
2025 IMF PATIENT AND FAMILY SEMINAR
CHICAGO, IL

OCTOBER 3 & 4, 2025
Thank you to our sponsors!











IMF PATIENT AND FAMILY SEMINAR
CHICAGO
FRIDAY AGENDA





OCTOBER 3 & 4, 2025
Thank you to our sponsors!













Presentation Slides: Are available by scanning the QR code, Instructions are on the QR code handout on each table.
Program Evaluations: Please be sure to complete your program evaluation and return your evaluations at the end of the program or on your way out.
Restrooms: Turn left exiting the meeting room and bathrooms are on your left before the lobby Badge Holders: Please return your badge holders and we can recycle them

Wifi: Network – Marriott Bonvoy Conference, Password - patient104
Parking: Onsite parking in the South Lot is complimentary
We greatly appreciate your time and feedback!






S. Vincent Rajkumar, MD
IMF Board Chair


Thomas Martin, MD
UCSF, Helen Diller Family
Comprehensive Cancer Center


Wee Joo Chng, MD
National University of Singapore


María-Victoria Mateos, MD, PhD
University of Salamanca


Vania Hungria, MD, PhD Santa Casa de São Paulo


Joseph Mikhael, MD, MEd, FRCPC, FACP IMF Chief Medical Officer


Sigurður Yngvi Kristinsson, MD, PhD
University of Iceland


Philippe Moreau, MD
University Hospital of Nantes


Shaji Kumar, MD Mayo Clinic


NIkhil Munshi, MD Dana-Farber Cancer Institute



Sagar Lonial, MD, FACP
Winship Cancer Institute, Emory University

Jesús San Miguel, MD, PhD
University of Navarra


Saad Zafar Usmani, MD, MBA, FACP, FASCO Memorial Sloan Kettering Cancer Center
• Support Groups empower patients & care partners with information, insight & hope
• The IMF provides educational support to a network of over 150 myeloma specific groups

150+ US Support Groups
Over 200 Support Group Visits/year


Univ. of IL at Chicago
Meets virtually on the 2nd Tuesday of each month at 6:30 PM Central Time
Aurora
Meets hybrid on the 1st Wednesday of each month at 6:00 PM Central Time

University of Chicago
Meets virtually on the 2nd Wednesday of each month at 10:30 AM Central Time
Mokena
Meets virtually on the last Thursday of each month at 4:00 PM Central Time
Northbrook
Meets virtually on the 1st Wednesday of each month at 7:00 PM Central Time


Fort Wayne
Meets hybrid on the 1st Tuesday of each month at 6:00 PM Central Time

Bloomington
Meets hybrid on the 2nd Tuesday of each month at 5:30 PM
Central Time
Indianapolis
Meets in-person on the 1st Monday of each month at 6:00 PM Central Time

Special interest groups are designed as a supplemental support for specific populations of patients, in addition to their local Support Groups
MM Families
Founded in 2021
For patients & care partners with young children
Las Voces de Mieloma
Founded in 2022
For Spanish speaking patients & care partners
Living Solo & Strong
Founded in 2022
For patients without a care partner

Click here for more info
Smolder Bolder
Founded in 2023
For smoldering myeloma patients & care partners

Veterans SIG
Founded in 2025
For those who served our country
High Risk Multiple Myeloma
Founded in 2023
For high-risk myeloma patients & care partners
Care Partners Only
Founded in 2024
For myeloma care partners only





































4 PATIENT & FAMILY SEMINARS including world-renowned experts
10 MYELOMA COMMUNITY WORKSHOPS including local myeloma experts

Locations







1. Ensure Access to Care: We advocate to ensure all myeloma patients have equitable, comprehensive, patient-centered care without insurance barriers that limit options or delay treatment initiation.
2. Eliminate Financial Barriers: We advocate for policies that allow myeloma patients access to treatments and supportive care interventions without facing financial hardships.
3. Advance Myeloma Research: We advocate for annual appropriations funding for myeloma research and the advancement of clinical trial eligibility and research protocols that ensure representation from diverse populations.

