





















LEANORA MINAI
Have you heard of coccidioidomycosis?
I wish I had when I visited Scottsdale, Arizona, last year to hike, play golf and gaze at the stars in a certified Dark Sky Zone.
Little did I know a wedding anniversary trip would land my wife, Heather, in a Florida emergency room a few weeks later. She was first misdiagnosed, then back in the ER before finally being admitted for several nights. This all unfolded while I was working remotely from Florida for Duke, before we moved back to Durham earlier this year.
Doctors eventually discovered the cause was a microscopic fungal spore Heather inhaled as we hiked side by side on a windy day in the McDowell Sonoran Conservancy. That particle, unearthed from the dusty desert soil, set off an illness that left Heather battling Valley fever, or coccidioidomycosis, an infection found most often in Arizona and California. Each year, about 20,000 cases are reported in the United States, a figure expected to climb as climate shifts push the disease into new regions.
When Valley fever strikes, it can bring crushing fatigue, a relentless cough and fever. Some people develop chest pain and aching joints, and in certain cases, tender red bumps flare across the skin. Heather experienced all this. In most cases, according to the Valley Fever Center for Excellence, the body fights it off, but she fell into the 5% to 10% who develop pneumonia with lung nodules and cavities.
Valley fever is largely overlooked and little studied, which is why federally funded clinical research is so important. This issue’s cover story shows how Duke’s research is not only advancing medicine but also helping our own colleagues when they need it most.
Dr. Susanna Naggie, Director of Infectious Diseases at the Duke Clinical Research Institute, with colleagues and collaborators, recently led an observational Valley fever study in Arizona and California that enrolled nearly 500 patients with pneumonia. Testing confirmed a high prevalence of Valley fever. The study also showed wide variation in treatment, underscoring the need for clearer guidelines and earlier testing.
“Ultimately, the reason for research is to improve human health and to impact the outcomes for patients that we take care of,” Naggie told me. “Without research, frankly, we will not be able to take as good a care of patients, and ultimately patients will suffer from that.”
I am grateful to the infectious disease doctors and researchers whose care and discoveries not only support Heather’s recovery but also expand the knowledge that will guide treatment for patients in the future.

Federal funding has long been essential to Duke’s research, driving medical discoveries, new treatments for rare and chronic diseases and lifesaving innovations. This year, however, new federal policies have sharply reduced funding at Duke and other universities. For the Duke employees in this story, federally funded research has made a real difference in their lives.
About one in four American workers wears a uniform, according to Gallup. At Duke, where jobs span hospital care, research, dining and more, uniforms go beyond dress code. They foster pride, trust and unity. From scrubs to chef coats, colleagues share what their uniforms mean to them.
At Duke’s Hock Family Pavilion, hospice workers create small but profound miracles—fulfilling last wishes and bringing comfort to patients.
Leanora Minai
Executive Director of Communications/Editor (919) 681-4533 leanora.minai@duke.edu
Paul S. Grantham Assistant Vice President (919) 681-4534 paul.grantham@duke.edu
Stephen Schramm Senior Writer (919) 684-4639 stephen.schramm@duke.edu
Jodie Valade Senior Writer (919) 681-9965 jodie.valade@duke.edu
Sonja Likness Social Media Manager (919) 660-8780 sonja.likness@duke.edu
Travis Stanley Multimedia Producer (919) 684-4262 larry.stanley@duke.edu
Working@Duke is published by Duke’s Office of Communication Services. We invite your feedback and story ideas. Send email to working@duke.edu or call (919) 681-4533. Visit Working@Duke daily on Duke Today: working.duke.edu



The period for Duke staff and faculty to enroll in or adjust their 2026 medical benefits will be extended to three weeks this year, starting at 8 a.m. on Oct. 6 and ending at 6 p.m. on Oct. 24.
Another change for 2026 is the transition to Cigna Healthcare, which will serve as the administrator for all of Duke’s medical plans.
While Duke will continue to offer the same five plans as 2025, there will be a new plan, Duke Advantage, with a lower monthly premium but higher deductible. This plan will be paired with a Health Savings Account (Duke HSA).
Duke’s 2026 monthly premiums for health insurance will increase between $4 and $24 per month for individual coverage, depending on the plan. The dental plan premiums will include modest increases for 2026, but there will be no increases in copays or deductibles for Duke’s health, dental or vision plans. There are no increases in premiums for vision coverage next year.
Read more about the move on Page 12 inside this issue. Visit hr.duke.edu/enrollment2026 for more details.
Find new ways to leverage the potential of artificial intelligence with this fall’s Learn IT @ Lunch series from Duke’s Office of Information Technology (OIT).

Hour-long Zoom-based sessions will be offered at noon every other Wednesday through early December.
Experts from OIT and other campus partners will lead workshops on AI-related topics such as using Duke’s new suite of AI tools, AI productivity boosts and how to use AI responsibly.
“We want to anticipate what people are interested in and excited to learn about,” said Duke OIT Training & Education Practitioner Trina Rodriguez. “We want to cast a wide net and get AI training to people who may not realize what they can do with it yet.”
For the schedule, visit oit.duke.edu/service/learnitlunch

Benefits eligible staff and faculty can reserve two free tickets to Duke’s home football game against visiting Virginia on Saturday, Nov. 15, at Brooks Field at Wallace Wade Stadium. Up to two additional tickets can be purchased at the discounted price of $5 each.
The tickets for the Duke Football Employee Appreciation Day game provide access to a pre-game meal and kid-friendly activities on the practice field next to the stadium.
Registration for employee tickets will open on Oct. 13. Find more information, including the registration link, at hr.duke.edu
Between October 2024 and April 2025, North Carolina had 530 influenza-related deaths, the most for a flu season since 2009, a stark reminder of the importance of getting vaccinated against the flu.

