

Vitals
2025 IMPACT REPORT
SERVING VETERANS
New VA Hospital will anchor OSU Academic Medical District

Dear friends,
As we look ahead to a new year, I continue to be amazed by what our team at the Center for Health Sciences achieves. Through a dedication to doing what’s right, even when it’s hard, we are living out the Cowboy Code each and every day.
As we go to print with this year’s Vitals issue, we have just wrapped up a celebration for the new James Mountain Inhofe VA Medical Center in downtown Tulsa, which is covered on page 4. More than 200 community, legislative and philanthropic partners came together to help mark the transfer of ownership to the VA, which plans to officially open the building next summer.
The VA hospital serves as a cornerstone to the new OSU Academic Medical District, which also includes a greatly expanded OSU Medical Center, the Oklahoma Psychiatric Care Center, OSU Medicine clinics and a new biomedical research lab. All of this is slated for completion in 2028 and will truly revitalize this part of downtown and transform the health care landscape here.
We’re also making an impact by innovating around virtual care, using technology to connect our physicians — from cardiology to psychiatry and more — with rural hospitals and even rural school districts to make a difference for the health of Oklahomans. Our first free-standing hybrid virtual clinic opened last April in Antlers, Oklahoma, in partnership with the Choctaw Nation.
All of this growth is also showing up in our enrollment numbers. We set a new record this fall semester with graduate program enrollment surpassing 2,000 students. Overall, the programs experienced a 23% increase in enrollment, with Health Care Administration increasing by 35% and Forensic Sciences increasing by 19%.
I’m proud to say our work is resulting in top national rankings. For the second time in three years, our OSU College of Osteopathic Medicine was ranked number one in the nation by U.S. News and World Report for graduates who practice in health care shortage areas, commonly known as medical deserts. This further underscores how we are meeting our mission for the state of Oklahoma.
Finally this fall, OSU President Jim Hess announced an ambitious, system-wide fundraising campaign that calls each of us to live up to the Cowboy Code (see details, page 28). As I reflect on those principles that define OSU, I could not be prouder that here at CHS, we truly do dream as big as the sky, stand for what matters and end the day knowing we gave it everything we had.
Wishing you the happiest new year — and Go Pokes!

Johnny Stephens, PharmD President of OSU Center for Health Sciences
Vitals



Leaders, lawmakers celebrate transfer of new VA hospital
Federal, state and local lawmakers, leaders, stakeholders and supporters celebrated Veterans Day at the ownership transfer ceremony of the new James Mountain Inhofe VA Medical Center.
The $181.4 million project, funded by the CHIP IN Act and $70 million in community donations, was a public-private partnership between Oklahoma State University, the United States Department of Veterans Affairs and Veterans Hospital in Tulsa (VHiT) LLC, a subsidiary of the Anne & Henry Zarrow Foundation.
“By partnering with local, state and federal governments, the VA, and philanthropic organizations, OSU continues to live up to its founding mission of training physicians and others to meet the health care needs of Oklahomans,” said OSU Center for Health Sciences President Johnny Stephens.
The ceremony on Nov. 7 commemorated the ownership transfer of the facility from VHiT and OSU to the VA, which will complete the 273,000-square-foot, 58-bed hospital and begin accepting patients in 2026.
“It’s a celebration of collaboration at its very best,” said Tulsa Mayor Monroe Nichols. “This facility will mean shorter wait times, expanding access to specialists, better coordination with OSU medical staff and the students who are going to take care of veterans later in their careers.”
Oklahoma Gov. Kevin Stitt said with the addition of the nearby Oklahoma Psychiatric Care Center also slated to open in 2026, the

dream of creating the OSU Academic Medical District is becoming a reality.
“What’s happening here is bigger than just a hospital. We’re standing in the heart of a new $515 million academic medical district that’s really transforming our great city of Tulsa,” Stitt said. “This is a moment of gratitude and momentum. Gratitude for our veterans and Sen. Inhofe’s legacy of service to our state, and momentum for Tulsa and Oklahoma’s future in health care, innovation and economic development.”










OSU Medical Center breaks ground on $175 million expansion
OSUMC receives $30 million for the project from TSET Legacy Grant
In March 2025, the OSU Medical Center broke ground on a major project to enhance patient care and medical education. The OSU Medical Authority and Trust approved a $175 million hospital expansion with potential additions bringing the total investment to $200 million. During its last session, the Oklahoma legislature approved an added $6 million annually to support the medical center.
And, in November 2025, the medical center received word that the Tobacco Settlement Endowment Trust (TSET) had named OSUMC as the recipient of the TSET Legacy Grant, providing $30 million in grant funding to support the hospital’s ongoing expansion project.
The nearly 180,000-square-foot expansion includes eight new surgical suites, a pharmaceutical research lab and a sky bridge connecting OSU Medical Center to the new James Mountain Inhofe VA Medical Center, located just north of the hospital.
The groundbreaking took place after the OSU Medical Center had completed the addition of a new, $30 million on-site parking garage.
These projects represent a transformative development in downtown Tulsa, anchored by the OSU Academic Medical District. This expansion showcases OSU Medical Center’s dedication and commitment to educating future physicians and providing top-of-the-line medical care.






New vivarium and Barson building renovations
In April, work was completed on a new state-of-the-art vivarium as well as extensive renovations to one of the first buildings on the OSU Center for Health Sciences campus to meet the needs of the growing and evolving institution.
The entire top floor of the Biomedical and Forensic Sciences Building was completely renovated and is now a 12,200-square-foot vivarium research space that triples the size of the former vivarium lab space.
The advanced facility was designed to meet a wide range of research needs and includes a biosafety level 2 containment area. It also includes modern equipment and controls, surgical and procedure areas, and a dedicated behavioral testing space.
The expanded lab spaces will support groundbreaking research in a broad range of areas, including addiction, cancer, gastrointestinal diseases, neuroscience, pain management, pharmacology, vaccine development and weight loss.
The new vivarium provides top-tier training environments for students, researchers and staff with access to the latest tools and technology in research.
Four floors of the 43,400-plus square foot John W. Barson Building also underwent a renovation. Former labs were converted into dedicated medical student spaces with 260 study carrels and eight study conference rooms.
The renovated Barson building also includes 73 offices, four staff breakrooms, three staff conference rooms, a personal health room and large board room.

Dr. Kyle Simmons, OSU researcher studying how GLP-1s may help treat alcohol use disorder
9 pieces of coverage


368M




5.42K
1.63M

U.S. News rankings highlight the success of our mission
For the second time, Oklahoma State University Center for Health Sciences has earned the No. 1 ranking in the percentage of graduates practicing in medically underserved areas in U.S. News & World Report’s annual medical school rankings.
Medically underserved areas, or Health Professional Shortage Areas, are areas and population groups, both rural and urban, that are experiencing a shortage of health professionals. These areas are also called medical deserts.
According to U.S. News data, 73% of OSU College of Osteopathic Medicine graduates are practicing in HPSAs.
“Being recognized again by U.S. News & World Report for the dedication of our graduates in serving patients in physician shortage areas underscores the core mission of OSU College of Osteopathic Medicine,” OSU-CHS President Johnny Stephens said. “I am incredibly proud of our institution, our graduates, and our faculty and staff for their steadfast commitment to this mission. Through a focus on innovation and a deep passion for
community service, OSU-COM continues to produce graduates who are driven to make a difference in these medically underserved areas.”
OSU-CHS was also ranked No. 11 in graduates practicing in rural areas, an improvement from last year’s No. 19 ranking.
According to the National Rural Health Association, the patient-to-primary care physician ratio in rural areas is 39.8 physicians per 100,000 people, compared to 53.3 physicians per 100,000 people in urban areas.
The OSU College of Osteopathic Medicine was founded in 1972 with the mission to educate and train physicians to meet the health care needs of rural and underserved Oklahomans.
The 2024-25 U.S. News & World Report rankings are from a survey of 197 fully accredited allopathic and osteopathic medicine schools in the United States, which grant MD and DO degrees, respectively.

Dr. Caitlin Spinney works during her residency with Dr. Terry R. Gerard II at the Durant Family Medicine Clinic.

