate real care environments, using equipment such as profile beds, hoists, and medication trolleys to support roleplay and simulation. This approach accommodates different learning styles and allows carers to practise without fear, resulting in staff who are prepared to apply learning consistently in real settings.
Hanash notes that inspectors increasingly look for impact rather than volume of certificates.
Evidence that training is effective is found in confident staff, consistent practice and improved outcomes. Crucially, organisations that embed learning and development into their workforce culture often see wider benefits, including stronger retention and better inspection outcomes. Continuous development, rather than reactive training, becomes the norm.
At Kara Healthcare, this shift is framed even more explicitly around outcomes. Chief Executive Officer, Nitesh Somani, is clear that while compliance matters, it should never be the primary driver of training. Too often, he says, learning is rushed through in the weeks before an inspection, designed to demonstrate readiness rather than deepen understanding. The files are completed, but the residents’ lived experience remains unchanged.
Kara Healthcare has responded by embedding training into everyday practice through the Kara Training Academy. Learning is not confined to classrooms or inspection cycles; it is reinforced through supervision, reflection and leadership conversations. The guiding question is not what inspectors will ask for, but what will make life better for the people who live in the home. When training is aligned to compassion, dignity and connection, compliance follows naturally.
Person-centred care at Kara is treated as a daily discipline. Training focuses on understanding life stories, preferences and routines, reinforcing that excellent care is
delivered through empathy and presence rather than policy alone. The Kara Cadets Programme invests early in future carers, shaping values before habits form and reinforcing that care is a profession built on purpose and responsibility.
Resident and family feedback plays a central role in shaping learning. Positive feedback is shared and celebrated, while concerns are explored and reflected upon to improve practice. This ensures training remains responsive to real experiences, strengthening accountability across the organisation. Evidence, when presented, tells a story: training records reflect learning applied in practice, supervision is developmental, and audits support growth rather than fault-finding.
Avoiding last-minute training is fundamental to this model. By planning learning well in advance and reinforcing it through observation and coaching, Kara replaces fear with confidence. Inspection becomes a moment of validation rather than a period of panic, and standards are sustained rather than staged.
Across these approaches, a consistent message emerges. Compliance and care quality are not competing priorities. When training is shaped by people, informed by feedback, and embedded in daily practice, it becomes a driver of culture, confidence, and consistency. In that environment, compliance is no longer the goal; it is the outcome of care delivered well.
Gemma Christie, Business Account Manager at Miele Professional, discusses the importance of having a strong infection prevention plan in place in care homes.
Infection control is a daily concern for care homes, and rightly so. With residents living in close proximity and staff working across shared spaces, the risk of pathogens spreading is ever-present. Yet one of the most significant risks to resident safety is often found in the laundry room. Without a clear infection prevention plan, even routine housekeeping tasks can become a weak link in the chain.
Laundry is one of the most active touchpoints in any care setting. Bedding, towels and clothing can carry bacteria and viruses long after they appear clean. Even the most conscientious team can struggle to control infectious diseases without clear guidelines; a documented infection control plan is essential. Every care home should have documented procedures that guide staff in handling, washing, and storing laundry.
The process begins before the wash cycle. Staff must be equipped with gloves and aprons, and contaminated items should be placed in colour-coded or watersoluble bags. These bags should be loaded into the machine unopened, allowing them to dissolve during the cycle and reducing the risk of airborne transmission.
Temperature matters more than many realise. To meet thermal disinfection standards, laundry must be washed for 10 minutes at 65°C, 3 minutes at 75°C, or 1 minute at 85°C to effectively kill harmful bacteria and viruses. Machines used in care settings must reliably reach and maintain these

