



OUR PRESENTATION AND WORKSHOP OBJECTIVES
This workbook provides a holistic approach to treating dementia patients using massage therapy, natural remedies, movement therapy, and integrative wellness strategies. It is designed for massage therapists seeking to expand their knowledge and skillset in dementia treatment and rehabilitation.
Participants will gain a comprehensive understanding of dementia as a progressive neurological condition involving memory loss, impaired planning, sensory vulnerability, and changes in emotional regulation. The course explains how neuroplasticity continues throughout the lifespan and how therapeutic touch, routine, and sensory grounding help stabilize function.
• Overview of Alzheimer’s, vascular dementia, and mixed dementia
• How inflammation, metabolism, and vascular health influence cognitive decline
• Principles of neuroplasticity and how the brain adapts even in later stages
• Musculoskeletal and movement changes seen in dementia
• How manual therapy supports sensory pathways and calming responses
This workbook provides a holistic approach to treating dementia patients using massage therapy, natural remedies, movement therapy, and integrative wellness strategies. It is designed for massage therapists seeking to expand their knowledge and skillset in dementia treatment and rehabilitation.
Participants will learn how holistic approaches can reduce agitation, improve sleep, stabilize mood, and support clearer daily functioning. The goal is to create a calmer, more regulated internal environment that supports brain resilience.
• Herbal medicine for anxiety, sleep disturbance, and agitation
• Anti-inflammatory and low-sugar nutrition to reduce metabolic stress
• Breathwork techniques caregivers can use with patients
• Vagus nerve stimulation to reduce sympathetic overload
• Daily routines that stabilize mood and reduce behavioral escalation
This workbook provides a holistic approach to treating dementia patients using massage therapy, natural remedies, movement therapy, and integrative wellness strategies. It is designed for massage therapists seeking to expand their knowledge and skillset in dementia treatment and rehabilitation.
Participants will develop hands-on skills tailored to cognitive decline, focusing on calming, grounding, and safe mobilization. Techniques address sensory overload, chronic pain, frailty, and gait instability while promoting comfort and emotional security.
• Lymphatic drainage and gentle circulatory work
• Warm infused oil therapy to reduce tension and improve sleep
• Slow guided movement, rocking, and rhythmic mobilization
• Hand-over-hand techniques to reduce fear and resistance
• Supportive positioning and safety practices for unstable gait
This workbook provides a holistic approach to treating dementia patients using massage therapy, natural remedies, movement therapy, and integrative wellness strategies. It is designed for massage therapists seeking to expand their knowledge and skillset in dementia treatment and rehabilitation.
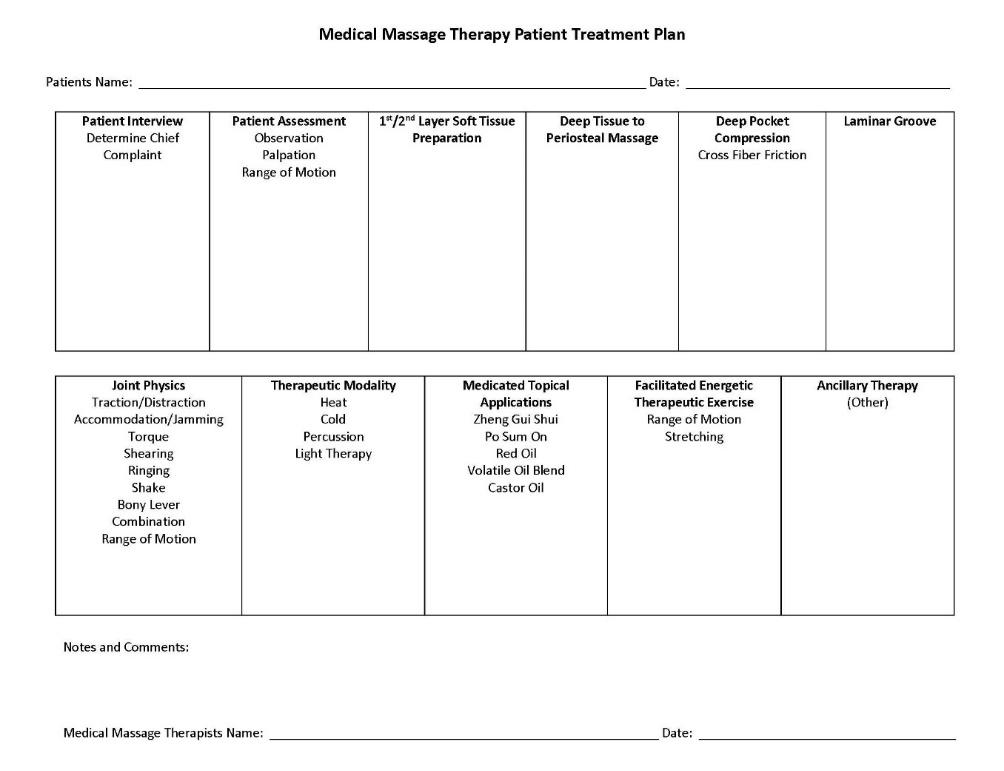
Participants will learn to assess functional status, sensory needs, mobility limitations, and behavioral patterns to build individualized care plans. These plans combine manual therapy, holistic support, caregiver techniques, and home routines that improve quality of life.
• Assessment of agitation triggers, overstimulation, balance, and sleep patterns
• Integrative planning with massage, herbal medicine, nutrition, and sensory techniques
• Daily routines that reduce confusion and increase cooperation
• Safety strategies for caregivers and therapists
• Long-term support plans for progressive cognitive decline

A medical massage therapist plays a vital role in the rehabilitation and recovery of dementia patients, working in collaboration with physician's, physical therapists (PTs) and occupational therapists (OTs) during the various stages of the patient's illness. In the early stages, the therapist may provide supportive care but as the disease progresses, the role of the medical massage therapist often becomes more central, often assuming a major role in ongoing treatment and therapy.
Gregory T. Lawton, D.N., D.C., D.Ac., N.D.
Dr. Lawton is national board certified in chiropractic, physiotherapy, radiology, and acupuncture.
Former vice president of large state- wide physical therapy group practice.
Founder of the Blue Heron Academy.
Founder of American Health Source.
Over 50 years in private practice at Clinical Health Maintenance.
Undergraduate and graduate studies in psychology at Arizona State University, a graduate of the National College of Naprapathic Medicine, the National University of Health Sciences, and the International Medical Acupuncture Association.
Gregory T. Lawton, D.N., D.C., D.Ac., N.D.
40+ years of research in the field of brain, spinal and peripheral neurology.
Author of over 100 books and numerous health science articles.
Licensed in 4 healthcare professions in 3 US states.
50+ years as a health science educator.
Former vice president of large medical psychology practice with a neuro-psych testing center.
Former youth probation officer and co-founder of the Berrien County Drug Rehabilitation Center
Gregory T. Lawton, D.N., D.C., D.Ac., N.D.
Consultant to major hospital systems including:
– Baptist Medical Center, Jacksonville, Florida
– Harper-Grace Hospitals, Detroit, Michigan
– William Beaumont Hospital, Royal Oak, Michigan
Creator and developer of 21 outpatient clinical programs for hospitals and medical centers.
Designer of nationally recognized Cardiac Rehabilitation and Pulmonary Rehabilitation programs.
Developer of 19 additional specialty outpatient services including:
– Stress management and lifestyle intervention programs
– Chronic pain and musculoskeletal rehabilitation programs
– Integrative health education, nutrition, and preventive medicine services
– Community-based chronic disease management initiatives
Expertise includes program creation, implementation, staffing models, clinical protocols, compliance, and patient-outcome–driven metrics.
Functional chiropractic medicine is a holistic approach to healthcare that combines traditional chiropractic techniques with principles of functional medicine. This approach aims to treat the root causes of health issues rather than just addressing symptoms. Functional chiropractic medicine seeks to create a balanced and healthy state within the body by addressing the interconnected systems and promoting overall wellness. This approach can be particularly beneficial for chronic conditions, complex health issues, and patients looking for a natural and integrative approach to their health.
Holistic Assessment: Practitioners conduct a comprehensive evaluation of the patient, considering physical, biochemical, and emotional factors. This may include a detailed health history, physical examination, laboratory tests, and lifestyle assessments.
Spinal Adjustments: Traditional chiropractic adjustments are used to correct misalignments (subluxations) in the spine, which can improve nervous system function and overall health.
Functional Medicine Principles: This involves identifying and addressing underlying imbalances in the body. Functional medicine looks at aspects such as gut health, hormone levels, nutrition, and detoxification pathways to understand the root causes of disease.
Personalized Treatment Plans: Based on the holistic assessment, a customized treatment plan is developed. This plan may include dietary recommendations, nutritional supplements, exercise programs, stress management techniques, and lifestyle modifications in addition to chiropractic adjustments.
Patient Education and Empowerment: Functional chiropractors place a strong emphasis on educating patients about their health and wellness. They empower patients to take an active role in their healing process through lifestyle changes and preventive measures.
Integration with Other Healthcare Providers: Functional chiropractors often work collaboratively with other healthcare professionals, such as primary care physicians, nutritionists, and physical therapists, to provide comprehensive care.
Focus on Prevention: Preventive care is a key component, aiming to optimize health and prevent the onset of chronic diseases by maintaining proper alignment, reducing inflammation, and supporting the body’s natural healing processes.
About Your Presenter
“For hundreds of years and countless centuries herbal medicine has been an important part of the practice of traditional healthcare as well as massage and manual therapy. During the 1970's I had the great privilege of training with physicians and therapists who went to school or practiced during the late 1800's and early 1900's. A common denominator among them all was their use of herbal medicines for the treatment of their patients. Over the last 50 years of my teaching career, I have been bringing this knowledge to my students and teaching them about the value and benefits of herbal medicines and preparations, whether used internally or externally.”
The Blue Heron Academy of Healing Arts and Sciences mission is to build a healing community founded on unity, diversity, and racial harmony. Our mission is to cultivate a nurturing and inclusive community where every individual feels valued, respected, and empowered. We are dedicated to fostering unity and racial harmony by promoting understanding, compassion, and mutual support among all members of our diverse society. Through active engagement, individual and community service, education, and collaborative efforts, we strive to create an environment where healing and growth are possible for everyone. Together, we aim to break down barriers, celebrate our differences, and build a foundation of trust and solidarity, ensuring a brighter, more equitable future for all.
"Building a Healing Community" is a visionary 55-year initiative dedicated to uniting people of all backgrounds and races through the transformative power of holistic and alternative healing arts. This endeavor aims to create a space where diverse healing traditions converge, fostering understanding, compassion, and mutual respect among individuals and communities. By embracing practices such as herbal medicine, yoga, meditation, massage, and other integrative approaches, the initiative seeks to break down barriers and promote a sense of shared purpose in the pursuit of health and wellbeing. Through collective healing, education, and cultural exchange, "Building a Healing Community" aspires to cultivate a more inclusive, connected, and compassionate world, where everyone can experience the profound benefits of holistic wellness.

Building a Healing Community is the practice of bringing people together in an environment of compassion, knowledge, and shared purpose. It recognizes that healing is created through connection among caregivers, families, patients, and professionals. A healing community provides comfort, learning, and support so that every person feels valued and understood.
Unconditional service means offering care freely without expectation of reward. It is an expression of humility and generosity that places the needs of others at the center. When service is given with sincerity, the caregiver becomes a source of safety and comfort.
Individuals living with dementia are often vulnerable and uncertain.
Unconditional service provides stability and reassurance during moments of confusion. Slow movement, a soft voice, and gentle touch help the patient feel protected and reduce fear and agitation.
A healing community is grounded in empathy and dignity. It encourages gentle communication, patient listening, and thoughtful care. When people feel respected and safe, they relax into the healing process and simple acts of kindness contribute to emotional, physical, and spiritual wellbeing.
The mission is to unite scientific understanding with the human qualities that give care its meaning. It aims to educate caregivers and professionals while strengthening families and supporting patients. This mission encourages service that is both knowledgeable and compassionate.
A healing community grows when kindness becomes the guiding principle of daily life. Each person contributes through thoughtful actions, consistent care, and a willingness to help others. When compassion is practiced regularly, the community becomes a safe place where healing can occur naturally.
When caregivers, families, and professionals unite around a shared purpose, their actions become aligned and harmonious. Shared purpose creates resilience and trust. Healing becomes more meaningful when everyone works together with the intention to comfort and support.
Healing is a journey that no one walks alone. Each compassionate action and moment of understanding strengthens the path ahead. Building a healing community reminds us that care offered with love has the power to bring comfort, peace, and hope.

Spiritual well-being provides meaning, identity, and emotional comfort. Even when memory fades, many individuals maintain deep spiritual awareness. Supporting spiritual life reduces fear, quiets agitation, and strengthens inner peace.
Spiritual practices calm the nervous system and help regulate emotions. Familiar prayers, sacred words, chants, or melodies often remain accessible long after other memories fade. These patterns bring comfort and orientation to the patient.
People with dementia come from diverse religious and cultural backgrounds. Spiritual support honors traditions across faiths and cultures. The purpose is not persuasion but connection, dignity, and emotional peace.
Caregivers can read meaningful passages, play sacred music, offer gentle touch, or sit quietly with the patient. Familiar spiritual objects or images can provide grounding. The goal is to nourish the patient’s inner life with sensitivity and respect.
Human connection is a powerful form of medicine. Social engagement protects against confusion, depression, and rapid decline. Even brief interactions can stabilize mood and support a sense of belonging.
Social interaction stimulates emotional and cognitive centers of the brain. It reduces loneliness and promotes healthier sleep cycles. Shared activities encourage connection and help maintain memory pathways.
Successful socialization requires calm, predictable environments. Small groups, soft voices, and familiar people work best. Comfort and reassurance are essential for positive interactions.
Spiritual practices and social engagement complement one another. Group singing, shared readings, prayer, meditation, or simple acts of kindness strengthen emotional comfort and deepen connection.
The caregiver’s voice, breath, and compassion create safety for the patient. Consistent spiritual cues and gentle companionship help the patient experience comfort and belonging despite cognitive changes.
Supporting spiritual well-being and socialization is essential to whole-person dementia care. These practices honor dignity, reduce suffering, and bring peace to patients and caregivers alike.
Dementia is a clinical syndrome that affects memory, judgment, communication, and daily functioning. It results from progressive injury to brain tissue rather than normal aging.
Understanding the underlying cause is essential for effective care.
• Decline in at least two cognitive domains
• Interferes with independence and daily functioning
• Not a normal part of aging
• Caused by brain injury, degeneration, or vascular compromise

