A Recognized World Center for Advancing Health Care through Science, Education & Technology

A Recognized World Center for Advancing Health Care through Science, Education & Technology

Plus... The Space Between Appointments: Learning from a Patient-Professional’s Journey; Clinical Insights from the Other Side of Care
“Everyone has the power to transform their life and overcome the challenges of obesity. At Roxborough Memorial Hospital, we’re here to support your journey toward better health and a brighter future.” — Dr. Piotr Krecioch, General and Bariatric Surgeon

Bariatric Surgery and Wellness Program



A trained professional facilitates an in-person session in your patient’s home. We get to know the person while gauging their cognitive, physical and emotional abilities. Directly following the session, we offer our recommendations to the older driver followed with a detailed report of our findings and recommendations.
The cost is just $450
Ask about our Senior Living Placement Solutions where we work with the family to find appropriate senior living arrangements.
Philadelphia County Medical Society
2100 Spring Garden Street, Philadelphia, PA 19130 (215) 563-5343
www.philamedsoc.org
EXECUTIVE COMMITTEE
Walter Tsou, MD, MPH President
David A. Sass, MD, FACP President Elect
John M. Vasudevan, MD Past President
Brian A. Hannah, MD, MSc Secretary
Sharon Griswold, MD Treasurer
Victoria Cimino, MD, MPH
Cadence A. Kim, MD, FACS
William King, MD
Pratistha Koirala, MD
Dale Mandel, MD
Elana McDonald, MD
Max E. Mercado, MD, FACS
Gillian Naro, MD
Natalia Ortiz, MD, DFAPA, FACLP
Dhruvan Patel, MD
FIRST DISTRICT TRUSTEE
Michael A. DellaVecchia, MD, PhD
EXECUTIVE DIRECTOR
T.J. Huckleberry www.philamedsoc.org
Editor Kevin Bezler

The Space Between Appointments: Learning from a PatientProfessional’s Journey; Clinical Insights from the Other Side of Care
Physicians Set Health Policy Agenda at Annual House of Delegates




the Summer 2025 issue of Philadelphia Medicine, the author of the article “250th Anniversary of the US and the History of Medicine” was incorrectly credentialed. The author is Sebastiano Porcu, MD. We regret the error.

Walter H. Tsou, MD, MPH President Philadelphia County Medical Society

By reopening the federal government without extending the premium tax credits for the Affordable Care Act, the average Marketplace premiums will increase by 114% according to the Kaiser Family Foundation. And to add insult to injury, if you received the tax subsidy in 2024, but now have a job and earn more than 400% of poverty, you will have to repay the government part of your tax credit when you file your taxes in 2025. And it gets worse, because in 2026, you will be asked to repay any excess tax credits including possibly all tax credits which could be thousands of dollars that you must pay in taxes. And if you thought being below the 150% of poverty will be low income enough to qualify for special enrollment, think again. Beginning this past August, being poor is not enough of a reason to enroll in the ACA Marketplace outside of the open enrollment period which ends January 15, 2026.
Who are the ones who get ACA Marketplace insurance? They are your self-employed, gig or shift workers whose incomes are highly variable and could easily get trapped into extraordinary tax bills. To help these workers (who could be priced out of the market), the new law can offer “catastrophic health plans” with annual deductibles of a mere $21,200 for a family plan in 2026. Pretty outrageous.
The new law has special rules for lawfully present immigrants making them ineligible for either Medicaid or the ACA Marketplace, ensuring that they remain uninsured. Even DACA recipients who were children brought here under age 18 and have only known America are ineligible for the Marketplace. Undocumented immigrants have never been eligible for these programs.
Confused yet? In the past, CMS funded patient navigators to help figure out how to get insurance, but CMS this year cut the navigator program by 90%. Pennsylvania runs its own ACA Marketplace called Pennie, but it is unclear if the navigator program will be impacted.
An estimated 20 million Americans will see a rise in the health insurance premiums. Already, Pennie is seeing 2 disenrollments for every enrollment and it is estimated 250,000 Pennie enrollees will disenroll because of the premium increases.
When the private insurers lose that many customers, they will raise premiums for everyone else. And they will put the squeeze on their most expensive claims, namely, hospitals, and doctors. Think prior authorizations and narrow networks on steroids.
Many have stated repeatedly that our health care system is broken, but it has been precariously balanced between private and public insurance. We are witnessing the affordability “death spiral” playing out in front of us. As more lose their insurance, doctors and hospitals will raise their prices which will force the remaining insurers to raise their premiums which will make insurance even more unaffordable. And so on.
The GOP promised a vote on the ACA tax subsidies before January, but they are under pressure to come up with their own plan. Trump despises “Obamacare” and rather than extend the tax subsidies has proposed giving the money to Americans through a “health savings account” rather than to insurers. Of course, depriving the insurers of tens of millions in subsidies will almost ensure the acceleration of their demise (not that we are crying). But it

Scott Nash, AWMA™ Senior Vice President Wealth Management Advisor
856.231.5575
snash3@ml.com
Merrill Lynch Wealth Management
1200 Howard Boulevard Suite 300
Mount Laurel, NJ 08054
advisor.ml.com/sites/nj/mount-laurel-nj/nash-wealth-management-group
Merrill Lynch, Pierce, Fenner & Smith Incorporated (MLPF&S) is a registered broker-dealer, registered investment adviser, and Member SIPC. MLPF&S is a wholly owned subsidiary of Bank of America Corporation. The Bull Symbol and Merrill are registered trademarks of Bank of America Corporation. The College for Financial Planning Institutes Corp. owns the service marks Accredited Wealth Management Advisor℠, AWMA™, and the AWMA™ logo, and the certification marks Accredited Wealth Management Advisor™, AWMA™, and the AWMA™ logo. © 2025 Bank of America Corporation. All rights reserved.

also means that the federal government is wiping their hands of any responsibility for your care. Here’s some cash. Use it for health care and good luck on your own. Anyone see a potential problem here?
It is hard to know what to recommend to the medical profession. We will be squeezed even further to keep insurers profitable. And our patients will be faced
with untenable choices of trying to figure out how to get health care for their families with no or limited insurance and huge deductibles. Stay tuned for my next essay.

Walter Tsou, MD, MPH President, PCMS

T.J. Huckleberry Executive Director Philadelphia County Medical Society

The last time I openly cried was 20 years ago on the westbound shoulder of I-76 about a quarter mile away from the Spring Garden exit. As I was sobbing, my fiancé (now wife) was in the passenger seat. All my belongings were in the back of my truck, and my University of Drexel diploma was on the floor. While I was excited to start my new life and was extremely proud to be a newly crowned Drexel Alumni, I was devastated that I was leaving my beloved city of Philadelphia.
My career took me back to Berks County where I spent my first 10 years of employment as an aide in the Pennsylvania State Senate. Later I took the job as Executive Director of the Berks County Medical Society (BCMS) where my passion for organized medicine flourished. And while I loved my physicians, my job and the partnerships I made…it was never Philly.
So, when opportunity presented itself at the PHILADELPHIA County Medical Society (PCMS), I jumped at the offer. I was back, baby!!! Moreover, I was able to continue to do the job I love, in the city I love.
Seriously, I am so darn happy I might be the only one smiling ear to ear while parked on the Conshohocken Curve!
Before I share with you some of my initial goals for PCMS, I want to once again thank my predecessor, Mark Austerberry. Mark has been a friend and mentor to me since I started in Berks. Moreover, he has built and maintained one of the best run and healthy county medical societies in the nation. I am excited to build on what he established and thankful for his leadership, especially through the COVID crisis and the Hahnemann closure.
My first point of business is to address the membership gap created by the pandemic. Unfortunately, due to COVID, we had our “farm team” of early career physicians, residents, and medical students drastically depleted. Rebuilding our relationships with these important future leaders and their faculty is our goal number one for 2026.

