MEDICINE
THE UNIVERSITY OF TENNESSEE HEALTH SCIENCE CENTER

Advancing Care and Discovery in Tennessee






Dear Friends and Colleagues,
The University of Tennessee Health Science Center’s College of Medicine has long been a vital force for the health of our state. For generations, we have trained physicians who serve Tennesseans with skill, compassion, and integrity. I continue to be filled with optimism about the extraordinary opportunities that lie ahead.
That optimism begins with leadership. We are proud to welcome our new Executive Dean of the College of Medicine, Dr. Michael Hocker, whose vision and energy will guide us into our next chapter. With a deep commitment to education, research, and clinical care, his leadership will strengthen our mission and expand our impact across Tennessee.
Equally exciting is the possibility of a new interdisciplinary building for the College of Medicine. More than bricks and mortar, this facility would symbolize our commitment to collaboration and innovation. Imagine a space where physicians, scientists, nurses, pharmacists, and other health professionals learn and work side by side, advancing solutions to the most pressing health challenges of our time. Such a building would enhance our educational environment and accelerate discoveries that improve lives across our state.
The future of health care in Tennessee depends on our ability to adapt and innovate. With new leadership and the promise of expanded facilities, we will be even better equipped to confront chronic disease, address health disparities, and train physicians who serve with both skill and humanity. Our partnerships with hospitals, clinics, and communities will ensure that every Tennessean benefits from our work.
The horizon is bright. Together, we will honor our legacy while embracing innovation, ensuring that Tennesseans today and tomorrow have access to the very best in medical education, research, and care.

With gratitude and anticipation,
Peter Buckley, MD Chancellor of the University of Tennessee Health Science Center
The First 90 Days and Beyond



Education = Prevention A Legacy of the Heart

Leading the Fight One College of Medicine RESEARCH AND INNOVATION Jaw in a Day

Chancellor
Peter Buckley, MD
Executive Dean of the College of Medicine
Michael Hocker, MD, MHS
Dean, College of Medicine – Chattanooga
James Haynes, MD, MBA, FAAFP
Dean, College of Medicine – Knoxville
Robert Craft, MD
Associate Dean of Clinical Affairs and Graduate Medical Education – Nashville
A. Brian Wilcox, Jr., MD
Vice Chancellor for Advancement
Brigitte Grant, MBA
Assistant Vice Chancellor for Alumni and Constituent Engagement
Chandra Tuggle
Executive Director of Development College of Medicine
Kelly Davis
Editors
Chris Green
Peggy Reisser, MASC
Writers
Lee Ferguson
Chris Green
Aly Lawson
Aimee Chazal McMillin
Haley Overcast
Peggy Reisser
Designers
Adam Gaines
Shunjie (Jason) Zhang
Photographer
Caleb Jia
On The Cover: College of Medicine
researchers are using innovative technology to explore ways to combat certain deadly brain infections. (Page 30)
All qualified applicants will receive equal consideration for employment and admissions without regard to race, color, religion, sex, marital status, parental status, sexual orientation, gender identity, national origin, disability, age, genetic information, veteran status, or any other characteristic protected by federal or state law.
Eligibility and other terms and conditions of employment benefits at The University of Tennessee are governed by laws and regulations of the State of Tennessee, and this non-discrimination statement is intended to be consistent with those laws and regulations.
In accordance with the requirements of Title VI of the Civil Rights Act of 1964, Title IX of the Education Amendments of 1972, Section 504 of the Rehabilitation Act of 1973, and the Americans with Disabilities Act of 1990, The University of Tennessee affirmatively states that it does not discriminate on the basis of race, sex, or disability in its education programs and activities, and this policy extends to employment by the University.
Inquiries and charges of violation of Title VI (race, color, national origin), Title IX (sex), Section 504 (disability), ADA (disability), Age Discrimination in Employment Act (age), sexual orientation, or veteran status should be directed to the Office of Compliance, 920 Madison Avenue, Suite 825, Memphis, Tennessee 38163, telephone 901.448.7382 (V/ TTY available). Requests for accommodation of a disability should be directed to the ADA Coordinator at the Office of Compliance. 70-700302(001-260671)

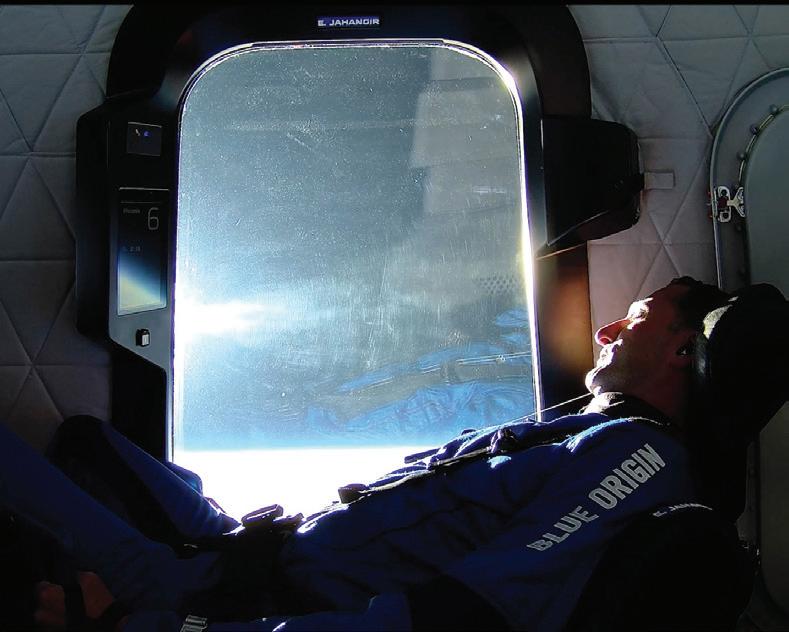
‘Our
Is Really
Michael Hocker, MD, assumed the role of executive dean of the College of Medicine in July 2025. As he completed his first 90 days, he reflected on his time at UT Health Science Center and shared his exciting vision for the college as it trains the state’s future physician workforce, cares for the people across Tennessee, and researches the cures of the future.

AQYou’ve been here roughly three months. What has struck you the most about the College of Medicine?
The incredible quality of our students, our staff, our faculty, and the impact they’re having, not in just one region, but throughout the state. It’s incredible to hear the alumni talk about the experience they’ve had here, but I also get to see firsthand what the faculty are doing. And I think the thing that I’m really excited about is our why is really strong. And as I look at how our vision of Thriving Communities. Healthy Tennesseans really resonates with our people. Whether I’m here in Memphis, Chattanooga, Knoxville, Nashville, Jackson, East Tennessee, everyone has the same vision and mission, and we’re all driving toward that.
QWhat drew you to UT Health Science Center?
AI wanted to come here because it’s a wellestablished medical school with a long history of excellence, and the opportunity to lead that with a statewide presence was really important for me, not just personally, but professionally. And to know that medicine can have an impact, not just at the hospital or the region you’re in, but also within the state, where the health indices are not what they should be. I think at the core of what I do as an emergency physician is improving health and access to care. And again, I think that’s where academic medicine is strong here at UT Health Sciences, and it’s strong throughout the state. It’s not just in one hospital or one region.
“When
I look at the students who are entering our medical school, they would be competitive at any medical school in the country.”
–
Executive Dean Michael Hocker, MD

QIs there anything that has surprised you?
AI wouldn’t say surprised. I would say that the complexity of what we’re doing is a challenge, but it’s also an opportunity. Dr. Buckley and the team really did a good job of making sure I understood where the challenges and opportunities were. One thing that I’m delighted to hear moving forward was discussed at the time I was getting recruited. There was discussion about a new College of Medicine Interdisciplinary Building, but I wasn’t sure if that was a pipe dream or really could become reality, knowing the size and scope of that project. I’m not surprised, but I’m just thankful that the leadership team here, from the president through the chancellor and all the vice chancellors, really have rallied around the need for a new College of Medicine building, which I think is really going to have, not just a short-term, but a long-term impact on how we grow medicine and move medicine forward in this state through class size expansion, both in our MD program, PA program, and the interdisciplinary work we’ll be able to do in the building.
AQYou mentioned challenges and opportunities. We just talked about operating a College of Medicine across an entire state. What else would you mention?
I would say the challenges of medicine right now, with the landscape, both at the state and federal level, and the uncertainty of so many things in medicine. I look at this as a great opportunity as a leader. One of my philosophies is to adapt, improvise, and overcome. We are leaders in our state, and as the federal government and state shift, we as leaders have to be adaptable and have to lead our people through that. The people who are going to come out on the other side of that stronger are organizations like us that work together as a UT System, that have a bigger mission, and that have really strong leaders who aren’t afraid to look at innovative ways to change education, to change clinical practice, and to adapt to ever-changing research needs. And so, I really look at that as an opportunity.

AQWhat would you want people to know about the proposed new College of Medicine Interdisciplinary Building?
It’s not just a building. This really represents a history of medicine that started in 1911 (when the university was founded) and has endured so many changes throughout the decades. This will be a home, where we train the next generation of leaders in medicine. When I say home, I don’t know what we’ll look like in four or five years, as we expand our regional sites, which we’re going to need to do, and we need to grow our class size. This new building will allow interprofessional education. This new building will allow class expansion, which is much needed. By 2035, there’s predicted to be a shortage of 6,000 physicians in Tennessee. As Tennessee’s statewide public medical school, the state needs us to make sure that we are filling that pipeline of future physicians for the state of Tennessee.
If we increase the class size, we also need those students to have opportunities locally and regionally and within the state. We will continue to push residency expansion, not just in urban areas, but also rural opportunities. And so, equally as important is increasing the number of residents or on-the-job training. But one will help drive the other.

AQIs there anything else you’d like to share?
In the first 90 days, I’ve been to every part of this state. Everybody’s been welcoming. Everyone is passionate about our mission of training the next generation of health care leaders, taking care of patients and providing high-quality clinical care, and conducting life-changing discoveries and research. And we have people across the state doing that. Everyone is passionate about our mission of commitment and dedication and service that we provide in each one of our communities.
The other thing I would say is about the students coming into our medical school class. When I look at the students who are entering our medical school, they would be competitive at any medical school in the country. That’s a good sign for us, and when I look at the other metrics of success for our students and residents, all the quality indicators are some of the top in the country.
Our medical school is recruiting good, really wellqualified candidates. And the product that comes out, they’re well-trained; they’re viewed as some of the best students, and then ultimately some of the best residents, and they can get jobs anywhere. We need to make sure that that pipeline continues to get full. I’d say one of the things that I want to bring to the college is, we’re going to continue to do what we do well and continue to be innovative in our pipeline programs, our early admission programs, our three-plus programs, where we work to get students and residents through programs and out into the workforce in an expedited, but still high-quality fashion, with a focus on filling the need in Tennessee.
By Chris Green