Dementia describes a pattern of symptoms, not a diagnosis by itself. Many different diseases can cause dementia, each with distinct pathology and clinical behavior. Treatment must be tailored to the underlying mechanism.
• Multiple diseases can produce the same outward signs
• Different mechanisms require different clinical strategies
• Overlaps between diseases are common
• Mixed presentations increase with age
The most common causes are Alzheimer’s pathology and vascular disease, but many other conditions mimic or overlap with them. Identifying the origin helps families understand the progression and care priorities.
• Alzheimer’s disease
• Small vessel and large vessel vascular disease
• Lewy body disease
• Frontotemporal degeneration
• Parkinson’s-related cognitive decline
Alzheimer’s disease involves changes in memory-related regions of the brain, including amyloid plaques, tau tangles, loss of synapses, and shrinkage of the hippocampus. These changes disrupt communication between neurons.
• Early impairment in forming new memories
• Disorientation and spatial difficulty
• Gradual steady decline
• Increased neuroinflammation and metabolic stress
Vascular dementia results from impaired blood flow and repeated small injuries to brain tissue. This disrupts the white matter pathways that connect different regions of the brain.
• Slowed thinking and planning
• Gait problems early in the disease
• Mood shifts and executive dysfunction
• Stepwise or fluctuating decline
Alzheimer’s often begins with memory loss, while small vessel disease begins with slowed processing and gait instability.
Recognizing the pattern helps predict care needs and progression.
• Alzheimer’s: memory and language affected early
• Small vessel: planning, attention, and mobility affected early
• Alzheimer’s: steady progression
• Small vessel: stepwise changes after small strokes
Most adults over age 70 do not have a single type of dementia. Instead, they show a combination of Alzheimer’s pathology and vascular injury. Treating both pathways improves quality of life.
• Memory loss + slowed thinking is common
• Vascular disease accelerates Alzheimer's progression
• Inflammation links both conditions
• Lifestyle changes benefit all mixed presentations

Chronic inflammation, insulin resistance, poor sleep, stress, and reduced blood flow all increase brain vulnerability. These factors influence speed of decline and responsiveness to holistic care.
• High glucose and insulin resistance damage neurons
• Poor sleep disrupts waste clearance
• Chronic stress increases neuroinflammation
• Vascular health determines oxygen delivery
Emerging research shows that amyloid plaques may begin as protective structures attempting to sequester harmful substances and inflammatory byproducts.
Over time, this response becomes overwhelmed and contributes to dysfunction.
• Early plaques may reduce toxicity
• Chronic inflammation reduces clearance
• Plaques accumulate faster than the brain can manage
• Result is disruption of communication between neurons
The brain’s response in Alzheimer’s parallels the changes seen in arthritis. In joints, scar tissue forms to stabilize damage but later restricts movement. In the brain, plaques may serve a similar early-purpose before becoming harmful.
• Body’s initial intent is protection
• Chronic inflammation shifts repair into dysfunction
• Explains memory loss and communication problems
• Helps caregivers understand what is happening inside the brain
Comorbid medical conditions strongly influence the progression of dementia. They affect brain oxygenation, inflammation, sleep quality, and daily functioning. Managing these conditions improves stability and slows decline.
• Comorbidities accelerate cognitive loss
• Many contribute to agitation, fatigue, or confusion
• Proper management reduces caregiver burden
• Therapists must adapt treatment based on medical status
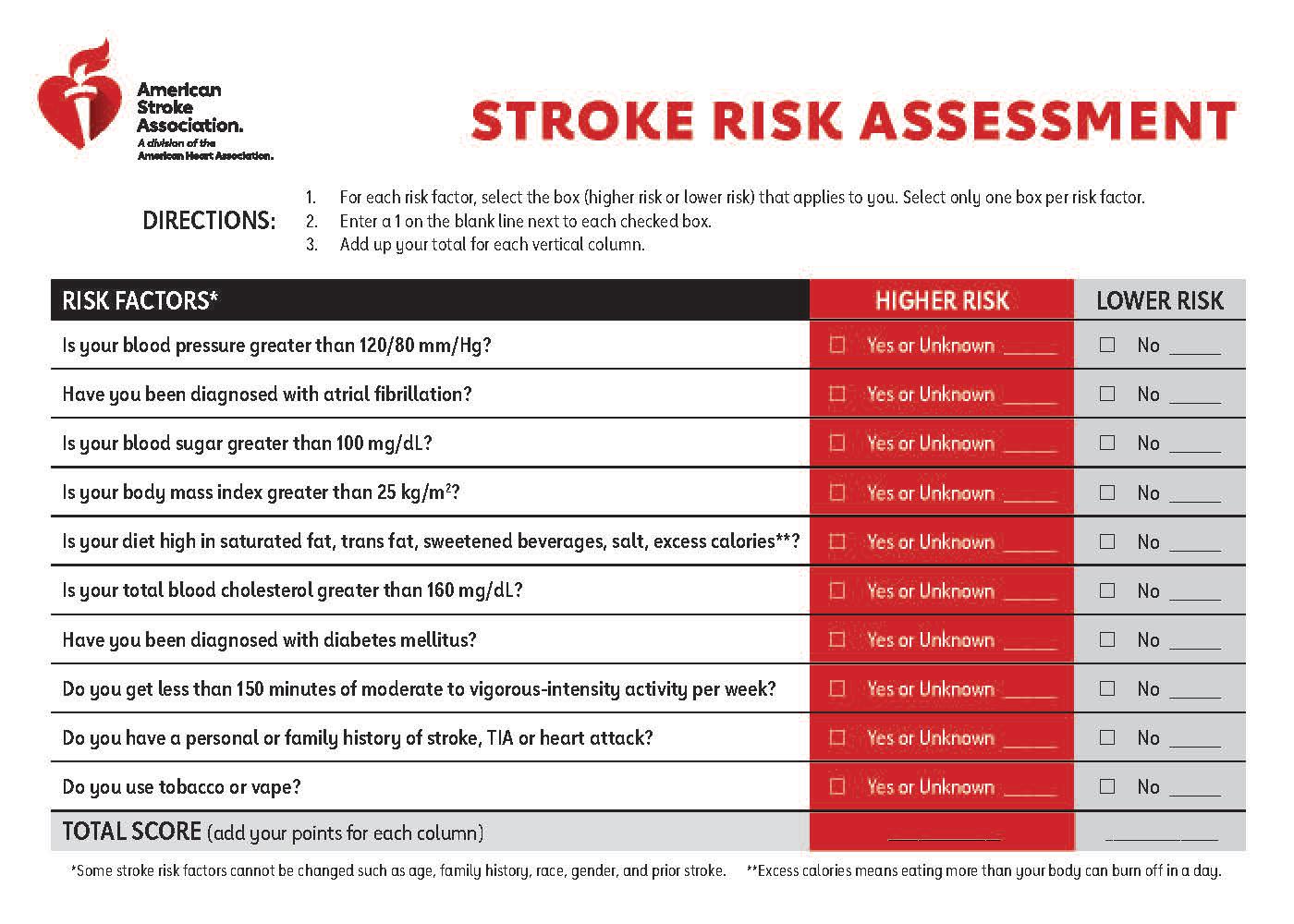
Heart and metabolic health affect the brain’s ability to receive oxygen, glucose, and nutrients. Hypertension, diabetes, and obesity all increase the rate of cognitive decline and worsen day-to-day functioning.
• Hypertension reduces blood flow and damages white matter
• Diabetes contributes to nerve damage and brain insulin resistance
• Atrial fibrillation increases stroke risk
• High lipids accelerate vessel disease and inflammation
Depression, anxiety, and sleep disorders commonly coexist with dementia and often worsen the clinical picture. These conditions contribute to fluctuations in mood, irritability, and confusion. Recognizing them improves overall care.
• Depression may appear as withdrawal or irritability
• Anxiety increases pacing and resistance to care
• Sleep fragmentation worsens agitation and memory issues
• Delirium episodes often follow infection or medication changes
Joint pain, osteoporosis, frailty, and balance problems are frequent in dementia and directly affect safety and mobility. These conditions change how therapists' position, mobilize, and support patients.
• Osteoarthritis increases guarding and agitation
• Osteoporosis raises fracture risk
• History of falls predicts future falls
• Frailty limits treatment time and tolerance
Breathing difficulties, constipation, and urinary problems are common and directly influence behavior, sleep, and physical comfort. These conditions often present as agitation rather than verbal complaints.
• COPD reduces oxygenation and increases fatigue
• Constipation triggers pain and confusion
• GERD causes irritability and nighttime discomfort
• UTIs are a leading cause of sudden behavioral change
Dementia patients often take multiple medications. Many have cognitive side effects, including sedation, confusion, and increased fall risk. Therapists must understand medication effects to modify treatment safely.
• Anticholinergic drugs impair memory
• Sedatives increase instability
• Blood thinners limit deep pressure techniques
• Drug interactions can mimic or worsen dementia symptoms
Hearing and vision loss significantly worsen dementia symptoms. Sensory deprivation increases confusion, social withdrawal, and the risk of misinterpreting the environment. Supporting sensory input improves daily functioning.
• Hearing loss accelerates cognitive decline
• Vision changes increase fall risk
• Sensory impairment heightens agitation
• Enhanced lighting and clear communication reduce confusion
Early dementia often presents with subtle changes that families may overlook.
These include short -term memory lapses, difficulty learning new routines, and slow adaptation to change. Identifying early signs helps guide treatment planning.
• Repeating questions
• Misplacing objects
• Difficulty following multi-step tasks
• Getting lost in familiar areas
Mood instability, irritability, apathy, and increased anxiety are common. These changes reflect impaired regulation of emotion and stress responses rather than personality shifts. Understanding this reduces caregiver frustration.
• Sudden emotional swings
• Withdrawal from social interaction
• Increased fearfulness or suspicion
• Reduced motivation or initiative
Communication challenges include word-finding difficulty, slower speech, and trouble organizing thoughts. These problems increase confusion and resistance during care tasks and require patience and simplified instruction.
• Word retrieval problems
• Difficulty following directions
• Slower thinking and response time
• Trouble planning or sequencing tasks
Motor changes vary by dementia type. Alzheimer’s patients typically show late motor problems, while vascular dementia and small vessel disease show gait issues early. Recognizing these patterns improves safety.
• Shuffling or magnetic gait
• Balance instability
• Slowed fine motor movement
• Increased fall risk
Disrupted sleep-wake cycles are common. Patients may nap during the day, be restless at night, or experience confusion and agitation in the late afternoon. Stabilizing sleep is central to reducing behavioral issues.
• Difficulty falling or staying asleep
• Daytime drowsiness
• Evening agitation or disorientation
• Reversal of sleep patterns
Dementia reduces the ability to filter sensory input. Noise, movement, clutter, and chaotic environments can overwhelm the patient, leading to agitation or withdrawal. Therapists and caregivers must reduce sensory load during care.
• Loud environments increase confusion
• Fast movements cause fear or resistance
• Visual clutter increases stress
• Gentle touch and slow pace improve tolerance
Consistent routines reduce anxiety, stabilize behavior, and provide a sense of safety. Dementia patients depend on predictable patterns because their ability to adapt to change is impaired.
Structured days improve sleep, mood, and participation in care.
• Keep the same timing for meals, hygiene, rest, and activities
• Reduce unexpected changes in environment
• Use simple visual or verbal cues to guide transitions
• Maintain calm, steady pacing throughout the day
This technique helps guide movement, reduce fear, and build cooperation. Placing your hand gently over the patient’s hand provides direction through physical cueing rather than verbal instruction. It is especially helpful during grooming, eating, and mobility tasks.
• Helps the patient start or continue an action
• Reduces frustration when words fail
• Stabilizes tremors or restless hands
• Builds trust through guided touch
A sensory anchor helps the patient settle when anxious or overstimulated. It focuses attention on one calming sensory input, such as warm touch, rhythmic breathing, or gentle pressure. This technique reduces confusion and restores grounding.
• Use warm hands or warm infused oil
• Apply slow, steady palm contact to the shoulder or back
• Match and gradually slow the patient’s breathing
• Maintain quiet, stable surroundings during the anchor
A stable evening rhythm reduces sundowning, improves sleep quality, and decreases nighttime wandering. The goal is to gradually lower stimulation while increasing a sense of calm and predictability before bedtime.
• Dim lights and reduce noise after late afternoon
• Avoid demanding tasks or difficult conversations
• Use warm, calming touch or gentle foot and hand work
• Keep bedtime consistent every night
Sundowning often begins subtly. Early detection allows caregivers to intervene before agitation escalates. These early signs reflect fatigue, sensory overload, or unstable circadian rhythms.
• Restlessness or pacing in late afternoon
• Increased confusion or difficulty following instructions
• Irritability, fear, or clinginess
• Visual misinterpretations as light decreases

Too much sensory input causes overwhelming sensations. Patients may react with agitation, withdrawal, or sudden emotional shifts. Recognizing overstimulation allows caregivers to adjust the environment before behavior escalates.
• Covering ears or closing eyes
• Startle responses to touch or noise
• Rapid breathing or tension in the shoulders
• Increased wandering or abrupt emotional reactions
Subtle body signals indicate instability or risk of falling. Therapists and caregivers must watch for these cues to prevent injury during transfers, walking, or standing.
• Swaying or leaning while standing
• Slow reaction to balance loss
• Stiff or shuffling gait
• Reaching for walls or furniture
Simple, clear communication reduces frustration and improves cooperation.
Patients respond best to calm tone, short sentences, and generous time to process information. Avoid arguing or correcting.
• Speak slowly and use short phrases
• Ask one question at a time
• Present choices instead of commands
• Pause long enough for the patient to respond
Manual therapy for dementia focuses on comfort, stabilization, circulation, and calming the nervous system. The goal is not to treat the disease but to improve quality of life, reduce agitation, and support safer daily function.
• Improve circulation and tissue comfort
• Reduce tension, anxiety, and restlessness
• Support safe movement, gait, and transfers
• Enhance sleep and relaxation
Grounding techniques help patients feel oriented and safe. Slow touch initiation avoids startling or overwhelming the patient and builds trust. Anchoring contact reduces wandering attention and stabilizes mood.
• Begin with slow, visible approach
• Use sustained palm contact on shoulder or upper back
• Let the patient feel your presence before adding movement
• Slow, rhythmic pacing reduces confusion
Many patients have balance issues, frailty, or difficulty transitioning between positions. Proper support during transfers and body positioning prevents injury and improves comfort during treatment.
• Support the trunk and pelvis during transfers
• Avoid sudden changes in head or neck position
• Keep treatments semi-reclined if breathing issues occur
• Ensure feet are grounded when seated or standing
Frailty limits the intensity and duration of treatment. Gentle oscillation, light stretching, and low-load soft tissue methods are more effective and safer than forceful techniques.
• Shorter sessions may be better tolerated
• Use gentle mobilization instead of deep pressure
• Monitor breathing, fatigue, and facial expressions
• Allow frequent rest breaks
Slow joint mobilization, light myofascial work, and rhythmic movement can support balance, gait, and coordination. These techniques also reduce stiffness and improve comfort during ambulation.
• Slow, graded range-of-motion work
• Gentle mobilization of ankles, hips, and thoracic spine
• Rhythmic rocking to reduce rigidity
• Improve proprioceptive awareness and postural control
Pain is often underreported in dementia. Patients communicate discomfort through behavior rather than words.
Manual therapy can reduce pain responses and help calm the nervous system.
• Look for nonverbal pain cues
• Use warm infused oils for comfort
• Apply gentle positional release or nerve glides
• Reduce tension patterns that worsen agitation
Dementia often disrupts autonomic regulation. Manual therapy can help shift the patient toward a calmer, more parasympathetic state, improving digestion, sleep, and emotional stability.
• Slow diaphragmatic pacing
• Gentle rib and thoracic cage work
• Head, face, and cervical soft tissue calming techniques
• Reduce sympathetic overdrive from fear or confusion
Certain herbs and nutritional factors help calm agitation, improve sleep, and stabilize the nervous system. These supports should complement manual therapy and be matched to the patient’s specific needs.
• Skullcap, passionflower, and chamomile for calming
• Kava and valerian for stronger sedation
• L-theanine, magnesium, and glycine for relaxation
• Avoid stimulants and excess sugar that increase agitation
Low-dose cannabinoid blends may support relaxation, reduce anxiety, and improve sleep when combined with nervine herbs. Care must be taken with dosing, timing, and patient sensitivity.
• Start with hemp-derived, low-THC (1.25 mg.) products
• Combine with calming herbs to reduce dose needs
• Use in evening to improve sleep stability
• Monitor for drowsiness, imbalance, or interaction effects

