Mission Statement
We, at Catholic Health, humbly join together to bring Christ’s healing mission and the mission of mercy of the Catholic Church expressed in Catholic health care to our communities.
St. Francis Hospital Service Area
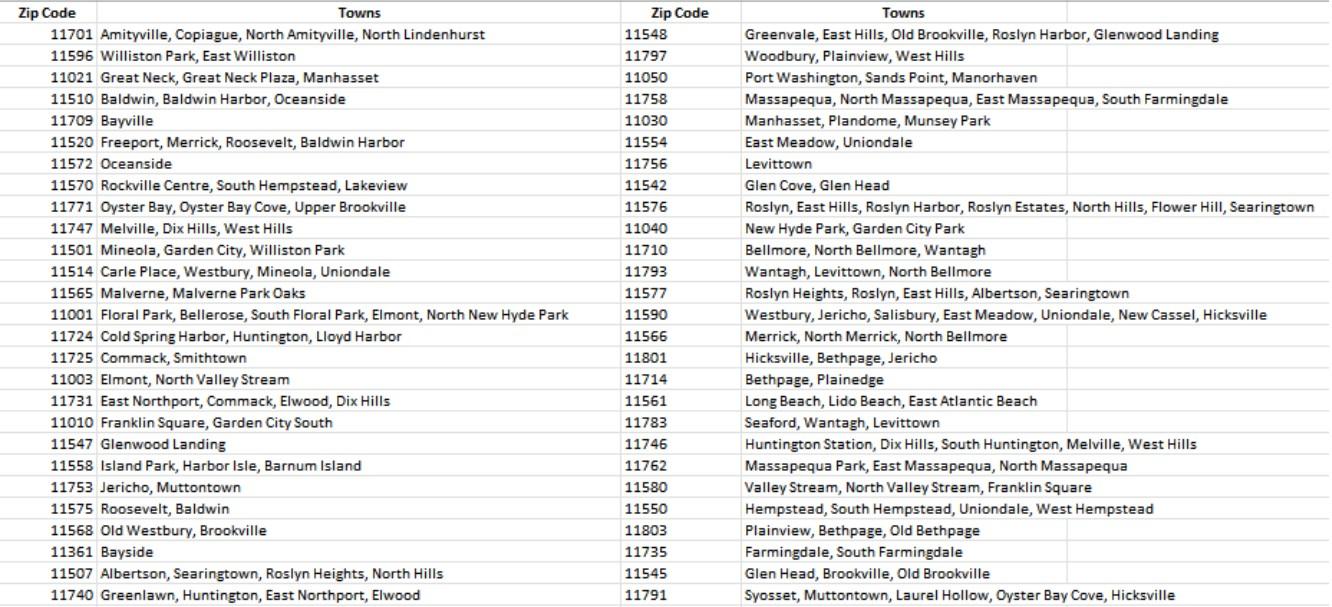
Founded by the Sisters of the Franciscan Missionaries of Mary, St. Francis Hospital is a 306-bed hospital that has served the residents of Nassau County and nearby communities since 1922. St. Francis Hospital is located in Roslyn, NY. St. Francis’ primary service area is Nassau County, but the hospital also serves patients from eastern Queens and western Suffolk. The chart below defines the zip codes and municipalities comprising the service area.
Demographics
Nassau County’s total population as of 2020 is 1,395,774 (47.3% male; 49.8% female). Those ages 15-44 represent 35.1% of females; 37.5% of males; ages 60 plus represent 22.6% of males and 26.6% of females; 18 plus represent 77.3% of male and 79.5% of females. The region is predominately White at 58.5% with 10.9% Black/African American (a decrease from 11.5% last report) and 11.7% Asian (up from 9.1%). Hispanic or Latino represent 18.3% of the population1, a two percent increase from the last report.