temperatures every time. To prevent contaminated water from entering the mains supply, all appliances should comply with Category 5 water regulations, with a one-way valve fitted as standard.
Detergent use is equally important. Staff should follow manufacturer instructions on dosage and temperature to ensure effective disinfection. Once washed, items should be checked for damage or discolouration before being dried and stored separately from soiled laundry. To prevent cross-contamination, clean laundry must never come into contact with dirty items. A sluice sink can also help remove residue from heavily soiled materials before the wash cycle begins.
Systems like Miele’s 360PRO offer a joined-up approach to infection control, combining commercialgrade laundry, dishwashing and cleaning solutions with tailored support. Designed specifically for care environments, 360PRO helps
homes meet hygiene standards while reducing the risk of crosscontamination. It’s a system built to support staff, protect residents and simplify compliance.
But equipment and process alone aren’t enough. Infection control plans must be communicated clearly and reinforced regularly. This is especially important in areas like laundry rooms, where staff movement is frequent. Visual reminders in key hygiene areas, quick-reference guides and regular training sessions can all help embed best practice.
Ultimately, infection prevention relies on consistency. A clear plan, the right equipment and well-briefed staff can make a measurable difference to resident safety. For care homes looking to strengthen their approach, working with a specialist partner like Miele Professional can help ensure that laundry processes are not only compliant, but genuinely effective.
miele.co.uk

Find out how Anoushka Farouk, founder of Aventurine Therapies, is transforming care teams through her emotional resilience workshops. Aimed at tackling burnout and stress, Anoushka’s approach promotes emotional well-being, strengthens peer connections, and enhances staff retention, performance, and the overall quality of care delivered.
Aventurine Therapies provides Thrive Together workshops aimed at helping care teams manage one of the key challenges in social care: the emotional toll of their work. While caregiving is rewarding, it often involves emotional strain that may go unnoticed until it results in burnout, exhaustion, or staff leaving roles they once enjoyed.
Anoushka collaborates directly with care teams to explain why emotional fatigue happens, how to spot early stress signals in themselves and colleagues, and how to adopt practical strategies to handle stress and build resilience. Her focus is on creating a space where people feel seen, valued, and supported because when staff are emotionally healthy, all other aspects improve.
These workshops are designed to be part of a broader retention strategy, rather than a one-time wellbeing activity. Retention is built on culture, trust, and the daily experiences of staff.
The sessions increase awareness of both self and others, helping teams understand the emotional toll their work takes and gain insight into colleagues’ experiences. This deeper awareness strengthens compassion, connection, and mutual support across teams. By focusing on emotional wellbeing and peer connections, the workshops reinforce the
foundations that support staff retention. When staff feel emotionally supported, training and leadership development initiatives become more impactful. Follow-up support ensures that the lessons learned are embedded into everyday leadership and work culture.
For frontline staff, the biggest benefit is often simply being heard. Many report that the sessions are the first time their emotional challenges have been openly acknowledged.
The workshops provide practical tools, including breathing exercises for emotional regulation, gratitude practices, journaling to process emotions, affirmations to build selfworth, and the Emotional Freedom Technique (EFT) to relieve stress. Importantly, the workshops also foster a sense of reconnection among team members. In some sessions, staff share words of affirmation and appreciation, deepening their bonds and leaving them more inspired and united.
Staff consistently report feeling calmer, lighter, and more emotionally resilient after attending the workshops. Many say they feel a sense of relief that they hadn’t realised they were carrying. Employees also report greater confidence, improved communication, and a better ability

to handle the emotional demands of caregiving.
As emotional well-being improves, teams experience greater engagement, reduced tension, and more openness in communication. This shift not only impacts the team but also the quality of care delivered to residents.
Care providers who incorporate Aventurine Therapies into their culture often see reduced burnout, fewer stress-related absences, and better staff retention. Emotional challenges are addressed early, preventing them from escalating into larger issues such as sickness absence or staff turnover. Managers also spend more time leading and less time addressing crises.
Anoushka is confident that this approach will continue to build healthier, more stable workplaces where staff feel valued, residents notice improved care, and employees are more likely to stay long-term. aventurinetherapies.com