Flu vaccinations for 2025-26 are available through Duke Employee Occupational Health clinics at Duke South, Duke Regional Hospital, Wake County Clinic at Duke Raleigh Hospital and Duke Health Lake Norman Hospital. Peer vaccinations will be available at clinical locations. Pop-up clinics will also offer vaccinations at locations around Duke.
While the Centers for Disease Control and Prevention (CDC) has recommended flu vaccination whenever influenza viruses are circulating, September through November remains the best time for most people to get vaccinated.
Updated 2025-26 flu vaccines protect against all three strains of the virus expected to be circulating this season.
“Severe flu seasons can occur in any given year,” said Duke Employee Occupational Health Executive Co-Director Dr. Carol Epling. “That’s why it’s important to get vaccinated and reduce the risk of getting a severe case of the flu or needing hospitalization.”
Getting a flu vaccine or an approved exemption is a condition of employment for Duke University Health System and Duke School of Nursing and School of Medicine employees.
For more information, visit vaccines.duke.edu
Get ready for the holiday season with both a special Duke Farmers Market and fitness challenge from LIVE FOR LIFE, Duke’s employee wellness program.
The “Spooktacular” farmers market on Oct. 30 will allow for one last opportunity this season to enjoy local fresh produce and goods amid a festive atmosphere.
The market takes place from 11 a.m. to 2 p.m. on the Duke Medical Pavilion Greenway and features favorite Halloween activities: trick or treating at vendor booths, a costume contest for both individuals and groups, a photo booth, festive recipes and more. Expect a few new seasonal treats, too, along with a nutrition taste-testing table featuring healthier versions of some classic fall snacks.
“It will be festive and fun,” said Brian Zelanko, Health Promotion Manager for LIVE FOR LIFE.
For the winter holidays, “Festive Fit Focus” will help staff and faculty stay on track with a healthy lifestyle throughout the season.
The self-guided, eight-week program runs from Nov. 3 to Jan. 2 and provides support, tips and encouragement for employees who want to maintain weight and overall wellness during the winter holiday season.
Participants receive weekly emails with tips, healthy recipes, stress management tools, physical activity suggestions, and encouragement.
Registration opens Oct. 29.
For more information, visit hr.duke.edu/liveforlife


From breast cancer to rare pediatric diseases, federally funded Duke research has helped its own employees

For a stretch of nearly two years beginning in late 1984, Kent Weinhold would work overnight every Tuesday in an isolation facility at Duke setting up experiments of hope for the desperate.
That year, at the height of the HIV/AIDS epidemic, an estimated 130,400 people were infected by the disease that had no treatment and was emerging as a leading cause of death among young adults. Tuesdays were the only day Duke’s Adult Infectious Disease Clinic saw patients with the disease, as others stayed away in fear.
Weinhold, a virologist at Duke, would gather blood samples from HIV patients willing to help Duke researchers collaborating with Research Triangle Park’s Burroughs Wellcome and the National Institutes of Health (NIH) find a treatment or a cure for the deadly virus.
The research project, led by Duke virologist Dani Bolognesi, was established at the urging of the NIH’s Robert Gallo, who was one of the first to discover HIV caused AIDS. Gallo knew Duke was among the rare places that had the experts, the facilities and the innovation to make a difference, so he made a request to his friend Bolognesi to get to work.
After one Tuesday in February 1985, Weinhold saw a compound decrease virus replication to nearly zero but didn’t realize he’d witnessed something groundbreaking.
“The first thing I thought was, ‘Oh, I must have forgotten to add something,’” he told Working@Duke.
Except when Weinhold repeated the experiment, he got the same result.
The effectiveness of the antiretroviral drug AZT was confirmed in parallel by the team at NIH, and by July 1985, HIV patients at Duke were some of the first to receive AZT in human trials. Duke researchers later developed another drug to treat HIV. And Duke immunologist Barton Haynes, who was also a colleague of Gallo’s, began work on an HIV vaccine that continues today at the Duke Human Vaccine Institute, despite the NIH terminating funding in 2026 for its centerpiece Duke Consortia for HIV/AIDS Vaccine Development (CHAVD).
The support from the NIH, which funded 90% of the early HIV research, according to Bolognesi, was “indispensable,” he said.
Federal funding has long played a crucial role in supporting research at Duke, a point underscored in a 1989 letter to the editor in The New York Times, co-signed by Bolognesi, Weinhold and others, which highlighted Duke’s role in the development of AZT, the first drug to offer a substantial improvement in quality of life for AIDS patients.
Genetic testing revealed Duke Clinical Nurse Kimberly Ross, at left, carried an increased cancer risk, leading her to choose preventive surgery. Duke physicians were part of the team that first identified the BRCA1 gene in 1994.