“There’s going to be a need for continual improvements in our space as we continue to strive to put forward technology and educational experiences for all our learners.”
– Jarrod Young
When the Center for Healthcare Improvement and Patient Simulation (CHIPS) opened in 2018, it transformed how the University of Tennessee Health Science Center prepared students for clinical care. With a recent round of major technology upgrades, CHIPS is again redefining what is possible, making high-quality simulation training more accessible, flexible, and forward-looking than ever.
Over the past year and a half, CHIPS has undergone a major upgrade to its audio-visual systems, a transformation that not only enhanced the quality of simulation recordings but also expanded the center’s reach far beyond the Memphis campus.
“We began an assessment to look at upskilling our audio-visual equipment,” says Jarrod Young, director of Operations, Technology, and Business Development at CHIPS. “This technology helps us be able to support medical education by capturing simulation activities, whether it’s manikin scenarios or encounters with standardized patients.”
These recordings are critical for both assessment and self-reflection. Students can review their performances to identify areas for improvement, and instructors can evaluate clinical competencies with precision. “It allows us to have a one-stop shop, basically, for all learners to come through, pull up their account, and either see the evaluations or self-assess their performance,” Young says. But the upgrade wasn’t just about sharper cameras and clearer audio. It marked a strategic shift from a fixed, on-site system to a cloud-based model that dramatically increases flexibility, scalability, and longevity.
“The new upgrade helps with the volume of information we must store, enhanced speed for accessing simulation recordings, and better integration of assessment tools and data metrics for individual students or aggregate performance of groups. The performance of the technology itself is superior in many ways,” says Tara Lemoine, DO, executive director of CHIPS. “All that can fundamentally streamline our faculty’s workload and provide a better experience for students.”
More importantly, Dr. Lemoine says, the technology now allows for simulation-based education in locations outside the Memphis campus. From anywhere with internet access, students can use their handheld devices to record simulations and push the recordings into the cloud for faculty review. “You could be in your house or out of the country, and we could have you log into your phone or another device, remotely activated by us, and do a simulation in real time,” she says.
Developing remote capabilities will be especially valuable for students and instructors across the statewide campuses. “We can capitalize on this technology to incorporate engagement of more programs across the state and create a more robust simulation footprint for learning,” Dr. Lemoine says. “For example, audiology students could participate in interprofessional simulation with students from other colleges or have access to our expertise here at CHIPS for their educational experiences. We can do things in ways never before possible for all our UT Health Science Center students, no matter where they are located.”
Young emphasizes that the upgraded system was retrofitted directly to the center’s needs and represents “the top-of-the-line system that’s available on the market.” The investment, he says, was a testament to senior leadership’s commitment to advancing education.
That commitment is reflected in CHIPS’s standing among peer institutions. In January 2025, Becker’s Hospital Review included CHIPS in its list of “64 simulation and education programs to know.” The introduction to the list reads, “By leveraging state-of-the-art technology and lifelike simulations, these programs drive better patient outcomes, lower health care costs, and improve patient safety. They provide a secure environment where providers can develop expertise through hands-on practice.”
As an accredited simulation program since 2021, CHIPS adheres to foundational principles of simulation education, including the use of best-in-class technology. But staying at the forefront requires more than a one-time upgrade — it demands ongoing support.
“Just like your laptop or your phone, every couple of years technology advances and changes,” Young says. “There’s going to be a need for continual improvements in our space as we continue to strive to put forward technology and educational experiences for all our learners.”
That includes reinvesting in high-functioning equipment like manikins and staying informed about emerging technologies such as artificial intelligence, augmented reality, and virtual reality. “This field is always changing, so we always have to stay on the front end of assessing what we need to invest in for the future of our learners or what is maybe a catchy, flashy new feature that isn’t worth spending money on,” Young says.
Maintaining and servicing specialized equipment also requires financial and operational support. “We rely on all of our equipment to provide simulation education,” Young says. “So, we have to keep warranties, stay educated on how to troubleshoot and put in corrective maintenance, or know who to call to get this equipment back up and running whenever it breaks or needs service.”
Ultimately, the success of the latest technology upgrade was a collaborative endeavor. “It was a multi-departmental effort between CHIPS, executive leadership, and campus IT,” Young says. “Without all those parties together, we wouldn’t have had such a smooth transition and smooth integration of this technology.”
With the new system fully operational, CHIPS is still exploring how to work with programs statewide to fully leverage the upgraded features to expand opportunities. It is clear, though, that this investment has reinforced the center’s standing among the nation’s best, positioning it to continue leading the way in simulation-based medical education.
To learn more about CHIPS and how you can support it, contact Jay Atkinson, director of development, at jatkin22@uthsc.edu.
By Peggy Reisser
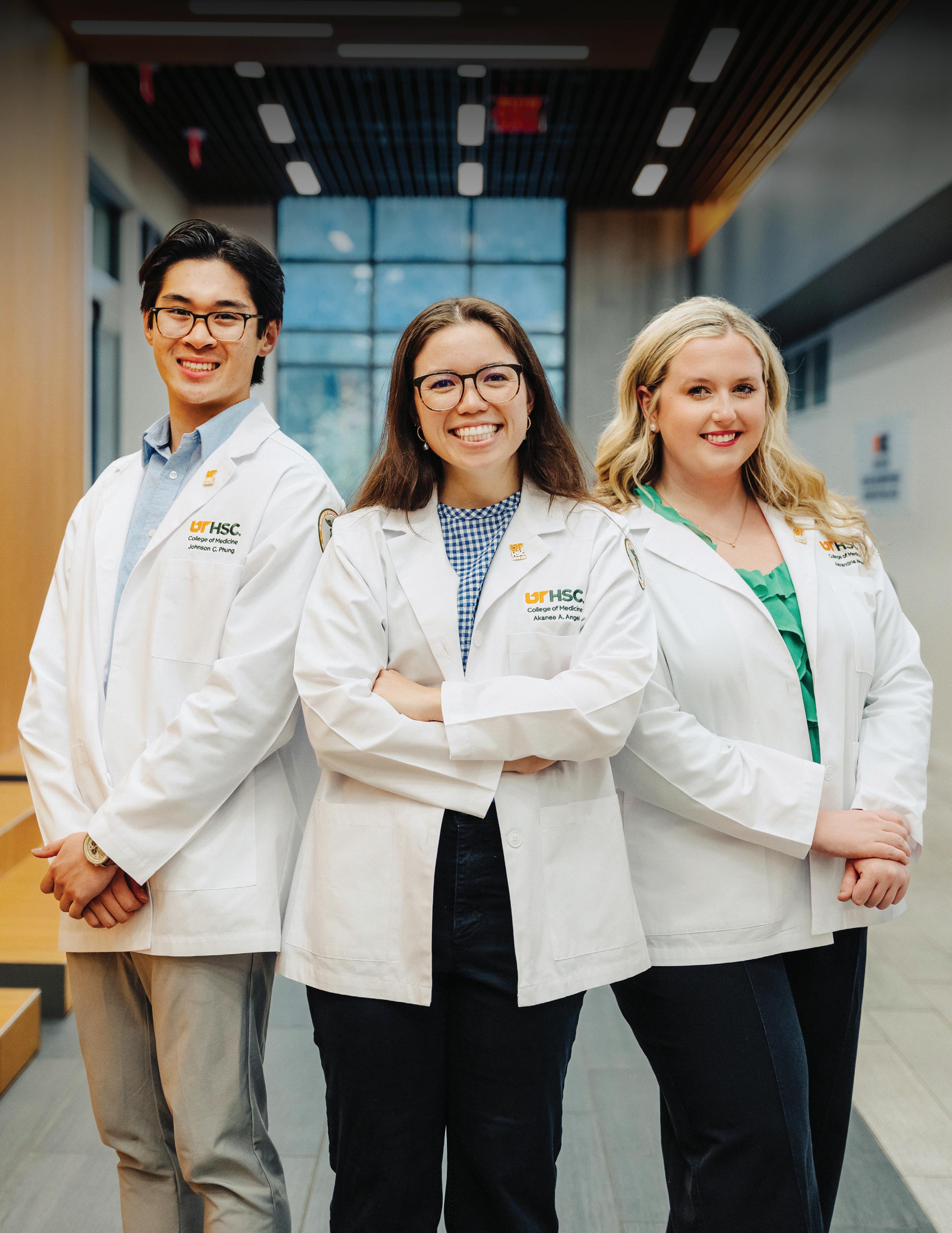
First-year medical student Johnson Phung, 22, aspires to be an internal medicine physician. Akanee Angel, 23, also a first-year medical student, wants to practice family medicine. Both want to stay in Tennessee after they graduate.
Phung and Angel are students in the College of Medicine’s accelerated Three-Year MD Program. Launched in 2021, the program allows highly motivated students committed to practicing in certain fields to complete medical school more rapidly and with reduced cost.
It is available to students who know they want to enter the fields of Family Medicine, Internal Medicine, Medicine-Pediatrics, Pediatrics, Neurology, Pediatric Neurology, and Psychiatry. Participants have a direct pathway to one of these residency programs in the UT Health Science Center system upon graduation from medical school.
“I came into medical school for sure knowing I wanted to do two things,” Angel said. “One was to be a family medicine doctor. I had a whole year of working as a medical assistant in a family medicine clinic, and I knew that it was right for me. I knew that I loved it so much and I couldn’t see myself doing anything else.
“And the other thing I wanted to do was work in Tennessee and stay close to family, stay close to home, and kind of give back to all of these communities that have helped shape me,” Angel, who is from Clarksville, added. “The three-year program, I thought, was a great opportunity to do both of these things and faster than a traditional medical student.”
The accelerated program is special for many reasons, said Catherine Womack, MD, the associate dean of Student Affairs and Admissions at the College of Medicine.
“It is wonderful if students accepted to medical school here know the primary care specialty they are interested in applying to, because they are able to save a year of medical school tuition,” she said. “We need more practicing physicians, as we have a physician shortage, which will only continue to worsen as our population ages. Graduating our students early helps UT Health Science Center increase the number of graduates, helps the student with their debt, and helps our residency programs match excellent students who they know well, as they have mentored and taught them over the three-year program.”
Phung, who is from Lebanon, Tennessee, and Angel graduated from Belmont University and are a couple. “We met during undergrad and are now pursuing our dreams of medicine together at UT Health Science Center,” he said.
In addition to being certain about his future goals, Phung had specific ideas about the institution that would help him achieve them.
“When I was applying to schools, I wanted to make sure I applied to a school that was very collaborative,” he said. “I toured UT Health Science Center twice upon getting accepted and just the environment and the collaboration between the students was probably my favorite thing. Everyone just seemed so ready to support each other instead of competing against one another.
“And then, I also know that I have career goals of staying in Tennessee and practicing in Tennessee,” he said. “I consider Tennessee to be my home state, so it just made a lot of sense to me to train where I was going to eventually practice. And the
three-year program allows me to. First, it’s shorter, so it’s one less year I’m in school, and that’s a year sooner I could get to see patients. Because there’s a conditional match, I get to pour my efforts into things that I want to pour into instead of trying to fill out an application (for residency) or do something just to make sure my application looks good. I get to be a little more particular with my time and point to things I really care about.”
Students in the three-year curriculum achieve the same program objectives and curricular goals as those in the traditional four-year curriculum. The timeline, however, is condensed.
“Because you know what you’re going to want to do, they’re going to give you fewer optional rotations and less elective time,” Phung said. “So, you lose some of your fourth year, and then you also lose, I think, all your summers. Your summers are cut down from two months to two weeks.”
Accelerated programs are increasing at medical schools across the country, said Tina Mullick, MD, an associate professor and the assistant clinical dean for the Three-Year MD Program at UT Health Science Center.
“In terms of national data, we know that people who are in threeyear programs compared to a traditional four-year cohort are equally successful, have equivalent board pass rates, and they do great as physicians,” she said. “And actually, there’s even some data saying they may even be slightly superior in terms of their higher rates of chief residents, for example, amongst the three-year cohorts compared to the four-year cohorts.”
The program has already produced two graduating classes. It began in Memphis, but has expanded to the college’s campuses in Jackson, Chattanooga, Knoxville, and Nashville.
“Probably the biggest thing that I would say for our students and for applicants about this program at an institutional level is that it’s great because hopefully we’re attracting really highcaliber applicants and hopefully we’re keeping these people on as physicians, for certain through residency, but then keeping them beyond as our faculty and as our fellows and as our community physicians,” Dr. Mullick said.
Alex Wood, 22, is from Lexington, Tennessee, and wants to be a pediatrician and practice in West Tennessee as close to her hometown as possible. “Honestly, there is need in all of West Tennessee,” she said.
“Just growing up here, the communities here have always served me. I’m where I am because of the state of Tennessee, and just the kindness of people in my hometown,” said Wood, a UT Knoxville graduate and HOPE and Volunteer Scholarship recipient.
“And so now, I feel like it’s my turn to serve the people of Tennessee back. I just feel like that’s what I was born to do, be a Volunteer.”
To learn how you can support students in the Accelerated MD Program, contact Cameron Mann, director of development, at c.mann@utfi.org.
Match Day 2025 saw nearly half of the College of Medicine’s graduating class match into residencies in Tennessee. Of those 75 students staying in the state, 54 are remaining at UT Health Science Center for their residencies. The numbers speak volumes as UT Health Science Center works to train Tennessee’s future health care workforce.
“This is what we’ve worked for. We have spent hours and hours in hospitals and classrooms and clinics, and we’ve gotten to a point where we get to do what we want to do—be doctors,” said then-fourth-year medical student and class president Grace Anne Holladay, as she awaited the news of where she would spend the next phase of her training to become an OB-GYN.
Dr. Holladay, who earned her MD degree in May, was one of the 168 students who gathered with family and friends on March 21 at Beale Street Landing overlooking the Mississippi River in downtown Memphis for the College of Medicine’s Match Day celebration. When Dr. Holladay opened her envelope, she was thrilled to learn she would be staying at UT Health Science Center for her OB-GYN residency.
“This is exactly where I want to be,” she said. “I feel really blessed to get to stay here and keep training at the place where I fell in love with OB.”
Match Day is a highly anticipated event where medical students nationwide simultaneously discover where they will train for residency. The moment students open their envelopes is often filled with emotion, excitement, and joy as they take the next step in their medical careers. It is a pivotal milestone for medical students, marking years of perseverance and dedication to the field of medicine.
“I want you to hold something in your heart: that you are all amazing people and you are going to be amazing physicians,” Associate Dean of Student Affairs Catherine Womack, MD, told the students moments before the countdown started.
“The reason you are here is that you care about taking care of others. Wherever you go, you will do great things.”
Similar celebrations took place at the College of Medicine’s campuses in Knoxville and Chattanooga. Fourteen students at the Knoxville campus learned their residency placements at a celebration at the Women’s Basketball Hall of Fame. In Chattanooga, six students gathered with their supporters at The Walden Club to learn where they had matched. After a welcome brunch, Dean James Haynes, MD, addressed the group, encouraging students to reflect on their time in medical school and reminding them to support their colleagues in the next phase of their training.



Of the 168 total students who matched:
• 75 (45%) matched to residencies in Tennessee.
• 54 (32%) stayed at UT Health Science Center for residency.
• 76 (45%) matched to primary care specialties
• 61 (36%) matched to non-primary care specialties.
• 31 (18%) matched to surgical specialties.
• 4 (2%) matched to military residency.

By Allyson Lawson

Medical school is hard enough, but students like Avery Dargie add another challenging layer. In Dargie’s last year, the University of Tennessee Health Science Center student leadership funnel led her to Medical Student Executive Council (MSEC) president.
“MSEC acts like an umbrella,” she says, “with numerous committees falling under it that allow for leaders to act as a conduit between the student body and faculty.”
A Memphian from birth, Dargie followed her father’s path to UT Health Science Center. He attended the university and practices emergency medicine locally. After attending Lausanne Collegiate School and
earning her undergraduate degree from the University of Alabama, she returned to Memphis for medical school and is pursuing emergency medicine as well. Her fiancé, Robert “Renn” Eason, also a Class of 2026 medical student, serves as Honor Council president.
“Memphis built us, inspired us, and continues to drive us forward,” she says. “We’re proud to call Memphis our home, and we hope to continue serving this community for many years to come.”
A planning aspect she didn’t anticipate is how she has developed a passion for staying at UT Health Science Center and transitioning into academic medicine to help build the institution.
Students develop within MSEC through four-year elected positions. As president, Dargie serves on the Student Government Association Executive Council, representing the College of Medicine alongside the other five colleges. Dargie’s leadership began as an MSEC representative her first year, then treasurer, vice president, and president.
Class presidents — Ben Finder serves the Class of 2026 — typically hold four-year roles and work closely with MSEC. The council spearheads projects and oversees subcommittees that involve everything from water fountain filters and student resources to security and curriculum changes.
“Once I was elected to MSEC, I was sitting on this committee, voting my peers into these subcommittees, and so that was something I found out on the fly,” she says of her learning curve. “What a great honor and privilege, to get to elect your peers to different subcommittees that really make incredible differences.”
Finder says he basically had no leadership experience before medical school, and the student leaders learn and go through a lot together. While nothing can change the challenge of medical school, he says, it’s much more doable and enjoyable for everyone when you have a network around you. Dargie has worked hard to drive that spirit of community as well as represent the students to administration, he says.
“People like Avery are the ones who step up to the plate and take action when needed.”
Dargie and Finder talk every other day. The executive team shares constant voice notes. Leadership meets monthly; executive leadership weekly. Administration is accessible by text or call. All this while juggling classes and out-of-town rotations.
As medicine evolves, students’ needs change, Dargie says. They strive to address issues with communication and collaboration, so they can accomplish important things efficiently.
“What UT Health Science Center has created is a really good community, where students and faculty come together to make the university the best institution it can be.”
Across student leadership, Dargie has noticed a variety of backgrounds and experiences but a unified purpose.
“Our leaders come up with incredible solutions. I’m fortunate enough to be a sort of bridge for what they want to see happen. We all have different thought processes but always come together to support each other and find solutions.”
The council’s reach spans the breadth of what medical school is, Dargie says.
Curriculum changes go through MSEC subcommittees. Leadership gains student feedback on academic programs and surveys resources students need. For campus life, MSEC worked with the Campus Police Department to increase security before exams. The police now have exam schedules, so students have additional safety during late-night studying.
Student leaders also help fund social events, such as sponsoring the photobooth for the Med Gala. Clubs can request MSEC funding for projects; the council funded holiday baskets for community children through a student organization.
Council members also serve as a positive feedback channel, sharing with administration if an event, effort, or even small thing the dean did was well-liked or successful.
Dargie is busiest as MSEC president during her fourth year, the least demanding academically. This timing by design allows more energy to be dedicated during peak leadership periods. Plus, team members chip in extra when it’s busy.
“I was studying for my second board exam, my VP, who’s a year younger, picked up the slack. It takes a village…We look at the year as a whole and say, let’s do as much as we can to plan for things we know are going to happen.”
The previous president created documentation on what to do and when, and Dargie is building on that for the future. What has become a well-oiled team effort makes balancing academics and governance sustainable, she says.
“Avery is truly one of a kind,” says Alayna Robinson, who also serves on MSEC. “She’s one of the kindest, most genuine individuals I’ve ever met, always the first to lend a hand and support those around her. Avery fosters a culture of positivity, inclusivity, and compassion, and her deep love for this school and its students shines through in everything she does.
“Since M1 year, she has consistently stepped up to volunteer, contribute, and lead. She’s a natural leader, not just because of her dedication and work ethic but also because of her heart. Avery leads by example and sets a standard for what it means to be a servant leader…I genuinely strive to be more like her.”
Physician Called to Educate Public on Disease Prevention
By Peggy Reisser

Here’s how Chinelo Animalu, MD, describes her role as an infectious disease physician:
“We deal with those cases that make everybody else run in the opposite direction,” she says.
An associate professor in the Division of Infectious Diseases in the College of Medicine, Dr. Animalu is the medical director for Infectious Disease and Geographic Medicine for Methodist Le Bonheur Healthcare. Her primary clinical practice is at Methodist University Hospital in Memphis.
Born in Nigeria, Dr. Animalu says her early years set the stage for the work that is her passion today.
“Growing up in Nigeria, I was very sickly and had to take medicines for different types of infections,” she recalls. She would see the devastating results, including blindness, disfigurement, and death, from common infections that were left untreated due to a shortage of physicians, a lack of medications, and inadequate health care facilities.
“I used to be traumatized seeing these people,” she says.
“I’m like, ‘Why can’t somebody help them?’ And so, that’s not only what gave me that foundation in medicine, but also the foundation in infectious disease, because what kills us the most in Africa is going to be infections.”
Dr. Animalu earned her medical degree from the University of Nigeria and completed a residency there. She married and immigrated to the United States. An internal medicine residency at St. Joseph Hospital in Chicago followed. She later earned a master’s degree in public health at Tulane University.
“That’s my calling,” she says. “My specialty when I was in Nigeria was actually public health.”
Dr. Animalu moved to Memphis for a fellowship in infectious disease at UT Health Science Center. She joined the College of Medicine faculty as an assistant professor in 2016 and became an associate professor in 2022.
“I do two different kinds of work — my clinical work at Methodist and then my outreach,” she says. The latter role she does as a volunteer because she sees a need that must be met.
Dr. Animalu speaks at meetings, churches, schools, community events, and in the media about the prevention of infectious diseases.
“Based on the experiences back home in Nigeria and in Africa in general, because I’ve been to so many African countries, the problem is still the same — lack of knowledge, people just dying from preventable causes,” she explains.
She is particularly vocal about preventing HIV infections. Memphis has the second-highest rate of new infections in the county, with most new cases among those ages 15 to 24.
“This is devastating, because obviously there’s something we’re doing wrong,” Dr. Animalu says.
“The clinic is for treatment. My own work — what I want us to do is prevention, not treatment.”
Her selfless outreach efforts recently earned her a Health Care Heroes Award from the Memphis Business Journal and the Volunteerism and Community Service Award from the American College of Physicians, Tennessee Chapter.
However, awards are not her goal. Educating the public is.
Earlier this year, she launched a talk show on YouTube, “Medical Class 901 with Dr. Chi,” to do just that. She has educated viewers on antibiotics, HIV, common respiratory infections, and other infectious diseases. The program, also available on Facebook and Instagram, has more than 2,000 followers.
“The whole idea of ‘Medical Class 901’ was just to share information. I have other physicians I invite to come on this show to talk about primary care in whatever their own specialties are,” she says. “Because in Memphis, even though we have major hospitals and health care organizations, the average public, they are lacking so much in terms of health care issues and understanding.”
Dr. Animalu has received numerous awards for her efforts to educate the public about the prevention of infectious diseases.