The IMF Grassroots Advocacy Program is multi-faceted and growing
• Advocacy Training & Leadership Development
• Policy and Legislative Education
• Grassroots Campaign Planning
• Health Policy Forums & Roundtables
• Advocacy Resource Development
• Storytelling and Personal Narratives






Heather Cooper Ortner
Incoming President & CEO
International Myeloma Foundation

“I am humbled to serve alongside so many who are making a different every day for patients and families affected by myeloma, and I look forward to building on the IMF’s legacy of impact”


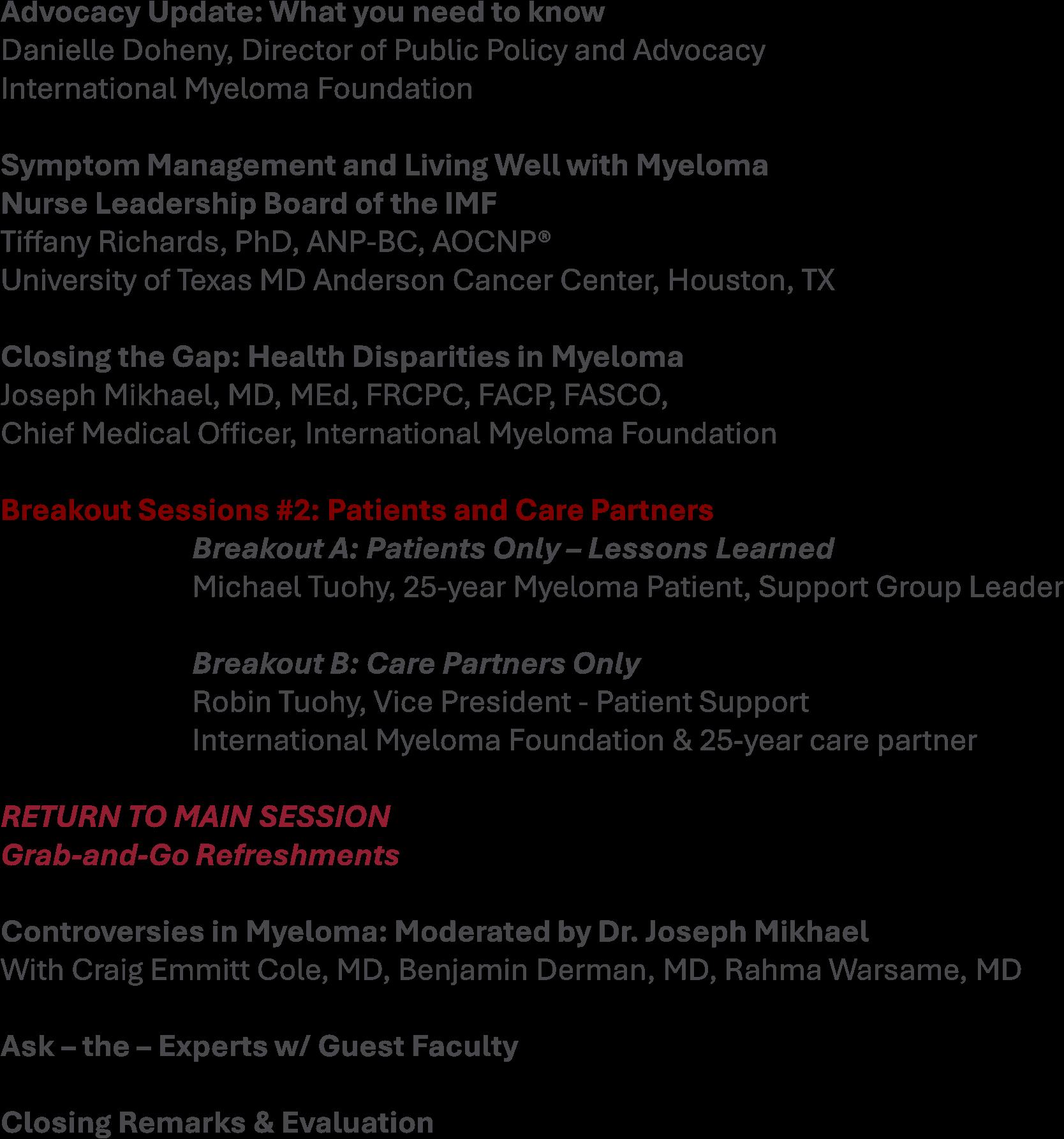
Joseph Mikhael, MD, MEd, FRCPC, FACP, FASCO Chief Medical Officer, International Myeloma Foundation

Tiffany Richards, PhD, ANP-BC, AOCNP®
University of Texas MD Anderson Cancer Center, Houston, TX

Tiffany Richards, PhD, ANP-BC, AOCNP® Manager, Myeloma Advanced Practice Providers Department of Lymphoma/Myeloma MD Anderson Cancer Center

IMF Nurse Leadership Board Member


A world where every myeloma patient can live life to the fullest, unburdened by the disease.
OUR MISSION:
Improving the quality of life of myeloma patients while working toward prevention and a cure.