PentaHealth is an independent, physician-led group of dedicated providers located throughout Southeastern Pennsylvania who proactively deliver seamless, high quality, and accessible care to all, one person at a time. Call 610-423-8181 or visit www.pentahealth.com

















































Secondly, in the same vein, we need to define the values and goals of the next generation of physicians and incorporate them into our medical society. We need to incorporate programs and events that are tailored to their lifestyles. We plan to address that need via programs like our new Revelry Club and our very successful Doctors Lounge events, where our members can socialize or discuss important issues in smaller, more intimate venues.
Our final 2026 goal is to improve member engagement. Enhancing our social media engagement, broadening the scope of this magazine through innovative podcast discussions, and improving our digital newsletter will ensure that our members receive timely and comprehensive information.
To conclude, I want to use a quote with which I ended many of my Berks County Medical Record articles. I feel it is a perfect summation of my expectations for my new role as your executive director: “Far and away, the best prize that life has to offer is a
L to R: Dr. Bradley, Dr. DeMario, Dr. Holgado, Dr. Kalman, Dr. Khalifa, Stacey Yantis (CRNP), Dr. Belfiglio, Dr. McAuley, Dr. McGuire, Elizabeth Facciolo (CRNP), Sarah Smith (CRNP), Dr. Kummer, Dr. Leath, Dr. Lewis, Dr. Oodal, Carrie Karhnak-Glasby (CRNP), Suzannah Maynard (CRNP), Dr. Atlas, Dr. Ausaf, Dr. Baig, Dr. Chin, Dr. Pagano, Dr. Sunoo, Diana Wadlund (CRNP), Dr. Kohli, Dr. Kumanova, Dr. Nikas, Dr. Rowan, Dr. Uhler, Dr. Vadher, Erin Lender (CRNP), Denise Meli (CRNP), Dr. Boucher, Dr. Catania, Dr. Hornick, Dr. Sissy John, Dr. Sony John, Dr. Wood, Dr. Wu, Peyton Holowsko (CRNP), Anita Snyder (CRNP), Sue Villarini (CRNP), Dr. Bamezai, Dr. Bonnes, Dr. Brosius, Dr. DiCicco, Dr. Gallagher, Dr. Peri, Dr. Schleusner, Dr. Schurtz, Dr. Yeh, Laurie Taylor (CRNP)
chance to work hard at work worth doing.” ~President Theodore Roosevelt
I look forward to working hard for all of you at work worth doing.
Go Birds.

T.J. Huckleberry, Executive Director Philadelphia County Medical Society


By Marilyn Howarth, MD, and Adrian Wood, MPH, Perelman School of Medicine, University of Pennsylvania; Reema Persad-Clem, PhD, MS, MPH, Department of Public Health, Arcadia University; Jerald Fagliano, PhD, MPH, Dornsife School of Public Health, Drexel University; Harriet Okatch, PhD, MPH, College of Population Health, Thomas Jefferson University; Inkyu Han, PhD, MPH, and Aimee Palumbo, PhD, MPH, College of Public Health, Temple University; Hilliary Nelson, PhD, MPH, Master of Public Health Program, University of Pennsylvania; and Robert Sharrar, MD, The College of Physicians of Philadelphia
Throughout its 238-year history, The College of Physicians of Philadelphia has brought together medical and public health professionals across the region to address important health issues impacting the public. Understanding and addressing the health impacts of climate change is the latest focus of their attention. Specifically, the Section on Public Health and Preventive Medicine, chaired by Dr. Robert Sharrar, has been consistently working on educational and convening efforts on climate change health impact.
A grand rounds in February of 2020, “Climate Change and the Air We Breathe,” was followed by a grand rounds in February of 2022, “Addressing Climate Change with Innovation.” Throughout this time there were discussions about why physicians and public health professionals were not at the forefront of action.
In October of 2023, the Section brought in Dr. Ann-Christine Duhaime, author of Minding the Climate: How Neuroscience Can Solve Our Environmental Crisis, for a public discussion of her book and an exploration of its themes about the motivators and barriers to climate action based in brain physiology. In the Public Health Section, questions were raised, such as, “Are public health professionals currently being adequately trained on climate change preparedness, effect mitigation and adaptation strategies and if not, is this a barrier to action in Philadelphia?” and “What climate change and health content are students in masters of public health (MPH) currently receiving?”
The Section determined that it was important for every MPH student graduating from an MPH program in our region to have the requisite knowledge and skills on climate change and
health to take positive action on behalf of the public. Over the last two years, the Environmental Health Committee, chaired by Dr. Marilyn Howarth from the Perelman School of Medicine, has convened MPH program leaders (hereafter referred to as the MPH Committee) to answer these questions and design a plan to achieve this goal.
The MPH Committee first convened key representatives from all the master’s level public health programs in the region: Arcadia University, Drexel University, La Salle University, Temple University, The University of Pennsylvania, Thomas Jefferson University and West Chester University. An informal survey asking what climate change and health learnings were currently incorporated into required courses versus elective courses was undertaken. This preliminary survey confirmed that the climate change and health learnings that are an existing part of required courses are generally limited to one to three lectures. Some programs offered electives with robust content on climate change as the focus, but a minority of public health students took those courses and there was limited focus on constructive action that public health professionals could take to engage the public, government or other policy makers.
Recognizing the need for a benchmark by which to evaluate current curriculum offerings, the Committee engaged Cecelia Sorensen, MD, Director of the Global Consortium on Climate and Health Education of Columbia University’s Mailman School of Public Health. She and her colleague, Haley Campbell, MPH, the Project Director for the Consortium, met with the MPH Committee and described how their Global Consortium on
Equipping the Region’s Public Health Workforce with Climate Change and Health Tools continued from page 9
Climate and Health Education Core Competencies (GCCHE) was developed and provided examples of how those competencies have been applied. The MPH Committee, having reviewed their programs’ course offerings before this meeting, recognized areas for potential improvement in their own curricula after the presentation and conducted a formal evaluation of their programs’ course content through the lens of the GCCHE core competencies.
The process of curriculum examination was lengthy and difficult but clearly identified the areas of strengths and weaknesses of each program. Of note, the strengths and weaknesses were not consistent among programs, suggesting varying expertise and emphasis of faculty in different institutions as well as opportunities to fill educational gaps through improved collaboration with local talent. To adequately address some gaps
WEBINAR TOPIC AREAS
Extreme Weather and Flooding in Philadelphia
Vulnerabilities of Working Populations to the Risks of Climate Change
Engaging Communities in Preparedness: Weathering Extreme Events in Our Changing Climate
Extreme Heat, Air Quality, and Adaptation Strategies
Climate Change and One’s Health
in competencies, experts outside of traditional health and public health faculty would be required.
After much discussion about strategies to achieve the aim of more consistent and robust education on climate change and health for all public health students, it became clear that the best approach was a flexible design model that allowed each program to incorporate the learnings consistent with their needs and course structure. The MPH Committee determined that a recorded webinar series where each webinar could stand alone and address a topic gap for a program would provide for the greatest flexibility. Additional webinars could be added and original ones updated as needed. Collaboratively, the MPH Committee identified six topic areas for the initial set of webinars:

Sustainability in Philadelphia
WEBINAR ORGANIZER
Marilyn Howarth, MD Perelman School of Medicine, University of Pennsylvania
Jerald Fagliano, PhD, MPH Dornsife School of Public Health, Drexel University
Reema Persad-Clem, PhD, MS, MPH Department of Public Health, Arcadia University
Inkyu Han, PhD, MPH College of Public Health, Temple University
Hilliary Nelson, PhD, MPH Master of Public Health Program, University of Pennsylvania
Harriet Okatch, PhD, MPH College of Population Health, Thomas Jefferson University

