catholichealthli.org
A note from Catholic Health’s President & Chief Executive Officer
We’re all part of the solution.
Dear Colleagues,
Catholic Health has a comprehensive plan for enhancing Health Equity across our service area. The pages you’re about to read through will show you just how and where you play an indispensable role.
The sad truth is that many people, both nationally and regionally, suffer a vastly disproportionate amount of preventable disease. These are largely driven by the social determinants of health (SDOH): dietary habits, neglect and lack of access to quality health care.
We can do something about this, and Catholic Health is committed to doing so. Under the leadership of Dr. Lawrence Eisenstein, we have a comprehensive program to address the economic and social obstacles to good health.
Rooted in mission, Catholic Health believes health care is a right, not a privilege. That’s why we treat all patients in need of our services, regardless of their ability to pay. It’s also why we have proactive programs designed to bring exceptional health care to our underserved communities.
By working together, we can bend the disease curve. As you ramp up access to quality care, you address those SDOH. As you screen for and detect disease at its earliest stages, you make it possible to preempt serious, long-term debilitating diseases.
And that computes to longer, healthier lives as well as sharp reductions in health care costs. I thank you for being part of this all-important effort.
Patrick O’Shaughnessy, DO, MBA President & CEO
Catholic Health is a faith-based health care delivery organization, predominantly serving the residents of Nassau and Suffolk counties on Long Island. Comprised of 6 hospitals, 3 skilled nursing facilities, vibrant home care service delivery, home hospice and thousands of providers across Long Island, Catholic Health is proud of our mission of mercy, and considers mission and health equity as part of everything that is done at Catholic Health facilities and by its providers.
St.
St. Joseph Hospital
Catholic Health Ambulatory Care hubs – Commack – East Hills – Flushing – Lake Success – Merrick – Patchogue – Riverhead – West Babylon – Westbury – Woodbury
Executive Summary
Urgent Care – Ronkonkoma
Catholic Health
Ambulatory & Urgent Care – Centereach – Melville
In 2022, Catholic Health set out to establish and incorporate a strategy and path forward for a newly formed Community and Public Health Program, of which health equity would be at the core. The inaugural Health Equity Written Strategic Plan 2023–2024 was released in the Fall of 2023. Guided by data, and following a model of defined goals and objectives, we present the third annual edition of Catholic Health’s written Health Equity Strategic Plan, 2025–2026. This year’s plan looks back on the second full year of efforts, and provides an update on objectives and direction. Further, this plan adds new objectives based on the incredible growth of Catholic Health’s equity initiative.
In line with Catholic Health’s Mission and Vision, and for compliance with regulatory requirements, Catholic Health continues to advance work towards health equity. Led by our Director of Epidemiology and Public Health Analytics, this year’s data is presented with a higher degree of stratification and analysis. Data collection is done with purpose and intent, and measures have been evaluated to assess the specific needs of the communities we serve, and to guide strategic operations going forward. With an emphasis on identifying and impacting health disparities, all of this work is done with the goal of achieving maximal health outcomes for our patients.
Catholic Health Physician Partners Practices
Babylon
Bay Shore
Bethpage
Deer Park
East Islip
East Setauket
Fresh Meadows
Garden City
Great Neck
Greenvale
Hampton Bays
Hicksville
Huntington
Islip
Levittown
Lynbrook
Massapequa
Medford
New Hyde Park
Oakdale
Plainview
Port Jefferson
Port Jefferson Station
Rockville Centre
Ronkonkoma
Roslyn – Smithtown – St. James
Valley Stream – Wantagh
West Babylon – West Islip – West Sayville
Catholic Health has committed to improving the health and wellness of all people within the communities we serve. With the support of Catholic Health leadership and the Board of Directors, the pillars of the Community Health Roadmap (see Figure 1.0) have not changed. This Health Equity Strategic Plan describes efforts to achieve objectives within the pillars. This report evaluates opportunities for improvement, and identifies deliverables and objectives, along with associated timeframes. Much of the design and implementation of this work is carried out by the volunteer members of Catholic Health’s health equity taskforce, referred to as the Health Equity Leadership Council (HELC). With representation from all campuses and major departments, the HELC and its four subcommittees continued to make great strides during their second year. These efforts are summarized in the Plan and the HELC is a vital source of objectives moving forward.
Much has changed since last year’s plan was released. One thing that has not changed is Catholic Health’s commitment to serving all of our patients, to help them live a life of wellness including successful preventive care and to assist in overcoming obstacles. Guided by our Ethical and Religious Directives we provide care for everyone, and as health equity is defined as the opportunity for everyone to achieve their highest level of health outcomes, our efforts continue and grow. This report summarizes the health equity efforts undertaken by Catholic Health and provides a strategic plan going forward.
Catholic Health’s Mission and Health Equity
As described in the definitions section which follows, health equity is defined as “the state in which everyone has a fair and just opportunity to attain their highest level of health. As a Catholic health care provider organization, Catholic Health is bound to follow the Ethical and Religious Directives for Catholic Health Care Services, 6th Ed. (ERDs), a book published by the United States Conference of Catholic Bishops. The ERDs guide us and not only support health equity work, but also require it. Catholic Health’s Mission aligns with the ERDs. As such, health equity is not seen as a political topic for debate. Rather, health equity simply refers to the care we provide, with an emphasis on ensuring that we care for the most vulnerable, with the goal that all patients have their best potential health outcome.
The most relevant ERD connecting with our mission is ERD#3: In accord with its mission, Catholic Health should distinguish itself by service to and advocacy for those people whose social condition puts them at the margins of our society and makes them particularly vulnerable to discrimination: the poor; the uninsured and the underinsured; children and the unborn; single parents; the elderly; those with incurable diseases and chemical dependencies; racial minorities; immigrants and refugees. In particular, the person with mental or physical disabilities, regardless of the cause or severity, must be treated as a unique person of incomparable worth, with the same right to life and to adequate health care as all other persons.
Further, following these directives are mandatory for Catholic health care providers as expressed in ERD #5: Catholic Health care services must adopt these directives as policy, require adherence to them within the institution as a condition for medical privileges and employment, and provide appropriate instruction regarding the directives for administration, medical and nursing sta and other personnel.
Caring for our patients and helping them achieve their highest health outcomes remains our objective. This Health Equity Strategic Plan is based on the tenets of our mission and follows the requirements of being a Catholic health care provider. Deliverables described within this plan are reported and discussed at Mission and Ministry Committee meetings. This written Strategic Plan is presented to the Board of Directors for approval via the Quality Management Committee meeting (QMC).
Key definitions
Health equity
Catholic Health defines health equity using the Centers for Disease Control and Prevention’s (CDC) definition: “Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health.” Catholic Health also ascribes to the CMS advancement of health equity actions including:
• Identify health disparities.
• Define specific and actionable goals for addressing any disparities identified.
• Prioritize populations and communities that are historically underserved.
• Establish and implement their organization’s health equity strategy.
• Determine what tools and resources their organization needs to implement its strategy.
• Monitor and evaluate progress in addressing health disparities.
Priority populations
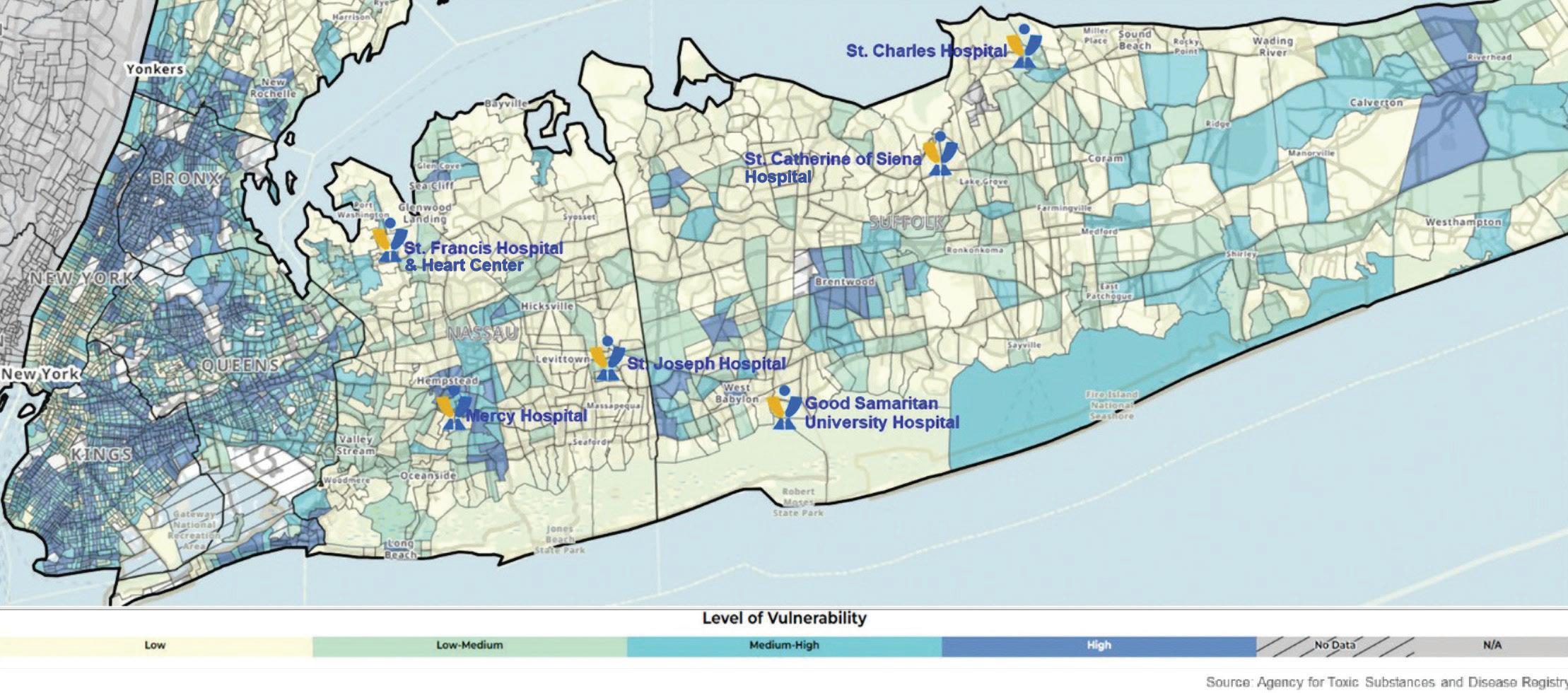
Catholic Health serves a diverse population across Long Island. Our patients, who represent nationalities from all across the world, speak more than a dozen primary languages. In evaluating population health and demographics on Long Island, including race, ethnicity and language data, along with geography (see figures 1.1.1–1.3.1), Catholic Health’s equity strategy defines the system-wide priority population as those living in zip codes with the highest quartile of social vulnerability, as defined by the Social Vulnerability Index (SVI). The highest SVI quartile represents approximately 15% of our patient population and significant health disparities can be found when comparing the highest quartile to the rest of our patients (see figure 2.0).
Social Determinants of Health (SDOH)
Social Determinants of Health (SDOH) are the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, worship and age. This includes but is not limited to factors including economic, environmental, built environment, literacy and access to healthy food.
Social Vulnerability Index (SVI)
The SVI is a database of the CDC and Agency for Toxic Substances and Disease Registry (ASTDR), which refers to “the resilience of communities (the ability to survive and thrive) when confronted by external stresses on human health.” There are 16 factors that are formulated into a geographic map of social vulnerability, including demographics (e.g., race and ethnicity, socioeconomics) and numerous SDOH (e.g., housing situation and transportation access).
REaL
The term REaL refers to data collected on race, ethnicity and preferred language. Appropriate collection of demographic data plays a key role in understanding health equity. Both CMS and the American Hospital Association (AHA) have published numerous points of information emphasizing the need to collect REaL data. As explained by the AHA, “collecting and stratifying patient REaL data are crucial for hospitals and health systems to understand the populations they serve and to implement the appropriate interventions for improving quality of care.”
New York State 1115 Medicaid Waiver
New York State approved the 1115 Medicaid Waiver and the waiver period began on April 1, 2024. The Waiver period runs through March 31, 2027. New York State has chosen nine Social Care Networks (SCN) to administrate the Waiver over nine regions. The Health and Welfare Council of Long Island (HWCLI), longtime partners of Catholic Health, have been chosen as the SCN of Long Island. The main goal of the Waiver will be to address SDOH in Medicaid patients, and connect them to ongoing social services through community based partners. The resulting improvement in health outcomes, and decrease in preventable downstream health care utilization, are the long term justifications for the project. Catholic Health is actively participating as screeners for SDOH.
Equity as the central theme of the Community Health Roadmap
In 2022, Catholic Health established a Community Health Roadmap, which incorporates health equity into every aspect. This roadmap describes specific objectives and action steps that will guide Catholic Health along the health equity journey. The specific pillars, objectives and system action steps to improve health equity are presented.
Pillars of community health on the equity journey
Organizational culture, systemic integration & education
Catholic Health is working to incorporate an improved organizational culture of health equity system-wide. Educating more than 17,000 employees at Catholic Health on the tenets and practices of health equity was achieved through numerous in-service and educational objectives. Since the launch of our health equity initiative in early 2023, we have successfully trained over 4,300 new employees during the system-wide orientation on the fundamentals of health equity. This foundational training is part of our commitment to create an inclusive health care environment that recognizes and addresses disparities in care. The goal is to ensure that all employees receive comprehensive education on essential topics, including unconscious bias, SDOH and health equity principles. The Education subcommittee of the HELC has developed a robust educational framework. This includes mandatory learning modules and resources that employees must complete. This prioritizes ongoing professional development aimed at fostering a culture of continuous learning and improvement in health equity practices.
Organizational culture, systemic integration and education
Social determinants of health
Data analytics and strategic planning
Equity programs must be based on appropriate collection, stratification and analysis of demographic and epidemiologic outcome data. It is imperative to improve the collection of REaL data to identify health disparities. The most appropriate geographic data (i.e. census tract, zip code, or SVI data) will be used to identify community needs and vital stakeholders, resources and strategic initiatives to decrease health disparities. Led by our Director of Epidemiology and Public Health Analytics, and with the incredible support of the Digital Transformation Systems (DTS) team, a new SDOH Dashboard has been launched to help ensure that all Catholic Health practitioners have access to the actual data within the communities they serve, so they can appropriately gear efforts at preventive health.
Screening for SDOH using the New York State Accountable Health Communities (NYSAHC) tool became the standard of care at Catholic Health, and a subsequent resource Database in Epic is expected to be activated soon to ensure there are resources for providers to offer to those who screen positive. Continual improvement in collection, stratification and analysis of data is paramount for any health equity program.
Community engagement/participation
Community member participation in their own health care will ultimately lead to improved outcomes. Access to care is a key component of achieving participation in care and outcome measures will be used to assess internal efforts at community engagement. Targeted community engagement based on statistical needs, health disparities and outcome measures, ensures the tenet that we provide tailored services to individuals and communities, with emphasis on serving the most at-risk. This aligns with our definition of health equity.
To help meet our goal of gaining community member participation in their own health care, we have numerous active initiatives in progress. This includes but is not limited to our speakers’ bureau (can present in 26 different languages), our telehealth access initiative at St. Brigid’s Parish, the growth of community health workers screening for SDOH, alignment and re-routing of our two Community Outreach buses to meet the needs of specific communities (with addition of bilingual social workers on the buses to help with insurance enrollment for those eligible), and hundreds of community health screening, education and resource-oriented events across Long Island.
Social Determinants of Health (SDOH)
Catholic Health supports a strategy of “well care” over the more traditional “sick care” often offered by hospitals and hospital systems. In our model of well care, addressing the SDOH as a means of helping people stay healthy and out of the hospital is a guiding principal. More than 80% of a person’s health outcomes are not clinical, but rather, are based on the social drivers and influences in their lives, along with their genetics. While we cannot alter genetics, Catholic Health endeavors to improve the controllable social drivers that lead positively to health, and negatively to illness and diseases, often chronic in nature. To launch Catholic Health’s work in this realm, in 2022, we launched a Food Insecurity Screening Program in all six of our Emergency Departments (ED). The initiative consists of screening all patients coming into the ED with the “Hunger Vital Signs,” published by the CDC. What differs this award-winning program from many others is that anybody who screens positive is provided with a “foodto-go bag” to ensure they do not go home to an empty kitchen. While that bag is only meant to cover food needs over the first couple of days post-discharge, social work teams spend those days addressing the social service need and ensuring ongoing food and nutrition services are implemented.
