‘Fascinating’
SARAH
GILBERT


‘Fascinating’
SARAH

‘Brilliant’
TIM SPECTOR
‘Excellent’
HENRY MARSH
Liam Shaw
The Bodley Head, an imprint of Vintage, is part of the Penguin Random House group of companies
Vintage, Penguin Random House UK , One Embassy Gardens, 8 Viaduct Gardens, London SW 11 7BW penguin.co.uk/vintage global.penguinrandomhouse.com
First published by The Bodley Head in 2025
Copyright © Liam Shaw 2025
The moral right of the author has been asserted
Penguin Random House values and supports copyright. Copyright fuels creativity, encourages diverse voices, promotes freedom of expression and supports a vibrant culture. Thank you for purchasing an authorised edition of this book and for respecting intellectual property laws by not reproducing, scanning or distributing any part of it by any means without permission. You are supporting authors and enabling Penguin Random House to continue to publish books for everyone. No part of this book may be used or reproduced in any manner for the purpose of training artificial intelligence technologies or systems. In accordance with Article 4(3) of the DSM Directive 2019/790, Penguin Random House expressly reserves this work from the text and data mining exception.
Typeset in 12/14.75pt Dante MT Std by Six Red Marbles UK, Thetford, Norfolk Printed and bound in Great Britain by Clays Ltd, Elcograf S.p.A.
The authorised representative in the EEA is Penguin Random House Ireland, Morrison Chambers, 32 Nassau Street, Dublin D 02 YH 68
A CIP catalogue record for this book is available from the British Library
HB ISBN 9781847927545
TPB ISBN 9781847927552
Penguin Random House is committed to a sustainable future for our business, our readers and our planet. This book is made from Forest Stewardship Council® certified paper.
Let us not, however, flatter ourselves overmuch on account of our human conquest of nature. For each such conquest takes revenge on us.
Friedrich Engels
The Klondike is a region of north-west Canada where the winters are long and cold. If you dig six feet into the ground you will hit the permafrost: frozen soil under the soft surface, iron-hard any day of the year. In the late nineteenth century, prospectors flooded to the region, drawn by news of gold in the ground, but they couldn’t dig past the permafrost. Instead, they dug holes in the topsoil, then set fires and watched them burn. Through the long winter nights, flames raged across the valleys as the fires melted down through the earth itself.
Without knowing it, the prospectors were melting history. Permafrost is a record of the past. Its layers hold ancient DNA in ideal preservation: the deeper you go into the ground, the further back you go in time, like rifling through a frozen stack of Ice Age postcards.
On a summer day in 2007, just a few kilometres from where the Klondike Gold Rush had begun, a group of scientists stood in front of a cliff of permafrost. It had been exposed by twentieth-century mining, when miners had moved on from shovels to more powerful machines that split open the frozen earth. The scientists approached the site like forensic investigators at a crime scene. They drilled horizontally into the cliff, pulling out a short cylinder of 30,000year-old permafrost. After shipping it back to McMaster University in Ontario, they worked on it in a dedicated cleanroom. They carefully sterilised their tools, then cut two small incisions across the icy cylinder and split it using a hammer and chisel: out popped a disc as thick as a hamburger. They punched chunks out of the hamburger and dissolved them in hot chemicals. At that point, frozen cells in
the soil that had been locked away for thousands of years melted, burst and released their DNA .
When the scientists sequenced the DNA , a whole world shimmered out of the fragments, summoning the molecular ghosts of extinct bison and woolly mammoths that had once wandered through a lost landscape of sage-grass and willow. But the scientists hadn’t gone in search of the ghosts of mammoths. They were looking for antibiotic resistance.
From the beginning, we have shared our world with trillions of microbes. Among them are the invisible assailants responsible for infectious diseases, which range from trivial ailments to the most notorious scourges of humanity. Some are viruses such as HIV: tiny bundles of genetic material with no cells of their own, which hijack our cellular machinery to churn out copies of themselves. Some are fungi, such as the Trichophyton moulds that cause athlete’s foot. Some are parasites, such as the Plasmodium species that cause malaria. And some are bacteria.
Bacteria live almost everywhere. They can be found on land, from the deepest gold mines to the highest peaks; in air, from the clouds over Antarctica to a packed commuter train; in water, from near- boiling geysers to the ocean’s darkest abyss. They can also be found inside us, coating our gums and lining our guts. There are far more bacterial species than science has reliably identified, but we know that most of the tens of thousands we have named are harmless. However, a minority have the capacity to cause infection and disease. In contrast to the blitzkrieg of deaths caused by a viral pandemic such as Covid- 19, bacterial infections are a slow attritional war. The number of culprits is small, but their impact is colossal: just over thirty bacterial species are linked to 1 in 8 of all deaths worldwide. Invisible to the naked eye, these minuscule creatures with strange and unwieldy names – Staphylococcus aureus , Escherichia coli , Streptococcus pneumoniae – are some of the world’s biggest killers. Our best defences against them are antibiotics.
An antibiotic is any medicine that works to kill or incapacitate bacteria.* Starting in the 1930s, effective antibiotics caused a transformation in human history without precedent. Within just a few decades, the world’s worst infectious diseases could be cured. Writing in the aftermath of that revolution, one British doctor in 1968 commented that ‘no one recently qualified, even with the liveliest imagination, can picture the ravages of bacterial infection which continued until little more than thirty years ago’. Antibiotics did more than vanquish diseases; they permitted the entire edifice of modern medicine to be built up on their foundation.