Clinical decisions should reflect the patient’s comorbidities, mobility status, sensory needs, and environmental factors. Working from real examples helps therapists adapt techniques safely and effectively.
• Modify based on cardiovascular or pulmonary status
• Adjust pacing for sensory sensitivity
• Use safe positioning with frail or unstable patients
• Involve caregivers when transferring or mobilizing
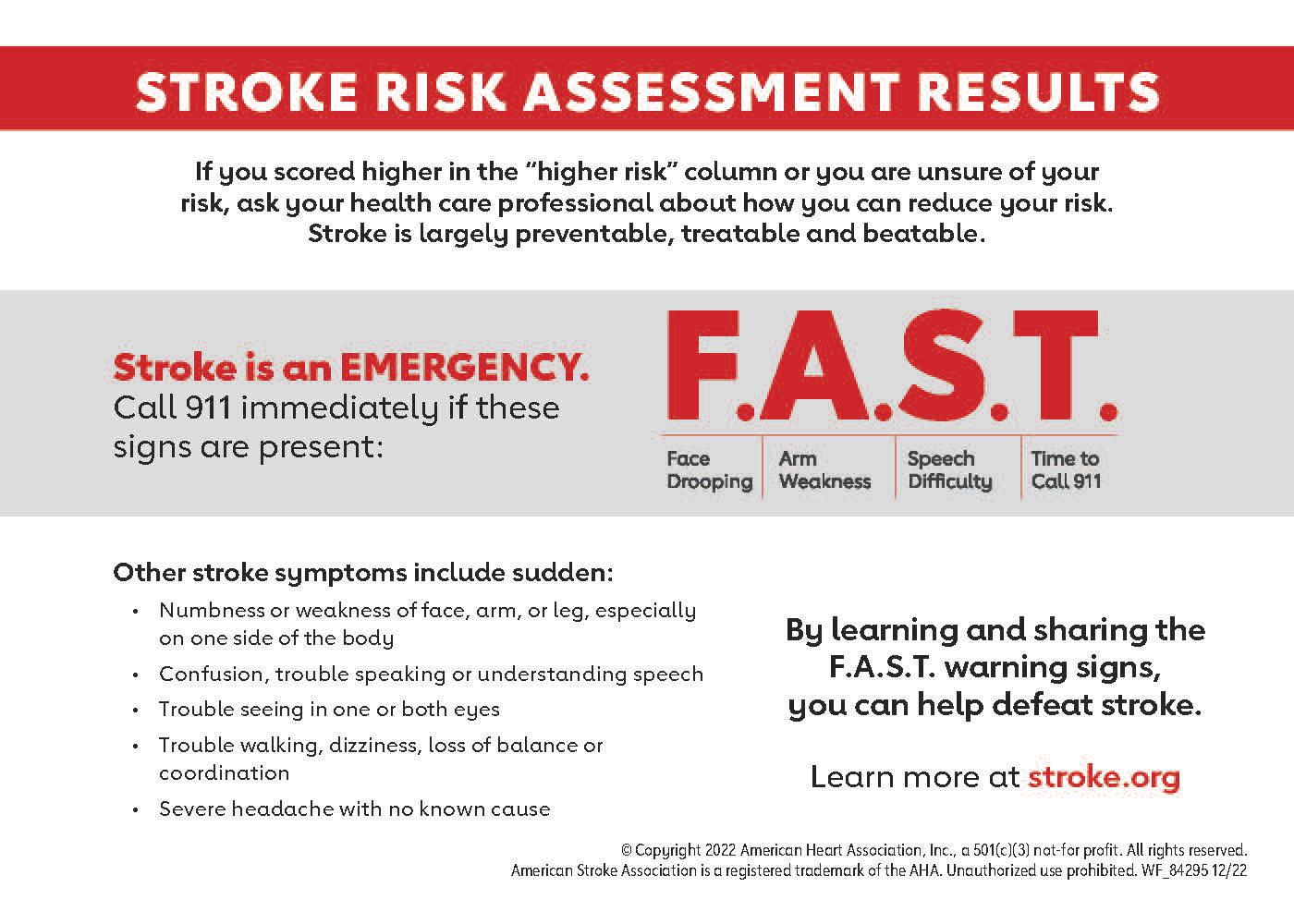
Certain sudden or severe symptoms in a patient with dementia require immediate medical evaluation. These changes often signal infection, stroke, cardiac issues, or acute metabolic imbalance. Early recognition prevents life-threatening complications.
• Abrupt confusion or sudden mental status change
• New weakness, slurred speech, or facial droop
• Severe shortness of breath or chest discomfort
• High fever, repeated vomiting, or signs of dehydration
A sudden shift in behavior, agitation, or personality may be the first indicator of medical distress in dementia. Behavioral symptoms often appear before physical symptoms because the brain cannot interpret discomfort normally.
• Abrupt agitation, fear, or aggression
• Rapid withdrawal or refusal of care
• Sudden hallucinations or intense confusion
• Marked change from the patient’s usual baseline
Pain can be difficult for dementia patients to report verbally. Mobility changes often highlight underlying injury, infection, or fracture. Therapists must recognize these signs quickly and halt treatment until medically evaluated.
• New limping, guarding, or reluctance to move
• Warm, swollen, or painful limb
• Inability to bear weight
• New nighttime crying or sudden pain behaviors
Therapists must stop treatment immediately if the patient becomes unstable, distressed, or medically compromised. Safety takes priority over treatment goals. When in doubt, pause and reassess the situation.
• Sudden pallor, sweating, or dizziness
• Sharp pain or difficulty breathing
• Escalating fear, agitation, or confusion
• Signs of cardiovascular or respiratory distress
Certain clinical situations require emergency medical attention. These conditions may indicate stroke, heart problems, infection, or dangerous dehydration. Delaying care increases risk.
• Stroke signs such as facial droop or slurred speech
• Severe chest discomfort or rapid heartbeat
• Very low fluid intake with confusion or dry mouth
• Warm, swollen, painful leg suggesting possible DVT
Some concerns do not require emergency care but do need prompt evaluation by a primary care provider, neurologist, or specialist. Early referral ensures proper management and reduces long-term complications.
• Gradual mobility decline or increased falls
• Persistent anxiety, sleep problems, or depression
• Recurrent UTIs or suspected untreated pain
• Increasing caregiver burnout or inability to keep the home safe
Daily routines that support calm, safety, and predictability help stabilize dementia symptoms. Caregivers benefit from simple, repeatable practices that reduce stress and provide gentle structure. These steps improve cooperation and reduce behavioral escalation.
• Keep routines steady from morning to evening
• Reduce noise, clutter, and unnecessary stimulation
• Use clear, simple instructions
• Allow extra time for every task to prevent rushing
The environment has a powerful impact on behavior and orientation. A stable, organized, low-stress home reduces agitation and supports safer mobility.
Thoughtful adjustments can significantly improve comfort and reduce caregiver burden.
• Improve lighting to reduce visual misinterpretation
• Maintain clear paths for safe walking
• Use contrasting colors for important objects
• Create quiet spaces for rest and calming
Therapists help coordinate care by observing changes, guiding caregivers, and supporting the patient’s physical and emotional stability. Consistent therapeutic contact can reduce restlessness, improve comfort, and strengthen the caregiver’s confidence.
• Teach caregivers grounding and calming techniques
• Monitor for red flags or sudden changes
• Support safer movement and transfers
• Provide feedback to family and healthcare providers
Dementia care requires understanding pathology, recognizing comorbidities, applying calming techniques, and ensuring safety. Integrating manual therapy with caregiver guidance creates a supportive, stable environment that benefits both patient and family.
• Use predictable routines and clear communication
• Support sensory grounding and gentle mobilization
• Adjust treatment for medical and behavioral changes
• Focus on comfort, safety, and emotional stability
Before dementia or Alzheimer’s disease becomes visible on CT or MRI, the process begins as a subtle but progressive biochemical disorder. This stage often develops years or even decades before structural brain changes emerge.
Biochemical dementia refers to the early metabolic and neurochemical imbalances that precede physical degeneration. These include:
• impaired glucose utilization in the brain
• insulin resistance within neural tissue
• mitochondrial dysfunction
• chronic inflammation
• oxidative stress
• disrupted neurotransmitter balance
• microvascular insufficiency
• altered sleep and circadian chemistry
These biochemical disturbances produce the earliest symptoms of cognitive decline:
• mild memory lapses
• increasing distractibility
• stress intolerance
• sleep disruption
• mood changes
• sugar cravings
• early agitation and fatigue
In this view, dementia does not begin as a structural disease but as a metabolic and biochemical collapse of the brain’s regulatory systems. Addressing this stage early through nutrition, herbal medicine, lifestyle correction, and targeted brain support may slow progression long before standard imaging can detect pathology.
I recommend a body system-by-system approach to patient evaluation and assessment based upon observation, palpation, and questioning. Dr. Lawton
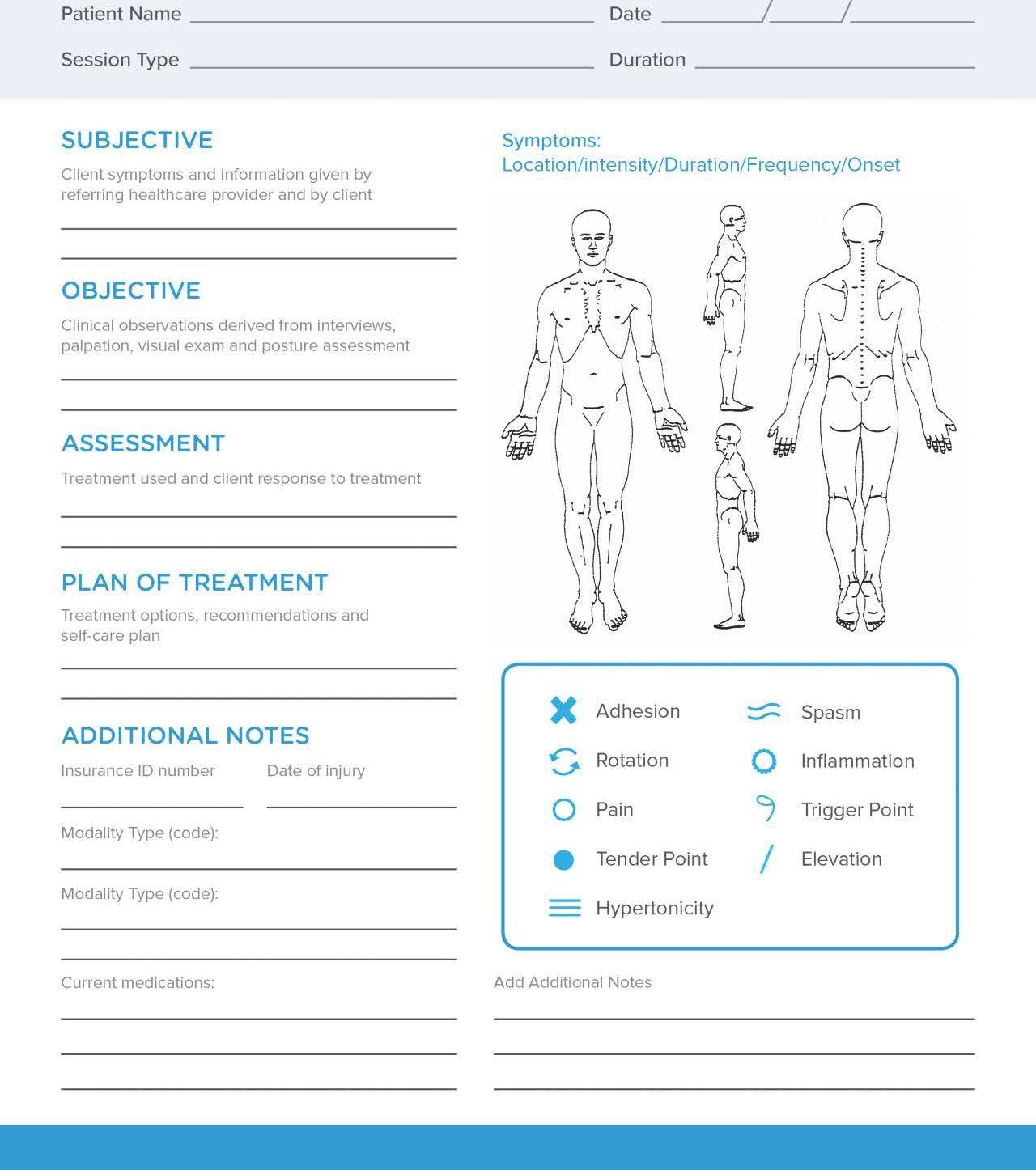
SOAP notes provide a structured format for documenting patient progress and treatment.
SOAP stands for: S (Subjective): Patient’s reported symptoms, concerns, and goals. O (Objective): Measurable findings, including range of motion (ROM), muscle tone, swelling, and postural analysis. A (Assessment): Therapist’s professional analysis of the patient’s condition, progress, and response to treatment. P (Plan): Treatment strategy, including future sessions, exercises, and patient self-care recommendations.
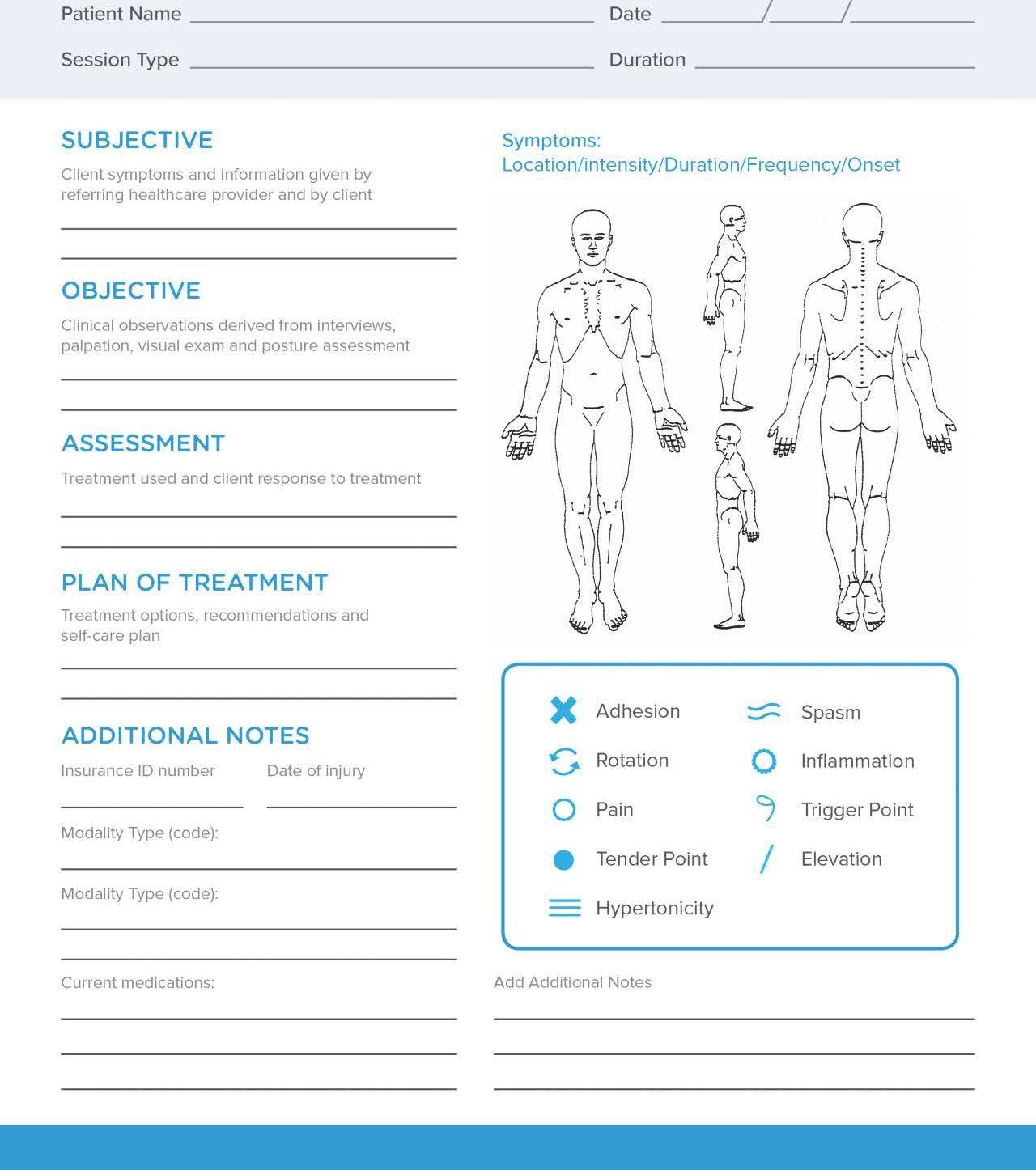
S: Patient presents with increased confusion, restlessness, and difficulty initiating movement in the right arm during grooming and dressing. Caregiver reports the patient has been more anxious in the evenings and is waking twice nightly. Patient expresses discomfort in the shoulder but is unable to quantify the intensity. Caregiver estimates discomfort at a mild to moderate level based on facial tension and protective movements.
O: Guarding noted in the right shoulder during passive movement. Mild rigidity with slow initiation of motion. PROM limited to approximately 50 percent of normal range in shoulder abduction and external rotation. Increased sensitivity to touch during fast or unexpected movements. Responds positively to slow palm contact, rhythmic rocking, and gentle warm infused oil application.
A: Limited ROM and increased tension contributing to difficulty with dressing, grooming, and transfers. Sensory overload and evening agitation consistent with early sundowning. Patient demonstrates reduced motor planning and hesitancy during movement initiation. Good calming response to slow, grounding techniques and myofascial release. Treatment well tolerated.
P: Continue weekly dementia-focused manual therapy emphasizing slow, rhythmic mobilization, gentle myofascial release, and sensory grounding. Incorporate guided movement sequencing and hand-over-hand initiation to support ADLs. Caregiver instructed in evening calming routine, warm shoulder compresses, and simple guided breathing. Plan to reassess ROM, agitation patterns, and sleep quality at next visit.
ROM: Range of Motion
MMT: Manual Muscle Testing
P/AROM: Passive/Active Range of Motion
B/L: Bilateral
Tx: Treatment
F/U: Follow-Up
Dr: Doctor
Sd: Said
Dx: Diagnosis
CNS: Central Nervous System
PNS: Peripheral Nervous System
Sp: Spasticity
TTP: Tender to Palpation
Lat: Lateral
Pt: Patient
Dr sd pt HA = Doctor said patient has headaches.
Dr sd pt LBP = Doctor said patient has low back pain (L5/S1).
Pt sd dr sd LBP = Patient said doctor said they have low back pain (L5/SI)
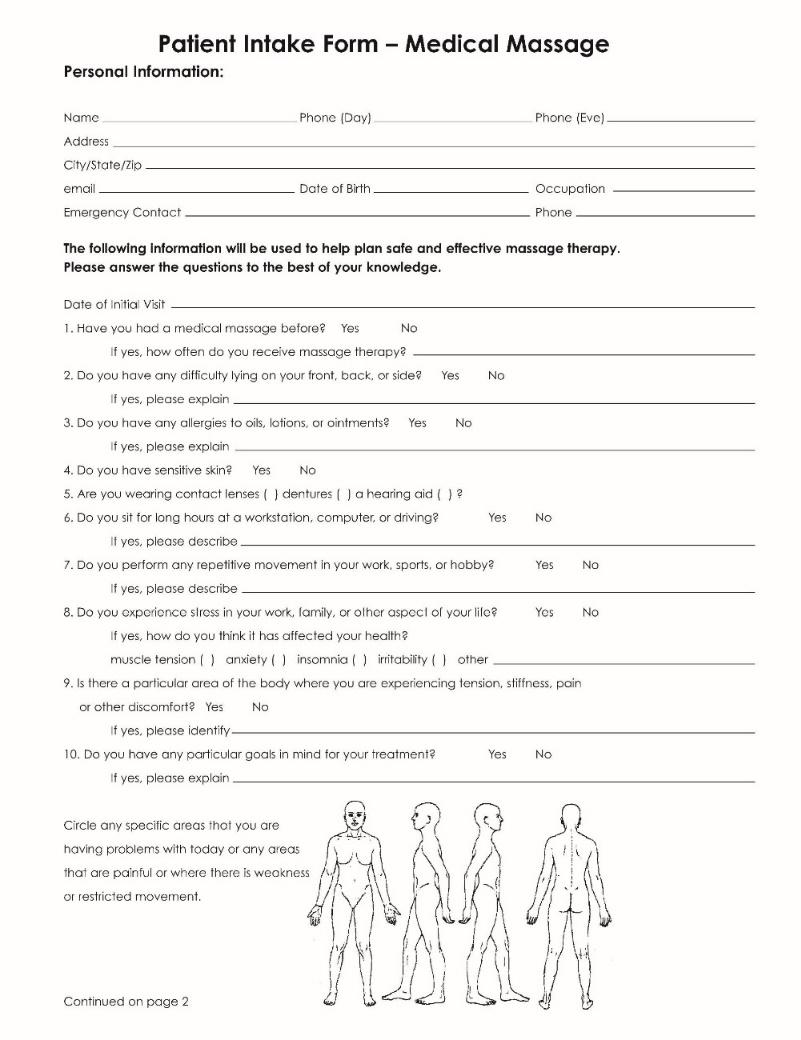
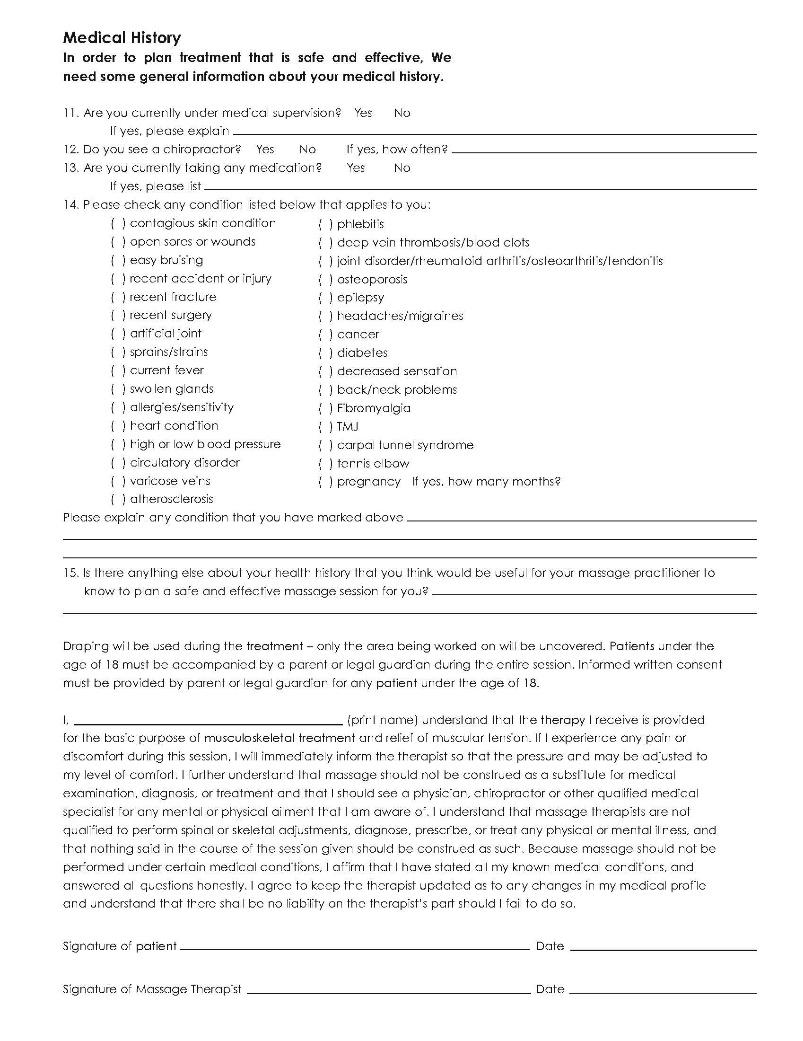
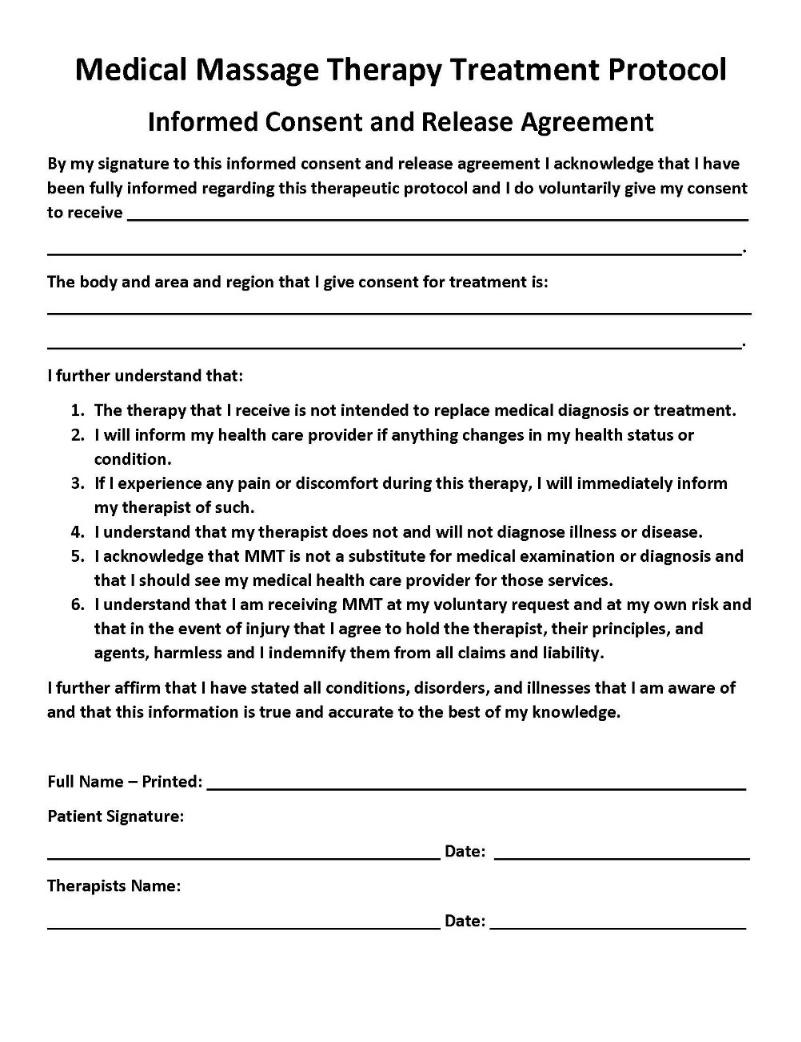
Patient Intake