Geographic description
Nassau County is situated east of New York City and spans 453 miles. It is one of two counties that comprise Long Island, the eastern-most part of New York State. Nassau County is comprised of two cities: Long Beach and Glen Cove and three townships: Hempstead, North Hempstead, and Oyster Bay. Long Island is bounded on the north by Long Island Sound and on the east and south by the Atlantic Ocean. The west of the county is joined to Queens County and Kings County (or Brooklyn). These are two of the five boroughs of New York City. In addition to Nassau County, Catholic Health (CH) serves patients in eastern Queens and parts of western Suffolk County.
1U.S. Census Bureau, 2020 Decennial Census Socioeconomic information
In terms of income, 31% of the population earn less than $74, 999 (up from 26.5% in the last report) with 13.5% of that group earning less than $34,999 annually. Of the population, 6.2% of those under 18 years of age live in poverty, while 5.1% of those ages 18 to 64 live in poverty and for those ages 18 to 34 years of age, 6.4% live in poverty.2 The percentage of the population (5 years and over) that speaks a language other than English at home is 28.8%, with Spanish the dominant other language spoken (12.8%) followed by other Indo/European languages (9.9%) and Asian languages (4.9%). In terms of education, for those age 25 and over, 91.6% are high school graduates or higher, 46.7% hold a bachelor’s degree or higher. The percent of the total population uninsured is 4.1%. Of that percent, non-citizens represent 36.3%, Hispanic Latino (43%) and Black/African American (13.6%), Asian (12.8%) and White (43.2%). Of the uninsured, 40.4% earn less than $74,999 household income and 10.1% earn under $25,000 household income. Approximately 8.5% of the total non-institutionalized population is disabled. By race/ethnicity, 11.4% of the Native Hawaiian/Pacific Islander population is disabled, 10.8% of the American Indian/Alaska Native population is disabled, 9.7% of the White population is disabled, 5.4% of the Hispanic Latino population is disabled and 7.1% of the Black/African American population is disabled. Native American/Pacific Islanders account for less than one percent of the county’s population.3
Income—one social determinant of health—precludes individuals from low-income communities from accessing preventive and/or medical care due to their difficulty to afford co-payments/deductibles (if insured) or care at all if they are uninsured. The inability to afford co-pays and deductibles consistently rises to the top as a barrier to health care on the LIHC’s Community Health Assessment Survey year after year. The median household income in the past 12 months by race is $124,300 (White), $105,331 (Black), $95,890 (Hispanic/Latino). Mean income for the past 12 months per capita by race is $60,972, $38,622 and $31,976, respectively.4 This is why income is such a driving factor for health disparity and why the region has selected to focus on interventions and strategies that level the playing field for communities that are pockets of poverty in a rather affluent region.
Key Health Partners
Partnering with community-based organizations is the most effective way to determine how the health priorities will be addressed As part of our collective impact strategies to promote health and well-being for residents in our communities, St. Francis Hospital has strong relationships with local and regional community-based organizations, libraries, schools, faith-based organizations, the local health department, local fire departments and municipalities that support and partner with us to reduce chronic disease, mental health and substance misuse, and to promote health equity. Some of St. Francis’ partners include: the Long Island Health Collaborative (LIHC), Nassau County Department of Human Services, Catholic Charities and Catholic Faith Network (CFN).
Public Participation
St. Francis Hospital, along with Catholic Health’s other five hospitals, worked with the Long Island Health Collaborative (LIHC) and the Suffolk County Department of Health Services (SCDOHS), and dozens of communitybased organizations, libraries, schools and universities, local municipalities, and other community stakeholders to produce the CHNA. SCDOHS representatives offered input and consultation, when appropriate, regarding the data analyses conducted by the LIHC and DataGen. Top, high-level findings include a continued prevalence of chronic
2U.S. Census Bureau, 2016-2020 American Community Survey, Five-Year Estimate
3U.S. Census Bureau, 2016-2020 American Community Survey, Five-year Estimates
4U.S. Census Bureau, 2016 – 2020 American Community Survey Five-Year Estimates
disease incidence, particularly heart disease, diabetes, obesity and cancer. Further, surging rates of mental health and substance misuse issues among all demographic categories was found, with disparity seen among youth, and low-income communities of color continuing to experience a higher burden of disease overall. In 2022, members of the LIHC reviewed extensive data sets selected from both primary and secondary data sources to identify and confirm New York State Prevention Agenda priorities for the 2022-2024 Community Health Needs Assessment cycle. Data analysis efforts were coordinated through the LIHC, which served as the centralized data return and analysis hub.