Food insecurity is not the only important SDOH and over the past year, Catholic Health has taken the major step of incorporating the New York State Accountable Health Communities (NYSAHC) social determinant screening tool as standard of care for all patients admitted to our hospitals. Further, we began the difficult task of preparing and providing a community resource data base which will be available in our Electronic Health Record (Epic) for all of our providers to use as a resource when patients screen positive. Practicing “well-care” will not be successful if we do not acknowledge the role of non-clinical and social factors. This brings us into realms outside of our book of business, so community collaboration is vital. Partnering with Community-Based
Organizations (CBOs) is a vital component of achieving health equity and meeting the SDOH needs of our patients. Catholic Health has established strong relations with the Health and Welfare Council of Long Island (HWCLI), including representation on the SCN governing body for the New York State 115 Medicaid Waiver, which is hosted by HWCLI. This helps us connect with many of the CBOs they represent.
All of this leads to helping patients proactively stay healthy and well, avoiding unnecessary hospitalization.
Quality and Patient Experience
Catholic Health values quality to the point that “there is no quality without equity.” As such, equity is to be treated with quality metrics and measures, and performance is to be evaluated in an ongoing fashion. The HELC is establishing quality metrics and measures, staff is being trained and there will be a culture of accountability for the results. Ensuring that we meet our patients’ needs, including their cultural and religious needs, is paramount in our patient experience strategy. Factors such as communicating with patients in their preferred language, is an example of the intersection of equity, patient experience and quality. Outcomes are impacted by a patient’s comprehension of medical discussions.
The intersection of health equity and quality is so important that the formal reporting of the minutes of the HELC is part of the system-wide QMC (a Board of Directors level meeting), and the HELC Chairman presents a report on equity activities at the meetings. This year’s Health Equity Strategic Plan represents increased collection, stratification, and analysis of data metrics as it relates to quality and patient experience. As an example, ensuring that we communicate with patients in a way they understand will surely lead to improved outcomes and decreased negative quality indicators.
Regulatory requirements
Catholic Health diligently monitors and updates new procedures and reporting regulations from major oversight, regulatory and evaluative bodies, including but not limited to CMS, the Joint Commission and Leapfrog. Training staff in new rules and reporting requirements is embedded in equity metrics and training.
Catholic Health strives to achieve the highest scores on reviews, meet all emerging measures and reporting requirements, and comply with new imperatives as it relates to health equity, health disparities, evaluation and any identified necessary corrective measures.
Health Equity Leadership Council (HELC)
Catholic Health has established a multidisciplinary system-wide HELC to further the mission of Catholic Health and its affiliated entities. The Council shall champion and steward the system’s continued advancements in health equity for its patients, its employees and the Long Island community in a manner consistent with the system’s responsibilities under state and federal law, and the ERDs for Catholic health care services as interpreted and applied by the Bishop of the Diocese of Rockville Centre.
Catholic Health defines “health equity” as being achieved when every person has a fair and just opportunity to attain his or her highest level of health. Specifically, Catholic Health is dedicated to ensuring, insofar as it depends on the system, that excellent health outcomes are available to every person who presents at one of the system’s facilities or physician practice locations, notwithstanding social, political, economic or other conditions that commonly result in and perpetuate injustice or inequity among individuals.
The six-pronged mission of the Council is as follows:
• Establish Catholic Health as the most trusted health care system on Long Island by its dedication to justice in the system’s delivery of health services.
• Align the system with its Catholic Mission to reach and serve all communities, especially the most vulnerable, through the stewardship and deployment of its resources for the advancement of health equity.
• Increase, improve and leverage community relationships and partnerships to inspire, empower and sustain individuals to augment their health.
• Integrate consideration of health equity into all aspects of the system’s operations.
• Address and ameliorate SDOH to improve overall health outcomes and decrease unnecessary hospital admissions and readmissions.
• Meet emerging regulatory and industry requirements relative to health equity.
Subcommittees of the Council
Scope by Subcommittee
• Catholic Health First: Address health equity related needs, objectives and deliverables within the workforce and walls of Catholic Health.
• Education: Address education and training, disseminate information and raise awareness of equity activities, system initiatives and regulatory.
• Long Live Long Island: Address community partnerships, patient engagement and social drivers.
• Quality and Data Analytics: Address screening tools, epidemiology and digital optimization for information collection and messaging.
Summary of year’s results by subcommittee
Catholic Health First (Paul Stuart, Chair)
Completed objectives:
• Evaluated and selected the eCornell equity-related certificate program as the foundational training for building our Health Equity Champion network.
• Graduated first cohort from the eCornell certificate program and secured funding for the second cohort in 2026.
• Identified four questions on the annual employee engagement survey to track as a measure of how our employees are feeling about belonging at Catholic Health as it relates to health equity.
• Compiled childcare resources available to our employees in one convenient location on the Catholic Health intranet.
• Increased employee awareness of the Employee Crisis Fund through incorporating it into the New Employee Orientation.
Ongoing objectives:
• Leverage the eCornell certificate program to establish and grow our campus equity champion network.
• Track engagement survey results related to health equity.
• Ensure our employees are aware of existing public and private childcare resources available to them.
• Increase visibility, accessibility and utilization of existing Catholic Health programs and offerings that support the health and welfare of our workforce.
Future objectives:
• Establish a formalized internal pathway for employees in crisis to follow in order to access assistance and resources.
– Leverage our internal Care Management expertise to support our employees in crisis through providing intake and referrals services.
• Leverage our Health Equity Champion network to gather deeper insight from our employees regarding our engagement survey results.
• Collaborate with the Long Live Long Island subcommittee to foster community relationships that support our recruitment strategy.
• Partner with our Center for Performance Excellence to increase awareness and utilization of existing Catholic Health programs and offerings that support career development and advancement.
Education subcommittee (Annmarie Smith and Dilys White, MD, Co-Chairs)
Completed objectives:
• Develop education programs that cover SDOH, implicit bias, cultural appropriateness and health equity frameworks.
– Inclusive Leadership Behavior workshop.
– Managing Difficult Conversation workshop.
• Require employee participation in continuing education sessions focused on health equity.
– Unconscious Bias online module, launched April 2024, refreshed April 2025.
– Health Equity education for new employees, implemented in 2023.
– SDOH education, launched 2024 and expanded January 2025.
• Expand GME curriculum.
– Education on health equity, and SDOH has been integrated into the physician resident program at Good Samaritan University Hospital and throughout the system.
• Activate Internal Speakers Bureau (equity education, system orientation speakers).
• Create an educational library on topics related to Health Equity (Catholic Health Academy).
Future objectives:
• Regularly evaluate the effectiveness of health equity education programs and make adjustments based on feedback and outcomes.
– Create tailored learning modules for different roles within the health care system.
• Support the Catholic Health first subcommittee with the Health Equity Champions Program. Equity Champions completed Cornell’s certificate program.
• Incorporate topics of health equity, SDOH and inclusive behaviors into the GME Series.
• Collaborate with educational institutions to improve learning resources.
Long Live Long Island (Lisa Santeramo, Chair)
Completed objectives:
• Established a Speakers Bureau: Currently 26 languages able to be presented by Catholic Health staff: Arabic, Bengali, Chinese, Creole, English, Filipino, French, German, Greek, Hindi, Italian, Korean, Malayalam, Mandarin, Polish, Portuguese, Punjabi, Romanian, Russian, Spanish, Tagalog, Tamil, Telugu, Turkish, Ukrainian and Urdu.
Ongoing objectives:
• Curate equity-specific community events based on data and mission.
• Expand collaboration with CBOs.
• Seek community grants in alignment with key equity priorities.
Future objectives:
• Volunteer Recruitment: Collaborate with the Human Resources Committee to create a system-wide program to better recruit employees for volunteer community outreach and speaking opportunities. This will enable Catholic Health to expand our reach within vulnerable communities.
• CBO Partnerships:
– Utilizing the listening session data: Identify and engage potential community partners that will support our mission goals.
– Bandwidth analysis: Establish internal mechanisms and processes to manage external partner relationships and address potential bandwidth challenges.
• Physician Partners and IPA synergy:
– Map practices with Health Equity focus
Develop and maintain an inventory of Catholic Health employed practices, facilities, and associated voluntary practices that either (a) operate a health equity initiative or (b) serve a patient panel with at least [20]% Medicaid or uninsured patients.
– Engage in listening sessions
Conduct structured listening sessions with leaders and frontline staff from the identified practices/facilities from item (i) to document their experiences and strategies in addressing social drivers of health outcomes.
– Align with Community Outreach
Identify actionable opportunities to align practice-level health equity and SDOH efforts with Catholic Health’s existing community outreach programs, with recommendations for cooperation and integration.
Data and Quality subcommittee
(Monique Ford and Jason Tagliarino, Co-Chairs)
Completed objectives:
• Establish and deploy system-wide SDOH screening tool.
• Expand SDOH mandatory education to Catholic Health employees.
• Develop an SDOH dashboard with stratification by unit and demographic information.
• Stratify patient experience data by demographic information with key improvement targets.
Ongoing objectives:
• Expand SDOH to all hospital outpatient departments and patient self-service during e-Check in.
• Implement action plans related to enhanced health equity data reporting to site to develop tailored action plans to address these gaps.
• Ensure equitable access to age-friendly care by systematically identifying and addressing the unique social, cultural, and clinical needs of diverse older adult populations, with the aim of reducing disparities in health outcomes and improving quality of life across all demographic groups.
• Implement the Epic Community Resource dashboard to track the most common resources recommended.
• Enable community resource directory in MyChart.
Future objectives:
• Implement new Epic encounter level dashboard to assess encounter-level instead of patient-level screening rates for SDOH. Compare screening and positivity rates across encounter types and combinations of departments and providers, and use metrics related to the specific questionnaires and modes of screenings to find factors contributing to success.
• Extract SDOH from notes using generative AI: Keep patients from falling through the cracks. Use generative AI to process visit notes and identify potential SDOH concerns. When the AI detects a risk, inline reminders prompt clinicians to complete a formal screening, which helps them ensure that patients can receive assistance and helps make your population-level reports more accurate.
• SDOH interventions shown front and center so that clinicians, care managers, community health workers, and others can see a full picture of how a patient’s social needs are being addressed. Social drivers include more information about interventions, such as whether an intervention might be needed, is in progress, or is not requested. They also show orders, procedures, and referrals that address a domain in addition to the Compass Rose Programs and community resource recommendations that already appear.
Demographics of Catholic Health’s patients
The following data are based on patient encounters from January 1, 2024 to December 31, 2024.
CHS System All Pts
Catholic Health’s Patient Population Overview
Patient race Figure 1.1.1: Patient race for all patients 18 years and older who had an encounter in 2024 (N=576,412). Source: Epic
Some
No answer/unknown
Preferred language Figure 1.3.1: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=576,412). Source: Epic
or Latino
No answer/ unknown
Ethnicity Figure 1.2.1: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=576,412). Source: Epic
CHS System Hosp Admiss
Catholic Health’s Hospital Admissions Patient Population Overview
Patient race Figure 1.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=75,278). Source: Epic
Ethnicity Figure 1.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=75,278). Source: Epic
Some other race
No answer/unknown
Preferred language Figure 1.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=75,278). Source: Epic
CHS System
ED Admiss
Catholic Health’s Emergency Department Patient
Population Overview
Patient race Figure 1.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=139,409). Source: Epic
Preferred language Figure 1.3.3: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=139,409). Source: Epic
Ethnicity Figure 1.2.3: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=139,409). Source: Epic
2020 Social Vulnerability Index by Census Tract for Queens, Nassau and Suffolk
Figure 2.0: SVI by Census Tract for Catholic Health service areas. Source: Epic
Identified System-wide Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. Statistical significance was considered to be a p-value of less than 0.05. If no statistically significant differences were found it is denoted by an asterisk (*).
All data were obtained through Epic and include all patients with any encounter in the Catholic Health System from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth. For the influenza vaccination measure, the time period followed the ’24 – ’25 flu season (August 1, 2024 –July 31, 2025).
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications. These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024.
Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Body Mass Index (BMI)
Table 1.1: Percent of patients 18 years and older with a BMI >25 by SVI
Source: Epic
Table 1.2: Percent of patients 18 years and older with a BMI≥25 by race
Source: Epic
Table 1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source: Epic
Table 1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language Source: Epic
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women that had an encounter with Catholic Health in 2024.
Table 2.1: Percent of patients 40– 75 years with a Breast Cancer screening by SVI Source: Epic
Table 2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 2.3: Percent of patients 40 –
Table 2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by preferred language Source: Epic
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provider documented in the electronic health record during 2024.
Table 3.1: Percent of patients 18 years and older with a PCP by SVI Source: Epic
Table 3.2: Percent of patients 18 years and older with a PCP by race Source: Epic
Table 3.3: Percent of patients 18 years and older with a PCP by ethnicity Source:
Table 3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
Table 4.2: Percent of patients 60 years and older with an
Table 4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
Table 4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic SVI
(zip code) Low
St.
Table 5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic OMB Race White Black or African American Asian
Table 5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic
5.4:
Good Samaritan University Hospital Health Equity Strategic Plan
A note from the President
Dear Colleagues,
Catholic Health defines health equity using the Centers for Disease Control and Prevention’s (CDC) definition—the state in which everyone has a fair and just opportunity to attain their highest level of health. As a faith-based institution, Good Samaritan University Hospital, the flagship for Catholic Health in Suffolk County, has a long-standing tradition of community outreach and support to areas that are underserved, have a high level of social determinants of health (SDOH) and historically, have barriers to accessing quality health care. This has been accomplished through direct outreach programs within areas of uninsured and underinsured residents, programs held local to the hospital, as well as collaborating with other not-for-profit organizations, municipalities and governmental agencies with similar goals. By providing a high level of education, robust screenings and vaccinations, Good Samaritan continues to impact the lives of all throughout the south shore of Suffolk County, bringing the theory of health equity to realization.
By identifying health disparities within various regions of Suffolk County, Good Samaritan’s Public and Community Relations Department is able to evaluate and assess the services needed for specific populations. Understanding that needs may vary between communities, Good Samaritan works closely with partners such as the Nassau-Suffolk Hospital Council, Suffolk County Department of Health and the Towns of Islip and Babylon to develop data-driven strategies and programs. One highlight of these partnerships was the hospital’s response to the COVID-19 pandemic. Good Samaritan provided both testing and vaccinations within the hamlet of Brentwood, one of the largest hamlets in New York State with more than 65,000 residents, many of whom are identified as being under the poverty-level. During the pandemic, Brentwood was a concentrated area of COVID positive residents, due to lack of access to health care, education and cultural differences from surrounding zip codes. Working with New York State and the Town of Islip at two different clinical locations, Good Samaritan assisted in providing nearly 80,000 residents with COVID testing, vaccinations and education in both English and Spanish.
Since the pandemic, Good Samaritan has continued to embed itself within the community, regularly hosting screening, education and vaccination events to communities of all needs and resources, with the goal of equal access to health care services for all. Physicians, nurses and support staff consistently volunteer their time and skills to help those in need, many of whom are their neighbors, family and friends. Through this outreach, we work together as one community to come ever closer to our goal of health equity for all.
Sincerely,
Justin Lundbye, MD, MBA, FACHE President, Good Samaritan University Hospital
Good Samaritan University Hospital Health Equity Activities
In your community 2025
Good Samaritan University Hospital has a consistent focus on caring for its communities and local residents. It is the foundation of the hospital, named after the well know biblical story of a samaritan providing assistance to an unknown traveler. Many who work at Good Samaritan also live in the area and take pride in helping their “neighbors,” many of whom are in need and have a lack of access to health care services. Through the hospital’s Public and Community Relations Department, both clinical and nonclinical staff are able to provide their time to assist at a number of events, lectures, educational symposiums, screenings, vaccination clinics and more. The goal is to reduce the barriers in accessing health care for all.
With the goal of intervening in areas that are identified as being impacted by high levels of SDOH, Good Samaritan focused on increasing flu vaccinations, breast screenings and educating patients without a primary care physician for its 2025 strategy plan. To impact these metrics, resources and efforts were shifted to allow for more screenings, vaccination clinics and events.
