Journal of the Irish Dental Association
Iris Cumainn Déadach na hÉireann

Journal of the Irish Dental Association
Iris Cumainn Déadach na hÉireann

HONORARY EDITOR Dr Cristiane da Mata BDS MFD (RCSI) Dip TLHE MPH Phd FFD RCSI journaleditor@irishdentalassoc.ie
DEPUTY EDITOR Dr David McReynolds BA BDentSC MFDS RCSEd DChDent (Pros) FFD RCSI
EDITORIAL BOARD
Dr Meriem Abbas BDS (NUI) MFDS RCSEd PGDip TLHE
Una Farrell Dip Dental Hygiene
Dr Geraldine McDermott BA BDentSc MFDS (RCSI) PGradDip ConSed (TCD) MSc Healthcare Leadership (RCSI)
Dr Clair Nolan BDS (NUI) MSc (Endo) U. Lond
Dr Adedeji Daniel Obikoya BChD MFDS (RCSI) MSc
Dr Judith Phelan BDS (NUI) MDS (NUI) MSc (U Lond) MRD (RCS Eng and Glas)
Dr Patrick Quinn BCL BDS LLM MDPH
Dr Catherine Vaughan BDS (NUI)
IDA PRESIDENT Dr Will Rymer
IDA CHIEF EXECUTIVE Fintan Hourihan
CO-ORDINATOR Liz Dodd
The Journal of the Irish Dental Association is the official publication of the Irish Dental Association. The opinions expressed in the Journal are, however, those of the authors and cannot be construed as reflecting the Association’s views. The editor reserves the right to edit all copy submitted to the Journal. Publication of an advertisement or news item does not necessarily imply that the IDA agrees with or supports the claims therein. For advice to authors, please see: https://jida.scholasticahq.com/for-authors
Published on behalf of the IDA by Think Media, 537 NCR, Dublin 1 T: +353 1 856 1166 www.thinkmedia.ie
MANAGING EDITOR Ann-Marie Hardiman ann-marie@thinkmedia.ie
EDITORIAL Colm Quinn colm@thinkmedia.ie
ADVERTISING Paul O’Grady paul@thinkmedia.ie
DESIGN/LAYOUT Rebecca Bohan, Tony Byrne

Audit issue January-December 2023: 3,867 circulation average per issue. Registered dentists in the Republic of Ireland and Northern Ireland.
Irish Dental Association Unit 2 Leopardstown Office Park, Sandyford, Dublin 18. Tel: +353 1 295 0072 Fax: +353 1 295 0092 www.dentist.ie Follow us on Facebook (Irish Dental Association).




A rare case of unilateral facial infiltrating lipomatosis: summary of medical and dental implications
Dental Surgeons
Autumn/winter CPD; IDA awards
All the latest news from the trade
From competence to confidence
Metachronous supernumerary teeth in a non-syndromic patient R. Craig, A. McBride, J. Marley, C. Johnson
A. Bode, F. Aslam, D. O’Kane, A. McIntosh, A.K. Humphreys
CLINICAL FEATURE
Crossbite correction: learning through simulation
D. Millett, K. Evans, J. Brown, C. Laide
A clinic that converts
A love of general dentistry




Dr Cristiane da Mata Honorary Editor
Following an extensive review process, big changes are coming for the Journal.
I am delighted to announce that, from the next edition (October/November) onward, we will be launching a new version of the JIDA
The editorial board and some IDA board members have worked diligently over a number of months, reviewing every aspect of the Journal, including its content, paper weight and advertisement spread. The aim was to bring you a more contemporary and professional publication, continuing its mission to educate IDA members in supporting sustainable health.
One of the most notable changes is the introduction of JIDA Science – a dedicated scientific publication that will now accompany the main Journal and be distributed exclusively to IDA members. JIDA Science will provide a focused space for highquality research, case reports, clinical updates, and peer-reviewed content. It will also feature Irish researchers, bringing their valuable work into the spotlight.
The updated JIDA also introduces a more contemporary and reader-friendly design. In response to members´ feedback, we’ve made thoughtful changes to how advertising appears – placing ads in clearly defined sections so as not to interfere with editorial content. This improves both the aesthetic and navigational experience, and we hope it will make the JIDA easier and more enjoyable to read.
Sustainability has been another guiding principle in the redesign. The new JIDA and JIDA Science will be printed on lighter paper stock and delivered in fully compostable packaging, aligning with our wider commitment to environmentally responsible practices.
As we move to a new era with mandatory CPD enshrined in law, we hope these changes will strengthen the JIDA’s role as the leading voice in Irish dental science and professional development. I firmly believe that the new Journal will be a winner with readers and advertisers alike.
All dentists in the island of Ireland will continue to receive both JIDA and JIDA Science until the end of 2025. However, from the first edition of 2026, only IDA members will receive JIDA Science
Dentists who wish to continue to receive both publications can either join the IDA or subscribe by contacting the IDA before the end of December 2025. Of course, we strongly recommend that you join the IDA if you are not already a member, as the new and improved JIDA is only one of the many benefits of membership. Dentists in Northern Ireland will be most welcome to subscribe. I would like to extend heartfelt thanks to all members of the redesign taskforce, including our CEO Fintan Hourihan, Deputy Editor Dr David McReynolds, Liz Dodd, Roisín Farrelly, Ronan King, and our past President Dr Rory Boyd. I also want to congratulate and thank Think Media who, after a competitive tender process, have been selected to continue producing the JIDA. Their collaborative spirit, creativity, and commitment to quality have been invaluable in helping us to bring this new version of the JIDA to life.
JIDA Science will provide a focused space for high-quality research, case reports, clinical updates, and peer-reviewed content. It will also feature Irish researchers, bringing their valuable work into the spotlight.
The opening of the new RCSI Dental School marks a significant and welcome development in dental education in Ireland. As the country continues to face a critical shortage of dental professionals, this new institution joins University College Cork and Trinity College Dublin in a shared mission to train the next generation of dentists. Together, these three schools will play a vital role in addressing workforce needs, enhancing access to care, and expanding opportunities for academic collaboration.
We warmly congratulate Prof. Albert Leung for leading such a significant enterprise, and wish him and his team every success in the years ahead.
The recent two-hour Dáil debate on dentistry will hopefully expedite the publication of a serious programme of oral health reform by the Minister for Health, Dr Jennifer Carroll MacNeill TD. The Association is determined to seize the opportunity to promote many of the ideas we have developed and published in various position papers in recent times.
The Journal will play a key role in hosting discussions and interviews with the key players central to the reform process over the coming years. We all face a busy and exciting time ahead, and I look forward to engaging with our readers, contributors and supporters as we travel the road to better oral health.


