



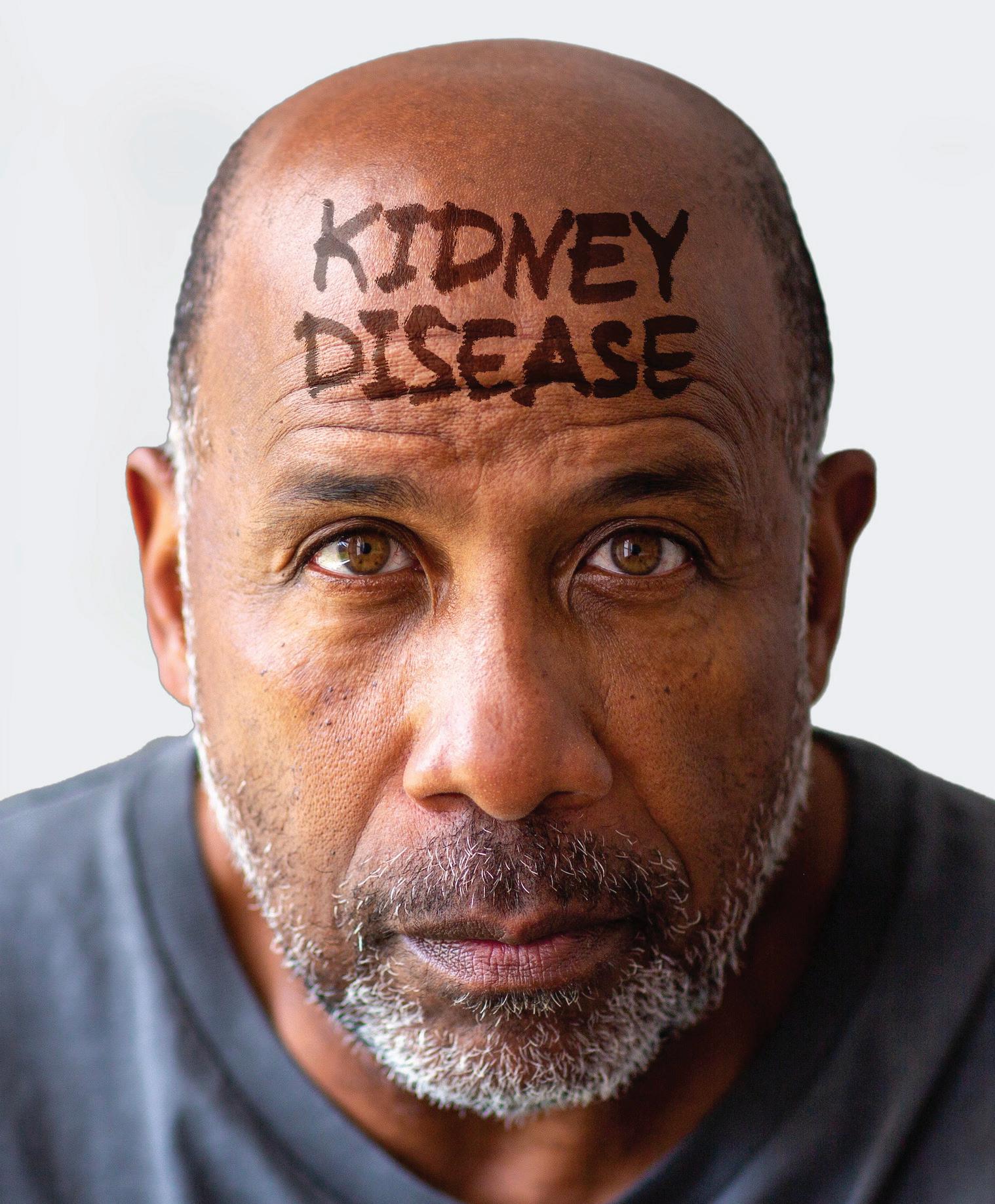
ALONZO MOURNING
The NBA hall-of-famer discusses his journey with kidney disease and transplantation






“Advances in research … make this a critical time to recognize the power of genetic testing in chronic kidney disease.”
“The U.S. organ donation system enables tens of thousands of safe, lifesaving transplants each year.”




For more than half of people who start dialysis, their first introduction to kidney disease occurs in the emergency room (ER) as a medical crisis. For these Americans, their lives, livelihoods, and economic stability are destabilized in an instant. Many become trapped in a resulting cycle of dependency, disability, and unemployment they may never have imagined. As a doctor, one of the saddest realizations is that so much of this burden and suffering is avoidable.
Why is this still happening in America in 2025? It is a result of the failure to educate the public about the risks of chronic illnesses and to prioritize prevention strategies that better align screening with advances in disease detection and intervention.
The silent epidemic
Kidney disease affects 37 million Americans. Federal spending on kidney care, courtesy of the American taxpayer, exceeds $100 billion annually, with dialysis alone costing the Medicare program over $30 billion. Major causes of kidney disease include high blood pressure, diabetes, and obesity with vulnerable communities most impacted, including communities of color, those in rural areas, and the elderly.
Beyond taxpayer expenditures, the human and societal consequences of kidney disease are profound, including destruction of personal aspirations, loss of household incomes and careers, destabilization of retirement, increases in Social Security Disability Income (SSDI) costs, and premature deaths.
New innovations are now available for detecting and intervening in kidney disease, so patients and professionals working together can delay and even avoid kidney failure. Yet, the problem is that our system remains focused on the repair of tissue and organ damage that has already occurred and doesn’t educate and empower Americans to avoid medical crises by undergoing screening and early preventative interventions.
In 2019, a historic Executive Order, Advancing American Kidney Health, charted a bold and

bipartisan-supported vision: earlier prevention, innovation, and patient-centered medicine. But since 2019, progress has stalled.
The U.S. Preventive Services Task Force (USPSTF), the federal body responsible for screening recommendations, has refused to update its approach to match national policy and innovations in disease detection. Despite overwhelming evidence on the burdens of kidney disease among patients and taxpayers, USPSTF has remained ineffective in the battle against it. The result? Millions remain undiagnosed until it’s too late, and taxpayers foot the bill for a reactive system that traps patients in dialysis, instead of working to preserve their kidney function.
Upstream kidney care is not just about cutting costs — it’s about human dignity and survival. A diagnosis of kidney failure should not come as a shock in an ER. Families should not face crisis decisions about dialysis or transplants in the middle of the night.
Our understanding of kidney disease must evolve to view it as both a healthcare and workforce issue. Too many working-age Americans are sidelined by disability and forced into SSDI because of late-stage kidney failure, while earlier screening and intervention could
keep people healthy, productive, and engaged in their communities.
We need leaders in Washington to act with urgency. That means replacing outdated advisory structures with bodies that include patients and frontline medical professionals. Other agencies like the U.S. Food and Drug Administration and the Centers for Medicare and Medicaid Services already incorporate patient input into decision-making. USPSTF should be no different.
As a healthcare professional, I know when we catch kidney disease upstream, we give patients years of health, independence, and hope. When we wait, we condemn them to crisis, suffering, and shortened lives.
America faces a stark choice. We can continue spending billions on dialysis and organ failure, or we can invest in education, prevention, and new innovations that give Americans better choices and access to the options that will help them manage kidney disease, and often avoid dialysis and an organ transplant altogether.