Consider surgery. Cutting people open and breaking the protective barrier of the skin had always been astonishingly dangerous, because it gave bacteria the chance to swarm into the body’s internal tissues. Before antibiotics, even the simplest procedures could result in blood poisoning, sepsis and death. With antibiotics, surgery became significantly safer and its remit expanded: heart surgery, intestinal surgery and liver transplants became routine. Or consider cancer: chemotherapy suppresses the immune system, leaving patients vulnerable and exposed to bacterial attack. Infections are one of the biggest complications of cancer care, and one in five cancer patients will receive antibiotics during their treatment. Cancer and surgery are not exceptions. In almost every area of medicine, the sophistication of our most advanced treatments relies on antibiotics. However, not every antibiotic kills every bacterium. The diversity of different bacterial species is reflected by the diversity of different antibiotics, resembling the range of weapons available in an armoury. There are over sixty different antibiotics in the World Health Organization’s list of essential medicines, each effective against a slightly different range of bacteria. A bacterium that can survive treatment with an antibiotic is resistant to it. Bacteria can
* Some scientists use ‘antibiotic’ to refer only to natural products produced by living organisms; for a more general term for bacteria-killing substances, they prefer ‘antibacterial’ or ‘antimicrobial’. In this book, I follow common usage and call all these medicines antibiotics.
either be resistant intrinsically – just as rock is ever impervious to scissors – or evolve to become so. They can resist an antibiotic in a number of ways: they can modify what it attacks, destroy it directly, pump it out of the cell before it can do damage, or stop it getting inside in the first place. The details of any particular resistance can be intricate, but the outcome is simple: antibiotic treatment fails.
From the introduction of antibiotics, doctors were horrified to find that this was possible. It seemed as if antibiotics themselves were capable of conjuring up even more fearsome bacteria. But resistance is nothing more than a simple consequence of evolution. Each time an antibiotic was used, it killed off the bacteria that could be killed and left behind those that could not. Whether because of a chance mutation in their genes or the possession of different genes altogether, they remained unaffected. Using an antibiotic caused susceptible bacteria to diminish and resistant bacteria to thrive, and those resistant bacteria could spread between people. Tragically, the miraculous powers of these new medicines could wane over time.
Over the twentieth century, each new antibiotic seemed to give rise to new resistance genes. Where were they coming from? In search of the origins of resistance, scientists turned to the freezers that lurked in the corners of universities, hospitals and departments of public health. These freezers contained old samples of bacteria from the start of the twentieth century, from before the discovery of antibiotics: samples from Italian dysentery epidemics or the ghastly wounds of WWI soldiers. When scientists searched these archives, they found that the bacteria in the freezers had few if any of the genes that caused modern antibiotic resistance. It was as if the introduction of antibiotics had prompted sudden changes in bacteria. Antibiotic resistance appeared to be a thoroughly modern story of technological hubris.
Others disagreed. In 2006, the Canadian microbiologist Gerry Wright showed that handfuls of dirt collected far from human settlements contained antibiotic-resistant bacteria in abundance. To many, that was an alarming surprise. But a common criticism was
that no corner of the world had been unaffected by humans: how could Wright be sure that the soil hadn’t somehow been contaminated with antibiotics? To address that objection, Wright needed to analyse soil from the deep past.
That was where the Klondike came in. Wright and his colleagues hoped to use the permafrost as a natural freezer. When they analysed its ancient frozen DNA , they found something extraordinary. Amid the fragments of mammoth and bison there were bacteria that were resistant to modern antibiotics. The scientists even found resistance genes against an antibiotic called vancomycin, which was relied upon as a last-ditch treatment for the resistant superbug known as MRSA . Vancomycin had first been used in 1955 – but the permafrost did not lie.
It seemed like a paradox. How could frozen bacteria from 30,000 years ago be resistant to an antibiotic created in the 1950s? The answer was that antibiotics were not invented in the twentieth century. They were far, far older.
Humans discovered antibiotics in the twentieth century, but we did not invent them. Most of the important antibiotics we rely on today are based on molecules made by single-celled microbes – the same forms of life that cause infectious disease. Killing one of these cells is easy: you can boil it into oblivion or dissolve it with acid. But we cannot use boiling water or acid to kill bacteria inside the body, because that would also harm us. This is where antibiotics are different. Over millions of years of evolution, bacteria and fungi evolved molecules to kill, maim or incapacitate each other. But our last common ancestor with bacteria lived billions of years ago. Evolution since has made the basic cellular architecture of humans very different from bacteria. A human cell has evolved to live only within the fluid maintained inside human bodies, where the concentration of molecules outside the cell balances what’s inside. If you place a cell from your body into pure water, it will slowly expand as water rushes in through its permeable membrane, before bursting like an overfilled balloon. In contrast, bacteria have a cell wall which keeps
them rigid in water, allowing them to survive in many different environments.
Antibiotics evolved in nature to target cellular components that bacteria possess and we do not. That simple fact means we can safely ingest antibiotics and leave our own cells largely unscathed. In this way, antibiotics are unique among medicines. Most drugs do their work by interfering with human cells: aspirin relieves your headache by dampening the chemical signals of pain and inflammation; caffeine wakes you up by blocking adenosine receptors, preventing drowsiness taking hold. In contrast, an antibiotic targets bacteria – an ancient curse in a language that humans no longer speak.
Antibiotics may be ancient molecules, but their deployment by humans is modern. Although history contains examples of people using antibiotic-producing moulds to treat wounds, the twentieth century was when humanity discovered how to concentrate antibiotics into medicine. That advance marks a division of history into two eras: before and after antibiotics. Like most scientific advances, it did not happen in one fell swoop. But if you had to pick a single year in which to draw the line, a reasonable choice would be 1928, when Alexander Fleming noted the activity of a strange mould juice that he called penicillin. As scientists began looking in earnest for antibiotics in the following decades, they discovered that soil contained an unimaginable bounty. By the middle of the twentieth century, what historians call the ‘golden age’ of antibiotics was in full swing.
