Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health
Indexed in MEDLINE
Education
1135 Resident-as-Teacher Curriculum: An Evidence-based Guide to Best Practices from the Council of Residency Directors in Emergency Medicine
J Jordan, M Gottlieb, M Estes, ME Parsons, K Goldflam, A Grock, BJ Long, S Nateson
1144 Large-Scale Combat Operation Education and Training Needs: Implications for Military and Civilian Medical Education
R Cole, K Crawford, M Farrell, L Vojta, SL Rudinsky
1154 Financial Burden of Emergency Medicine Residency Applications: Pre-, During, and Post-Pandemic
C Zeuthen, E Shappell, DJ Egan, E Barrall Werley, A Pelletier-Bui, CW Baugh, A Raynor, A Campbell, AP Mihalic, AD Luo
1162 Characteristics and Educational Support Resources Available to Emergency Medicine Core Faculty: A National Survey
J Jordan, LR Hopson, F Gallahue, JA Cranford, JC Burkhardt, KE Kocher, DL Robinett, M Weizberg, T Murano
1170 Building Connection and Resident Understanding of Local Resources Through Community Engagement
H Johnshoy, A Pavlic, S Khan, T Sonnenberg
Emergency Department Operations
1174 Accuracy of Triage Nurses in Predicting Patient Admissions: Retrospective, Large-sample
Evidence from a Community Emergency Department
C Armstrong, D Kanter-Eivin, M Dowling, G Sweeny, A El Galad, A Esleben, NK Duggirala, C Mitges, S Speck, S Strobel
1183 Prior Outpatient Care Use in Emergency Department Patients with Low- and High-acuity Conditions in Germany
YN Wu, M Möckel,D Huscher, A Fischer-Rosinský, T Keil, A Slagman






Penn State Health Emergency Medicine


About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.
Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania

FOR MORE INFORMATION PLEASE CONTACT:
Heather Peffley, PHR CPRP
Penn State Health Lead Physician Recruiter hpeffley@pennstatehealth.psu.edu


Western Journal of Emergency Medicine:
Emergency Care with Population Health Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Section Editors
Behavioral Emergencies
Bradford Brobin, MD, MBA Chicago Medical School
Marc L. Martel, MD
Hennepin County Medical Center
Ryan Ley, MD
Hennepin County Medical Center
Cardiac Care
Sam S. Torbati, MD Cedars-Sinai Medical Center
Emily Sbiroli, MD Palomar Medical Center
Climate Change
Gary Gaddis, MBBS University of Maryland
Clinical Practice
Cortlyn W. Brown, MD Carolinas Medical Center
Casey Clements, MD, PhD Mayo Clinic
Patrick Meloy, MD Emory University
Nicholas Pettit, DO, PhD Indiana University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Gabriel Wardi, MD University of California, San Diego
Joseph Shiber, MD University of Florida-College of Medicine
Matt Prekker MD, MPH Hennepin County Medical Center
David Page, MD University of Alabama
Erik Melnychuk, MD Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
John Broach, MD, MPH, MBA, FACEP
University of Massachusetts Medical School UMass Memorial Medical Center
Christopher Kang, MD Madigan Army Medical Center
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of MedicineIrvine, California
Shahram Lotfipour, MD, MPH, Managing Editor University of California, Irvine School of MedicineIrvine, California
Gary Gaddis MBBS, Associate Editor University of Maryland- Baltimore, Maryland
Rick A. McPheeters, DO, Associate Editor Kern Medical- Bakersfield, California
R. Gentry Wilkerson, MD, Associate Editor University of Maryland
Education
Danya Khoujah, MBBS
University of Maryland School of Medicine
Jeffrey Druck, MD University of Colorado
John Burkhardt, MD, MA University of Michigan Medical School
Michael Epter, DO Maricopa Medical Center
ED Administration, Quality, Safety
David C. Lee, MD Northshore University Hospital
Gary Johnson, MD Upstate Medical University
Brian J. Yun, MD, MBA, MPH Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of
Emergency Medicine
University of California, Davis
Emergency Medical Services
Daniel Joseph, MD Yale University
Joshua B. Gaither, MD University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD Yale School of Medicine
Stephen Meldon, MD Cleveland Clinic
Luna Ragsdale, MD, MPH Duke University
Health Equity
Emily C. Manchanda, MD, MPH Boston University School of Medicine
Faith Quenzer
Temecula Valley Hospital San Ysidro Health Center
Mandy J. Hill, DrPH, MPH UT Health McGovern Medical School
Payal Modi, MD MScPH
Michael Pulia, MD, PhD, Associate Editor University of Wisconsins Hospitals and Clinics- Madison, Wisconsin
Brian Yun, MD, MPH, MBA, Associate Editor Boston Medical Center-Boston, Massachusetts
Quincy Tran, MD, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston Texas
Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
University of Massachusetts Medical
Infectious Disease
Elissa Schechter-Perkins, MD, MPH Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Kevin Lunney, MD, MHS, PhD University of Maryland School of Medicine
Stephen Liang, MD, MPHS Washington University School of Medicine
Victor Cisneros, MD, MPH Eisenhower Medical Center
Injury Prevention
Mark Faul, PhD, MA Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH Prisma Health Richland
Taylor Burkholder, MD, MPH Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Melanie S. Heniff, MD, JD Indiana University School of Medicine
Greg P. Moore, MD, JD Madigan Army Medical Center
Statistics and Methodology
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS Pacific Northwest University
Rick Lucarelli, MD Medical City Dallas Hospital
William D. Whetstone, MD University of California, San Francisco
Neurosciences
Antonio Siniscalchi, MD Annunziata Hospital, Cosenza, Italy
Pediatric Emergency Medicine
Paul Walsh, MD, MSc University of California, Davis
Muhammad Waseem, MD
Lincoln Medical & Mental Health Center
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
Jacob Manteuffel, MD Henry Ford Hospital
John Ashurst, DO
Lehigh Valley Health Network
Tony Zitek, MD Kendall Regional Medical Center
Trevor Mills, MD, MPH Northern California VA Health Care
Erik S. Anderson, MD Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD Henry Ford Hospital
Phillips Perera, MD Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS Virginia Commonwealth University
Jeffrey R. Suchard, MD University of California, Irvine
Ultrasound
J. Matthew Fields, MD Thomas Jefferson University
Shane Summers, MD Brooke Army Medical Center
Robert R. Ehrman Wayne State University
Ryan C. Gibbons, MD Temple Health
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine



Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA.

Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org
No. 5: September 2025
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Editorial Board
Amin A. Kazzi, MD, MAAEM
The American University of Beirut, Beirut, Lebanon
Anwar Al-Awadhi, MD
Mubarak Al-Kabeer Hospital, Jabriya, Kuwait
Arif A. Cevik, MD
United Arab Emirates University College of Medicine and Health Sciences, Al Ain, United Arab Emirates
Abhinandan A.Desai, MD University of Bombay Grant Medical College, Bombay, India
Bandr Mzahim, MD
King Fahad Medical City, Riyadh, Saudi Arabia
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
David F.M. Brown, MD Massachusetts General Hospital/ Harvard Medical School
Douglas Ander, MD Emory University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Francesco Della Corte, MD
Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Hoon ChinStevenLim, MBBS, MRCSEd Changi General Hospital
Gayle Galleta, MD
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Jacob (Kobi) Peleg, PhD, MPH Tel-Aviv University, Tel-Aviv, Israel
Jaqueline Le, MD Desert Regional Medical Center
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jonathan Olshaker, MD Boston University
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Advisory Board
Kimberly Ang, MBA
UC Irvine Health School of Medicine
Elena Lopez-Gusman, JD
California ACEP
American College of Emergency Physicians
Amanda Mahan, Executive Director
American College of Osteopathic Emergency Physicians
John B. Christensen, MD
California Chapter Division of AAEM
Randy Young, MD
California ACEP
American College of Emergency Physicians
Mark I. Langdorf, MD, MHPE UC Irvine Health School of Medicine
Jorge Fernandez, MD
California ACEP
American College of Emergency Physicians University of California, San Diego
Peter A. Bell, DO, MBA
American College of Osteopathic Emergency Physicians Baptist Health Science University
Robert Suter, DO, MHA
American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Shahram Lotfipour, MD, MPH UC Irvine Health School of Medicine
Brian Potts, MD, MBA California Chapter Division of AAEM Alta Bates Summit-Berkeley Campus
Khrongwong Musikatavorn, MD
King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Nadeem Qureshi, MD St. Louis University, USA Emirates Society of Emergency Medicine, United Arab Emirates
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Rachel A. Lindor, MD, JD Mayo Clinic
Robert M. Rodriguez, MD University of California, San Francisco
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Samuel J. Stratton, MD, MPH Orange County, CA, EMS Agency
Scott Rudkin, MD, MBA University of California, Irvine
Scott Zeller, MD University of California, Riverside
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Editorial Staff
Ian Olliffe, BS Executive Editorial Director
Sheyda Aquino, BS WestJEM Editorial Director
Tran Nguyen, BS CPC-EM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Cassandra Saucedo, MS Executive Publishing Director
Isabelle Kawaguchi, BS WestJEM Publishing Director
Alyson Tsai CPC-EM Publishing Director
Isabella Choi, BS Associate Publishing Director
June Casey, BA Copy Editor
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine




Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Email: Editor@westjem.org
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
JOURNAL FOCUS
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
Table of Contents
1192 Analysis of Emergency Department-based Intensive Care Units on Coding and Revenue
MH Sherman, VL Kan, P Gibbons, J Garrell, MA Reznek
1202 Telehealth Emergency Department Transition-of-care Program: A Value-based Innovation
A Kreshak, I Fadlon, K Malaviya, V Tolia, L Pierce, T Chan,P Agnihotri, M Tai-Seale
1211 Characteristics of Emergency Department Patients Referred to an Undiagnosed Mass Clinic
B Beel, RT McKenna, JW St Clair, JM Irizarry-Alvarado, GE Coltvet, JM Sheele
1217 Emergency Department Utilization and Patient Acuity in the Setting of Care-Seeking Hesitancy: Insights from the COVID-19 Pandemic
E Frazier, N Modallalkar, N Dunn, B Chakravarthy, L Gonzales, S Saadat
1226 Foundations of Emergency Medicine: Application of a Flipped-Classroom Curriculum for Advanced Practice Clinician Education
S Lindsey, TP Moran, MA Stauch, AL Lynch, J Leaumas, K Grabow Moore
Health Equity
1232 Emergency Department Wait Times for Urgent Evaluation by Race, Ethnicity, and Language: A Single-center Retrospective Study
JA Carreras Tartak, AV Grossestreuer, D Chiu, B Stenson
1244 Accessibility of Urgent Care Centers: A Socioeconomic and Geospatial Evaluation
P Telagi, R Sadler, P Telagi, K McGurk
1250 Inequities in the National Clinical Assessment Tool for Medical Students in the Emergency Department
BZ Amin, CJ Dine, ER Tabakin, M Trotter, JK Heath
1260 Narrative Review of Emergency Medicine Clinical Research Examining Exclusion by Language
AM Curt, O Kahn-Boesel, M Lydston, MA Meeker, ME Samuels-Kalow
Emergency Medical Services
1265 Emergency Medical Services Time on Scene and Non- Transport: Role of Communication Barriers
E Kurkurina, C Rothenberg, K Couturier, A Breyre, D Yang, AR Nelson, A Cordone, AK Venkatesh, CJ Gettel
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Table of Contents continued
1274 Physician Attitudes on Integration of Prehospital Patient Care Report into Hospital Electronic Health Record
M Smith, C Given, S Saadat, K Leung, J Afraisiabi, R Katzer
1280 Emergency Medical Services Policies and Perspectives Leading to Ambulance Engine Idling
M Lyons, AR Kuzel, S Marks, C Ziegler, K Nix
1291 Refusal of Emergency Medical Transport After a Fall: Patient Characteristics and Outcomes of Repeat Callers
J Barr, K Selman, K Hunter, A Kuc
Cardiology
1296 Untreated Hypertension and Diabetes in the Chest Pain Observation Unit
BT Hutchison, NP Ashburn, AC Snavely, MD Shapiro, MA Chado, AP Ambrosini, AA Biglari, HA Cannon, MJ Millard, AG Dameron, SA Mahler
1305 Potential Impact of Using Canadian Syncope Risk Score on Emergency Department Hospitalizations for Syncope
AW Harris, L LaBonte, G Massaccesi, B Stryckman, BA Myers, DB Gingold, RG Wilkerson
1313 Does Single Dose Epinephrine Improve Outcomes for Patients with Out-of-Hospital Cardiac Arrest by Sex or Race?
BL Blaschke, NP Ashburn, AC Snavely, K Dev, TA George, BP Beaver, MA Chado, HA Cannon, JE Winslow, RD Nelson, JP Stopyra, SA Mahler
1322 Comparison of Cardiopulmonary Resuscitation Quality in a Simulated Model: At Incident Scene vs During EMS Transport
M Çetin, G Yilmaz, E Guvenç, V Ergun, E Şener Araz, B Bayram, BJ Long, M Gottlieb, WJ Brady
Climate Change
1321 Association of Rising Ambient Temperatures with Increased Violence Worldwide: Systematic Review and Meta-Analysis
V Chauhan, S Thakur, S Galwankar, S Temple
1338 Impact of Daily Maximum Temperature on Emergency Department Arrivals and Acuity Levels
C Giudice, NJ Arisco,Z Lu, B Stenson, C Dresser
1345 Emergency Department Management of Acute Heatstroke: A Retrospective Analysis from Phoenix, Arizona
JR Stowell, P Pugsley, M McElhinny, G Comp, J Pearlmutter, M Akhter, D Sklar
Trauma
1355 Report on the El Paso Mass Casualty Incident Hospital Response: Enhancing Surge Capacity
SF McLean, N Weber, A Adler, A Rios, S Flaherty, AH Tyroch
1367 Examining Canadian Trauma Centres’ Analgesic Protocols for Rib Fractures
S Yu, P Patton, K Vogt, F Priestep, R Hilsden, S Smith, I Ball
Critical Care
1374 Intubating Stylets in the Emergency Department: A Video Review of First-pass Success and Time
R Che, N Nazir, A Badar, A Honnur, M Newton, A-R Mohammed Samour, T Samour, D Clutter, A Pirotte
Western Journal of Emergency Medicine
: Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Table of Contents continued
1380 Impact of Interventions on Peri-Intubation Hypoxemia and Hypotension in Critically Ill Patients: Systematic Review and Meta-Analysis
CE Ren, JV Downing, S Cardona, I Yardi, M Zahid, K Tang, V Bzhilyanskaya, A Pourmand, QK Tran
Emergency Department Workforce
1392 Five-Year Trends in Emergency Medicine Match Results and Future Outlook
AY Sheng, EL Simon, T Friedmann, E Garcia, V Karalius, Michael Kiemeney, B Merritt, B Milman, M Mitchell, J Mugfor, M Patel, R Wong, EH Chen
1397 Burnout in the Emergency Department: Survey of Prevalence and Modifiable Risk Factors
M Kraus, M Fischer
Geriatrics
1404 Emergency Medicine Residents’ Perceptions of Geriatric Emergency Medicine and Careers: A Qualitative Study
K Selman, AE Jones, C Curran, L Cameron-Comasco, WC Coates, A Li, K Tyler, F Bellolio, SW Liu
1414 Pharmacogenomic Drug-Gene Interactions in Geriatric Emergency Department Patients Who Sustained Falls: A Pilot Study
RD Shih, G Engstrom, AS Pandya, GB Fields, B Furht, AA Danesh, SM Alter, H Munoz, LM Clayton, JJ Solano, T Buckley, O Hung, A Farag, M Wells
Technology in Emergency Medicine
1423 Multicenter Study Evaluating Impact of Patient and Sonographer Demographics on Quality of Focused Cardiac Ultrasounds
B Zimmerman, TE Madsen, G Giampaolo, J Rogers, H Davenport Stroud, C Turner Boulger, MI Prats, A Wu, M Leo, JR Pare, M Muruganandan, J Kaine, DS Brenner, P Cruz Soriano, N Aracelliz Villarroel, ML Schroeder, N Strokes. A Tyson, T Gleeson, M Hill, J Baird, AJ McGregor, KH Dwyer
1431 Supra-Short Ultrasound Protocol for Rotator Cuff Tears in the Emergency Department: Pilot Study
T Zitek. RA Farrow II, M Shalaby, D Puebla, A Sanoja, E Lopez, J McShannic, Y Lee, N Warren, D Lamour, J Perex, M Rosselli
Pediatrics
1438 Comparing Pediatric 72-Hour Emergency Department Returns: General vs Pediatric Emergency ` Departments
D Libov, M Zocchi, A Venkat, T Ruttan, C Allen, M Wilkinson, US Acute Care Solutions Research Group
Neurology
1446 Lorazepam in Managing Atypical Neuroleptic Malignant Syndrome: A Systematic Review of Case Reports
A Chen, M Bae
Behavioral Health
1454 Alcohol Intoxication in the Academic Emergency Department: Epidemiology and Facility-Fee Financial Impact
E Legome, W Bonadio, M Redlener, E Lavine, A Mealy, SE Sondheim
Toxicology
1459 Unmasking the Hidden Risk of Systemic Toxicity from Topical Salicylates
N Tabatabai, S Dash, JA Chenoweth, TE Albertson
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Injury Prevention
Table of Contents continued
1468 Self-Harm and Interpersonal Violence-Related Injuries: Retrospective Analysis of the American College of Surgeons Trauma Quality Programs Data
A El-Menyar, A Mekkodathil, R Consunji, S Rizoli, TS Abulkhair, R Peralta, R Latifi, H Al-Thani
Musculoskeletal
1478 Nerve Blocks for Hip Fractures in the Emergency Department: An Opportunity for Growth
R Allen, D Berzins, L Koroshetz, C Nok Lam, M Wilson, M Cruz, J Huang, D Sajed, T Mailhot
Clinical Practice
1485 Acute Care of Patients with Moderate Respiratory Distress: Recommendations from an American College of Emergency Physicians Expert Panel
CW Baugh, JF Neuenschwander, J Lenox, J Hoh, K Ward, S Muramoto, J Casey, A Anzueto, H Ishaq, J Mount, PM DeBlieux
Letters to the Editor
1495 Recent Interventions for Acute Suicidality Delivered in the Emergency Department: A Scoping Review
K Dowdell, MP Wilson
1497 Reply: Recent Interventions for Acute Suicidality Delivered in the Emergency Department: A Scoping Review
AP Hood, LM Tibbits, JI Laporta, J Carrilo, LR Adams, S Young-McCaughan, AL Peterson, RA DeLorenzo
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber
Alameda Health System-Highland Hospital Oakland, CA
Arnot Ogden Medical Center Elmira, NY
Ascension Resurrection Chicago, IL
Atrium Health Wake Forest Baptist Winston-Salem, NC
Baystate Medical Center Springfield, MA
Beth Israel Deaconess Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Capital Health Regional Medical Center Trenton, NJ
Carolinas Medical Center Charlotte, NC
Cedars-Sinai Medical Center Los Angeles. CA
Cleveland Clinic Cleveland, OH
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/Wayne State University Detroit, MI
Duke University Hospital Durham, NC
Eisenhower Health
Rancho Mirage, CA
Emory University Atlanta, GA
ESO Austin, TX
Franciscan Health Olympia Fields Olympia Fields, IL
Geisinger Health System
Danville, PA
George Washing University Washington, DC
HealthPartners - Regions Hospital St Paul, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Hospital Detroit, MI
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
Henry Ford Wyandotte Hospital Wyandotte, MI
INTEGRIS Health
Oklahoma City, OK
Kaweah Delta Health Care District
Visalia, CA
Kern Medical Bakersfield, CA
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Maimonides Medical Center Brooklyn, NY
Massachusetts General Hospital Boston, MA
Mayo Clinic College of Medicine Rochester Rochester, MN
Mayo Clinic College in Arizona Phoenix, AZ
Mayo Clinic College in Florida Jacksonville, FL
Medical College of Wisconsin Affiliated Hospitals Milwaukee, WI
Morristown Medical Center Morristown, NJ
Mount Sinai Medical Center Miami Beach
Miami Beach, FL
Mount Sinai Morningside (West) New York, NY
North Shore University Hospital Manhasset, NY
New York - Presbyterian Brooklyn Methodist Hospital Brooklyn, NY
NYU Langone Health - Bellevue Hospital New York, NY
Ochsner Medical Center New Orleans, LA
Ohio State University Wexner Medical Center Columbus, oH
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Prisma Health - University of South Carolina School of Medicine Greenville, SC
California Chapter Division of American Academy of Emergency Medicine
Riverside Regional Medical Center Newport News, VA
Rush University Medical Center Chicago, IL
Rutgers Robert Wood Johnson Medical School New Brunswick, NJ
Saint Louis University School of Medicine St Louis, MO
Sarasota Memorial Hospital Sarasota, FL
Seattle Children’s Hospital Seattle, WA
Summa Health System Akron, OH
SUNY Upstate Medical University Syracuse, NY
Swedish Hospital Part of NorthShore Chicago, IL
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
The University of Texas Medical Branch Galveston, TX
Trinity Health Muskegon Hospital Muskegon, MI
UMass Memorial Health Worcester, MA
University at Buffalo Buffalo, NY
University of Alabama Medical Center Birmingham, AL
University of Arizona College of MedicineTuscon Tucson, AZ
University of California, Davis Medical Center Sacramento, CA
University of California, San Francisco General Hospital
San Francisco, CA
UCSF Fresno Fresno, CA
University of Chicago, Chicago, IL
University of Cincinnati Medical Center Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida, Jacksonville Jacksonville, FL
Mediterranean Academy of Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all
please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
University of Illinois at Chicago Chicago, IL
University of Iowa Hospitals and Clinics Iowa City, IA
University of Kansas Health System Kansas City, KS
University of Louisville Louisville, KY
University of Maryland School of Medicine Baltimore, MD
University of Michigan Ann Arbor, MI
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Ottawa Ottawa, ON
University of Pennsylvania Health System Philadelphia, PA
University of South Alabama Mobile, AL
University of Southern California - Los Angeles General Medical Center Los Angeles, CA
University of Tennessee Knoxville, TN
University of Texas MD Anderson Cancer Center
Houston, TX
University of Utah School of Medicine
Salt Lake City, UT
University of Vermont Medical Center
Burlington, VT
University of Washington - Harborview Medical Center
Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
Valleywise Health Medical Center Phoenix, AZ
Wellspan York Hospital York, PA
West Virginia University Morgantown, WV
Wright State University Boonshoft School of Medicine
Dayton, OH
Yale School of Medicine New Haven, CT






Resident-as-Teacher Curriculum: An Evidence-based Guide to Best Practices from the Council of Residency Directors in Emergency Medicine
Jaime Jordan, MD, MAEd*†
Michael Gottlieb, MD‡
Molly Estes, MD§
Melissa E. Parsons, MD||
Katja Goldflam, MD#
Andrew Grock, MD*
Brit J. Long, MD¶
Sree Natesan, MD**
David Geffen School of Medicine at University of California Los Angeles, Department of Emergency Medicine, Los Angeles, California
Oregon Health & Science University, Department of Emergency Medicine, Portland, Oregon
Rush University Medical Center, Department of Emergency Medicine, Chicago, Illinois
Northwestern University, Department of Emergency Medicine, Chicago, Illinois
University of Florida College of Medicine, Department of Emergency Medicine, Jacksonville, Florida
Yale School of Medicine, Department of Emergency Medicine, New Haven, Connecticut
Brooke Army Medical Center, Department of Emergency Medicine, San Antonio, Texas
Duke University, Division of Emergency Medicine, Durham, North Carolina
Section Editor: Kendra Parekh, MD, MHPE
Submission history: Submitted December 14, 2024; Revision received May 17, 2025; Accepted May 17, 2025
Electronically published September 24, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.41493
Improving resident teaching skills is an expectation of training. Despite the recognized importance of resident-as-teacher (RaT) curricula, variability indicates the need for evidence-based guidelines to inform best practices. This paper outlines expert guidelines for the development, implementation, and evaluation of RaT curricula from the members of the Council of Residency Directors in Emergency Medicine Best Practices Subcommittee, based on a critical review of the literature. It is important to perform a needs assessment prior to creating and implementing a RaT curriculum. The RaT curricula should include instruction on adult learning theory, feedback, and classroom and bedside teaching techniques. Outcomes of RaT curricula should be assessed using multiple sources including direct observation and incorporate both knowledge and skill retention, as well as acquisition. [West J Emerg Med. 2025;26(5)1135–1143.]
BACKGROUND
Training future physicians to be teachers is an important curricular component of residency programs and supported by the Accreditation Council for Graduate Medical Education (ACGME), which states that residents are expected to participate in the education of patients, families, students, residents, and other health professionals and should be encouraged to teach using a scholarly approach.1 Residentas-teacher (RaT) curricula hold the potential to provide numerous benefits to residents, medical students, and patients by enhancing teaching skills that allow for transfer of knowledge.2-17 Benefits of RaT programs across medical specialties include improved teaching skills, self-reflection,
self-efficacy in teaching, and improved educational outcomes for both residents and their learners, as well as better outcomes for patient care.2-17
Despite recommendations to provide this training in residency and a substantial body of literature on the topic, there is no standard approach to RaT curricula.1 This deficit can lead to variability in education skill development for resident trainees. It also leaves education leaders uncertain about how to best provide this important training in their programs. While a few prior reviews have sought to address this topic, they include only a small number of papers, are narrow in scope (focusing on the benefits and effectiveness of RaT curricula rather than how to best deliver this type of
instruction), and may be outdated and not reflect the current literature available.6,9,13,17 Therefore, a critical need exists to develop best practices and evidence-based guidelines to optimize RaT curricular content, implementation, and evaluation in graduate medical education training programs.
Based on the best available evidence through a critical review of the literature, we offer expert guidelines on RaT curricular content, implementation, and evaluation from members of the Council of Residency Directors in Emergency Medicine (CORD) Best Practices Subcommittee. This paper provides readers with recommendations on the content, educational strategies, curricular implementation, and program evaluation for RaT curricula.
CRITICAL APPRAISAL
This is the 11th paper in a series of evidence-based best practice reviews from the CORD Best Practices Subcommittee.18-27 The author group consists of expert emergency medicine (EM) educators and education researchers with experience in residency program education and leadership. We conducted a literature search in conjunction with a medical librarian using MEDLINE with a combination of Medical Subject Heading terms and keywords focused on RaT curricula searching for papers published from inception to December 31, 2023 (Supplemental Appendix 1). We also reviewed the bibliographies of all included papers. Two authors (JJ and SN) independently screened and included papers that addressed RaT curricula development, implementation and evaluation. We excluded papers that were not related to RaT curricula development, implementation, or evaluation. We also excluded papers that were not in English, were abstracts only, or did not have full text available. Papers were included based on agreement of the two screeners. The two screeners resolved discrepancies through in-depth discussion and negotiated consensus.
Population Health Research Capsule
What do we already know about this issue? Resident-as-teacher (RaT) curricula are an important part of residency training and have many potential benefits.
What was the research question?
What are best practices for RaT curricular content, implementation, and evaluation in graduate medical education training programs?
What was the major finding of the study? This paper offers expert recommendations for best practices on RaT curricular content, implementation, and evaluation.
How does this improve population health? Improving teaching skills ultimately leads to better education outcomes for residents and better care of their patients.
The search yielded 1,486 papers, of which 89 were deemed to be directly relevant to this review (Supplemental Appendix 2). The author group derived their best practice recommendations based on the literature review and discussion among the expert author group. The level and grade of evidence were provided for each best practice statement implementing the Oxford Center for EvidenceBased Medicine criteria (Tables 1 and 2).28 When supporting data were not available, recommendations were made based upon the authors’ combined experience and consensus opinion. Prior to submission, the manuscript was reviewed by the CORD Best Practices Subcommittee and posted to the CORD website for two weeks for peer review by the entire CORD medical education community. Upon completion of the review period, there was general agreement, and no substantial changes to the guideline were recommended. Level of Evidence Definition 1a
Systematic review of homogenous RCTs
RCT
Systematic review of homogenous cohort studies
Individual cohort study or a low-quality RCT*
Systematic review of homogenous casecontrol studies
Individual case-control study**
Case series/Qualitative studies or lowquality cohort or case-control study***
Expert/consensus opinion
*Defined as <80% follow up; **includes survey studies and crosssectional studies; ***defined as studies without clearly defined study groups.
RCT, randomized controlled trial.
RESIDENT-AS-TEACHER CURRICULAR CONTENT AND EDUCATIONAL STRATEGIES
Of the reviewed papers, few included a formal needs assessment beyond a review of the literature. Residents’ responsibility to teach students, other residents, and other
Table 1. Oxford Centre for Evidence-Based Medicine levels of evidence.28
Table 2. Oxford Centre for Evidence-Based Medicine grades of recommendation.28
Grade of Evidence Definition
A Consistent Level 1 studies
B Consistent Level 2 or 3 studies or extrapolations* from Level 1 studies
C Level 4 studies or extrapolations* from Level 2 or 3 studies
D Level 5 evidence, or troublingly inconsistent or inconclusive studies of any level
*“Extrapolations” refers to data being used in a situation that has potentially clinically important differences than the original study situation.
staff is well recognized, as is the need to provide training to prepare residents for their roles as teachers.29 Reasons for implementing RaT curricula include the following: to teach a skill important to the resident role; meet residents’ desire for formal training in education; address regulatory requirements; and prepare trainees for future career roles.1,30 General curricular goals included improving resident formal and informal teaching skills in both classroom and clinical settings and increasing resident confidence in teaching skills.29,31 The RaT curricula reviewed contain diverse components. The topics most consistently included in RaT curricula were adult learning theory, creating a positive learning environment and setting objectives, clinical or bedside teaching techniques, classroom teaching techniques, and how to give feedback.10-12,14,15,29-60
Adult learning theory—which describes how adults learn best when material is problem-centered, relevant to their work, and when they are involved in the planning and evaluation of their instruction—was a major component of RaT curricula, both as a framework for the curricular development and a topic of instruction for learners.10,29,31-42 Adult-learning theory was often considered in how RaT curricula was applied.34,35,61 For example, RaT leaders factored this in for determining the length, frequency, and formatting of these educational sessions within the curricula. 34,35,61
Many curricula also include adult learning principles as part of their educational content.11,29, 33,35-42,49,56 Berger et al provided a primer for anesthesiology residents about adult learning principles by having the learners discuss effective and ineffective teaching moments that they remembered in their education.11 They also had learners review literature on adult learning principles and watch a video demonstration.11 Similarly, Chee et al had residents identify effective and ineffective teaching strategies observed in video clips to better understand adult learning theory.35 Choski et al had learners review two papers on adult learning theory to better understand adult education principles.36 Another group used formal lectures on adult learning theory followed
by debriefing.29 Tang Girdwood et al revised a previous curriculum by removing the PowerPoint lecture on adult learning theory and instead having residents teach the principles of adult learning theory to one another with a faculty facilitator present.42
Many RaT curricula sought to teach residents how to set the stage for learning.11,12,15, 31,32,34-36,38,43-49 Curricular content included how to create a positive learning environment and recognize behaviors that can lead to an environment of harassment or learner mistreatment.12,31,35,43,44 Understanding how to set goals and expectations with learners to facilitate knowledge and skill acquisition was also an important topic included in RaT curricula.11,15,31,32,34,36,38,44-49
Clinical or bedside teaching techniques and tools was another commonly included topic in RaT curricula.10,14,15,29-31,33,37-42,44,46-48,50-55 One survey study in EM found that 84% of programs reported bedside teaching to be a major focus of their educational curriculum.32 One of the most frequently included teaching tools was the One-Minute Preceptor.31,32,37,44,47,51,52.54,57,62 Ahn et al found that 45% of RaT programs in a single specialty incorporated training on the One-Minute Preceptor.32 In another example, curricula learners were asked to describe the elements of this model, apply the model to a simulated learner’s patient presentation, and use the model to assess the learner’s knowledge level and identify educational points.31 Content specific to procedural teaching was included in many curricula. 5,10,11,15, 29,32,33,35-37,41,46,53,55,57,59
In addition to the clinical setting, many RaT curricula also seek to prepare residents for teaching in the classroom by including content on didactic, small group, and case-based instruction.11,15,31,32,38,41,42, 45,46,48,50,53,54,56-58 While these content areas were often listed as topics or titles of educational sessions included in curricula, there was little additional description in the included studies as to what these content areas were comprised of. Many curricula also included content on the use of simulation in education.14,32,42,53,55,57,63
Feedback was also consistently included in RaT curricula.8,10-12,14,15,29,31-38,40-44,46-48,50,52,53,55,59,60 One study found that 96% of EM residency programs that had RaT curricula included feedback as a major focus.32 Specific content areas related to feedback included techniques and components of effective feedback, optimizing the environment for feedback, and how to receive feedback.33 Curricula often included interactive activities, during which the learners could practice feedback interactions via role-play and debrief with the other learners.30,33 Other RaT curricular content included education to augment teaching such as communication skills, professionalism, and how to deal with difficult learning situations.32,46,50,57,58 Some curricula also included content that could help prepare residents as education professionals such as mentorship and role modeling, curricular design, time management, and learner assessment.15,32,40,46,57,60,64 We provide a summary of RaT curricular content and educational strategies in Tables 3 and 4.
Resident-as-Teacher Curriculum: Evidence-based Guide to Best Practices
Table 3. Summary of content in resident-as-teacher curricula.
Curricular Content
Adult learning theory
Number of Papers
14 8, 10, 29, 31, 33-42
Assessment of learners 1 60
Case-based instruction
Clinical/bedside instruction
Communication skills
References
7 8, 11, 42, 46, 54, 57, 58
23 10, 14, 15, 29, 30, 31, 33, 37-42, 44, 46-48, 50-55
4 8, 46, 57, 58
Creating a positive learning environment 5 12, 31, 35, 43, 44
Curriculum design 2 8, 46
Didactic instruction 10 11, 15, 31, 38, 42, 45, 48, 50, 53, 54
Difficult learning situations 2 8, 50
Feedback 28 8, 10-12, 14, 15, 29, 31, 33-38, 40-44, 46-48, 50, 52, 53, 55, 59, 60
Mentorship 2 8, 40
Procedural instruction
Professionalism and role modeling
Setting goals and expectations
16 5, 8, 10, 11, 15, 29, 33, 35-37, 41, 46, 53, 55, 57, 59
5 8, 15, 46, 57, 64
13 8, 11, 15, 31, 34, 36, 38, 44-49
Simulation instruction 7 8, 14, 42, 53, 55, 57, 63
Small group instruction 7 8, 41, 46, 50, 53, 56, 57
Time management 2 8, 46
Table 4. Summary of educational strategies in resident-as-teacher curricula.
Educational Strategy
Didactic lectures
Direct observation and feedback
Iterative reminders / staged repetition
Simulation/role playing
Small groups
Virtual sessions/electronic handouts
Workshops
Best Practices Recommendations
Number of Papers
References
22 5, 7, 8, 12, 17, 29, 33, 37, 38, 42, 47, 57, 58, 64, 71, 75, 86, 87, 93, 95, 103, 104
13 29, 31, 49, 56, 57, 59, 66, 69, 71, 87, 88, 94, 104
4 29, 31, 61, 71
12 12, 14, 31, 37, 57, 64, 69, 70, 75, 87, 88, 91
6 12, 36, 37, 56, 69, 93
7 5, 41, 43, 61, 71, 86, 97
21 4, 15, 17, 31, 33, 37, 38, 44, 48, 52, 54, 57, 59, 62, 64, 65, 66, 83, 87, 98, 104
Resident-as-teacher curricula should include the following:
1. Teaching techniques applicable to both classroom and bedside settings (Level 1, Grade A).
2. Effective feedback techniques that educators can use to provide feedback to learners (Level 1, Grade B).
3. Adult learning theory as part of the framework of the curriculum and its delivery, as well as an educational component of the curriculum. (Level 2, Grade B).
RESIDENT-AS-TEACHER CURRICULAR LOGISTICS AND IMPLEMENTATION
Timing, duration, and frequency of interventions varied greatly among studies and specialties, with no overarching consensus on ideal approaches. The most common
approach included single interventions, usually early in intern year or during residency orientation, with most one-day curricula ranging from 4-8 hours.44, 47, 59, 60, 62, 65-67
According to a landmark paper published by Morrison et al in 2004, the average total time for a RaT curriculum was 11 hours, with their institutional published curriculum lasting for 13 total cumulative hours of longitudinal instruction.68, 69 Some longitudinal curricula had longer durations including those that spanned the entire length of resident training. 12, 29, 31, 38, 42, 49, 54, 55
Staffing of the educational sessions was largely by general residency faculty who participated in didactics, mentorship, or evaluations of resident teaching.56, 58, 59, 62, 69, 70 Sometimes faculty with additional training or specialization in education led or designed the curricula, which included
“educational experts,” designated education faculty, and education fellows.12, 15, 70 Additionally, residents themselves often contributed, including chief residents and teach-theteacher models.47, 58
Several barriers were identified in the implementation of RaT curricula, with the most frequently mentioned being the balance of workload on faculty and residents.71, 48, 58 Both the total time required for participation and instruction as well as real-time balancing responsibilities of patient care with teaching while working clinically were noted. 37, 57, 72, 73 Additionally, many residents felt it was challenging to teach topics that they themselves still did not feel quite familiar with, even for the sake of experiential learning. 37, 43, 57 Lastly, despite ACGME supportive program requirements, some program directors felt that RaT curricula were not a priority among other competing educational demands.1, 58,74
A needs assessment before creating and implementing a RaT curriculum can help confirm interest, elucidate clear, specific program goals for participants, and secure buy-in from faculty and leadership.37, 56, 58, 75 Buy-in from residents was less challenging, with many residents confirming that they lacked self-confidence in their own teaching abilities, wanted mentorship in this area, and were willing to spend time to gain this experience.5, 59, 76 Medical students, who along with junior residents, were frequently the recipients of the outcomes of RaT, identified residents as more approachable than faculty and appreciated near-peer teaching.73, 77-79
Administration of RaT curricula may be challenging due to the resources required for successful implementation. This includes the number of faculty needed and time for residents to participate in curricular sessions, as well as time to learn and practice these skills while working clinically.58,70 Through an online survey of 47 residency programs and iterative expert consensus building, McKeon et al proposed the following key components to a successful RaT curriculum: required trainee participation; evaluations and feedback of resident teaching; recognition of excellence through teaching awards; and faculty teaching evaluations
Best Practices Recommendations:
1. General residency faculty can teach, provide mentorship, and evaluate participants in RaT curricula (Level 2a, Grade B).
2. Perform a needs assessment prior to implementing a RaT curriculum (Level 3a, Grade B).
3. Identify and address barriers such as time limitations for residents and faculty when implementing a RaT curriculum (Level 4, Grade C).
RESIDENT-AS-TEACHER CURRICULAR OUTCOMES/EVALUATION
When evaluating a RaT program, it is critical to use a robust model, accounting for various inputs, outputs, and outcomes. Examples of relevant program evaluation frameworks include the Kirkpatrick framework, the Logic Model, and CIPP (Context, Input, Process, Products).81,82 Despite this, most studies did not explicitly state the program evaluation framework they used.
While many studies included only a single or limited number of outcome measures individually, when assessed as a whole, there were a wide range of potential outcomes assessed (Table 5). The most common form of learner assessment was self-surveys of perceived effectiveness after a RaT program.4-7, 9-12, 14, 31, 33, 35, 39, 42, 44, 48, 49, 51, 54-56, 58, 61, 62, 65, 66, 71, 74, 83-97 A few studies also conducted delayed self-assessments at 3-12 months following RaT course completion.11,44, 51 One study assessed differences in attitude toward teaching after the course, while others performed knowledge assessment tests.36, 43, 44 Another study assessed actual use of the skills in subsequent teaching.52
Skill assessments were performed using either direct observation or structured assessments in a simulated environment. Several studies directly observed resident teaching, while others video-recorded resident teaching for delayed assessments.6, 49, 71, 72, 74, 87 Other measures included end-of-shift teaching evaluations completed by faculty.56, 58, 74 The most common assessment, using simulation, was the Objective Structured Teaching Exercise (OSTE).6, 9, 36, 38, 41, 46, 49, 54, 63, 71, 74, 84, 87, 92, 96, 98 The OSTEs were incompletely reported; they often ranged from 6-8 stations and were 2-4 hours in length. One study used the Debriefing Assessment for Simulation in Healthcare (DASH) instrument instead of the OSTE.14 Another assessed both initial and delayed OSTE as part of a randomized trial.75
Additional measures were obtained via learners (eg, students, junior residents). Learner assessments used a variety of measures of teaching effectiveness, although most had limited validity evidence.4, 6, 9, 10, 14, 39, 47, 48, 62, 66, 71, 74, 84-89, 97, 99, 100
One study used the Stanford Faculty Development Program—a 25-item tool assessing learning climate, control of teaching sessions, communicating goals, promoting understanding and retention, evaluation, feedback, and promoting self-directed learning.47 Another study evaluated the effect of the intervention by comparing course/rotation evaluations from students.48
linked to annual faculty review but not to salary or promotion.80 Finally, a RaT curriculum should be iteratively refined to ensure optimization of its content.42
One study focused on the feasibility to inform broader implementation.38 A few other select studies assessed organizational changes and broader outcomes. Two studies found that the RaT program led to substantive changes, which resulted in residency programs converting to this model going forward.60,101 Others assessed downstream effects on student learning by comparing student Objective Structured Clinical Examinations (OSCE) or Objective Structured Assessments of Technical Skills (OSATS) between those taught by residents completing the RaT program vs those who did not.63, 102
RaT, resident as teacher.
Resident-as-Teacher Curriculum: Evidence-based Guide to Best Practices Jordan
Table 5. Summary of methods of outcome assessments in resident-as-teacher curricula.
Educational Strategy
Observed Structured Teaching Evaluation
Survey of faculty
Survey of learners
Semi-structured interview
Best Practices Recommendations:
Number of Papers References
12 14, 15, 17, 37, 41, 49, 54, 69, 70, 75, 87, 98
4 7, 17, 54, 58
36 4, 7, 8, 12, 14, 17, 29, 31, 33, 37, 38, 42, 44, 47, 48, 51, 54, 56, 57, 58, 61, 62, 65, 66, 71, 73, 83, 86, 91, 94, 96, 97, 100, 103-105
1 59
1. RaT outcomes should be assessed using multiple sources of data (Level 1b, Grade B).
2. Use OSTE or direct observation to directly assess RaT outcomes (Level 1b, Grade B).
3. Incorporate delayed assessment for skill retention (Level 1b, Grade B).
4. Use higher level outcome assessments, such as learner evaluations or assessments (Level 3b, Grade B).
RaT, resident as teacher; OSTE, Observed Structured Teaching Evaluation.
LIMITATIONS
Although we performed a comprehensive search guided by a medical librarian in conjunction with a bibliographic review and expert consultation to augment content when needed, we used a single search engine, and it is possible that we may have missed some pertinent papers. In instances where evidence in the form of high-quality data was limited or lacking, we relied upon expert opinion and group consensus for the best practice recommendations. Finally, in areas where evidence was not available, we used the consensus from the expertise of our authorship group. While our author group possesses experience in research and scholarship in both RaT curricula and medical education, there was a potential for bias to have been introduced during this process. Therefore, we also sought peer review from the CORD Best Practices Subcommittee and posted it online for open review feedback by the CORD community.
CONCLUSION
Resident-as-teacher curricula are a vital component of graduate medical education training programs. This paper provides guidance on best practices for developing, implementing, and evaluating RaT curricula.
ACKNOWLEDGEMENTS
The authors would like to thank the members of the Council of Residency Directors in Emergency Medicine (CORD) and the members of the CORD Best Practice Committee for their review and feedback of this manuscript. The authors would also like to acknowledge Samantha
Kaplan, PhD, Medical Librarian, Duke University, Durham, NC, for her contributions.
Address for Correspondence: Jaime Jordan, MD, MAEd, Oregon Health & Science University, Department of Emergency Medicine, 3181 SW Sam Jackson Park Road, Portland, OR 97239. Email: jaimejordanmd@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Jordan et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements (Residency). 2022. Accessed December 5, 2024. Available at chrome-extension:// bdfcnmeidppjeaggnmidamkiddifkdib/viewer.html?file=https:// www.acgme.org/globalassets/pfassets/programrequirements/ cprresidency_2023.pdf
2. Bordley DR, Litzelman DK. Preparing residents to become more effective teachers: a priority for internal medicine. Am J Med 2000;109(8):693‐696.
3. Julian KA, O’Sullivan PS, Vener MH, Wamsley MA. Teaching residents to teach: the impact of a multi‐disciplinary longitudinal curriculum to improve teaching skills. Med Educ Online 2007;12(1):4467.
4. Nejad H, Bagherabadi M, Sistani A, Dargahi H. Effectiveness of resident as teacher curriculum in preparing emergency medicine residents for their teaching role. J Adv Med Educ Prof 2017;5(1):21‐25.
5. Kobritz M, Demyan L, Hoffman H, Bolognese A, Kalyon B, Patel V. “Residents as teachers” workshops designed by surgery residents for surgery residents. J Surg Res. 2022;270:187-194.
6. Wamsley MA, Julian KA, Wipf JE. A literature review of “resident‐as‐
Resident-as-Teacher Curriculum: Evidence-based Guide to Best Practices
teacher” curricula: Do teaching courses make a difference? J Gen Intern Med. 2004;19(5 Pt 2):574‐581.
7. Ratan BM, Johnson GJ, Williams AC, Greely JT, Kilpatrick CC. Enhancing the teaching environment: 3‐year follow‐up of a resident‐led residents‐as‐teachers program. J Grad Med Educ 2021;13(4):569‐575.
8. Ahn J, Golden A, Bryant A, Babcock C. Impact of a dedicated emergency medicine teaching resident rotation at a large urban academic center. West J Emerg Med. 2016;17(2):143‐148.
9. Post RE, Quattlebaum RG, Benich JJ 3rd. Residents‐as‐teacher curricula: a critical review. Acad Med. 2009;84(3):374‐380.
10. Geary AD, Hess DT, Pernar LI. Efficacy of a resident-as-teacher program (RATP) for general surgery residents: an evaluation of 3 years of implementation. Am J Surg. 2021;222(6):1093-1098.
11. Berger JS, Daneshpayeh N, Sherman M, et al. Anesthesiology residents-as-teachers program: a pilot study. J Grad Med Educ 2012;4(4):525-528.
12. Santini VE, Wu CK, Hohler AD. Neurology Residents as Comprehensive Educators (Neuro RACE). Neurologist 2018;23(5):149-151.
13. Busari JO, Scherpbier AJ. Why residents should teach: a literature review. J Postgrad Med. 2004;50(3):205‐210.
14. Miloslavsky EM, Sargsyan Z, Heath JK, et al. A simulation-based resident-as-teacher program: the impact on teachers and learners. J Hosp Med. 2015;10(12):767-772.
15. Morrison EH, Rucker L, Boker JR, et al. A pilot randomized, controlled trial of a longitudinal residents-as-teachers curriculum. Acad Med. 2003;78(7):722-729.
16. Snell L. The resident‐as‐teacher: It’s more than just about student learning. J Grad Med Educ. 2011;3(3):440‐441.
17. Hill AG, Yu T, Barrow M, Hattie J. A systematic review of resident‐as‐teacher programmes. Med Educ. 2009;43(12):1129‐1140.
18. Chathampally Y, Cooper B, Wood DB, et al. Evolving from morbidity and mortality to a case-based error reduction conference: Evidencebased Best Practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2020;21(6):231–41.
19. Wood DB, Jordan J, Cooney R, et al. Conference didactic planning and structure: an Evidence-based Guide to Best Practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2020;21(4):999–1007.
20. Parsons M, Bailitz J, Chung AS, et al. Evidence-based interventions that promote resident wellness from the Council of Emergency Residency Directors. West J Emerg Med. 2020;21(2):412–22.
21. Parsons M, Caldwell M, Alvarez A, et al. Physician pipeline and pathway programs: an evidence-based guide to best practices for diversity, equity, and inclusion from the Council of Residency Directors in Emergency Medicine. West J Emerg Med 2022;23(4):514–24.
22. Davenport D, Alvarez A, Natesan S, et al. Faculty recruitment, retention, and representation in leadership: an Evidence-Based Guide to Best Practices for Diversity, Equity, and Inclusion from the Council of Residency Directors in Emergency Medicine. West J
Emerg Med. 2022;23(1):62–71.
23. Gallegos M, Landry A, Alvarez A, et al. Holistic review, mitigating bias, and other strategies in residency recruitment for diversity, equity, and inclusion: an Evidence-based Guide to Best Practices from the Council of Residency Directors in Emergency Medicine. West J Emerg Med. 2022;23(3):345–52.
24. Natesan S, Bailitz J, King A, et al. Clinical teaching: An Evidence-based Guide to Best Practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2020;21(4):985–98.
25. Estes M, Gopal P, Siegelman JN, et al. Individualized Interactive Instruction: a Guide to Best Practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2019;20(2):363–8.
26. Gottlieb M, King A, Byyny R, et al. Journal club in residency education: an Evidence-based Guide to Best Practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2018;19(4):746–55.
27. Natesan S, Jordan J, Sheng A, et al. Feedback in medical education: An Evidence-based Guide to Best Practices from the Council of Residency Directors in Emergency Medicine. West J Emerg Med 2023;24(3):479-494.
28. Phillips R, Ball C, Sackett D. Oxford Centre for Evidence-Based Medicine: Levels of Evidence. CEBM: Centre for Evidence-Based Medicine. 2021. Accessed December 5, 2024. Available at: https:// www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-ofevidence
29. Nguyen S, Cole KL, Timme KH, Jensen RL. Development of a residents-as-teachers curriculum for neurosurgical training programs. Neurosurgical focus. 2022;53(2):E6.
30. Al Achkar M, Hanauer M, Morrison EH, Davies MK, Oh RC. Adv Med Educ Pract. 2017;8:299-306.
31. Rowat J, Johnson K, Antes L, White K, Rosenbaum M, Suneja M. Successful implementation of a longitudinal skill-based teaching curriculum for residents. BMC Med Educ. 2021;21(1):346
32. Ahn J, Jones D, Yarris L, Fromme H, Yarris LM, Fromme HB. A national needs assessment of emergency medicine resident-asteacher curricula. Intern Emerg Med. 2017;12(1):75-80.
33. Anderson MJ, Ofshteyn A, Miller M, Ammori J, Steinhagen E. “Residents as teachers” workshop improves knowledge, confidence, and feedback skills for general surgery residents. J Surg Educ 2020;77(4):757-764.
34. Bensinger LD, Meah YS, Smith LG. Resident as teacher: the Mount Sinai experience and a review of the literature. Mt. Sinai J Med 2005;72(5):307-311.
35. Chee YE, Newman LR, Loewenstein JI, Kloek CE. Improving the teaching skills of residents in a surgical training program: results of the pilot year of a curricular initiative in an ophthalmology residency program. J Surg Educ. 2015;72(5):890-897.
36. Chokshi BD, Schumacher HK, Reese K, et al. A “Resident-asteacher” curriculum using a flipped classroom approach: Can a model designed for efficiency also be effective? Acad Med. 2017;92(4):511514.
Resident-as-Teacher Curriculum: Evidence-based Guide to Best Practices
37. Cullimore AJ, Dalrymple JL, Dugoff L, et al. The obstetrics and gynaecology resident as teacher. J Obstet Gynaecol Can 2010;32(12):1176-1185.
38. Friedman S, Moerdler S, Malbari A, Laitman B, Gibbs K. The Pediatric Resident Teaching Group: the development and evaluation of a longitudinal resident as teacher program. Med Sci Educ 2018;28(4):619-624.
39. Langer AL, Bernard S, Block BL. Two-week resident-as-teacher program may improve peer feedback and online evaluation completion. Med Sci Educ. 2018;28(4):633-637.
40. Mendoza D, Peterson R, Ho C, Harri P, Baumgarten D, Mullins ME. Cultivating future radiology educators: development and implementation of a clinician-educator track for residents. Acad Radiol. 2018;25(9):1227-1231.
41. Ricciotti HA, Freret TS, Aluko A, McKeon BA, Haviland MJ, Newman LR. Effects of a short video-based resident-as-teacher training toolkit on resident teaching. Obstet Gynecol. 2017;130:36S-41S.
42. Tang Girdwood S, Treasure J, Zackoff M, Klein M. Implementation, evaluation, and improvement of pediatrics residents-as-teachers elective through iterative feedback. Med Sci Educ. 2019;29(2):375-378.
43. Bettendorf B, Quinn-Leering K, Toth H, Tews M. Teaching when Time Is Limited: a Resident and Fellow as Educator Video Module. Med Sci Educ. 2019;29(3):631-635.
44. Tipton AE, Ofshteyn A, Anderson MJ, et al. The impact of a “residents as teachers” workshop at one year follow-up. Am J Surg. 2022;224(1 Pt B):375-378.
45. Gaba ND, Blatt B, Macri CJ, Greenberg L. Improving teaching skills in Obstet Gynecol residents: evaluation of a residents-as-teachers program. Am J Obstet Gynecol. 2007;196(1):87.e1-7.
46. Messman A, Kryzaniak SM, Alden S, Pasirstein MJ, Chan TM. Recommendations for the development and implementation of a residents as teachers curriculum. Cureus. 2018;10(7):e3053.
47. Moser EM, Kothari N, Stagnaro-Green A. Chief residents as educators: an effective method of resident development. Teach Learn Med. 2008;20(4):323-328.
48. Ostapchuk M, Patel PD, Hughes Miller K, Ziegler CH, Greenberg RB, Haynes G. Improving residents’ teaching skills: a program evaluation of residents as teachers course. Med Teach. 2010;32(2):e49-e56.
49. Zackoff M, Jerardi K, Unaka N, Sucharew H, Klein M. An Observed Structured Teaching Evaluation demonstrates the impact of a resident-as-teacher curriculum on teaching competency. Hosp Pediatr. 2015;5(6):342-347.
50. Achkar MA, Davies MK, Busha ME, Oh RC. Resident-as-teacher in family medicine: a CERA survey. Fam Med. 2015;47(6):452-458.
51. Burgin S, Zhong CS, Rana J. A resident-as-teacher program increases dermatology residents’ knowledge and confidence in teaching techniques: A pilot study. J Am Acad Dermatol 2020;83(2):651-653.
52. Burke S, Schmitt T, Jewell C, Schnapp B. A novel virtual emergency medicine residents-as-teachers (RAT) curriculum. J Educ Teach Emerg Med. 2021;6(3).
53. Farrell SE, Pacella C, Egan D, et al. Resident-as-teacher: a
suggested curriculum for emergency medicine. Acad Emerg Med 2006;13(6):677-679.
54. Liang JF, Cheng HM, Huang CC, Yang YY, Chen CH. Lessons learned from a novel 3-year longitudinal stepwise “residents-asteachers” program. J Chin Med Assoc. 2023;86(6):577-583.
55. Seelig S, Bright E, Bod J, et al. Educating future educators-resident distinction in education: a longitudinal curriculum for physician educators. West J Emerg Med. 2021;23(1):100-102.
56. Frey-Vogel A. A resident-as-teacher curriculum for senior residents leading morning report: a learner-centered approach through targeted faculty mentoring. MedEdPORTAL. 2020;16:10954.
57. Fromme HB, Whicker SA, Paik S, et al. Pediatric resident-as-teacher curricula: a national survey of existing programs and future needs. J Grad Med Educ. 2011;3(2):168-175.
58. Pien LC, Taylor CA, Traboulsi E, Nielsen CA. A pilot study of a “resident educator and life-long learner” program: using a faculty train-the-trainer program. J Grad Med Educ. 2011;3(3):332-336.
59. McKinley SK, Cassidy DJ, Sell NM, et al. A qualitative study of the perceived value of participation in a new department of surgery research residents-as-teachers program. Am J Surg 2020;220(5):1194-1200.
60. Roberts KB, DeWitt TG, Goldberg RL, Scheiner AP. A program to develop residents as teachers. Arch Pediatr Adolesc Med 1994;148(4):405-410.
61. Watkins AA, Gondek SP, Lagisetty KH, et al. Weekly e-mailed teaching tips and reading material influence teaching among general surgery residents. Am J Surg. 2017;213(1):195-201.e3.
62. Ofshteyn A, Bingmer K, Tseng E, et al. Effect of “residents as teachers” workshop on learner perception of trainee teaching skill. J Surg Res. 2021;264:418-424.
63. York-Best C, Bengtson J, Stagg A. A Simulation-Based Resident as Surgical Teacher (RAST) program. J Grad Med Educ. 2017;9(3):382384.
64. Patocka C, Meyers C, Delaney JS. Residents-as-teachers: a survey of Canadian emergency medicine specialty programs. CJEM 2010;12(3):249.
65. Aiyer M, Woods G, Lombard G, Meyer L, Vanka A. Change in residents’ perceptions of teaching: following a one day “residents as teachers” (RasT) workshop. South Med J. 2008;101(5):495-502.
66. Ryg PA, Hafler JP, Forster SH. The efficacy of residents as teachers in an ophthalmology module. J Surg Educ. 2016;73(2):323-328.
67. Wipf JE, Pinsky LE, Burke W. Turning interns into senior residents: preparing residents for their teaching and leadership roles. Acad Med. 1995;70(7):591-596.
68. Morrison EH, Friedland JA, Boker J, Rucker L, Hollingshead J, Murata P. Residents-as-teachers training in U.S. residency programs and offices of graduate medical education. Acad Med. 2001;76(10 Suppl):S1-4.
69. Morrison EH, Rucker L, Boker JR, et al. The effect of a 13-hour curriculum to improve residents’ teaching skills: a randomized trial. Ann Intern Med. 2004;141(4):257-263.
70. Ricciotti HA, Dodge LE, Head J, Atkins KM, Hacker MR. A novel
resident-as-teacher training program to improve and evaluate Obstet Gynecol resident teaching skills. Med Teach. 2012;34(1):e52-7.
71. Geary A, Hess DT, Pernar LIM. Resident-as-teacher programs in general surgery residency - a review of published curricula. Am J Surg. 2019;217(2):209-213.
72. Ilgen JS, Takayesu JK, Bhatia K, et al. Back to the bedside: the 8-year evolution of a resident-as-teacher rotation. J Emerg Med 2011;41(2):190-195.
73. Kaji A, Moorehead JC. Residents as teachers in the emergency department. Ann Emerg Med. 2002;39(3):316-318.
74. Bree KK, Whicker SA, Fromme HB, Paik S, Greenberg L. Residentsas-teachers publications: What can programs learn from the literature when starting a new or refining an established curriculum? J Grad Med Educ. 2014;6(2):237-248.
75. Dunnington GL, DaRosa D. A prospective randomized trial of a residentsas-teachers training program. Acad Med. 1998;73(6):696-700.
76. Benè KL, Bergus G. When learners become teachers: a review of peer teaching in medical student education. Fam Med. 2014;46(10):783-7.
77. Minor S, Poenaru D. The in-house education of clinical clerks in surgery and the role of housestaff. Am J Surg. 2002;184(5):471-5.
78. Weisgerber M, Flores G, Pomeranz A, Greenbaum L, Hurlbut P, Bragg D. Student competence in fluid and electrolyte management: the impact of various teaching methods. Ambul Pediatr. 2007;7(3):220–225.
79. Moore J, Parsons C, Lomas S. A resident preceptor model improves the clerkship experience on general surgery. J Surg Educ 2014;71(6):e16-8.
80. McKeon BA, Ricciotti HA, Sandora TJ, et al. A consensus guideline to support resident-as-teacher programs and enhance the culture of teaching and learning. J Grad Med Educ. 2019;11(3):313-318.
81. Frye AW, Hemmer PA. Program evaluation models and related theories: AMEE guide no. 67. Med Teach. 2012;34(5):e288-e299.
82. Hosseini S, Yilmaz Y, Shah K, et al. Program evaluation: an educator’s portal into academic scholarship. AEM Educ Train 2022;6(Suppl 1):S43-S51.
83. Donovan A. Radiology resident teaching skills improvement: impact of a resident teacher training program. Acad Radiol. 2011;18(4):518-524.
84. Gill DJ, Frank SA. The neurology resident as teacher: evaluating and improving our role. Neurology. 2004;63(7): 1334-1338.
85. Johnson KM, Rowat J, Suneja M. A 3-year rolling teaching skills curriculum for all residents in the ambulatory block. J Gen Intern Med. 2018;33(2):675.
86. Tischendorf JS, MacDonald M, Harer MW, Pittner-Smith CA, Zelenski AB, Johnson SK. Bridging undergraduate and graduate medical education: a resident-as-educator curriculum embedded in an internship preparation course. Wis Med J. 2020;119(4):278-281.
87. Dewey CM, Coverdale JH, Ismail NJ, et al. Residents-as-teachers programs in psychiatry: a systematic review. Can J Psychiarty. 2008;53(2):77-84.
88. Chochol MD, Gentry M, Hilty DM, McKean AJ. Psychiatry Residents
as Medical Student Educators: a Review of the Literature. Acad Psychiatry. 2022;46(4):475-485.
89. James MT, Mintz MJ, McLaughlin K. Evaluation of a multifaceted “resident-as-teacher” educational intervention to improve morning report. BMC Med Educ. 2006;6:20.
90. Haghani F, Eghbali B, Memarzadeh M. Effects of “teaching method workshop” on general surgery residents’ teaching skills. J Educ Health Promot. 2012;1:38.
91. Humbert AJ, Pettit KE, Turner JS, Mugele J, Rodgers K. Preparing emergency medicine residents as teachers: clinical teaching scenarios. MedEdPORTAL. 2018;14:10717.
92. York-Best C, Bengtson J, Stagg A. Laparoscopic salpingectomy: a simulation-based resident as surgical teacher (RAST) program. Obstet Gynecol. 2016;128:63S.
93. Katzelnick DJ, Gonzales JJ, Conley MC, Shuster JL, Borus JF. Teaching psychiatric residents to teach. Acad Psychiatry 1991;15(3):153-159.
94. Marcus CH, Newman LR, Winn AS, et al. TEACH and repeat: Deliberate practice for teaching. Clin Teach. 2020;17(6):688-694.
95. Grady-Weliky TA, Chaudron LH, Digiovanni SK. Psychiatric residents’ self-assessment of teaching knowledge and skills following a brief “psychiatric residents-as-teachers” course: a pilot study. Acad Psychiatry. 2010;34(6):442-444.
96. Dannaway J, Ng H, Schoo A. Literature review of teaching skills programs for junior medical officers. Int J Med Educ. 2016;7:25-31.
97. Geary AD, Hess DT, Pernar LIM. Resident-as-teacher programs in general surgery residency: context and characterization. J Surg Educ. 2019;76(5):1205-1210.
98. Zackoff MW, Real FJ, DeBlasio D, et al. Objective assessment of resident teaching competency through a longitudinal, clinically integrated, resident-as-teacher curriculum. Acad Pediatr 2019;19(6):698-702.
99. Hill AG, Srinivasa S, Hawken SJ, et al. Impact of a Resident-asteacher workshop on teaching behavior of interns and learning outcomes of medical students. J Grad Med Educ. 2012;4(1):34-41.
100. Loo BKG, Thoon KC, Tan JHY, Nadua KD, Chow CCT. Supporting paediatric residents as teaching advocates: changing students’ perceptions. Asia Pacific Scholar. 2020;5(3):62-70.
101. Litzelman DK, Stratos GA, Skeff KM. The effect of a clinical teaching retreat on residents’ teaching skills. Acad Med. 1994;69:433–4.
102. Thomas PS, Harris P, Rendina N, Keogh G. Residents as teachers: outcomes of a brief training programme. Educ Health. 2002;15:71–8.
103. Hoffman LA, Furman DT Jr, Waterson Z, Henriksen B. A novel resident-as-teacher curriculum to improve residents’ integration into the clinic. PRiMER. 2019;3:9.
104. Mann KV, Sutton E, Frank B. Twelve tips for preparing residents as teachers. Med Teach. 2007;29(4):301-306.
105. Fakhouri Filho SA, Feijo LP, Augusto KL, Nunes M do PT. Teaching skills for medical residents: Are these important? A narrative review of the literature. Sao Paulo Med J. 2018;136(6):571-578.
Large-Scale Combat Operation Education and Training Needs: Implications for Military and Civilian Medical Education
Rebekah Cole, PhD, MEd*†
Kiia Crawford, BS‡
Makinna Farrell, BS‡
Leslie Vojta, MD*
Sherri L. Rudinsky, MD*
Section Editor: Christopher Kang, MD
Uniformed Services University, Department of Military and Emergency Medicine, Bethesda, Maryland
Uniformed Services University, Department of Health Professions Education, Bethesda, Maryland
Uniformed Services University, School of Medicine, Bethesda, Maryland
Submission history: Submitted February 21, 2025; Revision received May 12, 2025; Accepted June 6, 2025
Electronically published September 1, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.43557
Introduction: Future large-scale combat operations (LSCO) with adversaries such as Russia or China are predicted to present unique challenges for medical personnel, including high casualty rates, limited resources, and austere environments. While traditionally associated with military conflict, the anticipated scale of future LSCO may overwhelm military medical systems, requiring civilian physicians to support wartime care or manage surges in casualties on the home front. Effective training early on is, therefore, critical to prepare both military and civilian physicians for these unique and demanding conditions.
Methods: We used interpretive phenomenological analysis in this qualitative study to explore key competencies needed for LSCO medical readiness. The first and seniors author interviewed 27 military physicians (active duty, retired, and reservists) and one military chaplain with extensive operational medical experience in the fall of 2023 and fall of 2024. We analyzed transcripts to identify recurring themes. Data analysis was conducted by a diverse and experienced research team.
Results: Five key themes emerged as essential for LSCO-focused medical training: 1) problemsolving in resource-limited environments, emphasizing critical thinking and improvisation; 2) ethical and emotional resilience, addressing psychological and moral challenges; 3) adaptive leadership, highlighting decision-making in high-stress settings; 4) mastery of core medical skills, ensuring competency in essential procedures; and 5) cultural competence and interoperability, supporting effective collaboration across military-civilian teams.
Conclusion: The competencies identified in this study are relevant to both military and civilian physicians who may be called upon to provide care during large-scale combat operations. Medical education must proactively incorporate these themes to ensure readiness across both sectors. Strengthening military-civilian collaboration in training and curriculum development will enhance national preparedness for future conflicts. [West J Emerg Med. 2025;26(5)1144–1153.]
INTRODUCTION
The United States Department of Defense predicts that future large-scale combat operations (LSCO) with peer/ near-peer adversaries such as Russia or China will take place in volatile, uncertain, complex, and ambiguous environments within the next 5-10 years.1 These imminent conflicts may
unfold in austere combat settings with restricted resupply, air evacuation, and access to surgical care.2 As a result, the death toll of LSCO is predicted to match that of World War II, where an estimated 15 million service members and 38 million civilians were killed, with many more wounded.3 Similarly, recent regional conflicts, such as those in Israel and Ukraine,
serve as stark reminders of the significant impact and stresses such conflicts place on both military and civilian medical infrastructure and communities.4 Physicians near war zones will face challenges related to high patient volumes, severe injuries, and limited resources, demonstrating the broad applicability of these concepts across civilian and military medical contexts.5
Both military and civilian medicine will need to overcome the formidable challenges of LSCO.3 Military physicians will lead healthcare teams in austere environments with limited resources, often requiring prolonged casualty care when evacuation delays stretch beyond the previous standard “golden hour.”6 Similarly, civilian physicians may be called upon to support wartime care and/or manage surges in casualties on the homefront.3 These realities necessitate a re-evaluation of how physicians—both military and civilian—are trained for wartime crisis response at home and abroad, as these unique conditions merit distinct educational considerations.
To ensure readiness, physicians must develop a multifaceted skill set to lead healthcare teams during LSCO. For example, they may be called to serve as leaders, trainers, and advisors who advocate for the health and welfare of their units.7 They also may be called to assume leadership roles in coordinating care across multiple agencies and institutions.8 Therefore, training physicians in leadership, adaptability, and resource management is essential for ensuring both mission success and improved patient outcomes. Medical students, especially, can benefit from this training as they represent a formative stage where foundational professional identity, leadership capacity, and adaptability are being developed. Early exposure to the realities of LSCOs can help frame future clinical decision-making, resilience, and operational readiness in unique military environments.9,10,11,12
Despite the urgent need for LSCO preparedness, there is little precedent or prior research on how to best equip medical students for such operations, as the United States has not engaged in such large-scale peer/near-peer warfare since World War II. Past research has shown that preparation in medical school increases physicians’ readiness and leadership abilities in volatile wartime environments.13Current educational programs focus on leadership, problem-solving, and resilience in the context of natural disasters and mass casualty events; however, LSCO are expected to involve extensive prolonged casualty care, limited evacuation capabilities, degraded communications, and heightened moral and logistical complexity.14,15,16,17,18,19 As a result, no existing programs are specifically designed to address the unique uncertainty, scale, and ethical challenges posed by LSCO, which are factors not typically covered in standard disaster medicine curricula. To begin addressing this gap, we conducted a qualitative study with experienced military medical educators to explore their perceptions of what education and training are needed during medical school to prepare future military and civilian physicians for LSCO.
Population Health Research Capsule
What do we already know about this issue?
Medical readiness for large-scale combat operations (LSCO) is underdeveloped in both military and civilian medical education.
What was the research question?
What competencies are needed to prepare physicians for future LSCO?
What was the major finding of the study?
Key themes emerged as vital for LSCO medical training: critical thinking and improvisational skills, emotional resilience, adaptive leadership, and cultural competence.
How does this improve population health? Identifying LSCO training needs helps prepare physicians for crisis care, improving survival and ethical decision-making in highstakes environments.
METHODS
We chose an interpretive phenomenological analysis (IPA) to guide our study, acknowledging our role as researchers, military physicians, and educators and the influence these roles had on our interaction with our participants and our interpretation of the data.20 The goal of IPA is to depict how the participants perceive a particular phenomenon. In our study we aimed to describe in depth how our participants made sense of military medical education and training in preparation for future large-scale conflicts.
The participants in our study were 27 active-duty, retired, and reserve military physicians and one military chaplain, convenience sampled from available faculty attending military medicine operations. All our participants had significant experience with military medicine in the operational environment. (See Appendix A for participant demographics.) The participants were selected for their military backgrounds and experience within military medical education. All participants had deployed in support of combat operations, primarily in Iraq and/or Afghanistan.
We also included one military chaplain in our study because of their extensive operational experience supporting medical teams during combat deployments and their unique insight into the ethical, emotional, and moral challenges faced by healthcare personnel in LSCO. We first recruited participants via email and in person while they were serving
as faculty at our university’s capstone Medical Field Practicum during the fall of 2023. All participants volunteered for the study. None were recruited or coerced by a military commanding officer. The participants received an institutional review board (IRB)-approved information sheet describing the study goals and research processes during participant recruitment. The study goals outlined on the information sheet provided to participants were 1) to explore how experienced military medical educators perceive the training needs of future physicians in the context of large-scale combat operations, and 2) to identify key educational priorities that could inform medical school curriculum development.
After analyzing our data and determining that saturation had not been reached, we recruited more participants during the fall of 2024 at the same exercise.21, 22 The first and senior authors conducted audio- recorded in-person, semi-structured interviews with each of these participants. No field notes were taken during the interview process, and no one else was present during the interviews. The first author is an experienced qualitative researcher with a doctoral degree. The senior author is a medical doctor and has completed graduate coursework in qualitative research methodology. The interviews averaged 43 minutes each. All participants were interviewed using the same semi-structured interview guide, which was developed based on our research questions and reviewed by our team prior to data collection. The same interview protocol was used across both recruitment cycles (Fall 2023 and Fall 2024), and all interviews were conducted in person by either the first or senior author. While follow-up questions were asked during individual interviews, these were used to clarify or deepen participant responses and were not part of a separate, standardized second interview.20
We then transcribed each of these interviews using an automated transcription service. To ensure the credibility of our data, we emailed the transcripts back to the participants, asking for their feedback on their interviews, which is a practice known as member checking. This study was approved by the IRB at the authors’ university (DBS.2021.248). No participants refused to participate or dropped out of the study.
Following the steps of IPA, our research team first reviewed Participant 1’s transcripts, noting important training aspects throughout.23, 24, 25 We continued this data analysis process by reading through each of the other participants’ transcripts one by one, on a case-by-case basis. We then approached the transcripts as a whole, making note of common themes that emerged across each of the participant’s responses. We reported these themes as the results of our study.25 Rather than using a numerical threshold for theme inclusion (eg, a minimum number of participants), we followed IPA’s emphasis on depth of meaning, recurrence across cases, and thematic coherence.26 Themes were identified through an iterative, case-by-case analysis of transcripts, followed by cross-case comparison. The final set of five themes was selected because they were both recurrent
across multiple participants and analytically rich in describing the training needs for LSCO readiness.
Our research team consisted of two military physicians, two military medical students, and one Ph.D. curriculum researcher. As educators and military healthcare professionals, we recognized the influence of our own knowledge and perceptions on our interaction with our participants and our interpretation of the data, which is an inherent aspect of IPA.27
For example, we asked follow-up questions to the participants regarding aspects that we thought particularly salient to the research question during the interviews. We also read through the data with our literature review in mind, understanding the potential challenges of future LSCO as we analyzed the participants’ responses. While minor differences in interpretation emerged during the analysis process, a common occurrence in qualitative research, they were addressed through iterative discussions among the research team. All discrepancies were resolved by consensus.28
RESULTS
Five themes emerged from the data regarding medical students’ education and training needs: 1) Learn to problem solve within a resource-limited environment; 2) Develop ethical and emotional resilience; 3) Engage in adaptive leadership development; 4) Master basic skills; and 5) Develop cultural competence and an interoperable mindset. These themes and example images are presented in Figure 1.
Theme 1: Learn to problem solve within a resource-limited environment.
The participants first described the need to teach students to problem-solve within a resource-limited environment. To do so, students must develop a new way of thinking “way outside the box, to use, really to find whatever is available, to use whatever” (Participant [P] 9). This new thought process includes “being able to focus on a methodological or a logical way of thinking through novel problems that may not have existed before” (P2). Additionally, the participants described how students must learn to act decisively, as one noted,