The Alzheimer’s Association®, the leading voluntary health organization in Alzheimer’s care, support and research, is dedicated to driving early detection and diagnosis of dementia. To help, the Association has created an easy-to-implement process to assess cognition during the Medicare Annual Wellness Visit. Developed by a group of clinical dementia experts, the recommended process outlined on Page 4 allows you to efficiently identify patients with probable cognitive impairment while giving you the flexibility to choose a cognitive assessment tool that works best for you and your patients.
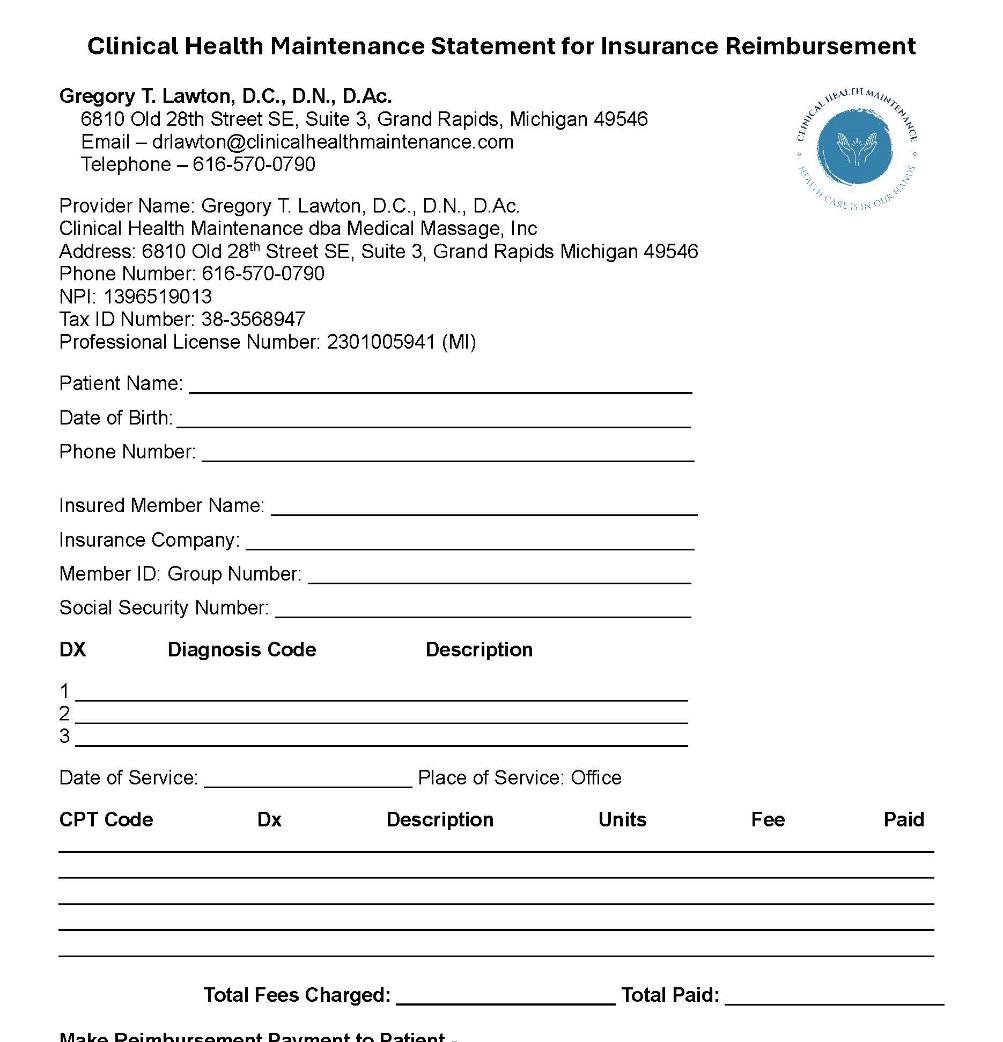
There are two main requirements for medical insurance billing:
A medical necessity for patient care (a diagnosis).
Documentation of ongoing improvement and clinical results.
If these two conditions are not met, medical insurance providers will not cover claims.
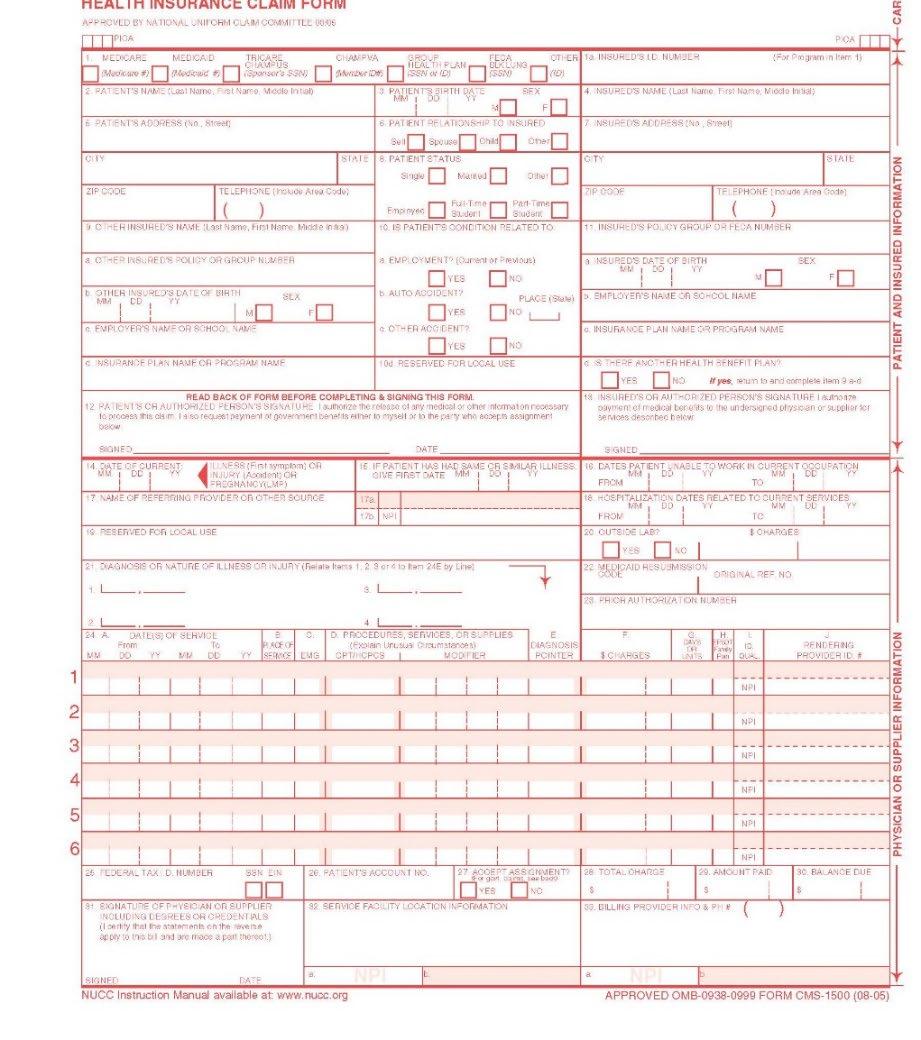
97124: Therapeutic procedure, one or more areas, each 15 minutes; massage, including effleurage, petrissage, and/or tapotement (stroking, compression, percussion).
97140: Manual therapy techniques (e.g., mobilization/manipulation, manual lymphatic drainage, manual traction), one or more regions, each 15 minutes.