At MADJ, we specialize in helping medical practices and health systems of all sizes thrive in competitive landscapes. From small beginnings to significant success, our tailored strategies have transformed healthcare providers into community cornerstones.
CASE STUDY HIGHLIGHTS:
59,000+ Annual Website Visits Enhanced Reputation 3x Growth in Practice Size
The MPH Committee set the expectation that the content and associated readings, activities and assignments would be geared for master’s level students. The webinars would be publicly available for educational purposes at other levels or by other interested parties. Members of the MPH Committee volunteered to be the webinar organizers and set out looking for content-matter-experts to build their webinars.
The webinars include members of the public providing their personal experience with climate change and health impacts; government officials discussing their role in preparedness and mitigation; and faculty from regional institutions with expertise outside of traditional public health domains. The College of Physicians of Philadelphia and the webinar organizers worked with Adrian Wood at the Perelman School of Medicine at the University of Pennsylvania to edit and produce the webinars.
Going forward, the MPH Committee plans to develop strategies to incorporate the webinars into their curricula. Recognizing that the MPH program accrediting agency, The Council on Education for Public Health, has its own set of competencies to be achieved through the climate change and health lens, the MPH Committee hopes to work with faculty throughout their MPH programs to incorporate climate change
perspectives into required courses such as epidemiology and biostatistics. In some cases, one or two webinars will be added to required course work to close gaps in learning. In other cases, the entire webinar series may be used as a framework to achieve MPH core competencies in communication, policy development and engagement with key stakeholders.
On November 19, 2025, The College of Physicians of Philadelphia held a grand rounds, “Climate Change and Public Health: Practice, Policy, and Education,” to describe the webinar series and showcase some of the content. The webinar series “Climate Change and Health in Philadelphia” is available through the College of Physicians of Philadelphia, Section of Public Health and Preventive Medicine’s website. While visiting the website please consider joining the Section to learn of and to work on important collaborative projects in Public Health in the region.

Reference:
& GCCHE Core Competencies, “Climate Change and Health:
Public Health Education Toolkit,” 2022.
By Hans Kersten, MD
Dr. Kersten (AΩA, Drexel University College of Medicine, 2013, Faculty) is Medical Director, Grow Clinic, St. Christopher’s Hospital for Children; and, Professor, Department of Pediatrics, Drexel University College of Medicine, Philadelphia, PA.
The other side of 50 is upon me and it can be a challenge to stay in shape. It is dark when the alarm goes off at five a.m., but I perk up after I brush my teeth, walk the dog, and head to the gym. I hear a, “Yo, what’s up?” and the familiar sound of a bouncing basketball when I arrive. Soon thereafter, teams are picked and the game starts.
There is a camaraderie among the guys and gals, but this is a serious “run.” In the cult classic, The In-Your-Face Basketball Book, a run is described as “playing ball,” and is typically a “full-court five-on-five” game that is the “ultimate test” of a player.1 This is what gets me up so early in the morning. The players have all played some level of organized basketball; high school, many college, and a few professionally overseas. They range in age from their 20s to late 60s. The games are spirited.
I have some skills, but at my age it is a tricky balance between expectations and nagging injuries. I keep coming back because there is nothing more gratifying than getting key rebounds; beating younger players down the court; setting a critical pick to free up a teammate for the winning shot; blocking the occasional shot; and sometimes making the winning basket. The competition is tough, and I cannot play like I could in my 20s, 30s, or 40s, but it is worth the stiffness, discomfort, and pain I will suffer later. It is exhilarating to work as a team to beat a younger, more talented, and overconfident team. Win or lose, playing in the run is energizing.
My morning run gets me in shape, makes me sore, but it also invigorates me for a busy day to come at the hospital.
A few hours later I am about to see a two-year-old for an annual check-up. Before I enter the room, I select the book Brown Bear, Brown Bear What Do

You See? from our Reach Out and Read bookshelf. After I say hello to the mother, I hand the book to the child. He takes the book, sits on a chair, begins looking at the book, and smiles. The child’s eyes light up when I point out a few of the illustrations and describe the images, and he repeats the words to me. His mother also smiles, asks if the book is for him, and I say, “Of course.”
This is such a simple, yet powerful, act that provides me with an opportunity to talk about a vital topic for many pediatricians: the importance of literacy and the promotion of reading aloud to children. This exchange is always one of the more gratifying moments of my day, and I owe it to the Reach Out and Read program.
Reach Out and Read is a national program that integrates reading aloud into pediatric care by providing books and coaching to promote literacy and make reading a daily routine for families.2 The Reach Out and Read model is an integral part of thousands of pediatric practices across the United States and is supported by a wealth of compelling evidence.
A recent study highlighted how children who have family members who read books to them every day hear more than a million more words than children who are not read to at home.3 The simple act of giving a book to a child and discussing the importance of reading aloud has increased reading in homes, the vocabularies of lowincome children involved in the program,4,5 and has developed the skills needed for children to be successful in kindergarten.6,7 Reach Out and Read is not only good for children, but also improves clinic morale and provider satisfaction.8 No wonder that giving a
continued on next page
Improving Resilence and Literacy continued from page 13
book to a child is one of the favorite parts of my day.
This scenario was not always the case for me. Several years ago, I was late for a patient panel one morning after a stressful night. The day before I had a panel of medically complicated patients who were difficult to manage. My panel went over the allotted time, and I had to complete my work at home. While I was completing charting and billing that evening, I also had to help my daughter with a paper that she was struggling to finish for school. I worked until after midnight. This scenario was compounded by the fact that my parents had recently died, I was tired and not sleeping well, felt overwhelmed, had stopped exercising, and realized my efforts to sustain our Reach Out and Read program had failed.
I was a mess—tired, stressed, frazzled, and grumpy. I cursed out loud as I opened our electronic health record (EHR) and received a task to complete an overdue bill, made a sarcastic remark to a colleague, and almost yelled back at a mother who was angry about her lengthy registration process. Not my best self. I grabbed a book and went to see my first patient. As I was furiously typing mom’s concerns into the EHR, I was startled when I felt a tap on my leg as the three-year-old patient walked up to me and asked me to open the book. Just like that, the child’s touch and request changed the course of that encounter, and provided me with a moment of clarity.
It dawned on me that I was ineffectively managing my personal and professional duties, and was experiencing symptoms of burnout. Something needed to change.
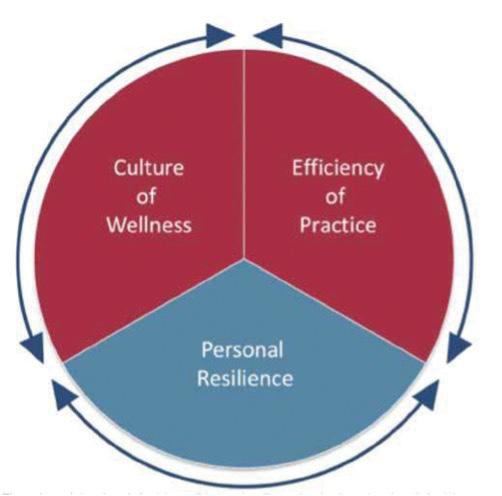
The importance of wellness was recognized centuries ago by Greek philosophers. Aristotle believed that there should be harmony between mind and body, and the father of modern medicine, Hippocrates himself, stressed the importance of a healthy mind and healthy body in his famous oath.9 Physical activity was also recognized as a critical part of physical and mental health. These ancient ideas about wellness quite closely match our modern ideas about wellness. Wellness is defined as “the quality or state of being healthy in body and mind,”10 and is impacted by work-life balance, social and family support, adequate rest, and regular physical activity.
Many providers struggle to balance providing quality patient care, spending time with their family, exercising consistently, and getting enough sleep. Physicians are also known to put their patients’ needs before their own, which can further exacerbate these challenges and lead to burnout.11 Providers who experience burnout have “emotional exhaustion,” “interpersonal disengagement,” and a “low sense of personal accomplishment.”11 This can lead physicians to feel “used up” and view patients “as
objects rather than as human beings.”12
Studies show that about one-half of physicians feel like their work schedule does not allow enough time for their personal life, and experience high levels of burnout.3 And, the problem is worsening.11,13,14 Physicians who once loved their practice are leaving because of the difficulty of balancing short visits, complicated patients, lack of control, EHR stress, and poor work-life balance.15,16 Burnout among physicians has become so common that it has become an epidemic,11 and is considered a public health crisis that has been exacerbated by the COVID-19 pandemic.17 Physician wellness must be urgently addressed.17-19
Physician well-being is related to three domains: efficiency of practice, culture of wellness, and personal resilience.11 The first two domains require systemic level changes in physician culture and productivity.20-22 However, the last domain is primarily on providers. Changing behaviors can be challenging, but when successful they offer measurable return on investment23 as burnout is usually reversible and preventable.12
Physicians should focus on their own personal resilience, should be able to maintain their health and wellness,24 and have self-awareness of their vulnerability to burnout.12 Studies show physicians can accentuate their own resiliency and productivity.12 This improved wellness leads to increased career satisfaction, an improved sense of well-being, increased empathy, and decreased burnout.16,25,26
After my encounter with the toddler, I realized I was emotionally exhausted, grieving the loss of my parents, and struggling to manage my clinical and family load.
I had lost control and needed to take ownership of my personal resilience. I first made a conscious effort to get more sleep, regardless of the amount of work I had to do. The work is always there in the morning, and I will be better prepared to complete it if I am better rested. I then made a conscious effort to turn off technology (the phone, mostly). It is easy to waste valuable time on the phone. I also began running to get into shape. Running a few miles is an efficient way of getting exercise, even if I run half as far in the same amount of time as I did in my 20s.
These commitments meant leaving work on a timely basis to get in a run before picking up my children and eating dinner with my family. I also made sure to schedule time to play basketball at least once a week.
These changes represented a huge change for me to prioritize my own personal resilience. I quickly improved my outlook, fitness, and overall productivity.
Since I reconnected with the basketball run I began to get in shape again, and experience that exhilarating feeling from playing basketball again. One Sunday at our pick-up game I was discussing our Reach Out and Read program and came up with the wild, but inspired, idea to combine our passions for basketball and literacy in a creative effort to raise more money. The fact that Reach Out and Read is so simple, evidence-based, and costeffective made it easy to convince sponsors to support it.
We created the Reach Out and Read Basketball Tournament, an annual, one-day, five-on-five, round-robin basketball tournament. For the first tournament we had seven teams, 10 sponsors and raised more than $7,000. I was reinvigorated!
In the years since that first tournament we tweaked our format and recruited more sponsors. Last year, we celebrated the tournament’s 10th Anniversary and raised over $226,000. Simply, we are astounded. These funds will support a dozen different programs throughout the hospital, but we also have the opportunity to expand our programming in ways we never thought possible.
One key to happiness for physicians is to connect with our purpose. Whether that be basketball, knitting, singing in the church choir, or cooking, it can be an energizing force in our lives that can reduce burnout.27
Being a physician is incredibly rewarding, but also quite stressful. I will always struggle with my work-life balance, but my improved personal resilience has reduced my burnout and improved my productivity. I consider myself fortunate that the tap of a toddler served as a wakeup call for me.
Amazingly, making time for one passion—basketball—saved another—our Reach Out and Read program. If physicians connect with their purpose it might prove to be an energizing and positive force in their lives that can serve a greater good.