OSU-COM alum focus of HBO documentary
“For me, it’s not just seeing patients, you’re seeing people. I’m not the world’s best doctor by any stretch, but I am kind. I am kind and I’m compassionate. That goes a long way. Just pay attention and give them your time.”
Those have been the guiding principles of OSU College of Osteopathic Medicine alumnus Dr. James Graham and his nearly 50-year career as a rural physician in Fairfax, Oklahoma.
His dedication to the health and well-being of his patients is why he is the centerpiece of the short-film documentary “Country Doctor” that premiered in October on HBO.
The film looks at the crisis of rural health care in the United States through the lens of Graham, his colleagues and his community who fought to keep their small rural hospital open.
“We wanted to tell a story that would show the challenges and issues facing a modern country doctor,” said Shari Cookson, one of the filmmakers and producers of the documentary. “Dr. Graham invited us into his world without conditions. The caring and comfort that Dr. Graham gives to his patients is unlike anything I’ve experienced living in a big city. I wish I had a country doctor.”
“There’s never enough money, never enough reimbursement, never enough providers. It’s a constant problem and we’re still facing it,” he said. In 2019, the hospital was on the brink of closing with a skeleton crew working without pay to keep the doors open.
“Fairfax hospital was very close to disappearing forever. But as Dr. Graham says in the film, he and the community didn’t quit in their efforts to save it. And because they fought and sacrificed, Fairfax has a hospital today,” Cookson said. “This was a great
source of inspiration for me about values and the power of perseverance.”
Cookson and her filmmaking partner, Nick Doob, visited Fairfax eight times between 2019 and 2022 and then spent another two years putting the film together.
“Dr. Graham inspired us. He’d known his patients for years, sometimes decades, and cared for them, addressing their needs,” Doob said, but his mission goes beyond Fairfax. “He was on a crusade to bring decent health care to the millions throughout the country who don’t have it.”
The documentary “Country Doctor” follows not only Graham, but the dedication of the hospital staff and the community in working to save their hospital.
“It isn’t just about me. It’s about the people that didn’t take any salary. We didn’t get paid for three months. It’s about those other 30 people that stood in here and worked when we didn’t have supplies just to keep the door open. They’re the real heroes,” Graham said.
Cookson said “Country Doctor” is a microcosm of the crisis affecting rural health care in the United States.
“We wanted to tell the hospital’s story from the inside, to see the situation through the eyes of the town’s residents — both the hopeful and the skeptical — as well as from the perspective of the new owner,” she said. “We are so excited to share our documentary with the country. Dr. Graham would often tell us the film could make a difference. We hope it will. The need for good, sustainable health care is vitally important for all of us.”

OSU-COM, Cherokee Nation honored by Harvard Kennedy School
The historic partnership between OSU College of Osteopathic Medicine and the Cherokee Nation to open the country’s first tribally affiliated medical school received High Honors recognition from the Harvard Kennedy School Project on Indigenous Governance and Development.
OSU College of Osteopathic Medicine at the Cherokee Nation, located on tribal land in Tahlequah, Oklahoma, is the culmination of a shared vision between leaders at OSU-COM and the Cherokee Nation who want to meet the need for more physicians in rural and tribal communities in Oklahoma and improve the health of citizens.
“This collaboration—rooted in trust, shared purpose, and a commitment to addressing longstanding health challenges in our Oklahoma communities—has always been about service and sovereignty,” said Dr. Natasha Bray, dean of OSU-COM at the Cherokee Nation.
The one-of-a-kind medical school welcomed its inaugural class of 53 students, 20% of whom were Native American, in August 2020. And in May 2025 the school graduated it’s second class of medical students, about half of which are in residency programs in rural or tribal communities.
Cherokee Nation Principal Chief Chuck Hoskin Jr. said the results of this partnership have already exceeded expectations.
“They exceeded our expectations because of the power of friendship and trust — trust between the OSU and Cherokee Nation leadership,” Hoskin said. “That’s the power of having a medical school in the heart of Indian Country where they’re experiencing our culture, our lifeways, seeing our challenges and discovering the opportunities that we all have.”
OSU-COM at the Cherokee Nation and the partnership between the university and the tribal nation was one of six finalists for Harvard’s Honoring Nations Awards, one of the most prestigious recognitions for tribal governance in the United States.
In November 2025, the partnership was named one of only three High Honors recipients.
Administered by the Harvard Project on Indigenous Governance and Development, the program highlights innovative, sovereignty-driven initiatives that strengthen tribal nations, improve services and elevate best practices.
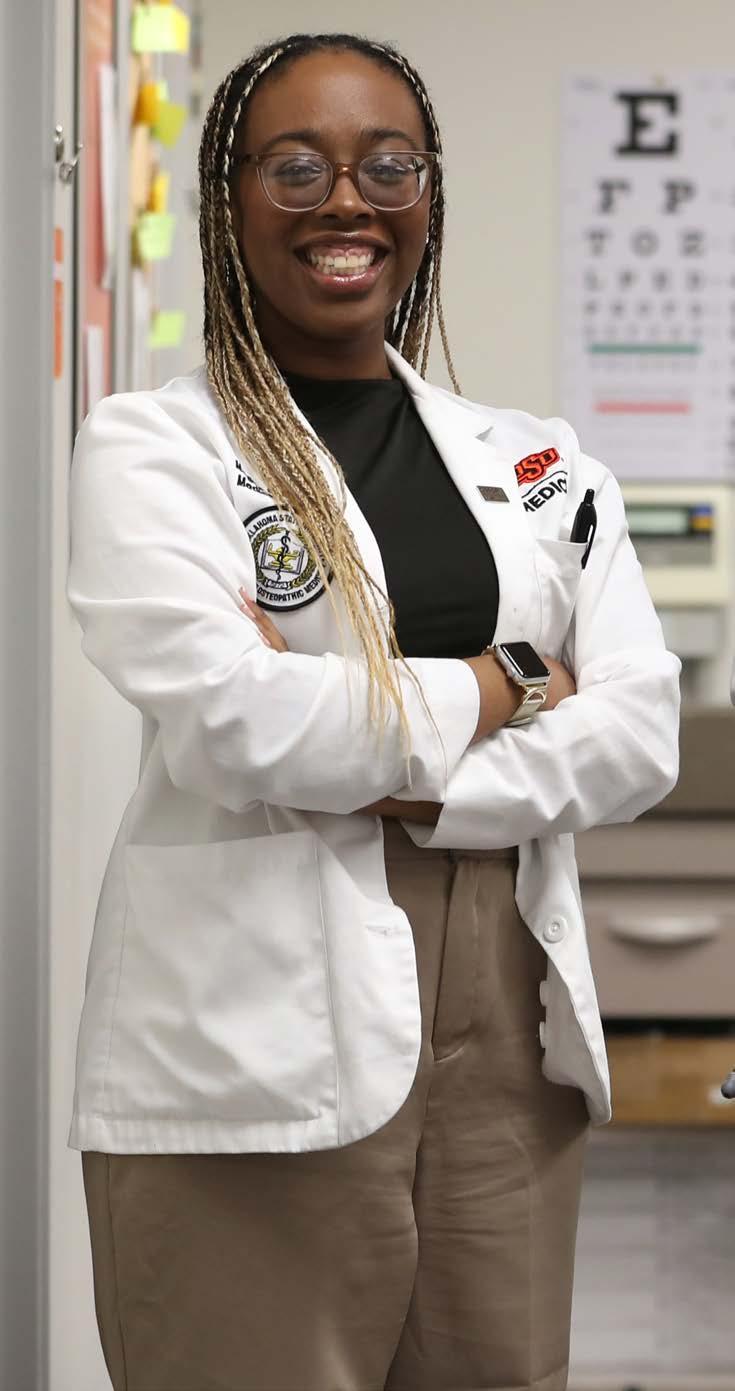
OSU student doctor of the year believes she’s on the right path
Emily Sowah, who graduated in May, was named the 2025 OSU Student Doctor of the Year earlier in the spring.
“I was amazed because I know there are so many amazing people and students at school doing wonderful things. So, to see that I had been named OSU Student Doctor of the Year just meant a lot,” Sowah said. “It means that everything I’ve been doing throughout my four years, and even before then, has been impactful. It just encourages me to keep doing what I’m doing and keep diving into my passions.”
One of her passions is helping patients navigate the health care system. Growing up with sickle cell anemia, a genetic blood disorder she shared with her mother, Sowah was no stranger to hospitals and clinics.
“I’ve learned that not only do I want to help other people understand their own health journeys and their own lab work and why an illness came about and how to best prevent it in the future, I also really want to help communities understand what resources they need, places they need to go,” she said.
Being recognized as the OSU Student Doctor of the Year was just one more sign that she is exactly where she’s supposed to be.
“It means I am on the right path in this journey of mine, that I’m helping the people that I’ve been put on this earth to help. It really means a lot,” she said, and she’s looking forward to her future in medicine.