Results of Community-Wide Survey
Primary data was obtained from a community health needs assessment sent to individuals and a similar survey to community-based organization leaders7. Additionally, we looked at results from two qualitative studies to round out our primary data.8 Secondary data was derived from publicly-available data sets curated by DataGen into its proprietary data analytics platform, CHNA Advantage ™, offering 200 plus metrics to determine health issues within Suffolk County.9 As such, priorities selected for the 2022- 2024 cycle remain unchanged from the 2019 – 2021 cycle selection, and the selected health disparities in which partners are focusing their efforts rests on the inequities experienced by those in historically underserved communities and communities of color. Additional Prevention Agenda priorities/disparities being addressed by St. Francis Hospital are outlined in the 2022-2024 work plan (See Appendix E).
Community Health Priorities for 2023-2025
Primary and secondary data demonstrate that residents living in Nassau and Suffolk County are experiencing poor mental health status. The 2021 Robert Wood Johnson Foundation County Health Rankings examining Suffolk County in Quality-of-Life Health Outcomes demonstrates an average of 4.0 poor mental health days per 30 days in Suffolk County.8 Mental health issues have soared in the past two years, spurred in part, by the effects of the pandemic. Using data from the U.S. Census Bureau’s COVID19 Household Pulse Survey (April 23, 2020 – October 26, 2020), a New York State Health Foundation analysis found that more than one-third of adult New Yorkers reported symptoms of anxiety and/or depression, with racial and ethnic groups of color as well as low-income New Yorkers, reporting the highest rates of poor mental health. However, the 18 – 34-year-old age group reported the highest rates (49%) of poor mental health.9 High school students (grades 9 through 12) fared just as badly. A number of studies found poor mental health along with suicide ideation intensified during the pandemic for high schoolers. An April 2022 analysis of data from the 2021 Adolescent Behaviors and Experiences Survey revealed that 37.1% of students experienced poor mental health during the pandemic, and 31.1% experienced poor mental health during the preceding 30 days.10 The pandemic made a bad situation worse, especially for
5U.S. Census Bureau, 2016 – 2020 American Community Survey Five-Year Estimates
6https://www.unitedwayli.org/ALICE2020
7Statewide Planning and Research Cooperative System (SPARCS), New York State Prevention Agenda dashboard, Behavioral Risk Factor Surveillance System (BRFSS), Extended Behavioral Risk Factor Surveillance System (eBRFSS), New York State Community Health Indicators by Race/Ethnicity Reports, Community Health Indicator Reports, Prevention Quality Indicators, CDC Places, and U.S. Census Bureau. The CHNA Advantage™ data analytics platform includes these and other state and national level indicators. It also encompasses social risk measures offered by Socially Determined, Inc.
8https://www.countyhealthrankings.org/app/new-york/2021/compare/snapshot?counties=36_059%2B36_103
9https://nyhealthfoundation.org/resource/mental-health-impact-of-the-coronavirus-pandemic-in-new-york-state/#:~:text=The %20proportion%20of%20New%20Yorkers,health%20throughout%20the%20survey%20period
10https://www.cdc.gov/mmwr/volumes/71/su/su7103a3.htm? s_cid=su7103a3_w
youth, as mental health issues and suicides were already increasing prior to the COVID-19 pandemic. 11 12 13 14
With the shortage of mental health care workers and the lingering psychological effects of the pandemic, mental health services remain a top priority for the region. The county also saw an uptick in opioid-related overdoses and deaths after having made some gains prior to the pandemic. New York State Department of Health statistics report that for 2020 in Nassau County there were 223 deaths from any opioid, 77 heroin overdose deaths, and 214 deaths involving opioid pain relievers (including illicitly produced opioids such as fentanyl).15 For 2019, the numbers were 173, 47, and 163, respectively via categories listed above.16
Another health disparity identified in primary and secondary research is adult obesity. Nassau County continues to experience high rates of obesity and overweight adults. Twenty three percent of the population (age 20 and older) reports a body mass index (BMI) greater than or equal to 30 kg/m.17 According to the New York State Department of Health, obesity is a significant risk factor for many chronic diseases including type 2 diabetes, high blood pressure, asthma, stroke, heart disease and certain types of cancer.