Historically, Good Samaritan provided two to three vaccination events related to influenza in the local community, often partnering with local municipalities. In 2025 through the first quarter of 2026, to intervene in the identified issue, Good Samaritan has already scheduled multiple flu shot clinics located throughout the hospital’s service area, with a focus on underserved communities. These clinics are in partnership with a number of community stakeholders and the Town of Islip and Babylon, who assists us in promotion of these events to those in need.
Good Samaritan was ground zero in the battle against breast cancer, being the location of one of the first mapping projects and identified cancer clusters in the United States. With an offsite Women’s Imaging Center, a robust Breast Health Center, the site of the Catholic Health Cancer Institute at Good Samaritan and strong partnerships with local breast cancer coalitions, the
hospital has been an early mover in providing the highest level of breast health care. This continues into the community outreach space where historically, two open house breast screening events were held annually. In 2024 and 2025, this was increased to four events and also included access to transportation through Uber Health for those who faced this social determinant. This service, though, went underutilized due to compliance issues in promoting transportation provided by the hospital to the public. This is in discussion with both our legal and compliance department to determine new ways to promote transportation services. Those without insurance were provided their screening through our partnership with the Cancer Services Program of Western Suffolk. Any patients found to have a positive test result were then paired with appropriate resources. Additional events focused on breast health education and early detection were also held with more being scheduled through the remainder of the year.
Good Samaritan treats more than 90,000 patients annually through its Emergency Department, which features a verified adult and pediatric trauma center, separate pediatric emergency department, a Geriatric Fracture Program and was recently recognized as a Geriatric Emergency department. It provides connections to high level hospital services including the Gary H. Richard and Family Stroke & Brain Aneurysm Center of Long Island and St. Francis Heart Center. Many of those who come through the Emergency Department doors are uninsured or underinsured and use this department as their source of primary care. During intake, patients are asked if they have a primary care physician, and if not, are provided a referral for one. This occurs through a new referral office through the hospital’s E-PACED program, as well as at the bedside prior to discharge. As an extension of this, Good Samaritan has developed a flyer that includes a focus on primary care providers and promotes those locations at all events within its service area. This allows for direct education on primary care providers local to the resident, in their community.
Demographics of Good Samaritan University Hospital patients
The following data were obtained from Epic and includes all patients who had an encounter with Good Samaritan University Hospital from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health. Patients who died during or prior to 2024 were excluded from the sample.
GSUH System All Pts
Good Samaritan University Hospital’s Patient Population Overview
Patient race Figure 3.1.1: Patient race for all patients 18 years and older who had an encounter in 2024 (N=152,686). Source: Epic
Preferred language Figure 3.3.1: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=152,686). Source: Epic
Ethnicity Figure 3.2.1: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=152,686). Source: Epic
GSUH System Hosp Admiss
Good Samaritan University Hospital’s Admissions Patient Population Overview
Patient race Figure 3.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=23,667). Source: Epic
Preferred language Figure 3.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=23,667). Source: Epic
Ethnicity Figure 3.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=23,667). Source: Epic
GSUH System ED Admiss
Good Samaritan University Hospital’s Emergency Department Patient Population Overview
Patient race Figure 3.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=52,261). Source: Epic
Preferred language Figure 3.3.3: Preferred language for all patients 18 years and older who had an emergency department encounter in 2024 (N=52,261).
Source: Epic
No answer/ unknown
Ethnicity Figure 3.2.3: Patient ethnicity for all patients 18 years and older who had an emergency department encounter in 2024 (N=52,261). Source: Epic
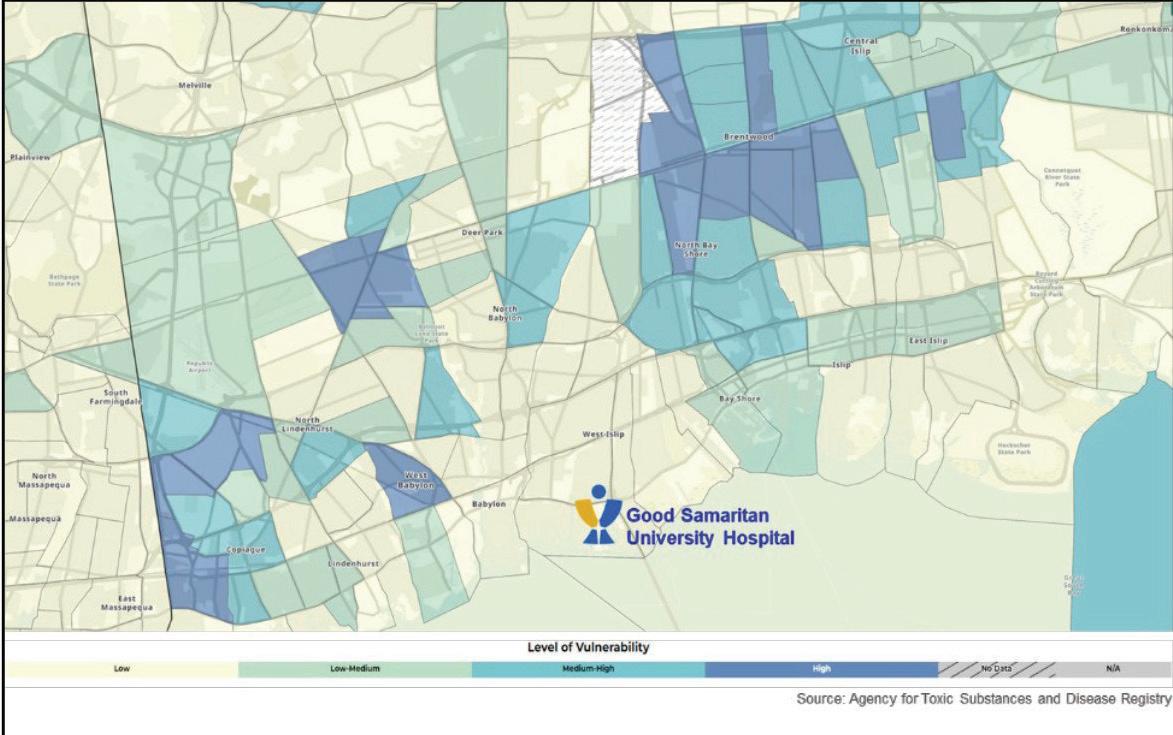
SVI
by Census Tract for Good Samaritan University Hospital Service Areas
Figure 4.0: SVI by Census Tract for Good Samaritan University Hospital service areas. Source: Epic
Good Samaritan University Hospital Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant. All data were obtained through Epic and include all patients with any encounter at Good Samaritan University Hospital from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth. For the influenza vaccination measure, the time period followed the ’24 – ’25 flu season (August 1, 2024 – July 31, 2025).
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024.
Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Body Mass Index (BMI)
Table 6.1.1: Percent of patients 18 years and older with a BMI ≥25 by SVI Source: Epic SVI 2020 overall percentile (zip code)
Table 6.1.2: Percent of patients 18 years and older with a BMI ≥25 by race Source: Epic
Table 6.1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source: Epic
Table 6.1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language Source: Epic Languages
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 6.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic
Table 6.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 6.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening by ethnicity Source: Epic
OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Table 6.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by language Source: Epic
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provided documented in the electronic health record during 2024.
Table 6.3.1: Percent of patients 18 years and older with a PCP by SVI Source: Epic SVI overall
(zip code)
Table 6.3.2: Percent of patients 18 years and older with a PCP by race Source: Epic
Table 6.3.3: Percent of patients 18 years and older with a PCP by ethnicity Source: Epic
Table 6.3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 6.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
Table 6.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 6.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
Ethnicity
Table 6.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Language English Spanish Other languages
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 6.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic
Table 6.5.2: Percent of patients 18 years and older with an
visit or physical exam by race Source: Epic
physical exam with AWV/ physical exam
Table 6.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic
OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Measures % patients with AWV/ physical exam # patients with AWV/ physical exam
Table 6.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by preferred language Source: Epic
Language English Spanish Other languages Measures % patients with AWV/ physical exam # patients with AWV/ physical exam
with AWV/ physical exam # patients with AWV/ physical exam
Market-specific Priority Population Equity Action Plan for Good Samaritan University Hospital
Below, please find the health disparities the hospital will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity: % patients with flu vaccine 60+
Identified intervention
• Increase in flu shot clinics in strategic locations.
Owner
• Public and Community Relations.
Key stakeholders
• Underserved community members who are highly vulnerable in target communities: Brentwood, Bay Shore and Central Islip.
Key milestones
• September: Brentwood Flu Clinic.
• October: Senior Center Flu Clinics/ TOI Employee Flu Clinic/ St. John the Baptist DHS Employee Flu Shot Clinic.
• 4th QTR 2025/1st QTR 2024: other targeted Senior Centers.
• November: Other targeted Senior Centers.
• February/November: Bay Shore Mall.
• 2026: Health Education Events in Partnership with Sen. Alexis.
Timeline to completion
• January 2026
Resources
• Administration, Pharmacy (vaccine), Public and Community Relations (promotions), Volunteer Clinicians, local partners.
Measures of success
• Goal: 5% increase in flu shots in highly vulnerable populations.
• Reach: 8% increase in highly vulnerable populations.
Health disparity: % patients with no Primary Care Physician (PCP)
Identified intervention
• Increase referrals to PCP from the emergency medicine population.
Owner
• Patient Access, Care Managers.
Key stakeholders
• Underserved community members who are highly vulnerable in target communities: Brentwood, Bay Shore and Central Islip.
Key milestones
• ED, Inpatient, Diabetes Education Center and PCP encounter.
• Opening of Patient Referral Office in the Emergency Department (E-PACED Program).
• Distribution and Education of PCPs within the Good Samaritan service area at health screenings and events.
Health disparity: % patients with breast cancer screening
Identified intervention
• Increasing the number of patients who have a breast screening through increased screening events and promotion to targeted stakeholders.
Owner
• Patient Access, Care Managers.
Key stakeholders
• Underserved community members who are highly vulnerable in target communities: Brentwood, Bay Shore and Central Islip.
Key milestones
• May: Women’s Health events; Mother’s Day.
• October: Breast Health Awareness Month, Breast Health Community Lecture, Pink Flags Celebration and Education Event.
• Radio/TV Interviews—Breast Surgeon Dr. Sophia Fu.
• Additional screening events in subsequent months.
• Promotion of transportation services to Imaging Center through key partners and stakeholders.
Timeline to completion
• January 2026
Resources
• Patient Access, Emergency Department Staff, Catholic Health Central Referral Office (CRO), Public and Community Relations (promotions), local partners, Huron Team.
Measures of success
• Goal: 5% increase in flu shots in highly vulnerable populations.
• Reach: 8% increase in highly vulnerable populations.
Timeline to completion
• January 2026
Resources
• Women’s Imaging Center, Catholic Health Physician Partners Breast Surgeons, Public and Community Relations (promotions), local partners.
Measures of success
• Goal: 5% increase in flu shots in highly vulnerable populations.
• Reach: 8% increase in highly vulnerable populations.
Mercy Hospital Health Equity Strategic Plan
A note from the President
Dear Colleagues,
Welcome to Mercy Hospital. As the President of Mercy Hospital, it is my honor to welcome you to a community deeply committed to providing exceptional health care while placing diversity, equity and inclusion (DEI) at the core of everything we do. At Mercy, we recognize that our strength lies in the diversity of our patients, staff, and the community we serve, and we are dedicated to fostering an inclusive environment where everyone feels valued, respected and cared for.
We are committed to ensuring that every individual who walks through our doors receives compassionate, high-quality care that is equitable and tailored to their needs. This commitment to health equity is evident in our daily practices and the initiatives we champion. We continually monitor and address health care disparities through disparity-driven quality improvement, such as enhancing primary care access, flu vaccinations and routine health screenings. These efforts are aimed at identifying and closing gaps in care, especially for underserved populations.
Mercy also integrates social determinants of health (SDOH) assessments into patient care to address factors like housing, food security and employment, which significantly impact health outcomes. Our approach ensures that patients needing additional support are connected with resources and follow-up actions to improve their overall well-being.
Our commitment to DEI extends to our workforce as well. We are focused on building a diverse and inclusive staff that mirrors the community we serve, from front-line employees to leadership positions. By promoting diversity in our workforce, we ensure that our caregivers are both reflective of and responsive to the diverse needs of our patients.
At Mercy Hospital, we are not only a place for healing, but also a beacon of progress, dedicated to promoting health equity and creating a more inclusive future for all. We are proud of our role in advancing these goals and we look forward to working together to continue making a positive impact on the lives of those we serve.
Sincerely,
Joseph Manopella President, Mercy Hospital
Mercy Hospital Diversity, Equity and Inclusion Committee Charter
Mission Statement
The Mercy Hospital Diversity, Equity and Inclusion Committee (DEIC) is dedicated to fostering a culture of inclusivity, diversity and equity within the hospital. Our mission is to ensure equitable access to care, improve patient experiences, enhance workforce diversity and promote an inclusive environment for both staff and patients. Through collaborative efforts, we aim to identify, address and reduce disparities in health care outcomes and workplace experiences, ensuring that Mercy Hospital is a place where diversity is celebrated, and all individuals feel valued and respected.
Vision
Our vision is a hospital community that embodies diversity, equity and inclusion (DEI) in all aspects of its operations, from patient care to employment practices. We envision Mercy Hospital as a leader in providing equitable health care, fostering a diverse and inclusive workforce and setting a standard for DEI excellence in the health care industry.
Equity domains and objectives
Disparity-driven quality improvement and social determinant of health screening:
Objective: Regularly monitor and analyze quality metrics related to disparities in patient care, focusing on primary care physician (PCP) follow-up, flu vaccine uptake and annual physicals for patients engaging in health care with Mercy Hospital.
Strategies: Implement targeted interventions to address identified disparities, engage in continuous quality improvement processes and report progress to stakeholders. Engage team in DEI education and SDOH impact on patient care/outcomes.
Measures outcomes: 1) Audit compliance of quality metrics in addition to SDOH screening tool, 2) Track/trend the number of screen positive patients that receive referrals and action items, 3) Identify and address opportunities for improvement in disparity metrics.
Patient Experience (completed in 2025)
Objective: Assess and improve patient experiences by trending patient experience (PX) data based on demographics to identify disparities.
Strategies: Develop and implement strategies to enhance patient satisfaction and experience, especially among marginalized groups, through customized care approaches and patient engagement initiatives.
Measured Outcomes: 1) Track/trend demographic data in correlation with patient experience scores, 2) Analyze the use of translator/language assistance for non-English speaking patients.
Strategies: Provide ongoing training and support for staff on the SDOH tool, integrate SDOH assessments into patient care plans and monitor the impact on patient outcomes.
Human Resources
Objective: 1) Monitor trends in staff diversity and inclusivity, ensuring that Mercy Hospital’s workforce reflects the diversity of the community it serves, 2) Promote and retain diversity in front-line employees and leadership positions that mirror the patient population of Mercy Hospital.
Strategies: Implement recruitment, retention and professional development practices that prioritize diversity and inclusion, conduct regular assessments of workplace culture and address barriers to inclusivity.
Structure and membership
The DEIC will consist of members from various departments within Mercy Hospital, including but not limited to patient care, administration, HR and community outreach. Membership will be diverse in terms of professional background, race, ethnicity, gender and other characteristics to ensure a wide range of perspectives.
Meetings and communication
Small group subcommittees will conduct analysis of the selected equity domains. Each committee will meet monthly to review progress, discuss new initiatives and address challenges. The large DEI committee will meet on a bi-annual basis to conduct small group report out and large group discussions. Each small group is responsible for designing and implementation of performance improvement (PI) processes in each domain.
Accountability and reporting structure of the committee
The DEIC will report directly to the hospital’s performance improvement patient safety committee. An annual report summarizing progress, challenges and future plans will be provided to all stakeholders, including hospital staff, patients and the community. Ongoing education and outcomes will be periodically disseminated to in the Mercy Hospital monthly meetings.
DEIC Performance Improvement Projects 2025 – 2026
Project #1:
Analyze disparities as it relates to annual wellness exams
Overview: Our aim is to increase the number of patients who complete their annual physical examinations. Mercy Hospital has appointed our Primary Care Physician Champions in the Family Care Center to charge the initiative on creating a streamline communication process for achieving compliance with annual wellness visits.