OSU-COM student named COSGP National Chair
For individuals like Megan Campbell, a fourth-year medical student at Oklahoma State University College of Osteopathic Medicine, leadership comes naturally. Now, as the National Chair for the Council of Osteopathic Student Government Presidents (COSGP), she aims to be a voice for all osteopathic medicine students.
Campbell’s dream of being an advocate led her to join the Student Government Association at OSUCOM, where she served as president for the 2023-24 academic year. She also became a member of COSGP and was elected the 2024-25 national diversity representative.
The leadership and drive Campbell displayed led her to where she is today – the COSGP national chair and the first OSU-COM student to hold the title.
“It gives me chills anytime I think about it. It’s so rewarding to have the chance to be the voice for all osteopathic medicine students,” Campbell said.
Angela Bacon, assistant dean of campus life and wellness at OSUCHS, said Campbell’s election to national chair reflects her hard work.
“It’s been a true pleasure to witness Megan’s remarkable professional growth and development over the past few years. Her recent appointment is a testament to her unwavering dedication, exceptional leadership skills and steadfast commitment to excellence. I do not doubt that she will represent OSU and the osteopathic profession with the utmost distinction,” Bacon said.
Checketts named outstanding resident of the year in orthopedics
Dr. Jake Checketts was no stranger to doctors’ offices and hospitals growing up. Born with Tetralogy of Fallot, a heart defect, he underwent several heart surgeries, but instead of being marred by the experience, he was inspired.
“As early as I can remember, I’ve wanted to go into medicine,” said Checketts, an OSU College of Osteopathic Medicine alumnus who completed his OSU Medicine orthopedic surgery residency earlier this year.
“I think it’s the instant gratification in a lot of ways. Someone comes in with a broken bone, you fix it. Or someone who can’t go to their grandkid’s soccer game because their knee hurts, you give them a knee replacement and it gets better. I like to see the impact these surgeries have on the patients, that means a lot to me with my history,” he said.
During his time as a medical student and as a resident, Checketts has been lead or co-author on about 75 research studies and has been heavily involved in a number of professional organizations and societies.
His hard work was noticed by his residency program director and several of his instructors who nominated Checketts for the American Osteopathic Foundation and American Osteopathic Academy of Orthopedics’ 2024 Outstanding Resident of the Year in Orthopedics.
Checketts said the opportunities to conduct research and be so involved with his profession during his residency at OSU are big reasons why he was honored with the resident of the year award and why he was selected for the prestigious University of Washington Orthopaedic Surgery and Sports Medicine Shoulder and Elbow Fellowship in Seattle.
“It really set me apart. My fellowship is one of the top fellowships in the country, and I was the only DO they interviewed, and I got a spot. I know that all of that has to do with the resources at OSU. The opportunities given to me by the school and residency program allowed me to build my CV,” he said.
Checketts said he will always be grateful to OSU-COM and the people who helped him along his journey through medical school and residency.
“I’ve always felt like coming to OSU was kind of a God thing for me. It was like the universe did that for me — being at OSU at the right time with the right mentors,” he said. “I’m just grateful. I think if I would have gone to another school, I don’t think I would have been given the resident of the year award. I’m so grateful to the orange and black.”

Dean recognized for contributions to osteopathic medical education
Dr. Natasha Bray, dean of the OSU College of Osteopathic Medicine at the Cherokee Nation, received the Robert. S. Kistner Leadership Award from the American Association of Colleges of Osteopathic Medicine (AACOM) in April 2025.
Bray said it is incredibly humbling and deeply gratifying to receive the Robert A. Kistner Award, which recognizes someone for their significant contributions to osteopathic medical education.
“My career has been fueled by a passion for advancing osteopathic medical education and preparing compassionate, skilled physicians who are ready to serve all communities, especially in rural, tribal and underserved populations,” she said. “This recognition is especially meaningful because it comes from AACOM, an organization dedicated to excellence in osteopathic medical education.”
Bray, who graduated from OSU-COM in 2003, returned to her alma mater in 2017 as a clinical professor and soon moved into leadership and administrative roles. She was instrumental to the team that developed and opened OSU-COM at the Cherokee Nation, the country’s first tribally affiliated medical school in Tahlequah, Oklahoma.
Dr. Robert A. Cain, president and CEO of AACOM, said Bray represents the very best of the osteopathic medical education community.
“From her lifelong service as an educator to her leadership as an advocate, Dr. Bray exemplifies the excellence and dedication that define our profession,” Cain said. “We are proud to celebrate her and honor her achievements as she inspires the next generation of leaders in osteopathic medicine.”
The recognition holds profound meaning for Bray, and she emphasized that the Robert S. Kistner Leadership Award truly belongs to the entire OSU-COM community.

“While I’m personally honored by this award, I see it primarily as recognition of our collective achievements and the positive impact the osteopathic community is making on health care access and outcomes across our state and beyond,” she said. “This honor reflects the dedication of our entire team — faculty, staff and students — who share a commitment to advancing osteopathic medicine and improving health care for all Oklahoma communities.”
Continued growth of graduate programs
OSU Center for Health Sciences broke a new record in the fall 2025 semester when its Graduate Programs surpassed 2,000 students for the first time ever, continuing a decade-long trend of record enrollment growth.
23%
enrollment growth from 2024 fall semester.
74 students enrolled
106 students enrolled
Athletic training faculty recognized for service and professional development
Over the summer, the National Athletic Trainers’ Association (NATA) recognized two faculty members from the athletic training program at OSU Center for Health Sciences for their dedication to the profession and the education of future practitioners.
Jennifer Volberding, athletic training program chair and director, was recognized as a Most Distinguished Athletic Trainer given to members who demonstrate exceptional commitment to volunteer service, advocacy and distinguished professional activities as an athletic trainer.
Throughout her career, Volberding has served on multiple committees and boards at the state, district and national levels. She said she is honored to be recognized for her service, but credits her peers for helping her earn it.
“It’s a testament to those who came before me, those I work with and those who are coming after me. I learned early on from my mentors that giving back to the profession is part of what makes you a good athletic trainer,” she said.
Aric Warren, athletic training professor, received the Professional Development Excellence Award given to an individual who has made outstanding contributions in the area of professional development for athletic trainers.
In addition to instructing and leading 13 professional development courses at the state, district and national levels since 2017, Warren helped create and launch OSU’s Athletic Training-Sports Medicine ECHO in 2023. It is the first athletic training-focused Project ECHO line in the nation.
“This award is very meaningful for me. The professional development side of athletic training drives me — helping to advocate for the profession, educating future and practicing clinicians and sharing knowledge to help people do their jobs better,” Warren said.

