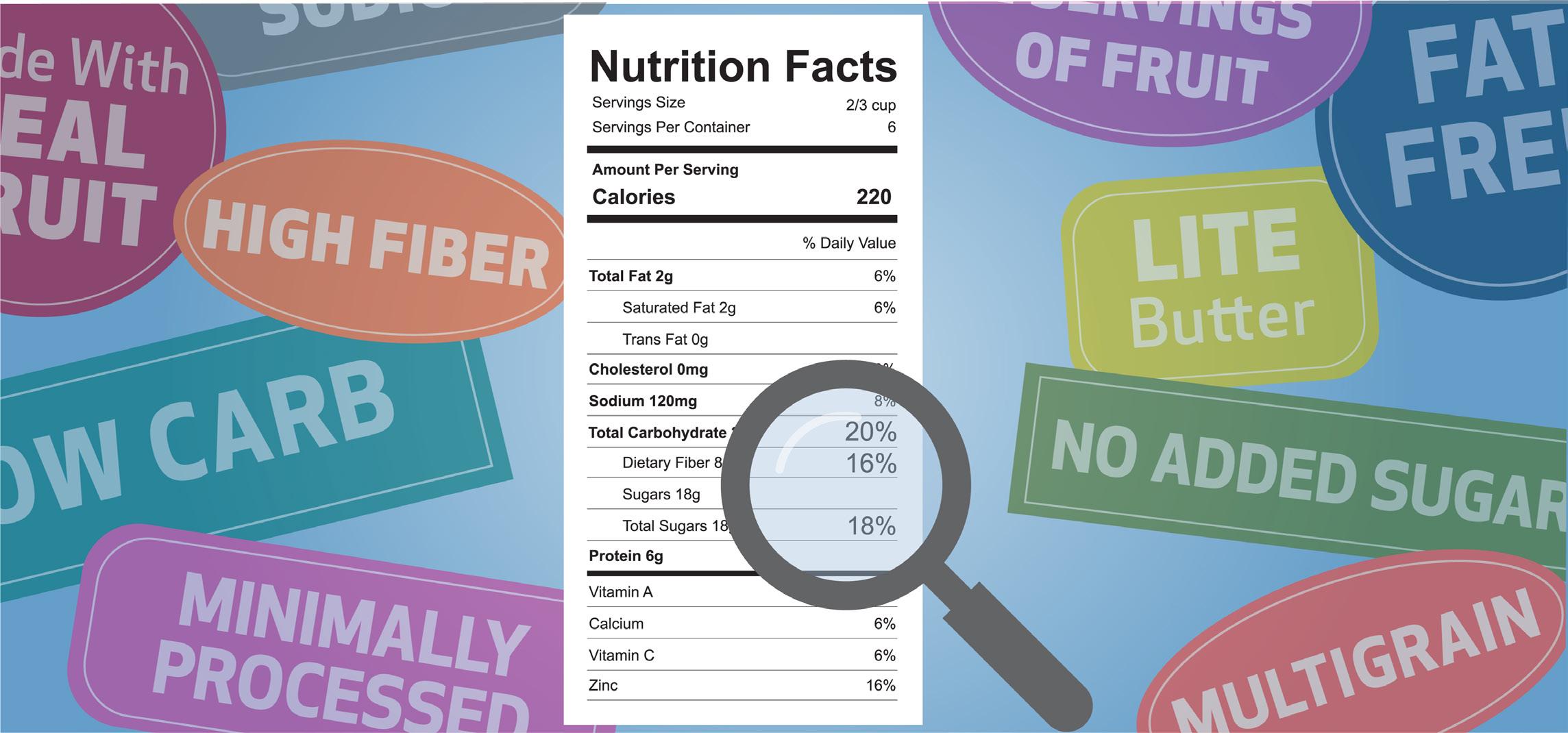


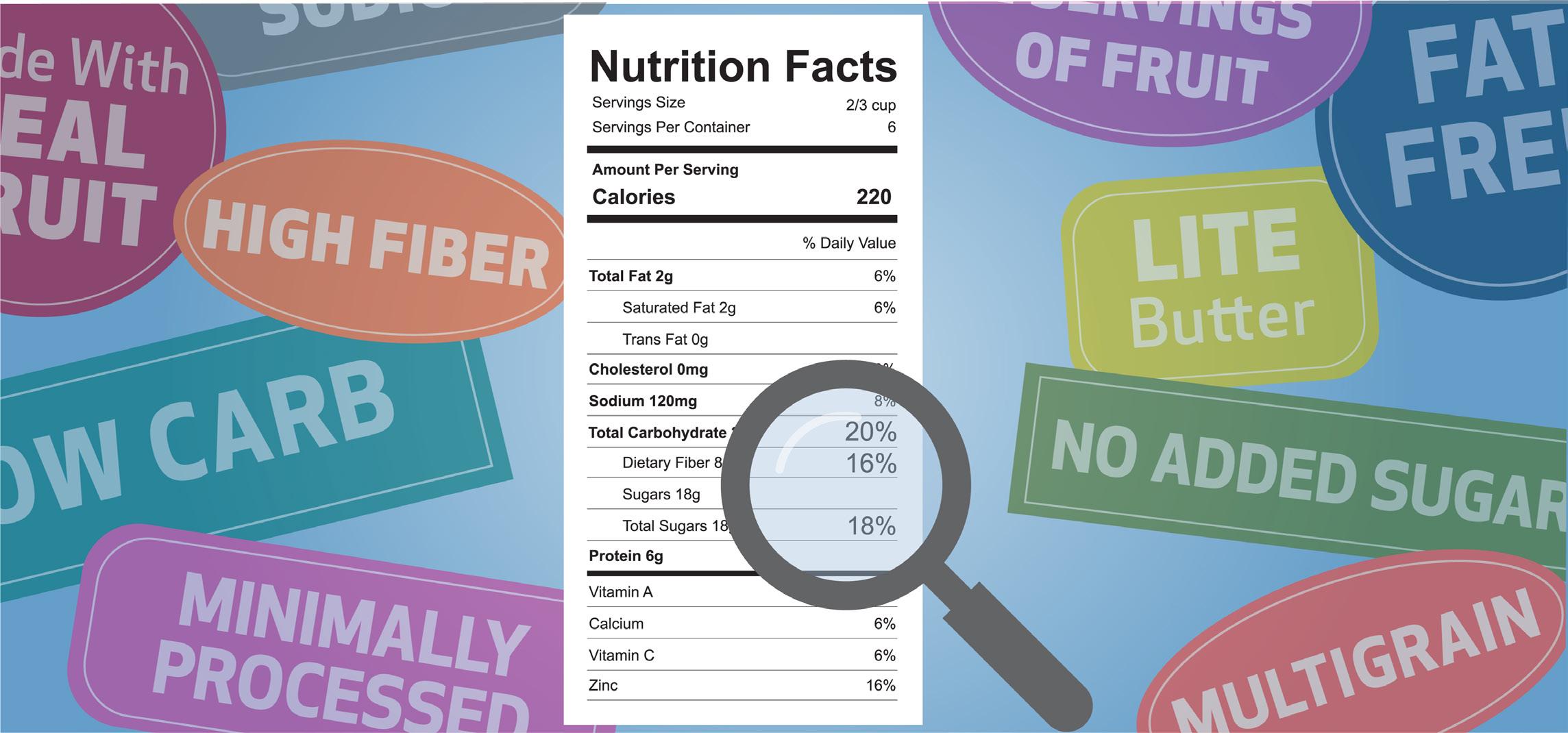
In every grocery store aisle, packaged food labels claim a host of health benefits: Fat free, reduced sodium, low carb — the list goes on. But what do these statements really mean for your health?
According to dietitian experts at Houston Methodist, five easy tips can help you make healthier food choices, despite the confusing labels.
Almost 60% of the average American’s calories come from processed foods. Choose fruits, vegetables, whole grains, lean meats and healthy fats (such as avocados) that provide the nutrients your body needs to function optimally.
You don’t need to eliminate processed food entirely. Instead, try to choose healthy options whenever possible and pay attention to the serving size on your food label. This will help you avoid the most misleading terms, including:
■ Fat Free or Sugar Free: “Free” doesn’t mean there isn’t any fat or sugar in the food. What it actually means is that there is 0.5 grams or less in the food. Make sure to read the serving size —those grams can add up quicker than you realize.
■ Reduced Sodium or Reduced Sugar: On a food label, “reduced” does not mean there is less salt or sugar. What it means is that the product contains at least 25% less salt or sugar compared to the regular version of the same food. Instead, choose a low-salt or low-sugar alternative.
■ “X” Servings of Fruit: If you don’t see real fruit in the ingredients list, the product doesn’t contain the nutrition of real fruit and likely is high in calories and sugar. A better choice would be fresh or frozen fruits with natural sugars.
3. AVOID TRANS FATS
Trace amounts of trans fats occur naturally in foods, but processed foods are often loaded with it. You really should try to limit this type of fat because studies suggest it can increase the risk of heart disease through high cholesterol.
4. GET PLENTY OF FIBER
Fiber is good for you, but it is normal to have gas and bloating with it as part of the digestion process. To combat this, eat high-fiber foods a little at a time throughout the course of the day instead of in one large meal.
5. CHOOSE WHOLE-GRAIN BREADS
Look for the words “whole grain” on the label. “Multigrain” or “enriched” is not the same thing. Whole grains are healthier and include whole wheat, corn and oats. •