By rethinking how familiar tabletop games are delivered, care homes can turn everyday activities into inclusive, person-centred experiences that promote connection, cognitive stimulation and wellbeing without the need for new resources or complex equipment.
For many care homes, tabletop games are a long-standing feature on the activities calendar. Cards, dominoes and board games are familiar, accessible and easy to resource. Yet when delivered in a traditional format, they can sometimes fail to engage residents meaningfully, particularly those living with cognitive or physical impairments. By introducing a small but deliberate “twist,” care homes can transform simple tabletop games into powerful tools for social connection, cognitive stimulation and emotional wellbeing.
This approach is not about introducing complex new games or investing in specialist equipment. Instead, it focuses on adapting what is already known and trusted, reframing play as a shared, supported experience rather than a test of skill or memory.
Tabletop games offer several advantages in the care home setting. They are inherently social, encourage face-to-face interaction and can be delivered in small groups, which often leads to deeper engagement amongst residents. For those who may struggle with confidence, mobility or communication, sitting around a table provides a sense of equality and inclusion.
From an operational perspective, tabletop games are low-cost,

flexible and easy to reuse, making them a practical option for busy activity teams. Importantly, they also align well with person-centred care principles by allowing activities to be tailored to individual abilities and preferences.
The challenge for operators is to ensure these sessions remain engaging, inclusive, and purposeful, rather than becoming passive or routine.
The most effective adaptations involve shifting the emphasis away from competition and rules towards participation, conversation, and shared enjoyment. This can be achieved in several ways.
Simplifying rules is often the first step. Traditional card or board games can be adapted to eliminate winning or losing, or to encourage collaborative play rather than
individual play. For example, a game of dominoes can become a group effort to build a chain together, with care staff guiding the process.
Adding prompts for conversation can significantly enhance engagement. Cards can be adapted with questions or discussion points written on them, encouraging residents to share memories or opinions during the game. A simple round of cards might include prompts such as “What was your favourite holiday?” or “Did you used to play games like this at home?”
Adapting equipment also makes a difference. Larger playing cards, high-contrast boards, tactile pieces or weighted items can help residents with visual or dexterity challenges to participate more confidently. These small adjustments can remove barriers that might otherwise lead to disengagement.
For residents living with dementia, tabletop games can be particularly effective when they focus on familiarity and repetition rather than recall. Games that rely on longterm memory, such as recognising card suits or matching colours, are often more accessible than those that require short-term memory or complex decision-making.
Matching games, simple sorting activities or familiar sequences can all be adapted into tabletop formats. The key is to allow residents to engage at their own pace, without pressure to “get it right.” Staff play a crucial role here, offering reassurance, gentle prompts and positive reinforcement throughout the session.
Importantly, success should be measured by engagement and enjoyment, not by completion of the game. Even brief moments of connection or recognition can be meaningful outcomes.
One of the most significant advantages of tabletop games with a twist is their ability to foster social connection. Small-group sessions naturally encourage conversation, eye contact and shared laughter, which can help reduce feelings of isolation.
For residents who are quieter or less confident in larger groups, tabletop games can provide a

structured yet informal setting for interaction. Over time, these sessions can help build relationships between residents and the staff involved.
Some homes have found that rotating seating arrangements or pairing residents who do not usually interact can lead to new connections, fostering a more inclusive community within the home.
From a staffing perspective, tabletop games are relatively easy to facilitate, but the quality of delivery is crucial. Staff leading sessions should be encouraged to view themselves as facilitators rather than instructors. Their role is to observe, adapt and respond to