The largest growth occurred in the School of Health Care Administration (HCA), which surpassed 1,200 enrolled students, the majority of which enrolled in the Doctor of Health Care Administration degree program.
SCIENCES
766 students enrolled
CARE ADMINISTRATION
1,278 students enrolled
1,278 944
960
613
Jennifer Volberding and Aric Warren

Project ECHO provides training and mentoring to health and education professionals
Project ECHO (Extension for Community Healthcare Outcomes) is a collaborative model of medical education and care guidance that empowers clinicians in rural and underserved communities to provide specialty care to more people where they live.
Utilizing a digital platform, primary care physicians, nurses, physician assistants and clinicians in rural and underserved areas can regularly receive training, consultation and mentoring with a team of specialists on patient cases, allowing them to provide specialty care and also save those patients time and money.
Project ECHO currently offers 15 health care ECHOs covering an array of topics including addiction medicine, congestive heart failure, diabetes management, hypertension management, psychiatry, veteran care and many more.
It has also expanded into education and is currently offering four ECHO lines for administrators, teachers, coaches, counselors and health professionals in Oklahoma schools to improve student learning, health and wellness.
With grants from the Tobacco Settlement Endowment Trust and Oklahoma
State Department of Health, Project ECHO launched 11 lines in FY24 including congestive heart failure, diabetes management in primary care, hypertension management in primary care, school nurses and diabetes care, and community health workers.
Project ECHO continues to partner with the OSU Human Performance and Nutrition Research Institute to offer ECHO lines in the Athletic Training-Sports Medicine and Pediatric Obesity. In 2025 they launched the Strength and Conditioning ECHO ensuring coaches and trainers have the skills and knowledge necessary to enhance athletic performance, reduce injury risk and improve the overall health of their athletes. The Building Healthy School Communities ECHO, which shares expert knowledge of best practices to build and maintain healthy school communities, had a successful pilot cohort and expanded to over 90 school districts joining the sessions.
With funding from the Brock Foundation, Project ECHO launched a first of its kind AI in Education ECHO to train educators and students on best and emerging practices using AI in the primary and secondary school environment.
Potential Health Cost Savings in 2025
8,046 participants in health care ECHO sessions
If participants treat 10 patients , that’s 80,460 possible patients treated.
If patients aren’t referred to an outside specialist for care, the potential cost savings is $1,173 per patient .
80,460 patients treated provides potential cost savings of more than $94 million .
All 77 Oklahoma counties served
8,990 Total ECHO attendance 8,046 Total health ECHO attendance
24 Average attendance per ECHO
Data as of Oct. 10, 2025*
Utilizing innovative technology to expand access to care in rural Oklahoma
Oklahoma State University continues to strengthen health care delivery in rural Oklahoma by utilizing current and future technologies to elevate care.
OSU Medicine Virtual Care has expanded its reach across the state to 16 rural hospitals, 16 rural school districts and a first-of-its-kind community clinic in partnership with the Choctaw Nation Health Services Authority. The Antlers Community Health Clinic, which opened in April, operates with a limited on-site staff, while health care providers remotely manage patient care through innovative virtual technology. OSU Virtual Care also deploys two mobile clinics that provide free primary care based at several OSU Extension offices in select rural counties.
From Boise City to Fairfax to Stilwell to Idabel to Colbert, OSU Virtual Care is touching all corners of our state and many points in between as we continue to innovate and transform care in rural communities. The legacy of service to others is a core value and part of our land-grant mission.
“I used the acute care today for my son, who’s a student at Atoka. He had an ear infection, and the whole process was incredibly easy. It made getting him seen, picking up his medication, and getting him back to school simple and stress-free for this working mom!”
— Parent of Atoka Public Schools student
“Our partnership with OSU Medicine’s virtual care services has been an extraordinary asset to McCurtain Memorial Hospital. This program has enhanced the quality, accessibility, and timeliness of care we can provide — especially for our rural community. Through virtual specialty support, immediate provider access, and streamlined care coordination, OSU has helped us reduce unnecessary transfers, improve patient outcomes and ensure our clinical teams feel supported around the clock. The excellence, responsiveness and genuine collaboration we’ve experienced have made a meaningful and measurable impact on our patients, our staff and the overall standard of care at the hospital. We are deeply grateful for the partnership and look forward to continued success together.”
— Lane Manginell, Chief Operating Officer, McMurtain Memorial Hospital, Idabel
OSU Medicine Virtual Care Network
Ser vice Location Type
Health Care Facility
County Extension O ce
School District
*November 2025

OSU Medicine Clinics expanding services and expertise
OSU Medicine continues to strengthen access to outpatient specialty care across Oklahoma through new and growing service lines.
OSU Orthopedics opened on the campus of OSU Medical Center, expanding services to include two new specialists providing comprehensive care for bone, joint and muscle conditions.
Two new service lines — gastroenterology and endocrinology — represent significant milestones in improving community health by providing essential diagnostic and therapeutic care for digestive and liver diseases and specialized expertise in managing complex hormonal and metabolic conditions, including
diabetes and thyroid disorders.
New physicians specializing in pulmonology, interventional cardiology and non-surgical sports medicine are enhancing the scope of care available to patients, bringing advanced diagnostics, treatments and procedures closer to home. The behavioral health team also continues to grow and develop new partnerships, ensuring more patients have access to critical mental and emotional health services.
In addition to expanding clinical services, OSU Medicine is investing in education and training with new fellowship programs in cardiology and addiction medicine to meet growing community needs.
OSU-CHS among three U.S. institutions to receive grant
A team from OSU Center for Health Sciences is hard at work on a grant-funded project to improve the treatment and health care outcomes of patients in rural Oklahoma who are diagnosed with venous thromboembolism, or VTE.
The American College of Emergency Physicians and the Pfizer/Bristol-Myers Squibb Alliance funded the competitive grant program “Improving the Outpatient Management of Emergency Department Patients with Venous Thromboembolism (VTE) in Rural Areas and Underserved Communities.”
OSU-CHS, along with Mount Sinai Health System in New York and Corewell Health in Michigan, were the only institutions awarded this grant funding. Annually, more than 3,000 Oklahomans receive outpatient treatment for VTE, which is most commonly caused by a sedentary lifestyle.
Enid family medicine residency established
In July, Great Salt Plains Health in Enid welcomed four residents as part of the new OSU Center for Health Sciences/Osteopathic Medical Education Consortium of Oklahoma (OMECO) family medicine residency program.
This is the first time since 2017 there’s been a family medicine residency program in Enid. The threeyear residency program will add four more residents each year for the next two years, growing to 12 residency spots total.
Currently, the residents are working primarily out of the Great Salt Plains Enid East clinic, but there are opportunities to also complete some subspeciality rotations in Tulsa at OSU Medical Center and Saint Francis Health System in the future.
OSU-CHS and OMECO received start-up funding from the Tobacco Settlement Endowment Trust (TSET) for the family medicine residency program.

A gap analysis by OSU-CHS revealed that rural emergency departments may lack key tools necessary for high-quality VTE management, and that many patients also face barriers to accessing outpatient therapy, including anticoagulant medications and follow-up care.
Given these challenges, rural areas may experience higher complication rates and potentially more than 400 preventable VTE-related deaths a year.
The grant team is using the almost $200,000 awarded to them to develop education programs, create new technology to support rural medicine providers, and directly help rural emergency departments implement programs to enhance the quality of patient care.
Landon Stallings, DO, James Cornwell, DO, Nick Thompson, DO and Chad Hanson, DO (doctors for orthopedics and sports medicine clinics).
OSU Medical Center, Saint Francis Health System partner to open Level 1 trauma center
Thanks to the passage of two bills in the Oklahoma legislature, OSU Medical Center and Saint Francis Health System partnered to open a Level 1 trauma center in Tulsa in September.
The new trauma center at Saint Francis Hospital provides 24-hour care from trauma surgeons, neurosurgeons and other specialists who are onsite, greatly reducing the need to transfer patients to Oklahoma City.
The partnership will also enhance the training and clinical experience of OSU medical students who will rotate through the trauma center, as well as strengthen OSU’s residency programs.


Project UPCAST is addressing the need for school-based mental health care
The need for childhood and adolescent mental health care is great. In Oklahoma, only six of the 77 counties have childhood and adolescent psychiatrists.
The OSU BRIDGE Center — Building Resources and Interventions for Districts Seeking Growth in Education — is working to transform mental health services in schools with Project UPCAST, a federally funded grant designed to address these needs.
The grant supports school-based mental health training through recruitment and mentoring. In collaboration between OSU’s School Psychology program and the Department of Psychiatry and Behavioral Sciences at OSU Center for Health Sciences, school psychology and school counseling students can complete their practicum work in local, high-needs schools.
Each trainee gets supervised, on-the-job training through UPCAST staff and funding. They also have the opportunity to collaborate across mental health and educational disciplines with advanced coaching on things such as Youth Mental Health First Aid.
Project UPCAST is entering its third year at OSU and has supported the training of 12 school psychology students and five school counseling students.
Bridgett McGill, a PhD student in school psychology, at Rosa Parks Elementary School in Tulsa.