The prevalence of chronic diseases is persistent in the county. Nationally, communities of color experience higher rates of chronic disease. Using diabetes as an example, the American Indian/Alaska Native population represents 14.5 percent of adults 18 or older who are diagnosed with diabetes followed by Black, non-Hispanic at 12.1% and Hispanic overall at 11.8% in the United States. Asians and Whites experience the disease at 9.5% and 7.4% respectively.18 Health providers report that many individuals delayed preventive care and routine screenings due to the pandemic, leading to more complicated cases and unfavorable outcomes. Chronic diseases are preventable conditions sensitive to lifestyle (diet/physical activity) habits but hampered by the obstacles presented by social determinant of health factorsincome/employment, race/ethnicity, food access, housing/neighborhood location, and level of education. The county and hospitals identified in this report through collaborative efforts and facility-specific programming acknowledge and address these determinants regularly.
11https://www.cdc.gov/mmwr/volumes/66/wr/mm6630a6.htm
12https://www.cdc.gov/nchs/fastats/mental-health.htm
13Weinberger, A. et al. (August 2017) Trends in depression prevalence in the USA from 2005 – 2015: widening disparities in vulnerable groups. Psychological Medicine, 1-10
14Bitsko, R et al. (2018) Epidemiology and impact of healthcare provider-diagnosed anxiety and depression among US children. Journal of Developmental and Behavioral Pediatrics, 1-9.
15https://www.health.ny.gov/statistics/opioid/data/pdf/nys_apr22.pdf
16https://www.health.ny.gov/statistics/opioid/data/pdf/nys_jan21.pdf
17https://www.health.ny.gov/statistics/prevention/injury_prevention/information_for_action/docs/2021- 02_ifa_report.pdf
18https://www.cdc.gov/diabetes/health-equity/diabetes-by-the-numbers.html
St. Francis Hospital Interventions, Strategies and Activities
Priority Number One: Prevent Chronic Disease
Goals and selected interventions concentrate on Focus Area 4: Chronic Disease Preventive Care and Management, with additional programming addressing other focus areas.
Interventions, Strategies and Activities:
1. Live Better Awareness Campaign: Promote healthy eating and food security to increase skills and knowledge to supply healthy food and beverage choices. The goal is to decrease the percent of adults over 18 with obesity in low-income communities of color.
Process measures:
The hospital’s Weight Management Program had approximately 453 patient visits. In addition, staff performed 2,584 Outreach BMI screenings and offered a Community Heart of Good Eating class; in 2025, 67 attended.
2. Offer screenings that improve the detection of undiagnosed hypertension in community settings.
Process measures:
To address undiagnosed hypertension, in 2025, we performed 785 blood pressure screenings in libraries, senior centers and the other community venues and another 2,780 on our Mobile Outreach Bus for a total of 3,565, resulting in 166 referrals made for those with ranges outside the norm.
3. The St. Francis community outreach bus offers health screenings, flu vaccines, education and referrals to care five days a week in underserved communities.
Process measures:
In 2025, the Mobile Outreach Bus screened 3,386 Long Islanders, offering blood pressure, BMI, glucose and cholesterol testing.
4. Cardiac screenings for high school athletes in grades 9 through 12 including free CPR/AED instruction to families who attend.
Process measures:
We assisted student athletes, providing free cardiac screening to 293 students with 55 in need of follow-up care in 2025.
5. Train St. Francis staff to become lifestyle coaches and offer a program to community members.
Process measures:
St. Francis has two coaches trained for the Stepping On Falls Prevention Program. We offered one workshop in the spring and plan to offer another series in the fall. We have hired a per diem nurse from a sister Catholic Health hospital who has had the Stepping On training, and has assisted with class sessions, so now we have three trained instructors. Additionally, we had three coaches trained in the Diabetes Prevention Program (DPP). We have an additional dietician who completed the training to be a lifestyle coach for the DPP in the fall.