‘Cancer Care Is All I Ever Wanted to Do,’
By Peggy Reisser

“When we train and teach learners — students, residents, and fellows — at UT Health Science Center, we have an opportunity to keep them here in Tennessee.”
– Dr. Martin Fleming
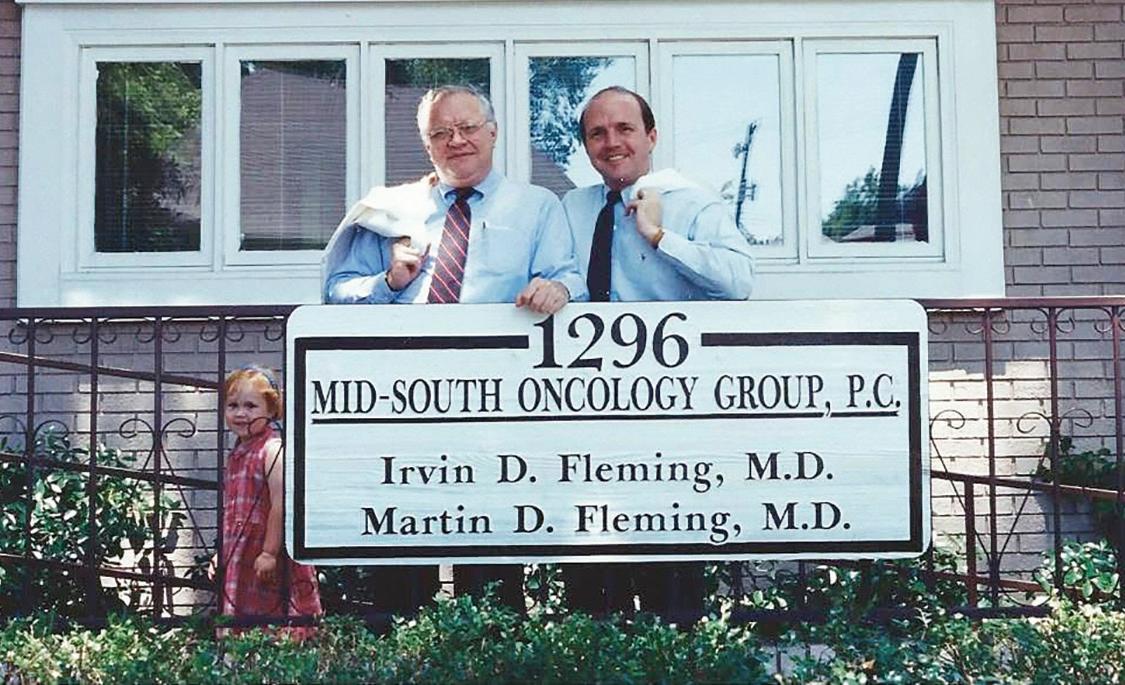
Martin Fleming, MD, chief of the Division of Surgical Oncology in the College of Medicine, remembers going door-to-door in Memphis as early as age 6 or 7 with his mother, a survivor of osteogenic carcinoma, to collect money for the American Cancer Society.
His father, the late Irvin D. Fleming, MD, also a Memphis surgeon and longtime UT Health Science Center professor of surgery, was a pioneer in cancer care and research and spent more than 50 years as a volunteer with the American Cancer Society, serving as its international president in the 1990s.
His son, Andrew Fleming, MD, is one of the chief surgery residents at the College of Medicine and soon to move to Tampa, Florida, to begin a surgical oncology fellowship at Moffitt Cancer Center.
You could say cancer care is a legacy of the heart for all three of these UT Health Science Center College of Medicine alums.
“Cancer care is really all I have ever wanted to do,” Dr. Martin Fleming says. A 1986 graduate of the College of Medicine, he is a nationally recognized authority on the treatment of melanoma, sarcoma, and breast cancer. He completed residency training at the University of Texas Southwestern in Dallas and a surgical oncology fellowship at the Medical College of Virginia. He returned to UT Health Science Center as an adjunct volunteer faculty member in 1993 and joined the faculty full time in 2001.
Since then, Dr. Fleming has made a major contribution in bringing the highest level of cancer care, state-of-the-art research, and treatment options to the people of Memphis and the Mid-South.
He established and leads the Division of Surgical Oncology, which has experienced robust growth and includes nine surgical oncologists. Dr. Fleming is also among the faculty physicians, who under the strong
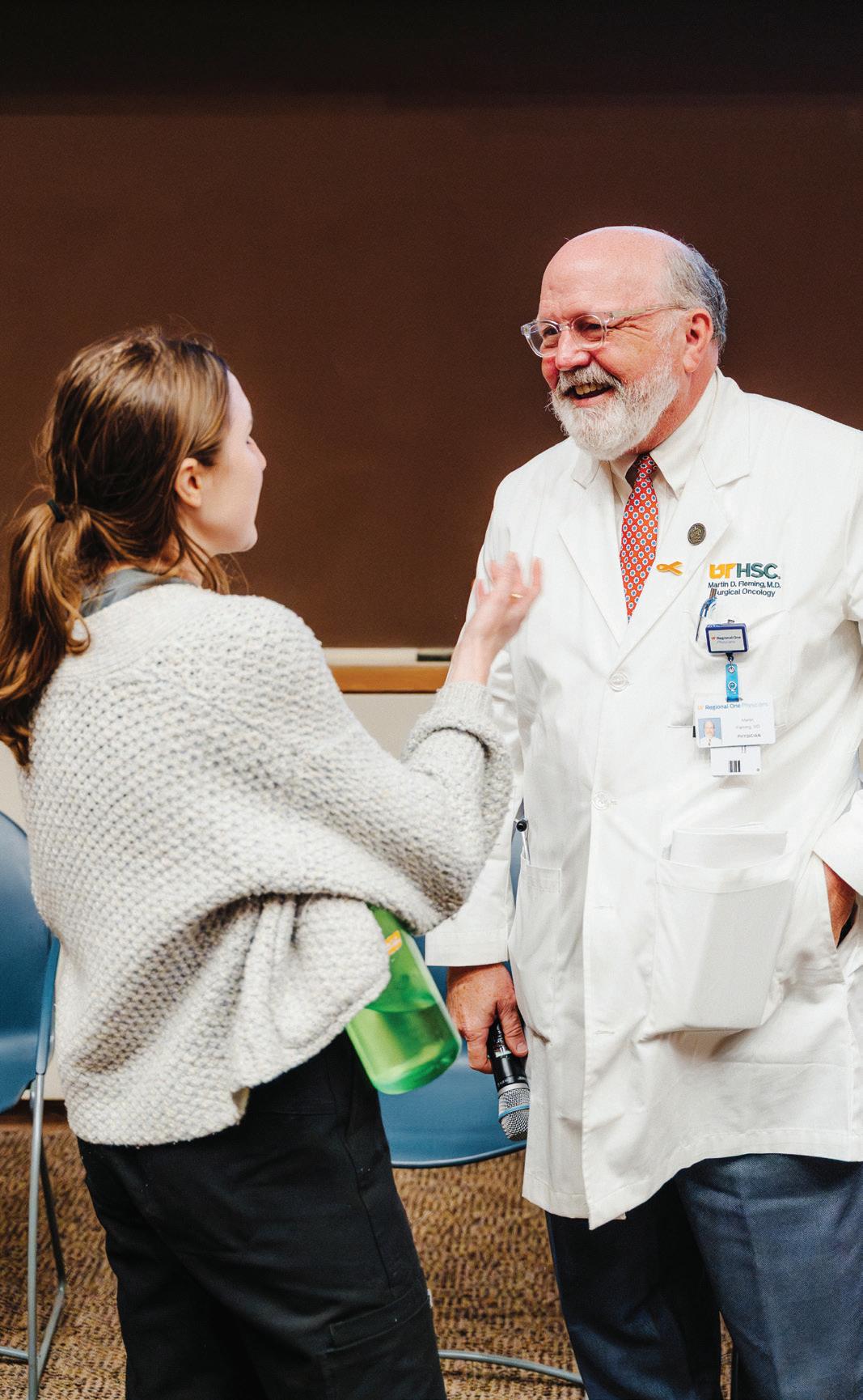
Dr. Fleming is also dedicated to mentoring future surgeons and surgical oncologists. “Having people who have chosen cancer care as their career path can, and does, transform the care we provide in Memphis and Tennessee.”
leadership of David Shibata, MD, chair of the Department of Surgery, established and operate the Regional One Health (ROH) Cancer Care Program, a collaboration between the university and its clinical partner ROH. Dr. Fleming chairs the program’s Cancer Committee, which links all providers who care for cancer in the hospital.
“It’s really important to have a multidisciplinary approach to each case,” he says. This would include medical oncology, surgical oncology, radiation oncology, and other services.
Earlier this year, the Regional One Health Cancer Care Program earned accreditation as an Academic Comprehensive Cancer Program from the Commission on Cancer, a national organization that recognizes hospital oncology programs that meet the highest standards of patient care.
Accreditation requires many national standards that include a robust tumor board, extensive tracking of screening efforts, and multidisciplinary presentation of cases.
Dr. Fleming, along with oncology program accreditation manager Leslie Stroud, led the initiative.
Sometimes, his teaching even allows him to cross paths with his son in the OR. “I got to operate with him yesterday,” he says proudly.
“One of our main opportunities in our partnership with Regional One Health is impacting the gaps in cancer care across all the populations of Memphis,” he says. “It gives us a unique opportunity to make a difference in the health care in our city.”
Dr. Fleming says accreditation is pivotal to the program. “It demonstrates excellence in cancer care and shows that we offer state-of-the-art, multidisciplinary care for all our patients. It puts us on the map as a place that’s doing it right.”
However, teaching is equally as important as patient care to Dr. Fleming. In his view, the two go hand in hand.
“One of the things I really enjoy is having the opportunity to participate in teaching students, residents, and surgical oncology fellows in the care of cancer patients,” he says.
“One of my first initiatives when I started the Division of Surgical Oncology was to start the process of having a surgical oncology fellowship,” he continues. UT Health Science Center received approval for its fellowship in 2017 and is among 34 accredited surgical oncology fellowships in the U.S. “I thought it important that we have one.”
In addition to instructing surgical oncology fellows and residents on their surgical oncology rotations, Dr. Fleming is the clerkship director, teaching third-year medical students about surgery.
“This is important because our patients deserve the best cancer care we can possibly provide them and to be cared for by physicians who have been trained specifically in that,” he says. “Having people who have chosen cancer care as their career path can, and does, transform the care we provide in Memphis and Tennessee.”
Dr. Fleming is a believer in the statistics that indicate roughly 60% of medical residents stay in the state or region where they trained.
“When we train and teach learners — students, residents, and fellows — at UT Health Science Center, we have an opportunity to keep them here.”
Chelsea Olson, MD, is proof of that. She is from Colorado, went to medical school in Virginia at Virginia Commonwealth University, and trained in general surgery at the University of South Alabama. However, she did her surgical oncology fellowship at UT Health Science Center, and upon completion, recently joined the Division of Surgical Oncology as an assistant professor.
“Dr. Fleming interviewed me, and the whole program was just very welcoming, so I made it my top choice,” she says. “Sometimes when you match into a place, it’s not what you think, but it pretty much lived up to all the expectations I had when I was interviewing, and I was excited to start the fellowship, especially with Dr. Fleming leading it.”
She says Dr. Fleming is careful to ensure everyone involved in a case has a role.
“He’s always making sure that people are involved in his cases and they’re learning something,” Dr. Olson says. “And the environment at UT Health Science Center is all about learning, and I couldn’t help but fall in love with that.”
By Chris Green

When Kenneth Ataga, MD, talks about his work, his focus is always on his patients. He has spent more than two decades caring for people with sickle cell disease and searching for better treatments for the condition that often causes unpredictable pain, threatens organs, and shortens lives.
“I was attracted to medicine because I wanted to help people,” says Dr. Ataga, the Plough Foundation Endowed Chair in Sickle Cell Disease, director of the Center for Sickle Cell Disease, and chief of Hematology at UT Health Science Center. “When I began to understand sickle cell disease and how it affects every aspect of a person’s life, I knew this was where I could make a difference.”
Dr. Ataga grew up in Nigeria, which has the highest number of people living with sickle cell disease in the world. He says he didn’t go to medical school planning to specialize in hematology or sickle cell disease. His original goal was to become a cardiologist.
“When I moved to the U.S. many years ago and started my residency training in Syracuse, New York, I realized that I no longer liked cardiology quite that much,” he says. “But the place where I trained had a very good group of hematologists and oncologists, and it was very easy to be inspired to want to be like them.”
During his training at the University of North Carolina (UNC) at Chapel Hill, he met the late Eugene Orringer, MD, who became a mentor and helped shape his career. “He was a hematologist who focused on sickle cell disease, and he pretty much changed my life,” Dr. Ataga says. “His enthusiasm was so infectious that I chose to go to Chapel Hill to work with him.”
At Chapel Hill, Dr. Ataga dedicated his clinical and research fellowship, and later his faculty career, to advancing care and understanding of sickle cell disease. He rose to the rank of tenured professor and served as director of the UNC Comprehensive Sickle Cell Program. While his initial interest in Memphis came from a career opportunity for his wife, the city’s large sickle cell population helped him decide to make the move in 2018.
“I knew that if I was going to leave Chapel Hill and go someplace else, it had to be a place where I could take care of patients but also perform the research I do,” he says.
At UT Health Science Center, Dr. Ataga leads a team that provides care for patients across the region at the university’s partner hospitals, including the Regional One Health Diggs-Kraus Sickle Cell Clinic and the Methodist Comprehensive Sickle Cell Center. His focus is on improving patient outcomes, expanding access to care, and developing new treatments.
“Patients with sickle cell disease experience lots of challenges, typically from when they are very young,” he says. “They have unpredictable episodes of pain, which are often referred to as pain crisis, and they experience fatigue. Sickle cell disease can affect pretty much every organ system, so patients are at risk of complications such as stroke, lung problems, kidney problems, and they have a shorter life expectancy than the general population, about 48 years on average. There just aren’t adequate treatments to help prolong their survival to match the general population.”
Over the years, Dr. Ataga has become an international leader in sickle cell research and treatment. He served as the lead investigator on the
clinical trial for crizanlizumab, a drug now approved by the U.S. Food and Drug Administration to reduce pain crises in people with sickle cell disease.
“I presented the initial results at the annual meeting of the American Society of Hematology in front of thousands of people,” he says. “Whenever I read that paper, I’m always pleased that I played a small role in making this drug available for patients, but I’m also reminded that we have a lot more work to do.”
Dr. Ataga’s team continues to be involved in several clinical studies and trials aimed at developing new therapies that can make the disease less severe. While some sickle cell patients can be cured through bone marrow transplant or gene therapy, most do not have access to those options due to the financial burden or health risks. Instead, their conditions are managed with medications to improve their quality of life and hopefully increase life expectancy.
“We do the best that we can. We want to be available as doctors who understand the problems they have and be advocates for these patients as well,” he says. “So, we try and provide medical care to help them live as normal a life as possible. That’s always the goal.”
While he has led successful studies and trials, Dr. Ataga is proudest of his ability to help patients regain stability and independence. He remembers one patient who was struggling through college because of his illness. Thanks in part to medical management by Dr. Ataga and his team, he not only finished college, but he went to medical school and now works as a sickle cell researcher and advocate.
“We often have patients referred to us because they have been experiencing lots of complications from their disease. Then they come see us, we start them on disease modifying therapies, and they get better. They get well enough that they’re able to go to school or go to work sustainably, and that changes their lives.”
After more than two decades as a hematologist, Dr. Ataga says his patients have also taught him a great deal. “It gives you patience,” he says. “Because they have pain as a common manifestation of their disease, and that’s not something you can objectively measure, it helps you to be even more empathetic. You have to believe them.”
Much like Dr. Orringer was to him, Dr. Ataga tries to be a visible mentor for younger faculty as well as students, residents, and fellows who rotate through his clinics and research programs. He often invites students to work with him, and many have served as co-authors on papers. “I think they find it gratifying,” he says. He hopes the next generation of physicians will continue to push the field forward and make improvements for patients.
“What gives me hope are the people who come after us,” he says. “I think about the enthusiasm that they have and the fact that they want to improve on the work that has already been done in the sickle cell space. That’s what give me hope.”
College of Medicine’s Knoxville Campus Embraces New Name in Line
By Chris Green

The College of Medicine – Knoxville has expanded its undergraduate medical education mission in recent years, allowing more students to train there.

For the last several years, the University of Tennessee Health Science Center’s medical campus in Knoxville operated with a name it had outgrown, according to the campus’s dean. On October 1, that changed.
Now officially the College of Medicine – Knoxville, the campus has stepped into a new identity that reflects its expanding role in undergraduate medical education as it grows to meet the needs of the statewide academic system.
The previous name, UT Graduate School of Medicine, reflected a historic focus on graduate medical education (GME), training residents and fellows. But as its undergraduate medical education (UME, training medical students) and research footprint grew, so did the need for a name that matched its evolving mission.
“Although training residents and fellows will always be core to our campus mission, we have significantly expanded our role within the statewide UT Health Science Center system,” says Robert M. Craft, MD, dean of the Knoxville campus. “Training medical students and doing groundbreaking research are increasingly important aspects of our mission. We are clearly now a College of Medicine.”
The College of Medicine – Knoxville, shortened to CoM-Knoxville, joins its counterparts in Memphis, Chattanooga, and Nashville to form the college’s statewide network of medical education. The updated name reinforces Knoxville’s expanded role in education and brings it into alignment with the naming conventions of the College of Medicine – Chattanooga, which was referred to as simply the Chattanooga Unit until approximately 15 to 20 years ago, and the College of Medicine – Nashville. According to Michael Hocker, MD, executive dean for the College of Medicine, who oversees all the college’s campuses, this consistency strengthens the connection between all campuses and aligns them more clearly with UT Health Science Center’s broader mission to serve communities across Tennessee.
The Knoxville campus’s former name dates to the 1990s, when University Health Systems began operating UT Medical Center — where the campus is housed — in concert with the college’s education and research missions. “‘Graduate School of Medicine’ was chosen because GME was the majority of our academic mission at the time. Our campus mission is now much broader,” Dr. Craft says.
The dean credits UT System President Randy Boyd’s “Be One UT” initiative and the leadership of Chancellor Peter Buckley, MD, for helping drive the change. “There was a change in vision by both the president of the university and by the chancellor of the Health Science Center to get the entire university system working together,” Dr. Craft says.
“We
are moving away from functioning in silos and moving toward leveraging each campus’s strength and best practices, growing together, and collaborating in tangible ways.”
That collaboration is already visible in the Knoxville campus’s growing clinical footprint. Grounded by its affiliation with
the 710-bed UT Medical Center and complemented by new partnerships, including one with East Tennessee Children’s Hospital, the campus now has a similar clinical capacity to the partner hospitals adjacent to the Memphis campus: Regional One Health, Methodist Le Bonheur Healthcare, Le Bonheur Children’s Hospital, and the Lt. Col. Luke Weathers, Jr. VA Medical Center.
CoM-Knoxville’s UME offerings have also expanded dramatically. Since 2012, students from the College of Medicine have been able to complete their third and fourth years entirely in Knoxville. The campus now hosts around 60 medical students at any given time, alongside 290 residents and fellows. Dr. Craft says that combination is beneficial for both medical students and graduate trainees.
“Integrating medical student training alongside residents and fellows in an academic medical center is optimal,” he says. “There’s a lot to be gained by the students from the residents’ perspectives, and the residents become teachers, which helps them solidify their own knowledge base. We often learn particularly effectively from people who are just up the experience ladder from us, so that’s another advantage from medical students learning with residents.”
Dr. Craft says the Knoxville campus is growing by “leaps and bounds, in every way.” In addition to larger medical student class sizes, CoM-Knoxville has laid the foundation for 25% growth of its GME programs from 2022 to 2027, and it is already halfway toward that goal. This growth, Dr. Craft says, is vital for the state.
According to Executive Dean Hocker, Tennessee needs additional physicians, and the state is projected to have a deficit of 6,000 physicians by 2030. “The College of Medicine and each of its campuses must be integral in ensuring that the state has enough physicians who can provide high-quality care to patients throughout the state,” he says.
The College of Medicine – Chattanooga is also increasing the number of physicians it produces. The campus is on track to expand its resident and fellow cohorts by 20% over three years. With 219 currently training in partnership with clinical partner Erlanger, the campus has already achieved 12% of that growth. Additionally, the number of third- and fourth-year medical students completing all their clinical training in Chattanooga increased this year to 24, up from a historical average of six to 10 annually. A total of more than 100 UT Health Science Center students rotate through the campus each year.
The College of Medicine – Nashville is also experiencing growth. What began with one residency program in partnership with Ascension Saint Thomas roughly 10 years ago, has blossomed with residency and fellowship program growth across multiple specialties, research collaborations, and rural care initiatives. The college is poised for future growth to serve the people of Middle Tennessee.
“With the name change in Knoxville, we’re reinforcing the fact that medical education in Tennessee is a team effort,” Executive Dean Hocker says. “This alignment connects our Knoxville campus even more closely with our colleagues in Memphis, Nashville, and Chattanooga. It opens the door to new opportunities for collaboration and helps us serve our learners and communities with even greater strength.”