• Review Shared Decision Making (SDM) Concepts
• Identify Influencing Factors To Treatment Decision Making
• Discuss Strategies To Enhance Patient Empowerment & Promote Shared Decision Making


“The aim of shared decision making is to ensure that:
• Patients understand their options and the pros and cons of those options.
• Patient's goals and treatment preferences are used to guide decisions.”

Image Credit: https://www.ahrq.gov/health-literacy/professional-training/shared-decision/index.html
Agency

https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html#6i1


Identify that a decision is needed: The HCP informs the patient that a decision is to be made and that the patient's opinion is important (Choice talk).
Understand the options:
The HCP explains the evidence-based options and their pros and cons. The patient expresses their preferences, and the HCP supports the patient in decision-making (Option talk).
Come to a decision:
The HCP and patient discuss the patient's wish to take part in the decision making and incorporate the patient's values and preferences into the decision (Decision talk).
Follow-up:
Review and evaluate the decision, adjust as needed



Patients, regardless of age, want to be a part of treatment decisionmaking
Reduces uncertainty and alleviates concerns
Decisions reflect personal and family values and preferences
Requires staying informed
Promotes patient and care partner engagement and sense of empowerment
Positive impact on QOL and continuation on therapy

“The 'efficacy' of treatment means different things to different patients, and treatment decision-making in the context of personalized medicine must be guided by an individual's composite definition of what constitutes the best treatment choice.” Terpos, et al.
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html#6i1. Choon-Quinones, M. et al. 2022; Terpos, et al. 2021


Disease-Derived
Biology: Risk stratification, Urgent intervention needed vs time to consider options
Treatment: Availability/access, effectiveness, toxicity, current research

Patient-Derived

Understanding complex treatment options
Physical and emotional wellness
Comfort in speaking up “Doctor knows best”
Financial, Cultural and Religious factors
Care partner & social network, transportation

Provider-Derived
Time limitations
Support for patient involvement
Provider bias and preference
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html#6i1. Choon-Quinones, M. et al. 2022; Terpos, et al. 2021 https://www.valueinhealthjournal.com/action/showFullTableHTML?isHtml=true&tableId=tbl4&pii=S1098-3015%2822%2900198-X





















myeloma.org


Seek Information, Understand your options
Use caution considering stories of personal experiences
Your healthcare team members are resources
Use reliable and current sources of information
IMF Website: http://myeloma.org
• Publications
• Videos and Replays
• Future Events, both in-person & virtual




Consider your priorities
Consider your goals/values/preferences
Include your care partner/network in the discussion


Be a part of the conversation, create a dialog
Ask questions & express your goals/values/preferences
Ask for time to consider options, if needed
Arrive at a treatment decision together
Arrange follow up to review and adjust the plan, if needed






Understand their different roles
Myeloma specialist and General Heme/Onc
Primary care: for health screening, general check ups, vaccinations
Sub-specialists: specialty needs
Stay connected
Keep a contact list of your providers
Know who to contact for more information










Prepare
Medications: Bring a current list of prescribed and over-the-counter
Questions: Prioritize questions & concerns including financial issues
Paperwork needing medical signature (ex FMLA, prior authorizations)
Inform
Updates: Medical or life changes since your last visit
Symptoms: How have they changed (improved, worsened, stable)? Keep a symptom diary. Bring it along
Communicate effectively so your health care team can help
Follow Up
“Next Steps”: Future appointments, medication changes, plan of care. Ask for the information in writing or on your patient portal
Include a care partner, especially for pivotal appointments