6. In a nonclinical setting, provide BP and BMI screenings, flu vaccinations, health education and referrals to follow up care as needed.
Process measures:
In 2025, on the Mobile Outreach Bus, we conducted 2,780 screenings (BP, total cholesterol and HDL, glucose and BMI), resulting in 166 referrals made for those with ranges outside the norm.
Flu vaccination program community sites were visited with our Mobile Outreach bus and Healthy Sundays parishes. A total of 1,266 flu vaccines were given in 2025.
On 9/20/25, Catholic Health hosted its annual health fair in Melville; more than 200 people attended, 54 screened and 27 flu shots were administered.
CH participated in Oyster Bay’s annual OysterFest on 10/18/24 and 10/19/24, providing a total of 269 blood pressure screenings and education over 2 days.
The hospital provides CPR training for the community. From Jan-Nov 2025, 1,907 people were trained.
In 2025, there were two DPP programs held. Four people participated in the program running from December 2024 through November 2025. Nine people are participating in a program that began in June 2025 and will conclude in June 2025.
7. American Lung Association Freedom from Smoking program.
Process measures:
The American Lung Association Freedom from Smoking program is open to participants who want to quit. Each program runs over seven sessions. We saw 13 patients in 2025.
8. Offer blood test for prostate specific antigen (PSA) at the hospital and some community locations.
Process measures:
Prostate screening programs were offered at the DeMatteis Center in September, for Prostate Awareness month. A total of six patients were screened. We also screened 17 at the ESRLI event in June, for a total of 23.
9. Conduct lectures and provide a speakers bureau program on health topics such as cardiovascular disease, diabetes, cancer, injury and disease prevention, and optimizing wellness to enhance quality of life and promote well-being.
Process measures:
Please see the below chart for dates/locations/number of people attending.
MISCELLANEOUS EVENTS 2025
Priority Number Two: Promote Well-Being and Prevent Mental and Substance Use Disorders
Interventions, Strategies and Activities:
1. Continue to distribute Catholic Health’s (CH) Mental Health Substance Use Disorder Services Guide to CH community partners at all outreach events, including hospital health fairs and Healthy Sunday’s events. The guide is available as a download from the CH website.
Process measures:
The Catholic Health Mental Health Substance Use Disorder Guide was available at all hospital health fairs and community events, including at our Mobile Outreach Bus screenings, community blood pressure screenings, and a variety of health education events.
2. Provide Narcan training classes for the community.
Process measures:
St. Francis Hospital is a designated American Heart Association training center for emergency care courses. In 2025, there were 1,907 people trained in CPR. Narcan training is also offered to the community. In 2025, two people were Narcan trained. We hope to expand this in 2026.
3. Offer community programs in: Diabetes Support, Stroke Support, Oncology Support, stretching/toning exercise movement and relaxation classes, and stress management to patients with chronic conditions and their family members.
Process measures:
In 2025, we hosted the following support groups and educational classes: Diabetes Support Group met monthly from January to November: 65 in total attended.
Stroke Support Group met monthly from January to November: 198 in total attended.
Stretch and Tone classes run as a 10-week series: 143 patient visits in total attended.
Stress Management runs as a weekly series in 6-week blocks of time: 290 in total attended.
Meditation runs as an 8-week series in 8-week blocks of time: 393 in total attended.
Total number of patients who attended these programs = 1,089
4. Patient and Family Advisory Committee
Process measures:
To ensure we have input from the community, we have a Patient and Family Advisory Committee. This group met 3/11/25.
5. Offer an education conference for health care professionals
Process measures:
February was Heart Month, and the DeMatteis Center hosted a Women’s Heart Symposium on 2/13/25 with educational information provided by: Endocrinologist Dr. Maria Pena, Diabetes educator Jane Giordano RD, CDCES, and health educator Maura Calio RN, MA. The program was free, and open to health care professionals and the public with 65 attending.