They wrote, “It does not serve anyone’s interest to nullify the importance of Government-sponsored research in solving problems of American public health.”
For decades, Duke research has furthered medical innovation and discovery, found treatments for rare and chronic diseases and saved lives.
“It’s part of our brand, it’s part of our identity,” said Jennifer Lodge, Duke Vice President for Research & Innovation. “It’s why faculty come here. It’s why students come here. It’s a big part of what we do and what so much of our staff does.”
This year, new federal policies and directives have severely cut research funding at Duke and other universities. For the Duke employees in the following stories, federally funded research has made a real difference in their lives.
Kimberly Ross always suspected there was a genetic link to her family history of cancer. Years ago, her aunt was diagnosed with breast cancer. Her grandfather had prostate cancer. So did her uncle and father.
That’s why as soon as her father told her he would be tested for a genetic predisposition to cancer, Ross made a plan. If he had the BRCA1 or BRCA2 mutation that correlates to an increased hereditary risk for cancer, she would get the genetic test, too.
And if her results were positive, she wouldn’t hesitate: she’d have a double-mastectomy and hysterectomy to reduce her risk. As a Clinical Nurse in the Duke Cancer Center who cares for gynecologic cancer patients, Ross has witnessed firsthand the benefits of proactive treatment.
“I really wanted to make sure that I did whatever I could do to reduce my risk to be here longer for my children and my family,” said Ross, who shares 11-year-old Ava and 7-year-old Camden with her husband, Chasen.
In 2021, at age 34, Ross learned she had two cancerlinked genetic mutations, BRCA2 and PMS2. But before her preventative double-mastectomy in February 2022, routine screening found something else: a small tumor. Suddenly, Ross’s preventative surgery became a treatment for triple-negative breast cancer.
“If there’s such a thing as luck in cancer, she was somewhat lucky in catching it,” said Dr. Jennifer Plichta, a Duke Surgical Oncologist.
Because Ross was not yet 40, the recommended age to begin annual mammograms, she likely wouldn’t have caught the tumor so early without the prophylactic

$863 MILLION Total of all federally sponsored research at Duke, FY 2024

treatment sparked by genetic testing. And the genetic test partly exists because of Duke physicians who contributed to federally funded research that helped identify the location of BRCA mutations.
Duke Drs. Andrew Berchuck and Jeffrey Marks, along with then-Duke physician James Iglehart, were part of a large research group that was involved in the discovery of the BRCA1 gene on chromosome 17 that is associated with a predisposition to breast and ovarian cancer. The findings were published in “Science” in 1994.
Since then, BRCA2 and other hereditary cancer markers have been identified, shaping how cancer is treated. Nearly 70% of patients with a BRCA mutation develop breast cancer, compared to 12.5% in the general population, according to the National Cancer Institute. Prophylactic surgery can reduce that risk to 5%.
For Berchuck, now Duke’s Chief of Gynecologic Oncology, the discovery was meaningful. His mother died from breast cancer in the 1970s at age 52, about two decades before he helped identify the genetic marker she may have carried.
“I have a very personal connection to it,” Berchuck said.
The groundbreaking discovery changed Ross’s life. She endured chemotherapy, had a preventative hysterectomy in 2023, and is now cancer-free—thanks to genetic testing sparked, in part, by work from Duke research.
“It was truly lifesaving,” Ross said.
The crash of ocean waves. A Tim McGraw song on the radio. The chatter of cicadas in summer.
F or Shelly Currie, all sounds are gifts.
Born deaf in her right ear and with weak hearing in her left, Currie knows what it’s like living in isolating silence. In 2018, a year before Currie joined Duke’s workforce, Duke doctors surgically placed a cochlear implant in her left ear, helping restore her hearing— a breakthrough developed at Duke.
“I don’t take this for granted,” said Currie, Grants & Contracts Administrator for the Duke Department of Medicine whose brown hair hides the implant’s quartersized processor behind her left ear. “Not a day goes by that I’m not happy to put this little thing on. I’m so grateful for everything that went into this.”
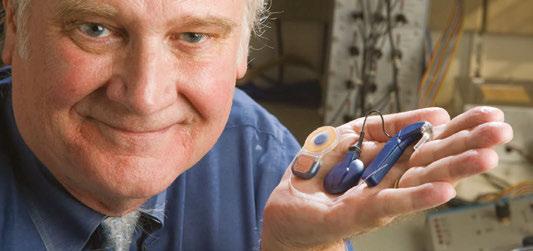
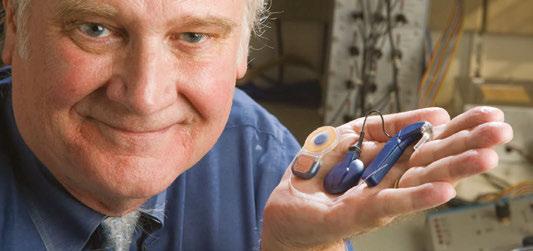
In 1984, Duke faculty member Blake Wilson cofounded Duke’s Cochlear Implant Program, one of the first of its kind, to study a promising-but-ineffective device that had been around for decades. Back then, he recalls, there were around 1,000 users of the implant, which provided awareness of environmental sounds, but not intelligible speech.
Using a head-mounted microphone and processor, and a surgically implanted receiver that electronically