The century since Fleming’s observation has been the antibiotic era – what historian Claas Kirchhelle has dubbed the Antibiocene. It is a young era: if Earth’s history was compressed into a single year, penicillin was discovered well into the final second. But antibiotics did not eliminate bacteria entirely. The biologist Joshua Lederberg once described microbes as ‘our competitors of last resort for domination of the planet’ – and the competition is far from over. Increasingly, there are warnings that rising levels of antibiotic resistance mean we may be approaching a third era: the post-antibiotic age.
The challenge of antibiotic resistance has often been
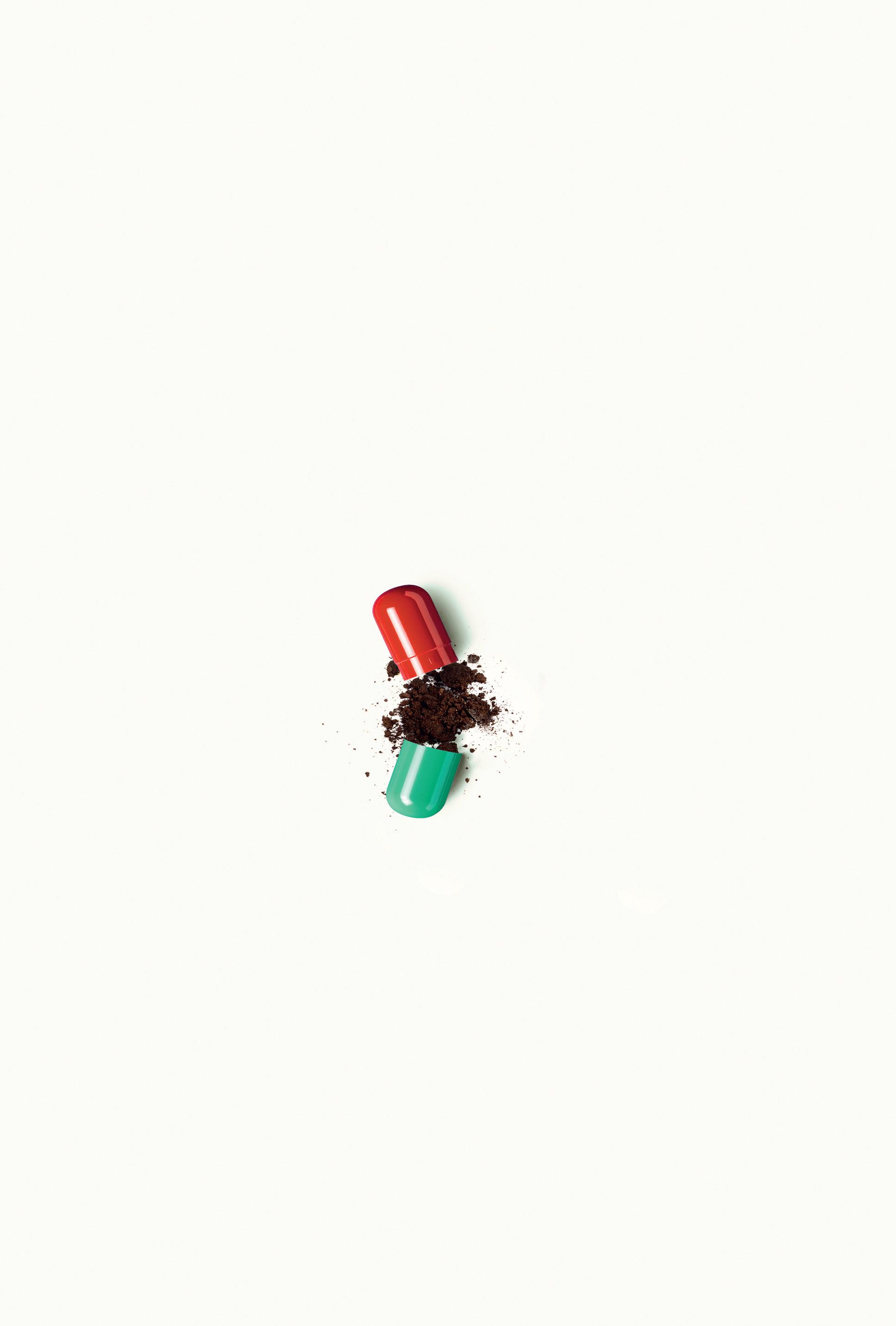
compared to climate change in its scale and scope. Indeed, there are striking similarities between fossil fuels and antibiotics. Both are natural resources that developed over millions of years before being extracted by humans. Both were mined heavily, fossil fuels powering the global economy and antibiotics fuelling modern medicine. And both offered a promise of cheap, miraculous and never-ending power that was taken as evidence of human ingenuity and mastery over the natural world. But that, of course, is only half the story. For both fossil fuels and antibiotics, their extraordinary power emerges not from human technology, but from their origins in life’s distant past. As the Earth’s geology transmuted dead plants into dense fuel, so evolution transmuted dead atoms into living molecules that we could use as medicines. Deep time – the near-unimaginable eons of life on Earth before humans – is a hidden wellspring from which modern civilisation flows. For the past hundred years, the extraordinary accomplishments of humanity have been powered by burning through the vastness of the past. We have been living, quite literally, on borrowed time. Antibiotics are the fossil fuels of medicine: they are fossil drugs.
To treat an antibiotic-resistant infection you need another antibiotic. Given the threat of rising antibiotic resistance, you might imagine that the discovery of new antibiotics would be proceeding at pace. The opposite is true. The dates paint a concerning picture: over half of essential antibiotics were discovered more than sixty years ago. Only one in six was discovered in the last thirty years.
Antibiotics are no longer being developed in anything like the numbers that scientists and doctors believe is necessary. In 2021, one survey of new medicines in development counted more than 4,000 molecules for cancer immunotherapy compared to fewer than forty antibiotics in clinical trials. Worse, most of those ‘new’ antibiotics were derivatives of existing medicines, meaning they would probably be vulnerable to similar forms of antibiotic resistance. In 2024, a report concluded that the number of scientists carrying out the crucial early stages of research into new antibiotics was ‘tiny’. The
world is running out of antibiotics, and new ones aren’t arriving quickly enough. Understanding how and why this happened is one of the themes of this book.