For people living with advanced chronic kidney disease, a novel therapy in clinical trials offers another option for treatment.
More than 35 million Americans are living with chronic kidney disease (CKD). For those who progress to advanced stages, treatment options are limited – most often dialysis, which carries significant drawbacks.
“Dialysis has a substantial impact on a patient’s quality of life,” noted Bruce Culleton, M.D., CEO of ProKidney, a leading late clinical-stage cellular therapeutics company. “While kidney transplantation offers better outcomes, the shortage of donor organs highlights the urgent need for new treatment options for patients with advanced CKD.”
Innovative therapy
CKD is classified into 5 Stages with Stages 1 and 2 indicating mild kidney injury and / or a minor loss in kidney function. In contrast, Stage 5 CKD indicates kidney failure where the majority of patients are treated by dialysis or kidney transplantation.
ProKidney has been working on an innovative treatment called rilparencel,
an autologous cell therapy made from the patient’s own kidney cells. The therapy is designed to stabilize kidney function in patients with CKD and type 2 diabetes but before the onset of Stage 5 CKD.
While kidney transplantation offers better outcomes, the shortage of donor organs highlights the urgent need for new treatment options for patients with advanced CKD.
Dr. Culleton outlined how it works:
“An interventional radiologist performs a standard kidney biopsy, taking a couple of small pieces of the patient’s kidney. That sample is shipped to our manufacturing facility in North Carolina where
cells from the biopsy are cultured and grown. We then select certain types of cells that we believe will have a positive impact on kidney function. Billions of those cells make up each dose of rilparencel.” Rilparencel is then injected into the patient’s kidneys by a trained interventional radiologist in an outpatient setting.
Rilparencel may utilize the patient’s own kidney repair mechanisms to reduce inflammation and fibrosis in the kidney and thereby preserve kidney function and delay the need for dialysis. Since the re-injected cells are the patient’s own cells, there’s no risk of rejection, and no need for immunosuppressive therapies or pre-treatments.
“We’ve treated close to 200 patients,” Dr. Culleton noted, “and we haven’t seen any serious safety issues directly related to rilparencel. The majority of patients also tolerate the procedures quite well.”
The FDA has given rilparencel a Regenerative Medicine Advanced
Therapy designation and recently confirmed an accelerated approval pathway for the therapy.
While the promise of rilparencel is exciting, the therapy is still being evaluated. ProKidney is currently enrolling patients in a Phase 3 clinical trial at sites across the United States, Mexico, and Taiwan. Topline results are expected in Q2 2027.
Dr. Culleton never forgets why ProKidney is doing this work: “Dialysis has a very high impact on not just the patient — it’s also their care team, their brother, sister, their mom or dad, their spouse. That’s why we want to transform the outlook for people living with advanced kidney disease – by giving them hope for an alternative to dialysis.”
Written by Jeff Somers
To learn more and check your eligibility for the Phase 3 clinical trial, visit hopeforckd.com

Primary care physicians play a pivotal role in preventing kidney disease progression, yet routine screening and clear communication remain inconsistent. Dr. Jay H. Shubrook, D.O., a member of the American Academy of Family Physicians, weighs in on how these providers can improve outcomes for their patients.
What are the biggest gaps in identifying and managing kidney disease in primary care?
There are numerous important opportunities for us to improve kidney disease management in clinical care. Primary care providers (PCPs) see the most people with kidney disease, but rarely is the visit focused on this. PCPs should incorporate asymptomatic screening of kidney disease in high-risk people. This starts with all people with hypertension or diabetes mellitus. Screen with both a blood and urine test. While most people at risk for kidney disease have had a blood test to check for the kidney flow, only about half have had the urine test to check the filtering capacity of the kidneys. Be clear in your communication with your patients. Often, we may soften our language or minimize abnormalities to not worry the patient. This only delays action to prevent further testing or treatment. Too many people find out that they have kidney disease at the time that they need renal replacement or have a complication of kidney disease.
Many people do not know that the diagnosis of chronic kidney disease (CKD) does not mean an inevitable decline to dialysis. In fact, only about 10% will ever need renal replacement therapies like dialysis. However, CKD increases the risk for cardiovascular disease, bone disease, hypertension, and heart failure. We have a lot we can do to help prevent the progression of kidney disease and in certain cases can help to reverse some of the damage. However, this is only possible if you seek care and get testing done.
Which early signs or risk factors should PCPs watch more closely?
Probably the most important thing I can share here is that the most common early symptom is nothing. Early kidney disease is silent and found on screening

blood and urine tests. Please do not wait for late symptoms like urinary changes, fatigue, or itching.
How can routine screening be improved to catch kidney disease earlier?
We need a national campaign. Know your kidney numbers. Since so many adults in the United States have more than one chronic disease, it is likely that most adults should have this screening at least annually. Since it involves blood and urine tests, we need PCPs to order them and strongly encourage the patients to get them done.
What impact does early intervention have on outcomes, and what practical steps can PCPs take now?
We can take several steps to prevent kidney disease and manage it once it occurs.
1. We can educate our patients about the diagnosis and all that can be done to prevent progression.
2. Maintaining a healthy weight or reducing excessive weight helps the kidneys.
3. Stabilizing blood pressure and glucose helps to prevent CKD.
4. Ask patients to check in with your medical team to make sure they are getting screened and that anything abnormal is explained to them and rechecked.

INTERVIEW WITH Dr. Jay H. Shubrook, D.O. Professor, Primary Care Department, Touro University California
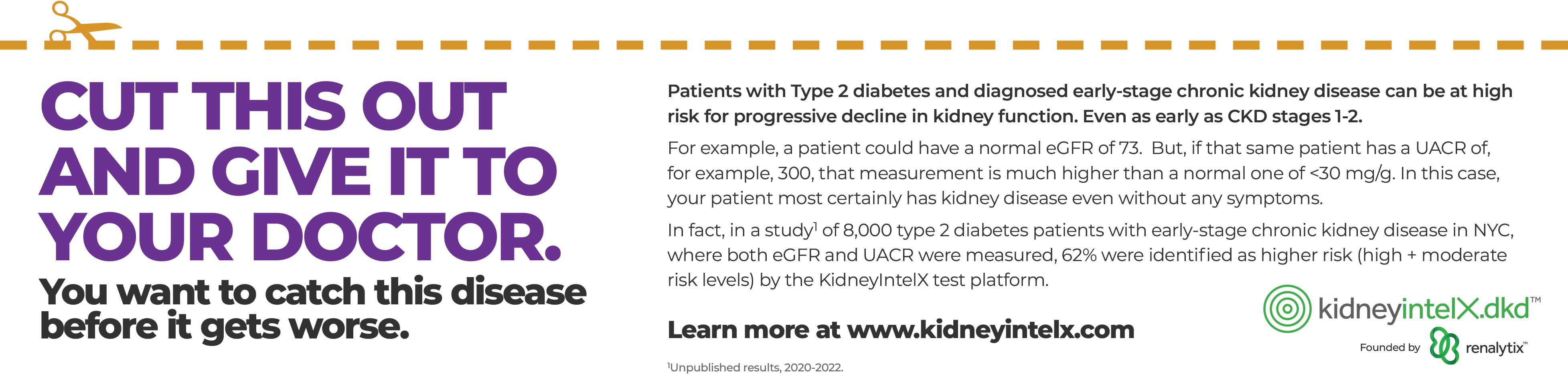
If you have type 2 diabetes, you could also have chronic kidney disease (CKD) and not even know it.
Approximately 40%1 of adult patients with type 2 diabetes will develop chronic kidney disease (CKD).
And if you’re one of these patients, your kidney disease could be progressing toward kidney failure and the need for dialysis or a transplant as we speak — even if you have no symptoms. In fact, most people have no symptoms in the early stages of the disease.
But there’s no need to panic. Just talk to your doctor about getting these two tests:
1. Get a UACR test to find out if you have early-stage CKD In the routine tests that your doctor orders annually, an eGFR is often used to determine how well your kidneys are functioning. Your doctor may have found your eGFR to be normal, if the reading was >60.
Even if your eGFR is normal, you could still have CKD. The only way to know for sure, is to get a simple urine test, a UACR, which detects early signs of kidney damage (i.e. protein in your urine).
That’s why the American Diabetes Association2 and the American Academy of Family Physicians3 both recommend adding the UACR test to each type 2 diabetes patient’s annual testing routine.
“Almost half of all adult patients with type 2 diabetes will be diagnosed with CKD,” said Michael Donovan, M.D., Ph.D., chief medical officer and laboratory director for Renalytix, an innovator in the kidney diagnostic space. “That’s why you need to find out right away by getting this simple urine test. The sooner you know, the sooner you can get the right treatment.”
2. Get the kidneyintelX.dkd blood test to understand your risk of kidney disease progression over the next 5 years If you have type 2 diabetes and are also diagnosed with early-stage CKD (stages 1-3b), you could be headed for dialysis.