PRESIDENT’S NEWS
Dr Will Rymer IDA President
When we reflect on what sustains a long, rewarding career in dentistry, we often think of clinical skill, professional development, or business acumen.
These skills are vital, of course. But one element quietly underpins them all, and that is mentorship.
When individuals have access to effective mentorship, they report feeling more confident, more connected, and more capable of navigating the inevitable challenges of clinical life. Mentorship also plays a key role in preventing professional stagnation, improving patient outcomes, and fostering leadership at all levels. Mentorship is not something confined to formal programmes or early career stages. It must be a living, breathing part of our professional culture. Whether you have been practising for two years or 20, there are always opportunities to both give and receive support. There are always moments when a quiet word of reassurance, the sharing of experience, or simply being present for a colleague can change the trajectory of someone’s day, or career. This responsibility extends beyond dentists alone. Our services depend on the entire dental team. Dental nurses, hygienists, practice managers, technicians and administrative staff all face their own pressures and uncertainties. Creating a culture where they too feel supported, valued, and able to grow is just as important as clinical mentorship.
That is why the IDA is reworking and reinvesting in the development of a dedicated, structured mentorship programme for members. This initiative is designed to complement the informal mentoring that already happens across clinics, branches, and workplaces, but also to address the gaps, ensuring that no one feels isolated or unsupported in their professional journey.
We envision a mentorship framework that reflects the diversity of our membership, and recognises the diverse needs at various career stages. We want to create a space where experience is shared freely, where questions can be asked without fear, and where the next generation of dentists and team members feel welcomed, guided, and confident to succeed.
Mentorship does not require perfection. You do not need to have all the answers or decades of experience. What it requires is a willingness to listen, to share your journey, to offer others the benefit of your perspective. Often, the most meaningful mentorship comes from honest conversations about the real-world challenges of our profession. Likewise, for those seeking mentorship, this programme is an invitation to engage, to connect, and to realise that the path through dentistry does not need to be walked alone. This is something that the IDA can help with, but it is also something we can each do, in our own small way.

Fintan Hourihan IDA CEO
A Dáil debate on dentistry took place on July 16.
1. The motion proposed by independent Deputy Brian Stanley (Laois) covered a wide range of concerns relating to the provision of dental care, especially children and adults entitled to care under the medical card and PRSI schemes.
2. Some 22 TDs from across the Opposition benches contributed to the debate, with responses provided by junior Ministers at the Department of Health, deputies Mary Butler and Kieran O’Donnell.
3. There is strong support for prioritising greater access to dental care for children especially, and the Opposition is keen to see progress on a new State scheme.
4. The decision that the Government would not be opposing the motion, and the fact that no Government TDs attended the debate, was an indication of a tacit admission of defeat regarding dental health by this Government.
5. Minister Butler announced that a final draft of the new Smile agus Sláinte threeyear implementation plan is with the HSE for observations and suggested that once its views are received publication will be expedited.
6. Deputy Stanley said his interest in the dental access crisis is informed as much by family members’ difficulties as by the severe difficulties faced by his constituents. Children in Laois do not receive a school screening appointment until fourth year in secondary school – the longest delays in the country.
7. There were specific references to IDA research and commentary by a number of Opposition deputies.
8. Many politicians see that dentistry is one area of healthcare where health status is directly linked to socioeconomic status. Many TDs also said that they had been approached by dentists, showing that dentists can play their part in supplementing the IDA’s advocacy work.
9. Government representatives focussed on the welcome opening of the new RCSI dental school as an important part of the solution to the dental workforce crisis.
10. Soundbite of the day went to Deputy Ruth Coppinger, who asked the Minister: “Why are teeth a luxury item in Ireland? Why are they considered an accessory?”
To read the full debate, go to: https://www.oireachtas.ie/en/debates/debate/dail/2025-07-16/9/.
Save the date – HSE Dental Surgeons
Seminar 2025
October 16-17, Hotel Kilkenny, Kilkenny