Project #2
Action plans: Electronic reminders are sent to patients, notifying them of upcoming appointments, vaccination requirements, annual wellness examinations and permitting pre-registration.
Measured outcomes: We will measure the no-show rate, and appointment creation via SMS push rate before and after interventions. Additionally, we will also measure the increase in visit volume to assigned providers.
Assignment of a Primary Care Provider during acute hospitalization
Overview: Mercy Hospital has appointed a physician champion and Chief of Family Medicine to function in the capacity of the key liaison between inpatient and outpatient care. The physician champion will charge an initiate to create a referral stream for patients to follow up in the Family Care Center after acute inpatient stay.
Project #3
Action plans: Hospitalists are contacting the outpatient Family Care Center for warm handoff and set up of follow up appointments. We have also expanded out specialist access to this initiative to enhance our referrals.
Measured outcomes: We will measure the rate increase in referral traffic (inbound and outbound), and rate of Emergency Room (ER) utilization for extremely low acuity issues. We anticipate an increase in referrals to the clinic and decrease in ER utilization.
Improving Influenza Vaccination Rates in the Mercy Hospital Primary Care Clinic
Overview: Our aim is to increase the number of patients who complete their annual influenza vaccinations. Mercy Hospital has appointed our Primary Care Physician Champions in the Family Care Center to charge the initiative on creating a streamline communication process for achieving compliance with annual wellness visits.
Action plans: Electronic reminders are sent to patients, notifying them of upcoming appointments, vaccination requirements, annual wellness examinations and permitting preregistration. We will also update our community event calendar published with influenza pod dates.
Measured outcomes: We will measure the number of influenza vaccines given during the course of influenza season in comparison to prior years.
Demographics of Mercy Hospital patients
The following data were obtained from Epic and includes all patients who had an encounter with Mercy Hospital from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health. Patients who died during or prior to 2024 were excluded from the sample.
MH System All Pts
Mercy Hospital’s Patient Population Overview
Patient race Figure 5.1.1: Patient race for all patients 18 years and older who had an encounter in 2024 (N=66,718). Source: Epic
Some other race No answer/unknown
Preferred language Figure 5.3.1: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=66,718). Source: Epic
No answer/ unknown
Ethnicity Figure 5.2.1: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=66,718). Source: Epic
MH System Hosp Admiss
Mercy Hospital’s Hospital Admissions Patient Population Overview
Patient race Figure 5.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=10,411). Source: Epic
Preferred language Figure 5.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=10,411). Source: Epic
Ethnicity Figure 5.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=10,411). Source: Epic
Mercy
MH System ED
Hospital’s Emergency Department Patient Population Overview
Patient race Figure 5.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=22,461). Source: Epic
Some other race
No answer/unknown
Preferred language Figure 5.3.3: Preferred language for all patients 18 years and older who had an emergency department encounter in 2024 (N=22,461). Source: Epic
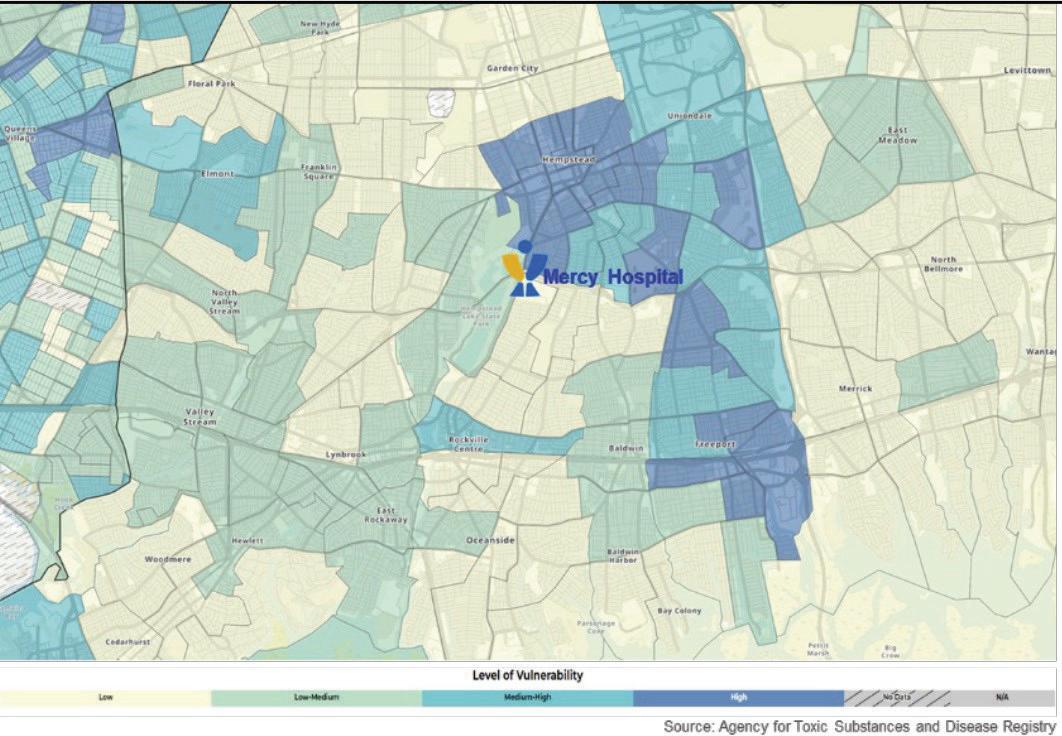
Social Vulnerability Index by Census Tract for Mercy Hospital Service Areas
Ethnicity Figure 5.2.3: Patient ethnicity for all patients 18 years and older who had an emergency department encounter in 2024 (N=22,461). Source: Epic
Hispanic or Latino
No answer/ unknown
Figure 6.0: SVI by Census Tract for Mercy Hospital service areas. Source: Epic Non-Hispanic or Latino
Mercy Hospital Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant.
All data were obtained through Epic and include all patients with any encounter at Mercy Hospital from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth.
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
Body Mass Index (BMI)
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024. Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Table 7.1.1: Percent of patients 18 years and older with a BMI ≥25 by SVI Source: Epic
SVI 2020 overall percentile (zip code) Low vulnerability High vulnerability
Table 7.1.2: Percent of patients 18 years and older with a BMI ≥25 by race Source: Epic
OMB Race White Black or African American Asian American Indian and Alaska Native Native Hawaiian and other Pacific Islander Two or more races
Table 7.1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source:
Table 7.1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language Source: Epic
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 7.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 7.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 7.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening by
Table 7.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by language Source: Epic Language English
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provided documented in the electronic health record during 2024.
Table 7.3.1: Percent of patients 18 years and older with a PCP by SVI Source: Epic
Table 7.3.2: Percent of patients 18 years and older with a PCP by race Source: Epic
Table 7.3.3: Percent of patients 18 years and older with a PCP by ethnicity Source: Epic
Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Table 7.3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic
Language
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 7.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic SVI overall percentile (zip code) Low
Table 7.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 7.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
Table 7.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Language
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 7.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic SVI
(zip code)
Table 7.5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic
with AWV/ physical exam
Table 7.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Table 7.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by preferred language Source: Epic
Language English Spanish Other languages
patients with AWV/ physical exam
patients with AWV/ physical exam
Market-Specific Priority Population Equity Action Plan for Mercy Hospital
Below, please find the health disparities the hospital will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity: Annual Wellness Visit (AWV) or physical examination
Identified intervention
• Electronic Notifications
Owner
• Catholic Health DTS Brian Massari
Key stakeholders
• Catholic Health DTS
• Mercy Hospital
Key milestones
• Electronic reminders will be sent to patients, notifying them of upcoming appointments, vaccination requirements, annual wellness examinations and permitting pre-registration.
Timeline to completion
• Rolling
Resources
Identified intervention
• Payer Partnerships
Owner
• Jeanine Cappello
• Chris Cells
Key stakeholders
• Mercy Hospital
• Managed Care Providers
Key milestones
• Healthfirst has dedicated office space in the Family Care Center to perform re-enrollments and assist patients whose Medicaid coverage has lapsed.
Timeline to completion
• Rolling
• Technology Resources
Measures of success
• No-show rates.
• Appointment creation via SMS push.
Health disparity: Flu vaccine
Identified Intervention
• Electronic Notifications
Owner
• Catholic Health DTS Brian Massari
Key stakeholders
• Catholic Health DTS
• Mercy Hospital
Key milestones
• Electronic reminders will be sent to patients, notifying them of upcoming appointments, vaccination requirements, and annual wellness examinations and permitting pre-registration.
Timeline to completion
• Rolling
• Office Space
Measures of success
• Increase in visit volume to assigned providers.
Identified Intervention
• Community Events
Owner
• Elizabeth Schwind
Key stakeholders
• Community Outreach
Key milestones
• Community event calendar published with influenza pod dates.
Timeline to completion
• Rolling Resources
• Technology Resources
Measures of success
• No-show rates.
• Appointment creation via SMS push.
• People
Measures of success
• Number of vaccinations given. (Note these are tracked manually, a process is needed to get these into our electronic health record).
Health disparity: Primary Care Physician (PCP)
Identified intervention
• Payer Partnerships
Owner
• Jeanine Cappello
• Chris Cells
Key stakeholders
• Mercy Hospital
• Managed Care Providers
Key milestones
• Healthfirst has dedicated office space in the Family Care Center to perform re-enrollments and assist patients whose Medicaid coverage has lapsed.
Identified intervention
• FQHC Alignment
Owner
• Chris Cells
Key stakeholders
• Mercy Hospital
• Harmony Health care
Key milestones
• Specialist access started (Q1 2024)— Endocrinology.
• Specialist access expanded (Q3 2024)— Pulmonology & Cardiology.
• Primary care access for uninsured (In process).
Identified intervention
• Parish Telehealth Initiative
Owner
• Christine Hendricks
• Dr. Lawrence Eisenstein
• Chris Cells
Key stakeholders
• Catholic Health
• Diocese of Rockville Centre
Key milestones
• Pilot program initiated at St. Brigid’s Parish (Q2 2024).
Timeline to completion
• Rolling Timeline to completion
Resources
• Office Space
Measures of success
• Reduction in lapsed Medicaid coverage (as noted by payer).
• Increase in visit volume to assigned providers.
• Rolling
Resources
• Physician Assignment
• Care Management
Measures of success
• Increase in referral traffic (inbound and outbound.
• Decrease in ER utilization for extremely low acuity issues.
Timeline to completion
• Rolling
Resources
• Technology
• Physician Assignment
• Care Management
Measures of success
• Service Utilization
St. Catherine of Siena Hospital Health Equity Strategic Plan
A note from the President
Dear Colleagues,
Welcome to St. Catherine of Siena Hospital. As President of St. Catherine of Siena Hospital, it is my honor and pleasure to inform and assure you of our unwavering commitment to health equity through the implementation of our strategic plan. As we strive to provide exceptional care for all members of our community, we recognize that achieving health equity is not just our goal—it is our responsibility. This plan is not just a document; it is a roadmap for action.
We are deeply committed to promoting health equity within our community. We recognize that health disparities exist and that systemic barriers often prevent individuals from receiving the care that they need. Our commitment is rooted in the belief that everyone deserves fair and just access to quality health care, regardless of their background. Some of the key initiatives of St. Catherine of Siena Hospital’s Health Equity Strategic Plan include:
• Actively engaging with diverse communities to help us better understand their needs and address health disparities.
• Promoting health equity by hosting community health fairs and providing free flu vaccines, blood pressure screenings, and a variety of resources, ensuring that everyone has access to essential health care services.
• Providing education about health resources, preventive care and healthy lifestyles to empower our patients and community members.
• Enhancing access to primary care physicians (PCP’s) in order to promote health equity and improve overall health outcomes.
• Screening patients who come through our emergency department for food insecurity. Patients identified are provided with “food-to-go” bags and our care management team provides additional referrals.
• Training our hospital staff in cultural competency to ensure that every patient feels respected and understood.
St. Catherine of Siena Hospital is fully committed to a future where every patient receives equitable care. Together, we can break down barriers and build a healthier community for all.
Sincerely,
Christopher J. Nelson President,
St. Catherine of Siena
Hospital
Demographics of St. Catherine of Siena Hospital patients
The following data were obtained from Epic and includes all patients who had an encounter with St. Catherine of Siena Hospital from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health. Patients who died during or prior to 2024 were excluded from the sample.
SCSH System All Pts
St. Catherine of Siena Hospital’s Patient Population Overview
Patient race Figure 7.1.1: Patient race for all patients 18 years and older who had an encounter in 2024 (N=62,049). Source: Epic
American Indian and Alaskan
Two or more races
Some other race
No answer/unknown
Preferred language Figure 7.3.1: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=62,049). Source: Epic
Non-Hispanic or Latino Hispanic or Latino
No answer/ unknown
Ethnicity Figure 7.2.1: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=62,049). Source: Epic
SCSH System Hosp Admiss
St. Catherine of Siena Hospital’s Hospital Admissions Patient Population Overview
Patient race Figure 7.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=8,224). Source: Epic
Preferred language Figure 7.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=8,224). Source: Epic
Non-Hispanic or Latino
unknown
Ethnicity Figure 7.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=8,224). Source: Epic
SCSH System ED
St. Catherine of Siena Hospital’s Emergency Department Patient Population Overview
Patient race Figure 7.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=16,787). Source: Epic
Ethnicity Figure 7.2.3: Patient ethnicity for all patients 18 years and older who had an emergency department encounter in 2024 (N=16,787). Source: Epic
Alaskan
Some other race
No answer/unknown
Preferred language Figure 7.3.3: Preferred language for all patients 18 years and older who had an emergency department encounter in 2024 (N=16,787). Source: Epic
Social Vulnerability Index by Census Tract for St. Catherine of Siena Hospital Service Areas
Figure 8.0: SVI by Census Tract for St. Catherine of Siena Hospital service areas.
Source: Epic
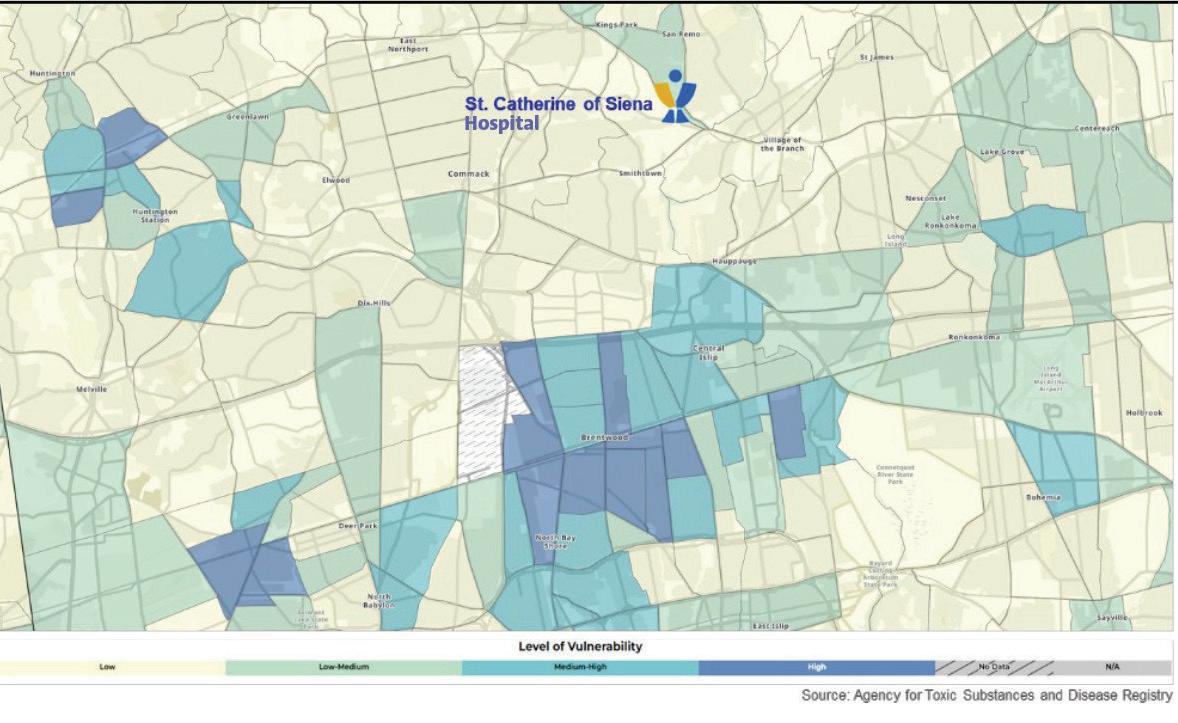
St. Catherine Of Siena Hospital Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant. All data were obtained through Epic and include all patients with any encounter at St. Catherine of Siena Hospital from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth. For the influenza vaccination measure, the time period followed the ’24 – ’25 flu season (August 1, 2024 –July 31, 2025).