Check with your healthcare team –
Is telemedicine an option?
What is the process and what technology is needed?
Are labs needed in advance? Do you need an order?
Preparation is similar for “in-person” appointment PLUS:
Location: quiet, well-lit location with strong Wi-Fi is best
Yourself: Do you need to show a body part - wear accessible clothing
Vital signs (blood pressure, temp, heart rate, weight) self-serve blood pressure cuff is available at many pharmacies and for purchase
Include a care partner, especially for pivotal appointments



Care partners assist in many ways

Myeloma causes the highest burden of symptoms, most commonly effecting people of older age with other medical issues. Care partner support is valuable in SDM

Attending medical appointments, being present to learn and discuss possible treatment options and alert the medical team of side effects to treatment
Some treatment options available only if care partner support exists
Care partners can be one person or a rotation of many people
Building a partnership is based in good communication
Finding the balance:



- helping the patient with needed activities while maintaining a sense of independence
- allowing the care partner to have time for good self-care




Evaluate where you are at in the process (What decisions need to be made?)
Absorb the information being presented (What are the options?)
Consider how the information impacts you and your family (What are your preferences?)
Create questions that will lead to better understanding (What more do I need to know before making a decision?)
Be an active member of your health care team




Joseph Mikhael, MD, MEd, FRCPC, FACP, FASCO, Chief Medical Officer, International Myeloma Foundation



Joseph Mikhael, MD, MEd, FRCPC, FACP, FASCO
Professor, Translational Genomics Research Institute (TGen),
City
of Hope
Cancer
Center Chief Medical Officer, International Myeloma Foundation







Environmental Factors:
• Exposure to some chemicals
• Radiation exposure
Examples:
Agent Orange
Burn pits
Pesticides, Herbicides
Firefighter/First Responder exposures
Individual Factors:
• Age
• Family History of related disorders
• Personal History of MGUS or SMM
• Obesity
VA Study Documents Health Risks for Burn Pit Exposures
Leukemia and Multiple Myeloma Set to Be Added to List of Conditions Linked to Burn Pits
In most cases, the honest truth
WE DON’T KNOW














Heavy Chain = M-Spike

65% IgG – most common
20% IgA – associated with AL Amyloid
5% to 10% light chain-only (kappa, lambda)
Less common: IgD, IgE, IgM



• AL-Amyloid
• POEMS
• Light or Heavy Chain Deposition Disease
• MGCS = Clinical
• MGRS = Renal
• MGNS = Neuro
Condition
Clonal plasma cells in bone marrow
MGUS1-4 (Monoclonal Gammopathy of Undetermined Significance)
SMM1-5,8 (Smoldering Multiple Myeloma) Active Multiple Myeloma6-8
Presence of Myeloma
Defining Events
Likelihood

* In clinical trial






Test Name
CBC + differential
Complete metabolic panel
Beta-2 Microglobulin (B2M)
Lactate Dehydrogenase (LDH)
Serum Immunofixation and Protein
electrophoresis (SPEP+IFE)
Immunoglobulins (G, A, M, D, E)
Free light chain assay with kappa/lambda ratio
Urine immunofixation & protein electrophoresis (UPEP+IFE)
What it means
Hemoglobin, WBC, Platelets
Creatinine, Calcium, Albumin, Liver function
Part of staging and risk stratification
Measures the level of normal and clonal protein
Identifies the type of clonal protein

Measures the level of normal and clonal protein
Identifies the type of clonal protein





Imaging:
– Skeletal survey: Series of X-rays; less sensitive than other techniques
– Whole body low dose (CTWB-LD CT )
– Positron Emission Tomography (PET/CT)
– Magnetic Resonance Imaging (MRI)

Healthy bone versus myeloma bone disease







Bone
Bone marrow genetics
• Cytogenetics
• Fluorescence in situ hybridization (FISH)
• Next generation sequencing (NGS)




• Updated as new information becomes available
• Helps to guide therapy and measure response to treatment
• Provides some prognostic value
• Standardizes terminology in medical practice








in more than 20% of sorted plasma cells
t(4;14) or t(14;16) or t(14;20) Gain/amp 1q
β2M ≥5.5mg/L (if creat <1.2mg/dL)
Avet-Loiseau et al. J Clin Oncol, in print, 2025

Initial Therapy (a.k.a. Frontline, Induction)
Quad Therapy (ex. CD38+ MoAb + VRd)
HD-Melphalan + Stem Cell
Transplant (ASCT)
Maintenance
Treatment for Relapse
Consolidation
Therapy
Supportive Care and Living Well
Treatment for Relapse