KILKENNY OCTOBER 16+17
Fascinating topics, including:
n contemporary caries management;
n paediatric oral medicine;
n interceptive extraction of first permanent molars;
n paediatric oncology dentistry; and,
n endodontic management of immature permanent teeth.
Fantastic clinical workshops:
n Dr Caitriona Ahern: Oral radiology;
n Dr Kirsten FitzGerald: Paediatric treatment planning; and,
n Dr Isabel Olegário: Materials for contemporary caries management
Trade show and social evening.
To register, log on to www.dentist.ie and choose ‘Book CPD’.
CPD verifiable.

Whether you’re a long-standing IDA member, recently joined, or still considering becoming part of our community, our new Membership Manager, Molly Conroy, would be delighted to speak to you. Molly is the IDA’s go-to person for:
n support and advocacy no matter what your career stage; n member queries and feedback; and, n enquiries about joining the IDA.
There’s never been a better time to join the IDA for access to a wealth of resources including expert guidance, exclusive events, professional development opportunities, and a supportive peer network.
TO FIND OUT MORE, CONTACT MOLLY AT MOLLY@IRISHDENTALSSSOC.IE , CALL OR WHATSAPP AT 087-095 9482, OR CALL IDA HOUSE AT 01-295 0072.
MAKE SURE YOU ARE USING YOUR IDA MEMBER INDEMNITY DISCOUNT
Molly will be happy to advise on the many benefits of IDA membership, including the huge savings in professional indemnity costs exclusive to members. As an IDA member, you are entitled to an 11.5% discount with Dental Protection (DPL) on your professional indemnity. This should be deducted automatically from your renewal quote. If you are unsure whether this discount has been applied, we encourage you to contact Dental Protection directly to confirm.
Make sure you're getting the full value of your IDA membership!
MEMBER’S VOUCHER






IS YOUR VOUCHER FOR 11.5% DISCOUNTON YOUR DENTAL PROTECTION FEE. DISCOUNT APPLIES TO ALL PAID UP MEMBERS

The IDA has made a number of awards to students in the two dental schools for outstanding undergraduate achievement. In Cork, Martha Woods was the winner of the IDA prize for achieving the highest result in final year. Dublin student Patricia Badan received the Award for Best Final Year

Academic Presentation (Dental Technology), while Martin McCormick was the recipient of the Award for Highest Result over the Five Years of the Dental Science Course.
Congratulations to all three on their outstanding achievements.




We are thrilled to announce the appointment of Molly Conroy as the new Membership Manager at the Irish Dental Association. With a strong background in member engagement and a sincere passion for supporting professionals in their careers, Molly brings a wealth of energy, empathy, and fresh perspective to the IDA team. Molly joins us with several years of experience in relationship management, where she has consistently demonstrated a talent for building meaningful connections and delivering exceptional support. Her approach is rooted in accessibility, collaboration and genuine care, values that align seamlessly with the IDA’s mission to serve and support dental professionals throughout Ireland.
“I’m truly excited to be joining such a respected and vibrant organisation,” Molly says. “The IDA plays a vital role in advocating for and supporting dentists at every stage of their careers, and I’m honoured to now be part of that mission. My focus will be on listening to our members, understanding their needs, and ensuring that they feel informed, supported, and valued.”
Molly is already eager to start meeting members across the country and looks forward to strengthening the IDA’s relationship with its growing membership base. Whether you’re a long-standing member, recently joined, or still considering becoming part of our community, Molly is your go-to person for anything membership related, from queries and feedback to advice and guidance. Her open-door policy reflects her commitment to building a strong, responsive, and inclusive community. “I want members to feel they can reach out anytime, whether they have a question, need support, or just want a chat,” she adds.
For those who haven’t yet joined the Irish Dental Association, there’s never been a better time. As a member, you’ll gain access to a wealth of resources including expert guidance, exclusive events, professional development opportunities, and a supportive network of peers. Molly would be delighted to speak with you about how the IDA can support your career and professional journey. Please join us in warmly welcoming Molly to the IDA team. We’re confident that her dedication and enthusiasm will make a positive and lasting impact on our members and the wider dental community. Molly can be contacted at molly@irishdentalsssoc.ie. Alternatively, you can call or reach her on WhatsApp at 087-095 9482 or you can phone her in IDA House at 01-295 0072.
The Irish Division of the International Association for Dental Research (IADR) held its Annual Scientific Meeting on Thursday, June 26, at the IADR/PER General Session and Exhibition, Centre de Convencions Internacional de Barcelona, Barcelona, Spain. There were a total of 11 presentations for the Irish Division IADR Postgraduate Research Prize and two non-prize presentations relating to ongoing clinical and laboratory-based research within the Island of Ireland. The prize winners were:
n Claire Curtin, University College Cork – winner of the 2025 Irish Division IADR Postgraduate Research Prize for ‘Oral Health in Residential Care; an Irish Cross-Sectional Study’;
n Paul Leavy, Trinity College Dublin – winner of Highly Commended Prize for ‘Factors Influencing General Dentists' Participation In State-Funded, Contracted Care’; and,
n Louai Alkababji, Queen’s University Belfast – winner of Highly Commended Prize for ‘Differential Expression of Neuronal TRP Channels Under Inflammatory Conditions’.