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
Body Mass Index (BMI)
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024. Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Table 8.1.1: Percent of patients 18 years and older with a BMI ≥25 by SVI Source: Epic
2020 overall percentile (zip code)
Table 8.1.2: Percent of patients 18 years and older with a BMI ≥25 by race Source: Epic
Table 8.1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source: Epic
Table 8.1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language Source: Epic
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 8.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 8.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 8.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening
Table 8.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by language Source: Epic
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provided documented in the electronic health record during 2024.
Table 8.3.1: Percent of patients 18 years and older with a PCP by SVI Source: Epic SVI overall
Table 8.3.2: Percent of patients 18 years and older with a PCP by race Source: Epic OMB
Table 8.3.3: Percent of patients 18 years and older with a PCP by ethnicity Source: Epic OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Table 8.3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic
Language
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 8.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
(zip
Table 8.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 8.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
Table 8.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Language English Spanish
Other languages
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 8.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic
(zip code)
Table 8.5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic
physical exam with AWV/ physical exam
Table 8.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown Measures
patients with AWV/ physical exam # patients with AWV/ physical exam
Table 8.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by preferred language Source: Epic
Language English Spanish Other languages
patients with AWV/ physical exam # patients with AWV/ physical exam
with AWV/ physical exam
patients with AWV/ physical exam
Market-specific Priority Population Equity Action Plan for St. Catherine of Siena Hospital
Below, please find the health disparities the hospital will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity:
% patients with no Primary Care Physician (PCP)
Identified intervention
• Education.
• Patient access documentation.
• Epic BPA build for provider notification.
• Patient referral.
• Develop PCP/Clinic List for distribution
• Promote after hours support line.
Owner
• Laurie Yuditsky (VP of Quality)
Key stakeholders
• President
• CMO
• CNO
• COO
• ED Director
• Hospitalist Director
• Direct patient access
• TOC physician
• Care management
Key milestones
• Education provided.
Timeline to completion
• End of year 2026
Health disparity:
% patients 40 – 75 years with a breast cancer screening
Identified intervention
• Visit local Hispanic community centers to offer Breast Cancer screening education and to assist with making appointments.
Owner
• Laurie Yuditsky (VP of Quality)
Key stakeholders
• President
• CMO
• CNO
• COO
• Director of Radiology
• PR and Community Relations
• Breast Program Coordinator
Key milestones
• Develop multi-language educational materials.
• Identify community needs and groups to provide support to.
• Begin hosting informational services.
• Make patient appointments.
Timeline to completion
• End of year 2026
Health disparity: % patients with flu vaccine (60 & older)
Identified intervention
• Education.
• Hx of influenza vaccine documented in immunization history section of Epic.
• Provide additional flu pods to vulnerable populations within catchment area.
Owner
• Laurie Yuditsky (VP of Quality)
Key stakeholders
• President
• CMO
• CNO
• COO
• Director of Clinical Services
• Nursing Leadership
• PR and Community Relation
• Director Pharmacy
Key milestones
• Increase in outreach events during Fall/Winter 2025 – 2026.
Timeline to completion
• End of year 2026 Resources
• Patient access representative
• Catholic Health Physician Partners Resources
• Personnel
• Educational materials in various languages
• Appointment availability Resources
• Education
• Epic screen in ASAP
• Influenza vaccinations
Measures of success
• 10% reduction in disparity between high and low vulnerable population.
• Incremental increase in percentage of patients with a PCP.
Measures of success
• Number of outreach events.
• Appointments made.
• 10% reduction in disparity between high and low vulnerable populations.
Measures of success
• 10% increase in number of patients documented influenza vaccination.
• Additional flu pods.
St. Charles Hospital Health Equity Strategic Plan
A note from the President
Dear Colleagues,
Part of our mission at Catholic Health is to have a comprehensive plan to enhance Health Equity across Long Island, serving those who are underserved and uninsured. At St. Charles Hospital, we are committed to fulfilling this mission by identifying social determinants of health (SDOH) in the communities we serve and subsequently, implement an all-encompassing community outreach program to address economic and social obstacles.
As part of Catholic Health’s deanery outreach program, St. Charles Hospital works closely with our local parishes in organizing “Healthy Sundays” in underserved communities. Healthy Sundays, staffed by our nurses, offers health education on a wide variety of topics and also offers free health screenings including blood pressure, cholesterol and glucose, as well as free flu vaccinations. The program aims to improve the quality of life in underserved and uninsured populations and reduce the risk of health issues, including obesity, diabetes and hypertension.
To address food insecurity, St. Charles Hospital launched a “Meals of Hope” food packing event as part of a Lenten project, where employees package soup ingredients (each package feeds six people). The soup packages are then distributed to our local parishes and shelters. This program helps to provide healthy, nutritious meals for thousands of Suffolk County residents in underserved communities.
In addition, Catholic Health and St. Charles Hospital, partnered with Long Island Cares, to provide “food-to-go” bags for individuals who come to the hospital’s emergency department and are identified through screening as food insecurity. If identified as such, individuals will receive a bag of food when they leave the hospital.
St. Charles Hospital also offers free, evidenced-based health improvement programs throughout the year. We collaborate with community-based organizations, such as the Suffolk County Department of Health and RSVP—Retired Senior Volunteer Program of Suffolk. Topics include Smoking Cessation, Diabetes Prevention, Falls Prevention and Living Healthy Workshops series.
All patients who come to St. Charles Hospital for medical care are offered services regardless of their ability to pay.
To better serve the uninsured and Medicaid patients, St. Charles Hospital recently opened its Maternity Clinic, which offers obstetrical routine prenatal care and delivery, obstetrical ultrasound, breastfeeding and lactation classes, post-partum education counseling and more. Over the past year, St. Charles has partnered with local pregnancy centers who counsel young women from underserved communities, and who need access to quality maternity care.
Most recently, St. Charles’ Stephen B. Gold Dental Clinic received an $800,000 grant from the Mother Cabrini Health Foundation, allowing us to add four more operatories and hire a fourth dental resident, with an additional two more to be hired over the next several years. This will allow us to provide even more comprehensive dental care to the underserved and underinsured.
For all of the health equity initiatives I have outlined above, it is because of all of you that we are successful in fulfilling our mission to make sure that everyone in our communities has the same access to high-quality medical care, as well as health education regarding preventable diseases and free health screenings. Together we can make a difference in the lives of so many.
Sincerely,
James O’Connor President, St. Charles Hospital
Demographics of St. Charles Hospital patients
The following data were obtained from Epic and includes all patients who had an encounter with St. Charles Hospital from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health. Patients who died during or prior to 2024 were excluded from the sample.
SCH System All Pts
St. Charles Hospital’s Patient Population Overview
Patient race Figure 9.1.1: Patient race for all patients 18 years and older who had an encounter in 2024 (N=63,636). Source: Epic
Preferred language Figure 9.3.1: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=63,636). Source: Epic
Ethnicity Figure 9.2.1: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=63,636). Source: Epic
St.
SCH System Hosp Admiss
Charles Hospital’s Hospital Admissions Patient Population Overview
Patient race Figure 9.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=7,614). Source: Epic
American Indian and Alaskan Native Native Hawaiian and Other Pacific Islander Two or more races
Some other race
No answer/unknown
Preferred language 9.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=7,614). Source: Epic
No answer/ unknown
Ethnicity Figure 9.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=7,614).
Source: Epic
SCH System ED
St. Charles Hospital’s Emergency Department Patient Population
Patient race Figure 9.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=13,769). Source: Epic
Preferred language Figure 9.3.3: Preferred language for all patients 18 years and older who had an emergency department encounter in 2024 (N=13,769). Source: Epic
Ethnicity Figure 9.2.3: Patient ethnicity for all patients 18 years and older who had an emergency department encounter in 2024 (N=13,769). Source: Epic
Social Vulnerability Index by Census Tract for St. Charles Hospital Service Areas
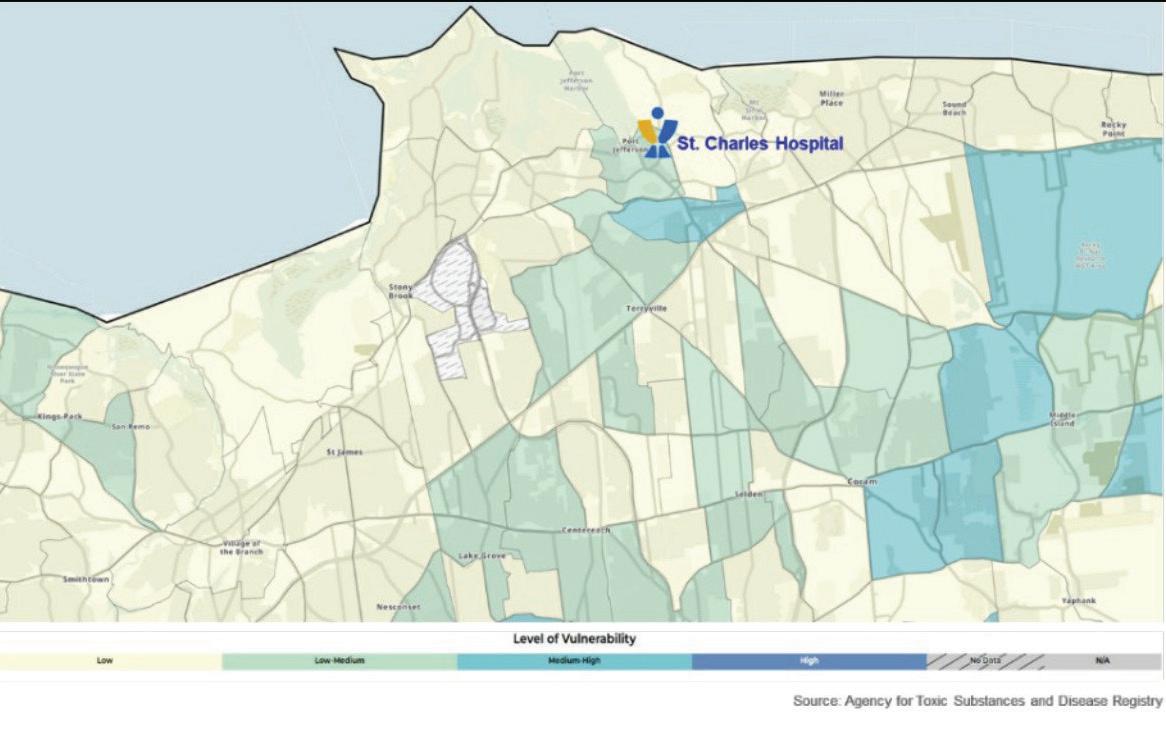
St. Charles Hospital Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. Statistical significance was considered to be a p-value of less than 0.05. If no statistically significant differences were found it is denoted by an asterisk (*).
All data were obtained through Epic and include all patients with any encounter at St. Charles Hospital from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth. For the influenza vaccination measure, the time period followed the ’24 – ’25 flu season (August 1, 2024 – July 31, 2025).
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications. These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024. Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Body Mass Index (BMI)
Table 9.1.1: Percent of patients 18 years and older with a BMI ≥25 by SVI Source: Epic
Table 9.1.2: Percent of patients 18 years and older with a BMI ≥25 by race Source: Epic
Table 9.1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source: Epic
Table 9.1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language Source: Epic
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 9.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 9.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 9.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening
Table 9.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by preferred language Source: Epic Language
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provided documented in the electronic health record during 2024.
Table 9.3.1: Percent of patients 18 years and older with a PCP by SVI Source: Epic
Table 9.3.2: Percent of patients 18 years and older with a PCP by race Source: Epic
Table 9.3.3: Percent of patients 18 years and older with a PCP by ethnicity Source: Epic
Table 9.3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic
Language
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 9.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
overall percentile (zip
Table 9.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 9.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
Table 9.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Language
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 9.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 9.5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic OMB Race White
Table 9.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic
physical exam
OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown Measures % patients with AWV/ physical exam # patients with AWV/ physical exam
with AWV/ physical exam
with AWV/ physical exam
Table 9.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by preferred language Source: Epic
Language English Spanish Other languages Measures % patients with AWV/ physical exam # patients with AWV/ physical exam
patients
patients with AWV/ physical exam # patients with AWV/ physical exam
with AWV/ physical exam
Market-specific Priority Population Equity Action Plan for St. Charles Hospital
Below, please find the health disparities the hospital will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity:
Primary Care Physician (PCP)
Identified intervention
• Staff education.
• Patient access documentation.
• Epic BPA build for provider notification.
• Patient referral and appointment with available PCP.
• Special accommodation for 5N, 5S, 2N and dental patients.
Owner
• Chukwuma Egbuziem
Key stakeholders
• President
• CMO
• CNO
• COO
• ED Director
• Hospitalist Director
• Director of Patient Access
• Director of Care Management
Key milestones
• Improved access and availability of PCPs including at Centereach hub.
• Beginning 10/2025, Daily reporting of patients presenting with no PCP with iPEARL rounding to assist with PCP placement.
• Monthly reports to track number of patients presenting with no PCP who are successfully referred to a new PCP.
Timeline to completion
• January 2027
Resources
• Ongoing staff education
• Epic report for referral
Measures of success
• Percent of patients presenting with no PCP who were successfully referred with an appointment made.
• 5% reduction in the number of patients documented with no PCP identified.
Health disparity: Annual Wellness Visit (AMV) or Physical Exam
Identified intervention
• Staff education.
• Patient referral and appointment with available PCP.
• Community engagement and education.
• Special accommodation for 5N, 5S, 2N and dental patients.
Owner
• Chukwuma Egbuziem
Key stakeholders
• President
• CMO
• CNO
• COO
• ED Director
• Nursing Leadership
• Hospitalist Director
• TOC Physician
Key milestones
• Beginning 10/2025, Daily reporting of patients presenting with no PCP with iPEARL rounding to assist with PCP placement.
• Monthly reports to track number of patients presenting with no PCP who are successfully referred to a new PCP.
Timeline to completion
• January 2027
Resources
• Ongoing staff education
• Epic report for referral
Measures of success
• Percent of patients presenting with no PCP who were successfully referred with an appointment made.
• 5% increase in the number of patients documented with an Annual Physical Exam.
Health disparity: Flu Vaccine
Identified intervention
• Staff education.
• Ongoing influenza vaccination in specialty clinics.
• Community engagement and awareness.
Owner
• Chukwuma Egbuziem
Key stakeholders
• President
• CMO
• CNO
• COO
• Nursing Leadership
• Director of Pharmacy
• ED Med Rec Pharmacists
Key milestones
• Continue to offer influenza vaccine in the specialty clinics.
• Improving patient education in our chemical dependency units to improve the vaccination rate.
• Ongoing community outreach programs with influenza vaccination offered.
Timeline to completion
• May 2026
Resources
• Ongoing staff education
• Influenza vaccines for Outpatient Specialty Clinics and community events
Measures of success
• Percent of patients in Outpatient Specialty Clinics, 5N, 5S and 2N who were vaccinated for the 2025/2026 flu season.
• 5% increase in the number of patients in highly vulnerable populations with documented influenza vaccination.
St. Francis Hospital & Heart Center Health Equity Strategic Plan
A note from the President
Dear Colleagues,
At St. Francis Hospital & Heart Center we are guided by our mission, vision and values to achieve excellence in all that we do. The Health Equity Plan is developed with the goal of improving the health and well-being of all. We believe health care is a right, not a privilege.
Unfortunately, some Long Islanders face barriers to good health and as a result are more likely to suffer from preventable disease. Disparities in health outcomes are closely linked to social, economic and environmental factors.
Our Health Equity Plan aims to reduce health disparities by providing access to quality care to under-resourced communities and by addressing the social drivers of health. It is intended to identify actual or potential health care disparities among population groups, and in the way demographic groups access, experience and receive health care. The plan considers both individual and community needs.