residents’ needs in the moment.
Preparation does not need to be time-consuming. A small selection of adaptable games, prompt cards and sensory-friendly equipment can be reused across multiple sessions. Involving residents in choosing which games to play can also increase engagement and reinforce a sense of autonomy.
Volunteers and family members can be invited to join sessions, adding variety and strengthening relationships with the wider community. With appropriate guidance, they can support residents one-to-one, helping to sustain attention and participation.
Reimagining tabletop games does not require a complete overhaul of activity provisions. Instead, it involves a shift in mindset: seeing familiar games as flexible tools rather than fixed formats. By introducing small adaptations and focusing on inclusion, care homes can unlock greater value from activities that residents already recognise and enjoy.
In a sector where meaningful engagement is central to quality care, tabletop games with a twist offer a simple, effective, and scalable way to enhance residents’ daily lives: proving that sometimes the most impactful innovations are found in the smallest details.
Rising energy costs are placing growing pressure on care providers, but well-designed solar solutions can offer a practical route to long-term savings. This case study explores how Solar4Good supported First Care Services Limited to significantly reduce electricity costs while maintaining reliable, high-quality care delivery.
First Care Services Limited is a locally owned, independent care home committed to providing essential healthcare and support services to residents in Birmingham and Solihull. As a care facility, it depends heavily on electricity to power lighting, heating, medical devices, and daily operational activities crucial for resident wellbeing. Ensuring a reliable and continuous energy supply is vital to deliver safe, high-quality care.
With rising energy costs placing increasing pressure on operational budgets, First Care Services Limited sought a long-term, sustainable solution that would reduce electricity expenditure while ensuring continuity of care and operational stability.
Energy demand within healthcare and care environments is both significant and consistent. Electricity is required throughout the day to support clinical
equipment, environmental controls and core operational needs, making facilities particularly vulnerable to fluctuating and rising energy prices. For First Care Services Limited, escalating energy costs were limiting financial flexibility and placing strain on budgets that could otherwise be directed towards care services, staffing and facility improvements.
To address these challenges, Solar4Good designed and implemented a tailored 77kW commercial solar PV system. The system was engineered to maximise daytime energy generation, aligning closely with the facility’s peak operational hours. This design strategy maximises selfconsumption, allowing the home to substantially lower its dependence on mains electricity during peak demand times.
By designing the system around the realities of a healthcare setting, Solar4Good delivered a solution that supports reliable, efficient operations while maintaining the uninterrupted energy supply required for high-quality care delivery.
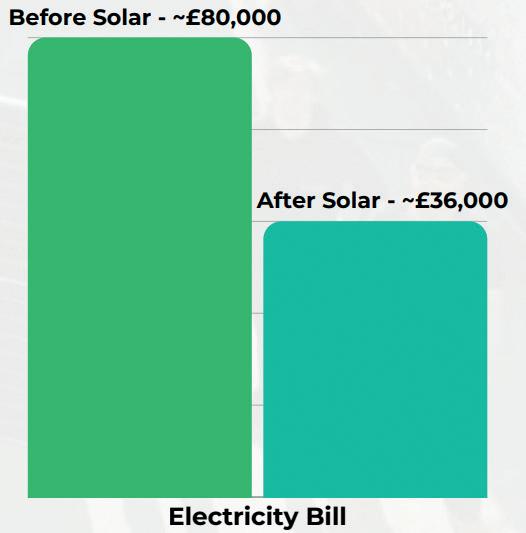
The installation has delivered substantial and measurable benefits. Annual electricity costs have decreased from approximately £80,000 to £36,000, resulting in significant ongoing savings for the home. These savings allow First

Care Services Limited to reinvest in staffing, resident comfort, facility enhancements, and long-term service quality.
Reduced energy overheads also provide greater scope for investment in improved care services, upgraded medical and support equipment and enhanced living environments. In addition to financial benefits, the solar PV system supports environmental responsibility, reducing the facility’s carbon footprint by an estimated 12–15 tonnes of CO2 annually.
This collaboration demonstrates how well-designed solar solutions can support both financial sustainability and high standards of care. By lowering energy costs and reducing environmental impact, the project has helped to futureproof operations while delivering meaningful benefits for residents and the wider community.



As the health and social care sector faces increasing pressure, staffing agencies have become essential for delivering care. However, health and social care recruitment specialists at Unity Plus warn that many providers may jeopardise resident safety by partnering with unsuitable recruitment agencies.
If an agency offers suspiciously low hourly rates, it’s important to question how it can sustain itself. Ross Hodgson, an expert in health and social care and CEO of Unity Plus, explains, “The basic cost to employ someone at minimum wage is £16.21 an hour. If their rates are below that, it suggests they might be cutting corners on pay, training, or compliance.”
Some agencies operate without formal contracts, relying on basic rate cards that obscure additional fees for emergency shifts, bank holidays, or cancellations, leading to unexpected costs and strained relationships. Cancellation policies vary; some allow last-minute cancellations without notice, leaving staff unpaid, while others penalise lateness without protecting workers. Ross advises caution with non-transparent agencies: “If terms aren’t clear, ask what else they might conceal. A proper contract should protect everyone.”
Unity Plus has assisted many overseas healthcare workers promised specific hours by agencies listed on their Certificate of Sponsorship. Often, these promises are unmet, and workers face unfair treatment due to a lack of awareness about their rights. They are pressured to work more than 20 hours, accept cash payments, and sometimes break the law, thereby exploiting their vulnerability and putting their visa at risk.
Frequent carer changes can disturb residents and lower care quality. Unity Plus stresses continuity is key, enabling residents to build trusting, secure relationships. Agencies valuing continuity should consider home needs and carefully select teams without rushing, to minimise adjustments. Homes should avoid frequent name changes and last-minute staff bookings, especially for unfamiliar staff.
5 4 3 2 1
Unlike care homes, care agencies are not regulated by the CQC, despite their vital role in staffing. Ross states: “It’s too easy for problematic agencies to operate without enforcement powers, and this situation needs to change.” He highlights that care homes must recognise warning signs when selecting agencies. The priority isn’t just to fill shifts; if an agency doesn’t meet standards, patient safety is compromised.