Dr Danielle McGeown is a dentist undertaking a PhD into the characteristics of dental aerosols in community dental surgeries, under the supervision of Prof. Máiréad Harding. As part of her research, Danielle hopes to capture the current thoughts of dental professionals in Ireland about dental aerosols, and has prepared a questionnaire for dental professionals on this topic. This research is taking place through UCC and has been approved by the college’s research ethics board. The questionnaire will take a few minutes of your time to complete, and is for all dental professionals – dentists, dental nurses, dental hygienists and dental administration staff are welcome to participate. The researchers thank you in advance for your time and support. For further information about the study, or to access the questionnaire, please go to: https://ucc.qualtrics.com/jfe/form/SV_2mzaGPp4nJaPoNg or scan the QR code.



The Commission for Communications Regulation (ComReg) is calling on all organisations that use SMS to communicate with customers to register their Sender IDs, as part of a national effort to combat the growing threat of scam texts. Under new regulations, a two-phase enforcement plan has already come into effect this summer:
n from July 3 to October 2, 2025, unregistered SMS Sender IDs will be automatically relabelled as ‘Likely Scam’, warning recipients that the message may be fraudulent; and,
n from October 3, 2025, messages from unregistered Sender IDs will be blocked entirely.
The initiative is part of ComReg’s broader strategy to protect consumers from fraudulent messages that impersonate trusted brands and public services. These scams, often indistinguishable from legitimate texts, have become a serious threat to both consumers and businesses.
To address this, ComReg has launched a free SMS Sender ID Registry. The registry acts as a secure database of verified Sender IDs, helping to ensure that only legitimate messages reach Irish mobile users.
A Sender ID is the name or identifier that appears on a text message, such as a bank name or Government agency. While this feature helps consumers to identify the source of a message, it has also been exploited by scammers to impersonate trusted entities.
How the Registry works
SMS providers will be required to cross-check all outgoing messages against the Registry. If a Sender ID is not registered, the message will either be flagged or blocked, depending on the enforcement phase.
Action required by businesses
Organisations that use SMS to communicate with customers must ensure that their Sender IDs are registered. If your SMS provider has pre-registered your Sender ID, you should have received an activation email. If not, you can:
1. Visit www.comreg.ie/senderid to check if your Sender ID is already listed.
2. Log in to senderid.comreg.ie to approve your SMS provider or register a new Sender ID.
Important notes:
n The Registry applies only to application-to-person (A2P) SMS messages, not to personal texts between individuals; and, n messaging apps like WhatsApp are not affected by this regulation.

SEPTEMBER 2025
September 4 – Southern Region meeting, Rochestown Park Hotel, Cork September 17 – Mouth Cancer Awareness Day webinar, 8.00pm September 18 – South East Region meeting, Viking Hotel, Waterford, 7.30pm
September 24 – Webinar, 8.00pm September 26-27 – The Magic of Composites, The Galmont, Galway

OCTOBER 2025
October 3 – Preparation Design for Implants, Portmarnock Hotel, Dublin
October 16 – South East Region meeting, Lyrath Estate, 7.30pm October 16-17 – HSE Dental Surgeons Seminar, Hotel Kilkenny
October 29 – Webinar, 8.00pm
NOVEMBER 2025
November 7 – Southern Region ASM, Fota Resort
November 8 – Colgate Caring Dentist Awards, InterContinental Hotel, Dublin
November 13 – South East Region meeting, Brandon House, New Ross, 7.30pm
November 14-15 – Composites course, Hilton Hotel Charlemont, Dublin 2
November 21 – Paediatric Dentistry in a Day, Hilton Hotel Charlemont, Dublin 2
November 26 – Webinar, 8.00pm November 26 – Northwestern Region meeting
November 28 – Endodontics and facial pain hands-on course, Sandyford, Dublin
DECEMBER 2025
December 10 – Webinar, 8.00pm
December 11 – Southern Region meeting, Rochestown Park Hotel, Cork, 7.00pm
To book these events, go to www.dentist.ie and click on ‘BOOK CPD’.




Dr Sandra Tai (pictured, right), a specialist orthodontist based in Vancouver, Canada, took centre stage in London at Invisalign Live 2025, Align’s flagship event for dentists and orthodontists, and she said: “The event showcased ground-breaking new technologies from Align Technology, including the Invisalign Palatal Expander System, a tool I have been actively using in my own practice, and I was excited to share my experiences”. Dr Tai sees this innovation not just as another product, but as a “paradigm-shifting solution” for treating growing patients. Historically, orthodontists have often taken a ‘wait and see’ approach with younger patients, monitoring dental development and deferring major treatment until the age of 12 or beyond: “When a young patient’s first permanent teeth erupt, they may come in rotated, in crossbite, or in a lingual position. Parents are understandably worried. In the past, we told them to wait until age 12, or worse, extract teeth early to create space. That’s now changing. We’re now at a tipping point, and the Invisalign Palatal
Many dentists in Ireland find themselves overwhelmed, under-supported, and wondering why their hard work isn’t reflected in their revenue.
According to Lisa Grogan (pictured, right), that’s where she comes in.