As the number of effective antibiotics diminishes, we face a corresponding rise in the number of deaths from bacterial infection. In 2024, the United Nations General Assembly agreed a declaration that called antibiotic resistance ‘one of the most urgent global health threats’. According to our best estimates, resistance is directly responsible for at least a million deaths a year worldwide. Over the next twenty-five years, drug-resistant infections will kill 40 million people, double the number that died in WWI . By 2050, forecasts predict that over 8 million people a year will die after contracting a resistant infection, and a quarter of those deaths will be for want of an effective antibiotic. Without new antibiotics, the entire structure of modern medicine will begin to crumble.
Recent patient stories from around the world reveal how antibiotic resistance can affect anyone, anywhere. Vanessa Carter from South Africa survived a serious car crash and needed a decade of facial reconstruction surgery, during which she spent three years battling a resistant infection that threatened her life. Mashood Lawal from Nigeria had a stent inserted into his urinary tract to treat a kidney stone, but developed a resistant infection that nearly killed him; he only recovered when doctors finally found the right antibiotic. In Lebanon, Nour Shamas’s mother had surgery on her spinal column and developed a resistant infection of her kidneys, commencing a series of hospitalisations and treatment failures. Gabriella Balasa from the US has cystic fibrosis, meaning she contracts recurrent lung infections which are becoming increasingly difficult to treat because of antibiotic resistance. She lives in constant fear that the next one will be untreatable.
The paradox of antibiotics is that their very success is their downfall: it is as if evolution has a dark sense of humour. The problem of antibiotic resistance has been inherent to antibiotics from the very moment of their discovery, but it has been repeatedly ignored and
evaded. To understand the crisis, we must examine where antibiotics came from and how we burned through them.
A history of antibiotics might sound like a rather dry exercise. For most of us, they don’t hold great romance or intrigue. When we encounter them they are simply another dull part of modern medicine: white powders, anonymous pills or clear fluids in syringes that we submit to in the hope of getting better. Their names are arbitrary and ugly, often as unpronounceable as they are meaningless. (Drug companies prefer words rich in Xs, Ys and Zs to convey a futuristic buzz, not for any scientific reason.) I have avoided this jargon wherever possible. Behind the pharmaceutical façade lies a sprawling epic spanning all the way from the origins of life on this planet to the cutting edge of modern science.
The story has a diverse cast of characters; not all are human, although the struggles of scientists and doctors to turn their discoveries into medicines have been just as dramatic as the bacterial warfare under the microscope. I begin with the development of germ theory in the nineteenth century, before which humanity was ignorant of the true cause of infectious disease. Each of the following ten chapters is framed around a different antibiotic, moving chronologically through the last hundred years of discovery. As we’ll see, each antibiotic has a story of its own: antibiotics have emerged from barrels of coal tar in Nazi Germany, congealed out of mud from the jungles of Borneo and even been predicted by computational algorithms. They range from drugs that have saved millions of lives to new molecules that, at the time of writing, have yet to be tested on humans. By providing the story of such different antibiotics together, my aim has been to produce a group biography – ten threads entwined into a single braid.
This is not an impartial account. I argue that the crisis of antibiotics is, at its heart, a crisis of exploitation. Antibiotics have been developed and used almost everywhere, but though I have searched out stories from around the world I cannot claim this is a truly global history. That is because my aim is to show not merely how antibiotics profoundly changed the relationship between humans and
bacteria, but how they helped to forge the modern pharmaceutical industry. To do so, I focus on that industry’s centres of power in the twentieth century: Europe and then, later, the United States. I want to explain how an industry that unleashed life-saving antibiotics on the world – and claimed the lion’s share of the credit – eventually came to abandon them. History helps not only to explain the reasons for this shift, but also to reveal other ways forward.
In the tale of the sorcerer’s apprentice, a young magician takes advantage of his teacher’s absence to cast a spell that he does not understand. Commanding a broomstick to fetch water to fill a bath, he rejoices as the spell works perfectly. Only as he watches the water level rise does he realise, with horror, that he doesn’t know how to make the broomstick stop. Soon, the whole room begins to flood. Goethe’s tale, memorably adapted in Disney’s Fantasia, is often taken as a parable for the hubris of humanity. Perhaps we are forever doomed to be the arrogant sorcerer’s apprentice, unaware of our inability to control the powers that we summon up until it is too late.
It’s a beguiling fable. But although we describe antibiotics as magical or miraculous, they operate within the powers of nature – not beyond them. I hope to convince you that bacteria aren’t evil spirits beyond our ken, but living beings that evolve and change just as we do. Through studying the history of antibiotics, we can deepen our appreciation for these varied and wonderful beings we share the world with. We can feel our connection with a deeper past. And we can, I believe, take inspiration for the future.
Our ability to comprehend antibiotic resistance at all is a mark of the phenomenal progress that we have made. Throughout human history, most people didn’t know that bacteria even existed. At a moment where we can see the problem clearly, it is hardly the time to look away.
The visible world is a late-arriving, overgrown portion of the microcosm.
Lynn Margulis and Dorion Sagan
All societies have recognised that there are two types of disease. Some afflictions are solitary affairs: ‘’Tis my sole plague to be alone,’ wrote Robert Burton in 1621 about his melancholy. Others are transferable, capable of spreading through the population like a stain soaking into cloth. These are infections, named from the Latin inficere – a verb that can mean to dye or contaminate. The great Roman doctor Galen wrote that such diseases could cause the breath of sufferers to become corrupted; the vapours they exhaled could then be inhaled by others, engendering the same sickness. The most spectacular realisations of these infectious diseases occurred as epidemics. The Black Death, which began in 1346, may have killed over half of Europe’s population in just a few years. To many it would have seemed like the end of the world.