Susan Watson, Home Manager at HC-One’s Pytchley Court Care Home, draws on over 50 years of nursing experience. This interview explores how values-driven leadership, early-career support, and meaningful staff engagement support long-term staff retention and excellent care results, offering practical lessons for care home managers facing ongoing operational challenges.
After more than 50 years in nursing, what do you believe most strongly influences whether care staff choose to stay long term?
In my experience, people stay where they feel valued, supported, given opportunity for growth and proud of the care they deliver. While pay and conditions matter, long-term retention is driven by meaningful relationships, visible leadership, and a culture where staff feel listened to and respected. When people feel psychologically safe, appreciated for their contribution, and confident that their development matters, loyalty follows naturally.
How did you build and sustain a culture at Pytchley Court that supported the journey to an Outstanding CQC rating?
Kindness, dependability, and high professional standards have always been the cornerstones of our culture. We set an example by ensuring that values are not only discussed but also lived out daily. Key elements have been open communication, shared accountability, and giving employees at all levels the freedom to voice their opinions and drive change. Achieving Outstanding involved fostering an atmosphere in which acting morally toward residents and co-workers is the standard, rather than preparing for inspections. In addition, we

promote involvement amongst all communities in the home, across the hierarchy of staff and residents’ families, and prioritise the ability to channel ideas to provide quality care services. For instance, we have 2 residents on the recruitment panel at the care home.
What role has developing and supporting professionalsearly-career played in staff retention at the home?
Supporting professionals in their early careers has been essential

to the stability of our workforce. We devote time to appropriate induction, mentoring, and continuing training and supervision because we believe that first impressions matter. Instead of seeing a position as temporary, we help people see a future for themselves within the organisation by fostering confidence, offering clear pathways for advancement, and recognising early successes.
Preceptorships and strong university partnerships allow us to support learners during a formative stage of their professional journey. Students who feel welcomed, supervised and valued are more likely to return as permanent staff, as they are mentored by our Nurse in the home. For instance, we have a student who expressed how impactful the mentorship and experience at the home was in her acquiring her degree at the university. These partnerships also promote reflective practice, evidence-based care and continuous learning, which directly
enhances the quality and safety of care we provide. In addition, we provide opportunities for students to participate in the social activities that take place in the home. For instance, students had a trip on the home minibus to the seaside with residents, to a West Northants Council forum, Namaste Therapy, and the Care Show in Birmingham, where they experienced the Dementia box. This involvement has helped improve their knowledge and compassion. We also have partnerships with Paramedic students.
In your experience, what leadershippracticalbehaviours make the differencegreatest to staff morale and loyalty?
The biggest impact is made by being transparent, truthful, and persistent. When leaders are present, personable, and consistent in their behaviour, staff members notice. Simple actions that foster trust include listening without passing judgment, appreciating effort, responding quickly to issues, and being fair. Service and integrity are more important in leadership than power. Also, I demonstrate a compassionate, supportive
leadership style by being approachable and readily available to listen, guide and support staff as needed.
What advice would you give to care home managers trying to balance pressuresoperational with creating a workplace people want to remain part of?
Although operational demands cannot be avoided, people should never be overshadowed by them. Prioritise relationship in addition to performance, in my opinion. Invest in your team, communicate honestly when things are tough, and never undervalue the impact of gratitude. A supported workforce is more resilient, more dedicated, and better prepared to provide outstanding care.
In conclusion, managers should adopt a people-centred approach, demonstrating fairness and approachability, remaining open and willing to listen, and maintaining a strong, visible presence on the floor. Greater emphasis should be placed on observing day-to-day practice and staff interactions, alongside administrative responsibilities, to ensure high quality care delivery.
Sara Catanzaro, Design Manager at Alsico, reflects on how better-designed uniforms can support wellbeing, improve day-to-day comfort and contribute to retention across the care workforce.
When staff wellbeing is discussed in care homes, the role of uniforms is often overlooked. Yet uniforms are a constant part of a care worker’s working day and play a meaningful role in how supported, comfortable and capable people feel at work.
Alsico’s latest research found that 58% of care workers believe uniform fit affects how well they can carry out their daily duties, with uniforms also ranking among the key contributors to overall job satisfaction. This highlights how closely clothing is linked to comfort and performance, particularly in roles that are physically demanding and require sustained focus over long shifts.
A uniform that restricts movement, pulls across the shoulders and traps heat doesn’t just cause some momentary inconvenience, but creates cumulative strain. Over a 12-hour shift, they can create ongoing discomfort and fatigue. Care work involves repeated bending, reaching, lifting and supporting, and garments that are not designed to accommodate this can add unnecessary physical strain. Welldesigned uniforms take movement into account, using engineered stretch, shaped patterning and appropriate fabric choices to support the body in motion, not just when standing still.
Care environments can vary significantly throughout the day,