Treatment for Relapse
Treatment for Relapse
Treatment for Relapse



(thalidomide)
(lenalidomide)
(pomalidomide)
Rev, Len
or Pom
(daratumumab)
(isatuximab)

Peptide Drug Conjugate*
BCMA Targeted Antibody Drug
Conjugate (ADC)*
Pepaxto (Melphalan Flufenamide) Melflufen
Blenrep (belantamab mafodotinblmf )
Bela, Belamaf, or B
Abecma (idecabtagene vicleucel) Ide-cel
CAR T Cell therapy
Bispecific Antibodies
Carvykti (ciltacabtagene vicleucel) Cilta-cel
Tecvayli (teclistimab)
Talvey (Talquetamab)
Elrexfio (Elranatamab)
Linozyfic (Linvoseltamab)


Pipeline
Tec Talq Elra Linvo SC/IV
Cevostamab, Iberdomide, Mezigdomide, Venetoclax
Linvoseltamab, LCAR-B38M, ABBV-383 …………………………… MORE TO COME!
* These agents are currently off the market but available through special programs

























Negative by next generation flow (NGF) (minimum sensitivity 1 in 10-5 nucleated cells or higher)*
mCR AND normal Free Light Chain ratio, Bone Marrow negative by flow, 2 measures
CR AND negative PCR
Complete Response: Negative immunofixation (IFE); no more than 5% plasma cells in BM; 2 measures
Very Good Partial Response: 90% reduction in myeloma protein
Partial Response: at least 50% reduction in myeloma protein
Minimal Response
Stable Disease: Not meeting above criteria
Progressive Disease: At least 25% increase in identified myeloma protein from lowest level
MRD = Minimal Residual Disease
sCR = Stringent Complete Response; BM = Bone Marrow
Kumar, S., Paiva, B., Anderson, K. C., Durie, B., Landgren, O., Moreau, P., ... & Dimopoulos, M. (2016). International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. The lancet oncology, 17(8), e328-e346.

MRD refers to the persistence of residual tumor cells after treatment and is responsible for relapse1
Current techniques can detect MRD with a sensitivity of 10-6 for MM cells2
MR→PR→
VGPR→CR →sCR











Reduce the amount of M protein (as measured by serum protein electrophoresis) or light chains (as measured via the free light chain test) to the lowest level possible.
Eliminate myeloma cells from the bone marrow (as measured via minimal residual disease [MRD] testing).
Improve quality of life with as few treatment side effects as possible.
Provide the longest possible period of response before first relapse.
Prolong overall survival.

1. Most patients will be given a combination of drugs to control the disease quickly- usually a QUADRUPLET
2. We don’t “save the best for last” because early therapies have a long term effect on survival
3. We seek a DEEP and DURABLE response
4. We mix and match from the 3 major classes of drugs and add steroids: Proteasome Inhibitors – most often botezomib (Velcade)
Immunomodulatory Drugs – lenalidomide (Revlimid)
Monoclonal Antibodies – daratumumab (Darzalex) and Isatuximab (Sarclisa)
5. We decide early on whether someone will have a stem cell transplant



Bi-Specific Antibodies
Talvey (Talquetamab) CAR-T


Antibody Drug
Empliciti (Elotuzumab)
Bi-Specific Antibodies



Bi-Specific Antibodies
CAR-T






Monoclonal Antibodies
Daratumumab and Darzalex Faspro
Sarclisa (Isatuximab)
TAK-079 MOR202

Immune Therapies
Abecma (Ide-cel CAR-T)
Carvykti (Cilta-cel CAR-T)
Tecvayli (Teclistamab)
Elrexfio (Elranatamab)




Other CAR Ts



Other Bi Specific Antibodies





1L = first line; 2L = second line; 3L = third line; 4L = fourth line; 5L = fifth line; LOT = line of therapy; MGUS = monoclonal gammopathy of undetermined significance; misc = miscellaneous; MM = multiple myeloma; M-protein = myeloma protein; SMM = smoldering MM.
Yong K, et al. Br J Haematol. 2016;175:252-264. Figure modified from Keats JJ, et al. Blood. 2012;120:1067-1076.