Figure 1. Five themes that emerged from interviews with 27 military medical faculty and one chaplain regarding medical education and training needs.
. . . even if the decision is the wrong decision, that’s better than no decision at all . . . I don’t care if it’s perfect, I just care that you did something.” (P25)
Thinking ahead in their problem-solving is essential:
Everyone’s going to have a little bit of prolonged casualty care on the second- and third-order effects. You can do the tourniquet, but most people don’t think, ‘Okay, I’ve done intervention, what are the secondary and tertiary effects out of injuries?’ (P13)
This problem-solving skill set will be key when facing large numbers of patients with fewer resources during LSCO, where students may confront “very, very complicated questions about resource utilization and decisions on how you can do the greatest good for the greatest number” (P16). As a result, the participants emphasized the need to learn how to take care of more patients with fewer resources, encouraging students to
[I]dentify a problem, a medical-related problem, big or small, and then just like if you had resources, how would you propose to fix it? Just kind of encouraging those thought processes.” (P4)
The participants also described how medical students should be challenged to make the most of limited supplies. For example, understanding that
in deployed environments, you can ask for whatever you want, but . . . it might be a couple months before you get them, so you need to learn to figure out how to solve problems with what you’ve got. (P25).
Theme 2: Develop ethical and emotional resilience.
As a result of needing to do more with less, students must be prepared to navigate complex ethical issues that may lead to moral injury. One participant described how students will
have the tools and abilities within themselves to save someone, but the situation doesn’t allow it. And especially if it’s one of their people, their friends, one of their loved ones. (P15)
The scale of future conflicts may further intensify this risk, as another participant noted,
The numbers of casualties that we are going to see are going to be five, ten times larger than what we have seen now . . . Being exposed to all that kind of stuff exposes us to the potential for moral injury. (P25)
The participants also reflected on the need for students to build resilience for such hardships, with one stating,
What we need to do is protect them from that moral injury . . . So we’ve got to prepare them for the pain and suffering and arduousness of real war. (P9)
Another participant noted,
We need to prepare them for the fact that patients are going to die . . . because we’re not able to get them the supplies that they want.
And this participant echoed,
Preparing them for the adverse outcomes that they’re going to see, preparing them for all the crazy, wild things that we’re going to let them do . . . because they’re doing everything they can to save their patients. (P19)
Without regular practice in facing challenges and adversity, another participant added, “We’re not just automatically going to be good at facing challenges and adversity” (P25), as they emphasized the need for immersive preparation to help students confront and manage the emotional weight of real-world combat scenarios and the complex medical decision-making that will be required.
Theme 3: Engage in adaptive leadership development.
Given the complexities of LSCO, the participants described a pressing need for adaptive leadership training for future military physicians, as these physicians will lead teams in high-stress environments and must regularly adapt to new challenges.
We need to develop leaders that can deal with the complexities of technology and the weaponry that’s going to be there because it’s not going to be necessarily a bunch of blast victims right in front of us. It might be people much farther away. (P11)
Participant 13 likewise explained that as we move toward more disaggregated operations, individuals will need to “know how to lead teams and operate independently based on mission command type order sets…So they’re going to have to be more comfortable being uncomfortable” (P13). Given the potential high stress of LSCO, Participant 15 emphasized that medical students need to learn to lead with “coolness and calmness…you need to be able to command respect without demanding respect” (P15). Additionally, fostering teamwork was highlighted as essential to effective leadership: “If you’re not being a good teammate, you’re not being a good leader, physician, officer, and human” (P19). This sense of shared
leadership was reinforced by the idea that leadership isn’t about a single authority, but rather about “empowering each team member based on their strengths, whether medics, nurses, or ambulance drivers” (P24).
In addition to leading and adapting under pressure during LSCO, our participants stressed that medical students must develop a flexible mindset.
You need a leader who can somehow balance the piece of being able to listen to feedback from people and take that as well as guiding the team toward an end. (P7)
Participant 15 described the need for flexibility in perspective as well, stating,
You have to be able to step back, see the big picture, understand the constraints of your environment, what is survivable, what is feasible, and what is reasonable. (P15)
Empathy and self-care were also identified as essential components of effective leadership. As one participant noted, “Leaders need to take time to care for themselves… you cannot give what you do not have” (P19).
Theme 4: Master basic skills.
In the midst of the new challenges that military physicians may encounter during LSCO, the participants emphasized the need for students to learn and remember fundamental lessons to “do the simple stuff in a really crappy environment” (P2). They highlighted that mastering the basics, such as applying a tourniquet, managing massive hemorrhage, managing an airway, and even knowing positioning techniques, is crucial for effective response. Underscoring the importance of a strong foundation in core knowledge and skills, one participant questioned,
If you can’t positively answer where you’re going to put a [needle decompression], how can you positively say where I’m going to put a chest tube or do a finger thoracostomy or at what phase of the treatment to do that? (P4)
Another noted the risk of skill decay in tactical medical skills, describing them as “very perishable,” which highlights the need for consistent practice in these essential areas (P4). Participant 16 also emphasized the importance of basic skills when practicing outside one’s specialty:
You’re not always going to have a full complement of specialists. And that it’s going to reinvigorate the art of the generalist and having a much broader, wider slice of the medical pie as part of your domain.
Finally, participants believed that teaching military history to students is an important part of their future preparation.
The only thing that we have right now is looking to the past, kind of studying that really closely and then figuring out the lessons learned there, like how we can apply those to the future. (P10)
Participant 8 echoed this perspective:
You can certainly go back in time, eons, and look at how it was dealt with through the Greeks or through the Romans . . . at many different levels.
Theme 5: Develop cultural competence and an interoperable mindset.
In preparing for future operations, participants highlighted the importance of developing cultural competence and an interoperable mindset. As one participant noted,
We need to learn other cultures, we need to learn intercultural relationships, we need to learn about other political systems, other social structures . . . especially as military leaders, we need to think wide.” (P20)
This cultural and political awareness is essential for effective communication and collaboration with partner nations. One faculty emphasized that understanding “their communication strategies and how they will work with other nations is also going to be...more important than it was in the last conflict.” (P21) Finally, in thinking about how to teach these skills, Participant 18 suggested that
having international students frequently integrated in the curriculum and within our exercises . . . working with partner forces throughout all four years [is key for military medical readiness].
DISCUSSION
Our study’s results revealed five focus areas for preparing medical students for LSCO: 1) Learn to problem solve within a resource-limited environment; 2) Develop ethical and emotional resilience; 3) Engage in adaptive leadership development; 4) Master basic skills; and 5) Develop cultural competence and an interoperable mindset. Given the complex operational environments of LSCO, civilian and military medical students must learn to solve problems with few resources, lead diverse teams under pressure, and rely on their foundational medical training to make effective decisions in this type of wartime environment. These themes are relevant for both military and civilian medical students, since the scale of LSCO may necessitate civilian physician involvement in care delivery, making these themes broadly applicable across training environments. These themes can be operationalized
by providing specific curricular strategies, such as embedding immersive simulation scenarios that replicate resourceconstrained settings, introducing ethical case studies focused on moral injury, and integrating team-based leadership challenges modeled on LSCO conditions. We also recommend cross-institutional training initiatives that allow military and civilian students to learn side by side, enhancing interoperability and shared preparedness.
The anticipated resource constraints in future large-scale conflicts highlight the necessity of equipping healthcare teams with the knowledge and skills to make complex decisions about resource allocation and to foster innovation in addressing novel challenges.29 Innovation in non-traditional patient care settings has long been a hallmark of military medicine, with significant advancements translating to civilian medical care over the past two decades.30 Similarly, civilian emergency response frameworks have informed military medical strategies, emphasizing the reciprocal benefits of military-civilian collaboration.31While we acknowledge that civilian medical students do not currently require the same degree of preparation as their military counterparts, we believe that our findings offer a forward-looking framework for potential curricular adaptation should civilian systems be more directly involved in future LSCO, as they are predicted to be.
Because both civilian and military medical students are in an early, formative stage of development, we advocate for a developmentally appropriate, scaffolded approach that introduces foundational concepts—such as ethical reasoning, resource-conscious thinking, and adaptive leadership mindsets—early in training and builds progressively across the undergraduate medical education continuum. Specific skills such as tactical triage would be introduced through guided simulation and interdisciplinary exercises, rather than full clinical implementation during early training years. Overall, these recommendations are not intended to duplicate existing curricula but to intentionally adapt and expand them to address the escalating demands of LSCO.
As our participants described, effective problem-solving and innovation require a strong foundation of basic knowledge, and skills.32
This foundation aligns closely with the concept of adaptive expertise, a critical competency in medical education. Adaptive expertise is defined as “the effective application of existing knowledge and skills to create innovative solutions for tasks or problems that are novel to the expert.”33 Unlike routine expertise, which focuses on mastering procedures and algorithms, adaptive expertise involves a deeper understanding of underlying principles and the flexibility to apply that knowledge in new and unexpected contexts.34 Key attributes of adaptive expertise—flexibility, problem-solving, innovation, and comfort with uncertainty—align closely with the enhanced roles and attributes required of modern healthcare leaders, both military and civilian.34 These characteristics also resonate with the themes highlighted by our participants,
underscoring their importance in preparing healthcare professionals for the complex and unpredictable challenges of future crisis environments.
Educational strategies that promote the development of adaptive expertise often emphasize conceptual knowledge to prepare learners for future learning, which refers to “the ability to learn new information, effectively utilize resources, and develop new procedures to support learning and problemsolving in practice.”35 Teaching methods that foster preparing learners for future learning include offering diverse experiential learning opportunities, allowing students to face challenges and occasionally fail, encouraging self-reflection, and providing timely direct instruction or feedback.36, 37
Simulation-based education, like the training environment in our study, serves as an excellent experiential learning tool. It enables learners to make and learn from mistakes in a safe environment, fostering adaptability, innovation, and a problem-solving mindset.38
Our study likewise emphasized the need for adaptive leadership training to prepare students for the uncertainties of LSCO and large-scale disasters, which will result in complex leadership challenges. This leadership training, for example, might focus on navigating issues such as moral injury and expectant casualty care due to the extensive numbers of casualties expected in such scenarios. This training should begin early (ie, during medical school) and continue throughout a physician’s career to ensure comprehensive preparedness for crisis leadership. By embedding leadership scenarios into early and ongoing training, medical students could practice managing complex team dynamics, implementing tactical triage, and working effectively in multidisciplinary, high-stakes environments. Additionally, simulations could be used to develop resilience, encouraging future physicians to recognize the emotional impact of crisis care and providing strategies for coping with the moral and psychological stressors unique to LSCO and disaster response.39
During LSCO, patient care prioritization and treatment protocols might shift in crisis scenarios, from life-saving interventions to symptom management and ethical end-of-life care.40 Our participants identified moral injury as a major challenge for healthcare professionals when making difficult decisions about resource allocation. The COVID-19 pandemic underscored the severe impact of moral injury on physicians’ well-being,41 and further studies highlight both military and civilian healthcare teams’ vulnerability to moral injury in crisis settings, with potential negative effects on mental health, decision-making, and resilience.10,11,42 Large-scale combat operations may introduce unique ethical tensions, such as dual loyalty and battlefield triage, which heighten moral distress and the risk of moral injury.43,44,45
Preparing healthcare teams for these ethical complexities is critical for both mission readiness and effective disaster re sponse.43,44,45,46,47Addressing these challenges requires building resilience by recognizing, anticipating, and
mitigating moral injury through support strategies for individuals and teams.48 Educating medical students about ethical decision-making frameworks and moral injury can increase self-awareness and normalize the concept within both military and civilian healthcare.49
Ethical frameworks provide principles for navigating morally complex situations in medical practice. Their effectiveness is well-documented in hospital settings50 and civilian emergency response.47,51,52 However, adapting them to large-scale crisis care requires addressing challenges like dual loyalty, constrained medical resources, and the inability to determine patient preferences in chaotic environments.53,54 Thus, specialized ethical frameworks and targeted education tailored to both armed conflict and civilian disaster response are essential for preparing healthcare teams.53,54 Additionally, clear guidelines for expectant casualty care from organizations like the Joint Trauma System, alongside training in these clinical practice guidelines, may reduce moral injury.11
In preparing for future operations, participants emphasized the importance of fostering cultural competence and an interoperable mindset. Military healthcare teams are increasingly required to collaborate with medical personnel from other countries as part of multinational forces. This collaboration is also seen between healthcare systems and agencies within the US who collaborate to manage disaster responses. The challenges of wartime collaboration and healthcare delivery in such settings are well-documented.55 While the benefits of international medical cooperation are widely acknowledged (RAND Corporation; North Atlantic Treaty Organization), there is a pressing need for innovative education and training programs within both civilian and military medical education that enhance interoperability.56,57 Such efforts can improve healthcare delivery, strengthen global alliances, and support more effective humanitarian initiatives worldwide.58
This emphasis on interoperability aligns with calls from the international education community, particularly after the COVID-19 pandemic, to define and integrate international leadership competencies into medical education.59 These competencies promote a collaborative approach to addressing global challenges and align with the skills identified by our faculty. Key competencies include “international specialized knowledge,” such as understanding differences among organizational and educational systems, and “integrated leadership skills,” including cultural competence, humility, respect for others’ customs and languages, empathy, and openness to diverse perspectives.59
Finally, a recently emerging concept, the “duty of mind,” emphasizes a physician’s responsibility to maintain ethical decision-making under crisis-induced stress. Failure to do so can lead to biased resource allocation and suboptimal decisions.60 While experience helps mitigate stress-related impacts, many healthcare professionals lack direct exposure to crisis scenarios, particularly in the current inter-war and
inter-disaster periods.60 Medical education plays a crucial role in bridging this gap and preparing professionals for expanded scopes of practice in evolving conflict and disaster scenarios.13,61
LIMITATIONS
Our participants consisted of faculty members teaching at our university’s capstone Medical Field Practicum who volunteered their time and expertise. Because these faculty had deployment experience only to Iraq or Afghanistan, they could only speculate about what future large-scale combat operations might consist of. In addition, our study lacks quantitative outcome data measuring the impact of various training approaches on medical student readiness. Future research should develop and evaluate curricula centered around the themes described in our study to quantify their utility for training future military physicians for LSCO. Finally, our participants were all military medical educators, not civilian medical educators. Any references to civilian training are framed as potential areas for exploration or cross-contextual relevance, rather than definitive claims. This distinction should help clarify the scope and positioning of the participants’ insights. Future research studies should explore civilian medical educators’ perception of needed educational training for LSCO as well, to offer a more comprehensive viewpoint and evaluation of training needs.
CONCLUSION
This study identified five core competencies—problemsolving in resource-limited environments; ethical and emotional resilience; adaptive leadership; mastery of core medical skills; and cultural competence with an interoperable mindset—that experienced military educators view as essential for preparing military and civilian medical students for large-scale combat operations. While many of these competencies overlap with those emphasized in disaster and mass casualty response, large-scale combat operations introduce distinct challenges, such as prolonged austere care, contested environments, and complex ethical dilemmas that require focused educational attention.
Our findings suggest that early, developmentally appropriate exposure to these concepts in undergraduate medical education can lay the groundwork for future crisis readiness. While we do not propose that medical students independently lead tactical triage or complex field care, foundational training in decisionmaking under pressure, leadership mindsets, and ethical reflection can support progressive competence across the medical education continuum.
Although our study’s participants consisted of military medical faculty, the themes identified are increasingly relevant for civilian physicians as well. Future LSCO may overwhelm military medical systems, requiring civilian clinicians to care for patients in similar high-stakes conditions. Integrating these competencies into civilian training—through case-based learning, simulation, and interprofessional exercises—can
strengthen cross-sector preparedness.
These findings offer an evidence-informed foundation for future curriculum development and call for expanded collaboration between military and civilian educators to prepare the next generation of physicians for the evolving demands of conflict and crisis medicine.
Address for Correspondence: Rebekah Cole, PhD, MEd, Uniformed Services University, Military and Emergency Medicine, 4301 Jones Bridge Rd, Bethesda, MD 20814. Email: rebekah. cole@usuhs.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The views expressed here are those of the authors and do not reflect the official policy of the US Department of the Army, the Department of Defense, or the US Government. The authors disclosed none. All information or material written in this article, including assertions and opinions, are the views and responsibility of the authors of this article and do not represent the official views, policies, or positions of the Uniformed Services University of the Health Sciences, the Department of Defense, or the US Government.
Copyright: © 2025 Cole et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Garamone J. General says deterring two ‘near peer’ competitors is complex. 2023. Available at: https://www.defense.gov/News/ News-Stories/Article/article/3496656/general-says-deterring-twonear-peer-competitors-is-complex/. Accessed December 19, 2023.
2. Maker JB, Northern DM, Frament C, et al. Austere resuscitative and surgical care in support of forward military operations-Joint Trauma System Position Paper. Mil Med. 2021;186(1-2):12-7.
3. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2):S180-4.
4. Carpiniello B. The mental health costs of armed conflicts-A review of systematic reviews conducted on refugees, asylum-seekers and people living in war zones. Int J Environ Res Public Health. 2023;20(4):2840.
5. Chauhan V, Secor-Jones S, Paladino L, et al. Emergency departments: preparing for a new war. J Emerg Trauma Shock. 2022;15(4):157-61.
6. Dilday J, Webster S, Holcomb J, et al. ‘Golden day’ is a myth: rethinking medical timelines and risk in large scale combat operations. BMJ Mil Health. 2024;e002835.
7. Cole R, Williamson SS, Hughes JR, et al. The military medical officer’s current-day professional identity: an enhanced model. Mil Med. 2023;188(11-12):e3667-74.
8. Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, Board on Health Sciences Policy, Board on the Health of Select Populations, et al. (2016). Overview of contemporary civilian and military trauma systems. In: Berwick D, Downey A and Cornett E (Eds.), A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury (73-112). Washington DC: National Academies Press, 2016.
9. Cole R, Remondelli MH. Confronting the mental health challenges of large-scale combat operations. Mil Med. 2025:usaf156.
10. Cole R, Shumaker J, Rudinsky S. “It’s there and you’re changed forever”: military physicians’ perceptions of moral injury. JME. 2025:1-13.
11. Cole R, Keenan S, Tadlock MD, et al. Expectant casualty care training needs for future conflicts. Mil Med. 2024;usae389.
12. Cole R, Crawford K, Farrell M, et al. The relationship between the military medical officer and commanding officer: implications for education and training. Mil Med. 2025;190(1-2):e382-7.
13. Cole R, Dong T, Rudinsky SL, et al. A comparison of Uniformed Services University and Health Professions Scholarships Program graduates’ first deployment readiness. Mil Med. 2024;189(45):e1190-5.
14. Satiani B, Sena J, Ruberg R, et al. Talent management and physician leadership training is essential for preparing tomorrow’s physician leaders. J Vasc Surg. 2014;59(2):542-6.
15. Del Carmen Cardós-Alonso M, Otero-Varela L, Redondo M, et al. Extended reality training for mass casualty incidents: a systematic review on effectiveness and experience of medical first responders. Int J Emerg Med. 2024;17:99.
16. Ghorbankhani M, Mousavian S, Mohammadi AS, et al. Enhancing disaster preparedness: developing competencies for military physicians in risk reduction. Int J Disaster Risk Reduct. 2024;103:104321.
17. Hershkovich O, Gilad D, Zimlichman E, et al. Effective medical leadership in times of emergency: a perspective. Dis Mil Med. 2016;2(4):1-5.
18. Donahue A, Brown S, Singh S, et al. Before disaster strikes: a pilot intervention to improve pediatric trainees’ knowledge of disaster medicine. Pediatr Emerg Care. 2022;38(2):e635-8.
19. King HC, Spritzer N, Al-Azzeh N. Perceived knowledge, skills, and preparedness for disaster management among military health care personnel. Mil Med. 2019;184(9-10):e548-54.
20. Smith JA. Evaluating the contribution of interpretive phenomenological analysis. Health Psych Review. 2010;5(1):9-27.
21. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2017;52(4):1893-1907.
22. Tight M. Saturation: An overworked and misunderstood concept? Qualitative Inquiry. 2024;30(7):577-83.
23. Charlick SJ, Pincombe J, Mckellar L, et al. Making sense of participant experiences: interpretative phenomenological analysis in
midwifery research. Int J of Dr Stud. 2016;11:205-16.
24. Smith JA, Osborn M. Interpretative phenomenological analysis as a useful methodology for research on the lived experience of pain. Br J Pain. 2015;9(1):41-2.
25. Rajasinghe D, Garvey B, Burt S, et al. Innovative interpretative phenomenological analysis (IPA) approach in a coaching research project: implications for future qualitative coaching research and beyond. Coaching: An International Journal of Theory, Research and Practice. 2024;17(2):301-18.
26. McCammon LC, Gillen P, McLaughlin D, et al. An interpretative phenomenological analysis that seeks to describe and understand the personal experience of burnout in general practitioners. Qual Health Res. 2024;35(1):118-31.
27. Nisbet M, O’Connor R, Mason A, et al. A qualitative study utilizing interpretative phenomenological analysis to explore disclosure in adolescents with Turner syndrome. Br J Health Psychol. 2022;27(3):990-1010.
28. Coates WC, Jordan J, Clarke SO. A practical guide for conducting qualitative research in medical education: Part 2 - coding and thematic analysis. AEM Educ Train. 2021;5(4):e10645.
29. Fandre M. Medical changes needed for large-scale combat operations: observations from mission command training program warfighter exercises. Military Review. 2020:37-45.
30. Kellermann AL, Kotwal RS, Rasmussen TE. Military medicine’s value to US health care and public health: bringing battlefield lessons home. JAMA Netw Open. 2013;6(9):e2335125.
31. Kyoung H, Cacchione PZ, Cannon J, et al. Military-civilian partnership to improve combat casualty care readiness among non-physician providers. Mil Med. 2024;usae425.
32. Adeoye MA, Jimoh A. Problem-solving skills among 21st-century learners toward creativity and innovation ideas. Thinking Skills and Creativity Journal. 2023;6(1):52-8.
33. Branzetti J, Gisondi MA, Hopson LR, et al. Adaptive expertise: the optimal outcome of emergency medicine training. AEM Educ Train. 2022;6(2):e10731.
34. Branzetti J, Hopson LR, Gisondi MA, et al. Training for adaptive expertise: why, what, and how. Acad Med. 2024;99(1):121.
35. Mylopoulos M, Kulasegaram K, Woods NN. Developing the experts we need: fostering adaptive expertise through education. J Eval Clin Pract. 2018;24(3):674-7.
36. Mylopoulos M. Preparing future adaptive experts: why it matters and how it can be done. Med Sci Educ. 2020;30(Suppl 1):11-12.
37. Mylopoulos M, Steenhoff N, Kaushal A, et al. Twelve tips for designing curricula that support the development of adaptive expertise. Med Teach. 2018;40(8):850-4.
38. Elendu C, Amaechi DC, Okatta AU, et al. The impact of simulationbased training in medical education: a review. Medicine (Baltimore). 2024;103(27):e38813.
39. Yates N, Purdy E, Braganza S, et al. Can simulation foster resilience in medical students? BMJ Simul Technol Enhanc Learn. 2020;7(1):50-1.
40. Akdeniz M, Yardımcı B, Kavukcu E. Ethical considerations at the end-
of-life care. SAGE Open Med. 2021;9:20503121211000918.
41. D’Alessandro AM, Ritchie K, McCabe RE, et al. Healthcare workers and COVID-19-related moral injury: an interpersonally-focused approach informed by PTSD. Front Psychiatry. 2022;12:784523.
42. Wilson MA, Shay A, Harris JI, et al. Moral distress and moral injury in military healthcare clinicians: a scoping review. AJPM Focus. 2023;3(2):100173.
43. Gignoux-Froment F, Martinez T, Derely J, et al. Ethical dilemmas faced by military health personnel during high-intensity conflict: the crucial issue of triage, Mil Med. 2024;9-10:234-8.
44. Ryu MY, Martin MJ, Jin AH, et al. Characterizing moral injury and distress in US military surgeons deployed to far-forward combat environments in Afghanistan and Iraq. JAMA Netw Open. 2023;6(2):e230484.
45. Bricknell M, Story R. An overview to military medical ethics. J Mil Veterans Health. 2022;30(2):7-16.
46. Beldowicz BC, Modlin R, Bellamy M, et al. Situational triage: redefining medical decision-making for large-scale combat operations. Military Review. 2022;July-August:115-22.
47. Prescott T, May S, Horne S, et al. Prehospital emergency care in a humanitarian environment: an overview of the ethical considerations. BMJ Mil Health. 2022;168(6):431-4.
48. Rushton CH, Thomas TA, Antonsdottir IM, et al. Moral injury and moral resilience in health care workers during COVID-19 pandemic. J Palliat Med. 2022;25(5):712-9.
49. King EL, Hawkins LE. Identifying and mitigating moral injury risks in military behavioral health providers. Mil Psychol. 2022;35(2):169-79.
50. Van Bruchem-Visser RL, van Dijk G, de Beaufort I, et al. Ethical frameworks for complex medical decision making in older patients: a narrative review. Arch Gerontol Geriatr. 2020;90:104160.
51. Cuthbertson J, Penney G. Ethical decision making in disaster and emergency management: a systematic review of the literature. Prehosp Disaster Med. 2023;38(5):622-7.
52. Leider JP, DeBruin D, Reynolds N, et al. Ethical guidance for disaster response, specifically around crisis standards of care: a systematic review. Am J Pub Health. 2017;107(9):e1-9.
53. Beardmore C, Bricknell MCM, Kelly J, et al. Commentary - a military health care ethics framework. Mil Med. 2024:usae351.
54. Bernthal EM, Draper HJA, Henning J, et al. ‘A band of brothers’ - An exploration of the range of medical ethical issues faced by British senior military clinicians on deployment to Afghanistan: a qualitative study. J R Army Med Corps. 2017;163(3):199-205.
55. Lin CY, Meagher K, Bricknell M, et al. The challenges of international collaboration in conflict and health research: Experience from the Research for Health in Conflict-Middle East and North Africa (R4HC-MENA) partnership. Confl Health. 2023;17:29.
56. Flanagan SJ, Down AM, Pezard S. Sustaining the Transatlantic Alliance: 75 years of RAND insights on NATO. 2024. Available at: https://www.rand.org/pubs/commentary/2024/07/sustaining-thetransatlantic-alliance-75-years-of-rand.html. Accessed November 4, 2024.
57. NATO. Military medical support. 2025. Available at: https://www.nato.
int/cps/ru/natohq/topics_49168.htm?selectedLocale=en. Accessed November 4, 2024.
58. Banatvala N, Zwi AB. Public health and humanitarian interventions: developing the evidence base. BMJ. 2000;321(7253):101-5.
59. Wu A, Preker A. Identifying international leadership competencies in medical education. Med Sci Educ. 2023;33(6):1405-8.
60. Chuang E, Cuartas PA, Powell T, et al. “We’re not ready, but I don’t think you’re ever ready.” Clinician perspectives on implementation of crisis standards of care. AJOB Empir Bioeth. 2020;11(1):1-12.
61. Dobiesz VA, Schwid M, Dias RD, et al. Maintaining health professional education during war: a scoping review. Med Educ. 2022;56(8):793-804.
Financial Burden of Emergency Medicine Residency Applications: Pre-,
Christopher Zeuthen, BS*
Eric Shappell, MD, MHPE*
Daniel J. Egan, MD, MBA*†
Elizabeth Barrall Werley, MD‡
Alexis Pelletier-Bui, MD§
Christopher W. Baugh, MD, MBA†
Abigail Raynor, MD, MPH*†
Alexis Campbell, BA, MA*
Angela P. Mihalic, MD||
Andrew D. Luo, MD, MBA*†
Section Editor: Sara Heinert, PhD, MPH
During, and Post-Pandemic
Massachusetts General Hospital, Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts
Brigham and Women’s Hospital, Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts
Penn State Health Milton S. Hershey Medical Center, Department of Emergency Medicine/Penn State College of Medicine, Hershey, Pennsylvania
Cooper University Hospital/Cooper Medical School of Rowan University, Department of Emergency Medicine, Camden, New Jersey University of Texas Southwestern Medical Center, Department of Pediatrics, Dallas, Texas
Submission history: Submitted March 11, 2025; Revision received July 1, 2025; Accepted July 11, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.46997
Introduction: Applying to emergency medicine (EM) residency programs is costly. In the past several years, the EM residency application process has undergone multiple changes in recommendations regarding away rotations and interview format, primarily but not solely driven by COVID-19 restrictions. To date, little is known about the financial impact of these changes on EM applicants. This study assesses recent trends and changes in the costs of the EM residency application.
Methods: We analyzed EM applicant survey data from the Texas STAR (Seeking Transparency in Application to Residency) database from 2019–2024. Application cycles were grouped into three time periods: pre-pandemic (2019–2020), pandemic (2021–2022), and post-pandemic (2023–2024). Applicants’ self-reported data for application fees, away rotation costs, interview costs, and total expenses were analyzed. We conducted Kruskal-Wallis testing to evaluate differences in expenserelated variables across the three time periods. We performed post-hoc analysis using the Dunn test if significant differences were detected.
Results: This study included 3,495 EM applicants, which represents 8.4% of the total 41,497 Texas STAR survey respondents from 2019–2024. Average per-applicant total costs were $5,412, $2,076, and $3,156 in the pre-, during-, and post-pandemic application cycles. Self-reported total applicant expenses decreased between the pre- and pandemic period and increased from the pandemic and post-pandemic period (P < .01). Applicants had the lowest overall costs in 2021. Away rotation, second look, application costs, interview travel and lodging, and virtual interview costs all reached their lowest levels during the pandemic period (P < .01). In the post-pandemic period, travel and lodging costs were higher than pre- and during pandemic levels, while interview costs remained lower due to the continued use of virtual interviews (P < .01). Applicants from the Western Region of the US saw the highest total costs compared to the Northeast, which saw the lowest.
Conclusion: The total expenses reported by medical students applying to EM residency programs were significantly reduced during the pandemic, compared to other years. Some expenses, notably away rotation and second look and application costs, have risen post-pandemic. To help reduce the financial burden of the EM residency process, the continued use of virtual interviews is an opportunity for cost savings. [West J Emerg Med. 2025;26(5)1154–1161.]
INTRODUCTION
Applying to residency programs is a costly endeavor. Historically, EM applicants have numerous application-related expenses including interview travel and away rotations to obtain a Standardized Letter of Evaluation (SLOE), which is an important component of the application process.1–3 Prior studies showed that the average pre-pandemic cost exceeded $8,000 per applicant in EM, over half of which stemmed from applications costs and interview-related travel expenses.4,5 The COVID-19 pandemic brought significant changes to graduate medical education recruitment, evaluation, and selection of applicants. Away rotations were temporarily suspended, and applicant interviews shifted from the traditional in-person format to virtual platforms.6–9 Although away rotations have largely resumed since 2023, recommendations such as virtual interviews have remained.
Before the 2020–2021 application cycle, advising for EM recommended that most applicants complete two core EM rotations, and most interviews were conducted in person.10 In 2020-2021, due to widespread COVID-19 restrictions and national recommendations, EM programs supported applicants completing only one home rotation, a policy shift seen across many specialties.11 Since the 2021–2022 cycle, guidance regarding away rotations has returned to pre-pandemic norms while maintaining virtual interviews.3
To help offset applicants’ financial burden, several evolving measures have been taken on the national or institutional level to help applicants navigate application costs. For example, the Association of American Medical Colleges (AAMC) revised the fee structure for the 2025–2026 application cycle. In addition, some specialties, including obstetrics/gynecology and EM, have transitioned from the Electronic Residency Application Service to Residency Centralized Application Service (ResidencyCAS), a centralized application system that may reduce applicant costs by up to 20%..12,13 Organizations such as the Council of Residency Directors in Emergency Medicine and the Emergency Medicine Residents’ Association have incorporated financial planning tips specific to EM into student advising guides.14 Lastly, there is growing availability of diversity, equity, and inclusion scholarships for applicants participating in away rotations.15
Over the course of these changes, little has been reported about the collective impact on the financial burden incurred by EM residency applicants. In addition, no reports examine how the costs for applicants vary across geographic regions or application years. Prior reports of EM residency application costs predate COVID-19-related changes, which underscores the need for updated research on the current financial landscape for EM. In this study we aimed to assess the changes in EM residency application costs over the pre-, during, and post-pandemic periods. Insights from our study may help stakeholders in the EM residency application process determine ways to better mitigate costs to applicants in the future, creating a more equitable residency application process.
Population Health Research Capsule
What do we already know about this issue? Residency application costs are high and can vary across years, regions, and interview format.
What was the research question?
How did average emergency medicine (EM) residency application costs change across the COVID-19 pandemic?
What was the major finding of the study?
Mean total costs: $5,412 (pre); $2,076 (during); and $3,156 (post-pandemic); P < .001.
How does this improve population health?
Sustaining virtual interviews may reduce cost burden and promote equity in EM residency access.
METHODS
We conducted a retrospective, cross-sectional analysis of the Texas Seeking Transparency in Application to Residency (STAR) database. The Texas STAR database, managed by the University of Texas Southwestern Medical Center in Dallas, TX, is a nationwide resource that compiles self-reported data from medical students at participating schools regarding their residency applications.16 The database represents six years of data from 155 medical schools. Data include application characteristics, expense variables, geographic region variation in costs, and other metrics.
Study Population
We evaluated survey data for EM residency applicants from the 2019–2024 application cycles. In this study, “cycle” refers to the year applicants matched and were slated to start residency training (eg, the 2024 cycle refers to the 2023–2024 application cycle, during which applicants applied in 2023 and then matched and entered residency programs in 2024). Our analysis included both US allopathic (MD) and osteopathic (DO) senior medical students. Responses from international medical graduates (IMG), previous graduates, and reapplicants are not collected in the Texas STAR database and, therefore, were not included in this study. Survey applicant demographic information was broken down by geographic region using the AAMC Group on Student Affairs classifications: Central; Northeastern; Southern; and Western.17
Cost of Emergency Medicine Residency Applications Surrounding the Pandemic
Variables
We collected demographic data for sex and underrepresented in medicine status (URM) and academic metrics, such as the US Medical Licensing Examination (USMLE) Step 1 pass-fail, USMLE Step 2 Clinical Knowledge score, honor society membership in Alpha Omega Alpha or Gold Humanism (Table 1). Additionally, we collected application metrics, including the number of programs applied to, interview offers, and interviews attended. Lastly, Texas STAR collected several expense-related variables: travel cost;
application fees; virtual interview cost; away rotation and second-look cost (collected as a single variable); and total cost; reported in US dollars within a range of values (eg, $500-$1,000).
Statistical Analysis
We categorized the 2019–2024 application cycles into three periods: pre-pandemic (2019–2020); pandemic (2021–2022); and post-pandemic (2023–2024). This categorization was chosen to reflect changes driven by the pandemic and
Texas STAR National Dataset
Texas STAR - Emergency Medicine Respondents
1Sex and under-represented in medicine demographic information was not collected on the Texas STAR database until 2022. AOA, Alpha Omega Alpha; EM, emergency medicine; MD, doctor of medicine; DO, doctor of osteopathic medicine; STAR, Seeking Transparency in Application to Residency; USMLE, US Medical Licensing Exam; CK, clinical knowledge.
Table 1. Demographics and characteristics of respondents to the Texas Seeking Transparency in Application to Residency survey: 2019–2024.
changes in program recruitment practices and recommendations during these periods.
To compare the range of costs reported within expenserelated variables, we calculated a weighted mean and standard deviation for each period’s expense variables, and the total reported costs in each geographic region, enabling comparisons for each group. These weighted means and SDs are presented in the tables and results. All values are reported in the format of weighted mean ± SD in our methods section. For a weighted average calculation, we assigned weights (number of applicants) to each value (midpoint of the range) in a set, after which they were averaged together and compared between years (represented as the weighted mean difference). Weighted mean = [sum of (value × weight)] / (sum of weights). We used a Shapiro-Wilk test to assess the normality of the data distribution. As the expense-related variables were not normally distributed, we applied non-parametric methods. A Kruskal-Wallis test was conducted to evaluate differences in expense-related variables across the three time periods. We performed post-hoc analysis using the Dunn test if significant differences were detected.
Lastly, we recognized inflationary changes throughout the three periods. To perform a sensitivity analysis, we adjusted the expense variables in each year to the 2024 real costs by applying the Consumer Price Index (CPI) as the inflation adjustment factor. Specifically, expenses from previous years were multiplied by the ratio of the CPI in 2024 to the CPI of the respective year, standardizing all costs to reflect their real value in 2024 US dollars (Supplemental Table 1a and 1b). We used R programming software v2023.12.0, (The R Foundation for Statistical Computing, Vienna, Austria) for all statistical analysis. The data used in this study did not meet the criteria for human subject research by the Mass General Brigham Institutional Review Board, and the study was deemed exempt.
RESULTS
From 2019 to 2024, 41,497 students completed the Texas STAR survey, including 3,495 EM applicants (8.4%). United States MD seniors comprised nearly 100% of respondents pre-pandemic and approximately 80% post-pandemic, with a
corresponding increase in DO respondents. Regional representation remained stable across application cycles, with applicants from the Western US representing the smallest proportion of respondents (Table 1).
Average total application costs were $5,412 ± $3,481 pre-pandemic, $2,076 ± $1,735 during the pandemic, and $3,156 ± $2,549 post-pandemic, representing a 62% drop during the pandemic and a 42% reduction from pre-pandemic levels (Table 2a, Figure 1). The greatest savings came from costs related to interview travel and lodging, which declined from $2,610 ± $2,276 pre-pandemic to $549 ± $353 during the pandemic. In 2021, at the height of COVID-19, 79% of applicants reported total spending of < $2,000. with 1% reporting spending > $6000. By 2024, 14% of applicants reported spending > $6,000, and 30% reported total costs of < $2000 (Figure 2).
Away-rotation and second-look costs decreased from $1,787 ± $1,498 pre-pandemic to $1,388 ± $1,384 during the pandemic but rose post-pandemic to $2,123 ± $1,828, surpassing pre-pandemic levels. In comparison, application costs followed a similar trend with post-pandemic costs reaching a high of $1,138 ± $647 and a low of $1,041 ± $682 during the pandemic (Table 2a-b, Figure 1).
Pre-pandemic applicants reported spending on average $2,610 ± $2,276 on interview travel and lodging costs, peaking in 2020 at $2,613 ± $2,303. During the pandemic, interview costs declined, with an average cost of $549 ± $353, with a low of $548 ± $427 in 2021. Post-pandemic interview travel and lodging costs rose to $700 ± $636, which remain below pre-pandemic levels. With a shift to primarily virtual interviews during and after the pandemic, applicant costs across these two periods were $79 ± $51 and $69 ± $42, respectively (Table 2a-b, Figure 1).
The Kruskal-Wallis test found statistical significance for all cost variables (P < .001). Post-hoc analysis identified significant differences between pre-, during, and postpandemic periods for total application costs, away-rotation and second-look costs, virtual interviews, and interview travel and lodging costs. The one outlier was application costs. The post-hoc analysis did not reveal statistical significance between pre- and pandemic period application costs (P = .23), but it did for pre- vs post-pandemic and the pandemic vs
Table 2a. Emergency medicine residency applicants’ yearly average cost with standard deviation, by category ($US).
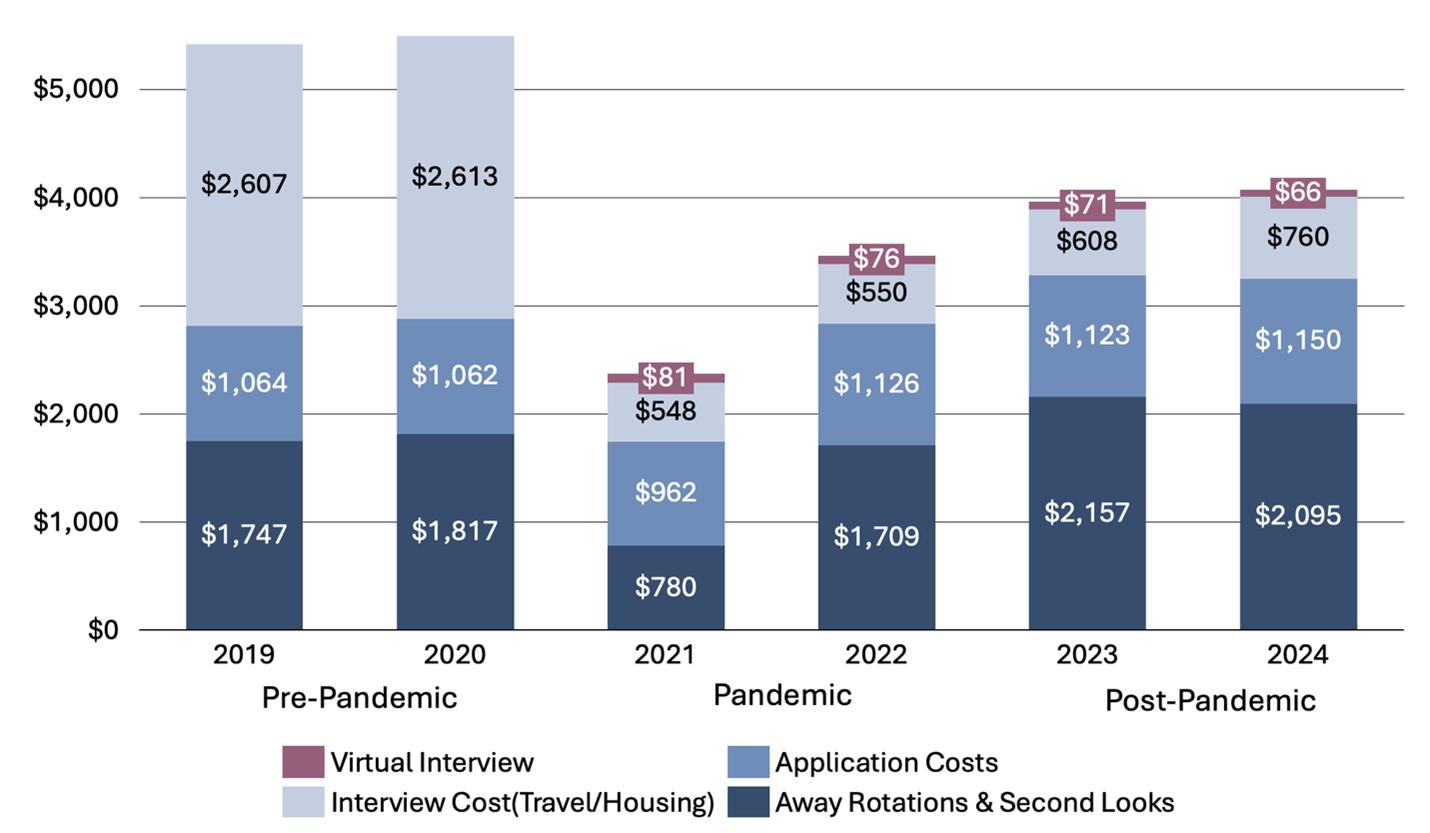
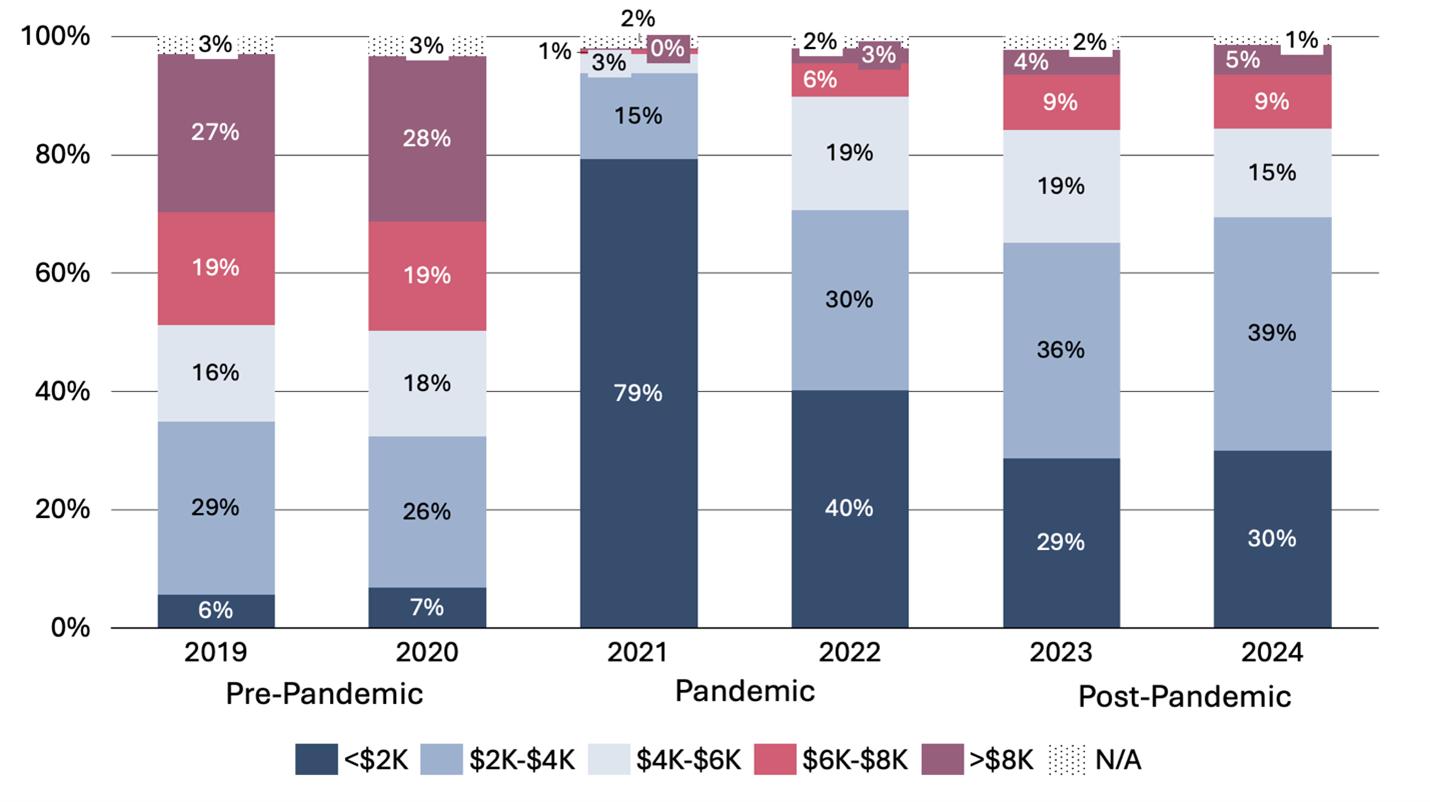
post-pandemic periods (P < .001).
Applicants from the Western region reported the highest total application costs across all periods: $7,744 ± $4,535 pre-; $3,077 ± $2,572 during; and $4,617 ± $3,459 post-pandemic. In comparison, applicants from the Northeast maintained the lowest average total costs during these periods, with a low at $1,781 ± $1,394 during the pandemic. Total costs declined during the pandemic across all regions and rose post-pandemic but remained below pre-pandemic levels. The Kruskal-Wallis test confirmed significant differences in total costs across the three periods within each region (P < .001) and Dunn post-hoc analysis identified significant pairwise differences between each region for each pandemic period (P < .001) (Table 3). Sensitivity analysis, grouped by pandemic period and adjusted to 2024 dollars to account for inflation, showed consistent statistical significance across all expense variables (Supplemental Table 1a-b).
DISCUSSION
In this study we evaluated recent cost trends in the EM residency application and interview process, considering COVID-19 restrictions and policy changes. This is the first study to assess EM residency application expenditures across various cost categories, offering a national analysis of how
COVID-19 policies affected applicants’ expenses.
Away rotations and second looks remain costly but represent impactful elements according to program directors and, therefore, represent necessary expenses.2 Initiatives like broader visiting student scholarships and subsidized housing have helped reduce these costs, but they remain limited.15 Continued advising regarding judicious use of away rotations is helpful. During the 2021 and 2022 application cycles, costs for away rotations and second looks significantly decreased, likely due to pandemic-related restrictions. The future impact of post-pandemic changes on these costs is uncertain. Notably, the Texas STAR database combines away rotations and second looks as one cost. The former occurs early and is an essential component, while the latter occurs later in the application season and is optional, yet both incur travel and lodging expenses.
Virtual interviews have helped minimize costs for applicants, as virtual interview equipment is inexpensive and reusable throughout the interview season. The shift to virtual interviews has increased accessibility, allowing applicants to attend more interviews, and enabled programs to interview more candidates, as shown in our analysis (Table 1). Many
Figure 1. Emergency medicine residency applicants’ average cost, by category (in United States dollars).
Figure 2. Distribution of emergency medicine residency applicants’ self-reported total application costs, in $2,000 increments, by application year (%). N/A, no answer.
Table 2b. Emergency medicine residency applicants’ average cost with standard deviation, by cost category ($US) and pandemic period.
Table 3. Emergency medicine residency applicants’ average cost with standard deviation, by category ($USD*) organized by pre-pandemic (2019-2020), pandemic (2021-2022), and post-pandemic (2023-2024), and by AAMC Student Affairs Region.
Geographical region Pre-Pandemic Pandemic Post-Pandemic P-value (Pre- vs During) P-value (During vs Post-) P-value (Pre- vs Post-)
Central $5,832 ± 3,862 $2,101 ± 1,800
±
± 2,177 < .001 < .001 < .001
Southern $6,836 ± 4,390 $2,248 ± 1,806 $3,525 ± 2,472 < .001 < .001 < .001
Western $7,744 ± 4,535 $3,077 ± 2,572 $4,617 ± 3,459 < .001 < .001 < .001
*USD, United States dollars; AAMC, Association of American Medical Colleges.
program directors note that virtual interviews sufficiently validate their perceptions of applicants.18–20 While further research is necessary to assess the effectiveness of virtual interviews in evaluating candidates and determining programs’ rank order lists, EM continues to support virtual interviews for reasons including applicant equity.21
Given the high costs of away rotations and second looks identified in our study, applicants could allocate financial savings from virtual interviews to participate in second-look days. Unlike pre-pandemic applicants who interviewed in person, post-pandemic applicants may rely more on secondlook experiences to assess programs, a trend noted in other specialties.22,23 Additionally, with the potential increase in second-look participation and the return of away rotations, applicants face rising travel and accommodation costs in the post-pandemic era.24 The future of virtual interviews remains uncertain, but their recent implementation has noticeably impacted costs.25
Similar to the findings in our dataset (Table 1), applications per applicant have decreased in the past several years from their peak in 2022, suggesting that the per-application cost has steadily risen.26 While ERAS fees per application increased incrementally across tiers under the previous structure (eg, $99 for the first 10 programs, then $26 per program beyond 30 applications in the 2021–2022 cycle), the AAMC implemented a simplified fee model beginning with the 2025 application cycle, setting costs at $11 per program for the first 30 programs and $30 thereafter. These structural changes may have influenced applicant behavior, although causality cannot be determined from the available data.12 Our findings align, at least in part, with national AAMC EM data, suggesting that our findings may be reflective of national trends; however, further extrapolation to the broader EM application pool would be required to confirm generalizability. Another factor contributing to the rising costs demonstrated in our dataset for the post-pandemic period is the proportion of DO applicants, which rose from near 0% in the pre-pandemic period to approximately 20% post-pandemic (Table 1). With osteopathic medical schools more geographically dispersed and with fewer residency program affiliations DO applicants may incur higher costs for traveling to away rotations and interviews.27 This evolving applicant pool may partially contribute to cost differences observed over time. Several initiatives aim to reduce applicant costs, including
the AAMC’s revised ERAS fee structure for the 2025 application cycle and the planned transition to ResidencyCAS by some programs in 2025–2026, which is projected to cut average application fees by up to 20%.12-13 However, these changes address only one part of the cost burden—primarily application submission fees. More expensive components, such as travel and lodging for away rotations, in-person interviews, and second looks, remain largely unchanged. While national guidelines recommend continuing virtual interviews to reduce costs, programs retain flexibility in their interview format. Given the significant financial savings associated with virtual interviews, they should be considered a key strategy to reduce applicant burden. As programs increasingly explore hybrid or in-person approaches, continued monitoring of total application and interview costs will be important. In addition, since application costs are self-reported, they may include broader expenses such as Visiting Student Learning Opportunities (VSLO) fees or ancillary services.
Applicants across all geographic regions experienced cost savings during the pandemic as away rotations and second looks were paused and virtual interviews were introduced. Despite the return of away rotations and some in-person second looks, applicants across all regions reported lower total costs post-pandemic, largely driven by reduced interview costs likely due to continuing virtual interviews. Western region applicants have particularly benefited from the transition to virtual interviews, as pre-pandemic, they demonstrated the highest travel and lodging expenses. However, Western region applicants still report the highest overall costs compared to other regions, especially those in the Northeast.
Regional cost differences are most likely driven by away-rotation and second-look attendance collectively. With many EM programs concentrated on the East Coast, Western region applicants face heightened travel and accommodation costs to attend away rotations and second looks.28 In comparison, Northeastern applicants can more readily commute regionally for away rotations and second looks. Moreover, the 2022–2023 ERAS applicant survey shows that 69% of EM applicants state that geographic location was the most important factor in where they applied.29 Finally, EM organizations and residency programs could continue to seek other ways to reduce applicant costs, such as grants, and to
emphasize that second looks are non-evaluative and optional, to minimize unnecessary expenses.
The reported costs in our analysis need to be considered in the context of inflation. Over the application years 2019-2024 examined in our study, the CPI ranged from 255.7 to 314.4, rising year over year to a high in 2024.30 Notably, we performed a sensitivity analysis to account for these changes, which yielded results consistent with our unadjusted analysis, highlighting that inflation did not substantially alter our observed trends or statistical significance across the examined periods.
Lastly, with the upcoming transition of EM to the ResidencyCAS platform, there will be a structural shift in the application process. This change is imminent and raises important questions about future cost implications However, it is important to note that ResidencyCAS addresses only one component of the overall cost burden—primarily application submission fees. Our study highlights that the most significant cost drivers for EM applicants have historically been away rotations and travel, which are not directly affected by the choice of application platform. Therefore, we hope that our findings will help inform future advising, equity discussions, and cost-containment strategies even as the logistics of application submission evolve.
LIMITATIONS
There are several limitations to this study. While the Texas STAR survey is a national database, survey respondents were primarily US MD seniors, with a smaller proportion of US DO seniors. It does not represent all US medical schools nor does it entail a proportional distribution of applicants across all geographic regions. Further, the study did not include responses from IMGs or those applicants who may have previously graduated from medical school. Osteopathic students and IMGs represent a substantial percentage of applicants to EM residency positions in a shifting applicant pool.25 In addition, with fewer home programs these applicants will require two away rotations to obtain the recommended two SLOEs. Notably, DO and IMG applicants often perform more away rotations due to fewer home EM programs, which may result in higher unmeasured costs. Thus, our calculated averages may underestimate true costs for the broader applicant population.
In addition, because the Texas STAR survey is anonymous and voluntary, it is susceptible to response bias. Respondents who choose to complete the survey may differ systematically from non-respondents in ways that affect cost reporting. Furthermore, because the survey is completed several months after expenses are incurred, the data are subject to recall bias. Another limitation is that the Texas STAR survey combines away rotation and second-look events into one cost variable when these are two separate events during an applicant’s cycle. Given the combined variable, it is challenging to determine which of these is the primary driver of costs. Additionally, the components contributing to “virtual
interview costs” are not well-defined, and we were unable to verify what applicants chose to include in this category. While in-person costs (eg, travel, lodging) are more straightforward, virtual costs may have included equipment, software, or internet upgrades. Finally, the Texas STAR survey does not account for instances by which applicants may have reduced their total expenditures, such as visiting student scholarships, housing discounts, or sublet/house swap opportunities, which may alleviate some of the costs reported by applicants.
CONCLUSION
Emergency medicine applicant costs were lowest during the pandemic, primarily due to travel restrictions and the shift to virtual interviews. Post-pandemic costs rose but remained below pre-pandemic levels overall, with increases in application, away rotation, and second-look expenses. The continuation of virtual interviews appears to be a key strategy for reducing applicant financial burden.
Address for Correspondence: Andrew D. Luo, MD, MBA, Massachusetts General Hospital, Harvard Medical School, 55 Fruit St, Boston, MA 02114. Email: andrewluo@alumni.duke.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No [other] author has professional or financial relationships with any companies that are relevant to this study. There are no [other] conflicts of interest or sources of funding to declare.
Copyright: © 2025 Zeuthen et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Keim SM, Rein JA, Chisholm C, et al. A standardized letter of recommendation for residency application. Acad Emerg Med 1999;6(11):1141-1146.
2. Negaard M, Assimacopoulos E, Harland K, et al. Emergency medicine residency selection criteria: an update and comparison. AEM Educ Train. 2018;2(2):146-153
3. Council of Emergency Medicine Residency Directors (CORD). 2023-2024 MyERAS Applicant and Advisor Guide for Emergency Medicine; 2023. Available at: https://www.cordem.org/siteassets/ files/2023-2024-myeras-applicant-and-advisor-guide-for-emergencymedicine.pdf. Accessed November 11, 2024.
4. Blackshaw A, Watson S, Bush J. The cost and burden of the residency match in emergency medicine. West J Emerg Med 2017;18(1):169-173.
5. Van Dermark JT, Wald DA, Corker JR, et al. Financial implications of
Zeuthen et
Cost of Emergency Medicine Residency Applications Surrounding
the emergency medicine interview process. AEM Educ Train 2017;1(1):60-69.
6. Davis MG, Haas MRC, Gottlieb M, et al. Zooming in versus flying out: virtual residency interviews in the era of COVID‐19. AEM Educ Train 2020;4(4):443-446.
7. Rajendran L, Nadler A. Virtual interviews in postgraduate medical education recruitment: Is there a future post-pandemic? J Grad Med Educ. 2022;14(4):377-381.
8. Daniel M, Gottlieb M, Wooten D, et al. Virtual interviewing for graduate medical education recruitment and selection: A BEME systematic review: BEME Guide No. 80. Med Teach 2022;44(12):1313-1331.
9. Ben Ammer A, Bryan JL, Asghar-Ali AA. The impact of COVID-19 in reshaping graduate medical education: harnessing hybrid learning and virtual training. Cureus. 2024;16(3):e56790.
10. Emergency Medicine Residents’ Association (EMRA). Applying for Away Rotations. EMRA Advising Guide for Medical Students. Available at: https://www.emra.org/books/msadvisingguide/applyingfor-away-rotations. Accessed January 11, 2025.
11. Emergency Medicine Residents’ Association (EMRA). Consensus Statement on the 2020-2021 Residency Application Process for US Medical Students Planning Careers in Emergency Medicine in the Main Residency Match. Available at: https://www.emra.org/beinvolved/be-an-advocate/working-for-you/residency-applicationprocess. Accessed January 27, 2025.
12. Fee Announcement for 2025 ERAS® Residency Applications. Students & Residents. Available at: https://students-residents.aamc. org/applying-residencies-eras/fee-announcement-2025-erasresidency-applications. Accessed November 11, 2024.
13. Council of Residency Directors in Emergency Medicine. Emergency Medicine Collaboration with ResidencyCAS. Available at: https:// www.cordem.org/resources/upcoming-changes-in-em/em-collab-withresidencycas. Accessed June 27, 2025.
14. Emergency Medicine Residents’ Association, Council of Residency Directors in Emergency Medicine. EMRA and CORD Student Advising Guide.; 2023. Available at: https://www.cordem.org/ siteassets/images/bod-elections/emra-studentadvisingguide-2023_ web-file.pdf. Accessed January 19, 2025.
15. Council of Residency Directors in Emergency Medicine. DEI Rotation Scholarships. Available at: https://www.cordem.org/resources/ professional-development/diversity-program-listings/dei-rotationscholarships. Accessed January 19, 2025.
16. Texas STAR. https://www.utsouthwestern.edu/education/medicalschool/about-the-school/student-affairs/texas-star.html. Accessed November 14, 2024.
17. GSA Member Schools by Region. 2024. Available at: https://www. aamc.org/career-development/affinity-groups/gsa/member-schoolsregion. Accessed December 6, 2024.
18. Domingo A, Rdesinski RE, Stenson A, et al. Virtual residency interviews: applicant perceptions regarding virtual interview
effectiveness, advantages, and barriers. J Grad Med Educ 2022;14(2):224-228.
19. Gotewal S, Feng SY, Bansal BBC, et al. Does virtual interviewing provide the information for a satisfactory rank decision? A perspective from the pediatric emergency medicine fellowship interviews. Pediatr Emerg Care. 2025;41(3):165-171.
20. Li-Sauerwine S, Weygandt PL, Smylie L, et al. The more things change the more they stay the same: factors influencing emergency medicine residency selection in the virtual era. AEM Educ Train 2023;7(6):e10921.
21. Council of Residency Directors in Emergency Medicine. Application Process Improvement Committee (APIC): Best Practices for the 2024-2025 Residency Application and Interview Season. Council of Residency Directors in Emergency Medicine. Available at: https:// www.cordem.org/involved/Committees/application-processimprovement-taskforce. Accessed March 1, 2025.
22. Keshwani S, Sullivan G, Govekar H, et al. General surgery residency applicant perspectives on alternative residency interview models with implementation of an optional second look day. J Surg Educ 2024;81(11):1784-1791.
23. England E, Kanfi A, Tobler J. In-person second look during a residency virtual interview season: an important consideration for radiology residency applicants. Acad Radiol. 2023;30(6):1192-1199.
24. U.S. Travel Association. Travel Price Index. U.S. Travel Association. February 13, 2025. https://www.ustravel.org/research/travel-priceindex. Accessed February 16, 2025.
25. Balch B. Do the benefits of virtual residency interviews outweigh the downsides? Association of American Medical Colleges (AAMC). October 17, 2024. https://www.aamc.org/news/do-benefits-virtualresidency-interviews-outweigh-downsides. Accessed January 29, 2025.
26. Association of American Medical Colleges. 2025 ERAS Residency Preliminary Report. Association of American Medical Colleges; 2025. Available at: https://www.aamc.org/media/81236/ download?attachment. Accessed January 19, 2025.
27. American Association of Colleges of Osteopathic Medicine. U.S. Colleges of Osteopathic Medicine. Published 2025. Available at: https://www.aacom.org/become-a-doctor/prepare-for-medical-school/ us-colleges-of-osteopathic-medicine. Accessed June 27, 2025.
28. Gaeta TJ, Ankel FK, Calderon Y, et al. American Board of Emergency Medicine report on residency and fellowship training information (2023-2024). Ann Emerg Med. 2024;84(1):65-81.
29. Association of American Medical Colleges. Supplemental ERAS® 2022-2023 Application Cycle: Results of the Applicant Reaction Survey.; 2022:8. Available at: https://www.aamc.org/media/64611/ download. Accessed January 19, 2025.
30. Federal Reserve Bank of Minneapolis. Consumer Price Index (Estimate) 1913-. Federal Reserve Bank of Minneapolis. Available at: https://www.minneapolisfed.org/about-us/monetary-policy/inflationcalculator/consumer-price-index-1913-. Accessed January 19, 2025.
Characteristics and Educational Support Resources Available to Emergency Medicine Core Faculty: A National Survey
Jaime Jordan, MD, MAEd*†
Laura R. Hopson, MD, Med‡
Fiona Gallahue, MD§
James A. Cranford, PhD‡
John C. Burkhardt, MD, PhD‡||
Keith E. Kocher, MD, MPH‡||
Drew L. Robinett, MD†
Moshe Weizberg, MD#
Tiffany Murano, MD¶
Oregon Health & Science University, Department of Emergency Medicine, Portland, Oregon
David Geffen School of Medicine at University of California Los Angeles, Department of Emergency Medicine, Los Angeles, California
University of Michigan Medical School, Department of Emergency Medicine, Ann Arbor, Michigan
University of Washington, Department of Emergency Medicine, Seattle, Washington
University of Michigan Medical School, Department of Learning Health Sciences, Ann Arbor, Michigan
Maimonides Midwood Community Hospital, Department of Emergency Medicine, Brooklyn, New York
Columbia University, Department of Emergency Medicine, New York, New York
Section Editor: Benjamin Holden Schnapp, MD, MEd
Submission history: Submitted February 8, 2025; Revision received May 17, 2025; Accepted May 21, 2025
Electronically published September 2, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.42503 *
Introduction: Core faculty are key to supporting the educational mission in emergency medicine (EM). Changes in the Accreditation Council for Graduate Medical Education (ACGME) requirements for minimum protected time for core faculty may no longer guarantee adequate support. We sought to assess EM core faculty characteristics, support, and the impact of the 2019 revisions to ACGME regulations. We explored the influence of individual and institutional characteristics on support and the impact of the regulatory changes.
Methods: This was a cross-sectional survey study of a convenience sample of EM core faculty. Participants completed an online survey of multiple-choice and completion items between April–June 2022. We calculated descriptive and comparative statistics to assess associations between individual (e.g., sociodemographics, rank) and institutional (e.g., region, program type) factors on resources and impact of ACGME revisions.
Results: A total of 596 individuals (57% male) from 116 residency programs participated, including 15 (3%) instructors/lecturers, 280 (47%) assistant professors, 182 (31%) associate professors, and 80 (13%) professors. Most (64%) were 36-50 years of age; 246 (41%) had completed a fellowship. Despite the change to the ACGME requirements in 2019, 417 (70%) reported no modification to their clinical work hours, and 420 (71%) reported no modification to their non-clinical responsibilities. There were statistically significant associations between number of residents per class (P < .001), duration of training program (P < .001), and type of institution (P < .001) with the number of administrative personnel. We also observed statistically significant associations between academic rank (P = .02), region (P =.01), number of residents per class (P = 0.02), and type of site (P = .01) with change to clinical work hours after changes to ACGME requirements.
Conclusion: A minority of participants reported a change to their clinical and non-clinical expectations after revisions to the ACGME regulations with disproportionate impact across faculty and program type. [West J Emerg Med. 2025;26(5)1162–1169.]
INTRODUCTION
Academic emergency physicians play a unique and valuable role in the US healthcare system. Although academic emergency departments (ED) make up ~2% of all US EDs, these centers provide care for 5-12% of all acute care patients (> 10 million annually), staffing ~20% of all trauma centers and ~25% of transplant centers.1,2 However, in addition to their complex patient care responsibilities, the core faculty of these academic centers are charged with multiple extra-clinical responsibilities: training residents and medical students; publishing scholarly work; and filling administrative and quality improvement positions both within and outside the hospital.3
Success in these multifaceted roles requires substantial investment in personnel, funds, education, and opportunity.4 But, as of 2019, such support may not be guaranteed. The Accreditation Council for Graduate Medical Education (ACGME) changed prior regulations on protected time for CF from a limit on clinical hours to a minimum percentage of support, potentially reducing the administrative and financial support they receive for extra clinical responsibilities of their job.5,6 This recent change has renewed a century-old discussion on the intrinsic value of academic faculty and how best to support and compensate their work.7,8 Researchers have investigated the characteristics of this complex issue related to academic faculty roles and support, but often from a top-down perspective in which they summatively assess departments through the responses of program directors or department chairs.1,9,10
To more deeply understand the core-faculty workforce and the resources they are provided to accomplish their critical responsibilities, the field would benefit from data reported directly by the core faculty themselves. In this study, we aimed to characterize this workforce including sociodemographics, roles, responsibilities, administrative support, protected time, and impact of ACGME regulations. We also sought to test the association of these sociodemographic and institutional characteristics on administrative time and funding resources. Understanding these relationships is crucial to informing regulatory bodies and institutional leadership to provide necessary resources and staffing systems that allow faculty to meet the demands of their job tasks and thrive in their uniquely multidimensional roles.
METHODS
Design, Setting and Participants
This is a cross-sectional electronic survey study of a convenience sample of core faculty in emergency medicine (EM). We included individuals who were reported as core faculty to the ACGME. We announced the study and directly recruited participants at the Council of Residency Directors in Emergency Medicine (CORD) 2021 Academic Assembly and through emails on the organizational listserv. We also directly reached out to programs to seek diverse representation with
Population Health Research Capsule
What do we already know about this issue? Core faculty are essential to the educational mission in EM but may not get adequate support to carry out their tasks.
What was the research question?
What support do core faculty receive, and how have they been impacted by changes in regulatory requirements re protected time?
What was the major finding of the study?
Approximately 70% of participants reported no change to their clinical work hours or non-clinical responsibilities after regulatory revisions.
How does this improve population health?
Insights from core faculty themselves on the impact of fewer protected hours illuminate potential downstream impact on teaching, publishing, and fulfilling administrative duties.
regard to region, duration of training, and institution type. We collected data between April–June 2022.
Study Protocol
We emailed participants a link to an online survey. Informed consent was implied by those who clicked the survey link. We sent up to three reminders to non-responders at regular intervals. We provided participants with a $10 gift card for survey completion. To maximize response rates and minimize guessing, we did not require participants to answer all items on the survey.
Instrument Development
Our study team of expert educators and education researchers developed the survey after literature review to optimize content validity. We developed the surveys according to best practices in survey design.11 The survey consisted of multiple-choice and completion items. We read all items aloud among the author group and piloted the survey with a small group of EM faculty to ensure response process validity. We made revisions for clarity and readability based on feedback. The final survey is available in Appendix A.
Data Analysis
As this was an exploratory study, we did not conduct
statistical power analyses or sample size estimates. We calculated descriptive statistics including percentages and measures of central tendency to detail respondent demographics and responses to survey items with discrete answer choices. We used chi-squared tests, independentgroups t-tests, and correlational analyses to examine associations between individual and institutional characteristics with outcome variables of number of administrative personnel, job responsibilities, clinical work hours, and non-clinical expectations. An alpha level of .05 was used for all analyses, and all statistical significance tests were two-tailed. We conducted all analyses with the SPSS software package v29.0 (IBM Corp, Armonk NY).
Institutional Review Board Statement
This study was reviewed by the Institutional Review Board of the University of Michigan and determined to be “exempt” based on federal exemption category 3(i)(B) at 45 CFR 46.104(d).
RESULTS
A total of 596 core faculty from 116 EM residency programs participated in this study. We report the characteristics of participants, programs, and institutions in Table 1. Participants were most motivated to be core faculty by the additional opportunities to mentor and teach trainees, to participate in the educational program, and obtain recognition of their educational work with 475 (80.0%), 429 (72.0%), and 261(44.0%) identifying these as one of their top three most important motivators, respectively. While participants received multiple benefits from being core faculty, they had additional responsibilities (Table 2). They found scholarship requirements, completion of assessments, and involvement in the didactic curriculum to be their most challenging responsibilities, with 336 (68.7%), 298 (60.9%), and 238 (48.7%) ranking these as their top three most difficult responsibilities, respectively.After the change to the ACGME requirements in 2020, 417 core faculty (70%) reported no change to their clinical work hours and 420 (70.5%) reported no change to their non-clinical responsibilities (Table 2). Of the 52 participants (11.1%) who reported that the change in ACGME requirements affected their clinical work hours, a greater percentage of assistant (11.3%) and associate professors (11.5%) were affected compared to professors (4.0 %) and instructors/lecturers (0%), P = .01. The average number of residents per class was statistically significantly lower among those who indicated that the change in ACGME requirements of July 2020 affected their clinical work hours (mean 11.1 ± 3.3) vs those who indicated that it did not (mean 12.1 ± 3.5), P = .02. Type of site was statistically significantly associated with change to clinical work hours after changes to ACGME requirements (P = .01) with 66.7% of military/ Veterans Administration (VA) sites, 14.8% of community sites, 9.2% of county/public sites, 8.8% of university sites, and
Table 1. Participant, program, and institution characteristics in a survey of emergency medicine core faculty.
Sex
MD, Doctor of Medicine; DO, Doctor of Osteopathic Medicine; MA, Master of Arts
Table 1. Continued
Total N = 596 n (%) MHPE
14 (2)
10 (2)
(21)
(0)
(0)
(0)
(0)
(2)
Table 1. Continued
Academic rank Instructor/Lecturer
Administrative roles**
Program Director
Assistant/Associate Program Director
Clerkship Director
Assistant or Associate Clerkship Director
Fellowship Director
Medical Director or Assistant/Associate
Medical Director
EMS Director or Assistant/Associate EMS Director
Ultrasound Director or Assistant/Associate
Ultrasound Director
Research Director or Assistant/Associate
Research Director
Vice Chair Chair
Designated Institutional Official Assistant/Associate
Institution has specific faculty promotion tracks
Specific faculty promotion track Clinical Administrator Clinical
Promotion track with tenure
(3)
(47)
(31)
(13)
(4)
(2)
(13)
(25)
(10)
(4)
(12)
(13)
(8)
(10)
(5)
(10)
(4)
(1)
(3)
(25)
(13)
(34)
(65)
(2)
(4)
(46)
(1)
(5)
(8)
(35)
(72)
(14)
(15)
(22)
(24)
MHPE, Master of Health Professions Education; PhD, Doctor of Philosophy; MBA, Master of Business Administration; EdD, Doctor of Education; JD, Juris Doctor; PharmD, Doctor of Pharmacy; EMS, emergency medical services.
Faculty employment model of primary training site
School of Medicine Employee Direct Hospital Employee Large Contract group (Covers > 10 EDs)
Small Contract group (Covers ≤ 10 EDs)
group
Contractor
of personnel in program administration (mean ± standard deviation) 3.6 ± 4
*Based on n = 246 who responded “Yes” to “Have you completed a fellowship training program?”
**Participants could select more than one role.
PGY, postgraduate year; VA, Veterans Administration; ED, emergency department.
7.1% of other sites reporting a change to clinical hours. Region was also statistically significantly associated with change to clinical work hours after changes to ACGME requirements (P = .09) with 18.0% of programs in the South, 11.7% of programs in the Midwest, 7.5% of programs in the Northeast, and 5.8% of programs in the West reporting a change to clinical hours.Of the 596 study participants, 400 (71.8%) reported that the previous ACGME requirements accurately reflected their commitments and responsibilities. Academic rank was statistically significantly associated with accurate reflection of responsibilities in previous ACGME requirements (P = .18) with 84.4% of professors, 85.4% of associate professors, 76.3% of assistant professors, and 62.5% of instructors/lecturers reporting that that the prior ACGME requirements accurately reflected their commitments and responsibilities. The average number of residents per class was statistically significantly higher among those who indicated that the previous ACGME requirements accurately reflected their commitments and responsibilities (mean 12.1 ± 3.4) vs those who indicated that the previous ACGME
Table 2. Reported benefits and responsibilities of being core faculty in emergency medicine,
Responsibilities and benefits received as core faculty*
Additional clinical time with trainees
Mean percentage of FTE reduction for being core faculty**
Mean additional CME funds (in dollars per year) for being core faculty***
Did the previous ACGME requirements accurately reflect your commitments and responsibilities?
Did the change to the ACGME requirements in July 2019 affect your clinical work hours?
Did the change to the ACGME requirements in July 2019 affect your non-clinical expectations?
If your group decreases their current level of support for core faculty in terms of shift numbers or non-clinical expectations, how would it change your willingness to serve as core faculty?
In the past two years, which of the following scholarship requirements for core faculty status have you met?* Peer-reviewed publications
at Local/ Regional/National organizations
*Participants could select more than one response.
*Based on responses from n = 53 participants.
**Based on responses from n = 232 participants. FTE, full-time equivalent; CME, continuing medical education; ACGME, Accreditation Council for Graduate Medical Education.
requirements did not accurately reflect their commitments and responsibilities (mean 11.2 ± 3.5), P = .02. There were no statistically significant differences between sex, race, academic rank, type of institution, region, residency duration, or number of residents per class on changes to non-clinical expectations after revisions to the ACGME requirements. There were statistically significant differences by program duration (three vs four years) and number of residents and number of personnel in program administration. The average number of personnel working in program administration was higher among participants from four-year programs (mean 5.0 [SD = 6.2]) compared to participants from three-year programs (3.1 [SD = 2.6]), P < .001. Programs with more residents also had more personnel in program administration (r(575) =.18, P < .001). The mean number of administrative personnel was also higher in county/public (4.5 [SD = 5.7]) and university (4.4 [SD = 4.3]) than community (2.4 SD = 2.0), military/VA (2.0 [SD = 0.0]) and other (2.8 [SD = 1.8]) training sites (P < .001) and higher in the West (4.6 [SD = 5.8]) and Midwest (4.0 [SD = 4.5]) than the South (3.3 [SD = 2.1]) and Northeast (2.7 [SD = 2.3]) regions (P < .001).
DISCUSSION
The previous EM program requirements had a 28 hours/ week ceiling on the amount of clinical time that core faculty were permitted to work.5 When considering a 40-hour work week, this allotted core faculty 12 hours per week for administration and educational activities. The 2023 requirements establish a floor of 0.1 full-time equivalent (FTE) of protected time for core faculty, or approximately four hours per week in the 40-hour work week model.15 Understanding the workforce composition, its responsibilities, and impact of the ACGME changes is critical to determining whether this model of support is adequate. Drawing from a broad cross-section of EM core faculty across geographic regions, program types, and training sites, we are able to describe the core faculty workforce. In comparison to other recent studies of EM, residency core faculty have similar sex distributions to large studies of national specialty organizations.16
Our study noted significant associations between academic rank and faculty responsibilities as well as clinical work hours. Most faculty indicated that the prior ACGME requirements accurately reflected their educational commitments, particularly those at the rank of professor and associate professor. These findings may reflect the solidification of responsibilities and alignment with regulatory requirements as faculty progress in their careers. Although at the time of data collection, only a small subset of participants (11%) had been impacted by higher clinical work hours, we found that faculty at the assistant or associate professor rank may be disproportionately affected. These mid-career faculty may have been at the sweet spot to squeeze. They have advanced beyond the very early career stage and may have some administrative time to lose in favor of
clinical work compared to clinical instructors who may have already been working substantial clinical time that could not be significantly increased. Yet they are not as advanced in their careers as professors who may have more secure means of protected time such as grant funding or advanced leadership positions.
It is not surprising that programs with larger numbers of residents had more program administrative personnel, highlighting the scaled requirement for resources to the size of the programs.3,15 This is evident in the ACGME requirements regarding the minimum number of program coordinators, which are scaled to increase with the increased size of a program.3,15 The higher numbers of additional personnel in program administration among four-year programs is likely a reflection of the relative sizes of four-year programs being overall larger.17 Similar associations between size and duration of program have been seen with other outcomes.18
Interestingly, although there was no change in the clinical expectations for most participants, there were changes in clinical hours associated with faculty from programs with fewer residents with the new program requirements. This may be due to a perception that smaller programs require less time to administer. While this may be true, there is still a significant amount of time required for engaging in other programmatic and education-related activities that take place regardless of the number of residents in a program (eg, attendance at weekly conference, preparation and delivery of didactic sessions, interview/recruitment efforts, medical student mentoring, scholarship efforts). The correlation between programs with fewer residents and faculty who experienced changes in their clinical work hours as well as their commitments and responsibilities suggests that the smaller programs may have less flexibility in redistributing the clinical and administrative workloads when the ACGME requirements were modified. This potentially places a higher burden on these faculty, expecting them to perform more administrative duties with less time to do so. We also detected associations between type of site and region on changes to clinical hours. This may reflect variations in employment models, funding streams, and institutional priorities.19
One of the problems with establishing the floor on protected time, rather than capping the clinical time, is that there is wide variability among institutions (and EDs) as to what is considered 1.0 FTE. Although hour ranges are not explicitly detailed in the literature, institutional definitions of an FTE have been noted to vary from 40 to ≈ 60 hours/week based on individual operational needs and expectations. Emergency departments also vary in what is considered a clinical FTE, 32 vs 36 hours/week.22-24 With this lack of standardization, the change in the protected time requirement left room for interpretation by organizational, institutional, and departmental leadership to mean that the minimum requirement is the only amount of time necessary for core faculty activities.
LIMITATIONS
This survey-based study was subject to sampling and response bias with those most engaged in educational programming or most impacted by the ACGME changes potentially being more likely to respond. Future surveys of EM core faculty could be strengthened by systematic assessment of potential non-response bias. While our participants only represent a fraction of the total number of core faculty in EM, they do appear to parallel specialty educator demographics.25-28 Our data cover a broad crosssection of program characteristics; however, the sample may not be completely representative of the whole.
CONCLUSION
This study highlights potential concerns about the impact of the changed ACGME requirements for core faculty support on the educational environment for EM residency training. Additional work will be needed to track temporal trends, the potential for disproportionate impact among faculty members and programs, the effect on the learning environment, and the quality of residency training.
Address for Correspondence: Jaime Jordan, MD, MAEd, David Geffen School of Medicine at UCLA, Department of Emergency Medicine, 1100 Glendon Avenue, Suite 1200, Los Angeles, CA 90024. Email: jaimejordanmd@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Jordan et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Reznek MA, Scheulen JJ, Harbertson CA, et al. Contributions of academic emergency medicine programs to U.S. health care: summary of the AAAEM-AACEM benchmarking data. Acad Emerg Med. 2018;25(4):444-52.
2. Reznek MA, Michael SS, Harbertson CA, et al. Clinical operations of academic versus non-academic emergency departments: a descriptive comparison of two large emergency department operations surveys. BMC Emerg Med. 2019;19(1):72.
3. Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency). 2023. Available at: https://www. acgme.org/globalassets/pfassets/programrequirements/ cprresidency_2023.pdf. Accessed February 7, 2025.
4. Yarris LM, Juve AM, Artino AR Jr, et al. Expertise, time, money, mentoring, and reward: systemic barriers that limit education
researcher productivity-proceedings from the AAMC GEA Workshop. J Grad Med Educ. 2014;6(3):430-6.
5. Greenberger SM, Finnell JT 2nd, Chang BP, et al. Changes to the ACGME Common Program Requirements and their potential impact on emergency medicine core faculty protected time. AEM Educ Train 2020;4(3):244-53.
6. Yuan CM, Young BY, Watson MA, et al. Programmed to fail: the decline of protected time for training program administration. J Grad Med Educ. 2023;15(5):532-5.
7. Duffy TP. The Flexner Report--100 years later. Yale J Biol Med 2011;84(3):269-76.
8. Gunderman RB. The perils of paying academic physicians according to the clinical revenue they generate. Med Sci Monit 2004;10(2):RA15-20.
9. Jarrett JB, Griesbach S, Theobald M, et al. Nonclinical time for family medicine residency faculty: national survey results. PRiMER 2021;5:45.
10. Accreditation Council for Graduate Medical Education. Data Resource Book. 2022-2023 Available at: https://www.acgme.org/ about/publications-and-resources/graduate-medical-education-dataresource-book/. Accessed February 7, 2025.
11. Rickards G, Magee C, Artino AR. You can’t fix by analysis what you’ve spoiled by design: developing survey instruments and collecting validity evidence. J Grad Med Educ. 2012;4(4):407–10.
12. Lincoln YS, Lynham SA, Guba EG. Paradigmatic controversies, contradictions, and emerging confluences, revisited. Sage Handbook Qualitat Res. 2011;4:97‐128.
13. Terry G, Hayfield N, Clarke V, et al. Thematic analysis. In: The SAGE Handbook of Qualitative Research in Psychology. Thousand Oaks, CA: SAGE Publications Ltd.; 2017:17‐37.
14. Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42:1758‐1772.
15. Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Emergency Medicine. 2023. Available at: https://www.acgme.org/ globalassets/pfassets/programrequirements/110_ emergencymedicine_2023.pdf. Accessed February 7, 2025.
16. Bennett CL, Ling AY, Agrawal P, et al. How we compare: Society for Academic Emergency Medicine faculty membership demographics. AEM Educ Train. 2022;6(Suppl 1):S93-6.
17. Gaeta TJ, Ankel FK, Calderon Y, et al. American Board of Emergency Medicine Report on Residency and Fellowship Training Information (2023-2024). Ann Emerg Med. 2024;84(1):65-81.
18. Jordan J, Hwang M, Kaji AH, et al. Scholarly Tracks in emergency medicine residency programs are associated with increased choice of academic career. West J Emerg Med. 2018;19(3):593-9.
19. Adelman L. 2023 State of the emergency medicine employer market. 2023. Available at: https://assets.ivyclinicians.io/content/2023%20 State%20of%20the%20EM%20Employer%20Market_Ivy%20 Clinicians.pdf. Accessed February 7, 2025.
20. Li K, Al-Amin M, Rosko MD. Early financial impact of the COVID-19
pandemic on U.S. hospitals. J Healthc Manag. 2023;68(4):268-283.
21. Gottlieb M, Sebok-Syer SS, Bawden A, et al “Faces on a screen”: a qualitative study of the virtual and in-person conference experience. AEM Educ Train. 2022;6(6):e10827.
22. Moorhead JC, Gallery ME, Hirshkorn C, et al. A study of the workforce in emergency medicine: 1999. Ann Emerg Med. 2002;40(1):3-15.
23. Nurok M, Flynn BC, Pineton de Chambrun M, et al. A review and discussion of full-time equivalency and appropriate compensation models for an adult intensivist in the United States across various base specialties. Crit Care Explor. 2024;6(4):e1064.
24. Medscape. Your income vs your peers’: medscape emergency medicine physician compensation report 2023. Available at: https:// www.medscape.com/slideshow/2023-compensation-emergencymedicine-6016356?icd=login_success_gg_match_norm. Accessed
February7, 2025.
25. Jordan J, Coates WC, Clarke S, et al. Exploring scholarship and the emergency medicine educator: a workforce study. West J Emerg Med. 2017; 18(1):63-8.
26. Golden A, Diller D, Riddell J, et al. A workforce study of emergency medicine medical education fellowship directors: describing roles, responsibilities, support, and priorities. AEM Educ Train. 2022; 6(5):e10799.
27. Coates WC, Gill AM, Jordan R. Emergency medicine clerkship directors: defining the characteristics of the workforce. Ann Emerg Med. 2005; 45(3):262-8.
28. Beeson MS, Gerson LW, Weigand JV, et al. Characteristics of emergency medicine program directors. Acad Emerg Med. 2006; 13(2):166-72.
Building Connection and Resident Understanding of Local Resources Through Community Engagement
Hannah Johnshoy, MD*
Ashley Pavlic, MD, MA*
Sehr Khan, MD*
Taylor Sonnenberg, MD, MSGH*
Section Editor: Jeffrey Druck, MD
Medical College of Wisconsin, Department of Emergency Medicine, Hub for Collaborative Medicine, Milwaukee, Wisconsin
Submission history: Submitted October 31, 2024; Revision received May 2, 2025; Accepted June 1, 2025. Electronically published September 1, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.39647
Introduction: Throughout graduate medical education (GME), it is crucial for learners to not only develop the skills necessary to manage a wide variety of medical conditions, but also to foster personal development and to gain a deeper understanding of the complex and multifaceted needs of our patients. We often refer patients to community sites to address needs such as homelessness, hunger, and domestic violence; however, we frequently make these referrals with only a superficial understanding of what each resource entails.
Methods: To address this issue, our department integrated a two-day Community Engagement Retreat into our curriculum. Twenty-two first-year residents participated in small group visits to three or four community organizations. There, residents engaged with community workers and the public to learn about the services each program offers. This was followed by a session of focused reflection and discussion on how to integrate this new knowledge into our care for patients in the emergency department. At the conclusion of the experience, residents completed an anonymous survey with a response rate of 77.3%.
Results: The results suggest that participants found the sessions highly useful, with 98.6% of residents reporting that they “agreed” or “strongly agreed” that the experiences at the community sites would better allow them to care for patients. They further stated that the program was one of the most impactful elements of their training and highly recommended it to future learners.
Conclusion: This initiative demonstrates the importance and utility of a novel, structured community engagement to begin to address this deficiency in GME and improve patient care. [West J Emerg Med. 2025;26(5)1170–1173.]
INTRODUCTION
Graduate medical education (GME) is a time of significant growth and challenges for emergency medicine (EM) residents. While most programs do an excellent job teaching procedural skills and pathophysiology of disease, we are becoming increasingly aware of the role the social determinants of health (SDoH) play in the varying presentations of our patients.1 Importantly, many residents feel this is not well covered in their programs.2
The emergency department (ED) is frequently referred to as the “safety net” of the healthcare system.3 The SDoH concerns
of domestic violence, homelessness, mental illness, and poverty frequently converge to influence our patients’ complex presentations to the ED.1,4 For example, one study found that 23.5% of respondents said they went to an ED as a “first-stop” site after becoming homeless.5 Intervening on SDoH in our patients is vital to providing optimal care,1,6,7 and we commonly find ourselves referring our patients to community services for this support. However, we often make these referrals without fully understanding these services ourselves, limiting our ability to select appropriate resources and to properly counsel our patients. While team members like social workers can be
helpful in bridging this gap, they are not always available. Having a general understanding of the resources available in our city to address our patients’ varying SDoH needs is a crucial component of providing complete care, as well as developing our own ability to have professional, compassionate discussions about these issues with them.7
In this paper, we describe a focused community engagement retreat for first-year EM residents and evaluate its feasibility and their reception of it. The goal in establishing this retreat was to educate residents on how to address SDoH with their patients, which has been noted as a gap in EM residency training; the retreat was tailored to the community that the EM residents are serving, an important consideration in the design of these types of experiences.2,7
METHODS
This retreat was provided for residents within an academic EM program that trains 12 residents per year and serves a major metropolitan area in the Midwest. The retreat was structured to give each resident an opportunity to experience several different community sites. Facilitators reviewed resources commonly used in our area and arranged for small group tours and informational sessions. The retreat was targeted toward first- year EM residents and occurred on the first Wednesday in October of their intern year. The resident class was excused from clinical duties for two days to participate in the retreat and follow-up discussion.
Residents toured three or four organizations known to be used by patients who are seen in our ED, chosen by faculty members who created this experience, mostly leveraging existing relationships. This included groups addressing food insecurity, domestic violence, emergency mental health service, and homelessness (see Table). Residents visited the sites in groups of 4-6. While at the site, residents engaged with community workers and members of the public to learn about the services offered at that location and the population they serve. The day typically included a tour of the facility, informational sessions with managers, and occasionally
Table. Organizations visited by first-year emergency medicine residents during their community engagement day.
1. Treatment center focusing on substance use disorder
2. Shelter for those experiencing homelessness and/or domestic violence
3. County program for mental health
4. Shelter for those experiencing homelessness
5. Mental health emergency department
6. Organization for food insecurity
7. Organization providing resources to those who are unhoused
8. Organization providing services to veterans with mental health disorders
Population Health Research Capsule
What do we already know about this issue?
While interventions targeting social determinants of health enhance patient care, residency programs lack sufficient training on their practical application.
What was the research question?
We examined the feasibility of a community engagement retreat for emergency medicine (EM) residents.
What was the major finding of the study?
98.6% of respondents reported improved understanding of resources, patient experience, and care capabilities.
How does this improve population health? Community engagement retreats enhance EM residency programs, leading to improved patient outcomes by integrating social determinants of health.
hands-on participation such as assistance with preparing meals, outreach, or a walk-through of the intake process. Residents spent an average of 2-3 hours at each site.
The site visits were followed by a two-hour session of small-group reflection and discussion between residents and facilitators to process, discuss, and share experiences. In this way, all residents were able to learn about all sites. At the end of the experience, we asked residents to complete an anonymous, voluntary survey that included a Likert scale, which asked residents about their understanding of each community resource and their comfort level in discussing it with patients after touring. The survey also asked for their free-text takeaways from the experience, and their free-text suggestions for improvement. The two faculty members who created the retreat also designed the unpiloted survey (see Figure). So far, two years of survey data have been completed and aggregated to provide overall data. Participating residents were asked about each of the community organizations that they visited. Additionally, qualitative data and quotes were collected from residents in the anonymous surveys to better characterize residents’ views of the retreat. The responses were reviewed and summarized, and representative comments by consensus of all the authors. This project was submitted to our institutional review board (IRB) and determined to be an internal institutional quality improvement project that did not
need IRB approval.
RESULTS
Of 12 residents, 11 participated in the retreat in 2021, and 11 of 12 residents participated in 2023. Seventeen residents (77.3%) responded to the survey. We collected 74 responses about eight community organizations. Feedback from participants was overall extremely positive. Of residents surveyed, 98.6% agreed or strongly agreed that they felt more familiar with resources available, had a deeper understanding of the experiences of the people who use these resources, and felt that they were able to provide better care to patients in the ED after participation in the community engagement retreat (Figure).
The specific quotes provided by residents provided more insight into their experience. In the open response section of the surveys, residents stated that this was one of the most impactful parts of their training and noted that it enhanced their ability to provide better patient care in the ED. One resident said “it was an absolutely fantastic experience—every class in the future should do this.” Another echoed this sentiment:
[It was an] incredible experience. I learned so much about our community and the resources available. Would highly recommend to future classes.
Indeed, the belief by current residents that this retreat should be offered annually was reflected in much of the feedback we received. The overwhelming majority of participants felt that their understanding of the different resources had improved greatly and indicated they felt more confident discussing these resources with patients. Additionally, residents felt that they were better able to not only understand the resources, but also the people who used them. “[I learned the importance of] meeting patients where they are at,” said one resident, after their tour of a homeless outreach center. Another resident noted: “[I] will be more aware of my own implicit biases” after this retreat. One resident noted improved empathy for patients experiencing homelessness.
DISCUSSION
This is an initial evaluation seeking to address the feasibility of and response to a focused community engagement retreat for first-year EM residents. Initial results suggest that residents did indeed find this retreat to be useful in terms of improving their ability to address the SDoH while on shift in the ED. Discussions revealed that residents felt that their experiences allow for improved rapport with patients and increased confidence in initiating discussions regarding SDoH with them. They discussed that the deeper understanding they acquired of the challenges faced by patients helped them to better meet patients at the point where they were in their journeys. This type of experience can also strengthen partnerships between programs and the community organizations to work together to help patients
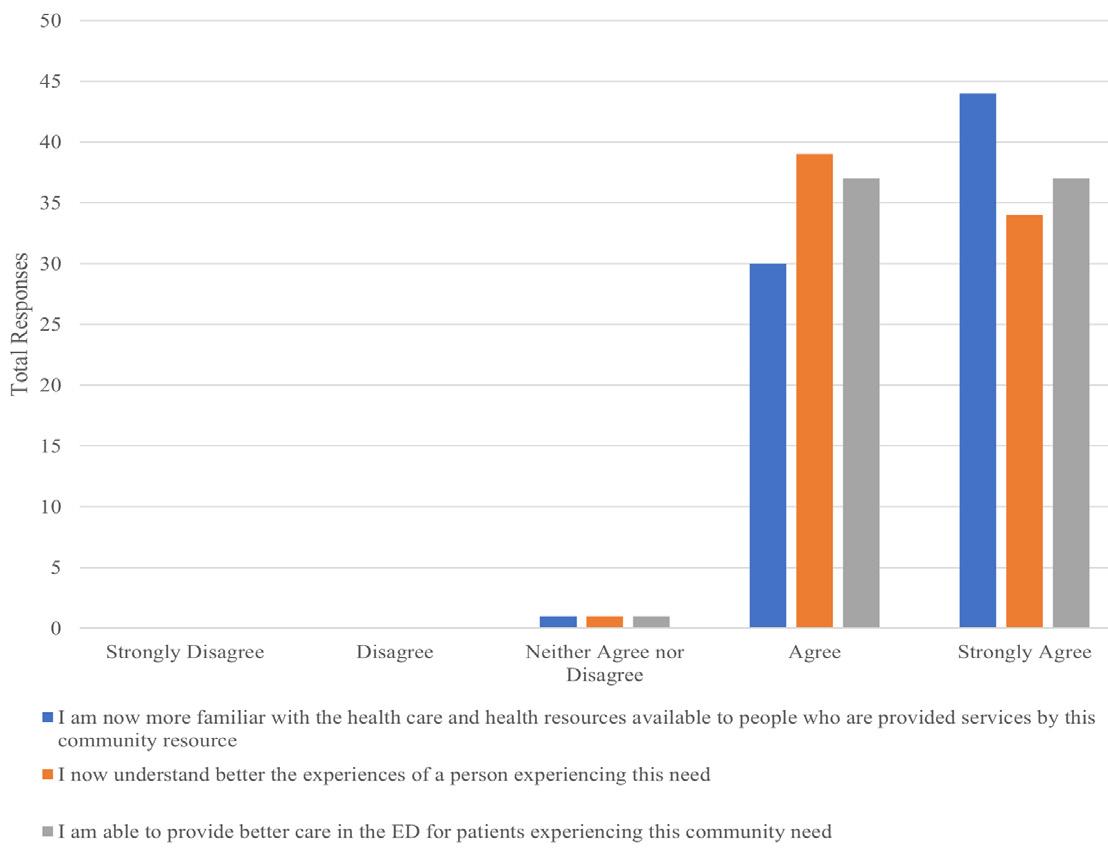
Figure. Combined feedback from first-year emergency medicine residents on five separate community site visits they made on Community Engagement Day 2021 and 2023. ED, emergency department.
affected by SDoH.
This is a unique program for EM residents. A recent review found only 12 studies on SDoH in GME curricula— many including community site visits—but none included EM reidency programs.2 A program like this would likely also be beneficial to other residency programs and could be adjusted to include different relevant facilities. However, care would need to be taken not to dilute the intimate small-group nature of the tours that was so highly praised by residents.
LIMITATIONS
One of the most significant limitations to this study is the small dataset and limited sample size. We implemented this intervention in one EM program in the Midwest with only 22 residents. We currently have two years of data, and we plan to have future classes participate in the program to strengthen the quality of data collected. Additionally, there had been data regarding residents’ confidence in providing community resources before the intervention. Finally, we believe that the true benefits of this program can best be appreciated in the qualitative data, which can be more challenging to analyze objectively than quantitative data. Future studies could evaluate the knowledge gained from this experience months after the retreat to better understand whether residents are incorporating their new-found knowledge into their clinical practice.
CONCLUSION
Integrating social emergency medicine into daily practice is now recognized as a crucial component of providing highquality care to our patients, but it is often overlooked in graduate medical education. In our study, residents reported that
the dedicated time they spent to learn about and engage with their community promoted a deeper understanding of local resources and increased their confidence in integrating social determinants of health into their care of patients in the ED. The program is still in its early years; however, based on the positive feedback thus far, it continues as an annual event for our first-year EM residents. We believe it could likely be adapted to most EM residency programs.
Address for Correspondence: Taylor Sonnenberg, MD, MSGH, Medical College of Wisconsin, Department of Emergency Medicine, Hub for Collaborative Medicine, 8701 Watertown Plank Rd, Milwaukee, WI 53226. Email: tsonnenberg@mcw.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Johnshoy et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFER ENCES
1. Axelson DJ, Stull MJ, Coates WC. Social determinants of health: a missing link in emergency medicine training. AEM Educ Train 2018;2:66‐8.
2. Hunter K, Thomson B. A scoping review of social determinants of health curricula in post-graduate medical education. Can Med Educ J. 2019;10(3):e61-71.
3. Gordon JA. The hospital emergency department as a social welfare institution. Ann of Emerg Med. 1999;33(3):321-5.
4. Molina MF, Li CN, Manchanda EC, et al. Prevalence of emergency department social risk and social needs. West J Emerg Med 2020;21(6):152-161.
5. O’Toole TP, Conde-Martel A., Gibbon JL, et al. Where do people go when they first become homeless? A survey of homeless adults in the USA. Health Soc Care Community. 2007;15(5):446-53.
6. National Academies of Sciences, Engineering, and Medicine. [Introduction.] In [National Academies of Sciences, Engineering, and Medicine (Eds.), A Framework for Educating Health Professionals to Address the Social Determinants of Health. (19-32). Washington DC: National Academies Press; 2016.
7. Anderson E, Lippert S, Newberry J, et al. Addressing social determinants of health from the emergency department through social emergency medicine. West J Emerg Med 2016;17:487–9.
Johnshoy
Accuracy of Triage Nurses in Predicting Patient Admissions: Retrospective,
Calvin Armstrong, BSc*
David Kanter-Eivin, BArtsSc*
Michaela Dowling, BMSc*
Grant Sweeny, BArtsSc*
Asil El Galad, BMSc*
Anil Esleben, BSc*
Large-sample Evidence from a Community Emergency Department
* † ‡
McMaster University, Michael G. DeGroote School of Medicine, Hamilton, Ontario, Canada
Niagara Health, Ontario, Canada
McMaster University, Division of Emergency Medicine, Department of Family Medicine, Faculty of Health Sciences, Hamilton, Ontario, Canada
Nanda Krishna Duggirala, PharmD, CHIM†
Corrine Mitges RN, MSc‡
Shauna Speck RN, MBA(c)†
Stephenson Strobel MD, PhD†‡
Section Editor: Tehreem Rehman, MD, MPH
Submission history: Submitted November 19, 2024; Revision received April 20, 2025; Accepted April 28, 2025
Electronically published September 1, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.39947
Introduction: Emergency department (ED) flow could be improved with quicker disposition decisions. One possible way to expedite decisions is for triage nurses to make predictions about whether patients require admission to hospital. The information contained in these predictions could be useful for disposition planning and for physician decision-making. Previous studies made use of prospective designs that introduced Hawthorne effects and have demonstrated mixed evidence on whether triage nurse predictions are accurate. We examined the accuracy of triage nurse predictions for patient admission in an ED in southeastern Ontario.
Methods: We examined a retrospective sample of 134,891 visits to an ED in Ontario from March 2019 – July 2024. Triage nurses made predictions about admission to hospital for these visits, from which we estimated measures of specificity, sensitivity, positive predictive value, negative predictive value, accuracy, and F1 scores.
Results: Of 134,891 visits, 13.7% resulted in hospital admission. We found the accuracy of the nurses in predicting admission to be 85.8% (95% confidence interval [CI] 85.7 - 86.1), while overall sensitivity was 36.6% (95% CI 35.9 - 37.3) and specificity was 93.7% (95% CI 93.5 - 93.8). The positive predictive value of admission was 47.9% (95% CI 47.1 - 48.7), and the negative predictive value of admission was 90.3% (95% CI 90.1 - 90.5). F1 scores were 0.415. These results were relatively stable over time, although there was notable variation in prediction ability between nurses. We also report that some presenting conditions lead to relatively higher prediction accuracy than others and that as overall case severity increases, sensitivity increases and specificity decreases.
Conclusion: These results suggest that although nursing staff predictions are insufficient to streamline disposition decisions completely, they could be useful in expediting certain decisions related to hospital admission and resource requirement, thereby improving flow in EDs. [West J Emerg Med. 2025;26(5)1174–1182.]
INTRODUCTION
Emergency departments (ED) face prolonged patient wait times and crowding due to limited resources. Despite goals of reducing wait times, patients in the province of Ontario, Canada, waited an average of 30 minutes longer in 2022/2023 than in 2013/2014—up to an average of 118 minutes—to see an emergency physician.1 In the United States, only a minority of hospitals consistently achieve recommended wait times for all patients,2 although this has improved over time.3 Extended ED wait times lead to patient dissatisfaction,4 patients leaving without being seen by a physician,1 poorer outcomes, and higher resource use per admission to hospital.5 Crowding has also been linked to increased patient mortality.6–8
A key challenge to improving ED wait times and crowding is flow: how can clinicians make quick yet accurate decisions about disposition of patients to hospital or discharge? Quicker disposition means freeing up resources such as beds and monitoring staff for other ED patients.9 However, disposition decisions require the emergency physician’s time, which is one of the most scarce resources in an ED. One possible solution is to leverage the skill of triage nurses in identifying patients who require more involved care.10 Using triage nurses to predict whether patients require admission could streamline resources toward high-risk patients, alert specialist physicians to patients who might require hospital care, and provide emergency physicians quick information to make quicker disposition decisions.
The success of this solution depends on ED nurses’ ability to make accurate predictions about patient disposition. Previous literature highlights notable variability in the accuracy of nursing predictions. Several studies report an accuracy rate of 70% or higher for predicting patient disposition or outcome, with nearly 90% accuracy for predicting patient discharge.11–13 Other research contradicts these findings, with one study demonstrating inappropriate patient triaging in >40% of patient presentations.14 There is also variability regarding the factors that influence nurses’ prediction accuracy. Some studies demonstrate a positive correlation between nurse experience and predictive capability,15 while others do not.11,16 Certain patient characteristics, including age and severity of presentation, have been correlated with high predictive accuracy, although other literature has failed to replicate these findings.12,13
Most existing studies on nurse prediction rely on prospective designs, which limit sample size and make predictions prone to Hawthorne effects where subjects of studies change their behavior because they are being observed.17 In contrast, we examined an ED operations change that required triage nurses to predict whether a patient required admission to facilitate earlier involvement of allied health. Our study makes two key contributions to the literature: 1) unlike prospective research, our results better reflect real-world conditions, providing evidence on how triage nurses predict “in the wild” when they do not think they
Population Health Research Capsule
What do we already know about this issue? Previous literature has reported conflicting evidence about the ability of emergency department (ED) triage nurses to predict patient admission requirement.
What was the research question? Can triage nurses accurately predict patient hospital admissions in a realworld, community ED?
What was the major finding of the study? Nurse prediction accuracy was 85.8% (95% CI 85.7 - 86.1), with sensitivity 36.6%, specificity 93.7%, and F1 score 0.415.
How does this improve population health?
Triage nurse predictions may help fasttrack care for certain patients, reducing ED delays and optimizing hospital resource use.
are being studied; and 2) by leveraging a large set of highquality administrative data, we were able to explore the nuances of triage nurse predictions. This enabled us to examine heterogeneity in prediction accuracy by patient type and other important characteristics. Our study adds to the literature on nurses’ predictive capabilities and to a smaller body of literature examining the heterogeneity in prediction by nurse and patient type.
MATERIALS AND METHODS Study Design
This was a retrospective cohort study that used administrative health data collected during March 2019 - July 2024.
Setting
We conducted the study using data from a community ED within the Niagara Health system in southeastern Ontario. This site sees 80 - 100 patients per day and 30,000 - 40,000 visits per year. The ED has approximately 20 - 30 regular nurses who are able to triage.
As part of a quality improvement (QI) initiative, triage nurses were asked to indicate within the electronic health record (EHR) system if they believed a patient would require hospital admission. Predictions began as a QI initiative to reduce potential admission time. Triage nurses flagged patients
whom they thought would be admitted so that allied healthcare like occupational therapy and discharge planning would quickly see patients who likely needed their services. Triage nurses received no specific training. For each triaged patient an additional question, “predicted admission y/n,” was added to the triaging screen after the nurse recorded the patient’s past medical history. Prediction could not be routinely bypassed except for rapidly evolving emergencies or when the EHR was down for maintenance. There were also exceptions for agency nurses who had not been hired fulltime. For these situations nurses could triage by paper and a prediction was not entered into the EHR.
This administrative data allowed us to measure admission outcomes and define surrogates for admissions to test how accurate nurses are at predicting. Specifically, in our primary outcome, we included the following as an admission:
1. Any admission to the hospital at the time of the index ED visit
2. Transfers to alternate hospitals
3. Deaths in the ED.
We also considered patients who returned to the ED for any reason within 30 days and subsequently required admission (or met one of the above criteria) as “admissions” for the purpose of evaluating prediction accuracy. Using this surrogate, we attempted to measure inappropriate discharges (i.e., patients who should have been admitted but were not) by the physician at the index visit. Our rationale for this broad, 30 - day window was that even if the return visit was for a seemingly unrelated issue, the need for admission indicated a potential clinical necessity that might not have been fully recognized at the initial presentation.
Outcome Measures
Our main measure of interest was the accuracy of a nurse predicting admission to hospital. We measured this by estimating sensitivity (1) and specificity (2) of admissions predictions.18 These are defined as
Sensitivity (TPR) = TP TP+FN (1) and
Specificity (TNR) = TN TN+FP (2)
We also provided estimates for (3) positive predictive value and (4) negative predictive value defined as
Positive Predictive Value (PPV) = TP TP+FP (3) and Negative Predictive Value (NPV) = TN TP+FN (4)
We treated the emergency physician’s decision to admit as the reference standard, supplemented by the admission surrogates noted above. The components of these measures
were as follows:
• True positives (TP): Patients predicted to need admission who are admitted, transferred, die in the ED, or return to the ED within 30 days (for any reason) and met one of these criteria.
• False negatives (FN): Patients predicted not to need admission but who were admitted, transferred, died in the ED, or returned to the ED within 30 days (for any reason) and met one of these criteria.
• True negatives (TN): Patients predicted not to need admission and who did not meet any of the above criteria at the index visit or within 30 days.
• False positives (FP): Patients predicted to need admission but did not meet any of the above criteria and did not return within 30 days requiring admission.
We also evaluate overall accuracy, defined as
Finally, because substantially more patients are discharged than admitted, we also calculated the F1 score, which balances sensitivity (recall) and positive predictive value (precision). This is commonly used in machine-learning and is useful in settings with imbalanced outcomes,19 such as ED visits where admissions are less common. The F1 score is determined by the following calculation:
F1 scores below 0.5 are considered poor, and scores between 0.5 and 0.8 are considered average.
Additional Analyses
We also estimated a prediction compliance rate as the number of predictions that are recorded over the total number of patients. We provided several extensions of our headline measurements of compliance, namely specificity, sensitivity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and F1 score. First, we examined how stable these outcomes have been over the period of observation, to see whether predictions vary with familiarity. Second, we examined the inter-nurse variation in predictions to check whether some nurses predict better than others. Finally, we examined whether prediction outcomes varied by a patient’s assigned triage acuity score and patient complaint. The former variable, the Canadian Triage and Acuity Scale (CTAS), is a computer-calculated measurement of the patient’s requirement for acute resources and corresponds to sickness of the patient.20 The CTAS categories correspond to a scale of 1-5, specifically resuscitation (1), emergent (2), urgent (3), less urgent (4), and non-urgent visits (5).
Finally, To examine how our definition of “admission” (which includes 30-day readmissions for any reason) impacts
our results, we also perform a sensitivity analysis that alters the outcome so that it only 1) includes seven-day readmissions, 2) one day readmissions and 3) excludes these return admissions entirely (i.e., only includes the index visit).
Inclusion and Exclusion Criteria
We made two data restrictions when examining prediction heterogeneity to avoid small sample sizes. For inter-nurse prediction, we only included nurses who registered ≥ 50 predictions over the study period. Our examination of nurse heterogeneity was also restricted to the period of January 2020 – July 2024, as we did not have information on which nurses made predictions prior to this. For examination of presenting complaints, we only included predictions for complaints that appeared at least 100 times throughout the study period.
Data Analysis
Analysis was performed with Stata 18 (StataCorp, LLC, College Station, TX). For our overall parameters of sensitivity, specificity, positive predictive value and negative predictive value, we provide a 95% confidence interval (CI) that is based on a two-sided test.
Ethics Approval
Ethics approval was obtained through the Hamilton Integrated Research Ethics Board under project number 17330.
RESULTS
During the study period of March 2019 – July 2024, 162,392 visits occurred at the ED. Triage nurses provided disposition predictions for 134,891 visits for an overall compliance rate of 83%. Of these visits, 16,022 resulted in admission to the hospital. Nurses correctly predicted 6,764 admissions (TP) but missed 11,700 admissions (FN), resulting in an overall sensitivity of 36.6% (95% CI 35.9 - 37.3). Additionally, triage nurses accurately predicted that 109,067 visits would not result in an admission (TN), while 7,360 visits that they predicted as admissions did not result in hospitalization (FP), yielding a specificity of 93.7% (95% CI 93.5 - 93.8). These findings correspond to positive and negative predictive values of 47.9% (95% CI 47.1 - 48.7) and 90.3% (95% CI: 90.1, 90.5), respectively. The nurses’ overall accuracy during the period of observation was 85.8% (95% CI
85.7 - 86.1). The F1 score of predictions was 0.415. Our checks on whether our outcomes of interest changed appreciably by altering outcome definition are summarized in Table 1. We found little evidence that they were affected by changes to inclusion of bouncebacks to ED. Figure 1 illustrates the stability of each of these outcomes over time. Compliance varied from a minimum monthly average of 63% in September 2023 to a peak of 94% in September 2021. Sensitivity also varied from a minimum of 28% in December 2021 to a maximum of 53% in April 2019. Relatively low PPV was observed across the period with an exception where it spiked to 71% in late 2022. There is, however, consistently high NPV observed over time. Specificity and accuracy were more stable over time, showing less variation in contrast to compliance or sensitivity. This stability is reflective of the high prevalence of patients who are not admitted to hospital. The relatively modest F1 score we estimated also reflects this and reflects poor sensitivity of nurse predictions. The exception to this pattern is that sensitivity was relatively high in the first month of prediction before it stabilized at a much lower baseline value in subsequent months.
In line with our observations across time, compliance and specificity were similar across nurses (Figure 2). The lowest non-outlier compliance rates were ≈ 90%, indicating that non-compliance was concentrated in a minority of outlier nurses. Specificity also remained consistently high across most nurses in our sample with the lowest prediction specificity for a nurse being 84%. However, there was considerable variation in the sensitivities of nurse predictions, which ranged from 0 - 100%. This resulted in most nurses having prediction accuracies between 77 - 97%. Negative predictive values had a limited range between 82100% whereas PPVs ranged between 18 - 91%. Nurse F1 scores ranged from 0 - 0.77.
We found that predictive abilities also varied by patient type (Figure 3). We first examined nurses’ prediction accuracy by patient triage score. Nurses had a reduced compliance of 52% in making predictions for very sick patients, classified as CTAS 1, likely because some of these patients were paper triaged and predictions were not entered into the administrative data. For those patients who did not have resuscitation-level presentations, which includes CTAS 2 - 4, nurses predicted admission probability for ≈ 80% of all visits. Among those patients who received a prediction, we found a positive correlation between
Table 1. Estimates of outcomes of interest by changing bounceback criteria.
Figure 1. Time series of outcomes of interest over the period of observation.
PPV, positive predictive value; NPV, negative predictive value.
triage score severity and sensitivity, and a negative correlation between triage score severity and specificity. Higher triage severity and need for emergency resources means higher sensitivity and lower specificity. This resulted in a positive correlation between triage score and prediction accuracy and a negative correlation between triage score and F1 score.
We found that most conditions had high prediction specificity and corresponding low sensitivities (Supplemental Table 1). However, some conditions had comparatively high sensitivities as compared to other complaints. This included a cluster of complaints that related to altered levels of consciousness, confusion, bizarre behavior, and social- and patient-welfare concerns. Prediction accuracy was relatively high in a set of conditions that corresponded to low overall
probability of hospital admission, such as bites and foreign bodies to the eye (Table 2). However, F1 scores were consistently poor with only the top 13 complaints demonstrating scores that could be considered average in terms of prediction. All remaining patient complaints had F1 scores that would be considered poor (Table 2).
DISCUSSION
We estimated the sensitivity, specificity, PPV, NPV, accuracy, and the F1 score of triage nurses at an ED in the province of Ontario, Canada, to assess how effectively they predicted patient admission to hospital. Our contribution to the literature is twofold: 1) these estimates were not contaminated by Hawthorne effects, which are characteristic of previous prospective studies; and 2) we used a much larger data sample than previous studies. This allowed us to provide evidence on temporal, nurse, and patient heterogeneity in predictions.
We observed that this sample of nurses achieved reasonably high prediction accuracy for hospital admissions. Prediction accuracy was 85.8% and relatively stable over the entire period that we examined. However, the estimated F1-score was 0.415, which is poor and due to the relatively low sensitivity and PPV of predictions. Thus, high accuracy is predicated on a relatively high specificity among a group of patients that are more likely to be discharged from hospital. This high specificity is also possibly grounded in the relatively large numbers of nonemergent presentations (i.e., CTAS 5 - 3). Performance in predicting admissions to hospital was more modest, with sensitivities of 30-40%.
There are several explanations for this modest sensitivity. Triage nurses, as the point of first contact, have much less information to base predictions upon relative to other healthcare
Figure 2. Variation in outcomes of interest across nurses. The center white line represents the median value; the edges of the box represent the 25th and 75th percentiles; and the whiskers indicate the upper and lower adjacent values. Estimates exclude values outside these adjacent values.
PPV, positive predictive value; NPV, negative predictive value.
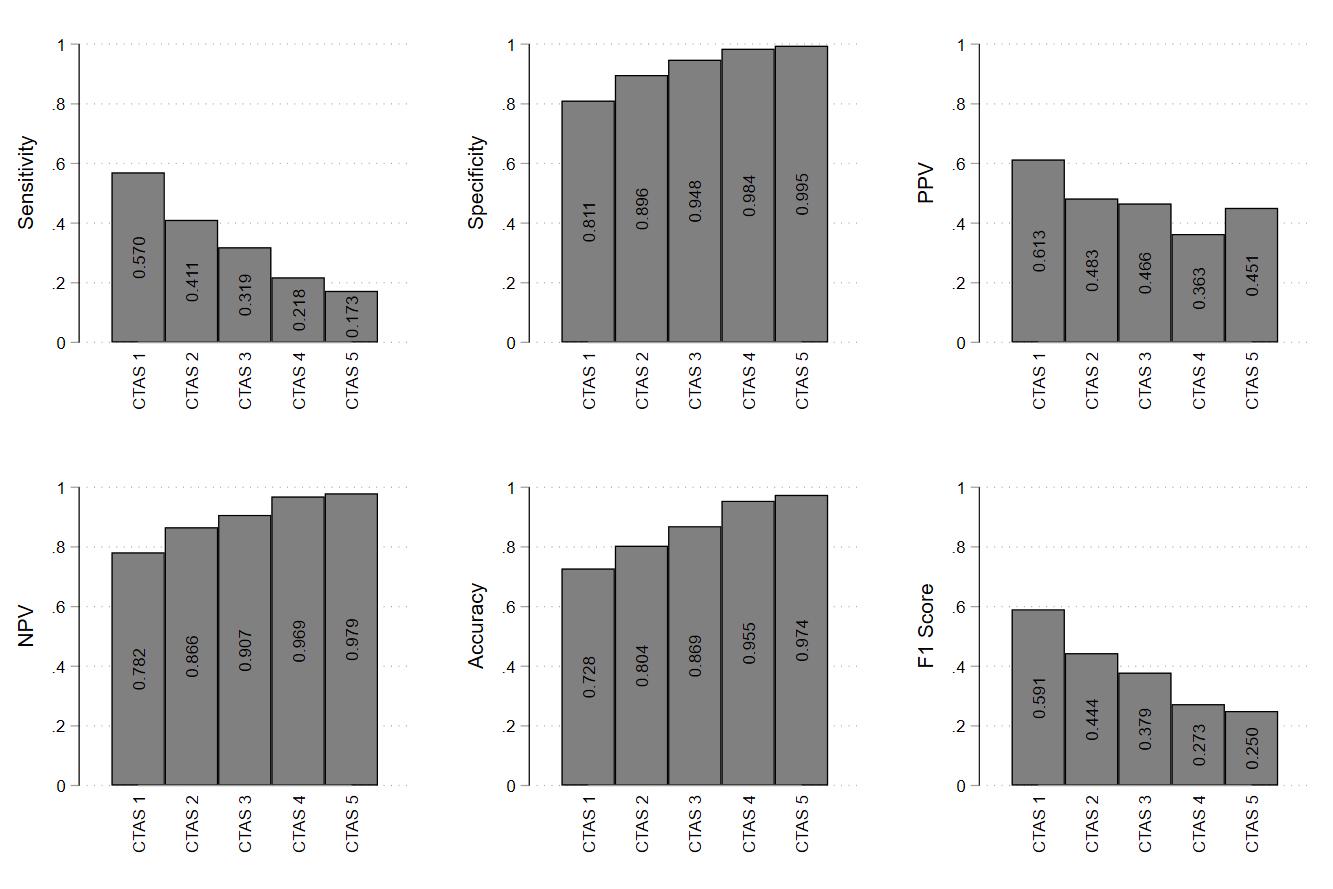
Figure 3. Outcomes of interest by triage scores. Canadian Triage and Acuity Scale scores range from 1-5: resuscitation (1), emergent (2), urgent (3), less urgent (4), and non-urgent visits (5). CTAS, Canadian Triage and Acuity Scale; PPV, positive predictive value; NPV, negative predictive value.
professionals in the ED. Prediction accuracy might improve if made by bedside nurses, who are able to use initial investigations and conduct a more involved physical exam. Another possibility is unfamiliarity with predictions. However, our accuracy results were stable over time, suggesting that nurses did not learn to improve their predictions with increased prediction practice. Feedback, training, and stakes may also be important to improve prediction sensitivity, but were absent in our setting. On this last point, predictions had no immediate impact on care within the ED and were largely supposed to improve inpatient care. Similarly, incentivization, also absent in our setting, has been demonstrated to improve performance in similar tasks.22 However, poor sensitivity may be more of a general issue in ED care than one specific to triage nurses. Even highly trained physicians only predict patient outcomes with equivocal, or only slightly greater ability.2
Our results, demonstrating that nurses had low sensitivity/ high specificity and high NPV/low PPV, have implications for ED operations. High specificity and low PPV suggest the potential for over-triage, where nurses predict admission for patients who do not require admission. Where there is relatively low prevalence in need for admission, as in our setting, emergency physicians cannot necessarily trust a positive admission prediction from the nurse. Low sensitivity and high NPV suggest a simultaneous but opposite issue. Nurses are under-triaging and suggesting discharge for patients who should actually be admitted. In ED settings where admission is relatively rare, this may be useful in that most of the people the nurse identifies as not needing admission are probably safe for discharge. However, our results suggest that it is not reliably safe to trust the triage nurse’s discharge decision either.
Despite this paradoxical issue of simultaneous over- and under-triage and a poor F1 score for overall need for admission,
our exploration of prediction heterogeneity suggests that emergency physicians should pay attention to certain predictions. Triage nurses are accurate at predicting admission for presentations related to mental health concerns, altered levels of consciousness, confusion, bizarre behavior, and social- and patient- welfare concerns. These had relatively higher sensitivities and could be used to accelerate admission planning. The internurse variation we observed in our outcomes also suggests that particular nurses may be able to provide more accurate information to a physician about a patient’s discharge disposition, and so predictions from these nurses should be paid particular attention. Both these findings are novel and suggest nuance in understanding when to trust nursing admission predictions. It may be reasonable to delegate admission decisions for certain complaints and certain nurses under narrow circumstances. Our findings are consistent with prior literature that indicates nurses are not able to predict patient admission with sufficient sensitivity,10,14,23–26 and from an operations perspective suggests against the direct streamlining of patients to admission based on triage nurse predictions. This is contrary to some literature that suggests triage nurses may be able to achieve satisfactory levels of sensitivity to implement triage prediction programs.11–13,15,27–29 It is unclear what drives this difference between our results and those found in the literature, but there are likely multiple factors. Site-specific circumstances and the nursing staff’s experience may have played a role. We also highlight that most of the prior literature is prospective, and nurses knew they were being monitored. Monitoring may alter prediction behavior and improve sensitivity and rule-in performance, possibly accounting for some of the superior sensitivities reported in earlier studies.17 In support of this, we found some suggestive evidence of these Hawthorne effects. Sensitivity was much higher in our first month of observation when nurses were being told to produce predictions and the system was novel to them than in subsequent months.
Although triage nurses were unable to accurately predict patient admissions at our site, they had high NPV. This finding is consistent with previous literature, which demonstrates that triage nurses are better at predicting discharge.11–13,23,26,28,29 This suggests that triage nurses may be useful in identifying patients who are likely to be discharged quickly. Emergency clinicians can then take a second, more involved examination and admit those patients that triage nurses may have under-triaged. This is already done using ED “see-and-treat” areas where patients deemed to require lower levels of care are streamed. Such streaming could help to reduce congestion and improve workflow in acute-care sections where most patients have been deemed to require admission. A version of this concept was demonstrated by Derlet et al (1995) who reported the successful diversion of 18% of adult ambulatory visits over a five-year period. This led to reductions in ED waiting times, the number of patients who left without care, and complications resulting from delayed care.27 This also reduced costs without any deaths within 72 hours of patients being triaged.27
Finally, we found evidence that triage nurses predicted well at the extremes of the triage distribution, having higher sensitivities in patients with low triage scores and who were more likely to be admitted, and higher specificities in patients with high triage scores and who were more likely to be discharged. This is consistent with previous literature, which suggests that prediction accuracy increases at the extremes of case severity.12,13,23,25,28 While high and low admission rates for resuscitation and non-urgent triage scores, respectively, may make predicting dispositions easier, these categories only account for 5-9% of total ED visits.30,31 Of total visits, 45-60% are categorized as the middle category, or urgent, which are considerably less predictable, with admission rates of 28.249.4%.20,30,31 Our results on prediction accuracy by patient complaint reinforces this: triage nurses are most likely to accurately predict disposition among patients with complaints that are less likely to require admission to hospital. This result suggests that triage nurses may be most effective at making predictions when uncertainty is minimized.
LIMITATIONS
We note several limitations of this study. First, because this was a single-site study, findings may not be generalizable to other settings. Second, due to the retrospective design of this study, information such as prediction confidence ratings were not collected, which we note impacted the accuracy of predictions in previous literature. Third, we did not have data explaining the 20% rate of non-compliance observed. It is possible that nurses selectively made predictions for cases in which they felt more confident, artificially inflating our reported sensitivity and specificity. Fourth, admission prediction is not included in current triage training and, consequently, formal implementation may be required to acquire the most accurate measurements. Fifth, while using bounceback presentations with admission allows us to account for incorrect discharge by the physician, it may result in underestimation of specificity and overestimation of sensitivity if the subsequent admission is for a reason unrelated to the index presentation. Lastly, although a retrospective trial limits influence of the Hawthorne effect, the absence of consequences or incentives for incorrect or accurate predictions, respectively, may have reduced the intentionality of predictions made by triage nurses and, in turn, accuracy.
CONCLUSION
We found generally high accuracy but low F1 scores when triage nurses made admission predictions about patients at our site of interest in the province of Ontario, Canada. High accuracy stems from high specificities with modest sensitivities We found notable variation in nurse accuracy and variation based on patient characteristics. These results suggest that nursing staff predictions could be useful in expediting some resource allocation decisions and improving flow in EDs.
Address for Correspondence: Stephenson Strobel, MD, PhD, McMaster University, Division of Emergency Medicine, Department of Family Medicine, Faculty of Health Sciences, Hamilton, Ontario, Canada. Email: sbs296@cornell.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Armstrong et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Value-for-Money Audit: Emergency Departments. 2023. Available at: https://www.auditor.on.ca/en/content/annualreports/arreports/en23/ AR_emergencydepts_en23.pdf. Accessed October 5, 2024.
2. Horwitz LI, Green J, Bradley EH. US emergency department performance on wait time and length of visit. Ann Emerg Med 2010;55(2):133-41.
3. Bouda Abdulai AS, Mukhtar F, Ehrlich M. United States’ performance on emergency department throughput, 2006 to 2016. Ann Emerg Med. 2021;78(1):174-90.
4. Nyce A, Gandhi S, Freeze B, et al. Association of emergency department waiting times with patient experience in admitted and discharged patients. J Patient Exp. 2021;8:23743735211011404.
5. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med 2013;61(6):605-11.e6.
6. Wretborn J, Wilhelms DB, Ekelund U. Emergency department crowding and mortality: an observational multicenter study in Sweden. Front Public Health. 2023;11:1198188.
7. Woodworth L. Swamped: Emergency department crowding and patient mortality. J Health Econ. 2020;70:102279.
8. Eidstø A, Ylä-Mattila J, Tuominen J, et al. Emergency department crowding increases 10-day mortality for non-critical patients: a retrospective observational study. Intern Emerg Med 2024;19(1):175-81.
9. Smalley CM, Simon EL, Meldon SW, et al. The impact of hospital boarding on the emergency department waiting room. JACEP Open 2020;1(5):1052-9.
10. Peck JS, Benneyan JC, Nightingale DJ, et al. Predicting emergency department inpatient admissions to improve same‐day patient flow. Acad Emerg Med. 2012;19(9):E1045-54.
11. lipson AR, Miano SJ, Daly BJ, et al. The accuracy of nurses’ predictions for clinical outcomes in the chronically critically ill. Res Rev J Nurs Health Sci. 2017;3(2):35-8.
12. Alexander D, Abbott L, Zhou Q, et al. Can triage nurses accurately
predict patient dispositions in the emergency department? J Emerg Nurs. 2016;42(6):513-8.
13. Holdgate A, Morris J, Fry M, et al. Accuracy of triage nurses in predicting patient disposition. Emerg Med Australas 2007;19(4):341-5.
14. Göransson K, Ehrenberg A, Marklund B, et al. Accuracy and concordance of nurses in emergency department triage. Scand J Caring Sci. 2005;19(4):432-8.
15. Romero-Brufau S, Gaines K, Nicolas CT, et al. The fifth vital sign? Nurse worry predicts inpatient deterioration within 24 hours. JAMIA Open. 2019;2(4):465-70.
16. Copeland-Fields L, Griffin T, Jenkins T, et al. Comparison of outcome predictions made by physicians, by nurses, and by using the Mortality Prediction Model. Am J Crit Care. 2001;10(5):313-9.
17. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267-77.
18. Fawcett T. An introduction to ROC analysis. Pattern Recognit Lett 2006;27(8):861-74.
19. Rainio O, Teuho J, Klén R. Evaluation metrics and statistical tests for machine learning. Sci Rep. 2024;14(1):6086.
20. Lee JY, Oh SH, Peck EH, et al. The validity of the Canadian Triage and Acuity Scale in predicting resource utilization and the need for immediate life-saving interventions in elderly emergency department patients. Scand J Trauma Resusc Emerg Med. 2011;19(1):68.
21. Veldhuis LI, van der Weide L, Nanayakkara P, et al. The accuracy of predicting hospital admission by emergency medical service and emergency department personnel compared to the prehospital MEWS: a prospective multicenter study. BMC Emerg Med 2024;24(1):111.
22. Bonner SE, Sprinkle GB. The effects of monetary incentives on effort and task performance: theories, evidence, and a framework for research. Account Org Soc. 2002;27(4-5):303-45.
23. Beardsell I, Robinson S. Can emergency department nurses performing triage predict the need for admission? Emerg Med J 2011;28(11):959-62.
24. Buurman BM, Van Munster BC, Korevaar JC, et al. Prognostication in acutely admitted older patients by nurses and physicians. J Gen Intern Med. 2008;23(11):1883-9.
25. Cameron A, Ireland AJ, McKay GA, et al. Predicting admission at triage: Are nurses better than a simple objective score? Emerg Med J. 2017;34(1):2-7.
26. Afnan MAM, Ali F, Worthington H, et al. Triage nurse prediction as a covariate in a machine learning prediction algorithm for hospital admission from the emergency department. Int J Med Inform 2021;153:104528.
27. Derlet RW, Kinser D, Ray L, et al. Prospective identification and triage of nonemergency patients out of an emergency department: a 5-year study. Ann Emerg Med. 1995;25(2):215-23.
28. Stover-Baker B, Stahlman B, Pollack M. Triage nurse prediction of hospital admission. J Emerg Nurs. 2012;38(3):306-10.
29. Vaghasiya MR, Murphy M, O’Flynn D, et al. The emergency department prediction of disposition (EPOD) study. Australas Emerg Nurs J. 2014;17(4):161-6.
30. Dong SL. Emergency Triage: comparing a novel computer triage program with standard triage. Acad Emerg Med. 2005;12(6):502-7.
31. Mowbray F, Brousseau AA, Mercier E, et al. Examining the relationship between triage acuity and frailty to inform the care of older emergency department patients: findings from a large Canadian multisite cohort study. CJEM. 2020;22(1):74-81.
Prior Outpatient Care Use in Emergency Department Patients with Low- and High-acuity Conditions in Germany
Yves N. Wu, MPH*
Martin Möckel, Prof. Dr. med*
Dörte Huscher, Dr. rer. medic.†
Antje Fischer-Rosinský, Dr. rer. nat*
Thomas Keil, Prof. Dr. med, MSc‡§||
Anna Slagman, Prof. Dr. rer. medic., MSc*
*
Charité - Universitätsmedizin Berlin, Emergency and Acute Medicine (CVK, CCM), Berlin, Germany
Charité - Universitätsmedizin Berlin, Institute of Medical Biometry and Clinical Epidemiology, Berlin, Germany
Charité - Universitätsmedizin Berlin, Institute of Social Medicine, Epidemiology and Health Economics, Berlin, Germany
Institute of Clinical Epidemiology and Biometry, University of Würzburg, Würzburg, Germany
State Institute of Health I, Bavarian Health and Food Safety Authority, Erlangen, Germany
Section Editor: Brian J. Yun, MD, MBA, MPH
Submission history: Submitted November 25, 2024; Revision received March 21, 2025; Accepted April 23, 2025
Electronically published September 20, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.38466
Introduction: The key role of emergency departments (ED) is to treat severe and life-threatening cases. A rise in ED visits, particularly for low-acuity conditions, places a burden on resources which may hinder efficient care for high-acuity conditions. We investigated the association between previous outpatient healthcare services use and low-acuity visits in EDs in Germany.
Methods: We analyzed data from the Initiative for Emergency Department Evaluation and Data Collection project, with 454,747 ED visits by 353,926 patients collected from 16 EDs in Germany in 2016. We included a subset of 228,753 (64.6%) patients with 299,914 (66.0%) visits from 12 of the participating EDs for which outpatient care data was available. We categorized ED presentations into low- or high-acuity based on transportation to the ED, triage category, hospital admission status, and intrahospital mortality. By merging patient hospital records with outpatient billing information, we assessed outpatient care utilization prior to ED visits. Using a generalized mixed-effects model, we investigated the relationship between acuity level and outpatient care utilization, adjusting for age, sex, and type of residential area.
Results: Low-acuity patients were considerably younger than high-acuity (mean age ± standard deviation: 45 ±19 vs 58 ±21 years) and used outpatient services less often within 10 days prior to their ED visit: 40.6% vs 49.5%. Key associations for low-acuity ED visits included younger age (per 10-year categories: adjusted odds ratios 0.72, 95% confidence interval 0.72-0.73), urban residence (1.17; 1.13-1.22), and timing of the last outpatient contact. Longer durations since the last outpatient contact were associated with a higher likelihood of presenting to the ED with low-acuity symptoms. Compared to patients who visited their primary care physician (PCP) shortly before their ED visit, those with PCP contact 1-6 months (1.22; 1.19-1.25) and over six months prior (1.33; 1.26-1.41) were more likely to present with low-acuity conditions.
Conclusion: While almost half of both low- and high-acuity patient groups utilized outpatient services prior to the ED visit, low-acuity patients were generally younger and had fewer such contacts. The majority had accessed both primary care and the ED, challenging the assumption that low-acuity patients routinely bypass outpatient care before seeking emergency services. This raises the question of what limitations or unaddressed needs in outpatient care drive these patients to seek subsequent care in the ED. More research is needed to explore the structural and systemic factors influencing low-acuity ED visits. [West J Emerg Med. 2025;26(5)1183–1191.]
BACKGROUND
Emergency departments (ED) are crucial components of healthcare systems, ideally designed to manage serious and life-threatening cases. However, studies have shown that a significant proportion of patients visiting EDs have conditions that might not necessarily warrant emergency care.1,2 The evolving role of emergency and urgent care systems as well as outpatient care availability has been linked to increased use of EDs, particularly outside regular hours of primary care physicians (PCP). This pattern can be attributed to various factors, including the accessibility of services and patient anxiety surrounding health issues, prompting individuals to seek immediate attention in highly equipped medical settings.3,4
While ensuring timely access to emergency care is vital, a high influx of non-emergency visits can often strain ED resources and may hinder the efficient delivery of care to patients with urgent needs, resulting in ED crowding.5-7 To alleviate this burden, it is crucial to broaden the scope of research beyond the boundaries of the ED, directing attention to the roles of healthcare services outside the emergency setting. Emphasis should be placed on outpatient services, such as PCPs, medical specialists, and telehealth services, which can be attributed a gatekeeper function to the ED. These services serve as pivotal entry points in directing traffic toward the ED and have a key role in regulating the distribution of resources and directing patients to the most suitable care setting.8-10
The German healthcare system is primarily funded through a dual insurance model, comprising statutory health insurance (GKV) and private health insurance (PKV).11 Approximately 88.1% of the population (73.3 million people) are insured under the GKV, while 10.5% (8.7 million) are covered by PKV, which can serve as both primary coverage for eligible individuals and supplemental insurance for those in the GKV seeking additional services. Additionally, Germany has a high PCP use rate, with 30% of the population visiting a doctor three to five times per year 11 However, what is currently lacking is a nationwide gatekeeping system for urgent care services, and the relationship between prior outpatient healthcare engagement and ED use remains largely unexplored.12-13 In this study we aimed to determine whether low-acuity ED patients differed from high-acuity patients in terms of the timing and frequency of outpatient visits in the period leading up to their ED visit. Specifically, we investigated whether low-acuity patients were less likely than high-acuity patients to engage with outpatient healthcare services before seeking emergency care, thereby assessing the validity of the claim that low-acuity patients use the ED for convenience rather than as a last resort.
METHODS
Study Design and Setting
This study is based on data from the Initiative for Emergency Department Evaluation and Data Collection (INDEED) conducted across 16 German hospitals with EDs in
Population Health Research Capsule
What do we already know about this issue?
Low-acuity ED visits are common and often assumed to stem from poor outpatient care access, straining emergency services.
What was the research question?
Do low-acuity ED patients differ from highacuity ones in prior outpatient-visit timing and frequency?
What was the major finding of the study?
Low-acuity visits were associated with fewer recent outpatient contacts (OR 1.22-1.33; 95% CI 1.19-1.41).
How does this improve population health? Findings suggest that EDs supplement, not replace, outpatient care, which could guide resource planning and patient flow improvements.
2016. Patients were eligible if they had at least one ED visit recorded in 2016 and were insured by a German statutory health insurance provider. To ensure eligibility for outpatient care data linkage, patients had to be at least 20 years of age on January 1, 2016, corresponding to a minimum age of 18 at the start of the observation period (January 1, 2014). Routine hospital data from all ED patients were merged with statutory health insurance records covering outpatient care from two years before to one year after the ED visit (2014–2017), resulting in a dataset of 454,747 ED visits from 353,926 patients. Due to missing data required for the primary outcome or outpatient utilization, only 12 of the 16 EDs were included in the final analysis.
Study Population and Outcome Definition
To assess patient characteristics and prior outpatient care utilization, ED visit data was merged with patient-level outpatient data. The outcome definition followed the pragmatic framework by Slagman et al (2023), which allows for a reliable and replicable identification of high- and lowacuity ED visits in German routine data. This approach incorporates objective criteria such as hospital admission, triage category, and transport type, reflecting their consistent availability and utility in routine emergency documentation. It is particularly suited to the German healthcare setting and facilitates standardization across sites and studies, despite the absence of a gold-standard definition of “acuity” in routine
Prior Outpatient Care Use in ED Patients with Low- and High-acuity Conditions
data.2 High-acuity visits were identified by fulfilling at least one of the following criteria:
1. admitted to hospital or deceased, 2. medically accompanied transport, or 3. Manchester Triage System (MTS) or Emergency Severity Index (ESI) triage category of 1, 2 or 3.
The MTS is a structured tool that categorizes ED patients into five levels (immediate, very urgent, urgent, standard, and non-urgent), each with a corresponding maximum waiting time.14 The ESI is also a five-level triage system. However, it prioritizes patients by acuity and anticipated resource needs, ranging from immediate life-saving intervention needed to non-urgent/no resources required.15 Cases that met none of these criteria were classified as low acuity. If the triage category was missing, the case was labeled as “not assessable.” Applying this framework to the INDEED dataset, we excluded 83,991 visits due to missing acuity data. Since the integration of ED and outpatient billing data was required to evaluate previous use patterns of outpatient healthcare services, another 57,214 patients (corresponding to 70,842 visits) were excluded due to missing outpatient records. Additionally, four study sites were excluded due to incomplete data, leaving a final study population of 299,914 visits from 228,753 patients across 12 EDs. We conducted a comparison of included and excluded cases to assess potential selection bias (Appendix Table 2).
Definition of Influential Variables
We determined baseline patient characteristics using district code numbers to identify residential districts, crossreferenced with the BBSR (Bundesinstitut für Bau-, Stadt- und Raumforschung, German Federal Institute for Research on Building, Urban Affairs, and Spatial Development) INKAR (Indicators and Maps for Spatial and Urban Development) database, which provides detailed development indicators for Germany.16 Based on population density, districts were classified as follows: urban (>300 inhabitants per square kilometer [i/km²]); regions with signs of urbanization (150300 i/km²); or rural (<150 i/km²).16 We analyzed ED length of stay (LOS) only for non-admitted patients, as all inpatients were classified as high acuity. To ensure data reliability and avoid anomalies, a cutoff was defined, considering only cases within a range of 5 minutes to 24 hours (1,440 minutes).
Data Management
To assess outpatient healthcare utilization, the analysis relied on timestamps from outpatient billing data as indicators of service use. To ensure accuracy, we excluded outpatient billing data originating from the participating EDs, as our aim was to assess outpatient healthcare utilization outside of the emergency department setting. Non-relevant services (e.g., antibody testing, postage fees, and laboratory tests) were also excluded. Lastly, outpatient
contacts recorded on the same day as the ED visit were removed to prevent misclassification of ED services as outpatient care. We categorized PCP and specialist visits based on the last two digits of the German physician identification number, ensuring an accurate classification of outpatient services.18
Statistical Methods
We conducted descriptive analyses to compare ED visit characteristics by acuity level. Chi-square tests assessed categorical variables (sex, region type, weekday, and prior outpatient contact), while Wilcoxon rank-sum tests were used for continuous variables (age and ED LOS) due to their non-normal distribution, as it was confirmed via the Kolmogorov-Smirnov test. A mixed-effects multivariable logistic regression model estimated the impact of key variables on acuity level (low/high). This binomial model, fitted by maximum likelihood (the Laplace approximation), included random effects for ED site and individual patients to account for non-independence of observations. Since the analysis was case level (ED visit), each visit was treated independently. And since the analysis was done on ED visit-level, each visit was treated independently. For patients with multiple outpatient visits, only the most recent contact before each ED visit was considered, allowing outpatient contact timeframes to vary across visits. This ensured that prior outpatient use was assigned specific to each ED visit, preventing bias from cumulative visit histories. The model adjusted for age, sex, region type, and prior outpatient use, with model selection based on Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) to balance fit and complexity. We conducted analyses in R v4.3 (R Foundation for Statistical Computing, Vienna, Austria) using the tidyverse and lme4 packages.20-21
Adherence to Retrospective Review Studies criteria
This study adhered to the methodological standards outlined by Worster et al (2005) for retrospective chart reviews in emergency medicine research. These criteria address key methodological aspects, including case selection, data abstraction, variable definition, missing data management, and quality control measures.22 A detailed listing of each criterion and its application within this study can be found in Appendix Table 1.
RESULTS
The final study population included 228,753 individual patients and 299,914 ED visits, representing 64.6% of the total population and 66.0% of all visits. Of these visits, 70.0% were presentations with high-acuity and 26.4% with low-acuity conditions. For 3.5%, the acuity level was not assessed due to a missing triage score (Figure 1).
As seen in Table 1, patients with ED visits classified as low acuity were, on average, 13 years younger than those with
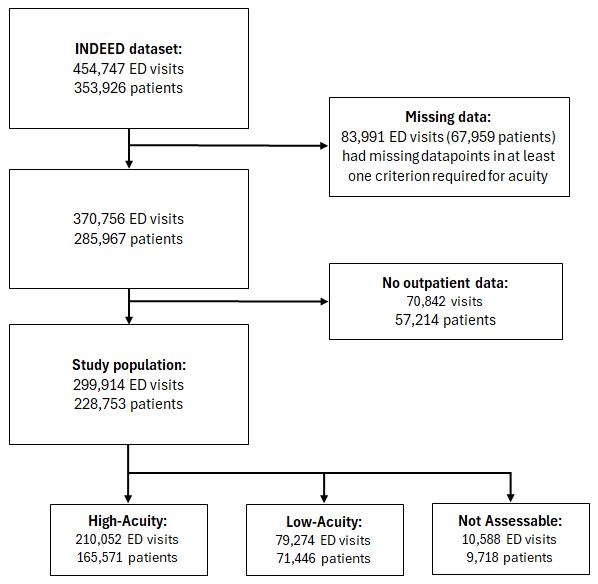
Figure 1. Selection of the study population from the INDEED* dataset. This flowchart outlines the exclusion process, where cases with missing acuity classification data or unavailable outpatient billing records were removed. Since patients can have multiple ED visits, the sum of patients across acuity groups exceeds the total study population.
*INDEED, Inanspruchnahme und Versorgungsmuster von Patienten in Notfallversorgungsstrukturen in Deutschland (Utilisation and Cross-Sectoral Patterns of Care for Patients Admitted to Emergency Departments in Germany); ED, emergency department.
likely than high-acuity patients to have had an outpatient contact within 10 or 11-30 days before their ED visit. This pattern was seen for both PCP and specialist visits. Furthermore, a higher proportion of low-acuity patients had their last outpatient visit over six months before their ED visit. To assess outpatient care use prior to an ED visit, we analysed the most recent contact within specific timeframes before the ED visit. We found that both groups demonstrated substantial engagement with outpatient healthcare services before their visit to the ED, while only a small proportion had no recorded contact within the previous 12 months. However, high-acuity patients were more likely to have had their last outpatient visit in a more recent timeframe compared to low-acuity patients. This difference was considerably larger within 10 days before the ED visit (Figure 2).
high-acuity visits. Both high- and low-acuity cases were similarly distributed across rural and urban areas, with urban regions accounting for most cases in each category. Although most visits took place on weekdays, low-acuity visits were more frequent during weekends compared to those of high acuity. The LOS in the ED varied considerably between both groups, with the median ED stay for low-acuity visits being significantly shorter than for high-acuity visits. Since many high-acuity cases were admitted as inpatients, only 35% of these visits were included, whereas we evaluated all lowacuity cases with available data on LOS (77.5%).
While most ED visits (82.0%) were from patients with 1-2 visits, high-acuity presentations were more common among frequent ED users. Among visits from patients with 3-9 ED presentations, 18.2% were high acuity compared to 13.2% low acuity. Very frequent ED users (≥10 visits) accounted for only 1.1% of all visits across both acuity groups. We assessed outpatient care use, focusing on the percentage of patients who visited outpatient healthcare services in general, a PCP, or specialist before their ED visit. Low-acuity patients were less
Based on these results, we performed a mixed-effects regression analysis to further study the variables of interest. Prior to regression analysis, the intraclass correlation coefficient (ICC) was estimated using a variance components approach, where the ICC represents the proportion of variance attributable to differences between ED sites. The ICC for the random effect study site on the outcome low- or high-acuity was estimated at 0.023 (95% CI 0.012-0.064). As depicted in Table 2, crude regressions, along with mixed-effects regression models that incorporated study site and patient as random effects were performed to assess the influence of outpatient attributes on low-acuity ED visits, while adjusting for sex, age, and region type. Each attribute was assigned to a mixed-effects model, with model 1 assessing last outpatient contact in general, model 2 last PCP contact, and model 3 last specialist contact of patients before their ED visit..Across all three models female patients (odds ratio [OR] 1.05) and those living in urban areas (OR 1.18-1.19) had a slightly higher likelihood of a low-acuity ED visit. In contrast, the likelihood decreased with increasing age (OR 0.72, per decade) and for patients in mixed urban-rural areas compared to those in rural areas (OR 0.85-0.87). Patients with a higher number of ED visits had lower odds of presenting to the ED with low-acuity conditions. Compared to those with 1-2 ED visits, patients with 3-9 visits had 20% lower odds of a low-acuity visit (OR 0.80), while those with ≥10 visits had 14-17% lower odds (OR 0.82–0.86). The odds of a low-acuity ED visit increased with increasing time since the last outpatient contact, regardless of the type of contact. Compared to patients who had outpatient contact within 10 days before their ED visit, those with contact 11-30 days prior had slightly higher odds of a lowacuity ED visit (OR 1.09-1.10). The odds further increased for those with contact 1-6 months prior (ORs 1.20–1.22) and six months to a year prior (OR 1.30-1.37). Having no prior outpatient or specialist contact in the past year was associated with slightly increased odds of a low-acuity ED visit (OR 1.06-1.07, Table 2). The Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) values were comparable across all three models, with Model 1 showing the
Table 1. Characteristics of adult emergency department (ED) visits in Germany in 2016, stratified by acuity level, presenting demographic characteristics, ED visit details, and prior outpatient healthcare utilization. Visits are categorized as high acuity, low acuity, or not assessable based on predefined criteria. Variables include age, sex, region of residence, ED presentation time, length of stay, and engagement with outpatient healthcare services before the ED visit.
Outpatient care use
¹includes only non-admitted patients.
PCP, primary care physician; I./km², inhabitants per square kilometer; NA, not applicable; ED, emergency department.
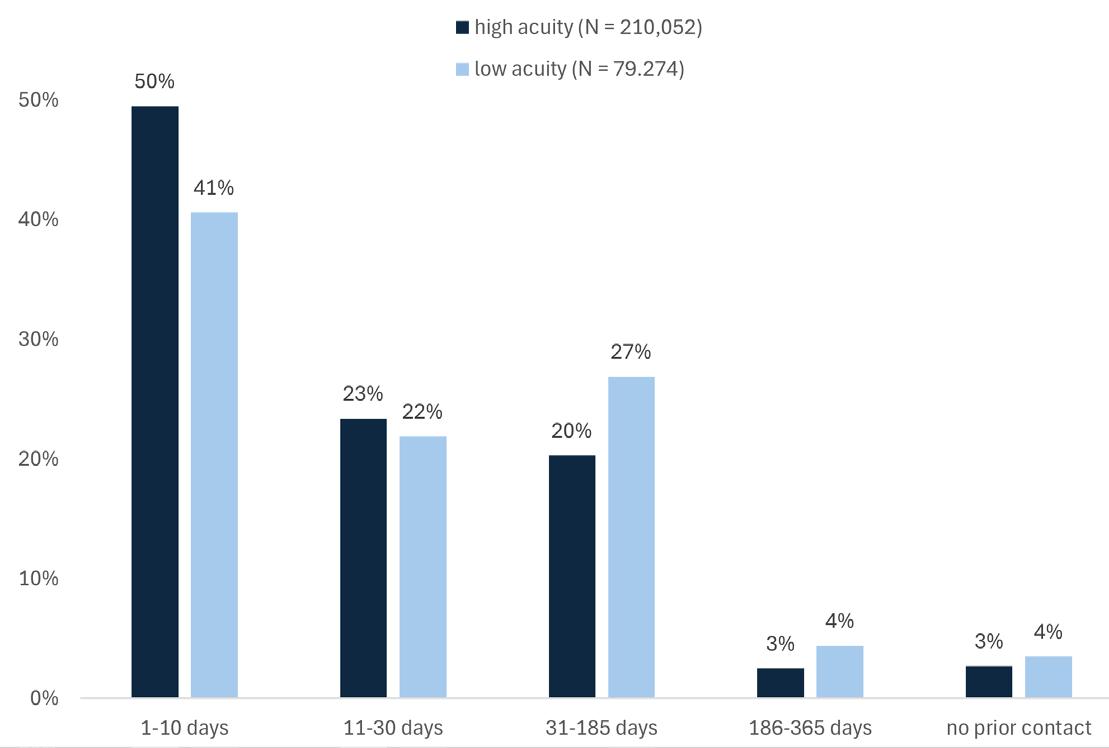
Figure 2. Bar chart displaying last outpatient contact within one year before emergency department (ED) visit, stratified by acuity level, displaying the percentage of high-acuity (dark blue) and lowacuity (light blue) ED patients who had their last outpatient contact within the timeframes 1-10 days, 11-30 days, 31-185 days, 186-365 days, or no contact at all prior to their ED visit from data based on 12 German hospitals included in the INDEED* dataset.
*INDEED, Initiative for Emergency Department Evaluation and Data Collection
highest values and Model 2 the lowest, which suggests that Model 2 provides the best fit (Table 2).
DISCUSSION
Summary of Main Results
In this study of 299,914 ED presentations from 228,753 patients in German EDs in 2016, we found that patients with low-acuity conditions were, on average, younger than those with high-acuity conditions. While a large proportion of low-acuity patients had engaged with outpatient healthcare services within a year before their ED visit, their use was slightly lower compared to high-acuity patients. Results from the multivariable mixed-effects model confirmed that age, region type, and prior healthcare use were associated with low-acuity ED presentations. Patients with recent outpatient, PCP, or specialist contact before the ED visit were less likely to present with low-acuity conditions. Additionally, frequent ED users had a lower probability of low-acuity visits, suggesting that repeated visits are more often associated with high-acuity cases. Among the models tested, the mixed-effects model incorporating prior PCP contact had the lowest AIC and BIC values, indicating a better balance between model fit and complexity, suggesting it to be the most generalizable for understanding prior outpatient engagement in ED patients.
Comparability of Findings
The findings of this study provide further understanding of who presents to the ED with low-acuity symptoms and why. While previous studies have emphasized lack of
accessibility as a key driver of ED attendance, the results of this study show extensive engagement of both high- and low-acuity patients with outpatient healthcare services before their ED visit.6,23-25 This suggests that the ED is not always the first point of contact for many patients and that some patients seek ED care for conditions that may not have been satisfactorily treated or had worsened following outpatient care. Beyond accessibility, patient awareness and decisionmaking processes also play a crucial role in ED use. Kümpel et al (2024) highlighted that limited awareness of alternative care options contributes to ED visits for non-urgent conditions, even when outpatient services are available.26 Similarly, a US-based study by Heinert et al (2020) found that a lack of awareness of nearby alternative care facilities was common among ED users, suggesting that educational interventions could help lower non-emergent ED visits.27 Furthermore, insurance status significantly influenced ED use, with Medicaid, Medicare, and uninsured patients disproportionately choosing the ED over urgent care centers.27
Despite having more limited access to outpatient healthcare services, patients from rural areas were slightly more represented in high- compared to low-acuity visits (19% vs 17%). This was further underlined by the mixed-effects regression models, which showed that residing in urban areas was associated with a higher likelihood of a low-acuity ED visit. These findings mirror the results of Schmiedhofer et al (2016), who found that patients from rural areas were more strongly connected to a PCP, whereas urban patients were often loosely connected or did not have a PCP.4 Given that urban areas typically have a higher density of outpatient services, the expansion of these services alone may not be sufficient to reduce ED crowding due to low-acuity visits.28-29
A combination of factors—including accessibility, personal beliefs, emotional distress, and knowledge about alternative care options—likely contributes to the decision to seek ED care.1, 4, 26, 27, 30 Aside from accessibility and geographic factors, the results also align with previous studies regarding age-related trends in ED use. Younger patients had a higher likelihood of presenting to the ED with low-acuity symptoms, a finding consistent with prior research.31-33 This is likely due to the higher prevalence of complex and chronic conditions among older adults, making high-acuity ED visits more common in this group.6, 31-33 However, the specific reasons why younger individuals frequently visit the ED for low-acuity conditions remain unclear. Based on international literature, potential explanations include a greater reliance on emergency services among young adults and an increasing number of psychiatric emergencies in this demographic.35, 36 Further research on low-acuity ED presentations among young adults should aim to explore these assumptions.
Efforts to reduce low-acuity visits have explored alternative care models, such as walk-in clinics (WIC). Kurian et al (2022) found that introducing a WIC led to an immediate decline in low-acuity visits, suggesting that providing accessible
Table 2. Multivariable mixed-effects logistic regression models for low-acuity emergency department (ED) visits. Results of multivariable mixed-effects logistic regression models estimating odds of a low-acuity ED visit compared to a high-acuity visit. Crude and adjusted odds ratios with 95% confidence intervals are reported for demographic and healthcare utilization variables, including sex, age, region type, and timeframe of last outpatient, primary care physician, or specialist contact before the ED visit. Models adjust for sex, age, and region type, incorporating study site and patient-level random effects.
Model 1
Model 2
Model 3
(ref.: <150 I./km²)
ED visit frequency (ref.: 1-2 visits)
Last outpatient contact (ref.: 1-10 days)
Last PCP contact (ref.: 1-10 days)
(1.12-1.17)
(1.43-1.59)
Last specialist contact (ref.: 1-10 days) 11-30
AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; CI, confidence interval; PCP, primary care physician; I./km², inhabitants per square kilometre; OR, odds ratio; ED, emergency department.
alternatives can temporarily divert non-emergent cases from EDs.37 However, this effect was not sustained over time, indicating that WICs alone are insufficient to change patient behavior long term.37 To create a lasting reduction, additional strategies, such as expanding patient awareness of alternative care options, removing barriers to outpatient care accessibility, and introducing referral mechanisms, may be required.
STRENGTHS AND LIMITATIONS
The strengths of the present study included the large sample of participating EDs across Germany and the unique dataset for which we merged routine hospital data from 2016 with billing data from statutory health insurance companies from 2014–2017 on an individual patient basis. However, several limitations should be noted. First, there is the possibility of data
loss due to the use of retrospective data obtained from different EDs, which involved different hospital information systems, and thus varying data collection processes between study centers. This led to a high amount of missing data, which in turn had the potential to introduce bias. Most importantly, the dataset was constrained by the information available from participating EDs, and potentially relevant data points could not be collected in a standardized manner.
Secondly, because only statutory health insurance data was available, it remains unclear whether results would be the same for the ≈10% of patients in Germany with private health insurance.11, 38 Third, since the participating hospitals were not selected randomly, these results cannot be considered representative for the whole country. However, the 16 hospitals are in different regions across Germany and can be considered representative for their catchment area. Although the INDEED project presents the first approach in providing cross-sectoral ED and outpatient data across Germany, more effort is required to standardize multicenter data availability to enable a comprehensive understanding of potential factors that contribute to low-acuity ED use across large geographical settings. An example in this direction is demonstrated by the German Emergency Department Data Registry, AKTIN, which has proven to be applicable even in low-resource settings with restricted system access to facilitates monitoring processes in EDs across Germany.39
CONCLUSION
This study showed that ED use, specifically for low-acuity patients, does not replace but rather complements prior outpatient care. This was reflected by the high outpatient use rates among both groups shortly before the ED visit. Additional research would be beneficial to discern whether these complementary visits are due to unmet patient needs, referrals from the outpatient sector due to resource constraints, or other factors.
Address for Correspondence: Yves Noel Wu, MPH, Charité - Universitätsmedizin Berlin, Notfallmedizinische Versorgungsforschung, Notfall- und Akutmedizin CCM & CVK, Augustenburger Platz 1, 13353 Berlin, GERMANY, Berlin, Germany. Email: yves-noel.wu@charite.de
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Wu et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Reinhold AK, Greiner F, Schirrmeister W, et al. Der Notfall „geht“ ins Krankenhaus: Eine Befragung von Patienten mit niedriger Dringlichkeit in einer Notfallaufnahme mit regionaler Alleinstellung. Med Klin Intensivmed Notfmed. 2021;116(6):511–521.
2. Slagman A, Fischer-Rosinský A, Legg D, et al. Identification of low-acuity attendances in routine clinical information documented in German Emergency Departments. BMC Emerg Med. 2023;23(1):64.
3. Hitzek J, Fischer-Rosinský A, Möckel M, et al. Influence of weekday and seasonal trends on urgency and in-hospital mortality of emergency department patients. Front Public Health 2022;10:711235.
4. Schmiedhofer M, Möckel M, Slagman A, et al. Patient motives behind low-acuity visits to the emergency department in Germany: a qualitative study comparing urban and rural sites. BMJ Open 2016;6(11):e013323.
5. McCarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med. 2009;54(4):492–503.e4.
6. Morley C, Unwin M, Peterson GM, et al. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. 2018;13(8):e0203316.
7. Sartini M, Carbone A, Demartini A, et al. Overcrowding in emergency department: causes, consequences, and solutions-a narrative review Healthcare (Basel). 2022;10(9):1625.
8. Blinkenberg J, Pahlavanyali S, Hetlevik Ø, et al. General practitioners’ and out-of-hours doctors’ role as gatekeeper in emergency admissions to somatic hospitals in Norway: registrybased observational study. BMC Health Serv Res. 2019;19(1):568.
9. Møller TP, Ersbøll AK, Tolstrup JS, et al. Why and when citizens call for emergency help: an observational study of 211,193 medical emergency calls. Scand J Trauma Resusc Emerg Med. 2015;23:88.
10. Van der Linden MC, Lindeboom R, van der Linden N, et al. Selfreferring patients at the emergency department: appropriateness of ED use and motives for self-referral. Int J Emerg Med. 2014;7:28.
11. Bundesministerium für Gesundheit. Das deutsche Gesundheitssystem. 2nd ed. 2022. Available at: https://www. bundesgesundheitsministerium.de/fileadmin/user_upload/Dasdeutsche-Gesundheitssystem_bf.pdf Accessed: March 14, 2025
12. Baier N, Geissler A, Bech M, et al. Emergency and urgent care systems in Australia, Denmark, England, France, Germany and the Netherlands - Analyzing organization, payment and reforms. Health Policy. 2019;123(1):1-10.
13. Fischer-Rosinský A, Slagman A, King R, et al. INDEED–utilization and cross-sectoral patterns of care for patients admitted to emergency departments in Germany: rationale and study design. Front Public Health. 2021;9:616857.
14. Mackway-Jones K, Marsden J, Windle J, editors. Ersteinschätzung in der Notaufnahme: Das Manchester–Triage–System. 5th ed. Göttingen: Hogrefe AG; 2020.
15. Gilboy N, Tanabe P, Travers D, et al. Emergency Severity Index (ESI): a triage tool for emergency department care, version 4. AHRQ
Prior Outpatient Care Use in ED Patients with Low- and High-acuity Conditions in Germany
Implementation handbook. 2012;12-0014.
16. Bundesinstitut für Bau-, Stadt- und Raumforschung (BBSR). INKAR - Indikatoren und Karten zur Raum- und Stadtentwicklung. 2020. Available at: www.inkar.de Accessed: September 5, 2023.
17. Bundesinstitut für Bau-, Stadt- und Raumforschung (BBSR). Raumbeobachtung - Siedlungsstruktureller Regionstyp. 2023. Available at: https://www.bbsr.bund.de/BBSR/DE/forschung/ raumbeobachtung/Raumabgrenzungen/deutschland/regionen/ siedlungsstrukturelle-regionstypen/regionstypen.html. Accessed: January 18, 2024.
18. Kassenärztliche Bundesvereinigung (KBV). zweistellige Fachgruppencodierung für die 8.+9. Stelle der LANR, BARSchlüsselverzeichnis, Anlage 35. Version 1.03. Available at: https:// applications.kbv.de/S_BAR2_ARZTNRFACHGRUPPE_V1.03.xhtml. Accessed: June 16, 2023.
19. Stoica P, Selen Y. Model-order selection: a review of information criterion rules. IEEE Signal Process Mag. 2004;21(4):36–47.
20. Wickham H, Averick M, Bryan J, et al. Welcome to the tidyverse. J Open Source Softw. 2019;4(43):1686.
21. Bates D, Mächler M, Bolker B, et al. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48.
22. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448–451.
23. McHale P, Wood S, Hughes K, et al. Who uses emergency departments inappropriately and when - a national cross-sectional study using a monitoring data system. BMC Med. 2013;11:258.
24. Holzinger F, Oslislo S, Möckel M, et al. Self-referred walk-in patients in the emergency department - who and why? BMC Health Serv Res 2020;20(1):848.
25. O’Keeffe C, Mason S, Jacques R, et al. Characterising non-urgent users of the emergency department (ED): A retrospective analysis of routine ED data. PLoS One. 2018;13(2):e0192855.
26. Kümpel L, Oslislo S, Resendiz Cantu R, et al. “I do not know the advantages of having a general practitioner” - a qualitative study exploring the views of low-acuity emergency patients without a regular general practitioner toward primary care. BMC Health Serv Res. 2024;24:629.
27. Heinert SW, Mumford M, Kim SE, et al. User characteristics of a low-acuity emergency department alternative for low-income patients. West J Emerg Med. 2020;21(6):162–171.
28. O’Cathain A, Foster A, Carroll C, et al. Health literacy interventions for reducing the use of primary and emergency services for minor
health problems: a systematic review. Southampton (UK): National Institute for Health and Care Research; 2022.
29. Hong M, Thind A, Zaric GS, et al. The impact of improved access to after-hours primary care on emergency department and primary care utilization: a systematic review. Health Policy. 2020;124(8):812–818.
30. Kirkland SW, Soleimani A, Rowe BH, et al. A systematic review examining the impact of redirecting low-acuity patients seeking emergency department care: is the juice worth the squeeze? Emerg Med J. 2019;36(2):97-106.
31. Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47-59. PMID:23379744; PMCID:PMC4156292.
32. Somasundaram R, Geissler A, Leidel BA, et al. Beweggründe für die Inanspruchnahme von Notaufnahmen – Ergebnisse einer Patientenbefragung [Reasons for Emergency Department Visits: Results of a Patient Survey]. Gesundheitswesen. 2018;80(7):621-627.
33. Singler K, Dormann H, Dodt C, et al. Der geriatrische Patient in der Notaufnahme. Notfall Rettungsmed. 2016;19:496–499.
34. Langhoop K, Habbinga K, Greiner F, et al; AKTINNotaufnahmeregister. Charakteristika älterer im Vergleich zu jüngeren Notfallpatienten: Analyse von über 356.000 erfassten Besuchen des AKTIN-Notaufnahmeregisters [Characteristics of older versus younger emergency patients: Analysis of over 356,000 visits from the AKTIN German emergency department data registry]. Med Klin Intensivmed Notfmed. 2024;119(1):18-26.
35. Fortuna RJ, Robbins BW, Mani N, et al. Dependence on emergency care among young adults in the United States. J Gen Intern Med 2010;25(7):663-669.
36. Bommersbach TJ, McKean AJ, Olfson M, et al. National trends in mental health-related emergency department visits among youth, 2011-2020. JAMA. 2023;329(17):1469-1477.
37. Kurian D, Sundaram V, Naidich AG, et al. Changes in low-acuity patient volume in an emergency department after launching a walk-in clinic. JACEP Open. 2023;4(4):e13011.
38. Verband der Ersatzkassen e. V. (vdek). Daten zum Gesundheitswesen: Versicherte. 2024. Available at: https://www. vdek.com/presse/daten/b_versicherte.html. Accessed: June 17, 2024.
39. Triefenbach L, Otto R, Bienzeisler J, et al. Establishing a data quality baseline in the AKTIN Emergency Department Data Registry - a secondary use perspective. Stud Health Technol Inform 2022;294:209-213.
Analysis of Emergency Department-based Intensive Care Units on Coding and Revenue
Michael H. Sherman, MD, MA*
Vincent L. Kan, MD, MSc†
Patric Gibbons, MD, MSCI†‡
Jacob Garrell, MD†
Martin A. Reznek, MD, MBA†
Boston University Chobanian & Avedisian School of Medicine, Department of Emergency Medicine, Boston, Massachusetts
University of Massachusetts Chan Medical School, Department of Emergency Medicine, Worcester, Massachusetts
University of Massachusetts, Department of Anesthesiology & Perioperative Medicine, Worcester, Massachusetts
Section Editor: León D. Sánchez, MD, MPH
Submission history: Submitted December 19, 2024; Revision received January 12, 2025; Accepted April 15, 2025
Electronically published September 27, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.41521
Introduction: Emergency department-based intensive care units (ED-ICU) address the increasing demand for critical care services and represent a transformative approach to the specialty’s management of critically ill patients within emergency medicine. However, data on their financial impact and operational effects remain limited.
Methods: We conducted a retrospective, quasi-experimental study at an urban, academic ED with approximately 90,000 annual visits. In July 2019, a nine-bed ED-ICU model, referred to as “Next Pod,” was implemented. We analyzed Current Procedural Terminology (CPT) coding data and professional revenue (charges billed and payments received) for 35 weeks before and after the intervention (November 2018–March 2020). The intervention involved repurposing a nine-bed ED area and adjusting physician and nursing staffing models. We compared critical and non-critical care CPT coding proportions and professional revenue using the Student t-test.
Results: During the study period, there were 38,283 ED visits pre-implementation and 36,424 visits post-implementation. Across the entire ED, critical care coding significantly increased following implementation (CPT 99291: 6.2 - 8.8% [total percentage increase of 41.94%]; 99292: 0.5 - 1.0% [total percentage increase of 100%]). Encounters where 99292 was billed multiple times increased by 128.1% (32 vs 73). Non-critical care coding (99282, 99283) decreased 23% (9.1% vs 7.0%, P< .001) / 29.6% (16.2 vs 11.4, P < .001), respectively. There was a non-statistically significant increase in 99284. Higher acuity codes (99285) increased by 10% (31.7% vs. 34.9%, P < .001). Average ED charges per visit increased by $40 (95% CI $37.2 – $45.5) post-implementation..
Conclusion: The implementation of an ED-ICU was associated with significant increases in critical care and high-acuity coding, as well as enhanced professional revenue. These findings suggest that ED-ICU models can improve both fiscal performance and operational efficiency. Further research is needed to explore the contributions of resource allocation, documentation improvements, and care practices to these outcomes. [West J Emerg Med. 2025;26(5)1192–1201.]
INTRODUCTION
The integration of intensive care units within emergency departments (ED-ICU) represents a transformative approach to the specialty’s management of critically ill patients.1,2 This innovation is grounded in the need for rapid, specialized care
amidst rising patient acuity and volume, alongside prolonged boarding times for critically ill patients in the ED.3 This has prompted several operational innovations, including different ED-ICU models within various EDs in the United States.4 First described in 2013, there are several different ED-ICU models
that seek to address the increasing demand for immediate critical care services in the ED.1 These units remain a growing area of ED quality improvement as each was designed to meet its specific institutional needs.4,5 While ED-ICUs are usually part of an ED, and thus not licensed or staffed as ICUs, they are generally focused on providing prompt acute care and increased resources during the early resuscitation and acute care afterward.
These ED-ICU models have been associated with a reduction in risk-adjusted, 30-day mortality among all ED patients, decreases in hospital and 24-hour mortality, and a reduction in ICU admissions from the ED, especially with a reduction in short-stay ICU admissions.6 The various ED-ICU models’ effects on improved healthcare delivery have been demonstrated.6-13 However, data are limited regarding the financial performance of these units, and concerns regarding their fiscal viability have been cited.7,14
Following a quality and flow improvement initiative supported by ED and hospital leadership to improve provision of care, our study site implemented a novel, hybrid-model resuscitation care unit as part of the ED, offering an opportunity to explore financial outcomes associated with such an ED operational change.4 Our primary objective in this study was to assess the effect of an ED-ICU model and its association with overall changes to ED professional services coding (Current Procedural Terminology [CPT], billing [charges generated], and realized fees for professional services [payments received]). We hypothesized that the integration of an ED-ICU model into the ED to care for high-acuity visits would result in a shift toward increased critical care CPT coding, resulting in increased professional revenue (both charges and payments).
METHODS
Study Design and Setting
We conducted a retrospective, quasi-experimental study at an urban, academic medical center in the US with approximately 90,000 annual ED encounters. The institutional review board at the University of Massachusetts Chan Medical School reviewed and approved this study.
Selection of Participants
On July 15, 2019, a nine-bed unit dedicated to the care of critically ill and other high-acuity patients was integrated into the adult section of the ED. The unit was referred to as the “Next Pod,” short for “North Pod Extension” given its geographic proximity to the “North Pod” of the ED. We examined CPT coding and billing data 35 weeks before and 35 weeks after the implementation of Next Pod (November 11, 2018–March, 15, 2020) of all patients ≥18 years of age who had at least one ED encounter. The study period was chosen because of the unanticipated effect of the COVID-19 pandemic on ED visits, which substantially affected the study site’s ED volume starting in March 2020 and limited the timeframe available for meaningful data collection and comparison that would otherwise have been included.
Population Health Research Capsule
What do we already know about this issue? ED-ICUs improve clinical outcomes, but their impact on billing practices and revenue generation has not been well characterized.
What was the research question?
Does implementing an ED-ICU change coding patterns and increase professional revenue?
What was the major finding of the study?
CPT 99291 to bill for critical care rose from 6.2% to 8.8%, 99292 from 0.5% to 1.0% (P < .001); charges/visit increased by $40 (95% CI $37.2 – $45.5, P < .001).
How does this improve population health? Observed increases in revenue generation may reflect better documentation and efficiency, supporting scalable, sustainable ED-models to improve healthcare delivery.
Measurements
Demographic variables collected included basic characteristics including age, sex (as identified by patient), race and ethnicity, and payor. We used the Emergency Severity Index (ESI) to adjust the results for disease severity variation between pre–Next Pod and post–Next Pod implementation groups.15 In accordance with best practices for retrospective chart review studies, as outlined by Worster and Bledsoe,16 this study adhered to key methodological standards. These included a clearly defined research question, standardized data collection protocols, a well-defined study population, and the use of validated measures such as CPT codes and professional revenue data. Data were sourced from a centralized administrative database to ensure consistency and accuracy.
Interventions
Following a dedicated multidisciplinary ED quality and flow Kaizen event to identify potential improvement initiatives, the study site implemented a dedicated nine-bed ED-ICU model in July 2019. The Next Pod was created by repurposing a smaller nine-bed area of the ED (~2,653 sq ft), with no physical space or floorplan change to ED layout. Capital improvements were limited, mainly comprised of the addition of a Pyxis MedStation. No specialized supplies were purchased or stocked in the Next Pod.
The Next Pod unit was continuously staffed by one attending emergency physician and one postgraduate year 2 or
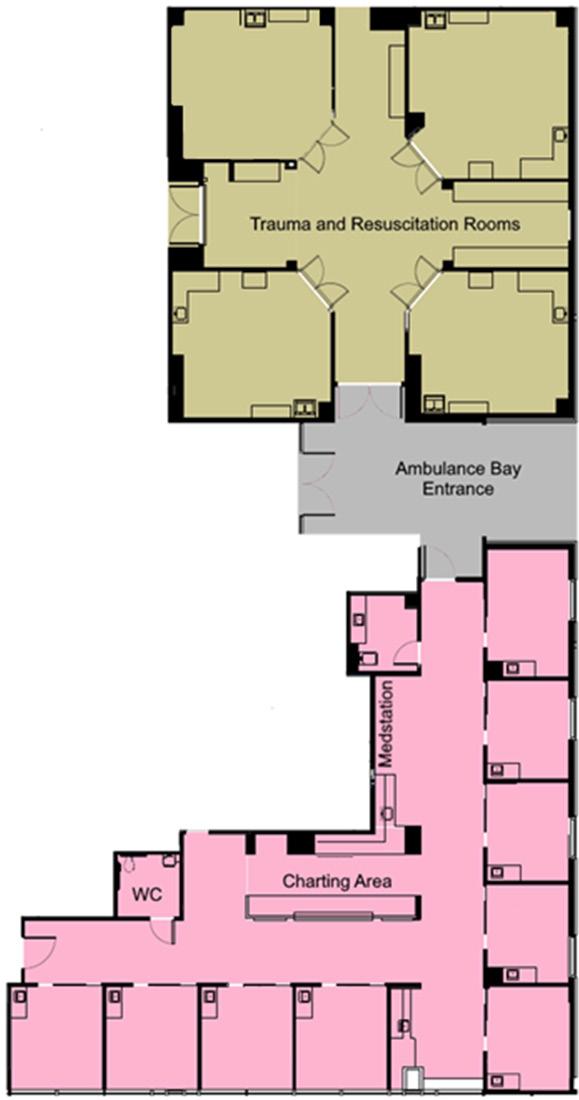
Pod, including resuscitation and trauma rooms. Note that Next Pod area is the ED-ICU. Next Pod, North Pod Extension; WC, water closet; ED-ICU, emergency department-based intensive care units.
3 emergency medicine (EM) resident. This represented an increase in staffing by an additional attending 24 hours per day. Only two ED faculty were board-certified in critical care and EM during this period. The EM-critical care faculty had a higher percentage of Next Pod shifts than non-critical care faculty, although the difference was minimal compared to total coverage. The overall daily resident staffing remained relatively unchanged by adjusting resident staffing models to optimize learning opportunities and in a budget-neutral fashion. This physician team would also respond to cover a dedicated resuscitation area (trauma bays) of the ED to perform the initial evaluation and management of trauma, ST-elevation myocardial infarction (STEMI) and acute stroke
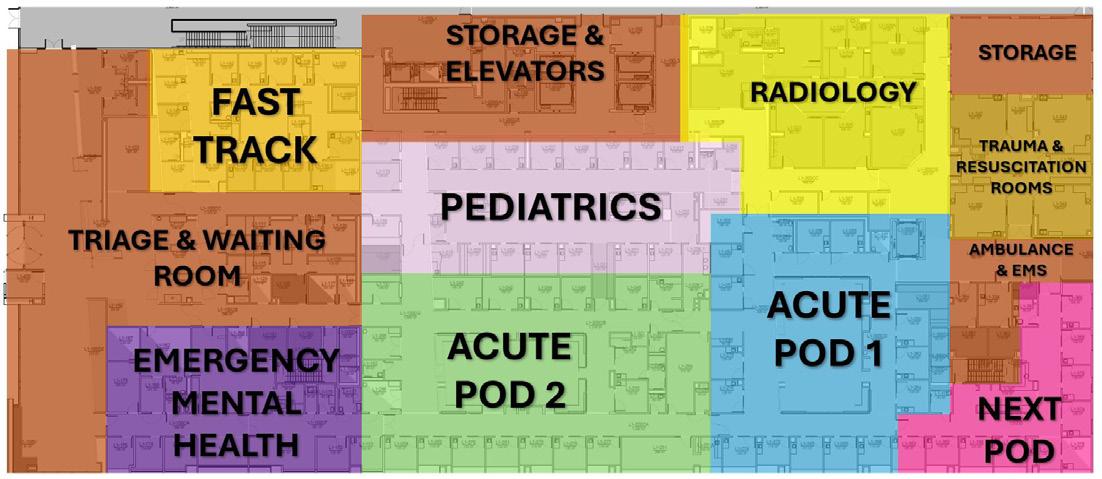
Figure 2. Layout of the study site emergency department. Total ED is 62,264 sq/ft. Next Pod is 2,653 sq/ft (occupying 4.26% of the total ED square footage). Note that Next Pod area is the ED-ICU.
EMS, emergency medical services; Next Pod, North Pod Extension; ED-ICU, emergency department-based intensive care units.
activations as well as patients with cardiac arrest in the field.
The Next Pod team managed high-acuity traumas, STEMIs, and strokes, providing care in the trauma bay until definitive treatment (eg, operating room, interventional radiology, catheterization lab), and then transitioning patients to Next Pod for continued monitoring, or handing off to other ED pods as needed; responsibility for patients remained with the Next Pod team until patients were physically transferred to other ED areas. On resident educational days, the ED-ICU was staffed by the ED attending without a resident for six hours. The unit was staffed with a minimum of three nurses, representing an increased patient-to-nurse ratio at a minimum of 3:1. Generally, patient-to-nurse ratios were ~5:1 in other areas of the ED. No additional training was required for nursing staff to care for patients in Next Pod; however, in general more senior/experienced ED nurses were assigned to work in the unit.
This Next Pod functioned as an integral part of the ED, and patients were triaged to or transferred to and from other parts of the ED depending on acuity and changes in clinical status. No specific conditions, treatments, or diagnoses mandated triage or transfer to Next Pod. In general, Next Pod cared for high-acuity medical and critical polytrauma patients presenting to the study site ED. Many of these patients were acutely ill on a background of chronic illness and often carried significant medical comorbidities typical of a tertiary- care facility. Due to limitations in the dataset abstracted from the billing network, and technical constraints of the electronic health record, we were unable to accurately track patients who were transferred into Next Pod from other areas of the ED. However, this area primarily received patients with Emergency Severity Index (ESI) scores of 1-2, and occasionally 3. Patients were either directly triaged to Next Pod upon arrival based on the severity of illness or were transferred there after being identified as critically ill during their ED course. Thus, the primary intervention was a model that increased nursing ratios and physician coverage, enabling
Figure 1. Layout of Next
*Pre-Next Pod dates: November 11, 2018 – July 14, 2019 (35 weeks).
*Post-Next Pod dates: July 15, 2019 – March 15, 2020 (35 weeks).
Note that Next Pod area is the ED-ICU.
ESI, Emergency Severity Index; Next Pod, North Pod Extension; EDICU, emergency department-based intensive care units.
more intensive patient management in a dedicated space that followed standard EM principles, focusing on acute care to optimize treatment for high-acuity patients and maintain ED workflow. No formal coding or billing educational program was implemented for the Next Pod initiative before, during, or after implementation. The department did engage in regular reviews of billing code distributions at staff meetings related to relative value unit (RVU) data; however, this was a longstanding initiative and was consistent and unchanged during and around the study period.
The study site was a Level 1 trauma center, a certified Advanced Comprehensive Stroke Center, and a percutaneous coronary intervention center (PCI). We identified an affiliated community ED in close geographic proximity (1.7 miles away) to serve as a natural control group for comparison variation between pre-Next Pod and post-Next Pod implementation groups concurrently. This community ED was part of the same hospital system as the study site but not a trauma center. The control and study EDs were located on separate but affiliated hospital campuses. Patients evaluated at the control hospital who required acute stroke, PCI, or trauma intervention and management were promptly transferred to the
Figure 3 Percentage of ED encounters with critical care time billed at study site before and after the implementation of Next Pod. Note that Next Pod area is the ED-ICU.
CC, critical care; ED, emergency department; Next Pod, North Pod Extension; ED-ICU, emergency department-based intensive care units.
study hospital campus for those services. On average, <5% of patients evaluated at the control campus ED required transfer to the study hospital campus. The control hospital had inpatient ICU services and most subspecialty services. Most ED patients were admitted to their respective hospitals, except those requiring management of acute stroke, acute PCI, or acute trauma services. Patients with acute transplant-related or acute oncologic issues may have been transferred to the study campus, although these cases were also rare. The natural control group ED was staffed by the same academic ED with nearly all the physicians practicing at that site also practicing at the primary study site.
Outcomes
The primary outcome of this study was the change in billing of critical care CPT codes (99291, 99292) following the implementation of Next Pod. Secondary outcomes included changes in billing of non-critical care EM CPT codes (99281–99285) and overall professional revenue. We compared average billing (charges generated per ED visit) and payments (collections received) between the pre- and postNext Pod implementation cohort to evaluate changes in ED professional revenue over time.
Overall, there were minor Centers for Medicare & Medicaid Services reimbursement changes from 2018-2020 during the study period. Total RVUs in 2018 and 2019 remained stable aside from a 0.4% decrease in 99291 and 99292 total RVUs. Between 2019 and 2020, there was an upward trend in 99281-4 billing, but 99285 work RVU remained unchanged. Overall reimbursement per RVU remains complex and is addressed in the Supplement.
Table 1. Patient characteristics.
Table 2. Pre- vs post-Next Pod implementation comparison.
data
Pre-ED-ICU dates November 11,2018 – July 14, 2019 (35 weeks).
Post-ED-ICU dates: July 15, 2019 – March 15, 2020 (35 weeks).
*Represents encounters where patients had at least one 99292 charge subsequent to 99291. 99292 charges only counted once, even if charged > 1 time during that encounter.
†Multiple 99292 charges are allowed during a 24-hour period.
Note that Next Pod area is the ED-ICU.
ED, emergency department; CPT, Current Procedural Terminology; CC, critical care; Next Pod, North Pod Extension; ED-ICU, emergency department-based intensive care units.
However, given the timeframe of small changes, this was felt not to substantially affect outcomes. Inflation was not accounted for as there is no established inflation adjustment in the healthcare sector7; it is also adjusted for in annual CMS RVU reimbursement changes (Supplement). Per the US Bureau of Labor Statistics, the consumer price index inflation between November 2018–March 2020 was 2.4%. Given this short period and outcomes, we believe inflation did not substantially affect outcomes.
Analysis
Descriptive statistics were presented as means ± standard deviations for continuous variables, and categorical variables as percentages. We compared proportions of CPT codes and professional fee revenue before and after implementation. We compared the proportion of each evaluation and management (E/M) code between before and after Next Pod implementation using a series of 2x2 chi-square tests. For each code (99281–99285, 99291, 99292), we tested whether its frequency differed significantly between the two groups. Differences in revenue (via charges and payments, total and per encounter) were examined using the Student t-test. Two-tailed values of P < 0.05 were considered statistically significant. We performed data analysis performed using STATA/MP v17 (StataCorp, College Station, TX).
RESULTS
There were 38,283 ED visits pre-intervention compared to 36,424 post-intervention during the 70-week total study period. During the post-implementation period, 5,159 patients were triaged initially to the Next Pod, for an average of 19.8 patients per day. Due to limitations in the electronic health record, this did not account for patients transferred to the Next Pod later in their ED course; so, it underestimates the total number of patients cared for in the unit. The mean ESI among all patients before and after implementation (2.84 pre vs. 2.85 post) were similar. The natural control site, an affiliated in-system hospital in close geographic proximity, showed no statistically significant changes in the primary outcome of critical-care CPT billing codes or percentage of total ED encounters with criticalcare billing codes pre and post implementation (2.89 vs 3.07) (Figure 4).
In the primary outcome of critical care CPT billing codes at the study site, we found a significant increase in both 99291 and 99292. In the pre-period, 6.2% and 0.5% of all CPT codes billed were 99291 and 99292, respectively. In the post-period, 8.8% and 1.0% of all CPT codes billed were 99291 and 99292, respectively. The implementation of Next Pod resulted in a 2.6% net increase (95% CI [confidence interval] 2.2-2.9%) of 99291 billed (total percentage increase of 41.94%) and a net
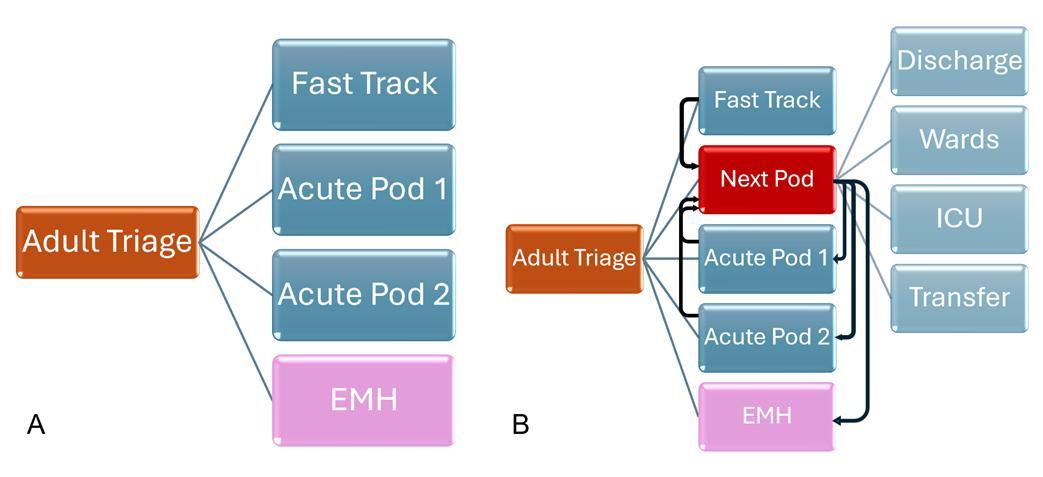
Figure Flow through the emergency department pre- and post-implementation of the Next Pod. Side A shows pre implementation, when trauma/resuscitation rooms were generally covered by Acute Pod 1. Side B shows post implementation where Next Pod generally covered the trauma/resuscitation rooms. Patients were triaged to the Next Pod primarily, or if deemed to need increased critical care resources, were transferred from other parts of the ED. If and when patients were stabilized or downgraded from the perspective of ED critical care resources, patients are then able to be discharged, cleared for EMH, or moved out to the main ED or hospital floors. N ote that Next Pod area is the ED-ICU. EMH, emergency mental health; ICU, intensive care unit; Next Pod, North Pod Extension; ED-ICU, emergency department-based intensive care units.
increase of 0.5% (95% CI 0.4-0.6%) of 99292 billed (total percentage increase of 100%). Encounters where 99292 was billed multiple times increased by 128.1% (32 vs 73).
In the secondary outcomes of non-critical care CPT codes, we noted a decline in lower complexity codes, and an increase in higher complexity codes. Compared to the pre-period, the
total percentage of 99282 decreased by 23% (9.1% vs 7.0%, P < .001) and 99283 decreased by 29.6% (16.2 vs 11.4, P < .001).
At the same time, the percentage of 99285 increased by 10% (31.7% vs. 34.9%, P < .001) in the post-period. There was a non-statistically significant increase in 99284. No changes were seen in the proportion of 99281 billed.
Figure 4. Percentage of emergency department encounters with critical care time billed at natural control site before and after the implementation of Next Pod. Note that Next Pod area is the EDICU.
CC, critical care; Next Pod, North Pod Extension; ED-ICU, emergency department-based intensive care units.
In review of charges and payments, we found a statistically significant increase in both post- implementation. We observed a mean increase of charges per encounter of $40.0 (95% CI 37.2 - 45.5, P < .001) following the opening of the unit, a 10% increase. We observed a mean increase of payments per encounter of $11.9 (95% CI 10.5 - 13.3, P < .001) of all ED encounters following the opening of the unit. There was a $37 net increase per critical care encounter (4% total increase).
Although the changes in critical care average charges were not statistically significant (P = .08), they did indicate an increased trend post- implementation of the ED-ICU. These trends were noted despite the post-group having a decline in total ED encounters of 4.85% (38,283 vs. 36,424).
DISCUSSION
In this study we sought to contribute to improved understanding of the fiscal impact of ED-ICU models by examining professional coding and revenue. We found that the integration of our Next Pod unit into the existing ED infrastructure was associated with an increase in the primary outcome of critical care CPT coding (99291, 99292), as well as secondary outcomes of increased proportion of higher complexity, non-critical care coding (higher 99285, lower
99282 and 99283). Associated with this was an increase in charges and payments per encounter for all ED encounters. Charges also increased per encounter for critical care, likely representing an increase in subsequent critical care coding (99292) and by encounters with multiple 99292 codes. This points toward the driver of increased revenue being an increased proportion of high complexity and critical care coding. Our observations in total provide evidence that implementation of these units can result in increased professional revenue generation (both charges and payments).
The significant rise in 99291 coding (initial critical care) may indicate operational enhancements within the ED,—by isolating the most critically ill to be cohorted by acuity while allowing other ED areas to better focus on throughput. This allocation of resources could also allow for more focused care and improved documentation accuracy. This supposition is supported by the trend toward higher acuity EM coding across the ED during the post-implementation period. Following implementation of the unit as part of the local process improvement Plan-Do-Study-Act cycle work, physicians and nurses reported that in the lower acuity areas of the ED, staff perceived that they could better balance their attention across all their patients when not burdened with a critically ill patient requiring prioritization of their attention. Whether the increase in 99291 coding reflected more resources dedicated to critical care or more time and attention for documentation practices across the ED, not just the Next Pod, remains unclear.
The increase in 99292 coding (subsequent critical care) in the post-implementation period represents a revenue stream that appeared to have been underused prior. In addition to single 99292 codes, the increase in ED encounters with multiple 99292 codes likely represented increased longitudinal critical care services provided in the ED. Gunnerson et al demonstrated the effect of an ED-ICU on improved patient-centered outcomes and resource utilization, and is likely reflective of increased bedside care and recognition of the longitudinal treatment of the critically ill.5,6,17 We surmise that the increase in 99292 coding likely reflected additional attending time spent in care of these patients, although it is possible that change in documentation practices may also have occurred with the unit’s implementation (more time to document or heightened awareness of critical care documentation). We suspect both contributed, but considering prior reports, additional time spent by the attendings with these patients was likely a significant component. If so, this increased capture of 99292 billing codes represents a direct acknowledgment of the continuous care of critically ill patients and demonstrates appropriate reimbursement for those services provided in an ED-ICU setting that have been demonstrated to improve outcomes.6
Analysis also revealed a shift in non-critical care E/M CPT codes, with a significant decrease in lower complexity code billing not solely explained by the increase in critical care coding. The cause for greater 99285 (higher complexity) coding and billing remains unclear. We have no reason to suspect a change in
the patient population or coding and billing practices during the period. The ESI, a surrogate marker for complexity, remained stable during the study period, and there were no departmental interventions related to coding and billing practices.15 It is possible this reflected the seasonality of ED presentations, although this remains unclear.18,19 The rise in higher complexity billing codes after ED-ICU implementation may reflect how exposure to a clinical environment might subtly shape physician behavior.20,21 This trend may also be influenced by better documentation habits over time vs the seasonal variability in ED visits. As the charge structure remained unchanged, the shift in coding likely reflects a real change in documentation practices rather than financial motivation.
The shift in coding may have reflected improved operations within the ED overall, not just in the care of critically ill patients. This is consistent with prior reports of other acuity-based, split-flow models such as practitioner in triage and/or low acuity “fast-tracks,” which have been associated with improved revenue generation, efficiency, and resource utilization.22,23 In effect, an ED-ICU-type unit functions as a third-line split flow: triaging or moving patients with high-acuity, resource-intensive conditions to a dedicated area with a different resource allocation. From an operational improvement standpoint, the idea that this would improve effectiveness makes intuitive sense.
Regardless of causality, our findings of increased professional fee generation associated with implementation of the Next Pod unit suggest a positive fiscal impact of ED-ICU care models. The fiscal gains highlighted by our study, particularly the 10% increase in charges per ED encounter ($40.0), signal a notable enhancement in the ED’s revenue stream of $11.9 payments per encounter. Assuming 90,000 encounters/year, this would result in an estimated increase of $1 million per year from professional fee payments alone. Of note, our investigation did not evaluate facility fee coding and billing, but in general these correlate with professional coding and are a multiple greater than the professional fees.24-26 Furthermore, ED-ICU care models have been shown to increase hospital transfer acceptance rates and provision of critical care and surgical services.11,27 A comparison study found a decrease in direct costs per ED encounter by 22.1% among critically ill patients, and those authors suggested that providing early, coordinated critical care in an ED-ICU could lead to overall cost reductions by preventing disease progression and complications.7 Therefore, we suspect that there was additional revenue and benefits to the hospital associated with the implementation of the unit not measured in our study.
Our investigation focused on charges and payments and did not examine cost association. The literature remains sparse in this regard. The implementation of an ED-ICU model has previously been associated with decreased, risk-adjusted 30-day mortality and reduction in ICU admissions, leading to an overall improvement in resource utilization.6 Prior studies by Bassin et al in a foundation-funded ED-ICU demonstrated that their ED-ICU was cost neutral, although their unique funding structure limits generalizability and applicability to other centers.7,14 Professional
billing analysis showed an increase in RVUs per encounter due to the provision of intensive care, but no significant change in overall E/M CPT coding ED billing when excluding ED-ICU encounters and no shift in billing practices. However, there was an increase in net revenue and direct margins per patient encounter post-implementation, suggesting financial benefits for the hospital.7
To our knowledge, our investigation and that of Bassin et al are the only two studies to report on the fiscal impact of implementating an ED-ICU. However, direct comparisons between the results of the two are difficult given that the two units operate differently on multiple levels. The unit studied by Bassin et al was foundation funded.6,7,14 In addition, it was separate from the main ED, with intensive care patients initially seen by traditional ED staff before transitioning to the unit. Our study site unit received no external funding and functioned as an integral part of the ED. Patients were either triaged directly to Next Pod for initial assessment or transferred as needed from the main ED. If, and when, patients no longer required critical care-level resources, they were then moved to other areas of the main ED. Thus, there appeared to be greater bidirectional flow than that in the unit studied by Bassin et al. Accordingly, we hypothesize that our observed shift of E/M coding and overall ED billing compared to Bassin et al may have been, in part, a result of improved overall ED operations from the integration of an ED-ICU-type unit within a ED, as opposed to a unit that functioned as a segregated, more independent unit.
With regard to the foundation support for the unit studied by Bassin et al, their unit grew from significant capital investment and increased staffing.7 In the case of our study site, the unit grew organically from our generalized, ongoing ED quality and flow improvement initiatives and likely had less financial investment. While there were costs associated with increased staffing (not measured in this investigation), the repurposing of an already functional area within the ED for dedicated high-acuity care required minimal capital investment. This model may represent one more easily adopted by EDs to address the problems of increased acuity and negative effects of increased ICU boarding,28-30 and could be feasibly implanted by an ED that has a small accessory space/unit with flexible usage.
Operational efficiency can be improved by either increasing RVUs through higher level CPT coding or enhancing patient throughput.31 Using CPT codes as a surrogate marker for RVUs per hour, a recognized measure of ED operational effectiveness,32-35 the data indicated substantial gains in performance, achieved without altering the ED’s physical footprint. By this measure, the unit, while occupying only 4.26% of the total ED square footage, improved overall efficiency.31 Additional studies will be required to address other fiscal effects of such units including the cost associated with increased staffing ratios, revenues generated from facility fees, costs associated with potential reduction in overall hospital length of stay, realization of cost-savings associated with changes in overall operational efficiencies of the ED,
potential indirect cost and revenue benefits related to medical legal risk changes, and patient experience changes.
LIMITATIONS
Because the Next Pod was created in a single-site, academic, tertiary-care center; its external reproducibility is unknown.27 Since the unit was integrated organically into an already functional area of the ED, accurately isolating the increased staffing costs for meaningful analysis was not feasible. As a retrospective, quasi-experimental study, our investigation did not involve randomization, limiting its ability to clearly demonstrate without possible bias a causal association between an intervention and outcome. Selection bias is also possible via geographic bias as clinicians were treating patients in an ED-ICU setting, although no formal billing education was undertaken. Reporting bias is prevalent in quasi-experimental studies.
This study was subject to the temporal limitations of the COVID-19 pandemic, which substantially affected the study sites ED volume starting in March 2020, limiting timeframe available for data collection that would otherwise have been included. This limitation did not account for the seasonality of ED presentations; however, the control site showed no change in the primary outcome of critical care billing during the study period. It is important to note that the study’s trends continue to be noted after ED volumes have returned to pre-COVID-19 levels and is an active area of ongoing, internal monitoring.
Due to technical electronic health record limitations, patient initial-triage destination was available, but flow in and through the Next Pod could not be differentiated from flow through the entire ED; thus, this study represents the effects on the entire department rather than just those treated in the Next Pod. The flow into, through, and out of an ED-ICU-type unit to optimize efficiency and resource utilization is an integral part of building the operational knowledge base of ED-ICU operations.
CONCLUSION
The ED-ICU model represents a promising approach to operational and quality improvement in emergency medicine and has been associated with improved patient outcomes. Fiscal sustainability is unknown due to the paucity of literature and questionable generalizability in previous models. In our evaluation of an organically developed ED-ICU, we observed an increased number of critical care charges, higher professional fee revenue, and improved documentation efficiency. Further studies, particularly those examining costs and facility fee revenue, are needed to fully assess the financial performance of an emergency department-based intensive care unit.
Address for Correspondence: Michael H. Sherman, MD, MA, Emergency Medicine & Critical Care Medicine, Department of Emergency Medicine, Boston University Chobanian & Avedisian School of Medicine, Boston Medical Center, Boston, Massachusetts. 800 Harrison Ave, BCD Building, Boston, MA 02118. Email: michael.sherman@bmc.org.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Sherman et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Weingart SD, Sherwin RL, Emlet LL, et al. ED intensivists and ED intensive care units. Am J Emerg Med. 2013;31(3), 617-620.
2. Mermiri M, Mavrovounis G, Chatzis D, et al. Critical emergency medicine and the resuscitative care unit. Acute Crit Care. 2021;36(1), 22-28.
3. Kiekkas P, Tzenalis A, Gklava V, et al. Delayed admission to the intensive care unit and mortality of critically ill adults: systematic review and meta-analysis. Biomed Res Int. 2022;(1), 4083494.
4. Leibner E, Spiegel R, Hsu CH, et al. Anatomy of resuscitative care unit: expanding the borders of traditional intensive care units. Emerg Med J. 2019;36(6), 364-368.
5. Weingart 2 SD, MD FCCM. EMCrit Wee – first study of the benefits of an EDICU. EMCrit Blog. Published September 10, 2019. Available at: https://emcrit.org/emcrit/ec3-study/. Accessed: December 20, 2023.
6. Gunnerson KJ, Bassin BS, Havey RA, et al. Association of an emergency department–based intensive care unit with survival and inpatient intensive care unit admissions. JAMA Netw Open. 2019;2(7), e197584-e197584.
7. Bassin BS, Haas NL, Sefa N, et al. Cost-effectiveness of an emergency department–based intensive care unit. JAMA Netw Open. 2022;5(9), e2233649-e2233649.
8. Powell E, Sahadzic I, Najafali D. Is the critical care resuscitation unit sustainable: a 5-year experience of a beneficial and novel model. Crit Care Res Pract. 2022;(1), 6171598.
9. Haa NL, Nafday A, Cranford JA, et al. Implementation of a multidisciplinary care pathway via an emergency department-ICU to improve care of emergency department patients presenting with leukostasis. Crit Care Explor. 2020;2(2), e0084.
10. Doan J, Perez S, Bassin BS, et al. Impact of emergency departmentbased intensive care unit on outcomes of decompensating boarding emergency department patients. J Am Coll Emerg Physicians Open. 2023;4(5), e13036.
11. Tran QK, Najafali D, Cao T, et al. Examining predictors of early admission and transfer to the critical care resuscitation unit. West J Emerg Med. 2023;24(4), 751.
12. Tran QK, O’Connor J, Vesselinov R, et al. The critical care resuscitation unit transfers more patients from emergency departments faster and is associated with improved outcomes. J Emerg Med. 2020;58(2), 280-289.
13. Hickey S, Mathews KS, Siller J, et al. Rapid deployment of an
emergency department-intensive care unit for the COVID-19 pandemic. Clin Exp Emerg Med. 2020;7(4), 319.
14. Kurz MC & Hess EP. Quality is not the only part of the emergency department–based intensive care unit value equation. JAMA Netw Open. 2019;2(7), e197570-e197570.
15. Gilboy N, Tanabe P, Travers D, Rosenau AM. (2012). Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook. 12th ed. Rockville, MD: Agency for Healthcare Research and Quality. AHRQ Publication No. 12-0014:15-25.
16. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005 Apr;45(4):448-51.
17. Morgenstern J. What can we learn from the ED ICU model? First10EM Blog. Published December 9, 2019-Updated November 28, 2019. Available at: https://first10em.com/what-can-we-learn-fromthe-ed-icu-model/. Accessed December 20, 2023.
18. Kakara RS, Moreland BL, Haddad YK, et al. Seasonal variation in fall-related emergency department visits by location of fall - United States, 2015. J Safety Res. 2021 Dec;79:38-44.
19. Lane M, Ebelt S, Wu Z, et al. Time-series analysis of temperature variability and cardiovascular emergency department visits in Atlanta over a 27-year period. Environ Health. 2024 Jan 23;23(1):9.
20. Ly DP, Shekelle PG, Song Z. Evidence for anchoring bias during physician decision-making. JAMA Intern Med. 2023 Aug 1;183(8):818-823.
21. Lee RY, Kross EK, Downey L, et al. Efficacy of a communicationpriming intervention on documented goals-of-care discussions in hospitalized patients with serious illness: a randomized clinical trial. JAMA Netw Open. 2022 Apr 1;5(4):e225088.
22. Franklin BJ, Li KY, Somand DM, et al. Emergency department provider in triage: assessing site-specific rationale, operational feasibility, and financial impact. J Am Coll Emerg Physicians Open. 2021;2(3), e12450.
23. Cheng I, Castren M, Kiss A, et al. Cost-effectiveness of a physiciannurse supplementary triage assessment team at an academic tertiary care emergency department. CJEM. 2016;18(3), 191-204.
24. McCarthy, M. (2014). Hospital prices for outpatient services far exceed those of community providers, US study finds. BMJ. 2014;348:g4322. Accessed July 25, 2025.
25. Norbeck TB. Drivers of health care costs: a Physicians Foundation white paper-second of a three-part series. Mo Med. 2013;110(2), 113.
26. Reschovsky JD, and White, C. Location, location, location: hospital outpatient prices much higher than community settings for identical services. NIHCR. 2014. Available at: https://www.nihcr.org/analysis/ improving-care-delivery/prevention-improving-health/hospitaloutpatient-prices/. Accessed March 1, 2024.
27. Scalea TM, Rubinson L, Tran Q, et al. Critical care resuscitation unit: an innovative solution to expedite transfer of patients with timesensitive critical illness. J Am Coll Surg. 2016; 222(4), 614-621.
28. Mohr NM, Wessman, BT, Bassin B, et al. Boarding of critically ill patients in the emergency department. Crit Care Med. 2020;48(8), 1180-1187.
29. Mathews KS, Durst MS, Vargas-Torres C, et al. Effect of emergency department and ICU occupancy on admission decisions and outcomes for critically ill patients. Crit Care Med. 2018;46(5), 720-727.
30. Shibata J, Osawa I, Fukuchi K, et al. The association between time from emergency department visit to ICU admission and mortality in patients with sepsis. Crit Care Explor. 2023;5(5), e0915.
31. Schweizer ML, Braun BI, Milstone AM. Research methods in healthcare epidemiology and antimicrobial stewardship—quasiexperimental designs. Infect Control Hosp Epidemiol. 2016;37(10), 1135-40.
32. Perotte R, Hajicharalambous C, Sugalski G, et al. Characterization of
electronic health record documentation shortcuts: Does the use of dotphrases increase efficiency in the emergency department? AMIA Annu Symp Proc. 2022 Feb 21;2021:969-978.
33. Bobb MR, Ahmed A, Van Heukelom P, et al. Key high-efficiency practices of emergency department providers: a mixed-methods study. Acad Emerg Med. 2018 Jul;25(7):795-803.
34. Addesso LC, Nimmer M, Visotcky A, et al. Impact of medical scribes on provider efficiency in the pediatric emergency department. Acad Emerg Med. 2019 Feb;26(2):174-182.
35. Bang S & Bahl A. Impact of early educational intervention on coding for first-year emergency medicine residents. AEM Educ Train. 2018 May 25;2(3):213-220.
Telehealth Emergency Department Transition-of-care Program: A Value-based Innovation
Allyson Kreshak, MD*†
Itzik Fadlon, PhD‡
Karna Malaviya, MA‡
Vaishal Tolia, MD MPH*†
Lindsey Pierce, MSN, RN*
Theodore Chan, MD†
Parag Agnihotri, MD*
Ming Tai-Seale, PhD, MPH*§||
Section Editor: Laura Walker, MD
University of California, San Diego Health, Population Health Services Organization, San Diego, California
University of California, San Diego Health, Department of Emergency Medicine, San Diego, California
University of California, San Diego, Department of Economics, San Diego, California
University of California, San Diego Health, Department of Family Medicine, San Diego, California
University of California, San Diego Health, Department of Medicine, Division of Biomedical Informatics, San Diego, California
Submission history: Submitted December 20, 2024; Revision received May 14, 2025; Accepted May 20, 2025
Electronically published September 1, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.41524
Introduction: Our Emergency Department (ED) and Population Health Services Organization developed a telehealth ED-transition of care program (TOC) for patients insured through valuebased contracts. This study’s goal was to determine the association of our ED-TOC on ED revisits. We hypothesized that the ED-TOC would decrease ED revisits.
Methods: This was a retrospective cohort study conducted between August 1, 2021 and July 31, 2023 at two EDs where an ED-TOC is available. Included were ED visits among discharged Medicare beneficiaries that occurred one year before and after the launch of the ED-TOC program. ED visits involving Medicaid beneficiaries served as the control. A difference-in-differences (DID) strategy was used to compare Medicare and Medicaid visits. The primary outcome measure was the association of the program with 14- and 30- day ED revisit rates. Secondary outcomes were the association of the ED-TOC with post-discharge PCP visits and hospitalizations and estimated costsavings associated with the program.
Results: Our sample size was 23,696 ED encounters (13,553 treatment group and 10,143 control group). At 14-days after ED discharge, Medicare beneficiaries were associated with a 1.77% decrease in the rate of ED revisits in the year after the ED-TOC launch relative to the control (p=0.03) or a 15.8% reduction relative to baseline (11.2% to 9.4%). At 14-days after ED discharge, PCP visits were associated with a 1.51% increase in the year after program launch relative to the control (p=0.03) or a 10.3% increase relative to baseline (14.6% to 16.1%). No difference was associated with Medicare beneficiaries’ ED revisits or hospitalizations at 30-days. PCP visits were associated with a significant increase at 30-days (p=0.005).
Conclusion: An ED-TOC is associated with a reduction in Medicare ED revisits during days 8-14 after an index ED visit but not during days 1-7 days or at 30-days. Cost savings over a 24-week period are conservatively calculated to be $215,779. [West J Emerg Med. 2025;26(5)1202–1210.]
INTRODUCTION
Emergency department (ED) follow-up care after discharge may ensure that a patient’s health issues addressed in the ED
are appropriately managed. In the United States in 2021, an estimated 140 million ED visits occurred, where 75% were dispositioned to outpatient follow-up.1 Adults ≥ 65 years of
age comprise 18% of these visits, and 65% of this age group are discharged to home.2 ED care transitions for older adults are rife with limited patient understanding of their clinical condition and suboptimal communication.3 Complicating the situation, ED discharge instructions are poorly understood with limited rates of adherence to prescription medications, followup plans, and reasons to return to the ED.4 Not surprisingly, ED revisits occur due to care issues relating to diagnosis, treatment, disease progression, challenges with securing follow-up care, non-compliance, and imperfect communication during the ED encounter.6-10 The percentage of patients who revisit the ED varies widely with estimates of up to 7.5% at 72 hours, 8.5% within seven days, 11.5% within 14 days, and 20% within 30 days.11,12 These ED revisits lead to increased costs, increased ED patient volumes, mortality, and treatment delays.13
Prevention of ED revisits and enhancing quality of care is a focus of ED transition-of-care programs (TOC).14 Models of ED-TOCs largely consist of telephone follow-up and have had varied outcomes. Two ED-TOCs feature nurse callbacks15 and automated callbacks with the option to speak with an advanced practice clinician;13 both programs resulted in decreased ED revisits at seven days. Additionally, an ED-TOC involving consultation with an ED nurse was associated with decreased Medicare expenditures.16 Other ED-TOCs with non-physician practitioner telephone follow-up, however, did not impact ED revisits at 30 days.17-19 Additionally, ED follow-up visits with primary care physicians (PCP) conducted via telehealth were associated with higher ED revisits at 30 days compared to inperson visits.20
The potential of these ED-TOCs to influence a patient’s care is important for improving quality of care and for addressing broader healthcare challenges. Emergency departments are experiencing increases in patient volume and acuity,2,21,22 attributed largely to a growing and aging population and inadequate access to care,4,22 while also facing crowding and boarding issues.23,24 Additionally, hospitals face rising costs, inpatient capacity constraints, and staff shortages.25,26 Programs that safely transition patients out of the ED have the potential to mitigate ED revisits and potentially hospitalizations and to enhance care management.14 The previously described ED-TOCs with mixed ED-revisit impact feature different modalities for ED follow-up and involve nurses, paramedics, and PCPs. The ideal training level of the practitioner providing TOC services remains in question as does the best TOC system. Our ED-TOC builds upon this work and provides emergency physician-led telehealth visits coupled with robust care navigation to eligible patients discharged from the ED.
The purpose of this study was to determine the association of our ED-TOC program involving emergency physician-led telehealth visits and robust care navigation with ED revisits.
METHODS
This quality improvement project was deemed non-human subjects research and exempt from institutional review board
Population Health Research Capsule
What do we already know about this issue? Revisits to the ED are associated with increased costs, mortality, and treatment delays. Previous models of ED transitions of care (TOC) have had varied impact on revisits.
What was the research question?
What is the association of an ED-TOC program involving physician telehealth visits and care navigation with ED revisits?
What was the major finding of the study? Medicare patients were associated with a 1.77% drop in the ED revisit rate, or a 16% drop in ED revisits (P = .03).
How does this improve population health?
An ED-TOC program with accountability for cost and quality may enhance care by decreasing the number of ED revisits.
review by the University of California San Diego Aligning and Coordinating Quality Improvement, Research and Evaluation Committee.
Study Design and Setting
In this retrospective cohort study we used data from two EDs in an academic health system: ED1 is a suburban, quaternary-care hospital ED; and ED2 is an urban hospital ED. The combined census is 89,000 patients per year with a discharge rate of 76%. Our health system’s Population Health Services Organization (PHSO) is a team focused on improving the health of specific populations through data analysis, targeted interventions, and collaboration with clinicians and community partners to achieve better health outcomes and reduce healthcare costs. The PHSO is the delegated entity for health plan oversight for our health system’s attributed health maintenance organization (HMO) patients, specifically commercial and Medicare Advantage plans. The PHSO is responsible for delivering high-quality, cost-effective care (ie, value-based care) for these insured patients. In this model, fixed payments per patient per month are available to the PHSO regardless of the number of services provided, and quality standards are established. Medicaid contracts are not part of the PHSO. The percentage of patients attributed to the PHSO is approximately 11% at ED1 and 7% at ED2.
Selection of Participants
Included in this study were beneficiaries covered by
Kreshak
Medicare Advantage plans, traditional fee-for-service Medicare, and Medi-Cal (California’s Medicaid program) who were discharged from either ED in the year before and year after the launch of the ED-TOC program. Traditional Medicare patients were included given that the Centers for Medicare & Medicaid Services (CMS), in a recent report, tied 90% of traditional fee-for-service Medicare payments to value.27 Importantly, this focus on value incentivizes health systems and clinicians to concentrate on care quality and costefficiency rather than just volume of services provided.
Intervention
In July 2022, our ED-TOC was established. This program is a collaboration between our ED and our health system’s PHSO. Patients eligible for the ED-TOC are those PHSOattributed ED patients and patients insured with traditional fee-for-service Medicare who are discharged from the ED. The ED-TOC staff contacts patients in the ED for participation and enrollment in the transition-of-care program or within 72 hours after ED discharge. Within 24 hours of enrollment, patients receive a telehealth visit with one of our ED-TOC physicians (an emergency physician designated to this role). The EDTOC physicians underwent eight hours of combined telehealth training and program-specific training prior to participation in the program. The telehealth visit addresses the patient’s acute medical issue for which s/he presented to the ED.
Depending on clinical needs, which are determined while the patient is in the ED or during the ED-TOC telehealth visits, patients may also receive home-health nursing, remote patient monitoring, in-home parenteral medications, inhome diagnostic studies (electrocardiogram, radiographs, ultrasound), physical therapy, wound care, and phlebotomy, if medically indicated. Patients remain active with the program until acute medical needs have stabilized or resolved. Inherent to the program is a robust care navigation team that assists every enrolled patient. The ED-TOC team schedules followup PCP appointments prior to the patients detaching from the program. Patients do not need to have an established followup PCP appointment prior to enrollment in the ED-TOC. The median length of stay within the ED-TOC is five days.
Measurements
For each ED encounter, we created a dataset of the 24 weeks that followed index ED discharges. We merged in the following information: ED visits; PCP visits; and inpatient hospitalizations. Data extraction was performed by professional staff in Information Services who were not blinded to the goals of the ED-TOC program.
Discharges from the ED in the year prior to program launch were defined “pre-period” (August 1, 2021–July 25, 2022), and those after the program’s start were defined “postperiod” (July 26, 2022–July 31, 2023), so that observations were split exactly around the launch date. For each patient we kept only the first encounter within our data range to
limit omitted-variable bias, as the program may influence the composition of cases associated with revisits. This restriction also reduced the risk of contamination, whereby outcomes at an encounter may have reflected the ongoing impacts of a previous encounter. By construction, this implies that more patient encounters were included in the pre-period (65% of analyzed encounters).
We estimated the association between the ED-TOC and ED revisits, PCP visits, and hospitalizations using a difference-in-differences (DID) strategy, which is widely used in social science research.28 The DID approach is an established method in clinical research for estimating the impact of an intervention or program when randomized trials are not feasible, such as in clinical settings where interventions are present in some groups but not others. The DID compares changes in established outcomes over time between a treatment and comparable control group to assess whether the intervention really had an impact despite other background changing conditions. Outcomes in both the treatment and control groups are measured before the intervention and after the intervention, and calculations are done to determine how much each group has changed over time. The DID methodology works with the assumption that, in the absence of the studied intervention, the treatment and control groups would have followed similar trends over time. This is known as the parallel trends assumption.
The treatment group was composed of traditional Medicare and Medicare Advantage patients who were eligible for the ED-TOC in the post-period. To address the challenge posed by general time trends unrelated to the program during the study period, we used Medi-Cal patients, whose participation in the ED-TOC was effectively null because they were not offered the program, as a control group. Although traditional Medicare and Medicare Advantage patients differ from Medi-Cal patients in demographics and potentially in the levels of outcomes of interest, DID methodology allows for such persistent levels of differences between treatment and control. The key assumption is that the change in outcomes experienced by Medi-Cal beneficiaries from the pre-period to the post-period approximated the change in outcomes that traditional Medicare and Medicare Advantage beneficiaries would have experienced if the ED-TOC program had not launched.
The assumption required for DID methodology to work for this analysis is that 14-day ED revisits for Medicare/ Medicare Advantage and Medi-Cal follow similar trends over time. The validity of this assumption was tested in Figure 1 with the standard parallel pre-trends test that studied the similarity of monthly average pre-period time trends across the treatment and control groups regarding 14-day ED revisit rates. The sample included 13,553 traditional Medicare and Medicare Advantage encounters and 10,143 Medi-Cal encounters, and trends were based on a linear regression in calendar time in months (estimated on encounter-level data).
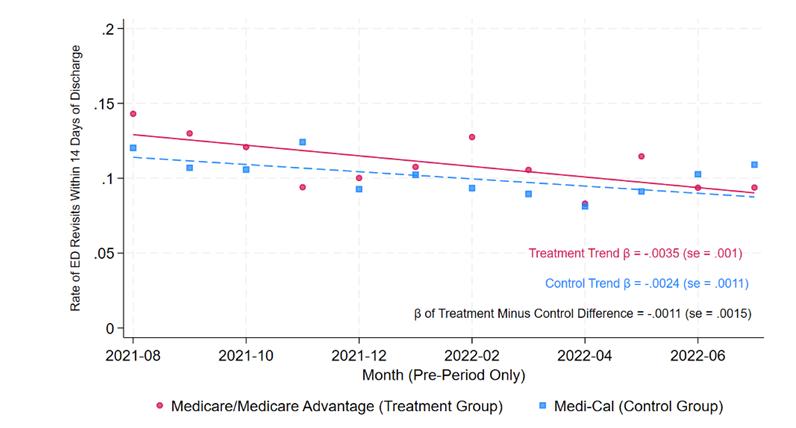
Figure 1. Time trends across the treatment and control groups regarding 14-day emergency department revisit rates.
Note: Points represent the average rate of ED visits in days 1-14 after discharge among Medicare/Medicare Advantage patients (treatment group) and Medi-Cal patients (control group) discharged in a given calendar month. The solid and dashed lines plot time trends for the treatment group and the control group, respectively, calculated with a patient-level linear regression of ED visits 1-14 days after discharge on month of discharge. The difference in slopes between treatment and control was calculated from a linear regression of ED visits 1-14 days after dischargeon-discharge month, a treatment-group indicator variable, and discharge month interacted with the treatment-group indicator variable. Robust standard errors are clustered at the patient level. ED, emergency department; Medi-Cal, California Medicaid.
The time patterns in 14-day ED revisit rates across the two groups showed no secular differences between them, thereby supporting the use of DID methodology for this analysis.
Outcomes
Our primary outcome measure was 14- and 30-day ED revisits. Secondary outcome measures were post-ED PCP visit rates and inpatient hospitalization rates up to 30 days after the index ED visit.
Analysis
Our DID methodology captured the differential change over time between the treatment and control groups, isolating the effect attributable to the ED-TOC under the parallel trends assumption described above. Conceptually, this methodology compared two changes. First, the “treatment difference” was the change in outcomes from the pre- to post-implementation period in the treatment group—patients eligible for ED-TOC enrollment. This change captured both the intervention’s effect and any temporal trends unrelated to it. Second, the “control difference” was similarly defined as the pre- to post-implementation change in outcomes among the control group—patients ineligible for the ED-TOC—capturing underlying temporal trends unrelated to the program. Finally,
we calculated the DID estimate of the program’s effect as the treatment difference minus the control difference, isolating the portion of changes over time that could be attributed to implementation of the ED-TOC.
We interpreted our DID estimates as intent-to-treat effects because treatment group assignment was based on eligibility for the ED-TOC, regardless of whether patients chose to enroll. Specifically, our findings reflect the impacts of offering the program to patients rather than the impacts of enrollment. This is the most program-relevant interpretation because, in practice, the program was available to eligible patients without mandating participation. To examine the program’s impact over time, we calculated separate DID estimates for each consecutive 14-day period after ED discharge up to 24 post-discharge weeks. Given previously reported rates of ED revisits11,12 and conventional reporting standards, we also calculated DID estimates for days 1-7, days 8-14, and for the full 30-day period after ED discharge.
To support clinical interpretation, we present our DID estimates of the ED-TOC program’s effects in three complementary forms. First, we report the change in outcome rates associated with the program: These are our raw DID estimates, representing the change in the percentage of discharges that resulted in ED revisits, PCP visits, and inpatient hospitalizations following ED-TOC implementation. Second, we express the effects as a percentage change relative to baseline by dividing the raw DID estimates by the treatment group’s pre-period mean. Third, we estimate the per-enrollee effect by dividing the raw DID estimate by the ED-TOC enrollment rate, approximating the change in outcomes among patients who participated in the program.
Statistical details of our DID regression analysis are described in the Appendix. All regressions controlled for seasonal trends and derived P-values from standard errors clustered at the patient level. To assess the sensitivity of our findings, we evaluated the stability of estimates with and without covariate adjustment for observed patient characteristics.
RESULTS
Summary Statistics
Our sample size was 23,696 ED encounters (Table 1). Differences in observable characteristics between treatment and control did not threaten our DID strategy, which compared changes in outcomes before and after program launch within each group. Furthermore, our main results were robust to controlling for these observable characteristics (see Appendix Table 2).
Main Results
Table 2 details the effects associated with the ED-TOC program in days 1-14 and 15-28 after discharge. For clinical interpretation, the table reports the change in outcome rates after program implementation (ie, the DID estimate) and
Experimental group
PHSO patient
ED encounters Control, n (%) Treatment, n (%) 10,143 (42.8%) 13,553 (57.2%)
Sex
Male 4,679 (46.1%) 6,156 (45.4%)
Female 5,459 (53.8%) 7,396 (54.6%)
Other 5 (0.0%) 1 (0.0%)
Race/Ethnicity
Non-Hispanic White 3,127 (30.8%) 8,019 (59.2%)
Hispanic 3,573 (35.2%) 2,195 (16.2%)
Black 1,499 (14.8%) 875 (6.5%)
Asian 541 (5.3%) 1,390 (10.3%)
Other 1,403 (13.8%) 1,074 (7.9%)
Mean age in years (SD) 45.0 (16.3) 68.9 (16.3)
< 65 years 9,207 (90.8%) 3,539 (26.1%)
> 65 years 936 (9.2%) 10,014 (73.9%)
Note: This table summarizes the characteristics of patients whose ED discharge outcomes were studied in our regression analysis. Patients were included in our analysis if they were insured by Medicare or Medicare Advantage (treatment group) and were eligible for Population Health Services Organization (PHSO) services, insured by or Medi-Cal (control group), were eligible for PHSO services, and were discharged from either of the university health system’s two EDs between August 1, 2021–July 31, 2023. We only considered each patient’s first ED discharge within the study period. PHSO, Population Health Services Organization; ED, emergency department.
the percentage change in outcomes relative to baseline for each primary and secondary outcome. Figure 2 provides the treatment group’s baseline outcomes after discharge in the pre-period. In the year after program implementation, 7.03% of treatment-group patients enrolled in the ED-TOC within
14 days after ED discharge (P < .001). Enrollment declined thereafter, consistent with the ED-TOC protocol.
We found that the program was associated with a 1.77% reduction in ED revisit rates in the treatment group relative to the control group in the 14-day period after discharge (P = .03). The decline is statistically significant in days 8-14 after discharge (-1.35%, P = .02) and smaller and statistically insignificant in 1-7 days after discharge (-0.67%, P = .34). No significant change in the ED revisit rate occurred during days 15-28.
To express the decline in ED revisit rates as a percentage change relative to baseline, we divided the DID estimates by the treatment group’s baseline pre-period ED revisit rate (Figure 2). This analysis shows that the program was associated with a 15.8% (-1.77%/11.2%) change relative to baseline in days 1-14 after discharge or equivalent to a decline from 11.2% to 9.4%. Dividing the ED revisit rate by the EDTOC enrollment rate approximates the effect per enrollee, indicating that the program was associated with preventing the 14-day ED revisits among 25.2% (-1.77%/7.03%) of enrollees.
Further, the program was associated with an equal-sized, opposite effect for PCP visit rates (Table 2). The results indicate an increase in the rate of PCP visits at both 1-7 days after discharge (0.76%, P = .20) and 8-14 days after discharge (0.33%, P = .52), although neither result is statistically significant. When considering days 1-14 after ED discharge, however, the increase (1.51%) was statistically significant (P = .03). There continued to be an increase in PCP visits at days 15-28 (P = .20). Relative to the baseline PCP visit rate, we found that the ED-TOC was associated with a 10.3% increase (1.51%/14.6%) in 14-day PCP visits, equivalent to an increase from 14.6% to 16.1%. Dividing the PCP visit rate by the EDTOC enrollment rate approximates the effect per enrollee, indicating that the program led to 14-day PCP visits for 21.5% (1.51%/7.03%) of enrollees. There were no statistically significant effects on inpatient hospitalization rates during days 1-14 and 15-28 after discharge (Table 2).
Appendix Table 1 provides outcomes for the 30-day
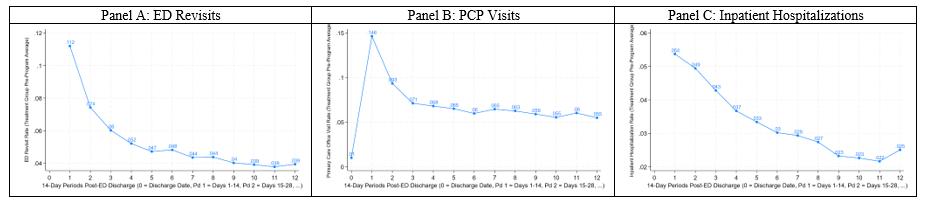
Figure 2. Outcomes following emergency department visit (14-day frequency)—baseline dynamics. Note: This figure displays mean outcomes in 14-day periods since ED discharge among Medicare and Medicare Advantage patients (the treatment group) in the 12 months prior to launch of the ED TOC program. ED, emergency department; PCP, primary care physician; TOC, transition of care.
Table 1. Patient characteristics for analysis sample of 23,696 emergency department encounters.
Table 2. Estimated difference-in-differences effects of the ED transition-of-care program on outcomes in the four weeks After ED discharge.
ED revisits PCP visits Inpatient hospitalizations
(P < .001) (P = .03) (P = .03) (P = .74)
[6.17,7.89] [-3.39,-0.14] [0.12,2.90] [-2.79,1.99]
1-7
8-14
15-28
(P < .001) (P = .34) (P = .20) (P = .92) [6.03,7.72] [-2.05, 0.71]
(P < .001) (P = .02) (P = .52) (P = .97)
(P < .001) (P = .66) (P = .20) (P = .59) [1.17,1.93] [-1.01,1.61] [-0.40,1.92] [-1.71,3.00]
Note: This table reports our difference-in-differences (DID) estimates of the ED-TOC program’s effects, capturing the differential change in primary and secondary outcomes across the pre- and post-implementation periods between the treatment and control groups. Under the parallel trends assumption, which implies that the control group’s change across the pre- and post-period captures temporal trends unrelated to the program, the DID estimates isolate the effects attributable to the ED-TOC. The “% program enrollment rate” column reports DID estimates of the ED-TOC enrollment rate among treatment group patients in the year after program implementation. For each primary and secondary outcome, the “outcome rate change” column represents our DID estimates, representing the change in percentage of ED discharges that resulted in the outcome of interest following program implementation. P-values and 95% confidence intervals are presented below each DID estimate in parentheses and brackets, respectively. The “% change relative to baseline” column expresses the DID estimate as a percentage change relative to baseline by dividing it by the treatment group’s baseline pre-period mean. The treatment group’s baseline pre-period mean outcomes for days 1-14 and 15-28 after ED discharge are shown in Figure 2. DID, difference-in-differences; ED, emergency department; TOC, transition of care; PCP, primary care physician
period following ED discharge. We found an associated 1.31% decline in ED revisit rates in the 30-days following discharge (P = .18); a 2.32% rise in PCP visit rates (P = .005); and insignificant associations with 30-day hospitalizations (P = .93).
Appendix Table 2 adds a vector of covariates to account for compositional differences across groups, showing the robustness of our results to their inclusion. The covariates include age at discharge, age at discharge squared, sex, and indicators for race/ethnicity.
DISCUSSION
The findings of this study demonstrate that a physicianstaffed, telehealth ED-TOC was associated with a 16% relative reduction in the ED revisit rate for Medicare beneficiaries up to two weeks after ED discharge and a 10% increase in visits to PCPs at 14 days after ED discharge.
When Medicare was considered the primary expected payor for an ED visit, this decline in ED visits translated to roughly $252,584 in cost savings during our 24-week study period if a historical cost of $1,040 per Medicare ED treat-
and-release visit is referenced29 and a baseline ED revisit rate of 11% at two weeks is used. When factoring the increased PCP visits and related costs ($36,805),30 the net savings over the study period (24 weeks) was calculated at $215,779 within the treatment group. These values are conservative given the annual growth in ED mean costs31 and that this study was conducted during the program’s first year of implementation when workflows were new and developing efficiency. The annual investment in the program was $1,400,000. The main expenses are the physician and supporting staff (nurse program manager, nurse case manager, and medical assistant) costs. From its inception, the program has leveraged the health system’s established electronic health record and telehealth processes and protocols. The potential cost-savings and health benefits of reduced ED revisits13 bring value to this type of program for organizations working with capitated health plans (eg, HMOs) in which a fixed payment per patient per month is available. Additionally, the harder-to-quantify benefits are in reduced ED patient volume in EDs that are already facing crowding and boarding issues.23,24
The association of our program with the ED revisit rate
was assessed for up to 30 days. We did not examine the 72hour revisit rate because patient enrollment in the program occurred up to 72 hours after ED discharge. We expected that the 1-7 day ED revisit rate among Medicare patients would have decreased. Interestingly, though, there was no difference in ED revisits up to seven days in the Medicare group when compared to the control group. Instead, the decline in ED revisits associated with our program occurred between 8-14 days. These findings align with the findings of Rising et al who suggested that a nine-day ED return visit rate is a more appropriate time frame to capture early ED return visits related to the initial ED visit rather than a 72-hour or 7-day return revisit timeframe.32 In this regard, our use of a 14-day ED revisit rate would meaningfully capture potential early ED revisits.
In addition to reducing ED revisits, our data suggest that our ED-TOC is also associated with enhanced access to PCPs after an ED visit. These findings are consistent with other ED follow-up programs. Luciani et al15 showed that implementation of nurse phone calls at 24-96 hours after ED discharge resulted in a 4.1% decrease in ED revisits and a 17% increase in 7-day follow-up PCP appointments. Fruhan and Bills13 studied patients who received an automated phone call at two days after ED discharge with the option to connect with an advanced practice clinician. At seven days postdischarge, they reported a decrease in ED revisits among patients who had ≤ 3 ED visits in the 180 days preceding the index ED visit.
Jacobsohn et al19 had paramedics conduct in-home patient visits 24-72 hours after ED discharge with subsequent coaching phones calls. They reported no change in ED revisits at 14 or 30 days but increased outpatient follow-up within one week after ED discharge. Hastings et al18 demonstrated that ED patients who received post-ED discharge calls up to 1-2 weeks after ED discharge had a higher rate of PCP visits at 30 days but no change in 30-day ED revisits. Biese et al17 studied the impact of nurse-led telephone calls after ED discharge. These follow-up calls did not reduce 30-day ED revisits or hospitalizations. Furthermore, a comparison by Shah et al20 of in-person vs telehealth PCP follow-up visits within 14 days of ED discharge to home revealed a higher rate of ED revisits and hospitalizations among the telehealth visit group, thereby suggesting the need for additional investigation into ED telehealth follow-up. Our ED-TOC with daily physician telehealth visits was associated with a higher increase in PCP follow-up and a higher decrease in early ED revisit rates than these previous studies. We attribute the drop in ED revisits and increased access to PCPs to the ED-TOC intervention in addressing patient diagnoses and response to treatment plans, patient adherence, and care navigation—factors that drive patients to return to the ED.6-10,33
The lack of effect of this ED-TOC on ED return visits beyond two weeks is reflective of the medically complex, quaternary-care population that our EDs serve. The overall
ED admission rate of our two EDs is 24.5%, reflecting the higher acuity of the patient population compared to EDs with a similar census at 15% and similar type at 12%.34 The implementation of other initiatives referenced in the literature may help reduce ED return visits further. These programs include the availability of telehealth for acute unscheduled visits, pre-ED telehealth triage, and engaging patients who are frequent ED users with a care plan.35
As the population of aging adults with complex care issues continues to grow, demand for ED services will also increase. Roughly 65% of older adults are discharged to home from the ED,2 but the medical issues that cause older patients to seek care in the ED have been associated with a decline in functional status.36 Historically, ED discharge has been accompanied by limited communication and understanding of care needs.3 The availability of ED value-based programs, such as a geriatric ED and an ED-TOC, allows for patient care needs to be identified and outpatient resources accessed.14,16,37 In this way, ED visits become further integrated into the care continuum. Currently, Medicare is the primary payor for 87% of patients ≥ 65 years of age,2 and approximately 47% of Medicare beneficiaries are covered by Medicare Advantage. With the CMS 2030 goal of having all fee-for-service Medicare beneficiaries engaged in a care program with accountability for quality and total cost of care, innovative value-based programs are becoming increasingly important.38 Additionally, the ability of a TOC program to decrease ED revisit rates and improve access to outpatient care is important to hospitals given the increasing rates of ED visits nationwide2,14 and the limited inpatient capacity of hospitals, which together contribute to ED boarding and long ED wait times.23,25,39
Under the traditional Medicare fee-for-service model, an ED-TOC such as ours would be costly and difficult to sustain, as reimbursement for these TOC services for a visit originating in the ED is not directly supported.40 Our ED-TOC represents a partnership between the ED and our health system’s PHSO, which manages the care of patients insured through HMOs. When part of a care relationship involving accountability for total cost of care and quality, an ED-TOC becomes a valuable innovation and potential costsaver through its ability to decrease ED revisits and enhance access to care. With the fragile fee-for-service payment model currently in place for US EDs,35 these value-based programs involving ED care may become increasingly important.
LIMITATIONS
This study was conducted at a single health system with an integrated PHSO; therefore, results may not be applicable to other health systems. Because this was a quality improvement project not designed as a randomized controlled trial, causality could not be determined. The results of the DID methodology suggest causation but rely on the assumption that the control group before-and-after change approximates the treatment group before-and-after change
in the absence of the TOC program. While the Medicare and Medi-Cal populations may differ in observable characteristics, Figure 1 shows parallel time trends between the groups in the pre-period. However, we cannot rule out the possibility that factors unrelated to the TOC program, such as economic changes, contributed to differential before-and-after changes for treatment and control. Restricting our sample to each patient’s first encounter limited the interpretation of our results to capture the program’s impact on initial ED encounters only. While this restriction implies that the post period mechanically contains fewer patients who frequently visit the ED, this factor acts upon both the treatment and control groups and did not pose a direct threat to our DID design.
CONCLUSION
An ED telehealth transition of care program was associated with a reduction in Medicare ED revisits to the emergency department during days 8-14 after an index ED visit but not during days 1-7 or at 30 days. Visits to primary care physicians visits were associated with a significant increase at 14 and 30 days. No association was found with 30day hospitalizations.
Address for Correspondence: Allyson Kreshak, MD, UC San Diego Health, Department of Emergency Medicine and Population Health Services Organization, 200 West Arbor Dr, MC 8676, San Diego, CA 92103. Email: akreshak@health.ucsd.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Kreshak et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Cairns C, Kang K. National Hospital Ambulatory Medical Care Survey: 2021 emergency department summary tables. Available from: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_ Documentation/NHAMCS/doc21-ed-508.pdf. Accessed May 7, 2024.
2. Sun R, Karaca Z, Wong HS. Trends in hospital emergency department visits by age and payer, 2006–2015. 2018. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb238-EmergencyDepartment-Age-Payer-2006-2015.jsp. Accessed March 18, 2025.
3. Musso MW, Perret JN, Sanders, et al. Patients’ comprehension of their emergency department encounter: a pilot study using physician observers. Ann Emerg Med. 2015;65:151-155e4.
4. Gettel CJ, Hastings SN, Biese KJ, et al. Emergency department-tocommunity transitions of care. Clin Geriatr Med. 2023;39:659-72.
5. Hastings SN, Barrett A, Weinberger M, et al. Older patients understanding of emergency department discharge information and its relationship with adverse outcomes. J Patient Saf. 2011;7(1).
6. Pierce JM, Kellerman AL, Oster C. “Bounces”: an analysis of shortterm return visits to a public hospital emergency department. Ann Emerg Med. 1990;19:752-7.
7. Hu SC. Analysis of patient revisits to the emergency department. Am J Emerg Med. 1992;10:366-70.
8. Cheng SY, Wang HT, Lee C-W, et al. The characteristics and prognostic predictors of unplanned hospital admission within 72 hours after ED discharge. Am J Emerg Med. 2013;31:1490-4.
9. Hiti EA, Tamim H, Makki M, et al. Characteristics and determinants of high-risk unscheduled return visits to the emergency department. Emerg Med J. 2019;37(2):79-84.
10. Hoek AE, Anker SCP, vanBeeck EF, et al. Patient discharge instructions in the emergency department and their effects on comprehension and recall of discharge instructions: a systematic review and meta-analysis. Ann Emerg Med. 2020;75(3):435-44.
11. Alshahrani M, Katbi F, Bahamdan Y, et al. Frequency, causes and outcomes of return visits to the emergency department within 72 hours: a retrospective observational study. J Multidiscip Healthc 2020;13:2003-10.
12. Sabbatini AK, Kocher KE, Basu A, et al. In-hospital outcomes and costs among patients hospitalized during a return visit to the emergency department. JAMA. 2016;315(7):663-71.
13. Fruhan S, Bills CB. Association of a callback program with emergency department revisit rate among patients seeking emergency care. JAMA Netw Open. 2022;5(5):e2213154.
14. Biese K, Lash TA, Kennedy M. Emergency department care transition programs – value-based care interventions that need system-level support. JAMA Netw Open. 2022;5(5):e2213160.
15. Luciani-McGillivray I, Cushing J, Klug R, et al. Nurse-led call back program to improve patient follow-up with providers after discharge from the emergency department. J Patient Exp. 2020;7(6):1349-56.
16. Hwang U, Dresden SM, Vargas-Torres C, et al. Association of a geriatric emergency department innovation program with cost outcomes among Medicare beneficiaries. JAMA Netw Open 2021;4(3):e2037334.
17. Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone followup for older adults discharged to home from the emergency department: a pragmatic randomized control trial. J Am Geriatr Soc 2018;66(3):452-8.
18. Hastings SN, Stechuchak KM, Coffman CJ. Discharge information and support for patients discharged from the emergency department: Results from a randomized controlled trial. J Gen Intern Med 2020;35:79-86.
19. Jacobsohn GC, Jones CMC, Green RK, et al. Effectiveness of a care transitions intervention for older adults discharged home from the emergency department: a randomized controlled trial. Acad Emerg Med. 2022;29:51-63.
20. Shah VV, Villaflores CW, Chuong LH, et al. Association between inperson vs. telehealth follow-up and rates of repeated hospital visits among patients seen in the emergency department. JAMA Netw Open. 2022;5(10): e2237783.
21. Mohr NM, Wessman BT, Bassin B, et al. Boarding of critically ill patients in the emergency department. Crit Care Med. 2020;48:1180-7.
22. National Center for Health Statistics. Estimates of Emergency Department Visits in the United States, 2016-2022. 2024. Available at: https://www.cdc.gov/nchs/dhcs/ed-visits/index.htm. Accessed September 23, 2024.
23. Carr BG, Hollander JE, Baxt WG, et al. Trends in boarding of admitted patients in US emergency departments 2003-2005. J Emerg Med. 2010;39(4):506-11.
24. Kelen GD, Wolfe R, D’Onofrio G, et al. Emergency department crowding: the canary in the health care system. NEJM Catal Innov Care Deliv. 2021; 5(2):1-26.
25. Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US health care spending, 1996-2013. JAMA 2017;318(17):1668-78.
26. American Hospital Association. 2021 Cost of Caring. 2021. Available at: https://www.aha.org/guidesreports/2021-10-25-2021-cost-caring Accessed September 9, 2024.
27. Health Care Payment Learning & Action Network. APM Measurement - Progress of Alternative Payment Models: 2019 Methodology and Results Report. 2021. Available at: https://ldi.upenn.edu/our-work/ research-updates/the-future-of-value-based-payment-a-road-mapto-2030/. Accessed July 25, 2025
28. Imbens GW, Woolridge JM. Recent developments in the econometrics of program evaluation. J Econ Lit. 2009;47(1):5-86.
29. Roemer M. Costs of Treat-and-Release Emergency Department Visits in the United States, 2021. 2024. Available at: https://hcup-us. ahrq.gov/reports/statbriefs/sb311-ED-visit-costs-2021.pdf. Accessed March 14, 2025.
30. Machlin SR, Mitchell EM. Expenses for office-based physician visits by specialty and insurance type, 2016. 2018. Available at: https:// meps.ahrq.gov/data_files/publications/st517/stat517.shtml. Accessed September 25, 2024.
31. Pickens G, Smith MW, McDermott KW. Trends in treatment costs of U.S. emergency department visits. Am J Emerg Med. 2022;58:89-94.
32. Rising KL, Victor TW, Hollander JE, et al. Patient returns to the emergency department: the time-to-return curve. Acad Emerg Med 2014.8:864-71.
33. Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826-34.
34. EPIC ASAP Key Performance Indicator Quarterly Benchmarking Report Quarter 1 2024 (internal institution report). www.epic.com. Accessed May 7, 2025.
35. Pines JM, Black BS, Cirillo A, et al. Payment innovation in emergency care: a case for global clinician budgets. Ann Emerg Med 2024:84:305-12.
36. Nagurney JM, Fleischman W, Han L, et al. Emergency department visits without hospitalization are associated with functional decline in older persons. Ann Emerg Med. 2017;69(4):426-33.
37. Galarraga JE, Pines JM. Costs of ED episodes of care in the United States. Am J Emerg Med. 2016;34:357-65.
38. Centers for Medicare and Medicaid Services. Innovation Center Strategy Refresh. Available at: https://www.cms.gov/priorities/ innovation/strategic-direction-whitepaper. Accessed September 9, 2024.
39. Hsia RY, Zagorov S, Sarkar N, et al. Patterns in patient encounters and emergency department capacity in California, 2011-2021. JAMA Netw Open. 2023;6(6):e2319438.
40. Medicare Learning Network, Centers for Medicare & Medicaid Services. Transitional Care Management Services. 2024. Available at: https://www.cms.gov/files/document/mln908628-transitional-caremanagement-services.pdf. Accessed September 9, 2024.
Characteristics of Emergency Department Patients Referred to an Undiagnosed Mass Clinic
Brittany Beel, MD*
Ryan T. McKenna, DO*
Jesse W St Clair IV, MD*
Joan M. Irizarry-Alvarado, MD†
Greg E. Coltvet, MBA, MHSA*
Johnathan M. Sheele, MD, MHS, MPH*
Section Editor: León D. Sánchez, MD, MPH
Mayo Clinic, Department of Emergency Medicine, Jacksonville, Florida Mayo Clinic, Division of General Internal Medicine, Jacksonville Florida
Submission history: Submitted January 8, 2025; Revision received May 29, 2025; Accepted June 9, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem. 41793
Introduction: The emergency department (ED) serves as an entry point to the healthcare system for many patients, and the increased use of advanced imaging has resulted in identification of masses of unclear significance. We describe patients presenting to an ED who were referred to an undiagnosed mass clinic (UMC).
Methods: We performed a retrospective observational cohort study of patients ≥16 years of age presenting to Mayo Clinic in Jacksonville, Florida, from October 31, 2018–March 31, 2023, who were referred to the UMC.
Results: There were 116 patients referred to the UMC with a median of 3.5 days from ED encounter to clinic date and a median of 14.5 days from ED encounter to biopsy. Using an analytic tool in the electronic health record, we estimated that of 16,872 patients, 116 (0.69%) Mayo Clinic Florida (MCF) ED patients ≥18 years of age who received computed tomography and were discharged from the ED were referred to the UMC. Ultimately, 35 of 65 patients (53.8%) seen in the UMC received a cancer diagnosis.
Conclusion: Our study shows a viable care path from ED encounter to undiagnosed mass clinic. Further research is needed to ensure timely transitions of care for patients who are uninsured or out of network. [West J Emerg Med. 2025;26(5)1211–1216.]
INTRODUCTION
Since its inception, the role of the emergency department (ED) has expanded from emergency and acute, unscheduled episodic care to becoming the gateway to the hospital and broader healthcare system for both established and new patients.1 For many of these patients, the ED is their first encounter with the healthcare system, serving as a bridge for temporizing care and obtaining referrals while awaiting specialty care. With the increasing number of advanced imaging studies, such as computed tomography (CT) and magnetic resonance imaging being performed in the ED, it is not uncommon for patients to have masses of unclear significance
found incidentally during their ED evaluation.2,3 Up to 50% of common cancers are diagnosed in the ED.4
Delays in treatment of as few as four weeks are associated with increased mortality in certain types of cancer and disproportionally affect patients from minority and low socioeconomic populations.5,6 Diagnosis of a potential new malignancy can be devastating, and patients need close followup to determine the need for further imaging, biopsy, staging, and treatment. Previous research has demonstrated the feasibility of transitioning care of patients with suspicious masses from the ED to the outpatient setting.7,8 In this paper, we describe our experience and the characteristics of patients presenting to the
ED at Mayo Clinic in Jacksonville, Florida (MCF), who were referred to an undiagnosed mass clinic (UMC).
METHODS
This was a quality improvement project that was approved by the institutional review board (IRB) after data was collected. We performed a retrospective chart review after the IRB deemed this study exempt. We collected data through manual chart abstraction from ED referrals made to the UMC at MCF, from the time the clinic opened on October 31, 2018, through March 31, 2023, for patients ≥16 years of age, until over 100 referrals were reached. The following data were obtained: patient demographics; ED chief complaints; ED diagnoses; ED and UMC arrival dates; documented reasons for loss to follow-up; and whether the patient had a new diagnosis of cancer, was receiving care at Mayo Clinic, or was deceased. We removed from the analysis any patient who had followed up in the UMC but was missing data for the variable of interest. This occurred in four instances. We followed all elements of retrospective chart review with one exception: An experienced ED administrator who was not blinded to the study objectives abstracted the data.9
RESULTS
During the study period, there were 141,316 patient visits to the ED. A total of 116 patients were referred to the UMC by 28 emergency clinicians. Using the SlicerDicer data visualization and reporting program in our electronic health record (Epic Systems Corporation, Verona, WI), we estimated that 116/16,872 (0.69%) MCF ED patients ≥ 18 years of age who received a CT and were discharged from the ED were referred to the UMC. The clinicians made a median (range) of three (1-28) referrals. The median (IQR) age for patients referred to the UMC was 62.5 (48.7-71.0) years, of whom 92 (79.3%) were White, and 63 (54.3%) were women. Patients were seen in the UMC a median (IQR) of 3.5 (22.3) days after the ED encounter. Among those patients referred to the UMC who were found to have a new diagnosis of cancer, the median (IQR) time from ED encounter to UMC appointment was four (2.3-5.8) days; from UMC appointment to biopsy was 7.5 (3.5-14.3) days; and from ED encounter to biopsy was 14.5 (7.0-19.3) days.
The most common chief complaints referred to the UMC were abdominal pain, headache, and chest or chest wall pain (Table). Among the 65 patients seen in the UMC, 35 (53.8%) received a diagnosis of cancer. Of those, 31 patients (88.6%) had a new cancer diagnosis, while for one (2.9%) patient the cancer diagnosis was not new and for three (8.6%) it was unclear whether it was a new cancer diagnosis. Among those with a new diagnosis of cancer, 20 (64.5%) were still alive at the time of publication of this paper and six (19.4%) had died; it is unclear whether the other five (16.1%) were still alive. Also, 23 patients (74.2%) with new cancer diagnoses were receiving cancer treatment at Mayo Clinic.
Fifty-one (44.0%) referrals to the UMC resulted in the
Population Health Research Capsule
What do we already know about this issue?
Masses of undetermined significance are often incidentally found in the emergency department (ED). Delays in evaluation and treatment can lead to increased mortality.
What was the research question?
Is referring ED patients to a clinic a viable method for transitions of care, and what gaps and opportunities exist?
What was the major finding of the study?
Of the 65 patients seen in the undiagnosed mass clinic, 35 (53.8%) were diagnosed with cancer, of whom 31 (88.6%) had a new cancer diagnosis.
How does this improve population health?
We describe an alternative to admitting stable patients with an undiagnosed mass, instead referring them to an outpatient clinic for expedited evaluation.
patient not being seen. Reasons for this include condition was out of the scope of the clinic (16); insurance was out of network (8); patients opted out who were self-pay or uninsured (4); the patient had other specialist follow-up or referral to another clinic (9), declined or canceled the UMC appointment (5), was not reachable (6), was hospitalized (2), or did not show for appointment (1). Of the five patients who died, three declined or canceled the UMC appointment and two had other specialist follow-ups or were referred to another clinic.
DISCUSSION
This study shows the viability of transitioning the care of patients seen in the ED with undiagnosed masses to an outpatient clinic such as the UMC at our institution, which can expedite workup. Previous studies have described the feasibility of accelerated coordination-of-care pathways from the ED and outpatient settings.7-9 A substantial portion (54%) of our study population received a new diagnosis of cancer, comparable to a similar ED pathway at a different institution (53%).8 Patients seen in a primary care setting had a lower percentage of incidental cancer findings (4%) than our patient population.11 In a retrospective study conducted at a Level I trauma center, only 15% of incidental findings were considered clinically concerning by the study authors, which included
Table. Characteristics of emergency department patients referred to an undiagnosed mass clinic (UMC).
aPatients may have more than one chief complaint documented. bAmong those who had a UMC appointment. ED, emergency department; NA, not applicable; UMC, undiagnosed mass clinic.
Table. Continued.
aPatients may have more than one chief complaint documented.
bAmong those who had a UMC appointment. ED, emergency department; NA, not applicable; UMC, undiagnosed mass clinic.
masses suggestive of primary malignancy and potential metastatic lesions.12 This difference is likely due to the baseline characteristics of patient populations presenting to each ED— one is a trauma center while ours is a complex, comprehensive medical center. A previous study at our institution from multiple referral sources found that most patients were seen within nine days from initial contact.9 Demographics were similar in this cohort; however, the mean time to follow-up in our study of exclusively ED patients was 3.5 days, instead of nine days, due to an established clinic scheduling protocol for expediting ED patient follow-up. Rapid follow-up is key during this period of uncertainty, fear, and anxiety for patients.
LIMITATIONS
This was a single-center, retrospective chart review at a complex, comprehensive medical center with limited racial diversity. The predominance of the White population referred to the UMC reflects the socioeconomic population that visits the ED and clinics at MCF. Our institution’s insurance payor mix may have also contributed to this limitation. The study was limited by a substantial number of patients lost to followup and by the limitations of retrospective chart review, which made it difficult to determine whether the patient received timely care outside our institution, leading to uncertainty about outcomes for these patients. Not all patients with a
newly diagnosed mass or suspected cancer were referred to the UMC, and emergency clinicians may have known if a patient was out of network for follow-up, which could have biased who was referred to the UMC. Age, comorbidities, shared decision-making about the findings from the ED encounter, access to timely primary care follow-up, and residential distance from Mayo Clinic may have also influenced whether the patient was referred to the UMC.
The UMC’s scope of practice includes any soft tissue, intraabdominal/retroperitoneal, and lymphatic masses without association to any single organ. Patients with masses associated with one organ are referred to already established pathways at Mayo Clinic (eg, patients with lung masses are referred to pulmonary medicine). These data may not be included in our analysis. Lastly, We collected our data shortly after the last patient was enrolled. Patients with earlier referrals to the UMC had more time for follow-up, treatment, and disease progression compared to those with referrals closer to when the data were abstracted.
While it would be instructive to know the total number of patients with incidental masses identified during the study period, this information was not available because of several limitations. To obtain an accurate assessment of the number of people who could potentially qualify for the mass clinic, we would need to have examined a convenience sample of patients ≥16 years of age at Mayo Clinic Florida, who had a concerning mass on CT and otherwise met criteria for referral to the mass clinic. However, other factors would invariably have been considered by the emergency clinician, which are difficult to quantify from a chart review study such as the location of the mass and whether it was new or known, etc. In addition, abstracting data from radiology reports will not accurately identify all patients with a “mass,” given the different words used to describe a “mass” such as “nodule,” “hypodensity,” “hyperdensity,” “enlarged lymph node,” “lymphadenopathy,” and “cyst.” Furthermore, keyword searches are often inaccurate for characterizing the radiology report findings as new, old, present, absent, or possible.
CONCLUSION
Patients who present to the ED with new solid tumors that do not meet admission criteria require expedited transitions of care to the appropriate specialist to avoid delays in diagnosis and treatment. We describe an ED referral process to an undiagnosed mass clinic, which can aid in triaging and examining patients expeditiously with undiagnosed masses before they are ultimately referred to the appropriate subspecialist once diagnosis is established.
Patients with incidental intraabdominal and intracranial masses have a high likelihood of malignancy. Emergency department patients are more likely to have an incidental finding of a malignancy as opposed to other patient populations, which is likely due to higher rates of advanced imaging use in the ED. Further research and quality
improvement should aim to assess similar transitions of care for minority, Medicaid, and underserved populations.
ACKNOWLEDGMENTS
It is with great sadness that we disclose the death of one of the authors, Greg Coltvet, MBA, MHSA, who died on November 27, 2024. He participated in all aspects of authorship of the manuscript as defined by the ICJME but died prior to submission. No significant changes have been made to the manuscript since his death.
Address for Correspondence: Brittany Beel, MD, Mayo Clinic, Department of Emergency Medicine, 4500 San Pablo Rd, Jacksonville, FL 32224. Email: beel.brittany@mayo.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Beel et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Cairns C, Ashman JJ, Kang K. Emergency Department Visit Rates by Selected Characteristics: United States, 2022. NCHS Data Brief 2024;(503):10.15620/cdc/159284.
2. Poyiadji N, Beauchamp N, 3rd, Myers DT, et al. Diagnostic imaging utilization in the emergency department: recent trends in volume and radiology work relative value units. J Am Coll Radiol 2023;20(12):1207-14.
3. Kempter F, Heye T, Vosshenrich J, et al. Trends in CT examination utilization in the emergency department during and after the COVID-19 pandemic. BMC Med Imaging. 2024;24(1):283.
4. Pettit NR, Bischof JJ. The emergency department: a key pillar in the cancer care continuum. Acad Emerg Med. 2023;30(12):1288-9.
5. Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 2020;371:m4087.
6. Pettit NR, Sarmiento E, Kline JA. Emergency department associated cancer diagnoses fraught with poor outcomes, with associated socioeconomic and racial disparities. J Emerg Med. 2020;59(5):771.
7. Berberabe T. Diagnosis program improves time to biopsy in emergency department, primary care clinic. Targ Onc. 2023;12(5).
8. Pettit N, Al-Hader A. Novel referral pathway for patients with new solid tumors discharged from the emergency department: a pilot study. Acad Emerg Med. 2022;29(4):500-2.
9. Ressler SW, Croghan IT, Girardo ME, et al. Development of an undiagnosed mass registry: lessons learned from our first 100 patients. J Prim Care Community Health. 2025;16:21501319251325650.
10. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
11. Koo MM, Rubin G, McPhail S, et al. Incidentally diagnosed cancer and commonly preceding ical scenarios: a cross-sectional descriptive analysis of English audit data. BMJ Open. 2019;9(9):e028362.
12. Munk MD, Peitzman AB, Hostler DP, et al. Frequency and follow-up of incidental findings on trauma computed tomography scans: experience at a Level one trauma center. J Emerg Med. 2010;38(3):346-50.
Emergency Department Utilization and Patient Acuity in the Setting of Care-Seeking Hesitancy:
Insights from the COVID-19 Pandemic
Eric Frazier, BS*
Nouri Modallalkar, BS†
Natassia Dunn, MD‡
Bharath Chakravarthy, MD, MPH§ Luis Gonzales, MS||
Soheil Saadat, MD, MPH, PhD§
Section Editor: Murat Cetin, MD
University of California, Irvine, School of Medicine, California
Independent Researcher, San Jose, California
Mount Sinai West, Department of Obstetrics and Gynecology, New York, New York University of California, Irvine, Department of Emergency Medicine, California University of California Irvine Medical Center, Orange, California
Submission history: Submitted February 15, 2025; Revision received June 16, 2025; Accepted July 9, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.43530
Introduction: The coronavirus disease 2019 (COVID-19) pandemic significantly altered emergency department (ED) utilization patterns. This study quantifies the statistics at a Level I trauma center in Southern California from 14 months before to nine months after the start of the pandemic (January 2019–December 2020). We hypothesized that during the COVID-19 pandemic, changes in ED use patterns impacted patient acuity, as measured by admission rate, mortality rate, ED volume, Emergency Severity Index (ESI), and female:male ratio, even when controlling for COVID-19 cases.
Methods: In this study we examined 97,793 ED visits from January 2019–December 2020 at the University of California, Irvine Medical Center in Orange, CA, via an administrative database comprised of anonymized datapoints from the electronic health record. We included all months from January 2019–December 2020 to account for potential secular trends by calendar month. Primary outcome measures were hospital admission rate and all-causes mortality rate among non-COVID-19 patients who presented to the ED. Secondary outcome measures included the mean number of ED visits per month, mean ESI, and female:male ratio among non-COVID-19 patients. Statistical analyses were performed.
Results: We found an increase in the mortality rate per ED visit of 0.8859% before the pandemic to 1.2706% (P < .001) during the pandemic. After excluding COVID-19 cases, the mortality rate per ED visit remained elevated at 1.1746% (P < .001), a relative increase of 32.6%. Hospital admission rate increased from 26.0% before the pandemic to 32.3% during the pandemic (P < .001). The mean number of ED visits per month decreased from 4,271.2 ± 193.1 before the pandemic to 3,558.7 ± 437.1 per month during the pandemic (P < .001), a relative decrease of 16.7% when excluding COVID-19 cases. The mean ESI of non-COVID-19 related cases during the pandemic decreased from 2.85 pre-pandemic to 2.84 during the pandemic (P = .03). The female:male ratio decreased from 1.003 pre-pandemic to 0.885 during the pandemic (P < .001).
Conclusion: This study reveals a decrease in patient volume with an increase in mortality and admission rate, demonstrating an association between shifts in ED utilization patterns and increased patient acuity during the pandemic. Understanding patients’ emergency care-seeking behavior during this period is essential for preparing for future large-scale public health crises and optimizing ED resource allocation and mobilization based on lessons learned from COVID-19. Overall, these findings highlight the need for further research into the development of strategies to address changes in care-seeking behavior during access-limiting scenarios. [West J Emerg Med. 2025;26(5)1217–1225.]
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic dramatically impacted and burdened our healthcare systems, changing individual perceptions of our system and the way medicine is practiced. By the end of 2022, there had been a reported total of 1,095,224 COVID-19 related-deaths, and COVID-19 remained a top 10 leading cause of death in the United States.1,2 This widespread impact on public health likely led to significant changes in patient emergency department (ED) care-seeking behavior. Early in the pandemic, reports from emergency medical services (EMS) and EDs showed a general decrease in EMS responses, patient transports, and ED patient volume.3,4
Fear of exposure to the virus may have contributed to patients avoiding the hospital, even for life-threatening conditions. For example, a study in Hong Kong found that patients experiencing acute myocardial infarctions (MI) during the pandemic had longer symptom-to-first medical contact time, and more patients presented outside of the revascularization window.5 Similar trends were observed for strokes, with more patients experiencing severe strokes while fewer patients were within the window to receive tissue plasminogen activator.6, 7 These trends suggest that fear of COVID-19 may have outweighed the perceived need for medical care, leading patients to delay seeking treatment.
Some low- or intermediate-acuity patients may have avoided seeking care altogether, perceiving their symptoms as low severity, fearing COVID-19, or adhering to stay-at-home orders. One survey examining fears of the risk of COVID-19 exposure in hospitals revealed that 16.9% of respondents prioritized avoidance of COVID-19 exposure in the ED over seeking appropriate care for symptoms consistent with MI, and 25.5% avoided care for symptoms of appendicitis.8 The fear of hospital exposure to the virus likely affected patients’ perception of symptom severity, leading them to postpone seeking care. Increases in risk tolerance and delays in referral to the ED may have led to increased acuity and corresponded to worse clinical outcomes when compared to pre-pandemic rates.
Across the US and globally, ED visits and hospital admissions decreased regardless of the severity of complaints.4,9-11 However, reported data on whether the decline in patient volume during the pandemic was also associated with a higher mortality rate have varied. Some studies reported no statistically significant increase in observed in-hospital mortality during the early pandemic,12 while others reported greater incidence of acute kidney injury and lactic acidemia and increased incidence of early in-hospital mortality.10 In high-acuity cases, whether due to local COVID-19 restrictions or fear, delays to seeking care posed the potential to impact patient outcomes. For patients experiencing acute MIs or strokes, the adage “time is tissue” best emphasizes the timesensitive nature of receiving treatment.
Our goal in this study was to better characterize the relationship between changes in patient volume and overall
Population Health Research Capsule
What do we already know about this issue? The COVID-19 pandemic put a significant strain on the healthcare system through increased patient mortality, and it posed various barriers to accessing healthcare.
What was the research question?
Did changes in emergency department (ED) utilization during the pandemic affect patient acuity when controlling for COVID-19 cases?
What was the major finding of the study?
Admission rose from 26.0% (25.6-26.3) to 28.0% (27.6-28.5) (P <.001) and mortality rose 0.89% to 1.17% (P <.001).
How does this improve population health? This study demonstrates shifts in ED utilization patterns and patient acuity, which contributes to knowledge that may support responses in future health crises.
acuity independent of COVID-19 cases by analyzing data from a Level I trauma center in Southern California. By controlling for COVID-19 cases, we contribute to the body of literature that delineates whether the observed decrease in patient volume correlated with an increase in mortality rates. We hope to provide insight into the impacts of delayed careseeking behavior, government restrictions, and healthcare system adaptations during the pandemic. We hypothesized that during the COVID-19 pandemic there were changes in ED utilization patterns that impacted patient acuity, as measured by admission rate, mortality rate, ED volume, Emergency Severity Index (ESI), and female:male ratio even when controlling for COVID-19 cases.
These measures provide quantitative evidence of the impact that changes in patient care-seeking behavior had on influencing changes in ED patient acuity during the pandemic. Understanding the effects of patient behavioral shifts and healthcare system adaptations is crucial for preparing for future large-scale public health crises and optimizing ED resource allocation and mobilization based on lessons learned from COVID-19.
METHODS
The study was performed at the University of California, Irvine Medical Center, a Level I trauma center in Southern California with over 58,000 annual ED visits and over 6,000 annual trauma visits; trauma represents about 10% of the
ED census. The ED serves a primarily urban population and also has a Level II pediatric trauma center designation. It is strategically located within 20 miles of two other Level II adult trauma centers and one Level I pediatric trauma center. We examined 97,793 ED visits queried from an administrative database comprised of anonymized datapoints from the electronic health record. Incomplete records were excluded listwise from the analysis, and no imputation methods were used. We have no reason to believe that the extent of missing data differed between the study periods. Data extraction was performed by the department’s data analyst, and no adjudication was required as missingness led to exclusion rather than disagreement. We included all patients who presented to the ED from January 2019–December 2020. We included that time frame to account for potential secular trends by calendar month. COVID-19 cases began presenting to the ED in March 2020. While we considered excluding January and February from both years to achieve symmetry in study periods, we concluded that the ability to compare trends between 2019 and 2020 in the absence of COVID-19 outweighed the benefits of having perfectly symmetrical durations.
Primary outcome measures were hospital admission rate and all-causes mortality rate among non-COVID-19 patients who presented to the ED. Secondary outcome measures included the mean number of ED visits per month, mean ESI, and female:male ratio among non-COVID-19 patients referred to the ED. We compared primary and secondary outcome measures before the pandemic (January 1, 2019–February 28, 2020) and during the pandemic (March 1–December 31, 2020). We made comparisons among all patients first, and then by excluding COVID-19 patients. This study received approval from the institutional review board (IRB) of the University of California, Irvine.
Statistical Analysis
We used Pearson chi-square tests to compare hospital admission rate, mortality rate, and female:male ratio between the study periods. We also used Mann-Whitney tests to compare the mean number of ED visits per month, and mean ESI between the study periods. For multivariate analysis, we used the logistic regression analysis method to compare the primary outcomes between the study periods, adjusting for sex, age, ESI, and primary diagnosis. To control for the confounder effect of age, we calculated the mean age for the patients before the pandemic and during the pandemic and input them into the logistic regression model. To control for the confounder effect of primary diagnoses, we classified them into 96 distinct groups and presented them into the logistic regression model.
We did not include age and primary diagnosis in the study outcomes because our primary goal was to isolate for the effects of the pandemic and not to test for statistical significance in the differences of these values. The statistical
analysis was repeated after excluding COVID-19 patients. and the results are presented separately. Odds ratio (OR) for the study period, P-value and Nagelkerke R2 are reported for the logistic regression analysis. Continuous variables are presented as mean ± standard deviation. Proportions are reported as percentages and 95% confidence intervals. P-values < .05 were considered statistically significant. We used IBM SPSS Statistics v27.0 (IBM Corp., Armonk, NY) for data analysis.
RESULTS
The study sample included 97,793 ED visits by 61,303 patients from January 1, 2019–December 31, 2020. Of the total ED visits, 59,937 occurred before the pandemic period and 37,856 occurred during the pandemic. Of the pandemic period visits, 2,269 (6%) were related to COVID-19 (Table 1). Hospital admission rate was 26.0% (25.6-26.3%) before the pandemic and rose to 32.3% (31.9-32.8%) during the pandemic (P < .001) (Table 1). After excluding COVID-19 cases, the hospital admission rate remained at 28.0% (27.628.5%), which was higher than before the pandemic (P < .001) (Figure 1). In logistic regression analysis, hospital admission was higher during the pandemic period compared to before the pandemic, adjusted for sex, age, ESI and primary diagnosis (OR 1.09, P < .001, Nagelkerke R2 0.34). The association did not change by excluding COVID-19 cases (OR 1.09, P < .001, Nagelkerke R2 0.39). The mean age of patients in the prepandemic period was 48.7 years (SD 19.13; median 48), and 48.4 years (SD 18.81; median 48) during the pandemic period. During the study period, 239 patients died in the ED, 524 died after admission, and 249 died after discharge (Table 1). Before the pandemic, the overall mortality rate per ED visit was 0.8859% (.8125- .9642%). During the pandemic, the overall mortality rate per ED visit rose to 1.2706% (1.16021.3886%). After excluding COVID-19 cases, the overall mortality rate per ED visit remained elevated at 1.1746% (1.0652-1.2920%) when compared to the pre-pandemic period (Figure 2), representing a relative increase of 32.6% in mortality rate even after excluding COVID-19 cases. In logistic regression analysis, the pandemic was associated with higher mortality after adjusting for sex, age, ESI, and primary diagnosis (OR 1.293, P < .001, Nagelkerke R2 0.35). The association did not change by excluding COVID-19 cases (OR 1.293, P < .001, Nagelkerke R2 0.35).
The mean number of ED visits per month was 4,271.2 ± 193.1 before the pandemic and decreased to 3,786 ± 476.8 per month during pandemic (P = .01). By excluding COVID-19 cases, the mean number of ED visits during the pandemic further decreased to 3,558.7 ± 437.1, which was significantly less than the pre-pandemic period (P < .001) (Figure 3).
Trauma represented 12.62% (N = 7,567) of ED visits before the pandemic and represented 12.1% (N = 4,608) of ED visits during the pandemic. While not included in the statistical analysis, supplemental data on the breakdown of trauma-
Table 1. Study samples before and during COVID-19 at a Southern California hospital, including and excluding COVID-19 cases. The data from January 1, 2019–December 31, 2020 includes both the primary outcome measures of hospital admission rate and all-causes mortality rate, and the secondary outcome measures of female:male ratio and Emergency Severity Index.
ED, emergency department.
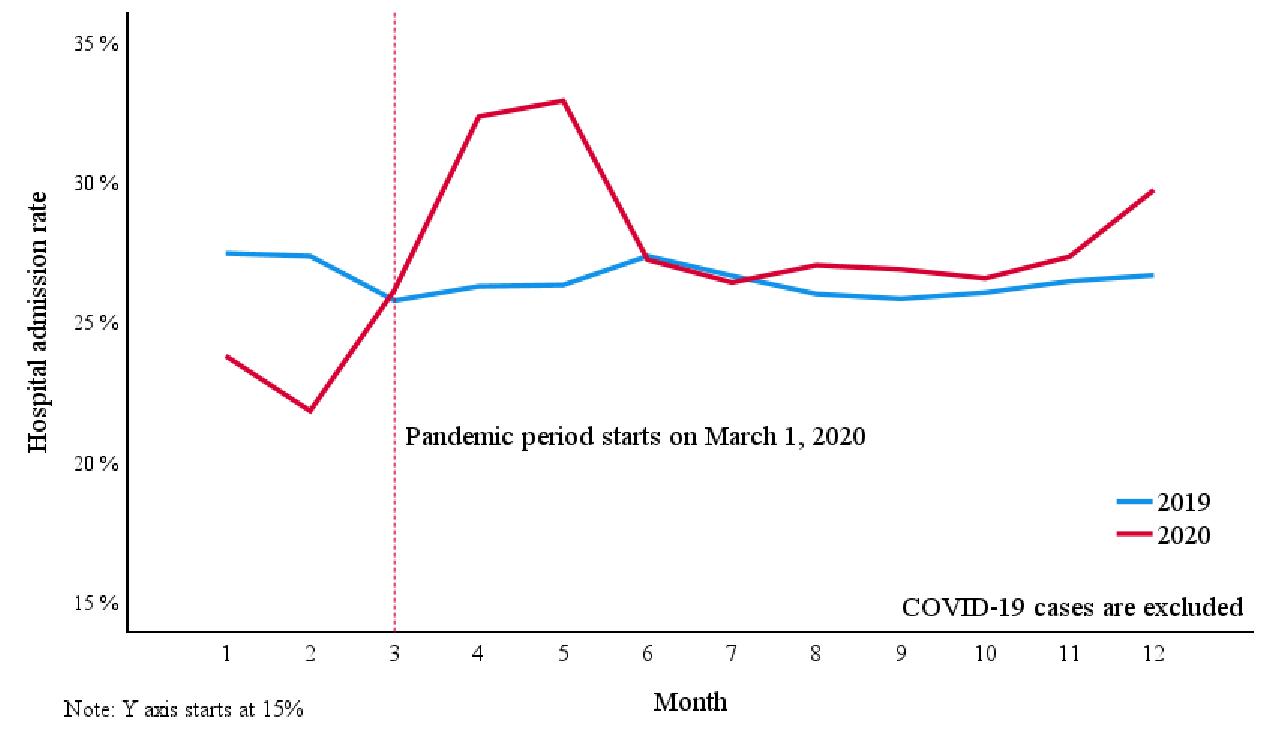
Figure 1. Hospital admission rates excluding COVID-19 cases following initial emergency department presentation, examining administrative data from January 1, 2019–December 31, 2020. This figure indicates the increase in hospital admission rate at the onset of the pandemic in March 2020 and the sustained elevation of admission rate compared to the year 2019, prior to the pandemic. The spike in admission rate is evidence of an increase in overall patient acuity throughout the time frame.
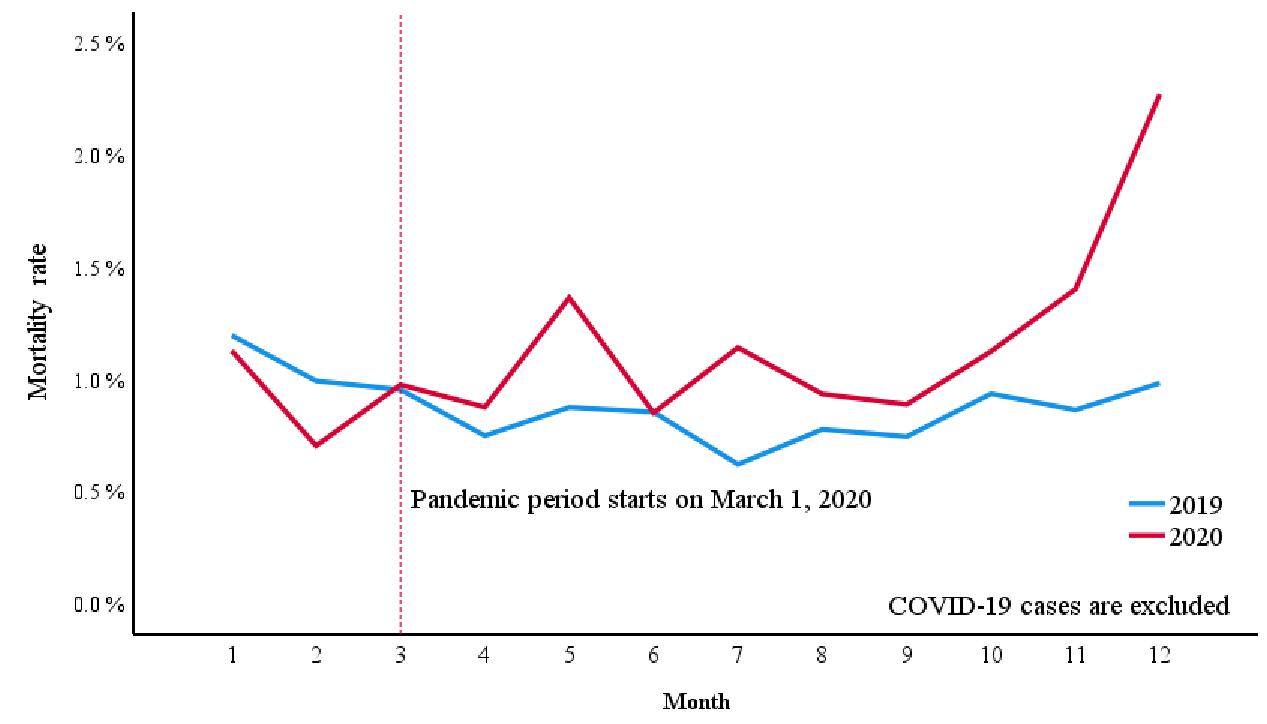
Figure 2. Overall emergency department mortality rate excluding COVID-19 cases before and during the COVID-19 pandemic, examining administrative data from January 1, 2019–December 31, 2020. The data show that at the onset of the pandemic in March 2020, mortality rate surged above the levels seen in 2019 and remained elevated throughout the remainder of the year
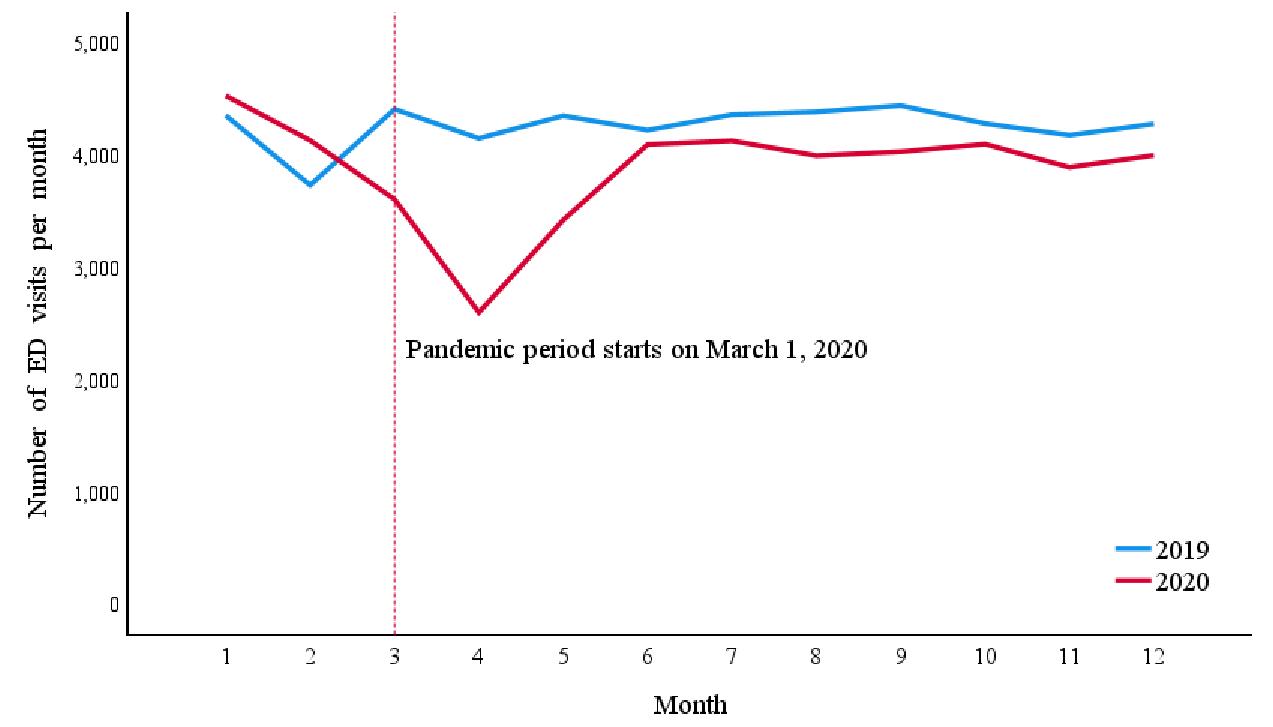
Figure 3. Number of emergency department visits per month excluding COVID-19 cases, examining administrative data from January 1, 2019–December 31, 2020. The data reveal a sharp decline in ED visits beginning in March 2020, coinciding with the onset of the pandemic. This decrease is sustained throughout the remainder of the year, with visits consistently lower in 2020 compared to 2019. ED, emergency department.
Insights from COVID-19
related presentations can be found in the appendix (Table S1).
The mean ESI of 59,205 pre-pandemic ED visits was 2.85 ± 0.707. During the pandemic, the mean ESI of 35,200 nonCOVID-19 ED visits was 2.84 ± 0.689 (P = .03). Figure 4 shows female:male ratio per different age groups before and during
the pandemic. Overall, female:male ratio was 1.003 (1.0031.004) before the pandemic and 0.885 (0.880 - 0.889) during the pandemic, excluding COVID-19 cases (P < .001) (Table 1).
DISCUSSION
Our results indicate that the decrease in the number of
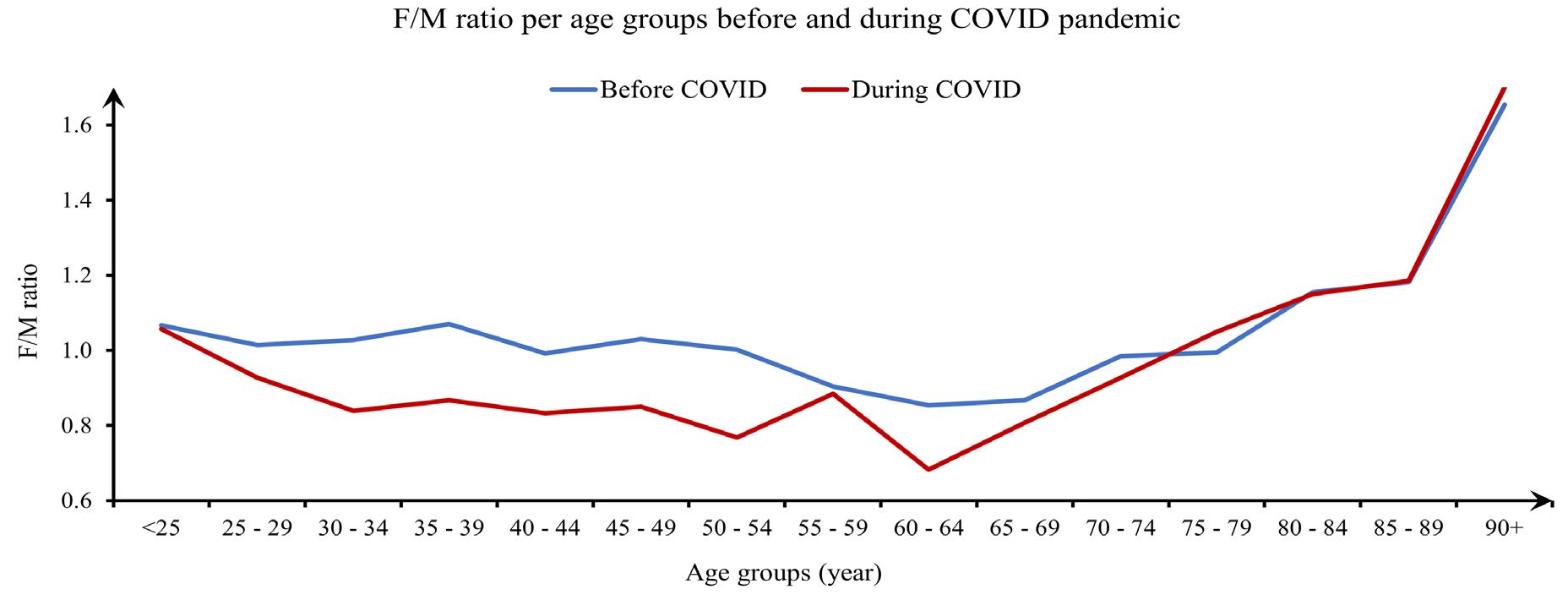
Figure 4. Female:male ratio for patients presenting to an emergency department before and during the COVID-19 pandemic, categorized by age groups, examining administrative data from January 1, 2019–December 3, 2020. The data reveal a consistent decrease in the female:male ratio throughout the measured pandemic period (March 1–December 31, 2020). F:M, female:male ratio.
visits during the pandemic was not limited to non-emergency cases; some patients in need of emergency care likely delayed seeking treatment. As a result, patient acuity increased as represented by higher admission and mortality rates, and the increase in mortality rate persisted even after excluding COVID-19-related cases. While the mean ESI demonstrated a statistically significant increase in patient acuity as well, this change was small and not clinically useful. The ESI does not accurately represent the increase in acuity in this period, which would be consistent with previous literature that ESI may not accurately represent acuity.13 With the limitations in the accuracy of ESI, ED leadership could consider using multiple measures of acuity in combination with ESI, or use more objective measures of acuity altogether. More objective systems have been proposed that have shown promise, such as early warning systems that predict urgency based on vital signs and level of consciousness scales.14 However, those systems would need to be validated and could potentially under-triage complaints with normal vital signs and level of consciousness such as giant cell arteritis or spinal cord injuries. Better systems would need to be developed and validated before any alternative to ESI could be recommended as a replacement.
The decline in overall number of ED visits during the pandemic aligns with other studies that demonstrated a 2058% reduction in visits.4,9,11 However, the significant increases seen in patient acuity throughout the literature emphasizes
the need to allocate resources properly in future health crises. Patient acuity refers to the intensity of care that a patient requires, and higher acuity places much greater demands on staff to provide both direct and indirect patient care. While not measured in this study, we acknowledge that changes to ED staffing, local protocols, and institutional policies during the pandemic may have influenced the observed outcomes.
In this study, we found that patient volumes decreased, and the mean ESI did not reflect a clinically useful change in acuity, despite the increased mortality and admission rates. This identifies the additional challenge of properly allocating resources during health crises, as it can be difficult to predict dynamic changes in patient acuity. To optimize an ED’s workforce, ensure maximum patient safety, and minimize mortality, it may be beneficial to consider metrics beyond patient volume and ESI when allocating staffing and resources. Measures could include the mortality rate, admission rate, or weighted diagnosis-related groups per month, although further research would be needed to identify and validate the best alternative measures of patient acuity to be used when determining resource allocation.
The significant decline in female:male ratio during the pandemic could reflect a difference in the ED use pattern between the sexes. One study conducted during the pandemic found that men were less likely to avoid ED visits (adjusted OR 0.53) compared to women.15 However, other studies reported no statistically significant difference in avoidance
behaviors between the sexes or that men were more likely to avoid ED visits.16,17 In the absence of a universal trend in data from other EDs supporting our measured decline in female:male ratio, it is unclear what drivers contributed to this finding. This observed sex difference could indicate anything from regional variations in self-triaging behaviors to distributions in underlying health conditions among sexes or local differences in sex-based behaviors such as caretaking responsibilities. Self-triage in the context of this discussion is a patient’s attempt to assess the priority of seeking care for their current medical complaint. Multiple factors influence self-triage decisions, including perceived risk and fear, which may have played a role in patients’ care-seeking behavior during the pandemic.
Understanding factors that influence patient decisions to seek emergency care are of foremost importance to managing future large-scale emergencies. Emergency situations can lead to damaged infrastructure, impact the economy, or overwhelm available resources. During the pandemic, transportation challenges and stay-at-home orders were significant barriers to seeking care.18,19 Fear of COVID-19 appeared to be a major factor influencing patient decision-making and selftriage behaviors during the pandemic. As discussed, one survey demonstrated that up to a quarter of patients may have prioritized avoidance of COVID-19 exposure over seeking lifesaving care in an emergency.8 In such cases, when patients delay seeking care based on perceived risk, an associated increase in acuity is expected.
The increased mortality rate seen in our study could reflect such self-triage behaviors, especially since this increased mortality rate was maintained even when excluding COVID-19 patients. There is a concern that severely ill patients may not have sought care in a timely manner, whether due to fear or barriers. If an increase in risk-taking behavior and severity of disease is associated with a significant decline in ED inflow, it could prove beneficial for healthcare forces to provide additional outreach services, such as telemedicine, to maintain patient safety and health during future accesslimiting situations.
Online tools guiding patients’ self-assessments might help optimize ED care-seeking decisions when patients choose to self-triage. Throughout the pandemic we saw the introduction of many novel algorithmic self-triage support tools ranging in complexity from healthcare worker flowchart screening to artificial intelligence chatbots integrated into existing health portals.20,21 Some of these were used on a large scale such as the US Centers for Disease Control and Prevention symptom-checker tool, and others were designed to target smaller populations such as college campuses.20 Multiple studies examining online symptom-checker tools observed trends of peak usage and/or symptom recognition preceding patient surges in local hospitals.22-24 It is likely that these tools encouraged sick patients to seek care, and further study of their data could yield the ability to anticipate healthcare
demand and provide additional information. The future development of these tools could help combat behaviors that contribute to hospital avoidance and delays in seeking care in access-limiting situations.
Throughout the pandemic, another common form of outreach was telehealth. While it can be difficult for EDs to incorporate telehealth given the nature of emergency situations, EDs could focus on forward triage as a means of telemedicine outreach. University of California Irvine Health incorporated a telemedicine system to provide 24/7 increased access to primary care clinicians during the pandemic. We acknowledge that this may have affected the results of this study as lower acuity patients may have sought care through alternative methods being offered within the same health system. Some studies have demonstrated feasibility and success with forward-triage.25-28 With an increase in barriers to care, stay-at-home mandates, and patient fears, telemedicine could help to increase access for lower acuity patients who are seeking care for non-life-threatening concerns. However, many challenges have been identified in the implementation of telemedicine, such as technical, legal, and ethical issues.29 Further research is required to characterize the feasibility and the effectiveness of these telemedicine systems to address challenges in access-limited scenarios.
This study demonstrates significant shifts in patient acuity and mortality during the pandemic, which could hold implications that extend to natural disasters or other public health crises. Our findings highlight the need to anticipate and address changes in patient behavior and barriers to seeking care during public emergencies when fear of the virus, hospital avoidance, or access barriers delay care and worsen outcomes. These findings also provide valuable data that contribute to our understanding of how the COVID-19 pandemic affected our healthcare system. Forms of outreach described here could be considered in future access-limiting situations to maintain patient safety. However, future research is needed to develop strategies that address the challenges posed by changes in care-seeking behaviors and local government restrictions to ensure minimal impact on patient mortality during future crises.
LIMITATIONS
This study is subject to the known limitations of a before-after study design. The study design may be limited by temporal confounding in which other unseen factors that occurred during the study period could have influenced the outcomes of the study, making it difficult to attribute the outcomes solely to the COVID-19 pandemic. Before-after study designs are also limited to discrete periods in time, and if initial measurements were different, the differences observed may represent a regression to the mean. Additionally changes to the methods of measurement may also occur during the period that data was being recorded, which can influence results. We addressed patient diagnosis variability by
Care-Seeking Hesitancy: Insights from COVID-19
categorizing primary diagnoses into 96 groups and adjusting for them in the multivariate analysis, but residual confounding may persist due to imperfect adjustment. Lastly, the singlecenter design of the study makes it subject to specific local policies, staffing changes, and pandemic response strategies, which limit generalizability.
Address for Correspondence: Soheil Saadat, MD MPH PhD, Department of Emergency Medicine, University of California, Irvine, 3800 W. Chapman Ave, Suite 3200, Orange, California, USA 92868. Email: saadat@hs.uci.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Frazier et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. US Centers for Disease Control and Prevention NCHS. Provisional COVID-19 Mortality Surveillance. 2024. Available at https://www.cdc. gov/nchs/nvss/vsrr/covid19/index.htm. Accessed October 22, 2024.
2. US Centers for Disease Control and Prevention NCHS. National Vital Statistics System, Provisional Mortality. Data are from the final Multiple Cause of Death Files, 2018-2022, and from provisional data for years 2023-2024. Available at http://wonder.cdc.gov/mcd-icd10provisional.html. Accessed October 22, 2024.
3. Satty T, Ramgopal S, Elmer J, et al. EMS responses and nontransports during the COVID-19 pandemic. Am J Emerg Med 2021;42:1-8.
4. Wai AK, Yip TF, Wong YH, et al. The effect of the COVID-19 pandemic on non-COVID-19 deaths: population-wide retrospective cohort study. JMIR Public Health Surveill. 2024;10:e41792.
5. Tam CF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv 2021;97(2):e194-e197.
6. Sheng S, Wang X, Gil Tommee C, et al. Continued underutilization of stroke care during the COVID-19 pandemic. Brain Behav Immun Health. 2021;15:100274.
7. Nguyen-Huynh MN, Tang XN, Vinson DR, et al. Acute stroke presentation, care, and outcomes in community hospitals in Northern California during the COVID-19 pandemic. Stroke. 2020;51(10):29182924.
8. Gale R, Eberlein S, Fuller G, et al. Public perspectives on
Frazier et al.
decisions about emergency care seeking for care unrelated to COVID-19 during the COVID-19 pandemic. JAMA Netw Open 2021;4(8):e2120940.
9. Finkelstein Y, Maguire B, Zemek R, et al. Effect of the COVID-19 pandemic on patient volumes, acuity, and outcomes in pediatric emergency departments: a nationwide study. Pediatr Emerg Care 2021;37(8):427-434.
10. Lyall MJ, Lone NI. Higher clinical acuity and 7-day hospital mortality in non-COVID-19 acute medical admissions: prospective observational study. Emerg Med J. 2021;38(5):366-370.
11. Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. Morb Mortal Wkly Rep. 2020;69(23):699-704.
12. Butt AA, Kartha AB, Masoodi NA, et al. Hospital admission rates, length of stay, and in-hospital mortality for common acute care conditions in COVID-19 vs. pre-COVID-19 era. Public Health 2020;189:6-11.
13. Hinson JS, Martinez DA, Schmitz PSK, et al. Accuracy of emergency department triage using the Emergency Severity Index and independent predictors of under-triage and over-triage in Brazil: a retrospective cohort analysis. Int J Emerg Med. 2018;11(1):3.
14. Schinkel M, Bergsma L, Veldhuis LI, et al. Comparing complaintbased triage scales and early warning scores for emergency department triage. Emerg Med J. 2022;39(9):691-696.
15. Mahmassani D, El Helou C, El Remlawi A, et al. Factors associated with emergency department avoidance during the COVID-19 pandemic and alternatives sought: a cross-sectional, telephonebased survey of frequent emergency department users in Beirut, Lebanon. BMJ Open. 2023;13(7):e072117.
16. Czeisler MÉ, Kennedy JL, Wiley JF, et al. Delay or avoidance of routine, urgent and emergency medical care due to concerns about COVID-19 in a region with low COVID-19 prevalence: Victoria, Australia. Respirology. 2021;26(7):707-712.
17. Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. Morb Mortal Wkly Rep. 2020;69(36):1250-1257.
18. Lam CN, Axeen S, Terp S, et al. Who stayed home under saferat-home? Impacts of COVID-19 on volume and patient-mix at an emergency department. West J Emerg Med. 2021;22(2):234-243.
19. Cochran AL, McDonald NC, Prunkl L, et al. Transportation barriers to care among frequent health care users during the COVID pandemic. BMC Public Health. 2022;22(1):1783.
20. Ziebart C, Kfrerer ML, Stanley M, et al. A digital-first health care approach to managing pandemics: scoping review of pandemic selftriage tools. J Med Internet Res. 2023;25:e40983.
21. Munsch N, Martin A, Gruarin S, et al. Diagnostic accuracy of webbased COVID-19 symptom checkers: comparison study. J Med Internet Res. 2020;22(10):e21299.
22. Galmiche S, Rahbe E, Fontanet A, et al. Implementation of a selftriage web application for suspected COVID-19 and its impact on emergency call centers: observational study. J Med Internet Res
Frazier et al.
2020;22(11):e22924.
23. Denis F, Fontanet A, Le Douarin YM, et al. A self-assessment webbased app to assess trends of the COVID-19 pandemic in France: observational study. J Med Internet Res. 2021;23(3):e26182.
24. Tozzi AE, Gesualdo F, Urbani E, et al. Digital surveillance through an online decision support tool for COVID-19 over one year of the pandemic in Italy: observational study. J Med Internet Res. 2021;23(8):e29556.
25. Bourdon H, Jaillant R, Ballino A, et al. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: patients’ point of view. J Fr Ophtalmol. 2021;44(3):e127-e129.
26. Nunziata F, Bruzzese E, Poeta M, et al. Health-care organization
Care-Seeking Hesitancy: Insights from COVID-19
for the management and surveillance of SARS-CoV-2 infection in children during pandemic in Campania region, Italy. Ital J Pediatr 2020;46(1):170.
27. Ko KJ, Kurliand MM, Curtis KM, et al. Launching an emergency department telehealth program during COVID-19. JGEM. 2020;1(7),1-7.
28. Smith NJ, Bausano BJ, Zachrison KS, et al. Emergency medicine telehealth: a pandemic becomes a gateway for virtual care in Missouri. Mo Med. 2022;119(5):452-459.
29. Sharifi Kia A, Rafizadeh M, Shahmoradi L. Telemedicine in the emergency department: an overview of systematic reviews. Z Gesundh Wiss. 2022:1-15.
Foundations of Emergency Medicine: Application of a Flipped-Classroom Curriculum for Advanced Practice Clinician Education
Steven Lindsey, MD*
Tim P. Moran, PhD*
Meredith A. Stauch, MSN, APRN†
Alexis L. Lynch, MSN, APRN*
Jordan Leumas, MD‡
Kristen Grabow Moore, MD, MEd*
Section Editor: Jeffrey Druck, MD
Emory University, Department of Emergency Medicine, Atlanta, Georgia
Emory University School of Medicine, Atlanta, Georgia
Wellstar Kennestone Regional Medical Center, Emergency Medicine Residency Program, Marietta, Georgia
Submission history: Submitted January 31, 2025; Revision received June 4, 2025; Accepted June 9, 2025
Electronically published September 12, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.42231
Introduction: Advanced practice clinician (APC) presence has increased in emergency departments (ED), leading to increased exposure to higher acuity patient conditions. Relatively few APCs have completed formalized postgraduate emergency medicine (EM)-specific training, creating uncertainty around how well prepared APCs are in identifying and treating life-threatening conditions. Foundations of Emergency Medicine (FoEM) offers free open-access curricula, including Foundations I (F1), a flipped-classroom course targeting fundamental knowledge for resident physicians. We sought to use F1 for APC learners to improve their knowledge in identifying and treating emergent conditions.
Methods: In our single-center study, 23 APC postgraduate learners (17 nurse practitioners and 6 physician assistants) completed the F1 course between 2020-2021. The F1 course consisted of 23 virtual meetings led by faculty and senior residents, each lasting one hour. The APCs were asked to review vetted asynchronous resources for a recommended two hours before participating in small group, case-based learning sessions involving real-time feedback, curated teaching points, and paired online assessments. Immediately before and following F1 course implementation, participants completed a 50-question multiple-choice test and attitudes survey to quantify knowledge acquisition and evaluate the course. We evaluated change in knowledge scores using a Friedman test. Changes in self-assessed knowledge were evaluated using mixed-effects ordinal logistic regression.
Results: Knowledge assessments showed APCs universally improved from the pre-course test (median score 23, 46%, IQR 20-26) to the post-course test (median score 33, 66%, IQR 31-37; adjusted P < .001). The APC self-assessments revealed improved overall EM knowledge (adjusted P = .02), yet respondents also reported an increased likelihood of seeking attending physician help (adjusted P < .001). Overall, 96% were satisfied with the course, 100% agreed that the course difficulty was appropriate, and 79% believed the course improved their performance in a clinical setting.
Conclusion: Implementation of the Foundations of Emergency Medicine, Foundations 1, curriculum was associated with increased classroom knowledge and self-assessed overall knowledge in EM among advanced practice clinicians, with high learner satisfaction in the course. Along with knowledge improvement, APCs also reported increased likelihood to seek guidance from an attending physician. These data form the basis for the use of FoEM in the APC learner population. [West J Emerg Med. 2025;26(5)1226–1231.]
INTRODUCTION
Advanced practice clinicians (APC), including nurse practitioners (NP) and physician assistants (PA), have a significant presence in emergency medicine (EM). It is estimated that over 13,000 PAs and 26,000 NPs currently practice in acute care settings,1,2 with over 75% of emergency departments (ED) having APC representation.3,4 The APCs are involved in at least 20% of all ED visits, and the proportion of billing for higher acuity conditions by APCs is expanding over time,5-7 as APCs may work in higher acuity areas under direct physician supervision.8,9
Although some APCs care for patients with higher acuity pathologies in the ED,7 a relatively small proportion have completed formalized postgraduate training in EM, with 10% of PAs and 21% of NPs having received such training.2,10 The American Academy of Emergency Nurse Practitioners and the Society of Emergency Medicine Physician Assistants acknowledge the importance of APCs being able to identify and manage high-acuity conditions.11,12 Despite this, no consistent standardized approach exists to address this gap in EM-specific training.13,14
Foundations of Emergency Medicine (FoEM) is a free, open-access curriculum that offers standardized, level-specific core content. It is widely used in EM resident education with demonstrated success in improving knowledge acquisition.15,16 Foundations I (F1) is a longitudinal, flipped-classroom course developed for first-year resident physicians and provides systems-based review of fundamental EM knowledge. We sought to address the potential gap in APC EM-specific education and improve APC knowledge of higher acuity pathologies by implementing the F1 course.
METHODS
Study Population and Design
For our single-site study from October 2020–June 2021, APCs were included if they practiced at a large, urban, county, primarily adult hospital in Atlanta, Georgia, and enrolled in the FoEM F1 course. While course enrollment was mandatory to work in the higher acuity areas of the ED, study participation was voluntary. All APCs chose to participate in the course. Using a flipped-classroom model, APCs were asked to spend two hours reviewing vetted, multimodal, asynchronous study materials prior to each of the 23 didactic sessions. Implementation guidelines and curricular resources can be found on the FoEM website.17,18 The topics included all F1 content apart from trauma- and pediatric-related modules, which are rarely seen in the intended area for the APCs after course completion (Appendix 1). During one-hour virtual active learning sessions, participants collaboratively worked through case-based scenarios in small groups guided by faculty or upperlevel EM resident group leaders. Instructors provided feedback on simulated clinical care and reviewed salient learning points, focusing on recognition, stabilization, evaluation, and treatment of higher acuity pathologies. While asynchronous studying was
Population Health Research Capsule
What do we already know about this issue?
Advanced practice clinicians (APC) see a significant number of patients, some of whom may have life-threatening conditions, yet their training curricula vary.
What was the research question?
Does the implementation of the Foundations of Emergency Medicine (FoEM) F1 course improve APC knowledge in emergent conditions?
What was the major finding of the study?
Knowledge improved from the pre-course (median [IQR] 23/50, 46%, [20-26]) to the post-course test (median [IQR] 33/50, 66%, [31-37]; P < .001).
How does this improve population health?
The FoEM F1 curriculum improved APC knowledge of life-threatening conditions, while also increasing the likelihood of seeking an attending physician for guidance.
not tracked, APCs were required to attend 75% of sessions for course completion.
To assess knowledge acquisition, study participants completed the same 50-question multiple-choice assessment pre- and post-course. Test items were curated by the two course directors (SL and KM) who referenced course objectives and selected, with permission, from assessment items that were developed and validated by Rosh Review specifically for use with FoEM courses. The APCs additionally completed a knowledge, attitudes, and practices (KAP) survey at the beginning and completion of the course (Appendix 2). The KAP survey was developed according to best practices in survey design.19,20 All survey items were piloted prior to administration. The post-course survey also included APCs’ impression of the course but was otherwise identical to the pre-course survey. This study was deemed exempt by the institutional review board of Emory University.
Statistical Analysis
We described categorical variables using frequencies and percentages. Continuous and scale variables were described using medians and interquartile (IQR) ranges. We evaluated change in knowledge scores between the pre-course and postcourse test sessions using the Friedman repeated-measures
rank-order ANOVA. Ordinal self-assessment variables were evaluated using a mixed-effects ordinal logistic regression. We used mixed effects to account for multiple responses from individual study participants. To avoid inflated false positives due to multiple testing, we adjusted P values using the method developed by Benjamini and Yekutieli.24 Statistical analyses were conducted using R v4 (The R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
A total of 23 APCs enrolled, with a median age of 37 (IQR 33-40) years and with the majority identifying as female (74%) (Table 1). Learners were primarily family NPs (48%), followed by PAs (26%) and emergency NPs (22%), with a median of five years (IQR 3-6) of postgraduate experience in EM. A small proportion reported completing formalized postgraduate training in EM (13%).
Table 1. Demographic characteristics of advanced practice clinicians enrolled in the Foundations of Emergency Medicine Foundations I Course, October 2020–June 2021.
Characteristic
Age, Median (IQR)*
Gender, n (%)
Female
Male
Certification, n (%)
Adult Gerontology Nurse
Practitioner
Family Nurse Practitioner
Family/Emergency Nurse
Practitioner
Physician Assistant
Postgraduate Experience in Emergency Medicine, Median (IQR), years
Completed Emergency Medicine
postgraduate training program, n (%)
IQR, interquartile range.
N = 23
37 (33-40)
17 (74%)
6 (26%)
1 (4%)
11 (48%)
5 (22%)
6 (26%)
5 (3–6)
3 (13%)
Knowledge assessments for the APCs significantly improved from the pre-course test to post-course test (P < .001, adjusted P < .001, Figure 1, Appendix 3), with a standardized median difference of 1.8 (95% CI 1.0-2.6). The pre-course test had a median (IQR) score of 23/50 (20-26) and the post-course test a median (IQR) score of 33/50 (31-37), with all APCs demonstrating improvement in their scores (Figure 2).
With respect to self-assessed overall knowledge in EM, 100% of participants reported average knowledge prior to the course,
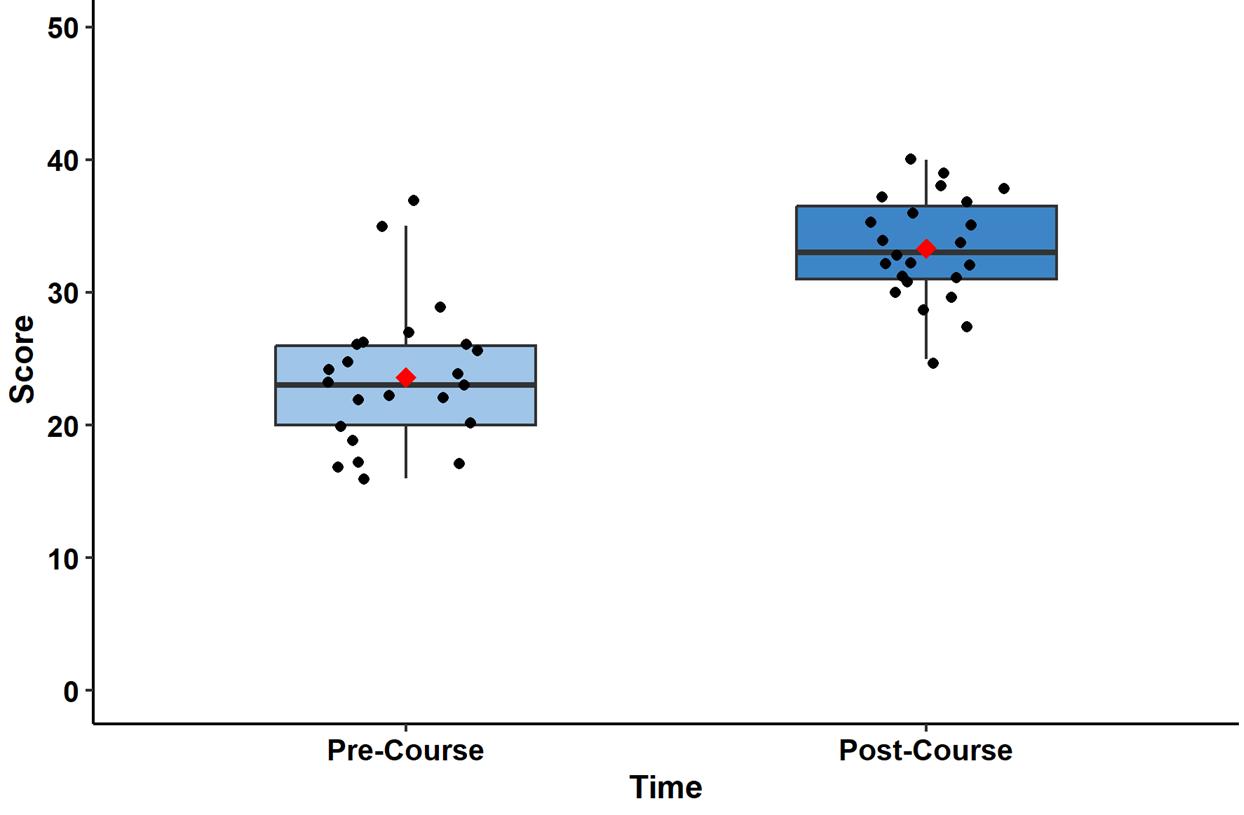
Figure 1. Objective knowledge acquisition of advanced practice clinicians before and after the Foundations of Emergency Medicine Foundations I course.
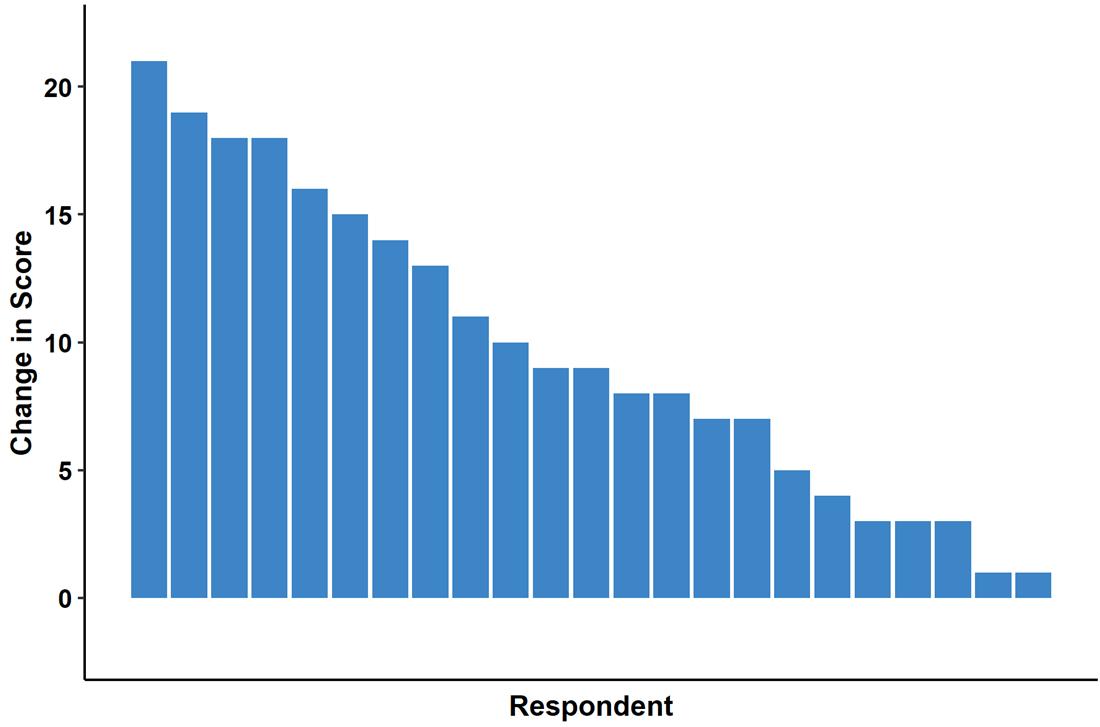
Figure 2. Change in individual knowledge test scores of advanced practice clinicians before and after Foundations of Emergency Medicine Foundations I course.
compared to 43.5% above-average knowledge following the completion of the course (P = .01, adjusted P = .02) (Figure 3).
Because the units of educational assessments are often specific to the assessment, the effects of an intervention are often expressed as standardized mean or median differences.21-23 We present the mean and median difference in knowledge assessment, the standardized mean and median differences, and 95% CI. 21-23 The CIs were computed using bias-corrected and accelerated bootstrap resamples (100,000 resamples). As a rough rule, standardized differences of 0.2 are considered small, 0.5 are considered medium, and 0.8 are considered large.
Results from the KAP survey (Appendix 4) revealed significant improvement in APCs’ perceived ability to communicate with consultants (P < .001, adjusted P = .001) when caring for Emergency Severity Index (ESI) level 2 patients. Participants were significantly more likely to approach an attending physician to seek help with medical decision-
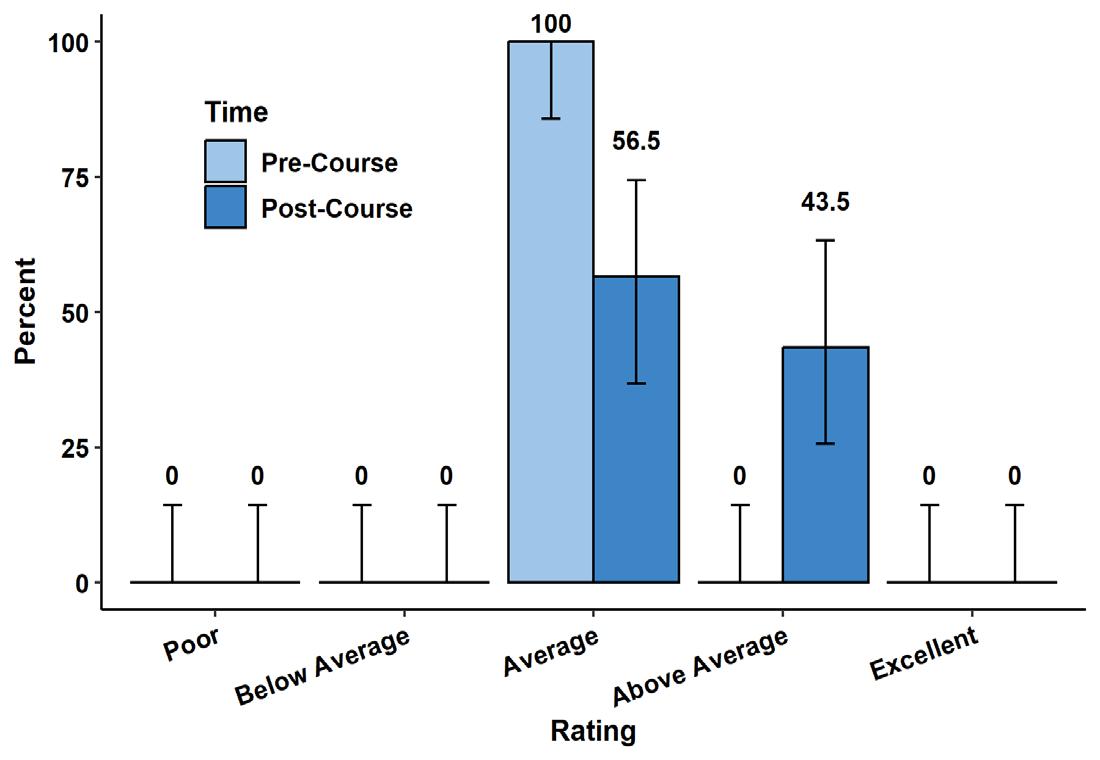
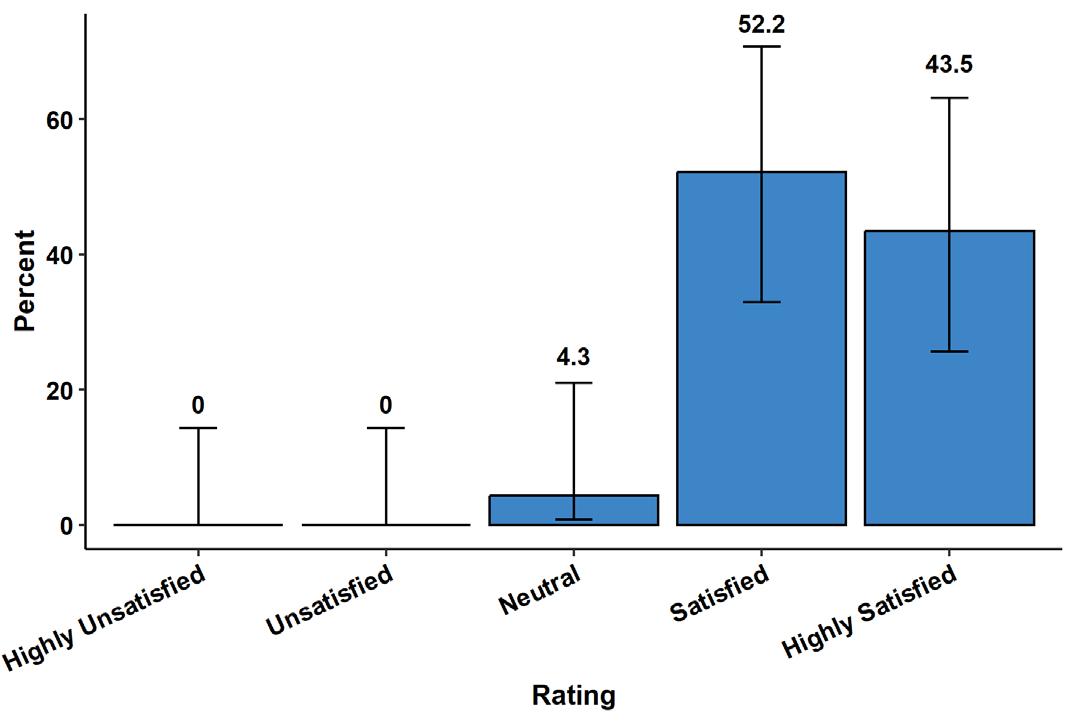
making (P < .001, adjusted P < .001). No significant change was observed with APCs’ self-assessed ability to stabilize ESI level 2 patients in the ED (P = .03, adjusted P = .09) or APCs’ perceived ability to rule out life-threatening illnesses (P = .03, adjusted P = .09).
In the post-course survey, 22/23 (96%) of APCs reported being either satisfied (52%) or highly satisfied (44%) with the course, while only 1/23 (4%) was neutral (Figure 4). When asked about the F1 course content being appropriate for the APCs’ level of learning, 23/23 (100%) responded as either agree (30%) or strongly agree (70%). The APCs either agreed (44%) or strongly agreed (35%) that the course improved their ability to manage high-acuity patients in the clinical environment. Only 5/23 were neutral, and no respondents disagreed.
DISCUSSION
Advanced practice clinicians represent a sizable portion of the EM workforce3,5 and can work in both triage and variable acuity settings in the ED,8,9 making it of paramount importance that they recognize patients with more subtle presentations of higher acuity illnesses or potential life-threatening conditions. Our study demonstrated significant improvement in APC objective and self-assessed knowledge acquisition, along with gains in several facets of caring for higher acuity patients following implementation of the FoEM F1 course. Although the post-course multiple-choice scores were still low on average, there was significant improvement from the pre-course exam. Most notably, our findings have a high median standardized difference change of 1.8, reflecting a sizable improvement in exam scores. (See Appendix 3 for more explanation.) Our findings mirror those observed for electrocardiogram interpretation in the same cohort, namely the likelihood of approaching a physician for guidance, self-assessed knowledge improvement, and objective knowledge acquisition.25
It is possible that some of these knowledge gains were due
to clinical experience and exposure; however, the curriculum was only nine months long and the APCs as individuals were infrequently in higher acuity areas of the ED over that time. While we are encouraged by the knowledge gained by the APCs in the F1 course, we recognize that classroom knowledge may not always translate to a meaningful change in practice. Our study does, however, provide a solid base on which to investigate the impact of F1 on clinical practice.
As is the case in some ED settings, APCs may not have immediate access to physician guidance.26 We advocate for direct physician supervision of APCs caring for higher acuity patients, and our study revealed that despite recognized knowledge gains, our APCs had increased likelihood of seeking guidance from an attending. We hypothesize that this may reflect better clinical understanding and more open lines of communication, although this would need better elucidation in future studies.
Improvement in APC knowledge and confidence in caring for subtle or overtly high-acuity ED patients is of great importance. To achieve this, APC learners must be motivated to engage in continuing education; thus, the delivery of educational material matters a great deal. The APCswho enrolled in our FoEM F1 course were overwhelmingly satisfied with the course and universally felt the content was appropriate for their level of training. Use of the case-based curriculum is in line with recommendations for APC education27 and translated to high engagement and knowledge acquisition.
LIMITATIONS
Our study included a small sample size with a relatively homogeneous study population. Additionally, our study cohort did not fully reflect the 2:1 distribution of NPs and PAs practicing in acute care settings, with our group having only 26% PA representation. Due to the inherent differences in selfreported knowledge and objective tested knowledge, we chose not to attempt to correlate the two, instead focusing on them
Figure 4. Advanced practice clinicians’ rating of overall satisfaction with the Foundations of Emergency Medicine Foundations I course.
Figure 3. Self-rated knowledge in emergency medicine of advanced practice clinicians prior to and following Foundations of Emergency Medicine Foundations I Course.
as individual findings in the study. Finally, our study did not include a control group with access to the curriculum, thereby allowing for the possibility of test/retest effects, although we believe this effect to have been small.28
CONCLUSION
Foundations of Emergency Medicine offers a ready-made and well-received, case-based interactive learning modality for advanced practice clinicians in EM. By exposing our APC learners to the Foundations 1 course, our study demonstrated significant knowledge and confidence gains, along with a greater willingness to seek guidance from attending physicians. Future directions call for implementation and analysis of the curriculum in other EM APC learners, in larger cohorts, in different practice settings, and with more patient-oriented outcomes with the goal of a more representative reflection of validity across all EM-practicing APCs.
Address for Correspondence: Steven Lindsey, MD, Emory University, Department of Emergency Medicine, 531 Asbury Circle, Annex Building, Suite N340, Atlanta, GA 30322. Email: steven.m.lindsey@emory.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Lindsey et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. American Academy of Nurse Practitioners website. NP Fact Sheet. 2025. Available at: https://www.aanp.org/about/all-about-nps. Accessed May 9, 2024.
2. National Commission on Certification of Physician Assistants. 2021 Statistical Profile of Certified PAs. 2022. Available at: https://www. nccpa.net/wp-content/uploads/2022/08/2021StatProfileofCertifiedP As-A-3.2.pdf. Accessed May 9, 2024.
3. Menchine MD, Wiechmann W, Rudkin S. Trends in midlevel provider utilization in emergency departments from 1997 to 2006. Acad Emerg Med. 2009;16(10):963-9.
4. Aledhaim A, Walker A, Vesselinov R, et al. Resource utilization in non-academic emergency departments with advanced practice providers. West J Emerg Med. 2019;20(4):541-8.
5. Wu F, Darracq MA. Comparing physician assistant and nurse practitioner practice in U.S. emergency departments, 2010-2017. West J Emerg Med. 2021;22(5):1150-5.
6. Gettel CJ, Schuur JD, Mullen JB, et al. Rising high-acuity emergency
care services independently billed by advanced practice providers, 2013 to 2019. Acad Emerg Med. 2023;30(2):89-98.
7. Pines JM, Zocchi MS, Ritsema T, et al. The impact of advanced practice provider staffing on emergency department care: productivity, flow, safety, and experience. Acad Emerg Med 2020;27(11):1089-99.
8. Wylie K, Crilly J, Toloo GS, et al. Review article: emergency department models of care in the context of care quality and cost: a systematic review. Emerg Med Australas. 2015;27(2):95-101.
9. Moretz, J. Emergency Department Care Models. 2018. Available at: https://www.thinkbrg.com/insights/publications/emergencydepartment-care-models. Accessed April 11, 2023.
10. American Academy of Nurse Practitioners. The State of the Nurse Practitioner Profession. 2021. Available at: https://www.aanp.org. Accessed April 12, 2023.
11. American Academy of Emergency Nurse Practitioners. Practice Standards for the Emergency Nurse Practitioner Specialty. 2018. Available at: https://www.aaenp-natl.org/assets/docs/practice_standards_for_the_ emergency_nurse_practitioner.pdf. Accessed April 11, 2023.
12. Society of Emergency Medicine Physician Assistants. Emergency Medicine Physician Assistant Practice Guidelines. 2021. Available at: https://www.sempa.org/about-sempa/guidelines-and-statements/ empa-practice-guidelines. Accessed April 12, 2023.
13. Kraus CK, Carlisle TE, Carney DM. Emergency medicine physician assistant (EMPA) postgraduate training programs: program characteristics and training curricula. West J Emerg Med 2018;19(5):803-7.
14. Chekijian SA, Elia TR, Monti JE, et al. Integration of advanced practice providers in academic emergency departments: best practices and considerations. AEM Educ Train. 2018;2(Suppl Suppl 1):S48-55.
15. Grabow Moore K, Ketterer A, Wheaton N, et al. Development, implementation, and evaluation of an open access, level-specific, core content curriculum for emergency medicine residents. J Grad Med Educ. 2021;13(5):699-710.
16. Jordan J, Wheaton N, Hartman ND, et al. Foundations of Emergency Medicine: impact of a standardized, open-access, core content curriculum on in-training exam scores. West J Emerg Med. 2024;25(2):209-12.
17. Foundations of Emergency Medicine. FoEM Courses. 2025. Available at: https://foundationsem.com/foundations-courses. Accessed June 12, 2024.
18. Foundations of Emergency Medicine. Quick Links for Leaders. 2025. Available at: https://foundationsem.com/quicklinks-forleaders Accessed June 12, 2024.
19. Artino AR, Jr., La Rochelle JS, Dezee KJ, et al. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach. 2014;36(6):463-74.
20. Rickards G, Magee C, Artino AR, Jr. You can’t fix by analysis what you’ve spoiled by design: developing survey instruments and collecting validity evidence. J Grad Med Educ. 2012;4(4):407-10.
21. Cohen J. (1998). The t Test for Means. In Statistical Power Analysis for the Behavioral Sciences (20-26). London, UK: Routledge Publishing.
22. Wilcox R. A robust nonparametric measure of effect size based on an analog of Cohen’s d, plus inferences about the median of the typical
difference. J Mod Appl Stat Methods. 2018;17(2):eP2726.
23. Cohen J, Cohen P, West, SG, et al. (2002). Bivariate correlation and regression.In Applied Mulitple Regression/Correlation Analysis for the Behavioral Sciences (23-25, 50-52). London, UK: Routledge Publishing.
24. Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. 2001;29(4):1165-88.
25. Lindsey S, Moran TP, Stauch MA, et al. Bridging the gap: evaluation of an electrocardiogram curriculum for advanced practice clinicians.
West J Emerg Med. 2024;25(2):155-9.
26. Clark A, Amanti C, Sheng AY. Supervision of Aadvanced practice providers. Emerg Med Clin North Am. 2020;38(2):353-61.
27. Breunig MJ, Herber AJ, Jenkins SM, et al. Characteristics of effective continuing medical education for physician assistants and nurse practitioners in hospital medicine. J Physician Assist Educ 2020;31(1):2-7.
28. Scharfen J, Blum D, Holling H. Response time reduction due to retesting in mental speed tests: a meta-analysis. J Intell. 2018;6(1):1-28.
Emergency Department Wait Times for Urgent Evaluation by Race,
Ethnicity, and Language:
A Single-center Retrospective Study
Jossie A. Carreras Tartak, MD, MBA
Anne V. Grossestreuer, PhD
David
Chiu, MD, MPH
Bryan
Stenson, MD
Section Editor: Laura Walker, MD
Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, Massachusetts
Submission history: Submitted February 11, 2025; Revision received May 8, 2025; Accepted May 30, 2025
Electronically published September 20, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.43480
Introduction: Black and Hispanic patients, and patients with a preferred language other than English experience longer emergency department (ED) wait times and delays in treatment. We aimed to evaluate racial, ethnic, and language-based differences in wait times to see a physician and get a disposition, as well as in the rates of objective vs subjective urgent evaluations.
Methods: This was a retrospective study of all ED visits in our tertiary-care, academic medical center from July 2021–June 2023. Using electronic health record data, we compared time-tophysician, physician-to-decision times, and frequency of triggers (urgent evaluations based on objective criteria) and priority assessments (urgent evaluations that can be based on subjective perception of patient acuity) by race, ethnicity, and preferred language. We used logistic regression, controlling for age, Emergency Severity Index, and sex to compare differences in trigger rates.
Results: We included 93,728 patient encounters in this study. Black patients had a median timeto-physician of 31 minutes compared to 24 minutes for White patients (adjusted median difference (aMD) 3.2, 95% CI 2.4-3.9]) and a median physician-to-decision time of 228 minutes compared to 213 for White patients (aMD 15.0, 95% CI 12.0-17.9). Hispanic patients had a median time to physician of 31 (aMD compared to White patients = 3.4, 95% CI 2.4-3.9) and a median physicianto-decision time of 233 minutes (aMD compared to White patients 21.3, 95% CI 17.5-25.2).
Patients with a preferred language other than English had a median time-to-physician of 33 minutes compared to 25 in English-preferring patients (aMD 4.6, 95% CI 3.7-5.6) and a median physician-to-decision time of 234 compared to 214 minutes for English-preferring patients (aMD 17.1, 95% CI 13.6-20.7). Black patients were less likely to have a trigger activated relative to White patients (adjusted odds ratio [aOR] 0.88, 95% CI 0.82-0.95). Black patients (aOR 0.72, 95% CI 0.67-0.77), Hispanic/Latino patients (aOR 0.78, 95% CI 0.71-0.86), and non-English-preferring patients (aOR 0.85, 95%CI 0.78-0.92) were less likely to have a priority assessment called compared to White patients.
Conclusion: Black, Hispanic, and patients who prefer non-English language experience delays in time-to-physician and physician-to-decision time. Black patients are less likely to have triggers activated. Black, Hispanic, and patients who prefer non-English language are less likely to have priority assessments activated compared to White patients. These findings underscore the need to develop additional mechanisms for mitigating biases in the triage process. [West J Emerg Med. 2025;26(5)1232–1243.]
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
INTRODUCTION
Emergency departments (ED) play a critical role in providing timely medical care for patients in acute situations where delays can lead to worse outcomes. However, evidence shows that disparities exist in how quickly patients from different racial, ethnic, and linguistic backgrounds are evaluated in the ED.1–6 Longer wait times can lead to patients leaving without being seen,7 as well as delays in timely diagnosis and treatment of time-sensitive conditions. Racial disparities in time-to-treatment of acute coronary syndrome,8 stroke,9 and appendicitis10 have been documented in the literature. Furthermore, Black and Hispanic patients are more likely to have longer lengths of stay (LOS) in the ED.11–13 Studies on LOS of patients with limited English proficiency (LEP) have been mixed, with some sites showing longer LOS for patients with LEP.14,15
While most EDs in the United States use the Emergency Severity Index (ESI) triage algorithm to signal to physicians the acuity of a patient’s condition, several studies have observed racial, ethnic, and language-based disparities in the assignment of ESI triage scores to ED patients with a given chief complaint,16,17 as well as higher instances of mistriage for Black patients.18 Even in hospitals that do not rely on ESI scores, Black and Hispanic patients with a given chief complaint are more likely to be triaged to lower acuity areas in the ED than their White counterparts.19
The purpose of this study was to evaluate racial, ethnic, and language-based differences in wait times for a physician and a disposition, as well as in the rates of objective vs subjective urgent evaluations. In this study, we aimed to quantify the following: 1) delays in time to see physician; 2) differences in physician-to-decision time; and 3) differences in the proportion of urgent evaluations across racial, ethnic, and linguistic groups in our own ED. At the time of this study, we used a proprietary electronic health record (EHR), which did not rely exclusively on ESI scores to mandate rapid evaluations of patients with concerning presentations. Furthermore, we employed a system of overhead calls and pages that alerted medical teams about a patient who needed to be urgently evaluated based on vital signs, symptoms, or nursing concerns. We hypothesized that these factors would mitigate the racial, ethnic, and language-based disparities in wait times and LOS reported at other sites. We also hypothesized that rates of urgent evaluations would be similar across all groups.
METHODS
Emergency Department Protocols
Our ED uses an overhead and paging alert system for patients requiring urgent evaluation by the medical team. There are two types of urgent evaluation: 1) triggers and rapid assessments; and 2) priority assessments. Both triggers and rapid assessments require a junior and a senior resident to immediately evaluate the patient in question. The main
Population Health Research Capsule
What do we already know about this issue?
Prior studies have shown that Black, Hispanic, and limited English proficiency (LEP) patients experience longer wait times in the ED.
What was the research question?
Do Black, Hispanic, and LEP patients experience longer wait times and lower rates of urgent evaluation?
What was the major finding of the study?
Black (aOR 0.72, 95% CI 0.67-0.77), Hispanic (aOR 0.78, 95% CI 0.71-0.86), and LEP patients (aOR 0.85, 95% CI 0.78-0.92) were less likely to get an priority assessment and more likely to wait longer.
How does this improve population health?
Our results could lead to interventions like increased outpatient access to care and interpreter availability.
difference between triggers and rapid assessments (besides the specific criteria for activating each) is that attending physicians are technically not required to respond immediately to the rapid assessments, but in practice nearly all of them do. Furthermore, triggers and rapid assessments (unlike priority assessments) are meant to be disruptive and summon clinicians immediately to a patient’s bedside. Because triggers and rapid assessments are in practice treated equally by the medical teams, they are hereby referred to collectively as “triggers.”
When a trigger is announced overhead and via the paging system, a team comprised of a junior and senior resident, and an attending physician must immediately evaluate the patient in question. Triggers can be activated by anyone on the medical team whenever a patient meets certain objective criteria, such as abnormal vital signs, if they are intubated or on positive pressure ventilation, or if they have an immediately life- or limb-threatening chief complaint such as a ST-elevation myocardial infarction, trauma, stroke symptoms, allergic reaction, or pulseless extremity. Alternatively, priority assessments are used to identify patients who should be seen next by a resident physician but do not require an immediate bedside evaluation by the entire medical team. While there are some objective criteria for activating
Carreras Tartak et al.
priority assessments, unlike triggers, priority assessments can also be activated subjectively if a member of the team is concerned about the patient. The criteria for activating each type of expedited evaluation are outlined in Figure 1.
Our EHR sorts patients waiting for a physician to assign themselves by the following criteria:
1. Triggers, sorted with the oldest on top
2. Priority assessments, sorted by most recently to least recently moved to the top
3. ESI levels 1 and 2 who have not been claimed in > 1 hour, sorted by longest to shortest wait time
4. Patients in a treatment room, sorted by longest time in room to shortest
5. Patients in the ambulance waiting area, sorted by longest to shortest wait time
6. Waiting room patients, sorted by longest to shortest wait time
Resident physicians are instructed to assign themselves to patients in the order in which they appear on the list of
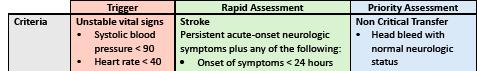
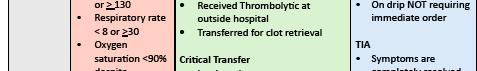
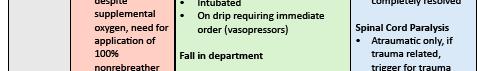
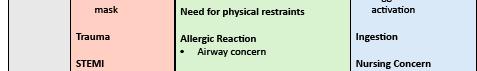