Improving uniform provision is a relatively simple and affordable way for care organisations to support wellbeing.
and for many women experiencing menopause, managing temperature and comfort can be particularly challenging. Alsico’s research found that 68% of respondents who had experienced menopause symptoms said their uniform did not help them cool down after a hot flush. In these cases, the issue is often not just the hot flush itself, but how quickly the body can cool and recover afterwards. Fabrics that retain heat or dry slowly can prolong discomfort and disrupt concentration, while breathable
fibres, moisture management and adaptable layering can make a meaningful difference.
In a sector facing ongoing retention challenges, these practical details matter. Improving uniform provision is a relatively simple and affordable way for care organisations to support wellbeing. When uniforms are designed to work with the body rather than against it, staff can focus their energy on delivering high-quality care.
alsico.com

From pharmacies to care homes and hotels, discover how Sukhi Gidar, CEO of Gold Care Homes, is redefining high-quality, person-centred care.
Sukhi’s journey into the care sector began not with a detailed plan but through hands-on experience and practical involvement. Originally trained as a pharmacist, Sukhi and his late brother operated pharmacies before engaging in a care home project in the Midlands. When the developer faced funding difficulties, the brothers invested in the venture, leading to three years of direct management of the home.
This period was crucial. Managing a care home offered insights into regulations, staffing, and operations, but also revealed the profound positive impact a well- managed environment can have on residents and their families. After this experience, Sukhi committed fully to the care sector, where he has now spent over 30 years.
A key drive has been to improve


how care homes are perceived. Sukhi has observed how poorly run homes erode trust and wellbeing, whereas high-quality care can uphold residents’ dignity and comfort, fostering a sense of belonging. He believes the sector is evolving, emphasising the creation of care environments where older people feel happy and supported, and where families are reassured rather than burdened with guilt.
Alongside his work in care, Sukhi has maintained a longstanding interest in hospitality. From childhood, he was drawn to hotels, which eventually led him to acquire a local Marriott hotel, an establishment he had known previously as a guest. This unexpected move underscored the operational similarities between hospitality and care.
Both sectors are peoplecentric and property-dependent, requiring well-maintained buildings, effective systems, and strong teams. Leadership is vital in both, with managers shaping culture, motivating staff, and maintaining standards.
Hospitality has influenced Sukhi’ s approach to care, especially regarding dining. In care homes, mealtimes are often the most significant part of the day for residents. Learning from hotel practices, there has been a greater focus on presentation, variety, personalisation, and choice, along with flexibility around meal times and preferences.
Despite these similarities, Sukhi recognises the key differences. Care homes are more specialised and are subject to stricter regulation and scrutiny due to their duty of care. While hotels operate commercially, care homes must remain fundamentally focused on providing care.
Looking ahead, Sukhi is planning further care home developments and aims to acquire new properties targeted for 2026. In hospitality, plans include expanding gym and spa facilities, adding padel courts, and extending restaurant offerings, demonstrating his ongoing dedication to well-managed, people-centred environments across both fields.