Theories abounded as to the cause of the calamity. Where some believed the plague was due to an unfavourable alignment of the planets, others decided that God was exacting His vengeance on a sinful world. There were also more sinister theories: some said the Jews, a minority long persecuted by the Christian majority, had poisoned the wells. Across Europe, entire Jewish communities were massacred in savage genocidal attacks. It was an age of terror and violence. Around thirty years after the Black Death had first arrived in France, the Duke of Anjou commissioned a vast set of tapestries depicting the story
of the Book of Revelation. In vivid threads of red, blue and gold, the Apocalypse Tapestry wove together images of death and destruction that would have been all too familiar to those who had lived through the period. Yet the real cause of this disastrous epidemic was imperceptible, many times smaller than the finest of the tapestry’s threads: an invisible bacterium called Yersinia pestis. Humanity would not catch its first glimpse of bacteria until three centuries later. In the mid-1670s, the Dutch draper Antoni van Leeuwenhoek in Delft probably became the first person ever to behold a bacterial cell. Using tiny beads of glass that he held up to the sunlight pouring into his room, Leeuwenhoek was able to penetrate to a layer of reality that was hidden beneath the everyday. He looked at so many things through his glass-bead microscopes, described in hundreds of letters to the Royal Society in London, that it would almost be easier to list what he didn’t look at. A brief list gives some idea of his vivid and madcap itinerary of the seventeenth-century Dutch world: from wine to frogspawn, tulips to snails. But his most spectacular discovery was that the world was swarming with previously invisible life.
Leeuwenhoek’s microscopes conjured living things out of everyday substances, including the plaque he scraped from his own teeth. The beasts he saw there were tiny, but they moved ‘very extravagantly’. Different types swam in characteristic patterns: straight lines, loops, corkscrews. (His observations were so accurate that it is possible today to be confident which bacteria he was describing.) These ‘little animals’ were indisputably alive. Using the mathematics he had learned during previous training as a surveyor, Leeuwenhoek made a simple calculation that there had to be more of these little animals in his own mouth than ‘the number of Men in a kingdom’. It may seem strange to a modern view where bacteria are synonymous with disease, but in all Leeuwenhoek’s voluminous writings there is no indication that he ever construed the little animals as a threat. If they were apparently everywhere, then how could they possibly cause disease?
For years after Leeuwenhoek, bacteria were seen as benign curios – if they were seen at all. Even in the eighteenth century,
the Swedish scientist Carl Linnaeus almost completely ignored bacteria in his system of taxonomy for dividing up the animal and plant kingdoms. Linnaeus’s system was meant to bring about order from chaos, but the few bacteria he was grudgingly aware of threatened his scheme. To accommodate their peculiarity meant creating a genus (a taxonomic division above the level of species) literally called Chaos. The nineteenth-century zoologist Ernst Haeckel followed Linnaeus in keeping bacteria to a dark taxonomic corner: they were part of the ‘formless worms’. Bacteria fell in between the cracks of the two great taxonomic systems of zoology and botany. To some they were closer to animals; to others they were more like plants. Either way, it hardly seemed to matter much.
Into the nineteenth century, most naturalists who looked at bacteria were similarly uninterested. Through the best microscopes, bacterial cells were still only small blobs, as simple as life could get. Even as new ideas about evolution surged through biology like alcohol, illicit and intoxicating, bacteria presented something of a problem. Evolution seemed to mean an increasing complexity of life. But in that case, why were such simple forms of life still around?
The French biologist Jean-Baptiste Lamarck thought that evolution was driven by an inevitable tendency towards perfection. Living organisms were climbing a ladder, forever ascending. Bacteria were an ugly blot on this noble idea. Lamarck felt compelled to assert that they must continually arise from nothing by spontaneous generation, spilling out of dirt and putrefaction. How else could one explain the way they clung stubbornly to life’s very lowest rung?
Some were less certain. Charles Darwin studied microorganisms like amoebae, and concluded that ‘every naturalist who has dissected some of the beings now ranked as very low in the scale, must have been struck with their really wondrous and beautiful organisation’. His point was that initial appearances could be deceptive unless you had the means to look closely. At the time, no microscope could penetrate within the smaller bacterial cell, but experience suggested there was no limit to the microscopic intricacies that evolution had produced. As it would turn out, Lamarck’s view that bacteria could
not be evolving because they had not turned into animals was a misunderstanding. Bacteria were still bacteria not because they had only recently emerged from nothing, but because they were already exquisitely evolved.
The deep past is dark and shadowy, but it seems likely that for at least 1.5 billion years after life on Earth emerged, the world belonged to bacteria. There was no organism beyond the cell itself: no plants, no animals, no bodies of any sort. Yet life was far from boring. The world that once stood barren and empty was soon crowded, as cells found their way into every crevice they could.
As soon as there was life, there was evolution. All life is based on genetic material stored in molecules of nucleic acids: DNA and its more flexible cousin RNA . In DNA, the script is written in four possible chemicals – by convention denoted A, T, C and G. The pattern of these ‘letters’ encodes an organism’s genome, protected from degradation and decay inside the secure wrapping of the DNA double helix. But every time a cell divides, the double helix must be copied: it is separated into its two strands, then each strand gains a new partner. The two strands of the helix thus become four, one double helix becomes two, and the cell divides.
Every genome in existence has sailed through millions of generations to arrive where it is now, a ship of Theseus with each part copied and replaced countless times. There is no more convincing evidence of the common heritage of all life than the conservation of the basic molecules that carry out these processes. Right now, enzymes are at work within your cells that share stretches of sequence identical to a similar enzyme in Escherichia coli, a bacterium that lives within the human gut. Such molecular motifs are rhyming couplets across the great poem of life. Whereas at other points evolution may extemporise, conjure great loops of digression or hit on a new turn of phrase that exceeds the original, there are some passages that cannot be changed.