References
1. Wielgus C, Wolff A. The In Your Face Basketball Book. New York: Everest House. 1980; 29,49.
2. DeWitt T, Gallagher B. Celebrating Together! Reach Out and Read: 20182019 Annual Report. 2019. Reach Out and Read. https://reachoutandread. org.
3. Logan J, Justice L, Yumus M, Chaparro-Moreno L. When Children Are Not Read to at Home: The Million Word Gap. J Dev Behav Pediatr. 2019; 40(5): 927-34.
4. High P, LaGasse L, Becker S, Ahlgren I, Gardner A. Literacy Promotion in Primary Care Pediatrics: Can We Make a Difference? Pediatrics. 2000; 105(4): 927-34.
5. Mendelsohn A, Mogilner L, Dreyer B, Forman J, et al. The impact of a clinic-based literacy intervention on language development in inner-city preschool children. Pediatrics. 2001; 107(1): 130-4.
6. Mol S, Bus A. To Read or Not to Read: A Meta-Analysis of Print Exposure From Infancy to Early Adulthood. Psychol Bull. 2011; 137(2): 267-96.
7. Diener M, Hobson-Rohrer W, Byington C. Kindergarten Readiness and Performance of Latino Children Participating in Reach Out and Read. J Community Med Health Educ. 2012; 2(3): 133-9.
8. Burton H, Navsaria D. Evaluating the Effect of Reach Out and Read on Clinic Values, Attitudes, and Knowledge. WMJ. 2019; 118(4): 177-81.
9. Kleisiaris C, Sfakianakis C, Papathanasiou I. Health care practices in ancient Greece: The Hippocratic ideal. J Med Ethics Hist Med. 2014; 7: 6.
10. Wellness. Definition & Meaning. Dictionary.com. https:// www.dictionary. com/browse/wellness.
11. Bohman B, Dyrbye L, Sinsky C, Linzer M, et al. Physician Well-Being: The Reciprocity of Practice Efficiency, Culture of Wellness, and Personal Resilience. August 7, 2017. N Engl J Med Catalyst online. https://catalyst. nejm.org/doi/ full/10.1056/CAT.17.0429.
12. Patel R, Bachu R, Adikey A, Malik M, Shah M. Factors Related to Physician Burnout and Its Consequences: A Review. Behav Sci. 2018; 8(11): 1-7.
13. Shanafelt T, Hasan O, Dyrbye L, Sinsky C, et al. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General U.S. Working Population Between 2011 and 2014. Mayo Clin Proc. 2015; 90(12): 1600-13.
14. Shanafelt T, Swensen S. Leadership and Physician Burnout: Using the Annual Review to Reduce Burnout and Promote Engagement. Am J Med Qual. 2017; 32(5): 563-5.
15. Agency for Healthcare Research and Quality; Physician Burnout. 2017. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html.
16. American Board of Pediatrics; Tackling Burnout. 2019. https://www.abp. org/news/annual-reports/tackling-burnout.
17. Jha A, Iliff A, Chaoui A, Defossez S, et al. A Crisis in Health Care: A Call to Action on Physician Burnout. Massachusetts Medical Society; 2019. 1-12.
18. Baptista S, Teixeira A, Castro L,Cunha M, et al. Physician Burnout in Primary Care during the COVID-19 Pandemic: A Cross-Sectional Study in Portugal. J Prim Care Community Health. 2021; 12: 1-9.
19. Bailey J, Wong M, Bailey K, Banfield J, et al. Pandemic-related factors predicting physician burnout beyond established organizational factors: crosssectional results from the COPING survey. Psychol Health Med. 2021; Oct 14: 1-15.
20. Shanafelt T, Schein E, Minor L, Trockel M, et al. Healing the professional culture of medicine. Mayo Clin Proc. 2019; 94(8): 1556-66.
21. Parks T. Physician Burnout; Detailing the Impact, Exploring the Solutions. December 14, 2016. American Medical Association. https://www.ama-assn. org/practice-management/physician-health/physician-burnout-detailingimpact-exploring-solutions.
22. Dillon E, Tai-Seale M, Meehan A, Martin V, et al. Frontline Perspectives on Physician Burnout and Strategies to Improve Well-Being: Interviews with Physicians and Health System Leaders. J Gen Intern Med. 2019; 35(1): 261-7.
23. Shanafelt T, Goh J, Sinsky C. The Business Case for Investing in Physician Well-being. JAMA Intern Med. 2017; 177(12): 1826-32.
24. Taub S, Morin K, Goldrich M, Ray P, et al. Physician health and wellness. Occup Med. 2006; 56(2): 77-82.
25. McClafferty H, Brown O. Physician health and wellness. Pediatrics. 2014; 134(4): 830-5.
26. Shanafelt T, Noseworthy J. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clin Proc. 2017; 92(1): 129-46.
27. Krall EJ. Ten Commandments of Physician Wellness. Clin Med Res. 2014: 12(1-2); 6-9.
This article originally appeared in The Pharos, Winter 2024. The author’s E-mail address is hk39@drexel.edu.