stimulates the cochlea—the boney tube containing the ear’s sound-detecting organ—cochlear implants relay information that the brain translates as sound.
Funded by the National Institutes of Health (NIH) from 1983 to 2005, Wilson’s interdisciplinary Duke team, in collaboration with the Research Triangle Institute, developed the signaling method modern cochlear implants use to deliver sound information that the brain can easily interpret.
The innovation allowed users to understand speech, making the device a biomedical engineering marvel now used by more than a million people worldwide.
At Duke, home to some of the earliest cochlear implant surgeries, 155 were installed during the 2024-25 fiscal year.
“It’s the golden child of cooperation between engineering and medicine,” said Wilson, now Director of the Duke Hearing Center. “We had that wonderful cooperation here at Duke.”
“Not a day goes by that I’m not happy to put this little thing on. I’m so grateful for everything that went into this.”
-Shelly Currie on her cochlear implant
Growing up with severe hearing loss, Currie tried traditional hearing aids, but they only amplified sound, offering no help understanding speech. She managed by reading lips and positioning herself in classrooms and conversations to catch sound with her functional left ear.
In her 20s, as her left ear worsened, Currie felt powerless, struggling to follow meetings and avoiding family holiday gatherings and cookouts because she couldn’t hear conversations.
“I felt my independence being taken away,” she said. “It was defeating.”
In 2018, Currie underwent the cochlear implant surgery at Duke.
After the appointment to activate the device, Currie walked through Duke Clinic’s busy corridors. Chatting with her mom, she heard footsteps, voices and ambulance sirens outside. Tears flowed as Currie, who describes her implant as life-changing, savored the beautifully noisy world she’d missed.


When their son Quinn was born in 2014, firsttime parents Jamie Mills and Liz Aronin experienced a whirlwind of joy and anxiety.
They adored their brown-eyed son but found reasons to worry. Quinn’s feedings were difficult. He didn’t babble like other infants. When they talked to him, his eyes drifted as if scanning distant horizons.
Soon, Quinn began having seizures and needed surgery for cataracts in both eyes. Weighing 12 pounds at age 1, he required a feeding tube. Regular periods of intense, unexplained pain left him inconsolable, once crying for 14 hours straight.
“We didn’t know why this was happening,” said Jamie, Administrative Director for the Duke Global Health Institute. “There wasn’t anything we could tie this to.”
Quinn saw several Duke doctors, but in December 2015, an inconclusive round of genetic testing left Jamie and Liz with no answers about Quinn’s condition and whether future siblings might face it, too.
That’s when they found the Undiagnosed Diseases Network, a research study backed by the National Institutes of Health (NIH).
Launched in 2013, the Undiagnosed Diseases Network unites doctors and researchers from 24 clinical sites—including North Carolina’s only site at Duke University—to solve challenging medical mysteries with advanced technology and collaboration. Patients undergo a series of exams and DNA sequencing. Experts analyze the results using computational models and compare them against global genetic databases.
Duke’s clinical site team, which has been approved for NIH funding through 2028, has evaluated roughly 300 patients and has a network-high diagnosis rate of roughly 40%. The team took Quinn’s case in 2016.
“I remember his parents saying, ‘If this doesn’t help us, maybe it will help someone else,’” said Dr. Vandana Shashi, Professor of Pediatrics and Principal Investigator for the Undiagnosed Diseases Network at Duke.
After Duke specialists studied Quinn’s symptoms and genetic makeup—and compared results with cases worldwide—Jamie and Liz got a call from Kelly Schoch,
their Genetic Counselor at Duke. A diagnosis had been found. A mutation in the NACC1 gene was affecting Quinn’s neurological development. Only six other children were known to have the condition. With no sign it was inherited, Jamie and Liz’s future children wouldn’t be at risk.
Nine years later, nearly 70 families of children with Quinn’s condition share support and advice in a Facebook group. Duke’s clinical site team has published research on the condition and neurologists elsewhere are studying it.
While still facing challenges, 11-year-old Quinn finds joy zipping down Durham’s American Tobacco Trail with Liz in his deluxe running stroller and in tickles from 8-year-old Josie, the oldest of his three little siblings.
“I can’t even imagine what our life would be like without Quinn’s diagnosis,” Jamie said. “It allowed us to build this family, this little team of people that love him."
By Jodie Valade and Stephen Schramm


Jay Dalton has become exceptionally quick at suiting up in the protective gear to enter the hyper-clean space in the Fitzpatrick Center for Interdisciplinary Engineering, Medicine and Applied Sciences.
Donning the required rubber gloves, safety glasses and pale gray polyester hood, veil, smock and booties usually takes researchers and students who work in the cleanroom a few minutes. But during a friendly contest with colleagues a few years ago, Dalton, a Senior Research and Development Engineer for the Shared Materials Instrumentation Facility (SMIF), did it in 59 seconds.
“Once you’ve done it a few times” he said, “it’s a nobrainer.”
Roughly 1 in 4 American workers wears a uniform on the job, according to a Gallup survey. At Duke, where work ranges from hospital care, research, dining and more, uniforms are more than just dress code. For many, they inspire pride, trust and a sense of unity.
In places like Duke’s cleanroom, the right gear isn’t just helpful; it’s essential to enabling potential
At Duke, uniforms provide protection and function and a sense of belonging
breakthroughs in medicine and engineering. The cleanroom, used by students, staff and faculty from engineering and medicine, features an air-filtration system that removes 99.99% of airborne particles. Inside, high-tech machines build circuits and coatings just nanometers thick. Even a single speck of dust could destroy delicate work.
“We wear this not to protect ourselves, but to protect the room from us,” Dalton said.
From hospital scrubs to chef coats, Duke colleagues share the meaning behind their uniforms.