Remember to cite the exact treatment procedures in your claim to ensure coverage.
Additionally, avoid citing both CPT codes 97124 and 97140 without modifier code 59, which indicates distinct and different procedures performed on the same individual within a single day or across a few days.
CPT Code 97112: Neuromuscular Reeducation
CPT Codes 97010: Hot/Cold Packs
CPT Codes 97110: Therapeutic Exercise

Remember to cite the exact treatment procedures in your claim to ensure coverage.
Additionally, avoid citing both CPT codes 97124 and 97140 without modifier code 59, which indicates distinct and different procedures performed on the same individual within a single day or across a few days.
CPT Code 97112: Neuromuscular Reeducation
CPT Codes 97010: Hot/Cold Packs
CPT Codes 97110: Therapeutic Exercise

Neuroplasticity is the brain’s ability to reorganize and form new neural connections throughout life, particularly following an injury such as a stroke. This adaptive process allows the brain to compensate for lost functions by rewiring undamaged neurons to take over the roles of affected areas. Neuroplasticity plays a crucial role in dementia, influencing motor function, cognitive abilities, and sensory processing. Rehabilitation strategies such as repetitive movement training, sensory stimulation, and mindfulness practices enhance neuroplasticity, helping patients maintain abilities or regain lost abilities over time. Nutritional support, herbal medicine, and manual therapies can further optimize the neuroplastic response, promoting long-term neurological healing and functional improvement.
Neuroplasticity is the brain’s ability to reorganize and form new neural connections throughout life, particularly following an injury such as a stroke.

More important than a patient’s condition is understanding who they are. A patient’s pre-existing health, lifestyle, diet, drug use and emotional resilience significantly influence their recovery journey. An active and independent individual with strong social support may experience a different recovery process than someone managing chronic illnesses, high stress, or social isolation. Factors such as cognitive and emotional well-being, support systems, and lifestyle choices before cognitive decline and dementia shape the rehabilitation process. Acknowledging these aspects allows therapists to provide tailored, patient-centered care that is both effective and compassionate.
Consider this:
What were the pre-existing conditions prior to the diagnosis?
Was the patient obese?
Did the patient have diabetes, heart disease, or high blood pressure?
Was the patient an alcoholic or did they have a drug problem?
A whole-person approach to dementia care combines manual therapy, herbal support, nervous system regulation, sensory grounding, and anti-inflammatory nutrition. These strategies help stabilize behavior, reduce agitation, and support clearer daily functioning.
• Reduce neuroinflammation through diet and herbal support
• Strengthen vascular health and blood flow to the brain
• Support sleep stability and daily rhythm
• Protect cognitive function through holistic care
A diagnosis of dementia is proof positive of living a lifestyle and following a diet that is destructive to the brain and nervous system. A healthy diet rarely results in dementia, brain atrophy, and neuron death. You do not catch dementia like a cold or flu, you construct it day by day with unhealthy behavior and eating habits.
Herbal therapies and nutritional strategies can calm the nervous system, reduce agitation, support memory, and improve overall brain resilience. Specific herbs help regulate mood, reduce inflammation, and provide neuroprotective benefits.
• Sage enhances cognitive function and neurotransmitter activity
• Skullcap calms anxiety and reduces sensory overload
• Blue vervain supports emotional stability
• Turmeric reduces inflammation and supports neuroprotection
• Polyphenol-rich foods improve vascular and brain health
These herbs help reduce agitation, support sleep, improve memory, and calm the autonomic nervous system.
• Sage improves cognition and supports memory pathways
• Skullcap reduces anxiety and supports relaxation
• Turmeric reduces neuroinflammation and oxidative stress
• Blue vervain relieves muscle tension and emotional stress
• Bioflavonoids support microvascular and capillary health
Nervine herbs help regulate the nervous system, reduce nighttime agitation, and improve sleep quality, common challenges in dementia care.
• Chamomile for gentle relaxation
• Passionflower for evening calming
• Kava for stronger anxiety relief when appropriate
• Lemon balm for mood stabilization
• Dosing tailored to individual reactivity
Nutrition plays a powerful role in brain function, inflammation, and behavior.
Reducing metabolic stress improves clarity, mood, and sleep.
• Omega-3 fatty acids for neuroprotection
• Polyphenols for vascular and antioxidant support
• Hydration for cognitive stability
• Avoid refined sugars to prevent agitation
• Reduce inflammatory oils and processed foods
Certain fats and processed foods increase inflammation, worsen blood sugar stability, and accelerate cognitive decline.
• Avoid vegetable oils (canola, soybean, corn)
• Avoid trans fats and hydrogenated oils
• Limit refined sugars and high-fructose corn syrup
• Reduce artificial sweeteners
• Minimize processed meats and fried foods
Healthy oils support vascular flow, reduce inflammation, and enhance neuronal resilience.
• Extra virgin olive oil: ideal daily oil
• Flaxseed oil: strong omega-3 support
• Walnut oil: balanced polyunsaturated profile
• Avocado oil: anti-inflammatory and stable for cooking
Extra virgin olive oil supports brain function through monounsaturated fats, polyphenols, and antioxidants that protect neurons and improve vascular flow.
• Enhances endothelial function
• Reduces oxidative stress
• Supports memory and cognition
• Stabilizes metabolic health
Flax seed oil provides ALA, a precursor to EPA and DHA, and is protective against inflammation and oxidative stress in the brain.
• Reduces neuroinflammation
• Supports neuronal repair processes
• Improves lipid balance
• Best used cold in food or smoothies
These oils support circulation, neuronal protection, and metabolic stability.
• Walnut oil for antioxidant and polyphenol benefits
• Avocado oil for cognitive support and stable cooking applications
• Both improve vascular flow to the brain
Polyphenols from plant foods protect neurons and support vascular health.
• Green tea catechins
• Blueberries and dark berries
• Pomegranate
• Dark chocolate in moderation
A supportive diet for dementia focuses on whole foods, stable glucose, vascular protection, and reducing inflammation.
• Mediterranean, Ornish, and Pritikin models
• Whole grains, legumes, vegetables, fruit
• Low fat, low sugar
• Minimize inflammatory foods
• Hydration supports cognitive stability
Certain nutraceuticals support neuronal health, improve energy metabolism, and reduce inflammation. These supplements offer targeted support for memory, attention, and nerve repair by addressing metabolic and vascular contributors to cognitive decline.
• Benfotiamine for glucose metabolism
• Methylcobalamin (B12) for nerve repair
• Activated B-complex for energy pathways
• Methyl folate for homocysteine control
• Omega-3s for neuronal membrane health
Benfotiamine is a fat-soluble form of thiamine that supports glucose metabolism in the brain and reduces advanced glycation end-products, which accelerate cognitive decline.
• Protects neurons from glucose toxicity
• Supports nerve healing
• Reduces inflammation and oxidative stress
• Helps stabilize cellular energy production
Methylcobalamin is the neurologically active form of vitamin B12 that supports myelin repair, nerve conduction, and cognitive clarity.
• Improves nerve regeneration
• Supports memory and focus
• Corrects deficiency-related cognitive symptoms
• Essential for methylation and neurotransmitter balance
An activated B-complex provides the brain with essential cofactors for energy metabolism, neurotransmitter synthesis, and stress resilience.
• Supports mitochondrial function
• Enhances mental clarity
• Improves stress tolerance
• Assists sleep-wake regulation
Methyl folate supports healthy methylation, reduces homocysteine, and enhances neurotransmitter synthesis, improving mood and cognitive stability.
• Reduces neuroinflammation
• Supports neurotransmitter production
• Protects vascular integrity
• Helps regulate emotional resilience

Omega-3 fatty acids DHA and EPA support brain structure, neuronal communication, and anti-inflammatory pathways.
• Improves memory and attention
• Supports vascular flow
• Reduces neuroinflammation
• Essential for neuronal membrane integrity
CoQ10 and PQQ support cellular energy production and mitochondrial repair, which decline with age and affect cognitive resilience.
• Boost ATP production
• Protect neurons from oxidative stress
• Support mitochondrial biogenesis
• Improve mental stamina
ALA is a potent antioxidant that improves glucose metabolism and reduces oxidative stress linked to cognitive decline.
• Enhances insulin sensitivity
• Protects neurons
• Supports metabolic flexibility
• May slow progression
Magnesium L-threonate crosses the blood-brain barrier and supports synaptic plasticity, sleep quality, and cognitive function.
• Improves memory formation
• Supports deep sleep
• Calms the nervous system
• Enhances neuroplasticity
NAC increases glutathione levels, reduces neuroinflammation, and supports detoxification pathways relevant to cognitive decline.
• Protects neurons
• Reduces inflammation
• Supports respiratory health
• May improve mood and drive
Herb infused oils are prepared by selecting an herb or herbal blend and then cutting or grinding the dried plant material to a size and consistency that allows the oil to permeate the herbal material and to draw out and dissolve the chemical constituents into solution. In the “long” method the mixture is allowed to sit in a cool dark place for up to 8 weeks. In the “fast” method or what is called the “alcohol intermediary method”, the dried plant material is cut or ground into an acceptable size and soaked in a very small amount of alcohol for 24 hours and then it is soaked in a carrier oil for 24 to 48 hours and finally strained. During the 24-to-48-hour period the mixture is warmed to a temperature of 110-degrees Fahrenheit. When the appearance of the solution is appropriate for the herb or herbs being infused, the solution is strained. The remaining mixture of herbs may be used for other purposes.
An herb-infused oil, also known as a macerated oil, consists of a carrier oil that has been permeated (“infused” or “macerated”) with one or more herbs. The benefit of using an infused oil is that it combines the properties of both the carrier oil and the herbs. Unlike essential oils, which are highly concentrated extracts, infused oils are gentler and less concentrated. They capture the whole essence of the herb and can be used for various purposes, from skincare to cooking. For example, on average an essential oil only captures 4 or 5 percent of the chemical constituents in an herb, whereas an herbinfused oil will extract over 90 percent of the herbal constituents.
For the fast or alcohol intermediary method of extraction heat is used to speed up the process. There are several ways in which heat is used:
Warm Infusion: Heat the oil and herbs gently on the stovetop.
Solar Infusion: Place the herbs in a jar with oil and let it sit in a sunny window for 4-6 weeks.
Stovetop Infusion: Simmer the herbs and oil together.
Oven Infusion: Use low heat in the oven to infuse the oil.
Yogurt Maker: Place the mixture into jars and into a yogurt maker at 110 degrees Fahrenheit.
Double Boiler: Place the jars in a double boiler with water and set to simmer lightly.