By T.J. Huckleberry Executive Director, PCMS
In the process of reviewing our archives as your new Executive Director, I stumbled upon the minutes of our Fall 1895 Board of Directors Meeting. I was amazed to find a fascinating club that was established during that time. I am happy to announce that we will be reviving this collegiality initiative in 2026. Below, please find the transcript detailing the creation of this event and the words of its founding physician, the esteemed Dr. I. Noah Party.
Ladies and Gentlemen of the Philadelphia Medical County Society I rise today to propose a new social club for our member-physicians. In the wake of Dr. Eli Brary’s well attended book club, and Dr. Harry Sideburns fascinating lecture series on handlebar moustaches and modern grooming techniques…I propose we start a club that is based solely about having fun and hanging around fellow physicians whom we deem awesome.
This club will meet monthly, with a new member hosting each month. It will be a small affair of perhaps 10 -15 physicians who, at the invitation of the host, will join in celebrating the hobby, sport, or venue chosen for the event! Of course, we could incorporate Dr. I.C. Robbin’s wildly popular birding club and the hiking group Dr. Roman Tufar has started.
This will be a good way for all of us to blow off some steam and network or perhaps reconnect with our fellow physicians. Let us not forget all the great theatres, stadiums and other locations this city has to offer, all just a mere carriage ride away!
I must reiterate dear colleagues that there are zero clinical or medical advancements made during these events but just good old fashion revelry. …In fact, that’s it! We will call it the Revelry Club!
All in favor say Houzah!
Secretary’s note: Dr. I. Noah Party’s motion was carried out unanimously.
- Dr. Stu F. Fedmoose’s taxidermy club was not invited or recognized to join the Revelry Club.
How the Revelry Club works:
Who: Any member who would like to host an event with fellow physicians.
What: A monthly collegiality initiative aimed at retaining and recruiting physicians and promoting the passions of our members
Where: Philly and the surrounding community
Why: …why not???
How: a member is selected monthly to host; the host invites 10-15 colleagues (preferably 3-4 nonmembers or new physicians). The host receives a stipend to support the gathering. Event happens; event will be highlighted in Philadelphia Medicine. Next month a new host is selected.
Respectfully submitted, Dr. Yul B. Reading, Secretary.
Approved by, Dr. Ira M. Overworked, President
As you all can see this is a great idea for our members to get involved and celebrate what they love to do outside of medicine. Whether it is tailgating at an alumni event, cookie baking during the holidays, biking your favorite trail, or teaching your friends your favorite hobby…this club is for you. So, if you are interested in following in the footsteps of the genius Dr. I Noah Party, please contact me at tjhuckleberry@philamedsoc.org!

Inever would have thought—
Let alone felt—
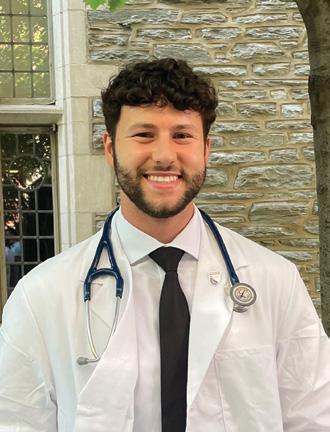
By Alan Napole
The inescapable grasp patients would have on my mind and heart.
The deeper I dive into medicine, The less of myself I remain, but not in the way you might think.
Instead, I become the king of the jungle with JP, conquering the slithering anaconda that is the influenza vaccine. Lions may be bitten in battle, but they still reign. Blood drips. Chest pounds. Pride soars. JP, triumphant, marvels at his battle scar.
Instead, I become MW’s son, the 26-year-old she lost to a stray bullet. In me, she sees him—an echo of love, loss, and hope. With that vision, she tells me to live the life so many cannot, a life she now lives for him. His essence, encapsulated in a locket close to her heart. We ask each other for a hug: hers for her son, mine for my grandmother, always 6,216 miles away. For a fleeting moment, distance evaporates, and someone impossibly far feels achingly near. I can only imagine she feels the same.
Instead, I become a best friend, an unbiased, privileged, reassuring confidant for DJ, whose world fractures with the weight of a new diagnosis. A sexually transmitted illness. Betrayal. Abandonment. Filth. Her words don’t come; they spill, raw and unrestrained, as a storm of tears. In that moment, I am who she needs. My voice becomes familiar: “You are not alone, and everything will be okay.” Twenty minutes stretch into the intimacy of twenty years. Vulnerability is met with peace, so we speak of life.
Instead, I step into the ring with DC as his sparring coach and he, the boxer. Every test becomes a fight. The scarf test transforms into a right hook. The strength test, into weights at the gym. His fists—the source of his identity, his strength, his being—are in jeopardy. He trusts me as his coach to push him when he needs it, and to bench him when he can take no more.
Instead, I become an astronaut, guiding AB for his next mission. Soon he is to board the spaceship known as the MRI. From fear springs the will to be braver than we believed we could
be. When alarms sound, I guide AB to swerve from the meteoroid. The rumble of the MRI transforms into engines roaring as we soar beyond the Milky Way—Earth, Mars, Jupiter fading behind us. When the time comes, I remind AB to trust in our training, to draw upon his strength, and to remember that he alone has what it takes to complete this mission. Steadying my voice, I say. “I’ll see you on the other side, Captain.”
Instead, I stand in the position of attention, bound by blood to my fellow soldier, DW. We sprint over the bullet casings and remnants of life—fallen bodies, families torn asunder, souls consigned to oblivion. Mission complete, right? DW and I salute—a gesture that echoed hollow in the silence. Who knew four years of service could unfurl into a lifetime of unseen wounds, only numbed by the solace of a bottle. I spoke, hoping my words might span days—maybe even weeks—of buoyancy just to keep him afloat. Yet, it tore at my soul, watching him drown, submerged beneath the weight of wars long past.
The lives my patients lead seep into the rooms we share.
I step into their worlds,
Privy to their fears, their dreams, their fragile hopes.
Shapeshifting into who they want me to be, only to become who they need in the end.
I’ve learned medicine is not solely in knowledge or technical skill,
But in the delicate cultivation of trust,
In asking not “Why the addiction?” but rather, “Why the pain?”, “Why the loneliness?”, “Why the fear?”
Through this lens, generational differences melt away; our shared humanity remains timeless.
I was always excited to become a physician.
Yet no one told me I’d also become a lion, a son, a best friend, a boxing coach, an astronaut, a soldier.
I do not know what the future holds—
But I do know this:
I await my next shapeshift.