To some, the blue scrubs worn by the roughly 150 colleagues in the Emergency Department at Duke Regional Hospital look the same. But for Cynthia Trail-Michowski, who has spent the past three years helping lead a department that sees about 200 patients a day, individuality still shines through.
She prefers breathable, stretchy polyester blue scrubs with eight pockets that hold her phone, flush syringes, trauma shears and
Growing up, Taniki Williamson loved watching the Food Network, where hosts often wore crisp white chef coats. Later, during culinary training at Wake Technical Community College, she felt a sense of awe watching instructors glide through the kitchen in their jackets.
Now, at the Wall Center for Student Life on East Campus, Williamson oversees the preparation of to-go items for the Trinity Café, slicing fresh strawberries and melons for fruit cups and assembling Caesar salads and tomato, pesto and fresh mozzarella sandwiches on ciabatta rolls.

stethoscope. And with her neon yellow and bright green running shoes and shark-themed badge reel—a nod to her scuba diving hobby—her daily ensemble features personal touches.
Trail-Michowski values how the scrubs and accessories bond colleagues who share highs and challenges together.
“They give us a sense of unity,” she said. “There’s always that connection when you’re wearing scrubs, a shared sense of professionalism and respect.”
Even after 11 years at Duke, Williamson still gets a thrill each time she puts on the white coat with her name embroidered in blue on the chest. Her chef jacket is built for the job, with pockets for markers and meat thermometers, sleeves that can be worn up or down and a reversible double-breasted front to conceal any spills and splatters.
“To wear my chef jacket, with my name on it, means I have earned it and I’m dedicated to this,” Williamson said. “I’ve got duties to perform to make sure the customer is satisfied and fulfilled and that they enjoy their food. There isn’t anything I’d rather do than put on my white chef coat every day.”
During a shift patrolling Duke University Hospital’s corridors, Staci O’Mary logs around 15,000 to 18,000 steps. Along the way, she leads staff safety workshops, checks for unlocked doors and helps visitors find family members.

No matter what, earning the trust of the next person she helps starts with looking the part. Her dark blue uniform must be sharp, her badge and nametag need to shine and the 25 pounds of gear she carries—including a radio, camera and Kevlar vest—must be perfectly in place.
“If my uniform is pressed and everything is in line, the way it’s supposed to be,” said O’Mary, now in her ninth year at Duke, “it sets the tone that I’ve got it together and you can trust me because I know what I’m doing.”
By Stephen Schramm
Effective Jan. 1, 2026, all Duke medical plans for employees will be administered through Cigna Healthcare. This change will help moderate projected plan expenses while preserving access to a broad network of providers.
Joyce Williams, Associate Vice President for Total Rewards in Duke Human Resources, explains what the transition means as staff and faculty prepare for Open Enrollment, which runs Oct. 6–24.
Why did Duke transition to a new administrator for medical plans?
Th e decision to transition to Cigna Healthcare came after a comprehensive review process. Our primary goal was to ensure that we are taking necessary steps to offer a modern and competitive benefits program with affordable premiums, while addressing the diverse needs of our employees who work and live across the country. Cigna was selected for its strong performance in a competitive bidding process and positive feedback from other employers that worked with Cigna.

Minimizing provider disruption was a key factor in transitioning to Cigna, and the Cigna network includes nearly all current providers, but some plans may differ. An online tool will be available on the open enrollment website ( hr.duke.edu/enrollment2026 ) to allow our staff and faculty to review the provider network to ensure that their provider is already included. Should a favored provider not be listed, there will be additional tools provided to enable employees to request Cigna outreach to their provider.
Wh at broader trends are we seeing nationally that help explain how health insurance costs are evolving for employers and employees?
Wh at should covered employees expect because of the change?
Th e transition to Cigna is intended to be seamless. Existing Duke medical plans—Duke Basic, Duke Select, Duke USA, Duke Options and Cigna Care (formerly called Blue Care)—will remain in place, and Cigna will serve as the single, third-party administrator.
In addition, a new health plan option, called Duke Advantage, will be added. Duke Advantage is a highdeductible health plan with a health savings account (Duke HSA). The new plan option offers lower monthly premiums but higher out-of-pocket expenses, so it may not be suitable for those with significant healthcare needs. Decision tools and information will be provided to assist staff and faculty in evaluating their respective health plan choices.
Co ntracting with Cigna and Express Scripts helped to moderate the anticipated expenses for 2026. However, the pace of medical and pharmaceutical expenses continues to trend high. Nationally, health care costs are rising by about 10% on average. Some of the main drivers include the growing number and complexity of chronic conditions and the high costs of treating those patients. Nationally, employers are seeing more highcost claims, especially related to cancer treatment and neonatal care. Add to that medical inflation, rising drug prices, and major—but costly—advances in how we treat serious illnesses. Each of these factors is contributing to the upward trend in premiums across the country. For 2026, Duke’s monthly premiums for individual health coverage will increase between $4 and $24, depending on the plan selected. Dental premiums will see a modest rise, but there are no changes to copays or deductibles for health, dental, or vision plans, and no increase in vision premiums.
By Stephen Schramm

For detailed information about all Duke medical plans and annual open enrollment, visit hr.duke.edu/enrollment2026.