Herbal blends and formulas include herbal infused oils using castor oil and flax seed oil as a carrier and adding essential oils such as poke root.
Castor Oil Packs
Infused Oil Treatment (IOT) (Poke Root)
Essential oils such as ginger and germanium
Mugwort infused oil

Mugwort is an effective ingredient for soothing even the most sensitive skin. It offers anti-inflammatory, antibacterial, and antioxidant benefits, and it could even help protect your skin against free radical damage.
Anti-Inflammatory Properties:
Mugwort soothes irritated skin and reduces redness. It’s excellent for calming inflammation caused by external factors like sun damage or pollution.
Antibacterial and Antifungal Benefits:
Mugwort has natural antibacterial and antifungal properties, making it effective against skindamaging bacteria. It helps maintain healthy skin.
Antioxidant Protection:
Rich in antioxidants, including vitamin E, mugwort protects the skin barrier from free radical damage. This contributes to preventing premature aging and other skin issues.
Softening, Moisturizing, and Toning:
Mugwort’s healing properties leave the skin soft and hydrated. Regular use can enhance overall skin health.
Ideal for Sensitive Skin:
It is well tolerated by most skin types. Its gentle nature makes it suitable for sensitive skin types.
Anti-Microbial Effects:
Mugwort’s compound called azulene has antimicrobial properties, helping maintain a healthy skin microbiome.
An herbal formulation refers to a dosage form that consists of one or more herbs or processed herbs in specific quantities. These formulations are designed to provide specific nutritional or therapeutic effects.

Arnica, Arnica montana (flowers) – Analgesic and Anti-inflammatory. Used topically or homeopathically.
Blue Vervain, Verbena hastata (all parts but mainly aerial parts) – Nervine, Relaxant, Sedative, Antispasmodic upper body.
Boswellia, Boswellia serrata - Anti-inflammatory and Analgesic, Contains boswellic acids that can treat pain and inflammation.
Calendula Flowers, Calendula officinalis – Anti-inflammatory, Anodyne, treatment of skin conditions and rashes.
California Poppy, Eschscholzia californica – Sedative, Anti-spasmodic, Anodyne, the bright orange flowers of the California poppy, leaves and other aerial parts are used.
Capsicum or Red pepper, Capsicum annuum – Vasodilatation, Anti-inflammatory, Anodyne. Use for arthritis and joint pain and inflammation.
Chamomile Flower, Matricaria chamomilla – Mild Nervine, Relaxant, Sedative.
Clove buds, Syzygium aromaticum – Anodyne, Anti-inflammatory, may be added to capsicum.
Cramp Bark, Viburnum opulus – Anti-spasmodic mainly female reproductive system and smooth muscle.
Devil’s Claw, Harpagophytum procumbens, Devil’s claw is a South African herb with medicinally active roots used to treat pain and inflammation.
Hops Flowers, Humulus lupulus – Sedative, Nervine, Relaxant, Anti-inflammatory.
Kava Root, Piper methysticum – Nervine, Relaxant, Sedative, Anti-spasmodic general and lower body.
Lavender, Lavandula spp. (aerial parts) – Nervine, Sedative, Relaxant.
Licorice Root, Glycyrrhiza glabra – Anti-inflammatory. Contains phyto sterols like hydrocortisone and estrogen.
Meadowsweet, Filipendula ulmaria (all parts but mainly flowers and leaves) – Antiinflammatory and Analgesic. Contains salicin.
Mugwort, Artemisia vulgaris (Roots, leaves, stems, and flowers) – Nervine, Sedative, Antispasmodic, Warming tonic.
Mullein Leaf and Flower, Verbascum Thapsus – Respiration, Expectorant, Anodyne, Antiinflammatory, Anti-tussive, skin irritation and inflammation.
Rosemary, Rosmarinus officinalis (all aerial parts but mainly the flowers and leaves) –Anti-inflammatory, Nervine, and Sedative.
Sage, Salvia officinalis (all aerial parts) – Anti-inflammatory, encourages new blood vessel growth and circulation, encourages nerve healing and regeneration, antispasmodic, nervine.
Skullcap, Scutellaria spp. (Aerial parts and roots) – Nervine, Sedative, Anti-inflammatory, Anti-spasmodic, Anti-convulsant, increases blood flow, prevents, and treats neuron damage in the brain.
Teasel Root, Dipsacus fullonum – Anti-inflammatory, Anodyne, Lyme disease excellent for joint pain, osteoarthritis.
Turmeric Root, Curcuma longa – Anti-inflammatory, Anti-microbial, and pain relief.
Valerian Root, Valeriana officinalis, Nervine, Sedative.
The following information provides a list of the various formulations and combinations I typically use for patient treatment:
Castor oil and flaxseed oil 50/50 blend.
Castor oil and flaxseed oil 50/50 blend plus dried skullcap infusion (nerve conditions).
Castor oil and flaxseed oil 50/50 blend plus dried sage infusion (increase circulation, edema, vascular insufficiency).
Castor oil and flaxseed oil 50/50 blend plus dried mugwort infusion (anti-spasmodic and warming tonic).
Safflower oil and dried red pepper (capsicum) infusion (increase blood flow and reduce pain).
Safflower oil and dried poke root (Phytolacca americana) infusion (for the treatment of lymphatic conditions, immune response, and lymphedema).
Castor oil and poke root infusion 50/50 blend.
The following formulation is recommended for general use for musculoskeletal conditions related to pain, inflammation, and muscle spasm.
The general formulation is blended by using flaxseed oil and adding castor oil, and mugwort infused oil.
Formulation: (Equal parts of each oil)
Castor Oil – 1 Part
Flaxseed Oil – 1 Parts
Mugwort Oil – 1 Part
To this formulation you may also add an essential oil according to correct dilution procedures.
The following formulation is used for nerve conditions and neuropathy as well as to encourage blood circulation and lymphatic activity around nerve tracks.
The nerve tonic is blended by using sweet almond oil and adding mugwort infused oil and skullcap infused oil.
Formulation: (Equal parts of each oil)
Sweet Almond Oil – 1 Parts
Mugwort Oil – 1 Parts
Skullcap Oil – 1 Parts
To this formulation you may also add an essential oil according to correct dilution procedures.
Sweet Almond Oil (Prunus amygdalus) – Mugwort Oil (Artemisia vulgaris) – Skullcap Oil
(Scutellaria lateriflora) – Castor Oil (Ricinus communis) – Flaxseed Oil (Linum usitatissimum) – Rosemary Oil (Salvia Rosmarinus) -Camphor Essential Oil (Cinnamomum camphora) – Eucalyptus Essential Oil (Eucalyptus) – Sage Oil (Salvia officinalis) - Rose Essential Oil (Rosa/Rosa damascene/Rosa centifolia) – Frankincense Essential Oil
(Boswellia Serrata) - Valerian Root (Valeriana officinalis) - Mullein Leaf and Flower (Verbascum thapsus) - Clove Bud Essential Oil (Syzygium aromaticum) - Lavender
(Lavandula spp) Essential Oil - Arnica (Arnica montana) - Calendula (Calendula officinalis)
Key Constituents: Curcuminoids and volatile oils.
Actions: Anti-inflammatory, antioxidant, neuroprotective.
Uses: Neuroinflammation, metabolic support, vascular health.
Cautions: Avoid with anticoagulants; may aggravate reflux.
Key Constituents: Punicalagins, ellagic acid, tannins.
Actions: Vascular-protective and antioxidant.
Uses: Vascular dementia support and endothelial health.
Cautions: High sugar content in juice; CYP interactions possible.
Key Constituents: Volatile oils, diterpenes, rosmarinic acid.
Actions: Cognitive support and antioxidant.
Uses: Mild to moderate cognitive decline.
Cautions: Avoid high-thujone chemotypes in seizure disorders.
Key Constituents: Flavonoids and volatile oils.
Actions: Nervine and anxiolytic.
Uses: Anxiety, agitation, sensory overload.
Cautions: Use reputable sources; avoid excess sedation.
Key Constituents: Kavalactones.
Actions: Anxiolytic and muscle relaxant.
Uses: Short -term agitation or severe anxiety.
Cautions: Hepatotoxicity risk; avoid in liver disease.
Key Constituents: Iridoids and flavonoids.
Actions: Nervine and mild sedative.
Uses: Tension, irritability, emotional stress.
Cautions: Bitter; may cause GI upset.
Key Constituents: Bisabolol, chamazulene, apigenin.
Actions: Mild sedative and antiinflammatory.
Uses: Evening calming and sleep initiation.
Cautions: Avoid with Asteraceae allergy.
Key Constituents: Flavonoids and trace alkaloids.
Actions: Anxiolytic and hypnotic.
Uses: Sundowning and evening agitation.
Cautions: Additive sedation possible.
Key Constituents: Volatile oils and rosmarinic acid.
Actions: Anxiolytic and mood supportive.
Uses: Irritability and evening calming.
Cautions: Theoretical thyroid interaction.
Key Constituents: EGCG, caffeine, Ltheanine.
Actions: Antioxidant and vascular support.
Uses: Cognitive clarity and mild stimulation.
Cautions: Caffeine sensitivity.
Key Constituents: Flavone glycosides and terpenoids.
Actions: Increases cerebral circulation and neuroprotection.
Uses: Vascular and mixed dementia, attention support.
Cautions: Anticoagulant effect; avoid pre-surgery.
Key Constituents: Bacosides A and B.
Actions: Memory-enhancing and anxiolytic.
Uses: Memory formation and anxiety reduction.
Cautions: Mild GI upset possible.
Key Constituents: Withanolides and sitoindosides.
Actions: Stress reduction and neuroprotection.
Uses: Anxiety, agitation, and sleep improvement.
Cautions: Avoid in hyperthyroid states.
Dementia reflects dysfunction across multiple interconnected body systems:
Body systems shape brain vulnerability
Metabolic and vascular health influence decline
Chronic inflammation links systems
Manual therapy and nutrition impact entire networks
The nervous system is the primary site of dementia pathology.
Loss of synaptic signaling
Impaired sensory processing
Autonomic dysregulation
Motor planning and gait issues
health shapes progression of dementia.
Hypertension damages small vessels
Reduced perfusion accelerates decline
Atrial fibrillation increases risk
Endothelial inflammation reduces oxygen delivery
Oxygenation is essential for brain metabolism.
Hypoxia increases confusion
Sleep apnea accelerates memory loss
Poor diaphragmatic function
Anxiety alters breathing patterns
Hormones regulate metabolism, inflammation, and stress.
Insulin resistance harms neurons
High cortisol worsens memory
Thyroid dysfunction affects cognition
Hormone decline reduces neuroplasticity
The gut-brain axis influences cognition and mood.
Gut inflammation increases neuroinflammation
B12 and folate deficiency impair clarity
Blood sugar swings worsen confusion
Microbiome imbalance alters neurotransmitters
Chronic inflammation drives cognitive decline.
Immune dysregulation injures neurons
Impaired microglial cleanup
Infections trigger delirium
Autoimmune issues increase vulnerability
Dementia affects movement, strength, and proprioception.
Reduced proprioception increases falls
Pain often shows as agitation
Rigidity reduces mobility
Frailty limits treatment tolerance
Skin, fascia, and sensory receptors influence patient comfort.
Reduced sensation increases injury
Poor circulation slows healing
Touch can overwhelm or calm
Lymph flow affects inflammation
UTIs and hydration strongly affect cognition.
UTIs trigger delirium
Dehydration worsens cognition
Incontinence affects skin health
Kidney issues alter medication clearance
Hormones influence neuroprotection and mood.
Hormone loss reduces repair
Increased inflammation with decline
Sleep disruption affects symptoms
Mood instability linked to endocrine issues
Brain and body rely on waste clearance pathways.
Reduced nighttime clearance
Lymph stagnation increases inflammation
Neck tension restricts drainage
Massage supports flow and calming

Dementia arises from multiple interacting systems.
Whole-body health supports resilience
Therapists stabilize these systems
Nutrition and herbs support metabolic pathways
Caregivers benefit from system-wide insight

I recommend a system-by-system approach to patient evaluation and assessment based upon observation, palpation, and questioning. Dr. Lawton

The skin often reflects a person's overall health and well-being because it can manifest signs of internal issues, deficiencies, and systemic conditions. By observing changes in the skin, healthcare providers can often identify and diagnose underlying health issues, making the skin an important diagnostic tool for overall health and well-being.
Nutritional Status
Deficiencies: Lack of essential nutrients like vitamins (A, C, D, E), minerals (zinc, iron), and fatty acids can lead to skin problems such as dryness, rashes, and poor wound healing.
Hydration: Dehydration can cause the skin to appear dry, flaky, and less elastic.
Hydration Levels
Skin Turgor: Well-hydrated skin is firm and elastic, whereas dehydration can make it look wrinkled and saggy.
Hormonal Balance
Acne and Breakouts: Hormonal imbalances, such as those seen in puberty, pregnancy, and conditions like polycystic ovary syndrome (PCOS), can lead to acne.
Changes in Texture and Color: Conditions like thyroid disorders can cause changes in skin texture and color.
Immune System Health
Rashes and Infections: A compromised immune system can lead to frequent skin infections, rashes, and delayed healing.
Autoimmune Disorders: Conditions like lupus and psoriasis often have skin manifestations.
Stress-Related Conditions: Stress can exacerbate skin conditions such as eczema, psoriasis, and acne.
Overall Appearance: Chronic stress can lead to dull, tired-looking skin and exacerbate the signs of aging.
Jaundice: Yellowing of the skin can indicate liver problems.
Uremic Frost: In severe kidney disease, urea can crystallize on the skin.
Cyanosis: A bluish tint to the skin can indicate poor oxygenation of the blood, often related to heart or lung problems.
Redness and Swelling: Conditions like rosacea and chronic venous insufficiency can indicate underlying vascular issues.
Acanthosis Nigricans: Dark, velvety patches of skin, often in body folds, can indicate insulin resistance or diabetes.
Delayed Healing: High blood sugar levels can impair wound healing and increase the risk of infections.
Hives and Rashes: Allergic reactions to foods, medications, or environmental factors can manifest as skin rashes or hives.
Dermatitis: Contact with allergens or irritants can cause eczema or dermatitis.
Premature Aging: Lifestyle factors such as smoking, excessive alcohol consumption, and poor diet can accelerate skin aging, resulting in wrinkles, fine lines, and loss of elasticity.
Systemic Infections: Diseases like chickenpox, measles, and Lyme disease have characteristic skin manifestations.
Cancer: Skin cancers, such as melanoma, can indicate exposure to harmful UV radiation and overall health risks.