Medical students tackling hospital processes through internships
The Oklahoma State University Center for Health Systems Innovation (CHSI) is equipping OSU College of Osteopathic Medicine students with the skills to address real-world problems in hospitals.
CHSI is a collaboration between the OSU Spears School of Business and the OSU Center for Health Sciences, leveraging both schools’ expertise to focus on business and clinical innovations in health care delivery.
One way CHSI is providing innovative health care solutions is through the Lean Healthcare Internship (LHI) program. LHI is an annual initiative that recruits up to 12 first-year OSU-COM students for a month-long, quality improvement (QI) internship that focuses on lean methodology.
“Lean methodology focuses on improving efficiency by identifying and eliminating activities that don’t add value or waste resources,” said Ipe Paramel, project manager at CHSI. “It’s a
process-oriented method of tackling real problems in health systems.”
The program is unique in that students are on-site performing analysis and gathering data. At the end of the internship, students present their findings and recommend improvements to hospital leadership and staff.
One problem studied by LHI interns is patients staying in the emergency department while they wait for an inpatient bed in the hospital. Student findings and recommendations reduced emergency room wait times by 13 minutes per patient, saving approximately 689 hours over nine months.
LHI expanded to the OSU-COM at the Cherokee Nation campus this last year, with three medical students as a part of the inaugural cohort. To date, LHI has completed six QI initiatives – five at OSU Medical Center in Tulsa and one at W.W. Hastings Hospital in Tahlequah.
Center for Health Systems Innovation (CHSI)
The Center for Health Systems Innovation (CHSI) is dedicated to transforming rural and Native American health through innovative care delivery models and advanced information technology solutions.
As a national leader in rural and tribal health innovation, CHSI combines the expertise of OSU Center for Health Sciences and the Spears School of Business to design, test and scale solutions tailored for rural and underserved communities. It’s core strengths span two domains — market care and delivery networks; and health analytics expertise.
The Rural Oklahoma Network and the Oklahoma Business Collective on Health guide innovation priorities and provide real-world platforms to test and deploy solutions that expand both primary and subspecialty care capacity. These initiatives address critical needs such as workflow efficiency, lean education, AI integration and health information technology implementation.
In the area of health analytics, CHSI leverages the largest known clinical dataset in existence, with de-identified records from more than 100 million U.S. patients collected over 25 years.
Center for Integrative Research on Childhood Adversity (CIRCA)
In the summer of 2025, Julie Croff, Ph.D. was named principal investigator for CIRCA, the Center for Integrative Research on Childhood Adversity.
CIRCA brings together scientists from across disciplines to study how Adverse Childhood Experiences (ACEs), such as abuse, neglect, parental mental illness, substance use, incarceration, and family instability, relate to health and development across the lifespan. While Oklahoma reports high rates of ACEs, CIRCA’s work also highlights the resilience and strength of Oklahoma families, emphasizing that these findings represent associations rather than causes of later outcomes.
Supported by a $9.5 million grant from the National Institutes of Health, CIRCA is midway through Phase 2 of its program, which mentors and trains early-stage

investigators and funds pilot studies. The center’s three research cores provide the infrastructure and scientific expertise needed to advance innovative, interdisciplinary research.
To date, CIRCA studies have collected biological samples from nearly 275 research participants, forming an integrated dataset that connects biological, behavioral, and social measures. By mid-2026, the CIRCA team aims to expand this resource to over 600 participants, building a foundation for future discovery that strengthens scientific understanding and the translation of solutions for community resilience.
Over the past decade, Croff has served in multiple roles including research project leader, associate director, core director, and now PI. This trajectory reflects her long-standing commitment to CIRCA’s mission and the center’s success in cultivating leadership among its own investigators.
$58.7M proposed $44M awarded
88 proposals submitted 114 awards accepted $46M sponsored program expenditures $9.4M research expenditures
Center for Indigenous Health Research and Policy (CIHRP)
The Center for Indigenous Health Research and Policy (CIHRP) at OSU-CHS brings together scientific collaborators and Indigenous and community leaders to eliminate health disparities and cultivate health and wellness in Native American communities.
CIHRP, with continued funding provided by a $10 million grant from the U.S. Department of Health and Human Services, is implementing nutrition and diabetes prevention programs for Native Americans in Oklahoma and across the US. Local partners include the Chickasaw, Osage, Quapaw and Choctaw nations. The project has led to significant improvements in food security, diet quality, cultural connectedness and self-rated health among participants.
In addition, CIHRP partnered with the Osage Nation to develop and test a community supported agriculture program to

promote healthy eating and reduce diabetes risk in Osage families. The program, supported by a $3.5 million grant from the National Institutes of Health, provided weekly boxes of vegetables from the Osage
Nation’s farm as well as cooking classes and dietary guidance.
The program not only improved nutrition and food security but also led to a significant improvement in hemoglobin A1c levels among participants. Study findings were highlighted and presented at the National Institutes of Health in August 2025.
CIHRP director and professor of Rural Health Valarie Blue Bird Jernigan, DrPH, MPH, successfully completed her twoyear term as the first Native American to serve on the National Advisory Board for United States Dietary Guidelines.
Jernigan was named chair of the International Congress of Nutrition’s Traditional and Indigenous Foods Task Force in October 2025. In this role she will develop recommendations for the World Health Organization to protect and strengthen Indigenous food systems worldwide.
Robberson Summer Dissertation Fellowship awarded to CHS biomedical sciences student
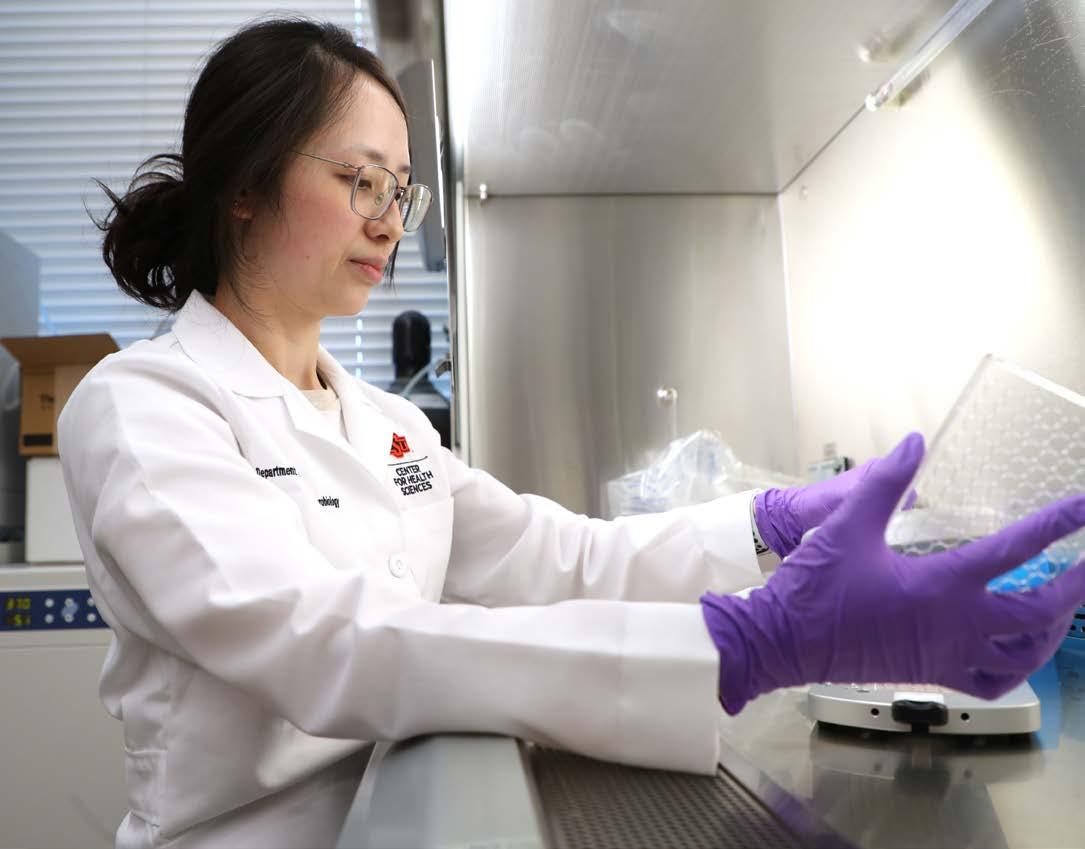
Serene Lim, a fourth-year doctoral student in the OSU Center for Health Sciences Department of Biochemistry and Microbiology, is researching connections between a bacteria found in the mouth and cancer.
“Fusobacterium nucleatum, it’s in everybody’s mouth. It appears throughout our digestive tract, but it’s most abundant in mouths. If you don’t take care of oral hygiene, it can be associated with some diseases,” Lim said. “Cancer is one of the systemic diseases linked to this bacterium.”
Earlier this year, she was awarded the Robberson Summer Dissertation Fellowship, which supports research for post-candidate doctoral students from OSU. Award winners are given an $8,000 stipend, a tuition waiver and three credit hours, which will help Lim continue her research and data analysis until she presents her dissertation in 2026.
Lim is conducting her research under George Huang, Ph.D.,
and an assistant professor of microbiology, who said Lim being awarded the Robberson fellowship demonstrates how important this research is to OSU.
Lim and the research team collected 116 saliva samples from people, some with oral cancer and some without. They isolated 11 different F. nucleatum strains and tested how the different strains of bacteria affected cancer cells, including inflammation levels, viability and growth rate and found that some strains are more likely to promote the growth of colon cancer cells.
Lim said the next step is to find out if their findings can be used to develop a treatment.
“If we can target this bacterium in the cancer cells, we have a better chance of treating cancer patients,” she said. “A precursor to cancer is inflammation; cancer cells like inflammation. So anything that can be developed to help decrease inflammation may slow down the cancer cells.”
OSU med student researches cancer biomarkers and clinical trials in externship
Amara Dike, a second-year OSU College of Osteopathic Medicine student, spent her summer as part of the Robert A. Winn Clinical Investigator Pathway Program (Winn CIPP), where she and 65 other medical students from around the nation completed externships at sites across the United States.
Winn CIPP exposes medical students to clinical research and community outreach in order to create a workforce with the skills and knowledge to improve participation in clinical trials.
Dike’s externship site was the University of Arizona Cancer Center in Tucson, which she chose because of her personal experience with losing two close family friends in high school to cancer.
Alongside her research partner and mentor, Dike’s objective was to design a research project that addressed real-world barriers that prevent patients from accessing clinical trials. She said addressing these barriers is essential to advancing the future of medicine.
The project focused on mapping biomarker-driven clinical trials in Arizona for genetic mutations such as BRCA1 and BRCA2, among several others, which are found in different types of cancer and cause severe disease progression when they mutate.
By mapping the locations of patients with the specific biomarkers against clinical trials that had been active or enrolling participants in the last five years, they discovered significant gaps in the preliminary data.
“Many patients live far away from trial sites that are relevant to their mutation,” Dike said. “Since these biomarker-driven clinical trials are very important and can improve patient outcomes, our goal was to help inform future trial placement and expand this project to other Southwestern states.”