By Kory Dillman
“Your heart is world-class,” the cardiologist reassured me after my successful cardiac ablation. Despite excellent medical care and technical success, I remained terrified to raise my heart rate. Every minor exertion triggered the same anxiety: What if my body can’t take it?
My journey began with a partial thyroidectomy following an accident. Months later, I developed supraventricular tachycardia requiring cardiac ablation. For ten years afterward, I heard a constant refrain that contradicted my lived experience: “Your numbers are fine.” Then why didn’t I feel fine?
Cardiac anxiety stemmed from multiple factors—psychological adaptation following procedures, years of dismissed symptoms across specialties, and natural concerns when your body betrays you. While my heart was medically cleared and TSH levels were “normal,” my confidence remained shattered.
What finally rebuilt that confidence wasn’t another medical intervention. It was a cycling training app—not a medical device— providing continuous monitoring and daily guidance, filling the space where traditional healthcare operates only episodically.
As a professional working with medical software and digital health, this patient experience revealed something profound: we excel at procedures but often abandon patients during critical recovery periods, precisely when psychological healing is most needed.
The cycling app succeeded where routine follow-up failed by providing what healthcare traditionally hasn’t: continuous, personalized attention during daily life. Each day, the app analyzed my biometric data using AI algorithms, offering simple guidance: “Ready to train” or “Focus on recovery”—based on heart rate variability, sleep quality, and stress response.
Where traditional healthcare provides snapshots during scheduled visits, patients experience symptoms, anxiety, and recovery continuously. The app filled that temporal gap with real-time feedback, giving me the information needed to trust my body again.
This shift represents a fundamental paradigm change in healthcare delivery. Digital technologies enable continuous collection of physiological and behavioral data, offering unprecedented insight into a patient’s status between visits. This data stream identifies patterns invisible to episodic care—subtle changes signaling successful recovery or early decompensation.
Yet not all digital therapeutics (DTx) deliver on this promise. Physicians considering the integration should proceed cautiously. A recent JAMA Internal Medicine systematic review found only 35% of digital therapeutics had effectiveness results available at release, with 34% having no clinical studies at all—even among FDA-regulated products.¹
continued
The Space Between Appointments: Learning from a Patient-Professional’s Journey; Clinical Insights from the Other Side of Care continued from page 19

Recent JACC expert consensus emphasizes that effective remote monitoring requires accurate, actionable signals coupled with systems that engage and empower patients through personalized algorithms.²
My cardiac anxiety highlights a specific clinical opportunity where continuous monitoring’s trust-building capacity becomes essential. Research confirms this experience is common, with studies showing significant anxiety and depression following cardiovascular procedures, even among patients in cardiac rehabilitation programs. Baseline psychological status strongly influences recovery outcomes, underscoring the need for tailored interventions that extend beyond traditional rehabilitation.³
The cycling app succeeded by moving beyond standard of care reassurance to individualized validation. Rather than hearing my heart was “normal” based on established parameters, I received daily confirmation that my specific physiological responses were appropriate for my recovery trajectory. This personalized feedback established trust that episodic clinical encounters couldn’t match.
Digital therapeutics for health anxiety can provide continuous support during vulnerable recovery periods, combining symptom tracking with cognitive behavioral therapy techniques to help patients distinguish between normal recovery sensations and warning signs requiring attention. The key is personalization— algorithms learning individual patient patterns rather than applying universal thresholds.
The most promising digital health solutions extend clinical judgment by providing continuous, personalized data. Integrating applications with electronic health records provides clinicians with longitudinal insights into patient symptoms, treatment adherence, and responses to interventions.
During my recovery, the convergence of proper medical management with continuous feedback proved transformative. When I found an endocrinologist willing to titrate thyroid medication based on symptoms rather than population averages, optimized dosing restored my energy levels. Continuous biometric monitoring reinforced what my body was telling me through daily objective data confirmation.
This illustrates how digital health can inform clinical decisionmaking through personalized insights rather than generic recommendations. Instead of applying standard protocols based on population data, providers access individual patient patterns— how specific patients respond to medications, their baseline vital signs, and symptom fluctuations over time.
Continuous data streams enable a sophisticated understanding of treatment response. Rather than relying solely on patient recall during appointments, providers observe objective patterns of daily function, symptom variations, and treatment adherence.
Effective healthcare delivery requires both episodic intervention and continuous support, with digital technologies bridging these domains. The cycling app established digital trust through consistent, personalized feedback that validated my recovery in real-time rather than waiting for the next appointment.
This addresses a fundamental healthcare delivery limitation: assuming patients exist in steady states between visits. Recovery is dynamic, with daily variations in symptoms, function, and psychological adaptation. Continuous monitoring technologies track these fluctuations and provide personalized guidance, adapting to individual patterns.
For conditions where psychological adaptation equals physical healing in importance—cardiac recovery, chronic disease management, anxiety disorders—continuous engagement may be essential. Digital therapeutics bridge gaps between successful medical intervention and complete recovery by providing ongoing support that builds trust through consistent validation.
Leading health systems are demonstrating this potential through advanced care-at-home programs that integrate remote monitoring, telehealth, and in-home services to deliver hospitallevel care with continuous support—reducing readmissions and improving patient satisfaction compared with traditional episodic care.
As digital health matures and demonstrates clinical value through rigorous studies, it may become standard in comprehensive care plans, particularly for conditions requiring ongoing behavioral support or symptom management. Current evidence underscores the need for continued clinical validation before widespread implementation.¹
Leading cardiology experts note signal specifications differ for high-risk patients requiring early intervention versus low-risk patients needing surveillance,² suggesting personalized approaches to digital health integration are essential.
Healthcare providers interested in DTx integration might consider:
• Prioritizing FDA-cleared applications relevant to their practice areas
• Identifying patient populations benefiting from continuous monitoring, particularly high-risk patients requiring actionable interventions versus those needing surveillance
• Evaluating personalization capabilities in digital health tools that adapt to individual patient patterns
• Assessing trust-building features in DTx applications through daily patient interactions
• Considering hybrid care models combining episodic clinical encounters with continuous digital support
• Monitoring clinical outcomes and patient engagement metrics
The technology exists, clinical evidence is growing, and regulatory frameworks are expanding. Given significant gaps in evidence supporting many digital therapeutics¹, the primary question isn’t whether these tools will become part of clinical practice, but how to integrate evidence-based, personalized DTx thoughtfully while maintaining appropriate clinical standards.
My experience rebuilding confidence through continuous, personalized feedback demonstrates the potential. For patients struggling between medical intervention and complete recovery, carefully selected digital therapeutics may offer the continuous, individualized support that traditional episodic healthcare cannot provide—when backed by appropriate evidence, clinical oversight, and trust-building design principles.

Kory Dillman is a healthcare consultant with 15 years of experience in software as a medical device (SaMD) and digital therapeutics. The article uses that perspective, plus his personal healthcare journey, to present DTx as a meaningful option. Mr. Dillman’s perspective is brought to us by Benjamin Alouf, MD, a member of the Philadelphia Medicine editorial board and Philadelphia County Medical Society physician who works in the digital therapeutics field.
References
1. Agarwal M, Phan NTT, Alshehri F. Mapping the Evidence Supporting Digital Therapeutics. JAMA Intern Med. 2024;184(10):1229-1231. doi:10.1001/jamainternmed.2024.0022
2. Stevenson LW, Ross HJ, Rathman LD, et al. Remote Monitoring for Heart Failure Management at Home: JACC Scientific Statement. J Am Coll Cardiol. 2023;81(23):2272-2291. doi: 10.1016/j.jacc.2023.04.010
3. García-Bravo S, Cuesta-Vargas AI, González-Sánchez M. Impact of cardiac rehabilitation on anxiety, depression, and health-related quality of life in cardiovascular patients. Egypt Heart J. 2025; 77:658. doi:10.1186/s43044025-00658-8
The Pennsylvania Medical Society (PAMED) held its annual House of Delegates (HOD) on October 18th in Hershey, PA, where physicians, residents, fellows and medical students representing Philadelphia County and from across the state converged to shape the organization’s official policies. The adopted resolutions tackle a range of critical issues, from public health threats and healthcare access to workforce sustainability and governance in medicine.
PAMED reaffirmed its support for pediatric vaccines and the recommended vaccination schedule as currently endorsed by the American Academy of Pediatrics. The society also committed to the sharing of broadcasting tools to improve communication between physicians and vaccine-hesitant parents/guardians, aiming to enhance acceptance of routine vaccinations.
PAMED will now promote the expanded distribution of drug adulteration test strips and advocate for better education on managing xylazine-associated wounds for healthcare professionals in shelters and rehabilitation centers.
Fossil Fuel-Related Pollution
PAMED passed a resolution acknowledging fossil fuel combustion as a major, modifiable contributor to air pollution and its subsequent harmful
health effects. As a result, the organization now supports the responsible adoption of fossil fuel-sparing energy sources.
PAMED took a strong stance in direct opposition to federal or state imposition of work requirements as a criterion for Medicaid eligibility, committing to partner with other medical organizations to oppose such policies.
PAMED committed to actively advocate for increased state and federal investment to expand rural healthcare infrastructure, including emergency and maternal care, behavioral healthcare, and essential services like mobile health units and transportation. This includes promoting legislation to secure financial and professional incentives, such as competitive reimbursement rates and targeted residency placement programs, to attract and retain healthcare professionals in rural communities.
PAMED supports the expansion of medical school enrollment and will advocate for additional Graduate Medical Education (GME) training slots and residency programs, especially in underserved areas. These efforts will be paired with incentives such as increased compensation and loan forgiveness for graduates who commit to practice in these
communities. Furthermore, the society will advocate for easing restrictions and for providing support to H-1B and J-1 visa applicants to integrate international medical graduates into the workforce in underserved regions.
PAMED resolved to advocate for legislation to restrict private equity acquisition of hospitals and to prohibit hospitals from participating in real estate investment trust (“REIT”) transactions. These actions aim to improve transparency and oversight of hospital mergers while ensuring clinical autonomy and operational authority for physicians in medical groups and ambulatory surgical centers.
Finally, emphasizing the importance of nonpartisan patient rights, PAMED adopted a resolution to support and to advocate for increased emergency ballot access efforts for hospitalized and longterm care patients.
The policies adopted at this year’s HOD provide the foundation for PAMED’s advocacy efforts for the near future, underscoring the commitment of Pennsylvania’s medical community to improving public health, ensuring equitable access to care, and safeguarding the integrity of the medical profession.