Some of our Health Equity initiatives include the Student Athlete Program, providing cardiac screening for high school students free of charge; the Gift of Life Program, providing corrective cardiac procedures for children who cannot access this care in their own countries; a Community Outreach Program, providing a multitude of educational classes, screenings and vaccinations; and the Food is Medicine Program, providing a ready bag of food and referrals to nutrition resources for patients who are in need.
Together, we are making great strides towards improving health outcomes for all. Thank you for your ongoing care for our patients and our communities. I am proud of the work we’re doing and look forward to continuing to improve access to the exceptional health care at St. Francis Hospital & Heart Center.
Peace and all good,
Charles Lucore, MD, MBA President, St. Francis Hospital & Heart Center
Demographics of St. Francis Hospital & Heart Center patients
The following data were obtained from Epic and includes all patients who had an encounter with St. Francis Hospital & Heart Center from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health. Patients who died during or prior to 2024 were excluded from the sample.
SFH System All Pts
St. Francis Hospital and Heart Center’s Patient Population Overview
Patient race Figure 11.1.1: Patient race for all patients 18 years and older who had an encounter in 2024 (N=142,834). Source: Epic
Alaskan
Two or more races
Some other race
No answer/unknown
Preferred language Figure 11.3.1: Preferred language for all patients 18 years and older who had an encounter in 2024 (N=142,834). Source: Epic
No answer/ unknown
Ethnicity Figure 11.2.1: Patient ethnicity for all patients 18 years and older who had an encounter in 2024 (N=142,834). Source: Epic
SFH System Hosp Admiss
St. Francis Hospital & Heart Center’s Hospital Admissions Patient Population Overview
Patient race Figure 11.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=20,757). Source: Epic
No answer/unknown
Preferred language Figure 11.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=20,757). Source: Epic
No answer/ unknown
Ethnicity Figure 11.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=20,757). Source: Epic
SFH System ED
St. Francis Hospital & Heart Center’s Emergency Department Patient Population Overview
Patient race Figure 11.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=35,122). Source: Epic
Ethnicity Figure 11.2.3: Patient ethnicity for all patients 18 years and older who had an emergency department encounter in 2024 (N=35,122). Source: Epic
Some other race
No answer/unknown
Preferred language Figure 11.3.3: Preferred language for all patients 18 years and older who had an emergency department encounter in 2024 (N=35,122). Source: Epic
Social Vulnerability Index by Census Tract for St. Francis Hospital & Heart Center Service Areas
Figure 12.0: SVI by Census Tract for St. Francis Hospital & Heart Center service areas.
Source: Epic
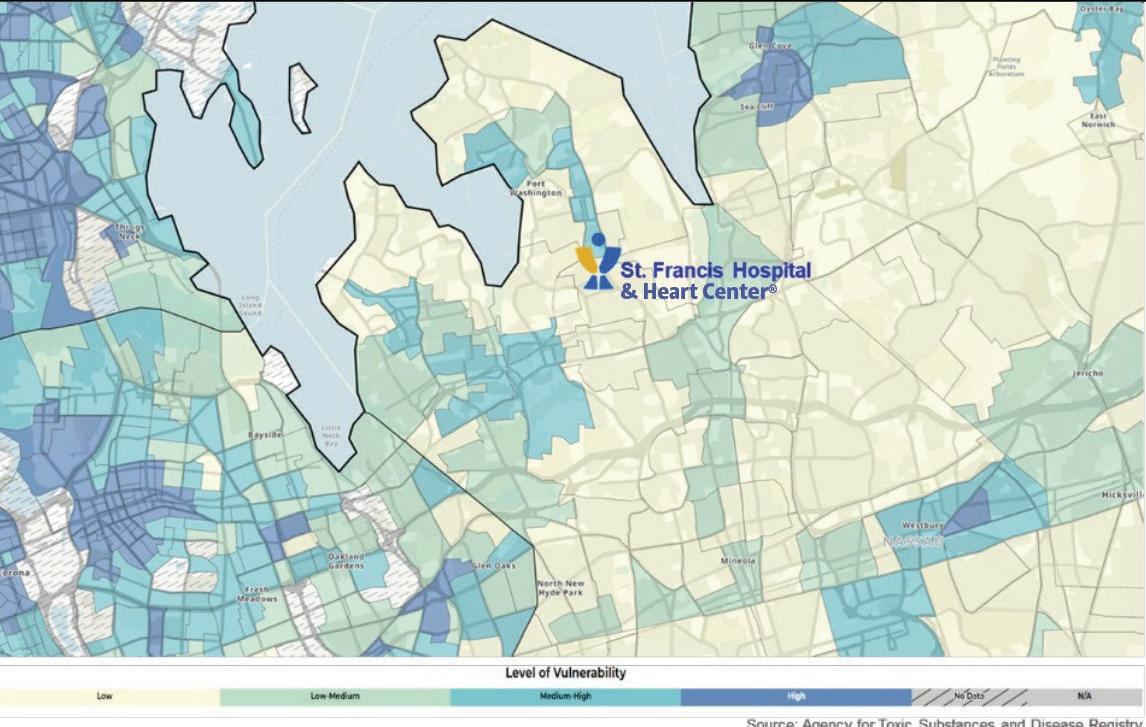
St. Francis Hospital & Heart Center Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant.
All data were obtained through Epic and include all patients with any encounter at St. Francis Hospital & Heart Center from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth. For the influenza vaccination measure, the time period followed the ’24 – ’24 flu season (August 1, 2024 –July 31, 2025).
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
Body Mass Index (BMI)
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024. Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Table 10.1.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic SVI 2020 overall
(zip code)
Table 10.1.2: Percent of patients 18 years and older with a BMI ≥25 by race Source: Epic
Table 10.1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source: Epic
Table 10.1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language
Source: Epic
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 10.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 10.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 10.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening by ethnicity Source: Epic
OMB Ethnicity Not
Table 10.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by language Source: Epic
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provided documented in the electronic health record during 2024.
Table 10.3.1: Percent of patients 18 years and older with a PCP by SVI Source: Epic
Table 10.3.2: Percent of patients 18 years and older with a PCP by race Source: Epic
Table 10.3.3: Percent of patients 18 years and older with a PCP by ethnicity Source: Epic
Table 10.3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 10.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
Table 10.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 10.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
Table 10.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 10.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic
SVI overall percentile (zip code) Low vulnerability High vulnerability
patients with AWV/ physical exam
Table 10.5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic OMB Race White Black or African American Asian American Indian and Alaska Native Native Hawaiian and other Pacific Islander Two or more races Some other race No answer/ unknown with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam
Table 10.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic
Table 10.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by
Market-specific Priority Population Equity Action Plan for St. Francis Hospital & Heart Center
Below, please find the health disparities the hospital will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity: Flu vaccine
Identified Intervention
• Increase influenza vaccination pods in communities with high SVI.
Owner
• Quality and Performance Improvement
Key stakeholders
• Executive Leadership
• Community Health and Outreach Program
• Community Partners
• Pharmacy Department
• Community Advisory Board
• Patient Family Advisory Council
• Employee Health
Key milestones
• Identify communities with high SVI.
• Strategize with community partners to establish influenza vaccination calendar of events.
• MyChart reminders of vaccination status.
Timeline to completion
• End of NYS Flu Season
Resources
• Epic reporting
• Marketing
• Pharmacy
• Education
• Outreach Bus
Measures of success
• Additional influenza vaccination pods scheduled in communities identified with high SVI.
Health disparity: Primary Care Physician (PCP)
Identified Intervention
• Identify a PCP for all patients.
Owner
• Quality and Performance Improvement
Key stakeholders
• Executive Leadership
• Patient Access
• Care Management/Social Work
• Nursing
• Transitions of Care Program
• Catholic Health Physician Partners
• Community Outreach Program
• Community Advisory Board
• Patient Family Advisory Council
Key milestones
• Staff education on PCP referral process and electronic health record documentation.
• Community Health and Outreach events.
• MyChart reminders of upcoming appointments.
Timeline to completion
• Rolling
Resources
• Epic reporting
• Compass Rose
• Find-a-Doctor referral
• Catholic Health Physician Partners
• Catholic Health Central Referral
Measures of success
• Increase in number of patients assigned to a PCP.
Health disparity: Annual Wellness Visit (AWV) or physical examination
Identified Intervention
• Increase in number of patients with annual physical exam.
Owner
• Quality and Performance Improvement
Key stakeholders
• Executive Leadership
• Patient Access
• Care Management/Social Work
• Nursing
• Transitions of Care Program
• Catholic Health Physician Partners
• Community Outreach Program
• Community Advisory Board
• Patient Family Advisory Council
Key milestones
• Staff education on PCP referral process and electronic health record documentation.
• Community Health and Outreach events.
• MyChart reminders of upcoming appointments.
Timeline to completion
• Rolling
Resources
• Epic reporting
• Compass Rose
• Find-a-Doctor referral
• Catholic Health Physician Partners
• Catholic Health Central Referral
Measures of success
• Increase in number of patients with documented annual physical exam.
St. Joseph Hospital Health Equity Strategic Plan
A note from the President
Dear Colleagues,
As President of St. Joseph Hospital, it is my honor and pleasure to inform and assure you of our unwavering commitment to health equity through the implementation of our strategic plan. As we strive to provide exceptional care for all members of our community, we recognize that achieving health equity is not just our goal—it is our responsibility. This plan is not just a document; it is a roadmap for action.
We are deeply committed to promoting health equity within our community. We recognize that health disparities exist and that systemic barriers often prevent individuals from receiving the care they need. Our commitment is rooted in the belief that everyone deserves fair and just access to quality health care, regardless of their background. Some of the key initiatives of St. Joseph Hospital’s Health Equity Strategic Plan include:
• Actively engaging with diverse communities to help us better understand their needs and address health disparities.
• Promoting health equity by hosting community health fairs and providing free flu vaccines, blood pressure screenings and a variety of resources, ensuring that everyone has access to essential health care services.
• Providing education about health resources, preventive care and healthy lifestyles to empower our patients and community members.
• Enhancing access to primary care physicians (PCP) in order to promote health equity and improve overall health outcomes.
• Screening patients who come through our emergency department for food insecurity. Patients identified are provided with “food-to go” bags and our care management team provides additional referrals.
• Training our hospital staff in cultural competency to ensure that every patient feels respected and understood.
St. Joseph is fully committed to a future where every patient receives equitable care. Together, we can break down barriers and build a healthier community for all.
Sincerely,
Joseph Manopella President, St. Joseph Hospital
Demographics of St. Joseph Hospital patients
The following data were obtained from Epic and includes all patients who had an encounter with St. Joseph Hospital from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health. Patients who died during or prior to 2024 were excluded from the sample.
SJH System All Pts
St. Joseph Hospital’s Patient Population Overview
Patient race Figure 13.1.1: Patient race for all patients 18 years and older who had and encounter in 2024 (N=49,614). Source: Epic
Some other race
No answer/unknown
Preferred language Figure 13.3.1: Preferred language for all patients 18 years and older who had and encounter in 2024 (N=49,614). Source: Epic
Non-Hispanic or Latino Hispanic or Latino
No answer/ unknown
Ethnicity Figure 13.2.1: Patient ethnicity for all patients 18 years and older who had and encounter in 2024 (N=49,614). Source: Epic
SJH System Hosp Admiss
St. Joseph Hospital’s Hospital Admissions Patient Population Overview
Patient race Figure 13.1.2: Patient race for all patients 18 years and older who had a hospital admission in 2024 (N=7,737). Source: Epic
Some other race No answer/unknown
Preferred language Figure 13.3.2: Preferred language for all patients 18 years and older who had a hospital admission in 2024 (N=7,737). Source: Epic Non-Hispanic or Latino
Ethnicity Figure 13.2.2: Patient ethnicity for all patients 18 years and older who had a hospital admission in 2024 (N=7,737). Source: Epic
St. Joseph Hospital’s Emergency Department Patient Population Overview
SJH System ED
Patient race Figure 13.1.3: Patient race for all patients 18 years and older who had an emergency department encounter in 2024 (N=23,665). Source: Epic
Ethnicity Figure 13.2.3: Patient ethnicity for all patients 18 years and older who had an emergency department encounter in 2024 (N=23,665). Source: Epic
Non-Hispanic or Latino
Preferred language Figure 13.3.3: Preferred language for all patients 18 years and older who had an emergency department encounter in 2024 (N=23,665).
Source: Epic
Social Vulnerability
Index by Census Tract for St. Joseph Hospital Service Areas
Figure 14.0: SVI by Census Tract for St. Joseph Hospital service areas.
Source: Epic
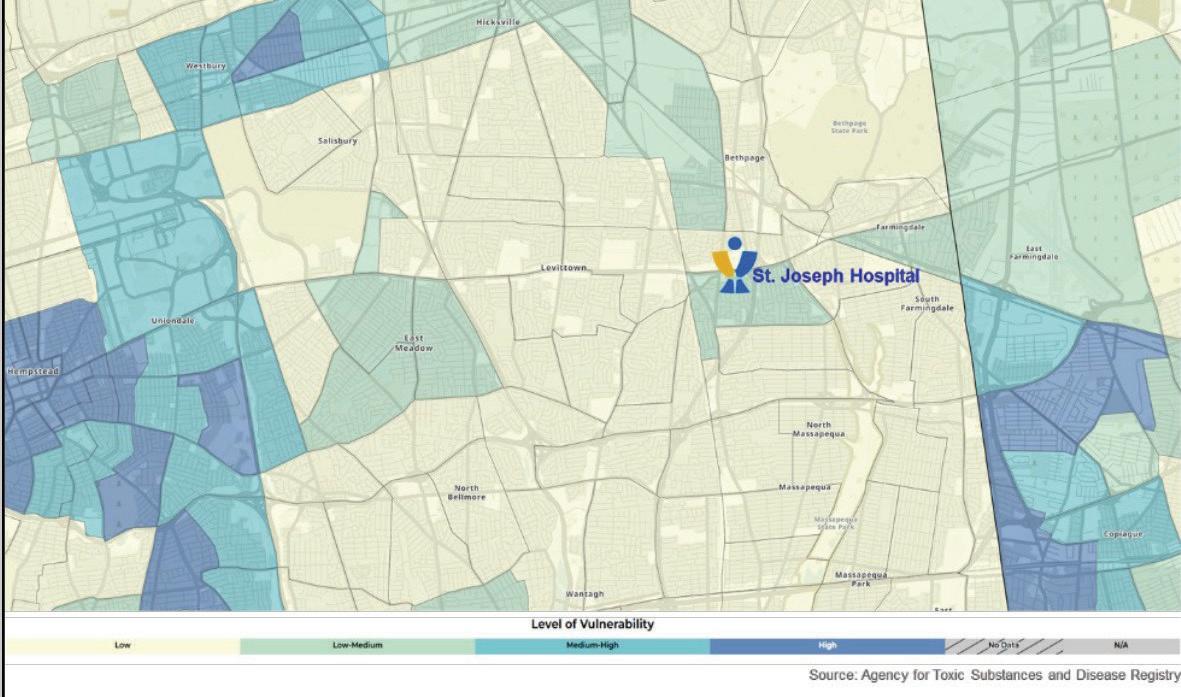
St. Joseph Hospital Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant. All data were obtained through Epic and include all patients with any encounter at St. Joseph Hospital from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth. For the influenza vaccination measure, the time period followed the ’24 – ’25 flu season (August 1, 2024 – July 31, 2025).
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
Body Mass Index (BMI)
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research. Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024. Language data were disaggregated by our top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Table 10.1.1: Percent of patients 18 years and older with a BMI ≥25 by SVI Source: Epic
Table 10.1.2: Percent of patients 18 years and older with a BMI ≥25 by race Source: Epic
Table 10.1.3: Percent of patients 18 years and older with a BMI ≥25 by ethnicity Source:
Table 10.1.4: Percent of patients 18 years and older with a BMI ≥25 by preferred language Source: Epic
Breast Cancer screening
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 10.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 10.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 10.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening by
Table 10.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by language Source: Epic
Primary Care Physician (PCP)
Having a PCP was defined as having a health care provided documented in the electronic health record during 2024.