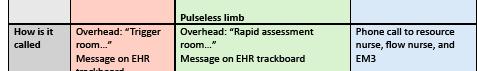
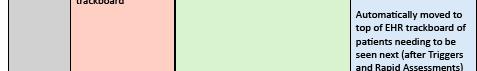
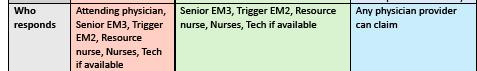
Figure 1. Criteria to activate “trigger,” rapid assessment, and priority assessment in emergency department patients. BIPAP, bilevel positive airway pressure; EHR, electronic health record; EMS, emergency medical services; PGY, postgraduate year; TIA, transient ischemic attack; VS, vital signs.
patients to be seen to avoid skipping over potentially ill patients. In our ED, physician teams are not confined to specific geographical zones or room numbers and can see patients throughout the department in the appropriate order as determined by their acuity. This also means that patients can be evaluated while in the waiting room, where they can receive limited interventions such as lab draws and imaging that does not require intravenous contrast. Therefore, we evaluated “time-to-physician” rather than “time in waiting room” to more accurately measure patient wait times.
Data Analysis
This was a retrospective study of all ED visits from July 2021–June 2023 in our tertiary-care academic medical center with a Level I Trauma and Comprehensive Stroke Center designations and an annual census over 50,000 visits. Our hospital does not have pediatric services; thus, patients < 18 years of age presenting to the ED are either transferred to a pediatric facility or evaluated at our facility on a case-by-case basis. All data were abstracted from the EHR by a single abstractor using best practices outlined by Worster and colleagues,20 which included pre-defined inclusion and exclusion criteria, variable definition prior to abstraction, and institutional review board approval (Protocol #: 2023P000990). We evaluated time-to-physician, defined as the time between a patient arriving to the ED and a physician claiming that patient in the EHR, and physician-to-decision time defined as the time elapsed between a physician assigning themselves to a patient and a disposition being selected for the patient. We included only encounters with a disposition other than “admission from the ED,” “discharge from the ED,” or “ED observation.” Encounters with missing timestamps for their time-to-physician and/or physician-to-decision were excluded. No specific patient populations were excluded.
We also evaluated the frequency of triggers and priority assessments in that set of visits. As the total number of encounters was high (> 100,000) and the number excluded was low (1%), we did not employ any statistical methods to address missing data. We had two exposures, race and language, and four outcomes: 1) time-to-physician; 2) physician-to-decision time, 3) proportion of triggers; and 4) proportion of priority assessments. Each outcome was assessed considering the exposure of interest. A secondary analysis stratified the above analyses on disposition (admission, observation, or discharge).
Patient demographics including age, sex, race, ethnicity (Hispanic/Latino/a/x vs non-Hispanic/Latino/a/x), and primary language are reported by patients upon initial registration into our system and were obtained from the EHR. To avoid potential collinearity between race and ethnicity, these variables were analyzed in combination, and the following racial categories were used: “Hispanic/Latino/a/x”; “Black, non-Hispanic”; “White, non-Hispanic”; “Asian, nonHispanic”; “American Indian/Alaska Native, non-Hispanic”;
Carreras Tartak et al.
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
“Native Hawaiian/other Pacific Islander, non-Hispanic”; and “Other or Unknown.” Some research suggests that Hispanic/ Latino/a/x respondents better identify with questions on race and Hispanic ethnicity when a one-question format is used given that many Hispanic/Latino/a/x patients do not relate to standard racial categories provided by the US Census.21–23 Language categories were classified as “English” and “other.” We excluded patients without available language data from the analysis regarding language.
With regard to demographics among groups, we compared continuous variables using a one-way ANOVA with a Bonferroni correction or a Student t-test, based on the number of groups. Categorical variables were compared between groups using a chi-squared test. For unadjusted hypothesis testing, we compared medians between racial/ethnic groups using a Kruskal-Wallis test and between language using a Wilcoxon rank-sum test. Differences in groups in terms of time-to-physician or physician-to-decision were estimated from quantile regressions controlling for age, ESI, and sex and were provided as adjusted median differences (aMD) with a 95% CI. Proportions of triggers were presented with 95% CI calculated using the binomial exact method, and we used logistic regressions controlling for age, ESI, and sex to compare differences in trigger rates with regression estimates provided as adjusted odds ratios (aOR) with a 95% CI. All analyses were then stratified by ED disposition to evaluate how potential differences in patient acuity affected results and the methods above were repeated on each stratum. A P-value of < .05 was a priori established to indicate statistical significance. All analyses were performed using Stata 18.5 (StataCorp, LLC, College Station, TX) 24 We adhered to STROBE reporting guidelines for this study.25
RESULTS
There was a total of 103,370 encounters during the
selected time period, of which the following were excluded: 1,503 because of a missing door-to-physician time; two due to a negative door-to-physician time; and 9,640 due to a lack of decision time, leaving a total of 93,728 eligible patient encounters. (Encounters could have more than one exclusion.) We also excluded 56 encounters from the language analysis only for missing language. The mean age was 55.0 ± 20.9 years, 54.5% were female, and the median ESI was 3 (IQR 2, 3). Demographic information can be found in our supplemental tables. Patients of Black race had a median time-to-physician of 31 minutes compared to 24 minutes for White patients (aMD 3.2, 95% CI 2.4-3.9). Patients of Hispanic/Latino ethnicity had a median time-to-physician of 31 (aMD compared to White patients: 3.4, 95% CI 2.4-3.9). These differences in wait time remained even when we stratified the analysis by ED disposition. There was no statistically significant difference in median physician wait times between patients of White race and those of Asian, American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, or other/unknown/unspecified race. In terms of language, patients with a preferred language other than English had a median time-to-physician of 33 minutes compared to 25 in English-preferring patients (aMD 4.6, 95% CI:3.7-5.6) (Table 1).Patients of Black race had median physician-to-decision times of 228 minutes compared to 213 for White patients (aMD 15.0, 95% CI 12.0-17.9). Hispanic/ Latino patients had a median physician-to-decision time of 233 minutes (aMD compared to White patients: 21.3, 95% CI 17.5-25.2). Patients of Asian race had shorter median physician-to-decision times when discharged (median difference: -9.2, 95% CI -14.8 to -3.6) as compared to White patients. Patients with other/unknown/unspecified race had significantly shorter physician-to-decision times that those of White race when admitted (median difference: -34.9, 95% CI -42.0 to -27.8 minutes) and longer when under observation
Table 1. Quantile regression of time to-physician, controlling for Emergency Severity Index, age, and sex.
All dispositions
Race
(9,
Language
Table 1. Continued
Admitted from the ED Race (n = 35,352)
Adjusted median difference (95% CI) minutes P-value
White (n = 22,487) reference
Black (n = 6,019)
Hispanic/Latino (n = 2,602)
Unadjusted median (IQR) minutes
3.0 (1.8-4.2) < .001
2.0 (0.3-3.7) .02
Asian (n = 1,639) 2.0 (-0.1-4.1) .06
American Indian/Alaska Native (n = 111) -1.0 (-8.9-6.9) .80
Native Hawaiian/other Pacific Islander (n = 27) -2.0 (-17.9-13.9) .81
Other/unknown/not specified (n = 2,467) -2.0 (-3.8, -0.2) .03
Language (n = 35,343)
English (n = 31,070) reference
Other (n = 4,273) 3.0 (1.6-4.4) < .001
Discharged from the ED Race (n = 48,017)
White (n = 21,468) reference
Black (n = 12,712) 2.4 (1.2-3.5) < .001
Hispanic/Latino (n = 7,167) 3.7 (2.3-5.1) < .001
Asian (n = 3,596) 0.3 (-1.6-2.2) .76
American Indian/Alaska Native (n = 137) 3.4 (-5.5-12.3) .46
Native Hawaiian/other Pacific Islander (n = 47) -4.5 (-19.7-10.6) .56
Other/unknown/not specified (n = 2,890) 1.9 (-0.2-4.0) .07
Language (n = 47,974)
English (n = 41,704) reference
Other (n = 6,270) 6.0 (4.6-7.4) < .001
Observation Race
White (n = 701) reference
Black (n = 2625) 4.6 (2.3-7.0) < .001
Hispanic/Latino (n = 999) 3.7 (0.3-7.1) .03
Asian (n = 528) 0.4 (-4.1-4.8) .88
American Indian/Alaska Native (n = 39) 17.0 (1.3-32.7) .03
Native Hawaiian/other Pacific Islander (n = 6) 34.0 (-5.9-73.9) .10
Other/unknown/not specified (n = 461) -2.7 (-7.5-2.1) .27
Language (n = 10,355)
English (n = 9,286) reference
Other (n = 1,069) 4.0 (0.8-7.3) .02
IQR, interquartile range; ED, emergency department.
(median difference: 24.0, 95% CI 4.9-43.1). Patients with a preferred language other than English had a median physicianto-disposition time 17.1 minutes longer (95% CI 13.6-20.7) compared to patients who preferred English (Table 2).We then evaluated the proportion of triggers and priority assessments in that same population (Tables 3 and 4). Black patients (aOR 0.88, 95% CI 0.82-0.95) were less likely to have a trigger activated, whereas patients with other/unknown/unspecified
race (aOR 1.63, 95% CI 1.48-1.79) were more likely to have a trigger activated relative to White patients. There was no significant difference regarding language overall; however, non-English preferring patients who were eventually placed in observation (aOR 1.39, 95% CI 1.04-1.85) were significantly more likely to have a trigger called than English-preferring patients. Similarly, Black patients (aOR 0.72, 95% CI 0.670.77]), Hispanic/Latino patients (aOR 0.78, 95% CI 0.71-
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
Table 2. Quantile regression of physician-to-decision time controlling for Emergency Severity Index, age, and sex. Adjusted median difference (95% CI) minutes
All dispositions
Race (n = 93,728)
White (n = 49,656) Reference
Black (n = 21,356)
Hispanic/Latino (n = 10,768)
(12.0-17.9)
(17.5-25.2)
Asian (n = 5,763) -1.0 (-5.9-4.0)
American Indian/Alaska Native (n = 287) 19.3 (-1.6-40.1)
Native Hawaiian/other Pacific Islander (n = 80) 23.2 (-16.3-62.7) .25
Other/Unknown/Not specified (n = 5,818) -21.0 (-26.0, -16.1) <
Language (n = 93,672)
English (n = 82,060)
Other (n = 11,612) 17.1 (13.6-20.7) < .001
Admitted from the ED Race (n = 35,352)
White (n = 22,487) Reference
Black (n = 6,019) 20.8 (16.0-25.6) < .001
Hispanic/Latino (n = 2,602) 27.9 (21.4-34.8) < .001
Asian (n = 1,639)
(-1.8-15.1) .12
American Indian/Alaska Native (n = 111) 14.3 (-17.1-45.6) .37
Native Hawaiian/other Pacific Islander (n = 27) 36.6 (-26.9-100.0) .26
Other/unknown/not specified (n = 2,467) -34.9 (-42.0, -27.8) < .001
Language (n = 35,343)
English (n = 31,070) Reference
Other (n = 4,273) 18.5 (12.9-24.1) < .001
Discharged from ED
Race (n = 48,017)
White (n = 21,468) reference
Black (n = 12,712) 0.9 (-2.5-4.4) .59
Hispanic/Latino (n = 7,167) 9.8 (5.5-14.0) < .001
Asian (n = 3,596) -9.2 (-14.8, -3.6) < .01
American Indian/Alaska Native (n = 137) 14.3 (-12.1-40.7) .29
Native Hawaiian/other Pacific Islander (n = 47) 10.8 (-34.2-55.8) .64
Other/unknown/not specified (n = 2,890) -2.4 (-8.6-3.7) .44
Language (n = 47,974)
English (n = 41,704) reference
Other (n = 6,270) 8.7 (4.5-13.0) < .001
Placed in ED observation
Race (n = 10,359)
White (n = 5,701) reference
Black (n = 2,625) 10.3 (1.0-19.6) .03
Hispanic/Latino (n = 999) 11.2 (-2.4-24.7) .11
Asian (n = 528) -1.0 (-19.1-17.0) .91
American Indian/Alaska Native (n = 39) 7.7 (-55.4-70.8) .81
Native Hawaiian/other Pacific Islander (n = 6) -15.2 (-175.6-145.3) .85
Other/unknown/not specified n = 461) 24.0 (4.9-43.1) .01
IQR, interquartile range; ED, emergency department.
(129, 328)
(141, 343)
(148, 344)
(127, 315)
(154, 334)
(143, 313)
(102, 301)
(130, 329)
(146, 345)
Carreras Tartak et al.
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
Table 2. Quantile regression of physician-to-decision time controlling for Emergency Severity Index, age, and sex.
Adjusted median difference (95% CI) minutes P-value Unadjusted median (IQR) minutes
Language (n = 10,355)
English (n = 9,286) reference
Other (n = 1,069) 21.6 (8.5-34.7) < .01
IQR, interquartile range; ED, emergency department.
Table 3. Logistic regression of proportion of triggers controlling for Emergency Severity Index, age, and sex. Proportion (95% CI) aOR (95%) P-value
All dispositions
Race
White (n = 49,656) 0.112 (0.109-0.114)
Reference
Black (n = 21,356) 0.073 (0.070-0.077) 0.88 (0.82-0.95) < .01
Hispanic/Latino (n = 10,768) 0.072 (0.067-0.077) 0.94 (0.85-1.04) .22
Asian (n = 5,763)
(0.080-0.095)
(0.95-1.19) .28 American Indian/Alaska Native (n = 287)
Native Hawaiian/other Pacific Islander (n = 80)
(0.075-0.150) 1.15 (0.74-1.79) .53
(0.044-0.188) 1.15 (0.43-3.06) .78
Other/unknown/not specified (n = 5,818) 0.191 (0.181-0.202) 1.63 (1.48-1.79) < .001
Language
English (n = 82,060) 0.103 (0.101-0.105) Reference
Other (n = 11,612) 0.094 (0.089-0.100) 1.00 (0.92-1.08) .99
Admitted from the ED
Race (n = 35,352)
White (n = 22,487) 0.179 (0.174-0.184) Reference
Black (n = 6,019) 0.161 (0.143-0.171) 0.99 (0.90-1.08) .79
Hispanic/Latino (n = 2,602) 0.157 (0.143-0.171) 0.93 (0.81-1.07) .31
Asian (n = 1,639)
0.173 (0.155-0.192) 1.02 (0.87-1.19) .80
American Indian/Alaska Native (n = 11) 0.162 (0.099-0.244) 1.14 (0.62-2.09) .67
Native Hawaiian/other Pacific Islander (n = 27) 0.222 (0.086-0.423) 1.41 (0.43-4.66) .57
Other/unknown/not specified (n = 2,467) 0.378 (0.359-0.397) 1.82 (1.62-2.04) < .001
Language (n = 35,343)
English (n = 31,070)
0.189 (0.185-0.193) reference
Other (n = 4,273) 0.179 (0.168-0.191) 0.94 (0.85-1.04) .27
Discharged from ED
Race (n = 48,017)
White (n = 21,468)
0.053 (0.050-0.056) reference
Black (n = 12,712) 0.037 (0.034-0.040) 0.90 (0.79-1.03) .12
Hispanic/Latino (n = 7,167) 0.042 (0.037-0.047) 1.02 (0.87-1.19) .83
Asian (n = 3,596) 0.050 (0.043-0.057) 1.11 (0.92-1.35) .27
American Indian/Alaska Native (n = 137) 0.088 (0.046-0.148) 1.56 (0.77-3.16) .22
Native Hawaiian/other Pacific Islander (n = 47) 0.043 (0.005-0.145) 0.86 (0.13-5.67) .88
Other/unknown/not specified (n = 2,890) 0.048 (0.041-0.057) 1.10 (0.89-1.36) .38
Language (n = 47,974)
English (n = 41,704)
0.048 (0.046-0.050) reference
Other (n = 6,270) 0.040 (0.035-0.045) 1.13 (0.97-1.33) .12
CI, confidence interval; aOR, adjusted odds ratio; ED, emergency department.
Table 3. Continued
Placed in ED observation
Race (n = 10,359)
White (n = 5,701)
Proportion (95% CI) aOR (95%) P-value
0.067 (0.060-0.074) reference
Black (n = 2,625) 0.048 (0.040-0.057) 0.88 (0.70-1.12) .31
Hispanic/Latino (n = 999) 0.070 (0.055-0.088) 1.18 (0.86-1.63) .30
Asian (n = 528) 0.078 (0.056-0.104) 1.49 (1.02-2.19) .04
American Indian/Alaska Native (n = 39) 0.026 (0.001-0.135) 0.50 (0.07-3.67) .49
Native Hawaiian/other Pacific Islander (n = 6)
0.000 (0.000-0.459) Unable to be assessed due to no triggers in this group
Other/unknown/not specified (n = 461) 0.089 (0.065-0.119) 1.19 (0.77-1.84) .44
Language (n = 10,355)
English (n = 9,286)
0.062 (0.058-0.068) Reference
Other (n = 1,069) 0.076 (0.061-0.093) 1.39 (1.04-1.85) .02
CI, confidence interval; aOR, adjusted odds ratio; ED, emergency department.
Wait Times and Urgent Evaluation by Race, Ethnicity, and Language 0.86), and non-English-preferring patients (aOR 0.85, 95% CI 0.78-0.92) were less likely to have a priority assessment called than White or English-speaking patients.
DISCUSSION
Our study found that in an EHR system where ESI is not the only factor used in signaling patient acuity to physicians, Black, Hispanic, and non-English-preferring patients experienced delays in seeing a physician and in waiting for a disposition, regardless of the final disposition. While the adjusted median differences, which ranged from a few minutes to over half an hour for some populations, may seem small and of doubtful clinical significance, their aggregate effect over the ≈ 100,000 encounters studied translates into many hours of delays in initial evaluation and reassessments that could impact patient outcomes. The reasons behind these disparities are likely multifactorial, involving both interpersonal and structural factors. From a triage standpoint, implicit bias among healthcare physicians may influence triage decisions and the perceived urgency of a patient’s condition.26–29 Prior literature suggests that heightened time pressure and higher patient loads can exacerbate reliance on implicit biases,30–33 meaning that systemic factors such as ED crowding could be affecting physician decisions and heightening racial and ethnic disparities in wait times.
Structural factors such as limited access to outpatient care might also influence racial and ethnic disparities seen in our analysis, as patients without primary care or outpatient specialists may not have as much documentation about their medical conditions readily available in the EHR for a triage nurse or physician to review. Studies have shown that Black and Hispanic patients have lower use of outpatient services.34–36 Some patients may also lack the advocacy that outpatient medical teams can offer by requesting an admission
on their behalf or by documenting specific concerns that the patients themselves may have difficulty conveying. This might lead to some patients undergoing more extensive workups given higher levels of uncertainty about their diagnosis and plan, which can delay their disposition.
Our analysis showed an association between LEP and longer wait times. Limited availability of interpreters can further exacerbate delays in patients with LEP. In fact, Wallbrecht and colleagues found that although there was no statistically significant difference in ED LOS between patients with LEP and English-speaking patients, when they stratified by interpreter vs no interpreter use, patients who required an interpreter did have longer LOS than patients with LEP who did not require an interpreter.14 In our department, we have the ability to request phone interpreters from our hospital interpreter services for certain languages commonly spoken in our ED. During off-business hours or for less common languages, we also have video and audio interpreters available via smart tablets. Given that the process of requesting an interpreter can take time—particularly during off hours or for less common languages—it is possible that our door-tophysician metric is falsely underestimating the time that non-English-preferring patients who required an interpreter waited to see a doctor. Similarly, interpreter wait times could be adversely affecting the physician-to-decision times, as physicians may delay communicating with these patients if an interpreter is not readily available.
Our analysis of urgent evaluations showed an association between Black race and a lower likelihood of trigger activation. It is possible that Black patients were less ill upon presentation to the ED. While criteria for triggers are meant to be as objective as possible, the role of racial bias should also be considered. For example, while stroke symptoms are part of the criteria for a trigger activation, prior literature shows that Black patients
Carreras Tartak et al.
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
Table 4. Logistic regression of proportion of priority assessments controlling for Emergency Security Index, age, and sex. Proportion (95% CI) aOR (95% CI) P-value Race
White (n = 49,656)
Black (n = 21,356)
0.088 (0.086-0.090) reference
0.050 (0.047-0.053) 0.72 (0.67-0.77) < .001
Hispanic/Latino (n = 10.768) 0.050 (0.046-0.054) 0.78 (0.71-0.86) < .001
Asian (n = 5,763)
0.067 (0.061-0.074) 0.93 (0.83-1.04) .18
American Indian/Alaska Native (n = 287) 0.073 (0.046-0.110) 0.85 (0.53-1.34) .48
Native Hawaiian/other Pacific Islander (n = 80)
0.050 (0.014-0.123) 0.81 (0.28-2.29) .69
Other/unknown/not specified (n = 5,818) 0.079 (0.072-0.086) 1.05 (0.94-1.17) .37
Language
English (n = 82,060)
Other (n = 11,612)
Admitted from the ED Race (n = 35,352)
White (n = 22,487)
Black (n = 6,019)
0.075 (0.073-0.077) reference
0.060 (0.056-0.064) 0.85 (0.78-0.92) < .001
0.117 (0.113-0.121) reference
0.089 (0.081-0.096) 0.82 (0.74-0.90) < .001
Hispanic/Latino (n = 2,602) 0.085 (0.075-0.097) 0.79 (0.68-0.92) < 0.01
Asian (n = 1,639) 0.110 (0.095-0.126) 0.96 (0.81-1.13) .60
American Indian/Alaska Native (n = 111) 0.108 (0.057-0.181) 1.08 (0.58-2.02) .81
Native Hawaiian/other Pacific Islander (n = 27) 0.074 (0.009-0.243) 0.73 (0.16-3.25) .68
Other/unknown/not specified (n = 2,467) 0.116 (0.104-0.129) 1.08 (0.94-1.24) .28
Language (n = 35,343)
English (n = 31,070) 0.110 (0.107-0.114) reference
Other (n = 4,273) 0.100 (0.091-0.110) 0.93 (0.83-1.04) .21
Discharged from ED
Race (n = 48,017)
White (n = 21,468)
0.056 (0.053-0.059) reference
Black (n = 12,712) 0.031 (0.028-0.034) 0.68 (0.60-0.77) < .001
Hispanic/Latino (n = 7,167)
0.034 (0.030-0.039) 0.78 (0.67-0.90) < .01
Asian (n = 3,596) 0.048 (0.041-0.056) 1.01 (0.85-1.20) .95
American Indian/Alaska Native (n = 137)
Native Hawaiian/other Pacific Islander (n = 47)
Other/unknown/not specified (n = 2,890)
Language (n = 47,974)
English (n = 41,704)
Other (n = 6,270)
Placed in ED observation
Race (n = 10,359)
White (n = 5,701)
Black (n = 2,625)
Hispanic/Latino (n = 999)
Asian (n = 528)
American Indian/Alaska Native (n = 39)
Native Hawaiian/other Pacific Islander (n = 6)
Other/unknown/not specified (n = 461)
Language (n = 10,355)
English (n = 9,286)
Other (n = 1,069)
0.044 (0.016-0.093) 0.68 (0.29-1.59) .38
0.021 (0.001-0.113) 0.52 (0.07-3.99) .53
0.042 (0.035-0.050) 0.90 (0.74-1.10) .30
0.046 (0.044-0.048) reference
0.033 (0.029-0.038) 0.81 (0.70-0.95) < .01
0.098 (0.090-0.106) reference
0.058 (0.049-0.067) 0.62 (0.51-0.75) < .001
0.071 (0.056-0.089) 0.80 (0.61-1.04) .10
0.066 (0.047-0.091) 0.66 (0.46-0.94) .02
0.077 (0.016-0.209) 0.68 (0.21-2.27) .54
0.167 (0.004-0.641) 2.53 (0.26-24.21) .42
0.108 (0.082-0.140) 1.30 (0.94-1.78) .11
0.087 (0.081-0.093) reference
0.056 (0.043-0.072) 0.62 (0.47-0.82) < .01
CI, confidence interval; aOR, adjusted odds ratio; ED, emergency department.
Carreras Tartak et
Tartak et al.
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
experience longer ED wait times and delayed treatment for stroke relative to White patients.9 Interestingly, non-English-language preferring patients who were placed in observation were significantly more likely to have a trigger called than Englishpreferring patients. The nature of this analysis did not allow us to evaluate the timing of triggers with respect to disposition, making it difficult to ascertain whether these were patients who had a trigger activation prior to their disposition being set or had triggers activated while they were in ED observation.
Our analysis also showed an association between Black race, Hispanic/Latino ethnicity, and LEP, and priority assessment activation. Although there are some objective criteria for priority assessments, they can also be activated subjectively; they are meant to give nurses and physicians the ability to have urgently evaluated a patient with a concerning history or presentation who doesn’t meet criteria for a trigger activation. Thus, priority assessments are more susceptible to bias as well as to the over-reliance on external historians and prior documentation available in the EHR previously discussed.
This study highlights the pervasive racial, ethnic, and language-based differences experienced by Black, Hispanic/ Latino, and non-English-language preferring patients and underscores the need to develop solutions to address these disparities. Potential interventions to mitigate these disparities include implicit bias training and subsequent education on debiasing strategies.37,38 Another area of opportunity that remains to be explored is leveraging artificial intelligence models to aid in triage decisions. A scoping review of the use of artificial intelligence in ED by Tyler and colleagues found that machinelearning models used in triage can reduce under- and over-triage, alleviate the workload of medical staff, optimize resource allocation, predict patient disposition, and improve identification of critically ill patients.39 However, prior studies have shown racial and ethnic bias in currently available models.40
LIMITATIONS
Our analysis did not incorporate other important variables in determining patient acuity and complexity during the triage process, such as patient comorbidities, initial vital signs, and chief complaint. While we did not account for differences in patient acuity beyond stratifying our analysis by ED disposition, other studies that have controlled for patient acuity have found that Black and Hispanic patients as well as patients with LEP are more likely to be jumped over in line by patients with similar acuity.3,16 In addition, even if Black, Hispanic, and LEP patients were presenting with lower acuity complaints, this would not necessarily explain why the physician-to-decision times are longer for these groups. It’s difficult to ascertain why 9,642 encounters had missing or nonsensical timestamps. An initial theory was that timestamps were missing because some of these patients were critically ill and required timely interventions that prevented timestamps from being adequately recorded. However, as outlined in Supplemental Table 4, 7% of excluded patients (vs 4% of excluded patients) had an ESI of 1,
making it unlikely that being more critically ill was the leading factor behind the missing timestamps.
In our trigger analysis, we only evaluated patients who had a trigger activated; there might have been patients for whom triggers should have been activated who did not have one activated at all. In addition, the reason for trigger activation was beyond the scope of this analysis. We also did not evaluate for other variables that may be correlated with triage decisions, such as history of being undomiciled, insurance status and type, primary care physician or specialist within our system, or prior visits within our ED. For our patients with LEP, we were unable to determine whether they required an interpreter, as this data was not available at the encounter level. We also did not have ED census data available to us to control for crowding on a given date at a given time.
It is important to note that race, ethnicity, and preferred language data collected from EHRs can often be inaccurate and incomplete.41,42 Lastly, any adverse effects caused by delays in time-to-physician and physician-to-decision, as well as by any potential missed triggers, remain to be determined and could serve as the basis for future studies within our health system.
CONCLUSION
This study evaluated racial, ethnic, and language-based disparities in delays seeing a physician, waiting for a disposition, and having an urgent evaluation in an ED where urgent evaluations rather than Emergency Severity Index scores alone are used to signal patient acuity to physicians. Black, Hispanic, and non-English-preferring patients experience delays in seeing a physician and in waiting for a disposition, regardless of their final disposition. There is an association with Black race and lower likelihood of trigger activation. There is also an association with Black race, Hispanic ethnicity, and LEP; and lower likelihood of having priority assessments activated. While the effects of these delays and potentially missed urgent evaluations remains to be determined, these findings underscore the need to develop additional mechanisms for mitigating biases in the triage process.
Address for Correspondence: Jossie A. Carreras Tartak, MD, MBA, Beth Israel Deaconess Medical Center, Department of Emergency Medicine, One Deaconess Road, Rosenberg Building, 2nd Floor, Boston, MA 02215. Email: jcarrera@bidmc.harvard.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Carreras Tartak et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http:// creativecommons.org/licenses/by/4.0/
Carreras
REFERENCES
1. James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3):e310-5.
2. Lu FQ, Hanchate AD, Paasche-Orlow MK. Racial/ethnic disparities in emergency department wait times in the United States, 2013-2017. Am J Emerg Med. 2021;47:138-44.
3. Sangal RB, Su H, Khidir H, et al. Sociodemographic disparities in queue jumping for emergency department care. JAMA Netw Open 2023;6(7):e2326338.
4. Sonnenfeld N, Pitts SR, Schappert SM, et al. Emergency department volume and racial and ethnic differences in waiting times in the United States. Med Care. 2012;50(4):335-41.
5. Qiao WP, Powell ES, Witte MP, et al. Relationship between racial disparities in ED wait times and illness severity. Am J Emerg Med 2016;34(1):10-5.
6. Valderrama G, Badolato GM, Diaz P, et al. Improving wait times for children with caregivers with limited English proficiency in the emergency department. Pediatr Qual Saf. 2023;8(3):e656.
7. Clarey AJ, Cooke MW. Patients who leave emergency departments without being seen: literature review and English data analysis. Emerg Med J. 2012;29(8):617-21.
8. Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004;292(13):1563-72.
9. Ikeme S, Kottenmeier E, Uzochukwu G, et al. Evidence-based disparities in stroke care metrics and outcomes in the United States: a systematic review. Stroke. 2022;53(3):670-9.
10. Goyal MK, Chamberlain JM, Webb M, et al. Racial and ethnic disparities in the delayed diagnosis of appendicitis among children. Acad Emerg Med. 2021;28(9):949-56.
11. Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16(5):403-10.
12. Karaca Z, Wong HS. Racial disparity in duration of patient visits to the emergency department: teaching versus non-teaching hospitals. West J Emerg Med. 2013;14(5):529-41.
13. Lowe JT, Monteiro KA, Zonfrillo MR. Disparities in pediatric emergency department length of stay and utilization associated with primary language. Pediatr Emerg Care. 2022;38(4):e1192-7.
14. Wallbrecht J, Hodes-Villamar L, Weiss SJ, et al. No difference in emergency department length of stay for patients with limited proficiency in English. South Med J. 2014;107(1):1-5.
15. Mahmoud I, Hou XY, Chu K, et al. Language affects length of stay in emergency departments in Queensland public hospitals. World J Emerg Med. 2013;4(1):5-9.
16. Joseph JW, Kennedy M, Landry AM, et al. Race and ethnicity and primary language in emergency department triage. JAMA Netw Open. 2023;6(10):e2337557.
17. Dennis JA. Racial/ethnic disparities in triage scores Among pediatric emergency department fever patients. Pediatr Emerg Care 2021;37(12):e1457-61.
18. Sax DR, Warton EM, Mark DG, et al. Evaluation of the Emergency
Severity Index in US emergency departments for the rate of mistriage. JAMA Netw Open. 2023;6(3):e233404.
19. Peitzman C, Carreras Tartak JA, Samuels-Kalow M, et al. Racial differences in triage for emergency department patients with subjective chief complaints. West J Emerg Med. 2023;24(5):888-93.
20. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005 Apr;45(4):448-51.
21. Baker DW, Cameron KA, Feinglass J, et al. A system for rapidly and accurately collecting patients’ race and ethnicity. Am J Public Health 2006;96(3):532-7.
22. Laws MB, Heckscher RA. Racial and ethnic identification practices in public health data systems in New England. Public Health Rep 2002;117(1):50-61.
23. Institute of Medicine (US) Subcommittee on Standardized Collection of Race/Ethnicity Data for Healthcare Quality Improvement. (2009). Defining Categorization Needs for Race and Ethnicity Data. In: Ulmer C, McFadden B & Nerenz DR, Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement (p. 61-92) Washington (DC): National Academies Press (US).
24. StataCorp. Stata Base Reference Manual Release 19. 2025. Available at: https://www.stata.com/manuals/r.pdf. Accessed May 5, 2025.
25. von Elm E, Altman DG, Egger M, et al. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-7.
26. Boley S, Sidebottom A, Vacquier M, et al. Investigating racial disparities within an emergency department rapid-triage system. Am J Emerg Med. 2022;60:65-72.
27. Dehon E, Weiss N, Jones J, et al. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med. 2017;24(8):895-904.
28. Oliver MN, Wells KM, Joy-Gaba JA, et al. Do physicians’ implicit views of African Americans affect clinical decision making? J Am Board Fam Med. 2014;27(2):177-88.
29. Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for Black and White patients. J Gen Intern Med. 2007;22(9):1231-8.
30. Stepanikova I. Racial-ethnic biases, time pressure, and medical decisions. J Health Soc Behav. 2012;53(3):329-43.
31. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry 2007;29(6):481-8.
32. Burgess DJ. Are providers more likely to contribute to healthcare disparities under high levels of cognitive load? How features of the healthcare setting may lead to biases in medical decision making. Med Decis Making. 2010;30(2):246-57.
33. Johnson TJ, Hickey RW, Switzer GE, et al. The impact of cognitive stressors in the emergency department on physician implicit racial bias. Acad Emerg Med. 2016;23(3):297-305.
34. Marcondes FO, Normand SLT, Le Cook B, et al. Racial and ethnic
Carreras Tartak et al.
Carreras Tartak et al.
differences in telemedicine use. JAMA Health Forum 2024;5(3):e240131.
Delays in Wait Times and Urgent Evaluation by Race, Ethnicity, and Language
35. Olfson M, Zuvekas SH, McClellan C, et al. Racial-ethnic disparities in outpatient mental health care in the United States. Psychiatr Serv 2023;74(7):674-83.
36. Cai C, Gaffney A, McGregor A, et al. Racial and ethnic disparities in outpatient visit rates across 29 specialties. JAMA Intern Med 2021;181(11):1525-7.
37. Zeidan AJ, Khatri UG, Aysola J, et al. Implicit bias education and emergency medicine training: Step one? Awareness. AEM Educ Train. 2019;3(1):81-5.
38. Devine PG, Forscher PS, Austin AJ, et al. Long-term reduction in implicit race bias: a prejudice habit-breaking intervention. J Exp Soc
Psychol. 2012;48(6):1267-78.
39. Tyler S, Olis M, Aust N, et al. Use of artificial intelligence in triage in hospital emergency departments: a scoping review. Cureus. 2024 May 8;16(5):e59906.
40. Samorani M, Harris SL, Blount LG, et al. Overbooked and overlooked: machine learning and racial bias in medical appointment scheduling. Manuf Serv Oper Manag. 2022;24(6):2825-42.
41. Freed GL, Bogan B, Nicholson A, et al. Error rates in race and ethnicity designation across large pediatric health systems. JAMA Netw Open. 2024;7(9):e2431073.
42. Johnson JA, Moore B, Hwang EK, et al. The accuracy of race & ethnicity data in US based healthcare databases: a systematic review. Am J Surg. 2023;226(4):463-70.
Accessibility of Urgent Care Centers: A Socioeconomic and Geospatial Evaluation
Parnika Telagi, BS*
Richard Sadler, PHD, MPH†
Praval Telagi, BS‡
Kevin McGurk, MD§
Medical College of Wisconsin, Milwaukee, Wisconsin
University of Illinois, Department of Computer Science, Urbana, Illinois
Michigan State University College of Human Medicine, Department of Public Health and Family Medicine, East Lansing, Michigan
Medical College of Wisconsin, Department of Emergency Medicine, Milwaukee, Wisconsin
Section Editor: Shahram Lotfipour, MD, MPH
Submission history: Submitted September 24, 2024; Revision received April 23, 2025; Accepted June 15, 2025
Electronically published [date] (Add date right before publishing in Articles in Press)
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.35583
Introduction: Urgent care centers (UC) play an important role in addressing non-emergent health concerns, offering a convenient alternative to emergency departments (ED). However, accessibility to UCs can vary based on transportation availability and socioeconomic factors. In this study we evaluated the geospatial accessibility of UCs and EDs in Milwaukee County, Wisconsin, and sought to characterize the relationship between transit options, socioeconomic vulnerability, and access to care.
Methods: We included 13 EDs and 13 UCs in the study. Public and private transit times between census tracts in Milwaukee County and the nearest UC or ED were calculated using an application programming interface that recorded data from Google Maps. We employed socioeconomic vulnerability index (SEVI) scores to define community vulnerability. Statistical analyses, including Mann-Whitney U tests and Pearson correlation coefficients, were used to determine differences in commute times and their relationship with socioeconomic status.
Results: Private transit times were shorter than public transit times when commuting to the nearest ED (7 minutes vs 22 minutes, P <.001) and the nearest UC (9 minutes vs 31 minutes, P < .001). The EDs were generally more accessible than UCs, with shorter transit (22 vs 31 minutes, P < .001) and walk times (11 vs 14 minutes, P <.001). Socioeconomically disadvantaged communities with higher SEVI scores had longer private transit times to UCs (r = 0.17, P = .003) while having shorter public transit times to EDs (r = -.21, P < .001).
Conclusion: Access to urgent care centers and EDs in Milwaukee County is influenced by socioeconomic factors and transportation modes. While EDs are more accessible to socioeconomically vulnerable communities, UCs are less accessible, which may contribute to higher ED utilization for non-emergent needs. These findings highlight the need to address transportation limitations as a social determinant of health that can impact how disadvantaged populations seek care and the implications for non-emergent ED use and ED crowding. [West J Emerg Med. 2025;26(5)1244–1249.]
INTRODUCTION
Urgent care centers (UC) play an increasingly important role in delivering expedited care to patients with non-emergent health concerns. Utilization has steadily increased in the US since their advent in the 1970s and growth through the 2000s, with more than 29% of adults having at least one UC visit
annually.1-4 While no consensus definition exists for what constitutes an UC, these facilities are generally capable of caring for patients with mild injuries and ailments, do not require appointments, and provide service over extended business hours.5,6 Urgent care centers are often viewed by patients as an appealing alternative to emergency department
(ED) or primary care physician (PCP) visits for reasons of cost, convenience, or both.7,8 As many will ultimately seek ED care for non-emergent needs, redirecting these cases to UCs has the potential to confer savings to the healthcare system.6
The choice of where to pursue care for non-emergent healthcare needs is impacted by a multitude of factors including insurance, timing, access to a PCP, socioeconomic status and available transportation.9 Transportation represents an essential social determinant of health and can affect how patients access healthcare and the facilities they visit.10-14 Regardless of the presence of reliable or timely transportation, patients may prioritize geographic proximity over other factors when choosing a location for their care.15 Patients may use public or private transportation to visit UCs and EDs. When neither is appropriate or accessible, individuals may also use emergency medical services (EMS) to go to the ED.
Milwaukee County is the most populous county in Wisconsin and home to nearly one million residents in a geographically and socioeconomically diverse area. The demographic composition of its population is 51% White, 26% Black, 18% Hispanic/Latino, 10% multiracial, 5% Asian, and 8% other races. Within the county, 14% of families live below the poverty line, and unemployment rates exceed state and national averages. Approximately 60% of the county’s population resides within the City of Milwaukee. The remainder of Milwaukee County is comprised of a mix of suburban areas and a few outlying rural communities.16
Public transportation within the county includes bus lines and limited streetcar services. While UCs have previously been associated with urban areas, higher income levels and a greater prevalence of private insurance, the accessibility of these facilities via different modes of transit is generally unknown. Given the expanding role that UCs play and the importance of transportation on how and when patients seek medical care, we sought to quantify the accessibility of UCs by public and private transit and to characterize the association between accessibility and the socioeconomic status of communities.
METHODS
While many facilities advertise as UCs, widely disparate clinical and diagnostic capabilities exist across these centers. As no uniformly accepted definition exists, we employed criteria in accordance with Urgent Care Association of America standards and consistent with previously published research.17,18 These criteria include extended hours of operation, weekend availability, the option to be seen without an appointment, basic lab and imaging capabilities, and the ability to perform minor procedures.
We performed statistical analyses using R 4.2.3 (The R Foundation for Statistical Computing, Vienna, Austria).19 Group differences were calculated using the Mann-Whitney U test. We calculated the relationship between socioeconomic vulnerability index (SEVI) scores and transit times using the Pearson correlation coefficient. We used ArcMap 10.8
Population Health Research Capsule
What do we already know about this issue?
Emergency department (ED) visits have increased for non-emergent issues that could otherwise be seen at an urgent care center (UC). Transportation often impacts how patients seek care.
What was the research question?
Do commute times to the nearest ED and UC differ, and is there an association with a community’s socioeconomic standing?
What was the major finding of the study?
Commute times to EDs were shorter than UCs via public transit (22 vs 31 minutes, P < .001) and private transit (7 vs 9 minutes, P < .001) and were correlated with socioeconomic status as poorer areas had longer private commutes to UCs (r = .17, P = .003) and shorter public commutes to EDs (r = -.21, P < .001).
How does this improve population health?
Transit times and geographic proximity to the nearest ED or UC are associated with socioeconomic status and may influence how and where patients seek care.
(Environmental Systems Research Institute, Inc, Redlands, CA) to combine all spatial data, including the location of UCs and EDs, travel time to UCs and EDs by census block, Social Vulnerability Index (SVI) and SEVI scores, and the boundaries of Milwaukee County and the city of Milwaukee.
All EDs and UCs meeting inclusion criteria within Milwaukee County were included for analysis. We sought to address potential errors introduced by the edge effect, a phenomenon by which spatial error is introduced when features outside a study area that individuals are likely to visit are excluded from analysis (typically leading to artificially poorer calculated access). To do so, we also included facilities outside Milwaukee County if they were the closest care center by transit time, generally for communities on or near the county’s border.20,21
We used publicly available data online from the US Census Bureau, Centers for Disease Control and Prevention (CDC), and Agency for Toxic Substances and Disease Registry to characterize the census tracts in Milwaukee County and their relative social vulnerability as measured by the SVI. This index has further subclassifications grouped by theme including a summation of socioeconomic factors we have abbreviated as the SEVI. The SEVI includes factors such as poverty, unemployment, levels of education, and lack of health insurance. The SEVI ranges from 0 to 1, with higher
values indicating increased socioeconomic vulnerability.
We used Google Maps to compute the public and private transit information between each census tract to its nearest UC and ED. We wrote a program using the Google Maps application programming interface to collect the data, which compared transit times between each census tract to each UC and ED, saving the shortest times. For public transit information, we computed and recorded total transit time, number of bus transfers, and walking time, Transit times were computed over multiple days and times, including mornings, evenings, weekdays, and weekends. While the data presented represents transit at 8 am on a Monday, the statistical trends were unchanged across all time points assessed.
This study was declared exempt by the Medical College of Wisconsin Institutional Review Board.
RESULTS
We included 13 EDs and 13 UCs for analysis (10 each inside Milwaukee County and three each just outside its borders). Median commute times to the closest ED and UC using public and private transit are shown below (Table). The Mann-Whitney U test results shown compare transit times to the nearest UC vs the nearest ED.Private transit times were faster than public transit times when commuting to the nearest ED (7 minutes vs 22 minutes, P <.001) and the nearest UC (9 minutes vs 31 minutes, P < .001). The longest private and public transit times to the nearest ED were 16 and 77 minutes, respectively. The longest private and public transit times to the nearest UC were 15 and 62 minutes, respectively. When comparing commutes to the nearest ED vs UC, private transit time, public transit time, and total minutes of walking were all shorter for EDs than UCs. We found no statistically significant difference in the number of bus transfers needed to travel to the nearest UC vs ED.
Socioeconomic vulnerability was associated with increased public and private transit times to the nearest UC (P = .10 and P = .003, respectively) as shown in Figure 1. Conversely, SEVI score was associated with decreased public and private transit times to the nearest ED (P < .001 and P = .15, respectively) as shown in Figure 2.
The relationship between the SEVI score of each census tract and its proximity to the nearest ED is well represented
Table. Median commute times to the closest emergency department and urgent care using public and private transit.
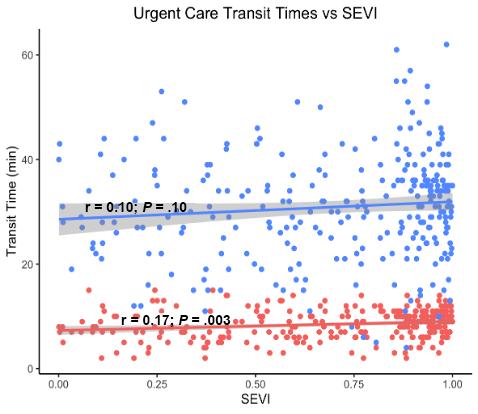
Figure 1. Association between socioeconomic vulnerability and transit times to the nearest urgent care.
Note that blue indicates public transit and red indicates private transit.
SEVI, Socioeconomic Vulnerability Index.
using a map of Milwaukee County (Figure 3). The length of commute from each tract to the nearest ED corresponds to the size of the blue dot within that municipality. The most socioeconomically vulnerable communities grouped by quintile are shown to have shorter commutes to the nearest ED as compared to wealthier census tracts. Commuting to UCs shows the opposite relationship. When comparing private transit times to the nearest UC, the most vulnerable census tracts have longer commute times in general than less disadvantaged communities (Figure 4).
DISCUSSION
Unsurprisingly, our study demonstrated that private transit times were shorter than public transportation to both UCs and EDs. While no commute via private transit took longer than 16 minutes, in certain communities public transit took as long as 77 minutes and frequently required multiple bus transfers
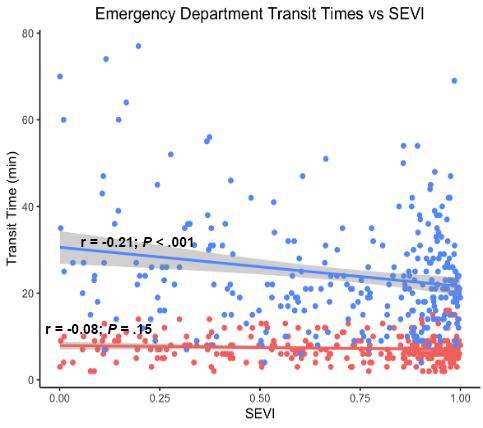
Figure 2. Association between socioeconomic vulnerability and transit times to the nearest emergency department
Note that blue indicates public transit and red indicates private transit.
UC, urgent care center; ED, emergency department.
SEVI, Socioeconomic Vulnerability Index.
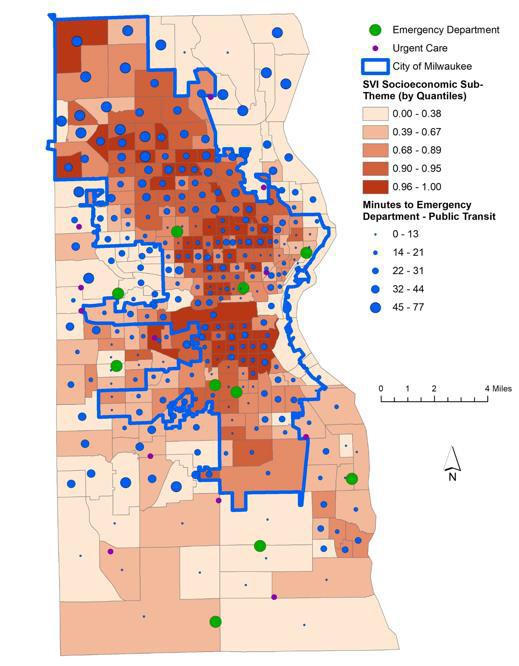
SVI, Social Vulnerability Index,
and lengthy walks. This is particularly impactful when considering patients with disabilities or impaired mobility for whom lengthy commute or walk times may be untenable.
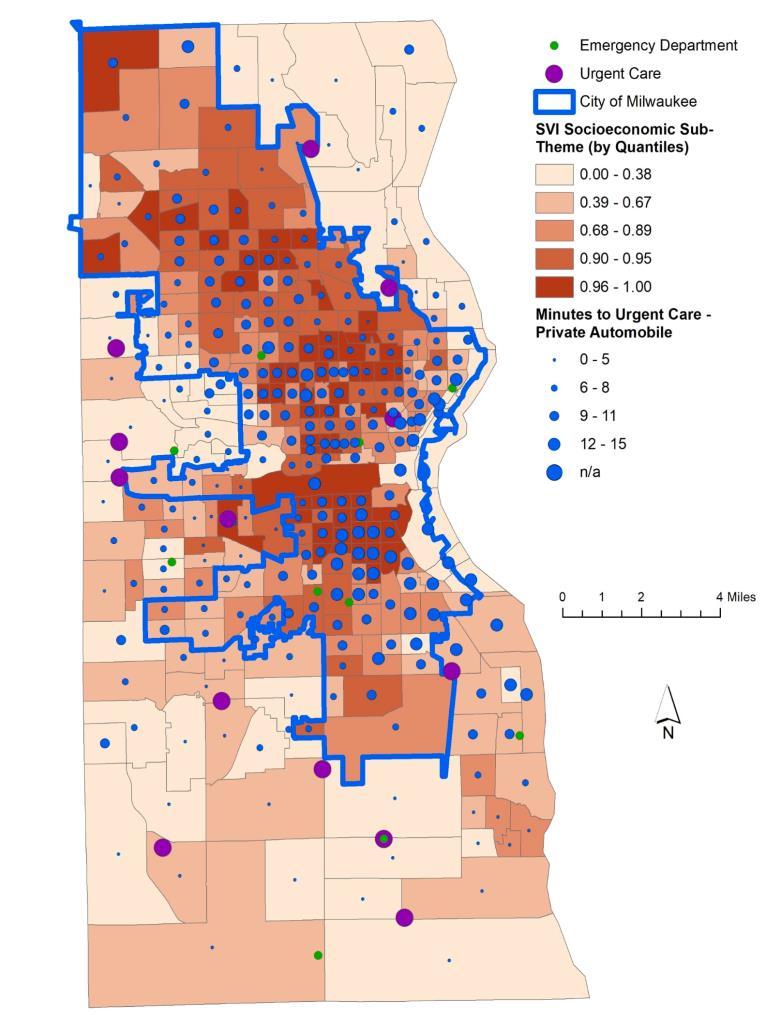
SVI, Social Vulnerability Index.
Importantly, we found disparate commute times to both types of healthcare facilities when compared to the socioeconomic vulnerability of each census tract. Socioeconomically disadvantaged communities had a statistically significant increase in private transit times to UCs and a decrease in public transit times to the nearest EDs. The general trend for all modes of transport was that individuals in more affluent communities had easier access to UCs, whereas EDs were more accessible to patients from poorer communities. These results mirror some of the findings from prior research investigating the accessibility of hospital-based vs freestanding EDs in some large metropolitan areas.22 The freestanding EDs, like the UCs in our study, were less accessible by public transportation as compared to hospitalbased EDs and were generally located in more affluent areas. As EDs deal with a sustained crowding crisis, minimizing
use for non-emergent complaints has generally been viewed as an important mitigation step.23,24 In particular, medical concerns that could be adequately addressed in alternative care settings have been the focus of substantial study.9,25 While primary care represents an important alternative, resource limitations also impact the availability of expedient appointments even for those with established PCPs.26-29 Thus, UCs are often viewed as another release valve for ED crowding with respect to the care of patients with minor injuries and ailments. However, the extent to which UCs might help to alleviate ED crowding is likely tempered in communities with limited access to these centers.
Decisions on where to seek care can be complex, and the influences are multifactorial. Urgent care centers are not beholden to the same federal care mandates, and the increasing number of UCs and decreasing number of hospitals nationwide is testament to the current financial, legal, and regulatory climate for US healthcare.30,31 While treatment in the ED is regarded as a more expensive mode of healthcare delivery than
Figure 4. Map of Milwaukee County displaying socioeconomic vulnerability and private transit times to healthcare facilities by private vehicle.
Figure 3. Map of Milwaukee County displaying socioeconomic vulnerability transit times to healthcare facilities by public transportation.
UCs, this may not be true at the individual level when accounting for considerations such as insurance status and visit copays.32 How and why patients choose a particular type of healthcare facility for non-emergent needs remains an important field of inquiry, and this study adds valuable context to a body of literature that also examines novel approaches to reduce low-acuity ED visits.33,34 Our findings indicate that when evaluating where patients seek care, geographic proximity and public transit accessibility should be considered. Socioeconomic status and transit times to EDs and UCs were significantly correlated, which may asymmetrically impact communities with higher socioeconomic vulnerability. The ease of access or lack thereof to UCs has implications for both ED use for nonemergent concerns and patterns of EMS use.
LIMITATIONS
This study measured the accessibility of healthcare facilities in one county in the state of Wisconsin. While Milwaukee is geographically and socioeconomically diverse, it is not necessarily nationally representative. As population density and public transit infrastructure differ in other regions, the geospatial considerations related to healthcare access may also change. Additionally, different states and municipalities may have statutes or regulations that directly or indirectly influence the location of these care facilities. Lastly, while this study examined transit times to UCs, proximity to care does not necessarily ensure accessibility. Variable UC payment models and upfront patient costs could affect the pattern of use independent of transit times, particularly for socioeconomically vulnerable populations.
CONCLUSION
Commute times to the nearest EDs and urgent care centers via public or private transit were associated with the socioeconomic vulnerability of census tracts in Milwaukee County. Further study is needed to determine the impact of this disparity in transit time on healthcare use for non-emergent medical needs.
Address for Correspondence: Kevin McGurk, MD, Medical College of Wisconsin, Hub for Collaborative Medicine, Department of Emergency Medicine, 3rd Floor, 8701 Watertown Plank Rd, Milwaukee, WI 53226. Email: kjmcgurk@mcw.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Telagi et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Black LI, Adjaye-Gbewonyo D. Urgent care center and retail health clinic utilization among adults: United States, 2019. NCHS Data Brief. 2021;(409).
2. Buttorff C, Heins SE, Al-Ibrahim H. Changing care settings for injuries. Med Care Res Rev. 2022;79(6):861-70.
3. Poon SJ, Schuur JD, Mehrotra A. Trends in visits to acute care venues for treatment of low-acuity conditions in the United States from 2008 to 2015. JAMA Intern Med. 2018;178(10):1342.
4. Zimmerman B, Punke H. 20 things to know about urgent care. 2017. Available at: https://www.beckershospitalreview.com/lists/20-thingsto-know-about-urgent-care-2017.html. Accessed May 23, 2024.
5. American College of Emergency Physicians Policy Statement: Urgent care centers. Ann Emerg Med. 2017;70(1):115-6.
6. Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood). 2010;29(9):1630-6.
7. Allen L, Cummings JR, Hockenberry J. Urgent care centers and the demand for non-emergent emergency department visits. 2019. Available at: https://www.nber.org/system/files/working_papers/ w25428/w25428.pdf. Accessed June 1, 2024.
8. Allen L, Cummings JR, Hockenberry JM. The impact of urgent care centers on nonemergent emergency department visits. Health Serv Res. 2021;56(4):721-30.
9. Coster JE, Turner JK, Bradbury D, et al. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med. 2017;24(9):1137-49.
10. McAndrews C. Transportation and land use as social determinants of health: the case of arterial roads. In: Deakin E, Ed, Transportation, Land Use, and Environmental Planning. Amsterdam, Netherlands: Elsevier; 2020:35-53.
11. Mirza NA, Hulko W. The complex nature of transportation as a key determinant of health in primary and community care restructuring initiatives in rural Canada. J Aging Stud. 2022;60:101002.
12. Flores G, Abreu M, Olivar MA, et al. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152(11):1119-25.
13. Cordasco KM, Ponce NA, Gatchell MS, et al. English language proficiency and geographical proximity to a safety net clinic as a predictor of health care access. J Immigr Minor Health 2011;13(2):260-7.
14. Liu X, Ben Liu Q. Superior medical resources or geographic proximity? The joint effects of regional medical resource disparity, geographic distance, and cultural differences on online medical consultation. Soc Sci Med. 2024;350:116911.
15. Carlson LC, Raja AS, Dworkis DA, et al. Impact of urgent care openings on emergency department visits to two academic medical centers within an integrated health care system. Ann Emerg Med 2020;75(3):382-91.
16. Health Compass Milwaukee. Available at: https:// healthcompassmilwaukee.org/topics/PCT?topic=demographics Accessed June 1, 2024.
17. Weinick RM, Bristol SJ, DesRoches CM. Urgent care centers in the U.S.: findings from a national survey. BMC Health Serv Res. 2009;9:79.
18. Weinick RM, Bristol SJ, Marder JE, et al. The search for the urgent care center. J Urgent Care Med. 2009;3(4):38-40.
19. R Project. The R Project for Statistical Computing. 2022. Available at: https://www.R-project.org/. Accessed March 1, 2023.
20. Gao F, Kihal W, Le Meur N, et al. Does the edge effect impact on the measure of spatial accessibility to healthcare providers? Int J Health Geogr. 2017;16(1):29.
21. Sadler RC, Gilliland JA, Arku G. An application of the edge effect in measuring accessibility to multiple food retailer types in Southwestern Ontario, Canada. Int J Health Geogr. 2011;10(1):34.
22. Carlson LC, Baker ON, Schuur JD. A geospatial analysis of freestanding and hospital emergency department accessibility via public transit. West J Emerg Med. 2019;20(3):472-6.
23. Lindner G, Woitok BK. Emergency department overcrowding: analysis and strategies to manage an international phenomenon. Wien Klin Wochenschr. 2021;133(5-6):229-33.
24. Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402-5.
25. Penson R, Coleman P, Mason S, et al. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department? Emerg Med J. 2011;29(6):487-91.
26. Ansell D, Crispo JA, Simard B, et al. Interventions to reduce wait times for primary care appointments: a systematic review. BMC
Health Serv Res. 2017;17(1):295.
27. Gotlieb EG, Rhodes KV, Candon MK. Disparities in primary care wait times in Medicaid versus commercial insurance. J Am Board Fam Med. 2021;34(3):571-8.
28. Grande D, Zuo JX, Venkat R, et al. Differences in primary care appointment availability and wait times by neighborhood characteristics: a mystery shopper study. J Gen Intern Med 2018;33(9):1441-3.
29. Parks A, Hoegh A, Kuehl D. Rural ambulatory access for semi-urgent care and the relationship of distance to an emergency department. West J Emerg Med. 2015;16(4):594-9.
30. Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA 2011;305(19):1978-85.
31. Yee T, Lechner AE, Boukus ER. The surge in urgent care centers: emergency department alternative or costly convenience? Health Syst Change. 2013;(26):1-6.
32. Ho V, Metcalfe L, Dark C, et al. Comparing utilization and costs of care in freestanding emergency departments, hospital emergency departments, and urgent care centers. Ann Emerg Med 2017;70(6):846-57.e3.
33. Heinert SW, Mumford M, Kim SE, et al. User characteristics of a low-acuity emergency department alternative for low-income patients. West J Emerg Med. 2020;21(6):162-71.
34. Wolfe MK, McDonald NC. Innovative health care mobility services in the US. BMC Public Health. 2020;20(1):906.
Inequities in the National Clinical Assessment Tool for Medical Students in the Emergency Department
Bushra Z. Amin, MD*
C. Jessica Dine, MD, MSHP*†§
Erica R. Tabakin, MD*‡
Michael Trotter, MD*‡
Janae K. Heath, MD, MSCE*†
Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania
Hospital of the University of Pennsylvania, Department of Medicine, Philadelphia, Pennsylvania
Hospital of the University of Pennsylvania, Department of Emergency Medicine, Philadelphia, Pennsylvania
Leonard Davis Institute of Economics at the University of Pennsylvania, Philadelphia, Pennsylvania
Section Editor: Jeffrey Druck, MD
Submission history: Submitted February 20, 2025; Revision received June 3, 2025; Accepted June 12, 2025
Electronically published October 3, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.43506
Introduction: The National Clinical Assessment Tool for Emergency Medicine (NCAT-EM) was designed to standardize medical student assessments during emergency medicine clinical rotations. While multiple assessment tools implemented in medical education have been prone to inequities, it remains unknown how student and rater demographics impact NCAT-EM scores. In this study we examined how a student’s gender and status as under-represented in medicine (URM) affected NCAT-EM scores.
Methods: This was a retrospective cohort study of all NCAT-EM assessments of clerkship medical students at a single institution in 2022. We performed mixed-effect ordinal logistic regression analyses to determine the association between the seven NCAT-EM domains (history/physical, prioritized differential, formulation of plans, observation/monitoring, emergency management, communication, and global assessment) and student gender, as well as the NCAT-EM domains and students’ URM status (specifically in domains of race and ethnicity). We adjusted our analyses for the site of rotation, time, the rater’s role (attending or resident), and rater demographics (gender, URM status). We then evaluated the interaction in gender concordance and URM-status concordance on outcomes.
Results: A total of 1,881 NCAT-EM assessment forms were submitted on 142 students completed by 266 raters. There were no significant associations between student gender and NCAT-EM ratings across the seven domains. We found an association between URM students and lower scores in multiple NCAT-EM domains, including global assessment (odds ratio [OR] 0.50, CI 0.25-0.99, P = .01); history/physical (OR 0.38, CI 0.19-0.77, P = .01); and prioritized differential (OR 0.47, CI 0.26-0.88, P = .02). This effect was moderated by a significant positive interaction effect with URM concordance between raters and students in the prioritized differential and observation/monitoring domains.
Conclusion: This is the first study to highlight differences in both gender and status as underrepresented in medicine within the nationally implemented NCAT-EM assessment tool. Women students were overall rated similarly across the NCAT-EM domains compared to men, with no association of gender on ratings. However, students’ URM status was associated with lower scores in multiple NCAT-EM domains. This finding was mitigated by URM concordance between faculty and resident raters. Our findings support the need for additional studies to understand bias and inequities in the application of the NCAT-EM tool nationally. [West J Emerg Med. 2025;26(5)1250–1259.]
INTRODUCTION
A longstanding challenge in medical education has been to accurately assess medical students on clinical rotations with assessment tools that have strong validity and reliability evidence.1,2 The fairness and accuracy of clinical assessment of medical students is critical as it informs clinical grades, Medical Student Performance Evaluation (MSPE), or “dean’s letters”, and—for those applying to emergency medicine (EM) residency—the Standardized Letter of Evaluation (SLOE).3 As EM residency program directors have consistently ranked SLOEs and EM rotation grades as some of the most important criteria when offering interviews and ranking applicants,4 ensuring fairness and accuracy in these assessments plays a paramount role in achieving equity among EM applicants.
In an effort to improve the fairness and accuracy of EM medical student assessments (and thus that of SLOEs and EM rotation grades), the National Clinical Assessment Tool for Emergency Medicine (NCAT-EM) was developed in 2016 via consensus as a standardized assessment tool.5 This tool allowed for post-shift assessment of students by faculty or residents across six clinical performance domains: history and physical exam skills; prioritized differential diagnosis; ability to formulate a plan; observation, monitoring, and follow-up; emergency recognition and management; and patient- and team-centered communication. This tool has begun to replace institution-specific tools in numerous EM rotations across the United States,2,5,6 and was the first nationally standardized, specialty-specific, entrustable professional activities-based assessment tool for medical students.5
Prior work evaluating early implementation of the NCAT-EM suggests it is achieving some of its stated goals. Specifically, Hiller et al noted high internal consistency in scores within a given institution,6 suggesting that this tool supports reliable comparison of students within an institution during the residency application process. However, this work showcased some gaps in the validity evidence, specifically noting site-specific variation in ratings, perhaps suggesting limitations in the response process of the validity (how the raters differentially use the tool) or the generalizability of the tool.1 Additionally, this prior work was predominantly limited to medical students in their fourth year (with a high percentage interested in EM residency), limiting generalizability. Additionally, although they found site-specific differences based on student and rater gender, they were unable to examine the association of race or ethnicity on NCAT-EM scores (despite known racial disparities in other standardized EM assessments,7,8 such as the SLOE9–11). Additional work to investigate the various domains of validity of this tool would add to the literature.
Unfortunately, such disparities in assessment have been observed throughout medical education,12 potentially contributing to the known leadership disparities and pay-based disparities based on gender and race.13–18 Studies have identified gender- and race-based differences in language used
Population Health Research Capsule
What do we already know about this issue? Clinical assessment tools in medical education often show racial and sex disparities in scoring and narrative feedback.
What was the research question?
Do student and rater demographics affect National Clinical Assessment Tool for Emergency Medicine (NCAT-EM) scores in emergency medicine clerkships?
What was the major finding of the study?
Under-represented in medicine (URM) students had lower global scores (OR 0.50, 95% CI 0.25-0.99, P =.048), which was mitigated by URM rater concordance.
How does this improve population health?
Identifying disparities in clerkship assessments supports equitable evaluation, critical for building a diverse physician workforce.
in the MSPE19,20 and language used in clerkship evaluations.7,19,21 Gender- and race-based differences have also been observed through clinical grades (with lower clinical grades for non-White students, even after adjusting for variables such as scores on Step 1 of the US Medical Licensing Exam)7,22 and overall recommendations on SLOEs.9–11 These differences likely represent inequities, especially when the observed variations are not explained by the student performance but instead by other factors such as the clinical learning environment or the evaluator.23,24 It is not known whether such differences persist despite the implementation of a nationally standardized tool such as the NCAT-EM.
To address this gap, our goal in this study was to analyze the association between student and rater demographics and NCAT-EM scores of clerkship students rotating through various emergency department sites at a single institution. Given prior evidence suggesting that concordance in demographics may impact ultimate evaluation,25,26 we similarly assessed how concordance in student and rater demographics was associated with NCAT-EM scores.
METHODS
Setting and Participants
We performed a retrospective, single-center cohort study
Inequities
in the NCAT-EM for Medical Students
of all electronically completed NCAT-EM assessments of clerkship medical students at the University of Pennsylvania. Individualized NCAT-EM forms were made available electronically through a Qualtrics (Qualtrics International Inc, Provo, UT) QR code. The dataset included all submitted NCAT-EM assessments from January–December 2022, as assessments completed during this year were unaffected by the COVID-19 pandemic. Given our interest in the impact of demographics on NCAT-EM scores, we excluded assessments for which demographic information (for either the student or the rater) was unavailable.
The Perelman School of Medicine curriculum includes 1.5 years of pre-clerkship content, followed by a one-year clerkship year, consisting of eight core clerkships (emergency medicine, family medicine, internal medicine, neurology, obstetrics and gynecology, pediatrics, psychiatry, and surgery) graded on an honors/high pass/pass/fail basis. During the clerkship year, students additionally complete an additional month of otolaryngology, orthopedic surgery, anesthesia, and ophthalmology (one week each, graded on a pass/fail basis). The EM clerkship is a four-week core clerkship completed at either one or two of six affiliated clinical sites.
The NCAT-EM has been used for clinical assessment of EM clerkship students in this institution since 2018. The NCAT-EM consists of six clinical performance domains rated on a four-point entrustability scale, a global assessment domain, a professionalism section, and mandatory free-text comments for strengths and suggestions for improvement (Supplemental Table 1). Students are required to present a QR code linking the NCAT-EM to attendings or EM residents during every shift, which is completed at the rater’s convenience on an online platform.
During the EM clerkship, students were assigned to work 14 eight-hour shifts (or total hourly equivalent for sites with 10- or 12-hour shifts) for the duration of the clerkship. Students were required to present the QR code to at least one rater per shift (either an attending or a supervising resident ranging from postgraduate year [PGY] 2-4). The dataset did not include discrete PGY-level data for resident raters. Prior to and during this study, the clerkship directors performed annual education focused on the NCAT-EM tool and the process of assessment, which consisted of an introduction to the tool, a brief overview of the scale, and a review of medical student evaluation processes. This information session included both faculty and residents at all sites (for all individuals who would be working with students).
Data Collection and Analysis
Data collected in addition to completed NCAT-EM forms included student factors (gender and under-represented in medicine [URM] status) and rater factors (gender, URM status, and role, either resident or faculty). We extracted gender and race data for students from admissions demographics based on self-identification. For faculty,
self-reported gender and race were obtained through the university’s faculty affairs database. We defined URM status for both faculty and students using the Association of American Medical Colleges (AAMC) definitions. The URM status was specifically chosen as a binary variable (as opposed to race and ethnicity data), to improve power in our statistical analysis. Importantly, the definition of URM can broadly include groups that are minoritized, such as first-generation, low-income students, or students with disabilities, although for this work we used the AAMC definition of URM based on race and ethnicity. The dataset also included the quarter of year in which the student was completing the clerkship (block 1, 2, 3, or 4), and the clinical site where they were rotating. All data were deidentified prior to data analysis.
We performed univariate ordinal logistic regression analyses to determine the association between the global assessment on the NCAT-EM tool (bottom third, middle third, top third, or top 10%), with student gender, student URM status, faculty gender, faculty URM status, clerkship site, and rotation block. We then performed mixed-effect ordinal logistic regression analyses to determine the association between NCAT-EM scores and student gender, clustered by student, after adjusting for site of rotation, time, role of rater, student URM status, and rater demographics (gender, URM status). To assess the association with URM status, we performed mixed-effect ordinal logistic regression analyses to determine the association between NCAT-EM scores and student URM status, clustered by student, after adjusting for site of rotation, block, role of rater, student gender, and rater demographics. Given the hypothesis that concordance in rater gender and student gender and URM status might be associated with NCAT-EM scores, we also assessed the interaction between student gender and rater gender, and student URM status and rater URM status.
For each analysis, the model was clustered on student (random effects) and rater (random effects). This model was used intentionally to adjust for the non-independent nature of students and/or raters throughout the dataset, as this model provides adjusted standard errors accounting for student and/ or rater clustering (random effects) throughout the dataset. Based on prior factor analyses showing each domain in the NCAT-EM assessed unique domains, we repeated the above analysis for each of the six clinical performance domains of the assessment. (See Supplemental Table 1 for the NCATEM domains.)
While our primary analysis included URM (as per AAMC definition) as a binary variable, we aimed to further understand our findings in the context of URM categories, recognizing that URM individuals who spanned different identities might have had different experiences with assessment. Thus, we performed a sensitivity analysis using racial and ethnic groups within the AAMC definition of URM (African- American/Black, Hispanic/Latino, Native American, including American Indian, Alaska Native, and Native
Hawaiian, Pacific Islander, and mainland Puerto Rican). We then performed a second sensitivity analysis comparing individuals identifying as Black compared to other individuals (noting the large proportion of individuals within the cohort identifying as URM were Black and the distinct experiences of this population27,28).
We completed statistical analysis using STATA v18.0 (StataCorp, LLC, College Station, TX). Statistical significance was determined using a P-value of .05 (not adjusting for multiple comparisons given the exploratory nature of the analysis, to reduce the risk of type 2 error). This study was deemed exempt by the University of Pennsylvania Institutional Review Board.
RESULTS
Over the course of 2022, 1,881 complete NCAT-EM assessment forms were submitted on 142 distinct students (consisting of 74 women [52%] and 68 men [48%], including 34 [24%) who identified as URM) completed by 266 different raters. We excluded 122 NCAT-EM forms prior to analysis, due to incomplete demographic information for the rater. The median number of completed forms per student was 13 [(IQR 11- 15), which was similar between genders (13.4 for men vs 13.1 for women, P = .59). There were fewer NCAT-EM assessments completed on those who identified as URM within the sample (with a mean of 11.8 vs 13.8 assessments for non-URM students, P = .01). Most assessments were completed by raters who identified as men (n = 1,070, 60%), and 11% (n = 195) were completed by raters who identified as URM. The racial demographics of faculty identified as URM (as per AAMC definitions) was 119 (61%) Black, 55 (28%) Hispanic or Latino, and 21 (11%) Pacific Islander. The racial demographics of students identified as URM (as per AAMC definitions) was 224 (56%) Black, 38 (10%) Hispanic or Latino, and 138 (35%) spanning multiple groups. Complete demographic information of completed NCAT-EM forms are included in Table 1.
Distribution of scores for each of the six clinical performance domains on the NCAT-EM as well as the global assessment domain (see Supplemental Table 1) are summarized in Table 2. Global assessment scores were skewed leftward (consistent with prior national data5), with 38 ratings (2.1) ratings representing the lower third in the global assessment, 506 (28%) in the middle third, 878 (49%) in the upper third, and 387 (21%) in the top 10% (“exceptional”).
The results of the univariate ordinal logistic regression are shown in Table 3. In the univariate analysis, there was a significant association based on rater role, with faculty raters being less likely to rate students in the higher entrustment scores compared to resident raters for all domains (P < .001 for all domains); thus, this was included in the multivariate analysis. There was also an association between rotation block and NCAT-EM scores, and site of the rotation and NCAT-EM scores; thus, these variables were included in the final
Table 1. Student characteristics, rater characteristics, clinical site and block of completed NCAT-EM assessment forms.
Characteristic Completed NCAT-EM forms (n, %)
Student gender 1881 (100.0%)
Men 913 (48.5%)
Women 968 (51.5%)
Student URM status
African American/Black
(100.0%)
(56%)
Hispanic/Latino 38 (10%)
Multiple AAMC URM Groups 138 (35%)
Non-URM 1481 (78.7%)
Rater Role
Resident
Rater Gender
(27.3%)
(72.7%)
(40.0%)
Rater URM Status 1759 (100.0%)
URM
care site
(100.0%)
(36.9%)
All results are expressed as number of NCAT assessment forms completed within each category, followed by percent of assessments for which data are available.
NCAT-EM, National Clinical Assessment Tool for Emergency Medicine; URM, under-represented in medicine; AAMC, Association of American Medical Colleges.
regression model.
The results of the multivariate ordinal logistic regression, clustered by student and rater, are shown in Table 4, using a significant threshold of P = .05 (rather than adjusting for
Table 2. Overview of ratings for National Clinical Assessment Tool for Emergency Medicine clinical performance domains and global assessment.
NCAT-EM Domain n (%)
Focused history and physical exam skills
Unable to assess
Pre-entrustable
Mostly entrustable
Fully entrustable/Milestone 1
Outstanding/Milestone 2
1,879 (100%)
25 (1%)
118 (6%)
742 (40%)
754 (40%)
240 (13%)
Ability to generate a prioritized differential diagnosis 1,866 (100%)
Unable to assess
Pre-entrustable
Mostly entrustable
Fully entrustable/Milestone 1
Outstanding/Milestone 2
31 (2%)
152 (8%)
818 (44%)
664 (36%)
201 (11%)
Ability to formulate plan (diagnostic, therapeutic, disposition) 1,861 (100%)
Unable to assess
Pre-entrustable
Mostly entrustable
Fully entrustable/Milestone 1
Outstanding/Milestone 2
34 (2%)
163 (9%)
894 (48%)
592 (32%)
178 (10%)
Observation, monitoring, and follow-up 1,861 (100%)
Unable to assess
Pre-entrustable
Mostly entrustable
Fully entrustable/Milestone 1
Outstanding/Milestone 2
Emergency recognition and management
Unable to assess
Pre-entrustable
Mostly entrustable
Fully entrustable/Milestone 1
Outstanding/Milestone 2
Patient- and team-centered communication
Unable to assess
Pre-entrustable
Mostly entrustable
Fully entrustable/Milestone 1
Outstanding/Milestone 2
Global assessment
Lower third
Middle third
Top third
Exceptional (top 10%)
42 (2%)
120 (6%)
683 (37%)
747 (40%)
263 (14%)
1,851 (100%)
385 (21%)
98 (5%)
673 (36%)
523 (28%)
172 (9%)
1,848 (100%)
40 (2%)
65 (4%)
605 (33%)
794 (43%)
344 (19%)
1,809 (100%)
38 (2%)
506 (28%)
878 (49%)
387 (21%)
All results are expressed as number of NCAT-EM assessment forms completed within each category, followed by percentage of assessments for which data are available.
NCAT-EM, National Clinical Assessment Tool for Emergency Medicine.
multiple comparison due to the exploratory nature of the study). As there was no significant interaction between the student gender and rater gender in each analysis, this interaction term was excluded from the final regression model. The final regression model included the rater gender and student gender, rater and student URM status (and the interaction between them), rater role (faculty vs resident), clinical site, and rotation block. The results of the mixed regression identified no significant associations between student gender and NCAT-EM scores for each NCAT-EM domain (Table 4). There was a significant interaction effect between student gender and rater gender in the domain of history and physical exam (OR 0.31, CI 0.11-0.83, P = .02). There were no other significant interaction effects in the remainder of the domains.
Student URM status was associated with lower scores for the global assessment, (OR 0.50, CI 0.25-0.99, P = .05), history/physical exam domain (OR 0.38, CI 0.19-0.77, P = .01) and the prioritized differential diagnosis domain (OR 0.47, CI 0.26-0.88, P = .02) after multivariate adjustment, as shown in Table 4. These findings were moderated by a significant positive interaction effect between student and rater URM status in the observation/monitoring domain (OR 4.55, CI 1.21-17.1, P =.03), suggesting that concordance in URM status between raters and students lessened (and in some instances, reversed) the negative effect of URM status on NCAT-EM scores. More specifically, when assessing the significant domains for a given student, the adjusted ORs for URM-concordant dyads were adjusted OR 0.83 for the global assessment (suggesting the difference persisted); adjusted OR 1.06 for history/physical domains; and adjusted OR 1.76 for observation/monitoring (suggesting reversal of the score, and URM-concordant dyads had higher odds of receiving a higher score than the reference cohort).
The sensitivity analysis using racial and ethnic groups within the URM status (Black, Hispanic/Latino, Native Americans, including American Indians, Alaska Natives, and Native Hawaiians, Pacific Islanders, and mainland Puerto Ricans demonstrated a poorer fit to the data—based on likelihood ratio tests and Bayesian information criterion and Akaike’s information criterion comparisons—than the original model. As this approach risked underestimating the true effect, it was not included in the results. In our sensitivity analysis comparing individuals who were Black to other individuals in the cohort, we found significant associations with NCAT-EM ratings in the domains of history/physical domain (OR 0.32, CI 0.14-0.76, P = .01); prioritized differential domain (OR 0.36, CI 0.17-0.79, P =.01); the ability to formulate a plan domain (OR 0.46, CI 0.59-1.48, P =.05), with significant interaction effects noted in the majority of domains. (See Table 5 for full details.)
DISCUSSION
Our study demonstrates important associations between both rater and student demographics and NCAT-EM scores
Student gender
Student URM-status
Rater role
(0.38, 0.57)
(0.28, 0.42)
Rater gender
(0.88, 1.26)
Rater URM-status
(0.53, 0.93)
(1.06, 1.51)
(0.82, 1.43)
OR, odds ratio; NCAT-EM, National Clinical Assessment Tool for Emergency Medicine; URM, under-represented in medicine.
within our cohort, with notable findings based on student URM status. Our multivariate analysis did not find any gender-related differences in NCAT-EM domains. However, the multivariate analysis showed that students identified as URM received lower NCAT-EM scores in several domains, including the history/physical exam domain and the prioritized differential diagnosis domain. This effect was mediated (and in some cases reversed) by concordance of URM status between raters and students in some of the domains, such that concordance in URM status between students and raters was associated with higher NCAT-EM scores.
The association between student URM status with lower NCAT-EM scores is consistent with prior literature
documenting longstanding racial disparities in clerkship grading.21,29,30 Despite the NCAT-EM being noted to have excellent internal consistency based on prior studies,6 this suggests that the use of the tool continues to be impacted by its differential use by raters and raises some concern about additional domains of validity with the tool.1 It is important for us as medical educators to ensure the assessment tool widely used to guide clerkship grading does not introduce any construct irrelevance variance at all.31,32
In this study, the observed score differences by URM status may be the result of implicit bias of raters affecting both their global perception and perception of competency-related behaviors of students, lack of mentorship leading to
Table 3. Univariate associations between ratings for National Clinical Assessment Tool for Emergency Medicine domains and student and rater characteristics.
Table 4. Multivariate associations between ratings for National Clinical Assessment Tool for Emergency Medicine domains and student sex and under-represented in medicine (URM) status, after adjusting for rater sex and URM status, concordance of student-rater URM status, clinical site, and time.
Student Sex
Interaction between rater and student gender
(0.49, 1.09)
Student URM Status
Interaction between rater and student URM-status
OR, odds ratio; NCAT-EM, National Clinical Assessment Tool for Emergency Medicine; URM, under-represented in medicine.
Table 5. Multivariate associations between ratings for National Clinical Assessment Tool for Emergency Medicine domains and Black vs non-Black race, after adjusting for rater sex and race (Black vs non-Black), concordance of student-rater race, clinical site, and time.
Student Race
between Black Raters and Black Students
OR, odds ratio; NCAT-EM, National Clinical Assessment Tool for Emergency Medicine.
inequitable opportunities, or different lived experiences of URM students impacting their experience, and performance in the clinical environment (including stereotype threat, microaggressions, patient mistreatment, being tasked with being a racial ambassador, unrewarded labor, limited resources, and othering).17,21,33–35 The complexity of this amalgam of factors that exacerbates disparities in clerkship grading has been described as the “social milieu of medical education,”35 and may ultimately contribute to the inequities observed in other standardized assessments used in EM, such as the SLOE. Improved understanding of these disparities in the EM clerkship setting and further evaluation of the validity evidence of the NCAT-EM tool is critical to identify solutions to mitigate these issues.
Perhaps more interestingly, some of the findings of a differential score based on URM status were mitigated (and in some cases, reversed) by URM concordance between the student and rater, specifically within the prioritization of a differential, and the observation and monitoring domains. As a possible explanation, URM concordance may reduce implicit bias of the rater as well as the other effects of racism on the medical student, such as stereotype threat. Concordance between the rater and student can also enhance performance of the student through the role-model effect.33 This aligns with prior studies that have shown the importance of racial concordance in multiple domains, including patient care, professional development,17 and medical education assessment,36,37 further highlighting the critical nature of supporting equity initiatives to advanced diversity across EM faculty and residents.
It is not clear why this phenomenon would be present for only two of the NCAT-EM domains, although it could represent something unique about those domains, including that they may capture more direct interaction between students and raters (such as prioritizing differentials) and, thus, concordance would be more heavily impacted. Regardless, this further suggests that additional robust validity studies of the NCAT-EM tool are needed. Additionally, while we noted various impacts of URM concordance on the NCAT-EM scores, the impact on the overall disparities identified in our study may be negligible, and further work is needed to examine this phenomenon across a larger sample of more diverse learners and raters.
Another interesting observation within our study was that URM students had fewer submitted NCAT-EM forms in the full cohort, which persisted after adjusting for minor site differences. The structure of the NCAT-EM within our institution requires learners to seek out designated feedback and collect assessments via a QR code. This difference could indicate differences in self-promotion behavior,38 which may uniquely disadvantage URM students. Specifically, there is a complex interplay between evaluations, biases, and the associated impact on confidence, self-esteem, and motivation. In URM students, negative evaluations, even if biased, may
Inequities in the NCAT-EM for Medical Students
reinforce stereotype threat—defined as a fear of confirming negative stereotypes about their group—17 and ultimately hinder professional growth. Understanding this, as well as other unique barriers to seeking evaluation by URM students as observed in this study, should be further evaluated.
We also found no difference in NCAT-EM scores based on gender, with no significant difference in scores between men and women in the cohort. This absence of gender associations across the NCAT-EM performance domains was surprising, and in contrast to prior work analyzing the NCAT-EM in medical students. Specifically, in a study by Hiller and colleagues, there were student gender-based differences in composite NCAT-EM scores at 4 of the 13 sites included in their study.6 However, this prior work was conducted with limited demographic data and an overrepresentation of male students, with predominantly students in their final year of medical school. It is possible that gender disparities across diverse assessment domains become apparent at later stages in training (as has been observed in residency assessments). 39,40
As NCAT-EM scores inform clinical grades, and subsequently the SLOE and MSPE, it is critical to mitigate disparities in use of the NCAT-EM tool as found in our study. The NCAT-EM has features of prior recommendations to reduce grading inequity, including workplace-based assessment, criterion-based rubrics, and competency-based grading. Our data show that rating disparities are still present, despite high internal consistency metrics of the NCAT-EM. This argues that the tool itself does not contribute to disparities, but real-world use of the tool by raters contributes to these differences. Ultimately, the scoring differences found in our study support the use of rater training, which has been shown to improve the accuracy of workplace-based entrustment ratings of medical learners.41
Additionally, ongoing efforts to promote an equitable and diverse workforce are necessary, noting the role of concordance on some of these disparities. Ultimately, achieving fairness and accuracy in NCAT-EM assessments is crucial to promoting gender and racial equity among EM applicants, especially with national implementation of the NCAT-EM tool. In addition, clerkships in other specialties should note that despite the positive impacts of using a standardized and national assessment instrument with strong reliability, testing by itself is not the solution for overcoming observed differences not explained by student performance.
LIMITATIONS
Although we identified compelling findings, this study had several limitations. Our study analytic approach involved multiple regressions, and we did not adjust for multiple comparisons due to the exploratory nature of the study, which increased the risk of type 1 error in our conclusions. However, we feel the presence of findings in our sensitivity analysis suggests that this finding is a true trend. In addition, the study
Inequities in the NCAT-EM for Medical Students
was limited to a single institution. Although it included six different sites within the institution (each with a unique culture and patient population), obtaining a multicenter study across distinct geographical regions is an important next step to fully evaluate the effect of student and rater demographics on NCAT-EM performance nationally. Furthermore, it is not yet clear whether these findings among second- and third-year clerkship students can be generalized to more senior medical students on sub-internships or electives, and additional work evaluating the impact of URM status on advanced students is needed. Our study did not include individuals who identified as gender diverse, which would also be important to include in future research. Finally, while we importantly noted some differences in NCAT-EM use by site and by level (residents NCAT-EM scores were higher as compared to faculty), we were unable to assess PGY level in residency training nor the impact of faculty development on the tool. This is an important area of future work.
CONCLUSION
While we found no association between student gender with NCAT-EM scores, we did find an association between student under-represented in medicine status in two of six NCAT-EM performance domains, an effect that was mediated by concordance in URM status with the rater. Future multiinstitution research is needed to verify grading disparities based on student and rater characteristics on the national level, which would further support the use of multifaceted interventions to mitigate disparities in ratings, including diversity efforts in recruitment practices, equitable access to medical school resources, gender- or URM-specific student support and rater training to ultimately promote equity among emergency physicians.
Address for Correspondence: Janae K. Heath, MD, MSCE, Hospital of the University of Pennsylvania, Department of Medicine, 3600 Spruce St, 822 West Gates Building, Philadelphia, PA 19104. Email: Janae.heath@pennmedicine.upenn.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Amin et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Cook DA, Beckman TJ. Current concepts in validity and reliability for
Amin et al.
psychometric instruments: theory and application. Am J Med 2006;119(2):166.e7-16.
2. Lawson L, Jung J, Franzen D, et al. Clinical assessment of medical students in emergency medicine clerkships: a survey of current practice. J Emerg Med. 2016;51(6):705-11.
3. Negaard M, Assimacopoulos E, Harland K, et al. Emergency medicine residency selection criteria: an update and comparison. AEM Educ Train. 2018;2(2):146-153.
4. Katzung KG, Ankel F, Clark M, et al. What do program directors look for in an applicant? J Emerg Med. 2019;56(5):e95-101.
5. Jung J, Franzen D, Lawson L, et al. The National Clinical Assessment Tool for Medical Students in the emergency department (NCAT-EM). West J Emerg Med. 2018;19(1):66-74.
6. Hiller K, Jung J, Lawson L, et al. Multi-institutional implementation of the national clinical assessment tool in emergency medicine: data from the first year of use. AEM Educ Train. 2021;5(2):e10496.
7. Gauer JL, Mustapha T, Violato C. Race and gender bias in clerkship grading. Teach Learn Med. 2024;36(3):304-11.
8. Nguemeni Tiako MJ, Ray V, South EC. Medical schools as racialized organizations: how race-neutral structures sustain racial inequality in medical education—a narrative review. J Gen Intern Med 2022;37(9):2259-66.
9. Winfield A, Amin DP. To the Editor: Where Is equity in the SLOE? J Grad Med Educ. 2022;14(3):357.
10. Calles I. To the Editor: For equity in assessment: a comment on bias in the emergency medicine Standardized Letter of Evaluation. J Grad Med Educ. 2023;15(1):129.
11. Kukulski P, Ahn J. Validity evidence for the emergency medicine Standardized Letter of Evaluation. J Grad Med Educ. 2021;13(4):490-9.
12. Colson ER, Pérez M, Blaylock L, et al. Washington University School of Medicine in St. Louis Case Study: A Process for Understanding and Addressing Bias in Clerkship Grading. Acad Med. 2020 Dec;95(12S Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments):S131-5.
13. Cheng D, Promes S, Clem K, et al. Chairperson and faculty gender in academic emergency medicine departments. Acad Emerg Med 2006;13(8):904-6.
14. Madsen TE, Linden JA, Rounds K, et al. Current status of gender and racial/ethnic disparities among academic emergency medicine physicians. Acad Emerg Med. 2017;24(10):1182-92.
15. Wiler JL, Wendel SK, Rounds K, et al. Salary disparities based on gender in academic emergency medicine leadership. Acad Emerg Med. 2022;29(3):286-93.
16. Jena AB, Khullar D, Ho O, et al. Sex differences in academic rank in US medical schools in 2014. JAMA. 2015;314(11):1149-58.
17. Bullock JL, Lockspeiser T, Del Pino-Jones A, et al. They don’t see a lot of people my color: a mixed methods study of racial/ethnic stereotype threat among medical students on core clerkships. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S58-S66.
18. Ackerman-Barger K, Boatright D, Gonzalez-Colaso R, et al. Seeking
inclusion excellence: understanding racial microaggressions as experienced by underrepresented medical and nursing students. Acad Med. 2020;95(5):758-63.
19. Ross DA, Boatright D, Nunez-Smith M, et al. Differences in words used to describe racial and gender groups in Medical Student Performance Evaluations. PLoS ONE. 2017;12(8):e0181659.
20. Axelson RD, Solow CM, Ferguson KJ, et al. Assessing implicit gender bias in Medical Student Performance Evaluations. Eval Health Prof. 2010;33(3):365-85.
21. Hanson JL, Pérez M, Mason HRC, et al. Racial/ethnic disparities in clerkship grading: perspectives of students and teachers. Acad Med 2022;97(11S):S35-S45.
22. O’Sullivan L, Kagabo W, Prasad N, et al. Racial and ethnic bias in medical school clinical grading: a review. J Surg Educ 2023;80(6):806-16.
23. Lucey CR, Hauer KE, Boatright D, et al. Medical education’s wicked problem: achieving equity in assessment for medical learners. Acad Med. 2020;95(12S Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments):S98-S108.
24. Kakara Anderson HL, Govaerts M, et al. Clarifying and expanding equity in assessment by considering three orientations: Fairness, inclusion and justice. Med Educ. 2025;59(5):494-502.
25. Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open. 2020;3(11):e2024583.
26. McOwen KS, Bellini LM, Guerra CE, et al. Evaluation of clinical faculty: gender and minority implications. Acad Med 2007;82(10):S94.
27. Nguemeni Tiako MJ, Wages JE 3rd, Perry SP. Black medical students’ sense of belonging and confidence in scholastic abilities at historically Black vs predominantly White medical schools: a prospective study. J Gen Intern Med. 2023 Jan;38(1):122-4.
28. Ghanem N, Goldberg DG, Granger E, et al. A critical qualitative study to understand current Black women medical student perspectives on anti-racist reform in US medical education. Med Educ Online. 2024;29(1):2393436.
29. Boatright D, Anderson N, Kim JG, et al. Racial and ethnic differences
in internal medicine residency assessments. JAMA Netw Open 2022;5(12):e2247649.
30. Low D, Pollack SW, Liao ZC, et al. Racial/ethnic disparities in clinical grading in medical school. Teach Learn Med. 2019;31(5):487-96.
31. Downing SM. Threats to the validity of locally developed multiplechoice tests in medical education: construct-irrelevant variance and construct underrepresentation. Adv Health Sci Educ Theory Pract 2002;7(3):235-41.
32. Tavakol M, Dennick R. The foundations of measurement and assessment in medical education. Med Teach. 2017;39(10):1010-5.
33. Wheeler M, de Bourmont S, Paul-Emile K, et al. Physician and trainee experiences with patient bias. JAMA Intern Med 2019;179(12):1678-85.
34. Colson ER, Pérez M, Chibueze S, et al. Understanding and addressing bias in grading: progress at Washington University School of Medicine. Acad Med. 2023;98(8S):S64.
35. Osseo-Asare A, Balasuriya L, Huot SJ, et al. Minority resident physicians’ views on the role of race/ethnicity in their training experiences in the workplace. JAMA Netw Open. 2018;1(5):e182723.
36. Heath JK, Dine CJ, LaMarra D, et al. The impact of trainee and standardized patient race and gender on internal medicine resident communication assessment scores. J Grad Med Educ. 2021;13(5):643-9.
37. Berg K, Blatt B, Lopreiato J, et al. Standardized patient assessment of medical student empathy: ethnicity and gender effects in a multi-institutional study. Acad Med. 2015;90(1):105-11.
38. Pololi L, Conrad P, Knight S, et al. A Study of the relational aspects of the culture of academic medicine. Acad Med. 2009;84(1):106.
39. Dayal A, O’Connor DM, Qadri U, et al. Comparison of male vs female resident milestone evaluations by faculty during emergency medicine residency training. JAMA Intern Med. 2017;177(5):651-7.
40. Santen SA, Yamazaki K, Holmboe ES, et al. Comparison of male and female resident milestone assessments during emergency medicine residency training: a national study. Acad Med. 2020;95(2):263.
41. Kogan JR, Dine CJ, Conforti LN, et al. Can rater training improve the quality and accuracy of workplace-based assessment narrative comments and entrustment ratings? A randomized controlled trial. Acad Med. 2023;98(2):237-47.
Narrative Review of Emergency Medicine Clinical Research Examining Exclusion by Language
Alexa M. Curt, MD†
Olivia Kahn-Boesel, MD‡
Melis Lydston, MLS§
Melissa A. Meeker, PhD†
Margaret E. Samuels-Kalow, MD, MPhil, MSHP†
Section Editor: Sara Heinert, PhD, MPH
Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts
Massachusetts General Hospital, Department of Medicine, Boston, Massachusetts
Massachusetts General Hospital, Treadwell Virtual Library, Boston, Massachusetts
Submission history: Submitted March 4, 2025; Revision received June 30, 2025; Accepted July 2, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.46547
Introduction: Over 20% of the United States population speaks a language other than English, and many use the emergency department (ED) to access healthcare. However, there remains concern that patients preferring languages other than English are under-represented in clinical research. Thus, our goal was to assess the proportion of ED studies that excluded patients for recruitment due to language.
Methods: We conducted a narrative review using seven search engines for 2018–2023. We included studies if they mentioned language of participants and prospectively enrolled patients in an ED or prehospital setting. We excluded studies if they only included patients <18 years and/or were conducted exclusively outside the US. Two independent reviewers reviewed studies. Analyses included descriptive statistics.
Results: Of the 10,513 studies we identified, 281 were eligible for review; 163 (58%) excluded nonEnglish language preferred (NELP) patients. Among the 107 interventional studies, 69% excluded NELP patients. Of the 135 studies focused on health equity/social emergency medicine, 47% excluded NELP patients.
Conclusion: We found 163 (58%) studies conducted in the ED that mention language and excluded NELP patients. Additional work is needed to encourage and support inclusive study designs. [West J Emerg Med. 2025;26(5)1260–1264.]
INTRODUCTION
The United States is increasingly multilingual, with an estimated 22% of the US population speaking languages other than English according to the 2020 US Census,1 which is a 52% increase from 2000.1 These are likely underestimates given their fears centered on immigration status and inability to complete the census form.2 Despite the growing percentage of the general population preferring languages other than English, this population remains significantly under-represented in clinical research,3 with ongoing disparities in health outcomes compared to English-speaking patients.4-6 This disparate participation in clinical research limits the ability of the work to inform policy to improve care and equity.
The emergency department (ED) serves a significant proportion of racial and ethnic minority patients7 and thus has the potential to be a key location within the healthcare system to mitigate disparities in clinical research recruitment. Despite this, enrollment and consent for clinical studies is more likely to occur in middle-aged White patients.8 Many variables could influence this disparate rate of participation, such as mistrust of the healthcare system, fear of additional documentation, or lack of compensation for time.9 Although there is likely a complicated web of variables interacting to drive this disparity, studies that explicitly limit recruitment and enrollment to patients who speak English form a critical bottleneck to increasing racial and ethnic minority participation in clinical research.
A recent study showed that 65% of clinical trials conducted in the pediatric population enrolled only English-speaking patients.10 However, it is not known how often clinical studies conducted in adult EDs exclude non-English language preferred (NELP) patients from being approached for clinical research studies. Thus, we conducted a narrative review to investigate the number of published or described studies that prospectively enrolled patients in the ED or prehospital setting and reported language of enrollment but excluded NELP patients.
METHODS
Our review adhered to the Scale for the Assessment of Narrative Review Articles (SANRA) guidelines for narrative reviews.11 In March 2023, a medical librarian conducted electronic searches for published literature using Ovid MEDLINE, PubMed Central, Embase.com, Web of Science Core Collection, Cochrane Central Register of Controlled Trials via Ovid, and ClinicalTrials.gov. The search strategy incorporated controlled vocabulary and free-text synonyms for the concepts of emergency care, language limitations, and methods. The full database search strategies are documented in Appendix Supplemental Tables 1-6. We placed a date limit from 2018–2023. The literature search pulled studies within this time frame that occurred in the ED and mentioned language in any capacity. We used a variety of search terms to encompass language for our search, as listed in Supplemental Tables 1-6. Studies were reviewed independently by two reviewers. We resolved discrepancies between reviewers with discussion and consensus. We included studies that approached patients for research consent for any type of clinical research conducted in an ED or in the prehospital setting with emergency medicine services personnel. We also included studies that enrolled patients in additional settings beyond the ED and prehospital setting if they contained an ED or prehospital component. We excluded studies with study populations composed solely of patients < 18 years, although we included studies with populations < 18 years of age if they also enrolled patients > 18. We excluded studies conducted exclusively outside the US. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram reflecting this process is demonstrated in Figure 1.
We combined and de-duplicated all identified studies ed in a single reference manager (EndNote12). We then uploaded the citations into Covidence systematic review software (Veritas Health Innovation Ltd, Melbourne, Australia). Extraction variables are listed in Supplemental Table 7 and include the following: title; year published; authors; journal; journal publication or conference presentation; abstract or manuscript; study design; objective of study (one line describing goal of study); topic of study (health equity/social emergency medicine vs other); primary enrollment or secondary analysis; presence of an intervention; languages recruited (if described); other inclusion criteria for the study; and exclusion criteria. We defined health equity/social emergency medicine as factors related to
Population Health Research Capsule
What do we already know about this issue?
Non-english language preferred (NELP) patients are frequently under-represented in clinical research, limiting equitable evidence and policy development.
What was the research question?
Of studies published in emergency medicine journals between 2018-2023, how many excluded NELP patients?
What was the major finding of the study?
Of 281 studies, 58% excluded NELP patients. Among interventional studies, 69% excluded NELP patients.
How does this improve population health?
This study highlights the need for more inclusive study designs with support for diverse research populations to better reflect and serve patient populations.
social determinants of health, social risk, and social needs.13 We ascertained the primary outcome (language of inclusion) by reading the study methods and demographic tables (if included) of the abstracts or manuscripts. We used the inclusion and exclusion criteria on ClinicalTrials.gov to determine whether the clinical trials were excluding patients based on language. We categorized studies as “English only,” “not English only,” and “did not specify” based on the languages of patients recruited for the s-tudy. We then completed descriptive analyses stratified by language recruitment.
RESULTS
As indicated in the PRISMA flow diagram (Figure 1), a total of 10,513 studies were identified. After removing duplicates, 7,499 abstracts were screened for inclusion criteria by two reviewers (AC, OKB). Next, 603 studies underwent full text review. Finally, 281 studies were extracted as demonstrated in Supplemental Table 7. As shown in Table 1, 163 (58%) of the 281 studies excluded NELP patients and eight (3%) did not specify language of patients recruited. Regarding topic of study, 135 (47%) investigated a research question related to health equity or social emergency medicine. Within these 135 studies, 63 (47%) excluded NELP patients, 70 (52%) included NELP patients, and two (1%) did not specify. The remaining 146 studies covered any other topic
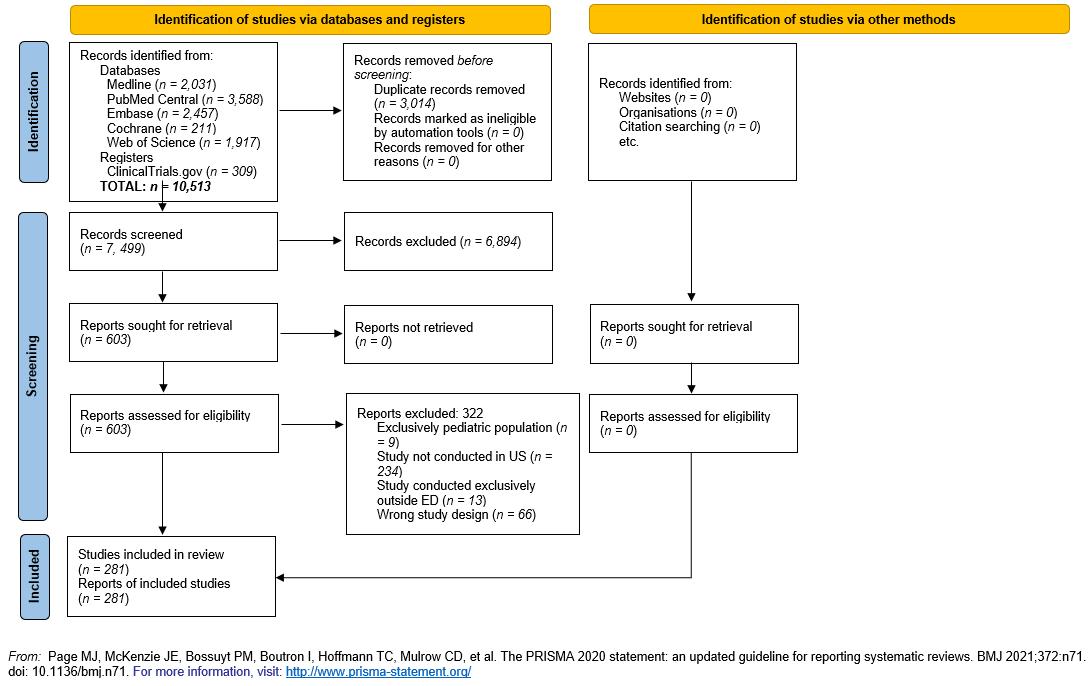
Figure 1. PRISMA* flow diagram demonstrating study evaluation for emergency medicine clinical research examining exclusion by language.
*PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; US, United States; ED, emergency department.
of clinical research, of which 100 (68%) excluded NELP patients, 40 (27%) included NELP patients, and six (4%) did not specify. Of the 107 studies (38%) that included an intervention, 74 (69%) excluded NELP patients, 29 (27%) included NELP patients, and four (4%) did not specify languages recruited. For the 174 non-interventional studies, 89 (51%) excluded NELP patients, 81 (47%) included NELP patients, and four (2%) did not specify.
Of the 268 (95%) studies conducted exclusively in an ED or prehospital setting, 157 (59%) excluded NELP patients, 105 (39%) included NELP patients, and six (2%) did not specify. For the remaining 13 studies conducted in additional clinical settings, six (46%) excluded NELP patients, five (38%) included NELP patients, and two (15%) did not specify. Of the 231 studies (82%) that performed analyses on primary enrollment data, 134 (58%) excluded NELP patients, 89 (39%) included NELP patients, and eight (3%) did not specify. For the 50 (18%) studies that performed secondary analyses on data, 29 (58%) datasets excluded NELP patients and 21 (42%) included NELP patients. Within the 50 (18%) abstract publications, 25 (50%) excluded NELP patients, 23 (46%) included NELP patients, and two (4%) did not specify.
For the remaining 231 (82%) papers published, 138 (60%), excluded NELP patients, 87 (38%) included NELP patients, and six (3%) did not specify. Twenty-four (8%) studies included patients < 18 years of age, of which 14 (58%) excluded NELP patients, nine (38%) included NELP patients, and one (4%) did not specify. Of the 244 (86%) that did not include patients < 18
years of age, 145 (59%) excluded NELP patients, 93 (38%) included NELP patients, and six (2%) did not specify. Thirteen studies did not define what ages were recruited; within this group, four (31%) excluded NELP patients, eight (62%) included NELP patients, and one (8%) did not specify.
DISCUSSION
In this narrative review of prospective ED studies from 2018–2023 that mention language, we found that 163 (58%) studies excluded NELP patients. Among interventional studies, 74 (69%) excluded NELP patients, despite an increasing number of people in the United States who do not speak English.1 Interventional studies often have more stringent regulations regarding consent and follow-up, and interpretation of these well-intended regulations may have the unintended consequence of excluding NELP patients. Translating study materials, performing ethical consent, and creating follow-up infrastructure in a non-English language requires significant funds and time. Researchers should be encouraged to request this funding in grants, and institutions should invest in the infrastructure to support multilingual enrollment. This is particularly important with the increasing diversity of the US population to ensure that data driving important policy changes and practice norms are representative.
Among those studies that focused on heath equity/social emergency medicine, it is still worth noting that 47% excluded NELP patients. For this topic in particular, including NELP
Table 1. Descriptive statistics of extracted studies examining clinical research conducted in the emergency department and prehospital setting.
ED, emergency department; NELP, non-English language preferred; EM, emergency medicine.
patients is imperative given the differential rates of social determinants of health experienced by patients who identify as racial and ethnic minorities in the US.4-6
Additional work is needed to determine how to optimize infrastructure for the ethical inclusion of NELP patients in clinical research. This will likely require a multifaceted effort. Regulatory bodies such as institutional review boards (IRB), grant funders, and journal editors are all key to improving the inclusivity of research studies. The IRBs could encourage studies to include NELP patients and require stringent review of studies with plans to exclude NELP patients. Similarly, journal editors could critically question methods that exclude NELP patients purely for convenience or cost reasons. Institutions could consider separate funds to support the additional steps required to include NELP patients, such as translating study materials and hiring multilingual research staff. Grants could require a section dedicated to explaining how funds from the grant will be used toward the equitable enrollment of NELP patients.
It is important to note we did not review any studies that did not mention language in the abstract or manuscript. Thus, it is possible that these studies excluded NELP patients without explicitly describing this in their paper, which could further exacerbate disparities in enrollment. This underscores the importance of creating a standard that requires
publications to state the languages their participants speak and of reading studies through a critical lens if they exclude NELP patients.
It is an unrealistic expectation for every study to have the capacity to consent and enroll every non-English language. We advocate for a minimum of one non-English language with encouragement and incentive for more. The non-English language(s) included should be reflective of the general population served by the institution.
LIMITATIONS
Although our methods covered a diverse set of search engines and terms, a limitation of this study is the potential for missed studies, including those published prior to 2018 and studies that did not discuss language of participants. However, it is possible that studies that do not discuss language excluded NELP patients from participating without explicitly remarking on this aspect of their enrollment process. Other limitations include the absence of information about reasons for exclusion or other barriers to inclusion (eg, time of enrollment availability), or size of the study (eg, multisite vs single site). Additionally, we were able to perform only descriptive statistics with these data, which limited our ability to draw conclusions regarding associations between characteristics of studies and the exclusion of NELP patients
CONCLUSION
This focused narrative review fills an important gap in the current literature describing the rates of exclusion of nonEnglish language preferred patients in adult ED clinical research. Over half of the studies reviewed excluded NELP patients, with higher rates among interventional studies. It is imperative that interventional studies improve their NELP patient participation to be reflective of the general population. Institutional review boards, grant funders, and journal editors can encourage researchers to prioritize inclusionary practices. Future studies can include more robust statistical analyses that investigate associations between NELP patient research inclusion and study type.
Address for Correspondence: Alexa M. Curt, MD. Massachusetts General Hospital, Department of Emergency Medicine. 125 Nashua Street, Suite 920 Boston, MA, 02114. Email: acurt@mgh. harvard.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Curt et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Dietrich S, Hernandez E. Language Use in the United States: 2019. 2022. Available at: https://www.census.gov/content/dam/Census/ library/publications/2022/acs/acs-50.pdf. Accessed April 27, 2024.
2. Horse AY. 2020 Census miscounted Americans – 4 questions answered. 2022. Available at: http://theconversation.com/2020-
census-miscounted-americans-4-questions-answered-179612. Accessed April 27, 2024.
3. Glickman SW, Ndubuizu A, Weinfurt KP, et al. Perspective: the case for research justice: inclusion of patients with limited English proficiency in clinical research. Acad Med. 2011;86(3):389.
4. John-Baptiste A, Naglie G, Tomlinson G, et al. The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med. 2004;19(3):221-8.
5. Cohen AL, Rivara F, Marcuse EK, et al. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116(3):575-9.
6. Divi C, Koss RG, Schmaltz SP, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care J Int Soc Qual Health Care. 2007;19(2):60-7.
7. Parast L, Mathews M, Martino S, et al. Racial/ethnic differences in emergency department utilization and experience. J Gen Intern Med. 2022;37(1):49-56.
8. Glickman SW, Anstrom KJ, Lin L, et al. Challenges in enrollment of minority, pediatric, and geriatric patients in emergency and acute care clinical research. Ann Emerg Med. 2008;51(6):775-780.e3.
9. Urban Wire. When researchers build trust, “hard-to-reach” undocumented communities aren’t so hard to reach. 2022. Available at: https://www.urban.org/urban-wire/when-researchers-build-trusthard-reach-undocumented-communities-arent-so-hard-reach. Accessed April 27, 2024.
10. Rees CA, Stewart AM, Portillo EN, et al. Reporting of important social determinants of health in pediatric clinical trials. Am J Prev Med. 2023;64(6):918-26.
11. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. 2024 Available at: https://support.clarivate.com/ Endnote/s/article/Citing-the-EndNote-program-as-areference?language=en_US. Accessed April 27, 2024.
12. Schoenfeld EM, Lin MP, Samuels‐Kalow ME. Executive summary of the 2021 SAEM Consensus Conference: From Bedside to Policy: Advancing Social Emergency Medicine and Population Health Through Research, Collaboration, and Education. Acad Emerg Med. 2022;29(3):354-63.
Emergency Medical Services Time on Scene and NonTransport: Role of Communication Barriers
Elina Kurkurina, MPH* Craig Rothenberg, MPH†
Katherine Couturier, MD, MPH†
Amelia Breyre, MD†
David Yang, MD, MHS†
Alexander R. Nelson, MD†
Alexis Cordone, MD, MPH†
Arjun K. Venkatesh, MD, MBA, MHS†‡
Cameron J. Gettel, MD, MHS†‡
Section Editor: Scott Goldstein, DO, EMT-T/P
* † ‡ Quinnipiac University, Frank H. Netter MD School of Medicine, North Haven, Connecticut
Yale University School of Medicine, Department of Emergency Medicine, New Haven, Connecticut
Yale University School of Medicine, Center for Outcomes Research and Evaluation, New Haven, Connecticut
Submission history: Submitted December 16, 2024; Revision received May 3, 2025; Accepted May 14, 2025
Electronically published August 20, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.41212
Introduction: Clear communication is essential for emergency medical services (EMS) clinicians to assess a situation and make appropriate transport decisions. When barriers are present that impede communication between emergency responders and patients, EMS clinicians report difficulty navigating these encounters. As communication barriers potentially delay definitive care, it remains unclear the amount of time that EMS clinicians spend on scene during these encounters and how often they result in non-transport. In this study we sought to characterize the association between the presence of communication barriers, time spent on scene, and non-transport.
Methods: We conducted an observational analysis using 2022 data from the ESO Data Collaborative, a deidentified national prehospital electronic health record dataset. Encounters were restricted to 9-1-1 responses in which the responding ambulance was first on scene, the patient was alive, ≥ 18 year of age, and able to refuse transport. The primary outcomes were time on scene and non-transport. We used logistic regression models to estimate non-transport by communication barrier (including non-English language preference, speech disability, deaf or hard of hearing, and blind or low vision) and control for key patient and encounter characteristics.
Results: Of 3,477,008 EMS responses, 233,084 (6.7%) resulted in non-transport and 99,263 (2.9%) had a communication barrier identified. Among encounters with a communication barrier identified, EMS clinicians spent more time on scene with patients who were not transported (21.0 minutes) compared to patients who were transported for definitive care (15.9 minutes). Compared to those without an identified barrier, encounters with a patient who had a non-English language preference (odds ratio [OR] 0.51, confidence interval [CI] 0.49-0.53, P < .001), patients who had a speech disability (OR 0.36, CI 0.33-0.40, P < .001), were deaf or hard of hearing (OR 0.71, CI 0.66-0.76, P < .001), or were blind or had low vision (OR 0.80, CI 0.69-0.92, P < .001) were less likely to result in non-transport, with non-transport rates of 3.6%, 1.9%, 4.0%, and 4.4% respectively.
Conclusion: Encounters with communication barriers were less likely to end in non-transport. When communication barriers were identified, EMS clinicians spent 32% (5.1 minutes) longer on scene on encounters that resulted in non-transport, showing that EMS clinicians may be dedicating additional time and resources caring for this population. [West J Emerg Med. 2025;26(5)1265–1273.]
I NTRODUCTION
Clear and effective communication between patients and clinicians is an important component of safe, high-quality, and informed medical care.1 Communication barriers are common, affecting millions of adults in the United States. Recent estimates suggest that 67.8 million individuals in the US speak a language other than English at home,2 37.5 million are deaf or hard of hearing,3 three million have a speech disability,4 and six million are blind or have low vision.5 These communication barriers potentially limit individuals’ ability to effectively communicate with emergency medical services (EMS) clinicians during an acute illness or injury and possibly result in delayed or missed diagnoses and treatment.6,7 National estimates project an increase in these conditions and limitations, and current efforts are underway to improve equity and accessibility across multiple healthcare settings to better serve these patients.8-12
Emergency medical services clinicians face numerous challenges when barriers to communication are present, including delayed dispatch and frequent on-scene transport priority changes.13 Qualitatively, EMS clinicians describe these situations in which communication barriers are present as high-stress scenarios, express concern about their ability to accurately assess acuity, and acknowledge increased instances of poor rapport with patients.14 Meanwhile, quantitative assessments of key metrics, such as time on scene, have varied in their findings. Some studies have found that EMS clinicians spend less time on scene with patients who have communication barriers,15,16 potentially indicating a desire to quickly transport patients to a facility equipped to meet their acute illness and communication needs.17 Conversely, other studies found no difference in transport time for patients with communication barriers.18 Despite advancements in EMS practice and the critical role of communication, existing literature offers conflicting and limited insight into how communication barriers impact prehospital care.
Previous studies on communication barriers have focused primarily on language discordance and have been restricted to smaller, regional samples, leaving significant gaps in our understanding of the broader implications of these barriers on EMS operations and patient outcomes. Given the uncertainty in encounters where patients have communication barriers, investigation of on-scene times and non-transport rates is critically important to address potential areas for improvement and/or inequities, especially for less frequently discussed communication barriers such as patients who are deaf or hard of hearing, have speech disabilities, and are blind or have low vision. Excess time on scene and non-transport may delay time-sensitive care,19,20 especially if the acuity was not properly conveyed,14 while simultaneously limiting the unit’s ability to respond to other calls, which can lead to further delays given EMS staffing shortages21 and the closure of EMS agencies. To better understand the influence
Population Health Research Capsule
What do we already know about this issue? Communication barriers in Emergency Medical Services (EMS) encounters may complicate care and delay necessary transport, but time impacts and outcomes are unclear for less frequently studied barriers.
What was the research question?
What is the impact of communication barriers on EMS on-scene time and nontransport rates?
What was the major finding of the study? EMS encounters with communication barriers resulted in 5.1 minutes longer on-scene times for non-transported patients and had lower odds of non-transport (OR 0.51, CI 0.49-0.5).
How does this improve population health? Identifying encounters with communication barriers helps EMS clinicians allocate time, training, and resources appropriately.
of communication barriers on EMS operations, we used a nationally representative dataset to characterize the association between four common communication barriers (non-English language preference, speech disability, deaf or hard of hearing, and blind or low vision), time on scene, and non-transport.
METHODS
Study Design and Data Source
We conducted an observational analysis using data from the ESO Data Collaborative. Used previously in numerous prehospital evaluations,22-25 the ESO Data Collaborative is a national, deidentified, prehospital electronic health record dataset in which participating agencies voluntarily submit data for research and benchmarking purposes. The dataset is compliant with National EMS Information System 3.4 standards, and captures dispatch-, demographic-, and encounter-specific variables.26 For the 2022 year of analysis, the dataset included 12,803,154 records from 2,705 participating agencies. The study was deemed exempt from review by the Yale University Institutional Review Board.
Study Population
All 9-1-1 responses between January 1–December 31,
2022, in which the responding ambulance was first on scene and the patient was alive were included. We excluded records where the disposition was “dead on scene,” the primary impression was “obvious death,” or the location type was “morgue.” As the range of disability varies, we also excluded patients who may be deemed unable to refuse care, including those who had a developmental or psychological disability, were unconscious, or had an Alert, Voice, Pain, Unresponsiveness (AVPU) scale score of 1, indicating they were unresponsive. Similarly, patients < 18 years of age were excluded as their ability to consent to care independent of a guardian varies by age, state, and condition. We also excluded records with covariates that could influence time on scene or non-transport such as sex, race, ethnicity, agency, location, chief complaint, level of service, and medical/ trauma designation data.
Data Management
To capture similar response categories, we collapsed responses for three variables: disposition; level of service; and encounter location. Dispositions were classified into mutually exclusive categories of treatment on scene, transport, and non-transport based on the patient’s status at the end of the encounter. We excluded encounters with dispositions not collapsible within these three categories (Figure 1). For the level of service variable, we reclassified discrepancies between the “level of care” and “level of service” variables by selecting the lower of the two options to account for the training level of the crew or available resources on the ambulance. For example, if the level of care was categorized as Advanced Life Support (ALS) and the level of service was categorized as Basic Life Support (BLS), the final determination was BLS given that was the highest level at which the crew could perform. Location was reclassified into home or residence, medical (for encounters where the location was a medical setting), and public (for encounters that occurred in publicly accessible areas).
Classification tables for the disposition, level of service, and encounter location are available in the Supplemental Appendix.
Outcome Measures and Covariates
The primary outcomes of interest were time on scene and non-transport. We defined time on scene as the interval between “at patient time” and “depart scene time” data fields, rounded to the nearest minute. We excluded records that did not have a valid time interval, defined as < 0 minutes or > 240 minutes, as these calls were more likely to be atypical, complex, or multi-patient responses.
Independent variables of interest included time-on-scene intervals, age, sex, race/ethnicity, level of service, location type, agency type, type of encounter, chief complaint system, and communication barriers. To account for extreme values, we winsorized age at the 99th percentile, effectively capping
12,803,154
11,082,190 9-1-1 calls
9,753,410
2,354,061
Figure 1. Analytic sample flow diagram in a study of EMS onscene time with patient/paramedic communication barriers.
age at 95 years. For race and ethnicity calculations, an “or” statement was used to classify patients as Hispanic or Latino if the race or ethnicity variables were marked as such, consistent with prior ESO literature approaches.22 Those with communication barriers were inclusive of encounters in which a “language barrier,” “hearing impairment,” “speech impairment,” or “vision impairment” were identified and documented by the responding EMS clinician. It is important to note that the language used surrounding communication barriers in the ESO dataset may not necessarily reflect the language that patients and first responders may use. For example, the dataset uses the term “hearing impairment.” While some people with hearing loss may use this term, it does not necessarily reflect the language that may be used by those who are deaf or hard of hearing, and may be found offensive by others.27 Although these were the terms used in the dataset, we refer to these conditions using more culturally appropriate language.
Statistical Analysis
We calculated descriptive statistics at the patient and encounter level. The mean time on scene and standard deviation were then calculated for encounters with and without documented communication barriers. Mean was
chosen over median given the normal distribution of the time on scene data. We used logistic regression models to characterize the relationship between communication barriers and non-transport, adjusting for the aforementioned covariates. Race, agency type, and chief complaint system were treated as binary variables and were compared to not having the variable documented. For example, a biracial patient who had two races documented would be captured within each of the indicated races. All analyses were completed using R v4.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
The analytic sample consisted of 3,477,008 encounters
(Table 1). Most responses were medical (80.6%) compared to trauma (16.6%), at the ALS level (72.1%) compared to BLS (27.9%), and to a patient’s home or residence (64.2%) compared to medical (15.4%) or public (20.4%) locations. The sample was predominantly female (53.5%) and White (71.7%), and the mean age (SD) was 60.2 (20.6). Of the > 3 million encounters, 57,117 (1.6%) were patients with an identified non-English language preference, 20,311 (0.6%) had an identified speech disability, 21,025 (0.6%) were deaf or hard of hearing, and 4,701 (0.1%) were blind or had low vision.
Time on Scene
Prior to transport, EMS clinicians spent a mean (SD) of
Table 1. Sample characteristics by communication barrier, N (%) in a study of EMS on-scene time with patient/paramedic communication barriers.
ALS, Advanced Life Support; BLS, Basic Life Support.
15.9 (8.1) minutes of on-scene time with patients who had communication barriers compared to 14.9 (8.2) minutes with patients who had no communication barriers. Time on scene varied by communication barrier (Figure 2). More specifically, EMS clinicians spent a mean of 15.1 (7.9) minutes with patients who had a non-English language preference, 16.0 (7.9) minutes with patients who had speech disabilities, 17.7 (8.6) minutes with patients who were deaf or hard of hearing, and 16.9 (8.3) minutes with patients who were blind or had low vision.
Among all encounters, EMS clinicians spent more time on scene caring for patients who were not transported compared to those who were transported. When a communication barrier was present, EMS clinicians spent a mean of 21.0 (13.7) minutes on scene with patients who were not transported compared to 15.9 (8.1) minutes with patients who were transported for definitive care (P < .001). More specifically, EMS clinicians spent 20.7 (13.8) minutes with patients who had documented non-English language preference, 21.7 (13.6) minutes with patients who had documented speech disabilities, 21.5 (14.1) minutes with patients who were deaf or hard of hearing, and 21.7 (11.4) minutes with patients who were blind or had low vision. These differences were statistically significant (P < .001).
Non-Transport
A total of 233,084 (6.7%) encounters resulted in nontransport. More specifically, 2,048/57,117 (3.6%) encounters with a documented non-English language preference, 384/20,311 (1.9%) encounters with a documented speech disability, 843/21,025 (4.0%) encounters with a patient who was deaf or hard of hearing, and 205/4,701 (4.4%) encounters with a patient who was blind or had low vision ended in non-transport. Additionally, patients with communication barriers, including non-English language preference (odds
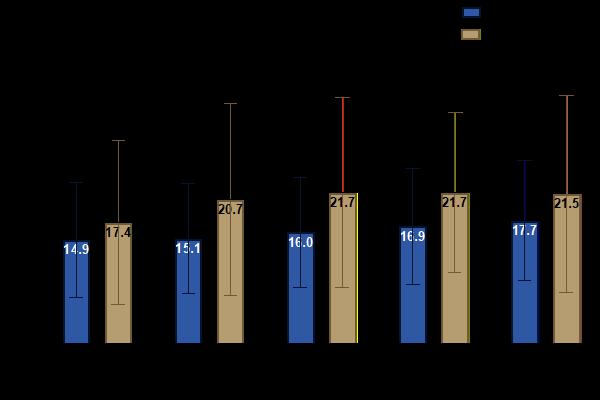
ratio [OR] 0.51, confidence interval [CI] 0.49-0.53, P < .001), speech disabilities (OR 0.36, CI 0.33-0.40, P < .001), who were deaf or hard of hearing (OR 0.71, CI 0.66-0.76, P < .001), or were blind or had low vision (OR 0.80, CI 0.69-0.92, P < .001) were less likely to have the encounter end in non-transport (Figure 3).
DISCUSSION
In this analysis of > 3 million EMS records, we identified four major findings. First, in a nationally representative sample, approximately 3% of prehospital encounters had evidence of a communication barrier. Second, prior to transport, average on-scene time was approximately 7% greater for encounters with a documented communication barrier compared to those without a communication barrier. Third, when communication barriers were present, EMS clinicians spent approximately 32% more time on encounters that ended in non-transport compared to encounters where the patient was transported for definitive care. Fourth, encounters with identified communication barriers were less likely to result in non-transport. These findings provide important and actionable information for EMS leaders, agencies, and policymakers.
Compared to national estimates,2-5 the prevalence of communication barriers among prehospital encounters was low. There are several possible explanations for this finding. If a communication barrier is mild, it may be under-reported by the patient or undocumented by the clinician, especially if the EMS clinician can navigate around the barrier by implementing other communication strategies and techniques. Since the degree of impact on communication is not defined for it to be reported, each clinician must use individual judgment regarding the magnitude of a barrier that warrants documentation. The low prevalence of communication barriers in this sample may also be reflective of larger barriers faced by this population. Patients with communication barriers have reported hesitancy and uncertainty about contacting 9-1-1, difficulty communicating with dispatchers, and trouble understanding instructions issued by dispatchers,6,7,14 all of which can lead to lower engagement with EMS. With an aging and increasingly more diverse national population, it is likely that the prevalence of these communication barriers and, therefore, the relevance of these findings will increase.
Emergency medical services clinicians spend more time on scene with patients who have communication barriers and are more likely to transport them for definitive care. Agencies that receive federal funds are required to evaluate the need for language services and implement solutions accordingly.28 Patients might benefit from EMS clinicians being equipped with training and resources to improve and expedite care. Multiple strategies may be deployed in the prehospital setting to overcome communication barriers that address ambulance design and
Kurkurina et al.
Figure 2. Time spent on scene by emergency medical service responders by documented communication barrier.
Characteristics
Time on Scene
Male Sex (vs Female) Age
Race and Ethnicity (vs Not Selected)
Black or African American White
Hispanic or Latino
American Indian or Alaskan Native Asian
Hawaii Native or Other Pacific Islander
Level of Service
Location ALS (vs BLS)
Medical (vs Residence)
Public (vs Residence)
Agency Type (vs Not Selected)
Non-Profit/Community
Non-Fire Government Fire Department
Non-Hospital Private
Type of Encounter Tribal
Medical (vs Trauma)
Medical and Trauma (vs Trauma)
Chief Complaint System (vs Not Selected)
Reproductive
Skin or Musculoskeletal Pulmonary Renal
Lymphatic or Immune
Gastrointestinal
Endocrine or Metabolic
Central Nervous System or Neurologic
Behavioral or Psychiatric Cardiovascular
Communication Barriers
Non-English Language Preference (vs English Preference)
Speech Disability (vs None)
Deaf or Hard of Hearing (vs None)
Blind or Low Vision (vs None)
Less likely to have an encounter end in nontransport
Odds Ratio
More likely to have an encounter end in nontransport
Figure 3. Associations between non-transport and encounter and patient-level characteristics Table 1. Sample characteristics by communication barrier, N (%) in a study of EMS on-scene time with patient/paramedic communication barriers. OR, odds ratio; CI, confidence interval; ALS, Advanced Life Support; BLS, Basic Life Support.
clinician practices. Regarding system-level changes to ambulance design, ambulances could be engineered to reduce background noise in patient care areas and incorporate assistive listening devices, magnifiers, and mobile interpreting software. The EMS clinicians can also employ individual practice strategies to improve communication, including minimizing disruptions such as background noise, using hearing amplifiers/assistive listening devices, moving to well-lit areas, writing down or
drawing instructions for patients, learning basic instructions and maintaining refusal forms in commonly spoken languages, verbalizing actions to patients with decreased visual acuity, and incorporating available family members to advise the crew regarding accommodation strategies.
Training programs in EMS have developed workshops aimed at improving communication with patients who have disabilities impacting speech or are hard of hearing.29 Similarly, other programs have piloted resources such as
communication boards to target patients who are hard of hearing or speak another language.30 When interacting with patients with a non-English language preference, EMS clinicians report preferring ad hoc interpreters, such as bystanders or children, and translation apps over formal telephonic interpretation due to difficulties accessing timely telephonic interpretation.14 However, this may be problematic as family members, friends, and especially minor children are prone to omissions, additions, and substitutions.31,32 Given the preference for on-scene interpretation, EMS agencies may reduce on-scene time of encounters by recruiting and training bilingual staff. These measures can help reduce the time on scene and ensure that patients with communication barriers receive appropriate and timely care.
Responders spend more time on scene with patients who ultimately refuse transport compared to those who are transported for definitive care. Proper patient education and adherence to documentation may explain the increased time on scene for this patient population. The EMS clinicians may take more time to appropriately ensure the patient is competent to decline further care, understands the implications of their decision, and signs appropriate documentation. Depending on the population call density and geography, five additional minutes (32% more) of on-scene time may have an impact on overall system productivity and unit hour use. As EMS systems strive to care for more complex patient populations, integrating specific communication training programs and assistive tools, such as hearing amplifiers and multilingual support systems, may alleviate some prehospital care challenges.
Our analyses also identified that encounters with documented communication barriers were less likely to result in non-transport. Many EMS protocols consider the presence of communication barriers as high-risk refusals, and EMS clinicians may be more apt to strongly recommend or be required by protocol to transport.33 There may also be contributory social and cultural factors (eg, patients with a non-English language preference may feel less comfortable refusing care or may have difficulty conveying refusal). In addition, there may be scenarios in which patients with disabilities that impact vision, speech, or hearing, may present a challenge for EMS clinicians to assess whether they have the capacity to refuse care as some presentations may overlap with emergent presentations of illness. Understanding that communication barriers lead to fewer non-transport instances can inform EMS protocols and encourage the development of standardized approaches to manage high-risk refusals effectively.
Central to this research question, EMS practice often varies based on clinical condition and setting that dictates whether shorter or longer on-scene times are more beneficial to patient outcomes.6 Research assessing the safety of non-transport has evolved over the years with studies
focusing on and finding mixed results for paramedic-initiated non-transport.34-37 The success of these encounters and decisions remains contingent on clear communication between patients and EMS clinicians. Unique challenges may persist for patients with communication barriers in this changing landscape. Future research should examine whether on-scene time impacts outcomes for patients with communication barriers. Additionally, research should explore outcomes following non-transport for patients with communication barriers. As EMS agencies move away from operational metrics, such as response times, to performance measures focusing on the administration of appropriate treatment in a timely manner, more research is needed to determine whether disparities exist for patients with communication barriers.38
LIMITATIONS
The ESO Data Collaborative is a retrospective database with several limitations. Communication barriers were documented as a binary variable in the dataset. Therefore, we were unable to describe the degree of impact of the disability or the fluency with which the patient or EMS responder spoke a common language. It is also unclear whether the identified disability was perceived by the EMS clinician or disclosed by the patient during the encounter, and causation cannot be ultimately inferred as this was an observational study. However, if it is likely that communication barriers with minimal impact were less likely to be reported, then it is possible that the prevalence estimates calculated are underestimates of the true prevalence, thereby further reinforcing the importance of this issue for EMS clinicians. Although over 2,000 EMS agencies submit data for research and benchmarking purposes, the ESO database does not capture all national EMS encounters. The voluntary nature of submission may restrict generalizability as EMS agencies in urban areas or urban clusters have previously been shown to be more likely to submit their data.39 Lastly, there may be regional variation in protocols that dictate treatment and transportation decision-making (such as a requirement to contact medical control for high-risk refusals) that could not be captured from this dataset.
CONCLUSION
In this nationally representative prehospital analysis, approximately 1 in 30 encounters had evidence of a barrier to communication. Encounters impacted by communication barriers were associated with a longer average time on scene compared to encounters without communication barriers. Encounters associated with communication barriers were less likely to result in non-transport. Emergency medical services clinicians may benefit from being equipped with training and resources to communicate effectively with these vulnerable populations and anticipate longer on-scene time to provide appropriate care.
Address for Correspondence: Elina Kurkurina, MPH, Frank H. Netter MD School of Medicine at Quinnipiac University, 370 Bassett Rd, North Haven, CT 06437. Email: Elina.kurkurina@ quinnipiac.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Drs. Venkatesh, Gettel and Breyre report receiving support from the Centers for Medicare & Medicaid Services to develop quality measures for ambulance service responders. Dr. Gettel is supported by the National Institute on Aging of the National Institutes of Health (R03AG073988) and the American Board of Emergency Medicine fellowship through the National Academy of Medicine of the National Academy of Sciences (SCON-10000824). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation or approval of the manuscript.
Copyright: © 2025 Kurkurina et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Ratna H. The importance of effective communication in healthcare practice. Harv Public Health Rev. 2019;23:1-6.
2. Dietrich S, Hernandez E. Language use in the United States: 2019. 2022. Available at: https://www.census.gov/library/publications/2022/ acs/acs-50.html. Accessed May 17, 2025.
3. National Institute on Deafness and Other Communication Disorders. Quick Statistics About Hearing, Balance, & Dizziness. 2021. Available at: https://www.nidcd.nih.gov/health/statistics/quick-statistics-hearing. Accessed May 17, 2025.
4. National Institute on Deafness and Other Communication Disorders. Quick Statistics About Voice, Speech, Language. 2016. Available at: https://www.nidcd.nih.gov/health/statistics/quick-statistics-voicespeech-language. Accessed May 17, 2025.
5. Flaxman AD, Wittenborn JS, Robalik T, et al. Prevalence of visual acuity loss or blindness in the US: a Bayesian meta-analysis. JAMA Ophthalmol. 2021;139(7):717-23.
6. Tate RC. The need for more prehospital research on language barriers: a narrative review. West J Emerg Med. 2015;16(7):1094-105.
7. James TG, Sullivan MK, McKee MM, et al. Emergency department patient-centred care perspectives from deaf and hard-of-hearing patients. Health Expect. 2023;26(6):2374-86.
8. Haile LM, Kamenov K, Briant PS, et al. Hearing loss prevalence and years lived with disability, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet. 2021;397(10278):996-1009.
9. Varma R, Vajaranant TS, Burkemper B, et al. Visual impairment and blindness in adults in the United States: demographic and geographic variations from 2015 to 2050. JAMA Ophthalmol. 2016;134(7):802-9.
10. Martinez EM, Carr DT, Mullan PC, et al. Improving equity of care for patients with limited English proficiency using quality improvement
methodology. Pediatr Qual Saf. 2021;6(6):e486.
11. Ramirez N, Shi K, Yabroff KR, et al. Access to care among adults with limited English proficiency. J Gen Intern Med. 2023;38(3):592-9.
12. Department of Health and Human Services. Improving communication access for individuals who are blind or have low vision. In: Centers for Medicare & Medicaid Services, ed.2023. Available at: https://www.cms. gov/files/document/omh-visual-sensory-disabilities-brochure-508c.pdf. Accessed May 17, 2025.
13. Meischke HW, Calhoun RE, Yip MP, et al. The effect of language barriers on dispatching EMS response. Prehosp Emerg Care 2013;17(4):475-80.
14. Stadeli KM, Sonett D, Conrick KM, et al. Perceptions of prehospital care for patients with limited English proficiency among emergency medical technicians and paramedics. JAMA Netw Open 2023;6(1):e2253364-e2253364.
15. Grow RW, Sztajnkrycer MD, Moore BR. Language barriers as a reported cause of prehospital care delay in Minnesota. Prehosp Emerg Care. 2008;12(1):76-9.
16. Sterling MR, Echeverria SE, Merlin MA. The effect of language congruency on the out-of-hospital management of chest pain. World Med Health Policy. 2013;5(2):111-23.
17. American College of Emergency Physicians. Use of Medical Interpreters in the Emergency Department. 2022. Available at: https:// www.acep.org/patient-care/policy-statements. Accessed May 17, 2025.
18. Weiss NR, Weiss SJ, Tate R, et al. Language disparities in patients transported by emergency medical services. Am J Emerg Med. 2015;33(12):1737-41.
19. Pringle RP, Jr., Carden DL, Xiao F, et al. Outcomes of patients not transported after calling 911. J Emerg Med. 2005;28(4):449-54.
20. Vilke GM, Sardar W, Fisher R, et al. Follow-up of elderly patients who refuse transport after accessing 9-1-1. Prehosp Emerg Care. 2002;6(4):391-5.
21. American Ambulance Association. AAA/Newton 360 2021 Ambulance Industry Employee Turnover Study. 2021. Available at: https:// ambulance.org/wp-content/uploads/2021/07/2021-AAA-EMSTurnover-Study.pdf. Accessed May 17, 2025.
22. Crowe RP, Kennel J, Fernandez AR, et al. Racial, ethnic, and socioeconomic disparities in out-of-hospital pain management for patients with long bone fractures. Ann Emerg Med. 2023;82(5):535-45.
23. Niederberger SM, Crowe RP, Salcido DD, et al. Sodium bicarbonate administration is associated with improved survival in asystolic and PEA out-of-hospital cardiac arrest. Resuscitation. 2023;182:109641.
24. Breyre A, Crowe RP, Fernandez AR, et al. Emergency medical services clinicians in the United States are increasingly exposed to death. J Am Coll Emerg Physicians Open. 2023;4(1):e12904.
25. Aceves A, Crowe RP, Zaidi HQ, et al. Disparities in prehospital non-traumatic pain management. Prehosp Emerg Care 2023;27(6):794-9.
26. National Emergency Medical Services Information System (NEMSIS) NEMSIS - Using EMS Data. 2025.Available at: https://nemsis.org/. Accessed May 17, 2025.
27. National Association of the Deaf. Community and Culture — Frequently Asked Questions. 2025. Available at: https://www.nad.org/ resources/american-sign-language/community-and-culture-frequentlyasked-questions/. Accessed May 17, 2025.
28. US Department of Justice. Executive Order 13166: Improving Access to Services for Persons with Limited English Proficiency. 2000. Available at: https://www.federalregister.gov/ documents/2000/08/16/00-20938/improving-access-to-services-forpersons-with-limited-english-proficiency. Accessed May 17, 2025.
29. Rotoli JM, Hancock S, Park C, et al. Emergency medical services communication barriers and the deaf American Sign Language user. Prehosp Emerg Care. 2022;26(3):437-45.
30. Eadie K, Carlyon MJ, Stephens J, et al. Communicating in the pre-hospital emergency environment. Aust Health Rev 2013;37(2):140-6.
31. Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111(1):6-14.
32. Tate RC, Hodkinson PW, Meehan-Coussee K, et al. Strategies used by prehospital providers to overcome language barriers. Prehosp Emerg Care. 2016;20(3):404-14.
33. Connecticut Department of Public Health. Connecticut Statewide Emergency Medical Services Protocols. 6.12 Refusal of Care2020. 2024. Available at:https://portal.ct.gov/dph/emergency-medicalservices/ems/statewide-ems-protocols. Accessed May 17, 2025.
34. Fraess-Phillips AJ. Can paramedics safely refuse transport of non-urgent patients? Prehosp Disaster Med. 2016;31(6):667-74.
35. Knapp BJ, Kerns BL, Riley I, et al. EMS-initiated refusal of transport: the current state of affairs. J Emerg Med. 2009;36(2):157-61.
36. Marsan RJ Jr, Shofer FS, Hollander JE, et al. Outcome of travelers who refuse transport after emergency medical services evaluation at an international airport. Prehosp Emerg Care. 2005;9(4):434-8.
37. Millin MG, Brown LH, Schwartz B. EMS provider determinations of necessity for transport and reimbursement for EMS response, medical care, and transport: combined resource document for the National Association of EMS Physicians position statements. Prehosp Emerg Care 2011;15(4):562-9.
38. Redlener M, Buckler DG, Sondheim SE, et al. A national assessment of EMS performance at the response and agency level. Prehosp Emerg Care 2024:1-8.
39. ESO Data Collaborative. Data and Reseach. (https://www.eso.com/ data-and-research/). Accessed May 17, 2025.
Physician Attitudes on Integration of Prehospital Patient Care Report into Hospital Electronic Health Record
Maren Smith, BS*
Caroline Given, BSN, RN*
Soheil Saadat, MD, PhD‡
Kenneth Leung, MD†
Julia Afrasiabi, MSN, RN‡
Robert Katzer, MD, MBA‡
University of California, Irvine School of Medicine, Irvine, California
University of California, Irvine Medical Center, Department of Internal Medicine, Orange, California
University of California, Irvine Medical Center, Department of Emergency Medicine, Orange, California
Section Editor: Shira A. Schlesinger, MD, MPH
Submission history: Submitted December 29, 2024; Revision received May 8, 2025; Accepted May 30, 2025
Electronically published September 2, 2025
Full text available through open access at http://escholarship.org uc/uciem_westjem DOI: 10.5811/westjem.41540
Introduction: Prehospital information is valuable but often under-used by physicians. In both the emergency and inpatient settings, information about a patient’s condition prior to their arrival is important to provide optimal care. Historically, prehospital responders’ electronic patient care reports (ePCR) have not been integrated with the hospital’s electronic health record (EHR). In this study, we aimed to assess physician attitudes towards the ePCR and patient care decisions before and after integration of prehospital ePCR and hospital EHR systems. We hypothesized that this would increase accessibility and use of prehospital ePCR in patient care decisions.
Methods: In 2023, our local academic health center implemented software that made prehospital documentation available to hospital staff within 30 minutes of patient arrival to the emergency department (ED). Before this, we surveyed attendings, fellows, and residents from both the ED and internal medicine (IM) department on their attitudes and behaviors regarding ePCR and clinical practice. We administered the same survey six months after implementation, and compared responses with a Wilcoxon signed-rank test.
Results: Sixty-six physicians responded to the pre survey, including 39 (59.1%) from the ED and 27 (40.9%) from the IM department. Fifty-two completed the post survey, including 33 (63.5%) emergency physicians and 19 (36.5%) IM physicians. The pre- survey response rates were 92.9% and 54% for the ED and IM groups, respectively, while the post-survey response rates were 84.6% and 70.4%. Change in rank was significant (P < .01) for the following categories: knowledge;, ability; ease of use; time to access; and frequency of accessing the ePCR. Change in rank was not significant for the importance of ePCR in patient care and medical decision-making, and whether the ePCR would be used more frequently if it were easier to access.
Conclusion: Pre- and post-survey responses regarding accessibility showed a significant change in rank, while the importance of the ePCR on clinical decision-making did not. This suggests that while system integration increased accessibility to prehospital information, it did not significantly alter patient care decision-making. [West J Emerg Med. 2025;26(5)1274–1279.]
INTRODUCTION
Structural challenges to efficient handovers between prehospital emergency medical service (EMS) responders and physicians in the emergency department (ED) are welldocumented in the literature. Multifactorial barriers, including time limitations, high-acuity environment, and participation of multidisciplinary healthcare workers, have been noted in prior research.1-3 These challenges existed prior to the adoption of hospital electronic health records (EHR) and prehospital electronic patient care reports (ePCR). In fact, studies have
demonstrated these challenges regardless of whether handover between EMS responders and physicians consists of verbal, electronic, or hardcopy communication tools.2, 4, 5
In 2015, legislation was passed in California requiring 9-1-1 prehospital responders to chart electronically. The ePCR allows EMS professionals to document demographics, vitals, assessment data, and any interventions performed en route to the hospital. This information ultimately generates a patient record that is digitally accessible to the receiving hospital.6 However, multiple studies have shown how this process is disrupted at the point of patient transfer, specifically when the ePCR must be downloaded, printed, and uploaded into the hospital EHR during patient registration.4, 7-9 This process obstructs efficient access by clinicians to the ePCR and encourages reliance on verbal handover or hardcopy printouts, leading to inconsistent, delayed, or omitted information sharing.4, 5, 10
In June 2023, our local academic health center adopted a new software that directly integrated the prehospital ePCR into the receiving hospital’s EHR, consequently forgoing this time-consuming clerical step. Although previous studies evaluating clinician attitudes toward the ePCR suggest that they would be more likely to use ePCR information if it were readily available,7, 11 there is little evidence to support this conclusion. Evidence is also sparse on clinician attitudes, their use of ePCR, and ePCR influence on patient care decisionmaking in response to ePCR/EHR integration. We sought to assess clinician attitudes toward ePCR accessibility and its role in patient care decision-making before and after ePCR/ EHR integration. We hypothesized that this integration would increase accessibility and thus use of ePCR in patient care decision-making by in-hospital physicians.
METHODS
Study Setting and Population
We conducted a prospective, cohort, web-based survey of emergency physicians and IM physicians regarding use and accessibility of prehospital records; we collected and managed study data using Research Electronic Data Capture (REDCap) tools hosted at the University of California Irvine. This survey was administered before and six months after the ePCR/ EHR integration. We established a protocol and developed a 15-question survey in which responses were ordered on a five-point Likert scale. Questions 1-2, 4-8, 10, and 13 gauged ePCR accessibility. The third question assessed how often clinicians received a direct verbal handoff from prehospital responders. Questions 9, 11, and 12 surveyed importance of ePCR to patient care. Questions 14 and 15 asked participants to identify their clinical role (resident, fellow, or attending) and department (ED or IM). Our institutional review board reviewed the protocol and granted self-exemption.
In June 2023, software that integrated prehospital ePCR and the hospital EHR went live. In May 2023, an invitation to complete the pre-software integration survey was sent to
Population Health Research Capsule
What do we already know about this issue? Prior studies suggest clinicians would be more likely to use information from prehospital electronic patient care reports (ePCR) if it were available.
What was the research question? Does integration of prehospital patient charts with in-hospital health records affect clinician decision-making?
What was the major finding of the study? There was no significant change in rank regarding importance of ePCR accessibility to patient care delivery.
How does this improve population health? Our findings indicate that emergency medical services-to-emerency department information transfer is ineffective and suggests that electronic integration is a potential topic of research and solution.
the emergency and internal medicine departments to assess pre-integration attitudes on ePCR accessibility and utilization. A period of six months was arbitrarily chosen to conduct the post survey. We considered this to be ample time for physicians to alter, if at all, their workflow. Participation was voluntary, and all participants were employed as residents, fellows, or attending physicians in the ED or IM department. Survey reminders were automatically sent out to those who did not complete the survey weekly for three weeks. To incentivize participation, all who completed the survey were automatically entered into a raffle to win one of five $20 gift cards.
Six months later, in November 2023, an invitation to complete the post-software integration survey was sent to all who had completed the pre-integration survey. Similarly to the pre-survey, reminders were automatically sent weekly for three weeks to those who had not completed the survey. Additionally, all who completed the survey were automatically entered into a raffle to win one of five $20 gift cards.
Statistical Analysis
Data are presented as count (percentage). By using a paired analysis approach, we compared respondents’ answers in the post-intervention survey to their pre-intervention survey answers. The changes are reported as negative ranks, positive ranks, and ties. The Wilcoxon signed-rank test was used to
examine whether the change was statistically significant. Type I error was set to 5%. Following data collection, we performed data analysis using SPSS Statistics for Windows v28.0 (IBM Corp, Armonk, NY). We compared pre- and post-survey responses with a Wilcoxon signed-ranked test.
RESULTS
Pre-intervention Survey
Sixty-six respondents, consisting of 35 (53.0%) residents, four (6.1%) fellows, and 27 (40.9%) attendings from the ED and IM department completed the preintervention survey (Table 1). The pre-survey response rates were 92.9% and 54%, respectively. Fifty-eight (87.9%) agreed or strongly agreed that having access to the ePCR is important for patient care in the ED or after admission. At the same time, 47 (71.2%) reported that physicians in their department have access to the written ePCR only 0-20% of the time (Figure 1).
Twenty-six (39.4%) respondents reported that 80% of the time physicians do not receive direct verbal report from an emergency medical technician (EMT) or paramedic. At the same time, 47 (71%) reported that if the physician did not receive a direct verbal report from the EMT or paramedic, they would only access the written ePCR 20% of the time; 47 (71.2%) were unaware that physicians could access the written ePCR; and 23 (34.8%) believed that accessing the written ePCR would take > 30 minutes. On the other hand, 62 respondents (93.9%) agreed that physicians would read the written ePCR more frequently, if it were easier to access.
Post-intervention Survey
A total of 52 respondents returned the post-intervention survey (Table 1). The post-survey response rates were 84.6% and 70.4% for EM and IM groups, respectively. Nine had a change in their clinical role compared to the pre-intervention period.
Table 2 shows the statistically significant change in respondents’ answers from the pre- to post-intervention period. We did not observe a statistically significant change in respondents’ answers from the pre- to post-intervention period with regard to the following survey items: 1) How often are physicians able to access the written ePCR and/ or receive verbal report from the EMT or paramedic before they examine the patient? (P = .05); 2) Is having access to the written ePCR important for patient care in the ED and/or during hospitalization (P = .53); and 3) Would physicians read the written ePCR more frequently if it was easier to access (P = .59); 4) Over the past three months, how often did you make important patient treatment decisions based on verbal report from EMT or paramedic (P = .12); and 5) Over the past three months, how often did you make important patient treatment decisions based on the written ePCR (P = .24).
When stratifying the results based on department, there was no significant change in ranking regarding attitudes toward the importance of ePCR accessibility to patient treatment decisions in either the EM or IM groups. Similarly, when stratifying the results based on role, there was no significant change in rank regarding importance of ePCR accessibility to patient care delivery in either the resident or attending groups.
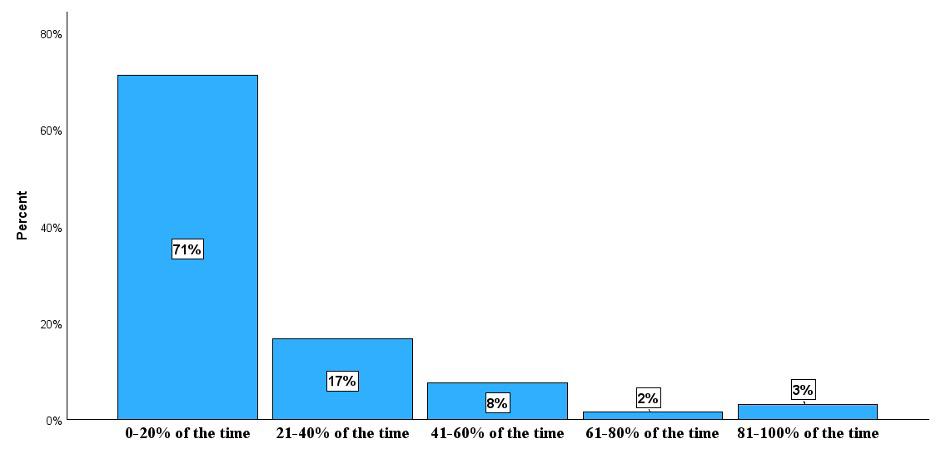
Figure 1. Responses of clinicians regarding their access to patient care summaries written by first responders prior to integration of prehospital and receiving hospital health records systems. ED, emergency department. Overall, how often do physicians in your department access the written prehospital care report to care for a patient who has presented to the ED via ambulance?
Katzer et al. Integration of Prehospital Patent Care Report into Electronic Health Record
Table 1. Clinical roles of participants in pre- and post-intervention surveys regarding use of prehospital patient data.
*Nine respondents in the post-intervention survey had changed their clinical roles since completing the pre-intervention survey
Table 2. The change in respondents’ answers from the pre- to post-intervention period regarding access to first responders’ patient care reports.
Physicians know how to access the written ePCR for a patient presented ED via ambulance.
ePCR.
If physicians do not receive direct verbal report from the EMT bringing the patient, it is easy for them to access written ePCR.
If physicians do not receive a direct verbal report from the EMT bringing the patient, how often do they access the written ePCR?
How long does it take physicians access the written ePCR for a patient brought via ambulance?
How often do physicians access the written ePCR to care for a patient who is brought via ambulance?
If you did not receive direct verbal report from the EMT, it is easy to determine whether the patient presented to the ED via ambulance.
*Only statistically significant changes in rank are included. ePCR, electronic patient care report; ED, emergency department; EMT, emergency medical technician.
DISCUSSION
This study looked at whether implementing an electronic interface between prehospital ePCR and the receiving hospital
EHR affected physician perspectives on access to the ePCR. Additionally, we assessed perceived differences in patient treatment decisions in response to ePCR/EHR integration. This
integration resulted in both a more consistent understanding of how to access the ePCR as well as increased use of the ePCR. Previously, research identified that valuable information is lost during the EMS to ED handoff process.3 In systems that transitioned from handwritten PCRs to ePCRS, paramedics indicated that they often still feel the need to provide additional information at the time of verbal handoff. 11 Furthermore, prior studies have demonstrated that physicians prefer ePCRs over handwritten PCRs for reasons of legibility and accuracy. Of note, the printed version of that ePCR was usually not available at the time of physician patient assessment.7,10 One study identified the processes that contributed to a system’s failure to make the printed version of the ePCR available to physicians. Challenges included coordination of both the external processes of paramedics completing the ePCR, the ePCR being faxed to the ED, and the manual internal process of the unit clerk retrieving the faxed report and placing it in the patient record.8 A study evaluating the challenges to effective EMS to ED patient care handoffs identified harnessing technology as one way to close the gaps in this information exchange.5 We believe that the direct automatic integration of the ePCR into the receiving hospital’s EHR uses technology to address many of the identified shortcomings of the current EMS to ED patient handoff.
Our pre-software integration surveys demonstrate that physicians at our institution experienced similar challenges with accessing the written ePCR to those previously documented in the literature. Additionally, our results suggest that our software interface succeeded in improving reported physician knowledge of how to access the ePCR as well as reported physician ease of access to the ePCR as demonstrated by the significantly decreased reported time in which physicians can access the ePCR. These findings are significant as they address many of the barriers to efficient EMS to ED handoff previously reported in the literature.
Our study does not demonstrate that increased access to the written ePCR resulted in increased perception that prehospital information influenced important patient care decisions. This finding will require further inquiry. An important function of the ePCR should be to provide the physician with the information needed to make important patient care decisions. This study does not answer the question of why physicians did not have that perception. Some possibilities include that physicians historically have not used the printed PCR and have yet to fully integrate the electronic version into their decisionmaking process. It may be that the physicians do not trust the assessments of EMTs and paramedics to the extent that they use them for important patient care decisions. Furthermore, it may be that the information on the ePCR corresponds to the physician’s assessment of the patient and, therefore, does not change the management decisions. Regardless, further study is required.
LIMITATIONS
Our study had several limitations. As a convenience sample of emergency physicians and internal medicine physicians at
our institution, the risk exists for selection basis of those who participated as compared to those who chose not to participate. Furthermore, 14 fewer people responded to the post- than the pre- intervention survey, and this may have resulted in selection bias of the post-intervention group. We worked to minimize these effects by sending several reminder emails to encourage physicians to participate. A second potential limitation is that the physicians’ perceptions of the system and its use may not reflect actual practice. To mitigate this, our methods included many questions phrased to elucidate perceptions of the group and not necessarily individual perceptions. Finally, the culture of high-quality EMS handoffs in this ED specifically should be noted as a potential confounding factor as to why physicians viewed ePCRs to be of low importance regarding patient care decision-making.
CONCLUSION
Overall, pre- and post-survey responses regarding accessibility to prehospital patient data did exhibit a significant change in rank while the importance of the electronic patient care report in clinical decision-making did not differ significantly. This suggests that while integrating prehospital ePCR and hospital electronic health record systems increased accessibility to prehospital information, this increase in access did not significantly alter patient care decision-making by inhospital physicians. These findings align with the consensus in the literature on the ineffectiveness of this information transfer and, more importantly, suggest electronic integration as a potential solution to this problem. However, more research is needed to better understand physician use patterns of prehospital information so that it may be optimized. The consistent ease of access to ePCRs will hopefully foster a better understanding of its utility for clinicians and likely present opportunities for future focused studies.
Address for Correspondence: Robert Katzer, MD, University of California, Irvine Medical Center, Department of Emergency Medicine, 3800 W. Chapman Ave., Suite 3200, Orange, CA 92868. Email: rkatzer@uci.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Katzer et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Troyer L, Brady W. Barriers to effective EMS to emergency
Katzer et al. Integration of Prehospital Patent Care Report into Electronic Health Record
department information transfer at patient handover: a systematic review. Am J Emerg Med 2020;38(7):1494-1503.
2. Jensen SM, Lippert A, Østergaard D. Handover of patients: a topical review of ambulance crew to emergency department handover. Acta Anaesthesiol Scand 2013;57(8):964-70.
3. Bost N, Crilly J, Wallis M, et al. Clinical handover of patients arriving by ambulance to the emergency department - a literature review. Int Emerg Nurs 2010;18(4):210-20.
4. Lubin JS, Shah A. An incomplete medical record: transfer of care from emergency medical services to the emergency department. Cureus 2022;14(2):e22446.
5. Meisel ZF, Shea JA, Peacock NJ, et al. Optimizing the patient handoff between emergency medical services and the Emergency Department. Ann Emerg Med 2015;65(3):310-17.e1.
6. Short M, Goldstein S. EMS documentation. In: StatPearls. Treasure Island, FL: StatPearls Publishing. 2024. Available at https://www.ncbi.
nlm.nih.gov/books/NBK448107/. Accessed January 1, 2025
7. O’Connor K, Golding M. Assessment of the availability and utility of the paramedic record in the emergency department. Emerg Med Australas 2021;33(3):485-90.
8. Shelton D, Sinclair P. Availability of ambulance patient care reports in the emergency department. BMJ Qual Improv Rep 2016;5(1).
9. Afzali F, Jahani Y, Bagheri F, et al. The impact of the emergency medical services (EMS) automation system on patient care process and user workflow. BMC Med Inform Decis Mak 2021;21(1):292.
10. Bledsoe BE, Wasden C, Johnson L. Electronic prehospital records are often unavailable for emergency department medical decision making. West J Emerg Med 2013;14(5):482-8.
11. Altuwaijri EA, Budgen D, Maxwell S. Factors impeding the effective utilisation of an electronic patient report form during handover from an ambulance to an emergency department. Health Informatics J 2019;25(4):1705-21.
Emergency Medical Services Policies and Perspectives Leading to Ambulance Engine Idling
Matthew Lyons, DO*
Aaron R. Kuzel, DO, MBA*
Stephen Marks, DO*
Craig Ziegler, PhD†
Kahra Nix, MD*
Section Editor: Muhammad Waseem, MD
University of Louisville, School of Medicine, Department of Emergency Medicine, Louisville, Kentucky
University of Louisville, Office of Graduate Medical Education, Louisville, Kentucky
Submission history: Submitted April 6, 2025; Revision received July 2, 2025; Accepted July 11, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.47186
Introduction: Ambulances are often left to idle, which may contribute to maintenance costs, environmental harm, and resource inefficiencies. Engine idling affects the health of first responders due to the consequences of exhaust. Our study objective was to gain understanding of current emergency medical services (EMS) policies and perspectives on ambulance engine idling.
Methods: We designed an anonymous, 48-question survey that was distributed to all levels of EMS clinicians. There were 684 total survey responses from 11 states. We excluded those that only included demographics, yielding 507 responses. The response rate was 10.8%. The questions surveyed demographics, service characteristics, and current policies and perspectives on idling. We used multiple question types, including some that asked participants to rate their level of concern on a five-point Likert scale. “Strongly disagree” was coded as 1, and “strongly agree” was coded as 5. “Neither agree or disagree” was considered a neutral response and was coded as 3. Additionally, we conducted a thematic analysis on data derived from the free-text responses to identify themes.
Results: Few (12%) respondents reported written policies on idling. The biggest concerns regarding idling involved the following (reported as median (IQR, 25th and 75th percentiles): patient comfort (4, IQR 4-5); EMS clinician comfort (4, IQR 4-5), and medication compromise (4, IQR 4-5). There was a neutral level of concern regarding equipment failure (3, IQR 3-4) and response delays (3, IQR 3-5). There was a less than neutral level of concern regarding engine failure (2, IQR 2-4); vehicle theft (2, IQR 2-4), air quality (2, IQR 2-3); increased fuel usage (2, IQR 2-3); and carbon emissions (2, IQR 2-3). Six themes emerged: fear of harming patient; safety; effects on air quality; habits and indifference; cost of idling; and frustration.
INTRODUCTION
Each year, emergency medical services (EMS) clinicians in the US respond to more than 25 million calls.1 These calls continue to increase; Medicare beneficiary use of EMS rose by 15% between 2007–2015.2 Emergency medical services call responses typically involve one or more ground ambulances powered by internal combustion engines, running on unleaded
Conclusion: Emergency medical services clinicians mainly hesitate to turn off their engines out of concern for patient/personnel harm and potential equipment failure. The theme of frustration, noted in free-text responses, describes EMS clinicians’ feelings of suspicion and concern for an ulterior motive behind the study, which highlights the need for a collaborative effort at addressing this collective issue. [West J Emerg Med. 2025;26(5)1280–1290.] or diesel fuel. Ambulances are often left to idle while at healthcare facilities and while “available” for service. The vehicles have needs beyond propulsion that require power, including housing equipment, storing medications, and ensuring safe and comfortable compartment temperature. The physical hazard of an EMS clinician’s exposure to weather, which motivates the choice to idle, is a safety concern that
goes beyond just comfort.
Engine idling also causes concerns for the health of first responders from exposure to diesel particulate matter.3 Diesel exhaust was classified as a human carcinogen (group 1) by the International Agency for Cancer Research in 2012.4 The Occupational Safety and Health Administration does not have a standard for diesel exhaust as a single hazard; however, it does have standards for specific components of diesel exhaust such as carbon monoxide, sulfur dioxide, and nuisance dust.5 These diesel pollutants can have both short-term (headache, dizziness, and mucosal irritation) and long-term (respiratory disease, cardiovascular disease, cardiopulmonary disease and lung cancer) health consequences.5
Research has shown other negative impacts of idling, such as higher maintenance costs. For example, every hour of engine idling may be equivalent to 25 miles of driving.6 A study by the US Department of Energy (DOE) found that emergency response vehicles including ambulances routinely idle, and these idling vehicles cost their organization thousands of dollars every year in fuel.7 A DOE study that examined use of idling reduction technologies, including auxiliary power units (APU) in emergency response vehicles, found that departments saved an average of $2,600 per year per vehicle.8 Additionally, there are environmental and other cost impacts.
No prior studies have investigated the viewpoints of first responders who are fire department based, hospital based, or who work for private and third service-based EMS agencies regarding their attitudes toward engine idling and the preferences and policies motivating this practice. These concerns and the paucity of data about EMS idling practices underscore the need for targeted research. In this study we aimed to obtain quantitative and qualitative data to better understand EMS clinicians’ concerns and perceptions about engine idling.
METHODS
Study Design
We distributed an anonymous, 48-question survey using REDCap, a secure, web-based platform (Research Electronic Data Capture hosted at the University of Louisville). There were various question types: five-point Likert scale response items; closed-ended questions; and free-text fields. The questions surveyed the following elements: respondent demographics; vehicle and fuel type; patient population served; and both policies and perspectives around idling. We reviewed the literature and spoke with current EMS clinicians to compile a list of common concerns regarding idling. We ensured the survey’s content validity through literature review and author content expertise (ML, AK, and SM).
We piloted the survey on eligible EMS clinicians who are also content experts, followed by a debrief via cognitive interviewing. We performed additional response-process validity with people outside the EMS community sample, and we consulted a statistician (CZ). The full survey is available as
Population Health Research Capsule
What do we already know about this issue? Engine idling has been previously connected to environmental harm and occupational exposures that affect human health.
What was the research question?
What are the current policies and EMS clinician motivations and concerns surrounding ambulance engine idling?
What was the major finding of the study? The biggest concerns were patient comfort, clinician comfort, and medication compromise (Median=4, IQR=4, 5).
How does this improve population health? Expanding policies on engine idling could decrease environmental and occupational harm. However, EMS clinician concerns should be addressed when creating solutions.
supplementary material. The study was deemed exempt by the University of Louisville Institutional Review Board.
Participants
Inclusion criteria included active and retired EMS clinicians: emergency medical responders (EMR), emergency medical technicians (basic, advanced, and intermediate), paramedics, and physician EMS medical directors. The survey was distributed by list-servs, social media, and a flyer posted in the emergency department (ED) of the University of Louisville, an urban, academic medical center and tertiary-care center in Louisville, KY. The consent was included on the first screen; thus, completion of the survey acted as implicit consent. The survey was open from July 31–October 5, 2024. There were 684 total responses. Responses that only included demographics were excluded, yielding a total of 507 responses.
Using the American Association for Public Opinion Research standard definition, the response rate for this survey was 10.8%.9 Respondents were defined as individuals who potentially received the survey from one of two list-servs or other sources but did not respond. It is not known whether these individuals did not respond because they were ineligible or because they were eligible but chose not to respond. We took a conservative approach when calculating the response rate, and all these individuals were included in the denominator. It is likely that the actual response rate was higher, as it is unlikely that every individual was eligible.
Statistical Methods
We calculated simple descriptive statistics for all demographic and auxiliary variables. For continuous variables, we calculated means and SDs or medians and IQR (25th and 75th percentiles) depending on the normality of the distributions. For nominal variables, frequencies and percentages were calculated. For data analysis, we converted the five-point Likert response format items to numerical values. “Strongly disagree” was coded as 1 and “strongly agree” as 5. “Neither agree or disagree” was considered a neutral response and was coded as 3. Medians of these items are reported in the text, while percentages are depicted in Figure 1.
In Figure 1, Stratum A illustrates responses about current preferences of respondents regarding ambulance engine idling, considering agency policy and whether respondents believe ambulance engine idling affects patient care. Stratum B illustrates potential concerns regarding not idling the ambulance engine. Stratum C illustrates potential concerns regarding idling the ambulance engine. Data values are based on a Likert scale from 1 (not at all concerned/strongly disagree) to 5 (extremely concerned/strongly agree).
We used a Kruskal-Wallis non-parametric test to assess the difference among levels of training and practice settings on the items in Likert response format. For practice setting, when an item was statistically significant, we performed pairwise comparisons between the groups using a Dunn post hoc test with a Bonferroni correction to adjust for possible inflated type I error rates. For levels of training, using the Dunn-Bonferroni correction showed no significant pairwise comparisons with a Bonferroni correction to adjust for the fact that testing multiple outcomes inflated the experiment-wise type I error rate. Key findings are reported in the text as medians.
We used a Spearman correlation coefficient to assess the association between length of service with the Likert response format items. When the Benjamini Hochberg test was performed to minimize the risk of type 1 error rates, only one correlation was significant; thus, we report non-adjusted P-values due to the risk of making a type 2 error. All P-values were two-tailed. Statistical significance was set by convention at P < .05. We used SPSS v29.0 (SPSS Statistics, IBM Corp, Armonk, NY) to analyze the data, and we used the R Package ggplot2 (The R Foundation for Statistical Computing, Vienna, Austria) to produce Figure 1.
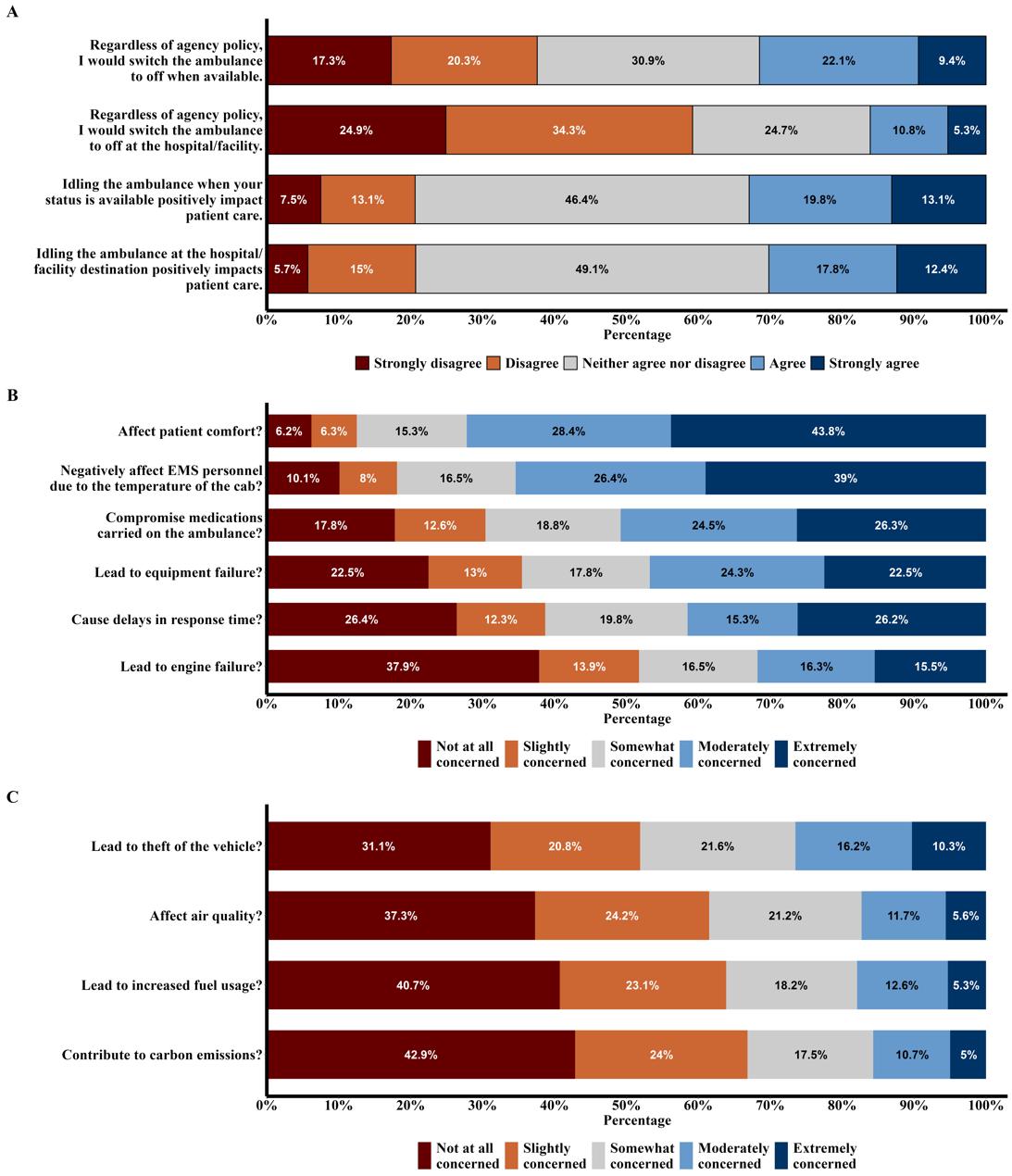
Figure 1. Emergency medical services clinicians’ responses regarding their level of concern about policies and common issues surrounding ambulance engine idling.
Table 1. Demographics of emergency medical services clinicians who participated in a survey regarding existing policies and their perspective on ambulance engine idling.
Age, mean (SD)
(11.9) IQR, interquartile range; SD, standard deviation.
There were seven free-text prompts. Two allowed clarifications of existing written idling policies when the ambulance was at a facility destination and while it was “available” for service. Two prompts each allowed participants to clarify why they felt idling at the facility destination or while “available” for service positively affected patient care as a follow-up to two Likert-scale quest--ions. One prompt followed Likert-scale questions to allow clarification of any additional concerns regarding idling. Participants also had a free-text response option to share their personal opinions regarding idling in general while at the facility destination and while “available” for service. To identify and interpret the themes in the qu-alitative dataset, we conducted a systematic thematic analysis through the six steps described by Naeem.10 ML performed the initial review, coding of responses, derivation of themes, and conceptualization. AK, SM, and KN reviewed and verified the selection of keywords, coding of the data, development of themes, and conceptualization.
RESULTS
Descriptive Data
Demographic characteristics are reported in Table 1. Respondents varied in level of training, years of service,
practice setting, and shift duration. Participants characterized their current or previous service. These are reported in Table 2.
Quantitative Analyses
Respondents had a neutral response when asked whether idling positively impacted patient care either while the ambulance was “available” (Median 3) or at the hospital/facility destination (Median 3). When asked if given the option, regardless of agency policy, respondents had an overall neutral opinion on turning the engine off both when “available” (Median 3) and at the hospital/facility destination (Median 2). Respondents were asked how concerned they were about various impacts of idling, and the results are illustrated in Figure 1. The most prevalent concerns leading to the decision to idle were patient comfort and clinician comfort. Results showed a slightly greater than neutral concern regarding medication compromise, equipment failure, and delays in response time. Responses declared a slightly less than neutral concern for engine failure, theft of vehicle, air quality, increased fuel usage, and contribution to carbon emissions.
To identify confounders, concerns were differentiated based on level of training, practice setting, and length of service.
median level of concern among different levels
Table 2. Practice setting and service characteristics of emergency medical service’s clinicians represented in the survey. Which of the following best describes your service? n,
Which of the following best describes your service? n, %
your service offer Advanced Life Support services, or Basic Life Support services only? n, %
Does your ambulance have an auxiliary power unit to enable you to switch your engine off and still have access to power? n
(operated independently of a fire department)
of training are represented in Table 3. Differences in median level of concern among EMS clinicians in urban, suburban, and rural practice settings are represented in Table 4. There were statistically significant correlations between EMS clinicans’ length of service with their concern for patient comfort (R s = .108, P =.02); compromise of medications (R s =.153, P < .001); and increased fuel usage (R s = .097, P = .03).
Qualitative Analyses
We performed a qualitative analysis to identify concerns that were not anticipated in the survey during study design. Nine codes were derived: fear of equipment failure;
temperature; security; time at facility; unit readiness; air quality; economics; indifference; and frustration. The most common code was “fear of equipment failure” (n = 167), followed by “temperature” (n = 87). There were six themes derived: fear of harming patients; perceived level of safety; effects on air quality based on ambulance bay design and age of ambulance; idling due to previously established habits and indifference; perceived cost of idling; and frustration. Representative quotes are presented in Table 5.
Theme 1: Fear of Harming Patients
This was the most prevalent theme in the analysis and
Table 3A. Emergency medical service clinicians’ concerns regarding the potential effects of NOT idling the ambulance engine, on a Likert scale from “not at all concerned” (1) to “extremely concerned” (5). Medians and IQRs are presented.
delays in response time?
to engine failure?
Superscript lettering in a cell indicates where significant pairwise comparisons between roles are found. For example, in looking at the item “cause delays in response time,” the overall significance of .02 indicates that somewhere among the different levels of training there is a significant difference. The role “physician” is designated [E], and the superscript lettering that shows the ratings were significantly different from EMTs [B], advanced EMTs [C], paramedics [D], retired personnel [F], and other [G]. We used the Dunn test to assess post hoc pairwise comparisons.
EMR, emergency medical responder; EMT, emergency medical technician; EMS, emergency medical services.
encompassed a range of concerns that EMS clinicians felt would ultimately impact patient safety. Respondents cited degradation of medications outside acceptable temperature ranges as a common concern. Additionally, EMS clinicians were concerned that turning off the engine would cause equipment or engine failure; they were also concerned that this could cause a delay in response time or an inability to even respond to calls. This likely reflects how operational readiness is a core EMS value.
Theme 2: Perceived Level of Safety
This highlighted a reason that some EMS clinicians choose not to idle. It was noted by some to be an especially important consideration in rural areas. However, it was mentioned that newer ambulances have anti-theft devices that are active with the engine idling.
Theme 3: Effects on Air Quality Based on Ambulance Bay Design and Age of Ambulance
Some respondents shared concern about the consequences that idling has on air quality. They identified poorly designed ambulance bays that did not include appropriate ventilation or emission controls. Concerns were directed toward ambulance bay design and age of the ambulance more than the act of engine idling. Respondents were not as concerned about emissions from newer trucks, but they did acknowledge that older ambulances might contribute more to poor air quality.
Theme 4: Engine Idling Due to Previously Established Habits and Indifference
Respondents stated that they idle simply because it is what they have historically done. Additionally, there were
The significance level is based on the Kruskal-Wallis test. Because only one respondent was an EMR, that data was not included in the analysis.
EMR, emergency medical responder; EMT, emergency medical technician; EMS, emergency medical service.
Table 3B. Emergency medical service clinicians’ concerns regarding the potential effects of idling the ambulance engine.
Table 4A. Emergency medical service clinicians’ concern regarding the potential effects of NOT idling the ambulance engine, based on their service location.
Urban Suburban Rural P = (n = 135) (n = 166) (n = 202)
Affect patient comfort?
Negatively affect EMS personnel due to the temperature of the cab?
Compromise
, emergency medical services.
EMS clinicians who reported indifference to whether there could be impacts from idling suggesting that idling may be a habit, rather than a deliberate choice informed by operational or environmental needs.
Theme 5: Perceived Cost of Engine Idling the Ambulance
Administrative or supervisory personnel are more likely to highlight the potential costs of idling. These respondents emphasized cumulative costs across an entire department fleet. This highlights the role that improved efficiency may play in operational and budgetary challenges faced by EMS organizations.
Theme 6: Frustration
While there was constructive feedback, there were frustrations as well. Some respondents highlighted that the study was being conducted out of the ED rather than an EMS service, which led to a feeling of suspicion or concern for an ulterior motive regarding the study objectives. Others believed that the hospital or other public service agencies
should be the focus when addressing the negative consequences of idling.
DISCUSSION
Decreasing idling would lead to health, cost, and environmental benefits. In this survey of EMS clinicians, we explored the current policies and perspectives regarding engine idling. Only 12% of respondents reported that their agency has a written policy regarding idling, suggesting that the decision to idle is predominantly the choice of the individual responder. Open-ended responses in this study indicated that EMS clinicians are open to decreasing idling if these potential harms are addressed. Following are the foremost areas of concern identified in the thematic analysis and should each be considered when approaching solutions.
Patient Comfort
Patient comfort was a chief concern that EMS clinicians of all levels reported when asked about switching off the engine. Of the respondents, 72% indicated that they were
Table 4B. Additional concerns reported by emergency medical service clinicians regarding the potential effects of idling the ambulance engine, based on their service location.
The significance level is based on the Kruskal-Wallis test. Superscript lettering in a cell indicates where significant pairwise comparisons between roles are found. For example, by looking at the item “contribute to carbon emissions,” the overall significance of .04 indicates that somewhere among the different practice settings there is a significant difference. The location suburban is lettered [B], and the lettering shows the ratings are significantly different from urban [A] and rural [C]. We used the Dunn test with Bonferroni correction to assess post hoc pairwise comparisons. For the item “contribute to carbon emissions,” no significant pairwise differences were found between locations when the Bonferroni correction was used, so only the Dunn test (without a correction) is depicted. EMS, emergency medical service.
Table 5. Representative quotes used to derive themes from a survey of emergency medical service clinicians regarding their perspectives surrounding ambulance engine idling.
Theme 1 – Fear of harming patients
“Idling allows for the truck to stay at an appropriate temperature, protect equipment and medications, and prevents the truck from not starting when leaving the hospital en route to another call.”
“We have a lot of things in the ambulance that operate on battery including internet, GPS, MDT system, stretcher, etc. All of these things can drain the batteries relatively quickly, and if the ambulance’s battery is dead we cannot respond to the next emergency.”
“I would rather be idling in case the engine is off and would not start and cause a delay in transport.”
Theme 2 – Perceived level of safety
Theme 3 – Effects on air quality based on ambulance bay design and age of ambulance
Theme 4 – Engine idling due to previously established habits and indifference
Theme 5 – Perceived cost of engine idling the ambulance
“Ambulances can be and should be equipped with a safety feature that allows engine to idle with key out. Our ambulances allow you to idle the engine with the key out and vehicle secured/locked. If someone was to get in and touches the break, the engine will stop preventing theft.”
“I do worry about it being stolen, but I also worry about it not restarting.”
“I believe that ambulances should not be left idling in the ambulance bays. It’s led to multiple vehicle thefts in the county.”
“The design of the ambulance bay is up to the hospital administration. Most facilities I’ve encountered have fans or ventilation systems at the EMS entrance to their ED as well as two sets of doors that prevent exhaust fumes from entering the facility.”
“Turned off only if the air filtration system draws the exhaust fumes into the ER or hospital.”
“I could care less.”
“Frankly, I don’t think about these things.”
“It’s mostly idled due to habit. I’ve never been instructed by policy to keep it running but always have.”
“I believe that turning the unit off is more economically sound from a business perspective, however hospitals are not set up or equipped to dock/charge units that are turned off. “
“Waste of gas and higher theft chances.”
Theme 6 – Frustration “Hospital/facility destinations should not dictate the policies and procedures of the separate entities that own and operate ambulances.”
“Why are we so focused on ambulances, seems kinda like a vendetta.”
GPS, global positioning system; MDT, mobile data terminal; EMS, emergency medical services; ED, emergency department; ER, emergency room.
either moderately or extremely concerned that not idling could affect patient comfort. Medical directors had a significantly lower level of concern for patient comfort compared to all other types of EMS clinicians. There are national standards for the minimum and maximum temperatures that the cab and chassis must meet when manufactured.11 However, operating temperature standards are dependent on whether local policy exists. Washington, DC, is one area that has a written policy requiring that the patient compartment be between 50°F-85°F while awaiting a patient response.12 Aside from patient comfort, poorly regulated temperature in the patient compartment can also have effects on patient outcomes. Ambulances have a limited ability to quickly achieve and maintain these temperatures, particularly in winter months.4, 13
Emergency Medical Services Clinician Comfort
Emergency medical services clinician comfort, although less concerning to EMS clinicians than patient comfort, was a worry for respondents. In this study 61% of respondents reported working shifts longer than 24 hours. The amount of time spent in the ambulance varies based on several factors, including service structure, run volume, dynamic or fixed deployment models, and the size of the service area. It is not uncommon for some to be in the ambulance nearly the entirety of their shift. High levels of EMS clinician burnout are well documented in the literature, with one study reporting rates of nearly 60% across services in North Carolina.14 Regardless of burnout or the current nationwide EMS clinician shortage, comfort should be prioritized. Agencies should consider clinician access to a temperaturecontrolled area or an alternative system, like APUs, to control the temperature of the cab if the engine is to be switched off while occupied.
Medication Storage
Many respondents cited a concern about medication safety and quality in the absence of idling. Most medications on an ambulance are regulated by the United States Pharmacopeia (USP) to be stored at “controlled room temperature,” which is defined as approximately 59-86°F.15 In one observational study, it was found that across five different EMS services in different climate regions, no ambulance was able to consistently maintain a medication storage temperature within USP recommendations.13 This is likely exacerbated by switching the engine off. An APU or shore power would need to be employed to mitigate this issue when not idling.
Equipment and Engine Failure
Some ambulance components are dependent on a power supply. With the modernization of ambulances, such as the creation of the power stretcher, a reliable power supply is crucial for operational preparation. Forty-seven percent of respondents were moderately or extremely concerned that not idling could lead to equipment failure. The thematic analysis provided more context for this concern. “Fear of equipment failure” was the most common code in the thematic analysis. Review of free-text responses revealed that many EMS clinicians reported having to provide patient care in ambulances that are dated and poorly maintained. Recently, the US Centers for Disease Control and Prevention recognized that EMS services nationwide are “severely underfunded.”17 This in turn leads to a limited budget for maintenance, expansion, and modernization of the fleet.
There was discordance between some free-text responses and the Likert-scale responses regarding the concern for potential engine failure. Some respondents reported instances of an engine that would not restart after being turned off, which has obvious and notable implications for a service’s ability to provide timely emergency care. Respondents pointed out that this was particularly an issue in rural services where there are very few ambulances in service and patients are often transported longer distances for higher levels of care.
Delays in Response Time
The thematic analysis revealed that the concern for delays in response time was predominantly within the rural community. This concern was separate from the worry that the engine would not restart, and the motivator for this specific concern is unclear. Based on responses, this concern seems to be that the time required to start the engine could lead to a delay. There is no current literature to clarify this.
Theft of the Vehicle
Idling an ambulance leaves it vulnerable to theft and crimes of convenience. Twenty-six percent of respondents were moderately or severely concerned about idling leading to theft of the vehicle, and rural EMS clinicians were
significantly more concerned compared to others. A review from 2020 showed that ambulance thefts are increasing nationwide.18 There are devices commercially available that allow the key to be removed from the ignition while the vehicle is running, which would allow the doors to lock while idling.19 These devices address the issue of theft, but they do not provide the cost and environmental benefits of turning off the vehicle. Additionally, this could be limited in older ambulance models.
Air Quality and Emissions
Respondents reported, on average, that the engine is on for approximately 58% of their shift. The most commonly reported shift was 24 hours. It is well documented that idling has negative effects on the environment. Idling causes emission of harmful combustion products, including carbon monoxide, nitrous oxides, and other greenhouse gases.20 As mentioned by some respondents, the presence of these byproducts can be especially taxing in those who have respiratory diseases and are exposed while in the ambulance bay or ED entry. In this study 66.7% of respondents reported that their service’s vehicles primarily use diesel. Diesel engines, on average, emit 1.14 times the amount of carbon dioxide as compared to gasoline engines. Some respondents argued that filters can mitigate this discrepancy. A diesel particulate filter (DPF) is a modification to a diesel vehicle that can significantly reduce particulate matter, nitrous oxide, and carbon monoxide.21 Our survey did not ask respondents about the presence or absence of a DPF on their vehicles, and their prevalence on ambulances is unknown. Suburban EMS clinicians were significantly more concerned about air quality than rural EMS clinicians, although both had a low concern overall.
Increased Fuel Cost
Physician respondents were significantly more concerned about increased fuel usage due to engine idling compared to the others. Urban EMS clinicians were significantly less concerned about fuel usage than other EMS areas. A case study by Argonne National Laboratory found that with battery APUs, ambulance services saved at least $5,100 in annual fuel cost per ambulance.22 There is significant variability between APUs with varying cost savings.23 Given the general underfunding of EMS systems in the United States, reducing idling presents a potential area to decrease costs.
Potential Solutions
The issues surrounding idling are complex. We identified numerous variables that are concerns for EMS clinicians and deserve recognition when trying to address the issue: The first APU, a device that provides energy for functions other than propulsion, was designed for aviation use in the 1950s.25 Since then, usage has been expanded to fire and police vehicles, and ambulances. Generally, they can provide power to certain components of the ambulance when the
engine is off. There is significant variability between APUs, including the number of components it can power and how long it can run with the engine off. In addition to showing an annual cost savings of $5,100, lead-powered APUs reduced oil changes by at least 50%.23 Based on their calculations, the APUs would recuperate their cost in one to two years, making them an economical option for EMS services. In this study, 41.9% of respondents reported having an APU that would allow access to power while the engine is off. The frequency of APU use was not investigated in this study.
Electrified parking spaces (EPS) are another potential solution that would provide similar benefits to APUs. These are parking spaces that provide a shoreline or duct system to augment power while the engine is off. A study of one commercial EPS unit was shown to cost $0.75 per hour to operate, compared to an estimated $18.75 per hour to operate an ambulance that is running.4 One anticipated barrier to the use of EPS is that installation at hospitals would increase the facility’s electricity costs. Because of this, non-hospital-based EMS services may have difficulty with hospital buy-in on installation despite the promise of cost savings and lessening environmental and health effects. Furthermore, dynamic deployment models of EMS may preclude the ability of ambulances to connect to EPS.
It should be acknowledged that throughput time at healthcare-facility destinations is a notable contributor to idling. Compounding this is poor ambulance bay design, which limits ambulance movement or does not provide appropriate parking areas to allow an engine to be switched off. Improving these are potential solutions as well.
LIMITATIONS
We attempted purposive sampling; however, there were responses from only 11 US states with 92.6% of respondents working in Kentucky. The response rate was only 10.8%, and there was also greater representation of self-identified White (96.7%), males (75.6%), and paramedics (47.5%). However, a national survey of EMS clinicians with 87,471 respondents from 46 states found 82.4% to be White, 75.8% to be male, and 44.9% to be paramedics, indicating this greater representation closely mirrors the national EMS workforce.26 Clearly, a response rate of 10.8% leads to a rational concern that the responses may be biased. However, in most surveys, when bias occurs, it is typically those at the extremes of opinions and not the less extreme responses. In examining our data, the modal response to our survey in Stratum “A” in Figure 1 were the most neutral responses for three of the four questions posed. This suggests bias may be minimal. On the other hand, the modal responses for Stratum “C” were “not at all concerned” for all four questions in this stratum, and this could reflect bias. Thus, we believe we are receiving “mixed signals” regarding whether our low survey-response rate was a source of bias.
The survey was distributed during only one weather season, which could be a potential limitation to generalizability. Local EMS clinicians shared with us a fear of consequences due to the potential that their personal practices or opinions might conflict with their EMS agency, which could have introduced bias. We attempted to minimize this by making all questions optional and adding a preamble reminding respondents that the survey was anonymous and data would not be shared directly with employers. However, this could have added bias in allowing respondents to selectively answer questions. There was potential for recall bias when respondents were asked to describe written policy regarding idling. (Likert-scale survey questions were shuffled to avoid question-order bias.) Additionally, as with all surveys there was a potential for self-selection bias.
Initially, during the data analysis phase, we applied post hoc corrections to account for multiple testing and the risk of inflating type I errors rates. However, for some series of tests such as with levels of training, length of service, and one item within practice setting (“contribute to carbon emissions”), the corrections led to no significant results that could potentially have increased type II errors. Therefore, we report no post hoc corrections for these variables with the caveat that some caution should be taken with interpretation of the results.
CONCLUSION
Few survey respondents (12%) reported written policies on idling. Respondents recognized the potential benefits of decreasing idling, including lower fuel costs, fewer negative health effects and emissions, and a lesser likelihood of vehicle theft. However, responses suggested a hesitation to turn off engines due to concern for harm (patient and clinician) and potential engine or equipment failure. Each of these concerns should be considered and addressed when approaching solutions to idling.
Next steps include clarifying that solutions entail far more than issues of fuel cost or wear on the ambulance; exhaust exposure is a documented harm to EMS clinicians. As the thematic analysis revealed frustrations by EMS clinicians (evidenced by feelings of suspicion and concern for ulterior motives by study investigators), it is imperative that solutions be collaborative and efforts reflect that this is a collective issue that cannot be solved by EMS agencies alone.
ACKNOWLEDGMENT
We are grateful to Eric Yazel, MD, Martin Huecker, MD, Evan Kuhl, MD, Raymond Orthober, MD, Timothy Price, MD, and the Kentucky Board of Emergency Medical Services for their contributions to the study and critical review of the manuscript. Statistical support was underwritten by Office of Graduate Medical Education, University of Louisville, School of Medicine.
EMS Policies and Perspectives Leading to Ambulance Engine Idling
Address for Correspondence: Matthew Lyons, DO, University of Louisville, School of Medicine, Department of Emergency Medicine, 530 S. Jackson St, #C1H17 Louisville, KY 40202. Email: matthew.lyons@louisville.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Lyons et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Redlener M, Buckler DG, Sondheim SE, et al. A national assessment of EMS performance at the response and agency level. Prehosp Emerg Care. 2024;28(5): 719-26.
2. Birmingham LE, Arens A, Longinaker N, et al. Trends in ambulance transports and costs among Medicare beneficiaries, 2007-2018. Am J Emerg Med. 2021;Sept:47:205-212.
3. Firefighter exposures to diesel emissions and how to reduce the exposure. 2015. Available at: https://www.fireemsleaderpro. org/2015/09/29/firefighter-exposures-to-diesel-emissions-and-how-toreduce-the-exposure/. Accessed December 14, 2024.
4. IARC: diesel engine exhaust carcinogenic. 2012. Available at: https:// www.iarc.who.int/wp-content/uploads/2018/07/pr213_E.pdf. Accessed December 14, 2024.
5. Diesel Exhaust. 2013. Available at: https://www.osha.gov/dieselexhaust. Accessed December 20, 2024.
6. The ambulance anti-idling solution. 2014. Available at: https:// practicegreenhealth.org/sites/default/files/upload-files/medidock_ ambulance_docking_port_case_study_5-16.pdf. Accessed December 13, 2024.
7. Idling reduction for emergency vehicles: a case study. 2017. Available at: https://afdc.energy.gov/files/u/publication/idling_reduction_ emergency_vehicles_case_study.pdf. Accessed December 27, 2024.
8. Idling reduction technologies (IRT) installed on a fleet of emergency vehicles reduced annual fuel costs by $2,600 per vehicle. 2016. Available at: https:// www.itskrs.its.dot.gov/2017-b01158. Accessed December 13, 2024.
9. American Association for Public Opinion Research. (n.d.). Standard definitions: final dispositions of case codes and outcome rates for surveys, revised 2023. Available at: chromeextension://efaidnbmnnnibpcajpcglclefindmkaj/https://aapor.org/ wp-content/uploads/2023/05/Standards-Definitions-10th-edition. pdf. Accessed December, 15, 2024.
10. Naeem M, Ozuem W, Howell K, et al. A step-by-step process of thematic analysis to develop a conceptual model in qualitative research. Int J Qual Methods. 2023;22:1-18.
11. Ground Vehicle Standards for Ambulances. 2022. Available at: https://
www.groundvehiclestandard.org/wp-content/uploads/2022/06/CAAS_ GVS_V3_Final_07_01_2022_2.pdf. Accessed December 26, 2024.
12. District of Columbia Ambulance Interior Climate Standard. 2010. Available at: https://doh.dc.gov/sites/default/files/dc/sites/doh/ publication/attachments/Policy_EMS_2010_0010_Ambulance_ Interior_Climate_Standards.pdf. Accessed December 13, 2024.
13. Svendsen T, Lund-Kordahl I, Fredriksen K. Cabin temperature during prehospital patient transport—a prospective observational study. Scand J Trauma Resusc Emerg Med. 2020;28(1):64.
14. Kaplan GR, Frith T, Hubble MW. Quantifying the prevalence and predictors of burnout in emergency medical services personnel. Ir J Med Sci. 2024;193(3):1545-6.
15. Brown L, Krumperman K, Fullagar C. Out-of-hospital medication storage temperatures: a review of the literature and directions for the future, Prehosp Emerg Care. 2004;8(2):200-6.
16. Packaging and Storage requirements. 2017. Available at: https:// www.uspnf.com/sites/default/files/usp_pdf/EN/USPNF/revisions/659_ rb_notice.pdf. Accessed December 15, 2024.
17. Medication storage temperatures on U.S. ambulances: a prospective multicenter observational study. Pharmaceutical Forum 2003;29(2):540-544.
18. Emergency Medical Services (EMS): Local Authority, Funding, Organization, and Management. 2024. Available at: https://www.cdc. gov/ems-community-paramedicine/php/us/local-authority.html#:~:text =Unlike%20police%20and%20fire%20services,level%20and%20 often%20severely%20underfunded.Accessed December 16, 2024.
19. Sullivan RA, Kraus CK. Grand theft ambulance: media reports of stolen ambulances in the United States, 1980 to 2020. Am J Emerg Med. 2024;85:214-216.
20. Run lock systems explained. Available at: https://amber-valley.com/ run-lock-systems-explained. Accessed December 10, 2024.
21. Stocker TF, D Qin, Plattner M, et al. IPCC, 2013: Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Camb Univ Press.
22. Svendsen T, Lund-Kordahl I, Fredriksen K. Cabin temperature during prehospital patient transport - a prospective observational study Scand J Trauma Resusc Emerg Med. 2020;28(1):64.
23. Idling reduction for emergency vehicles. 2017. Available at: https:// afdc.energy.gov/files/u/publication/idling_reduction_emergency_ vehicles_case_study.pdf. December 10, 2024.
24. The ambulance anti-idling solution. 2012. Available at: https:// practicegreenhealth.org/sites/default/files/upload-files/medidock_ ambulance_docking_port_case_study_5-16.pdf. December 12, 2024.
25. Honeywell auxiliary power units make aviation history with new production milestones. Available at: https://www.honeywell.com/us/en/ press/2019/09/honeywell-auxiliary-power-units-make-aviation-historywith-new-production-milestones. Accessed December 27, 2024.
26. Rivard MK, Cash RE, Mercer CB, et al. Demography of the national emergency medical services workforce: a description of those providing patient care in the prehospital setting. Prehosp Emerg Care. 2021;25(2):213-220.
Refusal of Emergency Medical Transport After a Fall: Patient Characteristics and Outcomes of Repeat Callers
Jacob Barr, MD*
Katherine Selman, MD*†
Krystal Hunter, PhD*
Alexander Kuc, MD*†
Cooper Medical School of Rowan University, Camden, New Jersey Cooper University Health Care, Department of Emergency Medicine, Camden, New Jersey
Section Editor: Quincy Tran, MD, PhD
Submission history: Submitted August 1, 2024; Revision received December 21, 2024; Accepted February 19, 2025
Electronically published August 20, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.33524
Introduction: Lift assistance represents a high proportion of emergency medical services (EMS) calls, yet data is limited regarding the long-term outcomes of these patients who subsequently refuse transport. In this study, our objective was to examine the outcomes of patients who require lift assistance but refuse transport and to determine factors associated with repeated EMS utilization.
Methods: We conducted a retrospective, observational cohort study of EMS calls in southern New Jersey in patients ≥18 years of age who declined EMS transport after a fall between July 1, 2021–July 1, 2022. Repeat callers were defined as making one additional call within 30 days, and we defined super-users as those making ≥four calls within six months. The primary outcome was repeat emergency department (ED) visits within 30 days from the initial transport refusal visit.
Results: We analyzed 116 of 203 (57%) patients. The mean patient age was 66.3 years, and 53.6% were female. Forty-seven (37.9%) patients were repeat callers, and 27 (21.8%) were super-users. Repeat callers and super-users had increased odds of 30-day ED visits (odds ratio [OR] 17.2, 95% confidence interval [CI] 6.4-47.6, and OR 8.8, 95% CI 3.3-23.7, respectively), and six-month ED visits (OR 4.9, 95% CI 2.2-11.2, and OR 12.9, 95% CI 3.9-56.5). Similarly, there were increased odds of 30-day admission for repeat and super-user callers (OR 6.6, 95% CI 2.5-18.2, and OR 10.8, 95% CI 4.0-29.8, respectively), and six-month admissions (OR 3.0, 95% CI 1.4-6.5,and OR 6.8, 95% CI 2.6-19.9, respectively). No differences in death at one year were observed in either group (repeat callers OR 1.4, 95% CI 0.4-4.5; super-users OR 1.1, 95% CI 0.2-4.1) Repeat callers had higher proportions of anticoagulation/antiplatelet therapy and non-ambulatory status (42.9% vs 61.7%, P=.046 and 29.0% vs 56.8%, P=.006, respectively).
Conclusion: Repeat EMS calls for lift assistance may be used to identify patients at high risk for ED visits and hospitalizations. As patients decline transport, EMS may be their sole healthcare encounter. Future directions would entail training EMS personnel in screening or referring patients for more intensive outpatient interventions. [West J Emerg Med. 2025;26(5)1291–1295.]
INTRODUCTION
Older adults experience an estimated 36 million falls yearly in the United States, with 28% of adults >65 of age reporting falls in 2020.1,2 Falls account for nearly 2% of emergency medical services (EMS) calls, but rises to 11.5% in adults >60. 3,4 Falls are a national problem, with fall-
related EMS calls increasing by 268% from 2007 to 2017.4,5 Further concerning, while 5.1% of all EMS calls for adults result in refusal of care following EMS contact, fall-victim refusal rates range from 11-56%.6,7 Within this study population, 49% of fall victims had an unplanned healthcare encounter within 28 days.7 This suggests that lift
assists, or assistance after a fall without intent for EMS transport, may represent a sentinel event for patient care. Previous studies demonstrated that repeated calls for lift assists represent over a quarter of the study population, and half of lift-assist patients required that EMS return to the same address within 30 days, representing a large portion of EMS and paramedic resource utilization.3,8,9
While data exists that analyzes demographic, medical history, and social factors for those who refuse EMS transportation, limited data analyzes short- and long-term healthcare utilization of fall victims who refuse EMS assistance following their initial lift-assist encounter. Our objective was to describe the prevalence of repeat calls among patients who suffered falls or required lift assistance but declined initial EMS transport, to identify demographic information and factors that may contribute to increased EMS utilization, and to assess 30-day and six-month ED visits and hospitalizations.
METHODS
Study Design and Population
We conducted a retrospective cohort study of “fall victims” who refused transport in Camden County, New Jersey, treated by Cooper University Health Care (CUHC) EMS between July 1, 2021_July 1, 2022. Cooper EMS’ structure and volume are described in Supplement 1. We followed distinct criteria posed by Worster et al (Supplement 2).10
We identified patients were identified using the Zoll emsCharts system (Zoll Medical, Chelmsford, MA) to track community-dwelling patients ≥18 years of age classified as “fall victims” who then refused medical transport to the hospital following evaluation (Broomfield, CO, Supplement 2). Exclusion criteria included patients <18 years of age and those residing in assisted living, skilled nursing, long-term care, or memory care facilities. These individuals were excluded as they rarely refuse transport or may have access to appropriate medical resources (primary care, ancillary staff, etc) unavailable to community members.
The hospital electronic health record (EHR) (Epic Systems Corporation, Verona, WI) was assessed for our independent and outcome variables. Emergency medical services transport patients to CUHC, Virtua Camden, or Our Lady of Lourdes Hospital in Camden, NJ, all of which have Epic as their primary EHR. If patients were transported to hospital systems using different EHRs, their outcome variables would not be accessible. Demographic information and additional characteristics collected are described in Supplement 2.
High utilization in the emergency setting is defined variably in the literature. 11 The supplemental material describes our rationale for defining both repeat callers and super-users. Repeat callers were patients who required EMS services at least one additional time within 30 days following their fall.12 Super-user patients were defined as patients with ≥four calls in six months.
Population Health Research Capsule
What do we already know about this issue? Fall-victim refusal of EMS transport ranges from 11-56%, and half of fall victims have an unplanned healthcare encounter within 28 days.
What was the research question?
Assess ED visits and hospitalizations among patient who suffered falls, but declined initial EMS transport.
What was the major finding of the study? 30-day ED visits were increased in repeat callers (OR 17.2, 95% CI 6.4-47.6) and superusers (OR 8.8, 95% CI 3.3-23.7).
How does this improve population health? EMS responders may be the only medical personnel to be aware of patient falls. The approach to fall victims should be structured to address short- and long-term outcomes.
Outcomes
Our primary outcome was the odds of ED visits within 30 days from the initial transport refusal. Secondary outcomes included odds of ED visits in six months, hospital admission at 30 days and six months, and death. Data analysis methods can be found in the supplemental materials. This project received institutional review board approval from CUHC (IRB Number 22-245).
RESULTS
Demographics and Call Characteristics
Between July 1, 2021–July 1, 2022, 203 unique calls were made to EMS for “fall victims” who subsequently declined transport, and 194 fit our inclusion criteria. Of those calls, 18 patients accounted for 63 EMS encounters, while the remaining 131 patients accounted for only one encounter during the study period. Twenty-five patients did not have identifying information documented by EMS, and eight patients did not have a medical record number to connect their EMS and EHR documentation. This left 116 individuals for analysis (Figure S1). The initial call was chosen as the primary analysis point for patients with multiple EMS dispatches.
Of the 149 unique patients, 55% were Black and 53.6% were female, with a mean age of 66.3 years of age (Table 1). When comparing demographic information of repeat and non-repeat callers, repeat callers had higher rates of taking
Table 1. Characteristics of patient calls.
Characteristic All study subjects (N=149)
ED visits and Hospital Admissions of Repeat Callers and Super-users
Forty-seven (37.9%) patients were repeat callers, and 27 (21.8%) were super-users. The odds ratio (OR) of ED visits in 30 days for repeat callers compared to non-repeat callers was 17.2 (95% confidence interval [CI] 6.4-47.6) (Table 2). For 6-month ED visits, this relationship also held (OR 4.9, 95% CI 2.2-11.2). Repeat callers had increased odds of admission both at 30 days (OR 6.6, 95% CI 2.5-18.2) and six months (OR 3.0, 95% CI 1.4-6.5). There was no difference in one-year mortality. Super-users demonstrated no significant difference in demographics or vital signs from non-super-users (Table S1). Super-users had increased odds of ED visits within 30 days and six months (OR 8.8, 95% CI 3.3-23.7, and OR 12.9, 95% CI 3.9-56.5, respectively) (Table 2). Similarly, there were also increased odds of hospitalizations at 30 days and six months (OR 10.8, 95% CI 4.0-29.8, and OR 6.8, 95% CI 2.6-19.9, respectively). There was no difference found between anticoagulation or antiplatelet status in these patients (P=.543, Table S1). No difference in one-year mortality between the super-users and non-super-users was found.
DISCUSSION
(91.3)
Anticoagulation
Ambulatory status n (%)
Walking
Wheelchair/ bedbound
Unknown
(28.9)
72 (48.3)
(30.2)
(21.5)
BLS, Basic Life Support; ALS, Advanced Life Support.
anticoagulation or antiplatelet medications (42.9% vs 61.7%, P = .05) and being non-ambulatory (29.0% vs 56.8%, P =.001) (Table S1).
In the present study, we demonstrate an increased odds of 30-day ED visits and hospitalization and six-month ED visits and hospitalization for both repeat EMS callers and EMS super-users who decline transport after a fall. Our study is different from prior studies in several ways. Our patient population was 9-12 years younger than patients in prior studies, meaning EMS personnel should be aware that a younger cohort of patients is still at risk of needing medical assistance in the immediate future.3,13,14 Further, our study stratifies patients into either repeat callers or super-users of EMS to assess 30-day and six-month outcomes, while others looked at 14-day outcomes for lift-assist patients and did not further analyze this distinct subset of patients.3,15 Finally, Mikolaizak et al demonstrated that 49% of fall victims experienced unplanned healthcare assessments within 28 days.7 Our study shows a higher percentage of 30-day ED visits for both repeat callers and super-users (66% and 70.4%, respectively, Table 2). This suggests that the prehospital approach to fall victims should be structured to address shortand long-term outcomes.
Anti-coagulation and ambulatory status in repeat callers, but not super-users, was the only statistically significant medical history difference between repeat callers. Thus, the presence or absence of certain demographic or medical characteristics is unlikely to be generalizable, and we may need to consider other factors when triaging fall victim patients, including the fall location (public vs private space), fall-related EMS call history, depression, polypharmacy, and diabetes.16,17,18
The EMS responders may be the first or only medical personnel to be aware of patient falls, as patients may underreport falls to their primary care practitioners.19 One study has
Table 2. Proportion of repeat/non-repeat callers and super utilizers/non-super users and their odds ratio for specific emergency department visits and hospital admissions in 30 days/six months and deaths.
Non-repeat (n = 69)
Repeat (n=47) Odds ratio (95% CI)
ED Visits in 6 months, n
Non-super-user (n = 89)
Deaths n (%)
ED, emergency department; CI, confidence interval.
demonstrated EMS positively screened 61% of future fall risk.20 However, screening and education are tools for identifying at-risk patients but may not address risk factors for future falls.21 Emergency medical services referral programs also have demonstrated moderate success with patient referral for social service-related events.22
LIMITATIONS
This was a retrospective, observational study reliant on chart review. We were unable to determine living arrangements or ambulation status in almost one-third of patients, factors that may only be documented if the EMS responder thought it was relevant. Cognitive impairment and other potentially relevant characteristics may not have been charted by EMS. This limits conclusions for which patient characteristics are highly associated with increased EMS use and at risk for future healthcare utilization. Additionally, only calls classified as “fall victims” in the prehospital EHR were assessed. Because the calls are characterized by the EMS dispatchers, patients may have been misclassified. We may have also missed patients if they used a different EMS company for repeat calls and were transferred to hospitals outside of the CUHC EMS catchment area.
Additionally, we did not find a significant difference in patients with abnormal or incomplete vital signs. In instances where vital signs were abnormal, EMS may have been able to convince patients to go to the ED. This would represent patients who initially wanted to decline transport, but EMS intervened to persuade these higher risk patients to seek treatment.
CONCLUSION
Anticoagulation and non-ambulatory status are associated with patients who use EMS after a fall but subsequently decline medical transport. Patients with repeated EMS calls are significantly more likely to have ED visits and hospital admissions at 30 days and six months after the initial fall.
Address for Correspondence: Alexander Kuc, MD, Cooper University Health Care, Department of Emergency Medicine, 401 Broadway, Camden, NJ 08103. Email: kuc@rowan.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Barr et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Moreland B, Kakara R, Henry A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years - United States, 2012-2018. Morb Mortal Wkly Rep. 2020;69(27):875-81.
2. Kakara R, Bergen G, Burns E, et al. Nonfatal and fatal falls among adults aged ≥65 years - United States, 2020-2021. Morb Mortal Wkly Rep. 2023;72(35):938-43.
3. Leggatt L, Van Aarsen K, Columbus M, et al. Morbidity and mortality associated with prehospital “lift-assist” calls. Prehosp Emerg Care 2017;21(5):556-62.
4. Shankar K, Liu S, Ganz D. Trends and characteristics of emergency department visits for fall-related injuries in older adults, 2003-2010. West J Emerg Med. 2017;18(5):785-93.
5. Quatman CE, Mondor M, Halweg J, et al. Ten years of EMS fall calls in a community: an opportunity for injury prevention strategies. Geriatr Orthop Surg Rehabil. 2018;9:215145931878345.
6. Knight S, Olson LM, Cook LJ, et al. Against all advice: an analysis of out-of-hospital refusals of care. Ann Emerg Med. 2003;42(5):689-96.
7. Mikolaizak AS, Simpson PM, Tiedemann A, et al. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australas J Ageing 2013;32(3):147-57.
8. Cone DC, Ahern J, Lee CH, et al. A descriptive study of the “liftassist” call. Prehosp Emerg Care. 2013;17(1):51-6.
9. Schierholtz T, Carter D, Kane A, et al. Impact of lift assist calls on paramedic services: a descriptive study. Prehosp Emerg Care 2019;23(2):233-40.
10. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
11. Moe J, Kirkland SW, Rawe E, et al. Effectiveness of interventions to decrease emergency department visits by adult frequent users: a systematic review. Acad Emerg Med. 2017;24(1):40-52.
12. Evans CS, Platts-Mills TF, Fernandez AR, et al. Repeated emergency medical services use by older adults: analysis of a comprehensive statewide database. Ann Emerg Med. 2017;70(4):506-15.e3.
13. Liu SW, Obermeyer Z, Chang Y, et al. Frequency of ED revisits and death among older adults after a fall. Am J Emerg Med 2015;33(8):1012-8.
14. Donald IP, Bulpitt CJ. The prognosis of falls in elderly people living at home. Age Ageing. 1999;28(2):121-5.
15. Coster J, O’Cathain A, Jacques R, et al. Outcomes for patients who
contact the emergency ambulance service and are not transported to the emergency department: a data linkage study. Prehosp Emerg Care. 2019;23(4):566-77.
16. Jeruzal JN, Boland LL, Jin D, et al. Trends in fall-related encounters and predictors of non-transport at a US emergency medical services agency. Health Soc Care Community. 2022;30(5):e1835-43.
17. Tchalla AE, Dufour AB, Travison TG, et al. Patterns, predictors, and outcomes of falls trajectories in older adults: the MOBILIZE Boston Study with 5 years of follow-up. PLoS One. 2014;9(9):e106363.
18. Carpenter CR, Avidan MS, Wildes T, et al. Predicting geriatric falls following an episode of emergency department care: a systematic review. Acad Emerg Med. 2014;21(10):1069-82.
19. Hoffman GJ, Ha J, Alexander NB, et al. Underreporting of fall injuries of older adults: implications for wellness visit fall risk screening. J Am Geriatr Soc. 2018;66(6):1195-200.
20. Shah MN, Brooke Lerner E, Chiumento S, et al. An evaluation of paramedics’ ability to screen older adults during emergency responses. Prehosp Emerg Care. 2004;8(3):298-303.
21. Shah MN, Clarkson L, Lerner EB, et al. An Emergency medical services program to promote the health of older adults. J Am Geriatr Soc. 2006;54(6):956-62.
22. Kue R, Ramstrom E, Weisberg S, et al. Evaluation of an emergency medical services–based social services referral program for elderly patients. Prehosp Emerg Care. 2009;13(3):273-9.
Untreated Hypertension and Diabetes in the Chest Pain Observation Unit
Benjamin T. Hutchison, MD*
Nicklaus P. Ashburn, MD, MS*
Anna C. Snavely, PhD*†
Michael D. Shapiro, DO, MCR‡
Michael A. Chado, MD§
Alexander P. Ambrosini, MD||
Amir A. Biglari, MD*
Harris A. Cannon, MD*
Marissa J. Millard, BS*
Alexa G. Dameron, BS*
Simon A. Mahler, MD, MS*#¶
*
Wake Forest University School of Medicine, Department of Emergency Medicine, Wake Forest University, Winston-Salem, North Carolina
Wake Forest University School of Medicine, Department of Biostatistics and Data Science, Wake Forest University, Winston-Salem, North Carolina
Wake Forest University School of Medicine, Section on Cardiovascular Medicine, Department of Internal Medicine, Wake Forest University, Winston-Salem, North Carolina Ohio State University, Department of Emergency Medicine, Columbus, Ohio
Yale School of Medicine, Department of Internal Medicine, New Haven, Connecticut
Wake Forest University School of Medicine, Department of Epidemiology and Prevention, Wake Forest University, Winston-Salem, North Carolina
Wake Forest University School of Medicine, Department of Implementation Science, Wake Forest University, Winston-Salem, North Carolina
Section Editor: Mark I Langdorf, MD, MHPE
Submission history: Submitted January 4, 2025; Revision received March 30, 2025; Accepted May 6, 2025
Electronically published September 12, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.41560
Introduction: Hypertension and diabetes are common cardiovascular disease risk factors among emergency department observation unit (EDOU) patients evaluated for acute coronary syndrome (ACS). Our primary aim was to determine rates of untreated hypertension and diabetes in the EDOU. Our secondary aim was to identify rates of glycemic control assessment among patients with diabetes.
Methods: We conducted a retrospective, observational cohort study of patients ≥ 18 years old evaluated for ACS in a tertiary care center EDOU from March 3, 2019–February 28, 2020. Known diagnoses prior to EDOU encounter and new outpatient diagnoses within one year for hypertension and diabetes were identified by health record data. We defined untreated hypertension and diabetes as no antihypertensive or antihyperglycemic prescriptions or diabetes counseling within one year. We calculated treatment rates with exact 95% confidence intervals (CI). Multivariable logistic regression adjusting for age, sex, and race compared treatment rates among men vs women and White vs non-White patients. Rates of glycemic control assessment were defined by the proportion of patients with known diabetes who received hemoglobin A1c (HbA1c) measurement within one year.
Results: Among 649 EDOU patients, 59.5% (386/649) were female and 43.8% (284/649) were nonWhite with a mean age of 59 ± 12 years. Of these, 76.9% (499/649) had known hypertension and 31.3% (203/649) had known diabetes. Within one year, 3.1% (20/649) had newly diagnosed hypertension and 3.2% (21/649) had newly diagnosed diabetes. Among those with known or newly diagnosed hypertension, untreated hypertension occurred in 36.4% (189/519; 95% CI 32.3 - 40.7). Hypertension treatment rates were similar in men vs women (aOR [adjusted odds ratio] 0.82, 95% CI 0.57 - 1.19) and White vs nonWhite patients (aOR 0.95, 95% CI 0.66 - 1.38). Among those with known or newly diagnosed diabetes, untreated diabetes occurred in 25.0% (56/224; 95% CI 18.5 - 31.2). Diabetes treatment rates were similar in men vs women (aOR 1.41, 95% CI 0.72 - 2.74) and White vs. non-White patients (aOR 1.05, 95% CI 0.56 - 1.97). At one year, just 32.0% (65/203) of patients with diabetes had HbA1c testing.
Conclusion: Given that many patients evaluated for acute coronary syndrome in the ED observation unit do not receive treatment for hypertension and diabetes within one year of presentation, clinicians should consider initiating EDOU-based preventive cardiovascular care for these conditions. [West J Emerg Med. 2025;26(5)1296–1304.]
INTRODUCTION
Hypertension and diabetes are independent risk factors for atherosclerotic cardiovascular disease (ASCVD) and represent substantial causes of all-cause mortality and healthcare costs in the United States. Hypertension affects up to 46% of American adults and is the most prevalent cardiovascular risk factor worldwide.1,2 It is also the single most significant and modifiable risk factor for stroke and cardiovascular disease.3 Diabetes represents another consequential chronic disease and is the leading cause of preventable deaths in the US, currently affecting over 38 million Americans.1,4
Due to their strong association with ASCVD, hypertension and diabetes are commonly found in patients presenting to the emergency department (ED) with acute chest pain, which accounts for > 7.0 million ED visits per year.5-9 An estimated 25 million patients present to the ED with asymptomatic hypertension each year, but < 4% are discharged with antihypertensive therapy.10 Given the strong association of hypertension with all-cause mortality, the American College of Emergency Physicians (ACEP) guidelines recommend considering initiation of antihypertensive medication for asymptomatic hypertension in select patients, although this practice is rarely followed by emergency clinicians.10,11
Similarly, while some have recommended formally diagnosing and treating new diabetes in the ED, there is no widely accepted practice recommendation supporting these practices.9,12,13 Therefore, management of new or uncontrolled asymptomatic hypertension or diabetes in the ED is often viewed as an outpatient condition and rarely addressed in the acute care setting. Although emergency clinicians often advise these patients to follow up with their primary care physician for further management, many patients fail to receive appropriate outpatient care in a timely manner after ED discharge, including the recommended twice yearly hemoglobin A1c (HbA1c) testing of those with diabetes.14,15 Thus, there may be an opportunity for emergency clinicians to initiate preventive cardiovascular care for patients presenting with acute chest pain in the ED and ED observation units (EDOU) by treating hypertension and diabetes.
To assess the possible impact of EDOU-initiated preventive cardiovascular care for hypertension and diabetes, we evaluated a cohort of patients presenting with acute chest pain to the ED/ EDOU of a large, academic, tertiary-care center. Our primary aim was to evaluate rates of untreated hypertension and diabetes in the EDOU. We hypothesized that while many patients evaluated in the EDOU would have hypertension and diabetes, most would not receive treatment for their known hypertension or diabetes in the EDOU or within one year after EDOU discharge. We also assessed the proportion of patients without a previous diagnosis of hypertension or diabetes who received treatment for newly diagnosed hypertension and diabetes within the one-year followup period. As a secondary aim, we assessed rates of glycemic control testing in patients with known diabetes by determining whether these patients received HbA1c measurement in the EDOU or within one year of EDOU encounter. Given known
Population Health Research Capsule
What do we already know about this issue?
Hypertension and diabetes are common risk factors for cardiovascular disease among patients evaluated for acute coronary syndrome (ACS) in the ED observation unit (EDOU).
What was the research question?
Among those evaluated for ACS in the EDOU, what is the 1-year treatment rate for hypertension and diabetes?
What was the major finding of the study?
Over one year, untreated hypertension occurred in 36.4% and untreated diabetes occurred in 25.0%.
How does this improve population health?
Many patients in the EDOU have untreated hypertension and diabetes within one year of presentation, suggesting possible opportunities to initiate EDOU-based care.
disparities in cardiovascular care among women and non-White patients, we also evaluated for potential disparities in the treatment of these conditions and for glycemic control evaluations among patients with diabetes.16-20
METHODS
Study Design
We conducted a retrospective, observational, cohort study of patients presenting with acute chest pain and evaluated for possible acute coronary syndrome (ACS) in the EDOU of a large, academic teaching hospital from March 1, 2019 – February 28, 2020 by leveraging the Wake Forest EDOU Chest Pain Registry. The Wake Forest University Health Sciences Institutional Review Board reviewed and approved the study protocol and granted a waiver of informed consent for the study. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines helped direct the research and reporting processes.21
Study Setting and Population
The study included patients ≥ 18 years of age being evaluated for possible ACS in the EDOU at Atrium Health Wake Forest Baptist, a large, academic teaching hospital in North Carolina. The study cohort was comprised of a convenience sample of consecutive patients. The EDOU is a type 1, protocoldriven observation unit and is managed by emergency physician assistants and nurse practitioners who are supervised by board-
Hutchison
certified or board-eligible emergency physicians. Patients with ST-segment elevation myocardial infarction, hemodynamic instability (heart rate < 40 or > 120 beats per minute, systolic blood pressure < 90 millimeters of mercury mmHg, or oxygen saturation SpO2% < 90% on room air or normal home oxygen flow rate), high-sensitivity cardiac troponin I (Beckman Coulter Diagnostics Brea, CA) ≥ 100 nanograms per liter, or trauma were not eligible for EDOU care and, thus, were excluded from the study. The EDOU chest pain protocol is available in Supplemental Appendix A. Per the EDOU chest pain protocol, patients were evaluated for potential ACS with serial troponin measurements, telemetry, and possible stress testing or coronary computed tomography angiography. During the study, no specific additional training or guidance was provided to clinicians in the EDOU regarding hypertension or diabetes management.
Data Collection and Variables
Index encounter data (from initial ED presentation to discharge from the EDOU) through one year of outpatient follow-up were abstracted from the electronic health record (EHR) (Epic Systems Corporation, Verona, WI) by trained data abstractors and entered into the Wake Forest EDOU Chest Pain Registry. Outpatient follow-up included any primary care or specialty clinic visits captured in the EHR system for our health system network. All network hospitals and outpatient clinics share the same EHR, and the network is the largest in the region, making it likely to capture the vast majority of follow-up visits for patients in the study. We previously performed insurance claims analysis of our network EHR, which found very few events at outside network hospitals, confirming the reliability of in-network EHR follow-up visit rates.22
Hypertension and diabetes diagnoses, sex, race, and medication use were identified by patient self-report, International Classification of Diseases, 10th Rev, ICD-10 codes, and/or clinician documentation in the EHR. Initiation of antihypertensive medication, diabetes treatment, and/or measurement of HbA1c in the EDOU and future outpatient visits were also abstracted from the EHR. Data were entered into a Research Electronic Data Capture (REDCap) database hosted at Wake Forest University School of Medicine. We followed best practice guidelines for data abstraction, including data abstractor training and optimizing case selection criteria using variable definitions, as well as a data dictionary and standardized digital abstraction forms within REDCap.23,24 Data abstractor performance was monitored throughout the study period.23,24 Training included in-person instruction with the principal investigator (PI) where patient encounters and data were reviewed to ensure familiarity with accessing relevant data in the EHR and inputting data into REDCap. Additionally, the PI reviewed a random sample of entries to ensure accuracy.
Outcomes
Study outcomes were 1) the proportion of patients with known or newly diagnosed hypertension who received
antihypertensive treatment at their index EDOU visit and within the one-year follow-up period, and 2) the proportion of patients with known or newly diagnosed diabetes who received diabetes treatment at their EDOU index visit and within the one-year follow-up period. New diagnoses of hypertension and diabetes were defined by patients with new diagnoses by outpatient clinician documentation or ICD-10 code during the one-year follow-up period. We defined untreated hypertension as a patient with known or newly diagnosed hypertension who did not receive antihypertensive treatment at their index EDOU visit or within one year of follow-up. Untreated diabetes was defined as a patient with known or newly diagnosed diabetes who did not receive diabetes treatment at their index visit or within one year of follow-up. Consistent with prior studies, patients without documentation of one-year follow-up for either testing or treatment in the EHR (i.e., those “lost to follow-up”) were assumed to not have received care.
We defined antihypertensive treatment as any blood pressure-lowering agent, such as an angiotensin-convertingenzyme inhibitor, angiotensin-receptor blocking agent, beta blocker, calcium channel blocker, hydralazine, or diuretic (including loop diuretic, thiazide diuretics, and potassiumsparing diuretics). Diabetes treatment was defined as the composite of any anti-hyperglycemic drug treatment (insulin, metformin, dipeptidyl peptidase-4 inhibitor, or glucagon-like peptide-1 receptor antagonists) or documentation of diabetes counseling. A secondary outcome measure was rates of glycemic control assessment, defined as having an HbA1c measurement in the EDOU or in the one-year follow-up period among patients with a known diagnosis of diabetes.
Statistical Analysis
We used counts, percentages, and means with standard deviations to describe the study population. Rates of antihypertensive treatment, diabetes treatment (including drug treatment and counseling), and diabetes evaluation (HbA1c testing) during the index EDOU encounter and the one-year follow-up period inclusive of the index EDOU encounter were calculated and reported along with exact 95% confidence intervals (CI). We used Fisher exact test to compare rates of hypertension treatment, diabetes treatment, and diabetes evaluation at one year among White vs non-White patients and men vs women. To further evaluate the association of race and sex with hypertension and diabetes treatment at one year, we performed multivariable logistic regression adjusting for age (continuous), race (White vs non-White), and sex (male vs female). Unadjusted and adjusted odds ratios (aOR) with corresponding 95% CIs were calculated.
RESULTS
During the study period, 649 patients were evaluated in the EDOU for possible ACS, of whom 59.5% (386/649) were female and 43.8% (284/649) were non-White with a mean age
Hutchison
Untreated Hypertension and Diabetes in the Chest Pain Observation Unit
of 59.8 ± 12.3 years. Among these patients, 76.9% (499/649) had known hypertension and 31.3% (203/649) had known diabetes. During the one-year follow-up period, 69.7% (452/649) were evaluated in an outpatient clinic for any reason. Newly diagnosed hypertension occurred in 13.3% (20/150) of patients without a previous diagnosis of hypertension, and newly diagnosed diabetes occurred in 4.7% (21/446) of patients without a previous diagnosis of diabetes. Table 1 describes the cohort characteristics. Untreated hypertension occurred in 36.4% (189/519; 95% CI 32.3 - 40.7) of patients with known or newly diagnosed hypertension. These patients did not receive any form of antihypertensive treatment while in the EDOU or during the one-year follow-up period (Figure 1). In addition, untreated diabetes was observed in 25.0% (56/224; 95% CI 18.5 - 31.2) of patients with known or newly diagnosed diabetes. These patients did not receive any type of antihyperglycemic treatment or diabetes counseling while in the EDOU or during the one-year follow-up period (Figure 2). Differences in treatment rates for hypertension and diabetes among those with known or new diagnoses are summarized in Table 2. Finally, rates of glycemic control assessment among diabetics were low, as just 32.0% (65/203) of patients with known diabetes had a HbA1c measurement within one year of their EDOU encounter (Figure 3). Furthermore, only 11.3% (23/203) of patients with known diabetes received HbA1c evaluation in the EDOU. For hypertension, treatment rates at one year were similar in White vs. non-White patients (63.2% [172/272] vs 64.0% [158/247]; P = .93) and in men vs women (60.2% [124/206] vs 65.8% [206/313]; P = .23). The rate of diabetes treatment at one year
was also similar in White vs non-White patients (75.5% [74/98] vs 74.6% [94/126], P = 1.0) and in men vs women (79.8% [67/84] vs 72.1% [101/140], P = .26). After adjusting for potential confounders, hypertension and diabetes treatment rates remained similar between White vs non-White patients and between men vs women. Table 3 represents rates of hypertension treatment among race and sex subgroups, while Table 4 describes rates of diabetes treatment among race and sex subgroups.
DISCUSSION
This study demonstrates substantial rates of untreated hypertension and diabetes and reveals the potential for ED-initiated preventive cardiovascular care among patients with acute chest pain evaluated in an EDOU. Approximately 80% of chest pain observation patients had hypertension, and over one-third had diabetes. Despite the high prevalence of these key cardiovascular disease risk factors, many did not receive appropriate medical therapy within one year of their emergency care encounter. Even fewer patients received preventive care while in the EDOU. These findings suggest that we may be missing an opportunity to impact long-term health outcomes in patients during their EDOU visit. Given the enormous impact that hypertension and diabetes treatment have on ASCVD risk and overall mortality, the US Department of Health and Human Services aims to improve cardiovascular health with the Healthy People 2030 initiative, specifically encouraging advancements in adult hypertension control and ASCVD risk assessment.25 Lowering
Hutchison et al.
Table 1. Cohort characteristics of patients with known and new diagnoses of hypertension and diabetes.