By Chris Green
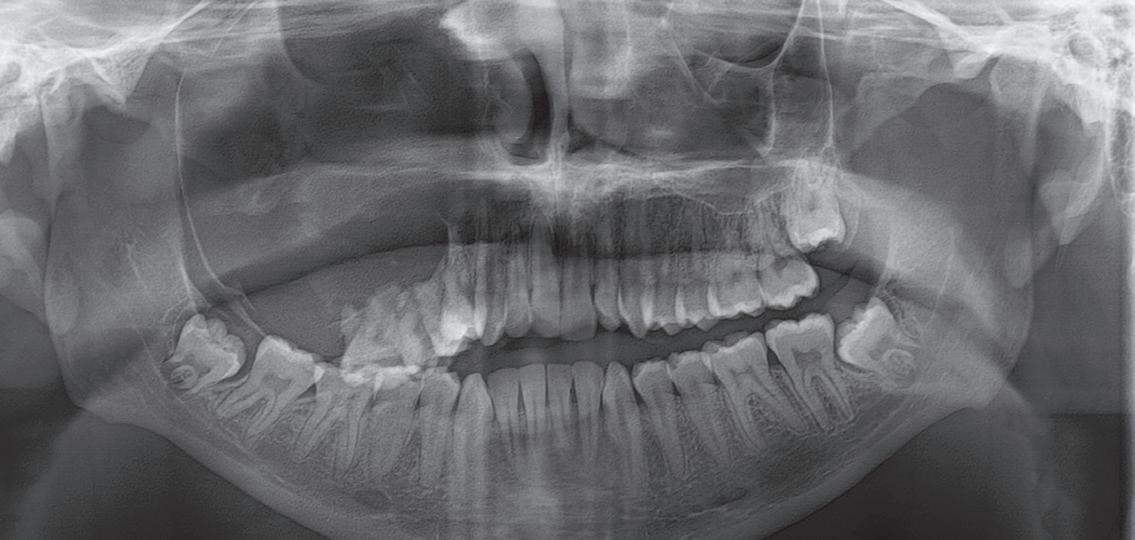
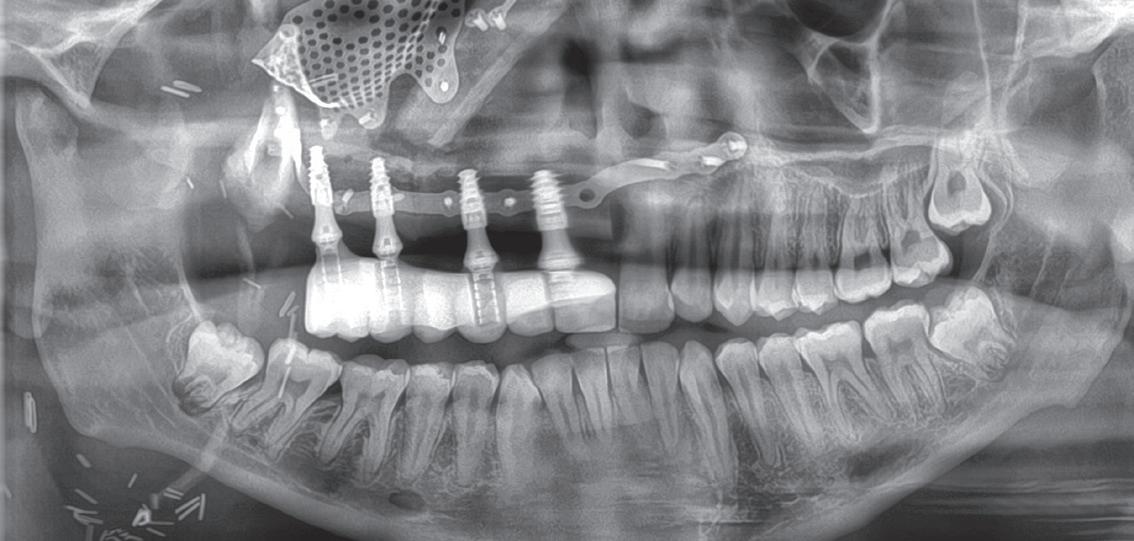
On an April morning in Memphis, James Wynn, then 17, prepared for a surgery that would change his life and make history in Tennessee. Diagnosed with a tumor destroying his jaw and facial bones, James became the first patient in the state and the Mid-South to undergo a groundbreaking “Jaw in a Day” procedure.
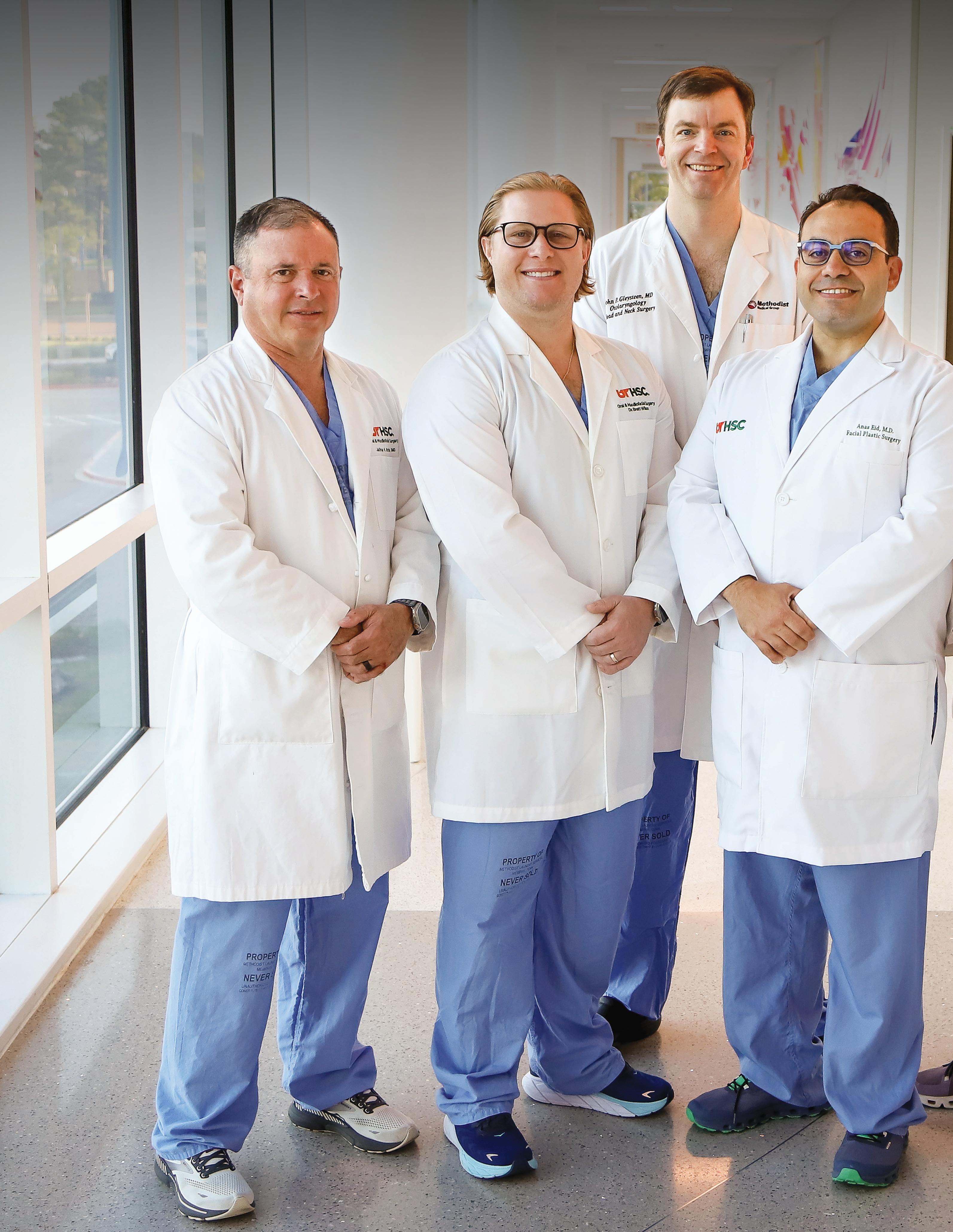
In a single operation at Methodist University Hospital, a multidisciplinary team of surgeons from the UT Health Science Center College of Medicine and College of Dentistry removed the tumor, rebuilt James’s facial bones and jaw using his leg bone, and placed custom dental implants and prosthetic teeth. The single-day approach dramatically shortened what would normally take months or years of procedures.
“Traditional methods could take several months, sometimes even years, to complete. In contrast, this procedure enables patients to receive a functional jaw in just one day,” said Anas Eid, MD, chief of facial plastic surgery and leader of the Jaw in a Day team.
For James, who was diagnosed with the tumor a few months earlier, the news that it could all be done in a single day brought relief. His mother, Alysha Wynn, recalled her nervousness before the operation but said her son’s resilience impressed her. “I was surprised by how good he looked, even though he was still kind of swollen,” she said. “I’m just thankful that he actually went through it and came out.”
The operation was the result of years of planning and collaboration across multiple specialties. In addition to Dr. Eid, the team consisted of the Department of Otolaryngology’s Assistant Professor C. Burton Wood, MD, and Associate Professor John Gleysteen, MD, along with the Department of Oral and Maxillofacial Surgery’s Chair and Professor Jeffrey Brooks, DMD, and Program Director and Associate Professor Brett Wilson, DDS. Using 3D models, custom hardware, and meticulous coordination, the surgeons united their skills to achieve a life-changing outcome.
“This surgery involves multiple steps from multiple surgeons that essentially build on one another,” Dr. Wilson said. “Each surgeon has to execute their part to set the next surgeon up for success, so the stakes can be high for everyone involved to bring the entire plan to fruition.”
The success of the surgery earned the Jaw in a Day team recognition beyond the operating room. In August, the Memphis Business Journal honored the group at its 2025 Health Care Heroes Awards, where four of the five winners and more than half of the 25 finalists were affiliated with UT Health Science Center.
Front row from
Brooks,
professor and chair of the Department of Oral and Maxillofacial Surgery; Brett Wilson, DDS, associate professor and program director for Oral and Maxillofacial Surgery; Anas Eid, MD, chief of Facial Plastic Surgery and lead surgeon; C. Burton Wood, MD, assistant professor of head and neck surgical oncology in the Department of Otolaryngology. In back, John Gleestyn, MD, associate professor in the Department of Otolaryngology. Photo by Natalie Clay
“Receiving the Health Care Innovations Award for our novel singlestage facial reconstruction technique was deeply gratifying,” Dr. Eid said. “It not only recognizes the novelty of our method, but it also underscores how a cohesive team of highly talented and specialized surgeons, through precise and orchestrated intervention, can dramatically improve patient outcomes and quality of life.”
The award also underscored how innovation in Memphis is shaping health care across Tennessee and beyond. “Innovations of this caliber are a direct product of the supportive and collaborative environment fostered by institutions like the University of Tennessee Health Science Center,” Dr. Eid said.
Since James’s surgery, the team has completed additional Jaw in a Day cases, proving the procedure’s success and reaffirming Tennessee’s leadership in advanced care. Each new patient benefits from lessons learned in the operating room and from the close partnerships that made the first case possible.
“In the state of Tennessee, this achievement sets a new benchmark for head and neck reconstructive procedures,” Dr. Eid said. “Our institution takes great pride in being a pioneer in this area, contributing significantly to the improvement of health care services in our state.”
For James, the impact was both immediate and long-lasting. He left the hospital within a week and quickly returned to daily life with only small scars as evidence of what he endured. His restored smile is a reminder not only of his own courage, but of what Tennessee’s health care teams can achieve when they work together.

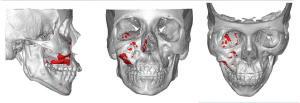




Dr. Eid and Dr. Wilson during surgery (top-left). James’s smile at the completion of surgery (top-right). The “Jaw in a Day” team included surgeons, residents, and a supporting staff of scrub technologists, nurses, clinic staff, and prosthodontists (bottom).

By Lee Ferguson
If clinical trials are the engine that drives new treatments and medical breakthroughs, then Giuseppe Pizzorno, PhD, PharmD, is the master mechanic working under the hood.
At Erlanger Health System in Chattanooga, he has quietly built the complex machinery — research teams, contracts, processes, and support systems — that allows dozens of cutting-edge trials to run without a hitch. Most patients never see this work, and many physicians simply rely on it in the background, but without it, those discoveries would stall before they ever reached the bedside. Now, after years of operating out of the spotlight, Dr. Pizzorno is being recognized for the vital role he plays with a Champions of Health Care Award from the Chattanooga Times Free Press.
Through his visionary leadership, Dr. Pizzorno, chief research officer at Erlanger and associate dean for Research at the UT Health Science Center College of Medicine – Chattanooga, has built a strong collaborative bridge between the two institutions. Under his guidance, Erlanger’s research program has grown into a powerhouse, supporting more than 50 physician-investigators in 11 therapeutic areas. Together, they are enrolling participants in roughly 40 active clinical trials, with another 25 to 30 in follow-up, advancing discoveries that span nearly every corner of modern medicine.
“We’ve created an environment where clinical research can thrive without disrupting clinical care,” Dr. Pizzorno says. “Physicians here don’t have protected research time, so our team supports them every step of the way — coordinators, regulatory staff, nurses — so that they can participate in high-impact research while continuing to care for patients.”
That model is working. Research conducted at Erlanger, in partnership with UT Health Science Center, has led to faculty publications in the New England Journal of Medicine, the Lancet, and other top-tier journals. Clinical trials span nearly every specialty, from AI-assisted colonoscopies in gastroenterology to advanced cardiac devices and phase 1 urology drug trials. “For some patients, participating in a clinical trial means getting the best care they’ve ever had,” he says. “That’s the kind of impact that motivates me every day.”
Dr. Pizzorno describes his own role in the process as “a little bit like Match.com,” pairing the right investigator with the right clinical trial and ensuring that each study is financially sustainable, scientifically rigorous, and operationally feasible.
“The clinical trial business is a $40 billion industry, and it’s going to double in the next five years,” he says. “We have to treat it like the serious business it is. That means negotiating contracts line by line, down to every needle and Band-Aid, and making sure our teams are delivering clean, usable data that sponsors can count on.”
One of his biggest innovations has been workforce development. Facing challenges recruiting experienced research coordinators, Dr. Pizzorno launched a pipeline program for local college graduates taking gap years before medical or graduate school. These young professionals receive foundational training in clinical research and contribute meaningfully to trial coordination, gaining critical experience and often, strong letters of recommendation, as they prepare for careers in medicine.
“We’ve had students from UT Chattanooga, Lee University, Kenyon College, and even Baylor University join our team,” he says. “Now we’re seeing some of them go off to medical school, and others are staying in clinical research. It’s become a real pipeline.”
Dr. Pizzorno also emphasized the unique advantages Chattanooga offers for clinical research: a high-volume, a varied patient population, engaged physician faculty, and a geographic position that bridges urban and rural communities, many of whom benefit from access to cutting-edge trials.
Jessica Snowden, MD, vice chancellor for Research at UT Health Science Center, also points to Chattanooga as a powerful example of why access to clinical trials matters statewide. “Clinical trials aren’t just about advancing science. They’re about ensuring that every patient has access to the very best care,” she says. “If we only reach urban centers, we miss the chance to serve the people who need these treatments most. Dr. Pizzorno’s work highlights the best of UT Health Science Center’s mission of bringing ’Healthy Tennesseans. Thriving Communities.’ to all corners of our state through cutting-edge science and exemplary care.”
While honored by the Champions of Health Care Award, Dr. Pizzorno remains focused on what’s next: advancing early-phase clinical trials, expanding academic collaborations, and giving every trainee, coordinator, and physician the chance to contribute to something meaningful.
“When you give people opportunities,” he says, “that’s when they shine.”

“For some patients, participating in a clinical trial means getting the best care they’ve ever had. That’s the kind of impact that motivates me every day.”
– Dr. Giuseppe Pizzorno
By Lee Ferguson

Inside a lab at the University of Tennessee Health Science Center, a transparent chip no bigger than a stick of gum could be changing the way scientists study the human brain and how they fight some of the world’s most dangerous viruses.
Colleen Jonsson, PhD (right), Harriet S. Van Vleet Chair of Excellence in Virology and director of UT Health Science Center’s Regional Biocontainment Laboratory and Institute for the Study of Host Pathogen Systems, is leading a project that pushes the boundaries of biomedical research.. Together with her graduate student, Walter Reichard, she is using a human brain-on-a-chip to explore how deadly brain infections take hold and how to stop them.