If your first few steps out of bed cause stabbing pain, you may be experiencing plantar fasciitis.
“Plantar fasciitis is one of the most common foot orthopedic complaints and the most common cause of heel pain,” said Dr. Travis Hanson, an orthopedic surgeon at Houston Methodist West Hospital.
The plantar fascia is a stretchy band of connective tissue that connects the heel to the ball of your foot and toes, encircling the bones to help support the arch. It is a shock absorber and can endure significant wear and tear over time.
Plantar fasciitis is a painful inflammation of the plantar fascia, often caused by microtears. “It typically resolves without surgery; however, some cases may become chronic and rarely surgical intervention becomes necessary,” Hanson explained.
It’s viewed as a temporary issue, primarily among athletes, those who are increasing their physical activity after an extended break, or runners enhancing their mileage for a long-distance race.
“Other risk factors include working on hard surfaces, being overweight and having tight calf muscles," Hanson added.
Anyone can develop plantar fasciitis, and your risk increases after age 40. And, if you’ve experienced heel pain in the past, you’re more likely to experience the condition again.
Tips to prevent plantar fasciitis include:
■ Replacing old, broken-down running shoes with a new pair
■ Wearing supportive shoes or shoe inserts
Scan this QR code to take a quiz and find out.
■ Starting a new exercise slowly and building intensity gradually
■ Adding rest, warmups and cooldowns, into your movement routine
“Stretching is the number one daily habit to prevent plantar fasciitis,” Hanson said. “It is especially important to stretch out the calf and the plantar fascia if you have any calf tightness.”
Plantar fasciitis does require treatment, but it doesn’t usually involve surgery.
“Conservative treatments, such as stretching both your calf and plantar fascia, massage, icing your arches by rolling your foot over a frozen water bottle, and wearing supportive shoes, are effective,” Hanson said.
Resting and taking breaks from high-intensity exercise are essential for healing. If you’re active, choose low-impact exercises like cycling or swimming to prevent overworking the plantar fascia.
“The vast majority of plantar fasciitis goes away without surgery,” Hanson noted. “I suggest starting with a combination of simple measures such as stretching, icing and using an over-the-counter heel cushion. Most patients will find relief with these measures. For those with persistent pain you could consider a formal course of physical therapy, steroid injections or a few weeks of immobilization in a walking boot.” You should also avoid wearing thin shoes without support, such as flip-flops. Being barefoot for prolonged periods can also worsen pain. If your pain lingers, you may consider physical therapy or other non-surgical treatments, but for most, the conservative approach will alleviate the pain. See a foot and ankle specialist if symptoms persist after a year of treatment. •