Central obesity, also known as abdominal obesity or visceral obesity, refers to the accumulation of fat around the abdomen and internal organs. This type of obesity is often measured by waist circumference and waist-to-hip ratio. Addressing central obesity early can significantly reduce the associated health risks and improve overall well-being and longevity.
Association with Metabolic Syndrome
Insulin Resistance: Central obesity is strongly associated with insulin resistance, a condition where cells in the body become resistant to the effects of insulin. This leads to elevated blood sugar levels and an increased risk of type 2 diabetes.
Dyslipidemia: It often coincides with abnormal levels of lipids (cholesterol and triglycerides) in the blood, specifically low HDL ("good") cholesterol and high LDL ("bad") cholesterol, which are risk factors for cardiovascular disease.
Hypertension: Central obesity is linked with hypertension (high blood pressure), which further increases the risk of heart disease and stroke.
Inflammatory and Immune Responses
Release of Inflammatory Substances: Fat cells in the abdominal area (visceral fat) release inflammatory substances and hormones that contribute to chronic inflammation. This chronic inflammation is implicated in the development of various diseases, including cardiovascular disease, type 2 diabetes, and certain cancers.
Immune System Dysfunction: Excess visceral fat can disrupt the normal functioning of the immune system, increasing susceptibility to infections and impairing wound healing.
Cardiovascular Disease
Atherosclerosis: Central obesity contributes to the development of atherosclerosis, a condition where fatty deposits (plaques) build up inside the arteries, narrowing and hardening them. This increases the risk of heart attacks, strokes, and other cardiovascular complications.
Heart Failure: Obesity, especially abdominal obesity, is a risk factor for heart failure, where the heart muscle becomes weakened and unable to pump blood efficiently.
Increased Cancer Risk: Central obesity is associated with an increased risk of several types of cancers, including colorectal cancer, breast cancer (in women), and prostate cancer (in men).
Non-alcoholic Fatty Liver Disease (NAFLD): Central obesity is a major risk factor for NAFLD, a condition where fat accumulates in the liver, potentially leading to liver inflammation and scarring (cirrhosis).
Kidney Disease: Obesity, particularly abdominal obesity, is linked to an increased risk of chronic kidney disease.
Psychological Well -being: Central obesity can impact self-esteem, body image, and mental health, leading to anxiety, depression, and social stigma.
Reduced Quality of Life: Health complications associated with central obesity can impair physical mobility, limit daily activities, and reduce overall quality of life.
Overall Mortality Risk: Individuals with central obesity have a higher risk of premature death compared to those with a healthy waist circumference and body composition.

Poor spinal posture can significantly impact both quality of life and overall health in various ways. Misalignment of the spine can cause conditions such as scoliosis, kyphosis, lordosis, and arthritis leading to discomfort and potential long-term health issues.
Chronic Pain:
Poor posture often leads to chronic back, neck, and shoulder pain due to increased strain on muscles and ligaments.
Reduced Flexibility and Mobility:
Poor posture can limit the range of motion and flexibility, making it difficult to perform daily activities and exercise.
Increased Risk of Injury:
Misalignment and muscle imbalances increase the risk of injuries, particularly in the back and neck.
Respiratory Issues:
Slouched posture can compress the lungs and diaphragm, leading to reduced lung capacity and breathing difficulties.
Digestive Problems:
Poor posture can compress abdominal organs, affecting digestion and potentially causing issues like acid reflux and constipation.
Chronic pain and discomfort can lead to fatigue, reducing overall energy levels and enthusiasm for daily activities.
Mood and Mental Health:
Persistent pain and physical limitations can contribute to stress, anxiety, and depression.
Self-Esteem and Confidence:
Poor posture can affect body image and self-esteem, leading to decreased confidence in social and professional settings.
Physical discomfort and pain can reduce concentration and productivity at work or school.
Reduced flexibility and pain can hinder participation in physical activities and hobbies, impacting social interactions and overall enjoyment of life.
Discomfort from poor posture can interfere with sleep quality, leading to insomnia or restless sleep.

Poor gait, which refers to an abnormal walking pattern, can have wide-ranging effects on a person's health and well-being. Identify underlying causes of poor gait, such as neurological, muscular, or skeletal issues and develop an effective treatment plan.
Musculoskeletal Issues:
Joint Pain and Damage: Abnormal gait patterns can lead to uneven weight distribution, causing stress and wear on the joints, particularly in the knees, hips, and ankles.
Muscle Strain: Compensatory movements due to poor gait can strain muscles, leading to pain and discomfort in the legs, lower back, and other areas.
Increased Risk of Falls and Injuries:
Poor gait can reduce balance and coordination, significantly increasing the risk of falls, which can result in fractures, sprains, and other injuries.
Foot Problems:
Abnormal gait can contribute to foot issues such as bunions, calluses, and plantar fasciitis, as well as exacerbate existing foot deformities.
Spinal Misalignment:
Poor gait can cause or exacerbate spinal alignment issues, leading to back pain and other spinal problems.
Reduced Physical Activity:
Difficulty walking can lead to reduced physical activity, which in turn can negatively affect cardiovascular health, contributing to conditions such as obesity, hypertension, and cardiovascular disease.
Decreased Independence:
Difficulty walking can limit a person’s ability to perform daily activities independently, leading to feelings of helplessness and decreased quality of life.
Mental Health Issues:
Chronic pain and reduced mobility associated with poor gait can contribute to mental health issues such as depression and anxiety.
Social Isolation:
Limited mobility can reduce social interactions and participation in community activities, leading to social isolation and loneliness.
Poor gait can limit a person’s ability to move around freely, affecting their ability to work, engage in hobbies, and participate in social activities.
Continuous pain and discomfort from poor gait can significantly impact daily life, reducing overall enjoyment and satisfaction.
Sleep Disturbances:
Pain and discomfort associated with poor gait can interfere with sleep, leading to insomnia or poor sleep quality, which in turn affects overall health and well-being.

Foot health is crucial to overall health and well-being for several reasons including all the reasons outlined under the Gait section of this workbook.
Musculoskeletal Alignment:
The feet serve as the foundation for the body. Problems with foot health can lead to issues in the ankles, knees, hips, and lower back due to misalignment and compensation for pain or discomfort.
Prevention of Chronic Conditions:
Proper foot health can prevent chronic conditions such as neuropathy, plantar fasciitis, bunions, and arthritis, which can cause long-term pain and disability.
Circulatory Health:
The feet are farthest from the heart, and good circulation is vital for delivering oxygen and nutrients. Poor foot health can be an indicator of circulatory problems, especially in individuals with diabetes or cardiovascular disease.

Hair, skin, and nails can serve as important indicators of a person’s overall health.
Changes in these areas can sometimes be the first signs of underlying health issues.
Regular monitoring of hair, skin, and nails can help detect early signs of potential health issues.
Hair Loss: Sudden or excessive hair loss can indicate hormonal imbalances (such as thyroid disorders), nutritional deficiencies (like iron or protein deficiency), stress, or certain medical conditions like alopecia areata or lupus.
Dry, Brittle Hair: This can be a sign of nutritional deficiencies, overuse of hair styling products, or underlying health issues such as hypothyroidism.
Thinning Hair: Could be a sign of aging, hormonal changes, or nutritional deficiencies.
Skin - Indicators of Health Issues:
Rashes and Itchiness: Conditions such as eczema, psoriasis, allergies, or infections can cause these symptoms.
Discoloration: Jaundice (yellowing of the skin) can indicate liver disease; cyanosis (bluish tint) can indicate respiratory or cardiovascular issues.
Acne: While common and often related to hormonal changes, severe or sudden acne can indicate underlying hormonal disorders such as polycystic ovary syndrome (PCOS).
Dry, Flaky Skin: Can be a sign of dehydration, hypothyroidism, or vitamin deficiencies.
Wounds That Don’t Heal: Can indicate diabetes or circulatory issues.
Nails - Indicators of Health Issues:
Brittle Nails: Can indicate nutritional deficiencies (like biotin), thyroid disease, or fungal infections.
Discoloration: Yellow nails can indicate fungal infections, respiratory issues, or lymphedema; white nails can indicate liver disease.
Spoon Nails (Koilonychia): This can be a sign of iron-deficiency anemia.
Pitting or Grooving: Conditions such as psoriasis or alopecia areata can cause these changes.
Clubbing: Enlarged, curved nails can indicate respiratory or cardiovascular diseases.


Poor oral health can be an indicator of broader health issues and can also contribute to various health risks. Maintaining good oral health is crucial not just for a healthy mouth but for overall health and well-being. Regular dental check-ups, proper oral hygiene, and a balanced diet are essential for preventing oral health problems and mitigating broader health risks.
Indicators of Health Issues:
Gum Disease (Periodontal Disease):
Systemic Conditions: Severe gum disease has been linked to systemic conditions such as diabetes, cardiovascular disease, and rheumatoid arthritis.
Diabetes: People with diabetes are more prone to infections, including periodontal disease, and uncontrolled gum disease can make it harder to manage blood sugar levels.
Oral Infections:
Immune System Issues: Frequent oral infections can indicate a compromised immune system, possibly due to conditions such as HIV/AIDS or leukemia.
Nutritional Deficiencies: Recurrent mouth sores or infections can be a sign of nutritional deficiencies, such as a lack of vitamin C (scurvy) or iron (anemia).
Heart Disease and Stroke: Inflammation and infections caused by oral bacteria can lead to cardiovascular problems. Studies have found links between periodontal disease and an increased risk of heart disease and stroke.
Respiratory Infections:
Pneumonia: Bacteria from the mouth can be aspirated into the lungs, leading to infections such as pneumonia, especially in vulnerable populations like the elderly or those with compromised immune systems.
Heart Disease and Stroke: Inflammation and infections caused by oral bacteria can lead to cardiovascular problems. Studies have found links between periodontal disease and an increased risk of heart disease and stroke.
Respiratory Infections:
Pneumonia: Bacteria from the mouth can be aspirated into the lungs, leading to infections such as pneumonia, especially in vulnerable populations like the elderly or those with compromised immune systems.
Indicators of Health Issues:
Adverse Pregnancy Outcomes:
Preterm Birth and Low Birth Weight: Pregnant women with periodontal disease are at a higher risk of delivering preterm or low birth weight babies.
Diabetes Complications:
Poor Blood Sugar Control: Infections and inflammation from gum disease can make it more difficult to control blood sugar levels, worsening diabetes and its complications.
Endocarditis:
Heart Infection: Bacteria from the mouth can enter the bloodstream and infect the inner lining of the heart, especially in people with damaged heart valves or other heart conditions.

Indicators of Health Issues:
Inflammatory Conditions:
Rheumatoid Arthritis (RA): This autoimmune disease not only affects joints but can also indicate a systemic inflammatory condition that may affect organs such as the heart, lungs, and eyes. RA is associated with an increased risk of cardiovascular disease.
Psoriatic Arthritis: Often linked with psoriasis, it indicates an underlying immune system disorder and can also involve the skin and other organs.
Metabolic Disorders:
Gout: Characterized by the accumulation of uric acid crystals in the joints, gout indicates a problem with uric acid metabolism and can be associated with other conditions like kidney stones, obesity, hypertension, and cardiovascular disease.
Indicators of Health Issues:
Inflammatory Conditions:
Genetic Predispositions:
Ankylosing Spondylitis: A type of arthritis that affects the spine, it often indicates a genetic predisposition and can also lead to inflammation in other parts of the body, such as the eyes (uveitis) and the intestines (inflammatory bowel disease).
Degenerative Conditions:
Osteoarthritis: While primarily a degenerative joint disease, it can also indicate mechanical stress on the joints due to obesity, injury, or overuse. It may reflect broader issues like obesity, which is a risk factor for various other health conditions.
Cardiovascular Disease:
Inflammatory Arthritis: Conditions like RA and psoriatic arthritis are associated with an increased risk of cardiovascular diseases, including heart attack and stroke, due to chronic inflammation.
Obesity:
Osteoarthritis and Gout: These conditions can be exacerbated by obesity, which also increases the risk of developing other health problems such as diabetes, hypertension, and cardiovascular disease.
Diabetes:
RA and Osteoarthritis: These conditions are often associated with an increased risk of developing diabetes. The inflammation and physical inactivity caused by joint pain can contribute to insulin resistance.
Indicators of Health Issues:
Reduced Mobility and Physical Activity:
Joint Pain and Stiffness: Arthritis can lead to decreased mobility and physical activity, which can result in muscle weakness, weight gain, and a higher risk of cardiovascular disease, diabetes, and osteoporosis.
Mental Health Issues:
Chronic Pain and Disability: Persistent pain and disability from arthritis can lead to mental health issues such as depression and anxiety, further impacting overall health and quality of life.
Respiratory Problems:
RA and Ankylosing Spondylitis: These conditions can cause lung complications, including interstitial lung disease and reduced lung capacity, leading to respiratory problems.

Eye and vision health are integral to overall health, and poor eye health can be both an indicator of and a contributor to broader health issues and risks. Eye and vision health are closely linked to overall health. Regular eye care and attention to vision changes can help detect systemic health issues early and reduce the risk of complications.
Diabetes: Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina. The presence of diabetic retinopathy can indicate poorly controlled blood sugar levels.
Hypertension: High blood pressure can cause damage to the blood vessels in the retina, leading to hypertensive retinopathy, which can be detected during an eye exam.
Autoimmune Diseases: Conditions such as lupus, multiple sclerosis, and rheumatoid arthritis can cause inflammation in the eyes, leading to symptoms like dry eyes, uveitis, or optic neuritis.
Cardiovascular Disease: Changes in the blood vessels in the eyes can sometimes indicate broader cardiovascular issues, such as atherosclerosis.
Impaired Vision: Poor vision increases the risk of falls and accidents, especially in older adults. This can lead to injuries, fractures, and a decrease in mobility and independence.
Reduced Independence: Vision loss can lead to difficulties in performing daily activities, reducing the quality of life and increasing dependence on others.
Mental Health Issues: Vision impairment is associated with an increased risk of depression and anxiety due to reduced independence and social isolation.
Link with Dementia: There is evidence to suggest that vision impairment is associated with an increased risk of cognitive decline and dementia. This may be due to decreased sensory input and reduced engagement in stimulating activities.
Digital Eye Strain: Prolonged use of digital devices can cause eye strain, headaches, and neck pain. This can affect productivity and overall well-being.
Uncorrected Vision Problems: Conditions such as astigmatism, hyperopia, and myopia, if uncorrected, can cause chronic headaches and fatigue.
Indicators of Health Issues:
Chronic Conditions:
Glaucoma and Age-Related Macular Degeneration (AMD): These chronic eye conditions, if not properly managed, can lead to significant vision loss and are often associated with aging and other systemic health issues.
Potential for Infections:
Contact Lens Use: Improper use and care of contact lenses can lead to eye infections, which, if severe, can result in vision loss and indicate poor hygiene practices.
Nutritional Deficiencies:
Vitamin A Deficiency: This can lead to night blindness and, in severe cases, complete blindness. It can also indicate poor overall nutritional status.
Other Nutrient Deficiencies: Deficiencies in vitamins C and E, zinc, and omega-3 fatty acids can affect eye health and may be indicative of poor dietary habits.