INTERVIEW WITH Steve Coca, M.D. Nephrologist, Mount Sinai New York; Co-founder, Renalytix, and Co-Inventor, kidneyintelX.dkd test
That’s where the kidneyintelX.dkd test comes into play.
This simple blood test will tell you your level of risk (high, moderate or low) for progressing to kidney failure, which could require dialysis.
By finding out your level of risk early, your doctor can more appropriately target medications and lifestyle changes previously shown to be effective at

INTERVIEW WITH Michael Donovan, M.D., Ph.D. Chief Medical Officer and Laboratory Director, Renalytix
slowing or preventing CKD from worsening.

“If you could predict your future kidney health by taking a simple blood test, wouldn’t you? Especially if you could avoid dialysis,” said Steve Coca, M.D., a nephrologist at Mount Sinai New York, co-founder of Renalytix and co-inventor of the kidneyintelX.dkd test. “Well, now you can. Ask your doctor about this test.”
There’s no reason not to get the kidneyintelX.dkd test if you’re eligible (type 2 diabetes + CKD stages 1-3b).
1. The test is FDA-approved, so you can trust its accuracy.
2. It only takes one test for you to know your level of risk for the next five years.
3. If you have traditional Medicare or Medicaid, the test is covered.
4. If you have Medicare Advantage or another private insurance, you will only pay the in-network laboratory cost for testing. And we will talk to you first, if we learn that you will owe more than $50. You can always decline the test.
5. Even if you don’t have insurance, we have a Patient Assistance Program to assist you further, if needed.
Written by Renalytix
REFERENCES
1 https://www.mdpi.com/2673-8236/2/3/38#:~:text=One%20 of%20the%20most%20frequent,epidemiology%2C%20and%20 causes%20of%20DKD.
2 https://diabetesjournals.org/care/article/48/Supplement_1/ S239/157554/11-Chronic-Kidney-Disease-and-Risk-Management 3 https://www.aafp.org/pubs/afp/issues/2019/0615/p751.html#:~:text=Microalbuminuria%20is%20the%20earliest%20detectable,patients%20who%20have%20comorbid%20hypertension.
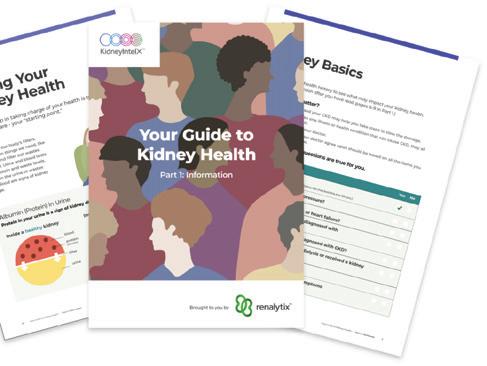






If you want to protect your kidney health, scan the QR code or go to kidneyintelx.com/ patient-guide, where you can get ONE FREE GUIDE TO KIDNEY HEALTH and ONE FREE WORKBOOK to help you have a conversation with your doctor. We’re also happy to answer any questions. Just call us toll-free at 1-833-393-7740
Justin Pham had dropped 40 pounds without trying. The 29-year-old e-commerce manager was sneaking naps at work, barely eating, and gasping for breath walking from his car to the office. Even his urine looked wrong — foamy and strange. It was 2020, and like many, Pham blamed COVID.
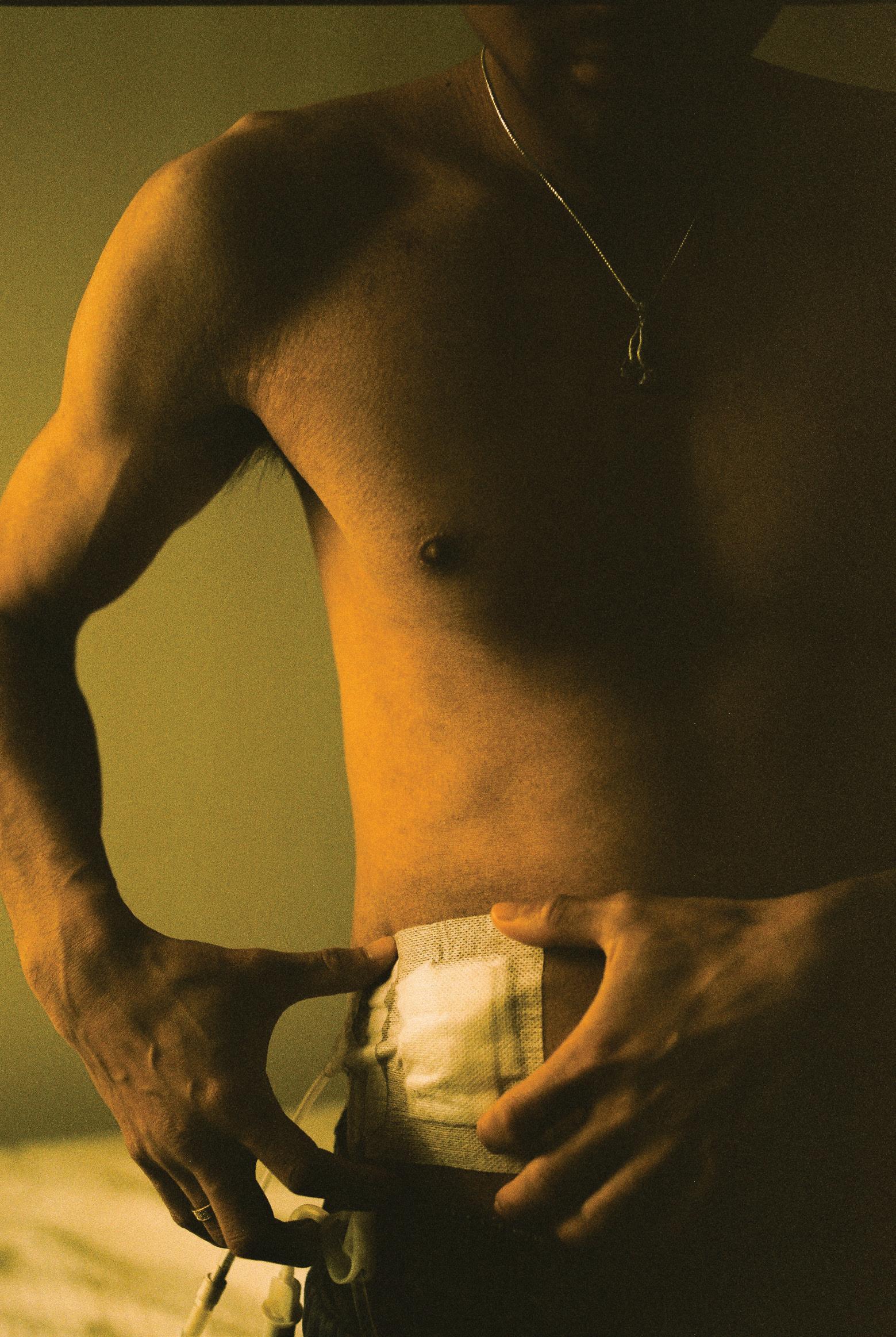
He was wrong. A routine blood test revealed the truth: complete kidney failure. “My doctor called me the next day while I was driving and said I needed to start dialysis right away,” Pham said. “He kept saying ‘pull over, call 911.’” Within an hour, Pham was in an emergency room with doctors inserting a catheter through his neck.
Pham’s story illustrates a critical gap in kidney care awareness. Chronic kidney disease (CKD) affects nearly 36 million Americans and often goes undetected until it reaches advanced stages.i Despite the prevalence of the disease, home dialysis, which could help preserve patients’ jobs, family time, and independence, is only utilized by 14.5% of dialysis patients in the United States.ii
Innovation offers another path Vantive, formerly part of healthcare company Baxter International, emerged as an independent company in 2025 with the singular focus of transforming vital organ therapies. Building on seven decades of experience in kidney care, Vantive aims to address what CEO Chris Toth calls “an under-recognized public health crisis” that will become the fifth-leading cause of death globally by 2040 if no action is taken.iii
“We view the patient we’re serving as our mother, father, brother, sister, or child,” Toth said. “We want them not just to survive chronic kidney disease, but to live longer, fuller lives. This philosophy drives our approach to care.”
For patients like Pham, Vantive’s home dialysis technologies represent more than medical equipment — they’re a pathway to a sense of normalcy. After six months receiving
dialysis in a center, Pham transitioned to at-home peritoneal dialysis (PD) with a user-friendly Vantive system that performs dialysis overnight while he sleeps.
“With PD, it’s on my time. If I want to go out to dinner or meet up with friends or be with family, I can come home late, and at worst, I’m just doing dialysis a little bit later,” Pham said.
We want them not just to survive chronic kidney disease, but to live longer, fuller lives. This philosophy drives our approach to care.
-Chris
Dialysis is necessary when kidneys can no longer filter waste from blood effectively. In-center hemodialysis depends on nurses and trained technicians, as well as specialized machines to pump blood through external filters under constant monitoring. Patients must travel to dialysis centers, typically three times weekly for four-hour sessions.iv
PD offers a different approach with flexible options: manual exchanges during the day or automated treatment overnight. Using the body’s own abdominal lining as a natural filter, PD enables patients to dialyze at home with portable equipment while gently and gradually removing fluid and toxins — a
process that more closely mimics how healthy kidneys actually work.v For people like Pham, who opt for automated PD while they sleep, the process typically takes 8-12 hours.vi
The impact on quality of life is measurable. Among working-age adults employed before dialysis, 68-73% of PD patients maintained employment at the same level compared to 57% of in-center hemodialysis patients.vii PD patients may have fewer restrictions on foods than hemodialysis patients.viii They also reported better quality of life scores than those on hemodialysis during the initial period after starting therapy, with differences persisting up to two years.ix
For the nearly 90,000 Americans waiting for a kidney transplantx — a process that typically takes three to five yearsxi — PD offers additional advantages: It can serve as an ideal bridge to transplant and is associated with favorable post-transplant outcomes, including lower risk of graft failure compared to hemodialysis.xii
From fear to confidence
While the benefits of home dialysis are clear, concerns about preventing infection and managing care at home may hold people back from exploring this option. Pham knows this intimately: “You kind of have to become your own nurse,” he acknowledged.
The antidote lies in comprehensive training combined with peer support. Pham spent a week and a half training with the equipment, building confidence through hands-on practice. But formal training was just the beginning. Seeing real people successfully manage their treatment on social media helped Pham feel confident he could do it, too.
Technology meets humanity
Vantive’s investment of more than $1 billion over five years in R&D and production capacity includes efforts to advance digitally enabled home dialysis.
xiii The Vantive system that Pham uses exemplifies this approach, as it automatically transmits treatment data like fluid volume, blood pressure, and weight to his care team while he sleeps. Beyond technology, Vantive is
constantly exploring opportunities to support patients throughout care. The company provides services and programs designed to allow patients to live life on their own terms — whether that means continuing to work or traveling the world.
Just because you need dialysis doesn’t mean your life stops.
-Justin Pham
The path to expanding home dialysis requires a multifaceted, patient-centric approach to care, particularly for communities that experience disproportionate rates of kidney failure. Asian Americans like Pham are 1.6 times more likely to develop kidney failure than white Americans, while Black and Hispanic populations face even higher risks.xiv Inclusive education materials and therapy demonstrations, peer support from patients who share similar backgrounds, and digital tools can all help patients make informed choices about their care.
Even when patients choose home dialysis, accessing it can be unnecessarily difficult. Vantive advocates for policies that both expand access and remove barriers to treatment. Supporting home dialysis requires integrating technology, services, and education into standard care — with reimbursement models that make it financially viable.
Today, Pham’s routine exemplifies the freedom PD can provide. He manages his freelance e-commerce business from home without worrying about dialysis center appointments. His gym sessions help him focus on the positive. “Staying mentally and physically strong is my way of fighting back,” he said.