Ranthony Clark once dreamed of playing basketball at Duke. But life happened, her ambitions shifted, and in 2024, Clark came to Duke not as an athlete but as an Assistant Research Professor of Mathematics.
Still, the echoes of her former aspirations dogged her as she settled into life in Durham. She thought about the first time she met Duke women’s basketball head coach Kara Lawson as a teenager when she attended a summer basketball camp at the University of Tennessee while Lawson played there.
And that led her to reflect on a viral motivational speech she watched online that Lawson, a former WNBA and Olympic champion, once gave to her Blue Devils team.
“We all wait in life for things to get easier,” Lawson said in the video seen more than 8 million times. “It’s what we do. … it’ll never get easier. What happens is you handle ‘hard’ better.”
Inspired by Lawson’s words, Clark began tackling the hard part of relocation by planting some roots for the first time in her professional career. She purchased Duke women’s basketball season tickets, which are offered at a discount to Duke staff and faculty. She sprung for two seats to encourage herself to invite colleagues.
She even upgraded to courtside seats last season, where her out-of-town family often spots her wearing her light-up blue devil horns when they watch games on television.
“I decided I’m just going to try to do the work of creating community here,” Clark said. “And a big part of that community has centered around women’s basketball games.”
And she began attending post-game “mingles” offered by the women’s basketball team after each home game. Mingles were instituted by Lawson in 2022 as a way for Blue Devil players to interact with the fans who are often difficult to individualize among a crowd. The eight-minute meet-and-greets happen after every home game, win or lose.
“If we were going to simplify it, it's called creating connection,” said Lawson, who joined Duke in 2020. “How do you create connection with another human? Well, you have to do it by interaction. It's pretty hard to create connection if you never interface with somebody else.
“Our goal is to create as many connections as possible across the campus, across the city, across the Triangle, across the state, across the nation.”
Clark met Lawson (again) at one of those post-game mingles following a come-from-behind Blue Devils’ victory. The coach shared that her halftime speech emphasized the importance of sticking to the game plan, a message that resonated with Clark as she pursued success in her new research role at Duke.
“I feel like she speaks in wisdom,” Clark said. “Not only about her team, but for me, personally.”
By Jodie Valade

The Duke Women’s Basketball season starts in November. For information on tickets, including discount season tickets, call (919) 681-BLUE.

At Duke’s Hock Family Pavilion, hospice workers regularly make miracles happen
The bell chimed three times at Hock Family Pavilion, and everyone knew what it meant. Hospice nurses and workers stepped into the hallway of Duke’s 12-person inpatient hospice facility, solemnly waiting in silence.
Anthony Wilkie, a Duke Clinical Nurse, had been bracing himself for the moment with a mixture of sorrow and humility.
When a bell rings three times at Hock Family Pavilion, a patient has just died and a ritual is about to begin. On Jan. 26, 2024, Erik Sundelöf took his last breaths in Room 12 after his 47-year-old body succumbed to colon cancer. After nearly two months at Duke’s hospice center, which cares for about 300 patients each year, Sundelöf had found relief from his pain and formed close bonds with the staff.
Wilkie held a piece of paper as he stepped into the hallway to pay his final respects as Sundelöf was wheeled through the staff-lined corridor toward the funeral home hearse. Wilkie had a special bond with the thoughtful and caring patient, and while he was honored to read aloud a letter Sundelöf wrote to the care team, he knew this goodbye would be one of the hardest.
“In December, I came to you in pain, in a leap of faith, hoping for a reprieve,” Wilkie read. “I did not come with great expectations, but it is in the hands of strangers that I found kindness. It is here that I found comfort and peace during the most challenging days of my life.”
In the letter, Sundelöf, a visionary in the tech world, thanked the staff who brought festive lights
and decorations for his “Charlie Brown Christmas tree,” tolerated his “rowdy crowd” of visitors during afternoon dominoes and supplied him with seeds for feeding birds and squirrels from his patient room porch.
These moments reflect the small yet profound ways Duke’s hospice workers, honored each November during National Hospice and Palliative Care Month, help make miracles happen and fulfill last wishes for the patients they serve.
“None of us is really there by chance,” Wilkie said. “Whether it’s the nurses, the physicians, the secretaries, the chef, the nursing assistants—everyone is there for a reason. It feels like we’re part of a team that’s going to do whatever we can for our patients in their final moments.”
Debra Harper-Crespo, Assistant Nurse Manager at Hock Family Pavilion, discovered hospice work suits her personality—“very holistic, very hands-on,” she said.
When Imer “Paul” Ramadanovic came to Hock as a chef after a career in restaurants, he had one demand: He would only accept the position if he could cook the final meals each patient requested.
Deb Davis went into hospice care 10 years ago as a second career. During a clinical rotation performing postmortem care, she felt a sense of calmness and peace, humbled to give families “one last gift.”
Wilkie, the Clinical Nurse, simply felt as if he could make the greatest impact in hospice.
Kara Andrade began volunteering at Hock a few months after her husband, Sundelöf, died in Room 12. Andrade, a writer and communications professor, now spends their former “date nights” volunteering in whatever ways the hospice center needs and has become an end-of-life doula.
“It’s a community there and they’re all there because they want to be there,” Andrade said of the staff. “You don’t just get placed in palliative care; you choose to go into palliative care.
“Grief is love that has nowhere to go, and I think a lot of people who are there have a lot of love.”
As a Clinical Nurse in admissions, Deb Davis is the first person many patients and their family members meet when they arrive at Hock. Every time, she asks some variation of, “What is most meaningful to you? If we can give you anything, what would it be?”
“The fact that you can make the absolute worst time in someone’s life a little bit bearable, that means a lot,” Davis said.
They’ve transformed patient rooms into beach scenes and holiday tableaus to recreate favorite memories. They’ve arranged for terminally ill patients to wed their true loves, and hosted weddings for the children of patients who would not live long enough to see the planned ceremony.
Treasured pets have been brought in to spend precious moments with their humans, and they’ve