Drawing on his experience in health and social care, Tyler Horton, Executive Chef at Askham Community Village, introduces a spaghetti meatballs dish shaped around dignity, adaptability and the practical realities of care kitchens.
In care environments, the success of a dish is rarely measured by technical complexity. Instead, it is judged by how well it meets individual needs, supports dignity and works within the practical constraints of a busy service; this dish was developed with those exact considerations in mind.
Having spent seven years in health and social care, Tyler understands that person-centred care extends well beyond care plans. Food, he says, is one of the most immediate and powerful ways to offer choice, reassurance and comfort, particularly for people who may feel a loss of control elsewhere in their day. This dish was designed to be adaptable at its core, with portion sizes that can be easily adjusted and components that can be modified without drawing attention to differences. The aim is simple: everyone receives the same meal, tailored quietly and respectfully to their needs.
Dietary requirements were another key consideration. In modern care settings, kitchens often balance multiple allergens, preferences, and clinical needs simultaneously. This recipe allows for straightforward adaptation, with the ability to remove all 14 major allergens where required. It can be made gluten-free with appropriate ingredient choices, while the sauce itself remains naturally gluten-free. By leaving out dairy, it also becomes suitable for vegan residents, offering a nutritious base that works across a wide range of diets without the need for multiple alternative dishes.
Nutrition, however, has not been sacrificed for simplicity. While

This recipe allows for straightforward adaptation, with the ability to remove all 14 major allergens where required.
the dish appears to be familiar comfort food, it delivers significant nutritional value, providing up to 4 portions of fruit and vegetables. The inclusion of olive oil provides beneficial monounsaturated fats that support heart health and blood sugar regulation, while the overall calorie density helps meet the needs of residents who may struggle to maintain weight or appetite.
Just as important is the emotional role of the meal. “There’s no ego in catering for care,” Tyler explains. “People want food they recognise and enjoy.” This dish leans into that reality, offering something comforting and familiar, but prepared with care and attention so that it feels considered rather than basic. It is designed to be enjoyed equally by rehabilitation service users and those in nursing care, without feeling patronising or overcomplicated.
The dish reflects the operational realities of care kitchens. Both the meatballs and the sauce can be
Allergens may include gluten, eggs, dairy, and sulphites, depending on the ingredients selected.
Spaghetti
(Your preferred brand. Homemade options are possible, but they tend to lack the texture that pairs well with soft meatballs)
Meatballs
(Makes 40-60, depending on how big you would like to make them)
1KG Beef Mince
1KG Good Quality Sausage Meat
6 Carrots
1 Celery Head
2 Onions
12 Large Garlic Cloves
Water to make a puree Thyme and Oregano (Small Bunch)
Tomato Sauce
Olive oil (around 100ml)
2.5KG Plum Tomatoes
400g Tomato Paste
1 Tablespoon of Sugar (if necessary)
12 Carrots
2 Celery Heads
4 Onions
2 Red and 2 Green Peppers
Garlic (Measured with your heart, I use as many cloves that fit in my hand)
Basil (Big Bunch) Thyme (Small Bunch) Oregano (Small Bunch)
400ml of either Milk or Double
Cream
prepared in advance and hold well, supporting consistency of service and easing pressure during busy meal periods. It performs reliably under hot-holding conditions, making it suitable for large-scale catering without compromising quality, appearance or taste.
For Tyler, and for the Askham Village Community he is proud to be part of, this dish represents more than a recipe. It is an example of how thoughtful food design can support dignity, choice and wellbeing, while still working in the real world of care.
Meatballs
Make a puree of carrots, celery, onions, herbs, and garlic, using as much ice-cold water as needed to achieve a viscous mixture.
Simply combine this mixture with both your beef mince and sausage meat, and mix either with a mixer or, if you are feeling strong, with your hands, until it comes together into a uniform mix.
Using wet hands, roll your meatballs onto a lined sheet pan to the size you think is most suitable for how you wish to present the dish.
Bake these, depending on size, at 180°c until golden brown, reaching an internal temperature of 74°c.
Sauce
The soffritto can be either cut to keep a rustic sauce or blitzed. Blitzing your soffritto can help it cook more quickly, achieve a more refined finish, and distribute the flavour better.
Blend together the carrots, onions, celery, peppers, and garlic into a fine paste, then fry in olive oil until aromatic.
Add your tomato paste and fry it for another five to ten minutes to cook out the raw flavour. If needed, deglaze with a little water, or proceed directly by adding your crushed plum tomatoes. Crush