Every day, new research suggests breast cancer may be more preventable than experts once thought.
“While there are cancer risk factors such as age and family history that are outside of your control, you can control your lifestyle,” said Dr. Candy Arentz, a breast surgeon at Houston Methodist Neal Cancer Center at West. “If you want to reduce your breast cancer risk, make changes that have a significant impact.”
Here are the top lifestyle changes to reduce your chances for developing breast cancer:
One of the most overlooked risk factors for breast cancer is weight gain after menopause. Having a high body mass index (BMI) post-menopause can significantly increase a woman’s risk of breast cancer — anywhere from 20% to 60%.
“Women can gain weight in menopause due to changing metabolism, and that excess weight leads to higher estrogen levels,” Arentz explained. “After menopause, your estrogen is made in fat cells. So having extra fat cells means extra estrogen, which increases your risk for breast cancer.”
The American Cancer Society recommends 300 minutes of moderate exercise weekly to help reduce cancer risk, which breaks down to about 42 minutes each day. This can include low-impact activities such as brisk walking, cycling, Pilates or swimming. If you’re up for vigorous activities — think jogging, playing tennis, jumping rope or taking a HIIT class — then that overall number drops down to just 22 minutes each day.
“Moderate to vigorous activity not only helps in managing weight and reducing your cancer risk, but also boosts your overall health,” Arentz added.
Alcohol intake is another often underestimated cancer risk factor. Many people enjoy a glass of wine with dinner or a drink at social events, but regular alcohol consumption is strongly associated with increasing your risk of developing breast cancer.
“More than one drink per day can significantly increase the risk,” Arentz warned. “For women who are at high risk of developing breast cancer or for breast cancer survivors, we recommend averaging less than one drink per day.”
Also, taking a daily multivitamin with folate or a folic acid supplement may mitigate breast cancer risk associated with alcohol consumption.
For many women, hormone replacement therapy (HRT) is a common treatment to

manage menopause symptoms, but knowing where to start and how HRT will impact your breast cancer risk is important.
“Hormone replacement therapy is really a discussion for each woman to have with her doctor — usually her gynecologist or primary care physician — about what options are out there,” Arentz explained. “Hormone replacement is important, because it can help maintain weight, improve bone density, and fight fatigue, hot flashes and insomnia— menopause symptoms that affect women’s everyday lives.”
Even if you follow all of this advice, every woman has at least a 12% risk of developing breast cancer, which is why it is extremely important to have screening tests, such as an annual mammogram beginning at age 40. Mammography is still the most effective tool to diagnose early-stage breast cancer, before tumors are large enough to feel or cause symptoms. •
Every woman is different, and your treatment should be tailored to your specific health needs. If you or a loved one has been diagnosed with breast cancer and would like to schedule an appointment, visit houstonmethodist.org/breast-cancer-hmw or call 713.790.2700.
To schedule your mammogram at a Houston Methodist Breast Care Center, visit houstonmethodist.org/mammogram-scheduling or call 346.356.PINK (7465)

The longer a woman breastfeeds, the greater the protective effect for fighting breast cancer. While the reasons behind the risk reduction aren’t clear, one possible explanation is that women who breastfeed have fewer menstrual cycles throughout their lives, and, therefore, less estrogen exposure.
Additional ways a woman can reduce her breast cancer risk

Studies indicate a diet rich in monounsaturated fats such as olive oil may protect against breast cancer, too. Olive oil also contains antioxidants and anti-inflammatory properties, both of which can help reduce breast cancer risk.
Your doctor may recommend tamoxifen and raloxifene medications if you're at an increased risk for breast cancer. Since these medications can produce menopause symptoms, talk to your doctor about the risks and benefits.

If you have a strong family history of breast cancer, ask your doctor if genetic testing is right for you. Mutations in certain genes, such as BRCA1 and BRCA2 genes, increase breast cancer risk. Women with this gene mutation may have more frequent screenings or prophylactic surgery (breast removal).