Figure 1. Untreated hypertension in the emergency department observation unit.
1New diagnoses of hypertension made at outpatient visits during the 1-year follow-up period of 150 of patients with no known hypertension prior to EDOU encounter.
2Treatment for hypertension at outpatient visit within 1 year of EDOU encounter of 519 of patients with known or new diagnoses of hypertension.
3No treatment in EDOU or within 1 year of 519 of patients with known or new diagnoses of hypertension, EDOU, emergency department observation unit.
blood pressure and controlling glucose levels in patients with hypertension and diabetes reduces rates of cardiovascular disease and improves mortality.2,26-31 While initiating appropriate preventive cardiovascular care can have lifesaving effects, current practice guidelines regarding this practice in the ED are limited and not uniformly followed.
Many patients with hypertension and diabetes may not receive guideline-directed care in the outpatient setting after ED discharge, which we redemonstrated in our EDOUspecific study.31-34 Although ACEP guidelines encourage emergency clinicians to consider providing lifestyle counseling and initiating low-dose pharmacotherapy in select high-risk groups in the ED, there is limited literature to inform current practice in the ED and EDOU.11,35 While initiating preventive care from the ED is not currently standard practice, the high rates of patients who are unable to receive outpatient care in the outpatient setting may highlight an opportunity to initiate potentially life-saving preventive care in the ED setting. We recommend further study and discussion to improve practice guidelines for preventive care in the EDOU.
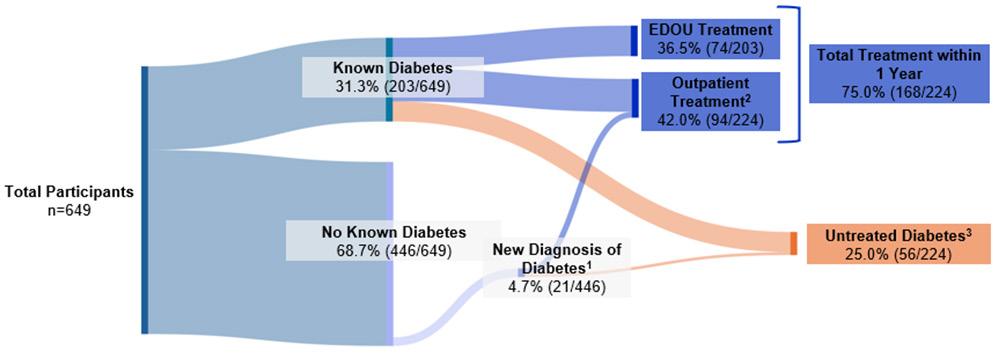
Figure 2. Untreated diabetes in the emergency department observation unit.
1 New diagnoses of diabetes made at outpatient visits during the 1-year follow-up period of 446 of patients with no known diabetes prior to EDOU encounter.
2 Treatment for diabetes at outpatient visit within 1 year of EDOU encounter out of n=224 of patients with known or new diagnoses of diabetes,
3 No treatment in EDOU or within 1 year of 224 of patients with known or new diagnoses of diabetes. EDOU, emergency department observation unit.
Table 2. Treatment rates of patients with known and new diagnoses of hypertension and diabetes.
Known hypertension n = 499, (%) New hypertension diagnosis1 n= 20, (%) Known diabetes n = 203, (%) New diabetes diagnosis1 n = 21, (%)
Untreated Condition2 184 (36.9) 5 (25.0)
(24.1) 7 (33.3)
Treatment in the EDOU 1 (0.2) N/A3 74 (36.5) N/A3
Treatment within 1 Year 314 (62.9) 15 (75.0) 80 (39.4) 14 (66.7)
1 New diagnoses of hypertension or diabetes made at outpatient visits during the 1-year follow-up period.
2 No treatment in EDOU or within 1 year.
3 Patients with new diagnoses of hypertension or diabetes within the 1-year follow-up period did not receive treatment while in the EDOU. EDOU, emergency department observation unit.
There may be barriers to implementing preventive cardiovascular care in the ED and EDOU. Potential barriers to ED-initiated preventive care include the loud, busy, and chaotic nature of the ED, which is not always conducive to preventive care practices such as lifestyle modification counseling. Furthermore, staff constraints, limited resources, and the presence of other high-acuity emergencies may also pose barriers to initiating care for hypertension and diabetes. Amidst these barriers, prior studies have highlighted the challenge for emergency clinicians to address public health concerns and preventive medicine.36 The EDOU may, however, be more conducive to implementing preventive care for these comorbidities. In the EDOU, patients can more easily receive serial blood pressure measurements, further diagnostic testing like HbA1c, and effective lifestyle counseling. Future work and implementation studies are needed to develop high-impact, evidence-based medical decision-making frameworks and best practice recommendations to help emergency clinicians deliver preventive care.
Data are limited on the use of the EDOU for treatment of hypertension and diabetes. While some studies have assessed the prevalence of asymptomatic hypertension and diabetes in the ED, few have examined the impact of treating these conditions in the ED or EDOU on patient-centered outcomes.8,10,37,38 A recent expert opinion review provided recommendations for hypertension management in the EDOU and emphasized the feasibility of accurate diagnosis and initiation of treatment in the EDOU.34 While a recent randomized controlled trial evaluated management of asymptomatic hypertension in the ED and demonstrated feasibility for ED-based treatment, this was in the ED setting rather than an observation unit.39 The data for diabetes treatment in the ED or EDOU are even more sparse, with no high-quality or clinical trial evidence to help guide emergency clinicians. Our own research group has previously described other untreated cardiovascular conditions in the EDOU and has highlighted the potential for emergency clinicians to initiate potentially life-saving therapies such as smoking cessation and lipid-lowering medications.40-43 Together, these findings suggest that the EDOU may be an appropriate location for initiating
comprehensive preventive cardiovascular care for multiple cardiovascular disease risk factors.
As we explored rates of glycemic control assessments among patients with known diabetes, we found there may be an opportunity to improve diabetes testing in the EDOU. Current guidelines recommend HbA1c testing at least twice per year in patients with known diabetes.44,45 While many patients being evaluated for ACS in the EDOU have known diabetes, just 32% of these patients were evaluated for diabetes within one year of their EDOU encounter, suggesting there may be a possible opportunity for EDOU-based glycemic control evaluation in some patients being evaluated for ACS.46 Additional studies are needed to further explore this
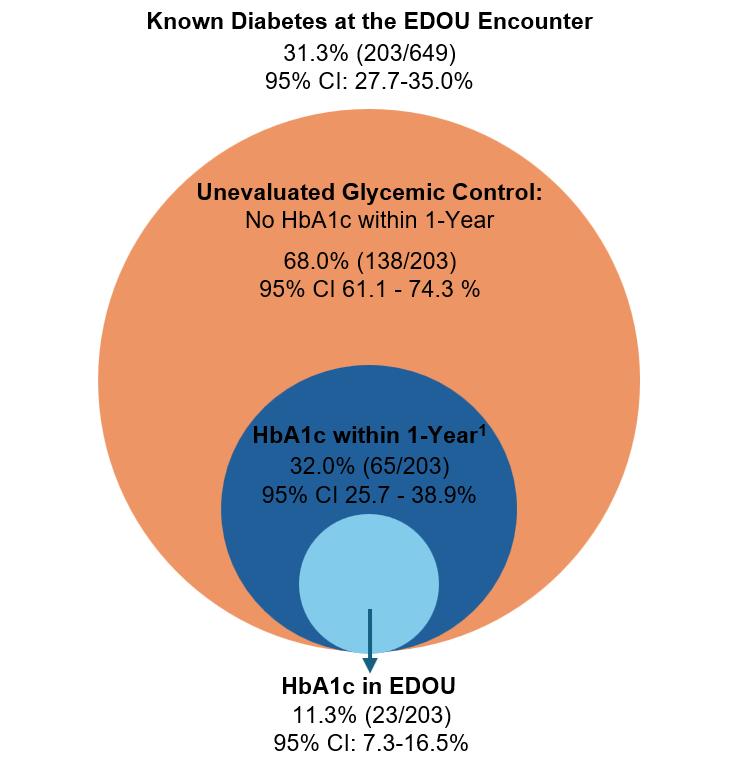
Figure 3. Rates of HbA1c testing in the emergency department observation unit among patients with known diabetes.
1HbA1c measurement in EDOU or outpatient clinic visit within 1 year of EDOU encounter. EDOU, emergency department observation unit; HbA1c, hemoglobin A1C; CI, confidence interval.
Table 3. Rates of hypertension treatment among patients with known and newly diagnosed hypertension by race (White vs non-White) and sex (male vs. female).
1Adjusted for age (continuous) and sex (male vs female).
2Adjusted for age (continuous) and race (White vs non-White).
3Unable to adjust due to the lower number of events. EDOU, emergency department observation unit; OR, odds ratio; CI, confidence interval.
potential missed opportunity.
Importantly, our study did not find significant differences in hypertension and diabetes treatment among sex or race groups. Of note, the rate of diabetes treatment within one year of the index EDOU visit was 8% higher among men than women. While not statistically significant, this could have been due to our cohort’s modest sample size. Given this finding and the ample literature highlighting disparities in diabetes and hypertension care among men and women, future ED and EDOU preventive cardiovascular care disparities research is warranted.16-20
LIMITATIONS
This study has limitations. While the study was conducted at one academic center and focused on EDOU patients, many EDs now operate protocol-driven EDOUs. Although this study was retrospective, best practices for retrospective review were used to enhance accuracy and scientific rigor. It is possible that patients may have had outpatient clinic visits or treatment initiated at outside medical systems not available in our EHR, thereby introducing a potential source of misclassification bias. However, our health system is the largest in the region
with all network hospitals and outpatient clinic sites sharing the same EHR.
While our study was able to evaluate for rates of glycemic control assessments by measuring rates of HbA1C ordering in diabetics, we were unable to similarly assess blood pressure control assessments in patients with known hypertension, as we did not have access to all blood pressure measurements within one year. However, we did assess new diagnoses of hypertension as reported by clinician documentation or EHR data. Similarly, for patients initiated on hypertension or diabetes treatment, we did not monitor treatment adherence over one year. While the study adhered to most best practices for optimal chart review, our data abstractors were not blinded to the study hypothesis, we did not report on interrater reliability, and we did not formally measure percentage agreement or Kappa.24 Lastly, the precision of our study was limited by the modest sample size.
CONCLUSION
This study highlights high rates of untreated hypertension and diabetes in the emergency department observation unit. Because large numbers of patients with
Table 4. Rates of diabetes treatment among patients with known and newly diagnosed diabetes by race (White vs non-White) and sex (male vs. female).
1Adjusted for age (continuous) and sex (male vs female).
2Adjusted for age (continuous) and race (White vs non-White).
EDOU, emergency department observation unit; OR, odds ratio; CI, confidence interval.
hypertension and diabetes did not receive appropriate treatment in the outpatient setting, the EDOU may be an appropriate place to bridge this gap in care. Similarly, most patients with diabetes did not receive an adequate glycemic control evaluation within one year, so there may be opportunity for EDOU-based HbA1c assessments in these patients. Given the potential life-saving risk reduction associated with hypertension and diabetes management, emergency clinicians may be able to help mitigate mortality by initiating proper treatment in the EDOU. We recommend additional investigation with pilot intervention models in the EDOU to assess the feasibility and effectiveness of EDOUinitiated hypertension and diabetes treatment programs.
ACKNOWLEDGMENTS
We would like to thank Spencer Kitchen, Gregory Noe, Ian Kinney, Ryan Morgan, Weston Colbaugh, Ravenna Chhabria, Benjamin Brendamour, James Black, and Philip Kayser for their assistance with data collection.
Address for Correspondence: Benjamin T Hutchison MD, Department of Emergency Medicine, Wake Forest University School of Medicine, Wake Forest University, Medical Center Boulevard, Winston-Salem, NC 27157. Email: benjamin.hutchison@ advocatehealth.org.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Dr. Ashburn receives funding from NHLBI (K23HL169929), AHRQ (R01HS029017), and the Emergency Medicine Foundation. Dr. Snavely receives funding from NHLBI (K23HL169929), Abbott Laboratories, HRSA (1H2ARH399760100), AHRQ (R01HS029017 and R21HS029234), and the Emergency Medicine Foundation. Dr. Shapiro is supported by institutional grants from Amgen, Arrowhead, Boehringer Ingelheim, 89Bio, Esperion, Novartis, Ionis, Merck, New Amsterdam, and Cleerly. He has participated in Scientific Advisory Boards with Amgen, Agepha, Ionis, Novartis, New Amsterdam, and Merck. He has served as a consultant for Ionis, Novartis, Regeneron, Aidoc, Shanghai Pharma Biotherapeutics, Kaneka, Novo Nordisk, Arrowhead, and Tourmaline. Dr. Mahler receives funding/support from Roche Diagnostics, Abbott Laboratories, QuidelOrtho, Siemens, Grifols, Pathfast, Beckman Coulter, Genetesis, Cytovale, National Foundation of Emergency Medicine, BlueJay Diagnostics, Duke Endowment, Brainbox, HRSA (1H2ARH399760100), the Emergency Medicine Foundation, and AHRQ (R01HS029017 and R21HS029234). He is a consultant for Roche, QuidelOrtho, Abbott, Siemens, Inflammatix, and Radiometer and is the Chief Medical Officer for Impathiq Inc. No other author has professional or financial relationships with any companies that are relevant to this study. There are no other conflicts of interest or sources of funding to declare.
Copyright: © 2025 Hutchison et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4):e1000058.
2. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.
3. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115.
4. Joseph JJ, Deedwania P, Acharya T, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation. 2022;145(9):e722-59.
5. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/ SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-454.
6. Cairns C, Kang K. National Hospital Ambulatory Medical Care Survey: 2019 Emergency Department Summary Tables. 2022. Available at: https://stacks.cdc.gov/view/cdc/115748 Accessed September 4, 2025.
7. MacLeod KE, Ye Z, Donald B, et al. A literature review of productivity loss associated with hypertension in the United States. Popul Health Manag. 2022;25(3):297-308.
8. Baumann BM, Cline DM, Pimenta E. Treatment of hypertension in the emergency department. J Am Soc Hypertens. 2011;5(5):366-377.
9. Schwartz X, Porter B, Gilbert MP, et al. Emergency department management of uncomplicated hyperglycemia in patients without history of diabetes. J Emerg Med. 2023;65(2):e81-92.
10. Akhetuamhen A, Bibbins-Domingo K, Fahimi J, et al. Missed opportunities to diagnose and treat asymptomatic hypertension in emergency departments in the United States, 2016-2019. J Emerg Med. May 2024;66(5):e562-70.
11. Wolf SJ, Lo B, Shih RD, et al. American College of Emergency Physicians Clinical Policies C. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013;62(1):59-68.
12. Sop J, Gustafson M, Rorrer C, et al. Undiagnosed diabetes in patients admitted to a clinical decision unit from the emergency department: a retrospective review. Cureus. 2018;10(10):e3390.
13. McNaughton CD, Self WH, Slovis C. Diabetes in the emergency department: acute care of diabetes patients. Clin Diabetes 2011;29(2):51-9.
14. Kilaru AS, Illenberger N, Meisel ZF, et al. Incidence of timely outpatient follow-up care after emergency department encounters for
Hutchison
acute heart failure. Circ Cardiovasc Qual Outcomes 2022;15(9):e009001.
15. Lin MP, Burke RC, Orav EJ, et al. Ambulatory follow-up and outcomes among Medicare beneficiaries after emergency department discharge. JAMA Netw Open. 2020;3(10):e2019878
16. Aggarwal R, Chiu N, Wadhera RK, et al. Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the United States, 2013 to 2018. Hypertension. 2021;78(6):1719-26.
17. Abrahamowicz AA, Ebinger J, Whelton SP, et al. Racial and ethnic disparities in hypertension: barriers and opportunities to improve blood pressure control. Curr Cardiol Rep. 2023;25(1):17-27.
18. Pana TA, Luben RN, Mamas MA, et al. Long term prognostic impact of sex-specific longitudinal changes in blood pressure. The EPICNorfolk Prospective Population Cohort Study. Eur J Prev Cardiol 2022;29(1):180-91.
19. Connelly PJ, Currie G, Delles C. Sex differences in the prevalence, outcomes and management of hypertension. Curr Hypertens Rep 2022;24(6):185-92.
20. Kautzky-Willer A, Leutner M, Harreiter J. Sex differences in type 2 diabetes. Diabetologia. 2023;66(6):986-1002.
21. Cuschieri S. The STROBE guidelines. Saudi J Anaesth 2019;13(Suppl 1):S31-4.
22. Mahler SA, Lenoir KM, Wells BJ, et al. Safely identifying emergency department patients with acute chest pain for early discharge: HEART pathway accelerated diagnostic protocol. Circulation. 2018;138(22):2456-68.
23. Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64(3):292-8.
24. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
25. Heart Disease and Stroke. Available at: https://health.gov/ healthypeople/objectives-and-data/browse-objectives/heart-diseaseand-stroke. Accessed: December 1, 2024.
26. Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903-13.
27. Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2(7):775-81.
28. Muntner P, Carey Robert M, Gidding S, et al. Potential U.S. population Impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71(2):109-18.
29. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74(10):e177-232.
30. Committee ADAPP. 10. Cardiovascular Disease and Risk
Management: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2021;45(Supplement_1):S144-74.
31. Nelson AJ, O’Brien EC, Kaltenbach LA, et al. Use of lipid-, blood pressure–, and glucose-lowering pharmacotherapy in patients with type 2 diabetes and atherosclerotic cardiovascular disease. JAMA Netw Open. 2022;5(2):e2148030.
32. Fan Z, Yang C, Zhang J, et al. Trends and influence factors in the prevalence, awareness, treatment, and control of hypertension among US adults from 1999 to 2018. PLoS One 2023;18(9):e0292159.
33. Fang M, Wang D, Coresh J, et al. Trends in diabetes treatment and control in U.S. adults, 1999–2018. N Engl J Med 2021;384(23):2219-28.
34. Vitto CM, Lykins V JD, Wiles-Lafayette H, et al. Blood pressure assessment and treatment in the observation unit. Curr Hypertens Rep. 2022;24(8):311-23.
35. Viera AJ. Hypertension update: hypertensive emergency and asymptomatic severe hypertension. FP Essent. 2018;469:16-19.
36. Fassas E, Fischer K, Schenkel S, et al. Public health interventions in the emergency department: a framework for evaluation. West J Emerg Med. 2024;25(3):415–22.
37. Oras P, Habel H, Skoglund PH, et al. Elevated blood pressure in the emergency department: a risk factor for incident cardiovascular disease. Hypertension. 2020;75(1):229-36.
38. Miller J, McNaughton C, Joyce K, et al. Hypertension management in emergency departments. Am J Hypertens. 2020;33(10):927-34.
39. Spieker AJ, Nelson LA, Rothman RL, et al. Feasibility and short-term effects of a multi-component emergency department blood pressure intervention: a pilot randomized trial. J Am Heart Assoc. 2022;11(5):e024339.
40. Ashburn N, Snavely A, Rikhi R, et al. Chest pain observation unit: A missed opportunity to initiate smoking cessation therapy. Am J Emerg Med. 2023;68:17-20.
41. Ashburn NP, Snavely AC, Rikhi R, et al. Rarely tested or treated but highly prevalent: hypercholesterolemia in ED observation unit patients with chest pain. Am J Emerg Med. 2023;71:47-53.
42. Ashburn NP, Snavely AC, Rikhi R, et al. Preventive cardiovascular care for hypercholesterolemia in US emergency departments: a national missed opportunity. Crit Pathw Cardiol. 2023;22(4):110-3.
43. Ashburn NP, Snavely AC, Stanek LS, et al. Emergency department observation unit patients want evaluation and treatment for hypercholesterolemia: a health belief model study. Crit Pathw Cardiol 2023;22(3):91-4..
44. Force UPST. Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA 2021;326(8):736-43.
45. American Diabetes Association. Screening for type 2 diabetes. Diabetes Care. 2003;26 Suppl 1:S21-4.
46. Mahler SA, Lenoir KM, Wells BJ, et al. Safely identifying emergency department patients with acute chest pain for early discharge. Circulation. 2018;138(22):2456-68.
Potential Impact of Using Canadian Syncope Risk Score on Emergency Department Hospitalizations for Syncope
Andrea W. Harris, MD, MS*
Lindsie LaBonte, BS†
Guido Massaccesi, MS†
Benoit Stryckman, MA‡
Bennett A. Myers, MD‡
Daniel B. Gingold, MD, MPH‡ R. Gentry Wilkerson, MD‡
Section Editor: David Thompson, MD
Johns Hopkins Hospital, Department of Emergency Medicine, Baltimore, Maryland University of Maryland School of Medicine, Baltimore, Maryland University of Maryland School of Medicine, Department of Emergency Medicine, Baltimore, Maryland
Submission history: Submitted January 22, 2025; Revision received May 10, 2025; Accepted June 16, 2025
Electronically published October 3, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.42019
Introduction: Syncope is a common emergency department (ED) presentation and frequently results in low-yield hospitalizations. The Canadian Syncope Risk Score (CSRS) is a validated risk stratification score that identifies 30-day risk of serious adverse events for patients presenting with syncope. In this retrospective, cross-sectional study we aimed to evaluate syncope admissions with the CSRS to determine potentially unnecessary hospitalizations.
Methods: We identified patient visits for syncope at 11 EDs from February 2019–January 2020. We excluded patients with additional serious diagnoses that would have independently required admission and those who were discharged. We then randomly sampled the remaining charts until finding 200 that met study inclusion criteria on full chart review. We retrospectively calculated CSRS via manual chart review and identified the proportion of patients with low-risk CSRS. We compared demographic characteristics between those with low- vs medium- and high-risk CSRS.
Results: We identified 5,718 adult patients hospitalized for syncope. Of these patient visits 3,999 were initially excluded, 336 were sampled, and 200 included for analysis. Of these, 39% (77/200, 95% CI 32-46%]) were low risk (CSRS < 1). Patients with low-risk CSRSs were younger (61.2 years vs 70.6 years of age; absolute difference [AD] 9.4 years; 95% CI 4.8-13.9), less likely to have heart disease (1.3% vs 61.8%; AD 60.5%, 95% CI -69.4% to -51.5%), and more likely to have substance use disorder (14.3% vs 4.9%; AD 9.4%, 95% CI 0.7-18.1%).
Conclusion: In this sample of patients hospitalized for syncope, 39% had low-risk Canadian Syncope Risk Score. Had the CSRS been used, these patients could have been safely discharged, as their estimated 30-day serious adverse event rate was < 1%. Wider adoption of the CSRS could potentially reduce unnecessary hospitalizations for patients with syncope.
[West J Emerg Med. 2025;26(5)1305–1312.]
INTRODUCTION
Background
Syncope, a brief, sudden loss of consciousness with spontaneous and complete return to baseline, is usually caused by transient global cerebral hypoperfusion.1 Syncope accounts for 1-3% of emergency department (ED) visits in the United States.2 Although its course is often benign, between 7-23% of patients will experience a serious adverse event within 30 days of hospitalization.3 However, 30-70% of ED visits for syncope result in hospitalization, likely because high-risk
etiologies have historically been difficult to differentiate at ED presentation or they required investigations beyond the scope of the initial ED evaluation.2,3
The Canadian Syncope Risk Score (CSRS) is a scoring system developed by Thiruganasambandamoorthy et al3 in 2016 to risk-stratify patients presenting to the ED with syncope and predict the risk of serious adverse events (SAE) in the 30-day period following presentation. The CSRS does not explicitly indicate what an emergency physician should do with regard to disposition of a syncope patient but rather guides decisionmaking using 30-day risk of SAEs for a given range of scores. Scores range from -3 (lowest risk) to 11 (highest risk). Scores < 1 indicate low- or very low-risk of 30-day SAE (1.2% in initial development study3). The risk of SAEs in this study is similar to the risk profiles seen in other clinical decision tools commonly used in the ED, such as the HEART score (history, ECG, age, risk factors, and troponin) Wells score, and the Pulmonary Embolism Rule-out Criteria.4-6 A low-risk CSRS (< 1) would support a clinical decision of discharge from the ED with clear instructions for return in the event of worsening symptoms. Medium-, high-, and very high-risk syncope in the CSRS scoring system are associated with a > 1.2% risk of SAEs and death and, therefore, may require hospitalization for further monitoring and evaluation.3,7,8
The CSRS has been validated in a prospective, multicenter cohort study of nine Canadian hospitals,7 which found patients with low- (CSRS of -1 or 0) and very lowrisk CSRS (< -1) had a SAE rate of 0.4% within 30 days of presentation. Another international validation of the CSRS in eight countries on three continents was completed in 2022, which found the 30-day SAE rate to be 0.6%.8 Further studies have confirmed the sensitivity and specificity of the CSRS in determining risk stratification in two Iranian EDs9 and one Australian ED.10
Importance
The CSRS may have value in identifying low-risk cases of syncope that can be safely discharged from the ED, which would reduce the burden of avoidable hospitalization. To our knowledge, only one prior study, based in Australia, has examined the potential impact of CSRS use. This hypothetical modeling study found that 16.9% of hospitalizations could be avoided if clinicians began consistently using the CSRS instead of usual care.12 The potential impact of using the CSRS on a cohort of actual patients in the United States has not been previously evaluated.
Goals of This Investigation
Our goal in this study was to identify the potential impact of using CSRS for patients hospitalized for syncope in whom a serious diagnosis was not identified during the initial ED evaluation. Using data from a large medical system in the US, we sought to determine the proportion of patients hospitalized for syncope who were determined to be low- or very low-
Population Health Research Capsule
What do we already know about this issue?
The Canadian Syncope Risk Score (CSRS) is a validated risk stratification score that identifies 30-day risk of serious adverse events for patients with syncope.
What was the research question?
We sought to determine the proportion of patients hospitalized for syncope who were low- or very low-risk using the CSRS.
What was the major finding of the study?
In our sample of patients hospitalized for syncope, 39% (77/200, 95% CI 32-46%) were low risk (CSRS < 1).
How does this improve population health?
Wider adoption of the CSRS in the disposition decision could potentially reduce unnecessary hospitalizations for patients with syncope.
risk for SAEs using the CSRS. The primary outcome was the proportion of hospitalized patients with a CSRS score < 1. These hospitalizations could have possibly been avoided had the CSRS been used during the ED evaluation.
METHODS
Study Design and Setting
This retrospective, cross-sectional, pilot observational study was performed at 11 EDs within the University of Maryland Medical System, including one academic and 10 community hospitals. The University of Maryland, Baltimore institutional review board (IRB) evaluated this study and determined it to be exempt from IRB review. We followed 10 of the 12 elements of medical record review studies as described by Worster et al, with the exception of blinding of the abstractors to the study objectives and formal testing of inter-rater reliability.13
Selection of Participants
Using Epic (Epic Systems Corporation, Verona, WI), the electronic health record for the medical system, charts were reviewed for inclusion if patients 18 years or older presented to the ED with a diagnosis of syncope per International Classification of Diseases, 10th Rev, codes (ICD-10 R55 for syncope found in the ED clinical impression as entered by emergency physicians at the time of evaluation, management, and disposition) between February 1, 2019–January 31, 2020.
Data collection was completed from February–September 2023. We excluded patient visits if patients were discharged from the ED, if the CSRS could not be used due to its own exclusion criteria (ie, syncopal episode > 5 minutes in length, > 24 hours since syncopal episode, no loss of consciousness noted), if the patient was noted to have an independent serious diagnosis requiring admission, or if there was a mental status change or other condition that limited history-taking or documentation per the ED note.
We also excluded visits if ICD-10 codes from the ED clinical impression included a serious diagnosis requiring admission, including cardiac arrest, pulmonary embolism, myocardial infarction, respiratory failure, intracranial hemorrhage, and seizure. At this stage, visits were also excluded via ICD-10 code for mental status changes, intoxication, head trauma causing loss of consciousness, and pregnancy. Additionally, we excluded visits with ICD-10 codes of R55 but selected character strings indicating near syncope or presyncope as these diagnoses preclude use of the CSRS.
Following initial exclusions completed by query, visits were randomized (Figure 1) for selection for manual chart review. Cases were reviewed sequentially and excluded if additional exclusion criteria were discovered after review was completed. This process was completed until 200 charts were eligible to be included in the analysis. Because this was a retrospective pilot study primarily designed to explore patterns rather than test a specific hypothesis, we initially selected a convenience sample of 200 charts to allow for feasibility within our available timeframe. However, a post hoc power calculation was performed to assess the adequacy of this sample size. Assuming an acceptable baseline rate of 20% for low-risk CSRS scores among admitted patients with syncope, our sample size of 200 provides a 77.8% power to detect a 15% absolute difference (AD) from this proportion.
Measurements
Data extraction was completed via chart review using a standardized abstraction instrument with Research Electronic Database Capture (REDCap) software (Vanderbilt University, Nashville, TN). Variables were precisely defined with an explicit protocol, and three medical student abstractors were trained on chart abstraction criteria. An initial pilot of 20 patient charts was performed and compared between extractors and attending emergency physician senior authors to ensure understanding of variable definitions; discrepancies during these pilot abstractions were resolved through consensus at regularly scheduled meetings to review coding rules. A senior medical student abstractor reviewed 5% of charts abstracted for quality review; just one data element was misclassified in that review and was corrected. Abstractors were not blinded to the study hypothesis.
Outcomes
We calculated the CSRS values based on abstracted data
Table 1. Canadian Syncope Risk Score components.3
syncope
*Symptoms triggered by being in a warm crowded place, prolonged standing, fear, emotion, or pain.
+Ischemic or structural heart disease, including coronary artery disease, atrial fibrillation or flutter, congestive heart failure, or valvular disease.
mm Hg, millimeters of mercury; ED, emergency department; ms, millisecond.
from patient charts based on CSRS scoring criteria (Table 1), including systolic blood pressures (abnormal: < 90 or > 180 millimeters of mercury) elevated troponin (> 99th percentile of normal population), abnormal QRS axis (< -30° or > 100°), abnormal QRS duration (> 130 milliseconds [ms]), and abnormal QTc (> 480 ms).3 All electrocardiograms (ECG) were interpreted by the treating clinician at the time they were obtained. If a patient had repeat vital signs, troponins, or ECGs measured during the time from ED arrival to ED disposition, any abnormal value could be used to accumulate CSRS points. If a troponin was not ordered or missing from a chart, it was presumed to be < 99th percentile for the patient population. This is consistent with the initial development of the CSRS, which calculated CSRS values by imputing normal troponins when they had not been ordered, and consistent with other previously published work on the topic.3,7,8
Syncope type (cardiac, vasovagal, or neither) was identified if the ED chart specifically identified either cardiac or vasovagal syncope as a diagnosis or if written portion of the chart included these specific terms; otherwise, syncope type was imputed as “neither.” History of structural or ischemic heart disease included coronary or valvular heart disease, cardiomyopathy, congestive heart failure, prior device implementation, or documented history of ventricular or atrial arrhythmias3 as identified by diagnoses in the patient’s prior medical history or as mentioned by the charting clinician in the history of present illness (HPI). Predisposition to vasovagal symptoms was identified either with a prior diagnosis of vasovagal syncope or mention in HPI of prior history of syncopal event triggered by a warm
crowded place, prolonged standing, fear, emotion, or pain.3 If no documentation of heart disease history or vasovagal symptoms was documented, patients were assumed to have no such history.
Medical history components of interest (hypertension, diabetes, malignancy, seizure, stroke, substance use disorder, kidney disease on dialysis, previous syncopal episode) were identified by the treating clinicians and included if either mentioned in the ED chart HPI or diagnosis and medical history portion of the patient’s chart at time of ED visit. Associated symptoms of interest (diaphoresis, nausea, vomiting, abdominal pain, vision changes, shortness of breath, chest pain) were identified by the treating clinician and included if mentioned in the ED chart HPI. We identified patient sex using information in the electronic health record upon patient registration.
Analysis
We calculated the proportion of patients with low- and very low-risk CSRS (total score < 1), and a 95% CI was obtained for all included visits, as well as for academic and community visits separately. We compared patient-level characteristics, including medical history and associated symptoms, between low- and medium-/high-risk CSRS groups as proportion of patients with each characteristic. We computed ADs of these proportions to compare these groups. We calculated CIs for all proportions with binomial exact calculations. Sensitivity analysis for troponin ordering status was completed by comparing the proportion of low-risk CSRS values for those with vs without troponin ordered. We performed data analysis using SAS v9.4. (SAS Institute Inc, Cary, NC) and Microsoft Excel v16.0 (Microsoft Corporation, Redmond, WA).
RESULTS
Characteristics of Study Subjects
A total of 5,718 adult patients presented to one of the study site EDs with a diagnosis of syncope (ICD-10 code R55) from February 1, 2019–January 31, 2020. After excluding patients with serious outcomes, seizure, mental status change, intoxication, head trauma, pregnancy, and presyncope, 1,719 had a disposition of admitted or placed in observation and qualified for randomization to chart review. Of these, 336 patient visits were randomly selected and reviewed. After further exclusions based on chart review, 200 charts were included in the analysis (Figure 1).
Mean patient age was 67 years, 101 (50.5%) were women, and 77 (35.5%) had a history of structural or ischemic heart disease (Table 2). Forty-one patients were hospitalized under inpatient status, and 159 were hospitalized under observation status. Electrocardiograms and at least one blood pressure reading were available for all patients included in the study. A troponin was not ordered for 16 patients: 10 low-risk CSRS visits and six medium- or high-risk CSRS visits.
UMMS ED visits for patients ≥ 18 years old for syncope, 2/2019-1/2020 (N=5,718)
Excluded by ICD-10 diagnosis following data query (n=1,219)
• Near or pre-syncope diagnosis (n=771)
• Serious diagnosis requiring admission (n=280)
• Altered mental status or intoxication (n=168)
Visits where CSRS may be applicable (n=4,499)
Excluded: disposition was not admission or observation (n=2,780)
Visits qualified for randomization to chart review (n=1,719)
Randomization (Simple Random Sample)
Visits sampled for study (n=336)
Excluded following chart review* (n=136)
• Not syncope (n=62)
• Serious diagnosis requiring admission (n=44)
• Loss of consciousness > 5 min (n=10)
• > 24h since syncope (n=12)
• History limited (n=15)
Visits included in analysis (n=200)
*Some charts excluded for multiple reasons
Figure 1. Flow diagram for patient visits with syncope. UMMS, University of Maryland Medical System; ED, emergency department; ICD, International Classification of Diseases; CSRS, Canadian Syncope Risk Score.
Table 2. Baseline characteristics of patients hospitalized for syncope included in study.
N = 200 Age, years (SD)
(17)
or ischemic heart
(%)
(%)
(67%)
(24%) Malignancy (%)
Seizure (%)
(17%)
(3%) Stroke (%)
Substance use disorder (%)
Kidney disease on dialysis (%)
(13%)
(9%)
(3%) Previous syncopal episode (%)
(21%)
SD, standard deviations.
Main Results
In this sample of patients hospitalized for syncope, 1% (2/200) had a very low-risk CSRS and 38% (75/200) had a lowrisk CSRS (Figure 2). In total, 39% (77/200) had calculated CSRS < 1, while 50% (99/200) had medium-risk CSRS (0 < CSRS < 4), 10% (19/200) had high-risk CSRS (3 < CSRS < 6), and 3% (5/200) had very high-risk CSRS (score > 5) (Figure 2).
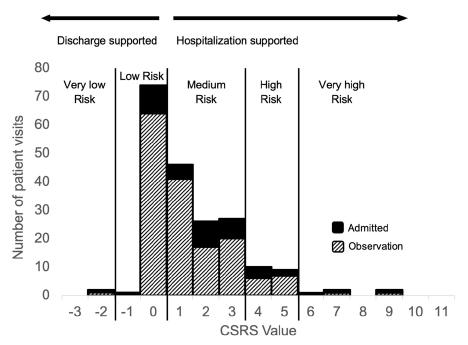
2. Histogram of Canadian Syncope Risk Score values for included patients.
CSRS, Canadian Syncope Risk Score
For patients who presented to EDs at the academic hospital, 45% (15/33; 95% CI 28-64%) of those who were hospitalized for syncope had a CSRS < 1. For patients who were treated at community EDs, this value was 37% (62/167; 95% CI 30-45%). Among all hospitals, of the 77 patients who were hospitalized with low-risk CSRS, 11 were admitted to inpatient care and 66 were placed in observation status.
The most common components of the CSRS that were present and scored points were abnormal systolic blood pressure (42/200 (21%, 95% CI 16-27%), abnormal QTc interval (31/200 (16%), 95% CI 11-21%) (Table 3), and history of structural or ischemic heart disease (77/200 (39%), 95% CI 32-46%) (Table 4), Of 200 patients, 197 (99%) did not have a specific diagnosis of either vasovagal or cardiac syncope in the ED chart.
Hospitalized patients with very low- or low-risk CSRS were younger compared to patients with medium-, high-, or very high-risk CSRS (61.2 years vs 70.6 years; AD -9.4 years, 95% CI -4.8 to -3.9 years). Those with CSRS < 1 were less likely to have a history of either structural or ischemic heart disease (1.3% vs 61.8%; AD -60.5%, 95% CI -69.4% to -51.5%) and more likely to have a history of substance use disorder (14.3% vs 4.9%; AD 9.4%, 95% CI 0.7-18.1%) (Table 4).
Of the included patients who did not have a troponin ordered, 63% (10/16, 95% CI 35-85%) were low-/very low-risk CSRS whereas 36% of those who had a troponin ordered were low-/very low-risk CSRS (67/184, 95% CI 29-44%); (AD 26%, 95% CI 1.4-51%). Of 184 patients with a troponin ordered, troponin levels were elevated in 11 (6.0%, 95% CI 2.6-9.4%) (Figure 3). Of these 11 patients, one died while hospitalized (CSRS 4) and one received a heart catheterization (CSRS 6). No patients with a low-risk CSRS had a positive troponin.
Table 3. Canadian Syncope Risk Score components by
to vasovagal
Abnormal QRS axis (< -30 or > 100 degrees)
Emergency department diagnosis
mm Hg, millimeters of mercury; CSRS, Canadian Syncope Risk Score; ms, millisecond.
DISCUSSION
In this retrospective analysis of ED patients hospitalized for syncope in a large, regional medical system, we found that 39% of patients hospitalized had a CSRS < 1, representing potentially dischargeable ED visits. Identification and discharge of these low-risk cases of syncope would help limit hospitalizations without increasing risk of serious adverse events. Although prior prospective studies have validated the CSRS and prospectively determined scores from patient visits,3-5 a unique contribution of this retrospective study is that it allows for observation of the impact that changing practice—using the CSRS on patients with a primary diagnosis of syncope rather than clinical judgment alone— may have on already stressed EDs and hospital systems. We believe this work should inform standardization of the approach to a syncopal patient using the CSRS.
These data indicate that emergency physicians may be more conservative in their decision-making than the CSRS suggests is necessary to avoid SAEs by hospitalizing patients presenting with syncope. Given the higher number of admitted syncope patients in the low-risk CSRS group, it appears that substance use, or factors related to it, may have contributed to an increased perceived risk of acute serious adverse events by the clinician. Concerns about the patient’s ability to follow up may have played a role, although other unmeasured clinical or complex, health-related social factors likely influenced these decisions as well.
While our primary analysis focused on the low-risk group, we acknowledge that some medium-risk patients may also be
Figure
Table 4. Comparison of patient-level characteristics between low-risk and medium- or high-risk Canadian Syncome Risk Score in sample.
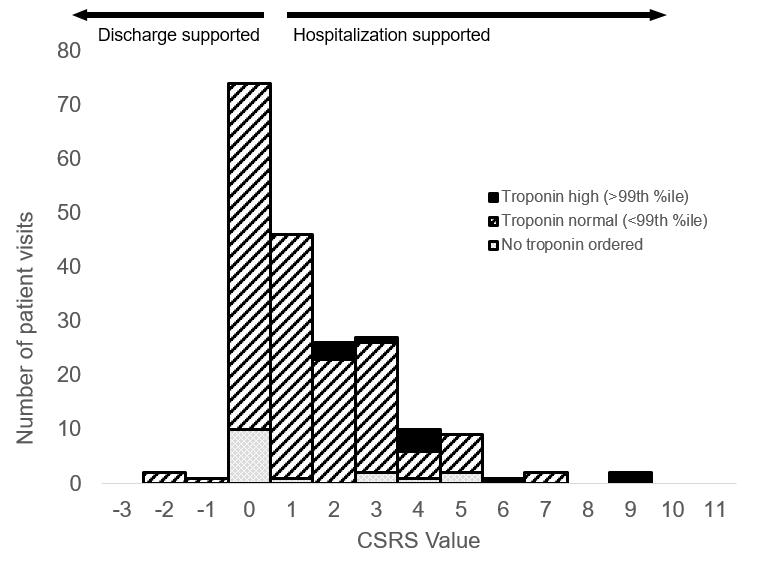
safely discharged in select cases, particularly in settings where shared decision-making, reliable outpatient follow-up, and ambulatory cardiac monitoring are available. However, this strategy is not yet standard practice, and there are currently no prospective data demonstrating the safety of routine discharge for medium-risk patients. Given this, we conservatively limited our analysis to the low-risk group. If some medium-risk patients could also be safely discharged, the potential benefits of CSRS implementation may be greater than our estimates suggest.
Given that syncope accounts for 1-3% of US ED visits,2 a potential decrease of 39% of hospitalizations for this population would be meaningful. Accordingly, a more informed decision-making process for ED evaluation of syncope has the potential to reduce costs substantially for patients and hospitals with a possible estimated costs savings of $627,599 from $1,132,908 to the hospital system using average direct variable costs.14,15 Further analysis of avoidable hospital costs and length of stay for patients with low-risk
CSRS, Canadian Syncope Risk Score; SD, standard deviations; CI, confidence intervals
Figure 3. Histogram of Canadian Syncope Risk Score values by troponin status.
CSRS, Canadian Syncope Risk Score
CSRS scores would be valuable.
One component of the CSRS that is unique among syncope risk stratification scores is the measure of clinician judgment of syncope etiology as being cardiac, vasovagal, or neither.16 This may be beneficial because most other externally validated risk scores have not been shown to perform better than clinician judgment alone.17 For nearly all visits in our study (197/200), the note writer did not specify which kind of syncope they suspected; for these diagnoses we imputed “neither” as the type of syncope. Our findings may indicate that emergency physicians are not regularly noting the etiology of syncope in their assessment once they have decided to hospitalize a patient based on other factors. Implementation of the CSRS may subsequently force clinicians to consider whether there is a likely etiology of syncope and be able to incorporate the CSRS into their disposition planning.
Future studies on the impacts of CSRS use would benefit from incorporating actual hospital costs and length of stay from patient visits into the analysis, including discharged patients who may have been hospitalized had the CSRS been used. A previous study in Australia found that using the CSRS compared to standard care could be a cost-effective intervention.12 Cost-effectiveness analysis in the US has yet to be published. Incorporation of data from multiple hospital systems or geographic areas may elucidate the extent of practice variation and the impact CSRS use could have in specific regions. A prospective study to determine the impacts of CSRS use in EDs would be valuable, particularly to understand how clinicians are using the score during patient evaluation and treatment.
LIMITATIONS
The study is subject to limitations inherent to retrospective analyses; clinician hospitalization and discharge decisions as well as use of CSRS may vary if these were to be studied prospectively. Also, there is potential for bias, including misclassification and selection bias, due to retrospective manual chart review and reliance on ICD-10 codes for identifying inclusion and exclusion diagnoses. Specifically, we relied on ICD-10 codes recorded in the ED clinical impressions, which are typically documented by emergency clinicians at the time of patient evaluation, management, and disposition. Only conditions known to the physician at the time of ED-to-hospital admission were included. However, we acknowledge some patients admitted with low-risk CSRS scores may have had additional conditions or reasons for admission not captured in ICD-10 codes.
We excluded many patients whose scores were not calculable based on the limited information available in the ED chart; had the score been used prospectively, treating clinicians may have had adequate information to calculate a CSRS. There may have been reasons treating clinicians decided to hospitalize patients that were not captured in the chart review, such as concerns about follow-up outpatient care due to health-related
social needs. This study also had limited ability to capture the clinician-decided syncope category of cardiac, vasovagal, or neither; chart review only identified cases as cardiac or vasovagal if the note specifically used this language or the clinician used a diagnosis code with one of these terms.
The analysis included 16 patients for whom a troponin level was not obtained, 10 in the very low/low-risk group and six in the medium-/high-/very high-risk group. However, a troponin is not required to calculate a CSRS; per the team that developed the score if a troponin is not done, the score for that component is zero.3 In the initial study from which the CSRS was developed, 52% of patients did not have a troponin measurement.3 In our study this was 8% of patients.
Our analysis was focused on a one-year period from February 2019–January 2020, prior to the start of the COVID-19 pandemic in the US, which was chosen to limit the impact of changing ED visit patterns on our analysis.11
The CSRS had been developed by this time, but international validation of the CSRS has been published since 2019.8 We do not know whether clinicians in the aggregate have altered their practice since 2019 to incorporate the CSRS in their evaluation of syncopal patients. The percentage of hospitalized syncopal patients that may be dischargeable could be lower than 39% if clinicians are now using the CSRS more often to make hospitalization and discharge decisions.
Our study focused only on EDs in a single state and a single hospital system. Practice variation is likely in other geographic areas, and the results of our study are not necessarily generalizable across the US or internationally. While charts were sampled based on the proportion of syncope-related ED visits at each hospital, the academic hospital may be slightly over-represented in our dataset. This could potentially have skewed our data, particularly if clinical practices differ between academic and community settings; however, the inclusion of both academic and community hospitals improves the generalizability of our findings.
Because we did not include in our analysis patients who were discharged, we could not draw conclusions about the impact of using the CSRS on patients who may have otherwise been discharged (ie, those who may have been discharged with high-risk CSRS). It is possible that universal use of CSRS could increase hospitalizations in this cohort, which would reduce potential hospitalization avoidance and cost savings. We did not examine the frequency of serious adverse events in this analysis; the validity of the CSRS has been demonstrated multiple times across institutions and countries in the literature,7–10 and we relied on these published estimates rather than re-evaluating the frequency of these events.
CONCLUSION
This study showed that a substantial proportion of patients hospitalized for syncope from the ED had low risk of 30-day serious adverse events as identified by the Canadian Syncope Risk Score. Wider adoption of the CSRS in emergency
departments may limit unnecessary hospitalizations for patients with syncope.
Address for Correspondence: Andrea W. Harris, MD, MS, Johns Hopkins Hospital, Department of Emergency Medicine, 1830 East Monument Street, Suite 6-100, Baltimore, MD 21287. Email: harris.andrea.w@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Dr. Wilkerson received research funding from Becton, Dickinson, and Company; Global Blood Therapeutics, Inc.; Novartis Pharmaceuticals; Egetis Therapeutics AB; EndPoint Health, Inc.; Janssen R&D LLC; Greiner Bio-One; CalciMedica; CSL Behring; and Pfizer Inc. He has received research funding from CoapTech, LLC, through an NIH/NIDDK grant (R44DK115325). He has received research support in the form of equipment and supplies from Cepheid and Eldon Biologicals A/S. He is a paid consultant for the National Foundation of Emergency Medicine. The other authors report no conflicts.
Copyright: © 2025 Harris et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Brignole M, Moya A, De Lange FJ, et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39(21):1883-1948.
2. Sun BC, Emond JA, Camargo Jr. CA. Characteristics and admission patterns of patients presenting with syncope to U.S. emergency departments, 1992–2000. Acad Emerg Med. 2004;11(10):1029-1034.
3. Thiruganasambandamoorthy V, Kwong K, Wells GA, et al. Development of the Canadian Syncope Risk Score to predict serious adverse events after emergency department assessment of syncope. CMAJ. 2016;188(12):E289-E298.
4. Kline JA, Mitchell AM, Kabrhel C, et al. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004;2(8):1247-1255.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780.
6. Six AJ, Cullen L, Backus BE, et al. The HEART score for the assessment of patients with chest pain in the emergency department: a multinational validation study. Crit Pathw Cardiol. 2013;12(3):121.
7. Thiruganasambandamoorthy V, Sivilotti MLA, Le Sage N, et al. Multicenter emergency department validation of the Canadian Syncope Risk Score. JAMA Intern Med. 2020;180(5):1-8.
8. Zimmermann T, du Fay de Lavallaz J, Nestelberger T, et al. International validation of the Canadian Syncope Risk Score. Ann Intern Med. 2022;175(6):783-794.
9. Chan J, Ballard E, Brain D, et al. External validation of the Canadian Syncope Risk Score for patients presenting with undifferentiated syncope to the emergency department. Emerg Med Australas. 2021;33(3):418-424.
10. Brain D, Yan A, Morel D, et al. Economic evaluation of applying the Canadian Syncope Risk Score in an Australian emergency department. Emerg Med Australas. 2023;35(3):427-433.
11. Baugh JJ, White BA, McEvoy D, et al. The cases not seen: patterns of emergency department visits and procedures in the era of COVID-19. Am J Emerg Med. 2021;46:476-481.
12. Zimmermann T, Du Fay De Lavallaz J, Florez D, et al. Validation of the Canadian Syncope Risk Score in a large prospective international multicenter study. Eur Heart J. 2020;41(Supplement_2): ehaa946.0701.
13. Safari S, Khasraghi ZS, Chegeni MA. The ability of Canadian Syncope Risk Score in differentiating cardiogenic and noncardiogenic syncope; a cross-sectional study. Am J Emerg Med. 2021;50:675-678.
14. Alshekhlee A, Shen WK, Mackall J. Incidence and mortality rates of syncope in the United States. Am J Med. 2009;122(2):181-188.
15. Malik M, Francis-Morel G. Impact of admission of patients with syncope in non-teaching hospitals versus teaching hospitals: a nationwide analysis. Cureus. Published online May 26, 2023.
16. Sutton R, Ricci F, Fedorowski A. Risk stratification of syncope: current syncope guidelines and beyond. Auton Neurosc. 2022;238:102929.
17. Costantino G, Casazza G, Reed M, et al. Syncope risk stratification tools vs clinical judgment: an individual patient data meta-analysis. Am J Med. 2014;127(11):1126.e13-1126.e25.
Original Research
Does Single Dose Epinephrine
Improve Outcomes for Patients with Out-of-Hospital Cardiac Arrest by Sex or Race?
Breanna L. Blaschke, MD*
Nicklaus P. Ashburn, MD, MS†
Anna C. Snavely, PhD*‡
Kristina Dev, BA†
Tyler S. George, MD§
Bryan P. Beaver, MD||
Michael A. Chado, MD#
Harris A. Cannon, MD†
Authors continued at end of article
Section Editor: Joseph Shiber, MD
* † ‡
University of North Carolina, Department of Emergency Medicine, Chapel Hill, North Carolina
Wake Forest University School of Medicine, Department of Emergency Medicine, Winston-Salem, North Carolina
Wake Forest University School of Medicine, Department of Biostatistics and Data Science, Winston-Salem, North Carolina
§
Wake Forest University School of Medicine, Department of Internal Medicine, Winston-Salem, North Carolina
Submission history: Submitted December 12, 2024; Revision received April 13, 2025; Accepted April 25, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.41482
Introduction: Recent evidence suggests that survival to hospital discharge in patients with outof-hospital cardiac arrest (OHCA) is similar among patients receiving a single dose epinephrine protocol compared to a multi-dose epinephrine protocol. However, it is unknown whether survival to hospital rates differ for single dose vs. multi-dose epinephrine within sex and race subgroups. Our objective in this study was to determine whether survival to hospital discharge rates varied for single dose vs. multi-dose epinephine protocols among men, women, White, and non-White patients.
Methods: We conducted a pre-post Single Dose Epinephrine Implementation Study from November 1,2016 – October 29, 2019 at five North Carolina emergency medical services (EMS) systems, involving patients ≥ 18 years old with non-traumatic OHCA. Data on race, sex, and the primary outcome of survival to hospital discharge were determined from the Cardiac Arrest Registry to Enhance Survival and from EMS records. We performed intention-to-treat analysis. We compared survival to hospital discharge rates between single dose vs multi-dose epinephrine protocols within sex and race subgroups using generalized estimating equations with a logit link to account for clustering among EMS agencies and to adjust for age, witnessed arrest, automated external defibrillator availability, EMS response interval, the presence of a shockable rhythm, receiving bystander cardiopulmonary resuscitation, and sex or race. In the model, we evaluated interactions between epinephrine protocol and race and sex.
Results: Of the 1,690 patients included, (899 multi-dose, 791 single dose), 38.7% (657/1,690) were female and 74.7% (1,262/1,690) were White. Survival to hospital discharge occurred in 13.6% (122/899) of patients in the multi-dose group and 15.4% (122/791) in the single dose epinephrine group (OR 1.19, 95%CI 0.89-1.59). Single dose epinephrine was associated with increased survival to hospital discharge rates in White patients (adjusted odds ratio [aOR] 1.17, 95% confidence interval [CI] 1.05-1.30). However, the rates were similar for single dose vs. multi-dose epinephrine among men (aOR 1.03, 95% CI 0.93-1.14), women (aOR 1.23, 95% CI 0.97-1.56), and non-White patients (aOR 1.08, 95% CI 0.78-1.51). Interactions between epinephrine protocol and subgroups were not significant.
Conclusion: Rates of survival to hospital discharge were similar in the single dose and multi-dose epinephrine strategies regardless of sex. Single dose epinephrine was associated with increased survival to hospital discharge among White patients but not in non-White patients, which may be due to unmeasured confounding or inadequate power. [West J Emerg Med. 2025;26(5)1313–1321.]
INTRODUCTION
In the United States approximately 350,000 patients experience out-of-hospital cardiac arrest (OHCA) annually, and only about 10% survive.1-3 Per the current Advanced Cardiovascular Life Support (ACLS) guidelines set by the American Heart Association, epinephrine should be administered every three to five minutes for OHCA as part of a multi-dose epinephrine protocol.4 However, while epinephrine is known to increase return of spontaneous circulation (ROSC) rates, it may not improve rates of survival to hospital discharge.5-7 Increased myocardial oxygen demand and risk of cardiac arrhythmias associated with epinephrine may contribute to adverse outcomes and decrease survival to hospital discharge.8-10
Our team recently implemented a single dose epinephrine protocol for OHCA in five emergency medical services (EMS) agencies. When compared with the traditional multi-dose protocol, we found that the single dose protocol was associated with decreased rates of ROSC but similar rates of survival to hospital discharge.11 Prior literature has established that cardiovascular care disparities exist between men and women and White and non-White patients.2,12–18 However, no study has compared the performance of single dose vs. multi-dose epinephrine approach within sex and race subgroups.
To address this gap in the out-of-hospital resuscitation literature, we conducted a pre-planned secondary analysis of the Single dose Epinephrine Implementation Study, which compared adult OHCA patients receiving resuscitation guided by single dose vs. multi-dose epinephrine. Our objectives were to determine whether survival to hospital discharge, ROSC, and favorable neurologic outcome rates differed for single dose vs. multi-dose epinephrine protocols among men, women, White, and non-White patients. We also explored survival to hospital discharge, ROSC, and favorable neurologic outcomes among patients presumed to have arrested from a primary cardiac etiology.
METHODS
Study Design and Oversight
We performed a secondary analysis of the Single Dose Epinephrine Implementation Study for OHCA. Data were collected from five EMS systems in North Carolina between November 1, 2016 – October 29, 2019. The Wake Forest University Health Sciences Institutional Review Board approved the study protocol and granted a waiver of informed consent. We used the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for reporting observational studies during the research process.19 The methods of the Single dose Epinephrine Implementation Study have been previously described.11,20
Study Setting and Population
Five counties were included in the study, each operating an Advanced Life Support (ALS) EMS system with medical direction from emergency physicians with subspecialty board
Population Health Research Capsule
What do we already know about this issue? It is unknown whether survival to hospitaldischarge rates differ for a single dose vs. multi-dose epinephrine protocol within sex and race subgroups.
What was the research question?
Do rates of survival to hospital discharge vary for single dose vs. multi-dose epinephrine protocols among men, women, White, and non-White patients?
What was the major finding of the study?
Single dose epinephrine was associated with increased survival to hospital discharge in White patients (aOR 1.17, 95% CI 1.05-1.30).
How does this improve population health?
Rates of survival to hospital discharge were similar in the single dose and multi-dose groups regardless of sex. Single dose was associated with increased survival among White patients only.
certification in EMS. These EMS systems serve populations within urban, suburban, and rural communities, totaling almost 850,000 individuals (Supplemental Table 1). Patients ≥ 18 years of age who underwent attempted resuscitation for non-traumatic cardiac arrest were included in the study. We excluded patients who were pregnant and prisoners. Pre-implementation, the traditional multi-dose epinephrine recommendations were followed. Under these guidelines, EMS responders administered 1 milligram (mg) of 1:10,000 intravenous (IV) or intraosseous (IO) epinephrine every 3-5 minutes. Post-implementation, responders followed the single dose epinephrine protocol, where patients received a single 1:10,000 dose of 1 mg IV or IO epinephrine. The protocol did not allow for additional doses of epinephrine. During the post-implementation period, the North Carolina Office of EMS also began allowing the use of ketamine for cardiopulmonary resuscitation (CPR)-induced consciousness. Two patients received ketamine for this indication over the study period. No other changes were made to the study protocol. The complete single dose and multi-dose epinephrine guidelines are found in Supplemental Appendix 1.
Data Collection and Variables
We collected data for one year before and one year after
the date of single dose epinephrine implementation, which differed for each county EMS system. Exact dates of implementation for each EMS system are included in Supplemental Table 1. All data were collected from November 1, 2016 – October 29, 2019.
We used the Cardiac Arrest Registry to Enhance Survival (CARES) to collect demographics, initial heart rhythm, interventions provided, and etiology of the arrest.21 The EMS systems submit data to CARES using standardized international Utstein definitions to help ensure uniformity in reporting.21 Sex and race were determined by the prehospital responder based on patient or family report, driver’s license, or by healthcare clinician impression. Race data in CARES was recently validated in a large cohort of Medicare data.22 The CARES registry defined shockable rhythms as ventricular fibrillation, ventricular tachycardia, and unknown shockable rhythm. Non-shockable rhythms were defined as asystole, idioventricular/pulseless electrical activity, and unknown unshockable rhythm. Per CARES, the etiology of the arrest was presumed to be cardiac, unless it was likely from a known respiratory cause, asphyxia, drowning, or electrocution. The CARES registry also provided patient outcomes, including survival to hospital discharge, ROSC, and neurologic status. When abstracting data from CARES and the prehospital electronic health record, we used best practices to enhance scientific rigor. We used trained data abstractors, case selection criteria, variable definitions, performance monitoring, an electronic abstraction form, and medical record identification.23
Outcomes
The primary outcome was survival to hospital discharge, defined by CARES as leaving the hospital alive regardless of neurologic status. The secondary outcome was ROSC, defined as the patient having a pulse for ≥ 20 minutes without additional chest compressions.21 An exploratory outcome was neurological outcome at time of discharge from the hospital. The CARES registry describes neurologic outcomes using Cerebral Performance Categories (CPC) 1-4, with categories 1 and 2 considered favorable due to patients being able to function independently and live a normal, or relatively normal, life. The CPC 3 and 4 are considered poor neurological outcomes, with patients having severe cerebral disability or being in a vegetative state, requiring daily support due to impaired brain function. The CARES registry does not use the CPC 5 (brain death) category.
Statistical Analysis
We described categorical variables such as sex, race, EMS system, rhythm types, performance of bystander CPR, as well as survival to hospital discharge and ROSC rates, with counts and percentages. Continuous variables, such as age and EMS response time, were described with medians and interquartile ranges (IQR). The unit of analysis was the OHCA encounter, and the analysis was by intention to treat. It was not possible
to conduct a per-protocol analysis because the number of doses of epinephrine administered was not available. We compared survival to hospital-discharge rates, ROSC rates, and neurological outcomes between the single dose and multi-dose epinephrine cohorts using generalized estimating equations (GEE) with a logit link to account for clustering within EMS agencies.
Models were fit within each subgroup, defined by sex (male or female) and race (White or non-White). Non-White patients were those who identified as American Indian/Alaska Native, Asian, Black, Hispanic/Latino, or Native Hawaiian/ Pacific Islander. Due to the study’s modest sample size, we analyzed race as a two-level variable: White and non-White. This dichotomous approach has been used in prior cardiovascular care studies.24-28 We also evaluated the interaction of single dose epinephrine implementation (multidose vs. single dose epinephrine) with sex and race.
Multivariable models were adjusted for age, witnessed arrest, automated external defibrillator (AED) availability, EMS response interval, presence of a shockable rhythm, receiving bystander CPR, and sex or race. Unadjusted and adjusted odds ratios (aOR) with corresponding 95% confidence intervals (CI) were calculated from the GEE models. Using the same analysis methods described above, we also conducted prespecified analyses among only those patients who experienced OHCA from a presumed primary cardiac etiology.
RESULTS
During the study period there were 1,690 OHCA encounters (899 pre-implementation with multi-dose epinephrine, 791 post-implementation with single dose epinephrine). The overall cohort was 74.7% White (1,262/1,690) and 38.9% female (657/1,690); the median age was 65 years (IQR 53-76). Survival to hospital discharge occurred in 13.6% (122/899) of patients in the multi-dose epinephrine group and 15.4% (122/791) in the single dose epinephrine group (OR 1.19, 95%CI 0.89-1.59),11 while ROSC occurred in 42.3% (380/899) of patients in the multi-dose epinephrine group and 32.5% (257/791) in the single dose epinephrine group. Figure 1 illustrates the study flow diagram. Patient characteristics are summarized in Table 1.
Single dose epinephrine implementation was associated with a 1.9% absolute increase in survival to hospital discharge among White patients (15.1% vs. 13.2%; OR 1.18, 95% CI 1.06-1.31) and a 1.7% increase among non-White patients (16.3% vs. 14.6%; OR: 1.17, 95% CI 0.68-2.02). After adjusting for potential confounders, single dose epinephrine implementation remained associated with higher survival to hospital-discharge rates among White patients (aOR 1.17, 95% CI 1.05-1.30) but not among non-White patients (aOR 1.08, 95% CI 0.78-1.51). Single dose epinephrine was associated with decreased ROSC rates among White patients (aOR 0.49, 95% CI 0.33-0.75), but relatively unchanged ROSC rates among non-White patients (aOR 0.82, 95% CI 0.47-1.41). The interaction between single dose epinephrine implementation and race was not significant for
Blaschke
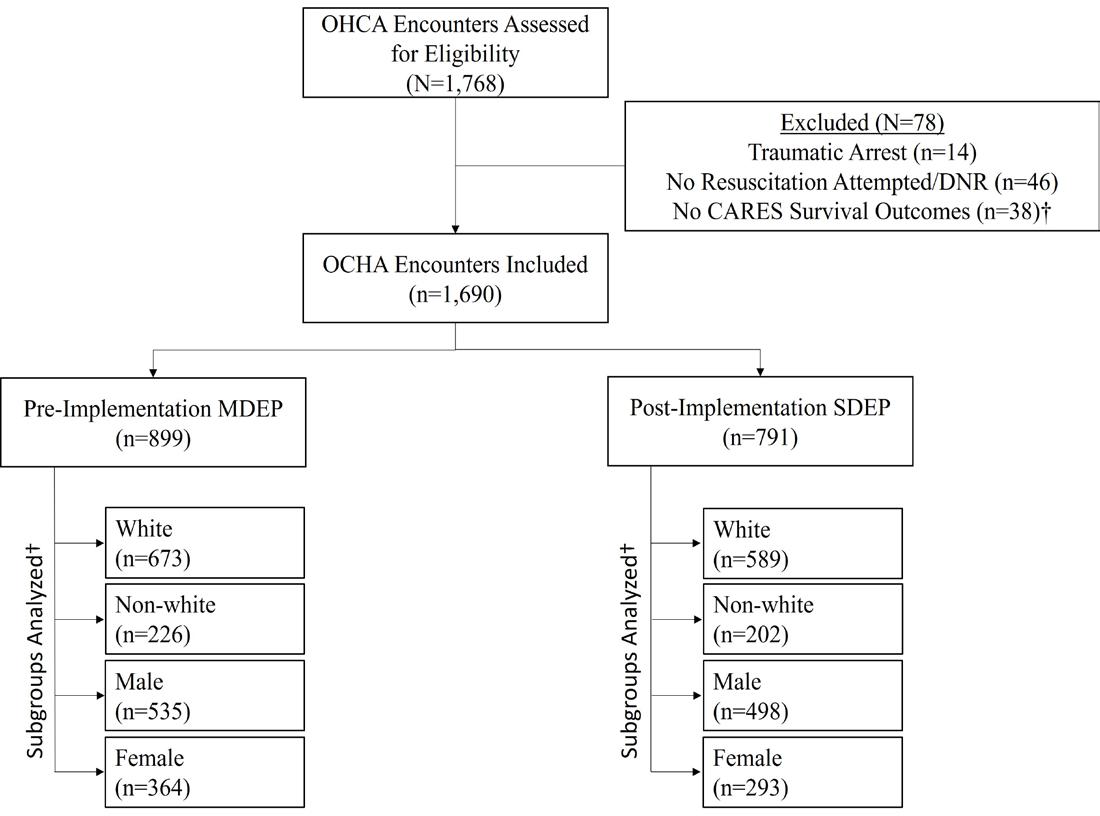
Figure 1. The study flow diagram.
†While 38 total encounters were without CARES outcomes, only 18 additional encounters were excluded once encounters for traumatic arrest and those with no resuscitation attempted/DNR were excluded.
OHCA, out-of-hospital cardiac arrest; DNR, do not resuscitate; CARES, Cardiac Arrest Registry to Enhance Survival; MDEP, multidose epinephrine protocol; SDEP, single-dose epinephrine protocol.
survival to hospital discharge (P = .84) or ROSC (P = .13). Table 2 and Figure 2 show the study outcomes by race. The exploratory outcome of favorable neurologic status is presented in Table 2.
Survival to hospital discharge rates did not differ between the single dose and multi-dose epinephrine periods among women (16.7% vs. 13.7%; OR 1.28, 95% CI 0.91-1.80) or men (14.7% vs. 13.5%; OR: 1.11, 95% CI 0.97-1.28). When adjusting for potential confounders, similar survival to hospital discharge rates persisted among women (aOR 1.23, 95% CI 0.97-1.56) and men (aOR 1.03, 95% CI 0.93-1.14). However, single dose epinephrine was associated with decreased ROSC in women (aOR 0.61, 95% CI 0.45-0.83) and men (aOR 0.54, 95% CI 0.35-0.83). The interaction between single dose epinephrine implementation and sex was not significant for survival to hospital-discharge rates (P = .47) or ROSC (P = .31). Table 3 and Figure 3 show the study outcomes by sex. The exploratory outcome of favorable neurologic status is presented in Table 3.
Among patients thought to have arrested from a primary cardiac etiology, we found that survival to hospital-discharge rates improved among non-White patients (aOR 1.22, 95%CI 1.01-1.48); however, single dose epinephrine was no longer associated with improved survival to hospital-discharge rates among White patients (aOR 1.28, 95%CI 0.84-1.95). Similar to the overall group, survival to hospital-discharge rates were similar between single dose and multi-dose epinephrine among men (aOR 1.17, 95% CI 0.73-1.87) and women (aOR 1.35, 95%CI 0.97-1.91) thought to have arrested from a primary cardiac etiology. Supplemental Tables 2-3 and Supplemental Figures 1-2
present study outcomes in these pre-specified subgroups.
DISCUSSION
The key finding of this subgroup analysis is that implementation of a single dose epinephrine protocol was associated with similar survival to hospital-discharge rates among men, women, and non-White patients. While we did detect an improvement in survival to hospital-discharge rates among White patients, we suspect that this was likely driven by unmeasured confounders and social determinants of health. We do not believe that there is a meaningful, biologically plausible reason for the single dose epinephrine protocol to improve outcomes among White patients but not among other key subgroups.17,18
Prior research has found that Black patients and other racial minority patients are more likely to suffer poorer outcomes from OHCA compared to White patients, including worse rates of survival - hospital discharge and neurologic recovery.15,16 This has been previously associated with several factors, including lower rates of bystander CPR and defibrillator use in non-White compared to White patients.15,16 No study to date has explored the effect of single dose vs. multi-dose epinephrine in race subgroups. In this analysis we found that White patients had improved survival to hospitaldischarge rates with the single dose epinephrine protocol while non-White patients had no significant difference in survival to hospital-discharge rates. Given that nearly 75% of our sample was comprised of White patients and that the point estimates for survival to hospital discharge with single-does epinephrine implementation were similar for White and non-White patients, we believe that our study was likely underpowered to detect a significant difference in survival to hospital discharge among non-White patients.
Furthermore, among the patients thought to have arrested from a primary cardiac etiology, we observed the opposite: non-White patients had improved survival to hospital discharge while White patients had similar rates of survival to hospital discharge. The difference in findings between all patients compared to just those with presumed arrest from a cardiac etiology suggests the possibility that there might not be an association at all between single dose epinephrine implementation and survival to hospital discharge. Our findings should be cautiously interpreted: We do not think there is a causative physiologic reason driving these differences in outcomes. Rather, it is more likely that race is a marker of risk, which may be driven by socioeconomic, environmental, or access-to-care factors.
Prior studies comparing survival to hospital-discharge rates between sexes in OHCA patients have not detected a difference between men or women after controlling for confounders.2,12,13 Ours is the first study to evaluate the effect of single dose vs. multi-dose epinephrine on subgroups by sex. In our study, rates of ROSC decreased post-implementation in both male and female subgroups without a significant difference between sexes. Despite this decrease in ROSC rates, SHD rates were similar between the single dose and
Table 1. Cohort characteristics
MDEP, multidose epinephrine protocol;SDEP, single-dose epinephrine protocol; IQR, interquartile range; CPR, cardiopulmonary resuscitation; AED, automated external defibrillator.
multi-dose epinephrine groups in both sexes. Thus, our findings add to existing literature indicating that a difference in OHCA outcomes driven by sex is unlikely.
Our exploratory outcome of favorable neurologic status remained unchanged post-implementation in all subgroups. Although the PARAMEDIC-2 trial found similar rates of favorable neurologic outcomes between the epinephrine and placebo groups overall, severe neurologic disability was more common in the epinephrine group.6 It is possible that a dose-dependent relationship with epinephrine drives neurologic outcomes. Therefore, we theorized that single dose
epinephrine patients might have improved neurologic outcomes compared to multi-dose epinephrine patients. However, we did not observe this in our study. Importantly, our study was not powered to examine for differences in favorable neurologic outcomes. Due to the modest sample size, we were unable to perform fully adjusted analyses for favorable neurologic outcomes in the race and sex subgroups. The ongoing Epinephrine Dose: Optimal vs. Standard Evaluation randomized controlled trial and other OHCA resuscitation studies may help us understand the relationship between epinephrine and meaningful neurologic recovery.
Table 1. Continued.
Pre-Implementation MDEP (N = 899), n (%)
Sex Male n=535 (%) Female n=364
Post-Implementation SDEP (N = 791), n (%)
All rows show n (%) unless otherwise indicated. MDEP, multidose epinephrine protocol; SDEP, single dose epinephrine protocol; IQR, interquartile range; CPR, cardiopulmonary resuscitation; AED, automatic external defibrillator.
LIMITATIONS
This study has limitations. First, the five participating EMS systems are all within North Carolina, limiting geographic generalizability. Next, use of the pre-post implementation study design exposed the study to unknown confounders that would not occur in randomized controlled trials. The CARES database does not contain the number of epinephrine doses administered or the time to administration. Nor is this information available from the local EMS agencies. Because our dataset was completely deidentified, we were unable to link encounters to the CARES registry or perform additional prehospital EHR review. Therefore, we were unable to restrict the cohort to only those who received
epinephrine, account for protocol violations, or determine which patients received the correct dose of epinephrine. Therefore, we were unable to conduct a per protocol analysis.
Additionally, CARES outcomes are not adjudicated, thus risking misclassification bias. It is also possible that some patients identified as multiracial or transgender, thus further risking misclassification bias. Although misclassification bias regarding race is often a concern, the race data in CARES was recently validated in a large cohort of nearly 25,000 patients. Investigators found a high degree of concordance between race data in the CARES database and Medicare data.22 Therefore, using CARES to determine a patient’s race is
Table 2. Race subgroups.
1 Adjusted for age, sex (male vs female), witnessed arrest (yes/no), location of the arrest (home, medical facility , other), automatic e xternal defibrillator availability (yes/no), emergency medical services response interval, the presence of a shockable rhythm (yes/no), and bystander cardiopulmonary resuscitation (yes/no).
2 Adjusted only for age and sex given the number of events. MDEP, multidose epinephrine protocol; SDEP, single-dose epinephrine protocol; ROSC, return of spontaneous circulation; SHD, survival to hospital discharge.
Interaction (Implementation cohort x sex)
Odds Ratio (95% CI)
Female
Unadjusted Adjusted 1
Post- implementation SDEP (n = 293), n (%)
Pre- implementation MDEP (n = 364), n (%)
Odds Ratio (95%CI)
Male
Table 3. Sex subgroups.
Unadjusted Adjusted 1
Post-implementation SDEP (n = 498), n (%)
Pre- implementation MDEP (n = 535), n (%)
1 Adjusted for age, race (White vs non-White), witnessed arrest (yes/no), location of the arrest (home, medical facility , other), automatic external defibrillator availability, emergency medical services response interval, the presence of a shockable rhythm, receiving bystander cardiopulmonary resuscitation.
2 Adjusted only for age and race given the number of events. MDEP, multi-dose epinephrine protocol; SDEP, single dose epinephrine protocol; ROSC, return of spontaneous circulation; SHD, survival to hospital discharge.
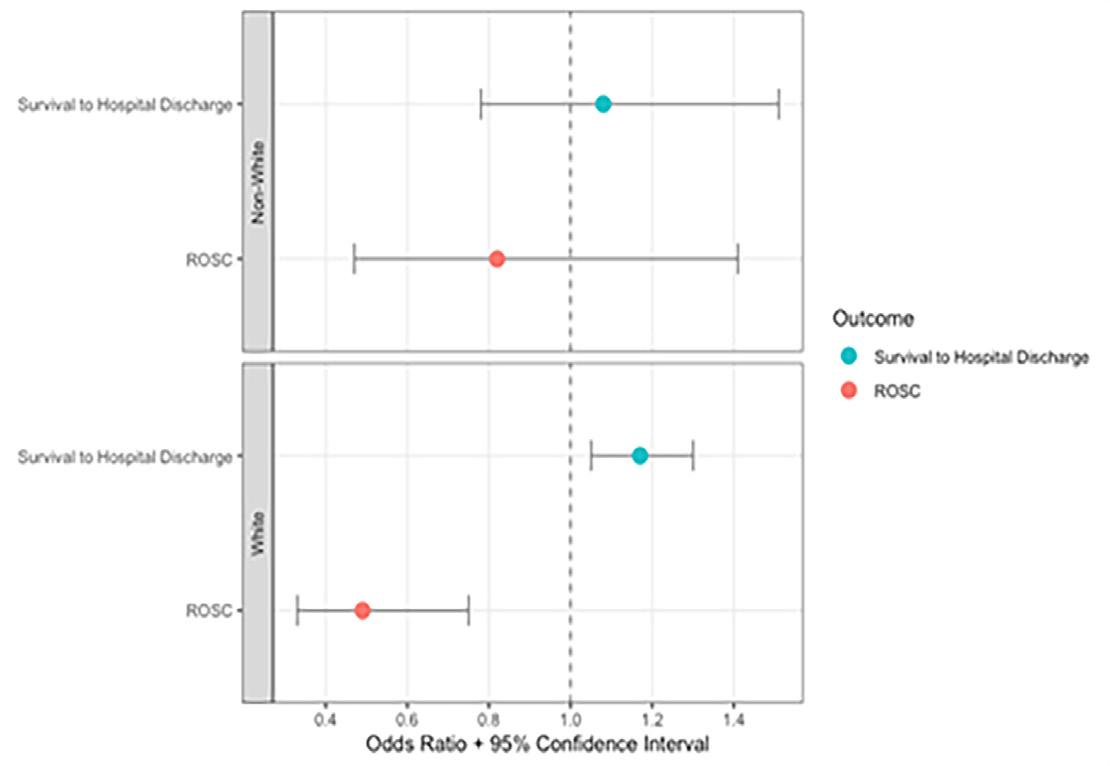
Figure 2. Single dose vs. multi-dose epinephrine adjusted odds ratios for study outcomes among all White vs non-White patients. Models were adjusted for age, witnessed arrest, location of the arrest, automatic external defibrillator availability, emergency medical services response interval, the presence of a shockable rhythm, receiving bystander cardiopulmonary resuscitation, and sex. ROSC, return of spontaneous circulation.
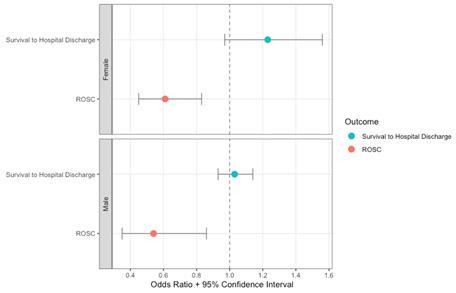
Figure 3. Single dose vs. multi-dose epinephrine adjusted odds ratios for study outcomes among all male vs female patients. Models were adjusted for age, witnessed arrest, location of the arrest, automatic external defibrillator availability, emergency medical services response interval, the presence of a shockable rhythm, receiving bystander cardiopulmonary resuscitation, and race.
ROSC, return of spontaneous circulation; CPR, cardiopulmonary resuscitation.
reasonable. Due to the modest sample size, we analyzed race as a dichotomous variable. This may have masked variation between race subgroups. However, making race a two- or three-level variable is a common statistical approach in studies with modest sample size.24-28 Lastly, tests for interactions and
within subgroups may be underpowered given the study’s sample size. This may have limited our ability to detect meaningful differences between groups, particularly among non-White patients given the smaller sample size.
CONCLUSION
Implementation of a single dose epinephrine protocol was associated with similar survival to hospital- discharge rates among men, women, and non-White patients compared to the multi-dose epinephrine. However, survival to hospitaldischarge rates did improve among White patients. In the subgroup of patients thought to have arrested from a primary cardiac etiology, we noted that survival to hospital-discharge rates improved with the single dose epinephrine protocol among non-White patients but were similar among men, women, and White patients. These differences are likely driven by unmeasured confounders or inadequate power. We do not believe there is a physiologic basis for the difference in outcomes between White and non-White patients with single dose epinephrine implementation. Future single dose epinephrine studies should continue to evaluate and monitor for potential OHCA care disparities and leverage larger cohorts so that more granular race findings can be reported.
AUTHORS CONTINUED
James E. Winslow, MD, MPH†
R. Darrell Nelson, MD†
Jason P. Stopyra, MD, MS†
Simon A. Mahler, MD, MS†¶**
||University of Kansas School of Medicine, Department of Emergency Medicine, Kansas City, Kansas
#The Ohio State University, Department of Emergency Medicine, Columbus, Ohio
¶Wake Forest University School of Medicine, Department of Epidemiology and Prevention, Winston-Salem, North Carolina
**Wake Forest University School of Medicine, Department of Implementation Science, Winston-Salem, North Carolina
Address for Correspondence: Nicklaus P. Ashburn, MD, Wake Forest University School of Medicine, Department of Emergency Medicine, Medical Center Boulevard, Winston-Salem, NC 27157. Email: n.ashburn@wakehealth.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Blaschke et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Sasson C, Rogers MAM, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63-81.
2. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254-e743.
3. Lee SY, Song KJ, Shin SD, et al. A disparity in outcomes of out-ofhospital cardiac arrest by community socioeconomic status: a ten-year observational study. Resuscitation. 2018;126:130-6.
4. Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S366-S468.
5. Jacobs IG, Finn JC, Jelinek GA, et al. Effect of adrenaline on survival in out-of-hospital cardiac arrest: a randomised double-blind placebocontrolled trial. Resuscitation. 2011;82(9):1138-43.
6. Perkins GD, Ji C, Deakin CD, et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med. 2018;379(8):711-21.
7. Ng KT, Teoh WY. The effect of prehospital epinephrine in out-ofhospital cardiac arrest: a systematic review and meta-analysis. Prehosp Disaster Med. 2019;34(5):532-9.
8. Overgaard CB, Dzavík V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation. 2008;118(10):1047-56.
9. Ristagno G, Tang W, Huang L, et al. Epinephrine reduces cerebral perfusion during cardiopulmonary resuscitation. Crit Care Med 2009;37(4):1408-15.
10. Callaway CW. Epinephrine for cardiac arrest. Curr Opin Cardiol 2013;28(1):36-42.
11. Ashburn NP, Beaver BP, Snavely AC, et al. One and done epinephrine in out-of-hospital cardiac arrest? Outcomes in a multiagency United States study. Prehosp Emerg Care 2023;27(6):751-7.
12. Ng YY, Wah W, Liu N, et al. Associations between gender and cardiac arrest outcomes in Pan-Asian out-of-hospital cardiac arrest patients. Resuscitation. 2016;102:116-21.
13. Dicker B, Conaglen K, Howie G. Gender and survival from out-ofhospital cardiac arrest: a New Zealand registry study. Emerg Med J 2018;35(6):367-71.
14. Zhao D, Post WS, Blasco-Colmenares E, et al. Racial differences in sudden cardiac death. Circulation. 2019;139(14):1688-97.
15. Mehta NK, Allam S, Mazimba S, et al. Racial, ethnic, and socioeconomic disparities in out-of-hospital cardiac arrest within the United States: Now is the time for change. Heart Rhythm O2 2022;3(6Part B):857-63.
16. Monlezun DJ, Samura AT, Patel RS, et al. Racial and socioeconomic
disparities in out-of-hospital cardiac arrest outcomes: artificial intelligence-augmented propensity score and geospatial cohort analysis of 3,952 patients. Cardiol Res Pract. 2021;2021:3180987.
17. Javed Z, Haisum Maqsood M, Yahya T, et al. Race, racism, and cardiovascular health: applying a social determinants of health framework to racial/ethnic disparities in cardiovascular disease. Circ Cardiovasc Qual Outcomes. 2022;15(1):e007917.
18. Churchwell K, Elkind MSV, Benjamin RM, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142(24):e454-68.
19. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. 2007. Available at: http://www.equator-network.org/reporting-guidelines/ strobe/. Accessed June 10, 2024.
20. George TS, Ashburn NP, Snavely AC, et al. Does single dose epinephrine improve outcomes for patients with out-of-hospital cardiac arrest and bystander CPR or a shockable rhythm? Prehosp Emerg Care. 2025;29(1):37-45.
21. Cardiac Arrest Registry to Enhance Survival (CARES). 2021 Data Dictionary. 2021. Available at: https://mycares.net/sitepages/ uploads/2020/Data%20Dictionary%20(2021).pdf. Accessed May 1 2024.
22. Chan PS, Merritt R, Chang A, et al. Race and ethnicity data in the cardiac arrest registry to enhance survival: Insights from Medicare self-reported data. Resuscitation. 2022;180:64-7.
23. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
24. Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329(9):600-6.
25. Garcia RA, Spertus JA, Girotra S, et al. Racial and ethnic differences in bystander CPR for witnessed cardiac arrest. N Engl J Med 2022;387(17):1569-78.
26. Veasey CJ, Snavely AC, Kearns ZL, et al. The high-sensitivity HEART pathway safely reduces hospitalizations regardless of sex or race in a multisite prospective US cohort. Clin Cardiol 2024;47(10):e70027.
27. Popp LM, Ashburn NP, Snavely AC, et al. Race differences in cardiac testing rates for patients with chest pain in a multisite cohort. Acad Emerg Med. 2023;30(10):1020-8.
28. Supples MW, Snavely AC, O’Neill JC, et al. Sex and race differences in the performance of the European Society of Cardiology 0/1-h algorithm with high-sensitivity troponin T. Clin Cardiol 2024;47(2):e24199.
Original Research
Comparison of Cardiopulmonary Resuscitation Quality in a Simulated Model: At Incident Scene vs During EMS Transport
Murat Çetin, MD*
Gökhan Yilmaz, MD†
İlhan Uz, MD‡
Turgay Yılmaz Kılıç, MD§
Erkan Guvenç, MD||
Volkan Ergun#
Ebru Şener Araz, MD#
Başak Bayram, MD¶
Brit Jeffrey Long, MD**
Michael Gottlieb, MD††
William J. Brady, MD‡‡
Department of Emergency Medicine, Izmir Dr. Behçet Uz Children’s Disease and Surgery
Education and Research Hospital, Izmir, Türkiye
Department of Emergency Medicine, Konya Meram Public Hospital, Konya, Türkiye
Department of Emergency Medicine, Faculty of Medicine, Ege University, Izmir, Türkiye
Department of Emergency Medicine, Izmir Faculty of Medicine, University of Health Sciences, Izmir Bayraklı City Hospital, İzmir, Türkiye
Department of Emergency Health Services, Izmir Provincial Directorate of Health, Izmir, Türkiye
Department of Emergency Health Services Training Unit, Izmir Provincial Directorate of Health, Izmir, Türkiye
Izmir Metropolitan Municipality Esrefpasa Hospital, Izmir, Türkiye
Department of Emergency Medicine, Brooke Army Medical Center, Fort Sam Houston, TX, USA
Department of Emergency Medicine, Rush University Medical Center, Chicago, IL, USA
Department of Emergency Medicine, University of Virginia School of Medicine, Charlottesville, VA, USA
Section Editor: Lesley Osborn, MD
Submission history: Submitted December 5, 2024; Revision received May 13, 2025; Accepted May 27, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.40234
Introduction: Out-of-hospital cardiac arrest remains a leading cause of death and significantly impacts global health outcomes. International guidelines emphasize the importance of high-quality CPR (cardiopulmonary resuscitation).
Objectives: Our goal was to compare CPR efficiency using the criteria recommended by international guidelines between two out-of-hospital cardiac arrest intervention scenarios: CPR at the incident site; and CPR during patient transport to the hospital by emergency medical services.
Methods: In each of the two scenarios, five full two-minute cycles of cardiac compression were applied to a manikin according to international guidelines. The CPR quality parameters were chest compression rate, chest compression depth recorded by the manikin, and investigator-evaluated correct hand placement on the manikin.
Results: We analyzed data from 240 CPR cycles provided by 24 healthcare professionals. The mean chest compression rate was higher (120.5±10.9/minutes vs 125.3±14.7/min, P = .001) and the mean chest compression depth was shallower (43.9±6.6 millimeters [mm] vs 37.9±7.2 mm, P = .001) in the on-the-move group. The two groups’ appropriate hand placement rates were similar (92.1±5.4% vs 92.2±4.5%, P = .48)
Conclusion: In this study, the moving ambulance simulation demonstrated that chest compressions were administered at a rate exceeding recommended guidelines and at a shallower depth than recommended, while the frequency of correct hand placement remained comparable. If the patient requires transportation from the scene of the incident, the healthcare team must be aware of the potential adverse effects on the chest compression quality. [West J Emerg Med. 2025;26(5)1322–1327.]
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) remains a leading cause of death and significantly impacts global health outcomes 1 Early recognition, early cardiopulmonary resuscitation (CPR), and defibrillation are the key components of the first response to immediately restore and maintain circulation, as emphasized in the CPR guidelines by major health authorities such as the American Heart Association (AHA) and the European Resuscitation Council (ERC).2,3 These guidelines emphasize the importance of high-quality CPR. Key components of high-quality CPR include maintaining an adequate chest compression rate of 100-120 compressions per minute and a chest compression depth of 5-6 centimeters (cm), allowing for full chest recoil and minimizing interruptions.4 Despite the critical nature of high-quality CPR, various factors can compromise its effectiveness, including human fatigue and logistical challenges during patient transport.
Performing effective, high-quality CPR is crucial for survival and prevention of morbidities in OHCA.5-8 However, previous studies revealed inadequate CPR efficiency and duration during the intervention and transportation of OHCA patients to healthcare facilities.9-11 Several more recent studies have demonstrated better CPR quality during the transport of OHCA cases.12 However, there have been variations in methodology prompting the need for studies in controlled settings with easily reproducible methods.
The decision to perform CPR on site or during transport in OHCA cases remains a significant challenge for prehospital healthcare responders. Various factors, including patientrelated factors, local circumstances, paramedic-related factors, and the organizational structure, can influence this decision.13 However, one of the most important questions is whether effective CPR can be performed in a moving ambulance. In this study we aimed to compare the efficiency of CPR performed on site vs during transport, using the latest criteria recommended by current CPR guidelines.
METHODS
Study Setting and Design
This manikin-based practice assessment study was conducted on 3-4 November 2022 to evaluate the compression quality comparatively between two settings common to OHCA incidents. Participants applied a standardized chest compression methodology recommended by AHA and ERC guidelines, with two minutes of chest compression cycles followed by 10 seconds of pulse check in both scenarios. No real-time feedback devices were used during CPR. The on-site scenario involved performing CPR on the scene of the OHCA event, while the on-the-move scenario involved beginning CPR while taking the manikin off the cot, continuing while loading it into the ambulance, and transporting it to the hospital.
Hypothetically, the OHCA scene was deemed a safe roadside location 10 kilometers (km) from the hospital point. In both scenarios, the healthcare team departed from the hospital
Population Health Research Capsule
What do we already know about this issue?
High-quality cardiopulmonary resuscitation (CPR) is essential for survival in out-ofhospital cardiac arrest (OHCA). However, CPR quality can be compromised by factors such as rescuer fatigue and patient transport conditions.
What was the research question?
Does the quality of CPR performed during ambulance transport differ from that performed at the incident scene?
What was the major finding of the study?
Chest compressions delivered in a moving ambulance were performed at a higher rate but were significantly shallower compared to those administered on site, while hand placement accuracy remained similar.
How does this improve population health?
Understanding the limitations of CPR quality during transport emphasizes the importance of on-site resuscitation, targeted training, and system-level planning. This knowledge can improve outcomes in OHCA by guiding EMS strategies to maximize CPR effectiveness before and during transport.
and arrived by ambulance at the scene of the incident. While the on-site scenario was managed entirely at the scene, the on-themove scenario involved transport from the scene of the event to the hospital with compression continued in the ambulance, returning to the hospital point at a 50 km/hour speed on the road with two bends and two bumps on the route. Each scenario was conducted for five cycles. Healthcare team members were selected from volunteer emergency medical technicians (EMT) with < two years of professional experience. Participants were not informed of the study hypothesis. Volunteers were excluded if they had conditions that might affect their CPR practice (eg, motion sickness, dizziness).
We evaluated CPR efficiency by measuring the chest compression rate (compression per minute) and chest compression depth (millimeters) recorded by the manikin during CPR and the appropriateness of hand placement on the manikin (correct/incorrect) per the evaluator’s judgment. We calculated the average values of the chest compression rate
and depth measurements and the percentage of correct hand placements from five cycles and recorded the values as the assessment result for each participant. The institutional review board at Necmettin Erbakan University, Konya, Türkiye (2022/4047), approved this study.
Statistical Analysis
After controlling for normal distribution assumptions, we presented the continuous data using mean score and 95% Cl for normally distributed variables. Categorical data were presented using frequency and percentage values. We compared continuous data using the independent samples t-test between independent groups and the paired-samples t-test between dependent groups. A type 1 error level of 5% was considered the statistically significant threshold in a 95% CI. A sample size estimation based on the two related groups designed to detect a difference of 0.7±1 cm difference for chest compression. Depth between the two scenarios with 80% of study power revealed that 19 participants were needed as the study population. With the addition of a 20% attrition margin, we recruited 24 participants for the study. All statistical analyses were done in SPSS 22 (IBM Corporation, Armonk, NY).
RESULTS
Twenty-four participants, with a mean age of 23.9 years of age (SD 1.7 years) and 18 of whom were males (75%), completed 240 cycles of CPR. The aggregated and per-cycle results for CPR assessments in the on-site and on-the-move groups are presented in Table 1 The mean chest compression rate was higher (120.5±10.9 /min vs 125.3 ± 14.7 /min) and the mean chest compression depth was shallower (43.9 ± 6.6 mm vs. 37.9 ± 7.2 mm) in the on-the-move group. The two groups’ appropriate hand placement rates were similar.
We also compared the CPR assessment criteria measurements between the first and last cycles (Table 2). The chest compression rate measurements were similar in both groups. The chest compression depth measurements were significantly higher in the first cycle in both the on-site (49.2 ± 7.5 mm vs 39.7 ± 6.5 mm) and the on-the-move groups (41.8 ± 8.4 mm vs 34.7 ± 8.5 mm). However, appropriate hand placement rates were higher in the last cycles of both groups (on site: 85.9 ± 9.8% vs 93.5 ± 3.7%; on the move: 85.8 ± 7.6% vs. 93.5 ± 4.3%).
DISCUSSION
A key component of OHCA cardiac arrest management is maintaining high-quality CPR. In this study we found that onthe-move CPR resulted in higher chest compression rates and shallower chest compression depths. Not maintaining an optimal chest compression rate is associated with inadequate recoil and ventricular filling, whereas non-optimal chest compression depth may result in inadequate cardiac output and perfusion. The previous evidence suggests that poor-quality CPR might affect return of spontaneous circulation since an appropriate chest compression rate is needed to establish an optimal
coronary blood flow to achieve spontaneous circulation.14 One factor affecting the differences between settings might be the relationship between the chest compression rate and depth. A previous CPR-focused manikin study showed that participants were unable to perform CPR at sufficient depth as their rate of administering chest compressions increased.15 Accordingly, chest compression depth could not be achieved in > 50% of applications when the chest compression rate was 120/min and in > 60% when the rate was 130/min. Our study supports the interconnectedness of these findings. Another study by Havel et al16 reported that the chest compression depth was lower than optimal on the scene and in the moving ambulance (the scene group 3.7 cm vs the moving ambulance group 3.6 cm). Our chest compression depth results in the on-the-move group were similar to those reported in the study by Havel et al, but our on-site group had higher chest compression depth than the reported values.
Based on these previous findings, we can postulate that EMTs might have felt more stressed in the moving ambulance and could not apply adequate pressure for a sufficient chest compression depth. This may also explain the higher chest compression rate, which eventually caused fatigue and further decreased the chest compression depth. Other potential factors could be the narrow range of motion in the ambulance, environmental problems like bumps and bend in the road, and other suboptimal conditions caused by the movement of the ambulance, which may complicate CPR and prevent the first responder from performing CPR at sufficient depth.
In our study, chest compression rate was similar between the first and last cycles in both scenarios. However, EMTs performed CPR closer to the recommended depth at the first cycle on site and below the recommended depth in the moving ambulance (Figure 1). In addition, they failed to achieve adequate chest compression depth through the later cycles. Bjorshol et al17 reported that only half of the subjects who completed chest compressions performed CPR at the desired quality, that the quality of CPR did not deteriorate in the first two minutes of CPR, and the CPR quality deteriorated due to fatigue in the CPR practitioner toward the end of CPR. Hightower et al18 also evaluated the temporal variation of chest compression quality and asked the subjects to perform CPR for five minutes; they found that the average compression efficiency decreased by 90% after the first minute. In the same study, the chest compression rate was preserved, but the chest compression quality decreased over time. Swapping the person performing chest compressions could potentially be an effective way to counteract fatigue. On the other hand, the hand placement in both scenarios improved over time. This might be related to the lack of experience of the EMTs using the manikin and implies the need for dedicated time to get used to the manikin to eliminate the initial stress.
The results of our study suggest that on-the-move CPR is more prone to decreased quality due to shallower chest compression depth and higher rate of chest compressions, both
Chest compression depth (mm)
1st
Appropriate hand placement (%)
/min, per minute; mm, millimeter.
/min, per minute; mm, millimeter.
of which might affect the outcomes in OHCA management. Some steps to be taken to avoid the negative consequences of OHCA management can include the following: applying all CPR on site until the patient is stabilized for transport; more focused training for on-the-move CPR; and monitoring of onthe-move CPR with directed feedback. Since the evidence in the literature varies between studies and settings, there is a need for a more standardized protocol to evaluate ambulatory EMT applications for OHCA management, which might also be used for internal assessment and training of these first responders.
Table 1. Aggregated and per-cycle cardiopulmonary resuscitation assessment in study groups
Table 2. Comparison of cardiopulmonary resuscitation assessments between the first and last of five cycles.
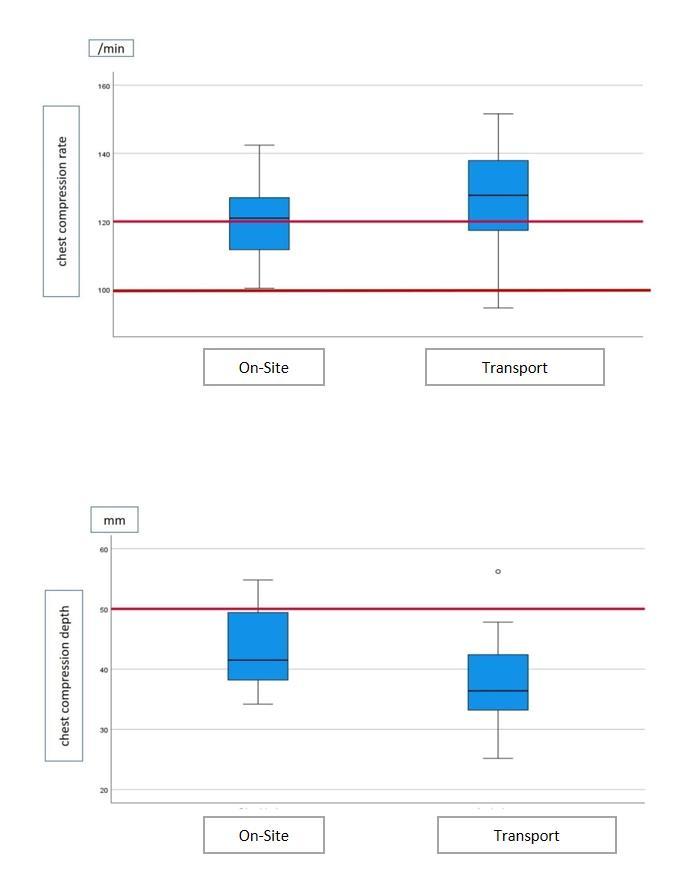
Figure 1. Status of the quality values of cardiopulmonary resuscitation performed by first responders in our study, compared to standard CPR. CPR, cardiopulmonary resuscitation; min, minute; mm, millimeter.
LIMITATIONS
Several limitations should be considered for this study. First, this was a manikin-based simulation study, which might not truly reflect the practice patterns in actual OHCA incidents. Second, because this study was conducted at a single site, the participants’ CPR performance may not be generalizable to all EMS personnel. In this study, we evaluated the CPR practices of EMTs with < two years of experience. It can be anticipated that the results might differ with more experienced healthcare professionals. Third, as the goal of CPR is the return of spontaneous circulation, our manikin simulation could not detect this outcome; however, given the emphasis in the existing literature on high-quality CPR as a key link in the chain of survival, we believe these findings remain highly relevant to patient care.
Lastly, we did not evaluate rebound time and compression fraction—important indicators of CPR quality—due to limitations of the manikin used in the study. Additionally, the absence of real-time feedback tools, such as a metronome, feedback device, or end-tidal carbon dioxide monitoring,
during both on-scene and on-the-move CPR represents another limitation. This lack of feedback may have affected the consistency and quality of CPR performance, potentially influencing the study outcomes. Regarding the use of mechanical chest compression devices, we believe that such equipment can offer consistent compression quality, especially in challenging environments. However, in many low- and middle-income countries, including our own, access to these devices is limited due to financial and logistical constraints. As highlighted in recent literature, the scarcity of essential medical equipment, including mechanical CPR devices, remains a significant barrier in resource-limited settings.
Besides these limitations, our study provides the most current data for local applications in Türkiye for OHCA management, according to the most recent guidelines, and highlights areas to improve the administration of CPR by first responders.
CONCLUSION
In this simulated model, performing CPR on the move resulted in a small increase in chest compression rate and significantly shallower chest compression depth compared with on site. Based upon these findings, we recommend performing CPR on site when possible. Future studies evaluating CPR quality in actual patients, comparing the effects of on-site vs transport CPR, would be valuable in characterizing the quality of resuscitation for out-of-hospital coronary arrest.
Address for Correspondence: Murat Çetin, MD, Department of Emergency Medicine, Izmir Dr. Behçet Uz Children’s Disease and Surgery Education and Research Hospital, Izmir, TÜRKİYE. Email: muratcetinn@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Çetin et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts Lancet. 2018;391(10124):9709.
2. Panchal AR, Bartos JA, Cabanas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Circulation. 2020;142(16_suppl_2):S366-S468.
3. Soar J, Bottiger BW, Carli P, et al. European Resuscitation Council Guidelines 2021: adult advanced life support Resuscitation 2021;61:115-51.
4. Perkins GD, Graesner JT, Semeraro F, et al. European Resuscitation Council Guidelines 2021: executive summary Resuscitation 2021;161:1-60.
5. Idris AH, Guffey D, Pepe PE, et al. Chest compression rates and survival following out-of-hospital cardiac arrest Crit Care Med 2015;43(4):840-8.
6. Cheskes S, Schmicker RH, Verbeek PR, et al. The impact of perishock pause on survival from out-of-hospital shockable cardiac arrest during the Resuscitation Outcomes Consortium PRIMED trial Resuscitation. 2014;85(3):336-42.
7. Stiell IG, Brown SP, Christenson J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40(4):1192-8.
8. Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest compression fraction determines survival in patients with out-ofhospital ventricular fibrillation Circulation. 2009;120(13):1241-7.
9. Braunfels S, Meinhard K, Zieher B, et al. A randomized, controlled trial of the efficacy of closed chest compressions in ambulances Prehosp Emerg Care. 1997;1(3):128-31.
10. Sunde K, Wik L, Steen PA. Quality of mechanical, manual standard and active compression-decompression CPR on the arrest site and during transport in a manikin model Resuscitation. 1997;34(3):235-42.
11. Roberts BG, Machine vs. manual cardiopulmonary resuscitation in moving vehicles EMT J. 1979;3(1):30-4.
12. Cheskes S, Byers A, Zhan C, et al. CPR quality during out-of-hospital cardiac arrest transport Resuscitation. 2017;114:34-39.
13. de Graaf C, de Kruif AJTCM, Beesems SG, et al. To transport or to terminate resuscitation on-site. What factors influence EMS decisions in patients without ROSC? A mixed-methods study. Resuscitation 2021;164:84-92.
14. Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association Circulation 2013;128(4):417-35.
15. Nagafuchi K, Hifumi T, Nishimoto N, et al. Chest compression depth and rate - effect on instructor visual assessment of chest compression quality Circ J. 2019;83(2):418-423.
16. Havel C, Schreiber W, Riedmuller E, et al. Quality of closed chest compression in ambulance vehicles, flying helicopters and at the scene Resuscitation. 2007;73(2):264-70.
17. Bjorshol CA, Sunde K, Myklebust H, et al. Decay in chest compression quality due to fatigue is rare during prolonged advanced life support in a manikin model Scand J Trauma Resusc Emerg Med. 2011;19:46.
18. Hightower D, Thomas SH, Stone CK, et al. Decay in quality of closed-chest compressions over time Ann Emerg Med 1995;26(3):300-3.
Association of Rising Ambient Temperatures with Increased Violence Worldwide: Systematic Review and Meta-Analysis
Vivek Chauhan, MD*
Suman Thakur, MD*
Sagar Galwankar, MBBS, MPH†
Sarah Temple, MD†
Section Editor: Gary Gaddis, MD
Indira Ghandi Medical College and Hospital, Department of Medicine, Shimla, Himachal Pradesh, India
Florida State University College of Medicine Emergency Medicine Residency Program at Sarasota Memorial Hospital, Department of Emergency Medicine, Florida
Submission history: Submitted January 26, 2025; Revision received April 15, 2025; Accepted April 14, 2025
Electronically published September 25, 2025
Full text available through open ccess at http://escholarship.org/uc/uciem_westjem
DOI 10.5811/westjem.42055
Introduction: Climate change has significantly impacted human health worldwide, contributing to the rise of emerging infectious diseases, allergies, pollution, natural disasters, non-communicable diseases, and malnutrition. One crucial but often overlooked area where climate change has had a notable effect is upon interpersonal violence.
Methods: Following PRISMA guidelines, we searched PubMed and Epistemonikos for studies measuring the effect of temperature on violence. Inclusion criteria encompassed peer-reviewed, English-language articles reporting an association between temperature and violence. Data extraction focused on various forms of violence including homicides, assaults, sexual assaults, suicides, intimate partner violence, riots, and civil wars, and we assessed article quality using Joanna Briggs Institute criteria.
Results: We included a total of 37 studies from 11 countries, three subcontinental regions, and two global-level analyses in this review. Of these, 46% originated from the United States. Rising ambient temperatures were significantly associated with increases in homicides (10 studies), assaults (15 studies), sexual assaults (8 studies), firearm violence (5 studies), intimate partner violence (9 studies), and suicides involving violent methods (9 studies). Conversely, no association was found between temperature and non-violent crimes. Civil wars and riots were also linked to temperature increases in all relevant studies. A meta-analysis of eight studies on violence showed that each 1°C increase in ambient temperature results in 1.64% (95% CI 1.23-2.19%) increase in violence (P<.01).
Conclusion: This review demonstrates a significant association between rising temperatures and increased worldwide incidents of violence and self-harm. These findings underscore the urgent need for public health strategies and interventions to mitigate the societal and health impacts of climate change-induced temperature increases. [West J Emerg Med. 2025;26(5)1328–1337.]
INTRODUCTION
The global rise in temperatures due to climate change is a well-documented phenomenon with widespread effects on the environment, economy, and human health. While attention has been focused on the physical and environmental consequences of climate change, less consideration has been given to its impact on social behavior. A recently published overview of 94 systematic reviews published since 2015 on the impact of
climate on human health showed that the reviews covered 10 health outcomes with the three most common being infectious diseases, mortality, and respiratory/cardiovascular/neurological diseases.1 One critical issue missing from the summary of these 94 systematic reviews was the link between increased temperatures and violence, both interpersonal and collective. Violence, broadly defined as physical force intended to cause harm, manifests in several forms including homicides,
assaults, intimate partner violence (IPV), sexual assaults, suicides, and collective violence such as riots and civil wars. Studies across diverse geographical regions have suggested that warmer temperatures can exacerbate violent behavior, likely due to a combination of physiological and psychological factors. For instance, higher temperatures are thought to increase irritability and aggression, reduce inhibition, and heighten arousal, all of which may contribute to violent acts.2 While the relationship between temperature and violence is becoming increasingly recognized, the mechanisms underlying this connection remain poorly understood.
Our goal was to review the existing evidence on the impact of rising temperatures on various forms of violence. Through examining studies from various nations, we sought to provide a comprehensive understanding of this neglected but critical public health issue, highlighting the need for interventions to mitigate violence in a warming world.
METHODS
We performed a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methods3 using the protocol published in the International Prospective Register of Systematic Review (PROSPERO) (CRD42024581202).
Search Strategy
We searched two open-access databases, PubMed and Epistemonikos, on July 30, 2024 for peer-reviewed articles on violence and temperature. We operationalized different permutations of each keyword for the two databases as follows: Pubmed: ((Temperature) OR (‘heat wave’) OR (‘extreme heat’) OR (‘cold wave’) OR (‘extreme cold’)) AND (“Violence” [Mesh]) Epistemonikos: (title:(Violence) OR abstract:(Violence)) AND (title:(Temperature OR “heat wave” OR “cold spell” OR “extreme heat” OR “extreme cold”) OR abstract:(Temperature OR “heat wave” OR “cold spell” OR “extreme heat” OR “extreme cold”))
Screening and Eligibility
We applied a series of inclusion and exclusion criteria. Articles were included if they were 1) written in English, 2) published in a peer-reviewed journal, and 3) studied the association of temperature with violence. We excluded articles if they 1) were not original, 2) did not describe the effect of temperature on violence, or 3) were a systematic review.
Extraction and Analysis
Extraction was performed by two investigators independently, who obtained the following information: study characteristics (first author, year of publication, country, years for which violence-related data was collected number of incidents studied); characteristics of violence (assaults, murders, sexual assaults, suicides, robbery, collective
Population Health Research Capsule
What do we already know about this issue? Research has shown an association between ambient temperatures and interpersonal violence.
What was the research question?
What is the impact of rising ambient temperature on various types of violence?
What was the major finding of the study?
The meta-analysis of 8 studies on violence showed that each 1°C increase in ambient temperature results in 1.64% (95% CI 1.23-2.19%) increase in violence (P<.01).
How does this improve population health?
Proactive preparedness during extreme heat events could help alleviate the burden of violence-related injuries and mental health issues on public health systems and law enforcement.
violence, civil wars, etc); and outcome data (effect of temperature on violence).
Study Quality
We used the Joanna Briggs Institute’s critical appraisal checklist for evaluation of the quality of the analytical, cross-sectional studies.4 The tool was applied to all studies that were included in the review. None of the studies were excluded based on the outcome of quality assessment. The tool assessed quality using eight questions. A score of 1 was assigned for the answer “Yes,” and a score of 0 was assigned for the answer “No,” “unclear,” or “not applicable.” The scores were graded as low, moderate or high if the total score was ≤ 3, 4-6, and ≥ 7, respectively. The quality assessment was performed independently by two investigators, and any disagreement was settled by discussion.
RESULTS
Literature Search
Our initial search resulted in 247 results in PubMed and 22 in Epistemonikos, which were imported into EndNote reference management software (Clarivate, London, United Kingdom). Of these 269 articles, 10 were duplicates, leaving 259 articles for the screening and eligibility stages (Figure 1). Of the 259 articles screened, we excluded 188 that did not meet the
Chauhan
inclusion criteria, leaving us with 73 articles for retrieval. We reviewed 71 full texts for eligibility as two could not be retrieved. Of these 71 articles, we excluded five systematic reviews, 11 non-peer reviewed articles, and 18 articles that did not describe the effect of temperature on violence, leaving a total of 37 articles to be included in the final review5-41 (Table 1). The process of screening and selecting studies is shown in the PRISMA flow diagram (Figure 1).
Study Characteristics
In our final analysis we included 37 studies from 11 countries (Australia, Belgium, Italy, USA, Switzerland, Hong Kong, South Korea, UK, Taiwan, Spain, and Finland), three subcontinental regions, and two global-level studies (Table 1). Among these, the USA accounted for the largest proportion, with 17 studies (46%), followed by the UK with three studies, and Italy, Australia, and Belgium with two studies each. Interpersonal assaults were the most frequently analyzed dependent variable—examined in 16 studies— followed by suicides involving violent methods in eight studies. Firearm violence, collective violence (riots or civil wars), and intimate partner violence (IPV) were each analyzed in four studies (Table 1). The number of studies exploring the association between temperature and specific forms of violence was as follows: homicides (10 studies); assaults (15 studies); IPV (9 studies); sexual assaults (8 studies); suicides (9 studies), robbery (7 studies); firearmrelated violence (5 studies); and civil wars and riots (2 studies each) (Table 2).
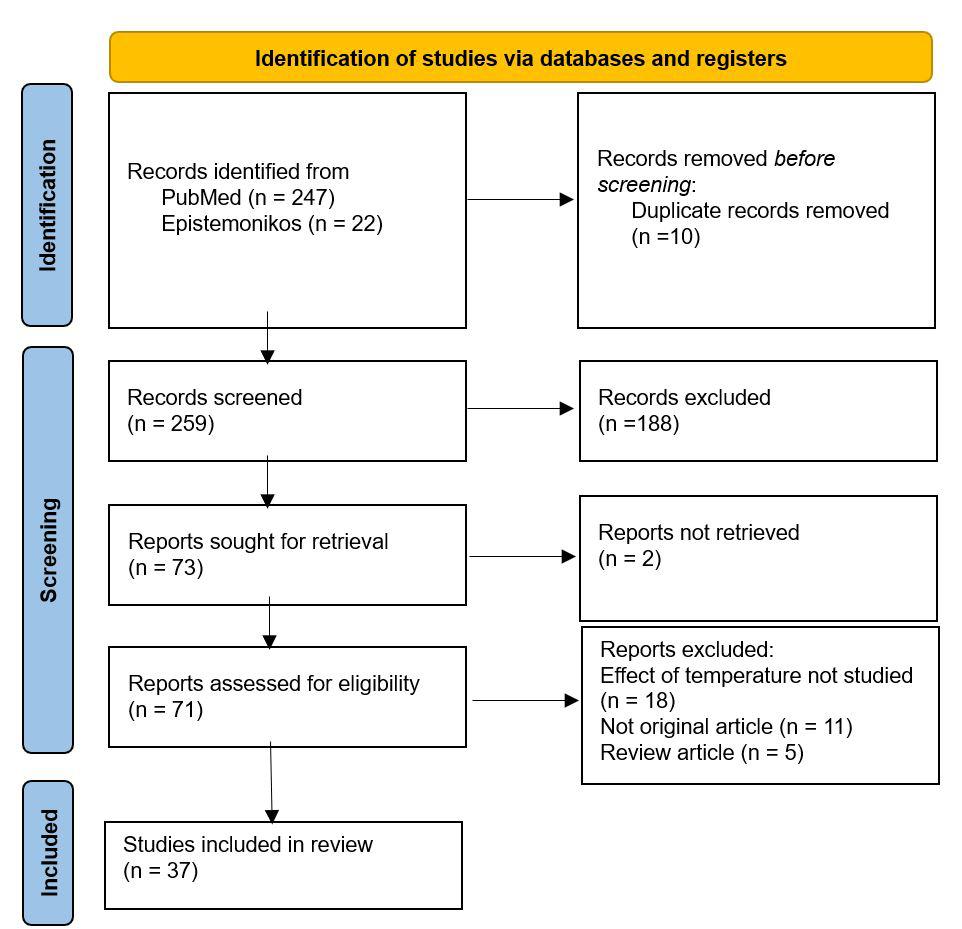
Of 37 studies, 28 reported absolute incident counts for various forms of violence (Table 3). The aggregated totals from these studies were as follows:
• Assaults: 5,590,523 incidents (across 12 studies)
• Suicides: 468,905 incidents (across 7 studies)
• Collective violence: 133,500 incidents (across 4 studies)
• Firearm-related incidents: 273,377 incidents (across 2 studies)
• Intimate partner violence: 164,123 incidents (across 4 studies)
Definitions
Violent Crime
The term violent crime encompasses a range of offenses as defined by the authors, including murder, assault, sexual assault, robbery, firearm-related violence, suicides, domestic violence, civil wars, and conflicts.
Non-violent and Violent Suicides
Suicides were classified based on International Classification of Diseases, 9th Rev (ICD-9) codes. Non-violent suicides (ICD-9 codes E950–E952) include those caused by poisoning with solids, liquids, gases, or vapors. All other forms of suicides were categorized as violent suicides (ICD-9 codes E953–E959).
Temperature
The measurement of temperature variations showed significant heterogeneity in the timeframes used across studies. The timeframes included 17 daily measurements, 10 monthly measurements, three 3- or 6-hourly intervals, three yearly measurements, two measurements at quarterly intervals, one at 6-monthly intervals, and one that recorded weekly measurements (Table 1).
Outcome Analysis: Effect of Temperature on Violence
All 37 studies used standard statistical methods to assess the relationship between temperature and violence. Of these, 36 studies reported a positive association between rising ambient temperatures and violence, including both self-harm and interpersonal violence. The one study that did not identify a positive association was hospital-based, focusing on assaultrelated Accident & Emergency Department visits. This study may not accurately reflect the true extent of violence occurring in the broader community.37
The studies summarized their data differently making it difficult for us to pool the data for a meta-analysis. However, eight studies that reported the risk of increase in violence for each degree Celsius rise of ambient temperature were pooled in the meta-analysis (Figure 2).
Homicides (Table 3)
The association between temperature and homicides was explored in 10 studies conducted over a cumulative 117 years in four countries: the USA (seven studies), Finland, Australia,
Figure 1. PRISMA flow diagram for the systematic review of association of ambient temperature with violence.
Table 1. Characteristics of the included studies in the systematic review of the association between
Assaults (Table 3)
and South Korea (one study each).5-7,9,15,23,24,26,38,39 The studies were carried out at the country (five studies), state (one study), and city levels (four studies), with temperature measured in the context of a yearly timeframe in one study, quarterly in one study, monthly in three studies, and daily timeframes in five studies. All 10 studies demonstrated a significant positive association between higher ambient temperatures and increased homicide rates.
Fifteen studies analyzed the relationship between temperature and assaults over a combined duration of 160 years. These studies spanned eight cities, six countries, one
Rising Ambient Temperatures and Their Association with Increased Violence
Table 2. Types of violence reported by the studies included in a systematic review of the association between temperature and violence 5-41
First author Years Region Temperature time unit Spatial unit Dependent variables
Anderson CA;1987 3 USA Daily City Homicide, Assault, Rape, Robbery, Theft
Anderson CA;1984 10 USA Quarterly Country Homicide, Rape, Robbery, Theft
Anderson CA;1997 45 USA Yearly Country Homicide, Assault, Rape, Robbery, Property Crime
Bar S;2022 22 Switzerland Daily Country Suicide
Basu R;2018 9 USA Daily State Homicide, Psychosis, Neurosis, Self-injury/Suicide
Bolfrass A;2015 21 Global Yearly Country Civil War
Carlsmith JM;1979 5 USA Daily Country Riot
Chau PH;2020 39 Hong Kong Monthly SAR Suicide (violent and non-violent)
Cook MR;2012 2 USA Daily City Assault
Dana EG;2018 5 USA Daily County Firearm violence
Heo S;2024 5 South Korea Daily Country Homicide, Assault, Robbery, IPV
Hodgkinson T;2023 12 Australia Quarterly State Assault, Rape, Robbery, IPV
Jude Kieltyka;2016 14 USA Daily City Firearm violence
Lemon DJ;2017 3 UK Daily County Assaults
Lin HC;2008 7 Taiwan Monthly Country Suicide (violent and non-violent)
Linkowsky P;1992 16 Belgium Monthly Country Suicide (violent and non-violent)
Lyons VH;2022 6 USA Daily Country Firearm violence
Maes M;1994 9 Belgium Weekly Country Suicide (violent)
Mares D;2013 20 USA Monthly City Homicide, Assault, Rape, Robbery
Michael RP;1983 4 USA Monthly Country Homicide, Assault, Rape, Robbery
Michael RP;1986 5 USA Monthly Country IPV
Michel SJ;2016 6 USA Daily City Homicide, Assault, Rape, Firearm Violence
Moore SC;2022 4 UK Daily City Assault
O’Loughlin J;2014 20 East Africa 6-Monthly Sub-Continent Riot
O’Loughlin J;2012 21 Sub-Saharan Africa Monthly Sub-Continent Civil War
Preti A;1998 12 Italy Monthly Country Suicide (violent and non-violent)
Preti A;2000 12 Italy Monthly Country Attempted suicide (violent, non-violent)
Rotton J;1985 2 USA Daily City Assault
Rotton J;2000 2 USA 3-hourly City IPV
Rotton J;2001 2 USA 6-hourly City Assault, IPV
Ruderman D;2021 6 USA Daily Country Firearm violence
Sanz-Barbero B;2018 9 Spain Daily City IPV
Sivarajasingam V;2004 6 UK Monthly City Assault related A&E admissions
Stevens HR;2024 6 Australia Daily City Homicide, Assault, Rape, IPV
Tiihonen J;2017 18 Finland Monthly Country Homicide, Assault
Zhou X;2024 30 Global Yearly Global Attempted suicide, IPV
Zhu Y;2023 9 South Asia Daily Sub-Continent IPV
USA, United States of America; UK, United Kingdom; SAR, Special Administrative Region; IPV, intimate partner violence; A&E, Accident and Emergency Department.
state, and one at a global level.5, 7, 13, 15, 16, 18, 23, 24, 26, 27, 33, 34, 37-39
Temperature variations were recorded at the following intervals: at 3-hour intervals in one study; daily in seven studies; monthly in four studies; quarterly in two; and yearly in two studies. All studies, except one that focused on a single hospital’s assault-related visits, found a
significant association between rising temperatures and increased assaults. 37
Sexual Assaults (Rape) (Table 3)
Eight studies investigated the link between rising temperatures and sexual assaults over a cumulative 100 years, six studies in the USA and two in Australia.5-7, 16, 23, 24, 26,
Table 3. Incidents of violence as reported by the studies included in the systematic review of the association between temperature and violence. First
Basu R;2018
38 Data were collected in three studies at the country level, one at the state level, and four at the city level, with temperature in three studies recorded daily, monthly in two studies, quarterly in two studies, and yearly in one study. All studies identified a significant increase in sexual assaults with higher ambient temperatures.
Firearm Violence (Table
3)
Five studies from the USA analyzed firearm violence over a combined 32 years, using daily temperature measurements.14, 17, 21, 26, 35 Data were collected in three studies at the country level and two studies at city levels. All studies found a significant positive association between rising daily temperatures and increased firearm violence.
Domestic or Intimate Partner Violence (IPV) (Table 3)
Nine studies, spanning 41 years, examined the association between ambient temperatures and IPV.15, 16, 25, 32, 34, 36, 38, 40, 41 Three studies represented the USA, two represented Australia,
and one each represented Spain, South Korea, and South Asia), with data collected in four studies at the city level, two at the country level, and one each at regional and state levels. In one study, temperature was recorded at 6-hour intervals, while temperature was recorded in five studies on a daily basis, and one study each recorded temperature at quarterly and monthly intervals. Seven studies provided actual numbers, reporting a total of 1,797,812 incidents. All nine studies showed a significant positive association between temperature and IPV.
Suicides (Table 3)
Nine studies conducted over a cumulative 147 years examined the relationship between temperature and suicides in six countries, and one study examined that relationship globally.8, 9, 12, 19, 20, 22, 30, 31, 40 Temperature was measured daily in two studies, weekly in one study, monthly in five studies, and yearly in one study. Seven studies reported a total of 468,905 suicide incidents, categorizing them as violent (ICD-9 codes
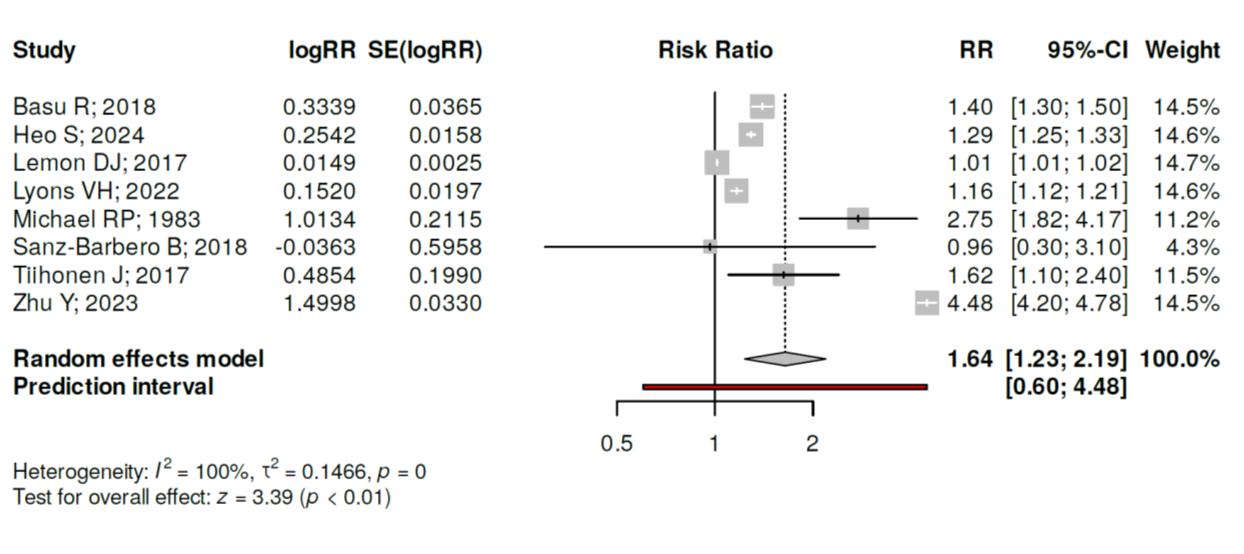
Figure 2. Meta-analysis of eight studies that reported risk of increased violence for each degree Celsius rise in ambient temperature. Based on the investigations performed using a random effects model with inverse variance method, a statistically significant effect can be observed. The summarized effect of each degree Celsius rise of temperature was an increase in violence by 1.64% with a 95% confidence interval of 1.23-2.19. The test for overall effect verified a statistically significant P value <.01. A significant heterogeneity was spotted (P<.01), suggesting fluctuating effects in extent and/or direction. The I2 value shows that 100% of the inconsistency among the cohorts originates from heterogeneity rather than random chance.
E953–959) or non-violent (ICD-9 codes E950–952). All studies found a significant association between rising temperatures and suicides, with two reporting an effect on only violent suicides, while one found a link to both types.
Civil Wars (Table 3)
Two studies examined temperature and civil wars.10, 29 One analyzed global incidents over 20 years, with yearly temperature variations, while the other focused on East Africa over 19 years, with 6-monthly temperature data. Both studies reported a significant association between higher temperatures and an increase in civil war incidents.
Riots (Table 3)
Two studies explored the relationship between temperature and riots.11, 28 One study in the USA used four years of daily temperature data, while the other, from SubSaharan Africa, spanned 32 years using monthly temperature variations. Both studies showed a significant positive association between high temperatures and riots.
Non-Violent Crimes (Table 3)
Non-violent crimes, including robbery, arson, theft, and property crimes, were analyzed by Anderson CA et al between 1971–1995 in the USA.5-7 Using daily, quarterly, and yearly temperature data, the study found no significant association between ambient temperature and non-violent crimes.
Trauma Center Admissions (Table 3)
Four studies found that trauma center admissions following assaults increased with rising temperatures, while one study reported no significant association.9, 13, 14, 26, 37
Psychiatric Illnesses
(Table 3)
One study examined the link between temperature and psychiatric illnesses presenting to hospitals.9 A 10°F increase in temperature during summer resulted in the following: psychosis, +2.9% (0.7-5.2); neurosis, +5.3% (3.8-7.6); self-injury, +5.8% (4.5-7.1); and inflicted injuries: +7.9% (7.3-8.4). During winter, the same temperature increase led to these results: psychosis, +3.9% (1.6-6.3); neurosis, +6.0% (4.5-7.5); self-injury, +7.2% (5.7-8.8); and inflicted injuries, +10.6% (9.8-11.4). The study found a significant association between ambient temperatures and psychiatric illnesses, with a stronger effect observed in winter.
DISCUSSION
Rising global temperatures, along with other effects of climate change, have shown a clear and significant impact on human health. Various issues such as vector-borne and infectious diseases, environmental pollution hazards, injuries due to natural disasters, allergies, respiratory illnesses, malnutrition, and the mental health impacts of disasters are well-documented concerns.42 However, one critical health issue often overlooked is the relationship between global warming and violence. This systematic review highlights the significant influence of rising temperatures on incidents of violence worldwide.
Violence is commonly defined as an act of physical force intended to cause harm and can be broadly categorized into interpersonal violence and group conflicts. Interpersonal violence includes homicides, assaults, sexual assaults, IPV, and firearm violence, while group conflicts cover riots and
Rising Ambient Temperatures and Their Association with Increased Violence civil wars.
Our review demonstrates that rising ambient temperatures are significantly associated with an increase in homicides, assaults, sexual assaults, IPV, and firearm violence. This relationship was observed across various timeframes of temperature measurement—daily, weekly, monthly, quarterly, and yearly—and across a wide range of global communities. Our meta-analysis of eight studies on violence showed that each 1°C increase in ambient temperature results in 1.64% (95% confidence interval 1.23-2.19%) increase in violence (P<.01).
Hsiang et al quantified the effect of climate on violence, finding that each one standard deviation increase in temperature results in a 4% increase in interpersonal violence and a 14% increase in intergroup conflict.43 Projections suggest that, by the end of the century, climate change could result in an additional 22,000 homicides, 1.2 million aggravated assaults, and 2.3 million simple assaults in the United States alone compared to 2010.44 Interestingly, temperature appears to primarily influence violent crimes, such as assaults and homicides, while non-violent crimes, such as robbery, arson, and property crimes, remain unaffected.5-7 Similarly, studies show a significant rise in violent suicides associated with higher temperatures but no such effect on non-violent suicides, such as those involving poisoning.9, 12, 19, 20, 22, 30, 31, 40
The Mechanisms Behind Temperature-Aggression
The General Aggression Model (GAM) provides a framework for understanding human responses to provoking situations. It suggests that a person’s reaction—thoughtful or impulsive—depends on their internal state, influenced by affect, cognition, and arousal.2 For example:
• Affect: Discomfort or pain increases anger and hostility.
• Cognition: Media or social priming can condition individuals to be more violent.
• Arousal: Situational arousal, such as from exercise, can amplify aggression in response to provocation (a concept explained by the excitation transfer theory).
High temperatures, as per the temperature-aggression hypothesis, lead to discomfort that heightens aggression across all three domains of GAM. This increases the likelihood of impulsive violent behaviors, even with minimal provocation.45
In regions where warm temperatures are not inherently uncomfortable, the routine activity theory offers an alternate explanation. It says that warmer temperatures encourage outdoor activities and social interactions, thereby increasing the likelihood of interpersonal conflicts and exposure to crimeprone environments.46
Implications for Public Health and Safety
Higher ambient temperatures place significant burdens on hospitals and emergency services as they deal with increased cases of heat-related injuries, trauma, assault,
mental health crises, and self-harm.9, 13, 14, 26, 31, 37 Targeted police interventions, informed by spatiotemporal analysis, have proven effective in mitigating violence in high-risk areas without displacing the issue to other regions.13 Advanced warning systems for heat waves and hotter days can enable hospitals to expect increased arrivals of patients due to violence. However, the extra numbers of arrivals may still be too small to meaningfully impact the needed staffing and resources that should be scheduled to address the increased number of violence-related emergencies that could be anticipated.
Temperature and Mental Health
While lunar cycles have long been associated with mental health (eg, the term “lunatic”), studies have found no substantial link between lunar phases and psychiatric admissions or discharges.47 Conversely, the relationship between temperature and mental health is well-established.9 A 10°F (5.6°C) increase in mean apparent temperature during warm seasons correlates with increases in emergency visits for the following: mental health disorders (+4.8%); self-injury/ suicide (+5.8%); and intentional injuries/homicides (+7.9%), Intimate partner violence rates are consistently higher on hotter days, even when partner interactions remain constant throughout the year. Zhu et al estimated that a 1°C increase in annual mean temperature results in a 4.49% increase in IPV prevalence.25
Need for Research and Interventions
Despite growing evidence linking temperature to violence, there is limited research on mitigating its effects through heat warning systems and public health strategies. Policymakers and researchers must prioritize developing novel interventions aimed at reducing aggression and violence during hotter days. These could include the following:
• Community-level public health campaigns to “cool tempers” during heatwaves.
• Enhanced preparedness for hospitals and police during extreme weather events.
• Investigation of technologies and policies to create safer environments amid climate change.
As global temperatures continue to rise, addressing this under-recognized public health concern is crucial to protecting communities and reducing the societal impacts of climate change.
LIMITATIONS
The included studies vary in terms of locations, timeframes, and methods for measuring temperature and violence, limiting generalizability across different regions and cultures. Many studies may not have controlled for other factors such as socioeconomic status, urbanization, or social tensions, which could influence both temperature sensitivity and violence rates. Most studies are cross-sectional, and the scarcity of longitudinal data makes it difficult to establish causal relationships between
Rising Ambient Temperatures and Their Association with Increased Violence
temperature increases and violence over time. Most studies come from high-income countries, especially the USA and Europe, with fewer from low- and middle-income regions, which limits the applicability to global populations.
Differences in how violence is defined and measured across studies, including official crime statistics vs hospital admissions, may result in discrepancies and fail to capture all forms of violence. Despite these limitations, the review highlights important trends and calls for more targeted research to better understand the link between temperature and violence.
CONCLUSION
This systematic review highlights a statistically significant relationship—of a small but detectable effect size—between rising ambient temperature and an increase in violence, including homicides, assaults, sexual assaults, suicides, intimate partner violence, firearm violence, riots, and civil wars. Violent behaviors, both interpersonal and group conflicts, are clearly influenced by ambient temperature increases, while non-violent crimes remain largely unaffected. Our findings emphasize the growing burden on hospitals, law enforcement, and public health systems during heat-related emergencies, including violence-related injuries and mental health crises. Targeted interventions, spatiotemporal analysis of hotspots, and early preparedness during extreme heat events are appropriate mitigation steps. As global temperatures continue to rise, integrating violence prevention into broader climate-adaptation frameworks is an appropriate consideration. Focused research and public health strategies are needed to mitigate the behavioral and societal challenges posed by climate change.
Address for Correspondence: Vivek Chauhan, MD, Indira Ghandi Medical College, Department of Medicine, Shimla, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India, 171001. Email: drvivekshimla@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliaions, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Chauhan et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Rocque RJ, Beaudoin C, Ndjaboue R, et al. Health effects of climate change: an overview of systematic reviews. BMJ open. 2021;11(6):e046333.
2. Allen JJ, Anderson CA, Bushman BJ. The General Aggression Model. Curr Opin Psychol. 2018;19:75-80.
3. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS med. 2009;6(7):e1000100.
4. Munn Z, Moola S, Lisy K, et al. Chapter 5: Systematic Reviews of Prevalence and Incidence. 2019. Available at: https://www. researchgate.net/publication/342593810_Chapter_5_Systematic_ Reviews_of_Prevalence_and_Incidence. Accessed March 15, 2023.
5. Anderson CA. Temperature and aggression: effects on quarterly, yearly, and city rates of violent and nonviolent crime. J Pers Soc Psychol. 1987;52(6):1161-73.
6. Anderson CA, Anderson DC. Ambient temperature and violent crime: tests of the linear and curvilinear hypotheses. J Pers Soc Psychol 1984;46(1):91-7.
7. Anderson CA, Bushman BJ, Groom RW. Hot years and serious and deadly assault: empirical tests of the heat hypothesis. J Pers Soc Psychol. 1997;73(6):1213-23.
8. Bär S, Bundo M, de Schrijver E, et al. Suicides and ambient temperature in Switzerland: a nationwide time-series analysis. Swiss Med Wkly. 2022;152:w30115.
9. Basu R, Gavin L, Pearson D, et al. Examining the association between apparent temperature and mental health-related emergency room visits in California. Am J Epidemiol. 2018;187(4):726-35.
10. Bollfrass A, Shaver A. The effects of temperature on political violence: global evidence at the subnational level. PloS one 2015;10(5):e0123505.
11. Carlsmith JM, Anderson CA. Ambient temperature and the occurrence of collective violence: a new analysis. J Pers Soc Psychol. 1979;37(3):337-44.
12. Chau PH, Yip PSF, Lau HYE, et al. Hot weather and suicide deaths among older adults in Hong Kong, 1976-2014: a retrospective study Int J Environ Res Public Health.2020;17(10).
13. Cook MR, Emick D, Foley C, et al. Daily temperature predicts assault and may allow more efficient policing. Am Surg. 2012;78(4):E194-5.
14. Dana EG, Kara ER, Jennifer A. Predictors of firearm violence in urban communities a machine learning approach. Health Place 2018;51:61-7.
15. Heo S, Choi HM, Lee JT, et al. A nationwide time-series analysis for short-term effects of ambient temperature on violent crime in South Korea. Sci Rep. 2024;14(1):3210.
16. Hodgkinson T, Corcoran J, Andresen MA. Violent assault geographies in northeastern Australia. PloS one. 2023;18(3):e0282522.
17. Kieltyka J, Kucybala K, Crandall M. Ecologic factors relating to firearm injuries and gun violence in Chicago. J Forensic Leg Med. 2016 Jan;37:87-90.
18. Lemon DJ, Partridge R, Pan-Dorset Cardiff Model team. Is weather related to the number of assaults seen at emergency departments? Injury. 2017 Nov;48(11):2438-2442
19. Lin HC, Chen CS, Xirasagar S, et al. Seasonality and climatic
Chauhan et al.
Rising Ambient Temperatures and Their Association with Increased Violence
associations with violent and nonviolent suicide: a population-based study. Neuropsychobiology. 2008;57(1-2):32-7.
20. Linkowski P, Martin F, De Maertelaer V. Effect of some climatic factors on violent and non-violent suicides in Belgium. J Affect Disord. 1992;25(3):161-6.
21. Lyons VH, Gause EL, Spangler KR, et al. Analysis of daily ambient temperature and firearm violence in 100 US Cities. JAMA Netw Open. 2022;5(12):e2247207.
22. Maes M, De Meyer F, Thompson P, et al. Synchronized annual rhythms in violent suicide rate, ambient temperature and the light-dark span. Acta psychiatr Scand. 1994;90(5):391-6.
23. Mares D. Climate change and levels of violence in socially disadvantaged neighborhood groups. J Urban Health. 2013;90(4):768-83.
24. Michael RP, Zumpe D. Annual rhythms in human violence and sexual aggression in the United States and the role of temperature. Soc Biol. 1983;30(3):263-78.
25. Michael RP, Zumpe D. An annual rhythm in the battering of women. Am J Psychiatry. 1986;143(5):637-40.
26. Michel SJ, Wang H, Selvarajah S, et al. Investigating the relationship between weather and violence in Baltimore, Maryland, USA. Injury 2016;47(1):272-6.
27. Moore SC, Woolley TE, White J. An exploration of the multiplicative effect of “other people” and other environmental effects on violence in the night-time environment. Int J Environ Res Public Health 2022;19(24).
28. O’Loughlin J, Linke AM, Witmer FD. Effects of temperature and precipitation variability on the risk of violence in Sub-Saharan Africa, 1980-2012. Proc Natl Acad Sci U S A. 2014 Nov 25;111(47):16712-7.
29. O’Loughlin J, Witmer FD, Linke AM, et al. Climate variability and conflict risk in East Africa, 1990-2009. Proc Natl Acad Sci U S A 2012;109(45):18344-9.
30. Preti A, Miotto P. Seasonality in suicides: the influence of suicide method, gender and age on suicide distribution in Italy. Psychiatry Res. 1998;81(2):219-31.
31. Preti A, Miotto P. Influence of method on seasonal distribution of attempted suicides in Italy. Neuropsychobiology. 2000;41(2):62-72.
32. Rotton J, Cohn EG. Temperature, routine activities, and domestic violence: a reanalysis. Violence Vict. 2001;16(2):203-15.
33. Rotton J, Cohn EG. Violence is a curvilinear function of temperature in Dallas: a replication. J Pers Soc Psychol. 2000;78(6):1074-81.
34. Rotton J, Frey J. Air pollution, weather, and violent crimes: concomitant time-series analysis of archival data. J Pers Soc Psychol. 1985;49(5):1207-20.
35. Ruderman D, Cohn EG. Predictive extrinsic factors in multiple victim shootings. J Prim Prev. 2021;42(1):59-75.
36. Sanz-Barbero B, Linares C, Vives-Cases C, González JL, LópezOssorio JJ, Díaz J. Heat wave and the risk of intimate partner violence. Sci Total Environ. 2018;644:413-9.
37. Sivarajasingam V, Corcoran J, Jones D, et al. Relations between violence, calendar events and ambient conditions. Injury 2004;35(5):467-73.
38. Stevens HR, Graham PL, Beggs PJ, et al. Associations between violent crime inside and outside, air temperature, urban heat island magnitude and urban green space. Int J Biometeorol. 2024;68(4):661-73.
39. Tiihonen J, Halonen P, Tiihonen L, et al. The association of ambient temperature and violent crime. Sci Rep. 2017;7(1):6543.
40. Zhou X, Li R, Cheng P, et al. Global burden of self-harm and interpersonal violence and influencing factors study 1990-2019: analysis of the global burden of disease study. BMC Public Health. 2024;24(1):1035.
41. Zhu Y, He C, Bell M, et al. Association of ambient temperature with the prevalence of intimate partner violence among partnered women in low- and middle-income South Asian countries. JAMA Psychiatry 2023;80(9):952-61.
42. Rossati A. Global warming and its health impact. Int J Occup Environ Med. 2017;8(1):7-20.
43. Hsiang SM, Burke M, Miguel E. Quantifying the influence of climate on human conflict. Science. 2013 Sep 13;341(6151):1235367.
44. Ranson M. Crime, weather, and climate change. J Environ Econ Manage. 2014;67(3):274-302.
45. Anderson CA, Anderson KB, Dorr N, et al. Temperature and aggression. Adv Exp Soc Psychol. 2000:32;63-133.
46. Cohn EG. Weather and crime. Brit J Criminol. 1990;30(1):51-64.
47. Gupta R, Nolan DR, Bux DA, et al. Is it the moon? Effects of the lunar cycle on psychiatric admissions, discharges and length of stay. Swiss Med Wkly. 2019;149:w20070.
Impact of Daily Maximum Temperature on Emergency Department Arrivals and Acuity Levels
Catharina Giudice, MD, MPH*†
Nicholas J. Arisco, PhD‡
Zilin Lu, MPH§
Bryan Stenson, MD*
Caleb Dresser, MD, MPH*†
Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, Massachusetts
Harvard T.H. Chan School of Public Health, Harvard Chan Center for Climate, Health and the Global Environment, Department of Environmental Health, Boston, Massachusetts
Harvard T.H. Chan School of Public Health Department of Global Health and Population, Boston, Massachusetts
Tufts University, Department of Public Health and Community Medicine, Boston, Massachusetts
Section Editor: Gary Gaddis, MD, PhD
Submission history: Submitted February 6, 2025; Revision received May 2, 2025; Accepted May 12, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.42263
Introduction: Heatwaves are becoming more frequent and severe globally. Heat is associated with increases in emergency department (ED) volumes and higher morbidity for a range of chronic conditions. We describe how temperature impacts ED arrivals at different acuity levels.
Methods: We obtained time-series records for daily ED arrivals stratified by Emergency Severity Index (ESI) from 2010 – 2019 from hospital records. Wet-bulb temperature was the exposure of interest; analysis was controlled for precipitation, snow, wind speed, day of week, and federal holidays. We fitted a Poisson model for each ESI category and estimated the association between temperature and ED arrival acuity with a distributed lag non-linear model with three days of lag to account for delayed health effects of temperature.
Results: We analyzed data for 3,652 days totaling 556,663 arrivals between 2010 – 2019. At lag 0, lower temperatures were associated with a reduced relative risk of arrival to the ED for ESI 2, ESI 3, and total arrivals. At higher temperatures, ESI 2 and ESI 3 showed an increased relative risk of arrival (wet-bulb exposure of 25°C at 0-day lag: ESI 2 RR = 1.06 [1.02–1.10]; ESI 3 RR = 1.04 [1.011.07]). While not statistically significant, ESI 1 exhibited a subtle increase in arrivals at the highest temperatures while ESI 4 & 5 displayed a subtle decrease in relative risk of arrivals under these conditions.
Conclusion: Extremes of temperature, particularly heat, appear to affect ED arrivals differently across different acuity levels. Medium- to higher-acuity presentations appear to be more responsive to heat, with a statistically significant increase in ED presentations on days with the highest heat burden. The highest acuity presentations became numerically but not statistically more frequent on days with the highest heat burden, while the lowest acuity presentations decreased numerically but not statistically in these conditions. [West J Emerg Med. 2025;26(5)1338–1344.]
INTRODUCTION
Climate change is becoming an increasingly important determinant of health, with potential operational implications for acute care systems. The global annual average temperature for 2024 has already surpassed pre-industrial era levels by 1.6 ℃1
and, under the most optimistic scenarios, are expected to exceed 2.7 ℃ during the 21st century.2 Episodes of extreme heat are becoming more frequent, prolonged, and extreme throughout the United States. By midcentury, heat indexes exceeding 37.8 ℃ are expected to triple in the Northeast under an intermediate
greenhouse gas emission scenario.3 This has profound implications for health and healthcare delivery, including increases in all-cause mortality, healthcare utilization, rates of death from cardiovascular and respiratory diseases,4 mental health issues,5 accidental and non-accidental trauma,6 and adverse birth outcomes.7 Broadly, heat is known to be a significant environmental contributor to mortality.
Emergency departments (ED), as the primary access point for acute healthcare delivery, also face increases in volume and operational burden due to extreme heat.8 Previous studies have shown a relationship between higher temperatures and increased overall ED use.8,9 However, there is wide variation in the disease severity of patients presenting to EDs and the level of resources required to provide appropriate care. Few studies have looked at how temperature and other environmental variables affect the acuity level of emergency arrivals.10-13 At a facility level, understanding how heat impacts patient presentations across each of the five Emergency Severity Index (ESI) levels may facilitate more informed resource allocation and staffing decisions.
At a community level, knowledge of the range of pathologies for which patients seek care during extreme heat may inform policies and programs intended to preserve health and reduce burden on acute care systems. Our aim in this study was to evaluate relationships between ambient temperature and ED arrival volume across the spectrum of acuity at an urban hospital in the Northeastern US.
METHODS
Setting
This study was completed at an urban, academic medical center in the Northeast region of the US with an annual ED volume of approximately 55,000 patients per year. We chose the study period 2010 – 2019 to exclude the COVID-19 pandemic, during which ED visits did not follow typical volume patterns. The predominant climate in the study region is humid subtropical, characterized by hot, humid summers and an average snowfall of 50 inches during the winter months. Thunderstorms are common from June–August.14
Data Sources
We obtained daily ED arrivals stratified by ESI from 2010–2019 from electronic health records (EHR) at a large, urban hospital. The ESI is a five-level scale used to assess patient stability, risk of deterioration, and anticipated resource needs.15 An ESI 1 is assigned to patients with severe medical conditions requiring immediate lifesaving interventions, while ESI 5 is assigned to patients who are stable and expected to require minimal resources for care. Due to the relatively low volume of patients in the ESI 4 and ESI 5 categories and their similar relative clinical stability and low resource needs, we combined these two groups in this analysis.
We obtained historic weather records from the National Oceanic and Atmospheric Administration, National Centers
Population Health Research Capsule
What do we already know about this issue? Heat is a significant environmental contributor to mortality and has been shown to increase overall emergency department (ED) utilization.
What was the research question? Does the temperature responsiveness of ED arrivals differ by case acuity level?
What was the major finding of the study?
Heat (25 °C) increased ED arrivals for Emergency Severity Index (ESI) 2 (RR=1.06 [1.02–1.10]) and ESI 3 (RR=1.04 [1.01–1.07]).
How does this improve population health? Understanding the impact of extreme heat on ED arrivals informs data-driven climate preparedness and may guide staffing and resource planning during heat waves.
for Environmental Information. Boston Logan International Airport Station (WBAN:14739) was selected due to its proximity to the study site (8.5 km). Federal holidays occurring during the study period were obtained from government historical records.
There is evidence suggesting equivalence between different temperature metrics used to assess heat exposure in population health research.16 For this study, we chose wet-bulb daily maximum temperature as the exposure index, as it combines both ambient temperature and humidity and may better correlate with physiological response to heat.
Statistical Analysis
We performed a Poisson regression time series analysis using a framework of distributed lag nonlinear models (DLNM) to estimate the effect of temperature (℃) on ED arrival volumes for each ESI category. Model specification and choice of control variables were based on prior ED arrival predictive modeling studies.17 We included several control variables, including daily precipitation (millimeters [mm]), wind speed (meters per second), snow (mm), day of the week, day of holiday, day before holiday, and day after holiday. Our exposure of interest was wet-bulb daily maximum temperature, which was modeled using a cubic B-spline with 2 degrees of freedom to account for seasonality and long-term trends in accord with previous studies.18,19 To evaluate for a possible “lag” effect, which is to
Giudice
Impact of
Maximum Temperature on ED Arrivals and Acuity Levels
say, to evaluate for the possibility that the influence of temperature extremes are most pronounced on one of the days subsequent to the day of the temperature extreme, we evaluated the influences of lags of 0, 1, 2, and 3 days.20
Lags were modeled using a cubic B-spline with 4 degrees of freedom. Wind speed was controlled for the day of ED arrival. To evaluate the possibility that the influence of snow and precipitation are most pronounced on one of the days after these events, we evaluated the influence of lags of 0, 1, and 2 days. In the cross-basis function, three internal knots were placed at the 10th, 50th, and 90th percentiles for each environmental variable. We defined the median value of temperature (11.7℃) as the baseline temperature or centering value for calculating the relative risk (RR). We plotted the RR against temperature for each lag and for all lags aggregated.
We conducted sensitivity analysis to test the robustness of changing model choices for daily lagged models, using average and minimum temperature instead of maximum temperature as the primary exposure, and altering the exposure variable choice to include dry-bulb temperature and humidity (Appendix). We used Akaike information criteria values to help guide model selection. All analysis was performed with R software v4.3.2 (R Foundation for Statistical Computing, Vienna, Austria) using package DLNM (v2.4.7) for the distributed lag nonlinear model.
Ethics
This study was approved by the Committee on Clinical Investigations at Beth Israel Deaconess Medical Center (institutional review board) Protocol 2022P000002).
RESULTS
The dataset included 3,652 days and totaled 556,663 arrivals during the study period from 2010 – 2019. The ESI 3 group accounted for the greatest number of arrivals at 297,074 (53%), followed by ESI 2 at 178,031 (32%), ESI 4 and 5 combined at 42,086 (7.6%), and ESI 1 at 39,472 (7.1%) (Figure 1). When aggregated over the study period, total ED arrivals were highest on Mondays and in July, and lowest on Sundays and in February, aligning with established trends in ED volume. Daily time series stratified by ESI indicate a high degree of variability across all ESI groups, without obvious cyclical patterns (Figure 2). Daily maximum wet-bulb temperature for the study period ranged from -13.8 °C to 27.2 °C with a mean of 10.8 °C (SD 8.6 °C).
Figure 3 shows the cumulative exposure-response curves for the different ESI categories with relative risk of 1 set at the median maximum temperature for the study period (11.7 °C). The temperature distribution highlights how, at the extremes of the temperature range, only a small number of hot or cold days occur. At lag 0, lower temperatures were associated with a reduced RR of arrival to the ED for ESI 2, ESI 3, and total arrivals. At higher temperatures, ESI 2, ESI 3, and total arrivals showed an increased RR of arrival. ESI 1 and ESI 4 & 5 did not demonstrate a statistically significant association with temperatures across most temperature ranges.
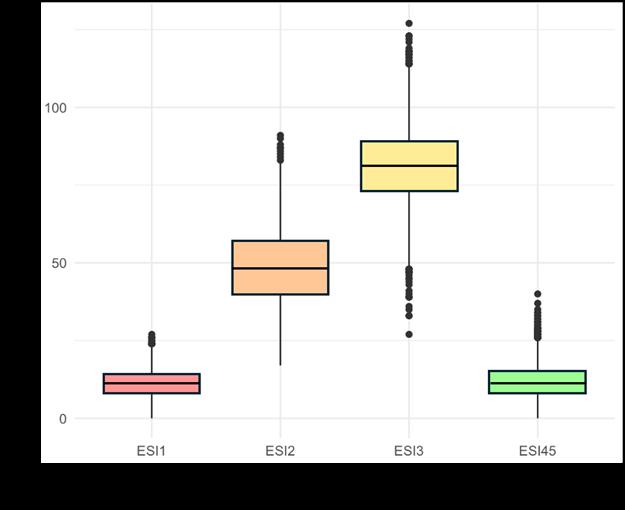
Figure 1. Box plot of total emergency department arrivals per day stratified by Emergency Severity Index category.
ED, emergency department; ESI, Emergency Severity Index.
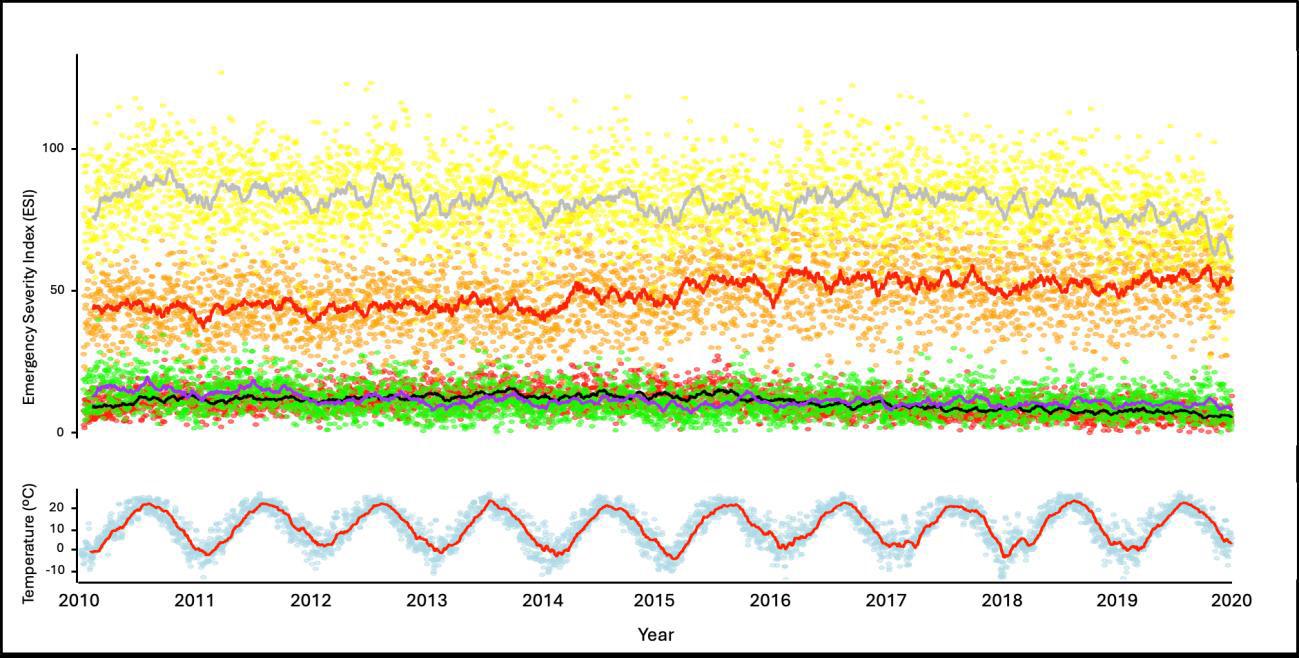
Figure 2. Daily time series of ED arrival for each Emergency Severity Index category and maximum wet-bulb temperature for the study period.
ED, emergency department; ESI, Emergency Severity Index.
On the hottest 5% of days, there was a small numeric increase in the RR of higher acuity arrivals (ESI 1 and ESI 2) and a small numeric decrease in RR of lower-acuity presentations (ESI 3 and ESI 4 & 5), but these effects did not
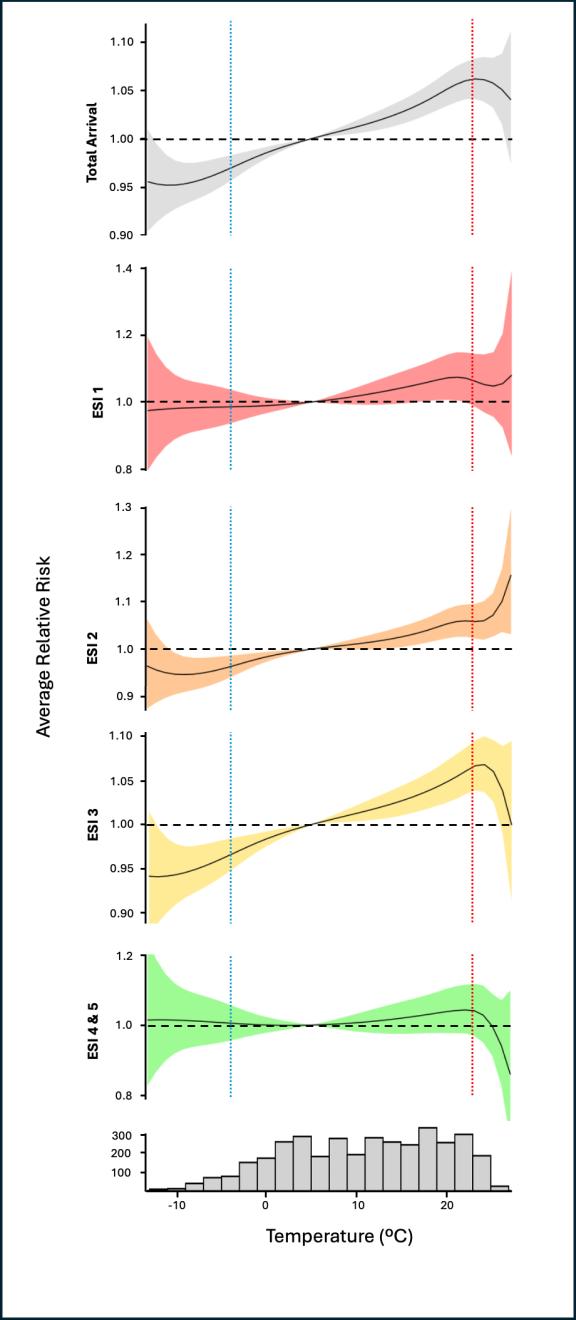
Figure 3. Relative risk (RR) of emergency department presentation in relation to daily maximum temperature at lag 0, stratified by Emergency Severity Index (ESI) category. Solid line is the exposure-response curve (best linear unbiased prediction) with 95% confidence interval (CI) shaded in light red (ESI 1), orange (ESI 2), yellow (ESI 3), and green (ESI 4 and 5). Horizontal dotted line represents RR = 1. Vertical dotted lines represent 5th percentile of temperature (blue = -3.9 °C) and 95th percentile of temperature (red = 23.3 °C).
accounting for lags and non-linear patterns.10-13 Here, we address this gap by employing a distributed lag non-linear Poisson regression to account for seasonality and the delayed health effects of heat across each acuity strata.
Total ED arrivals (aggregated across strata of acuity) increased with temperature, consistent with findings from other studies using EHR or claims data.8,21-23 When stratified by acuity, DLNMs revealed that most of the temperatureresponsiveness of ED arrivals was in medium- to high-acuity cases (ESI 2 and ESI 3). Arrivals in these groups increased with temperature, even at temperatures well below the threshold typically associated with heat-related illness (HRI). During the hottest 5% of days, our data suggest that RR for ESI 2 arrivals continues to increase, whereas for ESI 3, the RR returns toward baseline. The highest acuity (ESI 1) and lowest acuity (ESI 4 & 5) cases did not demonstrate statistically significant associations with temperature. However, on the hottest 5% of days, ESI 1 arrivals exhibited a subtle numeric increase in RR of arrivals with increasing temperature, while ESI 4 and 5 displayed a subtle numeric decrease in RR of arrivals on the hottest days.
At this temperate-zone site, most heat-related illness cases are expected to occur within the upper 10% of temperatures. It is plausible that very hot weather could influence decisions to seek or not seek care for low-acuity conditions. While caution is warranted when interpreting these edge cases, the opposing directions in the upper tails of the DLNM curves at the highest temperatures—an upward numeric change for higher acuity cases and downward numeric change for lower acuity cases— are suggestive of different dynamics affecting heat-sensitive pathologies and/or care-seeking behavior between high- and low-ESI groups. These findings warrant further investigation using larger datasets and/or at sites with higher levels of heat exposure.
With regard to the lagged impact of temperature, we found the overall strongest effect on current day of exposure (lag 0), which aligns with current literature,24-26 although some heterogeneity existed between different ESI groups.
reach statistical significance (Figure 3, Table 2). At extreme temperatures, confidence intervals widened due to the small number of extremely hot or cold days in the dataset, limiting statistical significance. Similarly, for extremes of acuity (ESI 1 and ESI 4 & 5), statistical significance may have been constrained by smaller sample sizes.
DISCUSSION
Our objective in this study was to analyze the relationship between temperature and ED arrivals across strata of patient acuity in a large, urban, academic medical center. To the best of our knowledge, the few studies examining the relationship between temperature and ED acuity have relied on predictive models, without specifically quantifying this relationship while
While additional studies, particularly in regions experiencing a higher frequency of extreme temperature days, will help clarify the relationship between temperature and the acuity of ED arrivals, the numeric effects noted in this study are worth examining. For instance, heat may increase the risk of decompensation of chronic conditions in addition to leading to cases of heatstroke or heat exhaustion, driving higher numeric RR values of high-acuity presentations in the hottest weather. This hypothesis aligns with existing literature that describes extreme heat as a driver for higher morbidity of cardiovascular, respiratory, renal, and psychiatric pathologies, which frequently lead to higher acuity arrivals.4-6,9 Conversely, for lower acuity presentations, adverse weather conditions may deter careseeking behaviors, contributing to lower numeric RR of presentation. Interestingly, prior epidemiologic studies exploring the mortality-temperature relation have suggested a U- or J-shaped exposure-response curve,19, 27 where both high
Table 1. Summary characteristics of variables used in the analysis, including the percentage of days with data for each variable (eg, only 6.3 % of days had snowfall data). Median and range are reported for continuous variables.
Arrival count outcome arrivals per day
[61 - 228] ESI level ordinal rank of ESI, (ie, 1-5)
Day of week calendar categorical day of the week (eg, Monday)
Day of holiday calendar holiday, yes or no 3%
Day before holiday calendar day following a holiday, yes or no
Day after holiday calendar day following a holiday, yes or no
ESI, Emergency Severity Index; mm, millimeter.
and low temperatures are associated with increased mortality, with greater effects observed at higher temperatures. Here, however, we found decreased risk of ED arrivals at lower temperatures, even in sub-zero winter weather.
LIMITATIONS
While the large sample size and extended study period are important strengths of this analysis, some limitations must be considered. First, the data are from a single urban center located in a geographical region with a limited number of extreme heat days. This limits the generalizability of our findings to other geographical regions with different characteristics, including differences in physiologic, cultural, and infrastructure-related resilience to the effects of temperature extremes. Second, as noted above, the small number of days at the extreme ends of the temperature spectrum limited the power of our analysis in detecting statistically significant trends at the extremes, particularly for extreme heat, which is of growing interest in the setting of climate change. Additionally, the 95th percentile wet-bulb temperature in coastal Massachusetts observed during the study period likely poses less heat stress compared to temperatures at other locations in the United States, such as the Southern and Southwestern states. This may have further limited the observed impact of the hottest days on acuity of ED arrival, which would be expected to be more pronounced in regions with greater heat extremes.
Finally, ED arrivals were not stratified by traumatic vs non-traumatic etiologies or by specific diagnosis, which likely respond differently to temperature variations. Here, we focused on the acuity level upon arrival to the ED, while differences in management, length of stay, or admission rates were beyond the
scope of this study. Future studies in diverse geographic regions, incorporating more detailed stratification of presenting etiologies, are warranted to address these limitations and enhance the power and generalizability of these findings.
Understanding the impact of extreme heat on ED arrivals and healthcare use is crucial for development of data-informed climate change adaptation and preparedness strategies. This study and future research examining how heat affects ED acuity may help administrators optimize staffing and resource allocation leading up to or during heat waves. Further stratification by clinical condition could provide valuable insight to inform targeted patient outreach and education programs, enabling healthcare systems to support patients in remaining safe during extreme weather events.
CONCLUSION
In this retrospective study focusing on a temperate region, we found that extremes of temperature, particularly heat, appear to affect ED arrivals differently across different acuity levels. Hotter weather was associated with increased relative risk of moderate-to-high acuity ED arrivals, but relative risks of very high and low acuity arrivals were less associated with extremes of temperature. A non-statistically significant numerical increase in ESI 1 presentations, and a non-statistically significant numerical decrease in ESI 4 and ESI 5 presentations were noted on the hottest days.
This study did not directly evaluate operational costs, staffing impacts, or patient outcomes associated with these changes. To understand the potential impact of extreme heat on ED operations nationwide and inform data-driven climate change preparedness strategies, additional research is necessary on both arrival
Impact of Daily Maximum Temperature on ED Arrivals and Acuity Levels
Table 2. Relative risk of emergency department arrivals and the corresponding 95% confidence interval for each Emergency Severity Index category at lag 0 associated with various temperature points. Blue boxes indicate a statistically significant relative risk < 1, while orqange boxes indicate a statistically significant relative risk > 1.
Note: The relative risk of ED arrivals stratified by acuity for lag 0, lag 1, lag 2, lag 3, and a lag aggregate can be found in the Appendix. ESI, Emergency Severity Index; CI, confidence interval; RR, relative risk.
volumes and on these operationally relevant endpoints in climatically diverse geographic regions that may experience more frequent temperature extremes, ideally incorporating more detailed stratification of presenting etiologies.
REFERENCES
1. Rohde R. Global Temperature Report for 2024. Berkeley Earth. 2025 Jan. Available at: https://berkeleyearth.org/global-temperature-reportfor-2024/. Accessed April 24, 2025.
Address for Correspondence: Catharina Giudice, MD, Department of Emergency Medicine, Beth Israel Deaconess Medical Center; Harvard Chan Center for Climate, Health and the Global Environment, Department of Environmental Health, Harvard T.H. Chan School of Public Health, Boston, Massachusetts. 1 Deaconess Road, Boston, MA 02215 Email: cgiudice@bidmc.harvard.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Giudice et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
2. Intergovernmental Panel on Climate Change (IPCC). Climate Change 2023: Synthesis Report. Contribution of Working Groups I, II, and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. IPCC. 2023. Available at: https://www. ipcc.ch/report/ar6/syr/. Accessed April 24, 2025.
3. Dahl K, Licker R, Abatzoglou JT, et al. Increased frequency of and population exposure to extreme heat index days in the United States during the 21st century. Environ Res Commun. 2019;1(7), 075002.
4. Liu J, Varghese BM, Hansen A, et al. Heat exposure and cardiovascular health outcomes: a systematic review and metaanalysis. Lancet Planet Health. 2022;6(6):e484-95.
5. Nori-Sarma A, Sun S, Sun Y, et al. Association between ambient heat and risk of emergency department visits for mental health among US Adults, 2010 to 2019. JAMA Psychiatry. 2022;79(4):341-9.
6. im Kampe EO, Kovats S, Hajat S. Impact of high ambient temperature on unintentional injuries in high-income countries: a narrative systematic literature review. BMJ Open 2016;6(2):e010399.
7. Nyadanu SD, Dunne J, Tessema GA, et al. Maternal exposure to
Giudice et al.
Impact of Daily Maximum Temperature on ED Arrivals and Acuity Levels
ambient air temperature and adverse birth outcomes: an umbrella review of systematic reviews and meta-analyses. Sci Total Environ 2024;917:170236.
8. Sun S, Weinberger KR, Nori-Sarma A, et al. Ambient heat and risks of emergency department visits among adults in the United States: time stratified case crossover study. BMJ. 2021;375:e065653.
9. Basu R, Pearson D, Malig B, et al. The effect of high ambient temperature on emergency room visits. Epidemiology. 2012;23(6):813-20.
10. Jiang S, Chin KS, Tsui KL. A universal deep learning approach for modeling the flow of patients under different severities. Comput Methods Programs Biomed. 2018;154:191-203.
11. Xu M, Wong TC, Chin KS, et al. Modeling patient visits to accident and emergency department in Hong Kong. IEEE, GBR. 2011:1730-4.
12. Sun Y, Heng BH, Seow YT, et al. Forecasting daily attendances at an emergency department to aid resource planning. BMC Emerg Med 2009;9:1.
13. Tai CC, Lee CC, Shih CL, et al. Effects of ambient temperature on volume, specialty composition and triage levels of emergency department visits. Emerg Med J. 2007;24(9):641-4.
14. Peel MC., Finlayson BL, McMahon TA. Updated world map of the Köppen-Geiger climate classification, Hydrol. Earth Syst. Sci 2007;11(5), 1633–1644.
15. Emergency Nurses Association. Emergency Severity Index Handbook, 5th Ed. 2023. Available at: https://californiaena.org/ wp-content/uploads/2023/05/ESI-Handbook-5th-Edition-3-2023.pdf Accessed: April 24, 2025.
16. Spangler KR, Adams QH, Hu JK, et al. Does choice of outdoor heat metric affect heat-related epidemiologic analyses in the US Medicare population? Environ Epidemiol. 2023;7(4):e261.
17. Jiang S, Liu Q, Ding B. A systematic review of the modelling of
patient arrivals in emergency departments. Quant Imaging Med Surg 2023;13(3):1957-1971.
18. Gasparrini A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med. 2014;33(5):881-99.
19. Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386(9991):369-75.
20. Bao J, Wang Z, Yu C, et al. The influence of temperature on mortality and its lag effect: a study in four Chinese cities with different latitudes. BMC Public Health. 2016;16:375.
21. Zhao Q, Zhang Y, Zhang W, et al. Ambient temperature and emergency department visits: time-series analysis in 12 Chinese cities. Environ Pollut. 2017;224:310-316.
22. Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117(1):61-7.
23. Bernstein AS, Sun S, Weinberger KR, et al. Warm season and emergency department visits to U.S. children’s hospitals. Environ Health Perspect. 2022;130(1):17001.
24. Rocklöv J, Forsberg B. The effect of temperature on mortality in Stockholm 1998--2003: a study of lag structures and heatwave effects. Scand J Public Health. 2008;36(5):516-23.
25. Lian T, Fu Y, Sun M, et al. Effect of temperature on accidental human mortality: a time-series analysis in Shenzhen, Guangdong Province in China. Sci Rep. 2020;10(1):8410
26. Yang J, Ou CQ, Ding Y, et al. Daily temperature and mortality: a study of distributed lag non-linear effect and effect modification in Guangzhou. Environ Health. 2012;11:63.
27. Curriero FC, Heiner KS, Samet JM, et al. Temperature and mortality in 11 cities of the Eastern United States. Am J Epidemiol 2002;155(1):80-7.
Emergency Department Management of Acute Heatstroke: A Retrospective Analysis from Phoenix, Arizona
Jeffrey R. Stowell, MD*†‡
Paul Pugsley, MD*†‡
Megan McElhinny, MD*†‡
Geoffrey Comp, DO*†‡
Jacquelyn Pearlmutter, DO*‡
Murtaza Akhter, MD*†‡§||
David Sklar, MD*†‡#
Creighton University School of Medicine, Phoenix, Department of Emergency Medicine, Phoenix, Arizona
University of Arizona College of Medicine, Phoenix, Department of Emergency Medicine, Phoenix, Arizona
Valleywise Health, Department of Emergency Medicine, Phoenix, Arizona
Penn State Health Milton S. Hershey Medical Center, Department of Emergency Medicine, Hershey, Pennsylvania
HCA Healthcare, Department of Emergency Medicine, Miami, Florida
Arizona State University, School of Medicine and Advanced Medical Engineering, Tempe, Arizona
Section Editor: Shahram Lotfipour, MD, MPH
Submission history: Submitted January 1, 2025; Revision received June 8, 2025; Accepted June 8, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.42051
Introduction: The global incidence and severity of severe heat illness is on the rise. The increasing number of summer heatwaves in Phoenix, Arizona, gave us a distinctive opportunity to better understand the impact on the clinical presentation and management of acute heatstroke. Our primary objective in this study was to describe the prehospital and emergency department (ED) clinical presentation, treatment, and outcomes of patients with acute heatstroke at a single hospital system during the summers of 2021 and 2022 in Phoenix.
Methods: This was a descriptive, retrospective observational study of heatstroke-associated adult ED presentations occurring from June 1 – August 31, 2021 and June 1 – August 31, 2022, to a single hospital system in Maricopa County.
Results: We identified 60 ED heatstroke encounters. The median environmental daily maximum (Tmax) and minimum (Tmin) were 106.0° Fahrenheit (interquartile range [IQR]) 102.0 - 109.0°F) and 84.0°F (IQR 79.0 - 88.0°F), respectively. The patients were commonly male (42, 70.0%, 95% CI 56.8 - 81.2%), White (26, 43.3%, 95% CI 30.6 - 56.8%), middle-aged (mean 52.7 years, 95% CI 48.4 - 56.9), Medicaid-insured (37, 61.7%, 95% CI 48.2 - 73.9%), and presenting via emergency medical services (60, 100%). Patients were commonly of high acuity (median Emergency Severity Index 1, IQR 1.0 - 2.0), and intubated (45, 75.0%, 95% CI 62.1-85.3%). Forty-seven (78.3%, 95% CI 65.8 - 87.9%) patients were found unresponsive outside with associated substance use (methamphetamines 22, 46.8%, 95% CI 32.161.9%; and fentanyl 14, 29.8%, 95% CI 17.3 - 44.9%). The average patient Tmax at ED presentation was 41.9°C (IQR 41.1 - 42.2). Forty-one patients (68.3%, 95% CI 55.0 - 79.7%) survived to hospital discharge or transfer, of whom 32 (82.1%, 95% CI 66.5 - 92.5%) were neurologically intact.
Conclusion: During the summers of 2021 and 2022, a significant number of heatstroke presentations were treated in a single healthcare system in Maricopa County, Arizona. A substantial number were successfully treated with cold water immersion and discharged neurologically intact. In this urban population, extreme weather exposure and associated substance use appeared to play significant roles. [West J Emerg Med. 2025;26(5)1345–1354.]
INTRODUCTION
Climate change has contributed to an increase in global heatwave frequency and severity, which is predicted to continue for decades to come.1-3 As a result, the global incidence of heat illness is on the rise.3 Severe heat-associated illness, such as heatstroke, is a significant cause of morbidity worldwide. Heatstroke mortality rates approach 50% in its most severe forms and disproportionately impacts the elderly and very young, as well as individuals with comorbidities, economic stress, and social disadvantages.2,4-9 Climate change modeling predicts the number of excess deaths due to heat illness to increase 233% by midcentury.10
In Phoenix, Arizona, the Maricopa County Department of Public Health (MCDPH) recorded an increase in heatstroke deaths from 61 in 2014 to 425 in 2022.11,12 In 2021 and 2022, the city of Phoenix experienced its 10th and 12th hottest years in recorded history, respectively.13 During the 2021 and 2022 summers, record maximum temperatures reached as high as 118°F, with 22 days of temperatures ≥ 110°F (43.3°C) in each of those years.13 Our primary objective in this study was to describe the prehospital and emergency department (ED) presentation of severe heat-associated illness, including the causes, clinical features, therapeutic approaches, and outcomes at a single hospital system during the summers of 2021 and 2022. A description of these patients will help expand our current understanding of the presentation and management of heat-associated illness, assist in developing additional preventative and therapeutic opportunities, and better prepare emergency physicians and public health professionals for the future impact of extreme heat events.
METHODS
Study Design
We conducted a retrospective, observational study of heatassociated, individual adult ED visits over two consecutive summers between June 1–August 31, 2021 and June 1–August 31, 2022, to a single hospital system located in the Phoenix, Arizona, metropolitan area of Maricopa County. The study protocol was approved by the local institutional review board. No author conflicts of interest were identified prior to data collection.
Study Population and Setting
The study was conducted across three EDs in a large, urban, multisite, safety-net healthcare system. The annual combined ED census of the hospital system is ≈ 107,000 total patient encounters. The ED uses a variety of approaches to patient cooling including non-immersion cooling (eg, the application of cold towels, ice packs, fans, etc) and cold water immersion.14 The selection and deployment of cooling therapy is at the discretion of the treating emergency medicine physician.
Located in the Sonoran Desert, Maricopa County has a population of ≈ 4.551 million people living in a catchment area of 9,224 square miles.15 The arid climate is traditionally hottest from May – October with relatively low humidity.11
Population Health Research Capsule
What do we already know about this issue? The incidence and severity of global heatwaves and heat illness are rising. Heatstroke is a significant cause of morbidity with mortality rates approaching 50%.
What was the research question?
We sought to describe the presentation of heatstroke, including the causes, clinical features, therapeutic approaches, and outcomes.
What was the major finding of the study?
68.3% (CI 55.0 - 79.7%) of heatstroke victims survived to hospital discharge, with 82.1% (CI 66.5 - 92.5%) neurologically intact.
How does this improve population health?
A description of how severe heat-associated illness presents to the ED helps expand our understanding of its presentation and management and develop preventative measures.
Annually during 2006 - 2016, the county had a mean of 140 days with daily maximum temperatures of ≥ 90 °F (32 °C) and a mean of 57 days with daily maximum temperatures ≥ 105 °F (40.5 °C).16 The Arizona Emergency Information Network defines “extreme heat” as at least 2-3 days with temperatures above 90 °F.17 In 2022, 424 heat-associated deaths were identified in Maricopa County, 58% of which occurred in July12; this was a 25% increase over 2021. A 2005 heat event in Maricopa County prompted the formation of the City of Phoenix Heat Relief Network.11 Cooling stations in Maricopa County were open and available to the public throughout the study time frame.18
Study Protocol
Adult patients ≥ 18 years of age who presented to the ED with heatstroke from June 1 – August 31, 2021, and June 1 – August 31, 2022, were included in the study. We defined heatstroke as the combination of a temperature of ≥ 40.0 °C and central nervous system dysfunction (eg, altered level of consciousness) during the prehospital or ED course, which was either attributable to or associated with environmental heat exposure 9,19 Heatstroke was further defined as “classic” if due to the inability to avoid or physiologically adjust to heat exposure (eg, elderly or chronically ill persons), or
“exertional” if associated with strenuous physical activity (eg, outdoor labor or activity).19 Encounters that could not be defined as either were classified as “unclassified.” We defined ED cooling as the time from the first ED core temperature recorded to the first temperature of ≤ 39 °C. We excluded from analysis pediatric patients < 18 years of age at the time of ED presentation, and those with presentations that could not be attributed to heatstroke after chart review.
We collected participant demographics, prehospital, ED, and hospitalization course information through chart extraction. We used multiple chart review and retrospective study best practices, including the Strengthening the Reporting of Observational Studies in Epidemiology guidelines, during study design, which included the creation of a standardized abstraction codebook20-23 (Supplemental Table 1). Three of the study investigators—experienced emergeny medicine physicians— extracted study data from the electronic health record (Epic Systems Corporation, Verona, WI). Prior to data collection they were trained per the study protocol, with ongoing education and review as needed. Training included an in-person guided review session with each extractor and supervised extraction of initial data. They used the codebook when extracting data from ED encounters that met study inclusion criteria. Discrepancy or disagreement was adjudicated through cross-abstractor validation.
Study Measurements
Demographics included patient age, gender, race, primary language, financial class, housing status, and primary heat illness diagnosis. The prehospital course included the following: pick-up location (ZIP code); initial non-core temperature; documentation of cardiopulmonary arrest; administration of naloxone and prehospital cooling; airway management; and narrative information regarding the circumstances of the heat exposure. The ED course included ED arrival method (private vehicle vs emergency medical services [EMS]), Emergency Severity Index (ESI) score, maximum core temperature (Tmax), Glasgow Coma Scale (GCS) score, ED intubation, urine drug screen (UDS) results, ethanol level, whether cardiopulmonary arrest occurred in the ED, ED cooling methods, and ED disposition (admit, discharge, death). Hospital course included admission level of care (intensive care unit [ICU], step-down, ward), hospital disposition (discharge or death), and neurologic status at the time of hospital disposition (per physician documentation, return to baseline neurologic status, new disabled, disposition needs, etc).
Investigators also collected publicly available Maricopa County 2021 and 2022 meteorologic, heat surveillance, and heat relief resources. Meteorologic data from June 1 – August 31, 2021, and June 1 – August 31, 2022, included maximum and minimum daily environmental temperatures, and heat advisory dates.24,25 The type of heat relief resources including locations of cooling center was obtained from the Office of Heat Response and Mitigation.26
Study Analysis
This study was designed as a descriptive analysis of ED heatstroke presentations that occurred in the summers of 2021 and 2022. We identified and described presentations of acute heatstroke, including patient demographics, diagnostics, and therapeutic cooling interventions. Confidence intervals for frequencies were calculated using the Aggresti-Couli method (Wald approximation with correction). We made group comparisons using means and the Student t-test for normally distributed data, and medians and Mann-Whitney U testing for non-normally distributed data. Additionally, we described Phoenix, Arizona, meteorologic data using mean, median, interquartile range, and CIs, where appropriate. A graphical representation of heatstroke presentations geolocated to heat relief resources was created using Google Maps (Google LLC, Mountain View, CA). If study participant data were incomplete or unavailable, those encounters were noted in the results as “unknown.” We performed statistical analysis using Microsoft Excel (Microsoft Corp, Redmond, WA) and R v4.0.5 (The R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
From June 1 – August 31, 2021, and June 1 – August 31, 2022, 45,428 total ED encounters occurred at the study site. Of these, we excluded 6,695 patients < 18 years of age at the time of ED presentation. Of the adult encounters, 32,468 were excluded due to a temperature < 40.0 °C. Of those patients with a temperature of ≥ 40.0 °C at the time of ED presentation, 6,199 were excluded because the presentation was unrelated to environmental heat exposure (eg, infection). Of the remaining encounters, we excluded an additional six patient encounters that were determined not to meet the definition of heatstroke as no central nervous system dysfunction was identified during either the prehospital or ED course (eg, heat exhaustion). A total of 60 adult ED encounters from June 1 – August 31, 2021, and June 1 – August 31, 2022, were determined to be due to acute heatstroke (Figure 1).
Heatstroke patients were most commonly male (42, 70.0%, 95% CI 56.8 - 81.2%), White (26, 43.3%, 95% CI 30.6 - 56.8%), middle-aged (mean 52.7 years, 95% CI 48.456.9%), Medicaid-insured (37, 61.7%, 95% CI 48.2 - 73.9%), presenting via EMS (60, 100%), of high acuity (median Emergency Severity Index [ESI] – 1, IQR 1.0 - 2.0), having associated substance use (32, 53.3%, 95% CI 40.0 - 66.3%), and being homeless (22, 36.7%, 95% CI 24.6 - 50.1%). During the study period, the general ED population was 49.6% male, 78.4% White, 44.9% Medicaid-insured, and arrived via EMS in 22.8% of encounters. In the study population, 26 (43.3%, 95% CI 30.6 - 56.8%), and 16 (26.7%, 95% CI 16.1 - 39.7%) patients’ UDS results were positive for methamphetamines and fentanyl, respectively, while 14 (23.3%, 95% CI 13.436.0%) were positive for both. Twenty-three patients (38.3%, 95% CI 26.1 - 51.8%) received naloxone prior to ED arrival; 45 (75.0%, 95% CI 62.1 - 85.3%) were intubated, three (5.0%,
Stowell et al.
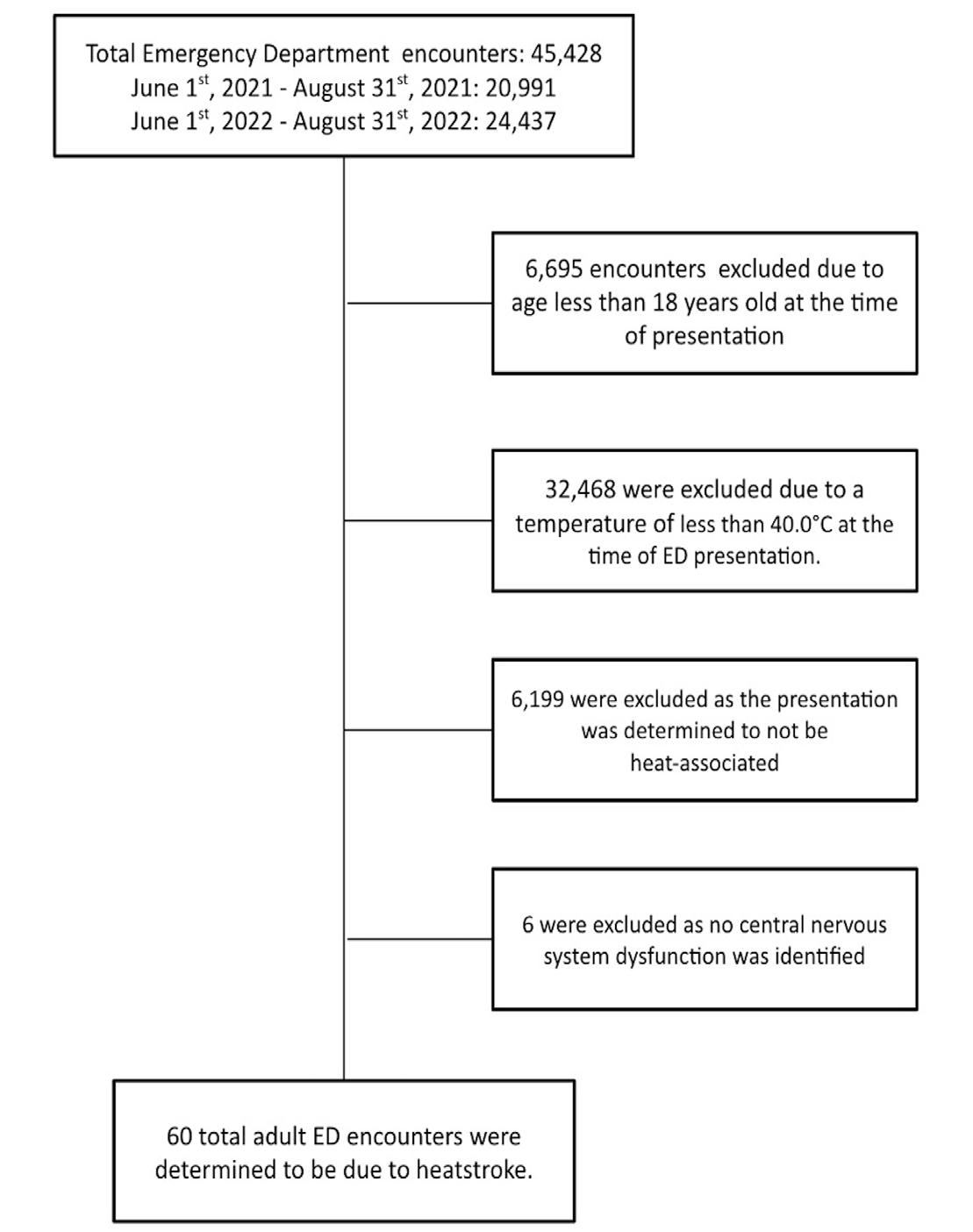
Figure 1. Total number of emergency department encounters and reasons for exclusion from heatstroke study. ED, emergency department
95% CI 1.0 - 13.9%) in the prehospital setting. Nineteen (31.7%, 95% CI 20.3 - 45.0%) of the heatstroke patients did not survive to hospital discharge, with 15 (25.0%, 95% CI 14.7- 37.9%) and four (6.7%, 95% CI 1.8 - 16.2%) dying in the ED and inpatient setting, respectively. Of 14 patients (23.3%, 95% CI 13.4 - 36.0%) who suffered prehospital cardiopulmonary arrest, none were successfully resuscitated in the ED and they contributed to all but one of the ED deaths. Of the 60 patients with heatstroke, 45 survived beyond the ED, with seven (11.7%, 95% CI 4.8 - 22.6%) discharged from the ED and 38 (63.3%, 95% CI 49.9 - 75.4%) admitted to the hospital. Of those admitted, 31 (81.6%, 95% CI 65.7 - 92.3%) were admitted to the ICU. A total of 41of the 60 patients (68.3%, 95% CI 55.0 - 79.7%) survived to hospital discharge or transfer. Of the 39 who were discharged, 32 (82.1%, 95% CI 66.5 - 92.5%) were neurologically intact at the time of discharge. Study participant demographics are in Table 1.
The median patient, prehospital non-core Tmax was 41.1°C (IQR 40.6 - 42.0 °C); core Tmax at ED presentation was 41.9°C (IQR 41.1 - 42.2) and post-cooling minimum temperature (Tmin) was 37.0°C (IQR 35.9 - 37.7°C). Thirty-six (60.0%, 95% CI 46.5 - 72.4%) patients had
Gender Male
Demographics
Adult heatstroke ED encounters (N = 60) (%, 95% CI)
-
Age
Years (mean) 52.7 (48.4 - 56.9)
Race
Indian or Alaska
Type of Insurance
(8.3%,
Domicile
ED, emergency department; IQR, interquartile range
documentation of EMS-initiated prehospital cooling interventions. Prehospital cooling techniques included the use of or combination of cold intravenous fluids (22 patients), placement of ice packs (16), placement of wet towels (3), cold blanket (1), and other “unspecified” cooling measures (11). The ED cooling techniques included cold water immersion in 38 (63.3%, 95% CI 49.9 - 75.4%), nonimmersion cooling (eg, cold towels, ice packs, fans, etc) in 13 (21.7%, 95% CI 12.1 - 34.2%), and no cooling in 9 (15.0%, 95% CI 7.1 - 26.6%) of the heatstroke patients. Patients treated with cold water immersion therapy demonstrated an overall higher acuity with higher median ESI (1.0 IQR 1.0-2.0 vs. 2.0 IQR 1.0 - 2.0), median Tmax (42.0°C,
Table 1. Demographics of patients who suffered heatstroke during the summers of 2021 and 2022.
95% CI 41.3 - 42.3°C vs. 40.7°C, 95% CI 40.2 - 41.6°C), intubation rate (78.9%, 95% CI 62.7 - 90.5% vs 68.2%, 95% CI 45.1 - 86.1%), rate of prehospital cardiac arrest (15.8%, 95% CI 6.0 - 31.3% vs. 7.7%, 95% CI 0.2 - 36.0%), and lower median Glascow Come Scale (3 (IQR 3.0 - 6.0) vs. 11 (IQR 7.0-13.0)) as compared to non-immersion cooling. In patients where the duration of cooling was documented, the median temperature reduction, duration, and rate of cooling was 3.06°C (95% CI 2.4 - 3.6°C), 35.0 minutes (IQR 26.356.3), and 0.08°C per minute (95% CI 0.05 - 0.12 °C) for cold water immersion therapy (34, 89.5% immersion encounters with documentation), and 2.65°C (95% CI 2.18 - 3.10 °C), 60.5 minutes (IQR 37.5 - 87.3), and 0.04 °C per minute (95% CI 0.03-0.06°C) for non-immersion (12, 92.4%). Cold Water Immersion study participant demographics and outcomes presented in Table 2.
The overall mortality rates were 28.9% (95% CI 15.445.9%) for cold water immersion cooling and 7.7% (95% CI 0.2 - 36.0%) for non-immersion cooling. The “no-cooling” patients demonstrated the highest overall prehospital acuity. Seven of the nine no-cooling patients presented to the ED in cardiopulmonary arrest, likely contributing to the decision to pursue immediate Advanced Cardiac Life Support (ACLS) measures rather than initiation of ED cooling.
Only nine (15.0%, 95% CI 7.1 - 26.6%) of the heatstroke presentations were attributable to a “classic” cause of heat exposure. Forty-seven (78.3%, 95% CI 65.8 - 87.9%) patients were found down outside and were difficult to classify distinctively as either classic or exertional heatstroke. These encounters were classified as “unclassified” causes of heatstroke Further, four (6.7%, 95% CI 1.8 - 16.2%) patients expired without sufficient clinical context to determine the cause of the heat exposure. The “classic” heatstroke encounters were 44.4% male (95% CI 13.7 - 78.8%), median 62.0 years old (IQR 56.0-72.0), 100% domiciled (95% CI 66.4 - 100.0%), 55.6% intubated (95% CI 21.2 - 86.3%), and 88.9% (95% CI 51.8-99.7%) survived to hospital discharge or transfer. Two (22.2%, 95% CI 2.8 - 60.0%) of these presentations had associated methamphetamine use. The “unclassified” heatstroke presentations were predominately male (36, 76.6%, 95% CI 62.0 - 87.7%), younger (49.8 years old, 95% CI 45.3 - 54.3), homeless (22, 46.8%, 95% CI 32.1 - 61.9%), and associated with substance use (methamphetamines 22, 46.8%, 95% CI 32.1 - 61.9%, and fentanyl 14, 29.8%, 95% CI 17.3 - 44.9%). A description of the 47 “unclassified” heatstroke presentations is available in Table 3.
The median environmental daily Tmax and Tmin during the study window was 106.0°F (102.0 - 109.0 °F IQR) and 84.0°F (79.0 - 88.0°F IQR), respectively. Figure 2 demonstrates the daily heatstroke survivors, deaths, and environmental Tmax and Tmin. Thirty-one (51.7%, 95% CI 38.4 - 64.8%) of the heatstroke presentations occurred in July, including seven (36.8%, 95% CI 16.3 - 61.6%) of the total study population deaths. The median July Tmax and Tmin were 106.5 °F (95% CI 102.3 - 111.0 °F) and 85.0°F (95% CI
Demographics
Cold water immersion encounters (N = 38) (%, 95% CI)
Age (Years, Mean) 50.2 (45.1-55.4)
Emergency Severity Index (Median, Interquartile Range) 1 (IQR 1.0-2.0)
Glasgow Coma Scale (Median, Interquartile Range) 3 (IQR 3.0-6.0)
Prehospital cooling 24 (63.2%, 46.0-78.2%)
Prehospital cardiopulmonary arrest 6 (15.8%, 6.0-31.3%)
Emergency department maximum temperature (median Fahrenheit) 42.0°F (41.3-42.3°F)
Prehospital intubation 2 (5.3%, 0.6-17.7%)
Emergency department intubation 28 (73.7%, 56.9-86.6%)
Outcome
Death 11 (28.9%, 15.4-45.9%)
Discharge neurologically intact 20 (52.6%, 35.8-69.0%)
Discharge with neurological deficit 6 (15.8%, 6.0-31.3%)
Unknown disposition 1 (2.6%, 0.06-13.8%)
IQR, interquartile range
80.3 - 89.0 °F), respectively. Heatstroke deaths represented 13.0% of all-cause ED deaths in July. In 2021 and 2022 there were 29 heat advisory dates. Nine (47.4%, 95% CI 24.571.1%) of the total heatstroke deaths occurred during heat advisory dates.
Heatstroke patients presented from 20 unique ZIP codes. Of these, 18 are in Phoenix and one each in the geographically adjacent cities of Glendale and Peoria. There were 23 and 31 publicly available cooling centers in the patient presentation ZIP codes in 2021 and 2022, respectively. The prehospital patient location and geographically available cooling resources are described by ZIP code in Figure 3.
DISCUSSION
As a result of increasing environmental heat and exposure, the incidence and severity of heat illness and heatstroke are on the rise.12,27 In this study, a total of 60 presentations of heatstroke were identified at a single center from June 1–August 31, 2021, and June 1–August 31, 2022, in Phoenix, Arizona, with as many as four acute presentations and two deaths in a single day. In this
Stowell et al.
Table 2. Demographics and outcomes of patients who underwent cold water immersion cooling therapy.
Table 3. Characteristics of patients with “unclassified” heat stroke.
Demographics
Gender
Male
Female
Unknown
"Unclassified" heatstroke encounters (N = 47) (%, 95% CI)
36 (76.6%, 62.0 - 87.7%)
8 (17.0%, 7.6- 30.8%)
3 (6.4%, 1.3 - 17.5%)
Age (Mean, Years) 58.3 (50.9 - 65.7)
Housing
Domiciled
Homeless
12 (25.5%, 13.9 - 40.3%)
22 (46.8%, 32.1 - 61.9%)
Unknown 13 (27.7%, 15.6 - 42.6%)
Temperature maximum (Median, Fahrenheit) 42.0°F (41.3 - 42.3)
Emergency department intubation 34 (72.3%, 57.4 - 84.4%)
Drug screen
Methamphetamine 22 (46.8%, 32.1 - 61.9%)
Fentanyl 14 (29.8%, 17.3 - 44.9%)
Alcohol 4 (8.5%, 2.4 - 20.4%)
"Other"
Negative
Not obtained
Prehospital naloxone
Emergency department cooling method
16 (34.0%, 20.9 - 49.3%)
2 (4.3%, 0.52 - 14.5%)
18 (38.3%, 24.5 - 53.6%)
20 (42.6%, 28.3 - 57.8%)
Cold water immersion 32 (68.1%, 52.9 - 80.9%)
Non-immersion cooling 9 (19.1%, 9.1 - 33.3%)
No cooling 6 (12.8%, 4.8 - 25.7%)
Outcome
Death 15 (31.9%, 19.1 - 47.1%)
Discharge neurologically intact 26 (55.3%, 40.1 - 69.8%)
Discharge with neurological deficit 5 (10.6%. 3.5 - 23.1%)
Unknown disposition 1 (2.1%, 0.05 - 11.3%)
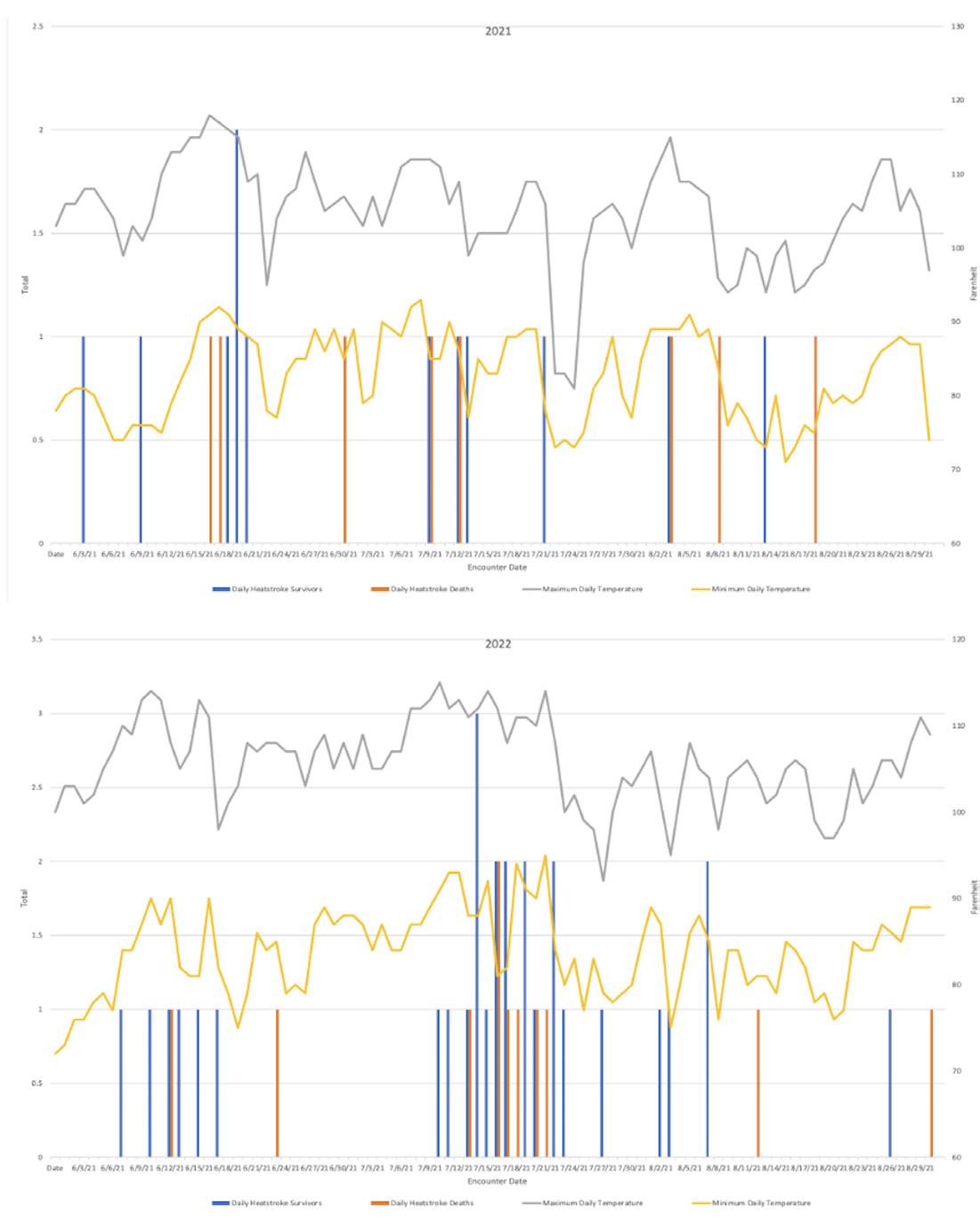
2. 2021 and 2022 heatstroke and heat-related death as compared to environmental temperatures.
of heat illness in the study population was significant with 85.3% requiring airway management, a 63.3% hospital admission rate, 81.6% of whom were admitted to the ICU, and 63.3% underwent cold water immersion. However, a substantial portion of the patients (68.3%) were ultimately discharged or transferred, 82.1% of whom were neurologically intact at the time.
population, heatstroke disproportionately impacted males (70.0%), persons experiencing homelessness (36.7%), and those with substance use disorder (53.3%). These results align with the 2022 MCDPH heat death report, which noted 424 heat-associated deaths, of which 81% of patients were male, 41.9% were experiencing homelessness, and 67% had associated substance use disorder.12 The acuity and severity
As compared to prior literature, a significant portion of the heatstroke presentations in this study population did not adhere to the classical or exertional models.19 The “classic” heatstroke presentation commonly affects those with preexisting health or socioeconomic conditions that result in the inability to appropriately avoid heat exposure.19,28,29 Alternatively, in the “exertional” presentation, patients are typically younger and exerting themselves beyond their ability to sufficiently dissipate heat.19 In this study, only nine (15.0%) presentations were clearly attributable to a classic cause of heatstroke. Most of the study population (47, 78.3%) presented after being found unresponsive in an outdoor urban environment, directly exposed to extreme heat. In this group, substance use disorder and homelessness appeared to play a significant role in their heat exposure and resultant illness. As compared to the remainder of the study cohort,
Figure
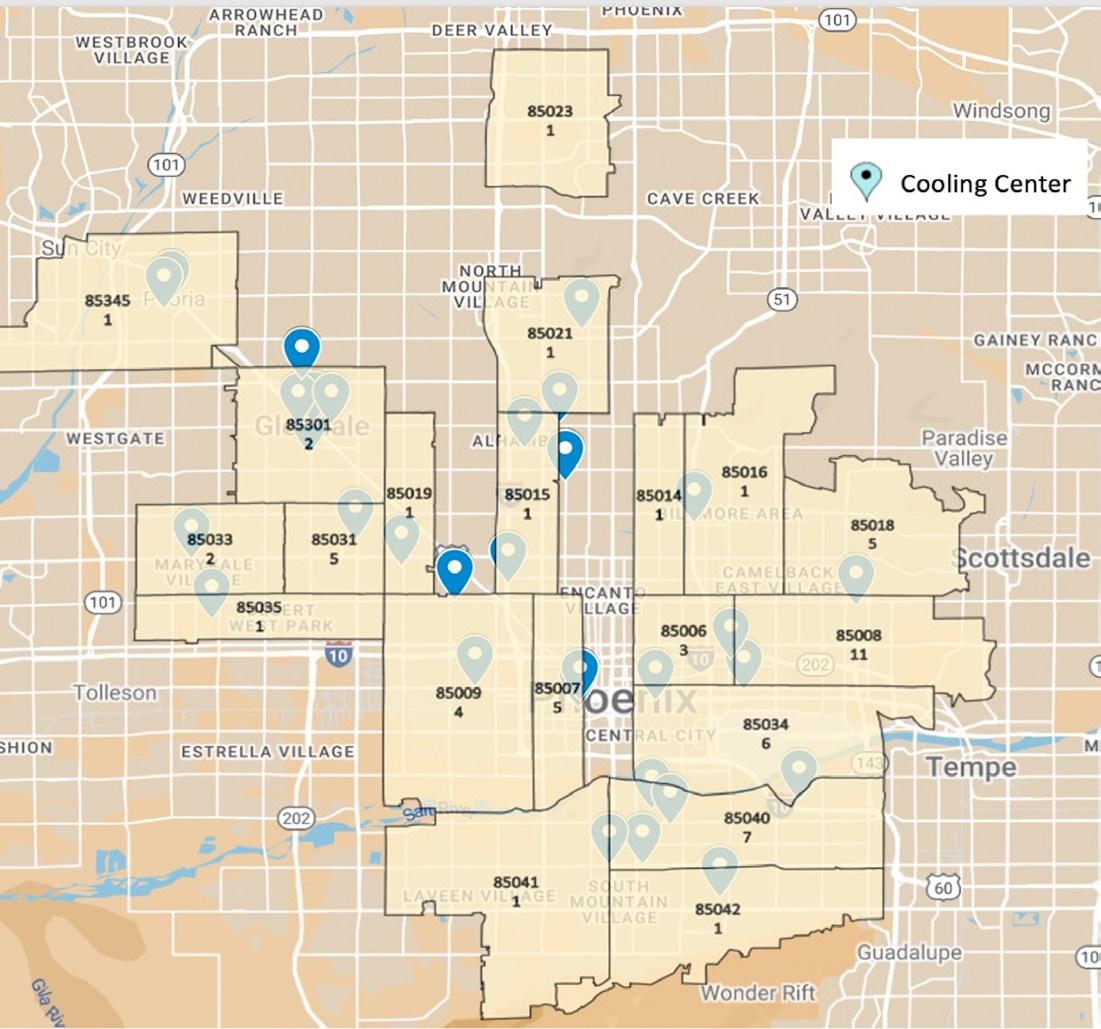
this novel group was largely male (76.6%), experiencing homelessness (46.8%), and associated with substance use (methamphetamines 46.8%, fentanyl 29.8%) in those who were tested, which potentially underestimates the absolute prevalence in this population.
Prior literature has demonstrated an increased mortality in heat-exposed patients with concomitant substance use, particularly stimulants.30-34 Substance use likely contributes to the patient’s inability to appropriately avoid or dissipate heat, resulting in a heat-associated toxidrome, or heat poisoning. In the study population, the risk of heatstroke presentation and death was most specifically associated with methamphetamine and fentanyl use, potentially limiting the patient’s access to cooling resources, inhibiting the patient’s ability to respond to the normal biological heat-avoidance triggers, and prolonging heat exposure. The 2022 MCDPH statistics similarly identified the association of substance use in 67% of all heat deaths, including methamphetamines and fentanyl in 93% and 44.4% of patients, respectively.12 This novel trend poses unique challenges to the prevention and treatment of heat illness due to the combination of extreme weather exposure and substance use. In a 2014 study of Arizona cooling centers, the most frequent reasons for turning people away were safety concerns due to individual behaviors (56%) and intoxication (32%).35 The unique role that substance use plays in exacerbating heatstroke presentations in Phoenix, and likely beyond, cannot be underestimated and is deserving of further study to identify additional heat exposure prevention strategies in this population.
The treatment of heat illness in the prehospital and ED settings is logistically challenging. Cooling strategies are
designed to induce rapid heat dissipation; these include the application of cold IV fluids and ice packs, evaporative cooling with fans, and cold water immersion.1,19 In the study population, 60.0% of the patients had documentation of prehospital-initiated cooling interventions. In the ED, cooling either continued or was initiated in 85% of encounters, with most undergoing cold water immersion (63.3%). While the overall non-immersion mortality rate was lower, cold water immersion was more commonly used in patients with a higher acuity (ESI 1 vs 2), intubation rate (78.9% vs 68.2%), rate of prehospital cardiac arrest (15.8% vs 7.7%), and core temperatures (median Tmax 42.0°C vs 40.7°C), which likely contributed to the higher mortality in this group. Despite this, cold water immersion therapy demonstrated a faster cooling rate (0.08°C per minute vs 0.04°C per minute) and shorter duration (median 35.0 minutes vs 60.5 minutes), cooling patients nearly twice as quickly as non-immersion therapy.5,36,37
Prehospital and ED cold water immersion therapy is often difficult to implement due to limited space, resources, and training.14 This is further complicated in patients presenting in cardiopulmonary arrest. In this study population, no heatstroke patients who presented to the ED in cardiopulmonary arrest survived to hospital admission. Of these patients 77.8% received no cooling interventions, potentially due to the challenging integration of cardiopulmonary resuscitation (CPR) with cooling interventions. However, prior studies have demonstrated simultaneous cold water immersion and ACLS, including CPR and defibrillation, to be safe and effective.38 The development of prehospital and ED cold water immersion therapy strategies, including the necessary resource allocation and training, which take into account cardiopulmonary arrest and the need for ACLS management, can potentially expedite cooling and improve outcomes in heatstroke patients with prehospital cardiopulmonary arrest, although they are challenging to implement.38,39
While the association between extreme environmental temperatures and the incidence of heatstroke and death is clear, a further understanding of the most relevant and predictable local weather metrics may help guide prevention strategies.40,41 In this study population, 36.8% of the patient deaths occurred in July, marked by the highest daily Tmax and Tmin. Similarly, in 2022 the MCDPH reported 58% of all heat deaths occurred in July and 25.2% occurred on days with an excessive heat warning.12 Predictive weather modeling is specific to the local climate. Warning systems use a variety of weather and heat metrics, such as daily mean, minimum, or maximum temperature, or composite indices of temperature and humidity, such as the heat index, to guide heat illness prevention strategies.17,34 Prior studies have also shown that heat-induced clinical presentations may counterintuitively begin to occur at moderate temperatures, below traditional advisory triggers.8,40 Heat advisory warning metrics and triggers may be challenging to standardize for both research and public health initiatives but should be adapted to local climates.8,42
Figure 3. Heatstroke presentations and available cooling centers by Phoenix metropolitan-area ZIP code.
A substantial portion of the study population was found to be undomiciled in an urban environment at the time of presentation. Similarly, Maricopa County heat death patients in 2022 were predominantly from outdoor and urban exposures (80%) and experiencing homelessness (41.9%).12 Prior literature has identified the highest heat mortality rates (0.3 per 100,000 population) in urban and metropolitan settings.8,12 Urban areas create “heat islands” due to the increased structural and impervious surface density, resulting in hotter daytime temperatures and limiting heat dissipation at night.43 The distribution and delivery of heat illness treatment and prevention resources to an urban and unhoused population can be challenging.32,44,45 “Heat vulnerability” maps, focused on urban areas and heat islands, may help predict areas at high risk for heat illness presentations, and guide the deployment of public health cooling resources.46
In this study population, the incidence and acuity of heatstroke presentation to a single urban system were significant and consistent with 2022 MCDPH data, which demonstrated 424 heatstroke deaths, a 25% increase in heat illness-associated deaths from 2021.12 For comparison, there were 660 motor vehicle deaths in Maricopa County in 2022.47 However, with timely cooling interventions, a substantial portion of the study patients were successfully discharged neurologically intact. These results demonstrate and support the need for significant and ongoing resource allocation to heat illness prevention and treatment. Additional investigation of this novel heatstroke presentation, including the associated risk of extreme weather, substance use, and outdoor and urban setting exposures is needed. Strategies should address the challenge of connecting public health and cooling resources to this high-risk patient population. Furthermore, the partnership of prehospital, public health, and emergency care systems is needed to optimize the prevention, early detection, and rapid treatment of heat illness.
LIMITATIONS
During the development and implementation of this study several potential limitations were identified. The study population presented via EMS transport and represented a specific geographical sample of the Phoenix heatstroke cohort for the catchment area of the hospital system. The generalizability of the study population may be limited in less arid or rural settings. While this may not fully describe the entirety of the Phoenix metropolitan area, we do believe it is representative of a significant and important cohort of heatstroke presentations and is consistent with concurrent local public health reports.12
Additionally, certain patient demographic characteristics could not be fully obtained through retrospective chart extraction at the time of study development and analysis, limiting the ability to describe a selection of study patients in this analysis fully. These patients were included in the analysis as “unknown” where appropriate but may have led
to underestimating certain study findings. Similarly, drug use or intoxication was defined by a positive urinary drug screen alone, but clinical features of intoxication could be consistently obtained through chart review.
Finally, the sample size was too small to be able to control for potential confounders; however, to our knowledge, this is the largest dataset of ED heatstroke patients reported. Future prospective and comprehensive studies in disparate climates and populations are warranted to better understand environmental and heat illness in this and dissimilar populations.
CONCLUSION
In a single-center study of an urban population during the summers of 2021 and 2022, a significant number of heatstroke presentations and heat-related deaths were identified in Phoenix, Arizona. In this population, the extreme weather and association of substance use appeared to play a major role in precipitating heatstroke risk. However, a substantial portion of patients were successfully treated, often through cold water immersion, and discharged neurologically intact. Future studies evaluating the combined roles of public health, prehospital, and emergency care are necessary for the prevention and treatment of this environmentally mediated public health emergency.
Address for Correspondence: Jeffrey R. Stowell, MD, Valleywise Health, Department of Emergency Medicine, 2601 E. Roosevelt St, Phoenix, AZ 85008. Email: Jeffrey_Stowell@dmgaz.org.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Stowell et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Sorensen C, Hess J. Treatment and Prevention of Heat-Related Illness. N Engl J Med. 2022;387(15):1404-1413.
2. Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021;398(10311):1619-1662
3. Diffenbaugh NS, Scherer M. Observational and model evidence of global emergence of permanent, unprecedented heat in the 20(th) and 21(st) centuries. Clim Change. 2011;107(3-4):615-624.
4. Rublee C, Dresser C, Giudice C, et al. Evidence-Based Heatstroke
Management in the Emergency Department. West J Emerg Med. 2021;22(2):186-195
5. Lipman GS, Gaudio FG, Eifling KP, et al. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Heat Illness: 2019 Update. Wilderness Environ Med. 2019;30(4S):S33-S46
6. Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397(10269):129-170.
7. Vicedo-Cabrera AM, Scovronick N, Sera F, et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat Clim Chang. 2021;11(6):492-500.
8. Vaidyanathan A, Saha S, Vicedo-Cabrera AM, et al. Assessment of extreme heat and hospitalizations to inform early warning systems. Proc Natl Acad Sci U S A. 2019;116(12):5420-5427.
9. Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978-1988.
10. Khatana SAM, Eberly LA, Nathan AS, et al. Projected Change in the Burden of Excess Cardiovascular Deaths Associated With Extreme Heat by Midcentury (2036-2065) in the Contiguous United States. Circulation. 2023;148(20):1559-1569.
11. Iverson SA, Gettel A, Bezold CP, et al. Heat-associated mortality in a hot climate: Maricopa County, Arizona, 2006-2016. Public Health Rep. 2020;135(5):631-639.
12. Maricopa County Department of Public Health Division of Epidemiology and Informatics. 2022 Heat Deaths Report. 2023. Available at: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/ https://www.maricopa.gov/ArchiveCenter/ViewFile/Item/565. Accessed April 21, 2024.
13. National Weather Service. 2021 Climate Year in Review for Phoenix, Yuma, and El Centro. 2021. Available at: https://www.weather.gov/ psr/yearinreview2021. Accessed January 12, 2025.
14. Feinstein BA, Kelley J, Blackburn P, et al. In reply. Ann Emerg Med. 2023;82(2):238-239.
15. U.S. Department of Commerce. The United States Census 2019. 2019. Available at: https://www.census.gov/programs-surveys/acs/ news/updates/2019.html. Accessed July 18, 2022.
16. The United States Census Bureau. Maricopa County. Available at: https://www.census.gov/search-results.html?q=maricopa+cou nty&page=1&stateGeo=none&searchtype=web&cssp=SERP&_ charset_=UTF-8. Accessed Febuary 9, 2024.
17. Arizona Office of the Governor. Arizona’s Extreme Heat Preparedness. Available at: chrome-extension:// efaidnbmnnnibpcajpcglclefindmkaj/https://mcusercontent. com/44a5186aac69c13c570fca36a/files/ada1d47f-83f5-4189-d8351eec1552aeea/2024.03.01_Extreme_Heat_Prepardeness_Plan.pdf Accessed April 21, 2024.
18. Maricopa County Department of Public Health. Weekly Heat Report. 2023. Available at: https://www.maricopa.gov/1858/Heat-Surveillance Accessed April 21, 2024.
19. Epstein Y, Yanovich R. Heatstroke. N Engl J Med. 2019;380(25):2449-2459.
20. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31-S34.
21. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-451.
22. Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996;27(3):305-308.
23. Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64(3):292-298.
24. National Weather Service. NWS Phoenix Heat Page. Available at: https://www.weather.gov/psr/heat. Accessed Febuary 9, 2024.
25. U.S. Department of Commerce. National Oceanic and Atmospheric Administration.Available at: https://www.noaa.gov/. Accessed Febuary 9, 2024.
26. City of Phoenix. Summer Heat Safety. Available at: https://www. phoenix.gov/heat/resources/heatsafety. Accessed Febuary 9, 2024.
27. Maricopa County Department of Public Health Division of Epidemiology and Informatics. 2023 Heat Related Deaths Report. Phoenix, Arizona; 2024. Available at: chrome-extension:// efaidnbmnnnibpcajpcglclefindmkaj/https://www.maricopa.gov/ ArchiveCenter/ViewFile/Item/5820. Accessed April 21, 2024.
28. Wondmagegn BY, Xiang J, Williams S, et al. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci Total Environ. 2019;657:608-618.
29. Kenny GP, Yardley J, Brown C, et al. Heat stress in older individuals and patients with common chronic diseases. CMAJ 2010;182(10):1053-1060.
30. Page LA, Hajat S, Kovats RS, et al. Temperature-related deaths in people with psychosis, dementia and substance misuse. Br J Psychiatry. 2012;200(6):485-490.
31. Cusack L, de Crespigny C, Athanasos P, et al. Heatwaves and their impact on people with alcohol, drug and mental health conditions: a discussion paper on clinical practice considerations. Morb Mortal Wkly Rep. 1998;279(22):1795-1800.
32. Marzuk PM, Tardiff K, Leon AC, et al. Ambient temperature and mortality from unintentional cocaine overdose. JAMA 1998;279(22):1795-1800.
33. Hall C, Ha S, Yen IH, et al. Risk factors for hyperthermia mortality among emergency department patients. Ann Epidemiol. 2021;64(209):90-95.
34. Petkova EP, Morita H, Kinney PL. Health impacts of heat in a changing climate: How can emerging science inform urban adaptation planning? Curr Epidemiol Rep. 2014;1(2):67-74.
35. Berisha V, Hondula D, Roach M, et al. Assessing adaptation strategies for extreme heat: a public health evaluation of cooling centers in Maricopa County, Arizona. Weather Clim Soc. 2017;9(1):71-80.
36. Armstrong LE, Crago AE, Adams R, et al. Whole-body cooling of hyperthermic runners: comparison of two field therapies. Am J Emerg
ED Management of Heatstroke Stowell et al. Med. 1996;14(4):355-358.
37. Comp G, Pugsley P, Sklar D, et al. Heat stroke management updates: a description of the development of a novel in-emergency department cold-water immersion protocol and guide for implementation. Ann Emerg Med. 2024:1-10.
38. Feinstein B, Kelley J, Blackburn P, et al. Synchronized cardioversion performed during cold water immersion of a heatstroke patient. Ann Emerg Med. 2023;81(1):70-72.
39. Jacobsen RC, Beaver B, Abo B. Out-of-hospital cold water immersion for classic (non-exertional) heat stroke guided by real-time core temperature monitoring: a case series. Prehosp Emerg Care. 2023;27(6):832-837.
40. Gasparrini A, Guo Y, Hashizume M. Mortalité attribuable au froid et à la chaleur: analyse multi-pays. Environ Risques Sante. 2015;14(6):464-465.
41. Lowe D, Ebi KL, Forsberg B. Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. Int J Environ Res Public Health. 2011;8(12):4623-4648.
42. Putnam H, Hondula DM, Urban A, et al. It’s not the heat, it’s the
vulnerability: attribution of the 2016 spike in heat-associated deaths in Maricopa County, Arizona. Environ Res Lett. 2018;13(9).
43. Saverino KC, Routman E, Lookingbill TR, et al. Thermal inequity in Richmond, VA: The effect of an unjust evolution of the urban landscape on urban heat islands. Sustainability. 2021;13(3):1-18.
44. Morano LH, Watkins S. Evaluation of diagnostic codes in morbidity and mortality data sources for heat-related illness surveillance. Public Health Rep. 2017;132(3):326-335.
45. Goodin K, Castle M, Martinez J, et al. Community Assessment for Public Health Emergency Response (CASPER) Heat Vulnerability and Emergency Preparedness Needs Assessment Maricopa County, Arizona. 2015;(March):1-35.
46. Kravchenko J, Abernethy AP, Fawzy M, et al. Minimization of heatwave morbidity and mortality. Am J Prev Med. 2013;44(3):274-282.
47. Centers for Disease Control and Prevention (CDC). Motor Vehicle Crash Facts. Natl Inst Occup Saf Heal (NIOSH), Centers Dis Control Prev. 2021. Available at: https://www.cdc.gov/niosh/centers/motorvehicle.html?CDC_AAref_Val=https://www.cdc.gov/niosh/motorvehicle/ resources/crashdata/facts.html. Accessed April 21, 2024.
Report on the El Paso Mass Casualty Incident Hospital Response: Enhancing Surge Capacity
Susan F. McLean, MD, MPH*
Nancy Weber, DO†
Adam Adler, MD‡
Alejandro Rios Tovar, MD§
Stephen Flaherty, MD**
Alan H. Tyroch, MD*
Section Editor: Pierre Borczuk, MD
* † ‡ § **
Texas Tech University Health Sciences Center El Paso, Department of Surgery, El Paso, Texas
Texas Tech University Health Sciences Center El Paso, Department of Emergency Medicine, El Paso, Texas
Texas Tech University Health Sciences Center El Paso, Department of Orthopedic Surgery, El Paso, Texas
University of Texas Health Rio Grande Valley, Department of Surgery, Edinburg, Texas
Del Sol Medical Center, Department of Trauma and Surgical Critical Care, El Paso, Texas
Submission history: Submitted June 27, 2024; Revision received May 12, 2025; Accepted May 15, 2025
Electronically published August 29, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.24991
Introduction: On August 3, 2019, a mass casualty incident (MCI)/active shooter event in El Paso, TX, left 21 people dead on scene and 27 transported. Our main objective in this article was to describe trauma center responses to a sudden patient influx after a MCI/active shooter event. We hypothesized that a triage practice in which two physicians providing care while simultaneously triaging would be equivalent to triage with a single physician providing triage only. The secondary objective was to describe patient injuries and treatment. Our third objective was to describe how a large, multidisciplinary team of hospital personnel were rapidly notified and arrived at the trauma center. Finally, we describe how the problems identified in a review of hospital response led to better results after implementing new practices in a 2023 MCI/active shooter event.
Methods: We conducted a retrospective cohort/medical record review and departmental survey. We performed the Fisher exact test using survival as an outcome to compare the two centers’ triage methods.
Results: A total of 15 patients arrived at the University Medical Center of El Paso, 14 of them within 35 minutes and one in a later transfer; 14 survived at 24 hours. Total patients included 10 females and 5 males, mean age 40.6 (1-88) years. Mean hospital length of stay (LOS) was 13 ± 16.4 days. For the six intensive care unit (ICU) patients the mean LOS was 5.7 (1-11) days. In comparing day 1 survival between the center where a surgeon and an emergency physician triaged patients while also providing care and the center where a sole triage physician was on duty, survival rates were equivalent (P = .56). Six surgeries occurred on day 1 with four laparotomies performed within 43 minutes. The trauma team expanded rapidly as 132 persons from 16 departments, notified by phone calls and text, arrived, improving communication and patient registration in two 2023 MCI responses.
Conclusion: The survival rate of victims of a mass casualty incident brought to a Level I trauma center and triaged by a surgeon and an emergency physician who simultaneously provided care did not differ significantly from the survival rate at a Level II trauma center with a single triage physician on duty. The rapid arrival of multiple specialists resulted in 14 patients treated within an hour. [West J Emerg Med. 2025;26(5)1355–1366.]
INTRODUCTION
On August 3, 2019, at 10:39 am, an active shooter instigated a mass casualty incident (MCI) in El Paso, Texas. This shooting left 22 people dead in the first 24 hours and sent
27 to local hospitals immediately.1 This event was the second of three active shooter events in the United States that week.2 The incidence of MCI active shooter events, defined as a wounding event with > 3 casualties,3 increased throughout the
early 2000s: >160 MCIs have occurred since 2000 with over 1,000 casualties.3 According to a Department of Justice report written in a collaboration with the Federal Bureau of Investigation and Texas State University, MCI/active shooter frequency has increased from one incident recorded in 2000 to an average of 16.4/year in the US.3 Thus, trauma centers continue to evolve their responses to these events. Hospital response is frequently reported per specialty.4-6 In-hospital response from triage to operating room (OR) is especially important.7-9 Most reviews focus on triage and surgical and emergency department (ED) response,5 with others delineating specialty response.10 Analysis of a hospital response in a Level 1 trauma center could assist planning for future MCI/active shooter events.
Our objective in this review was to characterize the in-hospital response of a Level I trauma center— University Medical Center (UMC) of El Paso—to a MCI/active shooter event. We hypothesized that using a triage system in which two triage physicians simultaneously treated patients would have a survival rate similar to that in a triage system in which there was a sole, designated triage physician who did not also provide care. Our secondary objective was to characterize patient injuries and treatments. We also sought to characterize the rapid influx of hospital staff and the methods used to notify them that the MCI was occurring. Finally, we describe the problems identified in reviewing the hospital response to the MCI and new practices implemented in a MCI/active shooter event four years later in 2023, and in a citywide mock MCI that same year, which resulted in improvements in responses.
METHODS
Our institution’s Investigational Review Board for Human Subjects Research approved this study. We conducted a retrospective cohort medical record review of only those patients arriving at the trauma center who had sustained wounds in the MCI/active shooter event; we also analyzed the performance of the Hospital Incident Command System (HICS). We used the Federal Bureau of Investigation definition of MCI/active shooter: an incident in which at least three persons are killed during a shooting event 3 Data sources were medical records and HICS data from the HICS incident commander at the Level I trauma center, who was also the trauma program manager. We also obtained data from three other hospitals: a Level II trauma center, Del Sol Medical Center, and two Level III trauma centers. Data was emailed to us by the trauma medical director at the Level II center and by the trauma program managers at the two Level III trauma centers. We obtained additional data on numbers of patients and overall survival rate at the Level II center.
We obtained data from the Level I trauma center in two ways: via survey and by medical record review. We surveyed department heads regarding how personnel were notified and the number who arrived at the hospital. This information was used to inform the section on expansion of the trauma team
Population Health Research Capsule
What do we already know about this issue? The number of mass casualty incidents (MCI)/active shooters has increased in the past 20 years in the US.
What was the research question?
Is a triage practice in which two physicians triage patients while simultaneously providing care equivalent to a single physician providing triage?
What was the major finding of the study? The two triage practices had equivalent survival rates (P = .56).
How does this improve population health? This comparison of triage practices and a summary of institutional response to a MCI may be helpful to hospital disaster planning committees.
and personnel deployment. Clinical data was obtained from medical records of patients identified to have a gunshot wound in the MCI/active shooter event. A separate team was created in medical records for patients injured in the event. We obtained all information regarding time to OR, and types of injuries, operations, and procedures from the medical records. We calculated surgical timing from ED arrival times and OR perioperative nursing documentation. Time to OR was calculated as arrival time to surgery start time. We obtained information regarding hospital administrative response from an after-report from the MCI/active shooter event, and an after-report from a mock MCI four years later. Two authors also were present during the subsequent MCI/active shooter event in February 2023 and recorded information concurrent with the incident. Data regarding total numbers of patients in the August 2019 MCI were obtained from the HICS commander. Information about the total numbers of patients in the 2023 MCI/active shooter event were obtained from news reports and the HICS commander. We were only able to access Injury Severity Score (ISS) data from the Level I trauma center. The Fisher exact test was used for categorical variable comparison (survival statistics).
The results of improvements made to the system after 2019 are reported in two incidents: the first in a February 15, 2023, MCI/active shooter event at a local shopping mall, and the second at a citywide, mock MCI drill in October 2023. We obtained this information through direct observation and via
news reports.11 The news reports were used to verify dates and numbers of victims at the scene. We obtained data regarding the citywide mock MCI from a report at the Level I trauma center.12 In addition, two authors (SFM and AHT) participated in the mock MCI.
RESULTS
Transport and Early Timeline
The initial 9-1-1 call occurred at 10:39 on August 3. 2019, followed by EMResource notification at 10:53. (EMResouce is a notification system to multiple clinicians in the region). By 10:54, an emergency medical services (EMS) captain notified UMC of multiple casualties. A surge of 14 victims arrived at the Level I trauma center within 34 minutes. Ten of these patients were Level 1, the highest level of trauma activation, and four arrived by private vehicle (Figure 1). Eleven patients arrived at the Level II trauma center, and two Level 3 patients were transported to two Level III trauma centers. Transport from scene was rapid: the Level I trauma center is 4 miles and the Level II center is 2.5 miles from the MCI scene. We were unable to obtain more specific triage, injuries, ISS, and death-at-scene data as this information was withheld for use in the criminal proceedings. In addition, we only had access to medical records or patient information from the Level I trauma center.
The Regional Area Council (RAC) for Trauma Service Area I supplied an ambulance bus, but it was not used.
Outcomes
At UMC, the mean ISS was 9.9 ±11.5 (1-38) of the 10 female and 5 male victims. Fourteen survived. Of the victims brought in the first hour, one patient arrived without vitals, underwent an ED thoracotomy, and died of injuries sustained during the shooting. Another patient arrived later that day as a transfer, thus totaling 13 patients who survived the first surge. A final patient arrived in transfer later, for a total of 14 survivors. Mean age was 40.6 ± 22.6 years (1-88 years). Mean hospital length of stay (LOS) was 13 ± 16.4 days. Six patients went to the intensive care unit (ICU): mean ICU LOS was 5.7 ± 4.1 days (2-11); hospital LOS for these six was 22.6 ± 19.6 (10-62.) Median ventilator days for three patients was eight days. The one death occurred at UMC due to a thoracic vessel wound that was discovered after resuscitative thoracotomy. Of the 11 patients brought to the Level II center, there were 9 survivors after 24 hours. The two deaths at that center were due to one patient experiencing an acute myocardial infarction during resuscitation and one elderly patient who received comfort care only and subsequently died. An additional death occurred at the Level II center months later.
Triage
At the Level I trauma center the first activation came at 10:57, and the first patients arrived at 11:03. Because the MCI/ AS occurred on a Saturday when few clinicians were present,
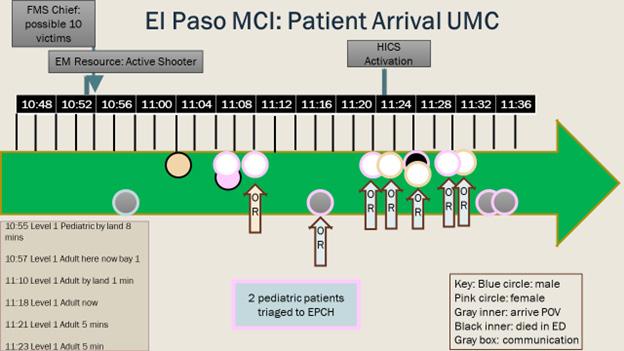
Figure 1. Timeline of patient arrival and Hospital Incident Command System activation at UMC.
*Note: FMS, The El Paso Fire Department and Emergency Medical Services work in combination.
MCI, mass casualty incident; UMC, University Medical Center; EMS, emergency medical services; HICS, Hospital Incident Command System; EM, emergency medicine; EPCH, El Paso Children’s Hospital; POV, privately owned vehicle; ED, emergency department.
it became necessary to both triage and care for patients at the same time. In prior mock MCI events patients arrived presorted with colored tags attached, but in the aftermath of the shooting we had to treat patients without tags and without a second physician to perform triage. In contrast, the Level II center had sufficient staff, which allowed for one physician to focus solely on triaging patients. Five of the initial 14 patients arrived with a level 1 activation (L1A). All patients would have been designated L1A if each had arrived outside the setting of an MCI, but some were not activated as such due to arrival by privately owned vehicle (Timeline, Figure 1). If a patient with normal vital signs arrived but had been shot, these patients were seen by emergency physicians and general surgeons; it wasn’t necessary to activate L1A because surgeons were already present in the ED, as were the radiology, laboratory, and respiratory therapy services. Neither was a patient sesignated LIA if they were initially seen in the hall, thereby bypassing the trauma bays and going straight to the OR. When the first patient arrived, the surgical trauma team on site included one general surgeon trauma attending, one fifth-year surgical resident, two second-year surgical residents, two interns, and an orthopedic team that consisted of one faculty attending and two residents. The ED had two faculty attendings present. Anesthesia had one faculty and two nurse anesthetists (CRNA) present. The ED attending and one general surgeon performed triage and patient care simultaneously. A general surgery attending and a surgical resident and an ED attending and an emergency medicine resident were in each of 12 trauma rooms. At triage the patients were sent to the OR, to a floor in the main hospital or children’s hospital, or to the ICU after imaging studies. No tagging systems were used (Figure 2). The disposition of 15 patients, including one later arrival, was as follows: four to
McLean
El Paso Mass Casualty Incident Hospital Response: Enhancing Surge Capacity McLean
regular floor; two to home from the ED; one directly to the ICU; five to ORs; one to the morgue; and two to an adjoining pediatric hospital. By the end of the day, five of the six patients who underwent surgery went to the ICU, and one to the regular floor (Figure 2). The overall triage system at the Level I trauma center functioned well because initially there were empty ORs, and the ICU space had been expanded into an empty pre-op area.
Our main objective in this study was to review the in-hospital response at our Level I trauma center; we received additional information from the Level II center and the two Level III centers. At the Level I trauma center, we had one general surgeon and one orthopedic surgery attending present at MCI onset. The Level I center subsequently called in eight additional attending surgeons (six general, one orthopedic, and one cardiac) totaling 10 attending surgeons. The Level II center had two general surgeons on duty and called in seven additional attending surgeons. Because the Level I center already had one general surgery attending on call, that surgeon did simultaneous rapid triage with the ED attending, as well as performing initial surgical treatment. In contrast, at the Level II center two general surgeons were on duty, including the trauma medical director, who served as triage officer and performed no initial surgeries. That center called a trauma surgeon over from a nearby Level III center, as well as orthopedic and neurosurgeons, and an additional general surgeon who had privileges at the Level II center.
At our Level I trauma center, 14 of 15 patients
survived—a 93% survival rate at 24 hours. Of the eleven arrivals at the Level II center nine survived, for 82% survival at 24 hours. We documented no significant difference in percentage survival (P = .56) between the Level II triage system, which had a separate triage physician, and the Level I center where one general surgeon and one emergency physician simultaneously triaged and treated patients.
Trauma Teams Personnel Surge: General Surgery and Orthopedic Surgery
The entire general surgery department was activated including subspecialists in pediatric, endocrine, oncology, colorectal, and cardiothoracic surgery. The subspecialists arrived 30-45 minutes after MCI activation, assisting with line placement and evaluations for Advanced Trauma Life Support. The cardiovascular surgeon assisted orthopedic surgery in one case involving an extremity. The first two orthopedic surgeons operated on an open thigh wound; and when that patient needed repeat surgery, a cardiovascular surgeon joined this team to stop the bleeding. This same patient had an exploratory laparotomy concurrent with orthopedic surgery. Among the procedures performed to stabilize fractures and treat orthopedic injuries using damage-control methods were the following: external fixation; irrigation; splinting; and debridement (Tables 1 and 2).Operative triage began at UMC with the first group; a patient had a trans-abdominal gunshot wound and went to the OR from the ED without occupying a trauma bay, with one general surgeon in the hospital and one chief resident arriving within 15 minutes of patient arrival. Four primary laparotomies were performed on day 1; one additional laparotomy was returned to the OR for bleeding within an hour (Table 1). Twenty-six surgeries were performed on the subsequent 2 through 191 days after the MCI. The mean initial laparotomy start time from arrival was 25.7 minutes. General surgery, orthopedic, and bedside procedures are listed in Table 2. Procedures performed later are listed in Table 3. The second procedure was an ED thoracotomy by a second general surgeon who arrived from outside the hospital. With his arrival two trauma surgeons were on site. The patient who had a thoracotomy performed in the ED died, thus freeing the second general surgeon to perform laparotomies. Two postgraduate year-5 and numerous lower-level residents arrived within 20 minutes. The second and third laparotomies occurred concurrently.
The first general surgeon who performed laparotomy 1, returned to the ED and assessed a new patient with indications for surgery. That patient needed both laparotomy for a transabdominal gunshot wound (GSW) and left thigh exploration for GSW to left thigh. This first general surgeon, freed up after laparotomy 1, then performed laparotomy 3 and adjunctive procedures concurrent with two orthopedic surgeons exploring an extensive bleed from a left thigh wound. This patient returned to the OR from the post-anesthesia care unit (PACU) within an hour after the thigh restarted bleeding; the
Figure 2. In-Hospital Triage of shooting victims at Level 1 Trauma Center ED,
Children’s
1. 00:01
Exploratory laparotomy
Hepatic packing
Evacuate duodenal hematoma
Pack back and flank wounds
AbThera placement
2. 00:36
Exploratory laparotomy
Small intestinal resection, multiple sigmoid resection
Bilateral tube thoracostomy
AbThera placement
3. 00:23 Left anterior resuscitative thoracotomy
Exploratory laparotomy
Splenectomy
Small intestinal resection
AbThera placement
4. 00:43 Left chest tube
Exploratory laparotomy, hepatic packing
Explore and ligate bleeding vessels left thigh
Right femoral CVP, right femoral arterial line
Left subclavian CVP
Pack wounds
5. 4:12
NA
NA
Re-exploratory laparotomy
Sigmoid colectomy
Diaphragm repair
Ligation IMA
AbThera placement (00:08)
Re-explore left thigh and ligate left femoral vein (01:40)
Debride left open humerus fracture, External fixation left open humerus fracture
6. 4:48 Bilateral thigh irrigation and debridement
Open arthrotomy and irrigation and debridement right knee
AbThera, temporary abdominal closure system; OR, operating room; hrs/min, hours/minutes; NA, no answer; IMA, inferior mesenteric artery; CVP, central venous pressure
cardiovascular surgeon assisted orthopedic surgery with femoral vein ligation. The second general surgeon, who was available after the ED thoracotomy, operated on a patient with multiple GSWs and a transpelvic GSW, laparotomy 3. A third general surgeon who arrived during these procedures took the fourth laparotomy to the OR. This fourth laparotomy was completed rapidly. After the fourth laparotomy patient entered the PACU, the patient had to return to the OR within an hour for bleeding. This bleeding required repeat laparotomy for hemorrhage control. A fourth general surgeon and a pediatric surgeon arrived at laparotomy 3 after the laparotomy had been performed, and they placed an additional central line. All four laparotomies were damage-control procedures. A fifth general surgeon (colon and rectal) arrived after the laparotomies had been done in the OR and started compiling a list of patients from the MCI/active shooter event. A sixth general surgeon arrived and attended to a patient in the ED who did not require surgery on day 1.
The surgeons had face-to-face communication in the PACU and later communicated via cell phone. The deployment of arriving attending surgeons was coordinated
verbally, by surgeons checking in and reporting back to the ED and PACU. Surgical residents and emergency physicians worked in the trauma rooms to identify patients who likely needed laparotomy or orthopedic procedures, thereby enhancing patient flow from the ED to the OR The adjacent locations of the ED/OR/PACU also helped patient flow. In summary, there were four primary laparotomies, one thigh exploration for the initial cases, and one ED thoracotomy. These cases required three general surgeons and two orthopedic surgeons who were present or who arrived within 30 minutes. The fourth general surgeon placed a central line on laparotomy patient 3. One patient returned to the OR for laparotomy for bleeding, and one returned for thigh bleeding. These cases occurred in the first 90 minutes after arrival of 14 patients. There were two additional orthopedic surgeries on day 1.
Trauma Team Surge at University Medical Center
To delineate total hospital staff response, we surveyed 16 departments for numbers and methods of call-in (Table 4). A total of 132 additional personnel arrived from the 16
Table 1. Initial six surgeries.
Table 2. Bedside procedures.
Case Day Procedures
1 1
2 1
Irrigation and splinting right index finger
Irrigation wound and excision bullet right gluteal cleft
4 1 Right lower extremity bedside incision and drainage
5 1 Right thigh wound care
6 1 Right tube thoracostomy
Left tube thoracostomy
eFAST ultrasound
Echocardiogram
7 3 Right internal jugular CVP
10 3 Echocardiogram
10 19
EGD/PEG
52 EGD and pancreatic stent removal
11 1 Irrigation and debridement left thigh wounds
13 1 ED resuscitative thoracotomy, right tibial IO catheter
14 3 Right internal jugular CVP
Comments
Discharge day 2 after MRI brain
Discharged from ED
Went to wound care 8 weeks post discharge from ED on day 1
Transfer to ICU
Frequent blood draws, patient had MI MRI, magnetic resonance imaging; ED, emergency department; ICU, intensive care unit; eFAST, extended focused assessment with sonography in trauma; CVP, central venous pressure; EGD, esophagogastroduodenoscopy; PEG, percutaneous endoscopic gastrostomy, IO, intraosseous; MI, myocardial infarction.
departments surveyed. Mean number of employees called in per department was 8.3 ± 7.1; mean 94.4% ± 25.5%. Notification methods included the following: text messaging, 12 departments (75%); phone call, 14 departments (87%); phone tree, three departments (19%); and pager, two departments (13%). Eight departments (50%) reported self-arrival (without specific call-in). Two departments used four methods of contact, four departments used three methods, seven departments used two methods, and one department used one method of contact.
Adjuncts to Personnel Surge Transfusions and Settings
A massive transfusion protocol aided in transfusion of 49 units of packed red blood cells (PRBC). Six patients received a mean of 8 PRBC, 6.4 fresh frozen plasma units (FFP), 12 platelets, and 8 × 10 pack units cryoprecipitate. The hospital settings themselves enhanced care for the trauma patients: nearly empty ORs on a Saturday, and ICU bed expansion into the empty pre-op area.
Problems with Mass Casualty Incident response at Level I trauma center, UMC, and Early Solutions
The first problem was limited information from the scene, which was resolved by trauma bay reports from EMS. A second problem was that the hospital switchboard became overwhelmed by calls from the community. A third problem— double registration with “trauma names” and real names—was resolved during physician rounding. A fourth problem was delayed HICS activation, which did not occur until 30 minutes post-patient arrival. The delayed HICS activation impelled
healthcare workers responding to use texts and phone calls to alert other practitioners that a MCI/active shooter event was occurring and to report to the hospital.
To address problems, the hospital disaster committee reviewed the HICS incident. To resolve registration confusion, the hospital adopted the Texas Wristband Project, in which a patient receives a wristband with a number that stays with the patient throughout the trauma episode, from incident scene through hospital admission. To prevent the hospital switchboard from being overwhelmed, the Regional Area Council for Trauma now designates multiple places around the city for family reunification centers. To assist with medical personnel notification, the Level I trauma center, as well as Texas Tech University Health Sciences Center at El Paso, have instituted emergency alert systems that go out over pager, cell phone, and email. To aid documentation, the ED faculty created a short emergency history and physical exam form.
The impact of these changes has been tested twice since 2019. A shooting incident with four victims occurred at the Cielo Vista Mall in El Paso on February 15, 2023. Three victims survived, and one died.11 Two patients were transferred to the Level I trauma center. The emergency notification mobilized > 50 physicians and nurses to the trauma center. Both victims survived. A mock MCI, modeled as a multiple plane crash with 100 victims, was staged on October 12, 2023, at the El Paso International Airport (EPIA) as the triennial citywide emergency exercise. Nineteen total patients including two pediatric patients were sent to the Level I trauma center at UMC (the center we report on here).
Improvements were seen in hospital and personnel activation (Table 5). Hospital activation occurred early, at the
Table 3. Subsequent surgeries.
Case Number of days since arrival Case description
3 4 Right elbow fracture irrigation and debridement, Integra and wound vac placement
37 Right elbow irrigation and debridement and split thickness skin graft 6 x 4 cm
8 4 Irrigation and debridement, exploration, open reduction and internal fixation of distal and proximal phalanx and rotational flap of right thumb
10 Right breast reconstruction with oncoplastic technique using an inferiorly based glandular cutaneous flap. Left mastopexy for symmetry
9 1 Re-exploration of open abdomen, abdominal fascial closure
Debridement and washout right back and flank wounds and removal foreign body × 2
Left thigh medial and lateral wound irrigation, debridement and wound vac placement, primary closure of lateral wound
5 Irrigation and debridement left leg wound, exploration femoral vessels, irrigation and debridement right medial leg wound, replace packing right flank wound
25 Irrigation and debridement left thigh wound after dehiscence with removal of skin ellipse 5 x 3 cm.
10 2 Re-exploratory laparotomy, left hemicolectomy, small bowel resection with anastomosis, transverse colostomy, traumatic diaphragmatic hernia repair, gastrorrhaphy, left abdominal wall component separation and abdominal wall closure
2 Cystoscopy, bilateral retrograde pyelogram, left ureteral stent placement
13 Incision and drainage abdominal wound and left upper back wound
29
11
12
Midline wound washout and placement of ACE ll wound matrix 7 x 10 x 2 cm and ACELL powder for enterocutaneous fistula; placement negative pressure wound therapy device
46 Isolation of enterocutaneous fistula with 24 Fr Foley catheter; split-thickness skin graft 187 cm squared
54 Cystoscopy and left ureteral stent removal
191 Colostomy reversal, enterocutaneous fistula resection, adhesiolysis, PEG removal, abdominal wall reconstruction with bilateral component separation
19 Excision of left buttock foreign body
2 Re-exploratory laparotomy, small bowel resection and anastomosis, segmental transverse colectomy with end colostomy, Moss feeding tube placement, proctoscopy, right thigh debridement, left tibia washout and removal foreign body
Right hand irrigation debridement and splinting
5 Exploratory laparotomy, repair of traumatic left iliac hernia, right lower extremity irrigation and debridement, right chest tube placement
6 Irrigation and debridement right hand gunshot wound, wound exploration, foreign body removal × 2.
10 Operative screw fixation of left anterior column acetabulum
6. Right hand gunshot wound irrigation, debridement, removal of foreign body fragments
13 Irrigation and debridement left gluteal gunshot wound for seroma
46 Irrigation and debridement and metacarpal fracture joint replacement with a Pyrocarbon implant
153 Colostomy reversal, proctoscopy, scar revision; right hand foreign body removal, left gluteus irrigation and debridement and foreign body removal.
14 4 Irrigation and debridement, open reduction and internal fixation of left Humerus shaft fracture
83 Removal of left antecubital fossa foreign body
15 1 Re-exploratory laparotomy, abdominal closure, debridement of right flank wound PEG, percutaneous endoscopic gastrostomy: wound vac, vacuum-assisted closure; cm, centimeter.
start of the incident. The HICS activation at the Level I trauma center occurred prior to the first patient leaving the scene: > an hour earlier than in the August 3, 2019, MCI. All patients had a numbered wristband and so were identifiable from scene to hospital. There were no duplicated entries. Personnel activation improved: Hospital notification occurred at 8:45
am; HICS personnel activation to group A (departmental leaders) occurred at 09:33 am; first patient left scene at 09:40 am; and a second HICS activation occurred at 10:28 am. At 11:03 am messaging advised of a meeting in the Level I trauma center boardroom for debriefing.12. These times for entire hospital activation were quicker than during the August
on call or backup were called automatically. Text messaging alerted department. 100% of those called came, if they were in town.
all people who came in would be ≈ 50% above average
total ICU nursing came in when not scheduled, 13% showed up and 2% called.
of department called, 50% of those came in, for 25% additional staff overall.
employees called in early; supervisor saw post on Facebook and self-arrived.
called in, and 9 stayed over shift time to make 12 total respondents.
of those called came in; 7 called and 5 additional came in. CRNA, certified registered nurse anesthetist; ED, emergency department; OR, operating room; ICU, intensive care unit, CT, computed tomography.
3, 2019, MCI. Thus, over one subsequent MCI/active shooter event and one mock MCI in 2023, the changes made after the initial August 2019 incident sped up hospital response and clarified patient identification from scene.
DISCUSSION
A Level I trauma center in El Paso, TX, responded to a rapid patient influx after an MCI/active shooter event. Practices that facilitated response were a simplified triage method, timely arrival of trauma team and associates, and immediate ICU expansion. Medical practices enhancing hospital response included damage-control surgery and massive transfusion policy. All patients who arrived with vital signs survived.
Triage: In Hospital
Triage is essential to differentiate patients requiring immediate surgery from patients requiring workup and disposition. There are two issues with expanding trauma teams in response to an MCI. One is personnel availability, and the
second is patient arrival times. When there are few personnel to handle a rapid patient influx, triage and care must be simultaneous, involving both emergency physicians and general surgeons. Two other hospitals in the US specifically used a combined triage with EM and trauma surgery after an MCI: 1) Beth Israel Deaconess Medical Center after the Boston Marathon bombing in Massachusetts (April 2013); and Scott & White Memorial Hospital during the Fort Hood, TX, MCI/active shooter event (November 2009), where an ambulance-bay triage team composed of emergency physicians and one general surgeon organized initial care.7,13 Hirschberg et al modeled trauma response in a computer simulation based on actual MCIs. He noted that up to 4.6 critical patients per hour could be treated with in-house trauma teams, but that with expansion an increase to 7.4 critical patients per hour was feasible.14 In El Paso, the Level I trauma center had one general surgeon available at the start; hence, initial triage was provided by the this general surgeon, the emergency physician, and associated residents. As in the Table 4. Hospital personnel arriving for response to
Table 5. Table of comparisons for the three mass casualty incident activations.
08/03/2019 141 10:53 11:05 11:20 13:05 15:00 13:17
MacArthur Elementary School.
02/15/2023 22 17:24 17:27 03
10/12/2023 17
18:20 Est. at Burgess High School
2 sent to EPCH, affiliated with UMC, the L1TC 08:45 9:504 09:33 11:03 12:12 Mock drill, no center established by office of emergency management or RAC.
Late HICS activation
Communication with public Family meeting area not publicized until late in day, leading to persons coming to hospital and crowding in ICU waiting area, which is near entry point.
Switchboard jamming at L1TC
Patients had dual registrations, causing clinicianss to take hours to clarify.
No HICS activation
Crowding due to staff who were not providing treatment lingering in ED treatment areas.
AOD asked the hospital operators to activate MCI; however. operators correctly activated HICS both overhead and on pagers/texts.
Triage area in ambulance bay was crowded; however, clinicians were well dispersed. No impediments to patient care.
Registration used Texas Wristband numbers, improved.
1. During event, at scene 4 injured, 1 dead on scene, 2 transported to UMC or L1TC, and 1 patient sent elsewhere.
2. 4 total victims, 1 dead on scene. 2 patients transported to UMC the L1TC.
3. HICS not activated. The L1TC security and police were activated. RMOC activated at 17:27 and deactivated at 21:34. Both patients admitted to UMC, the L1TC. HICS not activated due to smaller patient load but was noted to be a problem that could have corrective action, as there were problems with crowding. Emergency communications did not go out to associates.
This incident was a citywide mock massive casualty event, the EPIA Triennial Exercise. In this mock scenario a plane crashed at the airport. There were 100 victims, 72 sent to area hospitals. In the After-Action Report and Improvement Plan, first patient transported off scene from the EPIA at 09:40 am per EMResource. (EMResouce is a notification system to multiple clinicians in the region). The fastest that a patient might have arrived was at 11:40 am, although this was not recorded in the after-action report. The HICS activation was timely. Healthcare staff were in place for first patient arrival. Previous registration problems were resolved by using wristbands. With the Texas Wristband Project, trauma patients are issued a numbered wristband that stays with them through all encounter—ED, admission and even transfer to another facility. However, registrars noted that this number had to be entered into three places.
UMC, University Medical Center; L1TC, Level I trauma center; HICS, Hospital Incident Command Center; EPIA, El Paso International Airport; RMOC, Regional Medical Operations Center; RAC, Regional Advisory Council for Trauma, the BorderRAC.
computer model, bringing in more trauma team members increases the ability to care for more patients.
Having the emergency physician and general surgeon perform both triage and patient care is advantageous for treating patients when there are short patient-arrival times. With longer arrival times, more personnel can be redeployed from other areas or from home to increase trauma team size. During the El Paso MCI, the receiving hospitals had <10 minutes from initial notification until patient arrival. Similarly, during the Boston Marathon bombing, the five receiving hospitals were within two miles of the MCI scene, which led to short response times.6,13 Hospital responses for the Virginia Tech MCI/active shooter event in Blacksburg, VA (April 2007), and the Fort Hood MCI were longer at 23 minutes and >one hour to patient arrival, respectively.4,7 Thus, reported
patient arrival times after MCI activation has ranged from 10 minutes to >one hour. While both the Level I and II trauma centers receiving patients in El Paso had short patient arrival times, the two hospitals had equivalent survival rates. Having a general surgeon and emergency physician to treat victims while simultaneously triaging was associated with equivalent survival rates to having separate triage officers.
Triage for severity may be inaccurate during an MCI. It is reported that only 10-15% of patients arriving during an MCI are critically injured.14 In over-triage the limited resources of a trauma team are depleted on patients who are less severely injured than initially expected; conversely, under-triage leads to the most severely injured patients not getting rapid care. Perfect triage is difficult: a retrospective review of two MCIs in Israel noted that even experienced trauma surgeons initially classified
El Paso Mass Casualty Incident Hospital Response: Enhancing Surge Capacity
only 7 of 15 “severe” injuries as severe, (ie, undertriaged) and classified three mild-moderate injuries as “severe” (ie, overtriaged).15 A retrospective review of a binary triage that was used prehospital in the terrorist attacks in Paris, France, in November 2015 noted a 36% under-triage and 8% over-triage rate.16 Similarly, a prospective study of MCI in-hospital triage demonstrated 24% over-triage and 16% under-triage.17
These three articles demonstrated varying rates of overand under-triage in MCI events. It is critical to use resources efficiently in an MCI; hence, the presence of an emergency physician and a general surgeon at UMC to simultaneously triage and treat likely avoided delays in care from waiting until trauma personnel arrived from outside the hospital. In summary, when patient arrival times are fast, it is imperative for the trauma teams present to both triage and continue care, as happened at our Level I trauma center during the MCI/ active shooter event in 2019. Using the emergency physician and the general surgeon on duty to both triage and provide care was not associated with increased mortality.
Turnover by Damage Control
The Level I trauma center surgeons used the principles of damage control surgery (DCS) to preserve patient physiology as well as turn over trauma teams. In trauma surgery DCS refers to not completing the surgery but instead immediately treating life-threatening injuries.18 Advantages of DCS include the ability to correct physiological derangements before definitive surgery. Both orthopedic and general surgeons used DCS.19 Trauma surgeons used abbreviated laparotomy with temporary closure, and orthopedic surgeons used external fixation and washout. In trauma cases requiring > 3 transfusions per hour, DCS has been associated with increased survival after laparotomy.19 The use of DCS was key in other civilian traumatic MCIs: in Paris in 2015; in 12 civilian mass shootings in 2016; and for orthopedic injury management during the 2015 Amtrak derailment in Philadelphia, PA.10, 20, 21
A second reason for using DCS, besides physiology restoration, is that using DCS further helped turn over staff and ORs. Remick et al discussed that in military MCIs, surgeons need to maintain situational awareness of battles, the probability of further injuries, and resource utilization.9 This military DCS or “mDCS” combines physiological and clinical variables that prompt usual damage-control decisions in surgery (clinical DCS [cDCS”]) with combat variables that contribute to ongoing injuries). When civilian trauma teams used situational awareness to treat patients in a civilian MCI, combined with typical reasons for DCS patient physiological characteristics, this has been termed mass casualty DCS (mcDCS).9 In the El Paso MCI the initial laparotomies met criteria for cDCS due to hypotensive, acidotic, or blood loss criteria for DCS.10, 20, 21, 23 In addition, the use of DCS, which was clinically indicated, also aided patient throughput from ED to OR to PACU and, thus, could be considered “mcDCS.”
The practice of early DCS, correction of blood volume, and
having multiple teams perform surgeries has been reported in both military and civilian MCIs.24,20 In Paris, at the Bégin Military Teaching Hospital, five ORs were used for performing 24 surgeries in 24 hours.20 The four laparotomies at our Level I trauma center in El Paso occurred with an average time to OR of 25 minutes; comparably, in a review of the Paris 2015 terrorist attacks, it was found that average time to OR for the most injured was 147 minutes.16 In the El Paso MCI/active shooter event, DCS aided both transport to OR, if needed, and rapid re-deployment of surgeons and staff for further trauma care.
Transfusion
Massive transfusion protocols were used for six patients. In both the 2013 Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) study and the 2015 PROPPR (Pragmatic, Randomized Optimal Platelet and Plasma Ratios) clinical trial, the importance of maintaining a transfusion ratio of 1:1:1:1 of FFP: PRBC:platelets:cryoprecipitate was demonstrated to decrease day one mortality from hemorrhage.25, 26 The Level I trauma center had in place a massive transfusion protocol that specified the specific blood product components brought up to the ED and OR. This specification included products that, if given in order, would give the correct ratio of FFP:PRBC:platelets: cryoprecipitate to adhere to a 1:1:1:1 ratio. The massive transfusion protocol enforced adherence to the 1:1:1:1 transfusion ratio at our Level I trauma center has been reviewed and published elsewhere. 27
Team
Rapid expansion of all personnel departments was integral to the MCI response at the Level I trauma center. In simulation studies, increasing team numbers was associated with ability to care for more patients.14 Reports on the Boston Marathon bombing were similar to the El Paso MCI situation; the bombing occurred on a holiday, meaning there with fewer planned surgeries in the hospitals, and many staff arrived quickly as they lived nearby.6,13 At our Level I trauma center, the MCI occurred on a Saturday; hence, while the ORs were mostly empty, a smaller cohort of healthcare workers was present on the weekend, meaning staff did have to come in to the hospital. This might have caused a delay; however, all the patients who had surgery survived. In contrast, during the Fort Hood MCI, sufficient surgical staff were already present.7 At our Level I center, there was rapid expansion of other hospital staff in addition to surgeons, which was critically important for trauma management: environmental services for OR/ED room turnover; and nursing staff in the OR, ED, and ICU. Per an after-action survey, a total of 132 personnel arrived.
Mass Casualty Incident Problem Response
Problems in our Level I trauma center response included communications and registration, which were comparable to what has been previously reported. Often receiving hospitals did not have accurate information from the scene.4,7 During
the Fort Hood MCI, it was noted that the Level I center did not receive reports on intrahospital transfers until helicopter contact due to phone line obstruction. The sending hospitals suffered from switchboard jamming at the receiving hospital after the number was publicized.7 During the Virginia Tech MCI, there was a reported lack of communication from the scene to the hospital.4 Another issue is that short notification prior to arrival6,10 occurs when hospitals are close to the scene.
The second issue with communication/electronic medical record was patient identification and registration, including dual name registrations per patient, a problem solved during physician rounds and by in-person identification. During the Boston MCI, identification problems at Beth Israel Deaconess Hospital were solved by creating a special MCI team.13 The Texas Wristband Project, which introduced a scene-number wristband, will likely solve identification issues. The wristband project was initiated prior to 2019 and was piloted by nine Regional Area Councils for Trauma and Emergency Services from December 1, 2020–January 31, 2021. The project came to fruition approximately a year and a half after the 2019 MCI/ active shooter event. The wristband project was put into place by Texas Senate Bill 500 and the Department of State Health Services in Texas to keep track of patients being transferred by EMS in large-scale disasters. Using the wristband, a patient will have one alpha-numeric identifier throughout his course of care from scene to whichever hospital he is transferred. This identifies the patient, who will keep the the same identifier throughout the course of care.28
LIMITATIONS
This retrospective cohort study may have been subject to recall and reporting bias. The study is limited by legal aspects of the 2019 MCI including ongoing legal actions, which prevented precise description of ballistics, weapons, and cause of death on scene. Additionally, a retrospective study depends on health-record and time-reporting accuracy. An additional limitation was that the comparison cohort in this study was a nearby hospital that had a single, separate triage clinician on duty. Thus, there was not an identical patient comparison group, leaving the possibility of selection bias; our Level I trauma center may have had injuries more amenable to successful treatment. It should also be noted that we had limited access to patient medical records at the Level II center; therefore, those patients’ injuries are incompletely described. Neither was ISS data available to compare the Level II center to our Level I center. Thus, we were unable to compare patient severity.
We used the outcome “survival” when comparing the two triage systems. It is probable that survival was determined by specific injuries and their severity, and not necessarily by the triage system itself. Further, because it was not possible to capture data from all hospitals (eg, if a patient tripped and fell and sustained injury during the MCI, and then presented to the Level II or III centers and was not transferred to our Level I
center, we would not have captured that patient as an injury related to the MCI/active shooter event. Regarding the trauma team expansion, the survey data was compiled based on the recall of chiefs of service and could, therefore, have been affected by recall bias. The timing of surgeries was based on times reported from ED admission to the OR. Admission to the ED was listed as the time a patient was registered; however, because so many patients arrived in a short time, the registrar may have registered some at the same time, for convenience. Finally, at both the Level I and Level II centers, both groups had small numbers, increasing the risk of a type II error.
CONCLUSION
The seventh most deadly active shooter event in US history occurred in El Paso, TX, on August 3, 2019.2 We describe the hospital response at our Level I trauma center. In characterizing this response, multiple factors including rapid influx of hospital personnel, a massive transfusion protocol, and the use of damage- control surgery practices were likely helpful. These factors were not compared to other hospitals in the area since this data was not collected and not part of this study. Our Level I center had a small number of surgeons and emergency physicians initially to receive the injured patients. By necessity, the triage officers simultaneously provided care. Noting later that at the Level II center the trauma team had a separate triage officer, we hypothesized that survival rates between the two centers would be comparable. And, in fact, the two triage systems were associated with no significant difference in survival at the end of the first day between the two centers. Thus, we conclude that when a trauma center is pressed to provide initial triage and trauma care rapidly in a mass casualty incident/active shooter event of this size, a small group of clinicians can initiate trauma care and triage simultaneously.
ACKNOWLEDGMENTS
The authors would like to thank Surgery Chief Residents Ginger Coleman, William Klingsporn and Isaac Lee for their assistance during the MCI.
Address for Correspondence: Susan F. McLean, MD, MPH, Texas Tech University Health Sciences Center, Department of Surgey, 4800 Alberta Avenue, El Paso, TX 79905. Email: susan.mclean@ ttuhsc.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 McLean et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
McLean
REFERENCES
1. Gun Violence Archive. Report: Mass shootings in the United States all years. 2020. Available at: https://www.gunviolencearchive.org/ mass-shooting?sort=desc&order=%23%20Injured. Accessed November 13, 2020.
2. Federal Bureau of Investigation, U.S. Department of Justice. Active shooter incidents in the United States in 2019. Federal Bureau of Investigation and Department of Homeland Security. 2020. Available at: https://www.fbi.gov/file-repository/reports-and-publications/ active-shooter-incidents-in-the-us-2019-042820.pdf/view. Accessed January 24, 2024.
3. Blair JP, Schweit KW. A study of active shooter incidents, 2000-2013. Texas State University and Federal Bureau of Investigation, U.S. Department of Justice. 2014:2154-2156. Available at: https://www.fbi. gov/file-repository/reports-and-publications/active-shooter-phase-iqrg-active-shooter-incidents-in-the-us-between-2000-2013-2.pdf. Accessed January 24, 2024.
4. Kaplowitz L, Reece M, Hershey JH, et al. Regional health system response to the Virginia Tech mass casualty incident. Disaster Med Public Health Prep. 2007;1(1 Suppl):S9-S13.
5. Boston Trauma Center Chiefs’ Collaborative. Boston Marathon bombings: an after-action review. J Trauma Acute Care Surg 2014;77(3):501-3.
6. Gates JD, Arabian S, Biddinger P, et al. The initial response to the Boston Marathon bombing: lessons learned to prepare for the next disaster. Ann Surg. 2014;260(6):960-6.
7. Wild J, Maher J, Frazee RC, et al. The Fort Hood massacre: lessons learned from a high profile mass casualty. J Trauma Acute Care Surg 2012; 72(6):1709-13.
8. Biddinger PD, Baggish A, Harrington L, et al. Be prepared — the Boston Marathon and mass casualty events. N Engl J Med. 2013; 368(21):1958-60.
9. Remick KN, Shackelford S, Oh JS, et al. Surgeon preparedness for mass casualty events: adapting essential military surgical lessons for the home front. Am J Disaster Med. 2016;11(2):77-87.
10. Harper K & Rehman S. Orthopedic disaster management in the 2015 Amtrak derailment. J Trauma Acute Care Surg. 2016;80(6):1032-8.
11. Martinez, Aaron and Kolenc, Vic. Bystander shot Cielo Vista Mall gunman as suspect fled fight while pointing gun. El Paso Times. 2023. Available at: Cielo Vista Mall shooting: Bystander shot shooter as suspect fled, or https://www.elpasotimes.com/story/news/ crime/2023/02/17/by-stander-shot-cielo-vista-mall-shooter-assuspect-fled-scene/69917660007/. Accessed January 24, 2024.
12. Berger D, Zubia G, Camacho L, Janes D, Bastardo N. 23-1012 EPIA Triennial Exercise and After Action Report and Improvement Plan. October 12, 2023. Point of Contact: Donal Berger, MPA, CHSP. donald.berger@umcelpaso.org.
13. Tobert D, von Keudell A, Rodriguez EK. Lessons from the Boston Marathon bombing: an orthopaedic perspective on preparing for high-volume trauma in an urban academic center. J Orthop Trauma 2015;29 Suppl 10:S7-10.
14. Hirshberg A, Scott BG, Granchi T, et al. How does casualty load affect trauma care in urban bombing incidents? A quantitative analysis. J Trauma. 2005;58(4):686-95.
15. Ashkenazi I, Kessel B, Khashan T, et al. Precision of in-hospital triage in mass-casualty incidents after terror attacks. Prehosp Disaster Med. 2006;21(1):20-3.
16. James A, Yordanov Y, Ausset S, et al. Assessment of the mass casualty triage during the November 2015 Paris area terrorist attacks: towards a simple triage rule. Eur J Emerg Med 2021;28(2):136-43.
17. Kleber C, Cwojdzinski D, Strehl M, et al. Results of in-hospital triage in 17 mass casualty trainings: underestimation of life-threatening injuries and need for re-triage. Am J Disaster Med. 2013;8(1):5-11.
18. Waibel BH & Rotondo MF. Damage control in trauma and abdominal sepsis. Crit Care Med. 2010;38(9 Suppl):S421-30.
19. Savage SA, Sumislawski JJ, Croce MA, et al. Using critical administration thresholds to predict abbreviated laparotomy. J Trauma Acute Care Surg. 2014;77(4):599-603.
20. Barbier O, Malgras B, Choufani C, Bouchard A, Ollat D, Versier G. Surgical support during the terrorist attacks in Paris, November 13, 2015: experience at Bégin Military Teaching Hospital. J Trauma Acute Care Surg. 2017;82(6):1122-8.
21. Smith ER, Shapiro G, Sarani B. The profile of wounding in civilian public mass shooting fatalities. J Trauma Acute Care Surg 2016;81(1):86-92.
22. Savage SA, Sumislawski JJ, Zarzaur BL, et al. The new metric to define large-volume hemorrhage: results of a prospective study of the critical administration threshold. J Trauma Acute Care Surg 2015;78(2):224-30.
23. Savage SA, Zarzaur BL, Croce MA, et al. Redefining massive transfusion when every second counts. J Trauma Acute Care Surg 2013;74(2):396-402.
24. Propper BW, Rasmussen TE, Davidson SB, et al. Surgical response to multiple casualty incidents following single explosive events. Ann Surg. 2009;250(2):311-5.
25. Holcomb JB, del Junco DJ, Fox EE, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148(2):127-36.
26. Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471-82.
27. Qiao J, Ray B, Wians F, et al. Transfusion management of trauma from the 2019 El Paso mass shooting incident. Vox Sang 2022;117(3):299-312.
28. Reeves C, Villa F. “Texas Wristband Project Summary,” published on the website of the Piney Woods Regional Advisory Council for Trauma. pages 1-6, 2020-2021. 2021. Available at: https://rac-g.org/ wristband/Texas%20Wristband%20Project%20Summary.pdf. Accessed January 24, 2024.
Examining Canadian Trauma Centres’ Analgesic Protocols for Rib Fractures
Sammie Yu, BMSc*†
Petrease Patton, MD‡
Kelly Vogt, MD, MSc§||
Fran Priestep, MSc||
Richard Hilsden, MD, MBA§||¶
Shane Smith, MD§||
Ian Ball, MD, MSc‡||#¶
Western University, Faculty of Science, London, Ontario, Canada
Western University, Schulich School of Medicine and Dentistry, London, Ontario, Canada
Western University, Department of Medicine, London, Ontario, Canada
Western University, Department of Surgery, London, Ontario, Canada
Victoria Hospital, Trauma Program, London Health Sciences Centre, London, Ontario, Canada
Western University, Department of Epidemiology and Biostatistics, London, Ontario, Canada
Western University, Office of Academic Military Medicine, London, Ontario, Canada
Section Editor: Leslie Osborn, MD
Submission history: Submitted June 21, 2024; Revision received June 5, 2025; Accepted June 9, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.24945
Introduction: Rib fractures are common in patients with blunt thoracic trauma, and their associated pain causes significant morbidity and mortality. Adequate analgesia is crucial to prevent rib fracture-associated pulmonary complications. However, current analgesic modalities have drawbacks, and the optimal analgesia protocol remains elusive. Intravenous (IV) lidocaine infusions have a well-established safety profile and efficacy in other patient populations and may benefit patients with traumatic rib fractures. To better understand current practices and to inform the design of a multi-centre trial, we believe that a study to determine Canadian trauma centres’ current analgesic practices is warranted. This study describes the current familiarity and use of IV lidocaine infusions for management of rib fracture pain. Secondary outcomes included the identification of common Canadian analgesic protocols for rib fractures and willingness to participate in a future multi-centre trial of lidocaine for these traumatic injuries.
Methods: We distributed an online survey to 14 Canadian trauma centres. Study questions were designed to address four themes: trauma centre characteristics; pain management strategies; current use of IV lidocaine infusions; and interest in future study participation. The analysis included a frequencies analysis and a thematic analysis of descriptions.
Results: The medical directors of 12 trauma centres (85%) responded. Six of those centres (50%) experience > 450 annual trauma admissions with Injury Severity Scores > 12. Six sites (50% of respondents) have a rib-fracture analgesic protocol. Four centres (33% of respondents) frequently use IV lidocaine for rib fractures, and 10 (83% of respondents) believe further research with IV lidocaine is needed.
Conclusion: Canadian trauma centres’ current practices for rib-fracture pain management are variable. Prospective work is needed to evaluate IV lidocaine as an analgesic for traumatic rib fractures. [West J Emerg Med. 2025;26(5)1367–1373.]
INTRODUCTION
Traumatic rib fractures are relatively common in all trauma patients, with an incidence of 10%.1 The incidence increases to nearly 40% for blunt thoracic trauma patients.2 Among those patients, the elderly population suffers a mortality rate of 68%, while the general population experiences a mortality rate of approximately 20%.2 Medical comorbidities in elderly patients increase their mortality from rib fractures.3,4 Overall, rib fractures remain common in all trauma patients of all ages and cause significant morbidity and mortality.
Rib fracture-associated morbidity and mortality is due to the pain that patients experience,2,5-7 particularly with movement and breathing.8 Pain from rib fractures causes patients to cough less and clear secretions less often and less effectively. Retained secretions can increase bacterial colonization and, consequently, promote pneumonia.5-7,9 Rib fractures can also cause muscle spasms that cause atelectasis and reduced respiratory function. Patients may experience hypoxemia, increased shunt fraction, and ultimately respiratory failure requiring intubation and mechanical ventilation.5-7,9
Analgesia is essential to prevent life-threatening pulmonary complications and mitigate rib fracture-associated morbidity and mortality.10 However, there is currently no optimal recommendation for pain management.6 Current analgesic practices include acetaminophen, non-steroidal anti-inflammatory drugs (NSAID), intravenous (IV) opioids, and epidural catheters.10 Less common approaches include intercostal nerve blocks, intrapleural or intrathecal anesthesia, and thoracic paravertebral blocks.11,12
Current protocols for treatment of rib fractures present challenges, including inadequate analgesia provided to patients. The current standard for the London Health Sciences Centre in Ontario, Canada, is IV opioids; however, opioids have a narrow therapeutic index in rib fractures. High doses of opioids will reduce respiratory drive and secretion clearance, thereby exacerbating conditions contributing to mortality.11 In contrast, the Eastern Association for the Surgery of Trauma (EAST) guideline on pain management in blunt thoracic trauma conditionally recommends the use of epidural analgesia instead of opioids.13 However, common conditions in trauma patients such as fever and altered mental status may prevent epidural analgesia administration.12 Moreover, a review of retrospective trials highlights a use rate of epidural analgesia < 20% due to practical challenges such as anesthetist availability and patient cooperation.14
The ideal protocol for a safe and effective analgesic modality for rib fracture patients remains elusive. Currently, guidelines for pain management do not include IV lidocaine infusions, despite literature supporting its use in thoracic surgery patients.15-17 While IV lidocaine has not been extensively studied in trauma patients, a meta-analysis demonstrated its efficacy in reducing pain scores and the length
Population Health Research Capsule
What do we already know about this issue? Rib fractures cause significant pain and complications. IV lidocaine has a wellestablished safety profile, but its use for rib fracture pain is not widespread.
What was the research question?
What are Canadian trauma centres’ current analgesic practices and attitudes toward IV lidocaine for rib fracture pain?
What was the major finding of the study?
33% of trauma centres use IV lidocaine for rib fractures, and 83% support further research on its potential efficacy.
How does this improve population health?
This study highlights the potential of IV lidocaine for rib fracture pain. Supporting research could standardize management and reduce pain-induced complications.
of hospital stays after surgery in other patient populations.18 Furthermore, previous investigations showed that IV lidocaine might be the best alternative when epidurals are contraindicated, refused, unavailable or ineffectual. Compared to epidurals, IV lidocaine demonstrates no difference in subsequent pain intensity or postoperative complications.19,20 Most notably, a single-centre, randomized controlled trial has demonstrated the potential of lidocaine as a beneficial analgesic for patients with rib fracture.8 The study used the general IV dosing of 1-4 milligrams per kilogram (mg/kg) as a bolus, followed by 1-4 mg/kg/hour as an infusion.8
Systemic administration of IV lidocaine offers advantages over local infiltration of lidocaine in addressing broader pain pathways from rib fractures injuries. Rib fractures induce pain that can radiate from the site of fracture to surrounding muscles and dermatomes, exacerbating patient morbidity and mortality, especially during movement.8 Systemic lidocaine infusions have been shown to improve pain management by their anti-hyperalgesic properties.21,22 By contrast, IV lidocaine exerts its pharmacological action through sodium channel blockade in neural tissues. Studies also suggest systemic lidocaine may reduce or prevent the proliferation of sodium channels, thus interrupting neuronal transmission, particularly in traumatized tissues. 21,23 Additionally, studies have shown that IV lidocaine can decrease systemic inflammatory markers, demonstrating significant anti-inflammatory properties.24
Given these effects, combined with our understanding of rib fracture-associated mortality related to pain,2,5-7 as well as evidence supporting the effectiveness of IV lidocaine in thoracic surgery,15-17 we sought to investigate the use of IV lidocaine to blunt pain perception and reduce pain-induced, rib fracture complications as suggested by related studies.8,19,20
We surveyed current the medical directors of Canadian trauma centres regarding their current practices and experiences with rib fracture pain management, including their familiarity with and use of IV lidocaine infusions in Canadian trauma patients. Secondary outcomes of the study included a measure of the most common analgesic protocols for thoracic traumas and of those centres’ willingness to participate in future research.
METHODS
We developed an online survey for electronic distribution across 14 major Canadian trauma centres using REDCap (Research Electronic Data Capture) software hosted by the Lawson Research Institute. REDCap is an encrypted online application used to collect research data. We developed a 31item descriptive survey with an expected completion time of < 25 minutes, which was distributed to a convenience sample of the medical directors of 14 major Canadian trauma centres. Each respondent was given a unique, single-use link and was required to enter the name of the trauma centre they were representing to ensure no duplicated responses. There were no additional inclusion or exclusion criteria.
The survey was designed to address four major themes: trauma centre characteristics and demographics; current or preferred pain management protocol strategies; current use of IV lidocaine infusion in trauma patients, including rib fracture patients; and the medical directors’ opinions regarding the importance of IV lidocaine in trauma patient research and interest in participating in a multi-centre randomized controlled trial to examine the effectiveness of IV lidocaine infusions. Study questions were posed as a variety of multiple-choice questions, including Likert scale, rating-scale, ratio-scale and dichotomous responses, and situation-based questions. Situation-based questions included descriptive opportunities to allow elaboration, where appropriate, using free-form text boxes.
Completed response data was recorded using REDCap software. The collected data was only made available to members of the research team. Following data collection, responses were aggregated before analysis. The team collectively performed a narrative synthesis of the frequencies, patterns, variation, and consensus across treatment centres and conducted a thematic analysis of the descriptive answers to determine similarities and differences from the general trend. The study was unblinded to compare inter-provincial practice variation.
The survey was distributed in February 2023 through email to the trauma centre medical directors, or their delegates, of the following academic hospitals located
across five Canadian provinces: British Columbia (Royal Columbian Hospital, Vancouver General Hospital, Victoria General Hospital); Alberta (University of Alberta Hospital, Foothills Medical Centre); Saskatchewan (Royal University Hospital, Regina General Hospital); Ontario (Hamilton Health Sciences, London Health Sciences Centre, and The Ottawa Hospital, Kingston Health Sciences Centre, Sunnybrook Health Sciences Centre, St. Michael’s Hospital); and Nova Scotia (Halifax Health). A reminder email was sent three weeks after the initial contact to encourage survey completion.
RESULTS
Site Characterization
The survey was completed by 12 of 14 (85%) medical directors of Canadian trauma centres. Survey responses regarding trauma centre characteristics and demographic information are presented in Table 1. When surveyed, six (50%) of the responding centres reported > 450 severe trauma admissions annually (Table 1).
Table 1. Characteristics of 12 Canadian trauma centres.
Characteristic
(N = 12)
Dedicated trauma team to assess emergency department patients? Yes
Dedicated trauma service for admitted multi-system trauma patients?
of trauma patients
Available Trauma Clinic for follow-up? Yes
(16)
Note: Severe trauma admissions include patients admitted via trauma team activation. ISS, Injury Severity Score.
Pain Management
Six (50%) of the responding trauma centre directors described having an analgesic protocol for traumatic rib fracture patients (Table 2). Four (33%) of those centres uploaded a copy of their protocol. (See Appendix, Figure 1 and Figure 2 for protocol samples). The remaining two (16%) trauma centre directors who answered “yes” to having a protocol described their pain management protocol for traumatic rib fracture patients in the survey’s free-form text box . Most centres with protocols determine risk stratification using the rib fracture score and initiate multimodal analgesia, with escalation to acute pain service consultation for consideration of other analgesic modalities.
Table 2. Categorical pain management characteristics for traumatic rib fracture patients
Characteristic
Presence of traumatic rib fracture analgesic protocol?
Yes
Regarding the use of IV lidocaine for patients with traumatic rib fracture, 4/12 (33%) medical directors reported frequent use; 2/12 (16%) reported occasional use; 2/12 (16%) reported rare use; and 4/12 (33%) reported never using IV lidocaine (Figure 2). When asked how often IV lidocaine infusions are used in patients with ≥ 2 rib fractures, 3/12 (25%) reported frequent use. However, when asked how often IV lidocaine infusions were used in traumatic rib-fracture patients with flail chest, 5/12 (41%) centres responded that they frequently use IV lidocaine (Figure 2).
None of the surveyed trauma centres use IV lidocaine for first-line management. When asked under what circumstances IV lidocaine is used, medical directors provided the following responses: ‘routinely but not first line’, 5/12 (41%); and ‘infrequently’, 5/12 (41%). Two (16%) centres did not answer the question.
Future Study
6 (50) No
Pain management administrator for traumatic rib fracture patients
Trauma Team
Acute Pain Service
Admitting service
6 (50)
7 (58)
4 (33)
1 (8)
The medical directors of six trauma centres (50%) without an analgesic protocol for traumatic rib fracture patients ranked the centre’s preference for pain management strategies from a list. All respondents without a protocol reported using NSAIDs, acetaminophen, and systemic opioids in their pain management strategies for rib fractures; specifically, all respondents ranked ‘NSAIDS and acetaminophen’ as their first-choice option. The majority then ranked ‘systemic opioids’ as their second-choice option; only one respondent ranked it as their third choice (Figure 1).
Medical directors of trauma centres with a protocol were not asked to rank their preference for pain management strategies. However, consistent with the ranked preferences, all 12 (100%) surveyed centres use NSAIDs and acetaminophen as first-line management. In most centres (7/12; 58%), the trauma team is responsible for pain management in patients with traumatic rib fractures (Table 2).
Intravenous Lidocaine Infusions
When asked whether the centre could run an IV lidocaine infusion in trauma patients, medical directors provided the following responses: ‘Yes’, 6/12 (50%); ‘Yes, but limited to certain clinical areas’, 3/12 (25%); and ‘No’, 3/12 (25%).
Table 3 outlines Canadian trauma centre responses to dichotomous questions surrounding pain management for traumatic rib fractures, the need for future research, and willingness to participate in a future study. Most (10/12; 83%) respondents reported agreeing that further research regarding IV lidocaine infusions for pain management is needed and are interested in being part of a multi-centre randomized controlled trial examining the effectiveness of IV lidocaine infusions in patients with traumatic rib fracture (Table 3).
DISCUSSION
Our survey demonstrated that all responding trauma centres currently use NSAIDs and acetaminophen as first-line management for traumatic rib fractures. This is consistent with current practice patterns described in the literature.11 Several other trauma centre directors cited acetaminophen as the firstline therapy for traumatic rib fracture patients due to its painrelieving and opioid-sparing effects.25 Furthermore, the survey identified a lack of protocols as well as variations in existing analgesic protocols. Uploaded protocols reveal the use of different risk-stratification scores and procedural steps, further suggesting the absence of an optimal protocol. This lack of an optimal protocol and variation in protocols is expected, given the challenges of current analgesic modalities and their potential to exacerbate rib fracture complications.11,12
Importantly, our data also highlight the practices of Canadian trauma centres in their administration of IV lidocaine. Most surveyed centres demonstrated the ability to run IV lidocaine infusions in trauma patients and in patients with traumatic rib fractures, underscoring the applicability and generalizability of this analgesic modality for the Canadian trauma population. In fact, 8 of 12 (66%) respondents reported using IV lidocaine infusions for rib fracture treatment. Consideration of IV lidocaine infusion can also be found in the protocols provided in the Appendix, promoting the potential relevance of lidocaine as mainstay practice.
Multiple meta-analyses have emphasized lidocaine’s effect on lowering opiate requirements and improving recovery indices
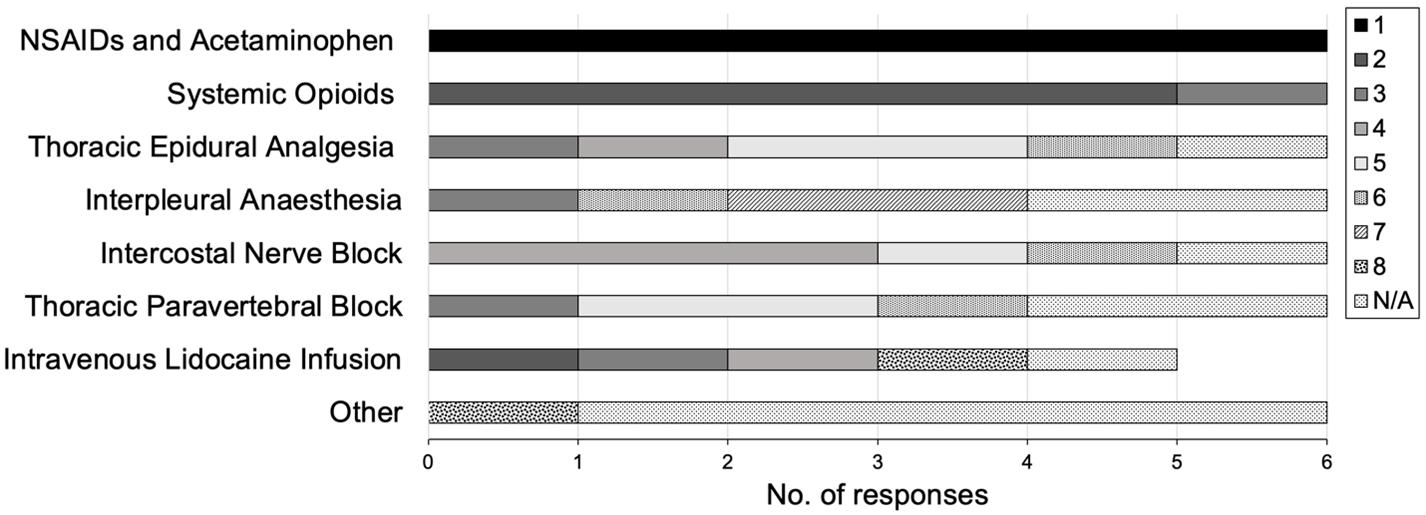
Figure 1. Rib fracture pain management in Canadian trauma centres without a protocol. Data represents the ranking preference of pain management strategies based on surveyed rating scale responses (N = 6; 50%), with 1 indicating the highest preference. NSAIDs, non-steroidal anti-inflammatory drugs; N/A, treatment strategies that were not used at the trauma centre were not ranked; Other, 1 centre reported using ketamine.
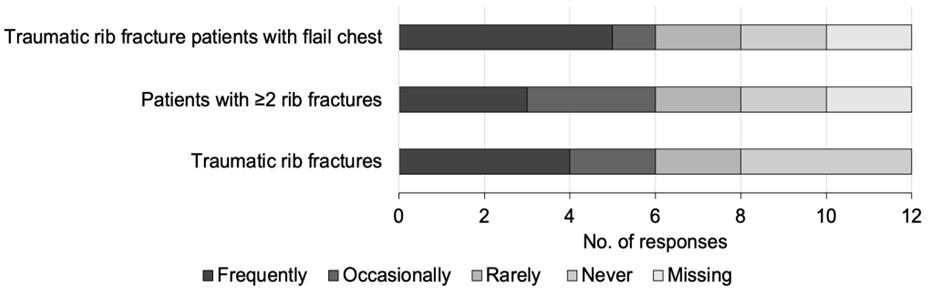
Figure 2. Current use of intravenous (IV) lidocaine infusions in Canadian trauma centres. Data shown represents centres’ Likert scale responses addressing the frequency of IV lidocaine use in rib fracture patients (N = 12). Missing, centres that did not answer.
following abdominal surgery.22,26,27 Nearly half the centres (41%) revealed frequent use of IV lidocaine in the escalation of traumatic rib fracture patients with flail chest, suggesting it may be beneficial in conditions deemed high risk for rib fracture complications, including compromised respiratory function. Previous literature suggests that an effective analgesic can reduce rib fracture-associated mortality.28 Altogether, if the efficacy of IV lidocaine observed in thoracic surgery patients can be demonstrated in traumatic rib fracture patients, it can safely improve their pain control and complication risks.
Half (50%) of the respondents expressed dissatisfaction with the level of analgesia currently provided, and most (83%) respondents agreed that further research is needed in Canadian trauma patients regarding the use of IV lidocaine infusions for pain management.
In 2022, a single-centre, double-blind, randomized
controlled trial evaluated the analgesic efficacy of a 72- to 96-hour IV lidocaine infusion. Pain scores were improved, patient satisfaction was higher, and morphine equivalent use was lower in the lidocaine group compared to the placebo group. However, these results did not reach statistical significance.8 Despite this, the observed beneficial trends of the study, combined with the results of our survey-based study and respondents’ support, a multi-centre trial evaluating the analgesic efficacy and safety of IV lidocaine infusions for rib fracture pain management is now warranted.
LIMITATIONS
The survey-based nature of this work is subject to several potential biases, including sampling bias, question-order bias, demand bias, non-response bias, response bias, and
Table 3. Canadian trauma centres’ interest in future studies on use of intravenous lidocaine for rib fracture pain.
Canadian-specific trauma research is important to develop, since much of the current trauma literature is derived from American trauma centres that serve very different populations with different injury patterns than we do in Canada.
Aggressive pain management is important in patients with traumatic rib fractures.
Satisfied with the level of analgesia currently provided to your trauma patients with severe thoracic trauma / multiple rib fractures.
Further research is needed in Canadian trauma patients regarding the use of IV lidocaine infusions for pain management.
In patients with traumatic rib fractures, randomizing to IV lidocaine infusion versus usual care is ethically justified.
Interest in being part of a multi-centre randomized controlled trial examining the effectiveness of IV lidocaine infusions in traumatic rib fracture patients.
IV, intravenous.
confirmation bias. The survey was completed by the medical director of each major Canadian trauma centre to represent the practice of the trauma centre and its trauma practitioners. While they were reminded to answer survey questions based on their centre’s common practice, personal biases and prior knowledge may have impacted responses regarding the centre’s standard practice. Additionally, participants were informed and given study questions that addressed the variation in practices regarding differences in trauma centre characteristics, pain management in the setting of trauma, and the role of IV lidocaine. The theme of questions, question options and increasing the role of IV lidocaine in treatment of rib fracture pain may elicit more extreme responses that support or oppose its use. Finally, the survey was also not piloted prior to distribution, potentially affecting the clarity of certain questions and resulting in misinterpretations or inaccuracies in the responses. Nonetheless, previous investigations and a randomized controlled trial support IV lidocaine as a beneficial analgesic for patients with rib fracture despite its varied use and potentially biased support.8,19,20
CONCLUSION
Traumatic rib fracture-management practices across Canadian trauma centres are variable. There was majority agreement among respondents in our study that further research on IV lidocaine for pain control in traumatic rib fractures is needed. Survey respondents also expressed interest in participating in a multicentre randomized controlled trial examining the effectiveness of IV lidocaine infusions in these patients.
Address for Correspondence: Sammie Yu, BMSc, London Health Sciences Centre, Victoria Hospital, 800 Commissioners Road East, London, Ontario, Canada N6A 5W9. Email: sammie.yu@ mailutronto.ca.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Yu et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Mayberry JC, Trunkey DD. The fractured rib in chest wall trauma. Chest Surg Clin N Am. 1997;7:239-61.
2. Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975-9.
3. Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478-85.
4. Holcomb JB, McMullin NR, Kozar RA, et al. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549-55.
5. Linton DM, Potgieter PD. Conservative management of blunt chest trauma. S Afr Med J. 1982;61:917-9.
6. Pattinson KTS. Opioids and the control of respiration. British J of Anaesthesia. 2008;100:747-58.
7. Carrier FM, Turgeon AF, Nicole PC, et al. Effect of epidural analgesia in patients with traumatic rib fractures: a systematic review and metaanalysis of randomized controlled trials. Can J Anesth. 2009;56:230-42.
8. Patton P, Vogt K, Priestap F, et al. Intravenous lidocaine for the management of traumatic rib fractures: a double-blind randomized controlled trial (INITIATE program of research). J Trauma Acute Care Surg. 2022;93:496-502.
9. Wu CL, Jani N, Perkins F, et al. Thoracic epidural analgesia versus intravenous patient-controlled analgesia for the treatment of rib fracture pain after motor vehicle crash. J Trauma-Injury Infection Crit Care. 1999;47:564-7.
10. Sirmali M, Turut H, Topcu S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eu J of Cardio-Thoracic Surgery. 2003;24:133-8.
11. Karmakar MK, Ho AMH. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615-25.
12. Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59:1256-67.
13. Bulger EM, Edward T, Klotz P, et al. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136:426-30.
14. Arendt K, Segal S. Why epidurals do not always work. Rev Obstet Gynecol. 2008;1:49-55.
15. Cherny N, Ripamonti C, Pereira J, et al. Strategies to manage the adverse effects of oral morphine: an evidence-based report. J Clin Onc. 2001;19:2542-54.
16. Nguyen M, Vandenbroucke F, Roy JD, et al. Evaluation of the addition of bupivacaine to intrathecal morphine and fentanyl for postoperative pain management in laparoscopic liver resection. Reg Anesth Pain Med. 2010;35:261-6.
17. Daykin H. The efficacy and safety of intravenous lidocaine for analgesia in the older adult: a literature review. Br J Pain. 2017;11:23-31.
18. Marret E, Rolin M, Beaussier M, et al. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J
Surg. 2008;95:1331-38.
19. Kaba A, Laurent SR, Detroz BJ, et al. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy Anesthesiology. 2007;106:11-8.
20. Wongyingsinn M, Baldini G, Charlebois P, et al. Intravenous lidocaine versus thoracic epidural analgesia: a randomized controlled trial in patients undergoing laparoscopic colorectal surgery using an enhanced recovery program. Reg Anesth Pain Med. 2011;36:241-8.
21. Koppert W, Weigand M, Neumann F, et al. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004;98:1050-55.
22. Sun Y, Li T, Wang N, et al. Perioperative systemic lidocaine for postoperative analgesia and recovery after abdominal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2012;55:1183-94.
23. Olschewski A, Hempelmann G, Vogel W, et al. Blockade of Na+ and K+ currents by local anesthetics in the dorsal horn neurons of the spinal cord. Anesthesiology. 1998;88:172-9.
24. Kuo CP, Jao SW, Chen KM, et al. Comparison of the effects of thoracic epidural analgesia and IV infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006;97:640-6.
25. Paydar S, Farhadi P, Ghaffarpasand F, et al. Acute trauma pain control algorithm. Bull Emerg Trauma. 2014;2:170-1.
26. Hollmann MW, Durieux ME. Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology. 2000;93:858-75.
27. Ventham NT, Kennedy ED, Brady RR, et al. Efficacy of intravenous lidocaine for postoperative analgesia following laparoscopic surgery: a meta-analysis. World J Surg. 2015;39:2220-34.
28. Mackersie RC, Karagianes TG, Hoyt DB, et al. Prospective evaluation of epidural and intravenous administration of fentanyl for pain control and restoration of ventilatory function following multiple rib fractures. J Trauma. 1991;31:443-9.
Intubating Stylets in the Emergency Department: A Video Review of First-pass Success and Time
Raymond Che, DO, RRT*
Niaman Nazir, MD, MPH†
Ali Badar, DO, MBA*
Anchitha Honnur, BA‡
Mark Newton, MD*
Abdel-Rahman Mohammed Samour, BA§
Tala Samour, MD||
Dane Clutter, BS, BA**
Andrew Pirotte, MD*
Section Editor: Dell Simmons, MD
University of Kansas Health System and University of Kansas Medical Center, Department of Emergency Medicine, Kansas City, Kansas University of Kansas Health System and University of Kansas Medical Center, Department of Population Health, Kansas City, Kansas University of Kansas School of Medicine, Kansas City, Kansas University of Kansas, Lawrence, Kansas
Al-Balqa Applied University, Faculty of Medicine, Salt, Jordan Kansas City University College of Osteopathic Medicine, Kansas City, Missouri
Submission history: Submitted April 10, 2025; Revision received July 7, 2025; Accepted July 10, 2025
Electronically published October 4, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.47204
Introduction: Effective airway management is critical for optimal patient outcomes in the emergency department (ED). Additionally, airway management is significantly influenced by the clinician’s selection of equipment, specifically the choice of intubating stylet. Also of note, the duration of intubation (time to intubate) impacts overall success. The choice of intubation device may influence first-pass success and intubation times. In this study we evaluated equipment trends for first-pass success and intubation duration. We collected data by reviewing a video database of recorded airways. Three commonly used intubating stylets were reviewed: the hyperangulated stylet; bougie (Eschmann stylet); and malleable stylet.
Methods: In this retrospective observational study, we reviewed 615 intubation videos. These videos were recorded via video laryngoscopy at the University of Kansas Medical Center and The University of Kansas Health System between February 2019–January 2022. We recorded device type, number of intubation attempts, and time to successful intubation (time from entry of laryngoscope blade to passage of endotracheal tube through vocal cords). We included and analyzed 575 intubations for first-pass success, while a random subset of 70 intubations was used to evaluate intubation times. We also conducted a survey to query current faculty and resident physicians regarding their preference for intubation modality.
Results: Among 575 intubations, the bougie (Eschmann stylet) was used in 47.1% of cases, the malleable stylet in 27.3%, and the hyperangulated (also known as “rigid” or “angular”) stylet in 25.6%. Overall firstpass success was 91.3%. The malleable stylet showed the highest success rate (94.9%), followed by the hyperangulated stylet (93.2%), and the bougie (88.2%) (χ² = 6.53, P = .04). In a separate analysis of 70 cases, the median intubation time was 35.5 seconds. For intubation time, we found a significant difference between the three modalities (χ² = 8.2019, P = .02), with pairwise differences between bougie vs malleable stylet (P = .01) and bougie vs hyperangulated stylet (P = .02), but not between hyperangulated and malleable stylets (P = .62). Bougie-assisted intubations had the highest median time of 40.5 seconds (mean 49.15 +/- 23.1) compared to malleable stylet 31 seconds (mean 33.8 +/- 16.4) and hyperangulated 31 seconds (mean 33.6 +/- 11). A survey of 52 physicians showed that 55.8% preferred the malleable stylet, 19.2% preferred the hyperangulated stylet, and 25% preferred the bougie.
Conclusion: The malleable stylet demonstrated the highest first-pass success rate and the most consistent intubation times, while the bougie had the longest times and lowest success rate in our ED. Physician preferences also favored the malleable stylet. First-pass success rates and intubation times vary depending on an institution’s familiarity with specific devices and the clinician’s preference. These factors should be considered when selecting intubation equipment to optimize airway management outcomes or facilitate training. [West J Emerg Med. 2025;26(5)1374–1379.]
INTRODUCTION
Effective and efficient emergency airway management is a keystone of success in the care of critically ill patients in the emergency department (ED). First-pass success during intubation is a meaningful metric in the ED, where rapid and effective airway management is essential. Each additional intubation attempt (after the first attempt) increases the risk of adverse events, including witnessed aspiration, oxygen desaturation, esophageal intubation, hypotension, dysrhythmia, and cardiac arrest.1 First-pass success rates vary based on several factors including the clinician’s experience,2-3 patient characteristics such as restricted neck extension or mouth opening,3 or choice of airway device.4
Commonly used devices to facilitate endotracheal intubation include the following:
1. Malleable stylet: a semi-flexible, plastic-coated metal device used to give shape to an endotracheal tube
2. Bougie (Eschmann stylet): a narrow, soft plastic introducer placed into the trachea first, over which the endotracheal tube is advanced
3. Hyperangulated (or rigid) stylet: a rigid metal introducer that maintains its fixed shape throughout the intubation process
Of note, recent expert recommendations suggest routine use of the bougie over the malleable stylet, while the rigid stylet is preferred when hyperangulated laryngoscope blades are used.5
Several studies have compared the effectiveness of different airway introducers across various clinical settings. These studies have served to evaluate first-pass success rates, with variable results. Several articles reported a significant increase in first-pass success with the use of a bougie.4,6-9 On the other hand, there have also been reports of no statistically significant difference between bougie and malleable stylets.10-12 Additionally, studies evaluating the difference in first-pass success when using a malleable stylet vs a hyperangulated stylet have had varying results.13-14 Notably, two prior observational studies assessing airway introducers were conducted in the prehospital setting, limiting their generalizability to ED intubations.7-9 In this study we aimed to leverage the University of Kansas Medical Center and The University of Kansas Health System airway video database (AVD) to contribute to the existing literature. By evaluating trends in first-pass success rates across all three devices, this study provides a real-world dataset of video-recorded intubations conducted in the ED.
METHODS
Design, Setting, and Population
This was a retrospective observational study conducted at the University of Kansas Medical Center and The University of Kansas Health System Emergency Department, an academic, tertiary-care facility and Level I trauma center with approximately 85,000 visits annually. We analyzed 615 videorecorded intubations collected between February 6, 2019–
Population Health Research Capsule
What do we already know about this issue?
Emerging data supports the bougie as superior for first-pass success, with expert consensus recommending it as a first-line device in endotracheal intubation.
What was the research question?
Which intubating stylet used in our ED is associated with the highest first-pass success rate?
What was the major finding of the study?
Malleable stylet had the greatest first-pass success rate (94.9%, CI .92-.98) vs bougie (88.2%, CI .84-.92), P = .04.
How does this improve population health?
Optimizing stylet choice improves first-pass success and reduces complications, enhancing airway outcomes and care quality in ED patients.
January 18, 2022, from the AVD. The primary objective was to evaluate intubation success rates for each device type and the duration of intubation attempts. A secondary objective was to assess physician device preferences via a survey.
Data Source: Airway Video Database (AVD)
The AVD is an independent, pre-existing, and ongoing collection of video laryngoscopies captured using GlideScope (Verathon, Inc, Bothell, WA) and C-MAC (Karl Storz SE & Co. KG, Tuttlingen, Germany) devices. It serves as a free, openaccess educational resource designed for airway education. We have no conflict of interest regarding the devices used. All patient identifying information, such as demographics, medical history, procedural circumstances, and performing clinician details, are removed to ensure confidentiality. The videos have no link to the electronic health record and cannot be traced to the patient. For organizational and repeatability purposes, each video is assigned a unique, arbitrary identifier composed of a patient age and a chief complaint.
Inclusion and Exclusion Criteria
We analyzed all recorded attempted intubations available in the AVD during the study period. Videos were excluded if data were missing, if the intubation involved multiple attempts using different devices, or if the intubation was a bimodal airway (e.g., bronchoscopy assisted). For intubation