brought patients into the facility’s vibrant flower garden for one last glimpse at a rare red moon.
They’ve held the hands of patients who do not have friends or family with them as they take their last breaths.
Now Hock’s Health Unit Coordinator, Ramadanovic, served as the chef in Hock for 10 years. He learned to prepare more final meals than he can count—from chicken and dumplings to vegan creations, ice cream sundaes and blood sausage.
“When we get patients here, they have very few smiles left,” Ramadanovic said. “But when I showed up with a plate, I got one. That satisfaction of making them the last meal, even if they only take one bite, it gave me great pleasure.”
Andrade and her husband, Sundelöf, saw the miracles daily. Once, after hearing the bells chime three times, Andrade suggested they find a way to thank everyone who had helped to ease their pain when the chimes would finally ring for Sundelöf.
“Your death wouldn’t be just another death,” Andrade remembers telling him. “It wouldn’t just sadden them. You could express your love and gratitude to them for the journey we all took with you—one of abundance and love.”
As Wilkie read Sundelöf’s letter to the hospice workers who gathered in early 2024, his voice began to quiver.
“Please know that you have made a significant and positive difference in our lives,” Wilkie read aloud. “Your work is not just a job; it is a calling and you answer it with compassion and professionalism. None of this goes unnoticed.”
Wilkie, sniffling, couldn’t help but add his own final line. “Thank you, Erik,” he said.
By Jodie Valade



One of the first things Silvia Cartagena did when she started working for Duke as a Medical Interpreter in 2017 was join the Duke Credit Union.
Cartagena has always joined her workplace credit union whenever one was available. So, she’s often surprised to meet Duke colleagues who have never heard of the Duke Credit Union, which has served members of the Duke community since 1968.
“It’s a benefit hidden in plain sight,” Cartagena said. “This is money that comes from us, that is for us—for our own benefit.”
Duke Credit Union is open to membership for all Duke University and Duke University Health System employees who are paid in North Carolina, along with students and alumni of Duke, retired employees, Duke-affiliated organizations and immediate family members of those who qualify.
Membership, which requires a $25 deposit into any account and a one-time $5 fee, gives access to a credit union that serves roughly 16,000 members. The credit union has a physical branch, and members can access accounts through online banking or a mobile app.
“We’re more of a boutique bank, in a way, in that we can offer really personalized service,” said Jennifer Sider, Director of Marketing at Duke Credit Union.
The Duke Credit Union offers payroll deduction for a variety of savings accounts and provides a range of products and services, including:
Auto loans, personal loans and credit card interest rates are generally lower than at most banks.
For instance, Duke Credit Union offers credit card rates as low as 8.5%, while the Credit Union National Association reports the average bank in North Carolina offers a credit card interest rate of 18.75%.
Each year, Duke Credit Union offers $3,000 undergraduate scholarships to three Duke Credit Union members or the child of a member.
Members can take advantage of estate planning services during scheduled "Wills Days," as well as participate in an annual Shred Event to securely discard sensitive documents.
As a nonprofit, Duke Credit Union diverts some dividends to its designated charity, Duke Children’s Hospital.
Cartagena worked with Duke Credit Union Financial Guidance Counselor Cassandra Taylor to establish short-term and longterm financial goals. When Cartagena had unexpected car repairs and expensive moving expenses, a low-interest loan was quickly approved, and money was deposited directly into her account.
Serving 16,000 members, Duke Credit Union offers a range of accounts and personal guidance
“For me,” she said, “it has been instrumental because I know I can get extra help—and you really are saving money with a low interest rate compared with other banks, and you are strengthening your FICO score when you repay your loan on time.”
By J odie Valade

As a Director of Research Administration, Deborah Martin leads a team that manages research grants in the Duke University School of Medicine.
Over the past year, a lot has changed in Martin’s world. Funding has shifted abruptly, with some research support lost altogether, reshaping how Martin and those around her work.

“We’re trying to implement and operationalize change that we know of, and we're still waiting for answers for things that may or may not be changing, but we can't guess what that looks like,” Martin said.
Change is hard. But, as the old saying goes, it’s the only constant in life. Martin has learned through past experiences how best to manage uncertainty to minimize anxiety and frustration. The first step, she says, is simply accepting reality.
“We are committed to the research mission, even in the midst of this change,” Martin said. “It’s our job to understand, ‘How can I best support this research even though I’m faced with things I can’t control?’”
Acceptance doesn’t mean you don’t care or are giving up, says Eric Chaiken, a counselor with Duke Personal Assistance Service (PAS). But it does involve recognizing what’s within your control and what isn’t.
“We often like this sense of stability and predictability, but when that gets shaken up, we have to work toward acceptance that life has changed,” he said. “That’s a natural part and rhythm of life.”
Martin continues to draw on lessons she learned from sudden upheavals in work and life, including the COVID-19 pandemic. Among them:
Have someone to lean on
Martin relies on conversations with close friends, her husband and several trusted colleagues to help her “maintain an attitude of positivity.” Chaiken says support can come in the form of a therapist or a journal.
“Knowing somebody’s there helps give us some degree of reassurance,” he said. “It helps us not feel alone and isolated.”
It’s important not to lose focus on people, Martin adds, and the importance of relationships during change.
“At the end of the day, we’re all in this together,” she said. Look for opportunities
Martin says a mentor once told her, “Never waste a crisis.”
“Every crisis is an opportunity to view something differently,” she said. “What’s the good that can come out of this?”
Recognize that you’ve survived past changes
Martin likes to upend the conventional interview question, “Where do you see yourself in five years?” Instead, she asks, “Did you see yourself here five years ago? In my mind, the answer is always, ‘No.’”
Five years ago, for instance, Martin never envisioned navigating a pandemic and remote work environment.
“Look at all the changes that I’ve already successfully managed,” she said. “Maybe the next change won’t be so scary.”
By Jodie Valade