Lisa helps ambitious practice owners to get clear on what’s really going on in their business, from where they’re losing money to where their greatest growth opportunities lie. Lisa says that with her support, dentists can streamline operations, build high-performing teams, and take back control of their time, energy, and business direction. Dental business coaching is still relatively new in Ireland, but it’s quickly becoming the advantage smart practice owners rely on. Lisa states that her coaching brings structure, clarity, and strategy to busy clinics, so owners can finally see how their practice is performing and exactly what to do to improve it.
Most importantly, according to Lisa, she helps her clients get clear on the kind of business and life they actually want. That means attracting more of the work they love, and making each day more fulfilling, while being able to switch off and enjoy their home life with peace of mind. Because, she says, the truth is:
n your revenue should reflect your effort; n your systems should support you, not drain you; and, n your clinic should give you time and freedom to thrive, not just survive.
If you've been feeling like the business is running you, not the other way around, dental coaching could be the game changer you've been looking for.

Expander System is the catalyst”. Designed for children aged six to 11, according to Invisalign, the device uses 3D-printed, custom-fitted expanders to gently and gradually widen the palate, making room for permanent teeth without the need for extractions or traditional metal appliances.

Coltene states that its CanalPro Jeni endomotor is an excellent digital assistance programme, designed to make canal preparation safer and more efficient through a simple and intuitive interface.
According to the company, file movements are controlled at millisecond intervals, rotary movements are constantly regulated, and intensity, torque and file stress are monitored. Coltene states that the endomotor continuously adapts to the contours of the individual root canal, guiding chemical and mechanical preparation every step of the way. According to Coltene, working length is measured throughout the procedure by the integrated apex locator, ensuring that your navigation through the root canal is aways on track. After attaining the required working length, the machine prompts you to switch to the next file until the desired preparation size is achieved. The company states that the CanalPro Jeni endomotor is built to last, and that futureproofing is built in with frequent updates that can be uploaded at any time.
Henry Schein Ireland has introduced the new EdgePower suite by EdgeEndo, one of the world’s largest NiTi rotary file suppliers. According to the company, the EdgePower suite offers a fully cordless endodontic handpiece, stand-alone apex locator, obturation pen, and heated downpack device, enabling clinicians to streamline workflows and optimise efficiencies.
Paolo Zanetti, Vice President and General Manager, Endodontics, at Henry Schein, said: “The addition of this new range of EdgeEndo equipment to our endodontic portfolio reflects our ongoing commitment to supporting dental professionals with reliable, high-quality, and cost-effective solutions. EdgeEndo is our fastest growing, global endodontic brand, focused on helping our customers to enhance patient care at the right cost”.
The new product line features: EdgeApex HP – an endodontic handpiece featuring a 360° rotatable mini contra-angle and built-in apex locator functionality; EdgeApex – a compact, standalone device combining an apex locator and pulp tester; EdgeFlow – an obturation pen designed to deliver high gutta-percha fluidity, helping to ensure a uniform, bubble-free fill for optimal canal filling and sealing; and, EdgePack – a companion heated downpack obturation device designed for compacting and cutting gutta-percha.
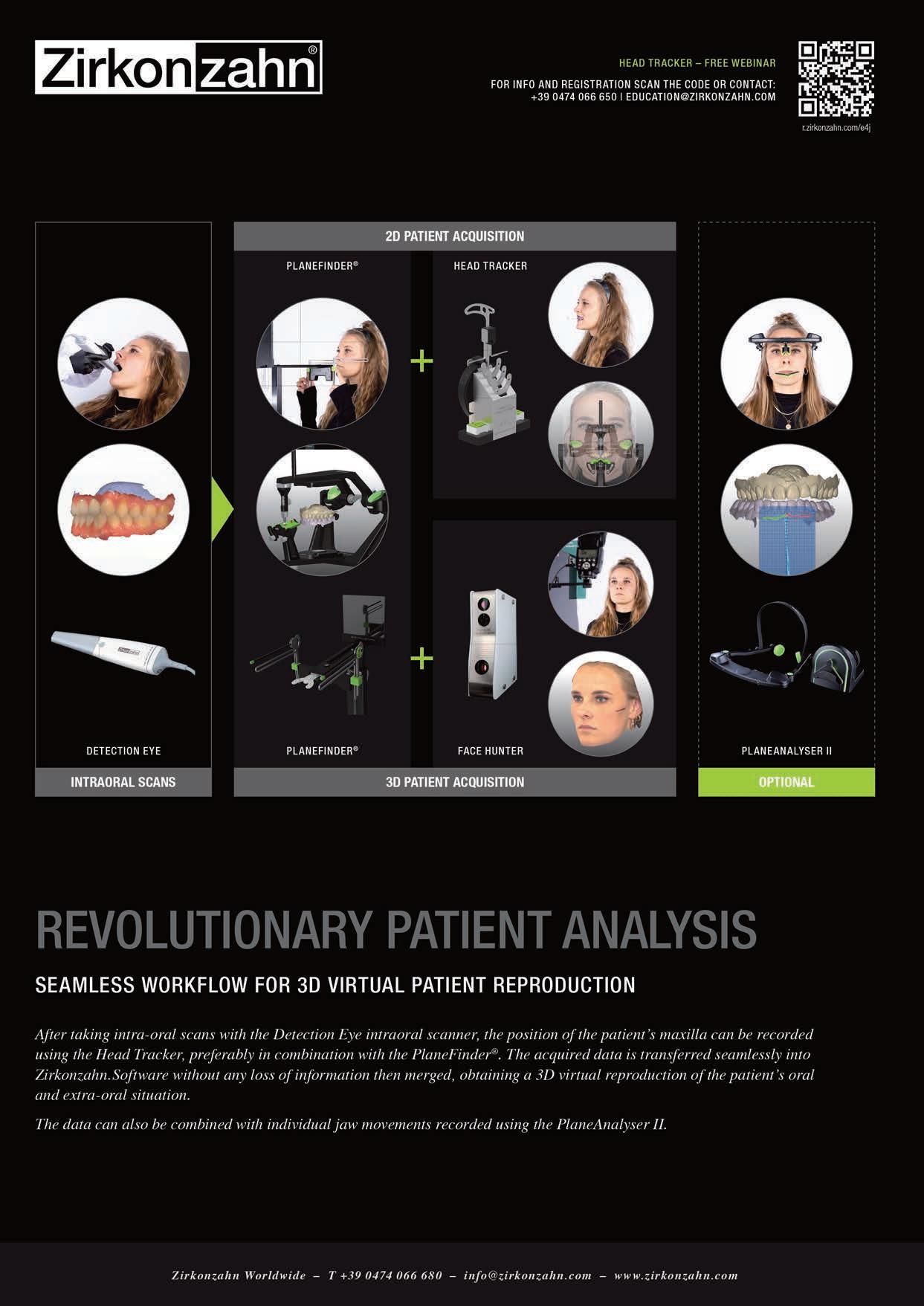
Zirkonzahn states that its new Detection Eye intraoral scanner stands out for its very high scanning accuracy and speed, which enables practitioners to digitise a patient’s jaw in less than 60 seconds. According to the company, Detection Eye provides real-time scanning with realistic colours, detailed preparation margins, and the scanning areas do not need to be pre-treated with powder, which simplifies the acquisition process.
The company calls the software intuitive and states that it allows the user to complete the scanning process using a one-touch command. In addition, the software can be operated via the ‘motion sensing’ technology: the user moves the scanner to send commands to the software. This simplifies handling and ensures a hygienic scanning process, as there is no direct contact with the PC. According to Zirkonzahn, using artificial intelligence the software automatically identifies and removes redundant data from the scans, resulting in a faster and optimised scanning process.