FEATURE continued
Pennsylvania Physicians Set Health Policy Agenda at Annual House of Delegates continued from page 23





Delegation
Enrique Hernandez, MD, FACS, FACOG (Chair)
Brian Hannah, MD (Secretary)
Gabriella Baldassarre
Victoria Cimino, MD, MPH
Katherine Jerakis
Julia Katcher
Stacie Kerbel
Alekhya Madiraju
Robert Medina
Curtis Miyamoto, MD
Ricardo Morgenstern, MD
Chioma Nwanonyiri
Anthony Padula, MD, FACS
Anika Patel
David Sass, MD, AGAF, FACG, FACP
Nicholas Wahba
Alternate Delegates
Noor Baban
Stephen Permut, MD, JD
Heather Raphael
Susan Robbins, MD
Kenneth Wasserman, MD
PCMS Participants (non-delegates)
Martina Bernstein
Theodore Christopher, MD, FACEP


Ex officio members of PAMED including several members of PCMS
Michael DellaVecchia, MD, FACS, FCPP, FICS, PhD, FAAO, FASLMS
Michael Feinberg, MD, PhD
Nicholas Felter
Teresa Hong
Cadence Kim, MD, FACS
Pratistha Koirala, MD
Lynn Lucas-Fehm, MD, JD
Dale Mandel, MD, FACS
Deepak Mehrotra, MD
Sarita Metzger, MD
Anant Mishra
Gillian Naro, MD
Oluwaseun Oguntunmibi
Sebastiano Porcu, MD
Benjamin Smood, MD
William Van Decker, MD
John Vasudevan, MD




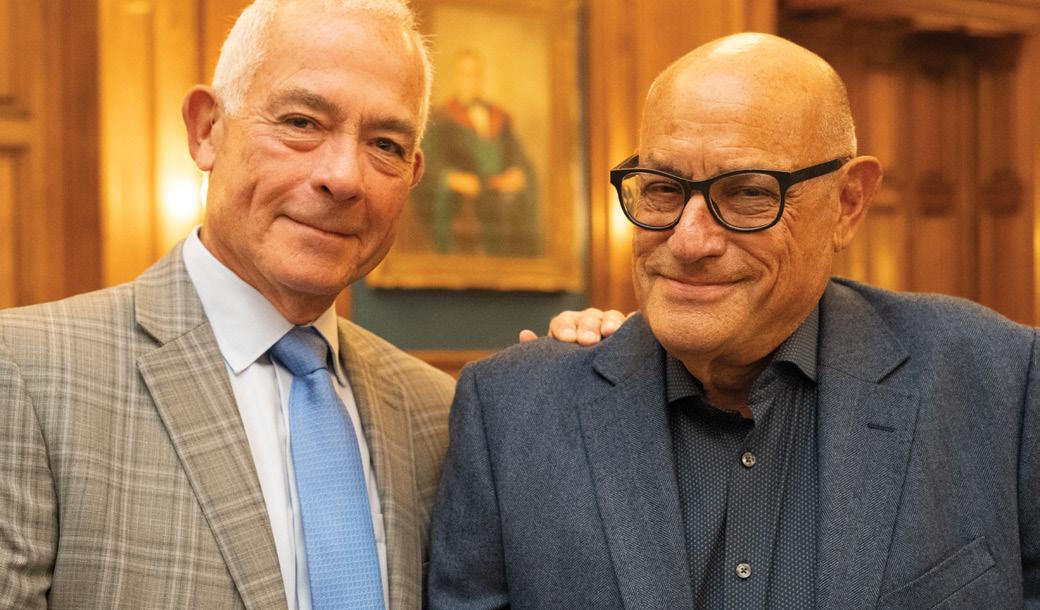
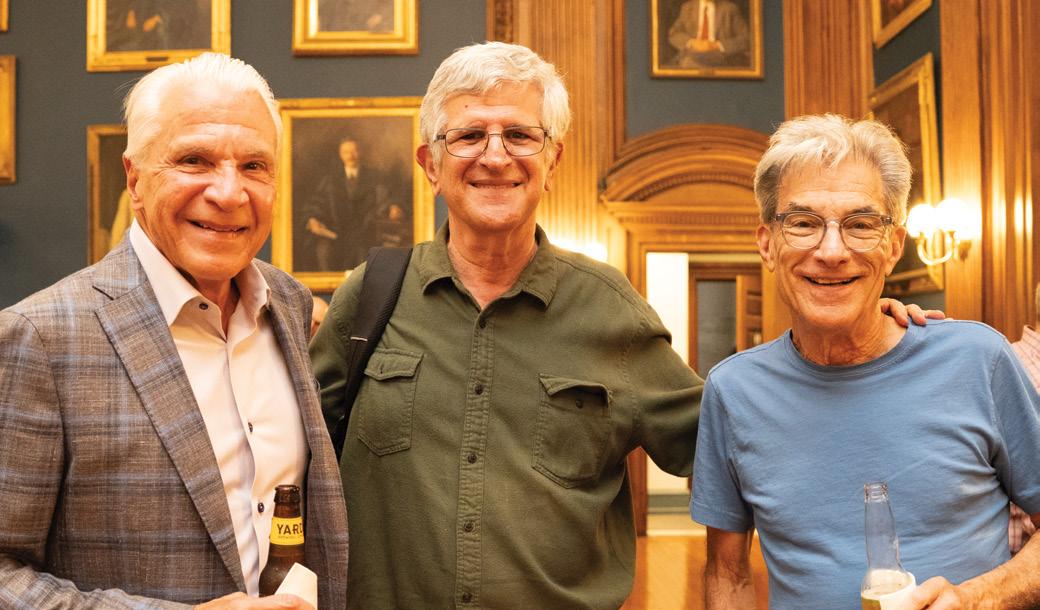
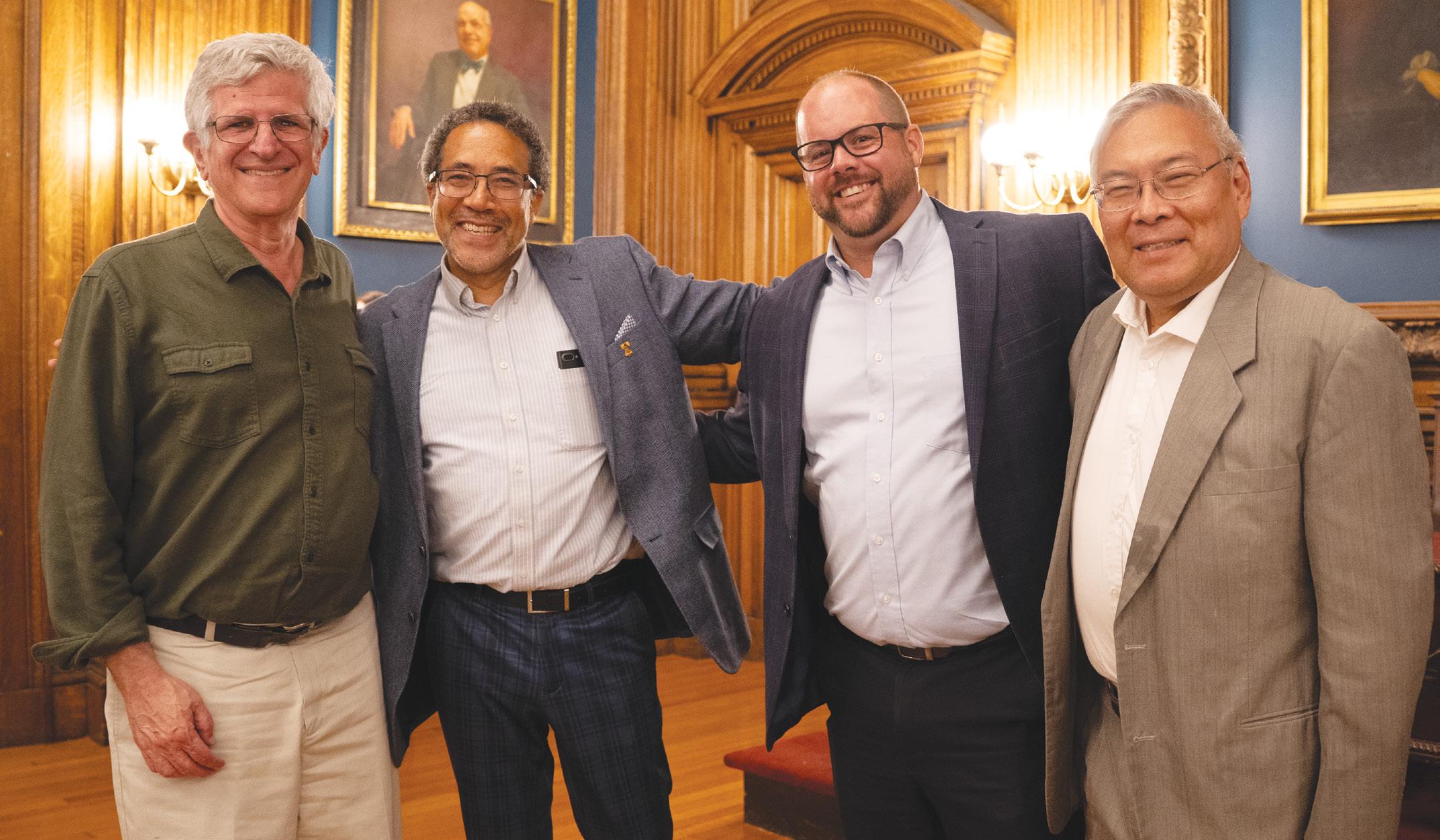
John Vasudevan introduced the mission of the Doctors Lounge: “This is what I hope to recreate in our Doctor’s Lounge events: a place where we mix socializing, food and drink, and casual conversations that might inspire us to maximize our skills as physicians.” John turned the microphone over and the almost-100 attendees settled in for a dynamic conversation, facilitated by Walter Tsou, our current PCMS president, and Bill King, PCMS board member.