His symptom awareness videos have garnered millions of views on TikTok (@platinumkidney), creating a community where those facing dialysis can find practical guidance and inspiration.
While awaiting a kidney transplant, Pham refuses to put his life on hold. “Just because you need dialysis doesn’t mean your life stops,” he said. “With PD, I can work, travel, spend time with friends — all on my schedule. I value my time more than anything.”
Pham’s story embodies Vantive’s mission: extending lives and expanding possibilities. As the company works to reshape kidney care through digital innovation and comprehensive support, patients like Pham demonstrate that dialysis doesn’t have to mean surrendering independence. For the millions facing kidney disease, that possibility alone makes the conversation worth starting.
Written by Vantive
To learn more about kidney health and peritoneal dialysis, visit pdempowers.com








Centers for Disease Control and Prevention. (2023). Chronic kidney disease in the United States, 2023 Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/ kidney-disease/php/data-research/index.html
ii United States Renal Data System. (2024). End-stage renal disease: Chapter 2 - Home dialysis. In 2024 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved from https://usrds-adr.niddk.nih.gov/2024/end-stage-renal-disease/2-home-dialysis
iii Foreman, K. J., Marquez, N., Dolgert, A., et al. (2018). Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016–40 for 195 countries and territories. The Lancet, 392(10159), 2052-2090.
iv National Institute of Diabetes and Digestive and Kidney Diseases. Hemodialysis. Updated 2018. Accessed October 7, 2025. https://www.niddk.nih.gov/health-information/kidney-disease/ kidney-failure/hemodialysis
v Blake, P.G., & Brown, E.A. (2023). Peritoneal Dialysis Prescription and Adequacy in Clinical Practice: Core Curriculum 2023. American Journal of Kidney Diseases, 81(1), 100-109. vi Cleveland Clinic. (2017, May 25). Dialysis: Types, How It Works, Procedure & Side Effects. https://my.clevelandclinic.org/health/ treatments/14618-dialysis
vii Muehrer RJ, Schatell D, Witten B, Gangnon R, Becker BN, Hofmann RM. Factors affecting employment at initiation of dialysis. Clin J Am Soc Nephrol 2011;6(3):489-496. doi:10.2215/ CJN.02550310
viii National Institute of Diabetes and Digestive and Kidney Diseases. Eating & nutrition for peritoneal dialysis. Updated August 2017. Accessed October 7, 2025. https://www.niddk.nih.gov/ health-information/kidney-disease/kidney-failure/peritoneal-dialysis/eating-nutrition ix Jung HY, Jeon Y, Park Y, et al. Better quality of life of peritoneal dialysis compared to hemodialysis over a two-year period after dialysis initiation. Sci Rep. 2019;9:10266. doi:10.1038/s41598019-46744-1
x United Network for Organ Sharing. 90,000 people are waiting for a kidney. Published February 20, 2025. Accessed October 7, 2025. https://unos.org/news/90000-people-are-waiting-for-akidney-heres-one-way-to-get-them-a-kidney-faster/ xi National Kidney Foundation. The kidney transplant waitlist. Accessed October 7, 2025. https://www.kidney.org/kidney-topics/ kidney-transplant-waitlist
xii Ngamvichchukorn T, Ruengorn C, Noppakun K, et al. Association between pretransplant dialysis modality and kidney transplant outcomes: a systematic review and meta-analysis. JAMA Netw Open 2022;5(10):e2237580. doi:10.1001/jamanetworkopen.2022.37580
xiii Vantive. (2025, January 15). Vantive to invest more than $1 billion in advancing kidney care and vital organ support through digitally-enabled therapies [Press release].
xiv National Institute of Diabetes and Digestive and Kidney Diseases. Kidney disease statistics for the United States. Updated 2024. Accessed October 7, 2025. https://www.niddk.nih.gov/ health-information/health-statistics/kidney-disease
In 2019, Valerie noticed a decline in her kidney function during a routine visit to her primary care physician. Repeated tests offered no answers, so she carried on with her life.
By 2022, Valerie’s kidney function had sharply declined. A nephrologist diagnosed severe anemia and borderline hypertension, prescribed medication, and scheduled a six-month followup. At that visit, he recommended a kidney biopsy, saying, “It’s the only way to know what’s causing your kidney disease.”
Wary of the procedure due to a bleeding condition, Valerie hesitated. She was curious about genetic testing, but since her nephrologist never mentioned it, she didn’t ask.
When severe fatigue set in during summer 2024, Valerie sought a second opinion. After reviewing her history and family kidney disease, the new nephrologist recommended genetic testing.
Six years and $20,000 later, Valerie was diagnosed with a rare genetic kidney disease: autosomal dominant tubulointerstitial kidney disease (ADTKD).
“I could have been genetically tested and known much earlier, saving time, money, and a whole lot of frustration!” Valerie said.
ADTKD is a chronic kidney disease caused by mutations that produce abnormal proteins, damaging the kidneys’ tubulointerstitium and leading to progressive loss of kidney function, ultimately requiring dialysis or transplant.
Key features include:
• Autosomal dominant inheritance: Affected individuals have a 50% chance of passing it to each child.
• Bland urinary sediment: Since it affects the tubulointerstitium and not the glomerulus, urine usually has no blood or protein.
• Variable progression: Age of onset and decline rate differ, even within the same family. Some reach end-stage kidney disease in their 20s, others in their 70s or 80s.
Treatment and research
There is currently no treatment for ADTKD. However, research originating in Dr. Anna