Table 10.3.1:Percent of patients 18 years and older with a PCP by SVI Source: Epic SVI overall percentile (zip code) Low
Table 10.3.2: Percent of patients 18 years and older with a PCP by race Source: Epic
Table 10.3.3: Percent of patients 18 years and older with a PCP by ethnicity Source: Epic
Table 10.3.4: Percent of patients 18 years and older with a PCP by preferred language Source: Epic Language
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination from August 1, 2024 to July 31, 2025. Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 10.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic SVI overall percentile (zip code) Low vulnerability
Table 10.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 10.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Table 10.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Language
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024. If a patient had an ICD code documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 10.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic
Table 10.5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic
exam with AWV/ physical exam
Table 10.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic
OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown Measures % patients with AWV/ physical exam # patients with AWV/ physical exam
patients
patients with AWV/ physical exam # patients with AWV/ physical exam
Table 10.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by preferred language Source: Epic
Language English Spanish Other languages Measures % patients with AWV/ physical exam # patients with AWV/ physical exam
patients % patients with AWV/ physical exam # patients with AWV/ physical exam
Market-specific Priority Population Equity Action Plan for St. Joseph Hospital
Below, please find the health disparities the hospital will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity:
% of patients 60 years and older with a flu vaccine
Identified intervention
• Schedule flu vaccination pods in several local communities with elevated SVI.
Owner
• Vice President of Quality and Performance Improvement
Key stakeholders
• Director of Pharmacy
• Manager of Public and Community Relations
• CNO
Key milestones
• Identify local communities with elevated SVI.
• Communicate with Community Relations/ Community Partners to establish dates and locations for flu vaccination pods.
• Schedule four additional flu pods in communities with elevated SVI as compared to 2024.
Timeline to completion
• Complete by the end of the 2025 – 2026 flu season.
Resources
• Pharmacist
• Registered Nurses
• Vaccines
Measures of success
• St. Joseph Hospital will schedule four additional flu pods in communities with elevated SVI.
Health disparity: % of patients with a Primary Care Physician (PCP)
Identified intervention
• Identify Spanish speaking patients without a PCP listed and refer patients to a local community PCP.
Owner
• Vice President of Quality and Performance Improvement
Key stakeholders
• Health care Navigator
• Care Management/Social Work
• ED Physicians
• Nursing Staff
• CNO
• CMO
• Patient Access
Key milestones
• Create a report to capture patients without a PCP and includes spoken language.
• Establish relationships with various community physician offices.
• Begin referring Spanish speaking patients to community PCPs and scheduling appointments.
• Create a process to enter PCP information into Epic to capture PCP data appropriately.
Timeline to completion
• December 2026
Resources
• Health Care Navigator
• Care Managers/Social Workers
Measures of success
• The percentage of Spanish speaking patients with a PCP will be monitored. The goal is to increase this percentage by 10% when compared to 2025.
Catholic Health Physician Partners Health Equity Strategic Plan
A note from the Chief Operating Officer
Dear Colleagues,
Welcome to Catholic Health Physician Partners. It is both an honor and a privilege to reaffirm our unwavering commitment and dedication to advancing health equity through the implementation of our strategic plan. As we continue our mission to deliver high-quality care to every member of our community, we understand that achieving health equity is not merely an aspiration—it is our collective responsibility. This plan serves not only as a guiding document, but also as a blueprint for meaningful action.
At Catholic Health Physician Partners, we recognize that health disparities persist and that systemic barriers often hinder individuals from accessing the care they need. Our commitment is grounded in the belief that every person deserves equitable access to high-quality health care, regardless of background or circumstances as evidenced at our Bishop McHugh centers, providing access to state-of-the-art care.
Some of the key initiatives outlined in Catholic Health Physician Partners’ Health Equity Strategic Plan are included in this communication.
Sincerely,
Joseph O’Doherty Chief Operating Officer & Senior Vice President of Finance
Demographics of Catholic Health Physician Partners patients
The following data were obtained from Epic and includes all patients who had an encounter with Catholic Health Physician Partners from January 1 to December 31, 2024. Patients are only included in the sample once, even if they had more than one encounter with Catholic Health Physician Partners. Patients who died during or prior to 2024 were excluded from the sample.
CHPP System All Pts
Catholic Health Physician Partner’s Patient Population Overview
Patient race Figure 15.1.1: Patient race for all patients 18 years and older who had an office visit or AWV in 2024 (N=300,966). Source: Epic
Ethnicity Figure 15.2.1: Patient ethnicity for all patients 18 years and older who had an office visit or AWV in 2024 (N=300,966). Source: Epic
Preferred language Figure 15.3.1: Preferred language for all patients 18 years and older who had an office visit or AWV in 2024 (N=300,966). Source: Epic
2020 Social Vulnerability Index by Census Tract for Queens, Nassau and Suffolk
Figure 16.0: SVI by Census Tract for Catholic Health service areas.
Source: Epic
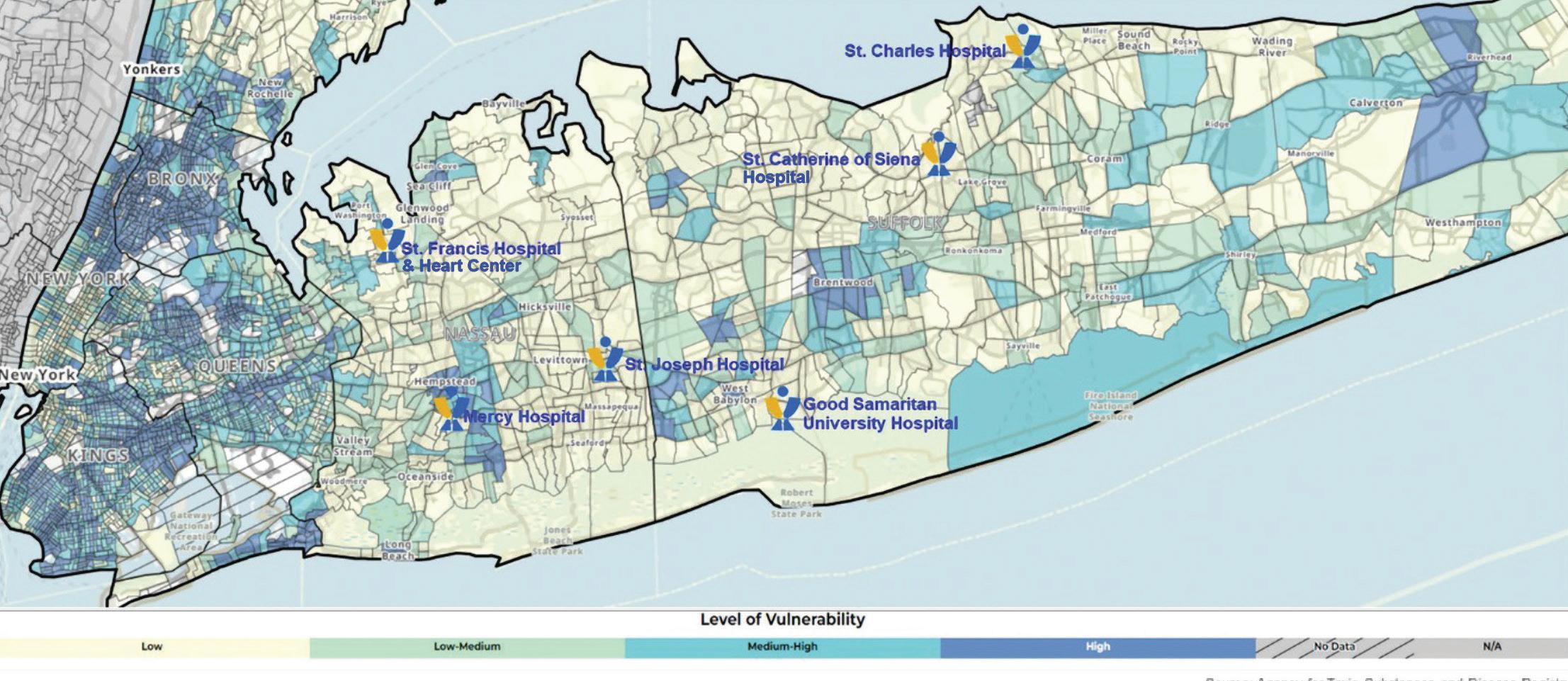
Catholic Health Physician Partners Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant.
All data were obtained from Epic Data includes all patients with at least one encounter marked as an annual wellness visit or an office visit, and the patient has at least one encounter in an ambulatory department in the Catholic Health System from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth.
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
Breast Cancer screening
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research. Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2024. Language data were disaggregated by the top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Breast cancer screening was defined as a patient having a breast cancer screening or mammography marked as completed from January 1, 2023 to December 31, 2024 for all women for all encounters in 2024.
Table 11.2.1: Percent of patients 40 – 75 years with a Breast Cancer screening by SVI Source: Epic
Table 11.2.2: Percent of patients 40 – 75 years with a Breast Cancer screening by race Source: Epic
Table 11.2.3: Percent of patients 40 – 75 years with a Breast Cancer screening by ethnicity Source: Epic
Table 11.2.4: Percent of patients 40 – 75 years with a Breast Cancer screening by language Source: Epic
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination during the ’24-’25 flu season (August 1, 2024July 31, 2025). Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre Syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 11.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
Table 11.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
Table 11.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic OMB Ethnicity Not
Table 11.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Annual Wellness Visit (AWV) or Physical Examination
Annual Wellness Visit or physical examination was measured by ICD codes related to an AWV or physical examination documented as visit diagnosis, billing diagnosis or on the patient’s problem list during 2024, procedure codes for AWV, and if the encounter type was an annual wellness visit. If a patient had an ICD code, procedure code, or encounter type as annual wellness visit documented during 2024, they were marked as “yes” having an AWV or physical exam during the 2024 year.
Table 11.5.1: Percent of patients 18 years and older with an annual wellness visit or physical exam by SVI Source: Epic
Table 11.5.2: Percent of patients 18 years and older with an annual wellness visit or physical exam by race Source: Epic
with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam with AWV/ physical exam
Table 11.5.3: Percent of patients 18 years and older with an annual wellness visit or physical exam by ethnicity Source: Epic
OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Measures % patients with AWV/ physical exam # patients with AWV/ physical exam Total # patients % patients with AWV/ physical exam # patients with AWV/ physical exam
Table 11.5.4: Percent of patients 18 years and older with an annual wellness visit or physical exam by preferred language Source: Epic
Language English Spanish Other languages
Measures % patients with AWV/ physical exam # patients with AWV/ physical exam Total # patients % patients with AWV/ physical exam # patients with AWV/ physical exam
# patients
patients with AWV/ physical exam # patients with AWV/ physical exam
Strategic Health Equity Plan Goals
Breast cancer screening:
Increase mammogram rates among eligible women in underserved communities
Community Engagement
Partner with FBOs, shelters, and local influencers/CBOs to provide educational materials.
Culturally and Linguistically Appropriate Communication
Provide materials in multiple languages (e.g., Spanish, Hindi, Chinese, etc.) tailored to cultural beliefs about cancer.
Access Expansion
Expanded hours of operations for mammograms.
Provider Engagement
Train providers, use EMR alerts to flag patients overdue for screening.
Patient Experience (PX)
Develop a Community Volunteer Cancer program to improve the patient experience.
Flu vaccine:
Achieve an increase in flu vaccination rates in high-risk, low-access populations annually
Community Engagement
Work with schools, workplaces and places of worship for flu vaccine clinics. Work with schools, workplaces and places of worship for flu vaccine clinics.
Culturally and Linguistically Appropriate Communication
Counter misinformation through multilingual campaigns and targeted social media.
Access Expansion
Provide evening/weekend flu clinics/pods.
Provider Engagement
Educate providers on disparities in vaccine uptake and how to build trust.
Patient Experience (PX)
Medical Interpreter training for medical assistants, which would ensure accurate communication, reduce medical errors and improve patient satisfaction.
Annual Wellness Visit (AWV) or physical examination:
Community Engagement
Use Quality team nurses to educate and assist with scheduling annual checkups.
Culturally and Linguistically Appropriate Communication
Send reminders using preferred language and channel \(text, phone, email).
Access Expansion
Use hybrid model for ease of access to annual checkups.
Provider Engagement
Increase outreach to no-show and overdue patients.
Metrics
Screening Uptake: Increased mammogram completion in target groups.
Vaccine Coverage: 10% of eligible population vaccinated by race/ethnicity/zip code.
Annual Wellness Visit Completion: Increased number of patients completing annual wellness visits by SVI scores.
Patient Satisfaction: Surveys focused on barriers reduced and improved experience of care based on Race, Ethnicity and Language (REaL) data.
Provider Engagement: 10% increase of trainings completed in cultural competence and equity-focused care across Catholic Health Physician Partners.
Catholic Health Home Care & Good Shepherd Hospice Health Equity Strategic Plan
A note from the President
Dear Colleagues,
At Catholic Health Home Care and Good Shepherd Hospice, we are guided by our mission, vision and I-CARE values. Part of our mission at Catholic Health is to enhance Health Equity across our demographic footprint, serving those who face barriers to access and disparities in health outcomes.
Social determinants of health (SDOH) comprise the economic and social conditions that shape a person’s health status. These factors impact health outcomes, depending on the availability and access to health care. Social determinants can adversely affect underserved populations with inadequately managed chronic and advanced health conditions. Managing health conditions at home is critical for improving patient outcomes and enhancing quality of life.
Catholic Health Home Care and Good Shepherd Hospice focus on strong partnerships with our health systems, extending care needs outside the hospital. We optimize our patient’s desire to remain in the comfort of their home. Many efforts concentrate on avoiding unnecessary patient re-hospitalizations.
Catholic Health Home Care’s history of health equity initiatives includes our Remote Patient Monitoring (RPM) Program and an integrated approach to address food insecurity among individuals with chronic disease. RPM enables greater outreach to people with identified health disparities. RPM allows the individual to participate in care using the real-time, advanced technology to generate prompt interaction of nurses who provide intervention, education and prevention with the patient’s primary provider. These efforts improve clinical outcomes, enhance quality of life and decrease the strain on the health care payer system. Our Food Insecurity Program addresses patients recently discharged from the hospital. It provides necessary nutrition for food-insecure individuals, offering meals and educational counseling sessions. This program improved health outcomes and decreased rehospitalizations.
Catholic Health Home Care’s additional initiatives aim to focus on primary prevention and reducing the incidence of disease among patients 60 years and older by race, ethnicity, preferred language and Social Vulnerability Index (SVI) as related to influenza vaccination.
While New York State continues to face the challenge of underutilization of hospice care, our health equity initiatives focus on access to hospice and palliative care, utilizing community-based measures including the Social Vulnerability Index.
As care at home grows, together, we are improving health outcomes and access for all. It is because of you and the trust of our communities that we can make a difference in the lives we serve.
Sincerely,
Kim Kranz President, Catholic Health Home Care & Good Shepherd Hospice
Demographics of Catholic Health Home Care patients
The following data—were obtained from Epic and includes all patients 18 years and older who had a home health certification period documented in Epic from January 1 to December 31, 2024. Patients who died during or prior to 2024 were excluded from the sample. Age was calculated based upon each patients’ date of birth.