Creating STEM opportunities for K-12 and undergraduate college students
OSU Center for Health Sciences hosts and sponsors several events throughout the year to introduce K-12 students and undergraduate college students to careers in the health sciences. Last fall, OSU Medicine partnered with Discovery Lab science
museum in Tulsa to give children an inside look at health professions by offering several interactive activities. We host several events on campus and around the state each year to recruit the next generation of health professionals for Oklahoma.

Lab Exhibit
In fall 2025, OSU Medicine partnered with Tulsa’s Discovery Lab science museum to give children an inside look at health professions through the Curiosity Clinic, a hands-on exhibit that featured interactive activities including cast-making, DNA experiments, surgery simulation and more.
OKStars


STRETCHED




Youth Medical Mentorship
Operation Orange
Scopes & Scrubs
Teddy Bear Clinic

HOW WILL YOU ANSWER?
The Code Calls — OSU’s historic fundraising campaign — will unlock opportunity, fuel innovation and elevate the Cowboy legacy, all grounded in the grit and generosity of the Cowboy Code. Our moment to lead is now. Every gift strengthens scholarships, learning, leadership and the communities we serve. Cowboys show up, work hard and follow through. Invest in OSU’s future today at osugiving.com/the-code-calls.
Academic Scholarships
OSU-CHS is committed to producing top-tier health care professionals who stay in Oklahoma to serve our communities, but we’re losing our top academic talent because we cannot offer competitive scholarship support. Almost 95% of OSU-CHS students qualify for financial aid, yet only 10% receive scholarship assistance. Scholarships, whether one-time gifts or endowed funds, can tip the scales and help recruit and retain the best and brightest to OSU-CHS.
FOR STUDENTS
They can pursue their calling without financial strain, choosing passion over debt.
FOR OSU-CHS
Attracting top-tier talent strengthens academic programs and elevates the institution’s national reputation.
Food and Dining Access
FOR OKLAHOMA
These students become doctors, health care professionals, researchers and educators who improve health outcomes and fuel economic growth.

At OSU-CHS, more than 700 future health care providers are learning the importance of nutrition and preventative care, yet there’s a lack of accessible healthy food options on or near campus. No modern dining facilities exist within a two-mile radius of the Tulsa campus. By investing in the CHS food service, donors help create a hub for nourishment and connection.
FOR STUDENTS
Access to healthy meals supports their academic and clinical success.
FOR OSU-CHS
A vibrant dining space enhances campus life and retention.
FOR OKLAHOMA
Graduates model healthy eating habits in every community they serve.

Wellness and Fitness Center
While students learn about wellness and preventative care, they have limited facilities that support their physical and mental health. By investing in the OSU-CHS wellness center, donors help build a sanctuary for movement, mindfulness and resilience.
FOR STUDENTS
They gain access to fitness and mental health resources, empowering them to thrive.
FOR OSU-CHS
We become a model campus for wellness, attracting top students and elevating our reputation.
FOR OKLAHOMA
Our graduates become advocates for holistic care, modeling wellness in every community they serve.
OSU foundation fundraising for OSU-CHS 2024-2025
$842,812 amount raised for scholarships $9.23M amount raised for institutional support and scholarship funding

To learn more contact Mindy Frech, Director of Development and Team Lead
OSU-CHS awards inaugural PA scholarships in Audrey Hendershot’s name
For the first time since its launch in 2021, the OSU Center for Health Sciences Physician Assistant program awarded five students with scholarships.
Three scholarships were established in Audrey Hendershot’s name to recognize physician assistant students committed to advancing the program’s mission – to enhance competent and compassionate health care in rural and underserved Oklahoma.
Hendershot, an OSU alumna and a lifelong supporter of the university, grew up in rural western Tulsa County where her family’s only access to health care was through the OSU Medical Center. It sparked her passion for improving health care access in rural areas.
Dylan Gardner and Brianna Maguire received the Rural Physician Assistant Scholarship; Macey Sexton was recognized with the Scholarship for Incoming Physician Assistant Students; and Darci Peach and Braden McKee earned the Academic Excellence Scholarship for Physician Assistant students.
Amy Harrison, director of the physician assistant program at OSU-CHS, said these scholarships serve as a reminder of the impact one person’s vision can have on generations of health care professionals.
“Audrey Hendershot never forgot where she came from and now, thanks to her generosity and that of her estate, our students are inspired to do the same,” said Harrison. “Her legacy is shaping the future of rural health care in Oklahoma, one physician assistant student at a time.”
White Coat Society
The OSU Center for Health Sciences’ White Coat Society fund is a vital resource that empowers the president of OSU-CHS to swiftly respond to the most pressing and immediate needs of students. Whether it’s financial assistance for educational resources or emergency aid during unforeseen circumstances, the White Coat Society helps ensure students have the support they need to thrive both academically and personally.
Membership in the White Coat Society begins with an annual gift or pledge starting at $5,000 or more. Contributions directly impact the well-being and success of future health care professionals, helping to remove barriers and create an environment where every student can pursue their educational aspirations.
White Coat Society members enjoy exclusive benefits, invitations to special events such as Orange Impact; personalized updates from OSU-CHS leadership; recognition from President Johnny Stephens; campus tours led by current OSU-COM students; and priority communications and stewardship reports that highlight the fund’s impact.