Dr. Offit, our dedicated pediatric infectious disease specialist, one of the developers of the RotaTeq vaccine, and intrepid defender of vaccinations across the country, was ready to help us understand the current hostile political climate at RFK Jr.’s Department of Human Services. Our second conversant of the night was Dr. Emanuel, Oncologist and Bioethicist, and policy advisor to the Obama White House during the development of the Affordable Care Act (ACA), ready to explain how the physician community might need to prepare for the upcoming assault on health care funding following passage of the “Big Beautiful Bill.”
Monday, September 15 6:00 PM - 8:30 PM
The College of Physicians of Philadelphia 19 S 22nd
The conversation was thrilling. Dr. Zeke Emanuel demonstrated his amazing ability to break down extremely complicated health policy with a few brief complete thoughts. “There are five goals to a healthcare system. There’s universal coverage at reasonable costs with consistent high quality, with minimal disparities and high satisfaction by patients as well as physicians and other providers. We were far from that in 2009 when we began on the Affordable Care Act, but the problem is we did make a lot of progress. We both brought the number of uninsured down from almost 17% down to 8%. But the last few months and looking forward, a lot of that’s gonna unravel. The
continued on page 28

The Doctors Lounge series is designed to bring physician and trainee members of the Philadelphia County Medical Society and College of Physicians of Philadelphia together over food and drink to socialize and learn from expert panelists on how to use one's medical degree to advance their goals in business, public health, leadership/administration, and politics. Attendees are welcome to bring a guest.








FEATURE continued
The Doctors Lounge—A Recap continued from page 27



one Big Beautiful Bill supposedly is going to throw 12 million people off of coverage. We’re going to have another big group of people lose coverage because the extra subsidies for the exchanges are going to go away. So, we’re going to lose a lot of people, maybe even half of the gains that we made from the Affordable Care Act.”
Dr. Offit was even more prescient in preparing us for hard times defending the gains of science and medicine. “But here’s the good news. So, we can end on a positive note. When Galileo was censured by the Roman Catholic Church for daring to put forward Copernicus’s notion that the earth revolved around the sun, he said to them, even as he was being carried away in chains. And yet he said, “it still moves.” That the earth revolves around the sun. And no matter how many times RFK Jr. says vaccines cause autism or how many sycophants or congressional representatives or fringe doctors or fringe scientists or media outlets he gets to echo, it doesn’t (cause autism). And science is a powerful thing to have on your side in the long run.”
As we listened to Dr. Offit and Dr. Emanuel answer our questions about the future of medicine, we were reassured that our profession is still striving to have dialogue and face the future while pursuing knowledge at the Doctors Lounge.
Check out the full podcast with Dr. Offit and Dr. Emanuel’s interview with PCMS: https://philamedsoc.org/ philadelphia-medicine-magazine-live-podcast-pilot-episode/.





The Doctors Lounge—A Recap continued from page 29







Each year, PCMS members are given the opportunity to participate in a rich diversity of committees that impact the practice of medicine in Philadelphia County, Pennsylvania and beyond. Because active participation in PCMS strengthens the voice of organized medicine, we encourage all members (including medical students, residents and fellows) to help make an impact on the role PCMS plays in the medical community.
• Editorial Review Board – Works on the Philadelphia Medicine magazine and newsletter.
• Delegate Caucus to Pennsylvania Medical Society’s Annual Meeting –Participates in PAMED’s House of Delegates as a representative of PCMS.
• Public Health Committee – Tackles issues related to public health and manages the Block Captain Healthcare Council.
• Membership Committee – Works on membership recruitment and retainment.
• Early Career Section – Represents the needs of early career physician membership.
• International Medical Graduates Section – Represents the needs of International Medical Graduate (IMG) membership.
• Senior Physician Section – Provides a platform for physicians aged 65 and above to remain active and involved in the medical community.
• Women Physician Section – A forum to encourage women physicians to participate in leadership, policymaking, advocacy, and other activities of PCMS.
• Residents/Fellows Section – Represents the needs of resident and fellow membership.
• Medical Student Section – Works to improve medical education and advocates for the future of medicine.
To find out more about specific committees, go to https://philamedsoc.org/pcms-committee-form/ or call us at 215-563-5343 or email us at stat@philamedsoc.org.