HC System All Pts
Catholic Health Home Care’s Patient Population Overview
Patient race Figure 17.1.1: Patient race for all patients 18 years and older who had a home health certification period in 2024 (N=21,055). Source: Epic
Preferred language Figure 17.3.1: Preferred language for all patients 18 years and older who had a home health certification period (N=21,055). Source: Epic
Non-Hispanic or
Ethnicity Figure 17.2.1: Patient ethnicity for all patients 18 years and older who had a home health certification period in 2024 (N=21,055). Source: Epic
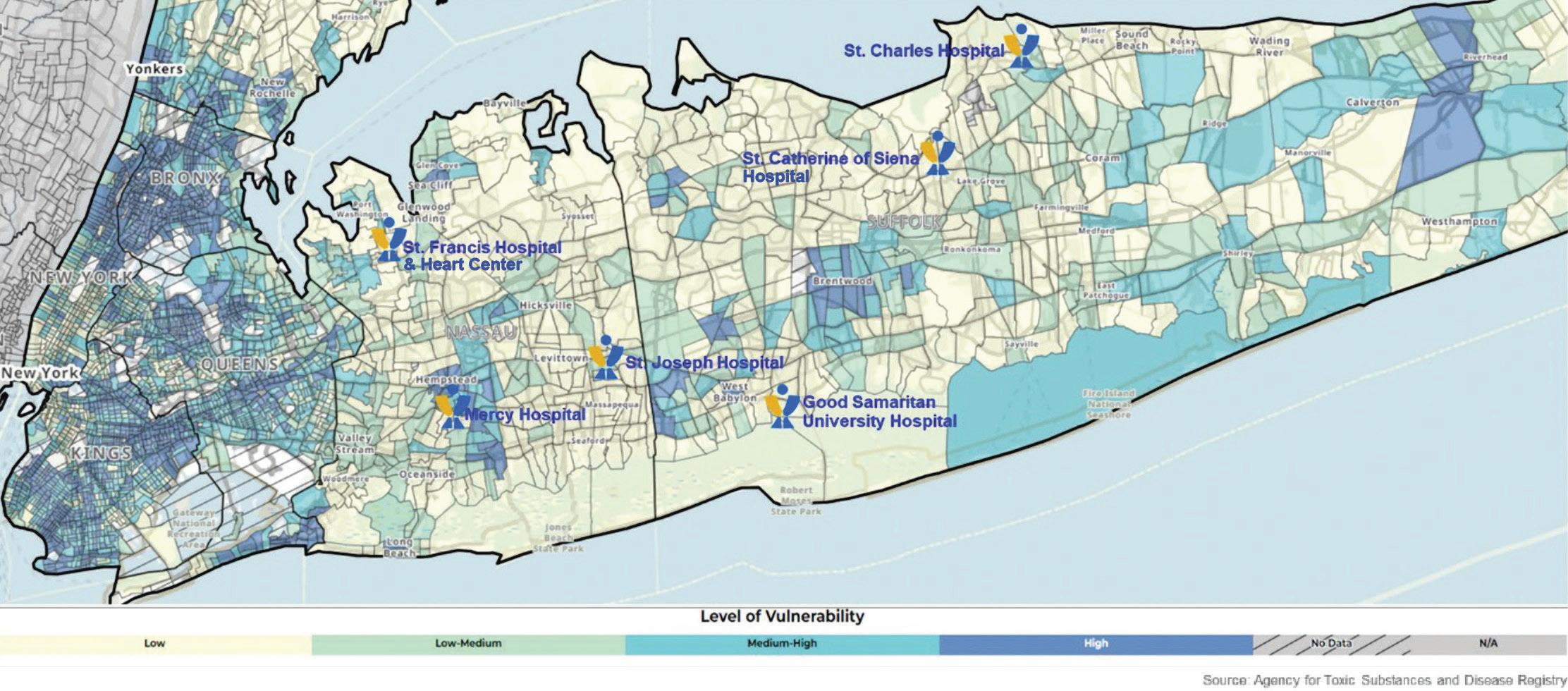
2020 Social Vulnerability Index by Census Tract for Queens, Nassau and Suffolk
Figure 18.0: SVI by Census Tract for Catholic Health service areas.
Source: Epic
Catholic Health Home Care Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. All analyses were statistically significant.
All data were obtained from Epic. Data includes all patients 60 years and older who had a home health certification period documented in Epic from August 1, 2024 to July 31, 2025. Patients who died during or prior to July 31, 2025 were excluded from the sample. Age was calculated based upon each patients’ date of birth.
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during the time period. Language data were disaggregated by the top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
Flu vaccine
Influenza vaccination was defined as all patients who received an influenza vaccination during the ’24-’25 flu season (August 1, 2024 –July 31, 2025). Influenza vaccination was defined through self-reported vaccination outside of Catholic Health and documentation of influenza vaccination administered in the electronic health record. Patients who were contraindicated for the flu vaccine were excluded. Contraindication was defined as hypersensitivity to eggs/thimerosal, had a prior negative reaction to a vaccination, had a bone marrow transplant within the last six months and had a history of Guillain-Barre Syndrome. Patients who refused to receive a flu vaccination and did not receive a vaccination at another encounter were excluded.
Table 12.4.1: Percent of patients 60 years and older with an influenza vaccination by SVI Source: Epic
SVI overall percentile (zip code) Low vulnerability High
Table 12.4.2: Percent of patients 60 years and older with an influenza vaccination by race Source: Epic
OMB Race White Black or African American Asian American Indian and Alaska Native Native Hawaiian and other Pacific Islander Two or more races Some other race No answer/
Table 12.4.3: Percent of patients 60 years and older with an influenza vaccination by ethnicity Source: Epic
OMB Ethnicity Not Hispanic/Latino Hispanic/Latino No answer/unknown
Table 12.4.4: Percent of patients 60 years and older with an influenza vaccination by preferred language Source: Epic
Language English Spanish Other languages
Market-specific Priority Population Equity Action Plan for Catholic Health Home Care
Below, please find the health disparities the home care will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity: Flu vaccine
Identified intervention
• Increase influenza vaccination rate in patients 60 years and older with a preferred language of Spanish.
Owner
• Operations, Quality and Performance Improvement
Key stakeholders
• Executive Leadership
• Team Managers
• Education
• Clinicians
• Community Partners
Key milestones
• Identify patients preferred language at Start of Care (SOC).
• Instruct clinical teams to provide to patients influenza vaccine information in Spanish.
• Compile a list of local flu vaccine providers and collaborate with community partners to coordinate influenza vaccination efforts.
Timeline to completion
• 2025 – 2026 flu season Resources
• Epic reporting
• OASIS data
Measures of success
• Increase in the number of patients, with a preferred language of Spanish, receiving an influenza vaccination by end of current flu season (as designated by NYSDOH).
Demographics of Good Shepherd Hospice patients
The following data were obtained from Epic and includes all patients who had a hospice episode from January 1 to June 30, 2025. The year 2025 was selected as the primary outcome of interest was referral to admission rate and referral data for 2024 was not reliable.
GSH
System All Pts
Good Shepherd Hospice’s Patient Population Overview
Patient race Figure 19.1.1: Patient race for all patients who had a hospice episode from January 1 to June 30, 2025 (N=1,716). Source: Epic
Preferred language Figure 19.3.1: Preferred language for all patients who had a hospice episode from January 1 to June 30, 2025 (N=1,716). Source: Epic
Ethnicity Figure 19.2.1: Patient ethnicity for all patients who had a hospice episode from January 1 to June 30, 2025 (N=1,716). Source: Epic
GSH System Hospice Ref
Good Shepherd Hospice's Referrals Patient Population Overview
Patient race Figure 20.1.1: Patient race for all hospice referrals from January 1 to June 30, 2025 (N=3,776).
Source: Epic
Preferred language Figure 20.3.1: Preferred language for all hospice referrals from January 1 to June 30, 2025 (N=3,776). Source: Epic
Ethnicity Figure 20.2.1: Patient ethnicity for all hospice referrals from January 1 to June 30, 2025 (N=3,776).
Source: Epic
2020 Social Vulnerability Index by Census Tract for Queens, Nassau and Suffolk
Figure 21.0: SVI by Census Tract for Catholic Health service areas.
Source: Epic
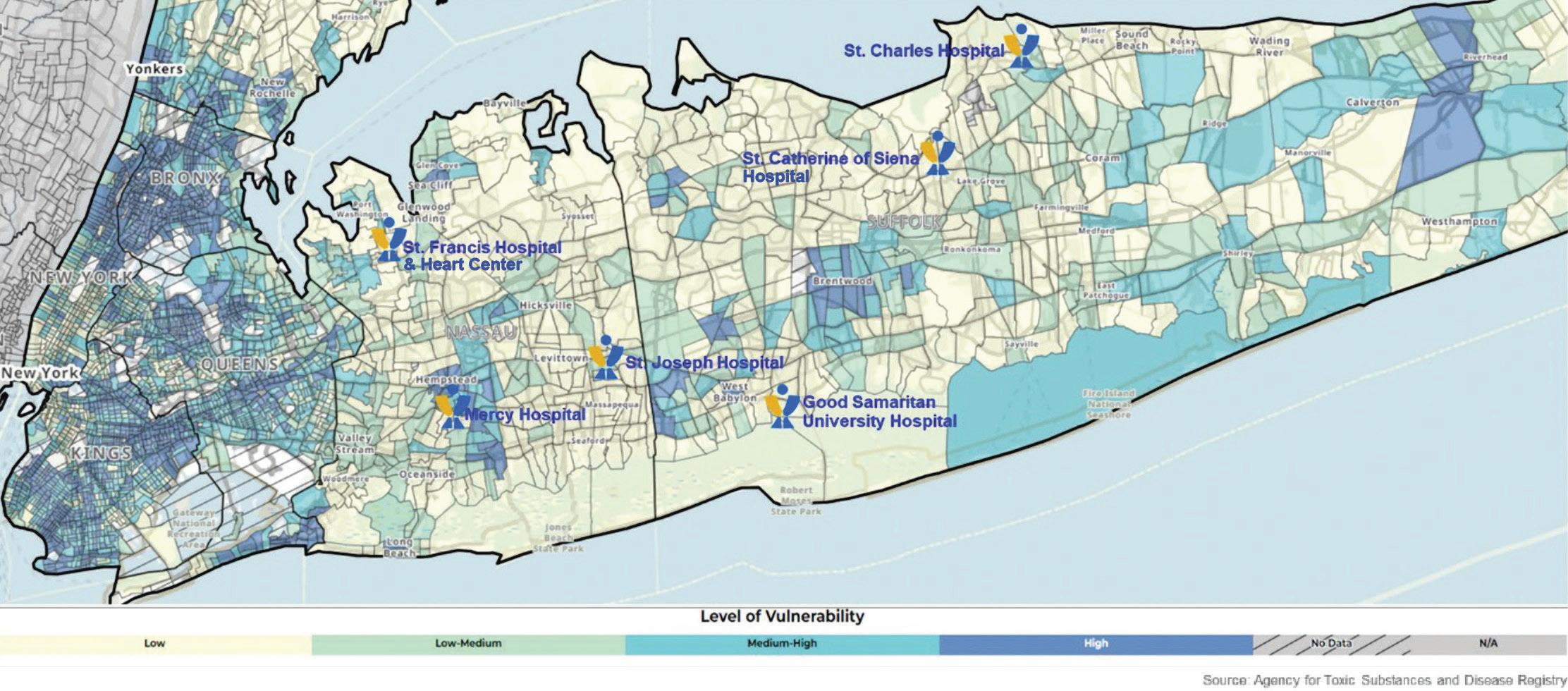
Good Shepherd Hospice Identified Health Disparities
All disparities have been measured using Chi-square tests for statistical significance. Statistical significance was considered to be a p-value of less than 0.05. If no statistically significant differences were found it is denoted by an asterisk (*).
All data were obtained from Epic. Data includes all referrals hospice referrals from January 1 to June 30, 2025. Referrals that were canceled or denied were excluded. 2025 data were chosen because 2024 data were deem unreliable to report on.
Race and ethnicity follow the Office of Management and Budget (OMB) federal race and ethnicity standard classifications.
Referrals to Admission (Conversion rate)
These are standard definitions provided by OMB to promote uniformity and comparability for race and ethnicity data. These categories are used in the decennial census, household surveys, administrative forms and medical/public health research.
Preferred language was categorized as English, Spanish or other languages from the patient’s last stored value during 2025. Language data were disaggregated by the top two languages to facilitate visualization and statistical analyses. Stratification by preferred language does not include changes in self-reported preferred language.
The percent of referrals that were admitted or conversion rate was measured as hospice referrals that were marked as admitted or discharged in Epic from January 1 to June 30, 2025. Referrals that were canceled or denied were excluded.
Table 13.1: Percent of hospice referrals that were admitted by SVI Source: Epic
Table 13.2: Percent of hospice referrals that were admitted by race Source: Epic
Table 13.3: Percent of hospice referrals that were admitted by ethnicity Source: Epic
Table 13.4: Percent of hospice referrals that were admitted by preferred language Source: Epic
Market-specific Priority Population Equity Action Plan for Good Shepherd Hospice
Below, please find the health disparities the hospice will focus on improving, including the discreet action steps that will be tracked to close the identified gap.
Health disparity: Equitable access to end of life care
Identified intervention
• Increase conversion rate (referrals to admission) for patients that speak languages other than English or Spanish.
Owner
• Business Development, Quality and Performance Improvement
Key stakeholders
• Executive Leadership
• Director of Performance Improvement
• Manager of Business Development
• Intake Specialist
• Hospital Based Liaisons
• Community Intake Coordinator
Key milestones
• Accurate identification and documentation of patients preferred language during the intake process.
• Explore options for identifying and documenting primary caregiver preferred language.
• Documented use of interpreter services for all patients/ caregivers as needed.
Timeline to completion
• Q3 2025 – Q3 2026
Resources
• Epic reporting
• VOYCE Interpreter Service
Measures of success
• Increase the percentage of admissions for patients with preferred language other than English or Spanish.
Acknowledgments
A special thanks to co-authors
• Lawrence Eisenstein, MD, MPH, FACP VP, Community and Public Health
• Gabriella Pandolfelli, PhD, MPH Director, Epidemiology and Public Health Analytics
Thank you to key contributors
• John Abalajon, RN, MS Systems Analyst, Population Health
• Monique Ford, MBA, CPXP VP, Human Experience
• Christine Hendriks, MA, MFA VP, Community Outreach
• Donna Mari Director, Brand & Advertising
• Emily Heath Marketing Manager, System Initiatives & Service Lines
• Randi Mednick, MHA VP, Strategic Planning
• Lisa Santeramo VP, Government Relations and Regulatory Affairs
• Annmarie Smith, EdD Director, Organizational Learning and Innovation
• Dilys Whyte, MD Pediatric Nephrology, Good Samaritan University Hospital
• Paul Stuart, MBA VP, Human Resources
• Jason Tagliarino, RN, MBA AVP, Population Health Systems
Campus Equity Leads
• Justin Jaycon, Director, Public and Community Relations, Good Samaritan University Hospital
• Christina Woods, Manager, Public and Community Relations, Good Samaritan University Hospital
• Nirvani Goolsarran, MD, FACP, CMQ, CHCQM Chair of Medicine & Chief Quality Officer, Mercy Hospital, System Vice President, Capacity Management
• Laurie Yuditsky, RN, MBA, BSN, CPHQ VP, Quality and Patient Safety, St. Catherine of Siena Hospital
• Chukwuma Egbuziem, MS, RN, CPHQ VP, Quality Management, St. Charles Hospital
• Stephen Trentowski, SHRM-CP VP, Human Resources, St. Charles Hospital
• Ingrid Collymore, MSN, RN, CCM Manager, Quality & Performance Improvement, St. Francis Hospital & Heart Center
• Laurie Nolan-Kelley, DNP, RN VP, Quality and Performance Improvement, St. Francis Hospital & Heart Center
• Melanie Ambrose, MSN, RN VP, Quality and Performance Improvement, St. Joseph Hospital
• Bari Rees, MSW, MBA, LCSW Assistant Director, Care Coordination, St. Joseph Hospital
Catholic Health Physician Partners Equity Leads
• Josepha Miranda, RN, MA VP, Ambulatory Clinical Practice, Catholic Health Physician Partners
• Fannie Cheng AVP, Physician Engagement, Catholic Health Physician Partners
Home Care and Good Shepherd Hospice Equity Leads
• Kim Kranz, MS, BSN President, Catholic Health Home Care and Good Shepherd Hospice
• Mary Frawley, DNP, RN AVP, Catholic Health Home Care
• Kim Pestour, RN, MHA, COS-C Director, Performance Improvement, Catholic Health Home Care
• Rivkah Brenenson, LCSW Director, Performance Improvement, Good Shepherd Hospice
Health Equity Leadership Council Committee Chairs
• Catholic Health First: Paul Stuart, MBA VP, Human Resources
• Long Live Long Island: Lisa Santeramo VP, Government Relations and Regulatory Affairs
• Education: Annmarie Smith, EdD Director, Organizational Learning and Innovation Dilys Whyte, MD Pediatric Nephrology, Good Samaritan University Hospital
• Quality and Data: Monique Ford, MBA, CPXP VP, Human Experience Jason Tagliarino, RN, MBA AVP, Population Health and Enterprise Analytics
Catholic Health Quality and Regulatory team leaders
• Monique Ford, MBA, CPXP VP, Human Experience
• Chhavi Katyal, MD, MBA, MS SVP, System Chief Quality Officer
• Anna ten Napel, PhD, RN, NP VP, Regulatory Affairs and Performance Improvement
992 North Village Avenue
Rockville Centre, NY 11570
Follow Catholic Health!