Greka’s lab at the Broad Institute at MIT and Harvard has helped identify a potential therapy, with plans for a clinical trial in the near future.
ADTKD is underdiagnosed due to limited awareness. Some researchers estimate that over 1 million chronic kidney disease patients worldwide have ADTKD, including 75,000-100,000 patients in the United States, making it the second most common genetic kidney disease in the nation, after polycystic kidney disease.
The Rare Kidney Disease Foundation (RKDF) is committed to halting the devastating impacts of ADTKD across generations by:
1. Raising awareness about ADTKD, the importance of genetic testing, and promising treatments on the horizon.
2. Encouraging patients with symptoms to seek a genetic diagnosis and join the



International ADTKD Registry at Wake Forest University School of Medicine.
3. Providing a supportive community of patients, families, nephrologists, and researchers.
All RKDF members are volunteers and have ADTKD or a family member affected, giving us a firsthand understanding of the urgency for a treatment, for ourselves, our children, and future generations.
Genetic testing is essential
For patients like Valerie, the road to diagnosis can be long and expensive. Advances in research, upcoming clinical trials, and a growing network of support make this a critical time to recognize the power of genetic testing in chronic kidney disease. Awareness saves time. Diagnosis changes lives. Together, we can transform the future of ADTKD for generations to come.

NephCure is the only kidney organization solely focused on nephrotic syndrome, FSGS, IgAN, and other rare, protein-spilling kidney diseases.
Since its founding in 2000, NephCure has invested more than $40 million in research and pushed for progress in innovation, awareness, and access to treatments.
Whether you are a patient, caregiver, or nephrologist, NephCure is here to serve as your partner and trusted resource.
For physicians: Make NephCure part of your patient’s treatment plan
Whether you see one or dozens of glomerular disease patients, we know keeping up with the rapidly evolving treatment landscape and ensuring patients receive wrap-around support is challenging. Let us help.
When your patient contacts us, we will provide personalized guidance on every aspect of their disease journey, including:
• Disease education
• Diet and nutrition
• Mental health
• Peer support
• Insurance coverage
• School support services
Also, our online resources about approved therapies and active clinical trials are helpful tools to support physician-patient shared decision-making.
“I refer all of my patients with glomerular disease to the NephCure website and highlight it as a resource and community,” said Dr. Myda Khalid, associate professor of clinical pediatrics and program director of the Pediatric Nephrology Fellowship Program at the Indiana University School of Medicine. “NephCure helps them know they are not alone, and many patients are relieved to find of a way they may be able to give back to others with similar struggles.”
By making NephCure a part of your glomerular disease patient’s treatment plan, you can increase patient adherence and improve outcomes.

trials, drug approvals, and community awareness
NephCure helps them know they are not alone, and many patients are relieved to find of a way they may be able to give back to others with similar struggles.
For patients with RKD: Lighten the load with help from NephCure
A rare kidney disease (RKD) diagnosis changes everything, but you don’t have to navigate this journey alone.
With more than 40,000 patients engaged in our community, NephCure:
• Fosters connections through monthly virtual support groups and in-person events
• Ensures your voice is heard among government officials, industry partners, and other key stakeholders
• Paves the way for more clinical
We also offer direct support through:
• One-on-one personalized patient navigation services to help you understand your options and navigate challenges
• A clinical trial matching tool that connects you directly with RKD studies offering access to the latest treatment options
• A searchable list of 200 NephCure Specialists; doctors who routinely treat rare, protein-spilling kidney disease
“I have never experienced such a passionate and driven community like NephCure,” said Lizette G., whose son has an RKD. “To the doctors, parents, and patients... I felt like I stepped into a world that I never knew existed. Hearing and seeing what doctors are
doing to find better treatments, hearing testimonies from parents and children, finding out that I don’t have to be alone in advocating for my son — just wow! I now have angels with me with NephCure.”
At NephCure.org/Resources, you can access a robust library of educational content including disease-specific handbooks, recorded webinars, kidney-friendly cookbooks, informational guides, and more!
You are not alone in the fight against rare, protein-spilling kidney disease. Learn more and get connected at NephCure.org or reach us at info@nephcure.org.