duration, we excluded any video that contained multiple attempts or had unclear visualization of the beginning or end of the intubation process. However, during data abstraction of intubation duration, no selected videos met exclusion due to poor visualization.
Abstractor Training and Blinding
One trained abstractor manually reviewed all videos and compiled data into a standardized spreadsheet. Before data collection began, the abstractor was oriented to the AVD interface and trained on how to enter data consistently. For the time-interval measurements, additional abstractors assisted in reviewing a subset of intubations, although most reviews were performed by a single individual. All reviewers were trained to identify the procedural start and end points, defined as the insertion of the laryngoscope blade and the passage of the endotracheal tube through the vocal cords, using embedded video timestamps. Abstractors were not blinded to the study’s objectives; however, the original spreadsheet used for data abstraction had been created prior to the study’s conception and remained unchanged to minimize bias.
Data Abstraction and Collection
Each video was assigned a unique numerical identifier from 1 to 615. Data were manually abstracted into a standardized spreadsheet, including the intubation device used and the number of attempts. For time-based analysis, we randomly selected 70 intubations using a computer-generated number list. If a selected video met exclusion criteria, a new random video was chosen. Duration was defined as the time in seconds from insertion of the laryngoscope blade to passage of the endotracheal tube through the vocal cords, determined using timestamps within the video.
Survey on Device Preference
To assess preferred intubation methods, we conducted a survey of emergency department faculty and residents. The survey included questions about device preferences. A total of 52 of 77 invited participants (67.5%) completed the survey. Participation was voluntary, and responses were anonymous.
Ethical Considerations
As this study involved a secondary retrospective analysis of de-identified video data, it was reviewed and deemed to be exempt by our institutional review board (IRB).
We adhered to the criteria set forth by Worster et al15 as follows: 1) Abstractors were trained in navigating and using the AVD; 2) inclusion and exclusion criteria were clearly defined; 3) study variables were defined; 4) data were collected using standardized spreadsheets; 5) abstractor performance was periodically reviewed by the principal investigator to ensure consistency and accuracy within data entries; 6) abstractors were not blinded to the study objectives, although the original data abstraction spreadsheet was created prior to study conception; (7) interobserver reliability is addressed in the limitations section; (8) formal interobserver reliability testing was not conducted due to the small number of abstractors and the fact that a single abstractor completed the majority, if not the entirety, of each dataset; 9) the AVD data source was thoroughly described; 10) the sampling method was clearly outlined; 11) any video missing predefined variables were removed; and 12) the study was reviewed by the IRB.
Statistical Analysis
We performed data management and statistical analyses using SAS software v9.4 (SAS Institute Inc., Cary, NC). We summarized categorical variables with percentages, and continuous variables by means and medians. The chi-square test was used to make global comparisons of categorical variables across the three device types. As the time data were skewed, we used a non-parametric Kruskal-Wallis test to make global comparisons of time across the three device types. Similarly, pairwise comparisons of time across devices were made using the Wilcoxon two-sample test. Two-sided P-values < .05 were considered statistically significant.
RESULTS
We analyzed 615 intubations. Twenty-five cases (4.0%) either had missing data or were excluded as multiple modalities had been used in addition to multiple attempts. Another 15 (2.4%) cases that used a bimodal technique (laryngoscope plus bronchoscope on split screen) were excluded. Among the 575 intubations included in this study, the bougie was the most frequently used device, accounting for 271 (47.13%) cases. The malleable stylet was used in 157 (27.30%) intubations, and the hyperangulated stylet in 147 (25.57%). The bougie was selected nearly twice as often as the hyperangulated or malleable stylet.
Figure 1. Quick response link to University of Kansas Medical Center airway video database, which was used to evaluate intubation success rates.
Table 1. This table displays the success rates of first-pass intubation attempts stratified by the type of stylet used. For each device type, the number and percentage of successful first attempts and those requiring multiple attempts are shown with 95% CIs and the total number and proportion of intubations performed using each device. Notably, the malleable stylet had the highest first-pass success rate (94.9%), while the bougie had the lowest (88.2%). A chi-square test was used to assess differences in success rates among devices.
First-pass Success by Device Type
Stylet Type
Hyperangulated
(88.2%)
χ²=6.53, P = .04.
Among 575 intubations analyzed, first-pass success rates varied by stylet type (χ² = 6.53, P = .04). The malleable stylet had the highest first-pass success rate (94.9%), followed by the hyperangulated stylet (93.2%) and the bougie (88.2%). The bougie was associated with the highest proportion of multiple attempts (11.8%), compared to 6.8% for the hyperangulated stylet and 5.1% for the malleable stylet. The overall total firstpass success rate was 91.3%
We selected 70 samples at random from the database, and the time of intubation was manually measured. Five cases had multiple attempts. These were excluded and replaced with another randomly generated case for the airway from the cases included in the airway database for a total sample size of 70. The median intubation time of the sample was 35.5 seconds.
Bougie-assisted intubations show the longest median time of 40.5 seconds (mean 49.15 +/- 23.1) and highest variability, with a maximum time of 93 seconds. Intubation time with the malleable stylet was 31 seconds (mean 33.8
+/- 16.4), and hyperangulated was 31 seconds (mean 33.6 +/- 11). Comparison of the distribution of intubation time intervals between all three modalities revealed a statistically significant difference between these groups (χ² = 8.2019, P = .02). The pairwise comparisons of intubation time between devices demonstrated a statistically significant difference between bougie vs malleable stylet (P = .01) and bougie vs hyperangulated stylet (P = .02). However, there was not a statistically significant difference between hyperangulated stylet vs malleable stylet (P = .62).
Survey of Clinician Preferences
To further explain such differences, we conducted a survey that sampled 77 total attending physicians, fellow physicians, and resident physicians regarding their preference for intubation modalities. This cohort consisted of most of the physicians composing the sample dataset. A total of 52 results were collected from the 77 who were surveyed. Results
χ²=8.2019, P = .02.
Table 2. Intubation time intervals for three device types: hyperangulated, bougie, and malleable. Time intervals were recorded for a subset of 70 intubations. For each device, the table shows the number of cases, percentage of total, minimum, median, mean, SD, maximum duration, and interquartile range (in seconds) required to complete intubation. We also report 95% CIs for median times tested. Ranked sum tests were used to compare time distributions across devices. The bougie group had the highest median and maximum times, while the malleable group had the shortest minimum time. Min, minimum; Max, maximum; IQR, interquartile range.
Intubating Stylets in ED: A Video Review of First-pass Success and Time
showed that 55.8% of responders preferred the malleable (gray) stylet, 19.2% the hyperangulated stylet, and 25% the bougie (Eschmann stylet).
DISCUSSION
There is conflicting research regarding the effect of stylet modalities on successful intubations.4,6-12 Some of this research focused on non-hospital settings, which limited reproducibility in ED intubations. This highlights the need for further analysis of intubation modalities in the ED setting. In this study we used AVD of the University of Kansas Medical Center and The University of Kansas Health System to stratify the effectiveness of stylet modalities through real-world emergent intubations.
At our institution, the bougie (Eschmann stylet) was the most commonly used stylet modality during endotracheal intubation. Despite this finding, our results indicate that the malleable stylet was associated with the highest rate of firstpass success, followed by the hyperangulated stylet. Both modalities outperformed the bougie, which demonstrated statistically significantly lower rates of first-pass success. The malleable and hyperangulated stylets achieved the fastest successful intubation times, with similar results, while the bougie required the longest time for successful intubation.
There has been previous expert recommendation for the routine use of a bougie which is supported by evidence of superior first-pass success in a variety of clinical scenarios.4-9 In this study we present a possible advantage of the malleable stylet over the bougie stylet in both first-pass success and intubation time. Institution-specific training, experience, familiarity with a device, and preference may contribute to higher first-pass success rates and reduced intubation times. It is important to acknowledge that many other variables may affect both intubation success and timing. For instance, laryngoscope selection may have an equal (or even greater) impact on stylet choice (e.g., in a cardiac arrest patient, the hyperangulated blade may be selected). This selection typically necessitates the use of the rigid/hyperangulated stylet and precludes selection of malleable stylet or bougie, as these stylets are not well suited for the geometry of a hyperangulated blade. In such cases, the laryngoscope dictates the intubating adjunct, rather than the stylet being chosen independently. This relationship suggests that device selection and clinical context may significantly influence intubation outcomes. Therefore, it may be important to consider not only the stylet itself but the broader clinical context when interpreting first-pass success and intubation time. We were unable to fully account for the interplay between laryngoscope and stylet selection or the clinical context in which each device is used, which represents an interesting and promising avenue for future research.
We found notable discrepancies when correlating data regarding clinician preferences (via the survey) and trends seen in the AVD. While the survey data showed that the
malleable stylet was the most preferred device, a review of the AVD showed that the bougie was the most employed device. This mismatch may reflect an institutional effort to promote bougie use in response to emerging literature supporting its effectiveness. However, the survey results suggest that clinicians may still feel less comfortable or experienced with bougie-assisted intubation. Despite this variance, the data do align with the malleable stylet as the most effective intubation modality in this ED.
LIMITATIONS
This study has several limitations. Because the AVD is de-identified for privacy concerns, the age, sex, presenting complaint, or comorbidities of the patient could not be correlated to the intubation. And given the single-center design of this study, the generalizability and external validity of the findings may be limited. Additionally, we did not formally address interobserver variability among the abstractors measuring intubation duration. While all abstractors used the same operational definitions for procedural start and end points, subtle differences in interpretation may have introduced variability, potentially affecting the precision of duration estimates. Furthermore, abstractors for the intubation duration dataset were not blinded to the study objectives, which could have introduced bias, particularly in the interpretation of time-based outcomes. However, the original abstraction spreadsheet had been created prior to the study’s conception and remained unchanged, which may have helped mitigate this bias.
These results may also have been biased by clinician preference for intubation modalities. For example, although the bougie stylet was the most common form of stylet used in the AVD, this was not the subjectively preferred method of intubation based on the physician survey. Another confounding variable was the motivation behind equipment selection, which could not be fully assessed due to the deidentified nature of the database. For example, a bougie may be selected for anticipated difficult airways. This would mean the difficulty of the airway itself, rather than the modality, could influence success rates and could be a potential direction for future research. User familiarity and experience level may also impact outcomes. Although our study favored the malleable stylet, there were numerous examples in the AVD where the bougie achieved rapid first-pass success or was used effectively as a rescue device when the initial modality had failed. Thus, these findings should be interpreted cautiously.
We analyzed intubation time intervals using a random subset of the original samples that were used to assess firstpass success by modality. Without a complete analysis of the entire database, the selected sample may not fully represent the overall trends. Time intervals were manually recorded by human reviewers, which introduced the potential of interobserver variability and potential timing inconsistencies, particularly when identifying precise start and end points
of the intubation process. As a result, the conclusions regarding intubation time may be limited, and the overall generalizability may be constrained. Finally, although most intubations were performed by emergency medicine residents or attendings, a small proportion may have been completed by off-service residents or learners under supervision. These cases were not explicitly identified, which may have introduced a minor degree of uncertainty regarding operator background.
CONCLUSION
The malleable stylet demonstrated the highest first-pass success rate and the most consistent intubation times, while the bougie had the longest times and lowest success rate in our ED. Physician preferences also favored the malleable stylet. First-pass success rates and intubation times vary depending on an institution’s familiarity with specific devices and clinician preferences. These factors should be considered when selecting intubation equipment to optimize airway management outcomes or facilitate training.
Address for Correspondence: Raymond Che, DO, University of Kansas Medical Center, Department of Emergency Medicine, 3901 Rainbow Blvd, Kansas City, Kansas 66160. Email: rche@ kumc.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Che et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Sakles JC, Chiu S, Mosier J, et al. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20(1):71-78.
2. Goto T, Oka S, Okamoto H, et al. Association of number of physician postgraduate years with patient intubation outcomes in the emergency department. JAMA Netw Open. 2022;5(4):p. e226622.
3. Jung W, Kim J. Factors associated with first-pass success of emergency endotracheal intubation. Am J Emerg Med. 2020;38(1):109-113.
4. von Hellmann R, Fuhr N, Ward A Maia I, et al. Effect of bougie use on first-attempt success in tracheal intubations: a systematic review and meta-analysis. Ann Emerg Med. 2024;83(2):132-144.
5. Mosier JM, Sakles JC, Law JA, et al. Tracheal intubation in the critically ill. Where we came from and where we should go. Am J Respir Crit Care Med. 2020;201(7):775-788.
6. Tollman J, Zubair A. Efficacy of tracheal tube introducers and stylets for endotracheal intubation in the prehospital setting: a systematic review and meta-analysis. Eur J Trauma Emerg Surg, 2021;48(3):1723–35.
7. Latimer AJ, Harrington B, Counts CR, et al. Routine use of a bougie improves first-attempt intubation success in the out-of-hospital setting. Ann Emerg Med. 2021;77(3):296-304.
8. Driver BE, Prekker ME, Klein LR, et al. Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation. JAMA. 2018;319(21):2179.
9. Ångerman S, Kirves H, Nurmi J. A before-and-after observational study of a protocol for use of the C-MAC videolaryngoscope with a Frova introducer in pre-hospital rapid sequence intubation. Anaesthesia. 2018;73(3):348–55.
10. Sheu YJ, Yu SW, Huang TW, et al. Comparison of the efficacy of a bougie and stylet in patients with endotracheal intubation: a metaanalysis of randomized controlled trials. J Trauma Acute Care Surg. 2019;86(5):902–08.
11. Batuwitage B, McDonald A, Nishikawa K, et al. Comparison between bougies and stylets for simulated tracheal intubation with the C-MAC D-blade videolaryngoscope. Eur J Anaesthesiol. 2015;32(6):400–05.
12. Brazil V, Grobler C, Greenslade J, et al. Comparison of intubation performance by junior emergency department doctors using gum elastic bougie versus stylet reinforced endotracheal tube insertion techniques. Emerg Med Australas. 2011;24(2):194–200.
13. Sakles JC, Kalin L. The effect of stylet choice on the success rate of intubation using the Glidescope video laryngoscope in the emergency department. Acad Emerg Med. 2012;19(2):235–38.
14. Jones PM, Loh FLC, Youssef HN, et al. A randomized comparison of the GlideRite® rigid stylet to a malleable stylet for orotracheal intubation by novices using the GlideScope®. Can J Anaesthes. 2010;58(3):256–61.
15. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
Impact of Interventions on Peri-Intubation Hypoxemia and Hypotension in Critically Ill Patients: Systematic Review and Meta-Analysis
Christine E. Ren, MD*†
Jessica V. Downing, MD†‡
Stephanie Cardona, MD§
Isha Yardi, BS‡
Manahel Zahid, BS‡
Kaitlyn Tang, BS‡
Vera Bzhilyanskaya, BS‡
Priya Patel, BS**
Ali Pourmand, MD, MPH||
Quincy K. Tran, MD, PhD†‡
Section Editor: Dell Simmons, MD
Oregon Health and Science University, Department of Emergency Medicine and Critical Care Medicine, Portland, Oregon
R. Adams Cowley Shock Trauma Center, Program in Trauma, Baltimore, Maryland
University of Maryland School of Medicine, Department of Emergency Medicine, Research Associate Program, Baltimore, Maryland
The Mount Sinai Hospital, Department of Critical Care, New York, New York
George Washington University School of Medicine and Health Sciences, Department of Emergency Medicine, Washington, DC University of Maryland School of Medicine, Baltimore, Maryland
Submission history: Submitted October 12, 2024; Revision received April 11, 2025; Accepted April 18, 2025
Electronically published September 27, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.41210
Introduction: Emergent endotracheal intubation is common in critically ill patients. Underlying pathophysiologic derangements puts these patients at increased risk of peri-intubation major adverse events (MAE) and have been associated with higher morbidity and mortality. Investigating the impact of interventions in the peri-intubation period on the rate of peri-intubation hypoxemia and hypotension can help improve management of emergent airways.
Methods: We searched PubMed, Embase, and Scopus databases from their beginning through April 2024 to identify randomized controlled trials (RCT) evaluating interventions to prevent periintubation hypoxemia and hypotension. Random-effects meta-analysis was used for the outcomes of peri-intubation hypoxemia and hypotension. We used the Cochrane risk-of-bias tool and Cochrane Q-statistic and I2 to assess the quality and heterogeneity of the included studies, respectively.
Results: We included 16 RCTs included in our analysis with a total of 7,778 patients. All studies reported incidences of peri-intubation hypoxemia, and 11 studies reported rates of hypotension. One study had some concern of bias; otherwise all others were found to have low risk of bias. The examined interventions were associated with a 25% reduction in rates of hypoxemia (OR 0.748, 95% CI 0.566 - 0.988, P = .04). The subgroup of preoxygenation techniques showed a 63% reduction in rates of hypoxemia (OR 0.37, 95% CI 0.23 - 0.61, P < .001). Interventions to prevent hypotension were not associated with a significant decrease in rates of peri-intubation hypotension (OR 0.848, CI 0.676 - 1.063, P = .15).
Conclusion: Preoxygenation interventions, in the form of noninvasive ventilation, are associated with lower odds of hypoxemia in the peri-intubation period. More research is needed to determine whether interventions can be successful at preventing cardiovascular collapse. [West J Emerg Med. 2025;26(5)1380–1391.]
INTRODUCTION
Peri-intubation major adverse events (MAE), including hypoxemia, hypotension, and cardiac arrest, occur in up to 30% of patients intubated in the emergency department (ED), intensive care unit (ICU), or on the medical floors. Among these patients, emergency airway management often occurs in the setting of physiological derangements, such as hypoxemia, acidosis, and hypotension, that increase risk for peri-intubation MAEs; as a result, almost 1 in 3 patients intubated emergently in the ED or ICU will experience a peri-intubation MAE, such as hypoxemia (15%) or cardiovascular collapse (18%).1 Studies have consistently demonstrated that peri-intubation hypotension and hypoxemia are strongly associated with increased in-hospital mortality, underscoring the importance of optimizing the airway management process.2–5 Pre-intubation hypotension has been identified as a risk factor for subsequent post-intubation cardiac arrest and prolonged ICU stays.6,7
Several studies have examined interventions aimed at reducing patient risk during the peri-intubation period. These include preoxygenation techniques (such as use of high flow nasal cannula [HFNC] or various forms of positive pressure ventilation [PPV] to increase mean airway pressure and alveolar recruitment); implementation of airway adjuncts (such as a gum elastic bougie or video laryngoscopy [VL]) to reduce apneic time and improve first-pass success; and preemptive fluid boluses during induction to increase venous return.5–8 The Society of Critical Care Medicine recently devised practice guidelines for rapid sequence intubation (RSI) including suggestions for preoxygenation with HFNC or non-invasive ventilation (NIV) in high-risk patients.9 However, gaps in high-quality evidence regarding optimal emergency airway management still remain, resulting in ongoing controversies in airway approaches and a wide range of clinical practices.
In this systematic review and meta-analysis, we examine the association between these interventions and rates of periintubation MAEs, including hypoxemia, hypotension, and cardiac arrest. In this study we aimed to contribute to the understanding of effective strategies in emergency airway management and guide clinical decision-making.
METHODS
Search and Selection Criteria
Our study was conducted in accordance with the 2020 Preferred Reporting Items for Systematic Reviews and MetaAnalyses (PRISMA) statement, and we used the PRISMA checklist when writing our report.10 We searched PubMed, Embase, and Scopus on June 1, 2021, September 4, 2022, and April 23, 2024, to identify eligible studies. The search terms used were ((adverse) AND (events) OR (hypoxemia) OR (hypoxia) OR (desaturation) OR (hypotension) OR (cardiac AND arrest) OR (hemodynamic OR cardiovascular) AND (collapse)) AND ((endotracheal AND intubation) OR (emergency AND airway AND management) OR (peri-
Population Health Research Capsule
What do we already know about this issue? Hypoxemia and hypotension are common during intubation. While interventions have been studied, evidence gaps remain as to their efficacy.
What was the research question?
What is the association between interventions and rates of peri-intubation hypoxemia and hypotension?
What was the major finding of the study?
Noninvasive ventilation or high flow oxygen preoxygenation decreased rates of hypoxemia (OR 0.37, 95% CI 0.23 - 0.61,P < .001).
How does this improve population health? Preoxygenation can reduce peri-intubation hypoxemia. Data on interventions to reduce peri-intubation hypotension are limited.
intubation)). We also searched included articles to identify additional potentially eligible articles. We did not contact authors for more data.
Any randomized controlled trial (RCT) investigating the effects of interventions on peri-intubation hypoxemia, hypotension, or cardiac arrest were eligible for inclusion. We excluded the following studies: 1) did not have specified criteria for adverse events; 2) included pediatric patients only or did not differentiate outcomes among adult and pediatric patients; 3) included operating room, post-anesthesia care unit, or out-of-hospital (ie, emergency medical services) intubations; 4) were published in non-English language; 5) were systematic reviews, meta-analyses, observational studies, conference publications, case reports, or abstracts; and (6) did not have primary or secondary outcomes of hypoxemia, hypotension, or cardiac arrest. We screened enrollment databases, locations, and years for each study to identify potential duplicate reporting of data across studies. We elected to omit observational studies, given a previous meta-analysis of literature that showed numerous RCTs on peri-intubation adverse events,1 which thus allowed for adequate power and sample size while minimizing risk of bias, lowering the heterogeneity of the effect size, and strengthening the level of evidence of findings.
Our systematic review and meta-analysis was registered with PROSPERO (CRD42022342134). We used Covidence (www.covidence.org, first accessed on November 25, 2022) to review eligible studies. Each study title, abstract, and
full text was reviewed independently by two investigators; disagreements were resolved by a third senior investigator. This systematic review, conducted solely through the examination of secondary data and without any direct interaction with human subjects or primary data collection, was not subject to formal ethics approval.
Outcomes
We examined three separate MAEs individually, as the interventions recommended to prevent or address them are distinct. We examined the rates of hypoxemia, hypotension (both as defined by study authors), and cardiac arrest in the peri-intubation period. The peri-intubation period was also defined by study authors.
Quality Assessment
We assessed the quality of included RCTs using the Cochrane risk-of-bias (RoB) 2 tool, which evaluates risk of bias in randomization, deviations from study protocol, outcome measurement, selection of reporting, and effect of missing data.11 Based on the investigators’ assessment of each domain, the tool characterized risk of bias as “low,” “some concerns,” or “high.” If any single domain is determined to have “high” risk or “some concern” for bias, the entire study is judged to have this level of bias. Two independent investigators assessed the quality of each study, and any disagreement was adjudicated by a third investigator. Heterogeneity was assessed by the Cochrane Q statistic, which tests against the null hypothesis that all analyzed studies share a common effect size and I2 statistic, which determines the percentage of total variance expected to occur because of differences in effect size across included studies.
Data Collection
Data was extracted into a standardized Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA). We included each study’s year of publication, geographic location, dates of data collection, setting (ED, ICU, or mixed), intervention studied, study outcomes of interest, and patients’ clinical variables (if provided), such as demographics, vital signs, laboratory values, preintubation intravenous fluid (IVF) or vasopressor use and preoxygenation techniques, reason for intubation, and presence of MAEs. Interventions were subsequently categorized as IVF bolus administration, preoxygenation with NIV, preoxygenation with HFNC, or other. Data was extracted independently by two investigators and then compared for discrepancies; any discrepancies were discussed and resolved by the investigators. All data was adjudicated by group consensus before finalization.
Statistical analysis
We presented continuous data as mean (SD); all data originally presented as median (interquartile range [IQR]) were
converted into mean (SD) using VassarStats (http://vassarstats. net/median_range.html, last accessed October 26th, 2024).12 Categorical data were presented as numbers and percentages. We used random-effects models to measure the prevalence of MAEs across the pooled population in our studies. Any two studies reporting the same results were eligible for analysis. Results were reported as odds ratios (OR), with a 95% confidence interval (95% CI) for each outcome. Moderator analyses were performed to identify potential sources of heterogeneity and to compare subgroups, based on studies’ World Health Organization (WHO) region, clinical setting (ICU, ED, ward or mixed), type of adverse event, and type of intervention (IVF bolus administration, preoxygenation with NIV, preoxygenation with HFNC, or other). We studied the effect of composite interventions on primary outcomes of hypoxemia and hypotension. Similar intervention groups were then categorized together—preoxygenation techniques, intubation tools and techniques, induction agents, and IVF administration. These categories were determined based on the selected studies and were not determined a priori. We performed meta-analyses of separate types of interventions if there were adequate studies in each category of interventions. If studies in the categories were too small or varied in intervention approach, we provided a narrative review of our findings.
Sensitivity analysis was performed by “remove-onestudy” random-effects meta-analysis, which sequentially removes one study at a time to assess the impact of each individual study on the overall effect size. We assessed publication bias using the Begg and Egger tests (with P > .05 suggesting low likelihood of publication bias for each of these tests), the Orwin fail-safe N test (which predicts the number of missing or future studies that might change the effect size of our primary outcome), and the funnel plot. We performed all statistical analyses using the software Comprehensive MetaAnalysis (www.meta-analysis.com).
RESULTS
Study Selection and Summary
We included 16 RCTs (Figure 1) with a cumulative 7,778 patients (range 49-1417; Supplemental Table 1). We considered duplicate enrollment likely in two pairs of studies: Casey et al 201913 and Janz et al 2019,14 and Semler et al 201715 and Janz et al 2018.16 In each of these cases, the study pairs in question investigated distinct interventions; thus, we included all four studies in our analysis (Supplemental Table 1). All but one study17 included intubations in the ICU; five studies14,17–20 included intubations that occurred in the ED. Hypoxemia was the primary outcome of interest for eight13,15,16,18,18,21–23 and was reported in all included studies; in studies reporting hypoxemia as a primary outcome, hypoxemia was defined as SpO2 <80% in four studies,13,22–24 <85% in one study,18 and <90% in one study15; two studies16,21 examined the lowest saturation without defining a cutoff.
Hypotension was the primary outcome of interest
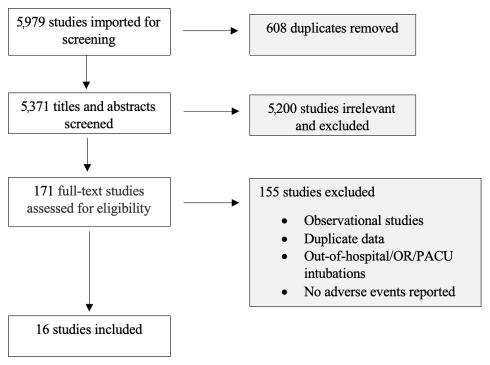
Figure 1. Flow diagram for the study selection process. Adapted from the PRISMA 2020 statement. OR, operating room; PACU, post-anesthesia care unit; PRISMA, Preferred Reporting Items for Systematic reviews and MetaAnalyses.
for four14,16,25,26 studies and was reported by an additional seven.13,18,20,23,24,27,28 In studies that reported hypotension as a primary outcome, hypotension was defined as a systolic blood pressure (SBP) <65 in two studies,14,26 a change in mean arterial pressure (MAP) from baseline in one study,25 and the lowest SBP without a predefined range in one study.16 Firstpass success was the primary outcome for five studies.17,19,20,27,28 Interventions included pre-oxygenation techniques (including NIV,18,21,23,24 HFNC,22,23 bag-valve mask [BVM]13), intubation tools and techniques (use of video laryngoscopy VL,20,27,28 use of gum-elastic bougie,17,19 patient positioning [ramped or sniffing],15 and the use of a pre-intubation checklist16), induction agent (reduced dose etomidate or a combination of ketamine and propofol25) and IVF administration (500 millilitersmL during induction14,26).
Study Quality
Fifteen of the 16 included studies were judged to have a low risk of bias (Supplemental Table 1). Grensemann 201827 was deemed to have some concern of bias, given that their study did not describe whether there was analysis to estimate effect of assignment to an intervention, such as intention to treat or per protocol analysis (Figure 2).
Outcome 1: Hypoxemia
Hypoxemia was reported in 16 studies and was the primary outcome for eight studies. The interventions examined were associated with an estimated 25% reduction in rates of hypoxemia (OR 0.748, 95% CI 0.566 - 0.988, P = . 04; Figure 3a). The prediction interval was wide and crossed 1 (0.280
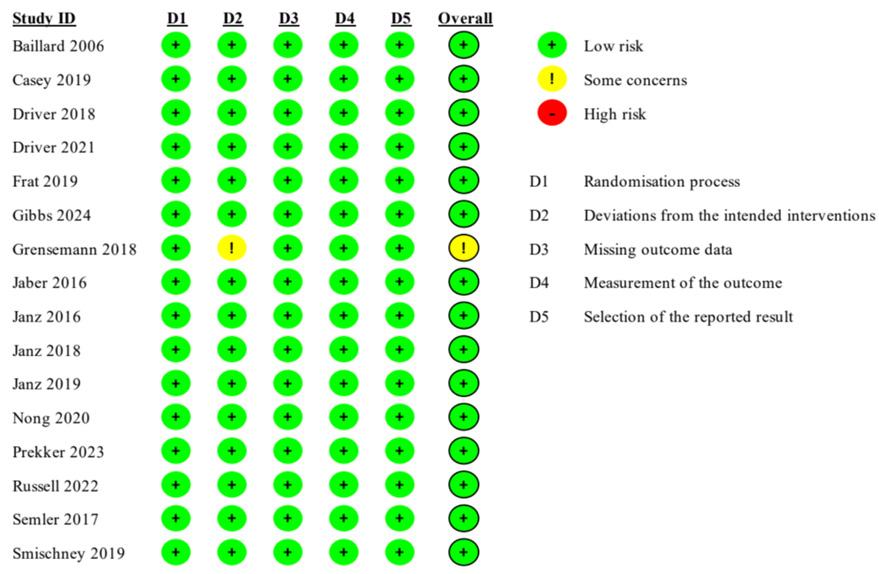
-1.997), indicating that the interventions studied could be expected to correlate with anywhere from a 70% reduction of hypoxemia to a 99% increase in rates of hypoxemia. There was a high degree of heterogeneity. The P-value for the Q statistic was 0.001, which suggests that the true effect varied among the included studies. The I2 statistic was 74%.
Moderator analysis suggested that among the interventions used to prevent hypoxemia, only studies using NIV (OR 0.35, 95% CI 0.17 - 0.72, P < 01) or other forms of preoxygenation were associated with a significant reduction in rates of hypoxemia (OR 0.39, 95% CI 0.23 - 0.67, P = .001) (Table 1). Multivariate meta-regression suggested that higher body mass index (BMI) was associated with higher rates of hypoxemia (Pearson correlation coefficient [r] 0.35, 95% CI 0.09 - 0.61, P=.01), and that patients intubated for respiratory failure had lower rates of peri-intubation hypoxemia than those with other indications for intubation (r -4.9, 95% CI -9.1 - [- 0.77], P = .02) Table 2).
Sensitivity meta-analysis using a “one-study-removed” approach identified similar results to our original analysis, suggesting no single study disproportionately affected our findings (Figure 3b). The Begg and Egger tests suggested low likelihood of publication bias (P = .39 and P = .36, respectively). The Orwin fail-safe determined that eight future or missing studies with an effect size of 1.6 favoring control would be needed to negate the significance of our findings. Our funnel plot demonstrated relative symmetry, also supporting a low likelihood of publication bias (Figure 3c).
We then examined the effects on hypoxemia of studies that looked at preoxygenation techniques, which included NIV,18,21,23,24 HFNC,22,23 and BVM.13 These were associated with a 63% reduction in rates of hypoxemia (OR 0.37, 95% CI 0.23 - 0.61, P < .001; Figure 3d). The prediction interval was large and crossed 1 (0.09 - 1.55), suggesting that the studies that looked at preoxygenation techniques could range from a 90% reduction of hypoxemia to a 55% increase in hypoxemia. There was substantial heterogeneity with an I² statistic of 62%. The
Figure 2. Cochrane risk-of-bias11 assessment for included studies. Each rating is based on consensus between two investigators.
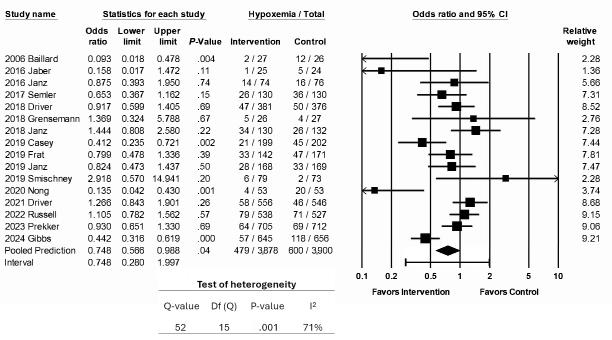
3a. Association of interventions with rates of peri-intubation hypoxemia.
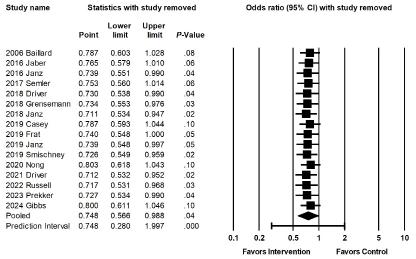
Figure 3b. Sensitivity analysis for the association of interventions with rates of peri-intubation hypoxemia.
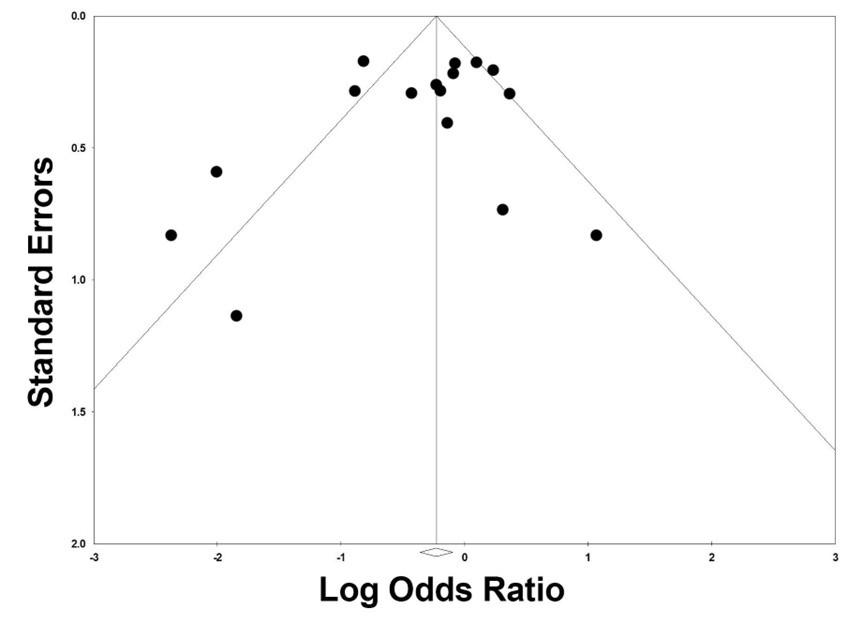
3c. Publication bias funnel plot of studies investigating effect of interventions on hypoxemia.
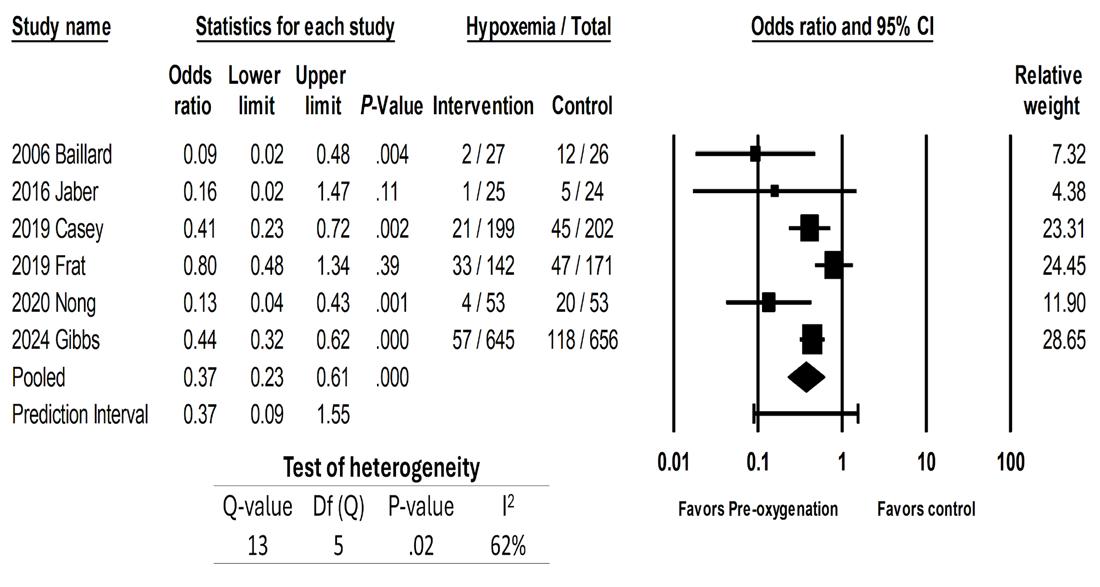
Figure 3d. Association of preoxygenation techniques with rates of peri-intubation hypoxemia.
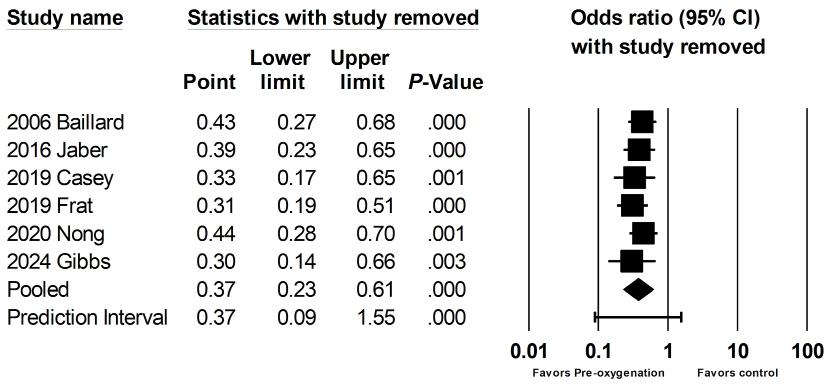
Figure 3e. Sensitivity analysis for the association of preoxygenation techniques with rates of peri-intubation hypoxemia.
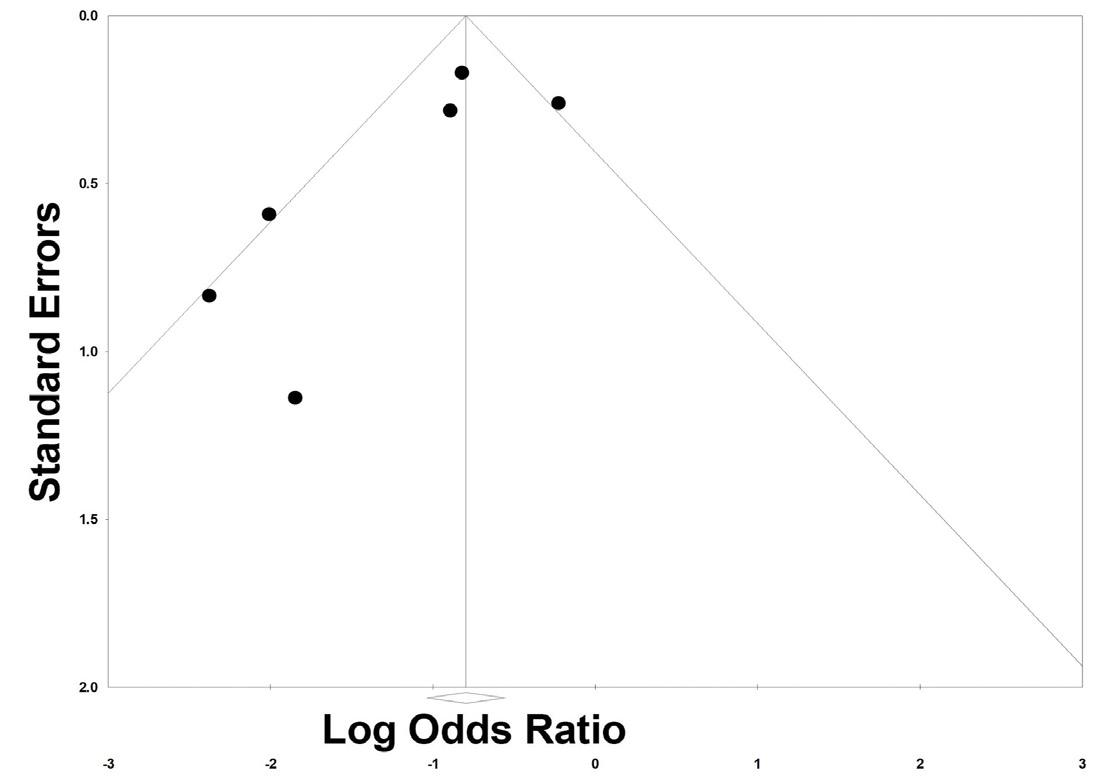
Figure 3f. Publication bias funnel plot of studies investigating preoxygenation techniques on hypoxemia.
Figure
Figure
Table 1. Moderator analysis for subgroup comparisons between studies, using categorical variables.
variables
Primary outcome 1: Hypoxemia
WHO region
Sample size
type
Primary Outcome 2: Hypotension
WHO Region
aIncludes patient positioning (ramped versus sniffing position), use of a gum-elastic bougie, and use of a standardized pre-intubation checklist.
bIncludes non-invasive ventilation, bag-valve mask ventilation. AMR, Regions of Americas; DL, direct laryngoscopy; EUR, Region of Europe; HFNC, high-flow nasal cannula; ICU, intensive care unit; NIV, non-invasive ventilation; WHO, World Health Organizations; WPR, Region of Western Pacific; VL, video laryngoscopy.
P-value for the Q statistic was .02. Sensitivity meta-analysis using “one-study-removed” suggested no single study disproportionately affected our findings (Figure 3e). The funnel plot of preoxygenation techniques on hypoxemia exhibited more studies laying to the left of midline, suggesting presence of publication bias and that most of these studies reported positive results from the intervention (Figure 3f).
Moderator analyses showed that studies from the Americas region13,18 were associated with low heterogeneity when compared to the European studies21,22,23 (Table 3). Multivariate meta-regression did not reveal any clinical factors that were associated with odds of hypoxemia (Table 4). Evaluation of the effect of airway adjuncts, such as gum-elastic bougie,17,19 showed no significant changes in rates of hypoxemia.
Table 2. Multivariate meta-regression evaluating the association between select continuous variables and peri-intubation major adverse events.
Outcome: Hypoxemia
% of intubation for respiratory failure
Outcome: Hypotension
(0.09 to 0.61)
(-3.8 to 4.6)
(-9.1 to -0.77)
of intubation for hemodynamic instability
of
Bolded values denote statistical significance. BMI, body mass index; SBP, systolic blood pressure; HFNC, high-flow nasal cannula; NIV, non-invasive ventilation.
Outcome 2: Hypotension
Eleven studies reported rates of hypotension, which was the primary outcome for three. The interventions examined were not associated with a significant decrease in rates of hypotension (OR 0.848, CI 0.676 - 1.063, p = 0.15; Figure 4a). The I statistic was 0, because no studies reported a significant change in rates of hypotension associated with the intervention.
Sensitivity meta-analysis using “one-study-removed” suggested no single study disproportionately affected our findings (Figure 4b). Begg and Egger’s tests suggested low likelihood of publication bias (p = 0.52 and p = 0.28, respectively). Our funnel plot demonstrated symmetry, suggesting a low likelihood of bias, but does raise the possibility of a small study effect with more studies associated with a higher standard error (Figure 4c).
Sensitivity meta-analysis using a “one-study-removed” approach identified similar results to our original analysis (Figure 5b). There were not enough studies to perform moderator analyses. Variables
Studies that looked at fluid boluses14,26 as interventions, showed no significant change in rates of hypotension.
Outcome 3: Cardiac Arrest
Eleven studies reported cardiac arrest as a secondary outcome; their interventions were not associated with a reduction in the rates of cardiac arrest (OR 0.962, 95% CI 0.6011-1.539; P = .87; Figure 5a). The overall reported prevalence of peri-intubation cardiac arrest was very low (the overall pooled prevalence was <1.3%, 1.2% among intervention groups as 1.3% among control groups).
Table 3. Moderator analyses using categorical variables for subgroup analyses in studies evaluating preoxygenation techniques.
Variables
Outcome: Hypoxemia WHO Region
AMR, Regions of Americas; EUR, Region of Europe; NIV, non-invasive ventilation; WHO, World Health Organizations; WPR, Region of Western Pacific.
Table 4. Meta-regression using continuous variables and the outcome for odds of major adverse events among patients undergoing pre-oxygenation.
DISCUSSION
We found that previously investigated interventions to minimize peri-intubation hypoxemia among patients undergoing emergent intubation in the ED or ICU demonstrated success, while those intended to minimize peri-intubation hypotension did not. Specifically, studies investigating NIV or other forms of preoxygenation were associated with a decreased risk of peri-intubation hypoxemia. The administration of IVF boluses in the peri-intubation period was not associated with decreased rates of hypotension. No examined interventions impacted rates of cardiac arrest.
Percentage receiving NIV
of intubation for respiratory failure
of intubation for airway protection
Corr. Coeff., Correlation Coefficient; HFNC, high-flow nasal cannula; NIV, non-invasive mechanical ventilation; NA, not enough studies reporting the variables for the analysis.
The heterogeneity in our study was high, likely due to diversity in the clinical settings and geographic locations of included studies (expected to reflect different practice patterns and resource use). Despite this, our sensitivity analysis confirms that our findings were not overly influenced by any single study, suggesting that our findings are likely accurate, while not precise.
Most of the studies included here investigated the effect of NIV—via BVM-assisted breaths with a positive end-expiratory pressure (PEEP) valve, bi-level positive airway pressure (BiPAP) ventilation with a face mask and mechanical ventilator, or a combination of techniques—on peri-intubation hypoxemia Three studies compared the use of NIV to low-flow preoxygenation techniques such as nasal cannula (NC), bag-mask device without manual
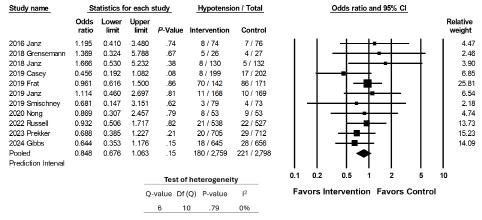
4a. Association of interventions with rates of peri-intubation hypotension.
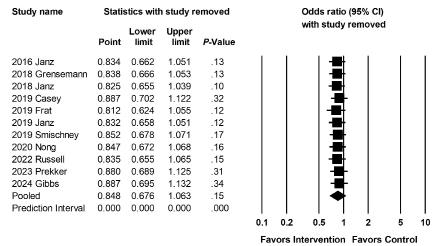
4b. Sensitivity analysis for the association of interventions with rates of peri-intubation hypotension.
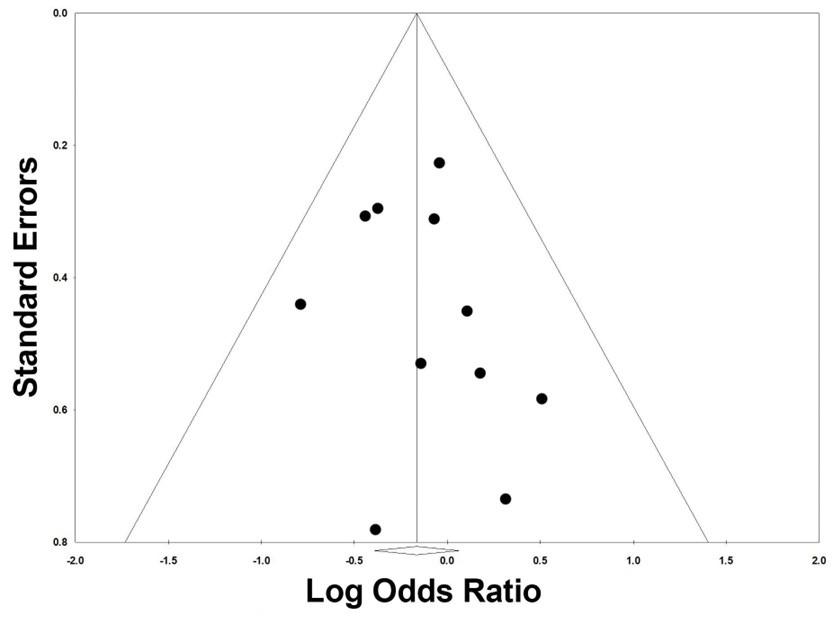
4c. Publication bias funnel plot of studies investigating interventions on hypotension.
ventilation, or non-rebreather mask (NRB); higher rates of severe hypoxemia (SpO2 < 80%) were found in the low-flow oxygen groups.13,18,21 One compared NIV to HFNC, which can deliver oxygen flow rates of up to 60 liters per minute (LPM) (for comparison, NRB masks typically deliver around 15 LPM) and a fraction of inspired oxygen (FiO2) as high as 100%.23 While we did not identify any significant difference in overall rates of severe hypoxemia (SpO2 < 80%), we did find that, among patients with moderate to severe pre-intubation hypoxemia (defined as PaO2:FiO2 ≤ 200), preoxygenation with NIV was associated with lower rates of severe hypoxemia during the intubation.
The means through which NIV were applied across studies varied widely. Gibbs et al compared preoxygenation with NIV using pressure support of >10 centimeters water (cm H2O) and a PEEP of >5 cmH2O with FiO2 100% to either a NRB or a bag-mask device without manual ventilation.18 Both trial groups underwent preoxygenation with these methods for three minutes before induction, and intubators were permitted to use a BVM between anesthesia induction and initiation of laryngoscopy. The NIV group was found to have lower rates of hypoxemia, with a greater effect noted in patients with a higher BMI. Nong et al compared BVM with a PEEP of 5 cmH20 and BiPAP with inspiratory pressures of 12 - 20 cmH20 and PEEP of 5 cmH20, with the BiPAP group continuing NIV throughout the intubation procedure.24 Patients allocated to the BVM were ventilated for three minutes prior to fiberoptic intubation accompanied by passive oxygenation via NC.
Patients in the BiPAP group underwent fiberoptic intubation through a sealed hole in the BiPAP face mask, allowing continuation of ventilation during the intubation procedure. While this study technically examined preoxygenation via NIV, it did not examine a type of preoxygenation easily implemented in most centers. In the BiPAP group, SpO2 levels before and during intubation were higher and rates of severe hypoxemia were lower, suggesting a positive impact of this novel approach. Other non-standard approaches described may be more feasible: Jaber et al compared NIV using pressure support of 10 cmH2O and PEEP of 5 cmH2O with FiO2 of 100 % to NIV plus HFNC with settings of flow 60 LPM and FiO2 100%; the combination of techniques was better at preventing periintubation hypoxemia.22 Overall, NIV appears effective in reducing risk of peri-intubation hypoxemia compared to other preoxygenation techniques. While therapies such as NC and NRB provide passive oxygenation, NIV also unloads respiratory muscles, lowering work of breathing and diaphragmatic work, increasing tidal volume and ventilation, and providing high fraction of inspired oxygen.29 In doing this, patients have a higher respiratory reserve (higher pO2 and lower pCO2 levels) when induction and paralytic agents are administered, leading to lower rates of hypoxemia
The use of NIV is not without risk; reported complications include gastric insufflation, aspiration, barotrauma, and
Figure
Figure
Figure
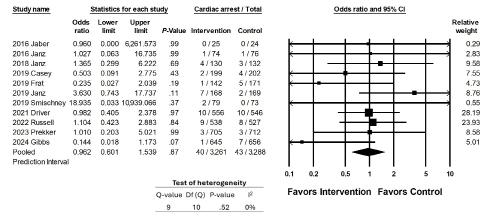
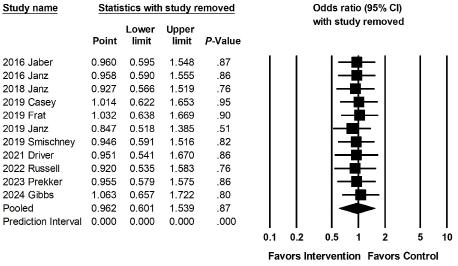
association
interventions
do so. Driver et al’s 2021 comparison of gum-elastic bougie and traditional stylet demonstrated a 2.2% increase in absolute risk of hypoxemia in the bougie group.17 Prekker et al found that VL was associated with 0.7% lower absolute risk of hypoxemia and 1.3% absolute risk of hypotension when compared to direct laryngoscopy, with no improvement in first-pass success despite improvement in glottic visualization.20 Grensemann et al, who studied the use of an endotracheal tube-mounted camera, found no difference in first-pass success, hypoxemia, or hypotension between these two groups,27
Of interest, in a meta-regression of studies reporting use of HFNC and percentage of patients intubated for respiratory failure, those intubated for respiratory failure had lower odds of peri-intubation hypoxemia. Use of HFNC did not impact rates of peri-intubation hypoxemia in this analysis. Based on these findings and clinical experience, we speculate this may be reflective of variations in pre-intubation resuscitation strategies: specifically, that clinicians are more likely to prioritize aggressive preoxygenation specifically (perhaps with NIV) among patients with respiratory failure, leading to lower rates of peri-intubation hypoxemia. Our data give limited insight into the explanation for this surprising finding but highlights it as an area for further investigation.
agitation.30 Three studies included in our meta-analysis compared rates of witnessed aspiration or a new infiltrate on post-intubation chest radiograph (CXR) between patients receiving NIV and those receiving low-flow oxygen therapy, and did not find any difference between the two groups.13,18,21 Similarly, there was no difference regarding rates of regurgitation, gastric distention, CXR infiltrates, hypotension, or agitation in patients who received NIV compared to HFNC or HFNC plus NIV.22,23 Although NIV exposes patients to positive pressure ventilation, which may not be tolerated by patients with hemodynamic compromise and may progress to cardiovascular collapse, this change in physiology mimics that introduced by invasive mechanical ventilation, and as such does not introduce a new risk profile. The studies included here that investigated rates of hypotension between patients preoxygenated with NIV or high and low-flow oxygen did not identify any significant differences in rates of hypoxemia 23,24 Studies examining techniques to improve first-pass success did not demonstrate any significant difference in rates of hypoxemia or hypotension, although they were not powered to
Two RCTs investigating the effect of a peri-intubation IVF bolus on rates of cardiovascular collapse were included in our meta-analysis; neither showed a difference in outcomes.14,26 Both studies included a set or average bolus volume of 500mL; it is unclear whether a different amount would have generated a different outcome. None investigated preemptive use of vasoactive medications. Other studies have shown promising results in the prevention of peri-intubation cardiovascular collapse, although the means through which these results were accomplished are difficult to narrow down. Jaber et al investigated the implementation of an “ICU intubation bundle,” which included 10 components: preoxygenation with NIV; presence of two operators; RSI; cricoid pressure, capnography, protective ventilation, fluid loading, and preparation and early administration of sedation; and vasopressor use if needed. The authors found significantly lower rates of life-threatening complications in the intervention group (21% vs. 34%, P = .03), and a 50% reduction in the incidence of severe hypoxemia and severe cardiovascular collapse.31 Further research is needed to determine which specific interventions, (such as the use of specific induction agents or early administration of vasopressors), can reduce rates of peri-intubation cardiovascular collapse.
LIMITATIONS
Most included patients were intubated in an ICU; so our findings may not be generalizable to other settings or populations. The implementation of interventions varied widely between studies. The number of included studies was small, particularly given the heterogeneity in practice location, practice setting, and interventions. We were unable to provide a standardized range
Figure 5a. Association of interventions with rates of cardiac arrest.
Figure 5b. Sensitivity analysis for the
of
with rates of cardiac arrest.
for hypoxemia or hypotension given the inconsistent definitions across our included studies. This introduced significant heterogeneity to our results and highlights the need for consensus of definition for peri-intubation adverse events.
There were differences overall in the control groups of the various studies we included. Some compared intervention to intervention in their studies, and some included overlapping interventions. Studies that looked at airway adjuncts, VL, endotracheal tube-mounted cameras, induction medications, and checklists all employed various modalities of preoxygenation in both their control and intervention groups. Although this closely mirrors the heterogeneity of approach in clinical practice, it may result in multiple confounding factors.
Only three studies investigated hypotension as a primary outcome, and both only examined the role of IVF boluses; additional research is needed to evaluate the impact of other interventions. The overall number of cardiac arrests observed in these studies was low, and none were powered to identify a change in the incidence of cardiac arrest. Lastly, multiple studies reported similar clinical outcomes as separate MAEs (eg, addition of vasopressors and hypotension, hypotension and cardiac arrest, or hypoxemia and cardiac arrest). It is likely that separately reported MAEs could have been related or overlapped.
CONCLUSION
Pre-oxygenation with NIV was associated with lower odds of peri-intubation hypoxemia. More trials are needed to determine whether interventions can successfully prevent periintubation hypotension
Address for Correspondence: Christine Ren, MD, Oregon Health and Science University, Department of Emergency Medicine and Critical Care Medicine, 3181 SW Sam Jackson Park Road, Portland, OR, 97239. Mail Code: CDW-EM, ATTN: Christine Ren, MD. Email: rench@ohsu.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Ren et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Downing J, Yardi I, Ren C, et al. Prevalence of peri-intubation major adverse events among critically ill patients: a systematic review and meta analysis. Am J Emerg Med. 2023;71:200-16.
2. Smischney NJ, Khanna AK, Brauer E, et al. Risk factors for and
outcomes associated with peri-intubation hypoxemia: a multicenter prospective cohort study. J Intensive Care Med. 2021;36(12):146674.
3. Heffner AC, Swords D, Kline JA, et al. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(4):417.e9-417.e13.
4. Green RS, Turgeon AF, McIntyre LA, et al. Postintubation hypotension in intensive care unit patients: a multicenter cohort study. J Crit Care. 2015;30(5):1055-60.
5. Ferrada P, Manzano-Nunez R, Lopez-Castilla V, et al. Meta-analysis of post-intubation hypotension: a plea to consider circulation first in hypovolemic patients. Am Surg. 2019;85(2):167-72.
6. Heffner AC, Swords DS, Neale MN, et al. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation. 2013;84(11):1500-4.
7. Kim WY, Kwak MK, Ko BS, et al. Factors associated with the occurrence of cardiac arrest after emergency tracheal intubation in the emergency department. Chen X, ed. PLoS One 2014;9(11):e112779.
8. Mosier JM, Joshi R, Hypes C, et al. The physiologically difficult airway. West J Emerg Med. 2015;16(7):1109-17.
9. Acquisto NM, Mosier JM, Bittner EA, et al. Society of Critical Care Medicine Clinical Practice guidelines for rapid sequence intubation in the critically ill adult patient. Crit Care Med. 2023;51(10):1411-30.
10. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021:372:n71.
11. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019:366:l4898.
12. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
13. Casey JD, Janz DR, Russell DW, et al. Bag-mask ventilation during tracheal intubation of critically ill adults. N Engl J Med 2019;380(9):811-21.
14. Janz DR, Casey JD, Semler MW, et al. Effect of a fluid bolus on cardiovascular collapse among critically ill adults undergoing tracheal intubation (PrePARE): a randomised controlled trial. Lancet Respir Med. 2019;7(12):1039-47.
15. Semler MW, Janz DR, Russell DW, et al. A multicenter, randomized trial of ramped position vs sniffing position during endotracheal intubation of critically ill adults. Chest. 2017;152(4):712-22.
16. Janz DR, Semler MW, Joffe AM, et al. A multicenter randomized trial of a checklist for endotracheal intubation of critically ill adults. Chest. 2018;153(4):816-24.
17. Driver BE, Semler MW, Self WH, et al. Effect of use of a bougie vs endotracheal tube with stylet on successful intubation on the first attempt among critically ill patients undergoing tracheal intubation: a randomized clinical trial. JAMA. 2021;326(24):2488-97.
18. Gibbs KW, Semler MW, Driver BE, et al. Noninvasive ventilation for preoxygenation during emergency intubation. N Engl J Med 2024;390(23):2165-77.
19. Driver BE, Prekker ME, Klein LR, et al. Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA. 2018;319(21):2179.
20. Prekker ME, Driver BE, Trent SA, et al. Video versus direct laryngoscopy for tracheal intubation of critically ill adults. N Engl J Med. 2023;389(5):418-29.
21. Baillard C, Fosse JP, Sebbane M, et al. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am J Respir Crit Care Med. 2006;174(2):171-7.
22. Jaber S, Monnin M, Girard M, et al. Apnoeic oxygenation via high-flow nasal cannula oxygen combined with non-invasive ventilation preoxygenation for intubation in hypoxaemic patients in the intensive care unit: the single-centre, blinded, randomised controlled OPTINIV trial. Intensive Care Med. 2016;42(12):1877-87.
23. Frat JP, Ricard JD, Quenot JP, et al. Non-invasive ventilation versus high-flow nasal cannula oxygen therapy with apnoeic oxygenation for preoxygenation before intubation of patients with acute hypoxaemic respiratory failure: a randomised, multicentre, openlabel trial. Lancet Respir Med. 2019;7(4):303-12.
24. Nong L, Liang W, Yu Y, et al. Noninvasive ventilation support during fiberoptic bronchoscopy-guided nasotracheal intubation effectively prevents severe hypoxemia. J Crit Care. 2020;56:12-17.
25. Smischney NJ, Nicholson WT, Brown DR, et al. Ketamine/ propofol admixture vs etomidate for intubation in the critically ill:
KEEP PACE randomized clinical trial. J Trauma Acute Care Surg 2019;87(4):883-91.
26. Russell DW, Casey JD, Gibbs KW, et al. Effect of fluid bolus administration on cardiovascular collapse among critically ill patients undergoing tracheal intubation: a randomized clinical trial. JAMA. 2022;328(3):270.
27. Grensemann J, Eichler L, Wang N, et al. Endotracheal tubemounted camera-assisted intubation versus conventional intubation in intensive care: a prospective, randomised trial (VivaITN). Crit Care. 2018;22(1):235.
28. Janz DR, Semler MW, Lentz RJ, et al. Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults. Crit Care Med. 2016;44(11):1980-7.
29. Kallet RH, Diaz JV. The physiologic effects of noninvasive ventilation. Respir Care. 2009;54(1):102-15.
30. Carron M, Freo U, BaHammam AS, et al. Complications of noninvasive ventilation techniques: a comprehensive qualitative review of randomized trials. Br J Anaesth. 2013;110(6):896-914.
31. Jaber S, Jung B, Corne P, et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive Care Med 2010;36(2):248-55.
32. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
Five-Year Trends in Emergency Medicine Match Results and Future Outlook
Alexander Y. Sheng, MD, MHPE*°
Erin L. Simon, DO†°
Timothy Friedmann, MD, MS-HPEd‡
Eddie Garcia, MD§
Vytas Karalius, MD, MPH§
Michael Kiemeney, MD||
Brian Merritt, DO#
Brian Milman, MD¶
Meghan Mitchell, MD, MEd**
Jared Mugfor, DO††
Mihir Patel, MD¶
Rachel Wong, MD‡‡
Esther H. Chen, MD§§
Warren Alpert Medical School at Brown University, Department of Emergency Medicine, Providence, Rhode Island
Northeast Ohio Medical University, Cleveland Clinic Akron General Emergency Medicine Program, Akron, Ohio
Icahn School of Medicine at Mount Sinai, Department of Emergency Medicine, New York, New York
Stanford University School of Medicine, Department of Emergency Medicine, Palo Alto, California
Loma Linda University School of Medicine, Department of Emergency Medicine, Loma Linda, California
University of Utah, Department of Emergency Medicine, Salt Lake City, Utah University of Texas Southwestern Medical Center, Department of Emergency Medicine, Dallas, Texas
Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois
Drexel University College of Medicine, Department of Emergency Medicine, Philadelphia, Pennsylvania
Icahn School of Medicine at Mount Sinai, Mount Sinai Morningside West, New York, New York
University of California, San Francisco, Department of Emergency Medicine, San Francisco, California
Section Editor: Asit Misra, MD, MSMEd
Submission history: Submitted May 22, 2025; Revision received June 4, 2025; Accepted June 7, 2025 Electronically published September 27, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.47915
[West J Emerg Med. 2025;26(5)1392–1396.]
BACKGROUND
Emergency medicine (EM) as a specialty attracts medical students due to its acuity of care, diversity of patients, pathologies, and procedures, accompanied by a uniquely flexible work-life balance. Except for a slight drop in 2014, the number of applicants to EM had steadily increased yearly since 2001, peaking in 2021 with 3,734 applicants. 1 In fact, prior to 2022 EM was so competitive that it had fewer than 30 unmatched residency spots per year for over a decade.2
THE BOTTOM FALLS OUT
In 2022, the National Resident Matching Program (NRMP) EM Match resulted in a drastic fall in the number of applicants by 17.5% from 3,734 in 2021 to 3,081 in 2022, leading to 219 unfilled positions. This trend culminated in 2023, when the number of applicants dropped by an additional 10.3% to 2,765. Before the Supplemental Offer and Acceptance Program, 554 (18%)
of 3,010 available positions went unmatched, leaving 132 (46%) of EM programs unfilled (Figure 1). 1 Emergency medicine suddenly faced an unprecedented number of unfilled residency positions for the first time in decades, sparking concerns about the future of the EM workforce.2
This recent sharp decline in medical student interest in EM was likely influenced by multiple factors. In 2021, a workforce study by the American College of Emergency Physicians (ACEP) projected that by 2030 there could be almost 8,000 more emergency physicians than would be needed in the United States.3 The authors cited multiple reasons for predicting an workforce oversupply, including expansion of medical school class sizes, rapid growth in the number of EM residencies, lower population growth rate, and increasing participation by advanced practice clinicians (APC) in the workforce. 3 This projection shocked the EM community, raising alarm about the future job market for emergency physicians. In 2023, a joint statement by ACEP suggested multiple reasons behind the decreasing number
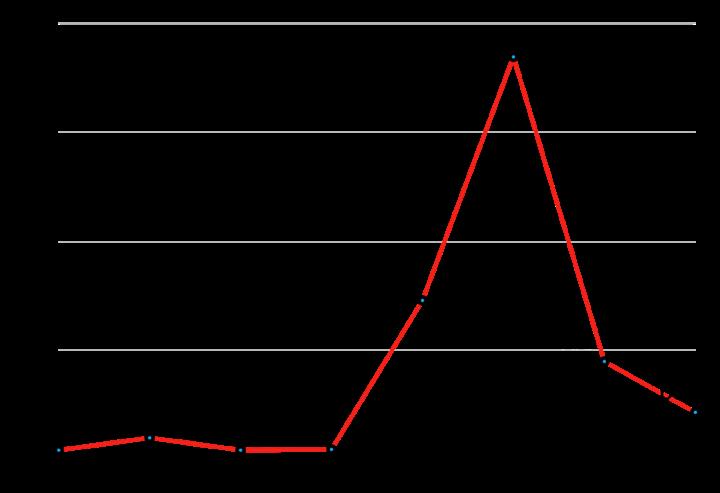
of EM applicants, including COVID-19, corporatization of medicine, emergency department (ED) boarding, economic challenges, and workforce projections.4
Also contributing to the increase in unfilled residency positions was the drastic rise in the number of residency programs, which could not be attributed solely to the transition from three accrediting organizations (the American Osteopathic Association [AOA], American Association of Colleges of Osteopathic Medicine, and Accreditation Council of Graduate Medical Education [ACGME]) to a single accreditation system within the ACGME. From 2001–2023, the number of EM residency programs increased from 117 to 287,1,5 with an overall increase in residency positions from 1,001 to 3,010.1 Although the increase in EM programs and positions was mirrored by the increase in applicants for two decades, this trend became unsustainable with the sudden drop in applicants from 2021 to 2023.
THE REBOUND
Emergency medicine is a resilient specialty. Following the 2023 Match cycle, educators and program leadership at the local and national levels went to work to gather data, modify recruitment and interview strategies, and identify ways to prevent another match like 2023. An EM Match Taskforce was established with representatives from major EM organizations to evaluate and address the factors that led to the suboptimal Match results in 2023.4 Data suggested that several factors—having unfilled positions in the 2022 Match; smaller program size; Mid-Atlantic or East North Central location; corporate ownership; and prior AOA and more recent accreditation (within the prior five years)—were all associated with unfilled spots in 2023.6,7 Based on this information, programs were deliberate in the
way that they recruited, interviewed, and ranked applicants to maximize their chance of filling their residency positions. 8
Concurrently, the ACEP EM Workforce Taskforce worked to prioritize patient care and education over business interests, increase support for emergency care in rural communities, ensure adequate supervision for advanced practice clinicians, and expand the scope of EM practice to provide acute unscheduled care outside the traditional walls of the ED.9 Nationwide efforts to address ED boarding, reduce profit-driven practices in staffing of APCs, resist the growth of private equity in medicine, and mitigate burnout are ongoing.10,11
As a result of these multipronged efforts, EM as a specialty has seen a rebound since 2023 (Figure 2). Going into the 2024 match, there was cautious optimism. The number of EM applications rose by 29.3% from 2023, totaling 3,574 applicants for 3,026 spots in 292 programs. While the number of positions continued to rise (2,665 in 2020, 2,840 in 2021, 2,921 in 2022, and 3,010 in 2023), the rate of expansion has slowed with 16 additional positions in 2024. The rise in applications was mainly driven by the increases in applications from osteopathic medical school students (DO) (by 43.9%) and international medical graduates (IMG) (by 81.6%). In contrast, there was a 15.4% decrease in the number of senior applicants from allopathic programs (MD) from 2020 to 2024, although there was a slight increase of 3.7% between 2023 and 2024.1
The 2024 Match results improved accordingly from 2023. Of the 3,026 available positions, 2,891 (95.5%) were filled with only 135 open positions in 2024 as compared to 554 in 2023. There were 1,386 MD senior applicants (38.8% of total applicants); of those, 1,285 matched into EM, which accounted for 44.4% of the filled spots. This compared to 2023 in which 1,337 MD seniors applied and 1,274 of
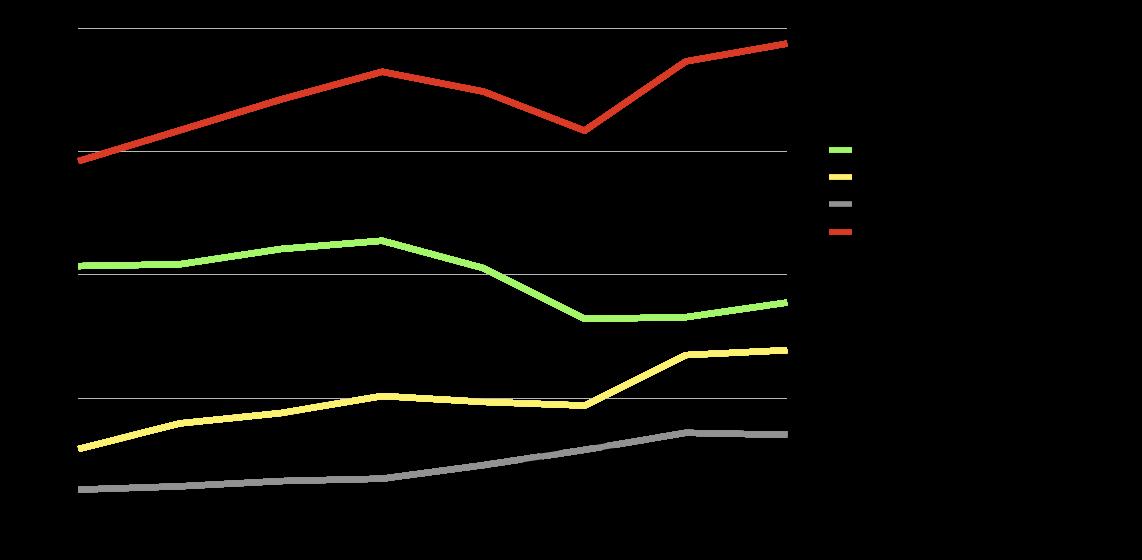
Figure 2. Five-year emergency medicine Match composition trends 2018–2025.
MD, doctor of medicine; DO, doctor of osteopathic medicine; US, United States
Figure 1. Unfilled emergency medicine Match positions, 2018-2025.
2,456 (51.9%) spots were filled by MD seniors.1 A total of 1,047 of 1,171 DO seniors who applied to EM successfully matched, representing 36.2% of the filled spots. In 2023, DO seniors accounted for 29.7% of positions filled.1
In 2024, there were 486 US IMG and 349 non-US IMG applications, totaling 835 IMG applicants. This represented a significant increase from 2023, with 487 total IMG applicants (366 US IMG, 121 non-US IMG). Thus, IMGs filled 448 positions (325 US IMGs and 123 non-US IMGs) in 2024, which accounted for 15.5% of the filled spots.2 In 2023, there were 350 positions filled by IMGs (14.3% of positions filled). In 2023, 71.9% of IMG applicants matched, but in 2024 this fell to 53.7%. (Table 1).
THE 2025 MATCH
The 2025 EM Match marked another year-over-year improvement. There were 3,753 applicants for 3,068 positions from 292 programs, an increase from the 3,574 applicants for 3,026 positions in 2024. The vast majority (3,003, 97.9%) of the positions were filled, leaving 65 open spots—much fewer than the 554 and 135 unmatched positions in the 2023 and 2024 Match.1 In 2025, 1,514 US MD seniors applied to EM, an increase of 128 students compared to 2024. Allopathic seniors accounted for 1,377 (45.9%) of the total filled spots, a marginal increase from 1,285 (44.4%) in 2024. However, this is still far below the peak of 1,765 (62.5%) in 2021.1
Applicants by seniors from US osteopathic medical schools accounted for 1,231 of 3,753 (32.8%) EM applicants, and 1,078 of them matched into EM, representing 35.9% of the total filled positions. This is stable from the 2024 season, in which 1,047 US osteopathic school seniors accounted for 36.2% of the total positions filled; but it is much higher than the 2021 Match, during which only 790 US osteopathic seniors matched into EM, representing 28% of the total filled positions.1
A total of 467 US IMGs and 336 non-US IMGs applied to EM in the 2025 NRMP Match, with 315 and 131 matching successfully, respectively. The US and non-US IMGs together filled 446 positions (14.6%), essentially unchanged from the 448 positions they filled in 2024 (14.8%) 1 (Figure 3)