6. Promotion of programs, events, education offered by Long Island Health Collaborative (LIHC) members who speak to the prevention of mental and substance use disorders. Posts in LIHC weekly communications newsletter, social media postings, cross promotion of member events, programs on all media platforms.
Promotion on Catholic Faith Network (CFN) and CH social media, website, and community-targeted publications.
Process measures:
St. Francis Hospital also relies upon the Long Island Health Collaborative (LIHC) to disseminate information about the importance of proper nutrition and physical activity among the general public to assist Nassau residents in better managing their chronic diseases and/or preventing the onset of chronic diseases. The hospital also relies upon the LIHC to disseminate information about mental health prevention and treatment services and programming, as well as relevant information about substance misuse. Dissemination of information is achieved through the bi-weekly Collaborative Communications e-newsletter, which is sent to 588 community-based organization leaders, and strategic use of social media platforms. These efforts are ongoing.
Priority Number Three: Promote a Healthy and Safe Environment
Interventions, Strategies and Activities:
1. Offer a fall prevention program designed to heighten awareness, reduce fall risks and build confidence in older adults.
Process measures:
In September, the Stepping On series was held over a 7-week period, with 28 patient sessions attended.
2. Classes: Moving for Better Balance, Healthy Back Wellness, Movement & Relaxation, Stretch & Tone, Renew, Relax & Restore, Chair Exercise for all ages, stress management & meditation
Process measures:
St. Francis offers the following classes. In 2025:
Moving for Better Balance: 59 attended.
Healthy Back Wellness: 102 attended.
Relax & Restore: 130 attended.
Stretch & Tone: 143 attended.
Chair exercise: 98 attended.
Stress management: 290 attended.
Meditation: 393 attended.
Total number of patients who attended these programs = 1,215
Priority Number Four: Prevent Communicable Diseases
Interventions, Strategies and Activities:
1. Offer free flu vaccinations at events in underserved communities, at Healthy Sundays outreach, hospital health fairs and other community venues.
Process measures:
Our Mobile Outreach bus and Healthy Sundays program visited a number of community sites, providing 1,266 flu vaccines in 2025.
Living the Mission
The CH mission is the driving force behind all community outreach activities. In addition to the interventions summarized above, St. Francis Hospital, along with the overall system and CH skilled nursing facilities, Catholic Health Home Care and Good Shepherd Hospice, provide additional outreach programs that promote the health care ministry of the Catholic Church and address social determinants of health.
Interventions, Strategies and Activities:
1. Virtual education series streaming on YouTube, providing short videos on various topics
Currently there is a Keeping Your Child Safe at Every Age, Child and Adolescent Mental Health, Alzheimer’s and dementia series. These have garnered more than 30,000 total views.
Catholic Health also offers an ongoing Health Tips series discussing topics such as Stroke vs. Aneurysm, What You Need to Know about C-Sections, and Prostate Cancer Awareness, among others. From January-December 2025, there have been 3 videos posted, with more than 90 views on YouTube.
The “On-Call with Dr. Jason Golbin” show is designed for physicians and advanced practice providers. In each monthly episode, Catholic Health’s Chief Medical Officer Jason Golbin, DO, speaks with our physician leaders about the system’s emerging technologies and newest clinical resources while offering a glimpse into their personal stories and the compassionate care delivered. From January to December, these videos have had more than 411,000 views across multiple platforms.
2. Broadcast health-related television shows for the public, in collaboration with Catholic Faith Network, provide education and prevention lectures to improve knowledge related to specific diseases and conditions, preventive care, and up-to-date treatment options.
From January-December 2025, seven new shows with Catholic Health Cardiologist David D’Agate, DO, aired on CFN and were posted to Catholic Health’s YouTube channel. The “Stronger Together” series with Dr. D’Agate discusses topics such as cardiac health, sleep, fertility, and access to care. This show airs on CFN every four to five weeks and is promoted via Catholic Health’s internal and external communications, including a substantial social media campaign. Across multiple platforms, these videos have more than 913,000 views. Additionally, a Catholic Health segment on CFN Live, “Trending Health Topics,” produced 2 segments from January-December 2025. These videos have more than 170 views on YouTube.