Via a QR code, dentists can share the 3D scans acquired, as well as clinical recommendations, with the patient on their smartphones for a better understanding of the individual treatment plan.


New IDA President Dr Will Rymer speaks about his plans for his year as President, and how the IDA can help dentists feel like part of a community.
The IDA was instrumental in helping to making Ireland feel like home, says new IDA President Dr Will Rymer. He is originally from England and says: “Through the IDA, I met on the GP Committee a group of really passionate, supportive colleagues advocating for the profession, along with mentorship and practical advice. Although the GP Committee has a bigger purpose than looking after a lost soul, it showed me the real sense of community in dentistry in Ireland”. Will trained in Wales, before taking an extra step across the Irish Sea to live and work here. He now runs Expressions Dental and Cosmetic Clinic in Roscrea, Co. Tipperary, with his wife and fellow dentist, Dr Sarah Rymer.
Following graduation from Cardiff University, Will worked for two years in a mixed NHS/private practice in Wales: “That gave me that invaluable hands-on experience and clinical skills, and experience in navigating the complexities of a national healthcare system. I also worked under the NHS foundation training
scheme. That would have been a year in general practice as a vocational training year, and then six months working in a maxillofacial unit in Swansea, and six months working in community dental service in Swansea. In terms of my career pathway, that was a major milestone. It gave me a real appreciation for the importance of mentorship and teamwork, which has stayed with me for the rest of my career”.
Family circumstances and career opportunities brought Will to Ireland, and he spent time in many different places and practices before establishing Expressions: “I worked in a mixed public and private setting, a combination of urban and rural. It gave me an opportunity to engage with the public dental service as well. So I worked in Limerick, Clare, Tipperary, and Galway, and that gave me a quite broad understanding of the challenges in rural Ireland, but also the potential in Irish dentistry”.
“I worked in a mixed public and private setting, a combination of urban and rural. It gave me an opportunity to engage with the public dental service as well. So I worked in Limerick, Clare, Tipperary, and Galway, and that gave me a quite broad understanding of the challenges in rural Ireland, but also the potential in Irish dentistry”.