Venezuelan and Eastern equine encephalitis viruses (VEEV and EEEV) are rare but devastating infections that can cause fatal brain inflammation, particularly in children and older adults. “They infect children and older adults and cause lethal disease,” Dr. Jonsson said simply. “The brain is extremely well protected, and these viruses can still find a way in.”
To understand and combat them, scientists have traditionally relied on mouse models. But Dr. Jonsson’s lab is testing a revolutionary alternative — a miniature, three-dimensional system that replicates the function of the human brain. Known as a brain-on-a-chip, the technology represents what the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) have been calling the future of non-animal research, or “NAMs,” new-approach methods.
“This is novel technology to advance biological and therapeutic discovery,” Dr. Jonsson said. “The human brain chip allows us to do testing in humans. Whereas otherwise, we’re limited to doing our preclinical research with mice.”
Reichard, who is completing his PhD under Dr. Jonsson, has spent months troubleshooting and optimizing the system to make sure it behaves as similarly to a brain as possible. The device consists of two microscopic channels separated by a porous membrane. “You have these pods on a rack that go into an instrument called a ZOE CM2,” he explained. “That system controls the flow rate of media — basically, the blood — through the chip.”
One channel contains human vascular cells, the kind that line blood vessels. The other holds neurons, astrocytes, microglia, and pericytes — key cell types that make up the brain’s structure and immune defenses. Fluid flows continuously through the system, mimicking blood circulation and creating a tight barrier between the two chambers. That barrier, just like the real blood-brain barrier, carefully filters what can and cannot enter the brain.
“The virus we study is able to sneak through this barrier and get into the brain,” Dr. Jonsson said. “The chip recapitulates this tight barrier between our brain and our body. It’s a 3D representation of the brain.”
The human cells used in the model are de-identified and commercially obtained from deceased adult donors. In Jonsson’s lab, these living tissues form an intricate, dynamic environment, one that can be infected, treated, and observed under near-realistic conditions.
While the system offers extraordinary promise, Dr. Jonsson is careful not to overstate its capabilities. “We’re at really early stages,” she said. “This is exploratory research to determine the ability of the human brain chip to bridge the gap from mouse to human.”
She doesn’t yet call it superior to animal models, but she believes it could dramatically accelerate translation to human medicine. “I don’t know if we’ll ever get rid of animal models, but having human cells to look at how our drug is working gives us better insight into translation.”
Cost is not the main advantage — Dr. Jonsson admits the technology isn’t cheaper — but the potential precision is. “It gets us right to whether or not the drug could be effective for humans,” she said.
Early tests in the Jonsson lab have been promising. The team has already shown that their antiviral drug candidates — developed in collaboration with Bernd Meibohm, PhD, distinguished professor and associate dean for Research in the UT Health Science Center College of Pharmacy, and Jennifer Golden, PhD, associate director of the Medicinal Chemistry Center at the University of Wisconsin — can protect mice from encephalitic virus infection. Now, they are using the brain-on-a-chip to see whether those same drugs inhibit viral replication in human brain tissue.
“We can see antiviral efficacy in this chip,” Dr. Jonsson said, referring to a recent proof-of-concept experiment using one compound called Badger 49. “This is a really promising series of antivirals that treat encephalitic infections.”
Reichard finds the system just as thrilling from a research standpoint. “I’d be most excited to see how the virus crosses into the brain channel,” he said.
“When we got our first data, we were instantly brainstorming all the things we could do next. There was a lot of excitement when we first started.”
The implications extend well beyond viral encephalitis. “This technology could be used for Alzheimer’s drugs, Parkinson’s, even brain cancer,” Dr. Jonsson said. “The system is being used elsewhere in the country for different applications, but when we started, we were a little ahead of the game.”
For Dr. Jonsson, the success of the project comes down to both innovation and mentorship. “You can have all the ideas and dreams,” she said, “but without the right student, it’s not going to go anywhere. Walter has really been the driver behind the project.”
Though Reichard had never worked with organ-on-a-chip systems before, he was willing to take on the challenge. “I had a lot of cell culture experience but not with this technology,” he said. “It’s been a big learning experience.”
Dr. Jonsson smiled. “I’ve always worked with a lot of different technologies,” she said. “I’m usually an early technology embracer.”
The project “Evaluation of Antiviral Efficacy using a Blood Brain Barrier Model” is being funded by the National Institute of Allergy and Infectious Diseases.

Meet the UT Health Science Center faculty members serving as the new executive co-directors of the Heart Institute at Le Bonheur Children’s Hospital: Chief of Pediatric Cardiology Jason Johnson, MD (left), and Chief of Pediatric Cardiac Surgery Bret Mettler, MD (right).

“There will be times when we have to make challenging decisions for the institution, for the health system, for the medical school, or for me personally, but I think if we always keep patients at the center, we will always lead to making the right decision.”
– Dr. Bret Mettler
By Chris Green
Long before he became a leader in pediatric cardiac surgery, Bret Mettler, MD, entered medicine through a love of science and discovery. But it was the moments at the bedside, where he saw the difference his care made in the lives of children and their families, that gave his career its true meaning.
“I kind of meandered my way into pediatric cardiac surgery,” Dr. Mettler says. “I fell in love with the technical sophistication, the complexity of the operations, and the range of pathology we see, but as important was being able to make a difference to someone for potentially a whole entire life — not just a few years of life, but 60, 70, 80, 90 years of life.”
That passion for making a lasting impact led Dr. Mettler to Memphis and the University of Tennessee Health Science Center, where he is chief of pediatric cardiac surgery, the Susan and Alan Graf Endowed Chair in Pediatric Heart Surgery, and executive co-director of the Heart Institute at Le Bonheur Children’s Hospital, the university’s primary pediatric partner. In addition to the professional opportunity, what brought him here was a convergence of personal roots, institutional vision, and the promise of growth.
Dr. Mettler came to Memphis from Johns Hopkins Children’s Center in Baltimore, Maryland, where he served as director of pediatric cardiac surgery and co-director of its heart center. Before that, he was director of cardiac transplantation and mechanical circulatory support at Vanderbilt University Medical Center in Nashville.
Because his move to Johns Hopkins happened during the COVID-19 pandemic, his family stayed in Tennessee and deepened their ties to the Volunteer State. “My family got used to being in Tennessee, and we went back and forth to see each other,” he says.
With a southern wife and two daughters who have only ever been Tennesseans, the chance to return felt like coming home. “We love being back in the South. We like the warmth, the openness, the inquisitiveness. I prefer to be back down in an environment with that southern hospitality, which is what we’ve known our whole lives and our daughters have grown up in,” he says.
But the move was about more than geography. Dr. Mettler was drawn to the unique opportunities at UT Health Science Center and Le Bonheur. Under the leadership of the previous executive co-directors — Chief of Pediatric Cardiac Surgery Christopher Knott-Craig, MD, and Chief of Pediatric Cardiology Jeffrey Towbin, MD — the Heart Institute advanced into a top 10 program. Additionally, U.S. News & World Report has named Le Bonheur one of the nation’s “Best Children’s Hospitals” for 15 consecutive years, and the hospital recently completed a $95.4 million expansion, much of which is dedicated to caring for children with congenital cardiac disease.
“There was a rich history of congenital cardiac care here, started by visionary leaders, and an administration who had desires to not only maintain but to grow a pediatric heart institute to levels which hadn’t been realized before,” he says.
For Dr. Mettler, this environment created the ideal conditions for both clinical excellence and innovation. “It’s an exciting place for someone like me, who wants to provide excellent clinical care and research to work our ideas and foster the next generation of ideas.”
That work is supported by UT Health Science Center and the Methodist Le Bonheur Healthcare system, which together foster a collaborative environment where new programs and research initiatives can thrive.
For Dr. Mettler, being part of the academic medical setting at Le Bonheur, where most physicians are affiliated with UT Health Science Center, has been critical. In addition to the resources the College of Medicine provides for obtaining and administering research grants, the academic environment brings together like-minded faculty committed to advancing their field.
“We have a mission as faculty members at an academic institution for scientific discovery and to improve care for the next generation. We take that responsibility in the Heart Institute and pediatric cardiac surgery extraordinarily highly,” he says. “Our mission is to continue to advance discovery within pediatric cardiac surgery across all parts of the Heart Institute, whether it be pediatric cardiology, pediatric cardiac critical care, or pediatric anesthesia.”
Since arriving in late 2024, Dr. Mettler has wasted no time building on this foundation. He recruited a partner from Johns Hopkins, Associate Professor Danielle Gottlieb Sen, MD, MPH; launched a pediatric cardiac research institute; and set ambitious goals for the future, including establishing subspecialty centers for complex conditions and advancing research in remote and device monitoring for children. Additionally, a top priority is to grow a program for adults born with heart disease.
“There are now more adults alive with congenital heart disease than kids. That tells us that we’ve gotten better at our job,” Dr. Mettler says.
“We have a bunch of these patients who are now adults, who have adult problems that need pediatric-type operations. That’s one of the things we do as congenital cardiac surgeons — care for adults with congenital heart disease.”
As a surgeon and a leader, Dr. Mettler says he has two main responsibilities. He strives to help the faculty reach their full potential, fostering their curiosity and ideas, and giving them the space to lead in clinical care. At the heart of it all, though, is a responsibility to patients and families, focused on excellent care and outcomes.
“We always want to keep the patients at the center,” Dr. Mettler says. “There will be times when we have to make challenging decisions for the institution, for the health system, for the medical school, or for me personally, but I think if we always keep patients at the center, we will always lead to making the right decision.”
As he looks ahead, Dr. Mettler is optimistic about what is possible. “The environment I’ve found myself in is real fertile ground for growth, development, and acceptance of us as new heart surgeons in the community, but also for us in regards to providing care for patients and families. I’m excited for what we can achieve together.”
By Haley Overcast
For Jason Johnson, MD, MHS, the path to a career in pediatric cardiology was not a straight line. Dr. Johnson initially studied animal sciences in college, with dreams of becoming a veterinarian or marine biologist. The biological sciences — specifically, the human heart — kept calling him, though. And the root of that call stems from a deeply personal place.
“My brother was born with severe congenital heart defects and only lived 11 months. I was 5 years old when he died,” Dr. Johnson says. “I think that experience is why I was drawn to this field; it felt like part of who I was.”
Recently, Dr. Johnson was named chief of Pediatric Cardiology and Bob and Paula McEniry Endowed Chair of Cardiology. He is also executive co-director of the Heart Institute at Le Bonheur Children’s Hospital, an appointment he says feels less like a new beginning and more like the next natural step in a journey more than a decade in the making.
Dr. Johnson joined the Heart Institute in 2013 following residency and fellowship training at Duke University, bringing with him a clinical passion for advanced cardiovascular imaging and a sense of purpose grounded in his personal experience.
“At the time, I was the 13th cardiologist on staff,” he recalls. “Now we have 34. I might not have envisioned all this program would become, but even then, I could see tremendous opportunity for growth and specialty expertise — the chance to help shape something with enormous potential, right from the ground floor.”
Asked about his greatest career achievement, Dr. Johnson states without hesitation that his proudest accomplishment is “the connections I’ve built with my families.
“You’re here long enough and you build meaningful relationships, and that’s why we’re here, is to take care of our patients,” he says.
In fact, Dr. Johnson is finding meaningful ways to care for patients not just in his clinical practice, but through his work on the global stage. As editor-in-chief of Cases of SCMR for the Society of Cardiovascular Magnetic Resonance, he helps educate providers from around the world on advanced imaging techniques, supporting knowledge-sharing across borders and empowering physicians to bring new modalities of care back to their home countries.
Dr. Johnson brings that same collaborative and holistic approach to leadership, helping to bridge knowledge gaps and build cohesion across disciplines.
“In subspecialty care, it’s easy to get siloed. But our patients deserve coordinated, expert care,” he says. “I see my role as making sure each team has what they need to do their best work.”
Thankfully, as a cardiac imager, Dr. Johnson often finds himself at the crossroads of multiple subspecialties.
“One day I’m in outpatient general clinic, the next I’m reading echocardiograms in the ICU, the next I’m doing MRIs or seeing patients at St. Jude Children’s Research Hospital,” he says. “I touch every aspect of our division and get to see everybody in action, and that perspective helps me understand what each team needs to succeed.”
As he steps into the role of chief, Dr. Johnson’s vision is rooted in this commitment to expertise-driven care. His goal? That no child in the Mid-South with congenital heart disease should ever need to leave the region for treatment.
“We will continue growing the infrastructure and recruiting the right people so that every child can get the exact care they need right here at Le Bonheur.”
That growth includes planned 4D enhancements to the hospital’s Virtual Reality Lab, allowing physicians to practice procedures on simulated, beating hearts that emulate blood flow in real time.
Yet for all the groundbreaking advancements, Dr. Johnson remains focused on what matters most.
“New technologies are incredible, and it’s inspiring to see the progress in our field over the last few decades,” he says. “But the core of our work will always be those relationships with families, helping them feel seen, heard, and cared for. That’s what keeps me coming back.”


Dr. Hae Won Shin Shapes a Brighter Future
By Chris Green
When Hae Won Shin, MD, was a child in South Korea, she spent months in a hospital bed recovering from a congenital heart defect.
“When I was born, I had ASD, atrial septal defect,” she says. “These days, there is a very simple procedure to fix that, but back then, it was not that simple, especially in South Korea.”
That experience gave her an early and lasting exposure to medicine and the power of compassionate care.
“I’ve always wanted to help others, and I realized being a physician is the career that can make the most positive impact on others in the most vulnerable times,” Dr. Shin says. “So that’s why I decided to be a physician.”
Today, as chair of the Department of Neurology and Semmes Murphey Professor of Excellence in Neurology at the University of Tennessee Health Science Center, Dr. Shin is leading a transformation in neurological care in Memphis that she believes will spread throughout the state and beyond.
Dr. Shin’s interest in neurology began with her fascination for piecing together a diagnosis like a puzzle. “Typically, neurology is more of the detective work. You need to put all the pieces together to find the right diagnosis,” she says. “You need to have a clear understanding of the anatomy and network — how all the different parts of the brain, spine, and peripheral nerve and muscle work, and how these are all connected — to find the right diagnosis.”
She specializes in epilepsy, an area she says offers the perfect blend of acute and long-term care. “With epilepsy, we have the acute care aspect of it where we can help the patient in the hospital when they have severe acute seizures, but I can also take care of the patient in the long term to get their seizures under better control, improve their quality of life, and build a relationship,” she says.
Before joining UT Health Science Center in January 2024, Dr. Shin led advancements in epilepsy care in New Mexico and North Carolina. When she arrived in Memphis, she saw both a challenge and an opportunity to rebuild and expand the department into a comprehensive center for neurological care, research, and education.
“In the past, Memphis had an impressive neurological program and epilepsy surgery until the 1990s. But for the past few decades, some of the subspecialty areas faded away, and it became like a neurology desert other than acute inpatient stroke care,” she says. “Even though we have a world-renowned vascular neurology/ stroke program, when I came here, we did not have much other subspecialty neurology programs.”
Dr. Shin’s goal has been to build the department’s subspecialties, including epilepsy, movement disorders, neuroimmunology/ multiple sclerosis, and neuromuscular care, as well as further strengthen the stroke and neurocritical care program.
“That’s why I came here, and that was my vision — to build a comprehensive neurological program through the University of Tennessee Health Science Center by collaborating with our health
care partners — Methodist Le Bonheur Healthcare, Regional One Health, and Baptist Memorial Health Care,” she says.
The Department of Neurology has grown to approximately 40 faculty members who care for patients across subspecialties at all three partner hospitals. According to Dr. Shin, the people are the department’s greatest strength.
“We have amazing faculty, staff, and trainees, who are dedicated to providing the best care possible and advancing the science. Many of them are well-known, well-respected leaders in the field,” she says. “As a leader, I strongly believe that I need to serve people. I’m not here to tell people what to do; I’m here to serve and help people succeed. When they succeed, all of us will be in a better place.”
Education is also a cornerstone of Dr. Shin’s vision. In addition to training residents, the department engages with medical students, college students, and high school students to create a pipeline to neurology and address a looming shortage of health care providers.
For Dr. Shin, the impact of her work is most powerfully felt in the lives of her patients. She recalls a young woman with epilepsy whose life was transformed by surgery.
“She started developing epilepsy in high school. Because she was having multiple seizures a day, she could not do much after graduating. She became house-bound, and her family had to take care of her,” Dr. Shin says. “After surgery, she became seizure free and got her life back. She was able to go to college, then she earned her master’s degree. She was able to have a career while also raising a family. So, when I see a patient like that, I feel fortunate to be part of her journey and be able to help her. That just gives me a lot of gratitude and joy to be a doctor.”
With a continued focus on patient care, Dr. Shin is excited to continue leading advancements that will reach beyond Memphis. She is quick to credit her team, saying:
“To our patients today, I can confidently say that whatever neurological problem they have, they will get the best, most advanced care by our neurology team.”
As she looks to the future, Dr. Shin hopes the work she is doing today will serve as a foundation for years to come.
“I want to be the first leader in neurology to build up the everlasting, sustainable, most advanced neurological program in Tennessee,” she says. “Hopefully, we’ll build a good infrastructure and foundation so future leaders can come and build upon it more. I want UT Health Science Center to have a comprehensive neuroscience program that serves patients not just here in Memphis, but from all over the state and beyond, through the most advanced clinical care, cutting edge research, and innovative education.”
By Peggy Reisser
A spring break trip to the Kennedy Space Center 20 years ago set University of Tennessee Health Science Center College of Medicine alumnus Eiman Jahangir, MD, on a trajectory that eventually launched him into space.
“I always had two passions,” says Dr. Jahangir, 45, now a professor of medicine and radiology and the director of the sections of general cardiology and cardio-oncology at Vanderbilt University Medical Center.
“It was medicine, and it was space, and I was able to pursue the second passion once I became a doctor.”
A 2005 graduate, he says the College of Medicine was the launchpad for both.
On August 29, 2024, Dr. Jahangir was a member of a six-person team of commercial astronauts onboard Blue Origin’s New Shephard rocket for a 12-minute, sub-orbital flight that climbed approximately 70 miles into space before returning to earth. He was selected by MoonDAO, an organization that supports space exploration, from more than 2,200 applicants for the life-changing excursion.
“I was the 704th person to ever go into space, and still less than 800 people, I think, have ever done it,” he says. “I was actually the first physician on a commercial spaceflight.”
It was a wild ride, for sure. Here’s how Dr. Jahangir describes it.
“It was surprisingly smooth going up; the rockets light up, and the whole inside of the capsule reflects the orange flame of the rocket,” he says. “It takes about seven seconds before the thing has enough power and thrust to lift off. So, you’re sitting on top of that rocket, you hear the countdown, it gets down to one and then zero, and then you hear the engine roar, and after seven seconds you just start lifting off into space.
“I think maybe it’s a little shaky, but you’re probably so excited that you don’t know it,” he continues. “It didn’t feel particularly shaky coming
back down. It definitely sounded loud. You could hear kind of like the whooshing as you’re coming back into the atmosphere. And it felt like an elephant sitting right on my chest. And you’re just saying, ‘OK, let’s hope these parachutes open up.’”
Dr. Jahangir is equally descriptive when he speaks of UT Health Science Center’s pivotal role in setting the course that led him to space.
“In 2005, right before I was graduating medical school, my family and I went down to the Kennedy Space Center, and I was looking at the rockets, and it just kind of rekindled that interest and desire,” he says. “I ran back to the hotel room, looked online to see what the requirements were to become an astronaut, and realized I met the requirements because of my training at the University of Tennessee. By getting the medical degree, that was enough to be able to apply.” He waited until 2008, when the first application cycle became available, and applied, making it as far as the finals.