Investment in Residency
OSU College of Osteopathic Medicine continues to strengthen its residency programs through important partnerships and invaluable legislative support.
Durant
Pedro Henrique Braga, D.O. Enid, Okla.
B.S., Oklahoma State University
Oklahoma State University Center for Health Sciences AllianceHealth, Durant, Okla.
Family Medicine
Cole DeWitt, D.O. Cherokee, Okla.
B.S., Oklahoma State University
Oklahoma State University Center for Health Sciences AllianceHealth, Durant, Okla.
Family Medicine
Sarah Eleanor Wilkinson, D.O.
Overland Park, Kan.
B.S.; B.A., Pittsburg State University
Oklahoma State University Center for Health Sciences AllianceHealth, Durant, Okla.
Family Medicine
Lawton
Mark Samuel Cieminski, D.O. Oklahoma City, Okla.
B.S., Oklahoma State University
Oklahoma State University Center for Health Sciences Comanche County Memorial Hospital, Lawton, Okla.
Emergency Medicine
Chase Edward Lee, D.O. Clarksville, Ark.
B.S., Arkansas Tech University
Oklahoma State University Center for Health Sciences Comanche County Memorial Hospital, Lawton, Okla.
Family Medicine
Robert Millhollon, D.O. Ardmore, Okla.
B.S., East Central University
Oklahoma State University Center for Health Sciences Comanche County Memorial Hospital, Lawton, Okla.
Emergency Medicine

Danielle O’Connor, D.O. Yukon, Okla.
B.S., University of Central Oklahoma
Oklahoma State University Center for Health Sciences Comanche County Memorial Hospital, Lawton, Okla.
Emergency Medicine
Chase Thomas Yager, D.O. Piedmont, Okla.
B.S., Southern Nazarene University
Oklahoma State University Center for Health Sciences Comanche County Memorial Hospital, Lawton, Okla.
Family Medicine
Norman Nicholas Boyne, D.O. Sapulpa, Okla.
B.S., Oklahoma State University
Oklahoma State University Center for Health Sciences Norman Regional Medical Center, Norman, Okla.
Emergency Medicine
Brian Jeffrey Burling, D.O. Oklahoma City, Okla.
B.S., Oklahoma State University University of Oklahoma College of Medicine, Oklahoma City, Okla.
Anesthesiology
Steven Bradley Fruit, D.O. Mustang, Okla.
B.S., Oklahoma State University
B.S.N., University of Oklahoma Health Sciences Center
Oklahoma State University Center for Health Sciences Norman Regional Medical Center, Norman, Okla.
Emergency Medicine
Cooper Hamilton, D.O. Calera, Okla.
B.S., Oklahoma State University
Oklahoma State University Center for Health Sciences
Norman Regional Medical Center, Norman, Okla.
Emergency Medicine
Madeline Camille LeeMatthesen D.O. Tulsa, Okla.
B.S., Oklahoma State University Osteopathic Medical Education Consortium of Oklahoma Griffin Memorial, Norman, Okla. Psychiatry
Hunter Moody, D.O. Norman, Okla.
B.S., Northeastern State University
Oklahoma State University Center for Health Sciences Norman Regional Medical Center, Norman, Okla.
Emergency Medicine
Caleb Peters, D.O. Noble, Okla.
B.S., University of Central Oklahoma
Oklahoma State University Center for Health Sciences Norman Regional Medical Center, Norman, Okla.
Emergency Medicine
Nicholas Subbie, D.O. Yukon, Okla.
B.S, University of Oklahoma Osteopathic Medical Education Consortium of Oklahoma Griffin Memorial, Norman, Okla. Psychiatry
Oklahoma City
Jessica Blalock, D.O. Fairland, Okla.
B.S., Northeastern State University INTEGRIS Health Southwest Medical Center, Oklahoma City, Okla. Emergency Medicine
Juan M. del Rosario, D.O. Edmond, Okla.
B.S., University of Oklahoma INTEGRIS Health Southwest Medical Center, Oklahoma City, Okla. Emergency Medicine
Ryan Elizabeth Emmert, D.O. Norman, Okla.
B.S., University of Houston University of Oklahoma Dean McGee Eye Institute, Oklahoma City, Okla. Ophthalmology
Kade Ezell, D.O. Banner, Okla.
B.S., Southwestern Oklahoma State University
INTEGRIS Health
Southwest Medical Center, Oklahoma City, Okla. Emergency Medicine

Trey Gooch, D.O. Bethany, Okla.
B.S., Southwestern Oklahoma State University INTEGRIS Health
Southwest Medical Center, Oklahoma City, Okla. Emergency Medicine
Angela Rachelle Hairston, D.O., M.S.
Edmond, Okla.
B.S., Alcorn State University; M.S., Georgetown University
SSM Health St. Anthony Hospital, Oklahoma City, Okla. Family Medicine
Dorsa Hajimirsadeghi, D.O. Oklahoma City, Okla.
B.S., University of Oklahoma INTEGRIS Health Great Plains, Oklahoma City, Okla. Family Medicine
Sireene Anwar Khader, D.O. Edmond, Okla.
B.S., Oklahoma City University
SSM Health St. Anthony Hospital, Oklahoma City, Okla. Obstetrics and Gynecology
Chase M. Kimbrough, D.O. Edmond, Okla.
B.A.; M.Ed., Southwestern Oklahoma State University
SSM Health St. Anthony Hospital, Oklahoma City, Okla. Family Medicine
Trevor Reed Magee, D.O. Norman, Okla
B.S., University of Oklahoma University of Oklahoma College of Medicine, Oklahoma City, Okla. Urology
Rohaan Muhammad Tai, D.O. Oklahoma City, Okla.
B.S., University of Oklahoma University of Oklahoma College of Medicine, Oklahoma City, Okla. Internal Medicine
Hunter Park, D.O. Meeker, Okla.
B.S., University of Oklahoma INTEGRIS Health
Southwest Medical Center, Oklahoma City, Okla. Emergency Medicine
Elissa Diann White Ray, D.O. Stillwater, Okla.
B.S., Oklahoma State University INTEGRIS Health Great Plains, Oklahoma City, Okla. Family Medicine
Kaylin Gayle Ray, D.O. Colcord, Okla.
B.S., Northeastern State University University of Oklahoma College of Medicine, Oklahoma City, Okla. Internal Medicine
Faiz Mohammad Safdar, D.O. Sacramento, Calif.
B.S., Northeastern State University University of Oklahoma College of Medicine, Oklahoma City, Okla. Neurology
Erhan Sarica, D.O. Broken Arrow, Okla.
B.S., University of Tulsa University of Oklahoma College of Medicine, Oklahoma City, Okla. Diagnostic Radiology
Class
Joseph Schnitker, D.O. Cartwright, Okla.
B.S., University of Oklahoma INTEGRIS Health Great Plains, Oklahoma City, Okla.
Family Medicine
Jensen B. Simmons, D.O. Mead, Okla.
B.S., Southeastern Oklahoma State University
INTEGRIS Health Great Plains, Oklahoma City, Okla.
Family Medicine
Cody Yelton, D.O. Jones, Okla.
B.S., University of Central Oklahoma INTEGRIS Health
Southwest Medical Center, Oklahoma City, Okla.
Emergency Medicine
Stillwater
Nicole Cueli, D.O.
Ft. Lauderdale, Fla.
B.A., Bates College
Oklahoma State University Center for Health Sciences Stillwater Medical Center, Stillwater, Okla. Internal Medicine
Tahlequah
James BeDelle Graham IV, D.O. Tulsa, Okla.
B.S., Oklahoma State University
Osteopathic Medical Education Consortium of Oklahoma, Tahlequah, Okla.
Family Medicine
Mackenzie Lynn Hattabaugh, D.O. Muldrow, Okla.
B.S., University of ArkansasFort Smith
Osteopathic Medical Education Consortium of Oklahoma, Tahlequah, Okla.
Family Medicine
matched to an Oklahoma primary care residency