From blow-in to President
Will’s first few years in Ireland were quite isolating, but he says that getting involved in the IDA helped him to turn a corner: “Just from a practical sense, moving to a new country brings all sorts of challenges. In dentistry there are different regulations, new systems, unfamiliar structures. But then there is the more subtle stuff of finding your place in the profession. I think the IDA was instrumental when I eventually engaged. It was instrumental with the events, the committees, informal networks, having a cohort of people that I can WhatsApp when there’s a minor crisis that I need help with. The IDA turned what was initially a very isolating experience into one where I felt supported and included”.
Many dentists are now completing their CPD online, and while this can be seen as less of a burden than in-person courses, Will says this often exacerbates isolation: “You miss even that simple social networking that goes on around the coffee machine. And that’s not a replacement for having a colleague in the building or up the road, but it is important. And I think sometimes, in the fast pace of our profession, we think we know what we want, which is: I just want to get this meeting done, and I’ll do it online because it takes up less of my time. But the reality is, you don’t know what it is that you’re missing until you’ve missed so much that you suddenly realise that you have isolated yourself”.
Starting anything new can be a challenge, but any initial discomfort doesn’t last long, says Will: “Anybody who’s recently moved to Ireland, whether it’s from the UK or further afield, I would say, get involved with the IDA as soon as possible. You have to sometimes risk the uncomfortable, awkward social engagements to build a network”.
Main aims
Will’s involvement in the IDA grew to where he is now President of the Association: “I actively participated in committees, started to contribute more and more to discussions around policy, professional development, and wellbeing of dentists. Then I was encouraged to take leadership roles in other committees, and ultimately, the role of President. I think that that is proof of the impact that those small invitations, going back to that initial invite I got to the GP Committee, can have. It can make a really profound difference in someone’s career”.
The role of IDA President is a busy one, and not something you put yourself forward for on a whim, says Will, but he felt it was time to step up and do his best for dentists in Ireland: “I think we have a responsibility to give back when we get the chance and shape the future of the profession. My emphasis in particular is on making sure that no other dentist feels that isolation I felt or that they go unheard”.
Will is interested in promoting unity in the profession, he says, not as a vague idea, but as a practical everyday approach to how we work. The profession is disparate and many can end up in siloes. One important change that has already been made was incorporating a broader mix of practitioners into the GP Committee, where previously it was seen as something for practice owners: “And it’s very much reinvigorated it. We’ve got associates, we’ve got dentists who work in the corporate part of dentistry. The IDA is an Association for everybody. So I really want to work for 12 months on breaking down those silos, promoting a sense of shared purpose, and emphasising the value of mentorship”.
Will would also like to ensure that the IDA remains a credible, respected voice in policy conversations: “I think that around the systemic failings in the medical card
Will lives in Roscrea, Co. Tipperary with his wife and fellow dentist Dr Sarah Rymer. His biggest passion outside of dentistry is cycling: “I think there’s something about the rhythm of cycling, the physical challenge, the sense of camaraderie in a group, the fact that you can’t sit on the front. This is the analogy for the leadership role. You can’t sit on the front thrashing it away for three hours.
scheme and the public dental service, and the pressures that creates directly on dentists and their stress levels, the IDA can really drive meaningful reform, but only if we present a united constructive front”.
Message for Government
Will has a simple but crucial message for the Government: “They must be willing to meaningfully engage with us”.
The profession is very clear in what it wants: “We are willing to talk and to be part of the solution in oral healthcare. We need the Government to listen, to collaborate and act in good faith. Policy decisions in dentistry have often been made in a vacuum without meaningful input. We had our oral health policy launched without really any meaningful consultation with the Association. The medical card scheme has all but collapsed. We have workforce shortages and a legal environment that discourages people from entering or staying in the profession. So we need the Government to see dentistry not as an afterthought, but as an essential part of public health policy. And it’s not an oral health policy. It’s just part of health policy. It’s just a small part of your overall health that shouldn’t be separate”.
Funding often fails to get close to what will address an issue, says Will, and the Association needs to analyse how it and other related bodies deal with those in power: “We need to collaborate with other unions and other professional bodies, because when I’m meeting representatives from those bodies, we’re hearing the same things about how Government deals with them: this token engagement, these last-minute briefings. I think our shared experience will help us achieve what we really need, a healthier healthcare system. I know that all of my predecessors have been aiming to do the same thing, so I’m not under any illusions that I’m suddenly going to crack this. But I think we just have to keep making the same argument that our profession has never been more willing to help to move this forward. We’ve never been in a worse situation for patients, so we have to be willing to sit down. I think the time for thumping the table is past. We need to work together constructively to try and improve the situation”.
Will says joining the IDA is one of the best decisions a young dentist will make in their career. From a practical point of view, the IDA provides best-in-class CPD and a plethora of professional resources, but Will says the most valuable aspect is the connection the Association offers: “When you graduate with a class of 40, 50 other dentists, you’re part of a great crew, and they’re friends for life, but then suddenly you’re on your own. The IDA offers that connection, support, and the chance to be part of something bigger than yourself. You don’t always know at the earlier stage of your career what you need, and the IDA puts it all at your fingertips”. It can be an overwhelming career, particularly in its early stages, says Will: “The IDA can help you navigate tricky situations with patients because when you’re having this crisis in a treatment plan or if there’s a complaint, there’s a dozen people
“You have to take your turn at the front, but you also sometimes need to cycle to the back of the group and let somebody else take a turn. I think that it’s taught me a lot about teamwork, resilience, trust, lessons that apply to dentistry just as much as they do on the road. I spend the winter on cold, wet Irish roads, getting ready for exciting challenges in warmer climes in the French and the Italian Alps”.
“We need to collaborate with other unions and other professional bodies, because when I’m meeting representatives from those bodies, we’re hearing the same things about how Government deals with them: this token engagement, these last-minute briefings. I think our shared experience will help us achieve what we really need, a healthier healthcare system.”
at your fingertips who will be able to tell you what they did in a similar situation”. And the IDA wants to hear from young dentists: “We need to understand what it is that young dentists are feeling to be able to provide the service that they need. We can’t shape the future of the profession unless we’re speaking to the future of the profession”.
Where the Association is going
Will says the IDA will continue to represent all dentists, and is at the moment trying to build a larger network of specialists and academics. The Association will also continue to speak strongly for HSE dentists.
A key part of the IDA’s mission is showing the public and policymakers that oral health is an integral part of overall health, explains Will: “It’s not that medical doctors are separate from dentists. Dentists make a major contribution to your overall health. If Covid taught us anything, it’s that healthcare needs to be approached holistically. And we’re often the forgotten profession. We were forgotten throughout Covid, and we’ll be forgotten again unless we speak up for ourselves”.
Finally, Will says that often when talking about dentistry, you get sucked into policy and politics, and it can sound quite negative: “But I think there’s a lot of reason to be optimistic about Irish dentistry. In a sense, when there’s so many things that have failed, we have a great opportunity to rebuild dentistry in Ireland as we want it. We’ve got a profession full of passionate, skilled, committed people”.