1. Depth of response matters
2. High risk vs standard risk - need more aggressive treatment in high risk
3. Balance efficacy and toxicity initially and constantly assess
4. Overcome drug resistance - change mechanism of action whenever possible
5. Shared decision making ensures patient preference is prioritized





How it works:
An antibody directed at a target (BCMA) combined with a cytotoxic agent (chemotherapy)
ADC = Antibody-Drug Conjugate
BCMA = B-Cell Maturation Antigen


ADCP/ADCC = Antibody-Dependent Cellular Cytotoxicity & Phagocytosis
Image Credit: https://creativecommons.org/licenses/by-nc/3.0/


• Incorporates 2 antibody fragments to target and bind both tumor cells and T cells
• Brings target-expressing MM cells and T cells into close proximity, enabling T cells to induce tumor-cell death


“Off the Shelf” Advantage
• No manufacturing process, unlike CAR T-cell therapy (but like ADC/belantamab therapy)
• Thus, no delay between decision to treat and administration of drug ADC = Antibody-Drug Conjugate; BCMA = B-Cell Maturation Antigen; CD3 = Cluster of Differentiation 3; FcRH5 = Fc receptor-homolog 5; GPRC5D = G-protein coupled receptor family C group 5 member D


CAR T therapy recommended. Insurance approved and ready to move forward.















Control is the immediate priority with active disease Cure remains the overall goal
Defining “Cure” has many considerations:
Minimal Residual Disease Negative (MRD-) Time Off Therapy
Functional Cure
Requiring Treatment Stable or Unmeasurable Disease, Receiving Treatment
Unmeasurable Disease, Receiving No Treatment Active Disease

Overall population (N=97); median follow -up: 61.3 months
Progression-free survival

32 of 97 (33%) patients were treatment- and progression-free at ≥5 years


New
Belantamab or Bispecifics?
SCT +/- More induction
Lenalidomide
Bortezomib
Ixazomib
Lenalidomide + PI
Carfilzomib
Dara + Lenalidomide
Bortezomib
Lenalidomide
Carfilzomib
Pomalidomide
Selinexor
Panobinostat
Daratumumab
Ixazomib
Elotuzumab
Isatuximab
Idecabtagene autoleucel
Ciltacabtagene autoleucel
Teclistamab Talquetamab
Elranatamab Linvoseltamab
CAR T or Bispecifics?
Iberdomide, Belanatamab or Bispecifics?
Novel CAR T Cell Therapies
Bispecific/Trispecific Antibodies
Iberdomide and Mezigdomide
Venetoclax?
Belantamab soon?
Multiple small molecules ++++++++
















Monica Bryant, Esq., COO
The slides presented at this meeting contain timely information and have been removed from sharing. For information on this topic please contact: Triage Cancer www.triagecancer.org

Joy Heimgartner, MS, RDN, CSO,
Mayo Clinic, Rochester, MN
Heimgartner.joy@mayo.edu
• To help patients and families appreciate nutrition goals across the continuum of MM care and learn practical strategies to help you live better with multiple myeloma
How dietitians think of care across the cancer continuum and how that is more complex in patients with MM
What are the most important nutrition concerns we have for patients with MM
The power of protein
The power of plants
• Continuum loop : prevention > active treatment > survivorship
Prevention & Survivorship
• Before diagnosis and after active treatment
• Similar nutrition recommendations
• Goal is to optimize long term health and reduce risk of other diseases or cancers






• Recommendations driven by treatment type and nutrition impact symptoms (NIS)
• Goal is to optimize the current body to withstand treatment and side effects to limit treatment interruptions, side effects and debility
recommendations may look very different during these phases…
And that is normal and expected - but can be confusing for patients.
• Before diagnosis and after active treatment
• Similar nutrition recommendations
• Goal is to optimize long term health and reduce risk of other diseases or cancers






• Recommendations driven by treatment type and nutrition impact symptoms (NIS)
• Goal is to optimize the current body to withstand treatment and side effects to limit treatment interruptions, side effects and debility
Tolerating treatment
• Fewer unplanned treatment breaks, dose reductions
• Limit treatment side effects
Maintaining Maintaining physical functionality
• Improve energy levels
• Maintain lean muscle
Preventing longterm complications
• Protect heart health
• Optimize metabolic and endocrine health
• Bonus benefit: improve eligibility for future treatments