Kirstien Minley, D.O. Henryetta, Okla.
B.S., Northeastern State University
Osteopathic Medical Education Consortium of Oklahoma, Tahlequah, Okla.
Family Medicine
Chet Rotton, D.O. Tahlequah, Okla.
B.S., Northeastern State University
Osteopathic Medical Education Consortium of Oklahoma, Tahlequah, Okla.
Internal Medicine
Megan Tramel, D.O. Grove, Okla.
B.S., Missouri Southern State University
Osteopathic Medical Education Consortium of Oklahoma, Tahlequah, Okla.
Family Medicine
Tulsa
Drake Allen, D.O. Tulsa, Okla.
B.S., University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Emergency Medicine
Joshua Autaubo, D.O. Broken Arrow, Okla.
B.S., University of Central Oklahoma University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Joshua Baer, D.O. Tulsa, Okla.
B.S., Northeastern State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Internal Medicine
Blake Andrew Barron, D.O. Durant, Okla.
B.S., Southeastern Oklahoma State University
University of Oklahoma School of Community Medicine, Tulsa, Okla. Family Medicine
Kyrsten Bené Valentine, D.O. Edmond, Okla.
B.S., Oklahoma State University
M.S., Oklahoma State University Center for Health Sciences
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Internal Medicine
Carly Blackshear, D.O. Topeka, Kan.
B.S., University of Tulsa Oklahoma State University Center for Health Sciences, Tulsa, Okla. Diagnostic Radiology
Timothy Floyd Blackstad, D.O. Broken Arrow, Okla.
B.S., Baylor University University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Kaleb Taylor Blackwell, D.O. Oologah, Okla.
B.S., Northeastern State University University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Asaad Chaudhry, D.O. Tulsa, Okla.
B.S., Northeastern State University University of Oklahoma School of Community Medicine, Tulsa, Okla. Internal Medicine
Priya Chetan, D.O. Guymon, Okla.
B.S., University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry

Caitlin Hillary Conetta, D.O. Tulsa, Okla.
B.S., University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Diagnostic Radiology
Paul Amellaly Delgado, D.O. Mexico City, Mexico
B.S., University of Oklahoma
M.S.C.M., Johns Hopkins University
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Internal Medicine
Emily DuBuc, D.O. Owasso, Okla.
B.S., Oklahoma State University University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Alexandria Kathryn Elmore, D.O. Salina, Kan.
B.S., Kansas State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry
Brendon Feliciano, D.O. Tulsa, Okla.
B.S., University of Tulsa University of Oklahoma School of Community Medicine, Tulsa, Okla. Internal Medicine
Merhawit Ghebrehiwet, D.O. Broken Arrow, Okla.
B.S., University of Oklahoma Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla. Pediatrics
Christopher Franklyn Godman, D.O. Muskogee, Okla.
B.S., Southwestern Oklahoma State University
M.P.H., University of Oklahoma Health Sciences Center
Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla. Pediatrics
Maison Q. Hall, D.O. Muldrow, Okla.
B.S., University of ArkansasFort Smith
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Emergency Medicine
Holly Harrison, D.O. Pueblo, Colo.
B.S., University of Tulsa In His Image, Tulsa, Okla. Family Medicine
Erin Ingham, D.O. Tulsa, Okla.
B.S., Kansas State University
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Internal Medicine
William Janes, D.O. Tulsa, Okla.
B.S., Oklahoma State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry
Garrett Jones, D.O. Blue Ridge, Texas
B.S., Oklahoma Christian University
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Otolaryngology
Jonathan B. Jones, D.O. Oklahoma City, Okla.
B.S., The University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Emergency Medicine
Kimberly Kaase, D.O. Owasso, Okla.
B.S., Oklahoma State University Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla.
Obstetrics and Gynecology
Abigail Elizabeth Kee, D.O. Republic, Mo.
B.S., Missouri State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Internal Medicine
Taimoor Ahmad Khan, D.O. Peshawar, Pakistan
B.S., Northeastern State University University of Oklahoma School of Community Medicine, Tulsa, Okla. Internal Medicine
Stephanie Laughlin, D.O. Tulsa, Okla.
B.S., University of Tulsa
Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla.
Family Medicine
Mercedes Andrea Lincoln, D.O. Tulsa, Okla.
B.S., Baylor University University of Oklahoma School of Community Medicine, Tulsa, Okla. Obstetrics and Gynecology
Sadaf Kouhi Luth, DO Tulsa, Okla.
B.S.; B.A.; M.S. University of Tulsa Oklahoma State University Center for Health Sciences, Tulsa, Okla. Emergency Medicine
Kaylee Ilene Mach, D.O. Yukon, Okla.
B.S., Oklahoma State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Diagnostic Radiology
Kennedi Nash, D.O. Norman, Okla.
B.S., Baylor University
University of Oklahoma School of Community Medicine, Tulsa, Okla. Psychiatry
Garrett Denny Owen, D.O. Woodward, Okla.
B.S., McPherson College In His Image, Tulsa, Okla. Family Medicine
Gunnar Phillips, D.O. Sand Springs, Okla.
B.S., Northeastern State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry
Jack Fenwick Rea, D.O. Oklahoma City, Okla.
B.S., University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Anesthesiology
Nick Richardson, D.O. Tulsa, Okla.
B.S., Northeastern State University In His Image, Tulsa, Okla. Family Medicine
Quanisha Monique Roberson, D.O. Tulsa, Okla.
B.S.N., Langston University
M.S.N., University of Oklahoma Heath Science Center University of Oklahoma School of Community Medicine, Tulsa, Okla. Obstetrics and Gynecology
Jake Allen Romoser, D.O. Tulsa, Okla.
B.S., Oklahoma Baptist University
M.S., Oklahoma State University Center for Health Sciences University of Oklahoma School of Community Medicine, Tulsa, Okla. Family Medicine

Breanna Sharp-Robertson, D.O. Tulsa, Okla.
B.S., University of Central Oklahoma University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Riley Smith, D.O. Stillwater, Okla.
B.S., Oklahoma State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry
Marissa Thoendel, D.O. Sperry, Okla.
B.S., Illinois State University Osteopathic Medical Education Consortium of Oklahoma Tulsa, Okla. Pediatrics
Lauren Triplitt, D.O. Newcastle, Okla.
B.S., University of Science and Arts of Oklahoma
M.P.H., Oklahoma State University
Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla.
Pediatrics
Katie Tucker, D.O. Verdigris, Okla.
B.F.A., Rogers State University University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Areli M. Villalobos, D.O. Ponca City, Okla.
B.S.A.G., Oklahoma State University
Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla. Pediatrics
Colton D. Wagoner, D.O. Talala, Okla.
B.S., Rogers State University Oklahoma State University Center for Health Sciences, Tulsa, Okla. Emergency Medicine
Jordan Brooke Webb, D.O. Tulsa, Okla.
B.S., University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry
Megan Lea Whorton, D.O. McLoud, Okla.
B.S., Southwestern Oklahoma State University
M.S., Oklahoma State University University of Oklahoma School of Community Medicine, Tulsa, Okla. Pediatrics
Clark E. Williams II, D.O. Tulsa, Okla.
B.S., Northeastern State University
Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla. Family Medicine
Carlo LeMonte Williams, D.O. Lawton, Okla.
B.A., University of Oklahoma Oklahoma State University Center for Health Sciences, Tulsa, Okla. Psychiatry
Andrew D. Wilson, D.O. Owasso, Okla.
B.S., Oklahoma State University
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Internal Medicine
Hannah Katherine Wingo, D.O. El Reno, Okla.
B.S., Southwestern Oklahoma State University
University of Oklahoma School of Community Medicine, Tulsa, Okla. Emergency Medicine
Jason Zabel, D.O. Portsmouth, Va.
B.S., Liberty University
Oklahoma State University Center for Health Sciences, Tulsa, Okla. Orthopaedic Surgery
Olivia Zabel, D.O. Bixby, Okla.
B.S., Liberty University
Osteopathic Medical Education Consortium of Oklahoma, Tulsa, Okla., Family Medicine
OSU Center for Health Sciences and Osteopathic Medical Education Consortium of Oklahoma (OMECO) Fellowships
positions Total Residency and Fellowship Programs 29 programs 538 positions 23 programs
positions
OSU Center for Health Sciences 6 programs