Headaches can bring varying levels of discomfort, from mildly annoying to more seriously impacting your day-to-day life. Each person’s experience with headaches is unique — sometimes they occur just occasionally, while other times they are a frequent hassle.
“Headaches are likely the most common complaint doctors encounter,” said Dr. Doha Ayish, neurologist at Houston Methodist West Hospital.
“In many cases, these are ‘primary headaches,’ meaning the discomfort is directly within the head and not caused by an underlying medical condition.”
COMMON HEADACHE TRIGGERS
“We don’t fully know why headaches occur,” Ayish explained. “We know that these pains usually come from changes in the nerves, blood vessels and muscles in your head or neck. This can create pressure that triggers pain signals in the brain.”
Understanding what may cause migraine headaches is important in avoiding them. Some common headache triggers are:
■ Alcohol
■ Caffeine
■ Certain foods or smells
■ Dehydration
■ Eye strain
■ Lack of food
■ Overusing headache medication
■ Poor posture
■ Sleep disturbances, particularly lack of sleep
■ Stress
While these common triggers play a role in headaches, how they impact the brain remains largely unknown. Additionally, the biology, the location of the pain and the best treatment all likely differ depending on the specific type of headache.
When headaches are mild or infrequent, you probably take a pain reliever and go about your business. But what about a migraine, which is characterized by more intense and lasting pain?
Migraines can disrupt both your home life and your work life, with particularly uncomfortable symptoms lasting up to 72 hours. They are characterized by throbbing, pulsing discomfort frequently on one side of the head that progresses and worsens over time. They are aggravated by light and noise and can cause nausea and vomiting.
“Migraines are primarily genetic,” Ayish noted. “If your mother or father gets migraines, you’re more likely to have them as well.”
The number one migraine trigger is stress. In women, hormones are often to blame, especially during ovulation or menses when estrogen drops. Another cause could be something as simple as a change in your routine, such as waking up late or skipping a meal.
Preventive measures for you to consider include doing cardio three times a week for 35 minutes, normalizing your meals and keeping a sleep schedule.
“The best thing you can do to avoid a migraine is to keep a headache diary to track what triggers your brain,” Ayish added. “Still, a quarter to a third of patients get migraines no matter what they do. Most doctors prescribe preventive medication if you endure six or more headache days in a month.” •


Many serious health conditions have genetic links that can run in families. Consequently, the more you know about your family’s health, the better snapshot you’ll have of your health.
“A family history is simply a record of the diseases and conditions that family members have experienced,” explained Dr. Ramsha Haider, a primary care provider (PCP) with Houston Methodist West Hospital. “If many family members have experienced the same condition, it can be a health risk factor to consider.”
Being familiar with your family members’ health can help doctors monitor both your mental and physical health.
Building a family health history means researching the health histories of your family’s first-, second- and third-level relatives on your paternal and maternal sides.
“First, ask your family about common health conditions, such as high blood pressure, diabetes and high cholesterol,” Haider said. “It’s also a good idea to discuss any behavioral or mental health conditions.”
Some questions to ask:
■ Has anyone in our family had cancer? If so, what type and at what age was he or she diagnosed?
■ Does anyone in our family have high blood pressure, heart disease, diabetes or asthma?
■ Does rheumatoid arthritis, multiple sclerosis or lupus run in our family?
■ Has anyone in our family experienced mental health concerns such as depression, schizophrenia, anxiety or substance use disorder? Has any family member died by suicide?
Females should ask their mothers what age she started menstruating and the age when she reached menopause.
Men should ask their fathers, specifically about prostate cancer. If your paternal family members were diagnosed at
around age 50 or younger, your PCP may recommend the prostate-specific antigen (PSA) screening lab test.
If you are estranged from your family, you may need to be creative and talk with relatives you still have contact with. If your family history is unknown, your doctor will follow the recommended guidelines for age-appropriate screenings.
Once your family history is built, routinely update any changes in a family member’s health information. Share it with your family and your doctor. Note if you have any family tendency for the same condition.
“Cancer is a major red flag, especially for breast and colorectal cancer,” Haider noted.
Let your PCP know if you have a first-degree relative or multiple second-degree relatives who were diagnosed with these cancers around age 40 or younger. They may recommend you start screening mammograms in your 20s or 30s or get your first screening colonoscopy 10 years prior to the age your family member was diagnosed.
“Sometimes we try to do all the right things — eat healthy, exercise and make sure we’re taking care of ourselves — but our family history may counteract that,” Haider said. “But by living a healthier lifestyle, you can develop a milder version of the same health condition your family member experienced, subsequently living longer and having a better quality of life.” •
To






Taking care of your breast health is important. And early detection starts with your annual mammogram. That’s why Houston Methodist Breast Care Centers offer:
• Innovative imaging technology
• Board-certified breast radiologists


• Online scheduling available when you are
• 13 convenient locations across Houston




Using cutting-edge breast screenings, such as 3D mammograms, to detect even the smallest lumps with accuracy, our breast experts have decades of experience and are all here to support you.
That’s the difference between practicing medicine and leading it. For you.