• Sarcopenia: loss of skeletal muscle mass, strength and function
• Age-related and disease-related
• Diminishes physical functioning
• Inhibits treatment tolerance
• Increases side effects
• Decreases quality of life

• https://youtu.be/pDSX_jaDCDM

Inadequate protein and/or calories
Rapid weight loss (for any reason)
Inflammation
Medications
Insulin resistance
Physical inactivity
• Quantity matters*
• 1.2 to 1.5 g/kg body weight daily – up to 2 g/kg/day
• 150 lb (68 kg) person: 81-102 g/day
• 200 lb (91 kg) person: 109-136 g/day
• Quality matters
• 65% animal sources during active treatment
• Timing matters
• 4 to 6 feedings per day
*patients with severe kidney impairment should talk to their medical team about if they need to limit protein intake
importance of protein sources to support muscle anabolism in cancer: An expert group opinion. Clin Nutr. 2022 Jan;41(1):192-201. doi: 10.1016/j.clnu.2021.11.032. Epub 2021 Nov 29. PMID: 34891022.


KL,
CM. The importance of protein sources to support muscle anabolism in cancer: An expert group opinion. Clin Nutr. 2022 Jan;41(1):192-201. doi: 10.1016/j.clnu.2021.11.032. Epub 2021 Nov 29. PMID: 34891022.
• When nutrition impact symptoms (NIS) are well controlled, emphasize a plant-forward diet that meets calorie and protein needs
• Plant foods provide:
• Fiber
• Vitamins and minerals
• Phytonutrients
• Pre-biotic fibers to feed a healthy gut microbiome
• Volume for satisfying hunger
• NUTRIVENTION studies

• 5 to 9 servings of vegetables and fruits daily
• Other plant foods: whole grains, nuts, seeds, beans
• Structured “diets” that can work as a starting point
• Mediterranean Diet
• Mayo Clinic Diet
• Whole Food Plant Based Diet

• Start small
• Focus on consistency not grand plans - “What can I do even on my worst day?”
• Create a supportive environment
• Built environment
• Social environment
• Be patient
• Just like MM, your habit change will be something you work on for the rest of your life
• Make it part of your identity
• Instead of “I’m not a vegetable eater” try “I am a person trying to diversify my gut microbes”
• Embrace the 80/20 rule
• Make the healthy choices MOST of the time, and over time you will improve
• It’s not about perfection, it’s about persistence: “All or something”



Presentation Slides: Are available by scanning the QR code, Instructions are on the QR code handout on each table.
Program Evaluations: Please be sure to complete your program evaluation and return your evaluations at the end of the program or on your way out.
Restrooms: Turn left exiting the meeting room and bathrooms are on your left before the lobby Badge Holders: Please return your badge holders and we can recycle them

Wifi: Network – Marriott Bonvoy Conference, Password - patient104
Parking: Onsite parking in the South Lot is complimentary
We greatly appreciate your time and feedback!


SATURDAY MORNING


SATURDAY
AFTERNOON


Living Well With Myeloma - Webinar
October 15, 2025
Regional Community Workshops
November 15, 2025 – Raleigh RCW – Sheraton Raleigh Hotel
Online Community Workshops
November 17, 2025
Patient and Family Seminars
March 13 - 14, 2026 – Boca Raton PFS – Marriott Boca
Raton at Boca Center

Thank you to our sponsors!











5:00 – 7:00 PM Welcome Reception

Please return to this ballroom


A world where every myeloma patient can live life to the fullest, unburdened by the disease.
OUR MISSION:
Improving the quality of life of myeloma patients while working toward prevention and a cure.

These are the core values we bring to accomplishing our mission each day.
The patient experience is the focus of everything we do. Every interaction is an opportunity to establish a personal connection built on care and compassion which is the basis for continued support.
As a team, we value honesty and transparency while creating a culture of mutual respect. We foster a myeloma community built on sincerity, authenticity, and kindness.
We value accountability, personal responsibility, and a steadfast commitment to excellence. We respect the legacy and reputation of our organization while seeking new solutions and advancements to improve outcomes, quality of life, and access to the best available resources for everyone impacted by myeloma.
We recognize each team member's skills and talents through collaboration and cooperation. Our programs aim to celebrate and support the diversity of our patients and their communities.