Dr. Jahangir proudly wears the flight suit from his trip to space, top photo, but his journey into space started when he was in medical school at UT Health Science Center, photo below left, during a trip to the Kennedy Space Center shortly before graduation, photo below right.

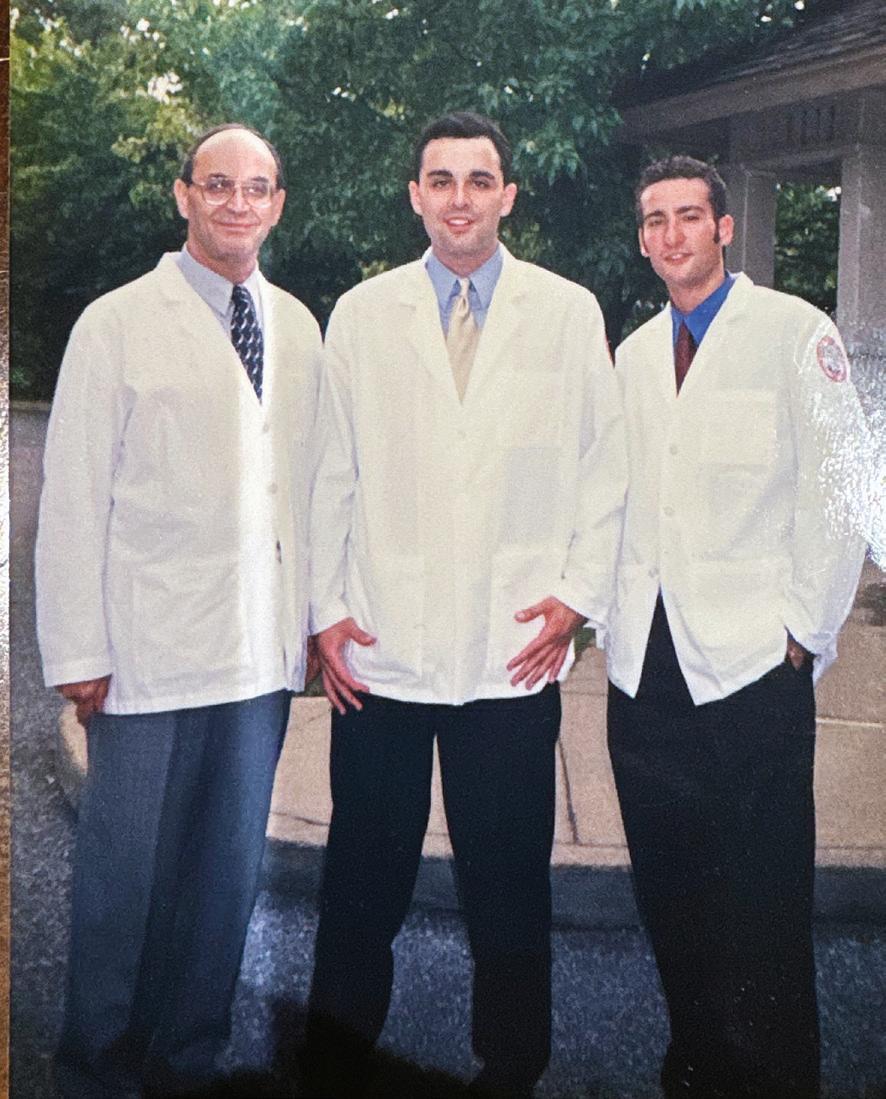


In total, Dr. Jahangir has applied to NASA five times to become a U.S. astronaut and made it to the finals twice.
Dr. Jahangir says his training in the College of Medicine equipped him to think independently and keep a level head and steady heart when faced with complex situations — all assets on his Blue Origin trip.
“When I was in medical school, we did a lot of work at The Med (now Regional One Health). So, you had a lot of experience managing patients and figuring out complex situations, because people would come in who had not had medical care for a long time and they’d come in with just very progressed or complex diseases,” he explains.
The proximity to St. Jude Children’s Research Hospital and opportunity to participate in research as a medical student helped guide him toward his specialty in cardio-oncology.
“One of the biggest things that the University of Tennessee did, that I don’t think happens at all health science centers or medical schools, is it gave a very strong sense of independence in both learning and practicing as a student.
“That independence leads to increased confidence. And that leads to, hopefully, becoming a better physician.”
He says the College of Medicine also provided him with a group of friends who have stayed in touch, even 20 years since graduation. “I think it is very important that you have those people that can support you through good times and bad, tell you that maybe your idea is crazy, but still be there to lift you up,” Dr. Jahangir says. “And I think the University of Tennessee Health Science Center provided that, because it was a very collegial environment, and it was a place that we could all learn together, work hard together, and build those connections and community together.”
One friend from medical school, Joe Mobley, MD, MPH, a urologist and chief of staff at West Tennessee Healthcare – Henry County Medical Center in Paris, says he and Dr. Jahangir bonded early in medical school over outside activities that helped them de-stress.
“Medical school can be challenging in and of itself, and for the most part, each of us was laser focused on the next step ahead: the next exam, the next lab, the next clinical task,” Dr. Mobley explains. “Despite this, Eiman had a variety of alternative interests and did communicate early on his love for space and a desire to be a future astronaut.
“Beyond his initial space flight, he is using his intelligence, kindness, and charisma to share his passion and path with children and others who have high aspirations. He is the perfect role model for
balancing a career, while still chasing your dreams and creating the life that you’ve dreamed of.”
Back on terra firma in Nashville, Dr. Jahangir’s spaceflight has served as a vehicle for outreach to promote STEM education and careers in medicine. “I just got back from Brazil. We spent a week down there with a not-for-profit and went to hospitals with kids with cancer, and we did art with them. All that art is going to be sent up to space on a Soyuz rocket in November.”
Dr. Jahangir worked for Blue Origin for six months after the spaceflight as an astronaut trainer and in Mission Control doing capsule communication. In addition to his clinical duties at Vanderbilt, he speaks to students, works with companies on aerospace technologies, and lectures on aerospace medicine.
“It’s great, because it’s always been one of my goals to excite kids and motivate the next generation.”
Scan the QR code to view a video of Dr. Jahangir talking about his space flight.

Neither the ascent nor descent portions of the short flight were particularly shaky, Dr. Jahangir said. Though coming down, “It felt like an elephant was sitting right on my chest.”
By Allyson Lawson
For many former medical students at the University of Tennessee Health Science Center, their inaugural course and pivotal gross anatomy subject also equate to the cherished Jack Wilson, PhD. From his teaching style and compassion to his calm and forward-thinking, more than 14,000 medical students have experienced his skilled and impactful pedagogy.
“I didn’t realize my career would be anatomy at first,” Dr. Wilson says of his journey into teaching; the education spark was ignited when he had a freshman biology teacher. “He always taught so well, and I thought if I was ever going teach, I would like to be like that.”
The university recently named Dr. Wilson, now an emeritus professor, as the 2025 Honorary Member of the College of Medicine Alumni Council. He retired in 2015 after 47 years at UT Health Science Center, though he still teaches now and then.
Born and raised in North Mississippi, he went on to attend the University of Southern Mississippi, then graduate school at the University of Mississippi Medical Center. After his PhD program, he accepted the position in the Department of Anatomy and Neurobiology at UT Health Science Center. The institution promoted him to professor in 1990, and he received the Distinguished Alumni Professor of Anatomy title in 2000. Dr. Wilson was also the gross anatomy course director for 27 years.
The heralded professor says one of the highlights of his career was the privilege of teaching medical students, having taught each one who came to UT Health Science Center all those years. He has about 140 letters previous students have given him with stories about their experiences, how much the course meant to them, and how much he motivated them.

“It was always a challenge, because I was the first person they’d see on the first day of medical school, the first class they’d come into.
“I always try to encourage them to not feel discouraged when maybe a grade or class doesn’t go the way they want. My philosophy was always, let the class know what they need to know in clinical anatomy. Make sure they understood. Lead them with firmness, but you also lead them with compassion. I was trying to get them to adjust to the emotional stress that’s there. With every one of them sitting there that first day, nervous and scared, I always tried to tell them, do the work one day at a time.”
At his retirement ceremony, opening remarks jokingly made clear how if a student was sitting through one of Dr. Wilson’s famously enriching lectures and paying any sort of attention — and you didn’t find you understood things pretty well by the end — well, you really had to be dumb as a post.
Dr. Wilson was there for his students. He would make concessions for specific ones when there was a major family issue, death, illness, or injury. Sometimes they ended up in the hospital from an accident or disease, and he would go over to the hospital and see them.
“Often over the years, I listened and talked to a number of students, keeping them from dropping out of school in their first year because of grades or many other reasons. I knew they could do it. Most of them at a later time let me know how appreciative they were of my encouragement for saving their careers.”
One time on the sidewalk, Dr. Wilson ran into a couple students who had skipped class. He asked them where they were headed. They admitted they didn’t go to class. He said they were missed and asked again where they were off to. They said breakfast and he responded, “OK, let’s go!”
Of his many teaching awards, Dr. Wilson says, “Those never got old. Every one of them was very appreciated. I was very thankful I had the opportunity to have a little bit of imprint in their lives. Awards were not old hat. Every one was unique and I was grateful for. Among those, there was one award I won 13 times, from the senior fourth-year graduating class.”
The university eventually discontinued the award, probably because he got it every year.
“Forty-seven years,” he says, reflecting. “What did I do? All I did was what I loved to do. I did what I thought I needed to do and how I needed to do it. Not for the awards but what students needed. The reward was kind of a dessert plate.”
The students certainly showed their gratitude for his teaching, awarding him about 70 teaching awards over the years, the most of any faculty at UT Health Science Center.
These awards include many Golden Apples and best first-year medical student course director awards. Dr. Wilson additionally served on many UT Health Science Center committees, including nine years on the admissions committee and several curriculum planning committees.
“I always took those committees very seriously. We were designing curriculum…that would be impacting their medical career but also impacting their daily lives. We wanted to provide a foundation in clinical anatomy, but at the same time it had to be something manageable on their end. Anatomy books would be 1,200 pages long, and there’s no way a student can learn all that. We would need to lead them. There were tremendous faculty members I worked with. It was always a team approach.”
The veteran professor realized it might be time to retire when he was teaching the grandchildren of former students, when students started to say a grandparent said to tell him hello.
Married to his wife Rosemarie for 60 years, they live in Southaven, Mississippi, and have three children, eight grandchildren, and 13 greatgrandchildren, almost all local.
“Almost every one of my children and now great-grandchildren are going to a pediatrician I taught. They always have to have a discussion about me before they look at the kid.”
Seeing former students who are now successful practicing physicians is most rewarding, he says.
“My wife always has a joke when we’re traveling across Tennessee. She says, how long is it going to be before some former student recognizes you?”
He can recognize faces but can’t remember all names, though he says they’re always kind enough to remind him and tell stories.
“That’s the reward, when you see the result of all your hard work.”
Dr. Wilson has nearly 150 letters from students, thanking him.
“One guy. Hundreds of surgeons. Thousands of patients.”
“Immense good you have done through one of the most fundamental courses in medical training.”
“You were my teacher but at that moment and others, you were a great mentor and friend.”
“The intelligent yet gentle professor, who helped ease my transition into the rigorous medical school curriculum.”
“We can all say Dr. Wilson has made us better as physicians.”
“Kindness, patience, and easy-going teaching style.”
“Words cannot begin to express the immense impact you had on not just me but the countless faces of young students.”
By Allyson Lawson

“Throughout my career, I’ve always felt you can accomplish more as a group.”
– Dr. John Howington
When someone is a cardiothoracic surgeon, has authored publications, held leadership and teaching roles, presented internationally, been listed in “Best Doctors in America,” trailblazed cancer prevention and treatment, and helped raise a family, you might think that person grew up surrounded by degrees and overflowing with confidence.
“Kind of the opposite,” says John Howington, MD, MBA, FCCP, FACS, a UT Health Science Center College of Medicine alumnus and practicing thoracic surgeon currently at Virginia Mason Franciscan Health, St. Michael Medical Center in Silverdale, Washington.
Dr. Howington grew up in the Nashville area, the youngest of eight. His father served in World War II in a submarine, later suffering from posttraumatic stress disorder and alcoholism. Attributes common to these illnesses led to his parents’ divorce before his 5th birthday. His mother rejoined the workforce after 20 years.
“She was my first example of servant leadership,” he says. “No one worked harder. She provided a loving home and a spirit of kindness to others.”
When he was in second grade, the school participated in a research project involving IQ testing. His mother was called to the school, and she thought it must be something mischievous like with her older boys. Instead, she learned her youngest was gifted.
“So, from that point forward, her expectations of my scholastic achievement were much higher,” he says.
His father was a pipefitter. His uncles were plumbers. His grandfather was a plumber. No male in his generation had finished college. But he kept working hard, learning from his community at church and from teachers how to care, apply yourself, and not focus solely on good grades but mastering a subject and achieving.
People started asking him what he wanted to be. He said a doctor, with no real reference other than TV, or when he was little and had seen his sister’s newborn baby in the hospital.
“Because of my background, a lot of people told me, ‘You’re a Howington; you aren’t meant for college. You’re not smart enough. You should think about trade school.’ But my mother believed in me. My siblings believed in me. And my friends and their parents believed in me. It was that love and support that carried me through my darkest hours of self-doubt.”
As to the naysayers, Dr. Howington says they became a driver, and he wanted to prove them wrong. He earned his undergraduate degree from Tennessee Tech University, where he met lifelong friend Max Moss in the fall of freshman year. They became fraternity brothers and later medical school roommates in Memphis.
Max Moss, MD, is a UT Health Science Center alumnus and diagnostic radiologist in Murfreesboro with Ascension Saint Thomas Rutherford Hospital. Dr. Moss says their careers crossed when they served together on a key lung cancer committee, where he saw firsthand Dr. Howington’s leadership capabilities.
Additionally, Dr. Moss’ son was in his first year of college when he acquired a life-threatening pulmonary complication.
“It was John who we trusted to operate and bring him back to good health,” Dr. Moss says.
When he completed medical school, Dr. Howington began seeing more patients and starting a family. Medicine became a way to help people, earn a living, and be a better man for his children, he says. He admits, though he’s not extremely competitive, his fellow students and colleagues drove him to improve and never remain stagnant. Surgery appealed to him and was “invigorating; they were the sickest patients.” He also met his wife, Anne, a nurse, on the second day of his University of Missouri-Kansas City residency in ICU room 322.
Dr. Howington at his UT Health Science Center graduation in 1989.

Researching what surgical specialty to pursue, he learned there were too few thoracic surgeons in America, and he found that unmet need to be a calling. However, he heard from the naysayers again — how a different surgical specialty could make 50% more money. He didn’t care; he knew what he wanted to do.
Dr. Howington matched at Vanderbilt University for a thoracic residency. A couple years after finishing, he was recruited to be a division chief at the University of Cincinnati.
That area, just like other parts of the country, was starved of a thoracic surgeon. Dr. Howington helped build a team, a training program, and widened the specialty’s leadership, as well as pioneered minimally invasive thoracic surgery.
In the past, if you had an operation on your lungs, Dr. Howington says doctors would make a large incision and open your chest like a mechanic opens a car hood. So, he sought additional training and learned how to do it with small incisions and a scope.
“I couldn’t stand having patients come back to the office, not able to stand up straight from the pain of the operation. That minimally invasive approach allowed them to have more normal function sooner. It reduced complications.”
Dr. Howington and his team taught others, those already practicing and residents. He says it was hard work, but the focus was on the patient. The less-invasive operation initially paid less, and people brought that up. Yet that didn’t deter the focus.
Because of his efforts and following exposure, he was recruited to Chicago to lead thoracic surgery. He was able to amplify his impact further through a large hospital system, its leadership, guidelines, tools, and a process that echoed through physicians to tens of thousands of patients.
The American Cancer Society states lung cancer is the second most common cancer in the United States and the leading cause of cancer death. Each year, more people die of lung cancer than colon, breast, and prostate cancer combined.
When Dr. Howington’s hometown called — and plenty of people would call him over the years — he knew Tennessee was in the top three for lung cancer death rates. (It’s not in the top anymore, he says.) He knew there was a need.
Like the rest of America, fewer than 10% of people were undergoing screenings, a measure that would reduce their risk of dying by 40%, Dr. Howington says. When he joined Saint Thomas Health in Nashville, the group was doing fewer than 15 screenings a week. He put that into perspective, saying that’s like a woman getting a mammogram and being one of only two or three patients that day. The team raised those screenings by more than 100 screenings a week.
The team also worked to gain private and public funding to take mobile CT scans into rural counties, changing lives free of charge.
Moreover, just last summer, the Supreme Court ruled to affirm that preventive services recommended by the U.S. Preventative Services Task Force, including lung cancer screening, must continue to be covered by most insurance plans at no cost to patients. Dr. Howington was part of that group effort through his work with the American College of Chest Physicians.
He is continuing to work to increase screenings everywhere in the same way individuals get mammograms and colonoscopies. He and his colleagues have already stage-shifted lung cancer, which aids survivability, and are continuing to develop newer, targeted therapies to improve overall lung cancer survival.
Most recently, Dr. Howington received his Physician Executive MBA from the University of Tennessee, Knoxville. He had heard it was a well-regarded program, and he liked that it was tailored to physicians. Dr. Howington is also presently serving as president of the American College of Chest Physicians.
“Throughout my career, I’ve always felt like you can accomplish more as a group,” he says, and he feels humbled to be recognized among his peers with a recent Outstanding Alumni Award from the UT Health Science Center College of Medicine.
“The College of Medicine gives you an outstanding clinical experience,” he says. “In your third and fourth year, you’re fully engaged in the care of patients. You’re there at the bedside. You’re scrubbed in the operating room. It was a hands-on, immersive experience.”
He gives examples of being able to make incisions, place chest tubes, and resuscitate. When he showed up as an intern later in general surgery, he had a head start, and that gave him an opportunity to do more in the operating room than his peers, he says.
“It gave me confidence that I had the skillset to be successful. It was the foundation for thinking I could do something beyond general surgery training, and entertaining doing cardiac and thoracic surgery.”
From brilliant surgeon mentors to instilling a desire to give back to academia and stay connected to the advancement of the profession and each other, Dr. Howington says those things helped him learn how to accomplish more for patients, based in science, even in challenging times.
When Dr. Howington and his wife moved to Washington as empty nesters wanting to enjoy the mountains, he left Tennessee with more thoracic surgeons than ever. All good people, all doing good work, he says.