FUTURE IMPLICATIONS
The 2025 NRMP EM Match demonstrated a continued reduction in the number of unfilled positions, since the peak in 2023. While the positions offered were still primarily filled by seniors from US allopathic medical schools (46%), this proportion has largely remained steady in the last three years and has yet to return to 2021 levels (62%). Of the remaining 1,628 EM positions, US DO seniors filled 66%, with the last third occupied by US IMG and non-US IMG seniors. These proportions have remained consistent over the last two Match cycles. It is too early to tell whether EM has reached a new steady state of EM-bound medical school graduates.
A recent development that could impact Match results in the near future is the ACGME proposed program requirements for EM intended to prepare trainees for successful practice for the next 25 years.12 If the proposed change in program length occurs, which would require
Table 1. Results from the emergency medicine Match 2020-2025.
Figure 3. MD United States;
all programs to provide 48 months of training, it could transiently dampen interest in EM as a specialty for some students, specifically those who come from lower socioeconomic status or prioritize lifestyle and income. While this may make EM less competitive in the short term, the numbers will likely rebound in future years with a potential shift in the type of applicants who apply, as students with greater commitment to EM will likely still choose the specialty.
Studies of US allopathic school seniors who chose or considered EM as a specialty cited various factors that played a role in their ultimate choice. These included lifestyle factors,13 concerns regarding the unpredictability of shiftwork, lack of flexibility in practice setting and scope, mistreatment and violence against ED staff, a potentially diminishing job market for graduates, burnout and career longevity, EM’s standing in the healthcare landscape, 14 and negative experiences of women clinicians who were perceived as not fitting the “EM stereotype.”15 A common thread to these studies is that a student’s EM clerkship experience significantly impacts their ultimate decision to pursue EM. Therefore, emergency clinicians and educators have a unique opportunity to leverage their interactions with medical students on their EM clerkship to share experiences and perspectives on these factors, while highlighting the positive, mission-driven, and serviceoriented aspects of our specialty.
Emergency medicine continues to see an increase in the number of positions offered compared to the growth in the number of applications, resulting in unfilled positions. Confidence in the job market did improve in 2022, with 92% of physicians reporting a high likelihood of finding a job. 16 However, concerns about a potentially diminishing job market in the future for emergency physicians persist from the physician workforce report published four years ago, 3 with only 50% of physicians reporting a high likelihood of finding a desirable job and 44% reporting high confidence in a future job.16 In light of continued uncertainty, the EM workforce may benefit from limiting the expansion of class sizes and the creation of new programs over the short term, except in non-metro areas where there are consistent estimates of physician shortages. 17
CONCLUSION
The number of unfilled positions continued to decrease in 2025 from the peak in 2023. The positions filled by US MD seniors remain mostly stagnant as compared to 2021 levels. Leaders in emergency medicine remain cautiously optimistic after a successful 2025 Match. However, to maintain the interest of medical students, EM must maintain momentum to keep the job market sustainable and clinical practice fulfilling for current and future physicians. Address for Correspondence: Alexander Y. Sheng, MD, MHPE,
Warren Alpert Medical School at Brown University, Department of Emergency Medicine, 55 Claverick St. Suite 100, Providence, RI 02903. Email: alexander_sheng@brown.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Sheng et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. National Resident Matching Program. Match Data. 2025. Available at: https://www.nrmp.org/match-data/. Accessed April 6, 2025.
2. Sheng AY, Gruppuso PA, Suner S, et al. The 2023 emergency medicine Match: alarming symptom of a health care system in crisis. AEM Educ Train. 2024;8(1):e10947.
3. Marco CA, Courtney DM, Ling LJ, et al. The emergency medicine physician workforce: projections for 2030. Ann Emerg Med. 2021;78(6):726-37.
4. American College of Emergency Physicians. ACEP Joint Statement on the Emergency Medicine 2023 Match Results. 2023. Available at: https://www.acep.org/news/acep-newsroom-articles/joint-statementmatch-2023/. Accessed November 25, 2024.
5. Lassner JW, Ahn J, Singh A, et al. Growth of for-profit involvement in emergency medicine graduate medical education and association between for-profit affiliation and resident salary. AEM Educ Train. 2022;6(4):e10786.
6. Preiksaitis C, Krzyzaniak S, Bowers K, et al. Characteristics of emergency medicine residency programs with unfilled positions in the 2023 Match. Ann Emerg Med. 2023;82(5):598-607.
7. Gettel CJ, Bennett CL, Rothenberg C, et al. Unfilled in emergency medicine: an analysis of the 2022 and 2023 Match by program accreditation, ownership, and geography. AEM Educ Train. 2023;7(4):e10902.
8. Kiemeney M, Fisher J, Calaway N, et al. Emergency medicine shows rebound in 2024 residency Match. ACEP Now. 2024. Available at: https://www.acepnow.com/article/2024-match-week/#. Accessed November 25, 2024.
9. American College of Emergency Physicians. Workforce Considerations: ACEP’s Commitment to You and Emergency Medicine. 2021. Available at: https://www.acep.org/siteassets/sites/ acep/media/workforce/workforce-report-brief-summary.pdf. Accessed June 4, 2025.
10. Adelman L, Fisher J, Dark C. Unpacking the 2023 Match Week. 2023. Available at: https://www.acepnow.com/article/a-profession-inperil/. Accessed April 23, 2025.
11. Rose C, Landry AI, Bowers KM. Will there be any emergency doctors to see you in the future? 2023. Available at: https://www.statnews. com/2023/03/20/emergency-medicine-residency-positions-unfilledthe-match. Accessed April 20, 2025.
12. Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Emergency Medicine: Summary and Impact of Major Requirement Changes. [Publishing Year]. Available at: https://www.acgme. org/globalassets/pfassets/reviewandcomment/2025/110_ emergencymedicine_impact_02122025.pdf. Accessed April 5, 2025.
13. Keith KC, Smith E, Reddy S, et al. Lifestyle factors and other influences on medical students choosing a career in emergency medicine. AEM Educ Train. 2020;5(1):37-42.
14. Akhavan AR, Kontrick AV, Egan H, et al. “Cold feet”: a qualitative
study of medical students who seriously considered emergency medicine but chose another specialty. AEM Educ Train. 2024;8(2):e10967.
15. Diaz R, Balgord S, Klekowski N, et al. Understanding clerkship experiences in emergency medicine and their potential influence on specialty selection: a qualitative study. AEM Educ Train. 2024;8(1):e10932.
16. Olson AS, Li Sauerwine S, Kraut AS, et al. Perceptions of the current and future emergency medicine workforce. J Am Coll Emerg Physicians Open. 2024 Aug 25;5(5):e13279.
17. HRSA Workforce. Physician Workforce: Projections, 2022-2037. 2024. Available at: https://bhw.hrsa.gov/sites/default/files/bureauhealth-workforce/data-research/physicians-projections-factsheet.pdf. Accessed April 5, 2025.
Burnout in the Emergency Department: Survey of Prevalence and Modifiable Risk Factors
Matthew Kraus, BS* Michelle Fischer, MD, MPH†
Penn State College of Medicine, Hershey, Pennsylvania Penn State College of Medicine, Department of Emergency Medicine, Hershey, Pennsylvania
Section Editors: Jeffrey Druck, MD, and Monica Gaddis, PhD
Submission history: Submitted June 17, 2024; Revision received February 27, 2025; Accepted April 4, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.24872
Introduction: We assessed the prevalence of burnout syndrome among emergency physicians and advanced practice practitioners (APP) in an academic emergency department (ED) to identify demographic and lifestyle factors associated with burnout.
Methods: We administered a cross-sectional survey including the Maslach Burnout Inventory (MBI) with a demographic/lifestyle component to emergency physicians, residents, and APPs at an academic ED. We reported descriptive data and performed chi-square analysis to identify significant variables, followed by logistic regression to quantify their effects. A factor count was performed to assess for additive effects of burnout risk factors.
Results: We collected 55 surveys (60% response rate) yielding an overall burnout prevalence of 52.7%. The following had a significant association with burnout: 0-6 days off per month; fewer than two major hobbies; thoughts of quitting one’s job “at least some of the time”; and spending less than four hours outdoors per week. Zero to six days off per month was associated with 4.70 times more burnout compared to ≥7 days off per month (95% confidence interval [CI] 1.24-17.82). Participants who met 3-4 vs 0-2 of the previously mentioned conditions had a 6.87 times increased burnout prevalence (95% CI 2.01-23.52).
Conclusion: This preliminary study highlights four unique factors associated with burnout. It also demonstrates that a specific number of days off may reduce burnout prevalence. Emergency department wellness efforts should consider focusing on strategically scheduling time off each month while encouraging individual habit generation and time spent outdoors to maximize burnout protection. Further research is needed to evaluate the efficacy of the proposed interventions. [West J Emerg Med. 2025;26(5)1397–1403.]
INTRODUCTION
The Maslach Burnout Inventory (MBI) defines burnout as a syndrome composed of three types of feelings: emotional exhaustion (EE); depersonalization (DP); and low sense of personal accomplishment (PA).1 Emotional exhaustion refers to feelings of mental fatigue and overextension from one’s work. Depersonalization refers to an unfeeling and impersonal response to recipients of one’s care. Personal accomplishment refers to feelings of competence and success within one’s area of work.1 The prevalence of burnout among US physicians is
elevated compared to the general US population (37.9 vs 27.8%).2 Burnout remains an ongoing area of concern as its effects are significant for physicians and their patients.3,4
Two concerning patient consequences, increased susceptibility to medical errors and lower quality care, have direct effects on patient safety and satisfaction.3
Consequences of physician burnout include depression, substance use disorder, poor habit generation, and suicide.3,4 Burnout has negative effects on the entire medical system as it leads to increased physician turnover and reduced
productivity.3 Emergency medicine (EM) consistently ranks among the highest in reported rates of burnout among medical specialties4,5,6,7 and has the highest burnout rate (65%) according to a recent Medscape Physician Lifestyle and Happiness Report.6 (Note that this report’s discussion reflects the presumed impact of the COVID-19 pandemic on these results.)
Unlike most specialties where hours worked directly correlate with increased burnout, emergency physicians experiences high burnout despite working fewer overall hours than those in many other specialities.4 This phenomenon may be partially explained by stressors that are unique to EM such as caring for multiple high-acuity patients simultaneously, frequent task-switching, patient and colleague rudeness, litigation stress, sleep-schedule switching, and being faced with constant uncertainty.4 Multiple studies have shown that factors associated with burnout include younger age or junior status, number and duration of night shifts, increased workload, acuity of care, decreased resilience, and a desire to quit one’s current job.5,7,8,9 There is less existing research focused on the additive effect of multiple burnout risk factors. Furthermore, prior studies have not shown a specific number of days off that markedly reduces burnout prevalence.
Our goal in this study was to identify the prevalence of burnout among attending physicians, residents, and advanced practice practitioners (APP) within a single, large, academic emergency department (ED). We sought to compare rates of burnout stratified by level of training and compare them to prior studies while correlating rates of burnout with lifestyle factors to identify interventions for burnout reduction.
METHODS
We employed a cross-sectional study design using a validated survey tool, the 22-item Maslach Burnout Inventory Human Services Survey for Medical Professionals (MBI-HSSMP) and a paired 24-item demographic and lifestyle factor survey that was created for this research. The study was submitted to an institutional review board and was deemed exempt due to lack of inclusion of identifying information. The survey was performed between September 2022–January 2023 within the ED at a single, large, academic medical center with a volume of over 80,000 visits per year and a three-year, Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program in the northeastern United States.
The survey was offered voluntarily to approximately 90 attending physicians, residents, and APPs within the ED. The primary outcomes were scores in the three domains of the MBI. A yes/no categorization of burnout presence was completed by defining burnout as a high-range score in either the EE or DP domains of the MBI. Although no formal method of characterizing the presence or lack of burnout exists according to the MBI, many prior studies using the MBI share this unofficial definition. The other variables measured
Population Health Research Capsule
What do we already know about this issue? Burnout is more prevalent among physicians than the general population and more prevalent among emergency physicians compared to other medical specialties.
What was the research question? What demographic and lifestyle factors in isolation or combination are associated with burnout?
What was the major finding of the study? Having 3-4 vs 0-2 of the identified risk factors increased burnout prevalence by 6.87 times (P=.0013, 95% CI 2.01-23.52).
How does this improve population health?
Recognizing key drivers of burnout among emergency physicians is essential to tailoring appropriate interventions to prevent and remedy burnout.
by the survey included demographic and lifestyle factors. A full copy of the survey is available upon request. We collected and managed survey data using Research Electronic Data Capture (REDCap)10 tools hosted at Penn State Hershey Medical Center. The survey was disseminated via email and QR codes posted in the ED. Emails were sent twice to all potential participants, and an announcement was made at a resident conference, attending physician meeting, and APP meeting to increase participation.
Statistical Analysis
We chose to group responses for continuous variables such as weekly hours worked, salary, etc, by combining them into five ranges of values equally spread across a range of values estimated to include most survey responses. To analyze the association of these variables with burnout, we analyzed burnout prevalence on either side of cutoffs marked by these ranges. Statistical analysis was performed using SAS v9.4 (SAS Institute Inc, Cary, NC).
We reported descriptive statistics for burnout prevalence and performed chi-square analysis to assess for association of demographic or lifestyle variables with burnout prevalence using relative risk. A multivariate binary logistic regression model was developed using the four variables with P-values <.05 in the univariate chi-square analysis. Given 55 study
subjects, the rule of 10 supported inclusion of four variables in the model. To assess for strength of the model, we generated a receiver operator curve (ROC) and calculated the area under the curve (AUC). For the final model we calculated sensitivity, specificity, likelihood ratios, positive predictive value, and negative predictive value. A chi-square analysis with odds ratio calculation was completed to assess for an association between the number of burnout covariates an individual reported and the prevalence of experiencing burnout.
RESULTS
A total of 55 survey results were collected from 26 residents, 20 attending physicians, and 9 APPs for an overall response rate of approximately 60%. The demographics of the respondents are reported in Table 1. Of the individuals surveyed, 52.7% met the criteria for burnout. The mean scores and standard deviations of the whole cohort for EE, DP, and PA were 25.7 ± 11.2, 10.5 ± 6.1, and 34.6 ± 8.0, respectively. Table 1 displays the overall burnout prevalence and the prevalence across the three burnout domains. Higher EE and DP and lower PA scores indicate a higher degree of burnout.
The burnout rates among residents, attending physicians, and APPs were similar at 50.0%, 55.0%, and 55.6%, respectively (P=.93). Residents yielded the highest DP scores (11.6 ± 7.8) while APPs had the highest EE scores (27.1 ± 7.3) and lowest PA scores (32.2 ± 5.3); however, these differences were not statistically significant (P=.46, P=.42, P=.29). Chi-square univariate analysis for possible burnout predictors showed four variables with a significant relationship to burnout prevalence (Table 2): having 0-6 days off per month (relative risk [RR] (relative risk) 1.94, 95% confidence interval [CI] 1.01-3.73), less than two major hobbies (RR 1.71, 95% CI 1.04-2.82), thoughts of quitting one’s job “at least some of the time” (RR 1.71, 95% CI 1.04-2.82), and spending fewer than four hours outdoors per week (RR 1.80, 95% CI 0.94-3.44). Although the CI for time outdoors per week crosses one, the P-value was noted to be significant at P=.0466 and, therefore, we included the variable in the multivariate logistic regression model.We created a multivariate binary logistic regression model to further assess the effect of these four variables on burnout (Table 3).When controlling for hobbies, time spent outdoors, and thoughts of quitting, number of days off per
APP, advanced practice practitioner.
Table 1. Study demographics and burnout prevalence.
Table 2. Association of burnout with demographics and lifestyle factors univariate analysis.
Table 2. Continued
*P-values are considered significant if <.05 to warrant inclusion in multivariate model.
**Chi-square P-value not calculated due to expected value <5. RR, relative risk; CI, confidence interval; OR, odds ratio.
month was found to be a significant predictor of burnout (adjusted OR 4.70, 95% CI 1.24-17.82). Greater than seven days off per month did not confer additional reduction in burnout prevalence. Other predictors did not have significant contribution to the model when controlled for other predictors. A ROC demonstrated a fair-to- good performance of the model (AUC 0.794, P<.0001, 95% CI 0.676-0.913) (Figure).
The model demonstrated a sensitivity of 79.3%, specificity of 61.5%, positive likelihood ratio of 2.06, negative likelihood ratio of 0.34, positive predictive value of 69.7%, and negative predictive value of 72.7%. The likelihood ratios indicate fair efficacy of the model in adjusting pre-test probability. If using 0-6 days off per month, < two major hobbies, thoughts of quitting “at least some of the time,” and < four hours spent outdoors per week as risk factors for burnout, chi-square analysis indicates that having 3-4 vs 0-2 of these conditions increased burnout prevalence by 6.87 times although the CI was notably wide (95% CI 2.01-23.52). This indicates that possessing more risk factors for burnout increases the likelihood that they will screen positive for burnout by the MBI.
DISCUSSION
This study demonstrated a burnout rate of 52.7% among emergency attending physicians, residents, and APPs at a single, large, academic ED, which is comparable to rates reported in prior studies.11,12,13,14 In a study of French ED staff
conducted by Moukarzel et al, 50.7% of emergency physicians met criteria for burnout.11 This was based on the definition of burnout as a high-range score in EE or DP, which has been used in several other studies but remains without clear consensus.11 A review article by Arora et al found emergency physician burnout rates to range between 60-65% using the MBI.12 Another review by Zhang et al showed that among 1,255 emergency physicians, 40% and 41% possessed high scores in EE and DP, respectively.13
Takeyesu et al performed a study among EM resident physicians and detected a burnout rate of 65%.14 They also determined that having a spouse or significant other, poor global job satisfaction, lack of administrative autonomy, lack of clinical autonomy, and intolerance of uncertainty were associated with increased burnout.14 We found no significant difference in the overall burnout rate or the various burnout domains (EE, DP, and PA) among the subpopulations of attending physicians, residents, and APPs. There was a trend toward residents displaying the highest depersonalization levels while APPs displayed the highest emotional exhaustion and lowest personal accomplishment levels, but these differences were not statistically significant.
This study identified four unique factors that showed an association with burnout: 0-6 days off per month, having < two major hobbies, having thoughts of quitting, and spending < four hours outdoors per week. Days off per month was the most significant variable contributing to burnout prevalence in
Table 3. Multivariate logistic regression model.
OR, odds ratio; CI, confidence interval.
our multivariate model. Prior studies have associated emergency physician burnout with a desire to quit one’s job, junior- learner status, and increased shift number and duration,7,11 which is partially congruent with our results. There appeared to be an additive effect on burnout prevalence when an individual reported more than one of these factors. In our study, an individual having 3-4 of the factors had seven times the risk of burnout when compared to having ≤2. Additional studies are required to validate these variables and assess their additive effects.
Burnout is highly prevalent in EM. Prior studies suggest that the most useful burnout inventories are completed on the departmental level to create interventions based on that department’s unique burnout profile. Examples of different burnout profiles include the disengaged type (high DP), overextended type (high EE), and ineffective type (low PA).15 This profile would be reflected by targeted feedback from members of the department’s workforce or collection of specific MBI survey data. In a recent article, Guille et al conclude that due to variation in measurements of burnout, assessment of depression may be a more fitting method of assessing healthcare workers’ well-being, which was supported by further correspondence with Bianchi.16,17
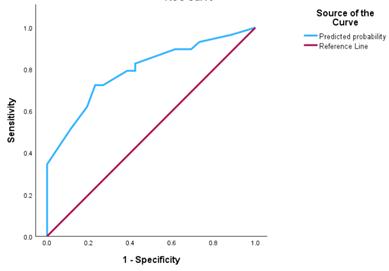
Figure. Receiver operator curve for multivariate model performance in a study on physician burnout in the emergency department. ROC, receiver operator curve.
While many risk factors may be universal to EM, department-specific factors may be easier to intervene upon. Montgomery et al suggested that optimizing the relationship between institutions and employees by empowering employees to have increased control over their work environment is helpful in reducing burnout.15 This is consistent with other literature related to burnout, which frequently suggests that burnout is inversely related to an individual’s sense of personal control or autonomy. This concept is highlighted by the findings of Takayesu et al, which associated EM resident physicians’ lack of administrative and clinical autonomy with increased burnout.14 There is evidence to suggest that systems-based interventions are far superior to suggestions of individual behavior modification when striving to reducing the rate of burnout.18 Additionally, departmental efforts focused on encouraging increased time spent outdoors and hobby generation may have direct effects on decreasing healthcare burnout.
Our study suggests that creating clinical schedules with at least seven days off per month may minimize burnout in EDs and should be implemented whenever possible. Regarding resident schedules, it may be necessary to consider a modification to the current ACGME work-hour rules to minimize burnout. Building in a minimum number of seven days per month with no scheduled clinical or didactic work could be a beneficial change from the current 24-hour free period that is required on a weekly basis. To accomplish this, EM programs may be required to assign more residents to ED-specific rotations simultaneously to fulfill necessary coverage of shifts. While such an intervention may be beneficial to EM residents, we recognize that its implementation would be challenging and that other factors must be optimized to improve the status of burnout in the ED. Guille et al highlight that in addition to high volumes of work hours, the actual workload and documentation responsibilities are key contributors to burnout.16 Individual departments and residency programs should focus on tailoring interventions to the specific feedback of their workforce in a way that prioritizes employee autonomy, multidimensional wellness, and specific elements of employee burnout profiles if collected.
LIMITATIONS
This study’s cross-sectional survey nature is an inherent limitation as it could not demonstrate causality. This study was
Kraus et al.
also limited by a self-selection bias due to voluntary participation. The single-center nature of this study may decrease external validity, particularly for EDs with volume and structure that is different from our institution. “Number of days off per month” were initially recorded in grouped ranges in our survey and may have biased respondents into choosing a middle value such as “4-6” without explicitly comparing to their true schedules. This study was also performed with a small sample size and was likely underpowered to detect additional significant associations of lifestyle factors with burnout prevalence. Additional risk factors associated with burnout may have been discovered with increased sample size and power.
Address for Correspondence: Matthew Kraus, MD, ChristianaCare, Emergency Medicine/Internal Medicine, 4755 Ogletown-Stanton Rd, Newark, DE, 19718. Email: matthew. kraus@christianacare.org.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Kraus et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Maslach C, Jackson SE. Maslach Burnout Inventory Manual, 4th ed. Menlo Park, CA: Mind Garden, Inc 2018; 1-2.
2. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
3. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516-529.
4. Stehman CR, Testo Z, Gershaw RS, et al. Burnout, drop out, suicide: physician loss in emergency medicine, Part I [published correction appears in West J Emerg Med. 2019 Aug 21;20(5):840-841]. West J
Emerg Med. 2019;20(3):485-494.
5. Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13(11):e0206840.
6. Medscape Physician Lifestyle and Happiness Report 2023. Available at: https://www.medscape.com/sites/public/lifestyle/2023. Accessed November 24, 2023.
7. Kansoun Z, Boyer L, Hodgkinson M, et al. Burnout in French physicians: a systematic review and meta-analysis. J Affect Disord 2019;246:132-147w
8. West CP, Dyrbye LN, Sinsky C, et al. Resilience and burnout among physicians and the general US working population. JAMA Netw Open. 2020;3(7):e209385.
9. Ramírez-Elvira S, Romero-Béjar JL, Suleiman-Martos N, et al. Prevalence, risk factors and burnout levels in intensive care unit nurses: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(21):11432.
10. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
11. Moukarzel A, Michelet P, Durand AC, et al. Burnout syndrome among emergency department staff: prevalence and associated factors. Biomed Res Int. 2019;2019:6462472.
12. Arora M, Asha S, Chinnappa J, et al. Review article: burnout in emergency medicine physicians. Emerg Med Australas 2013;25(6):491-495.
13. Zhang Q, Mu MC, He Y, et al. Burnout in emergency medicine physicians: a meta-analysis and systematic review. Medicine (Baltimore). 2020;99(32):e21462.
14. Kimo Takayesu J, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emerg Med. 2014;21(9):1031-1035.
15. Montgomery A, Panagopoulou E, Esmail A, et al. Burnout in healthcare: the case for organisational change. BMJ. 2019;366:l4774.
16. Guille C, Sen S. Burnout, depression, and diminished well-being among physicians. N Engl J Med. 2024;391(16):1519-1527.
17. Bianchi R. Burnout, depression, and diminished well-being among physicians. N Engl J Med. 2025;392(3):311-312.
18. Stehman CR, Clark RL, Purpura A, et al. Wellness: combating burnout and its consequences in emergency medicine. West J Emerg Med. 2020;21(3):555-565.
Emergency Medicine Residents’ Perceptions of Geriatric Emergency Medicine and Careers: A Qualitative Study
Katherine Selman, MD*
Abigail E. Jones, BS†
Christina Curran, BS‡
Lauren Cameron-Comasco, MD§
Wendy C. Coates, MD||
Angel Li, MD#
Katren Tyler, MD¶
Fernanda Bellolio, MD, MS**
Shan W. Liu, MD, SD†
Section Editor: Stephen Meldon, MD
Cooper Medical School of Rowan University, Cooper University Health Care, Department of Emergency Medicine, Camden, New Jersey
Harvard Medical School, Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts
University of California Irvine School of Medicine, Irvine , California
Oakland University William Beaumont School of Medicine, Corewell Health William Beaumont University Hospital, Department of Emergency Medicine, Royal Oak, Michigan Geffen School of Medicine, University of California, Department of Emergency Medicine, Los Angeles, California
The Ohio State University, Department of Emergency Medicine, Columbus, Ohio University of California Davis School of Medicine, Sacramento , California
Mayo Clinic, Department of Emergency Medicine, Rochester, Minnesota
Submission history: Submitted January 27, 2025; Revision received May 23, 2025; Accepted July 21, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.42061
Introduction: Geriatric emergency medicine (GEM) has emerged as a subspecialty of emergency medicine (EM) with seven fellowships available throughout North America and opportunities for career development in administration, clinical leadership, education, and research. Our objective in this study was to ascertain the perspectives and understanding of the subspecialty among EM trainees.
Methods: We recruited participants from four geographically diverse institutions. Three institutions were academic and had GEM faculty or divisions, and the fourth institution was a community site without geriatric-specific faculty. We conducted semi-structured interviews, adapted from a prior protocol, via teleconferencing and subsequently transcribed them. Codes were generated by two investigators and categorized into themes derived from the data.
Results: Seventeen trainees with an average age of 32.1 years across four institutions participated in the study. Three themes emerged, demonstrating that trainees’ perceptions of GEM were affected by 1) education and exposure; 2) perception of geriatrics; and 3) future career considerations. Trainees with exposure to GEM had greater appreciation for the specialty, but their understanding of career opportunities was mixed. Participants acknowledged broader clinical and social considerations for older adults and in general felt that specialty training would benefit older patients. However, most participants had no personal interest in pursuing GEM, with reasons for disinterest including belief that they would only see older patients, dislike of geriatric complexity, and uncertainty about GEM as a career. Many participants identified educational opportunities for GEM, including noting that curricula include dedicated time for other subspecialties such as pediatrics but not geriatrics. Fellowship decisions were influenced by duration of training, salary, job opportunities, practice settings, and career goals.
Conclusion: Emergency medicine trainees who participated in semi-structured interviews overall viewed geriatrics as an important aspect of EM with perceptions formed from exposure and education at both the institutional and individual level, perceptions of treating older adults, and future career considerations. However, interest in pursuing GEM was overall low, and participants expressed uncertainty about the subspecialty and career options, indicating opportunity for increased awareness, education, and mentorship. [West J Emerg Med. 2025;26(5)1404–1413.]
INTRODUCTION
Despite an anticipated 50% increase in demand for geriatricians due to growth of the older adult population in the United States, the number of geriatricians is projected to decrease.1 Older adults disproportionately use the emergency department (ED) and are more likely to receive imaging, laboratory testing, and admission to intensive care units.2,3 Furthermore, older emergency patients are more likely to have non-classic symptoms of serious diseases, polypharmacy, and cognitive impairment, considerations which if overlooked, can result in poor outcomes including inappropriate dispositions, adverse drug reactions, delayed diagnoses, or missed elder mistreatment.4 In response to these trends, geriatric emergency medicine (GEM) has emerged as a subspecialty for emergency clinicians to address the unique physiologic and social needs of older patients presenting for acute care.5
Geriatric emergency department (GED) innovations and accreditation via the American College of Emergency Physicians have expanded rapidly since publication of GED guidelines in 2013. Dedicated GEDs have been shown to decrease hospital length of stay and Medicare costs, indicating a crucial niche for emergency clinicians.6,7 In 2010, the Geriatric Competencies for EM residents were published to identify the key concepts in GEM for residents to master and to provide a basis for GEM curricula.8 Educational interventions based on these competencies have demonstrated improvement in geriatric knowledge and decision-making for emergency physicians at all levels of training.9,10,11 Seven fellowships in GEM are available in North America for further training with both one- and two-year options.12 Fellowship graduates in GEM have reported that fellowship training was helpful for career advancement applicable to both community and academic settings with opportunities for positions in research, education, and administration.13
Among emergency physicians, older patients are perceived as more difficult than younger patients with a higher burden of care.14,15 From the patient perspective, older adults’ experiences in the ED are marred by ageism and failure to accommodate for age-related changes or to address the needs of older adults.16 Prior research has demonstrated a perception among internal medicine trainees that geriatrics is less prestigious than other subspecialties, and there is a lack of support or enthusiasm from colleagues and mentors.17 While EM residents overall view older patients favorably, this attitude attenuates with each training year, and most GEM fellowship positions are unfilled each year.18
Despite advances in GEM and opportunities for career development within the subspecialty, little is known about EM trainees’ perceptions of the field or their experiences working with older adults, including formal GEM training during EM residency. To develop the most effective framework for training and patient care for the growing geriatric population, it is critical to understand EM trainees’ authentic experiences with and attitudes toward the aging population, the subspecialty of GEM, and factors that influence a decision to pursue a career in GEM.
Population Health Research Capsule
What do we already know about this issue? With a rising older population, geriatric emergency medicine (GEM) has emerged as a subspecialty to address the unique needs of older patients presenting for acute care
What was the research question? We sought to determine EM trainees’ experiences, understanding, and attitudes toward geriatrics in GEM.
What was the major finding of the study? Participants overall viewed geriatrics as an important aspect of EM, but their interest in pursuing GEM as a subspecialty was low.
How does this improve population health? Improved understanding of EM trainees’ views on geriatrics provides future direction to address gaps in training and to elucidate GEM career opportunities.
METHODS
We followed the checklist of Standards for Reporting Qualitative Research.19 This was a prospective, groundedtheory, qualitative study using an interpretivist paradigm, consisting of individual semi-structured interviews of residents in postgraduate years (PGY) 2 or 3 and recent graduates at geographically diverse institutions in the United States, three with an available GEM fellowship and one community-based site. We selected upper-level residents and recent graduates as it was expected that they would be actively considering subspecialties and career paths, including graduates pursuing GEM fellowships, for insight into their career choices. Participants were identified by convenience and purposive sampling on a volunteer basis. In the recruitment letter, participants were offered a $40 gift certificate or check upon interview completion. Interviews continued until thematic saturation was reached. This project was deemed exempt by the Massachusetts General Hospital Institutional Review Board.
We adapted the interview protocol from Raj et al, 2021 (Supplement 1).17 The interview was divided into five sections: 1) early exposures to medicine and family support; 2) current experiences as an EM trainee; 3) career goals including subspecialty selection; 4) identity as a physician and meaning in medicine; and 5) conceptualization of GEM and ideas for generating interest in GEM. Interviews were conducted via
teleconferencing by two undergraduate students AEJ and CC who had no prior relationship with participants and were trained by the study author SWL who has published multiple qualitative studies. Interviews lasted 30 to 45 minutes.
Interviews were recorded and transcribed using an automated transcription service (TranscribeMe, Inc, San Francisco, CA), and identifiable information was redacted prior to analysis. No repeat interviews were deemed necessary, and transcripts were not returned to participants. Codes were generated inductively by reading primary data and deductively from experience and grounded theory. Two study investigators KS and SWL read all transcripts independently. They then discussed common themes and ideas generated from first reading. Codes were then extracted and categorized into themes derived from the data (Figure S1).
RESULTS
Seventeen EM trainees participated in full interviews of 114 eligible to participate. Participants had a mean age of 32.1 years, and 41.1% were female (Table 1). Fifteen participants were EM residents or recent graduates not pursuing GEM, and two participants were recent GEM fellowship graduates. Three general themes emerged from the interviews: 1) education and exposure to geriatrics; 2) perception of geriatrics and GEM as a subspecialty; and 3) career considerations.
Age, mean in years
Sex, n (%)
Male 8 (47.0) Female 7 (41.2) Missing 2 (11.8)
Stage in training, n (%)
PGY-2 7 (41.2)
PGY-3 6 (35.3) Recent graduate 2 (11.7)
GEM fellowship graduate 2 (11.7)
Residency training setting, n (%)
Academic 12 (70.6)
Community 5 (29.4)
PGY, postgraduate year; GEM, geriatric emergency medicine.
Education and Exposure
Patient and family exposure. Participants described various experiences that contributed to their journeys as physicians and their views on older adults. Two participants had physician parents, and three participants described their own families as influences on their medical careers and perspectives:
One of the other things growing up was relationships with my grandparents and watching them get older and then pass away eventually. That process was unique and formative. Unidentified Interviewee (UI)-13
Another participant acknowledged that they did not have this relationship with older family members and felt that this influenced their experiences with older adults as patients.
He [husband] had a wonderful relationship with his grandmother, and she was one of the most important people in his life. I think that a lot of the times when he’s interacting with older folks, there’s definitely that memory and that strong natural affinity towards older folks. I didn’t grow up with grandparents and they all passed away. So, I never really had exposure to older folks until I got to medicine. UI-16
Similarly, participants described the influence that patients have had on their views. In some cases, this was presented as a contrast between the EM role and the perception of what was best for the patient. This was sometimes viewed as a conflict when participants recognized that the perceived traditional EM objectives of resuscitation and interventions may not align with patient-centered outcomes.
In emergency medicine, we can have patients coming in with a code, and our goal is to resuscitate them to the best of our ability. And a lot of times, for me, personally, just getting them back is not enough. Because a lot of times, you get them back, but then they have some chronic debilitating issue that they have to deal with […]. For me, it’s very much about what does the patient want and how do we get them to that point? UI-1
Participants expressed the patient encounters and aspects to their jobs that help them feel fulfilled, including several emphasizing the importance of patients feeling heard and being able to connect and to communicate meaningfully with patients. Participants also described helping patients feel better, providing reassurance, finding the cause of symptoms as personally satisfying (Table 2).
Institutional education and exposure. Five of 17 participants recalled being exposed to geriatrics as a field in medical school, including both participants who completed a GEM fellowship; only one participant reported geriatrics was a mandatory rotation during medical school. Four participants described their geriatrics rotations in medical school positively. One participant tailored their residency search
Table 1. Characteristic of emergency medicine trainees who participated in a qualitative study gauging career interest in geriatric emergency medicine.
Participants on what patient outcomes help them feel fulfilled
Addressing patient concerns and ensuring understanding
When I feel like they feel like I listen to them and address their concerns, and they understand what’s coming next. UI-4
I think that’s why a lot of us enter emergency medicine. We want to be able to handle those life-or-death situations. And I find that empowering, and then the second is we see a lot of folks that are worried about certain things that they don’t know who to go to and…being able to provide that reassurance is meaningful to me as well. UI-6
I think when you feel that they feel that they’ve been heard, like sometimes it’s like busy shifts and you know you’re not doing your patient justice sometimes, unfortunately like you’re just doing your best to just sort of stay afloat in a department that’s crazy busy and you’re just trying to do your best and there are times when you really feel like you’ve been able to explain everything in detail and provide all the follow-up information and resources and really walk your patient through everything and you really feel like you did right by them and that they acknowledge that and I think that’s those are probably the better moments in a sometimes challenging and really busy emergency department. UI-8
Addressing the patient’s underlying problem
In an ideal world, if you could figure out what’s exactly going on, that would be the best thing. But I feel like in emergency medicine, if you can help treat someone’s pain or make sure that whatever their problem is that day is not going to kill them immediately, then I feel like I’m fulfilling my role as their emergency physician. UI-13
What I enjoy that doesn’t always happen in EM is I really like when I have a sense of what’s happening with my patient. Sometimes the workup can be in process, but we don’t always have a clear answer of what’s going on. I find it really satisfying, though, when I can find the answer and when I know what’s causing their symptoms or their illness. I like that because then I feel more confident in the treatment that I’m giving them. And then, too, I feel more grounded in the recommendations I’m making or the discussions I’m having with family about what I think next steps may be. I find it less satisfying when somebody is really sick and we’re not sure why. I find that harder for the patient, for the family, for us. UI-17
Definitely when I can help them on that first visit and whether or not they leave the department … feeling better. That makes me feel like I did something … Also I enjoy being able to stabilize patients and be the first one to at the very least help them in probably what is a difficult time in their life, maybe one of [the] worst days of their life. UI-7
Gaps in education I think it’s a huge gap in training to not have specific geriatric principles. I don’t know that everyone needs to do a fellowship, but I think integrating more of those principles into the training pipeline, both in medical school and in residency, will only strengthen the emergency workforce. It’s not a unique thing to academic centers to have older populations. Almost every emergency department [patient population] is getting older. So, it’s definitely a skill set that will be needed if we’re going to keep up and keep providing good care. UI-9
UI, Unidentified Interviewee.
on availability of geriatrics programs following third-year clerkships in medical school.
In medical school, I had a fourth-year geriatrics rotation. It was medicine-based, not emergency-based, but it was a really cool rotation. We got to do a lot of homebased care. So, driving out to either assisted living facilities or patients’ homes, doing an
assessment of what their home environment was like, doing medication reviews, looking at what they were on, how we could pare down medication lists. I really liked that approach to care, but I had no specific exposure to geriatric emergency care. And in fact, it wasn’t something that I knew existed until I started poking around on my own towards the end of residency. UI-9
Table 2. Participant perspectives on the influences of patient exposure and education.
Participants at the community site who did not have GEM faculty or a geriatrics division at their institution overall had less awareness of the subspecialty. These participants also report overall decreased exposure to all EM specialties.
I did rotations in the emergency department, and there were geriatric patients, but I never did an explicit geriatric emergency medicine rotation or was really exposed to that as a specialty [...]. I didn’t even know it was a specialty. UI-4
In general, participants who had GEM faculty or divisions described more familiarity with GEM concepts and training. One participant discussed that seeing current fellows and faculty members in subspecialties showcase their interest in turn influenced excitement and interest in the subspecialty learning. However, even among participants at institutions with GEM exposure, some trainees felt that they were still unfamiliar with GEM, particularly as a career option.
I wonder if people with a geriatric subspecialty could […] share more about what they’re doing outside of the hospital, whether that be research work or advocacy […]. I think as a resident, a lot of times there’s a little bit of mystery in terms of what a week-to-week looks like for people in various specialties. I think, in general, more light on that would be helpful. UI-17
Many participants at both community and academic programs identified educational opportunities for geriatrics within their training programs, noting that their curricula included defined time for other subspecialties such as pediatrics and ultrasound but not geriatrics. In some cases, this was described as a didactic opportunity, whereas another participant described an opportunity for a structured rotation like other rotations within residency:
We intentionally set aside things for pediatrics every month, but we did not specifically set aside a separate time for geriatrics and we probably should have because it’s […] more than half of our population. UI-3
Regardless, participants acknowledged that improved education would improve care even if trainees were not pursuing geriatrics specifically.
Perception of Geriatrics
Broader considerations. Almost uniformly, participants acknowledged that geriatric populations have unique aspects to their care and require broader considerations in the ED.
Examples of the unique aspects of the population included appropriate medication prescribing, de-escalating interventions or considering quality of life, atypical disease presentations, delirium, and disposition considerations including discharge barriers and risks of hospitalization. Ten participants (58.8%) discussed social aspects to geriatric care. For some participants, this was an aspect of care that they felt was less emphasized in their training but would be beneficial to know more about:
Beyond the medical management, we haven’t touched on other topics like disposition, like should I go to a nursing home for a SNF [skilled nursing facility] or social determinants of health as much […]. I think the more pertinent thing is their care beyond the bedside. So, we have to think about, are they safe to go home, who lives with them, who’s their healthcare proxy; if we send them home now, where did it go? Are they safe to go home? That’s a distinction. So, for older folks, you have to be more thoughtful. Not only with their medical management, but also with their post-visit needs […]. It would be good to have more emergency physicians with a more comprehensive foundation in terms of how to manage these elderly patients beyond their immediate clinical needs. UI-6
For one participant who had gone through GEM fellowship, addressing this complexity was a key part of improved care, but even participants not interested in GEM described the importance of a more holistic approach to the care of older adults:
[T]he role of the geriatrician is actually a lot broader than I think most people realize […]. It ends up being very all-inclusive, kind of like it would be for the pediatric population, where you have an understanding that this is a vulnerable subset of people…where we have to, as geriatricians, make sure that we are giving a whole, well-rounded and allinclusive approach to their care. UI-15
Perception of geriatric EM as a subspecialty. At least one participant verbalized that they were unaware that GEM was a subspecialty available in EM. Most trainees viewed geriatric specialization in EM as necessary or beneficial for patients. Six participants specifically mentioned that having additional guidelines or algorithms for their geriatric patients would help improve their care:
I think that the specialty in general is important. The research, the literature, that can be produced that will help even the community doctor who sees the majority of
these [patients] is extremely valuable. And they certainly do present different and there is a lot of nuance in the care of a geriatric patient. UI-2
Three participants felt that it was not necessary to have a separate subspecialty. Participants expressed that older adults constitute a large proportion of their patient population and, therefore, geriatrics is already integrated into an emergency physician’s practice without the need for specialization. One participant voiced concern that separating older adults into a separate geriatric ED could result in patients not receiving appropriately aggressive interventions. However, all three agreed that specialized geriatric care was important and beneficial to patients:
I definitely think that every emergency doctor should have training in the things that affect geriatric patients as part of the bread and butter of emergency medicine […]. I think training in geriatrics is necessary as part of emergency training and maybe constitutes a significant percentage of the content that we learn as emergency doctors. As to whether that should be separated out as its own curriculum, I’m not sure. I think certainly there are things that we need to know to take care of older adults, that we also need to know to take care of certain young adults. I would hate for it to be the case that it was so separated that only some people had that training because it is so integral to our normal practice. UI-10
Despite the majority agreeing that GEM is necessary and beneficial, excepting the two participants who completed GEM fellowship, no other trainees expressed interest in pursuing GEM. For some participants, they expressed no specific disinterest in geriatrics but felt more drawn to other subspecialties. Specific reasons for disinterest in GEM include a dislike for the complexity with older adults or less satisfaction after geriatric encounters. There were also perceptions of GEM as a longitudinal care model or that GEM-trained physicians would only treat older patients, and these were cited as reasons for disinterest (Table 3).
Participants had variable perceptions of the role for physicians specializing in GEM and in some cases were unsure of exact responsibilities. Trainees also described geriatric emergency physicians acting as champions and advocates for older adults:
I feel like it would be necessary, especially with more of the proportion of the population being older adults to make sure that there
are people out there who are being more thoughtful and making sure that these adults are receiving appropriate care because I know there’s … ageism or elder bias. So, to help prevent or mitigate, lessen that bias, having champions for this specialized population to make sure there is a good standard of care for them as so many more people continue to age, and it becomes a larger proportion of people we take care of.
UI-13
Future Career Considerations
Fellowship. Participants cited several influences on fellowship considerations. For some participants, fellowship was not seen as necessary for employment outside an academic center. However, another participant interested in rural practice described how fellowship training in ultrasound or critical care could improve patient care in resource-limited areas. Two participants specifically referenced the ability to obtain board certification as influencing subspecialty selection. Some participants perceived that fellowship would not change their daily practice, whereas other participants expressed interest in fellowships that they felt would improve patient care:
I want a fellowship that gives me a tangible set of skills that makes me a better doctor. UI-17
It’s a patient population that we don’t provide the best care for in the ED, and I think there’s a lot of room with our existing science and knowledge to really improve care for these patients and make it a better experience for them. UI-11, on plans to pursue addiction medicine fellowship
Many participants mentioned the additional time that fellowship training requires, which would subsequently delay attending positions or require relocation:
Emergency programs are […] split between three years or four years. So, I’d already taken an extra year of residency training, which is a pay cut as opposed to doing a three-year residency and having a year of practice. Taking a fifth year to train, doing that fellowship, is an additional financial burden. I do have a wife and kid. […]. [T]hat definitely factors into the decision to extend my training is putting off another year of attending level pay. UI-9
Subspecialty training was also considered a way to incorporate flexibility for work-life balance in a future career.
Perception of GEM as a subspecialty physician should have at least some […] baseline competency because this is a non-trivial portion of our patient population. We’ve seen a lot of these patients. I think you definitely need a good knowledge base to really be a good physician generally. But I also think there’s a role [for] people who have a special interest in this to help educate, make sure we’re staying up to date and, at least in my view, like designing policies, protocols, and even order sets to really care for these patients. UI-11
I think it’s built into our everyday […]. There [are] different considerations that have to be taken for that subset of the population. But in that same vein, I think that there [are] special considerations that need to be had for a lot of different types of populations, right? You could probably say the same thing about women’s health or pediatric care, right? UI-15
I think that there’s increasing need in departments around the country to have a geriatric advocate to make sure that best practices are in place in emergency departments and health systems to accommodate those much like a lot. Even emergency departments that don’t have a formal pediatric department will have a pediatric advocate or someone in the group that’s helping to ensure that best practices are being followed for that population as well. UI-12
Reasons for disinterest in GEM as a career
Medical complexity I would like to say that I would consider it [GEM fellowship] because I do think it's really important. But I wouldn't [...]. Because old people talk so much. I'm trying to get information, and it's so hard […]. Generally, it's a harder population for me to work with because of my personality, and the workflow of the emergency department, and … they're complicated. They're oftentimes, not always complicated, they've lived so long, so much has happened to them medically. So, when you ask them for their medical history, there's so much to it. And just like everyone else, they don't know what's important. And you just get this dump of information and it's hard. It's like searching for a needle in a haystack sometimes to find what's important and find it in a reasonable amount of time. UI-4
Less satisfaction from encounters I think one of the reasons that I like working with pediatrics so much is because, as I mentioned, I feel like they can come into the emergency department unwell, and you can see them get better during your care of them, which sometimes is only a few hours. And I just find that so satisfying. And so maybe I haven't seen that same improvement as frequently with geriatric patients.
UI-17
Perceptions of GEM role I don’t want to just focus on the care of older adults. I want to take care of everyone in the [ED]. I want to take good care of everyone with serious illness. So, I think that’s probably the … one driver for me to not want to do that [geriatrics]. UI-5
It would not be a good fit for me because I knew for a long time that longitudinal care was not something that I was good at. And in the world of emergency medicine, geriatric care is probably the most like longitudinal medicine that there is.
UI-16
This was described in terms of having schedule flexibility, options beyond working shifts in the ED, such as working solely in a subspecialty or pursuing projects, and a proactive solution to burnout:
[O]ne day I probably may not practice emergency medicine as much and focus more like palliative care and hospice maybe in a clinic setting or a hospice setting. And so sadly, a geriatrics fellowship wouldn’t offer that same level of leaving the [ED] that I think a palliative care training would. UI-5
I think ultimately, for me, the calculation or the pros and cons were having a chance to carve out a subspecialty or a niche where I could have longitudinal projects or interests outside of just going in and working my shifts. Because I think my lifespan as an emergency physician, if I were to just go out into the community and work X number of shifts per month, I think I’d burn out fairly quickly. I think having dedicated training or a dedicated niche or subspecialty and the opportunity to continue projects in that area
Table 3. Participant perceptions of geriatric emergency medicine and reasons for disinterest.
GEM, geriatric emergency medicine; ED, emergency department.
is definitely something that will help with longevity in my career. UI-9
Future job options and opportunities. Participants had mixed responses on future job opportunities for geriatrictrained emergency physicians. Three participants described geriatrics training as a positive influence on future job options. Others expressed uncertainty about the benefit of geriatrics specialization on job opportunities, including reservation about whether geriatrics training would impact salary.
I thought about the geriatric fellowship quite a bit, both because I think it is an important population and the nuance of the care is underappreciated. But mostly, I wasn’t sure on how employable it was, like how important it would be to employers outside of academic medicine […]. I think things that dissuaded me were how employable, like how well I could market it in employment to get jobs at particular sites that I really want over […] someone else just applying. UI-12
I just don’t see it as being as much of an emphasis from institutions and from hospital levels. So, I think it’s hard to […] justify for a resident with all the debt to go to do more training to not really end up in a role that you know not being able to use those skills really in a meaningful way. UI-8
These comments paralleled some of the discussion around the role of a geriatric emergency physician in which trainees expressed uncertainty about what opportunities would be available after specialty training and what a GEM job would entail.
DISCUSSION
This qualitative study demonstrates that trainee interest in and perceptions of GEM are influenced by education and exposure from patients, family, institutions, and mentors; their own career goals; and their perceptions of geriatric medicine. While most participants acknowledged the importance of geriatric subspecialization within EM for patient care, only two participants were pursuing GEM as a career. Disinterest stems from competing interest with other subspecialties, complexity of older adults’ needs, and personal career goals. Leaders in GEM may consider proactively addressing more prevalent misconceptions such as that geriatric emergency physicians exclusively treat older adults.
Participants interviewed from institutions with GEM faculty had an appreciation for the subspecialty compared to participants who did not have exposure to GEM in their residency programs. This is consistent with prior work
among internal medicine trainees, which demonstrated that the presence of geriatricians generated interest and an understanding of the field’s importance even among residents not interested in geriatrics.17 Even among three participants who felt that GEM may not be a necessary subspecialization, all agreed it was important and all trained at institutions with GEM faculty, which may have predisposed these participants to increased comfort with GEM concepts and clinical practice. Mentors in GEM may promote interest in geriatrics, support trainees, and provide an understanding of GEM as a career path. Due to limited GEM faculty nationwide, there may be opportunities to promote virtual mentorship.
There are additional opportunities for early and ongoing exposure to geriatrics through medical training. Less than one third of EM trainees in our sample had been exposed to geriatrics as a field in medical school, but experiences from those who had had a geriatrics rotation were positive and. in two cases, influenced participants’ future career paths. Geriatric rotations address the unique physiological and psychosocial challenges geriatric patients face, emphasizing patient-centered care, managing atypical presentations, polypharmacy, and discharge planning. Trainees would benefit from this education even if not pursuing fellowship, and participants in our study felt that this could be better incorporated into the curriculum in the same way that other specialties such as ultrasound are. While there are published competencies for EM residents in GEM and these have been found to align with the American Board of Emergency Medicine (ABEM) competencies, these topics are still unevenly incorporated into curricula.8,20,21
Access to online shared resources such as the EM clerkship curriculum’s geriatrics section, virtual GEM journal club, published simulation cases, or the GEM-focused podcast GEMCast, could provide a framework for GEM education for training institutions that do not have GEM faculty.22,23,24 Incorporating GEM into curricula, in the form of structured rotations, didactics specifically on geriatric domains, geriatric case review and simulation, and quality improvement projects, both enhances care quality and meets growing demand for geriatric expertise in EDs, ensuring future emergency physicians are better prepared for the increasing number of older adults they will encounter.25,26,27 Participants reported that formal education and board certification would legitimize GEM. Currently, GEM leaders are working with ABEM to increase geriatric content, but a focused practice designation or board certification from accrediting bodies would likely further generate interest.
Participants also lacked knowledge of GEM career opportunities. Geriatric ED accreditation is expanding across the United States, and the accreditation process requires a board-certified emergency physician to act as a champion and demonstrate geriatric education.28,29 This represents a way that institutions can prioritize and support GEM, including recruiting geriatric emergency physicians and providing
protected time to spearhead geriatric initiatives. Geriatric EM is an academic discipline with viable opportunities within leadership, research, or education, as well as a focused area of clinical expertise, which trainees should be aware of when considering career development.
LIMITATIONS
This study was conducted primarily among trainees who had exposure to GEM faculty, leading to likely oversampling; only 15% of those eligible participated in interviews, leading to likely sampling bias. We attempted to minimize social desirability bias by maintaining participant’s anonymity and employing undergraduate students to perform the interviews. No PGY-4 residents were included, which may have provided different perspectives. Only two GEM fellowship graduates participated, which limited saturation of thematic analysis in this group. As with other qualitative studies, data interpretation relies on the judgment of the investigators, and the themes identified may not capture the complexities of participants’ experiences. Qualitative studies focus on understanding specific cases rather than broad generalizations. Therefore, the findings cannot be widely generalized to all EM trainees or institutions. Future studies may be useful to assess a larger sample of EM trainees or EM-applying students with more diversity in training institutions for further insight.
CONCLUSION
Emergency medicine trainees overall view geriatric emergency medicine as important and beneficial for patients; however, exempting GEM fellows in training, none expressed interest in pursuing GEM as a career. Geriatric exposure and education throughout medical training influence trainees’ perceptions of geriatrics, and career considerations including salary, schedule flexibility, board certification, knowledge of career opportunities, and misconceptions about GEM also impact trainees’ decisions.
Address for Correspondence: Katherine Selman, MD, 4401 Haddon Ave, 2nd Floor, Camden, NJ, 08103 USA. Email: selmankatherine@cooperhealth.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Selman et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Geriatrics workforce by the numbers. American Geriatrics Society. Available at: https://www.americangeriatrics.org/geriatrics-profession/ about-geriatrics/geriatrics-workforce-numbers. Accessed September 4, 2024.
2. Pines JM, Mullins PM, Cooper JK, et al. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc. 2013;61(1):12-7.
3. Ukkonen M, Jämsen E, Zeitlin R, et al. Emergency department visits in older patients: a population-based survey. BMC Emerg Med 2019;19(1):20.
4. Shenvi CL, Platts-Mills TF. Managing the elderly emergency department patient. Ann Emerg Med. 2019;73(3):302-7.
5. Hogan TM, Gerson L, Sanders AB. The history of geriatric emergency medicine. J Geriatric Emerg Med. 2023;4(2):1-21.
6. Kennedy M, Lesser A, Israni J, et al. Reach and adoption of a geriatric emergency department accreditation program in the United States. Ann Emerg Med. 2022;79(4):367-73.
7. Hwang U, Dresden SM, Vargas-Torres C, et al. Association of a geriatric emergency department innovation program with cost outcomes among Medicare beneficiaries [published correction appears in JAMA Netw Open. 2021;4(6):e2117178.
8. Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17(3):316-24.
9. Hogan TM, Hansoti B, Chan SB. Assessing knowledge base on geriatric competencies for emergency medicine residents. West J Emerg Med. 2014;15(4):409-13.
10. Biese KJ, Roberts E, LaMantia M, et al. Effect of a geriatric curriculum on emergency medicine resident attitudes, knowledge, and decision-making. Acad Emerg Med. 2011;18 Suppl 2:S92-6.
11. Hesselink G, Demirbas M, Rikkert MO, et al. Geriatric education programs for emergency department professionals: a systematic review J Am Geriatr Soc. 2019;67(11):2402-9.
12. Rosen T, Liu SW, Cameron-Comasco L, et al. Geriatric emergency medicine fellowships: current state of specialized training for emergency physicians in optimizing care for older adults. AEM Educ Train 2020;4(Suppl 1):S122-9.
13. Thatphet P, Rosen T, Kayarian F, et al. Impact of geriatric emergency fellowship training on the careers of emergency physicians. Cureus 2021;13(9):e17903.
14. Schumacher JG, Deimling GT, Meldon S, et al. Older adults in the emergency department: predicting physicians’ burden levels. J Emerg Med. 2006;30(4):455-60.
15. Carpenter CR, Lewis LM, Caterino JM, et al. Emergency physician geriatric education: an update of the 1992 Geriatric Task Force survey. Has anything changed? [abstract] Ann Emerg Med. 2008;52(4 Suppl 1):S156.
16. Goodridge D, Martyniuk S, Stempien J. At risk for emotional harm in the emergency department: older adult patients’ and caregivers’ experiences, strategies, and recommendations. Gerontol Geriatr Med
Selman et al.
Perception of GEM Careers 2018;4:2333721418801373.
17. Raj M, Platt JE, Anthony DL, et al. Exploring how personal, social, and institutional characteristics contribute to geriatric medicine subspecialty decisions: a qualitative study of trainees’ perceptions. Acad Med. 2021;96(3):425-432.
18. Hogan TM, Chan SB, Hansoti B. Multidimensional attitudes of emergency medicine residents toward older adults. West J Emerg Med 2014;15(4):511-7.
19. O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89(9):1245-151.
20. Ringer T, Dougherty M, McQuown C, et al. White Paper-Geriatric Emergency Medicine Education: Current State, Challenges, and Recommendations to Enhance the Emergency Care of Older Adults. AEM Educ Train. 2018;2(Suppl Suppl 1):S5-16.
21. Southerland LT, Willoughby LR, Lyou J, et al. Integration of geriatric education within the American Board of Emergency Medicine Model. West J Emerg Med. 2024;25(1):51-60.
22. M4 curriculum. Clerkship Directors in Emergency Medicine. Available at: https://www.saem.org/about-saem/academies-interest-groups-affiliates2/cdem/for-students/online-education/m4-curriculum. Accessed May 12, 2025.
23. Brazil V, Alsaba N, Shaw R. Geriatric emergency medicine. EM Sim
Cases. 2022. Available at: https://emsimcases.com/geriatric-emergency-medicine/. Accessed May 12, 2025.
24. GEMCast podcast. Geriatric Emergency Department Collaborative. Avilable at: https://gedcollaborative.com/resources/?type=podcast. Accessed May 12, 2025.
25. Rentsch S, Vitale CA, Zietlow K. Prioritizing geriatrics in medical education improves care for all. Med Educ Online. 2022;27(1):2105549.
26. Salter EK, Waldron M, Paniagua MA. Early exposure to geriatric care: developing an undergraduate internship in ethics and geriatric practice. Int J Med Educ. 2014;5:15-7.
27. Medina-Walpole A, Clark NS, Heppard B, et al. A user’s guide to enhancing geriatrics in an undergraduate medical school curriculum: the ten-step model to winning the “geriatric game”. J Am Geriatr Soc 2004;52(5):814-21.
28. Kennedy M, Lesser A, Israni J, et al. Reach and adoption of a geriatric emergency department accreditation program in the United States. Ann Emerg Med. 2022;79(4):367-73.
29. Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine. Acad Emerg Med 2014;21(7):806-9.
Pharmacogenomic Drug-Gene Interactions in Geriatric Emergency Department Patients Who Sustained Falls: A Pilot Study
Richard D. Shih, MD*†
Gabriella Engstrom, PhD, RN*
Abhijit S. Pandya, PhD‡
Gregg B. Fields, PhD§
Borivoje Furht, PhD‡
Ali A. Danesh, PhD||
Scott M. Alter, MD*†#
Humberto Munoz, BPharm, CPh, MHSA†
Lisa M. Clayton, DO*†#
Joshua J. Solano, MD*†#
Timothy Buckley, MD, MPH*†#
Olivia Hung*
Authors continued at end of article
Section Editor: Stephen Meldon, MD
Florida Atlantic University, Charles E. Schmidt College of Medicine, Department of Emergency Medicine, Boca Raton, Florida
Delray Medical Center, Department of Emergency Medicine, Delray Beach, Florida
Florida Atlantic University, College of Engineering and Computer Science, Department of Electrical Engineering and Computer Science, Boca Raton, Florida
Florida Atlantic University, Charles E. Schmidt College of Science, Department of Chemistry and Biochemistry, Boca Raton, Florida
Florida Atlantic University, College of Education, Department of Communication Sciences and Disorders, Boca Raton, Florida
Bethesda Hospital East, Department of Emergency Medicine, Boynton Beach, Florida
Submission history: Submitted March 4, 2025; Revision received June 23, 2025; Accepted June 23, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.46553
Introduction: Pharmacogenomic-assisted prescribing of medications uses individual genetic information to identify drug-gene interactions. We aimed to assess potential pharmacogenomic druggene interactions in geriatric emergency department (ED) patients who sustained a fall.
Methods: This was a prospective study involving 25 older adult ED patients with fall-related injury. Data collected included current medications, demographics, and mechanism of injury. All patients provided a DNA sample, which underwent pharmacogenomic testing by an accredited genetics lab, Each patient’s medications were reviewed against their pharmacogenomic report and categorized as Green (continue to use), Yellow (use with caution) or Red (stop use) based on their genetic information and published interactions by the Clinical Pharmacogenetics Implementation Consortium, Dutch Pharmacogenetics Working Group, and US Food and Drug Administration-approved drug label information. The main study outcome was pharmacogenomic drug-gene interactions.
Results: Of the 25 patients enrolled (median age, 81 years, IQR 76-85), 68% were female. Patients were taking a median of eight medications (IQR 5-11). The most common types were antihypertensives, statins, anticoagulants, and anti-platelet medications. Significant drug-gene interactions (Yellow or Red) were identified in 14/25 patients (56%; 95% CI 35-76%). Further, 6/25 (24%; 95% CI 9-45%) had one or more potentially serious (Red) interactions identified.
Conclusion: We found that in geriatric ED patients with a fall-related injury, most had a significant pharmacogenomic drug-gene interaction. DNA testing identifies these interactions and can assist with pharmacogenomic-guided medication prescribing, which may decrease adverse drug events and improve clinical outcomes. [West J Emerg Med. 2025;26(5)1414–1422.]
INTRODUCTION
As individuals age, they have more medical problems and are prescribed more medications. Polypharmacy, defined by
convention as taking more than five medications, has been associated with increased adverse drug events (ADE), hospitalizations and poor outcomes.1-4 Of these poor
outcomes, falling and fall-related injury are among the most important.1,5 Deprescribing (ie, stopping a medication) is a difficult process.6-8 Although several methods for medication assessment and possible discontinuation have been published, few have been widely adopted given the many challenges associated with stopping medications.9-13
Pharmacogenomic tests may identify drug-gene interactions that are responsible for some ADEs. By identifying genetic polymorphisms at high risk for ADE, this may provide a clinician iwith objective information to deprescribe or prescribe medications more precisely and appropriately.14,15 Authoritative organizations, including the Clinical Pharmacogenetics Implementation Consortium (CPIC) and Dutch Pharmacogenetics Working Group(DPWG), as well as. published clinical guidelines offer guidance on how to use pharmacogenomic results to decrease ADE risk.16-18
The use of pharmacogenomic prescribing of medications has been reported in pediatrics, psychiatry, oncology and geriatrics.14,15,19,20 In the emergency department (ED), several previous studies have shown its potential for use.21,22 However, these studies focused on one or two cytochrome P450 (CYP) metabolic enzyme systems (CYP2D6 and CYP2C19) or one class of medications (opioids). No previous ED studies have looked at multiple metabolic systems and classes of medications in patients who have fallen.21 Our objective in this study was to assess the prevalence of pharmacogenomic drug-gene interactions in geriatric ED patients who suffered a fall. The etiology of falls in geriatric patients is complex and has multifactorial etiologies. This study focuses only on gene-drug interactions that may contribute to falling.
METHODS
Study Design and Setting
We conducted an observational cross-sectional study involving 25 patients presenting to a single ED with an annual patient volume of 50,000. The study was approved by the hospital’s affiliated university institutional review board (IRB).
Selection of Participants
In this pilot study we used a convenience sample of older adults presenting to the ED after a ground-level fall. All eligible patients were approached by trained research assistants (RA) and invited to participate. Study enrollment occurred only during the hours that RAs were present in the ED (9 am to 11 pm daily). Participants in this study represented a subset of patients enrolled in a larger randomized controlled trial on falling in older adults (unrelated to pharmacogenomics). The specific inclusion criteria were patients ≥ 65 years of age who had presented to the ED with a fall-related injury. The criteria for exclusion from the study were failure to obtain consent; patients who had suffered penetrating injuries > 24 hours prior to presentation; patients transferred from another hospital; and patients who were in hospice care or had do not resuscitate status.
Population Health Research Capsule
What do we already know about this issue?
Geriatric emergency department (ED) patients may have drug-gene interactions that contribute to adverse drug events. DNA analysis and use for medication prescribing may prevent these.
What was the research question?
What is the prevalence of potential drug-gene interactions in geriatric ED patients who have fallen?
What was the major finding of the study?
In this small pilot study, 56% (95% CI 3576%) were found to have a potentially serious drug-gene interaction.
How does this improve population health? DNA testing can identify potential medication drug-gene interactions. This information may be useful to guide prescribing practices.
Data Collection
Identified patients who met the study’s inclusion criteria were approached to complete an IRB-approved informed consent form for study participation, and their data were collected by the RAs. Data collected included current medications (prescribed pre-injury), demographic data, mechanism of injury, past medical history, and ED diagnosis. In addition, patients provided a DNA sample obtained via a single cheek swab sample from inside the patient’s mouth. (The subjects were not allowed to eat, drink, or smoke for 30 minutes prior to swabbing.) We used the pharmacogenomic test MatchMyMeds (DNA Labs, Boca Raton, FL, https:// dnalabs.ca), which reports on potential drug-gene interactions for 134 medications. The genetics company is accredited by the Clinical Laboratory Improvement Amendments, the College of American Pathologists, the State of California Department of Public Health, the American Association of Blood Banks, and the New York State Department of Health. The MatchMyMeds test analyzes for 23 different metabolic enzyme systems and reviews potential drug-gene interactions for 134 different medications (see Supplementary Table). The report is based on the Clinical Pharmacogenetics Implementation Consortium,16 the Dutch Pharmacogenetics Working Group,17,18 and US Food and Drug Administrationapproved drug label information to provide detailed drug and dosing recommendations. In addition, based on the individual’s genetics, the report categorized 134 medications
Shih
as Green (go: use label recommended dosage and administration), Yellow (caution: use with caution and read detailed recommendations for potential dose adjustment), or Red (stop: select alternative treatment if possible and read detailed recommendation for detail). DNA Labs used the MassARRAY System (Agena Bioscience GmbH, Hamburg, Germany), to perform the genotyping.23 Copy number variant (CNV) analysis was performed using the Agena Veridose panel, to detect CNVs and hybrid alleles. The lab did not assess drug-drug interactions from medication coconsumption.
Outcomes
The main study outcome was to identify pharmacogenomic drug-gene Interactions. Yellow and Red medications were defined as serious interactions. A secondary outcome was to assess whether a medication with a significant gene-drug interaction was also identified in the Beers Criteria, which lists potentially inappropriate medications for older adults.24
Analysis
We conducted descriptive analyses to assess the prevalence and severity of drug-gene interactions, as well as to identify the specific drugs affected. We quantified the frequency of interactions within each risk category (Green, Yellow, and Red) and characterized the severity of these interactions based on their potential impact on patient safety and treatment efficacy.
RESULTS
We enrolled 25 patients. The median age was 81 years (IQR 76-85), and 68% were female. The most frequent co-morbidities were hypertension (64%), atrial fibrillation (32%), coronary artery disease (28%) and stroke (8%). All patients were on medications for pre-existing co-morbidities (see Table 1). Patients were taking a median of eight medications (IQR 5-11). The most common types were antihypertensives, statins, anticoagulants, and anti-platelet medications. All 25 patients had suffered a fall, as this was part of the criteria for inclusion in the study. Most had contusions, fractures, and wounds. Several also had significant medical problems such as stroke, head injury, and syncope. When considering the pharmacogenomic data and drug-gene interactions, of our 25 patients 14 (56%, 95% CI 35-76%) had one or more Yellow or Red medications (see Figure 1) for a total of 20 significant gene-drug interactions (see Table 2). Further, 6/25 (24%, 95% CI 9-45%) had one or more Red medications identified (Figure 1). The implicated medications were those that could increase risk of falling with several drugs with the potential for increased sedation (escitalopram, tramadol, trazodone, oxycodone, and duloxetine) and others potentially causing bradycardia or hypotension (metoprolol and amlodipine).
Table 1. Clinical characteristics of elderly patients with preexisting morbidities enrolled in a study of drug-gene interactions and increased risk of falling.
Past Medical History, n (%) Hypertension
(4)
DISCUSSION
As individuals get older, they develop more medical problems and are prescribed more medicines. The more medications that someone takes, the higher the risk for an ADE.25 Polypharmacy—taking five or more medicines—is a major risk factor for an ADE.26 One common ADE is a fall and fall-related injuries. These occur commonly, with approximately 30% of older adults sustaining a fall each year.27 Although a medication- related ADE can cause falls, there are other etiologic factors that contribute. Our study focused only on gene-drug interactions that may contribute to falling.
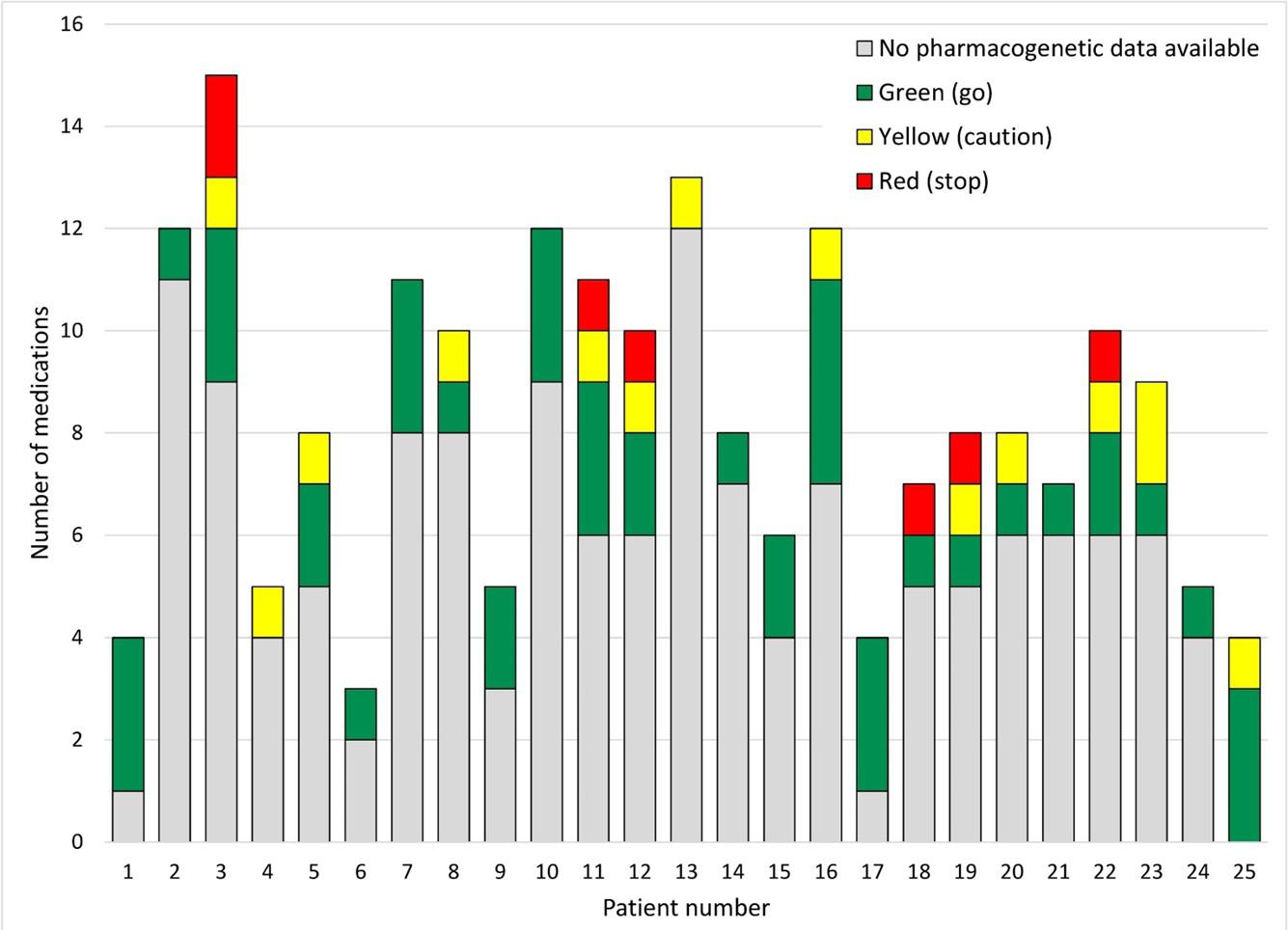
Shih
Figure 1. Possible drug-gene medication interactions for each patient.
Table 2. Significant drug-gene interactions.
Pt Drug
Enzyme system involved Flag
3 Escitalopram Reduced CYP2C19 activity
Metoprolol Reduced CYP2D6 activity
Clopidogrel Reduced CYP2C19 activity
4 Pantoprazole Reduced CYP2C19 activity
5 Tramadol Elevated CYP2D6 activity
8 Paroxetine Reduced CYP2D6 activity
11 Warfarin CYP2C9 and VKORC1 variants
Metoprolol Reduced CYP2D6 activity
12 Escitalopram Reduced CYP2C19 activity
Clopidogrel Reduced CYP2C19 activity
13 Pantoprazole Reduced CYP2C19 activity
16 Trazodone Reduced CYP3A4 activity
18 Metoprolol Reduced CYP2D6 activity
Possible clinical significance Action recommended
Yellow Serum levels increased
Red Serum levels increased –hypotension, bradycardia
Red Serum levels decreased –increased risk of thrombosis
Yellow Serum levels increased
Yellow Increased level of metabolite (morphine)
Yellow Serum levels increased
Yellow Variable effect on serum levels
Red Serum levels increased –hypotension, bradycardia
Yellow Serum levels increased
Red Serum levels decreased –increased risk of thrombosis
Yellow Serum levels increased
Be alert for drug-related adverse effects, especially with co-administration of other drugs that inhibit CYP2C19 enzyme activity.
Select alternative drug.
Select alternative drug.
Be extra alert for lack of efficacy and adverse effects, especially with coadministration of other drugs that inhibit CYP2C19 or CYP3A4 enzyme activity.
Reduce dose by 30% and be alert to adverse drug events.
Be extra alert, especially with coadministration of other drugs that inhibit CYP2D6 enzyme activity.
The genetic information below can be entered into the warfarindosing.org form to estimate the most appropriate therapeutic dose in patients new to warfarin.
Select alternative drug (eg, bisoprolol, carvedilol) or reduce dose by 50%.
Be alert for drug-related adverse effects, especially with co-administration of other drugs that inhibit CYP2C19 enzyme activity.
Avoid standard dose (75 mg) clopidogrel if possible. Use prasugrel or ticagrelor at standard dose if no contraindication.
Dose adjustment is not recommended, but be extra alert for lack of efficacy and adverse effects, especially with coadministration of other drugs that inhibit CYP2C19 or CYP3A4 enzyme activity.
Appears in American Geriatric Society Beers Criteria list15
No
No
No
Yes
Yes
Yes
Yes
No
No
No
Yes
Yellow Serum levels increased
Red Serum levels increased –hypotension, bradycardia
A lower dose of trazodone should be considered, especially if co-administered with a CYP3A4 inhibitor.
Select alternative drug (eg, bisoprolol, carvedilol) or reduce dose by 50%.
No
No
Yellow: use with caution; read recommendations for potential dose adjustment. Red: select alternative treatment if possible. The term reduced activity is used to indicate a poor metabolizer phenotype; similarly, elevated activity is used to indicate an ultrarapid metabolizer phenotype. No data are presented for patients 1, 2, 6, 7, 9, 10, 14, 15, 17, 21, and 24 as they had no significant drug-gene interactions. Pt, patient.
Table 2. Significant drug-gene interactions.
Pt Drug
Enzyme system involved Flag
19 Celecoxib Reduced CYP2C9 activity
Oxycodone Reduced CYP2D6 activity
20 Duloxetine Reduced CYP2D6 and elevated CYP1A2 activity
22 Pantoprazole Elevated CYP2C19 activity
Escitalopram Elevated CYP2C19 activity
23 Amlodipine Reduced CYP3A4 activity
Apixaban Reduced CYP3A4 activity
25 Simvastatin Reduced CYP3A4 and CYP2C6 activity
Possible clinical significance
Yellow Serum levels increased
Red Serum levels increased – toxic opioid effect
Yellow Serum levels increased
Yellow Serum levels decreased
Red Serum levels decreased
Yellow Serum levels increased –hypotension
Yellow Serum levels increased – increased bleeding
Yellow Serum levels increased –increased risk of rhabdomyolysis
Action recommended
Use lowest effective dose and be extra alert for adverse effects, especially with co-administration of other drugs that inhibit CYP2C9 enzyme activity.
Select alternate drug—not tramadol or codeine—or be alert to symptoms of insufficient pain relief, especially with coadministration of other drugs that inhibit CYP2D6 enzyme activity.
Caution is advised—insufficient evidence to support a dosage adjustment.
Consider dose increase by 400% and be extra alert to insufficient response.
Consider an alternative drug NOT predominantly metabolized by CYP2C19.
Use label recommended dosage and administration, and be extra alert for side effects including symptoms of hypotension and edema.
The reduction in CYP3A4 enzyme activity in this case may or may not be sufficient to significantly increase exposure; thus, there is insufficient data to support a dosage adjustment, although a dose reduction to 2.5mg twice daily could be considered.
Prescribe a lower dose or consider an alternative statin.
Appears in American Geriatric Society Beers Criteria list15
Yes
Yes
Yes
Yes
No
No
No
No
Yellow: use with caution; read recommendations for potential dose adjustment. Red: select alternative treatment if possible. The term reduced activity is used to indicate a poor metabolizer phenotype; similarly, elevated activity is used to indicate an ultrarapid metabolizer phenotype. No data are presented for patients 1, 2, 6, 7, 9, 10, 14, 15, 17, 21, and 24 as they had no significant drug-gene interactions. Pt, patient.
Shaver et al in 2021 showed that mortality risk from falls in older persons in the US increased steadily from 1999 to 2017, as the use of fall-risk increasing drugs rose. During that period, the percentage of older people taking a fa-risk increasing drug increased from 57% to 97%.3 On average, 750 older adults in the US are hospitalized each day due to an ADE, and 50% are taking ≥ seven medications.5,13 Further, it is estimated that 60% of older people take one or more medicines that are unnecessary.28 Among geriatric ED patients about 75% are prescribed one or more medication classified as “avoid” or “use with caution.”6 However, stopping a medication (deprescribing) has proven to be difficult for patients and physicians.13
Although various methods for medication assessment and possible discontinuation have been published, most have not been widely adopted.9-11,24,29 Deprescribing presents several significant
challenges in clinical practice including physicians who lack training in stopping medications or are concerned about worsening symptoms; patients who worry about worsening symptoms; concern regarding withdrawal and the time required to discuss medication changes; and patients who feel their doctor is “giving up” and is no longer treating their disease.13,16,30 Pharmacogenomics, a genetics-based method to assess for possible risk of ADEs, could one day become standard information for physicians to help provide more precise and personalized prescribing of medications. Pharmacogenomics involves gene testing to assess how an individual metabolizes medications. Hepatic enzymes in the P450 systems (ie, CYPD6, CYP3A4, and CYP2C19) are responsible for metabolizing many commonly used medications such as atorvastatin, diazepam, warfarin, rivaroxaban, sertraline, and many others).
In addition, CYP2D6 has many different genetic polymorphisms and, depending on the inherited alleles, the individual CYP2D6 system may function as a poor, normal or ultra-rapid metabolizer.3 Most people are normal metabolizers; and in our current “one size fits all” approach to dosing medications, the standard dose will generally provide concentrations in the therapeutic window predictably. However, if the individual is a poor metabolizer or an ultra-rapid metabolizer, a given medication may be in a toxic or ineffective concentration range due to the gene-drug interaction.
Previous studies suggest that most individuals have one or more gene phenotypes that can cause an adverse drug event with commonly prescribed medications.32-34 In a study of close to eight million Veterans Administration patients, based on genetic allele frequency and medication history, it was estimated that most (> 90%) of the individuals had at least one actionable pharmacogenomic variant.34
In our study each patient’s medications was assessed for a potential drug-gene interaction based on DNA Labs’ pharmacogenomic report. Of our 25 patients there were 20 (Red or Yellow) significant potential drug-gene interactions identified, with 56% taking one or more “Yellow” or “Red” medications (see Figure and Table 2). In addition, 20% had at least one “Red” drug-gene medication interaction identified. Examples of significant gene-drug interactions include the following:
• Reduced CYP2D6 enzyme activity in someone taking metoprolol. These individuals are poor metabolizers of metoprolol and have a three-to-tenfold higher concentration compared to a normal metabolizer. Further, poor metabolizers had a five times higher rate of ADE compared to non-poor metabolizers. These ADE include symptomatic bradycardia and dizziness.35
• Reduced CYP3A4 enzyme activity in someone taking trazodone may lead to changes in concentrations of the parent compound and active metabolites.36,37 This may lead to increased sedation, dizziness and falls.”36-38
An additional important finding is that many of the genedrug interactions identified are not on the American Geriatrics Society 2023 updated Beers Criteria (see Table 4).24 The Beers Criteria is a list of potentially inappropriate medications for older adults, which was developed by a panel of interprofessional experts who reviewed the published literature to establish this list. However, the medications involved in 11 of the 20 (55%) significant potential drug-gene interactions identified in our study are not on the Beers list (whose methodology does not attempt to identify drug-gene interactions).
An important question is whether drug-gene interactions have a causal link with falling. It was not an objective in this study to evaluate potential causality, but this is a critical issue to consider. It has been well established that multiple factors contribute to a risk of falling. It has also been well established that medications can be significant risk factors. Further, there is good preliminary evidence that there is an association between
the occurrence of falls in older adults and the metabolic capacity of certain enzyme systems (detectable through pharmacogenomic analysis).39 The interactions between the risk factors for falling have not been fully elucidated, nor has single-factor causality been clearly determined for any factor. However, medication optimization is one of the most easily addressed risk factors and, therefore, worthy of attention. Clearly, other factors may compound the effect of suboptimal medication therapy. In addition, not all drugs are likely to impart the same degree of risk or type of risk. In the end, however—irrespective of the case for causality related to falls—a strong consensus is emerging that personalized drug therapy is essential in older adults.40
Technological advances over the past several decades have drastically increased the speed of analyzing DNA samples and decreased the costs. (As of this writing, the consumer cost for DNA Labs MatchMyMeds testing is $275).41 While the results of pharmacogenomic testing performed in the ED are not yet available in real time, it is likely that pharmacogenomic data will be routinely integrated into the electronic health record. However, to be practically useful, this information would need to be accompanied by clinical decision-support alerts that would identify gene-drug interactions and how they should be addressed, at the point of prescribing. This could be an especially valuable tool when managing high-risk medications in patients at risk of falling.
When this pharmacogenomic information is already available, such as from previous outpatient testing, emergency physicians could use the data to identify medications that may be inappropriate or pose elevated risk, adjust or discontinue certain prescriptions to lower fall risk, and communicate relevant pharmacogenomic concerns to the patient’s primary care physician for ongoing management. Incorporating genetic testing into routine care would allow clinicians to personalize drug therapy, reduce the likelihood of adverse drug reactions, and improve treatment outcomes for older adults. There is convincing evidence that about half of all older adults are prescribed at least one pharmacogenomically actionable drug, and between 25-35% receive two or more such drugs. These findings indicate that exposure to multiple medications with drug-gene interactions is common, supporting the potential value of implementing broad, pre-emptive genomic testing.42 There is no reason this could not be introduced into the ED, as this is particularly relevant in older adults at risk of adverse drug events, even if not yet routine practice. This would address one of the core obligations of physicians to “first do no harm.”
The potential future utility of pharmacogenomics in emergency medicine is considerable, particularly as national healthcare systems move toward integrating genomic data into routine care. For example, the United Kingdom’s National Health Service (NHS)—citing evidence that it is possible to reduce adverse drug reactions and unplanned hospitalizations among older adults—has committed to embedding pharmacogenomic testing into clinical practice; NHS pilot programs focused on high-risk conditions are ongoing. While not yet ED-specific, the
Shih
availability of pharmacogenomic data at the point of care could allow emergency physicians to tailor prescribing and deprescribing decisions more safely and effectively. As pharmacogenomic-guided therapy becomes standard over the next decade, leaders in emergency medicine will need to address the associated challenges associated with this therapy, especially in terms of time demands. Integrating pharmacogenomic alerts into the EHR, potentially supported by clinical decision-support tools driven by artificial intelligence, may offer a practical and efficient way to enhance prescribing without increasing clinician burden. Nevertheless, further research is essential to evaluate the real-world impact of pharmacogenomic optimization in emergency care. Given the growing importance of precision medicine, this research should be a priority.
LIMITATIONS
This study enrolled a convenience sample of 25 patients without a control group. Although the sample was small, it was a subset of a larger study with the population characteristics of interest to us. Our main objective in this pilot study was to identify the real-world scope of the potential problem (druggene interactions) rather than provide an accurate population estimate of its prevalence. Despite the small sample size, the 95% CI revealed that even the lower limit of drug-gene interaction prevalence (35%) would constitute a clinically significant proportion of older adult patients. Since other studies have estimated up to a 90% theoretical prevalence of drug-gene interactions in older adults, this study, despite its limitations in generalizability. provides important confirmatory evidence. However, a larger study at multiple centers would likely provide more accurate estimates of the incidence and types of these interactions.
A second limitation is that the gene-drug interactions identified are potential, and ADEs were not examined as part of this study. Further, some of the drug-gene interactions that we identified may not cause significant ADEs and may be the reason that these drugs do not appear on the Beers list. Further, pharmacogenomics may identify drugs that are on the Beers list and may be useful to categorize the risk of harm of drugs on the list, in patients with pharmacogenomically detected vulnerability. A randomized controlled trial using the pharmacogenomic-assisted prescribing of medications would be the ideal method to assess for ADEs and the clinical impact of the significant gene-drug interactions that were identified.
A third limitation is that even if individual pharmacogenomic data were available, it is not clear whether physicians would use the data for improved prescribing. One of the barriers is the difficulty in interpretating the pharmacogenomic data, leading to an increased amount of time and lack of user-friendly guideline information.16,30,42 We did not assess this factor; it is another future area of research for the implementation of pharmacogenomicassisted prescribing practices.
Another limitation is that our study only assessed gene-drug interactions. Several other factors play a role in how cytochrome
p450 metabolism of medications occurs. Medications, foods, and medical conditions can augment or inhibit drug metabolism. An example of a common medication interaction is the CYP3A4 inhibitory effect of diltiazem. When co-administered with direct oral anticoagulants their metabolism may be inhibited, and a higher bleeding risk has been seen in these patients.44 Our study did not investigate these other factors and did not assess their effect on the gene-drug interactions reported.
Lastly, the patients’ use of medication was assessed by self-report. We did not assess drug levels or other confirmation of medication compliance. (For example, patients reporting medications that they were not actually taking would not represent true gene-drug interactions.)
CONCLUSION
In this pilot study our aim was to estimate the prevalence of pharmacogenomic drug-gene interactions in geriatric ED patients who had presented for a fall-related injury. We found that nearly 60% of these patients had significant pharmacogenomic druggene interactions with potential clinical impact. We did not attempt to establish a causal relationship between these interactions and the patients’ falls. Nonetheless, given the multifactorial nature of the risk of falling, these findings suggest that pharmacogenomic-guided medication prescribing (or deprescribing), could have the potential to decrease adverse drug effects and thereby reduce the negative impact of medications on the risk of falling. In the near future the results of DNA testing might be available in the electronic health record, which would make this possible, even in the ED.
AUTHORS CONTINUED
Alexander Farag*
Mike Wells, MBBCh, PhD*
Address for Correspondence: Richard Shih, MD, Florida Atlantic University Schmidt College of Medicine, Department of Emergency Medicine, 777 Glades Rd, BC-71, Boca Raton, FL 33431-0991. Email: rshih@health.fau.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. This study was supported by a grant from the Florida Medical Malpractice Joint Underwriting Association Grant for Safety of Health Care Services Grant RFA #2022-01. “The Geriatric Emergency Department Fall Injury Prevention (The GREAT FALL).” Principal Investigator: Richard D. Shih MD. The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or in the decision to submit the manuscript.
Copyright: © 2025 Shih et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Xing XX, Zhu C, Liang HY, et al. Associations between potentially inappropriate medications and adverse health outcomes in the elderly: a systematic review and meta-analysis. Ann Pharmacother. 2019;53:1005-19.
2. Budnitz DS, Shehab N, Lovegrove MC, et al. US emergency department visits attributed to medication harms, 2017-9. JAMA. 2021;326:1299-309.
3. Shaver AL, Clark CM, Hejna M, et al. Trends in fall-related mortality and fall risk increasing drugs among older individuals in the United States,1999-2017. Pharmacoepidemiol Drug Saf. 2021;30:1049-56.
4. Koehl JL. Adverse drug event prevention and detection in older emergency department patients. Clin Geriatr Med. 2023;39:635-45.
5. Flaherty JH, Perry HM 3rd, Lynchard GS, et al. Polypharmacy and hospitalization among older home care patients. J Gerontol A Biol Sci Med Sci. 2000;55:554-9.
6. Harrison L, O’Connor E, Jie C, et al. Potentially inappropriate medication prescribing in the elderly: Is the Beers Criteria relevant to the emergency department today? Am J Emerg Med. 2019;37:1734-7.
7. Stevens M, Hastings SN, Markland AD, et al. Enhancing Quality of Provider Practices for Older Adults in the Emergency Department (EQUiPPED). J Am Geriatr Soc. 2017;65:1609-14.
8. Skains RM, Koehl JL, Aldeen A, et al. Geriatric Emergency Medication Safety Recommendations (GEMS-Rx): Modified Delphi development of a high-risk prescription list for older emergency department patients. Ann Emerg Med. 2024;84:274-84.
9. O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213-8.
10. Boyé ND, van der Velde N, de Vries OJ, et al. Effectiveness of medication withdrawal in older fallers: results from the improving medication prescribing to reduce risk of falls (IMPROveFALL) trial. Age Ageing 2017;46:142-6.
11. Stevens M, Hastings SN, Markland AD, et al. Enhancing quality of provider practices for older adults in the emergency department (EQUiPPED). J Am Geriatr Soc. 2017;65:1609-14.
12. American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 updated AGS beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019;67:674-94.
13. Rubin R. Deciding when it’s better to deprescribe medicines than to continue them. JAMA. 2023;330:2328-30.
14. Cohn I, Manshaei R, Liston E, et al. Assessment of the implementation of pharmacogenomic testing in a pediatric tertiary care setting. JAMA Netw Open. 2021;4(5):e2110446.
15. Bohlen KN, Kittelsrud JM, Nelson ME, et al. Clinical utility of pharmacogenetics in a psychiatric and primary care population. Pharmacogenomics J. 2023;23(1):21-7.
16. Relling MV, Klein TE, Gammal RS, et al. The Clinical Pharmacogenetics Implementation Consortium: 10 years later. Clin Pharmacol Ther. 2020;107:171-5.
17. Bank PCD, Caudle KE, Swen JJ, et al. Comparison of the guidelines of the Clinical Pharmacogenetics Implementation Consortium and the Dutch Pharmacogenetics Working Group. Clin Pharmacol Ther. 2018;103:599-618.
18. Caudle KE, Sangkuhl K, Whirl-Carrillo M, et al. Standardizing CYP2D6 genotype to phenotype translation: consensus recommendations from the Clinical Pharmacogenetics Implementation Consortium and Dutch Pharmacogenetics Working Group. Clin Transl Sci. 2020;13:116-24.
19. Kotsopoulos J. BRCA mutations and breast cancer prevention. Cancers. 2018;10:524.
20. Kehr AM, Ayers G, Saxena S, et al. Integration of a pharmacist-led pharmacogenomic service in a geriatric clinic: barriers and outcomes. J Am Pharm Assoc. 2023;63:778-84.
21. Sheikh S, Fernandez R, Smotherman C, et al. A pilot study to identify pharmacogenomic and clinical risk factors associated with opioid related falls and adverse effects in older adults. Clin Transl Sci. 2023;16:2331-44.
22. Flaten HK, Kim HS, Campbell J, et al. CYP2C19 drug-drug and drug-gene interactions in ED patients. Am J Emerg Med 2016;34:245-9.
23. Ellis JA, Ong B. The MassARRAY system for targeted SNP genotyping. Methods Mol Biol. 2017;1492:77-94.
24. 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71:2052-81.
25. Shah BM, Hajjar ER. Polypharmacy, adverse drug reactions, and geriatric syndromes. Clin Geriatr Med. 2012;28:173-86.
26. Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17:230.
27. Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years - United States, 2014. Morb Mortal Wkly Rep. 2016;65:993-8.
28. Schmader KE, Hanlon JT, Pieper CF, et al. Effects of geriatric evaluation and management on adverse reactions and suboptimal prescribing in the frail elderly. Am J Med. 2004;116:394-401.
29. Shih RD, Carpenter CR, Tolia V, et al. Balancing vision with pragmatism: the geriatric emergency department guidelines- realistic expectations from emergency medicine and geriatric medicine. J Am Geriatr Soc. 2022;70:1368-73.
30. Relling MV, Klein TE. Clinical Pharmacogenetics Implementation Consortium of the Pharmacogenomics Research Network. Clin Pharmacol Ther. 2011;89:464-7.
31. Crews KR, Gaedigk A, Dunnenberger HM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin Pharmacol Ther. 2014;95:376-82.
32. Van Driest SL, Shi Y, Bowton EA, et al. Clinically actionable genotypes among 10,000 patients with preemptive pharmacogenomic testing. Clin Pharmacol Ther. 2014;95:423-31.
33. Bush WS, Crosslin DR, Owusu-Obeng A, et al. Genetic variation
Pharmacogenomic Drug-Gene Interactions in Geriatric ED Patients
among 82 pharmacogenes: The PGRNseq data from the eMERGE network. Clin Pharmacol Ther. 2016;100:160-9.
34. Chanfreau-Coffinier C, Hull LE, Lynch JA, et al. Projected Prevalence of Actionable Pharmacogenetic Variants and Level A Drugs Prescribed Among US Veterans Health Administration Pharmacy Users. JAMA Netw Open. 2019;2:e195345.
35. Wuttke H, Rau T, Heide R, et al. Increased frequency of cytochrome P450 2D6 poor metabolizers among patients with metoprololassociated adverse effects. Clin Pharmacol Ther. 2002;72:429-37.
36. Elens L, van Gelder T, Hesselink DA, et al. CYP3A4*22: promising newly identified CYP3A4 variant allele for personalizing pharmacotherapy. Pharmacogenomics. 2013;14:47-62.
37. Saiz-Rodríguez M, Belmonte C, Derqui-Fernández N, et al. Pharmacogenetics of trazodone in healthy volunteers: association with pharmacokinetics, pharmacodynamics and safety. Pharmacogenomics. 2017;18:1491-1502.
38. Bronskill SE, Campitelli MA, Iaboni A, et al. Low-dose trazodone, benzodiazepines, and fall-related injuries in nursing homes: a matched-cohort study. J Am Geriatr Soc. 2018;66:1963-71.
Shih et
39. Just KS, Pott LM, Sommer J, et al. ActiFE Study Group. Association of Polymorphic Cytochrome P450 Enzyme Pathways with Falls in multimedicated older adults. J Am Med Dir Assoc. 2024;25:105235.
40. David V, McInerney C, Fylan B, et al. We must start using pharmacogenomic information to optimise medicines for older people. Pharmaceutical J. 2022;309:1-14.
41. van Nimwegen KJ, van Soest RA, Veltman JA, et al. Is the $1000 genome as near as we think? A cost analysis of next-generation sequencing. Clin Chem. 2016;62:1458-64.
42. Samwald M, Xu H, Blagec K, et al. Incidence of exposure of patients in the united states to multiple drugs for which pharmacogenomic guidelines are available. PLoS One. 2016;11:e0164972.
43. Roth M, King L, St Cyr K, et al. Evaluating the prospective utility of pharmacogenetics reporting among Canadian Armed Forces personnel receiving pharmacotherapy: a preliminary assessment towards precision psychiatric care. BMJ Mil Health. 2024;170:440-5.
44. Xu Y, Chang AR, Inker LA, et al. Concomitant use of diltiazem with direct oral anticoagulants and bleeding risk in atrial fibrillation. J Am Heart Assoc. 2022;11:e025723.\
Original Research
Multicenter Study Evaluating Impact of Patient and Sonographer Demographics on Quality of Focused Cardiac Ultrasounds
Barret Zimmerman, MD*
Tracy E. Madsen, MD, PhD†
Giorgina Giampaolo, MD†
Jennifer Rogers, MD†
Hilary Davenport Stroud, DO‡
Creagh Turner Boulger, MD‡
Michael I. Prats, MD‡
Alice Wu, MD‡
* † ‡
Harvard Medical School / Mass General Brigham, Department of Emergency Medicine, Boston, Massachusetts
Alpert Medical School of Brown University, Department of Emergency Medicine, Providence, Rhode Island
The Ohio State University, Department of Emergency Medicine, Columbus, Ohio
Section Editor: James A. Meltzer, MD, MS
Submission history: Submitted [November 7, 2024]; Revision received [June 15, 2025]; Accepted [June 15, 2025]
Electronically published October 3, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI 10.5811/westjem.38462
Introduction: Demographic inequities in cardiovascular care have been well established, with evidence of effects from sex, age, and body mass index (BMI). For instance, women are less likely to receive guidelinebased care for acute myocardial Infarction, bystander cardiopulmonary resuscitation, or recognition of cardiac arrest. We investigated the impact of patient sex, along with other patient demographics such as age and BMI, on the quality of focused cardiac ultrasounds (FOCUS). We hypothesized that females would have lower overall FOCUS quality and more frequently omitted apical four-chamber (A4C) views due to breast tissue. Secondary objectives included evaluating differences in image quality and omission rates by BMI, and by age and sonographer sex and training level.
Methods: In this multicenter, retrospective study we investigated 1,200 total adult patients (100 females and 100 males per site) at six participating sites. The FOCUS quality was determined by two blinded experts per site using a 1-5 ordinal scale per view (parasternal long, parasternal short, A4C, and subxiphoid). The primary outcome, overall quality, was the summed score of the four views, with a maximum score of 20. This scale was then collapsed into three categories for the individual FOCUS views: images inadequate to support diagnosis; images meeting the minimum to support diagnosis; and images supporting the diagnosis well. Secondary outcomes were A4C quality and omission rate. We evaluated associations between sex and FOCUS overall quality using unadjusted mixed-effects models followed by multivariable mixed-effects models adjusted for patient age, BMI, operator sex, and operator experience level.
Results: The A4C images of female patients were of significantly lower quality (P < .001) and had been omitted more frequently (P < .001); male patients had > 60% higher odds of a diagnostic A4C view (95% CI 1.3 - 2.0). Overall FOCUS quality decreased as BMI deviated from normal and as age increased. There was no significant difference in overall FOCUS quality between female and male patients.
Conclusion: We did not find sex-based differences in overall FOCUS quality; however, we did find that females received lower quality apical four-chamber views and had this view omitted more frequently. Additionally, overall quality declined as BMI deviated from normal, and as age advanced. Future research should elucidate the clinical implications of these differences in quality and the explanation behind not obtaining high-quality views in older patients, in individuals whose BMI deviated from normal toward either underweight or overweight, or in female patients. [West J Emerg Med. 2025;26(5)1423–1430.]
INTRODUCTION
Heart disease is the leading cause of death in the United States and worldwide, and cardiopulmonary complaints are among the most frequent presentations to the emergency department (ED).1 Demographic discrepancies in cardiovascular care have been established, and patient sex has emerged as a significant factor. For example, women suffer greater mortality from myocardial infarction but are less likely to receive guideline-based pharmacological therapies or revascularization for acute myocardial infarction.2 Other sex disparities are evident along the trajectory of care in the ED from diagnosis to management, and women may experience higher rates of short-term mortality and adverse events.3 It has also been shown that women are less likely to receive bystander cardiopulmonary resuscitation and automated external defibrillator (AED) placement for witnessed out-of-hospital cardiac arrest, which is believed to be due to lack of recognition of this emergency in women as well as hesitancy in exposing a woman’s chest.4,5
Besides sex, other demographic factors have also been shown to significantly impact care. For instance, patient age seems to have profound impacts on care, and older adults have been understudied as a group.6 The importance of studying the relationship of patient demographic factors to cardiovascular care is underscored when considering patient weight, where a U-shaped relationship has been discovered. While underweight patients have worse outcomes and the most obese patients also do poorly, overweight or obese patients have exhibited better outcomes (the so-called “obesity paradox”).7
To our knowledge, no study has evaluated whether these disparities extend to focused cardiac ultrasound (FOCUS) in the ED. Point-of-care ultrasound is a fundamental aspect of modern emergency care8 and may have a particularly powerful role in changing management and outcomes in cardiopulmonary complaints by reducing morbidity, mortality and ED length of stay.9,10 One study evaluating sex-based differences among comprehensive echocardiograms actually found that men received more non-diagnostic studies.11 However, comprehensive echocardiograms are performed in a vastly more controlled setting, whereas ED FOCUS are often performed on patients wearing street clothing who are unstable with limited mobility and sometimes in very public spaces such as the hallway. We hypothesized that sex trends for FOCUS would be more aligned with the acute myocardial infarction and resuscitation literature, ie, more non-diagnostic FOCUS for female ED patients. The impact on FOCUS quality of other patient characteristics, such as body mass index (BMI) or age, is similarly unknown. Body mass index seems to affect a clinician’s approach to and interpretation of other forms of cardiopulmonary imaging, such as chest radiography,12 but to our knowledge the effect of BMI on FOCUS quality has not been investigated.
Demographic factors such as patient sex, BMI, and age affect the composition and arrangement of body tissues, which may affect ultrasound image quality. The FOCUS consists of four primary views of the heart, each view contributing different
Population Health Research Capsule
What do we already know about this issue? Demographic factors (sex, weight, etc) affect cardiac care, including imaging, but little is known about their impact on cardiac ultrasound, especially in the ER.
What was the research question?
Do demographic factors affect overall cardiac ultrasound imaging quality and omission of views in the ED?
What was the major finding of the study?
Females had lower Apical 4-Chamber (A4C) quality and more A4C omissions (p<0.001); overall image quality was the same.
How does this improve population health?
Demographic factors are associated with important and clinically significant differences; future education, design, and research should focus on these discrepancies.
clinical information, and no single view provides complete diagnostic information13 (Figure 1). The apical four-chamber (A4C) view is obtained just under the pectoralis muscle in the fourth or fifth intercostal space at the apical impulse and provides vital diagnostic information regarding ejection fraction, valvular disease, right heart strain, and diastology. In women, this is often within the breast crease. The positioning required for this view could be particularly susceptible to anatomic and social influences on image acquisition.
We postulated that clinician or patient discomfort with breast exposure and image-acquisition challenges unique to women may correlate with differences in clinician behavior and image quality. Establishing this relationship could help build a framework for quality improvement in FOCUS, which could support more accurate diagnosis and management of highly morbid conditions. Because this is a relatively unstudied topic, a large, multicenter study, evaluating existing patterns would help elucidate the status quo and prime what will hopefully be a fruitful area of research and intervention. Elucidating other areas where inequity occurs could inspire new educational interventions, modified techniques, or equipment innovations.
METHODS
Study Design and Setting
This study was a multicenter, retrospective chart review14 of ED patients who received a FOCUS between January 2018–January 2021 at six academic Level 1 trauma center
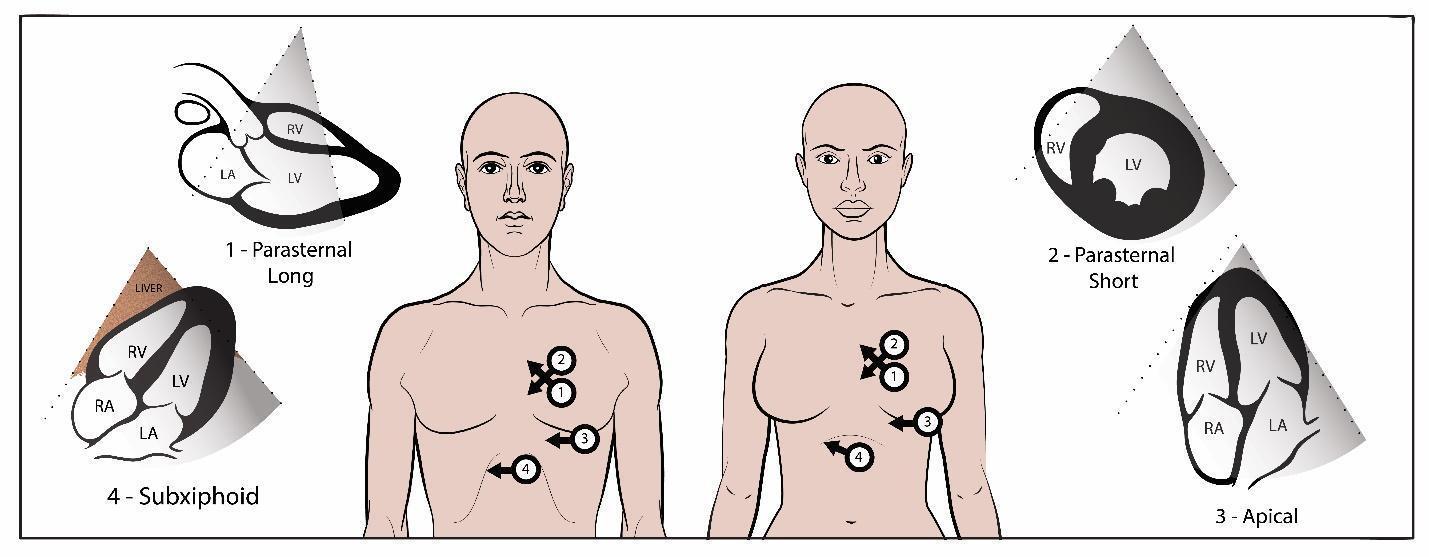
health systems in the United States. Annual ED volumes at the primary sites ranged from 95,000–130,000. Each site has a residency training program and an active emergency ultrasound education program for residents and fellows. The institutional review boards at each center approved this study. As per chart review best practices14 and to reduce bias, the blinded and trained abstractors were without bias and performed a systematic chart abstraction. The data abstracted was limited to basic demographics and was available in the chart. Missing data was not a significant issue.
Selection of Participants
Eligible for inclusion were all adult patients (≥ 18 years of age) with a FOCUS saved in each study site’s image storage solution (Qpath-e, Maple Ridge, BC, Canada; Ultralinq, Athlone, Ireland; or Synchronicity, Bothell, WA) during the study period and submitted for quality assurance. The FOCUS studies must have been performed by a physician operator (eg, resident, fellow, or attending), and operator experience level was determined by the highest level of training obtained by the physician listed as the operator in the storage solution software. (Often, more than one operator is listed as performing the study.) Each of the six sites identified 100 female and 100 male consecutive patients (1,200 total) who underwent FOCUS (Table 1a). Based on our primary outcome of overall FOCUS quality, our sample size of 200 per site was based on an a priori power calculation so that each site would be able to detect a two-point sex difference in the 20-point scale (β = 0.80, two-tailed ɑ = 0.05). Each site determined an enrollment start date within the data collection period, (or two start dates if dividing winter/summer, which sites were allowed to do) and identified consecutive patients in the image storage system who received a FOCUS until they had enrolled 100 female and 100 male patients. The data collection period spanned three years across all sites combined; however, for each individual site, the data collection period was a small fraction of that time. One trained individual at each site performed chart abstraction of deidentified patient demographic data such as age, BMI, and sex using a standardized data collection form. (Appendix 1) This individual was not one of the physicians scoring the FOCUS image quality.
Measurements
At each site, the two faculty members (ultrasound fellowship trained) performing quality review were blinded to the patient’s health record and to the other reviewer’s scoring. Reviewers scored each of the available four views (Figure 1): parasternal long axis; parasternal short axis; A4C; and subxiphoid. Scoring criteria ranging from 1-5 per view on an ordinal scale with 5 being highest (Table 2) Omitted FOCUS views were noted on the spreadsheet. The two expert reviewers
Figure 1. Probe positioning to obtain the four focused cardiac ultrasound views on a male and a female patient.
Table 1a. Baseline Characteristics of Patients
Table 1b. Baseline Characteristics of Sonographers
BMI, body mass index.
Collapsed Score Raw Score
1
2
3
Raw Score Criteria
1 No Recognizable Structures, Insufficient for Diagnosis
2 Minimally Recognizable Structures, Insufficient for Diagnosis
3 Structures Recognized with Some Technical Flaws, Minimal Criteria Met for Diagnosis
4 All Structures Imaged with Some Technical Flaws, Diagnosis Easily Supported
5 All Structures Imaged with Excellent Image Quality, Diagnosis Completely Supported
FOCUS, focused cardiac ultrasounds.
at each site scored the FOCUS exams independently using the same scoring rubric, and their scores were subsequently averaged. This rubric is suggested for use by an American College of Emergency Physicians clinical guideline.15
Statistical Analysis
Data collected from the six study sites were imported into SAS v9.4 (SAS Institute Inc, Carey, NC) for analysis. We investigated three outcome variables through separate mixedeffects regression models: overall FOCUS quality; A4C quality; and A4C omission. Our primary outcome was overall FOCUS quality, ie, the summed score of the four FOCUS views. Our secondary outcome measures were the individual FOCUS scores and omission rates. We aimed to evaluate the impact of patient and sonographer demographics on the FOCUS scores and omission rates. Other than patient sex, the demographics of interest were BMI (normal = 18.5-24.9 kg/ m2, overweight = 25-29.9 kg/m2, and obese = 30.0+kg/m2), age, sonographer sex, and sonographer training level.
Overall Quality of Focused Cardiac Ultrasound
The overall FOCUS quality was treated as a continuous outcome variable from 1-20 summed across the four views. The scores of the two raters per site were averaged to create one patient score for the site. First, we performed an unadjusted, mixed-effects linear regression model to determine the association between overall quality and patient sex, with study sites considered as random effects. The models were then adjusted for patient age, BMI, operator sex, and operator experience level. We tested interaction terms between patient sex and operator sex. Mean differences, 95% confidence intervals (CIs), and P-values were reported. P < .05 was considered to be statistically significant.
Quality of Apical Four-Chamber Views
For A4C quality, there were a limited number of FOCUS views with scores of 5. To address statistical modeling issues due to small cell sizes for scores of 5, we collapsed the 1-5 scores into three clinically relevant categories: category 1 comprised scores of 1-2 (poor image quality insufficient for diagnosis); category 2 comprised scores of 3 (adequate but
Collapsed Score
Imaging Insufficient for Diagnosis
Minimum Imaging Criteria Met for Diagnosis
Imaging Easily Supports Diagnosis
with flaws that could affect interpretation); and category 3 was comprised of scores of 4-5 (high quality images that allowed for a confident answer to the clinical question being asked of that view). We ran unadjusted, mixed-effects logistic regression models to evaluate the association between A4C quality and patient sex (A4C quality of 2 vs 1 and A4C quality of 3 vs 1 as the outcomes); study sites were included as random effects terms. We then adjusted models for patient age, BMI, operator sex, and operator experience level. As above, interaction terms between patient sex and operator sex were tested. We reported odds ratios with 95% CI.
Interrater Agreement Assessment
We calculated weighted kappas to evaluate the rating agreement between the two reviewers for each of the four views. Additionally, we used Kendall tau coefficients to measure the ordinal association between pairs of ratings.
RESULTS
Characteristics of Study Subjects
A total of 1,200 patients (50% female, 50% male) were included across six sites during the study period (January 2018–January 2021). Table 1a shows the demographic characteristics of the study sample. A significant portion of study participants were > 65 years of age (Table 1). The largest proportion of participants had a calculated BMI within normal range, followed by overweight (Table 1). Most sonographers were resident physicians, and a slight majority identified as male (Table 1b).
Image Quality and Omission Rates
Female patients had lower average A4C quality scores than male patients and were more likely to have the A4C view omitted, P < .001. However, male and female patients had similar overall FOCUS quality (Table 3b). Both the unadjusted and adjusted mixed-effects linear regression models showed no significant difference in total FOCUS score for female vs male patients (Appendix 3). Females had slightly higher PSS scores, and lower omission rates (Table 3a/b). The patient sex by sonographer sex interaction term was not significant. Patient sex was statistically significant in both the
Table 2. FOCUS Quality Score Rubric
Rate by Patient Sex
FOCUS, focused cardiac ultrasounds; PSL, parasternal long axis; PSS, parasternal short axis; A4C, apical four-chamber; SX, subxiphoid; IVC, inferior vena cava.
Table 3b. Overall FOCUS Quality Score by Sex (total and by view)
FOCUS scores compared to middle-aged patients (Figure 2b). Quality of FOCUS decreased with advancing age (Figure 2b).
Interrater Agreement:
On average, there was 30%-60% agreement on ultrasound scores between the two reviewers on the five-point scale ratings Furthermore, the ratings between the two reviewers had moderate (kappa minimum = 0.49) to strong (kappa maximum = 0.70) positive agreement, and the Kendall tau also showed the range of rater concordance to be moderate (0.34-0.68).16
DISCUSSION
FOCUS, focused cardiac ultrasound; PSL, parasternal long axis; PSS, parasternal short axis; A4C, apical four-chamber; SX, subxiphoid; IVC, inferior vena cava.
unadjusted and adjusted mixed-effects logistic regression models for the A4C quality outcome (Appendix 3). Unadjusted, male patients had higher odds of receiving a diagnostic A4C view compared to female patients (Appendix 3).
Sonographer Demographics
Scans performed by male sonographers, on average, scored lower than those performed by female sonographers (Appendix 3). Scans with attending sonographers had lower overall FOCUS quality scores than scans with resident sonographers (Appendix 3). Scans with male sonographers were less likely than scans with female sonographers to achieve an adequate A4C score (Appendix 3).
Body Mass Index and Quality of Focused Cardiac Ultrasound
Underweight and obese patients had lower total FOCUS quality scores compared to patients with normal BMI (Figure 2a). Total FOCUS quality scores decreased with deviation from normal BMI. Both obesity and being underweight were negatively associated with A4C score. Patients with an obese BMI had 62% lower odds of receiving a high-quality A4C compared to patients with a normal BMI, and this difference became more pronounced as weight increased to the highest weight category (BMI 40+) (Appendix 3).
Age and Quality of Focused Cardiac Ultrasound
On average, our youngest age category had higher total
We investigated whether there were discrepancies in FOCUS quality correlating with patient and sonographer demographics. In this large, retrospective, multisite study, A4C views on female patients were of lower quality and more often omitted, and male sonographers were more likely to achieve non-diagnostic A4C images; however, we found no significant difference in overall FOCUS quality for male compared to female patients. Although the absolute effect size of some of these differences was small (eg, 2.3 vs 2.6 score for A4C view on five-point scale for females vs males), that females were 30% less likely to receive a diagnostic A4C view that could have been clinically significant. The fact that we found differences in the A4C view but not in overall quality could signal that clinicians may be attempting to use alternative views to compensate for and obtain similar information among the sexes. Supporting this notion is that parasternal short axis scores for females were of slightly higher quality and less frequently omitted. Our trial was not designed to discern compensatory behavior.
The A4C view provides unique information, and we believe its omission has important clinical implications. If avoiding the A4C view in females is related to exposure of the chest, this would be in line with research on cardiopulmonary resuscitation and AED placement establishing that female chest exposure has been an impediment to ideal care, especially in public settings.5 This has further implications as “hallway medicine” becomes more commonplace in EDs. Given the potentially sensitive position in which the operator’s hand and probe must be placed to obtain the view—exposing the chest—and that breast tissue could obfuscate this view, it is not surprising that female patients had fewer diagnostic A4C views, and that male sonographers in particular are 30% more likely to obtain a non-diagnostic view.
Part of this discrepancy may also relate to biases inherent in training materials. For example, live ultrasound models and ultrasound simulation diagrams or manikins traditionally feature prototypical male anatomy. We should work to incorporate women into our ultrasound education and normalize examination of female anatomy in a patient-centered way.
Future research could elucidate the etiologies of these discrepancies. Whether they are social, anatomical, or environmental has implications for addressing them: if differences are predominantly due to social factors, clinician educational interventions could be instituted and paired with a
Table 3a. Overall FOCUS Omission
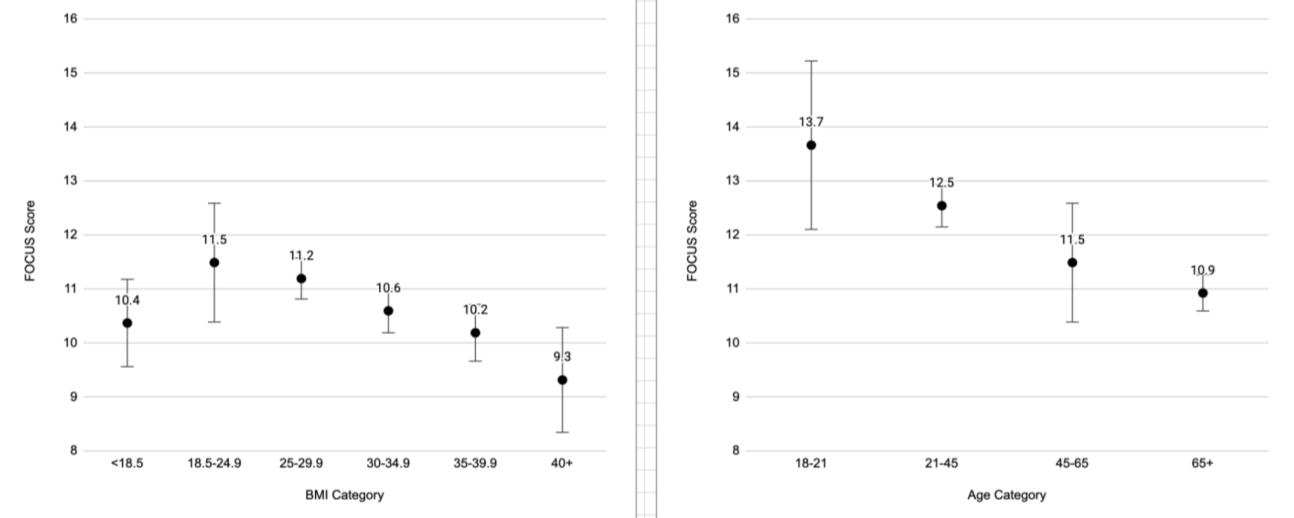
Figure 2. Total focused cardiac ultrasound score by (a) body mass index category (ref 18.5-24.9) and (b) age category (45-65). Bars indicate 95% CI.
dialogue script to facilitate communication and ease of the exam, similar to the way in which other sensitive examinations (eg, pelvic) are taught. If anatomy is found to be the larger factor, innovations that alter the chain between the patient’s body position, probe, hand, and operator could be engineered to address this. Finally, environmental effects, although sometimes beyond the control of individual clinicians, could reinforce the value of private rooms, privacy screens, or gowned patients.
As a patient’s BMI deviated from normal toward either underweight or overweight their FOCUS quality scores decreased (Figure 2a). Patients with a normal BMI had the highest overall quality FOCUS scores, suggesting that either sparse or abundant subcutaneous tissue presents challenges to obtaining high-quality views. Underweight individuals may be difficult to scan due to a lack of tissue to seat the probe between the ribs. This discrepancy is reminiscent of the “U-shaped” relationship that has been demonstrated regarding BMI and overarching cardiovascular clinical outcomes. In this case, patients with higher BMI may have additional tissue that obscures landmarks, creates a physical barrier to probe positioning, and introduces more tissue between the probe and the target organ. Higher BMI patients may also not be as physically able to cooperate with body positioning maneuvers to optimize the A4C view. Patient age also significantly impacted total FOCUS quality, with deterioration as age increased (Figure 2b). There are many possible reasons why younger patients might receive higher quality scans. These may include a greater ability to easily lie flat or on their left side, a lower acuity allowing for more time to perform the exam, a lower likelihood of receiving positive pressure ventilation, or a higher percentage of educational scans. Future work specifically targeting the underweight, overweight, and advanced-age populations should focus on optimizing technique and equipment (probes, sensors, software).
Clinician sex and training level are correlated with statistically significant changes in overall FOCUS quality. Although male physicians produced lower quality images, the
difference was minor, and it is unclear what may have led to this outcome. Previous studies have found inequity in cardiovascular care between sexes that was modified by the sex concordance of the clinician and patient17; however, in our sample, clinician-patient sex interactions were not significant. Attending physicians, as compared to residents, produced lower quality images, which most likely reflects the positive influence of contemporary medical education on ultrasound skills. As with other procedures, skill attrition may occur over time. Further studies should explore this relationship to optimize continuing education for attendings.
LIMITATIONS
This retrospective study could not account for the clinical scenario in which FOCUS was used. As a result, the information sought with FOCUS by the operator was uncertain; it is possible that the necessary clinical information in some studies was attainable without an A4C view and, therefore, it was deemed unnecessary by the clinician. It is also possible that some individual views or studies were never saved due to poor windows, and the retrospective design prevented us from knowing to what extent this happened in various groups. In our best attempt to account for this lack of context, the primary outcome of total FOCUS quality was a summed score reflecting the total amount of clinical information the operator obtained. It is also possible that some studies were never saved at all due to poor views, and the retrospective design prevented us from determining to what extent this happened in various groups. Additionally, we acknowledge that BMI reporting may not always have been accurate given that ED patients do not always have updated weights and heights measured in the ED due to the acuity of care and variability in availability of equipment.
A further limitation is that we included some educational scans in our study due to the heterogeneous nature of ultrasound logging culture at different institutions. In theory, educational scans may show biases toward young, healthy,
compliant, normal BMI, and male patients, a population to which learners may be drawn to select for the perceived ease of obtaining images. To minimize this, we interviewed each site regarding their cultural practices and the expected composition of their scans and concluded that most “educational” scans were clinically indicated scans performed on patients with acute pathology. Therefore, we feel that the data presented is representative of clinical FOCUS use at academic institutions.
We controlled for operator experience level in our adjusted model, and by finding an impact of operator experience level it seems logical that within our experience-level groups there was further experienced-based heterogeneity. The granularity of those differences could not be captured by our data. For instance, a junior resident may not obtain as high-quality images as a senior resident, and a recently trained attending may outperform an attending who was trained decades ago without formal ultrasound training.
Kappas in our study were moderate. The scale we used is, as far as we know, the most ubiquitous FOCUS scale that has been suggested for use by an ACEP clinical guideline15 and has been the default scale for quality assessment software. Despite this, it is unstudied, and its reliability and validity still need to be determined. As far as we know, our study is the first to explore point-of-care ultrasound quality quantitatively as it relates to patient sex, clinician sex, and other demographic factors. Previous literature in cardiology discusses diagnostic or non-diagnostic scans but did not use a quantitative score. For all categorical ordinal data, we chose a priori reference groups, and for each demographic we used our best judgment in selecting the a priori reference group.
Due to small cell sizes for a score of five, we condensed the individual view scores down to three categories for this separate analysis. However, the total score of 20 remained (four views with a possible score up to five for each view). This could have impacted results by failing to capture differences among the extreme ends of the scale. To minimize this, we selected categories that were overall clinically very similar (For example, grouping “no recognizable structures” with “minimally recognizable structures - insufficient for diagnosis” created a category in which none of the images were good enough to draw a diagnostic conclusion.) Scores of 4 or 5 are also very similar, and both easily support a diagnosis.
Finally, the allowed data collection period spanned three years across all sites combined; however, the identified echocardiograms for inclusion at each individual site occurred within the period of a a few months. The volume of FOCUS at each site was high, and 200 consecutive FOCUS scans were easily identified in a fraction of the full study period. Each site began their data collection at various times based on IRB approval and changes in image storage solutions. We do not believe that the ultrasound technology advanced significantly during this time frame. Neither do we believe that images taken earlier in the study period were of inherently lower quality than
those obtained later in the study period due to technological advancements.
CONCLUSION
While we found that females received lower quality images and more frequently omitted apical four chamber views on their focused cardiac ultrasound, we did not find a difference in overall FOCUS quality by sex. The A4C view provides information about the right ventricle and valves that cannot be obtained from other views. Females were significantly less likely to receive a diagnostic A4C view, and we believe that even small differences in data acquisition from the A4C view could represent a clinically important finding. Another important and clinically significant finding was that underweight and overweight patients receive lower quality images than patients with a normal BMI. Perhaps for our underweight patients we can apply a gel pad to better optimize their images.
Older patients, for whom cardiovascular disease is more common, also received lower quality FOCUS scores. It is of interest that male sonographers and attending physician sonographers both achieves lower quality scores. While it is unclear why male sonographers’ image quality was worse, the difference was slight. However, for older attendings, perhaps we were witnessing skills attrition vs attendings who graduated before ultrasound was core to resident education. Skills attrition is not unique to ultrasound.
Our study, which investigated some of the most important demographic factors and how they may affect FOCUS image acquisition and quality, represents an essentially unstudied aspect of a core modality in our specialty. It is also, to our knowledge, the first study to report kappas on a widely used quality assessment metric—the five-point echo scale used by many institutions for internal quality review of FOCUS images. Further studies should attempt to validate this quality scale and prospectively examine the relationship between demographic factors and ultrasound image quality. Ultimately, we should seek to explore the implications and rationale behind the tendency to omit or be unable to obtain a highquality view and the clinical rationale for performing or not performing views based on patient presentation.
AUTHORS CONTINUED
Megan Leo, MD§
Joseph R. Pare, MD, MHS†
Meera Muruganandan, MD§
Josh Kaine, MD||
Daniel S. Brenner, MD PhD||
Pam Cruz Soriano, MD||
Nadia Aracelliz Villarroel, MD¶
Michele L. Schroeder, MD¶
Natalie Strokes, DO¶
Anna Tyson, MD¶
Timothy Gleeson, MD**
Michael Hill, MD**
Impact of Patient and Sonographer Demographics on Quality of Focused Cardiac Ultrasounds
Janette Baird, PhD†
Alyson J. McGregor, MD†† Kristin H. Dwyer, MD†
Boston University Chobanian & Avedisian School of Medicine, Department of Emergency Medicine, Boston, Massachusetts
Indiana University School of Medicine, Department of Emergency Medicine, Indianapolis, Indiana
Baystate Medical Center, Department of Emergency Medicine, Springfield, Massachusetts
UMass Chan Medical School, Department of Emergency Medicine, Worcester, Massachusetts
University of South Carolina School of Medicine / Prisma, Department of Emergency Medicine, Greenville, South Carolina
Address for Correspondence: Barret Zimmerman, MD, Harvard Medical School / Mass General Brigham, Emergency Medicine, 75 Francis St, Boston, MA 02115. Email: bzimmerman1@bwh. harvard.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Zimmerman et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http:// creativecommons.org/licenses/by/4.0/
REFERENCES
1. Kuhlman J, Moorhead D, Kerpchar J, et al. Clinical transformation through change management case study: chest pain in the emergency department. EClinicalMedicine. 2019:10:78-83.
2. Reitan C, Andell P, Alfredsson J, et al. Excess mortality and loss of life expectancy after myocardial infarction: a registry-based matched cohort study. Circulation. 2024;150(11):826-835.
3. Liakos M, Parikh PB. Gender disparities in presentation, management, and outcomes of acute myocardial infarction. Curr Cardiol Rep. 2018;20(8).
4. Blewer AL, Starks MA, Malta-Hansen C, et al. Sex differences in receipt of bystander cardiopulmonary resuscitation considering neighborhood racial and ethnic composition. J Am Heart Assoc. 2024;13(5):e031113.
5. Munot S, Bray JE, Redfern J, et al. Bystander cardiopulmonary resuscitation differences by sex -- the role of arrest recognition.
Resuscitation. 2024;199:110224.
6. Pezzin LE, Keyl PM, Green GB. Disparities in the emergency department evaluation of chest pain patients. Acad Emerg Med 2007;14(2):149-156.
7. Ratwatte S, Hyun K, D’Souza M, et al. Relation of body mass index to outcomes in acute coronary syndrome. Am J Cardiol 2021;138:11-19.
8. Beeson MS, Bhat R, Broder JS, et al. American Board of Emergency Medicine. The 2022 Model of the Clinical Practice of Emergency Medicine. J Emerg Med. 2023 Jun;64(6):659-695.
9. Huang CT, Chang CH, Chen JY, et al. The effect of point-of-care ultrasound on length of stay and mortality in patients with chest pain/dyspnea. Ultraschall Med. 2023;44(4):389-394.
10. Goldsmith AJ, Shokoohi H, Loesche M, et al. Point-of-care ultrasound in morbidity and mortality cases in emergency medicine: Who benefits the most? West J Emerg Med. 2020;21(6):172-178.
11. Ellenberger K, Jeyaprakash P, Sivapathan S, et al. The effect of obesity on echocardiographic image Quality. Heart Lung Circ 2022;31(2):207-215.
12. Seo G, Robinson J, Punch A, et al. Understanding radiographic decision-making when imaging obese patients: a think-aloud study. J Med Radiat Sci. 2022;69(1):13-23.
13. Hall MK, Coffey EC, Herbst M, et al. The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance. Acad Emerg Med. 2015;22(5):583-593.
14. Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014 Sep;64(3):292-8.
15. Liu R, Blavias M, Moore C, et al. Emergency Ultrasound Standard Reporting Guidelines. American College of Emergency Physicians (ACEP). 2018. Available at [https://www.acep.org/siteassets/uploads/ uploaded-files/acep/clinical-and-practice-management/policystatements/information-papers/emergency-ultrasound-standardreporting-guidelines---2018.pdf]. Accessed March 28, 2025.
16. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276-82.
17. Harik L, Yamamoto K, Kimura T, et al. Patient–physician sex concordance and outcomes in cardiovascular disease: a systematic review. Eur Heart J. 2024;45(17):1505-1511.
18. Peitz GW, Troyer J, Jones AE, et al. Association of body mass index with increased cost of care and length of stay for emergency department patients with chest pain and dyspnea. Circ Cardiovasc Qual Outcomes. 2014;7(2):292-298.
19. Rich MW, Chyun DA, Skolnick AH, et al. Knowledge gaps in cardiovascular care of the older adult population: a scientific statement from the American Heart Association, American College of Cardiology, and American Geriatrics Society. J Am Coll Cardiol 2016;67(20):2419-2440.
Supra-Short Ultrasound Protocol for Rotator Cuff Tears in the Emergency Department: Pilot Study
Tony Zitek, MD*†
Robert A. Farrow II, DO*
Michael Shalaby, MD*
Daniel Puebla, MD*
Alejandro Sanoja, MD*
Edward Lopez, MD*
Joseph McShannic, MD*
Yonghoon Lee, MD*
Nicole Warren, DO*
Daniella Lamour, DO*
Jiodany Perez, MD*
Michael Rosselli, MD*
Section Editor: Matthew J. Fields, MD
Mount Sinai Medical Center, Department of Emergency Medicine, Miami Beach, Florida
Kaiser Permanente Modesto Medical Center, Department of Emergency Medicine, Modesto, California * †
Submission history: Submitted March 10, 2025; Revision received July 4, 2025; Accepted July 7, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.46984
Introduction: Although ultrasound is readily available to emergency physicians and known to be very accurate for diagnosing rotator cuff tears, it is rarely used for this purpose. Our goal in this study was to develop and preliminarily assess the accuracy of a simplified shoulder ultrasound protocol (the “suprashort” protocol), designed to be used by emergency physicians for diagnosis of supraspinatus tears.
Methods: We performed a pilot diagnostic accuracy study in which we assessed the accuracy of the supra-short protocol as performed by minimally trained emergency physicians for identifying supraspinatus tears in volunteers. As a criterion standard, a sports medicine physician also performed a complete shoulder ultrasound on each volunteer. We determined the test characteristics of the supra-short protocol for supraspinatus tears, as well as the median time to complete a scan and the percentage of images deemed adequate by expert review.
Results: Nine emergency physicians performed a total of 40 bilateral supra-short scans on six volunteers (two of whom were known to have shoulder pathology and four of whom had normal shoulders). Of the 80 shoulders scanned, there were 18 cases in which complete ultrasound performed by the sports medicine physician revealed a supraspinatus tear; 12 (66.7%) of those were identified by the novice sonographers using the supra-short protocol. Overall, the sensitivity of the supra-short protocol was 66.7% (95% CI 29.9-92.5%) and the specificity was 87.1% (95% CI 70.2-96.4%). The median time to completion of each shoulder was 133 seconds (interquartile range 88-182). Upon expert image review, 80.0% of the images were deemed adequate.
Conclusion: After minimal training, emergency physicians were able to quickly perform the supra-short US protocol but were only able to identify supraspinatus tears with moderate accuracy, suggesting the need for more extensive training before clinical use. [West J Emerg Med. 2025;26(5)1431–1437.]
INTRODUCTION
In 2021, over 1.47 million patients presented to an emergency department (ED) in the United States for a
shoulder injury,1 and many others presented for atraumatic shoulder pain. Emergency physicians often order a radiograph for patients with shoulder pain, which is the recommended
first-line test for both traumatic and atraumatic shoulder pain by the American College of Radiology.2,3 While radiographs are highly useful for identifying fractures and other bony pathology, they have limited value for the diagnosis of soft tissue pathology.2,3 When radiographs do not reveal the etiology of the shoulder pain, magnetic resonance imaging (MRI) is the recommended test for soft tissue pathology of the shoulder.2,3 However, given its high cost and limited availability, it is rarely used in the ED. Thus, patients who present to the ED often receive a non-specific diagnosis (such as “shoulder pain”), which they may justifiably feel is inadequate.
While MRI is expensive and often unavailable in the ED, point-of-care ultrasound (POCUS) is readily available and inexpensive. Although partial, rotator cuff tendon tears may be difficult to accurately diagnose on ultrasound,4 for complete tears, radiology,5 sports medicine,6 and orthopedic literature7 have all reported that MRI and ultrasound have comparable test characteristics. We believe that emergency physicians should try to diagnose complete rotator cuff tears to expedite referral to orthopedics for a potentially surgical problem.
Previous data have shown emergency physicianperformed POCUS to be highly accurate for shoulder dislocations and fractures,8,9 but there have been no published studies assessing the accuracy of emergency physicianperformed shoulder POCUS for soft tissue injuries. The published evidence is limited to a case series describing the use of POCUS for identifying rotator cuff pathology in four patients.10 Moreover, although the American College of Emergency Physicians lists musculoskeletal ultrasound as one of its core applications,11 there is no established protocol for soft tissue shoulder POCUS with regard to what structures should be assessed and how.
Given the potential of POCUS to substantially increase the diagnostic accuracy of emergency physicians assessing patients with shoulder pain along with the lack of data in this area, we developed a POCUS protocol for emergency physicians to evaluate the rotator cuff (called the “suprashort” protocol). We then performed a pilot study to assess the feasibility and accuracy of our POCUS protocol for diagnosing rotator cuff (specifically supraspinatus) tears.
METHODS
Study Design and Setting
We performed a pilot, diagnostic-accuracy study to preliminarily assess a novel POCUS protocol designed to be used by emergency physicians without fellowship training in sports medicine or ultrasound to diagnose supraspinatus tears. The study was performed on volunteers (not patients) who were recruited by two of the investigators from a pool of colleagues, friends, and family, some of whom had known shoulder pathology. Anyone (with or without shoulder pain) could volunteer. Volunteers signed written, informed consent and were not compensated. The study was approved by
Population Health Research Capsule
What do we already know about this issue?
Ultrasound is highly accurate for the diagnosis of rotator cuff tears but is rarely used for this purpose in the emergency department.
What was the research question?
Can emergency physicians use an abbreviated shoulder ultrasound protocol to accurately diagnose supraspinatus tears?
What was the major finding of the study?
The sensitivity was 66.7% (95% CI 29.992.5%), and the specificity was 87.1% (95% CI 70.2-96.4%).
How does this improve population health?
With further training, emergency physicians may be able to use this shoulder ultrasound protocol to rapidly identify and refer patients with rotator cuff tears.
Mount Sinai Medical Center Institutional Review Board. We followed the Standards for Reporting of Diagnostic Accuracy Studies guidelines.
Rationale and Development of the Supra-short Protocol
The supra-short protocol was designed by one attending physician in emergency medicine (EM) (who had no ultrasound- or sports medicine-fellowship training) and two emergency physicians with sports medicine- fellowship training. In the process of developing the supra-short protocol, they considered several issues. First, a complete shoulder ultrasound protocol generally requires the patient to place their arm in five different positions, and it includes an assessment (multiple views) of each of the following structures: long head of the biceps tendon; subscapularis tendon; coracoacromial ligament; supraspinatus tendon; infraspinatus tendon; teres minor tendon; the posterior glenohumeral joint recess; and the acromioclavicular joint. It can also involve a subacromial impingement test.12 The investigators involved in the development of the supra-short protocol believed that a complete shoulder ultrasound assesses for pathology that is not relevant to EM and that it is too cumbersome for emergency physicians without fellowship training. Additionally, they felt that ED patients with acute shoulder pain would be unable to place their arm in the five different positions required for a complete shoulder ultrasound, with the modified Crass position being especially difficult.13 They also felt that emergency physicians would still
likely obtain shoulder radiographs on ED patients who present with shoulder pain; thus, an assessment of bony pathology with POCUS would be duplicative.
Considering the above issues, the goal was to create an ultrasound protocol that was easy to learn, quick to perform, and high yield with regard to pathology seen in the ED. We focused only on the most common soft tissue injury of relevance to EM—rotator cuff tears. We focused on the supraspinatus tendon because supraspinatus tears are the most common rotator cuff tears.14 Indeed, a prior systematic review reported that traumatic rotator cuff tears involve the supraspinatus in 84% of cases.15 Ultimately, the supra-short protocol was designed to be used in conjunction with a shoulder radiograph to help identify patients with complete supraspinatus tears who might benefit from more rapid outpatient follow-up with sports medicine or orthopedic surgery.
Description of the Supra-short Protocol
First, the patient is placed in the lateral decubitus position with the affected shoulder up and with the hand of the side of the affected shoulder on their posterior hip (also known as the modified Crass position. (Figure 1).
Next, the sonographer places a high-frequency linear probe over the anterior shoulder, aligning the probe marker to point directly away from the umbilicus. In the correct location, this will provide a longitudinal view of the supraspinatus tendon (Figure 2).
Lastly, the ultrasound probe should be rotated toward the ear. This will provide a transverse view of the supraspinatus tendon (Figure 3). Although other pathology may be identified, the primary objective of the supra-short protocol is to identify a tear of the supraspinatus tendon, characterized by a visible discontinuity.