There are also quarterly shows on CFN with Catholic Health President and CEO Patrick O’Shaughnessy, DO. The shows with Dr. O’Shaughnessy and Monsignor Jim Vlaun bring the latest in research and information on medical procedures and advancements. There have been 3 videos posted in 2025, totaling more than 280 views.
Additionally, Catholic Health airs a “Catholic Health Update” weekly, highlighting events or activities taking place across the system. From January-December 2025, these videos received more than 2.1 million views across all platforms.
3. Promotion of all programs, events, and education is on the CH website and all CH social media outlets, including Facebook, Twitter, Instagram, and LinkedIn.
This includes the promotion of all education, healthy recipes, health tips and support groups. Some of these include education on how to stay hydrated during the summer, facts on various cancers and screening, children’s health and more.
4. Lectures in Catholic schools, local libraries, and other community organizations.
The Catholic Health Speakers Bureau provides speakers to community organizations. From JanuaryDecember 2025, there have been 84 speaking engagements. Topics have included Heart Health, Fitness for Seniors, Breast Health, Medication Management, Seasonal Depression, and Sleep Health.
Catholic Health has partnered with AARP to host a virtual lecture series. These lectures are being held monthly from June through December.
6/18/25 – Men’s Health; 40 attended.
7/16/25 – Keep Your Sight as You Age; more than 100 attended.
8/20/25 – Concepts of Grief and How to Cope; 45 attended.
9/17/25 – Food for Thought; more than 400 attended.
12/17/25 – Safely Stay Active During the Winter: 33 attended.
5. Community Outreach Screening Buses
The Catholic Health buses travel across Long Island to different community-based organizations, providing free health screenings, including blood pressure, cholesterol, body mass index and glucose. From January through December 12, the mobile buses screened 7,493 people.
6. Healthy Sundays
In this volunteer program, we partner with different community organizations to provide BP and BMI screenings, flu vaccinations, health education and referrals to follow up care. In this volunteer program, we partner with different community organizations to provide BP and BMI screenings, flu vaccinations, health education and referrals to follow up care. Twelve events were held through December; 471 people attended.
7. Additional Community Outreach
On 4/1/25, CH employees packed food for Meals of Hope. Forty-seven employees participated and 46 boxes of food were prepared, equaling almost 10,000 meals.
On 4/12/25, CH attended Tomorrow’s Hope 10th Annual Run in Garden City and provided cardiac screenings to 6 people.
On 5/23/25, 5/24/25, and 5/25/25, CH attended the Jones Beach Air Show and provided blood pressure screenings to a total of 195 people.
On 9/20/25, Catholic Health held its annual system-wide health fair; more than 200 people attended, 54 people received blood pressure, cholesterol, glucose and body mass index screenings and 27 flu shots were administered.
On 9/27/25, CH attended St. Vincent de Paul’s annual Friends of the Poor Walk, providing health information. More than 850 people attended.
CH participated in Oyster Bay’s annual OysterFest on 10/18/24 and 10/19/24, providing a total of 269 blood pressure screenings and education over 2 days.
Dissemination of the Plan to the Public
The St. Francis Hospital Community Service Plan will be posted on the hospital’s website at https://www.chsli.org/st-francis-hospital/community-health. Copies will be available at local free health screenings and can be mailed upon request.
By encouraging friends and neighbors to complete the LIHC Wellness Survey online or at local screenings, the Community Health Needs Assessment will help St. Francis continue to develop ways to best serve our community.
Conclusion
The Community Service Plan is intended to be a dynamic document. Utilizing the hospital’s strengths and resources, St. Francis, along with community partners, will work to continue to best address health disparities and needs. The hospital will strive to improve the overall health and well-being of individuals and families by expanding free health promotion and disease prevention/education screenings and programs in communities where they are most needed. St. Francis Hospital is committed to continue to develop ways to best serve the community.