Colorado.
“I am proud to be an alumnus of UT Health Science Center, and I look forward to continuing to contribute to its legacy…And I wasn’t supposed to be here. I was that poor kid, walking the streets of Nashville, a pipe-fitter’s kid.”


Born in Fürth, Germany, to a German mother and an American father, Natascha Thompson, MD, didn’t grow up dreaming of a career in medicine. After moving to the United States as a young child, she spent her formative years in Knoxville, where dance training filled her time outside of school.
“Dance was always a big part of my life,” she says. “I spent hours each week pursuing my training. Dance taught discipline, time management and teamwork — all skills that have served me throughout my schooling and career.”
Today, Dr. Thompson deploys those same strengths as she balances the rigor of a clinical internal medicine practice with more than 20 years on
By Aimee C. McMillin
the faculty at the UT Health Science Center College of Medicine, which recently honored her as a 2025 Outstanding Alumna.
During her undergraduate days at the University of Tennessee, Knoxville, Dr. Thompson was a member of the UT Pom Pon Squad, performing at games (“before scholarships were a thing for Pom team members,” she says) while maintaining her classical dance training. Starting as a business major, she soon realized her real strengths were in science, not spreadsheets, and switched to biology.
“I didn’t set out to be a doctor,” she says. “I just knew I loved science and excelled at it. I took the MCAT, thinking, ‘Why not?’ And before I knew it, I was heading to Memphis for medical school.”
That instinctive decision set Dr. Thompson on a lifelong career journey with the University of Tennessee System. After earning her medical degree from the College of Medicine in 1998, she searched far and wide for the best Medicine-Pediatrics (Med-Peds) residency program. She found none better than where she was. After she completed her internship and residency training at UT Health Science Center, Dr. Thompson stayed for a chief resident year in internal medicine. That formative experience introduced her to the administrative side of academic medicine.
“It shaped my path toward leadership,” she says. “It was my first real exposure to how programs run, how residents are supported, and how academic medicine functions beyond training.”
In 2003, Dr. Thompson joined the UT Health Science Center faculty as program director of the Medicine-Pediatrics residency and associate program director of Internal Medicine. Over the next 14 years, she grew the Med-Peds program into one of the largest in the nation, a testament to her commitment to both rigorous training and compassionate mentorship. In 2019, she was named associate dean for Graduate Medical Education (GME) at the College of Medicine, overseeing more than 70 ACGME-accredited residency and fellowship programs across Memphis, Nashville, and Jackson.
“It’s easy to support the mission of the College of Medicine. We train health care providers for the state of Tennessee. That’s what keeps me motivated every day.”
Dr. Thompson also points to the people as one of UT Health Science Center’s greatest strengths. “I’ve developed lifelong relationships here with colleagues, mentors, and my patients,” she says. “I’ve worked with many of the same physicians for nearly two decades in my practice. It’s a phenomenal group, and I feel fortunate to be part of it.”
Her clinical practice in internal medicine is through University Clinical Health, based at Baptist Memorial Hospital, where she has often cared for generations of families. “There’s incredible satisfaction in long-term patient relationships,” she says. “I have patients I first saw in their 50s and 60s, who are now in their 80s and 90s. I’ve cared for their children, too. That continuity is one of the joys of primary care.”
As associate dean for GME, Dr. Thompson plays a pivotal role in advancing the College of Medicine’s statewide mission. Her leadership ensures that residency programs not only meet accreditation standards but also respond to Tennessee’s urgent health care workforce needs, especially in rural areas where physician shortages are critical.
That mission is taking a significant step forward with the launch of a new residency partnership in Maury County in rural Middle Tennessee. UT Health Science Center’s collaboration with Maury Regional Health in Columbia marks a unique and vital investment in rural health. “This partnership is really inspiring,” Dr. Thompson says. “This is Maury Regional’s first residency program, and it has the potential to make a long-term impact on that community and the state.”
The three-year internal medicine residency will welcome its first class of 10 residents in July 2026. On maturation, the program will have 10 trainees per year with a total of 30 trainees during the three-year residency program at any given time. The goal is to train and inspire hundreds of new physicians over the next 20 years.
“Tennessee, like many states, faces a shortage of rural health care providers,” Dr. Thompson says. “By expanding training opportunities in communities like Columbia, we’re creating pathways for physicians who want to serve in these areas, plus we’re strengthening access to care for Tennesseans who need it most.”
The Maury County program reflects UT Health Science Center’s statewide model for medical education. While the College of Medicine’s home base is in Memphis, its reach extends across Tennessee through campuses in Knoxville, Chattanooga, and Nashville, and through partnerships in hospitals and health systems statewide.
“Our clinical training is incredibly robust because of those partnerships,” she says. “Residents rotate through a wide range of hospital systems — county, private, VA, and children’s hospitals — which exposes them to diverse patient populations and system structures. That diversity in training makes our graduates exceptionally well prepared.”
It’s a model she experienced firsthand as a trainee and one she now helps sustain. “When I completed my residency, I felt my training at UT had equipped me with the skills to handle most clinical situations,” Dr. Thompson says. “The depth and breadth of the clinical experience is one of UT Health Science Center’s strengths.”
Reflecting on her tenure with the university, Dr. Thompson has seen academic medicine evolve dramatically. The shift from paper charts to electronic medical records, the implementation of more rigorous accreditation standards, and an increased emphasis on work-life balance for trainees have all reshaped the field. She is also optimistic about the role of innovation, including artificial intelligence, in helping physicians manage the growing administrative and data demands of modern practice.
What hasn’t changed, she believes, is the heart of medicine. “Our students and residents still come to this profession because they want to make a difference,” Dr. Thompson says. “That commitment to service and helping others drives them.”
For her, the mission is also personal. “I’ve been part of the UT System since 1989,” she says. “It’s been an incredible journey. UT has been great for me, and I hope I’ve been good for UT. I’m proud to have dedicated my career to training physicians who will care for the people of Tennessee.” This dedication was recognized with a 2025 President’s Award, the highest honor the UT System gives to employees, in the Transparent and Trusted category.
When she’s not in the clinic or guiding the next generation of doctors, Dr. Thompson is often found near a ballfield, either cheering for her three sons or for the Tennessee Volunteers baseball team.
“It’s funny,” she says, “I started my UT journey dancing on the sidelines, and now I’m still cheering for Tennessee, just in a different way.
“Life has taken me where I’m supposed to be.”
By Aimee C. McMillin
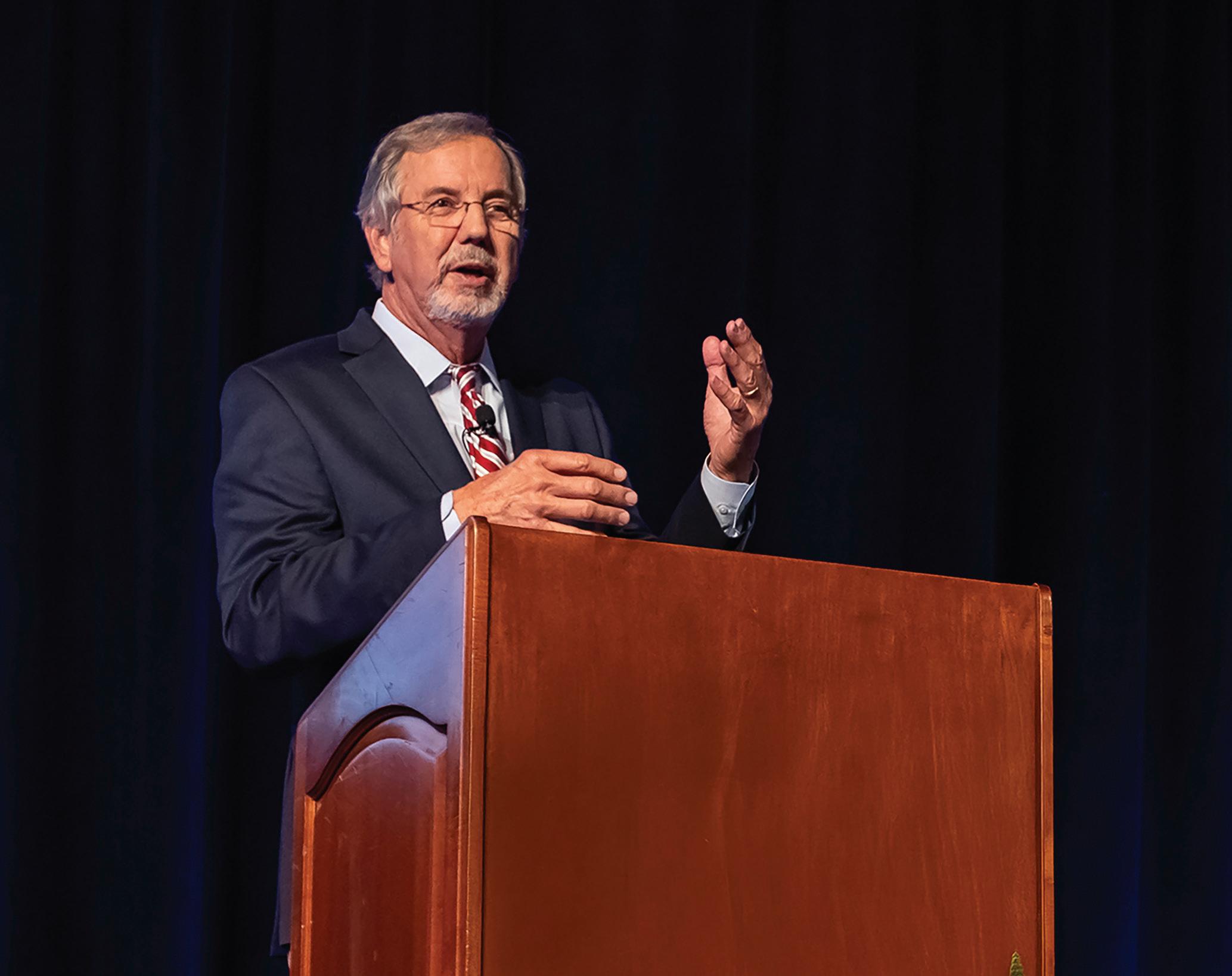
Other than his teachers, H. Lynn Massingale, MD, knew only one professional in his small hometown of Etowah, Tennessee: the town’s do-it-all family doctor, Herbert Whittle, MD. Growing up on his family’s farm in the foothills of the Smoky Mountains, he didn’t know what it took to become a doctor; he just knew he wanted to be the next Dr. Whittle.
Today, Dr. Massingale is co-founder and chairman of Knoxville-based TeamHealth, a physician-led, facility-based practice comprised of 18,000 affiliated physicians, advanced practice clinicians, and integrated operational team members, which cares for more than 29 million patients each year. From his early days on the farm to guiding TeamHealth’s national growth, Dr. Massingale’s journey is one marked by hard work, good timing, and deep gratitude for the education, support, and training he received at the University of Tennessee Health Science Center College of Medicine.
Dr. Massingale is quick to credit others for the encouragement and partnership that have fueled his many professional achievements, including his recent recognition as a 2025 College of Medicine Outstanding Alumnus.
“I was the first person in my family lucky enough to go to college,” Dr. Massingale says. “I grew up poor but not hungry. After high school, I didn’t think college was an option, so I considered working for the railroad. But the local hospital administrator called me and said, ‘I can’t get you the money for college, but if you can get through undergrad, I can get you the money for medical school.’”
That promise changed his life. After Dr. Massingale graduated from Tennessee Wesleyan College (now University) in nearby Athens, Woods Memorial Hospital kept its word. “They loaned me the money to study at UT Health Science Center in faraway Memphis. Dr. Whittle’s influence and the hospital’s belief in me made medical school possible.”
Coming from rural McMinn County, arriving on UT Health Science Center’s Memphis campus in the 1970s was “a bit of culture shock,” he says. “It was a huge adjustment, not only to city life, but to the campus and all that the College of Medicine offered.” He was awed by faculty like Gene Stollerman, MD, who “literally wrote the book on streptococcal disease”; Philip George, MD, head of pediatrics; Jim Pate, MD, in surgery; and Pat Wall, MD.
“At the College of Medicine, I interacted with people who knew everything I wanted to know — physicians, non-physician clinicians, and educators,” he says. “It was an incredibly nurturing environment.”
Upon graduating in 1977, Dr. Massingale planned to stay in Tennessee and follow in Dr. Whittle’s footsteps. After his rotations, however, he decided to pursue internal medicine. During his residency at what is now UT Medical Center in Knoxville, an emerging specialty caught his attention. “I did ER rotations and became totally intoxicated by emergency medicine,” he says. “Every case was different. You never knew what was next. I liked the variety, the pace, and the breadth of knowledge it required.”
At the time, emergency medicine was in its infancy. “Most hospitals didn’t have dedicated ER physicians,” he says. “A charge nurse would call whatever doctors were on duty. But a few years earlier, a group of doctors in Michigan said, ‘We’ll do this full time. We’ll run the ER and call specialists when needed.’ That was the beginning of emergency medicine.”
By 1978, Dr. Massingale was working full time in the ER. When the American Board of Emergency Medicine began its certification process, he earned his credentials based on both his clinical hours and board exam results. Soon after, Dr. Massingale began building a pioneering organization in the field of emergency medicine.
“I’d love to say we had a great business plan,” he says, recalling the early days of what became TeamHealth. “But 100% of the plan was two hospitals, UT Medical Center in Knoxville and LeConte Medical Center in Sevierville. They needed more and better doctors, and we decided we could help.”
Word spread quickly. Hospitals around East Tennessee wanted help with staffing their ERs. “We drew a two-hour circle around Knoxville and said, ‘That’s our universe — two hours in front of a problem, two hours in front of an opportunity,’” he says. “We worked hands-on as doctors in those hospitals, and on off days, worked on the business.”
That two-hour driving radius expanded, first to where Dr. Massingale could fly in his 37-year-old plane, and then nationwide. Within 15 years, TeamHealth had become one of the largest integrated physician practices in the country. “By that point, we knew we could do it nationally, and we brought in a non-physician business partner and did a ‘real’ business plan,” he says.
Under Dr. Massingale’s leadership as CEO until 2008 and chairman today, TeamHealth earned many recognitions, including as one of “America’s Most Trusted Companies” by Forbes and one of the “World’s Most Admired Companies” by Fortune. The company has been named one of Newsweek’s “America’s Greatest Workplaces” and Becker’s “150 Top Places to Work in Healthcare.” Dr. Massingale himself was honored with distinctions, including one of Modern Healthcare’s “Top 100 Most Influential People in Healthcare,” an American College of Emergency Physicians “Hero of Emergency Medicine,” and a 2018 inductee into the Tennessee Health Care Hall of Fame.
Yet, Dr. Massingale remains deeply humble. “Any honor I receive is really an honor for TeamHealth and for everyone who helped us achieve our success,” he says. “I’ve been fortunate to have a loving
and supportive family, great teachers, and dedicated colleagues. I’ve had the privilege of working as part of incredible teams.”
He remains deeply connected to the mission of the institution that launched his career.
“The College of Medicine produces the health care professionals our state so desperately needs,” he says. “That is the foundation of why it is so important. But the research, training, and collaboration at UT Health Science Center have a ripple effect that touches lives across the state.”
For Dr. Massingale, UT Health Science Center not only transformed his own life, but continues to shape the future of health care across the state and beyond. “If you train in a place, you’re more likely to stay there,” he says. “That’s why growth at the College of Medicine is crucial to Tennessee’s future. We need more doctors, nurses, physician assistants, and certified registered nurse anesthetists than ever before. The national demand has exploded, and our pipeline needs to keep up.”
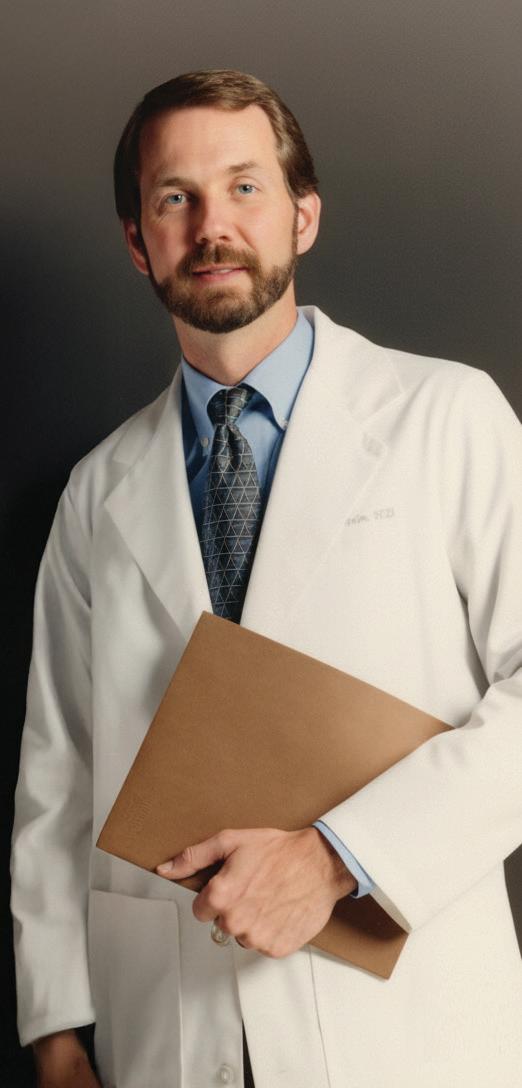
Dr. H. Lynn Massingale feels UT Health Science Center transformed his life and shapes the future of health care across Tennessee and beyond.
Even after decades in business leadership, he still considers himself, at his core, an emergency physician. During the COVID-19 pandemic, Dr. Massingale returned to clinical care as a telehealth doctor through TeamHealth, reconnecting with the field that first inspired him.
Looking back, he is grateful to the one small-town doctor who sparked his path and to the community for investing in him.
“For me, UT Health Science Center meant everything. It was a bridge between being a farmer and being a doctor.
“There’s nothing wrong with being a farmer, but I wanted to be a doctor.
“I’ve been fortunate to have a career that’s allowed me to serve patients, support physicians, and give back to the profession that gave so much to me.”
By Peggy Reisser
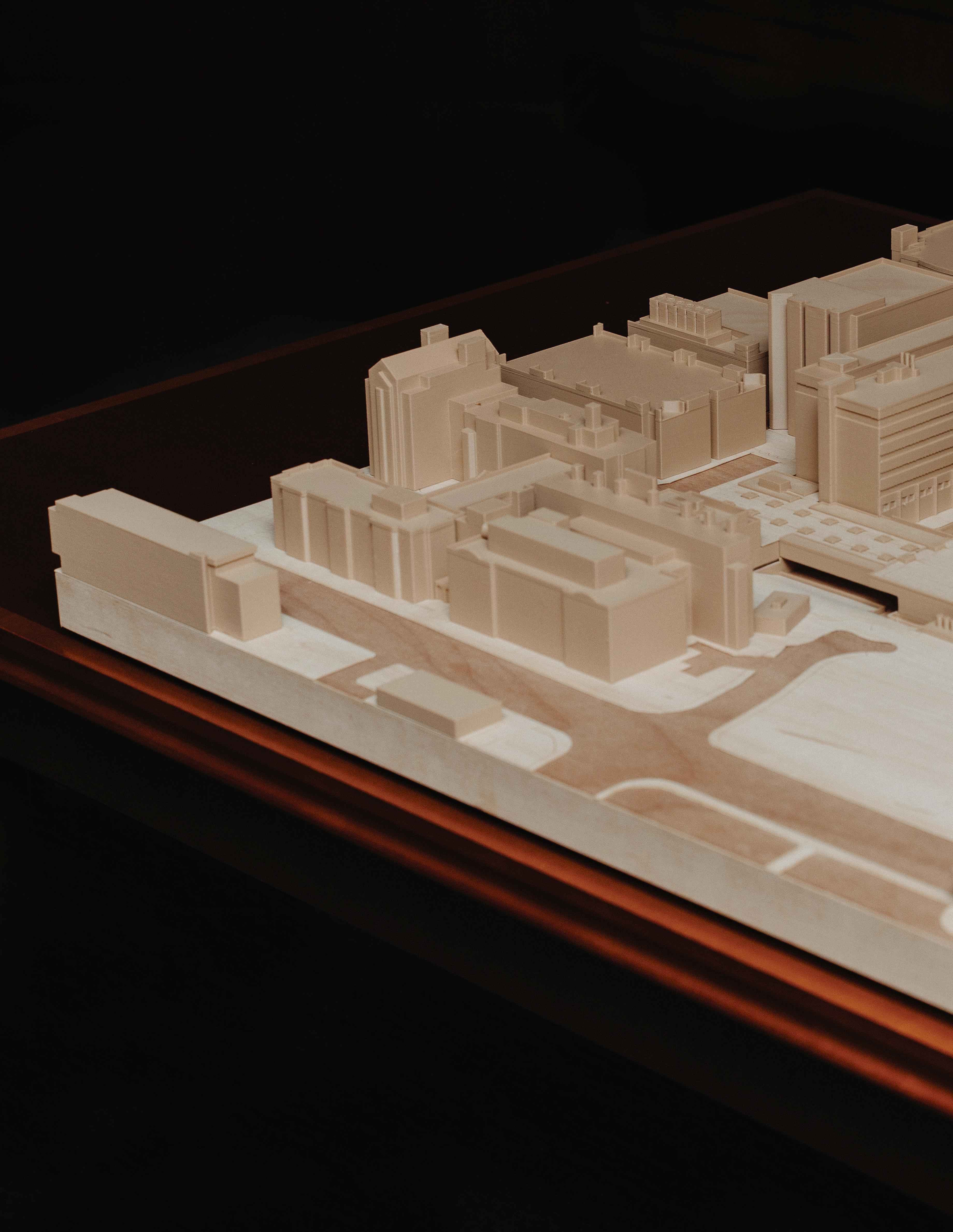
When a group of state leaders toured the University of Tennessee Health Science Center’s Memphis campus recently, the elevator they were taking from the College of Medicine on the 10th floor of the 910 Madison Building stalled during the descent.
The brief malfunction was evidence of what students, faculty, staff, alumni, and partners know — the building that houses Tennessee’s only statewide public academic medical school is past its prime.
A new $350 million building is proposed for the Memphis campus to house the College of Medicine and serve as a hub for training future health care professionals to practice collaborative, state-of-the-art care. This project requires multiple funding sources, including state/public support and significant private philanthropy.
Appropriately named the College of Medicine Interdisciplinary Building (COMIB), it represents “an investment for Tennessee,” said Executive Vice Chancellor and Chief Operating Officer Raaj Kurapati, who is leading the project.
“This is an investment in continuing to meet the significant deficit in physicians and physician assistants in the state of Tennessee, with projections suggesting that there will be a need for 6,000 additional physicians in the state by 2030.” Additionally, demand for interdisciplinary roles is expected to grow, such as nurse anesthetists by 40% and physician assistants by 28%.
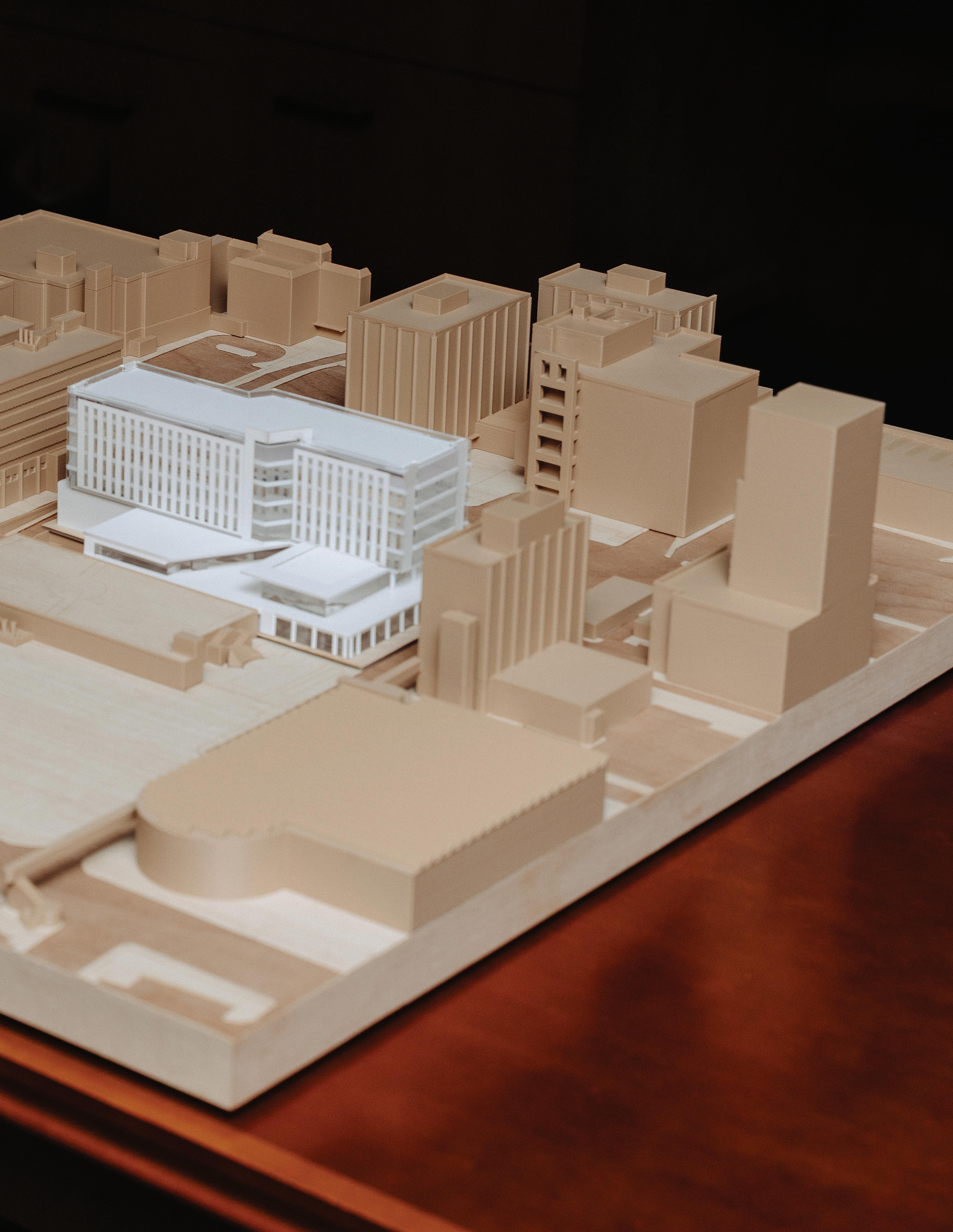