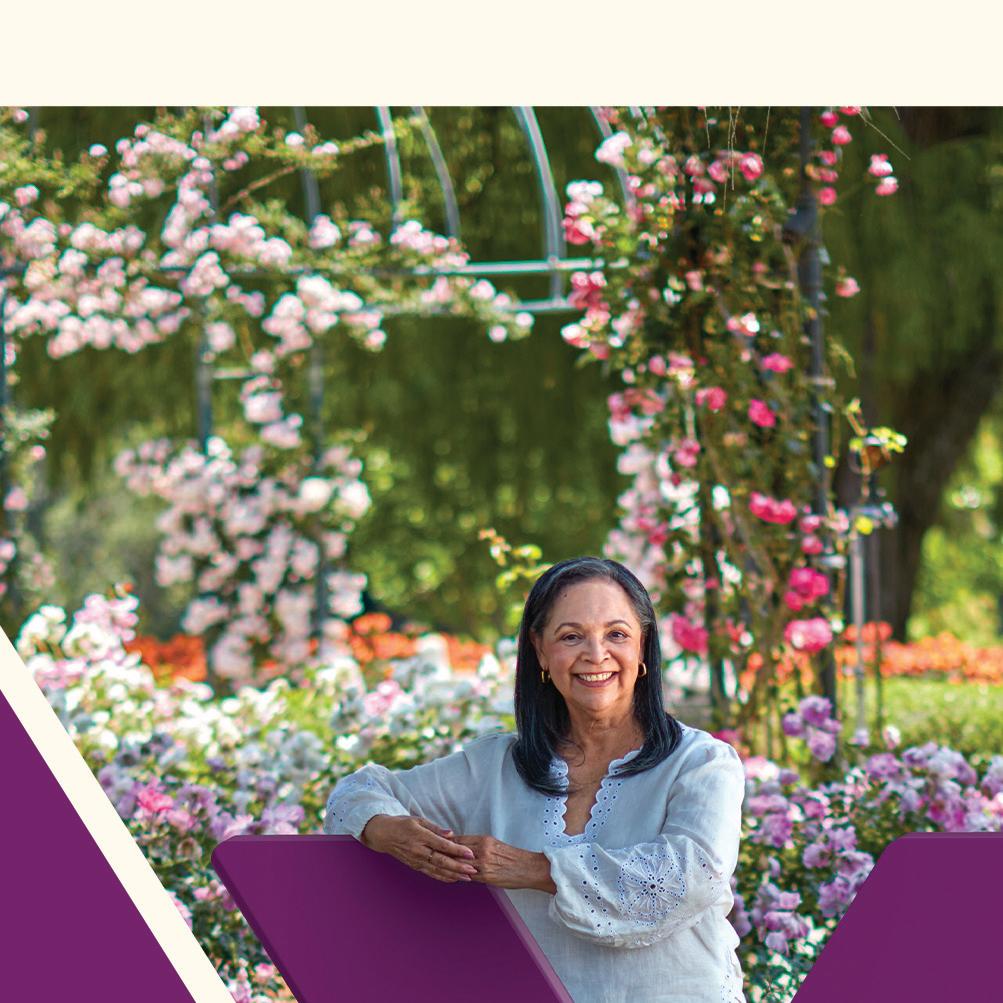
Retired NBA star Alonzo Mourning played 15 seasons of professional basketball, is a gold medal Olympian, and an NBA champ. But he’s not done. Now, he’s embracing his next role as a health advocate.
Mourning, a seven-time NBA All-Star who played center and power forward, was at the top of his game when he was diagnosed with a rare kidney disease.
“I had just won the gold medal with Team USA in the 2000 Summer Olympics in Sydney,” he said. “Coming back home, I began to notice troubling symptoms, extreme tiredness, and alarming swelling throughout my body. I basically chalked it up to all the grueling training I did that summer and the travel schedule.”
During a routine physical to prepare for the upcoming season with the Miami Heat, the team’s doctor noticed signs of kidney disease and conducted follow-up tests. He diagnosed Mourning with focal segmental glomerulosclerosis, a rare kidney condition that’s a form of APOL1-mediated kidney disease, an inherited kidney condition caused by variants (changes) in the APOL1 gene.
Good days and bad days “I thought my life was over,” said Mourning, who also played with the Nets and Hornets during his career. “I was just so ignorant to all of this, because I didn’t know people could live with kidney disease and people can get transplants.”
In 2003, Mourning received a kidney transplant from his cousin, Jason Cooper. He overcame a lot of pain, swelling, and stiffness to prepare his body for a return to professional sports, including eight months of training. He resumed his basketball career, including winning the 2006 NBA championship with the Miami Heat. He’s been vice president of Player Programs for the Miami Heat for more than 15 years.
He receives routine checkups every six


months and stays as healthy as he can.
“I have my good days and bad days, like everybody else,” Mourning said. “I don’t have to have dialysis and have this kidney in me still functioning.”
Still, Mourning has had health challenges. He was recently diagnosed with atrial fibrillation and had an ablation on his heart. In 2024, he was diagnosed with Stage 3 prostate cancer. He had his prostate removed and he’s cancer-free.
The Hall of Famer says it’s important to know your family history and to get genetic testing. For example, Mourning’s kidney condition is inherited, and people of African descent are at higher risk for the APOL1 variant.
Mourning contributed his DNA as part of the study that showed that variants in the APOL1 gene are associated
with a higher rate of severe kidney disease in African Americans.
He created a website, PowerForwardTogether.com, with Vertex Pharmaceuticals to empower people with kidney disease to get informed, especially about the APOL1 gene.
“I’m
a strong believer that in every adversity, there’s a seed of equivalent benefi t
Mourning encourages everyone to be proactive about their health by finding a doctor they trust and getting regular checkups. He suggests people get second or third opinions, too, as needed.
He also urges healthcare providers to take the time to get to know their patients. When patients and providers get comfortable, they can have honest conversations about health.
Mourning is grateful for his health and is honored to share his advice and support with others experiencing kidney disease and other health challenges.
“I’m a strong believer that in every adversity, there’s a seed of equivalent benefit,” he said. “I went through what I went through, to be a spokesperson, and that’s the blessing in all of this — to be a voice for the voiceless.”
Written by Kristen Castillo

Years of taxpayer investments in science and research have positioned America as the global leader in kidney medicine, transplantation, and breakthrough technologies that prevent or delay disease progression.

Sponsored
The American Kidney Fund wants to help you Know Your Kidneys. Here are four factors that could mean you are at a higher risk of developing kidney disease.

If you have one or more of these risk factors, take charge of your kidney health. Find free resources at KidneyFund.org/know-your-kidneys



Four years ago, when our 21-year-old son stepped forward to become a living kidney donor for his 19-yearold brother, it was a saliva kit test for hundreds of genes associated with kidney diseases that finally put us and his medical team at peace with his decision. The test confirmed he had not inherited my rare genetic kidney disease, the one that had significantly affected our youngest son’s life since infancy. Both definitively ruling out risk and identifying the root cause of symptoms are tremendously empowering for patients and families.
I encourage clinicians to forego concerns over sharing genetic results with patients. Being provided a scientifically confirmed diagnosis can be a gift leading to clearer treatment plans, better outcomes, and empowered patients. Genetic
In my role at Alport Syndrome Foundation, I’m in touch daily with newly diagnosed individuals. My story of misdiagnosis for 40+ years, resulting in misdiagnosis for my
youngest son, is not uncommon in our patient community. Neither is being denied a request for renal genetic testing by a physician.
Recently, I was honored to be a speaker for a group of professionals in drug development. After sharing my family’s journey with Alport syndrome, a nephrologist remarked that I was likely in the minority, that certainly most patients would not welcome genetic testing, which could lead to a medical diagnosis for a rare disease with currently no FDA-approved treatments or cure. My response: “If it were your child or grandchild, would you want to know?” With Alport syndrome, wouldn’t he want to know the genetic type and variant

Accessia Health® is a national charitable patient assistance organization that helps people afford their healthcare costs while navigating the complexities of living with a rare or chronic health condition.
Services Include
• Financial Assistance for:
• Health insurance premiums
• Screening and diagnostics
• Medication copays
• Travel costs

• Other medical expenses
• Free Legal Aid for SSDI & SSI Claims
• Case Management Navigation
• Educational Programs


to better understand risk for disease progression, evaluate recommended off-label treatment options, be monitored for associated hearing loss and eye conditions, understand who else in the family was at risk, participate in research and/or clinical trial opportunities, and get connected to the most knowledgeable clinicians and a group of other patient families? Perspective shifts when your own family is affected. He took a moment before acknowledging that he would indeed want to know.







Scan to learn how we support people living with Kidney Stones.



With renal malignancies on the rise, patients and providers must understand evolving diagnostic tools and management options.
Renal malignancy is the seventh most common cancer in the United States, accounting for almost 80,000 new cases in 2025. The incidence of renal malignancies has steadily risen in recent decades, partially due to increasing utilization of cross-sectional imaging. This has resulted in a stage shift with localized disease representing the majority of newly diagnosed renal malignancies. In early localized disease, the primary management options are active surveillance (AS), thermal ablation, or partial nephrectomy.
Active surveillance
AS is a safe option in the appropriately selected patient with a clinical T1a renal mass. The American Urological Association (AUA) recommends cross-sectional abdominal imaging every three to six months for two years with longer intervals afterward. Studies have used a tumor size of 3 centimeters, growth rate >0.5 cm/year, and stage progression as indications for intervention.
Nephrectomy
Partial nephrectomy is the preferred treatment for cT1a renal masses whenever technically feasible. The AUA particularly emphasizes nephron-sparing approaches in patients with chronic kidney disease, multifocal tumors, hereditary syndromes, solitary kidneys, or younger patients.
Thermal ablation
Percutaneous thermal ablation is also a viable nephron-sparing alternative for appropriately selected patients with tumors less than 3-4 centimeters. A variety of energy options currently exist, including cryoablation, microwave ablation, and radiofrequency ablation.