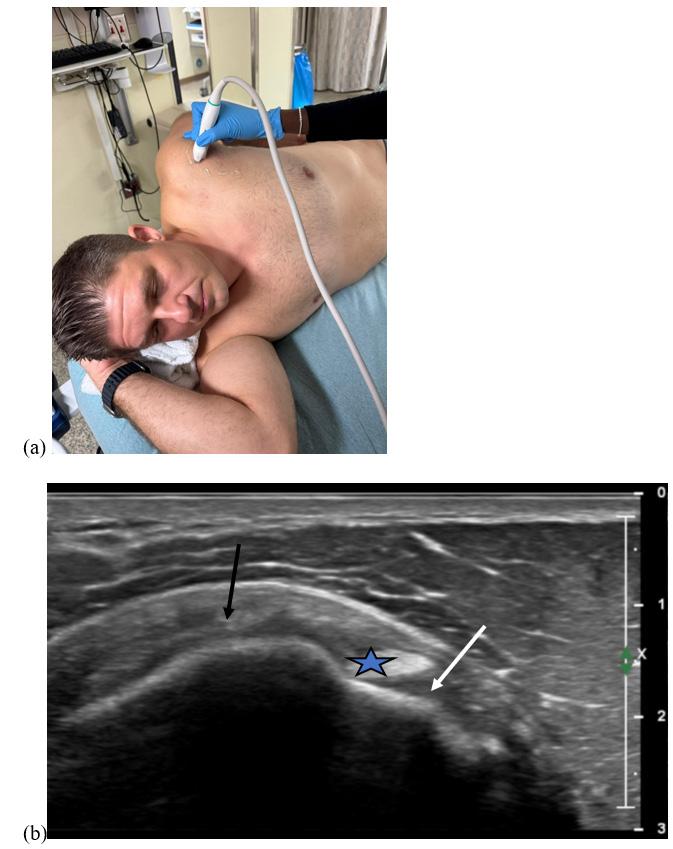
3. (a) Positioning of the ultrasound probe to obtain the transverse axis of the supraspinatus tendon using the supra-short protocol; and (b) normal transverse view of the supraspinatus tendon (black arrow). On this view, the biceps tendon (star) and subscapularis tendon (white arrow) are also visible (although not specifically assessed in the supra-short protocol).
Figure 1. Volunteer in modified Crass position for the supra-short ultrasound protocol.
Figure 2. (a) Positioning of the ultrasound probe to obtain the long-axis view of the supraspinatus tendon using the suprashort protocol; and (b) sonographic long-axis view of a normal supraspinatus tendon.
Figure
Sonographers and Training
The principal investigator sent an email to EM attendings, fellows, and residents in search of volunteers to learn the supra-short protocol and apply it to a second group of volunteers. Nine physicians agreed to participate: four EM residents (one postgraduate year [PGY] 3, two PGY 2, and one PGY 1); three ultrasound fellows, and two non-fellowship trained attendings. The four residents and two attendings had minimal to no prior experience with shoulder ultrasound. The three ultrasound fellows had received some training as part of their fellowship curriculum, but none had ever used POCUS to diagnose a rotator cuff tear in a clinical setting.
The nine volunteer sonographers underwent a one-hour training session about normal supraspinatus anatomy, the supra-short protocol, and rotator cuff pathology. The training included a lecture with example images of supraspinatus tears and hands-on training on healthy volunteers. The training was led by an attending physician in EM with fellowship training in sports medicine and an EM attending physician with fellowship training in emergency ultrasound and extensive experience in musculoskeletal ultrasound.
Data Collection
Nine days after their training session, all data were collected. We recruited six volunteer “patients,” two of whom had shoulder pain and four of whom did not. One volunteer had a recent MRI that demonstrated a complete supraspinatus tear of the left shoulder. The other volunteer with shoulder pain had not had an ultrasound or MRI prior to the day of data collection. A complete shoulder ultrasound performed by a sports medicine physician demonstrated this patient to have calcific tendinosis. The sonographers were blinded from the patient’s clinical history and performed no examination of the patient except for the supra-short ultrasound. Our initial plan was for all nine sonographers to perform the supra-short protocol on both shoulders of all six volunteers. However, variations in availability prevented every sonographer from scanning every volunteer (see Table 1).
A minimum of two images (one transverse and one longitudinal view of the supraspinatus) were saved for each shoulder. The supra-short ultrasounds were performed in the presence of an unbiased research staff member who timed each ultrasound. The start of each ultrasound was defined as the time when the sonographer’s hand first touched the probe, and the end of the ultrasound was defined as the time when the last image was saved. The research staff member asked the sonographer whether each shoulder had a supraspinatus tear (yes or no). Data from each ultrasound were recorded onto a paper data collection form. Sonographers were blinded to the scan results from earlier operators. Sonographers were not provided any information about what percentage of volunteers were expected to have pathology.
As a criterion standard, one practicing sports medicine physician performed complete shoulder ultrasounds on both
Table 1. The number of sonographers who scanned each volunteer using the supra-short ultrasound protocol.
US, ultrasound.
shoulders of all six volunteers. All ultrasounds were performed using a 15 MHz linear transducer of a Philips Affiniti 50 ultrasound machine (Philips Healthcare, Amsterdam, the Netherlands).
Ultrasound Image Review
After data collection, an EM attending with sports medicine-fellowship training reviewed all the images from the supra-short scans. This attending deemed whether each view was adequate to assess for the presence of a tear. If more than one image of a certain view was obtained (such as two transverse views of the supraspinatus), they reviewed both images and deemed the view adequate if either image was adequate. For images deemed inadequate, the reason for inadequacy was recorded.
Outcomes
Our primary outcome was the accuracy (sensitivity and specificity) of the supra-short protocol for supraspinatus tears. Secondarily, we calculated the median time to perform a supra-short ultrasound and the percentage of ultrasound images that were deemed adequate. While we used all ultrasound scans (from each shoulder of each volunteer) for the estimates of the secondary outcomes, only the right shoulder of each volunteer was used for the calculation of the test characteristics. This was done because each shoulder is not independent from the other; thus, calculation of test characteristics using each shoulder as a separate test would not have been statistically valid. Sonographers were unaware that the right shoulder would be used for calculation of test characteristics.
Data Analysis
In performing this pilot study, our goal was to preliminarily assess the supra-short protocol to determine
whether adjustments to the protocol would be beneficial before performing a larger study on patients in a clinical setting. Therefore, we did not perform a formal power analysis to determine the sample size. One research assistant tabulated the data from the data collection forms into Excel v16.90.2 (Microsoft Corporation, Redmond, WA). Using the sports medicine fellowship-trained physician’s complete shoulder ultrasound as the criterion standard, we calculated the sensitivity and specificity (with 95% CIs) of the supra-short protocol for supraspinatus tear using the right shoulder (only) of each volunteer “patient.” Using data from the scan from both shoulders of each volunteer, we calculated the median (interquartile range [IQR]) duration of each supra-short ultrasound. Lastly, we calculated the percentage of ultrasound images deemed adequate.
RESULTS
The nine emergency physicians performed a total of 40 bilateral supra-short ultrasound scans on six volunteers. Four volunteers were female, and two were male; they ranged in age from 25-62 years old. The complete ultrasound performed by the sports medicine physician revealed that one volunteer had bilateral supraspinatus tears (only the left shoulder had been known to have a tear prior to that date) and none of the other five volunteers had a supraspinatus tear. The volunteer with bilateral tears was scanned by all nine sonographers, which produced 18 shoulder views with a supraspinatus tear. Of those 18 cases, the sonographers using the supra-short protocol correctly identified the tear in 12 (66.7%). The supraspinatus tear from the right shoulder is shown in Figure 4.
The second volunteer “patient” who had shoulder pain was found to have pathology consistent with calcific tendinosis on complete ultrasound by the sports medicine physician. Four sonographers scanned this patient (for a total of eight shoulder
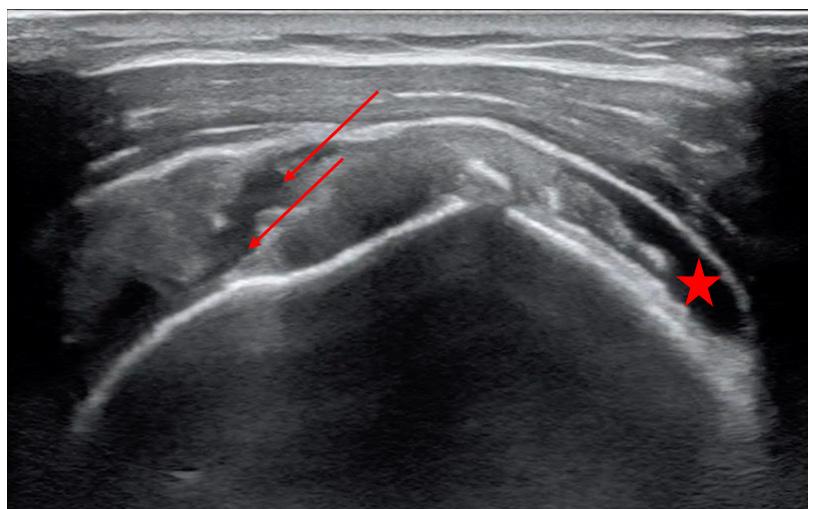
scans). In one of the four cases of the abnormal shoulder, the sonographer interpreted the calcific tendonosis as a partial supraspinatus tear. In the other three cases, the sonographer using the supra-short protocol correctly deemed there to be no supraspinatus tear. The four volunteers who had no shoulder pain had normal complete shoulder ultrasounds; however, in those volunteers, there were six cases in which the sonographer thought there was a supraspinatus tear.
Overall, the sensitivity of the supra-short protocol in this study was 66.7% (95% CI 41.0-86.7%), the specificity was 88.7% (95% CI 78.1-95.3%), and the accuracy was 83.8% (95% CI 73.8-91.1%). Results stratified by level of training are shown in Table 2.
The median time to complete a supra-short ultrasound was 133 seconds (IQR 88-182 seconds). Expert review deemed 80.0 % of the images to be adequate.
DISCUSSION
In this pilot study, we developed the supra-short ultrasound protocol, a novel POCUS technique designed to be used by emergency physicians without expertise in musculoskeletal ultrasound in conjunction with a radiograph to improve diagnostic accuracy in patients with shoulder pain. After one hour of training, a group of emergency physicians who were not experts in musculoskeletal ultrasound were able to obtain adequate views of the supraspinatus 80% of the time, and the median time to complete a scan was short—133 seconds. However, the sonographers were only moderately accurate in their ability to identify supraspinatus tears. In particular, EM residents (who were less experienced in the use of POCUS in general) were the least successful in identifying supraspinatus tears. These results suggest further training would be required before the supra-short protocol could be used diagnostically in the ED.
Despite the somewhat disappointing accuracy of the supra-short protocol in our study, we consider our results encouraging when accounting for the following statements. Currently, most emergency physicians rely on radiograph and physical exam maneuvers to make a diagnosis in patients with shoulder pain. Those assessments are unlikely to lead
Zitek
Figure 4. Long-axis view of the right supraspinatus tendon demonstrating an acute full thickness tear indicated by the red arrows with associated fluid collection. Also visible is a fluid collection superiorly (red star).
Table 2. Test characteristics of the supra-short ultrasound protocol for supraspinatus tears of the right shoulder, stratified by level of training.
to an accurate diagnosis of a rotator cuff tear. In particular, in expert hands, the “full can test” and the “empty can test” were found to be 75% and 70% accurate, respectively, for supraspinatus tears (lower than the accuracy of the suprashort protocol in the hands of novices).16 Additionally, our sensitivity may have been lower than expected because the volunteer “patient” we recruited with a known supraspinatus tear was found to actually have bilateral supraspinatus tears. In musculoskeletal ultrasound, the sonographer is encouraged to compare the affected side to the contralateral (normal) side to help determine whether there is an abnormality.17 This strategy was of limited use in this volunteer, as both shoulders were affected.
Some emergency physicians may believe that POCUS to assess for rotator cuff tears is unnecessary, as they might suggest that all patients follow up for an MRI or with a specialist regardless of the results. However, we would argue that a patient with a supraspinatus tear seen on ultrasound often warrants more urgent outpatient follow-up with orthopedic surgery while a patient with a negative supra-short scan (and no other concerning findings) could follow up first with primary care or a non-surgical specialist. This protocol might be especially useful in resource-limited settings.
Lastly, an additional goal of this study was to determine whether our abbreviated shoulder POCUS protocol should be adjusted. Given that the accuracy of the protocol was only moderate in a group of individuals who were motivated to learn it, we do not think that adding additional views of the shoulder would have been beneficial. We envision that the supra-short protocol could be the basic, soft tissue shoulder ultrasound technique for emergency physicians analogous to assessment for pericardial effusion with the subxiphoid view of the heart. Those with additional interest or training could learn additional views of the shoulder in the same way that some emergency physicians learn more advanced cardiac POCUS skills.
LIMITATIONS
The first limitation to our study is that we likely undertrained our sonographers. We hoped that by substantially simplifying the shoulder ultrasound to just two views we would be able to achieve high accuracy for supraspinatus tears with minimal training, but our data suggest that correct identification of supraspinatus tears requires more extensive training. Additionally, we performed this study on volunteers (rather than actual ED patients), which may have affected our results in multiple ways. For example, as mentioned above, the volunteer with a known supraspinatus tear ended up having bilateral tears, which likely made the diagnosis more difficult than it would be in a patient with an acute (unilateral) shoulder injury. On the other hand, four of the six volunteers had no shoulder pain at all, which might have made it easier to identify that they had no supraspinatus tear. However, given that sonographers were blinded to the patient’s symptoms and
that we had six false positives on these volunteers, we do not think that inclusion of asymptomatic volunteers would have substantially boosted our test characteristics.
Another limitation to consider is that not all sonographers scanned all volunteers; this may have affected our estimates of test characteristics given the expected variability in ultrasound skill of the sonographers and challenges in scanning different volunteers. Finally, even if a supra-short ultrasound is completed and interpreted correctly, it will not identify all rotator cuff tears since it only assesses the supraspinatus. However, considering that the supraspinatus is involved in most rotator cuff tears, the supra-short protocol still has the potential to substantially improve diagnostic accuracy of rotator cuff tears in the ED.
CONCLUSION
We developed a novel point-of-care ultrasound technique (the supra-short protocol) designed to be used by emergency physicians without expertise in musculoskeletal ultrasound to assess for rotator cuff (in particular, supraspinatus) tears. After minimal training, the emergency physicians learned how to obtain the views of the supra-short protocol and performed the scans quickly. They were only able to identify supraspinatus tears with moderate accuracy; thus, more extensive training on identifying pathology would be needed before this protocol could be used diagnostically. Nonetheless, the supra-short protocol may provide a means by which a non-expert in musculoskeletal US may assess for rotator cuff tears; further study is warranted.
Address for Correspondence: Tony Zitek, MD, Kaiser Permanente Modesto Medical Center, Department of Emergency Medicine, 4601 Dale Rd. Modesto, California, 95356. Email:Zitek10@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Zitek et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. US Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2021 Emergency Department Summary Tables. National Center for Health Statistics. Available at: [https://www.cdc.gov/nchs/data/nhamcs/web_tables/2021-nhamcs-
Zitek et al. Supra-Short Ultrasound Protocol for Rotator Cuff Tears in the
ed-web-tables-508.pdf]. Accessed [November 2, 2024].
2. Expert Panel on Musculoskeletal Imaging. Amini B, Beckmann NM, Beaman FD, et al. ACR Appropriateness Criteria® Shoulder PainTraumatic. J Am Coll Radiol. 2018;15(5S):S171-S188.
3. [3]Expert Panel on Musculoskeletal Imaging: Small KM, Adler RS, Shah SH, et al. ACR Appropriateness Criteria® Shoulder PainAtraumatic. J Am Coll Radiol. 2018;15(11S):S388-S402.
4. Itoi E. Rotator cuff tear: physical examination and conservative treatment. J Orthop Sci. 2013 Mar;18(2):197-204.
5. De Jesus JO, Parker L, Frangos AJ, et al. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192(6):1701-7.
6. Roy JS, Braën C, Leblond J, et al. Diagnostic accuracy of ultrasonographyMRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1316-28.
7. Farooqi AS, Lee A, Novikov D, et al. Diagnostic accuracy of ultrasonography for rotator cuff tears: a systematic review and metaanalysis. Orthop J Sports Med 2021;9(10):23259671211035106.
8. Secko MA, Reardon L, Gottlieb M, et al. Musculoskeletal ultrasonography to diagnose dislocated shoulders: a prospective cohort. Ann Emerg Med. 2020;76(2):119-128.
9. Gottlieb M, Patel D, Marks A, et al. Ultrasound for the diagnosis of shoulder dislocation and reduction: a systematic review and metaanalysis. Acad Emerg Med. 2022;29(8):999-1007.
10. Selame L, Walsh L, Schwid M, et al. Point-of-care ultrasound
unveiling rotator cuff injuries in the emergency department: a case series. Cureus. 2023;15(10):e47665.
11. American College of Emergency Physicians. Policy Statement. Ultrasound Guidelines: Emergency, Point-of-care, and Clinical Ultrasound Guidelines in Medicine. 2016. Available at: [https:// www.acep.org/siteassets/sites/acep/media/ultrasound/ pointofcareultrasound-guidelines.pdf]. Accessed January 15, 2025.
12. Musculoskeletal Ultrasound Technical Guidelines. I. Shoulder. European Society of MusculoSkeletal Radiology. Available at [https:// essr.org/content-essr/uploads/2016/10/shoulder.pdf]. Accessed [October, 15 2023].
13. Corazza A, Orlandi D, Fabbro E, et al. Dynamic high-resolution ultrasound of the shoulder: how we do it. Eur J Radiol 2015;84(2):266-77.
14. Zhao J, Luo M, Liang G, et al. Risk factors for supraspinatus tears: a meta-analysis of observational studies. Orthop J Sports Med 2021;9(10):23259671211042826.
15. Mall NA, Lee AS, Chahal J, et al. An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy. 2013;29(2):366-76.
16. Itoi E, Kido T, Sano A, et al. Which is more useful, the ‘‘full can test’’ or the ‘‘empty can test,’’ in detecting the torn supraspinatus tendon? Am J Sports Med. 1999;27:65–8.
17. Schmidt WA, Schmidt H, Schicke B, et al. Standard reference values for musculoskeletal ultrasonography. Ann Rheum Dis 2004;63(8):988-94.
Original Research
Comparing Pediatric 72-Hour Emergency Department Returns: General vs Pediatric Emergency Departments
Dana Libov, DO*
Mark Zocchi, MPH†
Arvind Venkat, MD‡||
Timothy Ruttan, MD§||
Coburn Allen, MD§||
Matthew Wilkinson, MD, MPH§||
US Acute Care Solutions Research Group||
Section Editor: Paul Walsh, MD, MPH
Northwell Health, New Hyde Park, New York Brandeis University, Heller School for Social Policy and Management, Waltham, Massachusetts
Allegheny Health Network, Department of Emergency Medicine, Pittsburgh, Pennsylvania University of Texas at Austin Dell Medical School, Department of Pediatrics, Austin, Texas US Acute Care Solutions, Canton, Ohio
Submission history: Submitted June 4, 2024; Revision received March 31, 2025; Accepted April 7, 2025
Electronically published August 29, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.21302
Introduction: There is limited data comparing pediatric return visits between pediatric emergency departments (PED) and general EDs. We hypothesized that the 72-hour return rate is higher for patients discharged from general EDs than from PEDs.
Methods: We analyzed all PED visits in a large, national emergency medical group that had a repeat ED visit to the same site within 72 hours between 2016–2019. Associated visit- and facilitylevel characteristics analyzed in the model included patient age, Emergency Severity Index and triage level, sex, insurance type, categorized reason for visit, facility type, facility size, trauma status, teaching status, year, and month. Diagnostic categories were defined using the Agency for Healthcare Research and Quality clinical classification software for diagnosis codes. The outcome variable was 72-hour returns. We analyzed returns at the visit-level using descriptive statistics and at the facility-month level using logistic regression to adjust for potential confounders.
Results: A total of 2,588,680 pediatric visits were included: 1,821,800 from 137 general EDs and 766,880 from 7 PEDs. The proportion of children returning to a PED within 72 hours was 1.1 percentage points higher than at a general ED (3.5% vs. 2.4%). The adjusted odds ratio for a 72hour return visit was 1.3 (confidence interval 1.15-1.38) in PEDs compared to general EDs.
Conclusion: Pediatric patients discharged from PEDs had a higher rate of 72-hour return visits than those discharged from general EDs. These findings merit further investigation into factors driving these differences to identify best practices and optimize care across ED settings. [West J Emerg Med. 2025;26(5)1438–1445.]
INTRODUCTION
More than 80% of children who seek emergency medical treatment are seen in a general emergency department (ED).1 Despite the large total volume of patients visiting general EDs, the individual facilities themselves often see very few pediatric patients, with some GEDs seeing as few as ≤10 patients per day.2 However, most pediatric patients are seen in
general EDs, which on average treat <14 children per day.3 Given the variability in pediatric exposure, there is concern that the care provided to pediatric patients in general EDs may be suboptimal when compared to specialized pediatric EDs (PED) that are attached to dedicated children’s hospitals. The 72-hour return visit is frequently used as an indicator of quality in emergency medical care. While these return visits
may represent progression of disease and be unavoidable or even desired in some instances, to the extent that these visits may be preventable and/or unnecessary they “represent an important quality indicator and benchmark for emergency department care.”5 In addition, potentially avoidable return visits have significant implications on use of resources, healthcare costs and reimbursements, and ED crowding.5
There are limited data comparing the frequency of ED return visits for pediatric patients by facility types, specifically PEDs as opposed to the general EDs that see most pediatric patients in the United States. We aimed to investigate the differences in 72-hour ED returns between general EDs and PEDs. We hypothesized that the rate of 72-hour return visits for children would be greater in general EDs than in PEDs based on the difference in frequency of pediatric visits and disparities in pediatric resources, as well as different levels of pediatric-specific expertise and training in facility staff.
METHODS
This was a cross-sectional study of pediatric ED visits treated at EDs staffed by a national emergency medicine staffing group over a four-year period (2016–19). The private dataset is part of the billing database of the staffing company and includes 137 general EDs and 7 PEDs in 22 states. Data elements in this dataset are automatically extracted from electronic health records and billing data at each site. Coding specialists employed by the national group audited the data. The study was approved by the Institutional Review Board of Allegheny Health Network.
We extracted visit characteristics for all patients <18 years of age as this was a study of pediatric patients presenting to the ED. Most of the pediatric hospitals included in this study admit patients up until their 18th birthday; so to ensure uniformity we used this age cutoff for all hospitals. Each visit’s primary diagnosis, per the International Classification of Diseases, Rev. 10 (ICD-10), was assigned to a clinical classification category using the Agency for Healthcare Quality Clinical Classifications Software Refined (CCSR v2019.1). The CCSR aggregates more than 70,000 ICD-10 diagnosis codes into 530 clinically meaningful categories. Members of the study team (DL and TR) then mapped each of these CCSR categories to 52 pediatric emergency reason-forvisit clusters. Additional visit characteristics extracted included age, sex, Emergency Severity Index (ESI) triage level, payor source (commercial, Medicaid, Medicare, selfpay, and other), disposition (discharged, admitted, transferred, etc), and primary treating clinician type (physician or advanced practice practitioner). Characteristics of the EDs included ED size (based on total annual adult and pediatric volume) and ED location classified using urban-rural classification codes (eg, large central metro, large fringe metro, medium metro, and small and non-metro).4
A 72-hour return was defined as a subsequent ED visit to the same ED within 72 hours following discharge from an
Population Health Research Capsule
What do we already know about this issue?
Most pediatric visits occur at general EDs as opposed to pediatric EDs, but little is known about how return rates differ by ED type.
What was the research question?
Do 72-hour return rates differ for pediatric patients seen at general vs pediatric EDs?
What was the major finding of the study?
Pediatric EDs had higher adjusted 72-hour return rates vs general EDs (3.5 vs. 2.4%, aOR 1.3, 95% CI 1.15-1.48, P < .001).
How does this improve population health?
These findings highlight opportunities to improve discharge planning, especially for pediatric patients presenting with high-risk conditions.
original ED visit (the index visit). The discharge date must have occurred between January 4, 2016–December 28, 2019 to allow a 72-hour follow-up period for all index visits. We excluded as index visits patients assigned a triage ESI level of 1 or 2 and those admitted to an inpatient unit or transferred from the ED, as well as those who left without being seen or against medical advice, as these patient groups could be consistently tracked throughout our database. As a result, all index visits had a disposition of discharged with an ESI triage level ≥ 3.
We used descriptive statistics (counts, proportions) to compare index visit and facility characteristics at PEDs and general EDs. To explore differences in 72-hour return rates between general EDs and PEDs, we used logistic regression models to calculate the proportional difference in return rates by visit characteristics and facility characteristics with standard errors adjusted for clustering at the facility level. To estimate the overall difference in return rates between general EDs and PEDs while controlling for potential confounding variables, we then used a multivariable logistic regression model also with cluster-adjusted standard errors. The model included the same index visit and facility characteristics described previously as well as dummy variables for the calendar year and month of visit.
RESULTS
A total of 2,588,680 patients were included across all EDs, with 1,821,800 from 137 general EDs and 766,880 from 7
General vs. Pediatric 72-Hour ED Returns
PEDs. The most common reasons to present to an ED—fever, upper respiratory infection (URI), abdominal pain, rash—were similar across facilities. Congestion and URIs, for example, were 18.9% of visits in general EDs and 22.2% in PEDs (Table 1). The proportion of children returning to a PED within 72 hours was higher than those returning to a general ED (3.5% vs 2.3%), yielding an unadjusted odds (aOR) ratio of 1.48 (confidence interval [CI] 1.35-1.64). When adjusted for sex, age, payor mix, ESI level, pediatric emergency reason-for-visit
clusters, clinician type, ED size, ED location, and year and month of visit, the aOR for a return visit was 1.30 (CI 1.151.48), suggesting the adjusted odds of re-presentation within 72 hours was 30% higher for children presenting to a PED than those seen at a general ED. This relative difference in 72-hour return visits was roughly consistent across ESI levels 3, 4 and 5 as well as facility size, sex, and age (Table 2).
The initial study design excluded ESI levels 1 and 2, as noted in the methods section, to focus on patients with more
Size of facility
Location of facility
Table 1. Characteristics of all index visits.
Table 1. Continued
ED, emergency department; ESI, Emergency Severity Index; ESI, Emergency Severity Index; APP, advanced practice privider.
comparable acuity across ED types. We observed many ESI level 1 and 2 patients discharged from general EDs compared to PEDs. This discrepancy raises the concern that factors unrelated to patient characteristics, such as overtriage due to limited familiarity with pediatric patients in general EDs, may be driving this difference. Importantly, even when we performed an analysis including all ESI levels, the aOR remained
consistent, suggesting that the observed trends were not solely driven by the distribution of ESI levels. The inclusion of these factors highlights the need for further investigation into their contributions to the variability in return visits.
Additional analysis revealed that the percentage of return visits was consistent across different facility sizes and patient age groups, indicating that these factors did not account for
Index visit characteristics
Sex
source
the higher rate of return visits observed at PEDs compared to general EDs. What remains unaccounted for is whether PEDs are disproportionately managing more complex cases, reflecting their role as specialized facilities.
DISCUSSION
We sought to compare 72-hour return visit rates between PEDs and general EDs within a large, national network of EDs. Despite the differences in pediatric volume and presumably familiarity, we found that children seen in a PED
were more likely to return to the same ED within 72 hours as compared to those cared for in a general ED. This finding was contrary to our initial study hypothesis. These findings held true across the most common conditions as well as younger age groups, all of which were less likely to re-present to a general ED than to a PED.
Studies dating back to at least 2004 have explored return rates in pediatric emergency medicine, often in the context of their use as a quality measure or initiatives to reduce these rates.5,13,14 Additionally, analyses using National Hospital
Table 2. Percentage of index visits that returned to the same emergency department within 72 hours.
Table 2. Continued.
ED, emergency department; ESI, Emergency Severity Index; dx, diagnosis; APP, advanced practice practitioner.
Ambulatory Medical Care Survey data have consistently reported pediatric return rates similar to those observed in our study.15 These findings indicate that return rates for pediatric emergency visits are not only well-documented but also consistent across different healthcare settings. However, to differentiate our work, we leveraged the strength of a large, networked ED system with detailed patient- and facility-level
data and explored the differences among general and PEDs. This approach allowed us to explore nuanced differences in return visit rates by facility type, patient age, and specific diagnostic categories. Our analysis revealed that PEDs exhibited higher return rates compared to general EDs, even after adjusting for potential confounders such as triage level and facility size.
We also observed that younger children were more likely to re-present to PEDs than general EDs and that the younger the child, the larger the absolute difference in return visit rates. The reason for this is unclear; our dataset does have limitations as we were unable to analyze the evaluation done on individual patients. For example, it may be that children in the general ED received more testing such as labs and imaging at the initial ED visit, which would have provided general emergency clinicians with more data to determine the extent of illness using objective criteria, as compared to the PED clinicians who may not have performed testing. This may have also decreased the chance of parents returning to the ED if they felt that prior testing excluded certain pathologies or they better understood the exact reason for the illness. It is also possible that there was a difference in the anticipatory guidance provided to families or some other factor that may have impacted the return rates. Additionally, prior research has shown that children with complex or chronic conditions are more likely to revisit EDs, a factor that may disproportionately affect return rates at PEDs.14
The most notable differences in revisit rates between general EDs and PEDs were observed for conditions such as head/neck trauma, seizure, asthma, fever, and congestion/URI (Table 2). Of these, seizures and fevers could potentially be related to medical complexity, although these could not be determined definitively (as noted above). Only congestion/ URI and fevers were in the top five initial presenting diagnoses. The reason for this variation is unclear but does persist across multiple diagnoses. It is unclear whether this was a reflection of care received in a general ED, the comfort of PED clinicians with discharging patients on initial visit, or some combination of factors.
Whether additional testing in a particular ED setting constitutes optimal initial care for both the patient and the medical system depends on the balance between the consequences of overtesting (such as cost, time, and radiation exposure) and the risks of missed pathology, including the outcomes of an ED revisit. Additionally, it is notable that there was a higher percentage of children < 6 years of age seen in PEDs when compared to general EDs in this study, which may have contributed to pediatric emergency clinicians being more comfortable sending younger patients home on the initial visit given the comparative volume of young children that are seen in general EDs. Balancing the value of this initial discharge with higher return rates also merits further investigation (Table 1).
For the most acute cases, care outcomes appeared similar, with comparable death rates for ESI 1 patients in general EDs and PEDs (5.1% vs 4.9%). However, the significantly higher discharge rate of ESI 1 patients in general EDs (60.9% vs 14% in PEDs) raises questions about discrepancies in initial triage based on the ED staff’s comfort level in dealing with children or something intrinsic to the patient population that presents to the different EDs. Recent research suggests that 15% of lower acuity cases (ESI 4 and 5) were undertriaged in general EDs
while over half of ESI 3 and 4 level visits were overtriaged in the general ED and that mistriage was more common in general EDs than in PEDs.16 This points to the possibility that initial triage in the respective settings may ultimately impact 72-hour return visits. Future research should further explore these factors and their implications for pediatric emergency care quality.
LIMITATIONS
Our primary challenge was the limitation of the dataset itself, because we had no way to identify patients who may not have re-presented to the same ED. It is possible that patients may have returned for their second visit to a PED rather than a general ED depending on local hospital availability and patient preferences, which may have skewed the results. That being said, we may safely assume that patients with high-acuity presentations would likely have returned to the closest ED, even if it was the same general ED they had previously visited.
In addition, this dataset encompasses only one large national emergency medicine physician group, and it is subject to data quality and reporting issues intrinsic to that group and its system. The hospitals included in this study represent a diverse network of institutions and patients across a wide variety of geographic regions. The proportion of children treated in pediatric EDs is much smaller when compared to general EDs in our dataset, but this reflects the national landscape that most PED visits do not occur in the pediatric setting, but rather in a community ED.
CONCLUSION
Contrary to our initial hypothesis, we found that pediatric patients discharged from pediatric EDs had a higher rate of 72-hour return visits than those discharged from general EDs. Further research is needed to identify whether this difference is due to systems factors, patient factors, or differences in the quality of care to identify best practices and optimize care across ED settings.
Address for Correspondence: Dana Libov, DO, Donald and Zucker School of Medicine at Hofstra/Northwell, Department of Emergency Medicine and Pediatrics, 300 Community Drive, Manhasset, NY 11030. Email: dlibov@northwell.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Libov et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Gausche-Hill M, Schmitz C, Lewis RJ. Pediatric preparedness of US emergency departments: a 2003 survey. Pediatrics 2007;120(6):1229-37.
2. American Academy of Pediatrics Committee on Pediatric Emergency Medicine, American College of Emergency Physicians Pediatric Committee, Emergency Nurses Association Pediatric Committee. Joint policy statement—guidelines for care of children in the emergency department. Pediatrics. 2009;124(4):1233-43.
3. Gausche-Hill M, Ely M, Schmuhl P, et al. A national assessment of pediatric readiness of emergency departments. JAMA Pediatr 2015;169(6):527-34.
4. Ingram DD, Franco SJ. 2013 NCHS urban–rural classification scheme for counties. Vital Health Stat 2. 2014;(166):1-73.
5. Navanandan N, Schmidt SK, Cabrera N, et al. Seventy-two-hour return initiative: improving emergency department discharge to decrease returns. Pediatr Qual Saf. 2020;5(5):e342.
6. Michelson KA, Hudgins JD, Lyons TW, et al. Trends in capability of hospitals to provide definitive acute care for children: 2008 to 2016. Pediatrics. 2020;145(1):e20192203.
7. Agency for Healthcare Research and Quality. Emergency Severity Index (ESI): a triage tool for emergency departments. 2020. Available at: https://www.ahrq.gov/patient-safety/settings/ emergency-dept/esi.html Accessed April 9, 2025.
8. Akenroye AT, Thurm CW, Neuman MI, et al. Prevalence and predictors of return visits to pediatric emergency departments. J Hosp Med. 2014;9(12):779-87.
9. Healthcare Cost and Utilization Project (HCUP). Clinical Classifications Software Refined (CCSR) for ICD-10-CM Diagnoses. 2022. Available at:https://hcup-us.ahrq.gov/toolssoftware/ccsr/ dxccsr.jsp. Accessed April 9, 2025.
10. United States Department of Agriculture Economic Research Service. Rural-Urban Continuum Codes: Documentation. 2020. Available at: https://www.ers.usda.gov/data-products/rural-urbancontinuum-codes/documentation/. Accessed April 9, 2025.
11. McDermott KW, Stocks C, Freeman WJ. Statistical Brief #242: overview of pediatric emergency department visits, 2015. 2018. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/ sb242-Pediatric-ED-Visits-2015.pdf. Accessed April 9, 2025.
12. Rasooly IR, Mullins PM, Alpern ER, et al. US emergency department use by children, 2001–2010. Pediatr Emerg Care 2014;30(9):602-7.
13. Alessandrini EA, Lavelle JM, Grenfell SM, et al. Return visits to a pediatric emergency department. Pediatr Emerg Care 2004;20(3):166-71.
14. Sills MR, Macy ML, Kocher KE, et al. Return visit admissions may not indicate quality of emergency department care for children. Acad Emerg Med. 2018;25(3):283-92.
15. Cho CS, Shapiro DJ, Cabana MD, et al. A national depiction of children with return visits to the emergency department within 72 hours, 2001–2007. Pediatr Emerg Care. 2012;28(7):606-10.
16. Geanacopoulos AT, Peltz A, Melton K, et al. Pediatric triage accuracy in pediatric and general emergency departments. Hosp Pediatr. 2025;15(1):37-45.
Lorazepam in Managing Atypical Neuroleptic Malignant Syndrome: A Systematic Review of Case Reports
Aaron Chen, MD Myungwook Bae, DO
Maimonides Medical Center, Department of Emergency Medicine, Brooklyn, New York
Section Editor: William D. Whetstone, MD
Submission history: Submitted December 24, 2024; Revision received May 2, 2025; Accepted May 15, 2025
Electronically published August 29, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.41514
Introduction: Neuroleptic malignant syndrome (NMS), comprising typical and atypical presentations, is a rare but life-threatening reaction to antipsychotic medications. While typical NMS is characterized by fever, rigidity, and autonomic instability, atypical NMS often lacks these hallmark features, complicating timely diagnosis in the emergency department (ED).
Methods: We conducted a systematic review of PubMed and citation databases (1988–2024) using the keywords “Neuroleptic Malignant Syndrome” and “Lorazepam.” Case reports were screened using strict inclusion criteria and appraised with the Joanna Briggs Institute Checklist.
Results: Lorazepam led to clinical improvement in 5 of 6 atypical and 7 of 9 typical NMS cases. Among five atypical cases, four demonstrated improvements in altered mental status (AMS), resolution of agitation, and reduction in neuromuscular symptoms within 72 hours, including two within 24 hours, compared to the usual 5-10 day recovery with supportive care alone. One atypical case presenting to the ED showed rapid improvement in AMS following early lorazepam administration, although catatonia ultimately necessitated electroconvulsive therapy. These findings highlight lorazepam’s potential benefit in both timely symptom control and diagnostic clarity in atypical NMS.
Conclusion: Lorazepam shows rapid efficacy in atypical NMS, with most cases improving within 72 hours. Yet its subtle presentation often delays diagnosis in the ED, reducing early treatment opportunities. Typical NMS cases demonstrated slower response. Emergency physicians should maintain a high index of suspicion for atypical NMS and consider empiric lorazepam therapy alongside antipsychotic discontinuation and supportive care. Prospective studies are needed to refine ED management strategies. [West J Emerg Med. 2025;26(5)1446–1453.]
INTRODUCTION
Neuroleptic malignant syndrome (NMS) is a rare and potentially fatal idiosyncratic reaction to antipsychotic medications, primarily dopamine antagonists, and disproportionately affect individuals with psychiatric illness. It exists in two recognized forms: typical and atypical NMS. Typical NMS, defined by the Diagnostic and Statistical Manual of Mental Disorders, 5th Ed as a drug-induced movement disorder, occurs in 0.01-3.2% of neuroleptic-treated patients.1 In contrast, atypical presentation of NMS, known as atypical NMS, offers unique challenges to emergency
physicians due to the absence of one or more hallmark features, such as hyperthermia or elevated creatine kinase (CK) levels, making early diagnosis difficult2 (Table 1).
Pathophysiology
First-generation (typical) antipsychotics exert their effects primarily by blocking dopamine receptors in the brain. In contrast, second-generation (atypical) antipsychotics both inhibit dopamine receptors and antagonize serotonin receptors, while modulating norepinephrine and histamine neurotransmission.3 The pathophysiology of NMS is largely
Table 1. Comparison of typical and atypical neuroleptic malignant syndrome. Typical NMS Atypical NMS
Exclusions The symptoms are not due to other substances or medical conditions.
Risk factor Expose to dopamine antagonist within 72 hours prior to the beginning of symptoms.
Major symptoms 1. Hyperthermia ( > 38oC, measured 2 times)
2. Muscle rigidity (generalized, severe)
Minor symptoms 1. Autonomic nerve system:
Tachycardia
Hypertonia
Sialorrhea
Urinary incontinence
Tachypnea
Dyspnea
Diaphoresis
2. Mental Status: AMS
Stupor to coma
3. Motor symptoms:
Tremor
Akinesia
Dystoria
Myoclonia
Trismus
Dysarthria
Dysphagia
4. Lab Finding: CK↑ Leukocytes↑ Myoglobin↑ Catecholamines↑ Creatinine↑ Metabolic acidosis
Hypoxia
↑, elevated levels.
1. Often absent or mild.
2. Muscle rigidity (mild to moderate)
1. Autonomic nerve system: Present, but less severe
2. Mental status: Less severe
3. Motor symptoms: Present, less severe
4. Lab finding: May present mildly abnormal, but often normal
NMS, neuroleptic malignant syndrome; AMS, altered mental status; CK, creatine kinase.
attributed to the blockade of dopamine D2 receptors in key regions such as the hypothalamus, striatum, and spinal cord, resulting in dysregulation of muscle control, thermoregulation, and autonomic function.4
Neuroleptic malignant syndrome has been associated with nearly all antipsychotics. However, high-potency typical antipsychotics are generally considered to pose a greater risk for NMS compared to low-potency atypical antipsychotics. Pharmacodynamic differences between these two classes are notable. Atypical antipsychotics tend to have a lower affinity for dopamine D2 receptors but are potent antagonists of the 5-HT2A serotonin receptor. This higher ratio of 5-HT2A to D2 receptor occupancy is believed to account for the reduced incidence of extrapyramidal side effects seen with atypical antipsychotics.5
Evidence from case reports and retrospective studies suggests the existence of atypical NMS, particularly in association with atypical antipsychotics such as quetiapine and clozapine.6, 7 However, it remains uncertain whether these atypical presentations represent early or impending NMS.
Additionally, the potential involvement of other neurotransmitter systems, beyond dopamine, in the pathogenesis of NMS induced by atypical antipsychotics is unclear. Clinicians should be vigilant in assessing for NMS in patients receiving any antipsychotics and should not prematurely rule out the diagnosis when classic features such as severe rigidity or hyperthermia are absent.8
Management and Therapeutic Strategies
Early recognition of atypical NMS in the emergency department (ED) is challenging, as it often requires considerable time to rule out other potential causes of symptoms. Even after excluding other possibilities, emergency physicians may struggle with the diagnosis because atypical NMS often deviates from standard diagnostic criteria and can closely resemble other similar conditions. Overlooking the possibility of atypical NMS from normal lab results could cause delay in withdrawing the offending medication and rapidly lead to severe complications or even death.9
Atypical NMS is most commonly associated with atypical antipsychotics, with only a few reported cases of haloperidolinduced atypical NMS in the literature. This increases the likelihood of misdiagnosis in patients taking typical antipsychotics, such as haloperidol.6, 10, 11 Given the medical history and clinical presentation of patients with suspected atypical NMS, the differential diagnosis should include atypical NMS, serotonin syndrome, malignant catatonia, and acute dystonia (Table 2). Seratonin syndrome is a life-threatening, adverse drug reaction caused by excessive serotonergic agonists, with the central triad of symptoms being altered mental status (AMS), autonomic hyperactivity, and neuromuscular abnormalities.12 Malignant catatonia is a subtype of catatonia characterized by stupor, mutism, catalepsy, waxy flexibility, negativism, posturing, pyrexia, autonomic dysfunction, rigidity, and elevated creatin kinase (CK) levels.13 Acute dystonia, while an emergency, presents as less life-threatening, extrapyramidal adverse effects induced by typical antipsychotics.14 Differentiating typical NMS from the other three conditions presents diagnostic challenges. For example, Desai and colleagues reported a case that was initially diagnosed as NMS but later confirmed as malignant catatonia, leading to a change in treatment.15 Additionally, patients can develop NMS alongside another condition, complicating diagnosis. Prakash found that NMS and serotonin syndrome can coexist in a single patient, especially when treated with a combination of neuroleptic and serotonergic agents.16 Nonetheless, the initial treatment for all three conditions is the same: immediate discontinuation of the causative agents and supportive care.17, 18
Another challenge associated with treating atypical NMS lies in the realm of pharmacotherapy (Table 3). Benzodiazepines, particularly lorazepam and diazepam, have emerged as an effective treatment option in both typical and atypical NMS. Lorazepam is preferred for its longer intracerebral half-life, higher potency (2-2.5 milligrams [mg] lorazepam equivalent to 10 mg diazepam) and lesser frequency of venous thrombosis.19 It exerts its effects by enhancing GABAergic (gamma-aminobutyric
acid) transmission, which reduces muscle rigidity and prevents further neuromuscular complications. Intramuscular or intravenous lorazepam are first-line treatments for muscle rigidity and sympathetic overactivity, including agitation and hyperthermia.20 Prior literature has demonstrated that all patients who received lorazepam within 24 hours of typical NMS onset or hospital admission experienced resolution of rigidity and fever within 24-48 hours, while other symptoms subsided within 64 hours. This contrasts with recovery periods of 5-10 days in patients who received supportive care alone.21 Recent literature supports the use of lorazepam as an effective treatment for atypical NMS as well.22, 23
In this article we aimed to evaluate the importance of recognizing atypical NMS in emergency settings and lorazepam’s role as a frontline treatment by analyzing published reports of NMS. Identifying atypical cases within the broader pool of NMS reports helps explore the nuances of recognizing atypical NMS and compare clinical responses to lorazepam between typical and atypical presentations. This approach both highlights the diagnostic challenges of atypical NMS in emergency settings and contributes to understanding lorazepam’s efficacy across the clinical spectrum of NMS.
METHODS
We performed a systematic literature search in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol. PubMed was queried for studies published between 1988–December 6, 2024, using the key terms “Neuroleptic Malignant Syndrome” and “Lorazepam.” To enhance the yield of relevant studies, we also performed a citation-based extension search by reviewing reference lists and citations of included articles.
Eligibility Criteria
Given the rarity of NMS and the predominance of case reports in the available literature, studies were included if they met the following inclusion criteria:
Table 2. Differential diagnoses of atypical neuroleptic malignant syndrome,
Differential diagnosis
Atypical NMS
Serotonin syndrome
Malignant catatonia
Acute dystonia
Key clinical presentations
• Muscle rigidity
• AMS
• Hyperreflexia
• Clonus
• AMS
• Catatonic behavior
• Waxy flexibility
• Autonomic instability
• Involuntary muscle contractions.
• Mental status preserved.
Diagnostic criteria
• Clinical presentations
• History of antipsychotic use
• Clinical presentations
• History of serotonergic agent use
• Clinical presentations
• EEG findings
• Clinical presentations
Treatments
• Discontinuation of antipsychotic use
• Supportive care
• Lorazepam
• Dantrolene
• Discontinuation of antipsychotic use
• Supportive care
• Lorazepam
• Cyproheptadine
• Lorazepam
• ECT
• Benztropine
• Diphenhydramine
NMS, neuroleptic malignant syndrome; AMS, altered mental status; EEG, electroencephalogram; ECT, electroconvulsive therapy.
Table 3. Pharmacologic treatment options for neuroleptic malignant syndrome.
Benzodiazepines:
• Lorazepam
• Diazepam
Mechanism
Enhanced GABAergic transmission
Bromocriptine Dopamine agonist
Amantadine Dopamine and anticholinergic effects
Recommended dose
• Lorazepam: 1-2 mg IM or IV every 4-6 hours.
• Diazepam: 10mg IV every 8 hours.
2.5 mg every 6-8 hours and titrated up to a maximum dose of 40 mg/day.
100-200 mg initially and is titrated upward as needed to a maximum dose of 200 mg every 12 hours.
GABA, gamma-aminobutyric acid; mg, milligram; IM, intramuscular; IV, intravenous.
1. Case reports or case series with a final diagnosis of NMS
2. Use of lorazepam as a primary treatment for NMS
3. Clear documentation of clinical outcomes following lorazepam administration
4. Papers published in English with accessible abstracts and full texts.
Studies were excluded based on the following exclusion criteria:
1. Papers not written in English
2. Papers lacking access to abstracts or full texts
3. NMS not being the final diagnosis
4. Treatment involved other medications either in place of or in combined with lorazepam.
We identified atypical NMS cases among eligible reports and analyzed them separately. The primary outcomes assessed included the number of patients and their clinical responses to lorazepam treatment.
Risk-of-bias Assessment
Therapeutic effects
• Treat agitation
• Muscle relaxation
• Reduce seizure risk
• Muscle relaxation
• Treat hyperthermia
• Improve mental status
• Muscle relaxation
• Alleviate tremors
• Improve mental status
We used the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Case Reports to assess the risk of bias in the included case reports and case series (https://jbi.global/criticalappraisal-tools). Only studies that fulfilled all eight criteria on the checklist were deemed eligible for final analysis.
RESULTS
Study Selection
The PubMed search identified 100 articles, with an additional 23 identified from citation searches. We inititally excluded 20 papers for the following reasons: five due to duplication; and 15 papers (14 in PubMed and one in citation search) not written in English or lacking an abstract or access to full text. An additional 77 studies were excluded (61 in PubMed and 16 in citation search for NMS-irrelevant diagnoses) because lorazepam had not been administered or more than lorazepam had been administered (Figure 1). Screening with the JBI checklist resulted in a total of 11
Figure 1. PRISMA flow chart outlining inclusion and exclusion criteria for articles that referenced use of lorazepam. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; NMS, neuroleptic malignant syndrome.
articles, five from the PubMed and six from citation search, comprising a total of 15 cases.
Patient Characteristics and Treatment Outcomes
Among the 11 articles reviewed, we identified a total of 15 cases (10 males and 5 females 17-83 years of age). Our cohort consisted of six atypical and nine typical NMS cases, in which lorazepam administration showed a significant improvement in 12 of 15 cases (Table 4). Among atypical NMS cases, 5 of 6 patients demonstrated a favorable response to lorazepam: two
Table 4. PRISMA search resulting in findings of 12/15 patients experiencing improvement with lorazepam administration.
Search results Patient demographics Diagnosis
Allonce J et al 202424
Verma K et al 201825
Hernandez SD et al 202126
Mayur Pandya, et al. 200427
43-year-old male Atypical NMS
69-year-old male Atypical NMS
44-year-old male Atypical NMS
28-year-old female
67-year-old female
83-year-old male Atypical NMS Atypical NMS Atypical NMS
Esang M et al 201928
Velosa A et al 201929
Yacoub A, et al 200630
59-year-old male Typical NMS
44-year-old female Typical NMS
66-year-old male
Rosebush P et al 200831
Ghio L et al 200932
Reilly T et al 201733
Foguet-Boreu Q et al 201834
62-year-old male
43-year-old male Typical NMS Typical NMS Typical NMS
17-year-old male Typical NMS
45-year-old female Typical NMS
49-year-old male Typical NMS
67-year-old female Typical NMS
Presenting complaint and diagnostic consideration Lorazepam use and outcome
Presented with AMS and afebrile. Atypical NMS was diagnosed.
Presented with AMS and afebrile, agitation, catatonia. Atypical NMS was diagnosed.
Presented with AMS and afebrile. Alcoholic encephalopathy secondary to alcohol intoxication was made as initial diagnosis.
Presented with AMS and afebrile. Atypical NMS was diagnosed.
Presented with AMS, afebrile and catatonia. Atypical NMS was diagnosed.
Presented with AMS and afebrile with normal CK. Atypical NMS was diagnosed.
Typical NMS presentation in the ED; diagnosis made based on standard symptom constellation.
Typical NMS presentation; diagnosis made based on standard symptom constellation.
Lorazepam improved muscle rigidity and recovery in 48 hours.
Lorazepam seems to have improved AMS prior to admission but did not improve catatonia.
Lorazepam resolved agitation.
Lorazepam improved AMS and tremors within 72 hours.
Lorazepam improved AMS within 72 hours.
Lorazepam improved muscle rigidity, gait, and AMS in 48 hours.
Lorazepam led to symptom resolution; stable at discharge.
Lorazepam produced no significant improvement. ECT needed
Lorazepam improved muscle rigidity and fever within 48 hours. All other NMS manifestations resolved in 9 days
Typical NMS presentation; diagnosis made based on standard symptom constellation.
Typical NMS presentation; diagnosis made based on standard symptom constellation.
Typical NMS presentation; diagnosis made based on standard symptom constellation.
Typical NMS presentation in the ED; diagnosis made based on standard symptom constellation.
Typical NMS presentation; diagnosis made based on standard symptom constellation.
Lorazepam improved muscle rigidity and fever within 72 hours. All other features resolved in 5 days.
Lorazepam improved muscle rigidity and fever within 72 hours. All other features resolved in 9 days.
Lorazepam resulted in substantial recovery by day 6 and full recovery by day 14.
Lorazepam progressively improved muscle rigidity.
Lorazepam gradually improved muscle rigidity and communication.
A trial with lorazepam was not successful. AMS continued. ECT and bromocriptine started for catatonia.
NMS, neuroleptic malignant syndrome; AMS, altered mental status; CK, creatine kinase; ED, emergency department; ECT, electroconvulsive therapy.
Lorazepam in Managing ANMS: A Systematic Review of Case Reports
improved significantly within 24 hours; two within 72 hours; and one case that lacked a specified recovery timeline. In the remaining case, lorazepam appeared to initially improve mental status but failed to resolve catatonia, which ultimately required electroconvulsive therapy (ECT). On the other hand, among typical NMS cases, 7 of 9 patients showed clinical improvement following lorazepam therapy. Only two patients were reported to have presented to the ED, and they both exhibited progressive improvement post-administration, consistent with the other five inpatient cases. Of the seven who responded favorably to treatment with lorazepam, three demonstrated significant improvement within 72 hours, two recovered over an extended course, and two lacked documented timelines.
DISCUSSION
The rarity of typical NMS, combined with the lack of clinical trials, makes treatment challenging, as most drug recommendations are based on pharmacokinetic theories and clinical observations.35 Given that atypical NMS is even rarer, its treatment is likely to be even more difficult. A step-by-step treatment approach has been proposed based on the severity of NMS, addressing both typical and atypical cases (Table 5). The Woodbury stage approach suggests that lorazepam may serve as a first-line pharmacologic intervention in stages II, III or IV, where patients present with mild or moderate symptoms. The Woodbury approach also suggests other commonly used medications, such as bromocriptine, dantrolene, and amantadine in advanced stages.36 However, it is important to note that the effectiveness of these drugs varies in different cases, and none
Woodbury Stage
Clinical presentation
Stage I
Drug-induced Parkinsonism
• Rigidity
• Tremor
Stage II
Drug-induced Catatonia
• Rigidity Mutism
• Stupor
Supportive care
• Reduce or switch antipsychotics
• Discontinue, reduce, or switch antipsychotic
have yet received approval from the US Food and Drug Administration.Our literature review reinforces these findings, with 12 of 15 patients with NMS demonstrating significant clinical improvement following lorazepam administration. When comparing outcomes between atypical and typical NMS cases, 5 of 6 atypical cases (83%) and 7 of 9 typical cases (78%) responded favorably to lorazepam. Notably, 4 of 6 atypical cases (67%) and 3 of 9 typical cases (33%) exhibited significant clinical improvement within 72 hours of lorazepam initiation. These results suggest that lorazepam may expedite hospital course by facilitating meaningful symptom resolution within 72 hours in most atypical NMS cases and approximately one-third of typical cases.
All six atypical NMS cases initially presented to the ED with AMS in the absence of fever. Only one case received timely intervention in the ED, which included discontinuation of antipsychotics, supportive care, and administration of lorazepam. It was also the only instance in which lorazepam alone proved insufficient. Although the patient’s AMS improved following initial lorazepam administration in the ED, persistent catatonia ultimately necessitated treatment with ECT during admission. Of note, this patient had previously responded favorably to parenteral lorazepam during an earlier episode of prodromal NMS in the ED, underscoring lorazepam’s potential role in addressing early neuroleptic toxicity—even if incomplete in complex or refractory presentations.
In contrast, the other five atypical NMS patients, although diagnosed later during hospitalization, demonstrated substantial clinical improvement following lorazepam
Stage III Mild, early NMS
• Mild rigidity
• Catatonia or confusion
• Temperature ≤ 38°C (100.4°F)
• Heart rate ≤100 bpm
• Discontinue antipsychotics
• Carefully monitor for progression
• Correct risk factors
Stage IV Moderate NMS
• Moderate rigidity
• Catatonia or confusion
• Temperature 3840°C (100.4-104°F)
• Heart rate 100-120 bpm
• Discontinue antipsychotics
• Manage fluids
• Initiate cooling
• Correct risk factors
• Provide intensive care
Stage V Severe NMS
• Severe rigidity
• Catatonia or coma
• Temperature ≥ 40°C (104°F)
• Heart rate ≥ 120 bpm
• Discontinue antipsychotics
• Manage fluids
• Initiate cooling
• Correct risk factors
• Provide intensive care
First- line intervention
Second- line intervention
• Anticholinergic agents
• Lorazepam
• Lorazepam
• Lorazepam, bromocriptine, or amantadine
• Consider ECT
• Dantrolene, bromocriptine, or amantadine
• Consider ECT
NMS, neuroleptic malignant syndrome; bpm, beats per minute; °C, degrees Celsius; °F, Farenheit; bpm, beats per minute; ECT, electroconvulsive therapy
Table 5. Woodbury stages for clinical presentation and treatment of neuroleptic malignant syndrome.
initiation, typically within 72 hours. This delay highlights the diagnostic challenges of atypical NMS in emergency settings, where its subtle and non-classic presentation may hinder early recognition, and suggests that prompt administration of lorazepam may offer a valuable therapeutic strategy for reversing key symptoms and improving patient outcomes.
LIMITATIONS
Given the rarity of NMS, our review is primarily based on case reports and case series, which inherently have certain limitations. These include a lack of generalizability, potential overestimation of lorazepam’s efficacy, selection bias, limited statistical power, and the influence of confounding variables such as patients’ comorbidities. Additionally, most reports lacked precise timelines, limiting our ability to assess the onset of lorazepam’s effect at the ED level. While some cases suggested early improvement, this could not be quantified. Future clinical trials are needed to validate lorazepam’s efficacy in both atypical and typical NMS.
CONCLUSION
Early recognition and prompt intervention for atypical neuroleptic malignant syndrome remain critical challenges in emergency medicine due to its subtle and varied clinical presentations. Our systematic review underscores lorazepam’s effectiveness as a first-line pharmacologic intervention, demonstrating significant symptomatic improvement within 72 hours in most atypical NMS cases (4 of 6), including two within 24 hours. This result is comparable or superior to outcomes observed in typical presentations (3 of 9). Notably, one of the two atypical NMS cases that did not fully respond to lorazepam received early administration of lorazepam in the ED and substantially improved the degree of AMS prior to admission, which reinforced the potential benefits of timely therapy. Future controlled studies are essential to refine diagnostic criteria and treatment protocols for this potentially lethal condition.
REFERENCES
1. Tse L, Barr AM, Scarapicchia V, et al. Neuroleptic malignant syndrome: a review from a clinically oriented perspective. Curr Neuropharmacol 2015;13(3):395-406.
2. Szota AM, Radajewska I, Araszkiewicz AS. Atypical neuroleptic malignant syndrome: case reports and diagnostic challenges. J Psychoactive Drugs. 2022;54(3):284-93.
3. Grinchii D, Dremencov E. Mechanism of action of atypical antipsychotic drugs in mood disorders. Int J Mol Sci. 2020;21(24).
4. Velamoor VR, Norman RM, Caroff SN, et al. Progression of symptoms in neuroleptic malignant syndrome. J Nerv Ment Dis 1994;182(3):168-73.
5. Ware MR, Feller DB, Hall KL. Neuroleptic malignant syndrome: diagnosis and management. Prim Care Companion CNS Disord 2018;20(1).
6. Collins A, Davies D, Menon S. Atypical neuroleptic malignant syndrome. BMJ Case Rep. 2016:bcr2016214901.
7. Sarkar S, Gupta N. Drug information update. Atypical antipsychotics and neuroleptic malignant syndrome: nuances and pragmatics of the association. BJPsych Bull. 2017;41(4):211-6.
8. Picard LS, Lindsay S, Strawn JR, et al. Atypical neuroleptic malignant syndrome: diagnostic controversies and considerations. Pharmacotherapy. 2008;28(4):530-5.
9. Zaidi S, Irfan N, Khalid Z. Neuroleptic malignant syndrome with normal creatine phosphokinase levels: an atypical presentation. J Coll Physicians Surg Pak. 2022;32(4):S47-8.
10. Zabel M, Kandukuri R. Atypical neuroleptic malignant syndrome in an incarcerated patient: a demographic who may be at increased risk. BMJ Case Rep. 2024;17(2).
11. Mogollon Diaz JP, Lizcano Toloza LY, Serrano Garcia AY, et al. Neuroleptic malignant syndrome associated with atypical antipsychotics: a case report. Rev Colomb Psiquiatr (Engl Ed) 2023;52(1):78-81.
12. Maitland S, Baker M. Serotonin syndrome. Drug Ther Bull 2022;60(6):88-91.
13. Oruch R, Pryme IF, Engelsen BA, et al. Neuroleptic malignant syndrome: an easily overlooked neurologic emergency. Neuropsychiatr Dis Treat. 2017;13:161-75.
Address for Correspondence: Aaron Chen, MD, Maimonides Medical Center, Emergency Medicine Department, 965 48th St, Brooklyn, NY 11219. Email: aachen@maimo.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Chen et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
14. Sridaran R, Nesbit CE. Acute dystonia versus neuroleptic malignant syndrome without fever in an eight-year-old child. Pediatr Emerg Care 2017;33(1):38-40.
15. Desai S, Hirachan T, Toma A, et al. Malignant catatonia versus neuroleptic malignant syndrome. Cureus. 2021;13(6):e15818.
16. Prakash S. A diagnostic confusion between serotonin syndrome and neuroleptic malignant syndrome. Am J Emerg Med. 2021;43:272-3.
17. Perry PJ, Wilborn CA. Serotonin syndrome vs neuroleptic malignant syndrome: a contrast of causes, diagnoses, and management. Ann Clin Psychiatry. 2012;24(2):155-62.
18. Apetauerova D, Patel PA, Burns JD, et al. Movement disorder emergencies. Neurol Clin. 2021;39(2):615-30.
19. Dundee JW, McGowan WA, Lilburn JK. Comparison of the actions of diazepam and lorazepam. Br J Anaesth. 1979 May;51(5):439-46.
20. Tan CM, Kumachev A. Neuroleptic malignant syndrome. CMAJ. 2023 Nov 6;195(43):E1481.
21. Francis A, Chandragiri S, Rizvi S, et al. Is Lorazepam a treatment for neuroleptic malignant syndrome? CNS Spectr. 2000;5(7):54-7.
22. Hor ESL, Singh GP, Omar NA, et al. Atypical neuroleptic malignant syndrome and non-alcoholic Wernicke’s encephalopathy. BMJ Case Rep. 2021;14(8).
23. Vellekkatt F, Kuppili PP, Bharadwaj B, et al. Atypical neuroleptic malignant syndrome - A case report. Asian J Psychiatr. 2019;43:7-8.
24. Allonce J, Khan S, Pulford B. Atypical presentation of ziprasidoneinduced neuroleptic malignant syndrome: a case report. J Investig Med High Impact Case Rep. 2024;12:23247096241262690.
25. Verma K, Jayadeva V, Serrano R, et al. Diagnostic, treatment, and system challenges in the management of recurrent neuroleptic malignant syndrome on a general medical service. Case Rep Psychiatry. 2018;2018:4016087.
26. Hernandez SD, Marotta DA, Goteti R. Atypical neuroleptic malignant syndrome in the setting of quetiapine overdose: a case report and review of the literature. Cureus. 2021;13(1):e12602.
27. Pandya M, Pozuelo L. A malignant neuroleptic spectrum: review of diagnostic criteria and treatment implications in three case reports. Int J Psychiatry Med. 2004;34(3):277-85.
28. Esang M, Goldstein S, Dhami R. The role of physical examinations in psychiatry as illustrated in a case of neuroleptic malignant syndrome versus viral encephalitis: a case report and literature review. Cureus 2019;11(6):e4840.
29. Velosa A, Neves A, Barahona-Correa JB, et al. Neuroleptic malignant syndrome: a concealed diagnosis with multitreatment approach. BMJ Case Rep. 2019;12(6).
30. Yacoub A, Francis A. Neuroleptic malignant syndrome induced by atypical neuroleptics and responsive to lorazepam. Neuropsychiatr Dis Treat. 2006;2(2):235-40.
31. Rosebush PI, Anglin RE, Richards C, et al. Neuroleptic malignant syndrome and the acute phase response. J Clin Psychopharmacol 2008;28(4):459-61.
32. Ghio L, Fornaro G, Rossi P. Risperidone-induced hyperamylasemia, hyperlipasemia, and neuroleptic malignant syndrome: a case report. J Clin Psychopharmacol. 2009;29(4):391-2.
33. Reilly TJ, Cross S, Taylor DM, et al. Neuroleptic malignant syndrome following catatonia: Vigilance is the price of antipsychotic prescription. SAGE Open Med Case Rep. 2017;5:2050313X17695999.
34. Foguet-Boreu Q, Coll-Negre M, Serra-Millas M, et al. Neuroleptic malignant syndrome: a case responding to electroconvulsive therapy plus bupropion. Clin Pract. 2018;8(1):1044.
35. Reulbach U, Dutsch C, Biermann T, et al. Managing an effective treatment for neuroleptic malignant syndrome. Crit Care 2007;11(1):R4.
36. Woodbury MM, Woodbury MA. Neuroleptic-induced catatonia as a stage in the progression toward neuroleptic malignant syndrome. J Am Acad Child Adolesc Psychiatry. 1992;31(6):1161-4.
37. Strawn JR, Keck PE, Jr., Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007;164(6):870-6.
Alcohol Intoxication in the Academic Emergency Department: Epidemiology and Facility-Fee Financial Impact
Eric Legome, MD*
William Bonadio, MD*
Michael Redlener, MD*†
Elyse Lavine, MD*
Avah Mealy, MPA*
Samuel E. Sondheim, MD, MBA*†
Icahn School of Medicine at Mount Sinai, Department of Emergency Medicine, New York City, New York
Icahn School of Medicine at Mount Sinai, Center for Healthcare Readiness, New York City, New York
Section Editor: León D. Sánchez, MD, MPH
Submission history: Submitted February 25, 2025; Revision received June 20, 2025; Accepted June 20, 2025
Electronically published October 3, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.43575
Introduction: Alcohol intoxication is a common patient presentation to urban emergency departments (ED). There is limited data on the healthcare financial impact of caring for alcoholintoxicated patients in the ED. In this study we examined the facility-based financial billings and collections related to ED visits for alcohol intoxication.
Methods: Using a retrospective cohort analysis of two large, urban EDs, with a combined yearly census of approximately 150,000 patient visits, we included all encounters between June 2018–December 2021 with a discharge diagnosis consistent with acute alcohol intoxication. We reviewed records of patient encounters with a final diagnosis consistent with acute alcohol intoxication who only had minimal or no interventions performed, implying the visit was solely consistent with acute alcohol intoxication. We reviewed the facility charges of these patients, along with insurance status and average payment by status to understand the financial impact.
Results: Of 495,436 patient presentations to the EDs during the study period, 13,454 met study criteria (2.7% of total patients). Patient length of stay in the ED had an average of 254 minutes and median of 240 minutes. In total, this cohort of patients occupied ED beds for 56,505 hours cumulatively, or an average of 43.2 bed hours per day for alcohol intoxication-related visits, representing 3.14% of all ED bed hours across both sites. The majority of patient encounters were billed as a level 3 facility code (76%). Facility charges for the cohort totaled $22,590,000. The estimated reimbursement based on the percentage reimbursed by payor mix was $1.7 million (7.5%), or an average of $126 per patient visit— less than one quarter of the general average visit collection.
Conclusion: Patients with acute alcohol intoxication and no other complaints are a minority of ED patients, yet their care results in substantial charges and ED resources. Based on the known facility collection rates per insurer, the weighted prevalence of insurers among this cohort yields an estimated collection rate of 7.5%. Opportunities to provide proven alcohol-related interventions should consider the unreimbursed costs of these visits when determining cost effectiveness. [West J Emerg Med. 2025;26(5)1454–1458.]
INTRODUCTION
Acute alcohol intoxication is a common patient presentation to urban emergency departments (ED). Given space and staffing constraints to safely monitor these patients, particularly those at high fall risk, these encounters can be expensive and resource intensive.1 Additional related challenges in the ED include increased crowding, longer length of stay (LOS), and abusive behavior toward staff and other patients.2-6 Alcohol use disorder in the US has a significant financial impact on the healthcare system at large, with estimated costs of $24.6
billion in 2006, of which only 10.3% were paid for by alcohol users and their families.7 Similar estimates from 2010 placed healthcare costs at $28.4 billion.8 From 2006 to 2014, the rate of acute alcohol-related ED visits increased 40% from 720.9 to 1,009.6 per 100,000 population 9
Undoubtedly, a large portion of the overall healthcare costs for these visits is attributable to emergency care, as it is the main safety net for receiving patients while acutely intoxicated or with complications related to alcohol consumption. Yet there is little ED-specific literature describing the facility-based financial charges, insurance status, and financial implications of alcohol-intoxicated patients in the ED. In this paper we provide specific financial estimates about patients who present to the ED with acute alcohol intoxication but do not require evaluation otherwise.
METHODS
In this retrospective cohort analysis of two large, academic, urban EDs within the same health system, with a combined yearly census of approximately 150,000 patient visits, we included all patient encounters between June 2018–December 2021 with a discharge diagnosis consistent with acute alcohol intoxication via a query through the electronic health record. We used International Classification of Diseases, 10th Rev. (ICD 10) F10.1-9 codes encompassing alcohol use and dependence (Table 1). As there is not a definitive code that every physician uses at discharge, we included those generally used for the acutely intoxicated patient. We excluded patients with ICD-10 codes that included other potential concomitant issues that may have required separate treatment, such as withdrawal, delirium, or another dysfunction. Patients were also excluded if they were admitted, had any additional lab testing on the same visit (excluding COVID-19 or blood glucose testing) or imaging studies, or had any treatment beyond an immunization administration (TDAP or influenza) strongly suggesting they had presentations or complaints for etiologies other than purely alcohol-related or that it was arrived at as a diagnosis after testing or interventions. We excluded mixed intoxications, although as diagnoses were generally made by patient or history/presentation to emergency medical services, this likely underestimated co-ingestions. In most cases, the diagnosis of acute alcohol intoxication was a clinical diagnosis.
The current practice at these facilities does not include routine testing for alcohol level or toxicological screening without clinical indications. This is a common practice in emergency medicine. In general, if the history is consistent with findings (eg, patient admits to alcohol consumption, odor of alcohol, and clinical picture, etc), and the patient clinically improves over time, alcohol testing is not required. If the patient fails to improve, or if there is evidence of head trauma or concern for altered mental status that is not sufficiently explained by alcohol, further testing is often required.10 Due to the retrospective nature of this study and the change in professional billing groups during the study time frame, we
Population Health Research Capsule
What do we already know about this issue?
Alcohol intoxication-related visits pose significant challenges to EDs. They require significant resources to ensure patient and staff safety and often face significant costs.
What was the research question?
How can we quantify the costs and reimbursements associated with alcoholrelated ED visits?
What was the major finding of the study?
Alcohol-related ED visits comprised over 3% of all ED bed hours, with the estimated reimbursement less than one quarter of the general average visit collection.
How does this improve population health?
The heavy resource use of alcohol-related visits to the ED often yields minimal financial collections.
were unable to obtain data on professional charges. Therefore, the financial charges are related solely to ED facility fees. As a proxy to quantify the clinical impact, we reviewed LOS for this cohort of patients as well. Charts were abstracted per prior standards, including case selection criteria and variable definitions.11This research was approved by the institutional review board.
RESULTS
Of 495,436 patient presentations to the two EDs during
Table 1. International Classification of Diseases codes and respective descriptors used for inclusion.
ICD 10
Code
F10.10
F10.120
Primary
Alcohol abuse, uncomplicated
Alcohol abuse with intoxication, uncomplicated
F10129 Alcohol abuse with intoxication, unspecified
F10.20 Alcohol dependence, uncomplicated
F10.220
F10.229
F10.920
F10.929
Alcohol dependence with intoxication, uncomplicated
Alcohol dependence with intoxication, unspecified
Alcohol use, unspecified with intoxication, uncomplicated
Alcohol use, unspecified with intoxication, unspecified
ICD-10, International Classification of Diseases, 10th Rev; dx, diagnosis.
the study period, 16,526 (3%) visits met criteria of a diagnosis of acute alcohol intoxication. Of these, 10,800 were unique medical record numbers with ED visits per patient ranging from 1-130 visits over that period, indicating these 10,800 unique medical record numbers yielded the 16,526 visits. A total of 13,454 ED cases met criteria of no billed testing or treatment other than blood glucose measurement, immunization, or COVID-19 testing (2.7% of total patients, 81% of patients with an alcohol-related diagnosis). Most patients with a final diagnosis included were billed as a level 3 facility code (76%), although the level was likely influenced by charting variability. Most were self-pay (69%) or Medicaid (20%), tailed by commercial insurance (8%) and Medicare (3%). Of these patients, 76% were male and 24% were female.
The total facility-fee billing was $22,590,000. Specific encounter collections were not available for analysis; therefore, estimates of collections were based on the hospitals’ collection rates for all visits broken down by the payors. That is, if payor x collection rate was 30%, the contribution to the overall collections was 30% of the amount payor x was billed. Using this methodology, the estimated reimbursement based on the percentage reimbursed by payor mix was about $1.7 million (7.5% collection rate). This represents an average collection of $126 per patient encounter, less than one quarter of the average visit collection at these sites. Patients’ LOS in the ED had an average of 254 minutes and median of 240 minutes. In total, this cohort of patients occupied ED beds for 56,505 hours
cumulatively, or an average of 43.2 bed hours per day for alcohol intoxication-related visits. This represented 3.14% of total bed hours used across both sites during the study period.
DISCUSSION
Alcohol intoxication is a common ED diagnosis. However, specific data on healthcare costs, charges, and uncompensated care of alcohol intoxication alone is lacking. We sought to identify and analyze a cohort of ED patients solely presenting with acute alcohol intoxication. We found this select group accounted for approximately 3% of the ED census. Patients with alcohol intoxication have been shown to be repeat users of ED services. In one study, many have been shown to present for over 100 annual visits for alcohol intoxication.14 Our range included up to 130 visits for a unique medical record number within the study period. Also consistent with our findings, lack of significant or complex intervention is not unusual.
Previous literature has demonstrated that the admission rate for patients with a diagnosis of alcohol intoxication is often less than 3%, far below national average hospital admission rates from the ED.12 Emergency medical services has likewise identified significant impact from alcohol-related calls, with over 30% of calls in one urban area as a result of alcohol consumption.13 Our dataset identified close to one third with multiple visits, ranging as high as 130 visits per year in one patient. This likely underestimates the actual revisits as some may have been registered under several different registration numbers due to difficulty in obtaining correct demographic information due to intoxication.
One commonality characterizing alcohol-related visits is that they generally impose a costly public health burden on EDs. One study from Australia found higher overall costs for alcohol-positive patients compared to those with negative alcohol levels, and a high weekly cost of over $144,000; while the cost included all alcohol-positive patients it was still felt to be an underestimation per the authors.14 Estimates of US data found ED costs related to acute alcohol consumption to be nine billion dollars per year, although the final diagnoses were more inclusive and likely included significant evaluations for other concerns or effects of alcohol.9 A prior cohort study from San Diego found a collection rate of 15.4% of ED visits related to alcohol use in a specific but far smaller cohort of 409 patients arrested for public intoxication.15 This aligns with our findings of a very limited collection rate of 7.5% in our cohort. Clinically, the cumulative 56,505 hours of ED time is substantial. These 56,505 hours occupied ED beds with the need for safety observation given the higher risk of falls among intoxicated patients, pulling staff from completing other tasks in the ED.
Not specifically addressed in this paper are the benefits and resources required to provide both alcohol reductions and cessations services as well as counseling to patients with alcohol intoxication in the ED. Strategies that are often
Figure 1. Flow diagram for cases included. ED, emergency department; ICD, International Classification of Diseases.
employed, such as SBIRT (Screening, Brief Intervention and Referral to Treatment) or other screenings, were not captured in the facility charges. Given the significant cost of care and poor collection rate, alternative strategies to address and treat alcohol intoxication are warranted. As demonstrated here, 81% of those visiting the ED solely for alcohol intoxication did not require further significant medical care.
One option, sobering centers, may represent an opportunity to decrease ED use and associated costs, when used within a specific EMS protocol.1 A 2017 study found costs per visit of $264.18 at a sobering center compared to an average ED cost per visit of $648.72.16 These centers have also demonstrated increased connectivity to further care and rehabilitation, which have further decreased downstream costs as well.1,16 Emergency medical services has demonstrated the ability to appropriately identify intoxicated individuals without other illnesses and transport them to sobering centers rather than to EDs. This highlights the capability and skillset of emergency medical technicians and paramedics—along with an evidence-based protocol or checklist criteria—to differentiate those patients who can safely consider alternative destinations outside the traditional ED.17-18
Visits to the ED may represent a unique opportunity to offer preventative care and treatment for this vulnerable population. Prior initiatives have included increased offerings of detoxification and rehabilitation programs, medication treatments, and psychosocial support from interdisciplinary teams.19-20 Yet these have also been found to be successful in sobering centers.1 Given the high costs, inconsistent uptake, resource needs, and variable success of these programs in EDs, alternative destinations may prove superior for the right cohort.
LIMITATIONS
It must be noted that this review included only facility fees. Due to current limitations of available data, professional fees were not reviewed. Future analysis is warranted to compare these collection rates against professional fees for this demographic. Unfortunately, individual patient-level collections were not available retrospectively due to a billing-related software change since the study period. As the encounter-level collections were not available for review, the $1.7 million in collections was estimated by the known collection rates specific to each of the respective insurances and weighted based on the respective prevalences. The collection rates may differ slightly for this specific demographic, but we believe they would likely be lower or equal to the general collection rates. Lastly, this cohort was identified by excluding encounters with mixed intoxications or co-ingestions. Further analysis of this stratification and/or review of a similar demographic presenting for drug use may be warranted given the similar patterns of resource utilization.
CONCLUSION
Patients presenting with acute alcohol intoxication and
Uncomplicated
no other complaints comprise a relatively small minority of ED visits, yet they result in substantial charges and ED resources. Of all ED visits, 2.7% were attributed to this cohort, and they occupied 3.14% of all ED bed hours. Based on the known facility collection rates per insurer, the weighted prevalence of insurers among this cohort yields an estimated overall facility collection rate of 7.5%. In general, self-pay, the source of most patients, is collected at a rate and amount markedly below all other payors. Opportunities to provide proven alcohol-related interventions should consider the unreimbursed costs of ED patients with intoxication when considering cost effectiveness.
Address for Correspondence: Samuel E Sondheim, MD, MBA. Icahn School of Medicine at Mount Sinai, Department of Emergency Medicine, 1111 Amsterdam Avenue, ED Administration Suite - 1st Floor, New York, NY 10025. Email: samuel.sondheim@ mountsinai.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Legome et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Marshall B, McGlynn E, King A. Sobering centers, emergency medical services, and emergency departments: a review of the literature. Am J Emerg Med. 2021;40:37-40.
2. Klein LR, Driver BE, Miner JR, et al. Emergency department length of stay for ethanol intoxication encounters. Am J Emerg Med 2018;36(7):1209-14.
3. McKenna P, Heslin SM, Viccellio P, et al. Emergency department and hospital crowding: causes, consequences, and cures. Clin Exp Emerg Med. 2019;6(3):189-95.
4. Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1-10.
5. Imlach Gunasekara F, Butler S, Cech T, et al. How do intoxicated patients impact staff in the emergency department? An exploratory study. N Z Med J. 2011;124(1336):14-23
6. Vardy J, Mansbridge C, Ireland A. Are emergency department staffs’ perceptions about the inappropriate use of ambulances, alcohol intoxication, verbal abuse and violence accurate? Emerg Med J 2009;26(3):164-8.
7. Bouchery EE, Harwood HJ, Sacks JJ, et al. Economic costs of
excessive alcohol consumption in the U.S. Am J Prev Med 2011;41(5):516-24.
8. Sacks JJ, Gonzales KR, Bouchery EE, et al. 2010 National and state costs of excessive alcohol consumption. Am J Prev Med 2015;49(5):e73-9.
9. White AM, Slater ME, Ng G, et al. Trends in alcohol-related emergency department visits in the United States: results from the Nationwide Emergency Department Sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352-9.
10. Walls R, Hockberger R, Gausche-Hill M, et al. Alcohol-related disease. In: Walls RM, Hockberger RS, Gausche-Hill M, et al (Eds.), Rosen’s Emergency Medicine: Concepts and Clinical Practice (1846-60). Philadelphia, PA: Elsevier, 2022.
11. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
12. Klein LR, Martel ML, Driver BE, et al. Emergency department frequent users for acute alcohol intoxication. West J Emerg Med 2018;19(2):398-402.
13. Joseph D, Vogel JA, Smith CS, et al. Alcohol as a factor in 911 calls in Denver. Prehosp Emerg Care. 2018;22(4):427-35.
14. Lingamanaicker K, Geelhoed E, Fatovich DM, et al. Direct cost of alcohol-related presentations to Royal Perth Hospital emergency department. Emerg Med Australas. 2019;31(6):1045-52.
15. Dunford JV, Castillo EM, Chan TC, et al. Impact of the San Diego serial inebriate program on use of emergency medical resources. Ann Emerg Med. 2006;47(4):328-36.
16. Smith-Bernardin S, Carrico A, Max W, et al. Utilization of a sobering center for acute alcohol intoxication. Acad Emerg Med. 2017;24(9):1060-1071.
17. Ross DW, Schullek JR, Homan MB. EMS triage and transport of intoxicated individuals to a detoxification facility instead of an emergency department. Ann Emerg Med. 2013;61(2):175-84.
18. Cornwall AH, Zaller N, Warren O, et al. A pilot study of emergency medical technicians’ field assessment of intoxicated patients’ need for ED care. Am J Emerg Med. 2012;30(7):1224-8.
19. Corace K, Willows M, Schubert N, et al. Alcohol medical intervention clinic: a rapid access addiction medicine model reduces emergency department visits. J Addict Med. 2020;14(2):163-171.
20. Gaume J, Bertholet N, McCambridge J, et al. Effect of a novel brief motivational intervention for alcohol-intoxicated young adults in the emergency department: a randomized clinical trial. JAMA Netw Open. 2022;5(10):e2237563.
Scoping Review
Unmasking the Hidden Risk of Systemic Toxicity from Topical Salicylates
Neelou Tabatabai, DO*
Swetaleena Dash, MD*†
James A. Chenoweth, MD, MAS*†
Timothy E. Albertson, MD, MPH, PhD*†‡
University of California, Davis, School of Medicine, Department of Emergency Medicine, Sacramento, California
VA Northern California Health Care System, Medicine Department, Mather, California
University of California, Davis, School of Medicine, Department of Internal Medicine, Sacramento, California
Section Editor: Howard Greller, MD
Submission history: Submitted March 3, 2025; Revision received April 30, 2025; Accepted April 30, 2025
Electronically published September 1, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.46538
Introduction: Topical salicylates are commonly found in over-the-counter medications and are applied for pain relief or to treat dermatologic conditions. While generally considered safe, they can cause systemic toxicity under certain conditions. We conducted a systematic review of topical salicylate toxicity. This comprehensive review of previously reported cases highlights the risks, clinical presentations, and management considerations of systemic toxicity from topical salicylates.
Methods: We present a new case of topical salicylate toxicity and conducted a comprehensive systematic literature search from 1952-2024 using PubMed, Google, and Google Scholar. Our search was supplemented by cross-referencing previous studies to identify cases and reviews of topical salicylate toxicity. We then performed a descriptive analysis of the cases, summarizing key information such as clinical presentation, blood levels, and outcomes. Findings were used to contextualize the risks and clinical manifestations of topical salicylate toxicity
Results: A total of 44 cases of topical salicylate toxicity, including our index case, were identified and included in our analysis. Most cases involved patients > 40 years of age, but all age ranges were represented, including neonates. The most frequently reported symptoms included tachypnea (32.5%) and vomiting (25.5%). The new case was an elderly male with further altered mental status from baseline dementia and elevated anion gap.
Conclusion: Both the new case and the literature review emphasize the continued potential systemic risks of topical salicylates among a broad demographic. Given the variable presentations, clinicians should maintain a high index of suspicion for salicylate toxicity in patients with unexplained altered metabolic and/or mental status. Early consideration, recognition, and intervention of topical salicylates-induced toxicity is essential for good outcomes. As many of these products are heavily advertised, patient education on the appropriate use of topical salicylates may be crucial to prevent inadvertent toxicity. [West J Emerg Med. 2025;26(5)1459–1467.]
INTRODUCTION
Derived from willow bark (Salix alba), topical salicylates are used for both pain and dermatologic concerns. They are found in many common over-the-counter (OTC) products including aspirin, bismuth subsalicylate, and oil of wintergreen. When salicylates are applied to the skin, they
work by acidifying the stratum corneum, promoting the desquamation of corneocytes, and reducing intercellular cohesion. This disruption weakens the skin’s barrier properties and facilitates topical absorption. Topical salicylates are available in a variety of formulations, including patches, gels, and creams, with concentrations ranging from 0.5% for
cosmetic purposes to 50% for treating conditions such as warts.1 Many of these OTC products are heavily advertised by famous, former pro athletes without any risk discussion.
Despite their widespread use, topical salicylates can be absorbed enough to cause systemic toxicity particularly when a large dose of high concentration (milligrams per milliliter [mg/mL]) salicylates are applied to large body surface areas (amount applied) or with repeated applications (frequency). Individuals with risk factors such as decreased renal function or compromised skin integrity are at greater risk.2 However, toxicity can also occur in individuals without traditional risk factors highlighting the need for greater public education and clinical awareness about topical salicylate products. The condition of the skin, the concentration of the salicylate product, the vehicle/diluent used in the product, the frequency of application, and the surface area applied are all important variables that determine topical dosing and the potential for toxicity.
A recent case of an elderly male with altered mental status secondary to topical salicylate toxicity emphasizes that this remains a potential source of salicylate toxicity. The patient’s presentation demonstrates the potential for significant systemic absorption even in the absence of well-known risk factors such as damaged skin or significant renal impairment. Additionally, we review previously published case reports of topical salicylate toxicity to emphasize associated risks and the importance of early recognition, intervention, and prevention of misuse particularly in high-risk populations such as pediatric and elderly demographics. The dermal route of salicylates absorption, although rare, remains a clinical problem seen in the emergency department (ED).
CASE REPORT
A 78-year-old male with achalasia type II, advanced dementia, alcoholic cirrhosis complicated by gastric varices, chronic heart failure with preserved ejection fraction, traumatic brain injury, and paroxysmal atrial fibrillation presented to the ED because of altered mental status over the prior three days. His family was concerned that he was less communicative and had a loss of appetite. He denied any symptoms of dizziness, lightheadedness, tinnitus, nausea, or vomiting. His medications included 12.5 mg of trazodone at night and 15 mL of lactulose twice daily. After a review of the chart and interviewing the family, there were no oral medications containing any formulations of salicylate in the household.
Initial vital signs included a blood pressure of 107/64 millimeters of mercury (mm Hg), heart rate of 85 beats per minute, and respiratory rate of 18 breaths per minute with an oxygen saturation of 98% on room air. The oral temperature was recorded as 36.9°C. The skin exam did not reveal any signs of lotions, patches, acute trauma, rashes, or infection. A basic metabolic panel revealed a creatinine of 1.02 mg per deciliter (mg/dL) similar to his prior values. Other initial lab work was notable for an elevated anion gap of 16 (sodium 141
millimoles (mmol) per dL; chloride 103 mmol/dL; carbon dioxide 22 mmol/dL; and potassium 4.0 mmol/dL); and a slightly elevated venous serum pH of 7.45. A comprehensive blood panel included a white blood cell count of 3.8 thousand cells per microliter (cells/μL), hemoglobin of 11.0 grams per dL (g/dL) and platelet count of 140 thousand cells/μL Urinalysis found moderate bacteria, trace leukocyte esterase and trace ketones. An arterial blood gas found a partial pressure of oxygen of 100 mm Hg, 94% saturated, a partial pressure of carbon dioxide of 31 mm Hg, and a pH of 7.54 consistent with a respiratory alkalosis/alkalemia with mild hyperventilation. Imaging results, including a computed tomography of the head without contrast and a chest radiograph, were both unremarkable for any acute findings.
In evaluating the cause of his change in mental status and elevated anion gap, a serum salicylate level was drawn. The serum salicylate level was elevated to 41.4 mg/dL. His ethanol and acetaminophen levels were undetectable. When the family was told about the elevated salicylate level, they remembered that he had applied a three-ounce tube of ICY HOT painrelieving cream (30% methyl salicylate and 10% menthol) to his back (estimated body surface area 18%) within a two-day period, prior to presentation to the ED. It is not known whether he washed his hands after applications. No occlusive dressings were used. The use instructions for the cream are vague and suggest applying a thin layer to the affected area and massage until thoroughly absorbed into the skin no more than 3-4 times a day. Washing hands after application is also suggested. Throughout his stay in the ED, his vital signs remained stable.
A sodium bicarbonate infusion (3 amps of sodium bicarbonate in a liter of dextrose 5% in water after removing 100-150 mL, and infused at 100 mL per hour) with potassium chloride was started in the ED. The patient was admitted to the intensive care unit for close monitoring of symptoms, and frequent repeat serum salicylate levels, blood gases, and electrolyte values. Additional potassium was given to maintain the serum level ≥ 4 mmol/dL Although the patient denied symptoms of a urinary tract infection, given his urinalysis findings and altered mental state, he was empirically treated with antibiotics. The sodium bicarbonate infusion ran ≈ 12 hours and was stopped when the serum salicylate decreased below 30 mg/dL. The anion gap returned to normal. While the family was adamant that the only salicylates to which the patient had access were the topical products, we could not completely rule out additional oral or chronic poisoning. The patient was discharged after two days of hospitalization at his baseline mental status and with the last measured serum salicylate level of 27.0 mg/dL. Figure 1 summarizes the serum salicylate levels in this patient.
METHODS
We performed a systematic and comprehensive review of cases of topical salicylate toxicity. A literature search using
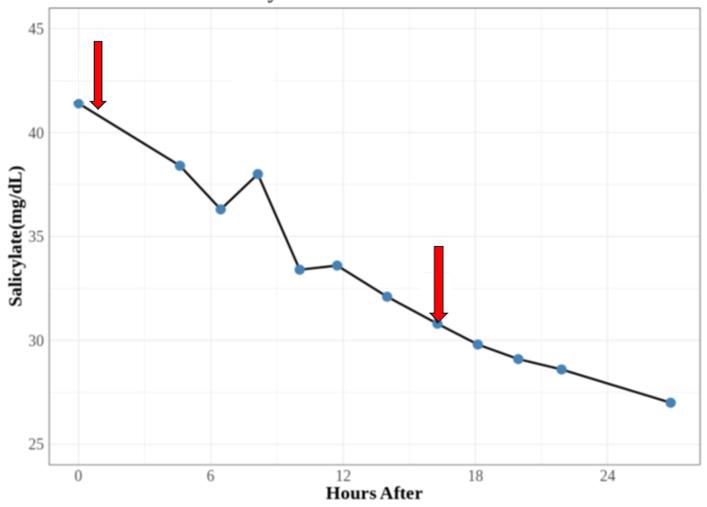
Figure 1. Trend of serum salicylate levels over two days. The arrows reflect the beginning and end of bicarbonate infusion. mg/dL, milligrams per deciliter.
for consistency. Intact skin was defined as having no compromised skin integrity secondary to underlying dermatological conditions.
RESULTS
We found an additional 12 new cases of topical salicylate toxicity from published literature not included in the previous reviews. This expanded the total reported cases to 44, including the current case presented here (Table 1). The first review published in 1996 reviewed 17 cases.3 The 2014 review expanded the number of cases found to 25 but did not include all the cases in the first review.2 Seven were abstracts only.9-15 Of the 43 previously published case reports, eight were published in languages other than English.9-11,16-21
PubMed, Google, and Google Scholar identified relevant publications from 1952–2024. The search strategy employed the following combinations of terms: “topical salicylate toxicity,” “poisoning,” “salicylate,” “methyl salicylate,” and “case reports.” The search resulted in all available publications and specifically targeted peer-reviewed case reports, case series, conference abstracts, reviews, and letters to the editor. It also included texts found in Dutch, English, French, German, Italian, Polish, and Turkish. We used two previous literature reviews on topical salicylate toxicity published prior to our study to ensure all the papers were included. The first, by Brubacher and Hoffman in 1996, reviewed 17 cases.3 A subsequent review by Madan and Levitt in 2014 expanded the dataset to include 25 cases but did not include all the cases in the first review.2 The case data extractions were done by all the authors.
Some published literature was available only in abstract form. In those cases, we extracted all relevant information provided, such as the highest plasma salicylate concentrations and patient symptoms. However, if critical details such as patient outcomes were missing, this limitation was noted as “not available.” If no specific information about the salicylate poisoning could be obtained from an article or from the prior reviews, we excluded the article from our review. We also excluded five case reports due to lack of availability of the paper or incomplete details such as salicylate blood levels and case data.4-8 From each case report, we recorded the year of publication, patient age, sex, concentration of topical salicylate/vehicle, peak reported salicylate concentration (mg/ dL), day of peak plasma levels, underlying diseases, case outcome, and physical exam findings. If available, we noted body weight, salicylate concentration, diluent, estimated surface exposure, length of exposure, and timing of administration. All salicylate units were converted into mg/dL
The cases reviewed included a wide age range; the youngest cases involved three newborns (< one month of age), and the oldest were two 80-year-olds.3,26,29,32,34 Demographic data showed that 67.4% (29/43) of cases occurred in males, 30.2% (13/43) in females, and one case (1/43) of no specified gender. Most cases occurred in patients > 40 years of age (18 cases). Children under one accounted for seven cases, while there were only four cases in children between 1-10 years of age. Two cases had no reported ages.
The lowest plasma concentration reported was 14.0 mg/dL, and the highest was 223.0 mg/dL.21,33 Two cases did not have recorded plasma concentrations, and one was sampled postmortem.26,40 The most common symptoms of salicylate poisoning noted included tachypnea (32.5%), vomiting (25.5%), nausea (21.0%), and tinnitus (21.0%). Of the 43 previously reported cases, the most common underlying medical conditions associated with topical toxicity were 17 patients with psoriasis, (35.5%) and 10 (23.2%) with ichthyosis. Seven cases involved toxicities with intact skin.17,22,24,26,27,33,44 Death occurred in five cases (11.6%). Death was observed in patients with psoriasis and tinea imbricata, and there was one isolated death reported in a patient with intact skin.9,26,40 The final outcome of seven cases was not available.10,11,36,37,42,43
DISCUSSION
Our case report exemplifies the rare but important instance of systemic salicylate toxicity resulting from topical application of methyl salicylate over a large surface area in an elderly patient with multiple comorbidities. Because he applied the topical salicylates on himself, the amount that he may have ingested intentionally or accidentally is unknown. Since the last published reviews on topical salicylate poisonings, 13 cases have been added with 12 new cases reported from the literature and one case reported here.2,3 Despite reduced use of topical salicylate in dermatology, cases of topical salicylate toxicity continue to be reported. When informed of the blood salicylate levels, the family disclosed that the patient had recently been using a popular, aggressively marketed, methyl salicylatecontaining cream with multiple applications to about 18% of his body surface area within a two-day period. Notably, despite
Tabatabai
Table 1. Cases of toxicity from topical salicylic acid: 1952 to present.
of age.
Table 1. Continued.
Table 1. Continued.
in a non-English language.
R, resolved; D, death; F, female; M, male; n/a, not available; pm, postmortem; BSA, body surface area, newborn, < 1 month of age.
Table 1. Continued.
*Published in a non-English language.
**Salicylate toxicity was the only recorded symptom/effect. R, resolved; D, death; F, female; M, male; n/a, not available; pm, postmortem; BSA, body surface area, newborn, < 1 month of age.
intact skin and near-normal renal function, the patient had significant absorption of salicylate and a prolonged salicylate half-life resulting in toxicity.
In a voluntary study involving human subjects, the half-life after complete absorption of dermal salicylate was obtained from plasma concentrations. Subjects wore from 2-8 adhesive patches impregnated with methyl salicylate. The harmonic mean terminal half-life of methyl salicylate was determined to be 3.0 ± 1.2 hours.4 The half-life of methyl salicylate in our case report was prolonged and suggests continued absorption, additional oral exposure, or chronic salicylate exposure.
In cases where data were available, as in the case presented here, toxicities typically manifested within a few days of topical salicylate use. Severe toxicities, including seizures, severe metabolic acidosis, cerebral edema, acute respiratory distress syndrome, hypoglycemia, hypoglycorrhachia, ketosis, and death, were most often linked to applications of high-concentration salicylate products involving large body surface areas over extended periods. Elevated and toxic doses of salicylate typically occur with blood levels above 20-30 mg/dL, and can disrupt key physiological processes, leading to a wide range of harmful effects. Elevated toxic salicylate levels can impair oxidative phosphorylation, resulting in adenosine triphosphate production failure while also increasing oxygen consumption, metabolic acidosis, and heat generation.
Clinical manifestations in early toxicity often occur from stimulation of the brain’s respiratory center causing initial tachypnea and respiratory alkalosis, as seen in this case. The inhibition of Krebs cycle enzymes reduces glucose availability systemically and in the brain. This promotes organic acid accumulation, which leads to metabolic acidosis. Resultant significant fluid and electrolyte losses lead to dehydration, sodium and potassium depletion, and reduced buffering
capacity. Once absorbed, salicylic acid is metabolized by the liver to more water-soluble byproducts.5 In considering topical dosing, the surface area treated, the concentration of salicylate used should not be excessive; the use of occlusive dressings, the frequency of application, and the patient’s underlying volume- and renal-status must be considered.6 A study with patients with active psoriasis found that after 10 hours with occlusive dressing over the topical salicylates, 60% of the salicylate was absorbed.6
The priority in treating any poisoned patient is assessing the airway, oxygenation, and maintaining perfusion of organs. Once toxicity is identified, it is critical to lower the salicylate levels. Resuscitation should begin with thorough skin decontamination with soap and water to remove any remaining drug and fluids, and dextrose 5% with 3 ampules of sodium bicarbonate to buffer the metabolic acidosis; added potassium chloride increases renal excretion and helps to prevent brain absorption by ion trapping of the salicylate. Potassium chloride is often added to prevent hypokalemia, the presence of which will inhibit alkalinization of the urine. Hemodialysis is indicated for severe acidosis, acute respiratory distress syndrome, severe altered mental status, seizures, kidney failure, refractory hypotension, and salicylate levels greater than 100 mg/dL for acute exposures and potentially lower levels for chronic exposure.7 The Extracorporeal Treatments in Poisoning workgroup recommendations and indications for salicylate poisoning are very useful.45
In addition to the concentration and surface area of application, different formulations of topical salicylic acid have different levels of systemic absorption. A study by Morra et al found that the methyl salicylate used in the current case demonstrated higher absorption compared to other formulations such as trolamine salicylate.8 Methyl salicylate reached detectable serum salicylate levels within one hour of application with cumulative absorption increasing after
Tabatabai et
repeated applications. In contrast, trolamine salicylate showed minimal skin absorption, with serum salicylate levels often undetectable and significantly lower recovery in urine.8 Our review of 43 previous cases plus the current case of topical salicylate toxicity corroborates this observation.
As summarized in Table 1, symptoms of topical salicylate toxicity are broad and generally develop within a few days of use, particularly when applied over large body surface areas, compromised skin, or with repeated applications. While the most common findings in the literature review were metabolic abnormalities, altered mental status, tachypnea, vomiting, nausea, and tinnitus, the current patient had altered mental status, metabolic acidosis with elevated anion gap, and tachypnea (with respiratory alkalemia) but only reported tinnitus after he regained his baseline mental status and the salicylate levels had fallen. This suggests that older patients or those with comorbid conditions like dementia can be a challenge to diagnose and demonstrates the need for heightened clinical suspicion when presented with a limited history and symptoms.
This case report and descriptive analysis of similar historical cases emphasizes the need for further patient education about the potential toxicity of OTC topical salicylates and their use to improve their safety among the general population and particularly in vulnerable populations such as children, renal-compromised patients, and patients with baseline altered mental status. This report reinforces the need for clinicians to suspect and inquire about topical salicylate use in patients with an elevated anion gap and altered mental status given its widespread use and availability.
LIMITATIONS
Retrospective literature research has several limitations. Some older publications, particularly those predating digital archiving, may have been excluded in the search due to their limited availability and not being included in the electronic databases searched. A few publications were not available. If available, abstracts were used, but some provided limited data such as patient outcomes, sex, age, and symptoms. Publication bias clearly favors publication of toxic cases but considering the limited number of cases found over 72 years, the incidence of topical salicylate toxicity must be low. Case reports have significant limitations. This case report also has limitations in terms of history and potential chronic or oral dosing of salicylates that was denied by the family but still could have happened.
CONCLUSION
Topical salicylates have the potential for systemic toxicity particularly when large doses of methyl salicylate are applied in high concentrations in vulnerable populations such as patients with compromised renal function, and in pediatric patients with a large surface-to-body ratio. The inappropriate use of methyl salicylate products in particular, especially in high concentrations over large body surface areas, on compromised skin, and with repeated applications can pose
significant health risks. Clinicians should maintain a high index of suspicion for salicylate toxicity in patients presenting with non-specific symptoms such as altered mental status, or unexplained metabolic acidosis or tachypnea especially in those with a history of topical salicylate use. Although salicylate toxicity is not common, early recognition and intervention are essential to prevent or reduce clinical toxicity and ensure rapid resolution. Widespread patient education about the toxicological risk of these heavily advertised topical salicylate products is also needed.
Address for Correspondence: Timothy Albertson, MD, MPH, PhD, University of California, Davis, School of Medicine, Departments of Emergency Medicine and Internal Medicine, 4150 V Street, Suite 3100, Sacramento, CA 95817. Email: tealbertson@ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Tabatabai et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Yeoh SC, Goh CF. Topical delivery of salicylates. Drug Deliv Transl Res. 2022;12(5):981-1001.
2. Madan RK, Levitt J. A review of toxicity from topical salicylic acid preparations. J Am Acad Dermatol. 2014;70(4):788-92.
3. Brubacher JR, Hoffman RS. Salicylism from topical salicylates: review of the literature. J Toxicol Clin Toxicol. 1996;34(4):431-6.
4. Martin D, Valdez J, Boren J, et al. Dermal absorption of camphor, menthol, and methyl salicylate in humans. J Clin Pharmacol 2004;44(10):1151-7.
5. Temple AR. Pathophysiology of aspirin overdosage toxicity, with implications for management. Pediatrics. 1978;62(5 Pt 2 Suppl):873-6.
6. Taylor JR, Halprin KM. Percutaneous absorption of salicylic acid. Arch Dermatol. 1975;111(6):740-3.
7. Runde TJ, Nappe TM. Salicylates toxicity. In (Okocha and Shumway, et al, Eds.), StatPearls. Treasure Island (FL): StatPearls Publishing, 2023.
8. Morra P, Bartle WR, Walker SE, et al. Serum concentrations of salicylic acid following topically applied salicylate derivatives. Ann Pharmacother. 1996;30(9):935-40.
9. Chodorowski Z, Anand JS, Waldman W. [Suicidal salicylate intoxications and unintentional percutaneous poisoning with salicylic ointment]. Przegl Lek. 2003;60(4):302-4.
10. Jongevos SF, Prens EP, Wolterbeek JH, et al. [Acute perceptive hearing loss and metabolic acidosis as complications of the topical
Tabatabai et al.
Risk of Systemic Toxicity from Topical Salicylates treatment of psoriasis with salicylic acid-containing ointment]. Ned Tijdschr Geneeskd. 1997;141(43):2075-9.
11. Treguer H, Le Bihan G, Coloignier M, et al. [Salicylate poisoning by local application of 20% salicylic acid petrolatum to a psoriatic patient]. Nouv Presse Med. 1980;9(3):192-3.
12. Maurer TA, Winter ME, Koo J, et al. Refractory hypoglycemia: a complication of topical salicylate therapy. Arch Dermatol 1994;130(11):1455-7.
13. Dwyer CM, McCloskey RH, Kerr RE. Poisoning from topical salicylic acid. Postgrad Med J. 1994;70(820):146.
14. Pec J, Strmenova M, Palencarova E, et al. Salicylate intoxication after use of topical salicylic acid ointment by a patient with psoriasis. Cutis. 1992;50(4):307-9.
15. Raschke R, Arnold-Capell PA, Richeson R, et al. Refractory hypoglycemia secondary to topical salicylate intoxication. Arch Intern Med. 1991;151(3):591-3.
16. Fil E, Dilek S, Umur O, et al. An infant developed intoxication following topical salicylate use: a case report. Ped Acad Case Report J. 2024;3(1):012-016.
17. Wong A, Mac K, Aneman A, et al. Modern intermittent haemodialysis (IHD) is an effective method of removing salicylate in chronic topical salicylate toxicity. J Med Toxicol. 2016;12(1):130-3.
18. Pertoldi F, D’Orlando L, Mercante WP. [Acute salicylate intoxication after trancutaneous absorption]. Minerva Anestesiol. 1999;65(78):571-3.
19. Germann R, Schindera I, Kuch M, et al. [Life-threatening salicylate poisoning caused by percutaneous absorption in severe ichthyosis vulgaris]. Hautarzt. 1996;47(8):624-7.
20. Abdel-Magid EH, el-Awad Ahmed FR. Salicylate intoxication in an infant with ichthyosis transmitted through skin ointment--a case report. Pediatrics. 1994;94(6 Pt 1):939-40.
21. Luderschmidt C, Plewig G. [Chronic percutaneous salicylic acid poisoning]. Hautarzt. 1975;26(12):643-6.
22. Renzetti M LE, Schenck E, Mailman J. Slathering salicylates: a topical story. Am J Respir Crit Care Med. 2021.
23. Vazquez Martinez JL, Stanescu S, Castrillo Bustamante S, et al. Unrecognized transcutaneous severe salicylate intoxication in an infant. Pediatr Emerg Care. 2015;31(9):e8.
24. Robinson K, Rauch A, Hannan L. Salicylate poisoning following topical administration of methylsalicylate. Emerg Med Australas 2015;27(4):374-5.
25. Oualha M, Dupic L, Bastian C, et al. [Local salicylate transcutaneous absorption: an unrecognized risk of severe intoxication: a case report]. Arch Pediatr. 2012;19(10):1089-92.
26. Chin RL, Olson KR, Dempsey D. Salicylate toxicity from ingestion and continued dermal absorption. Cal J Emerg Med. 2007;8(1):23-5.
27. Cull M, Vicas IM-O. Salicylate Toxicity with Topical Exposures on Intact Skin. Abstracts of the 2005 North American Congress of Clinical Toxicology. Clin Toxicol. 2005;43:640.
28. Bell AJ, Duggin G. Acute methyl salicylate toxicity complicating herbal skin treatment for psoriasis. Emerg Med (Fremantle) 2002;14(2): 188-90.
29. Yamamura S, Kinoshita Y, Kitamura N, et al. Neonatal salicylate poisoning during the treatment of a collodion baby. Clin Pediatr (Phila). 2002;41(6):451-2.
30. Peyriere H, Balmes N, Rouanet I, et al. Acute salicylate intoxication after percutaneous absorption in an HIV patient treated for psoriasis. AIDS. 2002;16(13):1843-4.
31. Chiaretti A, Schembri Wismayer D, Tortorolo L, et al. Salicylate intoxication using a skin ointment. Acta Paediatr. 1997;86(3):330-331.
32. Galea P, Goel KM. Salicylate poisoning in dermatological treatment. Arch Dis Child. 1990;65(3):335.
33. Chow WH, Cheung KL, Ling HM, et al. Potentiation of warfarin anticoagulation by topical methylsalicylate ointment. J R Soc Med 1989;82(8):501-2.
34. Ward PS, Jones RD. Successful treatment of a harlequin fetus. Arch Dis Child. 1989;64(9):1309-11.
35. Shupp DL, Schroeter AL. An unusual case of salicylate toxicity. J Am Acad Dermatol. 1986;15(2 Pt 1):300-1.
36. Smith WO, Lyons D. Metabolic acidosis associated with percutaneous absorption of salicylic acid. J Okla State Med Assoc 1980;73(1):7-8.
37. Anderson JA, Ead RD. Percutaneous salicylate poisoning. Clin Exp Dermatol. 1979;4(3):349-51.
38. Davies MG, Briffa DV, Greaves MW. Systemic toxicity from topically applied salicylic acid. Br Med J. 1979;1(6164):661.
39. Aspinall JB, Goel KM. Salicylate poisoning in dermatological therapy. Br Med J. 1978;2(6148):1373.
40. Lindsey CP. Two cases of fatal salicylate poisoning after topical application of an antifungal solution. Med J Aust. 1968;1(9):353-4.
41. Vonweiss JF, Lever WF. Percutaneous salicylic acid intoxication in psoriasis. Arch Dermatol. 1964;90:614-9.
42. Cawley EP, Wheeler CE. Salicylic acid poisoning in dermatological therapy. J Am Med Assoc. 1953;151(5):372-4.
43. Young CJ. Salicylate intoxication from cutaneous absorption of salicylic acid. South Med J. 1952;45(11):1075-7.
44. Thompson TM, Toerne T, Erickson TB. Salicylate toxicity from genital exposure to a methylsalicylate-containing rubefacient. West J Emerg Med. 2016;17(2):181-3.
45. Juurlink DN, Gosselin S, Kielstein JT, et al. Extracorporeal treatment for salicylate poisoning: systematic review and recommendations from the EXTRIP Workgroup. Ann Emerg Med. 2015;66(2):165-81.
Self-Harm and Interpersonal Violence-Related Injuries: Retrospective Analysis of the American College of Surgeons Trauma Quality Programs Data
Ayman El-Menyar, MD*†
Ahammed Mekkodathil, MPH*
Rafael Consunji, MD‡
Sandro Rizoli, MD, PhD§
Tarik S Abulkhair, RN§
Ruben Peralta, MD§||
Rifat Latifi, MD#
Hassan Al-Thani, MD§
Hamad Medical Corporation, Department of Surgery, Clinical Research, Trauma and Vascular Surgery, Doha, Qatar
Weill Cornell Medical College, Department of Clinical Medicine, Doha, Qatar
Hamad Medical Corporation, Department of Surgery, Trauma Surgery, Injury Prevention Program, Doha, Qatar
Hamad Medical Corporation, Department of Surgery, Trauma Surgery, Doha, Qatar
Universidad Nacional Pedro Henriquez Urena, Department of Surgery, Santo Domingo, Dominican Republic
College of Surgery, Department of Surgery, Pristina, Kosovo
Section Editor: Wirachin Hoonpongsimanont, MD, MSBATS
Submission history: Submitted January 24, 2025; Revision received April 18, 2025; Accepted May 24, 2025
Electronically published August 29, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.42044
Introduction: Violence-related injuries (VRI) such as interpersonal violence, intimate-partner violence, and self-harm injuries present a significant public health challenge in the United States. We aimed to explore interpersonal-violence and self-harm injuries, focusing on demographic disparities (age and sex) and mechanisms of injury, including firearm-related violence.
Methods: We conducted a retrospective study of VRIs among the US civilian population between 2017–2021. Data were extracted from the American College of Surgeons (ACS) Trauma Quality Programs Participant Use Files. We identified VRIs using the International Classification of Diseases, 10th Rev, with Australian modification E-code series. The dataset was categorized and compared by age, sex, ethnicity, violence intent, and mechanism of injury. This study was a secondary data analysis reporting interpersonal-violence and self-harm injuries among trauma cases from the national trauma database.
Results: The total number of trauma patients in the ACS database was 5,483,016 between 2017– 2021 (1.1 million/year). The final analysis included 584,417 (11%) patients with VRIs (interpersonal violence and self-harm), with a mean age of 35 years; 82% were male, 45% White, and 42% Black. Interpersonal violence accounted for 88% of injuries, while 12% were self-harm, with firearm-related violence the most common mechanism of injury (35%). Firearm-related interpersonal violence was common among younger individuals (19-39 years), while non-weaponized interpersonal violence was prevalent among older individuals (≥ 60 years). Blacks had a higher rate of firearm-related interpersonal violence (51%), and Whites had a greater frequency of non-weaponized interpersonal violence. There were 43,089 deaths (7.4%), with 68% resulting from interpersonal-violence and 32% from self-harm injuries. Firearmrelated injuries (interpersonal violence and self-harm combined) accounted for 78% of all VRI-related deaths. Mortality was higher in males (7.7%) than in females (5.9%) (P < .001).
Conclusion: There is a significant burden of violence-rated injuries in the US, particularly affecting males, racial minorities, and vulnerable age groups. Firearm-related injuries are the leading cause of death in both interpersonal-violence and self-harm cases. The increase in VRIs during the COVID-19 pandemic highlights the urgent need for targeted public health interventions focused on firearm safety, violence prevention, and mental health support. [West J Emerg Med. 2025;26(5)1468–1477.]
INTRODUCTION
Violence-related injuries (VRI) remain a significant public health concern; it is collectively responsible for 4.4 million deaths (8% of all deaths) worldwide.1 Self-harm or self-inflicted injury is the main mechanism of VRIs leading to death, followed by interpersonal violence.1 In the 15-29 years age group, interpersonal violence is the third leading cause of death, while self-harm ranked fourth.1 In addition to the immediate consequences, VRIs have a lifelong impact on individuals and communities, including mental health challenges, disabilities, healthcare costs, and diminished individual productivity.2,3
In the United States, violence-related fatalities remain a major concern, with homicide and suicide accounting for 14 and 7.8 deaths per 100,000 individuals, respectively, in 2020.4 Beyond mortality, nonfatal VRIs are also significant. Approximately 1.6 million individuals experience non-fatal interpersonal-violence injuries annually.5 The economic burden of violence is considerable, with the combined costs of homicides and suicides estimated at $670 billion6 and the inflation-adjusted medical and work-loss costs for VRIs among adults reaching $49.5 billion in a single year.7 Additionally, about 1.4 million adults sought emergency department (ED) care for VRIs, representing 1.6% of all adult ED visits in the US. Visits to the ED were disproportionately higher among young adults 18-25 years of age, males, nonWhites, uninsured or publicly insured patients, and residents of high-poverty urban areas.7
The demographic pattern of VRIs in the US aligns with global trends, as worldwide statistics reveal that males accounted for 84% of VRI fatalities between 2010–2015.8 In contrast, females represented 16% of VRI deaths, equivalent to an annual average of 64,000 deaths.8 However, analysis of ED visits for interpersonal-violence injuries shows only a slight male predominance, with rates of 4.9 vs 4.2 visits per 1,000 individuals for males and females, respectively.9 The highest rate of interpersonal violence -related ED visits was observed among young adults aged 18-24 years (9.2 visits per 1,000 individuals annually), declining slightly in the 25-44 age group (7.7 visits per 1,000) and further among older adults.9 Until 2015, most fatalities from interpersonal violence were attributed to firearm-related injuries.10 By 2022, firearm-related injuries accounted for over 48,000 deaths, approximately 132 deaths per day, with more than half due to suicides and over 40% resulting from firearm homicides.11 While VRIs, which include both interpersonal violence and self-harm, remain major public health concerns, significant knowledge gaps persist regarding the demographic disparities, mechanism of injury, and evolving trends influenced by the COVID-19 pandemic. In particular, the prominent role of firearm-related injuries in both interpersonal violence and self-harm contexts requires focused attention to guide prevention efforts. In this study we aimed to explore the patterns of interpersonal violence and self-harm injuries in
Population Health Research Capsule
What do we already know about this issue?
Violence-related injuries (VRI) such as interpersonal violence and self-harm have significant mortality and economic burden, with firearms a major factor in the US.
What was the research question?
What were the demographic disparities, mechanisms, and trends of interpersonalviolence and self-harm injuries in the US from 2017–2021?
What was the major finding of the study?
Among VRIs (88% interpersonal and 12% selfharm), firearms represented 35% of mechanism of injury. Males had higher VRI mortality than females (7.7 vs 5.9%), P < .001.
How does this improve population health?
Identifying high-risk groups will guide targeted interventions for violence prevention, firearm safety, and mental health support to reduce morbidity and mortality.
the US, focusing on demographic disparities, firearm-related mechanisms, and pandemic-associated trends. We sought to provide a comprehensive understanding to inform targeted public health interventions, violence prevention strategies, and firearm injury-prevention efforts.
METHODS
We conducted a retrospective study of VRIs in the US between 2017–2021. Data pertaining to VRIs within the civilian population were extracted from the American College of Surgeons (ACS) Trauma Quality Programs Participant Use Files. All data were obtained from an existing database (secondary data analysis); no individual chart abstraction was performed; therefore, specific chart-review methodologies, such as those described by Worster and Bledsoe, were not applicable.12 Over 99.5% of the data pertains to patients within the US; a small minority of international patients also contribute to the dataset. However, due to data protection regulations, specific geographic information on patients or facilities was not available. Since this study involved secondary analysis of de-identified data provided by the ACS files, institutional review board approval was not required. The selected external cause codes (E-codes) from the International Classification of Diseases, 10th Rev, with
Australian modification (ICD-10-AO) in the trauma registry— specifically T43, T51-T65, T71, T74, T76, X71-X83, X92-X99, Y00-Y08, and Y35-Y38—were used to identify VRIs. We excluded from the study injuries sustained by military personnel during military operations, war operations, and other legal interventions. We also excluded cases lacking age and sex data (only males and females were included) and those with missing information regarding the mechanism of injuries. This study reported intentional injuries focusing on VRIs (both interpersonal violence and self-harm) from all trauma cases in the database. The data were categorized based on violence intent, type of trauma, and mechanism of injury. The intent of trauma were interpersonal violence and self-harm. The violence intent, type of trauma, and mechanism of injury were assigned based on ICD-10-AO E-codes. Trauma types included blunt, penetrating, burn, and other forms (eg, asphyxiation, drowning, poisoning). Mechanism of injury included blunt assaults (eg, motor vehicle collisions, falls), penetrating injuries (eg, firearms, sharp objects), burns, and other mechanisms.
The World Health Organization defines violence as the intentional use of physical force or power, either threatened or actual, resulting in injury, death, psychological harm, mal-development, or deprivation.13 This inclusive definition spans interpersonal, self-directed, and collective violence. Interpersonal violence involves the intentional use of force against others by an individual or small group, manifesting physical, sexual, or psychological harm. Family or partner violence encompasses child maltreatment, dating and intimate partner violence, and elder maltreatment. Community violence involving non-family individuals includes youth violence, bullying, assault, and institutional violence in settings like schools and workplaces.13
In our study, non-weaponized interpersonal violence refers to physical harm inflicted through bodily force without the use of external objects such as firearms, blunt instruments, or sharp weapons. This category includes acts of physical abuse, sexual abuse, and physical assault involving personal force, such as punching, kicking, slapping, or other forms of direct contact. A perpetrator of maltreatment and neglect is an individual responsible for causing harm or failing to provide adequate care to a vulnerable person, such as a child, elderly individual, or dependent adult. Perpetrators are often caregivers or family members who abuse their responsibilities, leading to physical, emotional, or developmental harm to the victim.
Statistical Analysis
We used descriptive statistics to summarize the demographic profiles, mechanism of injury, and mortality rates of VRIs in different age groups, ethnicities, and sex. Continuous variables, such as age, were summarized using means and standard deviations, while categorical variables, including sex, race, mechanism of injury, and mortality, were reported as frequencies and percentages. We employed chi-
square tests to assess the association between categorical variables, such as sex, race, and mechanism of injury, with interpersonal violence and self-harm. Continuous variables such as age were compared using t-tests. The age groups were 0-18, 19-39, 40-60, and > 60. We compared injuries among US ethnicities (White, Black, Asian, Hispanic/Latino, and others). We employed the Python 3.0 pandas library (Python Software Foundation, Wilmington, DE) for data compilation and performed statistical analysis using SPSS v21 (IBM Corp, Armonk, NY). Case fatality rate was calculated as the proportion of deaths among patients with a specific injury mechanism, expressed as a percentage.
RESULTS
Between 2017–2021, the total number of trauma patients in the ACS database was 5,483,016 (1.1 million/year). The final analysis included 584,417 (11%) patients with VRIs (Figure 1).
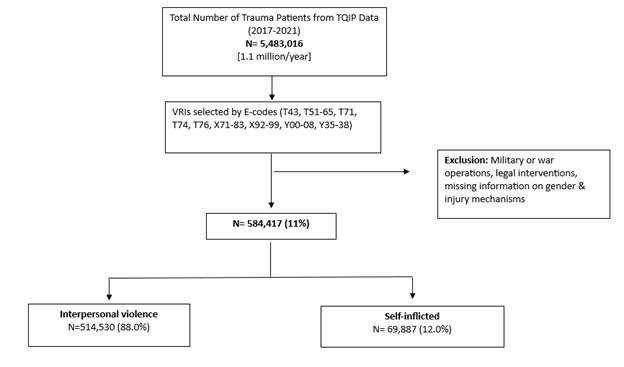
Figure 1. Selection flowchart of violence-related injury cases from the dataset of the American College of Surgeons Trauma Quality Programs Participant Use File, 2017–2021. TQIP, Trauma Quality Improvement Program; E-code, external cause code
The mean age of patients was 35 years (±15), and 82% were males (Table 1). The racial distribution was 45% White and 42% Black. Interpersonal violence accounted for 88% of VRIs, while self-harm constituted 12%. Firearm-related injuries were the most common mechanism of injury, comprising 35% of all VRIs, followed by non-weaponized interpersonal violence (28%) and cut or pierce injuries (23%) (Figure 2).
Mortality among patients with VRIs was 7.4%, with a significantly higher case fatality rate observed among males (7.7%) compared to females (5.9%) (P < .001). Firearmrelated injuries accounted for 78% of total VRI mortality (80% in males vs 66% in females, P = .001). Firearm-related interpersonal violence mortality was 52% of all VRI mortality (55% in males vs 40% in females, P = .001). In contrast, firearm-related self-harm mortality accounted for 25% of all VRI mortality (25% in males vs 26% in females) of total
Table 1. Description of patients with violence-related injuries in the United States (2017–2021) (N = 584,417)
Variable Values
Mean age 35 ± 15 years
Sex
Male 477,781 (81.8%)
Female 106,636 (18.2%)
Race
White 253,521 (45.1%)
Black 236,538 (42.0%)
Asian 6,944 (1.2%)
Hispanic/Latino 43,870 (7.8%)
Other 21,820 (3.9%)
Intent of violence
Interpersonal violence 512,834 (87.8%)
Self-inflicted/self-harm
Mechanism of injury
Firearm-related injuries
Physical/sexual abuse/other bodily force
(12.2%)
(34.6%)
(28.3%)
Cut or pierce injuries 136,252 (23.3%)
Injuries by blunt objects 48,234 (8.3%)
Other 17,098 (2.9%)
Injured body region
Head
245,654 (49.0%)
Neck 52,633 (10.5%)
Chest 139,271 (27.8%)
Abdomen, pelvis or spine 127,411 (25.4%)
Upper limb 157,395 (31.4%)
Lower limb 124,957 (24.9%)
Transport mode
Ground ambulance
437,552 (75.3%)
Helicopter ambulance 39,188 (6.7%)
Fixed-wing ambulance 1,937 (0.3%)
Private/public vehicle 88,519 (15.2%)
Police 9,884 (1.7%)
Other 4,136 (0.7%)
Work-related injuries 5,261 (0.9%)
Prehospital cardiac arrest 22,212 (3.8%)
Alcohol screening 354,430 (61.3%)
Mean GCS in hospital 13.4± 3.7
Median hospital length of stay 3 (1-1)
Death in emergency department 9,769 (1.7%)
Total mortality 43,089 (7.4%)
GCS, Glasgow Coma Scale
mortality (55% in males vs 40% in females). In contrast, firearm-related self-harm mortality of all VRI mortality was similar, 25% in males and 26% in females (Table 2).
The age-stratified analysis demonstrated that firearm-related interpersonal violence was most prevalent among children 0-18 years of age (51%) and younger adults (19-39 years of age; 42%), whereas non-weaponized interpersonal violence was more common in older adults ≥ 60 years of age (53%) (Table 3). Firearm-related self-harm injuries were also more common among older adults (46%) when compared to other age groups (P = .001). Similarly, racial disparities were evident. Blacks had disproportionately higher rates of firearm-related interpersonal violence, while Whites had a higher frequency of nonweaponized interpersonal violence. In self-harm, firearm injuries were more common in Whites, whereas cut or pierce injuries were more common among Asians (Table 4).
Trends over time revealed an increase in the proportion of VRIs during the pandemic years, rising from 18.9% in 2017 to 21.8% in 2020 before slightly declining to 21.4% in 2021. Mortality associated with VRIs also increased from 18.5% in 2017 to 23.2% by 2021 (Table 5).
DISCUSSION
This study provides a comprehensive analysis of VRIs in the US, revealing significant demographic disparities and highlighting the dominant role of firearm-related injuries in both interpersonal violence and self-harm. Young males, particularly Black individuals, were disproportionately affected by firearm-related interpersonal violence, while nonweaponized interpersonal violence was more common among older adults and White individuals. These findings emphasize the need for targeted interventions addressing firearm violence and demographic vulnerabilities.
In 2011, approximately 1.4 million people worldwide lost their lives due to violence, with 35% of these deaths attributed to interpersonal violence.14 Sumner et al5 described the burden of interpersonal violence in the US based on data from multiple health and law enforcement surveillance systems. Homicide rates significantly decreased from a peak of 10.7 per 100,000 in 1980 to 5.1 in 2013. Non-fatal interpersonal violence rates dropped by 45% from 1992 to 2012. Partner violence rates show that 32% of women and 28% of men have experienced physical violence in their lifetime. Intimate partner violence rates against women have decreased by 72% since 1994. Elder abuse affects 11% of community-dwelling adults ≥ 60 years of age.5
The US Centers for Disease Control and Prevention WISQARS compilation (Web-based Injury Statistics Query and Reporting System) shows the top causes of death for individuals 1-44 years of age in the US from 1981–2022. In 1981, unintentional injury was the leading cause with 58,500 deaths, homicide was third with 17,900 deaths, and suicide was
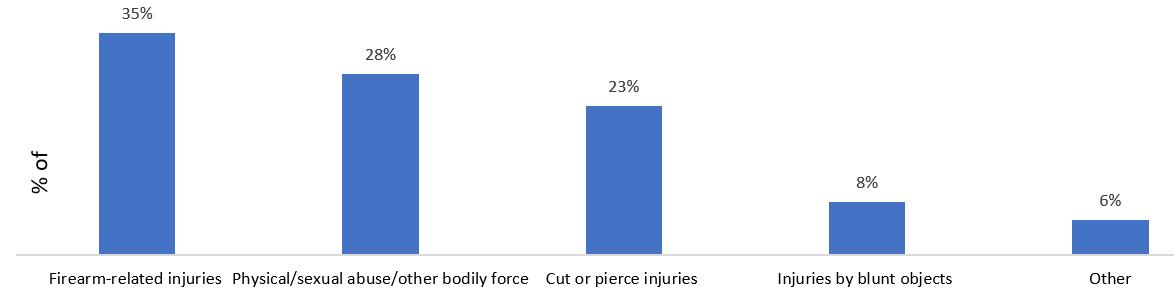
2. Distribution of violence-related injury mechanisms in the United States (2017–2021).
Table 2. Distribution of violence-related injuries by intent, mechanism, sex, and associated mortality (N = 584,417).
Intent of Violencerelated Injury (VRI)
fifth with 15,900 deaths. By 2012, suicide became the second leading cause with 18,200 deaths, while homicide dropped to fifth with 12,300 deaths. In 2020, homicide rose to third with
18,800 deaths, and suicide remained second with 22,400 deaths. In 2021, COVID-19 became the third leading cause with 23,700 deaths, but suicide stayed second with 23,900 deaths. By 2022,
Figure
Table 3
Type of violencerelated injuries Mechanism of injuries
Interpersonal -violence- related injuries (IPV)
Self-inflicted/ Self- harm injuries (SH)
suicide remained second with 23,400 deaths, and homicide was third with 18,600 deaths.15 Our study demonstrates that upward trends in VRI rates and mortality highlight a growing burden of VRIs across both sexes, with males consistently representing a larger share of the affected population. From 2020, VRIs and mortality demonstrated a rise in the post-COVID-19 years. Injuries increased from 19.1% in 2019 to 21.8% in 2020 and remained high at 21.4% in 2021. Mortality rose from 17.9% in 2019 to 23.2% by 2021, reflecting the impact of the pandemic on violence trends.
Previous reports show that older adults > 60 years of age accounted for 2% of ED visits following intimate partner violence, more frequently males and Black, sustained injuries due to cutting, lacerations, and injuries to the upper extremity.16,17 Meyer et al18 also reported that the older adult victims of firearmrelated violence were predominantly Black (50%) and males (85%). Hiranniramol et al19 studied patients presenting with VRIs and found that the average age was 33 years, with 70-80% being Black males. Homicide rates varied significantly by age and sex, with males 15–29 years of age experiencing nearly five times the homicide rate of females.20 Our study also demonstrated that young males are more likely to experience violence-related deaths, particularly from firearms. Interestingly, global data
show that female homicide rates doubled between ages 5–14 and 15–29 and in women ≥ 70 years of age. However, our study demonstrated high mortality rates among both older adults (12%) and children < 19 years of age (80%). Gitto et al21 reported that the most common cause of death among female victims was firearm-related wounds, followed by sharp force traumas, asphyxia, and blunt force injuries.
Carmichael et al10 studied more than 18,000 homicides based on data from the National Violent Death Reporting System. They found that most of the deaths were due to firearms (72%) or sharp objects (13%). More than half (53%) of the patients who died on the scene were neither seen by emergency medical services nor transported to an ED, most probably due to the severity of the injury or remaining unnoticed for a long time by someone other than the suspect. Seven of ten medically treated firearm injuries in youths result from interpersonal violence, with males 14-24 years of age accounting for 88% of these cases.22
Dowd et al23 reported that 18% of patients with penetrating firearm-related self-harm injuries had major psychiatric illnesses, 8% had alcohol use disorder, 6% had drug use disorder, and a few (0.6%) had dementia. The study reported an upward trend in the proportion of patients with major psychiatric illnesses, from
Table 4. Race-stratified distribution of violence-related injuries in patient population in the United States (2017–2021).
Type of violencerelated injuries
injuries
(N= 203,461)
(N = 227,533)
Table 5.Trends of violence-related injuries and mortality in the United States (2017–2021).
16% in 2013 to 19% in 2016, with a peak in 2015 at 21%. A high mortality rate (50%) was observed in firearm-related selfharm injuries when compared with attempted murder (7%) and accidental discharge of guns (3%). Blacks were more likely to get injured due to attempted murder than Whites (85% vs 40%), whereas rates of accidental discharge of gunshot (47% vs 13%) and self-harm injuries were higher in White patients.23
Young and Xiang24 reported that Blacks were heavily impacted by firearm homicide, with homicide age-adjusted
death rates almost seven times higher when compared to Whites. A scoping review of 19 studies conducted by Marineau et al25 indicated that Black men in the US face disproportionate risks of firearm-related interpersonal violence, primarily due to structural and social inequities. The review identified key risk factors across the social-ecological framework, such as firearm possession at the individual level, gang membership at the relationship level, socioeconomic status at the community level, and historical racist policies at the societal level.
Tennakoon et al26 studied domestic and intimate partner violence in the US and found that young males were more likely to become victims. Our study demonstrated that male mortality rates were significantly higher. Firearm-related VRIs remain a significant mechanism in both interpersonal violence and self-harm cases, contributing to 78% of total deaths. The gun homicide rate in the US was nearly 25 times higher than in other high-income countries.27 Bell et al28 reported a stable overall intentional injury rate among adolescents but highlighted an increase in self-harm injuries, particularly among younger females. Our study showed a high proportion of firearm-related self-harm deaths among older adults.
Hoefer et al29 studied 41,239 pediatric firearm-trauma patients and observed a significant rise in firearm-related self-harm incidence over a 12-year period, with a substantial proportion being White (67%), teenagers (90%), and males (87%). The firearm-related self-harm mortality rate was reported as 44%, with head gunshot wounds and higher Injury Severity Score significantly linked to mortality.29 DiVietro et al30 reported that non-Hispanic White children died at a rate that was 1.3 times greater than expected based on their proportion in the general population and were 2.6 times more likely to die by firearm suicide than non-Hispanic Black children.
The COVID-19 pandemic further exacerbated the firearm violence crisis. Shannon et al31 observed a rise in firearmrelated violence during the pandemic despite an overall 10% decrease in assault-related hospitalizations. Stevens et al32 found that pediatric firearm injuries surged during the pandemic, with a cumulative increase in 2020 compared to historical data. Risinger et al31 reported that from 2011–2021, Jefferson County, Kentucky, recorded 6,043 firearm injuries. During the COVID-19 period, 4,574 years of potential life were lost due to the pandemic, compared to 9,722 years lost to all-cause gun violence. In the pre-COVID-19 period, there were 5,723 years of potential life lost due to all-cause gun violence.33 Firearm violence incidents, injuries, and deaths surged following society’s re-emergence from the COVID-19 pandemic.
Additionally, mass shootings increased despite the initial decline during the pandemic, indicating that the “reopening phenomenon” exacerbated an already significant national firearm epidemic.34 This study period from 2017–2021 includes pre-pandemic, pandemic, and post-pandemic eras, providing the pattern of VRIs across these distinct timeframes. During the pandemic era (2020-2021), VRIs demonstrated a notable increase compared to pre-pandemic years. In 2020, the overall proportion of VRIs peaked, and this trend was consistent across sexes. Mortality associated with VRIs also demonstrated an increase during the pandemic years. These findings indicate that the pandemic era coincided with increased VRIs and mortality, possibly influenced by factors such as social isolation, economic challenges, increased stress, and disruptions to healthcare and social support systems. Also of concern is the high rate of trauma recidivism, wherein patients suffer subsequent VRIs. Studies have
reported five-year recidivism rates ranging from 25-44%, with one study reporting that recidivists accounted for 16% of trauma visits.35,36 El-Menyar et al37 analyzed 9,855 trauma patients and found that 8% had a history of violence prior to admission at a New York hospital . These patients were more likely to be younger, male, Black, Hispanic, and covered by low-income primary insurance payors compared to nonassault trauma patients. Multivariate logistic regression indicated that predictors of violence included being Black and male, with low-income primary insurance payor status, and Asian ethnicity, drug use, alcohol intoxication, and smoking.
Factors such as the mechanism of injury and behaviors are closely linked to higher recidivism rates.38, 39 This predisposition to repeat VRIs creates a worsening cycle of trauma, particularly with penetrating injuries and firearm-related incidents, which significantly increase the risk of death with each subsequent injury.35,38 These findings highlight the need for targeted public health interventions focused on firearm violence prevention among high-risk populations, particularly young males and racial minorities disproportionately affected by interpersonal violence. In addition, mental health support programs aimed at reducing self-harm injuries, especially among older adults, are essential. Interventions should focus on promoting firearm safety, preventing violent conflicts, and supporting communitybased programs to reduce the burden of VRIs. Public health efforts must also consider the demographic disparities and the impact of the COVID-19 pandemic on violence trends.
Schwartz et al40 examined firearm-related injuries in the US civilian population using prehospital data from the National Emergency Medical Services Information Systems database. Their findings revealed that prehospital responders most frequently classified injuries to four anatomical regions as Critical-Red: 63% of chest injuries; 54% of abdominal injuries; 48% of neck injuries; and 42% of back injuries. In our study, the head was the most frequently injured body region, accounting for 49% of injuries. Neck injuries were reported in 11% of cases, while chest injuries comprised 28%. Injuries to the abdomen, pelvis, or spine were noted in 25% of cases.
A recent review by Sakran and Lunardi41 highlights the critical role that surgeons play, emphasizing hemorrhage control, expeditious transport to a trauma center, and even prehospital blood administration as examples of systems coordination between EMS and trauma centers that can prevent deaths from VRIs. They also cite the need to fully understand the social and political determinants of firearm injury to decrease the number of VRIs. Hospital-based, violence prevention programs are of utmost value as studies showed that exposure to firearm violence increases the likelihood by twofold that a young person will be engaged in violence within two years with a higher retaliatory injury risk (88 times).42
LIMITATIONS
The retrospective design relies on existing data, which may be subject to reporting biases or missing information. The study
lacks information on socioeconomic factors, mental health status, and other potential risk factors that could inform more comprehensive prevention strategies. Future research should incorporate these variables and explore the intersectionality of various risk factors to develop more holistic and effective interventions. The lack of specific geographic information is a notable constraint and limits our understanding of geographical patterns and disparities in VRIs across different areas. Moreover, this study only reports trauma activations. Therefore, it likely has an underestimation of the total scope of interpersonal and self-harm violence-related injuries, much of which does not rise to the level of trauma activation at designated hospitals. In addition, individuals who died before hospital arrival may not be fully captured in the dataset, further contributing to the underestimation of the overall burden of violence-related injuries. Future research should incorporate more detailed geographic data, socioeconomic factors, mental health status, and other risk determinants to enable a more comprehensive analysis and targeted prevention strategies.
CONCLUSION
These findings highlight the increasing burden of violence-related injuries in the US, especially among males, racial minorities, and vulnerable age groups. Firearmrelated injuries remain the leading cause of death in both interpersonal violence and self-harm cases. The recent rise in VRIs during the pandemic period emphasizes the need for focused public health interventions addressing firearm safety, violence prevention, and mental health support.
ACKNOWLEDGMENTS
We thank the American College of Surgeons Trauma Quality Programs.
Address for Correspondence: Ayman El-Menyar, MD, Hamad Medical Corportation, Trauma and Vascular Surgery, Hamad General Hospital, PO Box 3050, Doha, Qatar. Email: aymanco65@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 El-Menyar et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. World Health Organization. Preventing injuries and violence: an overview. 2022. Available at: https://www.who.int/publications/i/
item/9789240047136. Accessed February 28, 2024.
2. World Health Organization. Injuries and violence. 2024. Available at: https://www.who.int/news-room/fact-sheets/detail/injuri es-andviolence. Accessed February 28, 2024.
3. Chapman AL, Dixon-Gordon KL. Emotional antecedents and consequences of deliberate self-harm and suicide attempts. Suicide Life Threat Behav. 2007;37(5):543-52.
4. Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). Available at: https://www.cdc.gov/injury/wisqars/. Accessed February 28, 2024.
5. Sumner SA, Mercy JA, Dahlberg LL, et al. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314(5):478-88.
6. Peterson C, Miller GF, Barnett SB, et al. Economic cost of injury — United States, 2019. Morb Mortal Wkly Rep. 2021;70: 1655-9.
7. Monuteaux MC, Fleegler EW, Lee LK. A cross-sectional study of emergency care utilization and associated costs of violent-related (assault) injuries in the United States. J Trauma Acute Care Surg. 2017;83(2):310-5.
8. Small Arms Survey. A gendered analysis of violent deaths. 2016. Available at: https://www.smallarmssurvey.org/resource/genderedanalysis-violent-deaths-research-note-63. Accessed February 28, 2024.
9. Davis D, Santo L. Emergency Department Visit Rates for Assault: United States, 2019-2021. 2023. Available at: https://www.cdc.gov/ nchs/data/databriefs/db481.pdf. Accessed February 28, 2024.
10. Carmichael H, Steward L, Peltz ED, et al. Preventable death and interpersonal violence in the United States: Who can be saved? J Trauma Acute Care Surg. 2019;87(1):200-4.
11. Centers for Disease Control and Prevention. National Center for Health Statistics Mortality Data on CDC WONDER. 2023. Available at: https://wonder.cdc.gov/mcd.html. Accessed January 25, 2025.
12. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
13. Krug EG, Mercy JA, Dahlberg LL, et al. The world report on violence and health. Lancet. 2002;360(9339):1083-8.
14. Mercy JA, Hillis SD, Butchart A, et al. (2017). Interpersonal violence: global impact and paths to prevention. In: Mock CN, Nugent R, Kobusingye O & Smith KR (Eds.), Disease control Priorities, 3rd ed: Vol 7. Injury Prevention and Environmental Health (first pagelast page of chapter). Washington DC: The International Bank for Reconstruction and Development / The World Bank.
15. Centers for Disease Control and Prevention. Injuries and Violence Are Leading Causes of Death. 2023. Available at: https://wisqars.cdc. gov/animated-leading-causes/. Accessed January 16, 2025.
16. Khurana B, Loder RT. Injury Patterns and Associated Demographics of Intimate Partner Violence in Older Adults Presenting to US Emergency Departments. J Interpers Violence. 2022;37(1718):NP16107-29.
17. Khurana B, Hines DA, Johnson BA, et al. Injury patterns and associated demographics of intimate partner violence in men
El-Menyar et al.
presenting to US emergency departments. Aggress Behav. 2022;48(3):298-308.
18. Meyer CH, Holstein R, McGeoch C, et al. Patterns of firearm related injury in the elderly: a single institution analysis. Injury. 2024;55(5):111307.
19. Hiranniramol K, Moran V, Israel H, et al. Characteristics of adult patients for violence-related injuries presenting to a Level 1 trauma center in Midwest United States. Hosp Top. 2023;101(4):352-9.
20. Stockl H, Devries K, Rotstein A, et al. The global prevalence of intimate partner homicide: a systematic review. Lancet. 2013;382(9895):859-65.
21. Gitto L, Tarozzi I, Arunkumar P. Female homicide victims in Cook County, Illinois: a retrospective review. Am J Forensic Med Pathol. 2024;45(1):15-9.
22. Carter PM, Walton MA, Roehler DR, et al. Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics. 2015;135(5):805-15.
23. Dowd B, Khan I, Boneva D, et al. Self-inflicted gun violence injuries epidemic in the United States: a closer look at the nation’s well-being. Am Surg. 2020;86(3):208-12.
24. Young LJ, Xiang H. US racial and sex-based disparities in firearm-related death trends from 1981-2020. PLoS One. 2022;17(12):e0278304.
25. Marineau LA, Uzzi M, Buggs SA, et al. Risk and protective factors for firearm assault injuries among Black men: a scoping review of research. Trauma Violence Abuse. 2024;25(3):2468-88.
26. Tennakoon L, Hakes NA, Knowlton LM, et al. Traumatic injuries due to interpersonal and domestic violence in the United States. J Surg Res. 2020;254:206-16.
27. Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266-73.
28. Bell TM, Qiao N, Jenkins PC, et al. Trends in emergency department visits for nonfatal violence-related injuries among adolescents in the United States, 2009-2013. J Adolesc Health. 2016;58(5):573-5.
29. Hoefer L, Camarena A, Twohig K, et al. Rising mortality in pediatric self-inflicted firearm trauma associated with distinct anatomic injury J Surg Res. 2023;283:259-65.
30. DiVietro S, Hunter AA, Schwab-Reese L, et al. Disparities among pediatric firearm suicides in the United States: an analysis of the National Violent Death Reporting System, 2014 to 2018. J Interpers Violence. 2024;39(13-14):3308-19.
31. Shannon B, Abasilim C, Friedman LS. Trends in assault-related hospitalizations during the SARS-CoV-2 pandemic. Injury. 2023;54(4):1106-12.
32. Stevens J, Pickett K, Kaar J, et al. The impact of the COVID-19 pandemic on pediatric firearm injuries in Colorado. J Pediatr Surg. 2023;58(2):344-9.
33. Risinger WB, Pera SJ, Bhutiani N, et al. A new pandemic and an old epidemic: the impact of COVID-19 and gun violence as measured by years of potential life lost in a US city. Surgery. 2022;172(5):1555-62.
34. Donnelly M, Kuza C, Sargent B, et al. Firearm violence surrounding the COVID-19 pandemic: a reopening phenomenon. J Surg Res. 2023;285:168-75.
35. Brooke BS, Efron DT, Chang DC, et al. Patterns and outcomes among penetrating trauma recidivists: It only gets worse. J Trauma. 2006;61(1):16-9.
36. McCoy AM, Como JJ, Greene G, et al. A novel prospective approach to evaluate trauma recidivism: the concept of the past trauma history J Trauma Acute Care Surg. 2013;75(1):116-21
37. El-Menyar A, Goyal P, Samson D, et al. Risk factors and predictors of violence: insights from the emergency department at a Level 1 trauma center in the USA. J Public Health (Oxf). 2023;45(1):245-58.
38. Nunn J, Erdogan M, Green RS. The prevalence of alcohol-related trauma recidivism: a systematic review. Injury. 2016;47(3):551-8
39. Nygaard RM, Marek AP, Daly SR, et al. Violent trauma recidivism: Does all violence escalate? Eur J Trauma Emerg Surg. 2018;44(6):851-8.
40. Schwartz DS, Thompson J, Locrotondo T, et al. Initial acuity of firearm injuries in the United States: Are civilian injuries similar to combat casualty statistics? Intern Emerg Med. 2022;17(3):857-63.
41. Sakran JV, Lunardi N. Reducing firearm injury and death in the United States. Adv Surg. 2022;56(1):49-67.
42. Cunningham R, Knox L, Fein J, et al. Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med. 2009;53(4):490-500.
Nerve Blocks for Hip Fractures in the Emergency Department: An Opportunity for Growth
Robert Allen, MD*
Dainis Berzins, DO†
Lydia Koroshetz, MD‡
Chun Nok Lam, PhD‡
Melissa Wilson, PhD§
Mayra Cruz, MD*
Jennifer Huang, MD*
Dana Sajed, MD*
Thomas Mailhot, MD*
Section Editor: Robert R. Ehrman, MD
Los Angeles General Medical Center, Department of Emergency Medicine, Los Angeles, California
Cedars Sinai Medical Center, Department of Emergency Medicine, Los Angeles, California
University of Southern California, Keck School of Medicine, Department of Emergency Medicine, Los Angeles, California University of Southern California, Keck School of Medicine, Department of Population and Public Health Sciences, Los Angeles, California
Submission history: Submitted February 13, 2025; Revision received May 5, 2025; Accepted May 28, 2025
Electronically published September 25, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.43500
Introduction: Hip fractures are a common reason for presentation to the emergency department (ED) and are associated with significant morbidity. Nerve blocks have emerged as a safe and effective tool to treat pain associated with hip fractures. In this study, we aimed to measure the frequency with which nerve blocks were performed for ED patients with hip fractures. Our secondary aims were to study the demographic and clinical characteristics of patients who received and did not receive a nerve block.
Methods: We performed a retrospective study at a single-center, urban, academic, Level I trauma center. We measured the frequency with which patients received a nerve block. We measured other demographics (age, ethnicity, insurance) and clinical data (comorbidities, Emergency Severity Index, National Emergency Department Overcrowding Scale, and hip fracture type). Lastly, we measured the types of nerve block performed, who performed the nerve block, and any associated complications.
Results: Overall, 17% (36/209) of the studied patients and 14% (36/257) of all patients with an acute hip fracture received a nerve block. Patients who were cared for by ultrasound (US) fellowshiptrained physicians were more likely to receive a nerve block compared to patients cared for by nonUS fellowship-trained physicians (20/35 vs 16/174; P-value < .001).
Conclusions: Nerve blocks were performed for a minority of patients presenting with an acute hip fracture. Patients who are cared for by ultrasound fellowship-trained physicians may be more likely to receive a nerve block than patients cared for by non-ultrasound fellowship-trained physicians in the emergency department. [West J Emerg Med. 2025;26(5)1478–1484.]
INTRODUCTION
Hip fractures are commonly diagnosed in the emergency department (ED). Such fractures are extremely painful and are associated with significant morbidity.1,2 Emergency physicians caring for such patients are primarily tasked with providing appropriate analgesia, which is associated with improved outcomes postoperatively.3 However, traditional analgesic
management, often involving intravenous opioids, is associated with oligoanalgesia, delirium, and hypoxia.4,5 The peripheral nerve block is a novel approach that, compared to standard care, has been found to reduce pain, reduce opioid use, encourage earlier mobilization, and decrease the incidence of pneumonia.6 Femoral nerve blocks and fascia iliaca compartment blocks in the ED are both feasible and
associated with improved outcomes.7-9 More recently, the pericapsular nerve group (PENG) block has shown promise as an alternative nerve block to treat hip fractures.10-13 Professional organizations within the specialties of emergency medicine, orthopedics, trauma surgery, and anesthesia now endorse the use of peripheral nerve blocks.14-17 Despite this endorsement, the frequency with which they are performed in the ED is unknown. Additionally, it is currently poorly understood what factors influence whether a patient receives a nerve block in the ED.
In this study we aimed to assess 1) the frequency with which nerve blocks are performed for patients with hip fractures in the ED and 2) the demographic and clinical characteristics of patients who received and did not receive nerve blocks. Lastly, we describe the characteristics of the nerve blocks performed.
METHODS
We conducted a retrospective, cohort study to describe the characteristics and experience of patients who presented to the ED at Los Angeles General Medical Center and were diagnosed with hip fractures. Los Angeles General Medical Center is an urban, academic, tertiary-care center serving the County of Los Angeles, with an annual census of over 150,000 ED visits per year. The primary outcome was to measure the proportion of patients who received a nerve block for treatment of hip fracture. The secondary outcomes were to report the demographic and clinical characteristics of patients with hip fractures who received and did not receive a nerve block. Institutional review board approval was granted for the study with a waiver of patient consent.
Inclusion criteria included adult patients (≥ 18 years of age) with an acute hip fracture diagnosed in the ED. Exclusion criteria included patients who were pregnant, incarcerated, had contraindications to receiving a nerve block (intubated patients, patients with an altered mental status, or presence of severe polytrauma), and patients transferred from another ED. (Appendix A)
We followed best practices for chart review as described by Worster et al.18 Blinding of abstractors (DB, LK) was not possible as the two abstractors were study investigators. A list of potentially eligible patients was generated from the International Classification of Diseases, Rev 10, (Appendix B) by an investigator (CL). From this list, the date of ED visit, Emergency Severity Index (ESI) score, National Emergency Department Overcrowding Scale (NEDOCS) score, and insurance were generated using hospital administrative data. Manual data abstraction was performed by two investigators (DB, LK). A coding guide was created prior to data abstraction (Appendix A). Abstractors reviewed notes from emergency physicians, orthopedic consult notes, and admission and discharge notes.
We developed a data abstraction form using REDCap (Research Electronic Data Capture tools hosted at University of Southern California)19 (Appendix C). The data abstraction form was pilot-tested before use. Discussions were held
Population Health Research Capsule
What do we already know about this issue?
Nerve blocks are a safe and effective tool to treat pain associated with hip fractures in the emergency department.
What was the research question?
We measured the frequency with which nerve blocks were performed for ED patients with a hip fracture.
What was the major finding of the study?
Overall, 17% (36/209) of the studied patients and 14% (36/257) of all patients with an acute hip fracture received a nerve block.
How does this improve population health?
The nerve block is an opioid-sparing method to treat pain. Future studies are needed to help improve the rate of nerve blocks performed in the ED.
throughout data abstraction to address questions. Both reviewers received the same random set of 10% study cases for initial training. We calculated inter-rater reliability (Cohen kappa) upon chart review of the first 5% of cases, and the lead author met with both reviewers to discuss data field abstraction methods to synchronize the approach. Upon completing the second 5%, we achieved a kappa value of greater than 0.8. The reviewers then received an evenly distributed set of remaining cases to review independently. For records that were found to be in disagreement from the first 10%, the lead author conducted chart review separately to serve as the tiebreaker.
Patients were first screened for inclusion and exclusion criteria. We excluded patients if the hip fracture was not acute (based on either radiology interpretation or emergency physician documentation.) Included patients had the following data abstracted: age; sex; ethnicity/race; comorbidities; hip fracture type; arrival method; name of emergency clinician; whether or not a nerve block was performed; who performed the nerve block; type of nerve block performed; and nerve block complication(s). The ESI and NEDOCS scores and insurance information were obtained from hospital administrative data by a third investigator (CL). The NEDOCS score is a validated measurement, collected every two hours at our hospital to monitor ED crowding.20,21 We used this as a surrogate measure to correlate with the subjective sense of how busy the ED may have felt to the emergency clinician at the time. Nerve block complications were determined by
reviewing the ED and admission notes (Appendix A.)
We determined who performed the nerve block by reviewing physician notes, procedure notes, and nursing documentation. A block was considered to be performed by a resident if both a resident and an attending were present for the procedure. This was done to separate blocks that were done independently by an attending. At our institution, most patients are treated primarily by residents, with attendings acting in a supervisory role. Attendings are required to be present for all ultrasound (US)-guided nerve blocks. We defined US-fellowship trained physicians to include fellows currently in an US fellowship and attending physicians who had completed an US fellowship or received Advanced EM Ultrasonography certification. Our center does not have an established protocol for performing nerve blocks in the ED for hip fracture patients. and the decision to perform a block is made by the treating emergency physician. In our experience, all nerve blocks in our department are performed with US guidance, typically using bupivacaine without epinephrine. Our institution does not have a formal nerve block-training program; however, residents and faculty are exposed to periodic didactic and hands-on training as part of the residency educational curriculum.
A priori, we anticipated, based on prior history, that approximately 480 patients would be available for analysis (20 patients/month over 24 months), with 10-20% estimated to receive blocks. Thus, assuming the block prevalence to be 20%, we calculated the precision with which we could estimate the prevalence of blocks within hip fractures, with 95% confidence to be between 16-24%. Demographics and clinical characteristics are reported as the median or count with frequency. We reported characteristics for the total population of patients with hip fractures, patients who received nerve blocks, and patients who did not receive nerve blocks. We used the Wilcoxon rank-sum test to test numeric variables and chi-square and Fisher exact tests to compare demographic and clinical factors by nerve block performed. All analyses were performed in Stata 15 (StataCorp, LLC, College Station, TX) with set to 0.05.
RESULTS
A total of 347 patients were reviewed for eligibility from August 1, 2021–July 31, 2023 (Figure). There was excellent agreement among reviewers from the first 10% of the sample (K = 0.93). We excluded 138 patients: 90 did not have an acute fracture; 18 were transferred from another facility; and 36 had a contraindication to receiving a nerve block. (Some patients had more than one exclusion criteria.) A total of 36 patients received a nerve block, representing 17% (36/209) of the studied patients and 14% (36/257) of all patients with an acute hip fracture. Demographics were similar for those patients who received a nerve block and those who did not (Table 1). We found no correlation between the likelihood of receiving a block and patient’s age, sex, ethnicity, language, or