Initial planning aims to optimize workspace, allow for growth and increased public-private partnerships, and facilitate more internal and external collaborations.
The proposed building allows room to expand the medicine class from 175 to 225 per cohort. There will also be space for the Physician Assistant Program to grow from 30 to 60 students a year.
New technology will facilitate interdisciplinary training. A specialty simulation space will allow for collaborative disaster and emergency response training, as well as other scenarios that demand health care providers in different fields to work together seamlessly. The building will also provide a hub for telehealth training in multiple fields.
State-of-the-art technology will support an increase in the use of online educational opportunities for the College of Medicine and other colleges and allow for eventual increases in the number of academic certificate programs and enrollment in those programs.
The building is expected to enhance the university’s response to rural health care challenges in Tennessee, expanding medical education, rural health training, and multidisciplinary team care.
Once constructed, the new facility will enable the university to graduate an additional 1,450 health care professionals practicing in various fields over its first five years of operation.
Currently, the College of Medicine is housed in the 910 Madison Building, which along with the 920 and 930 Madison Buildings comprise the Madison Plaza complex on the south side of Madison Avenue. Built in the 1960s as hospital and hotel space, the complex was donated to the university by Baptist Health Care System when it reduced its footprint in downtown Memphis.
“Our folks have done a commendable job over the years at trying to make the best use of that space to accommodate our colleges,” Kurapati said. “The space was not built to accommodate the needs of learning, to accommodate teaching, to accommodate clinical support and service for an academic setting.”
The new building would be situated across from the Madison Plaza between the College of Pharmacy Building at 881 Madison and the old Holiday Inn at the corner of Madison and Pauline Street, which is being demolished.
“We have a home for the College of Nursing, we have a home for the College of Pharmacy, we have a home for the College of Dentistry,” Kurapati continued. “Our largest college is the College of Medicine, and we don’t have a home for them that’s specifically dedicated to them.”
The project is the UT System’s No. 1 capital priority for 2026, recognizing UT Health Science Center’s statewide vision to improve overall health in Tennessee, which currently ranks near the bottom for health outcomes.
University leaders have been making the case for the new building with state government and legislative leaders, presenting the current state of the College of Medicine space versus that of the college’s competitors for faculty and students.
“This building is not only about ensuring that we have the type of spaces that our students deserve, modern learning environments, appropriate technology incorporated into the dynamic didactic and clinical settings that our students should rightfully have access to, but it’s also about ensuring that we’re able to stay current with the competition,” Kurapati said. “We are significantly behind the competition when it comes to the type of facilities that are out there and available currently to students seeking to pursue a career in medicine.”

UT Health Science Center has hosted key members of Governor Bill Lee’s administration and members of the State Legislature, as well as numerous business and community leaders, and friends of the university. This project requires multiple funding sources, including state/public support and significant private philanthropy.
“This is an investment in the state of Tennessee, as while the UT Health Science Center’s home campus is in Memphis, it carries out a statewide mission through campuses in Chattanooga, Nashville, Knoxville, and nearly 800 clinical sites across the state,” Kurapati said.
A strategic space inventory of the campus was done prior to the initial programming for the building to determine how it could support the current campus infrastructure and meet future needs.
HOK, a global design, architecture, engineering, and planning firm, conducted the inventory and designed the programming for the proposed building.
In August, the state approved the university’s spending up to $10 million on the planning and design of the building.
The university has selected brg3s architects, a Memphis-based firm with a long history in health care, to design the building and work in collaboration with HOK.
If the funding for the project is provided in the state budget, the Health Science Center is working to position itself to begin construction in late Summer of 2026.
“I think this is one of those landmark events at a college of medicine,” said UT Health Science Center College of Medicine Executive Dean Michael Hocker. “Thanks to the state-of-the-art technology, we’ll be able to expand interprofessional education, which is really how we practice medicine.”
To learn more about this project and how you can support it, contact Kelly Davis, executive director of development, at kdavis@uthsc.edu.
$350 Million
275,000 to 300,000 Square feet
175 to 225 Expansion of annual medicine cohort
30 to 60 Expansion of annual physician assistant cohort
1,450 Additional health care professionals graduate in first five years of operation
16,935 sq. ft. Public spaces (including lobby, wellness/quiet rooms, interdisciplinary health commons, student study rooms, seminar rooms)
38,300 sq. ft. Academic and support spaces (flexible configuration to meet cohort needs)
17,000 sq. ft. Interdisciplinary space (digital health and innovation space, specialty simulation area, external partnership space, health incubator, and technology innovation lab)
6,000 Projected shortfall of MDs in Tennessee by 2035
“At UT Health Science Center, they do a really good job of pairing us with good mentors. Faculty is super approachable. We get to go on rounds at the hospital, and we have a preceptor we’re assigned to during our pre-clinical years, and it just kind of gets you out of the regular schedule. It’s such a good reminder of what I’m here for. When you see a patient, it’s a different type of active recall. It’s more motivating to look back at the material you’ve studied and apply it to a patient, and that’s way more memorable, too.”
– Snehi Vaghela, second-year medical student
“I’m incredibly grateful for the opportunities offered through the College of Medicine – Chattanooga Family Medicine Residency, especially the new rural track. It’s inspiring to be part of a program that recognizes the importance of serving communities where access to care can truly change lives. I can already see how this experience will help me grow as a physician and deepen my connection to the people and places that make Tennessee so special!”
– Ryan Hall, MD, PGY-2, Family Medicine Residency Rural Track in Chattanooga
“My mom and dad served in the Army, and I’m really proud of that. I want my future family to be proud of my career. You get to find solutions to things. And seeing people crossing the street, or sleeping on the street, knowing you’re taking care of them, you’re able to contribute to a community as a medical student, as a resident, as a doctor. You’re part of something bigger.”
– Neyland Harmon, second-year medical student
“Let us not forget that while technological tools help us provide care, they do not care for the patient. Strive to be more connected to your patients than your electronic devices. Your ability to impart empathy, compassion, trustworthiness, and humility is encompassed in the humanity that is required to be a true healer.”
– Ryan Mire, MD, internal medicine physician in Nashville and president-elect of the College of Medicine Alumni Council, addressing the 2025 White Coat Ceremony
“My experience at UT Health Science Center has been challenging and so rewarding! I did my undergraduate studies at the University of Tennessee, Knoxville. So, staying within the UT System for my PhD, as well as collaborating with UTK and ORNL through UT-ORII for my thesis, has been an amazing opportunity. Getting to watch the partnerships across the UT System come together to address cancer and health disparities in Tennessee really fuels my passion for research.”
– Matthew Jung, second-year PhD student in the Department of Microbiology, Immunology, and Biochemistry
Through longstanding partnerships with major hospitals in Tennessee’s largest cities, as well as 779 clinical and education sites, our students, trainees, residents, and faculty from all our colleges provide the highest-quality health care to the people of Tennessee. In addition, the university is increasingly bringing care to areas in need through mobile health and telehealth.
Memphis
• Regional One Health
• Le Bonheur Children’s Hospital
• St. Jude Children’s Research Hospital
• Methodist Le Bonheur Healthcare
• Baptist Memorial Health Care
• Lt. Col. Luke Weathers Jr. (Memphis) VA Medical Center
• St. Francis Hospital
Statewide
• Ascension Saint Thomas Hospital, Nashville
• Erlanger Health System, Chattanooga
• The University of Tennessee Medical Center, Knoxville
• East Tennessee Children’s Hospital, Knoxville
• West Tennessee Healthcare – Jackson Madison County General Hospital, Jackson
• Maury Regional Health
CHANGE SERVICE REQUESTED
UT Health Sciences Weekend | Memphis, TN, April 16-18, 2026
Registration opens January 15, 2026. Accommodations available at the Peabody Hotel.
Schedule of Events (Details subject to change as needed)
Activities and events will be held at the historic Peabody Hotel, the UT Health Science Center campus, and various community venues and locations.
Thursday, April 16
Alumni Board and Council Member Dinner
Friday, April 17
Alumni Board and Council Meetings
ALL UT Health Science Center Campus and CHIPS tours
ALL UT Health Science Center Lunch and Campus Keynote Presentations
ALL UT Health Science Center College Receptions with the Deans
ALL UT Health Science Center Alumni Awards Dinner
Saturday, April 18
ALL UT Health Science Center Community Service Outreach Project
ALL UT Health Science Center Reunion Events at the Peabody Hotel and the Memphis Redbirds Game
Tuesday, April 21
Sixth Annual UT Health Science Center Giving Day
24-hour campaign that raises funds to support the university and its dedication to building a healthier community