Renowned transplant surgeon Dr. Robert Montgomery warns that long-term organ transplant survival depends on safer immunosuppressants and stronger antiviral defenses.

Why are kidney transplant patients more vulnerable to infections like COVID-19?
Kidney patients tend to be on more intense longterm maintenance immunosuppression drugs than other organ transplants, and this can affect their response to vaccines. Many will not develop neutralizing antibodies like non-immunosuppressed individuals, reducing their immunity to viruses like COVID-19 and increasing the severity and length of illness when they have a COVID-19 infection.
How does having a weakened immune system impact transplant patients in their day-to-day lives and long-term health?
People who are on immunosuppressive therapy, which is required for all organ transplants, are more likely to become infected with COVID-19, the resulting illness tends to be more severe and last longer, and they tend to shed the virus for longer periods of time. Immunosuppression makes any virally driven diseases — including certain cancers — and infectious diseases in general more likely. Cancers and infections become a major long-term threat to their health.
What kinds of medical innovations are most needed to better protect immunocompromised patients?
More effective preventive, prophylactic drugs and more potent treatments (when they become
infected) are most needed. We need new immunosuppressive drugs that have less toxicity and are more narrow in terms of activity — less permissive in terms of increasing susceptibility to infections and cancers, but still effective for preventing rejection. Also, we need approaches that create “tolerance” in which the organ is accepted and not attacked by the recipient’s immune system, and there is no need for immunosuppression.
How do you see advances in infection prevention and treatment shaping the future of transplant care?
Organ transplantation has become highly effective in short-term survival (one to three years) but has not shown the same progress in terms of long-term survival (five to 10 years). The immunosuppressive drugs have lots of side effects, many of which patients feel are intolerable or life-threatening long term. They also have toxicities (causing kidney failure) and increase the likelihood of serious infections and cancers.




Kidney disease is a growing public health crisis, yet kidney donation offers hope, restores health, and saves thousands of lives each year.





Every day in the United States, 17 people die waiting for an organ transplant, and 85% of these patients are waiting for a kidney.
Kidney donation remains one of the most powerful ways to save lives and restore health. A single kidney donor can change the trajectory of a patient’s life, freeing them from dialysis and offering a chance to return to work, family, and community. In 2024, more than 27,000 Americans received kidney transplants. Behind these transplants is the extraordinary generosity of thousands of donors and their families, whose decision brought hope amid hardship.
Recent analyses of donation practices by the Health Resources and Services Administration identified concerns with the management of potential organ donors. While these findings emphasize the need for improvement, it is crucial to remember that these cases are rare. The U.S. organ donation system enables tens of thousands of safe, lifesaving transplants each year. Unfortunately, public misperceptions about safeguards and procedures can discourage individuals from choosing to register as donors, limiting kidney availability when it is needed most. With over 100,000 Americans waiting for an organ transplant, public trust is critical. To understand recent discussions about donation, it is helpful to know that there are two primary types of deceased donation: donation after brain death (DBD) and donation after circulatory death (DCD).









In DBD, hospital physicians, who are not part of the donation or transplant teams, determine that a patient’s brain has completely stopped functioning. Once death is confirmed through multiple clinical exams and tests, and consent is obtained for organ donation, the patient is evaluated as a potential organ donor. If suitability for organ donation is confirmed, the organ recovery surgery proceeds, ensuring that the kidneys and other organs remain viable for transplant.
In DCD, the donation process is different. When a critically ill patient has sustained a significant brain injury with a poor prognosis and has not been declared brain dead, the family decides to withdraw support and allow for comfort care measures. Once this decision has been made, the family is approached for the consideration of organ donation. If the family gives consent, then the evaluation process for organ donation begins.
Once the suitability for organ donation is confirmed, medical support is withdrawn and comfort care is provided. When the patient’s circulation stops naturally and death is confirmed by a physician separate from the recovery team, surgeons begin organ recovery. If death does not occur within the necessary timeframe, donation does not proceed, and the patient continues to receive comfort care.
The key distinction is how death is determined, but in both DBD and DCD, the decision is made by


physicians independent of the recovery team. Both pathways save lives, with DCD now accounting for 45% of all deceased donations, according to the Organ Procurement and Transplantation Network.. This pathway has become essential as diabetes, hypertension, and other conditions increase the need for kidney transplantation.
Recent media reports on DCD practices highlight troubling cases but also show that oversight is functioning; problems are identified, investigated, and corrected; and lessons are applied to improve the system. These cases, while concerning, represent exceptions in a system that safely enables thousands of kidney transplants annually. Rather than undermine confidence, these reports should motivate us to strengthen policies and protections, ensuring families feel confident their loved one’s gift is honored with integrity.
As kidney disease grows alongside an aging population and rising rates of diabetes and obesity, the need for transplantation will only intensify. The solution is not to limit donation but to improve systems, align practices across hospitals, and ensure ethical, transparent processes.
Written by David P. Foley, M.D., President, American Society of Transplantation; Professor of Surgery and Folkert O. Belzer Chair, Division of Transplantation, University of Wisconsin School of Medicine and Public Health
Game-changing technology is revolutionizing organ transplantation, and it all began with a childhood wish. When Xiaoxi (Sofie) Wei was young, her grandfather needed a liver transplant. But he didn’t get one and later passed away.
Icould not save my hero, and I felt very sad,” Wei said. So, when her mother, a physician, told her that time was the reason her grandfather didn’t get a transplant, Wei decided to become a biohacker to solve this time issue for organs.
She studied biotechnology, earned her Ph.D. in chemistry, and co-founded X-Therma Inc., a biotech company that’s revolutionizing the preservation of organs and other “living” medicines to advance the future of transplantation and regenerative medicine.
Eleven years later, X-Therma is poised to change the world of transplantation.
“You have time” Currently, more than 107,000 Americans are waiting for an organ transplant, according to the United Network for Organ Sharing (UNOS). Timing is crucial with transplantation.
UNOS says kidneys can only be viable for transplantation within 24 hours of harvesting. Extending this window requires effective preservation at low temperatures. Until now, organs have mostly been stored at 2-4 degrees C in ice coolers, which only keeps the organs alive for a matter of hours.
New technology developed by Dr. Wei and X-Therma can preserve organs for longer periods at lower temperatures. X-Therma’s next-generation organ preservation system, called XT-ViVo® and TimeSeal®, can enable multi-day, ice-free organ preservation at subzero temperatures.
“Biological time limitations are no longer a given,” said Dr. Wei,
noting the company’s motto is “You have time.”
The impossible becoming possible
While subzero ice-free organ preservation once seemed like science fiction, it’s now achievable.
“We’re demonstrating something impossible becoming possible,” Dr. Wei said.
While frozen organs aren’t viable for transplantation, Dr. Wei wondered, “Can we come up with some super-effective antifreeze that is non-toxic so we can safely preserve the organs without the freezer burn?”
The X-Therma team drew inspiration from Nature to find a way to preserve organs at subzero temperatures but without freezer burn. That meant looking at how arctic species hibernate during harsh conditions and survive.
For example, the arctic squirrel can hibernate at almost -4 degrees C for nine months in the winter, with their heart nearly stopped.
“They’re basically being frozen, but not really frozen, and then they can come back to life nine months after,” Dr. Wei said.
The X-Therma team developed novel biomimetic molecules, called peptoids, that mimic the function of antifreeze proteins to safely preserve organs at -5 degrees C. Along with the smart transporter TimeSeal®, the cold tech platform extends organ preservation time from hours to multiple days under precise monitoring of temperature, storage duration, and location, without the need of external power, blood, or oxygen. In 2022, the FDA granted Breakthrough Device Designation to XT-ViVo® and