Figure. Flow diagram of how patients were chosen to receive nerve blocks for acute hip fractures.
*Some patients had multiple exclusion criteria, which is why the value does not total 48.
**Represents 17% of patients studied and 14% of total patients with an acute hip fracture.
insurance.22 The median age of all patients in the study was 77.1 years old. Approximately two-thirds of the patients were female. Over 50% of patients in our study were Hispanic/ Latino and did not speak English, reflecting the overall demographic of our medical center. Medicare and Medi-Cal were the most common insurances of patients, representing 87.1% of all included patients.
Patients who were cared for by US fellowship-trained physicians were more likely to receive a nerve block compared to patients cared for by non- US fellowship-trained physicians (P-value < .001) (Table 2). Ultrasound fellowshiptrained physicians performed 55.6% of total nerve blocks. Likewise, patients who did not receive a block were more likely to be cared for by non-US fellowship-trained physicians (91.3%) than by US fellowship-trained physicians (8.7%). A total of 20 blocks were performed by two full-time US fellowship-trained physicians, three part-time US fellowshiptrained physicians, and three US fellows. There were 63 nonUS fellowship-trained full/part-time physicians involved in the study. Other clinical characteristics were similar between patients who did and did not receive nerve blocks (Table 2). The fascia iliaca block was the most commonly performed nerve block followed by the PENG block (Table 3). Most nerve blocks were performed by emergency medicine residents on clinical shifts, followed by emergency medicine residents on an US rotation, and US fellows.
One potential complication was noted in a patient who received a nerve block and suffered a ventricular fibrillation arrest. However, the arrest occurred hours after the nerve block and was thought by the caring physicians to have been caused by hypoxia after receiving intravenous fentanyl.
*Chi-square, Fisher exact, and Wilcoxon rank-sum tests were performed. IQR, interquartile range.
Although local anesthetic toxicity can cause ventricular arrhythmias, this was thought to be less likely in this case, given the time course and a more likely explanation.
DISCUSSION
Despite strong evidence supporting peripheral nerve blocks for hip fractures, we found that at our Level I academic trauma center, nerve blocks were performed in a minority of patients. While our findings are limited to our single center, we believe our research should lead to future study to measure the rate of nerve blocks at other centers. We believe this to be an important opportunity for growth within our medical center and the greater emergency medicine community. Our findings are particularly noteworthy given it was conducted at an academic institution where most patients are cared for primarily by residents. We believe residents should be supported to perform nerve blocks in the expectation that they can continue this practice after completing their training.
Patients receiving nerve blocks were more likely to have been treated by US fellowship-trained physicians, despite the fact that US fellowship-trained physicians only represented a minority of the total treating physicians in our study. These results may not be surprising given that nerve blocks are commonly performed using US. A survey conducted in 2022 found that 100% of academic EDs with US fellowships perform US-guided nerve blocks at their institutions.22 However, the rate of nerve blocks performed at centers without an US fellowship is still uncertain. Future initiatives to improve the rate of nerve blocks may consider focusing efforts on increasing the rates of nerve blocks performed by
non-US fellowship-trained physicians.
There are multiple variables that may serve as potential facilitators and barriers to performing a nerve block. While we did not find any statistical significance other than the presence of an US fellowship-trained physician, it is possible and likely that there were other contributing factors. Prior studies have found that patients at extremes of ages and non-White patients receive different pain treatment modalities.23-25 Our study was underpowered to explore differences in demographic characteristics. Future studies of larger sample sizes could incorporate this potential factor.
In our study we did not consider the age or experience of the attending physician. Given that US-guided nerve blocks are a relatively newer skill, it may be possible that clinicians who more recently completed residency training may be more familiar with and, therefore, more likely to perform nerve blocks, compared to clinicians who completed residency earlier. This hypothesis could be tested in future studies.
Additionally, based on clinical experience, periods of larger patient volume may influence the likelihood of performing a nerve block. The ED census may be influenced by a variety of factors such as time of day, day of the week, and seasonal variation. Therefore, when an ED is “busier,” clinicians may feel that they have less time to perform a nerve block, which may be considered an optional procedure. While our study was not powered to detect differences in this predictor, it is possible that a larger study could test this hypothesis.
Although the fascia iliaca block was the most commonly performed block during the study time frame, it is possible
Table 1. Demographics of all patients with a hip fracture, stratified by those with and without a nerve block.
Table 2. Clinical characteristics of all patients with a hip fracture, stratified by those with and without a nerve block.
Total Population (N = 209)
Nerve Block (N = 36)
Nerve Block (N = 173)
US Fellowship-trained Physician Present
Hip Fracture type
Intertrochanteric
Femoral Neck
Femoral head
Greater trochanter
Lesser trochanter
Subtrochanteric
Heart Failure
Kidney Disease
*Chi-square, Fisher exact, and Wilcoxon rank-sum tests were performed. ESI, Emergency Severity Index; NEDOCS, National Emergency Department Overcrowding Scale; EMS, emergency medical services; IQR, interquartile range.
this may not reflect current or future practice. The PENG is a newer block, first described in the ED literature in 2020.11 It is, therefore, possible that as physicians become familiar with this block it may be used more frequently. A 2024 metaanalysis found that the PENG block may have better efficacy than both femoral and fascia iliaca blocks.10 Whereas the femoral nerve block was once preferred, none of the patients in our study received this block, perhaps reflecting the practice of our institution. Farrow et al in their review of nerve blocks in a community teaching hospital, similarly found a higher percentage of fascia iliaca blocks compared to PENG blocks, without any femoral nerve blocks performed.26 Likewise, Goldsmith et al in their multicenter observational registry, found fascia iliaca/femoral nerve block to be the most commonly performed nerve block.27 We would hypothesize that other centers and different time frames of studies may show different preferences for nerve blocks.
LIMITATIONS
Our study had multiple limitations. First, our study was limited by its retrospective design. It is possible, albeit unlikely, that patients received a nerve block without
documentation. It is standard practice that any procedure is documented in the electronic health record. As a safeguard, we reviewed all physician and nursing notes to determine whether a nerve block had been performed. Likewise, it is possible that an US fellowship-trained physician was present for the procedure but not documented. We chose a conservative approach of only stating that an US fellowship-trained physician was present if they were one of the treating physicians or if it was documented that they were present for the block. If US fellowship-trained physicians were present at blocks but not documented, this would further strengthen the statistically significant difference found in our study.
Second, we did not report pain scores of patients who received nerve blocks. This was due to the retrospective nature of our study. Third, the outcomes from our single-center study may likely differ from the outcomes at other institutions. Our medical center is an academic Level I trauma center where most patients are cared for by residents. Centers without residents or US fellowship-trained physicians, such as community hospitals, may perform fewer nerve blocks, especially if physicians are less familiar with the procedure. Future studies could consider studying the rate of nerve blocks
Table 3. Description of the type of nerve blocks performed, who performed the nerve block and any associated complications. Variable
Nerve block
Fascia Iliaca
PENG
Femoral
Not specified 27 (75) 7 (19.4) 0 (0) 2 (5.6)
Who performed the block?
ED Resident
ED Attending
ED US
ED
Complications
(77.7)
(5.6)
(16.7)
(2.8)
(97.2)
PENG, pericapsular nerve group; ED, emergency department; US, ultrasound.
for hip fractures, especially across different types of medical centers. Furthermore, the demographics of our patients likely differ from other centers. Future study could explore whether there are differences in the rate of nerve blocks performed in centers with different demographics. Lastly, it is possible that our study was too small to consider possible confounders in the analysis.
CONCLUSION
Our single-center, academic, retrospective study found that nerve blocks were performed in a minority of patients with hip fractures. Patients who are cared for by ultrasound fellowship-trained physicians may be more likely to receive a nerve block than patients cared for by non-ultrasound fellowship-trained physicians in the emergency department.
AVAILABILITY OF DATA AND MATERIALS
Data is available upon request from the corresponding author.
REFERENCES
1. Brauer CA, Marcelo Coca-Perraillon, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:15731579.
2. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458-1460.
3. Morrison RS, Magaziner J, Mclaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain 2003;103:303-311.
4. Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci. 2003;58:76-81.
5. Thompson C, Brienza VJM, Sandre A, et al. Risk factors associated with acute in-hospital delirium for patients diagnosed with a hip fracture in the emergency department. CJEM. 2018;20:911–919.
6. Guay J, Kopp S. Peripheral nerve blocks for hip fractures in adults. Cochrane Database of Sys Rev. 2020;11:CD001159.
7. Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound‐guided three‐in‐one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20:584-591.
8. Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients. Anesthesiology 2007;106:773-778.
9. Unneby A, Svensson O, Gustafson Y, et al. Femoral nerve block in a representative sample of elderly people with hip fracture: A randomised controlled trial. Injury. 2017;48:1542-1549.
10. Hayashi M, Yamamoto N, Kuroda N, et al. Peripheral nerve blocks in the preoperative management of hip fractures: a systematic review and network meta-analysis. Ann Emerg Med. 2024;83:522-538.
11. Luftig J, Dreyfuss A, Mantuani D, et al. A new frontier in pelvic fracture pain control in the ED: successful use of the pericapsular nerve group (PENG) block. Am J Emerg Med. 2020;38:2761.e5-9.
12. Sahoo S, Sahoo NK, Hansda U, et al. Ultrasound-guided pericapsular nerve block compared with IV opioids in hip injuries: a randomised controlled trial. Am J Emerg Med. 2024;81:99-104.
Address for Correspondence: Robert Allen, MD, Los Angeles General Medical Center, Department of Emergency Medicine, 1200 N State St, Los Angeles, CA 90033. Email: rallen3@dhs. lacounty.gov.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Allen et al. This is an open access article distributed in accordance with the terms of the Creative Commons
Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
13. Fahey A, Cripps E, Ng A, et al. Pericapsular nerve group block for hip fracture is feasible, safe and effective in the emergency department: a prospective observational comparative cohort study. Emerg Med Australas. 2021;34:884-891.
14. American College of Surgeons. Best Practice Guidelines for Acute Pain Management in Trauma Patients. 2020. Available at: https://www. facs.org/media/exob3dwk/acute_pain_guidelines.pdf. Accessed October 15, 2024.
15. American College of Emergency Physicians. Ultrasound-Guided Nerve Blocks. American College of Emergency Physicians. 2021. Available at:https://www.acep.org/patient-care/policy-statements/ultrasoundguided-nerve-blocks. Accessed October 15, 2024.
16. Griffiths R, Babu S, Dixon P, et al. Guideline for the management of hip fractures 2020. Anaesthesia. 2020;76:225-237.
17. O’Connor MI, Switzer JA. AAOS clinical practice guideline summary: management of hip fractures in older adults. J Am Acad Orthop Surg
2022;30:e1291–e1296.
18. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45:448-451.
19. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
20. Hwang U, Mccarthy ML, Aronsky D, et al. Measures of crowding in the emergency department: a systematic review. Acad Emerg Med 2011;18:527-538.
21. Weiss SJ, Derlet R, Arndahl J, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS). Acad Emerg Med 2004;11:38-50.
22. Goldsmith AJ, Brown J, Duggan NM, et al. Ultrasound-guided nerve blocks in emergency medicine practice: 2022 updates. Am J Emerg
Med. 2024;78:112-119.
23. Goyal MK, Kuppermann N, Cleary SD, et al. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr. 2015;169:996-1002.
24. Goyal MK, Johnson TJ, Chamberlain JM, et al. Racial and ethnic differences in emergency department pain management of children with fractures. Pediatrics. 2020;145:e2013370.
25. Brown JC, Klein EJ, Lewis CW, et al. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42:197-205.
26. Farrow RA, Shalaby M, Newberry MA, et al. Implementation of an ultrasound-guided regional anesthesia program in the emergency department of a community teaching hospital. Ann Emerg Med 2024;83:509-518.
27. Goldsmith A, Driver L, Duggan NM, et al. Complication rates after ultrasonography-guided nerve blocks performed in the emergency department. JAMA Netw Open. 2024;7:e2455847.
Expert Guideline
Acute Care of Patients with Moderate Respiratory Distress: Recommendations from an American College of Emergency Physicians Expert Panel
Christopher W. Baugh, MD, MBA*
Jim F. Neuenschwander, MD†
Jesslyn Lenox, MHA, RRT-NPS, AE-C‡
Jennifer Hoh, PharmD, BCCCP§
Kara Ward, MD||#
Sara Muramoto, MD¶
John Casey, DO, MA†
Antonio Anzueto, MD**
Hajirah Ishaq, DO, MS††
Jared Mount, BS‡‡
Peter M. DeBlieux, MD§§
Brigham and Women’s Hospital, Department of Emergency Medicine, Boston, Massachusetts
OhioHealth Doctors Hospital, Department of Emergency Medicine, Columbus, Ohio
South Shore Hospital, Pulmonary Function Lab and Neurodiagnostics, Weymouth, Massachusetts
University of Louisiana at Monroe, Department of Emergency Medicine, Monroe, Louisiana
Tammany Health System, Division of Pulmonary & Critical Care, St Covington, Louisiana
Robotic Critical Care Services
Louisiana State University’s Spirit of Charity Emergency Medicine Residency Program, New Orleans, Louisiana
UT Health San Antonio, South Texas Veterans Health Care System, Division of Pulmonary Medicine/ Critical Care, San Antonio, Texas
Indiana University School of Medicine, Department of Emergency Medicine, Indianapolis, Indiana
Ohio University Heritage College of Osteopathic Medicine, Department of Medical Education, Athens, Ohio
University Medical Center New Orleans, Department of Emergency Medicine, New Orleans, Louisiana
Section Editor: Tom Benzoni
Submission history: Submitted February 18, 2025; Revision received May 13, 2025; Accepted May 23, 2025
Electronically published September 27, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.43539
Introduction: Patients with respiratory distress are frequently encountered in the emergency department (ED). Efforts to assess, initiate treatments, and stabilize these patients require a systematic and rapid response. Emergency physicians need a comprehensive and efficient approach for evaluating, treating, and managing patients presenting to the ED with moderate respiratory distress.
Methods: The American College of Emergency Physicians convened an expert panel of academic and community emergency physicians, critical care specialists, respiratory therapists, hospitalists, and pharmacists to develop and subsequently disseminate consensus recommendations regarding the diagnosis and treatment of patients with moderate respiratory distress presenting to the ED.
Results: A digital tool using a consensus-based framework was developed to aid emergency clinicians in diagnosing and caring for patients with moderate respiratory distress. The tool can be employed at each step in the diagnostic and treatment process.
Conclusion: The evidence-based tool is a practical and freely available bedside instrument for emergency clinicians to diagnose and treat patients with moderate respiratory distress. Further studies are needed to examine the effectiveness of this approach. [West J Emerg Med. 2025;26(5)1485–1494.]
INTRODUCTION
Respiratory distress or shortness of breath represent the third most common reason for visiting the emergency department (ED) in the United States, with 5,918,000 visits in 2021.1 Shortness of breath is a common manifestation of a wide array of primary pulmonary and respiratory tract illnesses, as well as other potentially life-threatening conditions, such as acute coronary syndrome, pulmonary embolism, cardiac tamponade, severe anemia, toxic metabolic disturbances, and many others.2 Emergency physicians must manage these patients with limited time and information. They also initiate rapid assessment, diagnosis, and treatment to stabilize and begin reversing life-threatening pathophysiology amid increased stressors such as ED boarding and patients with higher morbidity.3 Frequent reassessment, adjustments to new data, and observed patient response to therapies are the mainstays of ED care for this patient population.
For emergency physicians faced with the challenge of caring for patients with respiratory distress, many resources, such as specialty society guidelines, are available for disease-specific assessment and treatment.4 Few resources are readily available for the initial care of patients with undifferentiated respiratory distress, especially those with moderate symptoms and elevated risk.5–7 Often, immediate aggressive maneuvers, such as rapid sequence intubation, are not indicated. Developing and disseminating digital tools easily accessed via smartphone or desktop computer, and explicitly designed to support real-time clinical care, is needed.8 Lastly, many authoritative guidelines are rarely updated due to rigorous and time-consuming processes for evidence review and consensus generation. This timing results in a delay between the time when innovative and emerging approaches, such as high-flow nasal cannula, are indicated for use and when they are subsequently incorporated into expert recommendations.
Expert panels can be convened to address challenges in clinical practice that students, physicians, nurses, physician assistants, and nurse practitioners may face and provide consensus recommendations. The initial assessment and optimal diagnostic and therapeutic approach to patients with respiratory distress in the ED can be complex and time sensitive. The American College of Emergency Physicians (ACEP) expert panel is a mechanism to address the diagnosis and management of moderate respiratory distress in the ED by providing a practical, consensus-based guide via an online tool and smartphone app at the point of care.
METHODS
Study Design
An expert panel to develop a consensus-based decision tool for emergency clinicians was convened by ACEP. Selected panel members conducted a literature review focusing on terms such as “respiratory distress” to examine recent ( ≤ 5 years) publications and specialty-society
Population Health Research Capsule
What do we already know about this issue? Patients frequently present to the ED with undifferentiated moderate respiratory distress.
What was the research question?
We convened an expert panel and developed a digital tool to assist clinicians’ bedside assessment of respiratory distress in an efficient and evidence-based manner.
What was the major finding of the study?
We emphasize a rapid yet thorough initial history and exam to guide diagnosis, initiate targeted treatments, and select the most appropriate disposition for this target patient population.
How does this improve population health?
As emergency clinicians face challenges to assess and treat complex patients, digital tools like the one we developed and implemented can help improve care for higher risk populations.
guidelines involving the approach to respiratory distress in the ED. The panel sought more recent literature to reflect the current and emerging science related to the target population. When possible, definitions and recommendations reflect study criteria and treatment processes. Otherwise, the expert panel sought to standardize definitions and processes. The panel participated in four virtual rounds of questioning to make recommendations using a modified Delphi rounds process to reach a consensus.9 Statements were discussed extensively during the virtual meetings and then serially modified based on discussions. The final expert panel recommendations represented consensus (defined as majority agreement with final adjudication by co-chairs) and majority opinions. This project relied on publicly available sources and was framed as a quality improvement project exempt from institutional review board oversight.
The definition of moderate respiratory distress is intricate and not easily defined. Our recommendations defined moderate respiratory distress as “a patient who requires more than basic respiratory care or is at risk of deterioration.” For example, this definition would include a patient with a respiratory rate > 24 breaths per minute, with or without hypoxia, and with the use of accessory muscles of respiration.
Setting
The multidisciplinary expert panel, which was diverse in geography and practice settings, was convened virtually between January–July 2024.
Selection of Participants
The American College of Emergency Physicians selected the expert panel; the chosen co-chairs Jim F. Neuenschwander and Peter M. DeBlieux then selected additional panelists. Criteria for selection included individuals with direct personal clinical experience in treating patients with respiratory distress in the ED, prior contributions to ACEP expert panels and/or academic contributions, and diverse clinical practice settings within the group. Clinical backgrounds included emergency medicine, critical care, respiratory therapy, pharmacy, and hospital medicine. The final panel consisted of three academic emergency physicians, two community emergency physicians, one ED pharmacist, one respiratory therapist, and one hospitalist, with panelists representing a broad geographic distribution across the US (eg, Southwest, South, Midwest, Northeast).
RESULTS
The ACEP moderate respiratory distress emergency medicine pointof care (emPOC) tool was developed to communicate the main steps in the evaluation, treatment, and disposition of patients presenting to the ED with moderate respiratory distress. The tool is available on the ACEP website and as a smartphone app for Apple and Android devices.
History and Physical Exam
Care begins with the initial assessment, which includes obtaining a history of present illness and performing a physical examination. The history may be obtained from the patient, emergency medical services, family, or other historians to assist with differential diagnosis, initial testing, and treatment strategy. Table 1a outlines the key elements of the history that should be obtained for patients presenting to the ED with moderate respiratory distress. In parallel with obtaining the patient’s history, a physical examination should begin immediately as the patient is assessed. We outline the key exam elements in Table 1b.
Testing
After the initial evaluation, the differential diagnosis generated from the encounter will drive a diagnostic strategy. Testing falls into three broad categories: laboratory studies; imaging studies; and other testing. We outline the key diagnostic considerations in Table 2, which may be modified by local resource availability and the evolution of the differential diagnosis as more information is gathered over the patient’s ED course.
Acute Care of Patients with Moderate Respiratory Distress
Table 1a. History elements for patients with moderate respiratory distress.
• Dyspnea at rest and with ambulation
• Chest pain quality, including pleuritic pain
• Increased sputum production
• Fever
• Heart failure
• Orthopnea
• Paroxysmal nocturnal dyspnea
• Cough
• Peripheral edema
• Fatigue
• Altered mental status
• Weakness
• Smoking/vaping use
• Chronic lung disease (e.g., chronic obstructive pulmonary disease, interstitial lung disease, pulmonary fibrosis)
• Anemia
• Asthma
• Increased sputum/color/production/volume
• Current oxygen requirement
• Prior intubation or known difficult airway
• Recent travel (e.g., elevation, exposure, pulmonary embolism)
• Known infectious contacts
• Prior personal or family history of venous thromboembolism
• Terminal diagnosis/condition
• Exogenous estrogen use
• Hemoptysis
• Hospitalizations
• Trauma/surgery (e.g., fat emboli, rib fractures, pulmonary contusion, flail chest)
• Dysphagia/severe reflux
• Environmental exposure (e.g., carbon monoxide, asbestos)
• Congenital anomalies (e.g., Marfan, cystic fibrosis, Ehlers-Danlos)
• Cancer
• Inflammatory (e.g., lupus, rheumatoid arthritis)
• Substance use disorder
• Goals of care
• Pain
• Anxiety
• Immunosuppressed state
Treatment
Treatments should be targeted at the clinical scene, addressing the underlying pathophysiology driving the patient’s presentation and helping support their work of breathing to avoid clinical decompensation. Initial maneuvers to re-position the patient, suction the airway, or other immediate interventions may be helpful to improve the
Baugh et al.
Table 1b. Physical examination elements for the patient with moderate respiratory distress.
• Vitals trending, including prehospital
• Tachypnea
• Tachycardia
• Hypotension
• Upper airway exam
• Voice quality
• Abnormal lung exam (e.g., wheezing, rhonchi, crackles)
• Hypoxia
• Tripoding or accessory muscle use
• Mental status
• Abnormal skin exam (e.g., pallor or discoloration, urticarial rash)
• Swallow
• Cough quality
• Grunting, nasal flaring, or abdominal contractions
• Diaphoresis
• Irregular breathing pattern
• Crepitus
• Extremity edema
• Screening for difficult airway assessment and management: (https://www.aliem.com/mnemonics-for-difficult-airway/)
History and physical exam elements for patients presenting to the ED with moderate respiratory distress.
patient’s work of breathing. Frequent reassessments are a critical aspect of the care of this patient population. The goal is to choose the best intervention to match the patient’s current and anticipated status with frequent evaluation of the need for respiratory support escalation or de-escalation.10 As a result, the clinician should proceed with continuous information gathering and optimization of a differential diagnosis, work of breathing, serial vital signs, serial mental status exams, repeat imaging (eg, point-of-care ultrasound), lab result analysis (eg, serial blood gasses), disposition trajectory, evolving goals of care, and delivery of more targeted treatments as the diagnosis becomes clearer.
When using a high-flow nasal cannula, the ratio of oxygenation (ROX) index predicts clinical decompensation and the need for intubation.11–13 The ROX index is the SpO2 (peripheral oxygen saturation)/FIO2 (fraction of inspired oxygen) (%) ratio to respiratory rate (breaths/minute). Values ≥ 4.88 measured at 2, 6, or 12 hours after high-flow nasal cannula initiation are associated with a lower intubation risk, whereas values < 3.85 indicate a high risk of high-flow nasal cannula failure and intubation consideration. Intermediate ROX values should be reassessed serially, 1-2 hours later. We illustrate an algorithm for treating and reassessing patients with moderate respiratory distress in Figures 1a and 1b for the adult and pediatric populations, respectively.14,15
Various respiratory therapies are available in the ED and should match the patient’s needs. Table 3 highlights the key similarities and differences between commonly available respiratory therapies, including nasal cannula, facemask, high-flow nasal cannula, non-invasive ventilation, intubation, and surgical airways. We provide additional detail for each treatment in Figure 2. For some patients, intubation and mechanical ventilation avoidance may be an important consideration, as intubation may increase the risk of peri-intubation complications. These patients may require special ventilation strategies and include examples such as status asthmaticus, severe metabolic acidosis, and untreated pneumothorax.
Medications are an essential component of treatment for most patients in the ED with moderate respiratory distress. Given the broad and variable causes of respiratory distress, we outline key pharmacologic treatments for selected common conditions in Supplement Table 1. This resource is not intended to be exhaustive, and once a specific diagnosis is strongly suspected or confirmed, we recommend that clinicians tailor treatments to best treat specific conditions.
Disposition
Disposition decisions should be made based on the severity of symptoms, concurrent comorbidities, and the social drivers of health that impact a patient’s ability to adhere to a care plan. Patients from the ED will be discharged home, admitted to the hospital (including inpatient or observation status), or admitted to the intensive care unit. Patients who want to focus on symptom control and quality of life can be directed to palliative care or hospice.
Patients with mild-to-moderate symptoms who respond well to initial therapy in the ED and do not require new or additional supplemental oxygen may be suitable for discharge home. Patients who are being considered for discharge home should meet the following additional requirements: able to ambulate without a new significant drop in oxygen saturation or return of presenting symptoms; able to obtain prescribed medications promptly; able to express an understanding of their medications and how to properly take them, patient or caregiver can perform discharge instruction “teach back” and demonstrate proper use of new and existing therapies; able to express understanding of return precautions (ie, worrisome signs and symptoms that warrant a return to the ED), and able to follow up with an outpatient clinic within 1-2 weeks of the ED visit. Discharge instructions should include a written discharge plan that contains a list of newly prescribed medications, including their purpose and directions (eg, frequency and duration), a list of all home medications, including any adjustments or changes, signs or symptoms that would warrant returning to the ED, and clear directions to follow up with a primary care physician or specialist in a specified time frame. For patients who smoke or live with
Baugh
Table 2. Diagnostic approach to the patient with moderate respiratory distress.
General Labs
Complete blood count (CBC) anemia, pneumonia/infections
Comprehensive metabolic panel (CMP)
ketoacidosis (diabetic ketoacidosis [DKA]/starvation ketoacidosis [SKA]/alcoholic ketoacidosis [AKA]), pulmonary edema (cardiorenal effects), electrolytes (cardiac arrhythmia), metabolic acidosis
Point of care blood gas
Targeted Labs
Blood gas: use pulse ox and bicarb on basic metabolic panel (BMP)
Co-oximetry
carbon monoxide, methemoglobinemia
Venous blood gas (VBG)
chronic obstructive pulmonary disease (COPD), asthma, respiratory failure
Brain natriuretic peptide (BNP) heart failure, cardiomyopathy, acute coronary syndrome (ACS)
International normalized ratio (INR) with a history of anticoagulation or coagulopathies
Anti-factor Xa test if actively bleeding
Troponin
acute coronary syndrome (ACS)/pulmonary embolism (PE)/venous thromboembolism (VTE)
D-dimer
PE rule out
Lactate seizure, sepsis
Procalcitonin
pneumonia or other infection
Blood cultures
Nasal swab for viral panel
C-reactive protein (CRP) chronic lung disease
Toxicology
salicylate
alcohol and urine tox
Targeted imaging/studies
Chest x-ray (CXR)
pneumonia, pleural effusion, enlarged cardiac silhouette, widened mediastinum, pneumomediastinum, rib fractures, pneumothorax, subcutaneous air, acute respiratory distress syndrome (ARDS), mass, atelectasis, small inspiratory lung volumes (neuromuscular disease)
Expiratory films for focal air trapping/unilateral wheezing
foreign body, mucous plug
Computed tomography chest with contrast
concern for mediastinal mass or pleural metastases without contrast
pneumonia, ground glass opacities, eval pulmonary nodule/mass seen on x-ray, pulmonary contusions, ARDS, pulmonary edema, rib fractures
Diagnostic testing considerations for patients presenting to the emergency department with moderate respiratory distress.
Table 2. Continued.
CT angiogram (CTA) Chest
PE aortic dissection, trauma
Ventilation/Perfusion (V/Q) scan - hard to interpret with existing pulmonary disease/abnormal CXR
PE
Point of care ultrasound
bedside: pneumonia, pneumothorax, pleural or pericardial effusion, pulmonary edema, cardiac tamponade, right heart strain (PE, right heart failure), left ventricular (LV) function, ability to tolerate fluids, inferior vena cava (IVC), lung windows
Consider Ancillary Testing:
End-tidal CO2 (ETCO2)
waveform analysis for overdose, asthma, and COPD
Electrocardiogram (EKG)
arrhythmia, ACS
Negative inspiratory force (NIF)
neuromuscular disease
Physical exam maneuvers
fluid status
passive leg raise-fluid responsiveness
Diagnostic testing considerations for patients presenting to the emergency department with moderate respiratory distress. ACS, acute coronary syndrome; CO2, carbon dioxide; COPD, chronic obstructive pulmonary disease.
Undifferentiated Respiratory Distress Elevated RR and WOB with SpO2 <92% on maximum supplemental oxygen via standard nasal cannula or facemask that does not meet
Consider escalation Initiate HFNC Flow 50-60
Figure 1. A. Adult moderate respiratory distress algorithm. B. Pediatric moderate respiratory distress algorithm.
†Criteria for immediate intubation include inability to protect the airway, anticipated clinical course, and failure of oxygenation or ventilation despite other treatments (e.g., supplemental oxygen, non-invasive ventilation, or not a candidate for those therapies).
‡The extent and reliability of ROX index validation in children remain limited and variable. Patient care algorithm for adult and pediatric patients presenting to the emergency department with moderate respiratory distress. Lpm, liters per minute; RR, respiratory rate; NIV, noninvasive ventilation; WOB, work of breathing; HFNC, high-flow nasal cannula; SpO2, peripheral oxygen saturation; ROX, ratio of oxygenation; PEEP, positive-end expiratory pressure; FiO2, fraction of inspired oxygen.
**Figure 1B adapted from: Mosier JM, Tidswell M, Wang HE. Noninvasive respiratory support in the emergency department: Controversies and state-of-the-art recommendations. J Am Coll Emerg Physicians Open. 2024;5(2):e13118. doi:10.1002/emp2.13118 and Kwon JW. Highflow nasal cannula oxygen therapy in children: a clinical review. Clin Exp Pediatr. 2020;63(1):3-7. doi:10.3345/kjp.2019.00626.
Table 3. Comparison of respiratory therapies.
Inexpensive, simple Intermediate cost, Increased resource intensity
Expensive, resource intensive No PEEP, No Pressure Support PEEP (Low level) PEEP +/- Pressure Support
Cooperation Not Needed
Patient clears secretions
†Patient participation is required.
Cooperation Needed† Not Needed
Assisted secretion clearance
Respiratory therapy options for patients presenting to the emergency department with moderate respiratory distress.
NC, nasal cannula; Mask, facemask; NRB, nonrebreather; HFNC, high-flow nasal cannula; NIV, non-invasive ventilation; ETT; endotracheal tube; FiO2, fraction of inspired oxygen; PEEP, positive end-expiratory pressure.
**Adapted from Baker K, Greaves T, Fraser JF. How to use humidified high-flow nasal cannula in breathless adults in the emergency department. Emerg Med Australas. 2019 Oct;31(5):863-868. doi: 10.1111/1742-6723.13372. Epub 2019 Aug 6. PMID: 31389171.
someone who smokes, smoking cessation information should be given with the discharge paperwork and discussed at the bedside before discharge.
Patients should be hospitalized if they have a new supplemental oxygen requirement. This includes those who have an increased need for supplemental oxygen above their baseline, advanced lung disease, and/or multiple comorbidities, and those who are otherwise unlikely to do well if discharged home. Additionally, those with a new concurrent condition, such as pneumonia, arrhythmias, heart failure, and sepsis, or who have persistent symptoms despite initial ED treatment and require constant monitoring or titration of ventilatory support, should be hospitalized. Finally, those not meeting the criteria for a safe discharge home, including those with social drivers of health likely to disrupt the discharge plan, should remain until a safe plan is identified. Many hospitals have disease-specific protocols that help emergency clinicians determine patient eligibility for observation vs inpatient care, including using ED observation units and home hospital services. We recommend that clinicians reference their local protocols to help direct patients toward the most appropriate site of care in their institution. Example ED observation protocols can be found on ACEP’s Observation Services Toolkit page.
Based on institution-specific capabilities and policies, consider intensive care unit admission for patients with moderate-to-severe symptoms who require escalating respiratory support, are hemodynamically unstable, are intubated, have severe acid-base disturbances, have a new altered mental status, or other symptoms that necessitate close monitoring. Complex patients who may exceed local capabilities or are better served at a higher resource facility require an interfacility transfer. Finally, patients who want to focus on symptom control and quality of life primarily can be directed to palliative care or hospice.
DISCUSSION
In this paper, we describe our process and consensus
recommendations generated by an ACEP-convened expert panel focused on ED care of patients presenting with moderate respiratory distress. Our recommendations emphasize a rapid yet thorough initial history and exam to create and narrow a differential diagnosis, initiate treatments, and select the most appropriate disposition for this target patient population. The framework is presented as a digital tool, available via smartphone app and desktop computer and designed for real-time accessibility to assist clinicians at the bedside for this challenging patient population.
Prior investigations and tools are overwhelmingly targeted at a specific diagnostic tool or therapy for a disease process. For example, evidence abounds for the roles of point-of-care ultrasound and high-flow nasal cannula for the initial evaluation and treatment of patients with undifferentiated respiratory distress.16–19 Disease-specific guidance for respiratory illnesses such as chronic obstructive pulmonary disease, heart failure, pulmonary embolism, and pneumonia is also available.4,20–22 Alternatively, other resources with a broad approach have not been designed as a tool for real-time clinical support.2,23 As a result, our novel approach of combining broad patient assessment and treatment guidance with a format optimized for bedside use is novel and designed for maximal clinical impact. This combination best reflects the real-world scenario of the initial ED encounter, where the diagnosis is not yet confirmed, and the support of a digital tool may be most helpful.
The role of electronic clinical decision-support tools is rapidly evolving. Following the framework of the five “rights” of clinical decision-support, our moderate respiratory distress tool aims to provide the right information to the right people in the right channel, format, and time in the workflow.24 Evidence is increasing for the use of interactive digital tools at the bedside for high-acuity scenarios, such as pediatric cardiac arrest.25 Enabling prompts for clinicians to gather key information and act quickly with evidence-based interventions has the promise of improving care for vulnerable patients,
Nasal Cannula (NC)
Pros: Comfortable, enables communication, eating & drinking. Well tolerated. Easily travels
Cons: Can be drying without humidification. Cannot provide a lot of oxygen
Indication: Low flow, Low FiO2 %
Flow (Lpm): 0.1→ 6
Oxygen %:
Fixed (f) or Variable (v) 24-40 (v)
Delivery Interface Nasal Cannula
Humidification Possible Simple Face Mask

Pros: Enables communication, easily removed for eating & drinking. Easily travels
Cons: Can be drying. Cannot provide a lot of oxygen. Dangerous at flows <6 Lpm
Indication: Med flow, Low FiO2 %
Flow (Lpm): 6 → 10
Oxygen %:
Fixed (f) or Variable (v) 35-60 (v)
Delivery Interface Face Mask
Humidification No
Aerosol Mask / Face Tent / Trach Mask

Pros: Generally well tolerated. Enables humidification & medication delivery
Cons: Cannot provide a lot of oxygen. Dangerous at flows <6 Lpm
Indication: Med Flow, Med Delivery
Flow (Lpm): 6 → 10
Oxygen %:
Fixed (f) or Variable (v) 35-60 (v)
Delivery Interface Face Mask
Humidification Yes
Non-invasive Ventilation


Pros: Fixed FiO2%. Enables single or bi-levels of pressure delivery. Cons: Requires a seal to deliver pressure, can cause skin damage. Inhibits communication. Can be very drying.
Indication: OSA, Augmentation of Oxygenation Support (CPAP), Ventilation Support (BiPAP), RR possible
Flow (Lpm):
Oxygen %:
Fixed (f) or Variable (v) 21-100 (f)
Delivery Interface Face or Nasal Mask, Nasal Pillows
Humidification Possible
High Flow Nasal Cannula


Pros: Optimal humidification control, enables communication, easily removed for eating & drinking. Travels
Cons: Unable to deliver high levels of pressure.
Indication: Higher Flow & FiO2 %, Augmentation of Oxygenation Support (some +pressure), Ventilation Support (Dead space washout)
Flow (Lpm): 2 → 70
Oxygen %:
Fixed (f) or Variable (v) 21-100 (f)
Delivery Interface Large Bore Nasal Cannula
Humidification Yes

Figure 2. Summary of respiratory therapy options.
Venturi Mask
Pros: Generally well tolerated. Uniquely allows for precise oxygen titration. Cons: Can by drying. Cannot provide high amounts of oxygen. Dangerous at flows <6 Lpm
Indication: Precise O2 titration
Flow (Lpm): 6 → 10
Oxygen %:
Fixed (f) or Variable (v) 24-60
Delivery Interface Aerosol Mask Humidification No "Higher Flow" NC


Pros: Comfortable, enables communication, eating & drinking. Well tolerated. Easily travels Cons: Can be very drying. Can not deliver higher than 15 Lpm flow, may be inadequate to meet pt's flow or O2 needs.
Indication: Med Flow & Med FiO2%
Flow (Lpm): 2 → 15
Oxygen %:
Fixed (f) or Variable (v) 24-60 (v)
Delivery Interface Nasal Cannula Humidification No
Non-Rebreather

Pros: Comfortable, enables communication, eating & drinking. Well tolerated. Easily travels Cons: Can be very drying. Can not deliver higher than 15 Lpm flow, may be inadequate to meet pt's flow or O2 needs.
Indication: Higher Flow & FiO2 %
Flow (Lpm): 15
Oxygen %:
Fixed (f) or Variable (v) 100 (f)
Delivery Interface Face Mask Humidification NO

Additional details for respiratory therapy options for patients presenting to the emergency department with moderate respiratory distress. BIPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; FiO2, fraction of inspired oxygen; Lpm, liters per minute O2, oxygen; RR, respiratory rate, pt, patient.
TABLE 4: Suggested outcome measures for patients with moderate respiratory distress.
• Emergency department door-to-disposition decision times
• Intensive care unit admission volume and rate
• Hospital length of stay
• Therapy switches (i.e., high flow nasal cannula to NIPPV) and escalations to intubation
• 30-day emergency department revisits and hospital readmissions NIPPV, non-invasive positive pressure ventilation.
including those with moderate respiratory distress. Future efforts should focus on iterating the content to keep it up to date and improve accessibility, perhaps allowing for electronic health record integration. Such integration may allow for incorporating clinical data feeds (eg, vital signs, laboratory results) and facilitating bedside orders, test result interpretation, and clinical documentation.26 While these suggestions have been thoughtful in their creation, we recommend outcome measures in Table 4 that can be used as measures of success.
LIMITATIONS
Convening an expert panel to develop recommendations and create a bedside tool for emergency physicians has several limitations. First, when evidence was lacking, some aspects of the best practices in the ED were derived only from expert panel discussions. A rigorous systematic literature review and grading consistent with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) standards or Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology were not performed, and specialty society treatment guidelines formulated via a structured or systematic review of the evidence are typically restricted to interventions with the highest quality of evidence.27,28 This expert panel’s recommendations are distinct from ACEP clinical policies, governed by the Clinical Policies Committee under a separate process. In addition, outside the relative cost information briefly provided in Table 3, recommendations from this expert panel do not include more detailed economic analyses of the direct and net financial impact of various treatment and disposition (ie, post-ED care) options.
CONCLUSION
The evidence-based emPOC tool was developed by a multidisciplinary panel of experts convened by ACEP to be a resource for emergency clinicians caring for patients with moderate respiratory distress. Studies examining the functionality of this tool in real-world practice are warranted, as data related to its daily use in the ED setting will allow for improvements and modifications to be rapidly incorporated over time, given the tool’s flexibility to be easily updated.
Future studies examining the impact of specific interventions, such as various respiratory therapies initiated during the ED visit vs deferring to the inpatient team, are important to demonstrate the real-world effect of digital tools and further support the benefits of specific interventions on patient outcomes.
Address for Correspondence: Christopher W. Baugh, MD, MBA, Brigham and Women’s Hospital, 75 Francis Street, Department of Emergency Medicine, Neville House 2nd Floor, 10 Vining Street, Boston, MA 02115. Email: cbaugh@bwh.harvard.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. Christopher W. Baugh is a paid speaker for CE Symmetry, Octapharma, and Roche Diagnostics, an investigator for Abbott Laboratories, Roche and Sanofi, an advisory board participant for Roche Diagnostics, Salix Pharmaceuticals, Pfizer Inc., and AstraZeneca, a consultant for Abbott Laboratories, Pfizer Inc., and Roche Diagnostics, and an advisor to Vera Health, Quai, and Lucia Health Guidelines. Jim F. Neuenschwander has received research funding from BridgeSource Medical, CSL Behring, and Siemens Healthineers USA and reports being a speaker and consultant for Abbott Laboratories, AstraZeneca, Janssen (now J&J Innovative Medicine), Thermo Fisher Scientific, Fisher & Paykel Healthcare, and Pfizer Inc.; and is an owner in AsceptiScope, Inc. EO has nothing to disclose. Antonio Anzueto is a consultant for GSK, AstraZeneca, Sanofi/Regeneron, Viatrix, and Pfizer. No other author has professional or financial relationships with any companies that are relevant to this study. There are no other conflicts of interest or sources of funding to declare.
Copyright: © 2025 Baugh et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Cairns C, Kang, K. National Hospital Ambulatory Medical Care Survey: 2021 emergency department summary tables. Available at: https://ftp. cdc.gov/pub/Health_Statistics/NCHS/ Dataset_Documentation/ NHAMCS/doc21-ed-508.pdf. Accessed December 10, 2024.
2. Schwartzstein R. Approach to the patient with dyspnea. UpToDate, Connor RF (Ed), Wolters Kluwer. Available at: Approach to the patient with dyspnea - UpToDate. Accessed: March 29, 2025.
3. Oskvarek JJ, Zocchi MS, Black BS, et al. Emergency department volume, severity, and crowding since the onset of the coronavirus disease 2019 pandemic. Ann Emerg Med. 2023;82(6):650-60.
4. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med 2019;200(7):e45-67.
5. Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical
Baugh
Acute Care of Patients with Moderate Respiratory Distress
Baugh et al. practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426.
6. Rochwerg B, Einav S, Chaudhuri D, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 2020;46(12):2226-37.
7. Ware LB. Go with the flow: expanding the definition of acute respiratory distress syndrome to include high-flow nasal oxygen. Am J Respir Crit Care Med. 2022;205(4):380-2.
8. Dubin J. How smartphones and apps are changing emergency department care. June 26, 2017. Available at: https://www. medstarhealth.org/blog/smartphone-medical-apps-emergencydepartment. Accessed: February 17, 2025.
9. Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401-9.
10. Baker K, Greaves T, Fraser JF. How to use humidified high-flow nasal cannula in breathless adults in the emergency department. Emerg Med Australas. 2019;31(5):863-8.
11. Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy Am J Respir Crit Care Med. 2019;199(11):1368-76.
12. Prakash J, Bhattacharya PK, Yadav AK, et al. ROX index as a good predictor of high flow nasal cannula failure in COVID-19 patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. J Crit Care. 2021;66:102-8.
13. Melo-Diaz LL, Kieling GA. The ROX index: “propelled” by high-flow nasal cannula therapy during the COVID-19 pandemic into greater applicability in respiratory support. Can J Respir Ther. 2022;58:182-4.
14. Mosier JM, Tidswell M, Wang HE. Noninvasive respiratory support in the emergency department: controversies and state-of-the-art recommendations. J Am Coll Emerg Physicians Open 2024;5(2):e13118.
15. Kwon JW. High-flow nasal cannula oxygen therapy in children: a clinical review. Clin Exp Pediatr. 2020;63(1):3-7.
16. Wimalasena Y, Kocierz L, Strong D, et al. Lung ultrasound: a useful tool in the assessment of the dyspnoeic patient in the emergency department. Fact or fiction? Emerg Med J. 2018;35(4):258-66.
17. Giorno EPC, Foronda FK, De Paulis M, et al. Point-of-care lung ultrasound score for predicting escalated care in children with respiratory distress. Am J Emerg Med. 2023;68:112-8.
18. Schibler A, Franklin D. Respiratory support for children in the emergency department. J Paediatr Child Health. 2016;52(2):192-6.
19. Long B, Liang SY, Lentz S. High flow nasal cannula for adult acute hypoxemic respiratory failure in the ED setting. Am J Emerg Med 2021;49:352-9.
20. Agustí A, Celli BR, Criner GJ, et al. Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary. Eur Respir J. 2023;61(4):2300239.
21. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17):1757-80.
22. Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603.
23. DeVos E, Jacobson L. Approach to adult patients with acute dyspnea. Emerg Med Clin North Am. 2016;34(1):129-49.
24. Osheroff J, Teich J, Levick D, et al. (2012). Improving Outcomes with Clinical Decision Support: An Implementer’s Guide, 2nd Ed. New York: HIMSS Publishing.
25. Corazza F, Arpone M, Tardini G, et al. Effectiveness of a novel tablet application in reducing guideline deviations during pediatric cardiac arrest: a randomized clinical trial. JAMA Netw Open 2023;6(8):e2327272.
26. Sutton RT, Pincock D, Baumgart DC, et al. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17.
27. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6(7):e1000097.
28. Malmivaara A. Methodological considerations of the GRADE method. Ann Med. 2015;47(1):1-5.
Recent Interventions for Acute Suicidality Delivered in the Emergency Department: A Scoping Review
Katherine Dowdell, MD* Michael P. Wilson, MD, PhD†
Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, Massachusetts
†
Carilion Medical Center, Department of Emergency Medicine and Psychiatry, Roanoke, Virginia
Section Editor: Mark I. Langdorf, MD, MPHE
Submission history: Submitted May 19, 2025; Accepted May 20, 2025
Electronically published October 3, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.47474
[West J Emerg Med. 2025;26(5)1495–1496.]
To the Editor:
We read with great interest the paper “Recent Interventions for Acute Suicidality Delivered in the Emergency Department: A Scoping Review” published by Hood et al in a recent issue of WJEM. We enthusiastically agree with the importance of emergency department (ED) expertise in the management of suicidal thoughts, as suicide prevention is a paramount public health concern. However, following careful reflection, we found methodological concerns regarding the exclusion of certain interventions and the manner in which conclusions were presented that warrant further discussion.
First, the authors excluded several ED interventions from this scoping review, including “screening, joint safety planning, patient education, lethal means counseling, followup contacts, and the involvement of friends and family.” The explanation for excluding these interventions is that they are “state-of-the-art practice (ie, generally accepted care)” as referenced in two textbooks, Rosen’s Emergency Medicine: Concepts and Clinical Practice and Kaplan and Sadock’s Comprehensive Textbook of Psychiatry 1,2 In reviewing the material cited from Kaplan, there is discussion of psychotherapeutic interventions and lethal means restriction as part of treatment for suicidal patients but no specific reference to these interventions being performed or evaluated in the ED setting.
The chapter cited from Rosen largely references “Caring for Adult Patients with Suicide Risk: A Consensus Guide for Emergency Departments” published in 2015.3 While this useful resource compiled best available information at the time, the authors explicitly state that the publication “is not intended to define a standard of care and should not be construed as one.” Excluding certain interventions based on documents that do not present a standard of care poses a danger of misrepresenting the evidence available in the field. As there are published papers regarding the excluded
interventions within the time frame of interest and the existing data on implementation of these interventions in the ED setting is limited, inclusion of these interventions would have generated a more robust description and called forth a need for further research to generate evidence-based guidelines.
One additional aspect of the paper that raised concern was the manner in which conclusions were presented. The authors engaged in a qualitative synthesis of evidence without a critical appraisal of evidence. While the PRISMAScR checklist notes critical appraisal of individual sources as optional, completion of this process would have enhanced the rigor of this scoping review.4 The exclusion of this step may lead readers to a biased interpretation of available data. For example, in the paper on crisis response planning (CRP) by Bryan et al in 2017, the authors concluded that “CRP is highly effective for use in the acute care setting for acutely suicidal patients.”5 While this study is important, a closer look reveals considerable potential for bias. First, this was a small (n=32-33 in each arm), single-center study that exclusively recruited active-duty US Army soldiers, who were predominantly young, male, and White. Hence, the findings may not be readily generalizable to other care settings or populations. Second, a higher number of patients in the control group had a history of at least one suicide attempt, which may have biased findings away from the null. Third, there was substantial (nearly 20%) loss to follow-up, underscoring the potential for informative censoring. The totality of these observations limits rigorous interpretation of the study findings.
Taken together, the authors should be applauded for a much-needed summary of available data concerning suicide prevention in the ED. However, the article’s conclusion should be approached with caution. Evidence syntheses— should they be included in a scoping review—must be approached with the appropriate rigor and equipoise.
Letter to the Editor: Comment
Without this critical step, attention to important gaps in the field may be diminished.
Address for Correspondence: Katherine Dowdell, MD, Beth Israel Deaconess Medical Center, Department of Emergency Medicine, One Deaconess Road, West/CC-251, Boston, MA 02215. Email: kdowdell@bidmc.harvard.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Dowdell et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Betz JM. “Suicide.” In: Walls R, Hockberger R, Gausche-Hill M, Erickson TB, Wilcox SR (eds.), Rosen’s Emergency Medicine: Concepts and Clinical Practice, 9th ed. Philadelphia, PA: Elsevier Inc; 2018:1366-1373.
2. Sudak H. “Suicide treatment.” In: Sadock B, Sadock V, Ruiz P (eds.). Kaplan and Sadock’s Comprehensive Textbook of Psychiatry,10th ed. Philadelphia, PA: Wolters Kluwer; 2017:5973-5985.
3. Capoccia LM. Caring for adult patients with suicide risk: a consensusbased guide for emergency departments. 2015. Available at: https:// sprc.org/wp-content/uploads/2022/11/EDGuide_full.pdf Accessed January 26, 2025.
4. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169(7):467-473.
5. Bryan CJ, Mintz J, Clemans TA, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. Army soldiers: a randomized clinical trial. J Affect Disord. 2017;212:64–72.
Recent Interventions for Acute Suicidality Delivered in the Emergency Department: A Scoping Review
Alex P. Hood, BA*†
Lauren M. Tibbits, MD*
Juan I. Laporta, BS*
Jennifer Carrilo, BS*
Lacee R. Adams, BS*
Stacey Young-McCaughan, RN, PhD‡
Alan L. Peterson, PhD, ABPP‡§
Robert A. DeLorenzo, MD, MSM, MSCI*
Section Editor: Mark I. Langdorf, MD, MPHE
University of Texas Health Science Center at San Antonio, Department of Emergency Medicine, San Antonio, Texas
Baylor University, Department of Psychology and Neuroscience, Waco, Texas
University of Texas Health Science Center at San Antonio, Department of Psychiatry and Behavioral Sciences, San Antonio, Texas
University of Texas at San Antonio, Department of Psychology, San Antonio, Texas
Submission history: Submitted July 27, 2025; Revision received July 27, 2025; Accepted July 27, 2025
Electronically published October 3, 2025
Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI 10.5811/westjem.53023
[West J Emerg Med. 2025;26(5)1497–1498.]
To the Editor:
We are delighted that the authors of the comment share our enthusiasm for emergency department (ED) expertise in the management of suicidality and appreciate their attention to our scoping review methodology. Their primary concern is the exclusion of standard and generally accepted techniques of screening, joint safety planning, patient education, lethal means counseling, follow-up contacts, and the involvement of friends and family. They rightly point out that the Rosen chapter1 and the guidelines from which it is derived2 should not be taken to define the clinical “standard of care,” which is why we avoided this terminology in our review. However, it is worth noting that the ICAR2E clinical guidelines published by the American College of Emergency Physicians demonstrate almost total overlap with the interventions described in Rosen.3,4
We concur with the authors’ argument that the interventions described in these textbooks merit further study, especially given their current evidentiary basis.3 However, the purpose of our review was to delineate what is on the horizon for the ED management of suicidality and not provide a comprehensive review of interventions that have already been established. Given the lag in publishing, we took the appearance in authoritative textbooks to indicate that the listed interventions are mainstream and, thus, not pertinent to a review of techniques that have been only recently described. Given the concordance of these interventions with current guidelines,3 this method appears to have been effective.
The authors of the comment highlight that critical appraisal of individual sources is optional in the PRISMAScR checklist,5 and we acknowledge their perspective
on its potential contribution in this topical area. We agree fully with their point that crisis response planning shows promise but that existing evidence for widespread adoption is wanting,6 as we clearly noted in our discussion and conclusion sections.
Suicidality is a significant clinical challenge in the ED, and we thank the comment authors for acknowledging our review.
Address for Correspondence: Alex P. Hood, BA, University of Texas Health Science Center at San Antonio, Department of Emergency Medicine, 703 Floyd Curl Drive, MC7736, San Antonio, TX 78229. Email: alex_hood1@baylor.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2025 Hood et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Betz JM. (2018). “Suicide.” In: Walls R, Hockberger R, Gausche-Hill M, Erickson TB, Wilcox SR (eds.). Rosen’s Emergency Medicine: Concepts and Clinical Practice, 9th ed (p.1366-73). Philadelphia, PA:
2. Capoccia LM. Caring for adult patients with suicide risk: a consensusbased guide for emergency departments. 2015. Available at: https:// sprc.org/wp-content/uploads/2022/11/EDGuide_full.pdf Accessed June 8, 2025.
3. Wilson MP, Moutier C, Wolf L, et al. ED recommendations for suicide prevention in adults: the ICAR2E mnemonic and a systematic review of the literature. Am J Emerg Med. 2020;38(3):571-581.
4. Kivela PD. Suicide and the creation of evidence-based guidelines: the ACEP perspective. Am J Emerg Med. 2019;37(12):2246-2247.
5. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169(7):467-473.
6. Bryan CJ, Mintz J, Clemans TA, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. Army soldiers: a randomized clinical trial. J Affect Disord. 2017;212:64-72.
Join




Learn

FEATURED SPEAKERS

Dr. Faith Quenzer President of CAL/AAEM




Victor
Joshua Faucher
Tyler Olson of OlsonFP