Just as an organism’s genome passes on its accumulated wisdom to its descendants, so human societies have sought to safeguard
their knowledge against the ravages of time. The outcome of just one of these endeavours shows the impossibility of that task. In the thirteenth century, the Goryeo dynasty of Korea commenced a grand undertaking. The three canonical collections of the Buddhist canon, known as the Tripit . aka, would be engraved onto white birch, wood so dense that it sinks, to be preserved for posterity. Logs of birch were soaked in seawater for three years and then cut into thousands of blocks, each one the weight of a newborn baby, which were then boiled in salt and left to dry outside for a further three years. Only then were their surfaces ready for carving. For over a decade, craftsmen carved more than 52 million characters into the blocks, reciting a prayer after each character was finished. Today, the Tripit . aka Koreana is stored in the Temple of Haeinsa, stacked up on shelves beneath elegantly curving roofs, nestled in the green foothills of Mount Gayasan. The low wooden buildings, protected by full-time security guards and a fire truck stationed within the grounds of the temple, house 80,000 individual blocks, each one a pure repository of perfect knowledge.
At least, that was the intention. Modern scholars have found that the Tripitaka Koreana, for all its breathtaking beauty, contains hundreds of mistakes that presumably arose from the everyday chaos of life – a smudge of ink, a misreading, or the slip of a craftsman’s knife.
A bacterial cell has much the same problem. Its genome must be copied every time it divides, which in its most vibrant growth phase may be as often as every twenty minutes. Escherichia coli has over 4 million characters of DNA in its genome. A long-term experiment established that, on average, in 1,000 generations of copying and recopying between cells, its genome had accumulated less than a single difference. Every twenty minutes, a tiny bacterial cell in your gut succeeds in doing what the Goryeo dynasty could not. But still, the transmission of information is not perfect. A mutation is an event where the letters of DNA change randomly. In terms of fidelity to the past, any mutation is an error, yet the unexpected beauty is that sometimes, by chance, it presents an improvement. It is this fundamental tension between order and disorder that is essential to all life.
The first life consisted of single cells. Yet it was impossible for these cells to be sealed units. Life is a process: without an ebb and flow of chemicals across a cell’s outer boundary, it would die. As chemicals flowed, the first bacteria began to evolve new networks for biochemical reactions, reaching new areas of molecular possibility. As these new molecules proliferated, the unwanted output of one cell could be the input of another. Simple pass-the-parcel exchanges between cells flourished into byzantine arrangements of interdependence and competition. As the microbes multiplied and diversified, they constructed a complex web of alliances and rivalries, like a sprawling medieval war. As bacteria banded together or floated free, they differentiated into separate species, each adapted to a different set of molecules and environments. The concept of a biological species as developed by Darwin and others had been one of reproductive isolation: each species was a delicate and separate branch on the great tree of life. But that concept does not apply to bacteria. The implications are mind-bending. ‘The entire bacterial world’, writes the doctor and scientist Stuart Levy, ‘can be thought of as one huge multicellular organism.’ From life’s earliest moments, genes were being carried by viruses and other rogue genetic elements between cells, shuttling back and forth as if on a molecular loom.
Within this chaos, bacterial species could still form, but they had to carve out a space for themselves. Given this, the evolution of chemical weapons was inevitable. Bacteria made molecules that poisoned their enemies and spared their allies. Such molecules were the first antibiotics. Soon, evolution produced in turn molecules that could defend against antibiotics. These developments were less sequential than this description implies; they must have unfolded in chaotic parallel. Resistant bacteria evolved and prospered wherever antibiotics did. The two were locked in an ecological balance: a rise in antibiotic production by one bacterium would drive a rise in resistance in another. Antibiotics and antibiotic resistance swirled around each other like yin and yang.
However, this single-celled world did not last. Around a billion
years ago, before most of the stars visible in our night sky had started shining, something strange happened. The cell which had served bacteria so well underwent a sudden change, creating a new form of life: the eukaryotes (yoo-KA-ree-ohts ). Most biologists believe that the origin of eukaryotes was spectacularly improbable – perhaps a once-in-Earth’s-lifetime event, with a fusion of two very different types of single-celled organism: archaea and bacteria. Explaining exactly how that happened remains a mystery – the biologist Nick Lane has called it ‘a black hole at the heart of biology’ – but somehow, it did. The new eukaryotes were fundamentally different from their ancestors. Their name comes from the Greek for ‘well-formed nucleus’, denoting their altered cellular structure. The genome no longer floated free in the cell but was bundled in a dense knot – a nucleus – like the yolk within an egg. The evolution of the eukaryotes marked an important milestone in evolution. Their cells were a complex fusion, and complexity began to develop at a level beyond the cell too. For reasons that are still debated by scientists, eukaryotic cells did something no bacterium had ever done and flourished into multicellular life, creating the first bodies. An organism was now no longer limited to a single cell but became an extended piece of real estate. A single being could contain multitudes.
The existence of multicellular organisms did not spell the end for bacteria; it presented an opportunity. The first bodies were rich concentrations of nutrients, sequestered into one space and guarded against the hungry microbial world with barriers of shell, skin or mucus. When a multicellular organism died, that imbalance was repaid. As the body decayed and broke down, microbes would flood in, reconfiguring the molecules of the body into new bacteria. Out of the raw materials death provides, bacteria could decompose a new symphony of life.
But bacteria didn’t need to wait for death. Like a cell, a multicellular body itself needed to be permeable, making it impossible to keep them out entirely. One of the first challenges for multicellular organisms was keeping that hungry world at bay. Organisms allowed some of the bacteria in, forming ecological systems within
early animals: the first microbiomes. Nascent immune systems evolved to control and even select these resident bacteria. Such bacteria could provide a multicellular organism with benefits, including that simply by occupying space they prevented more harmful bacteria from gaining a foothold. As eukaryotes continued to evolve, the bacterial species that gave up their freedom to live inside these increasingly complex bodies were a minority. But they were a concentrated minority. The mammalian gut created perhaps the richest assemblage of bacterial diversity in life’s history, where hundreds of different species coexisted in close proximity.