TimeSeal® for human kidney transplant preservation up to 120 hours.
Milestones
The technology is already a success. A surgical research team from Johns Hopkins University School of Medicine removed a kidney from a pig, preserved it at subzero temperatures for 48 hours, during which it was transported via commercial aircraft to Austria, where its viability and functionality was assessed and demonstrated at Medical University of Innsbruck. They repeated that transatlantic trip 10 times within a year (as of Sept. 2025), with preservation times ranging from 48-72 hours. As proof of concept of the technology, the team performed a life-supporting transplant in a pig, with the kidney maintaining normal renal function for 200 days post-transplant after 72 hours ice-free subzero preservation.
Benefits
Since this new organ cryopreservation system provides added
time for transplantation, providers and patients aren’t rushed. Patients may have better health outcomes, including less organ rejection. It may help eliminate the organ waiting list, increase the number of organs available for transplant, enable organ sharing worldwide, and significantly reduce organ waste.
Future applications
Dr. Wei is confident that in the years to come, X-Therma’s technology may be used for cell transplants, cell and gene therapy, precision oncology, and longevity applications, such as joint repair.
“With this platform, this is just the beginning,” she said.
Written by Kristen Castillo
Learn more about X-Therma’s organ and regenerative medicine preservation at x-therma.com


Chief medical officer of the United Network for Organ Sharing (UNOS), Dr. Andrew Klein, a liver transplant surgeon with nearly four decades of experience, shares how UNOS is working to save more lives through technology and reforming the system.
How many people in the United States are waiting for a kidney transplant?
As of mid-September 2025, nearly 93,000 people in the United States were waiting for a kidney transplant. Surgeons performed nearly 28,000 kidney transplants last year, but still, 11 people die every day waiting for a kidney.
What are some of the changes UNOS would like to see happen in the system?
First, the adoption of automated electronic deceased donor referrals would make it easier for hospital staff to report potential organ donors and would reduce errors.
Second, organs that are flown commercially from the site of donation to the location
of the transplant recipient should not be relegated to the cargo area of the aircraft, which is the current practice. They should be transported in the main aircraft cabin to ensure better handling.
Finally, a national tracking system should be adopted to prevent organs from being lost, delayed, or damaged. UNOS has developed an Organ Tracking Service that provides real-time location data for organs in transit. Solving these logistical challenges are important steps toward reducing non-use of organs.
What else is UNOS doing to maximize the benefit of donated organs?
UNOS is working to develop AI models to
Sponsored
For people with end-stage kidney disease, a transplant isn’t just a treatment — it’s a lifeline.
Compared to long-term dialysis, kidney transplantation offers better outcomes, improved quality of life, and renewed hope. Yet for one group of patients, that hope often remains frustratingly out of reach.
These are highly sensitized patients, individuals whose immune systems are primed to reject most donor kidneys due to previous transplants, blood transfusions, or pregnancies. Their bodies are ready to fight off what could otherwise be a life-saving organ. As a result, they face longer wait times, fewer matches, and limited access to care.
But the challenge goes deeper than biology.
Many patients don’t even know they’re highly sensitized. The key test, cPRA (calculated panel
reactive antibody), which identifies levels of sensitization, is often done too late in the care journey. Without early testing and clear communication, patients miss critical opportunities to be referred to specialized transplant centers that could offer them a chance.
The system is complex. The path is unclear. And the stakes are high.
To change this, we need coordinated action across the transplant community, including:
• Standardizing early cPRA testing
• Improving education and communication around results
• Strengthening referral pathways to specialized centers
• Ensuring the Kidney Allocation System continues to support equitable access
improve decision-making and place more organs. One tool, called offer filters, analyzes a transplant hospital’s historical organ acceptance data and automatically removes offers that are not a good match for that program so the kidney can be placed with a patient more quickly, leading to better transplant outcomes.
We are also using AI to convert standard imaging data, such as CT and MRI scans of an organ, into 3D models, which could be used to “virtually” transplant it into a potential recipient.
To register as an organ donor, visit registerme.org.


At Hansa Biopharma, we are committed to advancing transplant science and addressing the gaps that leave highly sensitized patients behind. These patients deserve more than hope, they deserve a system that works for them.
Written by Hansa Biopharma

Acute kidney injury (AKI), or acute worsening of kidney function, has no approved therapy, and yet its effects can be severe. For example, even milder forms of AKI can lead to proteinuria, hypertension, or chronic kidney disease (CKD).
Chronic kidney disease (CKD) itself is linked with a higher risk of heart disease and mortality. In particular, 1 in 4 patients with community-acquired AKI go on to develop CKD.
Affecting patients hospitalized for a variety of reasons, AKI has an incident rate between 14.7% and 31.5%.
Research shows 80% of AKI cases in lower- and lower-middle-income countries were community-acquired. In these countries, mortality rates from AKI ranged from about 12-15%. Most of those patients had no major comorbidities and were young without prior health issues.
The following 5R approach from the International Society of Nephrology can help providers achieve primary and secondary prevention of AKI, specifically in low-resource communities:
1. Risk assessment: Providers can use risk scores to predict AKI risk, and then identify risk factors that can be improved.
2. Recognition: A prompt diagnosis of AKI is key. This can be done with sequential serum creatinine and urine output. Point-of-care tests and diagnostic tools should be used if available.
3. Response: Providers should respond with proper interventions
Sponsored
for incipient and established AKI. Those interventions may include: identifying and treating sepsis when infection occurs; avoiding nephrotoxic drugs; managing protocol-based fluid and blood pressure; and figuring out the cause of AKI, treating related complications, reviewing the patient’s medication doses, and adjusting the patient’s fluid prescription as needed to prevent harm.
4. Renal support: Kidney replacement therapy (KRT) can be utilized in AKI, and ideally in a timely manner. Educating and training personnel for KRT is imperative.
In low-resource communities, peritoneal dialysis is an effective option. Hemodialysis may also be available in these settings.
5. Rehabilitation: After patients with AKI are discharged, providers should test their kidney function and look for signs of damage, take their blood pressure, conduct a urine exam, and perform medicine reconciliation. Patients should also be educated on reducing further exposure to AKI risk factors as part of their post-discharge care.
Written by Melinda Carter
Acute kidney injury (AKI) is a common, often fatal complication for ICU patients, yet no approved therapies exist today. CalciMedica’s investigational drug Auxora™ has shown promise in early trials, dramatically reducing mortality.
Acute kidney injury (AKI) is a devastating and all-too-common complication facing intensive care patients. “Of the millions of people who come through the ICU every year, about half will develop AKI,” shared Dr. Sudarshan Hebbar, chief medical officer at CalciMedica, Inc. (Nasdaq: CALC). “Once the kidneys are severely damaged, the mortality rate can climb above 50%.” Survivors often face lifelong risks of chronic kidney disease, heart disease, and other health complications. Despite its prevalence, there are no approved therapies to prevent or treat AKI. Doctors can only offer supportive medical care — such as managing fluids and blood pressure — in an effort to treat AKI. “There’s a significant unmet need,” Dr. Hebbar underscored.
CalciMedica’s investigational drug Auxora™ may fill that need. It works by calming inflammation and directly protecting organ tissue from further damage. “This sort of broad spectrum drug that affects multiple pathways involved in the pathophysiology of the disease hasn’t really been developed before,” Dr. Hebbar explained.
In a study of 261 patients hospitalized with severe COVID-19 pneumonia, Auxora was associated with a 56% relative reduction in mortality compared with placebo at 30 days — and the impact was even greater for patients who also had AKI. In this subgroup, Auxora was linked to a 63% relative reduction in mortality. Encouraged by this insight, the team began a Phase 2 trial in 150 patients with AKI and respiratory failure. As the team awaits the results expected in early 2026, they are already
preparing a Phase 3 trial, potentially initiating later that year.
Dr. Hebbar hopes the medical community will share his team’s excitement, and lend a hand: “We have the scientific evidence. What we need now is support from the community. I hope clinical trialists will be enthusiastic about helping us prove that this drug works and can save lives.”
Written by Emily Rose