the plum tomatoes by hand to break them down, which preserves better flavour and results in a thicker texture.
Add your sugar (if needed to balance any bitterness from the tomatoes or paste), then include the thyme and oregano leaves. Simmer gently for about an hour, stirring occasionally, and add water if the sauce thickens too quickly.
Finish with fresh basil and a small amount of milk or cream, to your preference for decadence, as it smooths out the sharp, acidic flavours into a more comforting taste.
Save some of the sauce to mix with your spaghetti, then add the meatballs to the remaining sauce and cook for an additional 20 minutes until the flavours meld.
Undercook your spaghetti by a couple of minutes, before finishing the cooking in the reserved tomato sauce and a little pasta water.
Serve the spaghetti with as many meatballs and sauce as you like, garnish with fresh herbs or your preferred cheese, and enjoy classic, comforting flavours.
Learn more about our visit to Dunham Care Homes’ flagship, Herne Bay Manor, where we had the chance to speak with Mike Wilson (COO) and Trisha King, the home’s Manager, about how thoughtful design, discreet technology, and a strong focus on staff development are shaping a quality-led approach to care.
With its opening approaching, Herne Bay Manor is set to become the flagship home for Dunham Care, and is a clear indicator of how the group sees the future of care. The emphasis is firmly on quality, consistency and creating an environment that works well for both residents and staff, with expansion and exciting growth very much in future plans.
Technology is integrated thoughtfully and without intrusion across the home. Sensors in residents’ rooms that monitor movement and falls alert staff via pocket devices rather than alarms or flashing lights. This will allow the home to remain calm and familiar for residents, while ensuring staff can respond quickly and confidently when support is needed. From our conversations, the management team is clearly forward-thinking about how technology can be used to personalise care, not replace human interaction.
Dining is another area where the focus is on maintaining a calm atmosphere. Residents are served by the home’s hospitality staff, allowing them to choose their meals with minimal noise and disruption in the dining space.
The home’s interior design has been designed in-house, giving it a distinct feel and a level of character often missing from more standardised developments. A

Herne Bay theme runs throughout the décor, which will help residents recognise local references and offer easy conversation starters for both staff and visitors.
On the dementia floor, design choices are subtle and residentled. Interactive stations along the corridors invite engagement without being directive, allowing residents to take part when it suits them. Memory boxes outside each room support recognition, alongside customisable door plaques engraved with residents’ preferred names or nicknames, reinforcing identity and familiarity.
One of the home’s most striking features is the first-floor balcony, which is unusually large for a care home and is likely to become a valued space during the spring
and summer months. It provides a lovely, accessible outdoor space protected from the wind by glass without residents needing to leave the floor.
The culture within the home feels positive and purposeful. The team is welcoming and enthusiastic about working in the home and using the new systems, and the senior leadership is focused on training and career progression, with a clear aim of ensuring staff feel supported and part of a wider family.
Herne Bay Manor also benefits from its position next to its sister retirement village. This allows residents from both settings to mix, and helps village residents become familiar with the care home’s environment, potentially easing any future transition.

Free, expert support on digitisation, data protection, cyber security and AI
Guidance
Step-by-step guides on key issues like cyber security and AI
Training and elearning
eLearning, interactive games, and training materials
Events and webinars
Free events with digital and data experts
Tools and templates
Practical checklists, audit tools and Data Policy Builder
Direct support
28 local support organisations plus national team
Research and information
Emerging evidence, case studies and news updates