Bodies came with other challenges. One organism could now contain many different types of cell, the same genome growing into an unruly menagerie that somehow pulled together in the same direction. Your body contains about 200 different types of human cell. From the tiny saucers of your red blood cells to the metre-long neurons that stretch along your spine, you are a teetering assemblage of difference bound together by natural selection. The same genome gave rise to all of these cell types, and each is regulated and balanced against the others in a tight social contract. Your body collectively maintains homeostasis, balancing conditions and resources to ensure continued survival of the total assemblage. A healthy cell obeys its orders and divides in a regulated way, even killing itself on demand if it receives the signal. But that social contract can sometimes break down. In cancer, a mutant cell just keeps doubling as if it has gone mad and forgotten its responsibilities: one, two, four, eight, sixteen . . . In twenty doublings there will be more than a million cells. Left unchecked, this rogue quest for infinite growth wreaks havoc on a finite body. Siddhartha Mukherjee has called cancer ‘a pathological mirror’ of our own existence. Its cellular atavism of uncontrolled growth is a return to an ancient state of life, the purest evolutionary expression of selfishness.
Bacteria cannot get cancer: they already have it. As single-celled organisms, they have not evolved to coordinate a complexity of cell types. While the good news is that no bacterium wishes you harm, the bad news is it may kill you anyway if its mindless passion for
growth overwhelms your body’s normal functions. To take one example, consider the rare bacterial condition known as infective endocarditis. As Leeuwenhoek observed in the seventeenth century, the human mouth contains many different bacteria growing on the gums and teeth. Normally, these bacteria pose no serious threat, as long as they are regularly removed by the brushing of teeth. But if these bacteria are given access to the bloodstream – say, through the removal of an abscessed tooth by a dentist – they can move elsewhere within the body. In rare cases, certain species can be pumped around the bloodstream and back to the heart where, if they are lucky enough to cling to the surface of a heart valve, they can grow and grow, forming a clump of infection analogous to a tumour. The heart is compromised: perforation or rupture is possible. Chunks of the infection may detach and float further through the bloodstream, causing chaos wherever they lodge in the body. As in cancer, in a body of many cell types the unchecked growth of just one can wreak havoc. Worse, some bacterial species manufacture their own toxic poisons to assist with their conquest, and have evolved to spread not just within but between human bodies. Bacterial infection is a form of single-celled revenge against the complexity of multicellular life.
The fact that bacteria can cause disease is so ingrained in us now that it is difficult to appreciate how ludicrous the idea of germs was when it first emerged. In the nineteenth century, cholera began to spread throughout the world, causing devastating outbreaks. Sufferers found themselves racked by severe diarrhoea and vomiting – the word ‘cholera’ may have arisen from a Greek word meaning ‘gutter’. Doctors were agreed that cholera was infectious. As the British doctor John Snow wrote, ‘It travels along the great tracks of human intercourse, never going faster than people travel’. Where they disagreed was the cause. Many continued to follow Galen and blamed bad air, but Snow thought otherwise. In 1854, he studied a cholera outbreak in the Soho neighbourhood of London, the worst that he had ever seen. Drawing up a map of cases and enquiring locally, Snow homed in on a single culprit: the water pump on Broad Street.
But when he first examined the water for contamination, he could see almost nothing. ‘I found so little impurity in it of an organic nature,’ he wrote, ‘that I hesitated to come to a conclusion’. He was certain that the water was to blame, but he couldn’t explain why.
Leeuwenhoek had seen little animals in water almost two centuries before. But how could little animals be responsible for disease if they were present almost everywhere – and in perplexing diversity? As the French philosopher of science Bruno Latour put it, falling sick from some invisible corruption was ‘all the more disturbing’ because it did not always happen. The enemy’s lair had been identified, but the enemy’s true identity remained as murky as the clouded water.
The only way that most people could see bacteria was in the spoiling of food and drink, and such a general form of corruption could not be attributed to a single species. It was only when scientists began to catalogue and enumerate bacterial diversity that they realised not all bacteria were alike. At first, mimicking the decay of food, bacteriologists tried to grow individual species on solids like meat, potatoes, eggs or bread. But the growth was erratic and too many different types grew together. The trick was to appreciate that bacteria prefer their food easily digestible – a soup of raw inputs – and to use liquid broth. Scientists became providers of bacterial haute cuisine : ‘One obtains a culture medium by leaving for twenty-four hours, in contact with twice its weight in water, finely chopped lean veal.’ The aim was to grow up pure populations of single species in order to study them in isolation.
To isolate a single bacterial species was an extraordinary achievement – a purity never seen in nature. Scientists began with broth sterilised by heat, as devoid of life as it was full of nutrients. They then impregnated the broth with the smallest amount of matter imaginable: a single bacterial cell. The French scientist Louis Pasteur praised the virtues of using a needle-thin glass rod as a means of transfer, so sharp its point was barely visible. Once in the broth, the cell would divide again and again, until the flask that had once been lifeless was teeming with unseen millions.
As further epidemics of cholera had raged through cities in the 1880s, it was in Kolkata in India that the German bacteriologist Robert Koch identified a comma-shaped bacterium as the real culprit: Vibrio cholerae. Like many bacteria, it could float unseen in water, but it alone was responsible for the devastating illness. If swallowed, it could multiply in the sufferer’s gut before exiting in their diarrhoea, contaminating more water and infecting fresh hosts. One doctor who didn’t believe Koch’s claim was Max Pettenkofer. Pettenkofer had founded Munich’s Institute of Hygiene and redesigned the city’s sewers to address previous epidemics, but he disagreed that bacteria were the only important factor. To prove it he wrote to Koch and requested a pure liquid culture of Vibrio cholerae ; when it arrived he drank it down. Fortunately, Pettenkofer survived. It’s thought that Koch was aware of his plans and deliberately sent him a weak concoction, preferring to lose the argument than be accused of murder.