To schedule an appointment with Duke Personal Assistance Service (PAS) for short-term counseling at no charge, call 919-416-1727 or visit pas.duke.edu
A stressful travel day ended on a high note thanks to a discount at Fast Park & Relax RDU
On Connie Nichols’ return trip from celebrating her grandson’s first birthday on Grand Cayman Island earlier this year, she lost 12 hours to travel delays, much of her energy and nearly her cell phone.
But thanks to Fast Park & Relax RDU, the airport parking facility she has used for years because of a Duke employee discount, and a conscientious shuttle driver who took time to locate her misplaced phone, at least one part of her trip was a little bit easier.
“I was already a Fast Park fan because of price and convenience, but I am a super fan now,” Nichols wrote in an email to the company.
Nichols, a Research Scientist in Infectious Diseases at Duke, has long used Fast Park & Relax RDU because of a 15% discount offered to Duke staff and faculty. In addition to the discount, customers enjoy covered parking, earn free parking days, reserve spots online and use electric vehicle chargers at no extra cost. Shuttles to RaleighDurham International Airport, about 4 miles away, run 24/7 and pick up and drop off at your vehicle.
“It’s a little farther away so you have to plan accordingly, but it has always been great—fast service for buses, nice parking and attendants who always make sure you know where you parked,” Nichols said.
And after the trip with her son and his family in April, a Fast Park shuttle driver showed how the personal touch can mean a world of difference.

Nichols’ original flight through Orlando was rebooked to one with a layover in Baltimore— making it a 12-hour trip.
By the time she arrived at Raleigh-Durham International Airport, it was past 11 p.m., and she was exhausted.

In her haste to get back to her car and return home to sleep, Nichols left her phone on the bench at the Fast Park pickup site just outside the terminal—something she realized halfway back to the parking lot.
Nichols told the shuttle driver, and after everyone else was dropped off at their cars, he took her back to Terminal 1 to find the phone. While Nichols searched, Patrick tried calling the phone, and they discovered someone had turned it into lost and found at Terminal 2.
“So off we went again,” Nichols said, noting the shuttle driver, Patrick, went into the terminal to retrieve her phone. “I was already exhausted from traveling, so having the driver help me find and fetch my phone was amazing.”
While the circumstances were unusual, Nichols said the story exemplifies Fast Park’s service and how they went “above and beyond.”
By J odie Valade
days.
Surrounded by waist-high seedlings at the Durham Public School Hub Farm’s Spring Soils Festival, Dr. Clay Bordley is spreading his love of trees.
Affectionally known as “The Tree Guy,” Bordley tells a festivalgoer how black walnut trees, like the one in a nearby pot, make beautiful wood. He tells another about pawpaw trees’ delicious, albeit fleetingly ripe, fruit.
Bordley, an Emergency Pediatrician at Duke University Hospital, raised these trees on his 28-acre Panther Creek Forest Farm in Durham County. Now he’s giving them all away for free to anyone willing to plant them.
“I just want to get them in the ground,” Bordley said.
Since arriving at Duke in 2003, Bordley, 65, has been passionate about helping Duke’s youngest patients. He’s also passionate about growing trees to help restore Durham’s tree canopy.
“Every tree I grow is given back to the people of Durham so they can help the environment, provide shade and make people’s health better,” Bordley said.
A decade ago, he bought his farm to grow organic vegetables with his daughter, Eliza Lawdley. Realizing the land was ill-suited for that purpose, they sought a Plan B.
That’s when Bordley became intrigued by how trees benefit community health by removing airborne pollutants and combating urban heat islands. Inspired by non-profits such as Keep Durham Beautiful, which adds trees to areas of Durham without adequate coverage, he found his farm’s new purpose: a native tree nursery for Durham.
After years of trial and error, including a tangled grove of oaks grown from acorns found on Duke’s East Campus, he’s refined his approach. He now collects seeds from across Durham to plant in soil-filled wooden boxes. After a year of minimal care, sprouts will be ready to thrive in Durham.
“I call this area the ‘test kitchen,’” Bordley said about the boxes housing tender seedlings. “We’re trying to see what wants to grow here.”
Be bold. Be the difference.

Emerging from the soil are pawpaws from seeds gathered along a greenway, white oaks from seeds found in a parking lot, and cherrybark oaks from seeds donated by a former Duke faculty member. Healthy redbuds and tulip poplars rise alongside struggling persimmons and buckeyes.
Each fall, volunteers from the Duke University Medical School and the Nicholas School of the Environment help Bordley separate and pot the seedlings. After a year in pots, the trees are ready to donate to Keep Durham Beautiful and be given away at community events.
After roughly three years and nearing 1,000 donated seedlings, Bordley said he’s still learning about growing trees. But surrounded by boxes and pots filled with young branches reaching skyward, he’s found something he loves.
“I’m a pediatrician, not an expert in trees,” he said. “But I’m a lifelong learner. So, this has been really fun.”
By Stephen Schramm