Reduced Blood Flow: Hearing loss can be an early indicator of cardiovascular disease. The inner ear is sensitive to blood flow, and reduced circulation from cardiovascular problems can damage the tiny hair cells in the cochlea.
Nerve Damage: Diabetes can lead to nerve damage and poor circulation, affecting the ears and leading to hearing loss. Studies show that people with diabetes are more likely to experience hearing loss than those without the condition.
Hypertension:
Blood Vessel Damage: High blood pressure can damage the blood vessels in the ear, leading to hearing loss. This can be an early sign of hypertension or poor blood pressure control.
Chronic Kidney Disease:
Shared Risk Factors: Hearing loss is more common in people with chronic kidney disease due to shared risk factors such as diabetes and hypertension. The kidneys and the ears share similar structural and functional characteristics, making them both susceptible to damage from these conditions.
Indicators of Health Issues:
Infections:
Viral and Bacterial Infections: Ear infections can be indicative of broader immune system issues. Chronic or recurrent ear infections can suggest underlying conditions that compromise the immune system.
Autoimmune Diseases:
Inflammation: Autoimmune diseases such as lupus and rheumatoid arthritis can cause inflammation in the ear, leading to hearing loss. Sudden hearing loss can sometimes be a sign of an autoimmune inner ear disease.
Ototoxic Medications:
Medication Side Effects: Certain medications, including some antibiotics, chemotherapy drugs, and diuretics, can be ototoxic (harmful to the ears) and cause hearing loss. This indicates the need for careful monitoring of medication use.
Cognitive Decline and Dementia:
Reduced Stimulation: Hearing loss has been linked to cognitive decline and an increased risk of dementia. Reduced auditory input can lead to decreased brain stimulation, contributing to cognitive deterioration.
Mental Health Issues:
Depression and Anxiety: Hearing loss can lead to social isolation, communication difficulties, and reduced quality of life, increasing the risk of depression and anxiety.
Safety Risks:
Accidents and Injuries: Hearing loss can compromise the ability to detect environmental sounds, such as alarms, traffic noises, and warnings, leading to an increased risk of accidents and injuries.
Cognitive Decline and Dementia:
Reduced Stimulation: Hearing loss has been linked to cognitive decline and an increased risk of dementia. Reduced auditory input can lead to decreased brain stimulation, contributing to cognitive deterioration.
Mental Health Issues:
Depression and Anxiety: Hearing loss can lead to social isolation, communication difficulties, and reduced quality of life, increasing the risk of depression and anxiety.
Safety Risks:
Accidents and Injuries: Hearing loss can compromise the ability to detect environmental sounds, such as alarms, traffic noises, and warnings, leading to an increased risk of accidents and injuries.
Social Isolation:
Communication Barriers: Difficulty hearing can lead to social withdrawal and isolation, impacting relationships and overall well-being.
Balance Problems:
Vestibular System: The inner ear is also responsible for balance. Hearing loss, especially when related to inner ear issues, can lead to balance problems and an increased risk of falls.




The “inconvenience” of adopting a healthy diet and way of life is nothing compared to the pain, suffering, limitations, and disabilities that result from a poor diet, bad health habits, and a lack of exercise.
Dr. Lawton’s Quote

Early indicators of dysfunction in the eleven major body systems can reveal underlying health problems and potential risks to overall health. Early indicators of dysfunction in these body systems can provide critical insights into overall health and potential risks. Recognizing and addressing these signs promptly through medical evaluation and intervention can prevent the progression of diseases and improve quality of life.
Skeletal System: Composed of bones and cartilages, the skeletal system provides mechanical support, protects internal organs, and assists in movement. There are 206 bones in an adult human body.
Muscular System: This system enables movement by contracting and relaxing muscles. It includes both voluntary (skeletal) and involuntary (smooth and cardiac) muscles.
Cardiovascular System: Responsible for circulating blood throughout the body, the cardiovascular system includes the heart, blood vessels, and blood. It transports oxygen, nutrients, and hormones while eliminating waste products.
Respiratory System: Involved in gas exchange, the respiratory system allows us to breathe. It brings oxygen into the body and removes carbon dioxide. Additionally, it helps regulate acid-base balance and is essential for phonation (speech).
Nervous System: The nervous system collects and processes information from the senses, regulates vital functions, and coordinates body movements. It includes the central nervous system (brain and spinal cord) and peripheral nerves.
Digestive System: Responsible for breaking down food mechanically and chemically, the digestive system absorbs nutrients into the body for energy. It includes organs like the mouth, esophagus, stomach, and intestines.
Urinary System (Renal System): The urinary system filters blood through the kidneys, producing urine to eliminate waste products and maintain fluid balance.
Endocrine System: This system produces hormones that regulate various bodily functions, such as the menstrual cycle, blood sugar levels, and growth.
Lymphatic System (Immune System): The lymphatic system drains excess tissue fluid, transports immune cells, and defends the body against pathogens.
Reproductive System: Responsible for producing reproductive cells (sperm and eggs), this system contributes to the process of reproduction. It differs between males and females.
Integumentary System: Comprising the skin and its appendages (hair, nails, sweat glands, and oil glands), the integumentary system provides physical protection, sensory reception, and even synthesizes vitamin D.
Cardiovascular System
Indicators: Chest pain, shortness of breath, irregular heartbeats, high blood pressure, swelling in extremities.
Health Risks: These symptoms can indicate heart disease, hypertension, or circulatory problems, increasing the risk of heart attacks, stroke, and other cardiovascular events.
Respiratory System
Indicators: Chronic cough, wheezing, shortness of breath, frequent respiratory infections.
Health Risks: These signs can suggest asthma, chronic obstructive pulmonary disease (COPD), infections, or lung cancer, leading to decreased oxygenation and increased risk of respiratory failure.
Nervous System
Indicators: Persistent headaches, dizziness, numbness, tingling, changes in vision, memory problems.
Health Risks: Such symptoms can indicate neurological conditions like multiple sclerosis, migraines, stroke, or neurodegenerative diseases, affecting cognitive and motor functions.
Cardiovascular System
Indicators: Chest pain, shortness of breath, irregular heartbeats, high blood pressure, swelling in extremities.
Health Risks: These symptoms can indicate heart disease, hypertension, or circulatory problems, increasing the risk of heart attacks, stroke, and other cardiovascular events.
Respiratory System
Indicators: Chronic cough, wheezing, shortness of breath, frequent respiratory infections.
Health Risks: These signs can suggest asthma, chronic obstructive pulmonary disease (COPD), infections, or lung cancer, leading to decreased oxygenation and increased risk of respiratory failure.
Nervous System
Indicators: Persistent headaches, dizziness, numbness, tingling, changes in vision, memory problems.
Health Risks: Such symptoms can indicate neurological conditions like multiple sclerosis, migraines, stroke, or neurodegenerative diseases, affecting cognitive and motor functions.
Digestive System
Indicators: Persistent abdominal pain, bloating, changes in bowel habits, heartburn, nausea.
Health Risks: These could be signs of gastrointestinal disorders like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), gastroesophageal reflux disease (GERD), or even cancers of the digestive tract, leading to malnutrition and systemic effects.
Indicators: Unexplained weight changes, fatigue, excessive thirst or urination, changes in skin or hair.
Health Risks: Such symptoms can indicate diabetes, thyroid disorders, adrenal dysfunction, or hormonal imbalances, which can impact metabolism, growth, and energy levels.
Immune System
Indicators: Frequent infections, slow wound healing, fatigue, swollen lymph nodes.
Health Risks: These can suggest immunodeficiencies, autoimmune disorders, or chronic infections, leading to increased susceptibility to diseases and prolonged recovery times.
Skeletal System
Indicators: Joint pain, stiffness, frequent fractures, back pain.
Health Risks: These signs can indicate osteoporosis, arthritis, or other bone and joint disorders, increasing the risk of immobility and chronic pain.
Muscular System
Indicators: Muscle weakness, cramps, tremors, muscle wasting.
Health Risks: Such symptoms can be signs of muscular dystrophies, neuromuscular disorders, or chronic conditions like fibromyalgia, impacting mobility and daily functioning.
Integumentary System (Skin, Hair, Nails)
Indicators: Rashes, persistent itching, changes in skin color or texture, hair loss, nail changes.
Health Risks: These can indicate skin conditions, infections, or underlying systemic issues like liver or kidney disease, affecting overall health and appearance.
Reproductive System
Indicators: Irregular menstrual cycles, pelvic pain, changes in libido, infertility.
Health Risks: Such symptoms can indicate hormonal imbalances, reproductive organ disorders, or sexually transmitted infections (STIs), impacting fertility and sexual health.
Urinary System
Indicators: Changes in urine color or volume, frequent urination, pain during urination, lower back pain.
Health Risks: These signs can suggest urinary tract infections, kidney stones, or chronic kidney disease, leading to impaired kidney function and systemic effects.

Dementia affects more than memory. It alters circulation, mobility, sensory processing, autonomic stability, and pain perception. Therapeutic modalities support comfort, reduce agitation, improve function, and help manage common comorbidities.
Calms sensory overload
Supports circulation and lymph flow
Reduces pain the patient cannot verbalize
Improves sleep and autonomic balance
Dementia requires modified safety protocols.
Avoid overstimulation
Approach slowly and from the front
Monitor non-verbal signs of discomfort
Begin with low-intensity modalities
Avoid treating during agitation or delirium
Protect fragile skin and frailty
In the Homeosomatic method we also use many ancillary techniques. The choice of which techniques, therapeutic modalities to use, is based upon the condition of the patient, their diagnosis, their age, and complicating factors. These ancillary techniques include:
Cupping
Red light or Bioptron Therapy
Laser
Micro Stim
High Frequency Percussion
Castor Oil Packs
Infused Oil Treatment (IOT)
Dry Needling
Dry Brushing
Gua Sha
Kinesio tape (KinesioStretch Method)
Herbal medicine and supplementation
Homeopathy



Cupping can improve circulation, warm tissues, and reduce fascial stiffness that contributes to agitation and discomfort.
• Increases superficial blood flow
• Reduces myofascial tension
• Helps calm sensory overload
• Useful in upper back and shoulders
Use caution or avoid cupping in:

• Fragile or bruised skin
• Patients on anticoagulants
• Severe anxiety or defensiveness
• Areas with edema or wounds
• Advanced frailty or cold intolerance


Low-level laser reduces inflammation and supports nerve healing.
• Improves microcirculation
• Reduces pain behaviors
• Supports neuroregeneration
• Helpful for neuropathic discomfort
Use caution or avoid:

Over active cancer sites
Over thyroid gland
In patients who cannot remain still
Direct exposure to eyes
Very thin or frail skin




Red light supports mitochondrial function and reduces inflammation, helping stabilize mood and cognitive clarity.
Enhances cellular energy
Reduces neuroinflammation
Supports sleep-wake regulation
Gentle, non-invasive calming effect
Use caution or avoid when:
Light sensitivity or photophobia
Seizure disorders triggered by light
Active skin infections
Avoid near the eyes

Microcurrent supports cellular repair and autonomic balance.
Increases ATP production
Reduces tension and rigidity
Calms overactive sympathetic response
Improves tissue healing
Use caution or avoid:

Pacemakers or implants
Seizure disorders
Open wounds or infection
Autonomic instability


Gentle percussion helps release tension and improve awareness.
Stimulates proprioception
Reduces rigidity
Improves circulation
Use lightly with dementia patients
Use caution or avoid:
Osteoporosis or fracture risk
High anxiety or overstimulation
Pacemakers or implants
Over bony prominences
Severe arthritis pain

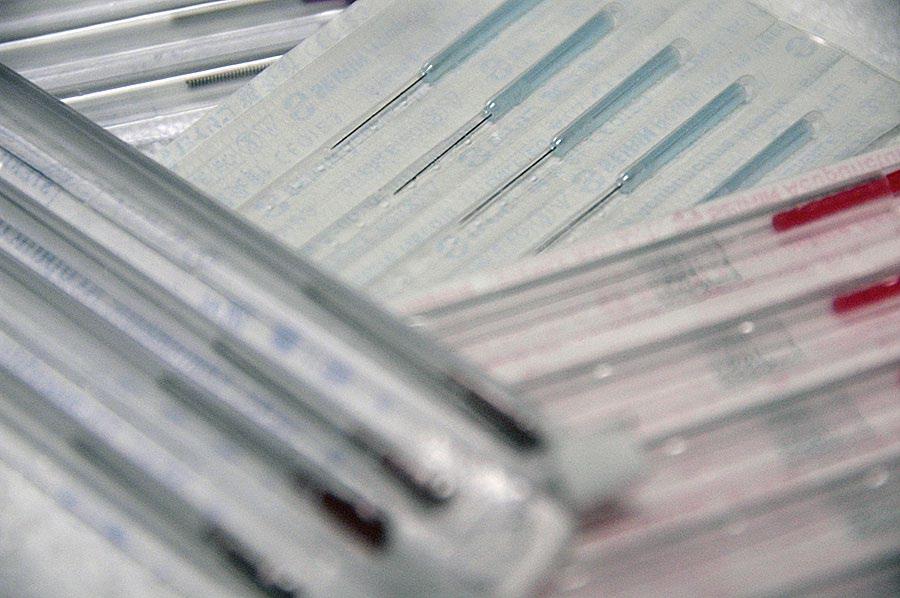
When appropriate, decreases muscle tension and pain.
Reduces trigger point activity
Improves mobility
Helps with chronic pain contributing to agitation
Use cautiously with frailty
Use caution or avoid:

Patients unable to stay still
Anticoagulant use
Bleeding disorders
Frail or atrophied muscles
Severe cognitive impairment limiting consent

Castor oil packs calm the nervous system and reduce inflammation.
Supports lymphatic flow
Reduces abdominal and thoracic tension
Helps evening calming
Improves comfort and sleep
Warm herbal oils ground the patient and improve sensory regulation.
Provides deep calming
Reduces agitation and fear
Nourishes skin and fascia
• Supports evening routines
Use caution or avoid:

Recent abdominal surgery
Heat intolerance or poor sensation
Active diarrhea or acute GI issues
Severe incontinence
Inability to report discomfort
Use caution or avoid:
Essential oil sensitivities
Strong scent intolerance
Skin infection
Fragile skin requiring minimal pressure

Use caution or avoid:

Fragile or bruised skin
Sensory defensiveness
Rashes or infection
Over bony areas in low BMI patients
Dry brushing stimulates lymphatic flow and sensory grounding.
Improves circulation
Supports detoxification
Calms sensory system
Increases body awareness


Gentle gua sha reduces stagnation and calms tension patterns.
Improves circulation
Reduces neck and shoulder rigidity
Supports lymphatic movement
Use mildly on frail patients
Use caution or avoid:

Thin or easily torn skin
Anticoagulants
Anxiety triggered by scraping
Painful joints or bony areas
Use only gentle strokes


Herbal and nutritional support reduces agitation and inflammation.
Calms nervous system
Supports cognition
Reduces metabolic and vascular stress
Complements manual therapy
Use caution or avoid:

Polypharmacy interactions
Anticoagulants with platelet-active herbs
Kidney or liver impairment
Sedating herbs with sedatives
GI sensitivity

Homeopathy can help reduce agitation and support emotional stability.
Gentle and safe
Supports sleep and mood
Can reduce fear and restlessness
Individualized remedies based on patient patterns

Generally safe but use caution:
Sugar pellets with severe diabetes
Patients with swallowing difficulties
Overstimulation from repeated dosing
Kinesio taping supports mobility and proprioception.
Improves posture
Reduces pain behaviors
Enhances sensory feedback
Supports gait and balance
Use caution or avoid:

Adhesive allergy
Fragile or papery skin
Edema with skin tension
Patients who may pull tape off repeatedly
NCBTMB APPROVED CONTINUING EDUCATION











This workbook is intended for educational and informational purposes only. It is not a substitute for professional medical evaluation, diagnosis, or treatment. The material presented here reflects current understanding in holistic health, manual therapy, and supportive care for individuals with cognitive decline and dementia, but it does not replace the advice of qualified medical practitioners.
Always consult a licensed physician, neurologist, or other appropriate healthcare professional regarding any questions or concerns about a patient’s medical condition, medications, or treatment plan. Never disregard professional medical advice or delay seeking it because of something you have read in this workbook.
The techniques and approaches described are intended to complement, not replace, conventional medical care. Practitioners and caregivers should use their professional judgment, stay within their scope of practice and state regulations, and adapt all recommendations to the individual needs and safety of each patient.
The author and publisher disclaim all liability for any outcomes resulting from the application of the information contained in this workbook. Use of this material is at the sole discretion and risk of the reader.