There is a strange intimacy between enemies. As work from Koch, Pasteur and other microbiologists became more widely accepted, the ‘germ theory’ became the dominant explanation for infectious disease. Bacteria had been transformed from Lamarck’s hapless blobs to demons under the microscope. The task of bacteriology was to examine them in the laboratory and work out how to defeat them. But though isolating single species was a spectacular feat, to the naked eye bacteria could still manifest only as cloudy liquids. Though contaminated broth was fertile with bacteria, in a visual sense it was barren – a medium of monotony. It was Koch who gave a vivid demonstration that turned the world of bacterial culture three-dimensional. Once again, it involved borrowing from cookery. He mixed broth with animal gelatine, the same substance used to make jellied desserts. Koch’s jellies were translucent reds and browns brewed from blood or beef. The resulting patch of jelly contained the nutrients the bacteria needed to grow on a flat surface. What Koch called a ‘moist chamber’ would come to be known, after refinement by his assistant Julius Petri, as the Petri dish. When Koch demonstrated the technique in London at an
international conference in 1881, people were astonished. Here one could see bacteria, plain as day. In one demonstration, an empty dish was left with its lid off outside in the London air for four hours. Koch then brought it back inside to show to spectators. Forty or fifty different spots had formed of varying colours, each corresponding to the slowly spreading circle of a single cell that had landed there by chance. As one spectator put it, it proved that the air itself contained species with different characteristics – what had been invisible now flourished ‘visible to the naked eye’.
The gelatine on the plate was later replaced by another substance using a suggestion from Fanny Hesse. Hesse, known as Lina by her family, was married to Walther, a microbiologist who worked with Koch. She herself worked with Walther as a microbiologist and suggested an alternative to gelatine. Hesse had grown up in New York, where from Dutch neighbours who had emigrated from Java she had learned of agar, a substance made from seaweed extract. Agar, a clear jelly with almost no taste, could be used as an alternative to gelatine in cookery to make set puddings. It proved to be even better than gelatine for bacterial cultures and remains at the heart of almost all bacterial research.
Koch and his colleagues had found a middle way between the figurative but intangible world of the microscopic cell, and the tangible but abstract world of broth. Just a few years earlier, Claude Monet and his fellow Impressionists had shocked art critics by giving them only an ‘impression’ of a scene, rather than attempting to reproduce it. Similarly, bacteria could now be understood through the ‘impressions’ they left behind in the lab. A single species could be painted onto a blank canvas for closer study, its opacity, pigmentation and texture on the dish becoming part of its identity. A language of streaks, circles and discs became part of the visual lexicon of science. Once bacteria became visible, they could not be unseen.
Cholera was not a fluke. As bacteriology grew as a discipline, one by one some of the world’s deadliest infectious diseases were unmasked as having a bacterial cause. Unfortunately, this knowledge
didn’t seem to translate into effective medicine. There were public health improvements, but these were mostly thanks to better sanitation and living conditions of the sort advocated by Koch’s intellectual adversary Pettenkofer, as well as better nutrition. In Britain in 1800, 329 in 1,000 children died before the age of five. By 1900 the figure was down to 228, and by 1930 it would more than halve again. As Latour put it, bacteriology was ‘far from being the source and cause of hygiene’ – it was ‘merely a ripple on the surface’. Prevention, not cure, was the way to save lives.
The few available treatments for bacterial disease used other bacteria. Once bacteriologists could isolate single species, they had been able to combine them, trying to build back from the purity of a single species to the messiness of the real world. Applying Darwinian ideas about evolution to microbes, bacteriologists had become intrigued by competition between different species of bacteria. Could these antagonisms be exploited for human benefit? In the late nineteenth century, scientists had discovered that the bacterium known as Pseudomonas aeruginosa could kill pathogenic bacteria. Unfortunately, it was itself a deadly pathogen, associated with a characteristic blue pus that oozed from infections. This dirty contaminated broth was hardly a reliable medicine. Eventually, a single molecule called pyocyanase was isolated from the blue broth, but its use was limited to eye-drops, spray or mouthwash because swallowing it was toxic.
Another approach used animals, not bacteria, to make medicine. Scientists had found that bacteria often released toxins that killed human cells. In 1890, the Prussian scientist Emil Behring and the Japanese bacteriologist Kitasato Shibasaburō discovered that injecting horses, guinea-pigs and goats with toxic bacteria allowed ‘antitoxin’ to be obtained from their blood serum. The antitoxin was a chemical that bound to the bacterial toxin and so, if injected into other animals, reduced the severity of the disease, known as diphtheria. Here was medicine manufactured by an animal’s own immune system. Applying the same principle to cholera also yielded a similar treatment. Two important bacterial diseases now
had treatments, even if they only diminished the virulence of the disease by mopping up toxin rather than directly attacking the bacteria. To manufacture diphtheria antitoxin, the most efficient method was injecting horses with bacteria, then extracting their blood and giving it to children. Such was the need that public health departments in America acquired their own stables. At one stables in New York, a seven-year-old bay gelding was bled nine times in a year, producing twenty-two bottles of serum.
Antitoxin serum and blue broth were attempts to bottle living elixirs. They worked, but they were messy magic. Would humanity need a different stable for every disease?
At the start of the twentieth century, some felt that searching for medicines in biology was misguided. Instead, they perceived a gleam of hope in a different scientific realm. Rather than trusting in living organisms, these scientists saw in the lifeless mysteries of chemistry a new and toxic possibility. In their test tubes they aimed to brew poisons of unprecedented power.