The General Practitioner Group of the IDA has published a position paper outlining the Association’s proposals for tackling the challenges currently facing dentistry in Ireland. Below is a summary of the document.
The position paper was informed by: a one-day meeting in March 2025 to consider key challenges and opportunities to delivery of a safe, sustainable and high-quality oral healthcare service for a growing and increasingly diverse population; contributions from 12 dentists in general practice together with two members of the IDA executive team; an IDA-commissioned GP survey; executive input from Drs Will Rymer and Eamon Croke; and, anticipation of the roll-out of the Smile agus Sláinte implementation plan.
A recent (March 2025) survey of general dental practitioners (GDPs) underscores the critical issues facing the profession, and highlights their perspectives on potential solutions and the future of dental care provision.
Significant challenges
n Soaring operational costs (81.43%);
n regulatory and compliance burdens (63.33%);
n staffing crisis (62.38%); and,
n shortage of skilled professionals (51.43%).
Views on State-funded schemes
n Strong support for universal access: an overwhelming majority (nearly 9 in 10) support the principle of State funding to improve dental care access for lowerincome groups;

Fintan Hourihan Chief Executive, Irish Dental Association
n hesitation regarding specific child schemes: however, there is significant reluctance (only 1 in 10) to participate in the under-7s scheme as currently outlined in Smile agus Sláinte; and,
n demand for pilot programmes: almost 90% advocate for piloting any changes to State schemes before full implementation.
Conditions for participating in State schemes
n Adequate funding and fair fee levels;
n financial support towards practice costs;
n clear referral pathways;
n clinical decision-making independent of third-party restrictions; and,
n efficient administration.
Regulation: a path towards higher standards
n Strong endorsement for mandatory continuing professional development (CPD): over 80% expressed positive views on the introduction of mandatory CPD for dentists; and,
n support for enhanced regulatory powers: half of respondents favour increased regulatory oversight, including practice inspections by the Dental Council and greater authority in disciplinary and enforcement matters.
Workforce crisis in Irish dentistry
The urgent need to address Ireland’s dental workforce crisis in both the public and private sectors regularly makes the news headlines.
Administrative and regulatory burdens are regularly cited as deterrents for new entrants, lifestyle-work balances have changed, and poorly funded or overly onerous State schemes only serve to exacerbate these trends. The uncertainty around the implementation of Smile agus Sláinte is not encouraging.
Modern oral healthcare delivery requires appropriately staffed public and private sectors and, currently, the public dental service is withering through a lack of funding and political support. The Register of the Dental Council requires updating to aid workforce planning.
1. Create a national dental workforce database to enable strategic planning.
2. Facilitate the development of supportive pathways to enable new and recent graduates to transition from a position of ‘competency’ to one of proficiency and ‘expertise’ in the delivery of general practice-oriented, high-quality oral healthcare.
3. Increase funding and capacity in dental schools for Leaving Certificate entrants (TCD, UCC, and the new RCSI school). Upgrade facilities and staffing to meet future demand.
4. Introduce a 20% intake cap on non-EEA students in dental schools, decreasing to 10% over the next three years. Commensurate extra State funding to compensate for lost student fees in dental schools.
5. Capital investment of ¤55m to deliver the overdue new dental hospital at UCC that was originally due for completion in 2023.
The scope of the workforce can be expanded by increasing the scope of practice of auxiliary registrants and the introduction of a new category of dental healthcare professionals with appropriate safeguards in place to ensure that the patient remains under the care and supervision of a dentist.
The Government must commit to properly fund and resource dentistry and oral healthcare to ensure equitable access to care.
The traditional model of dental practice has undergone significant changes in recent years and is expected to continue evolving with the increasing presence of large corporate groups. Factors such as burnout are increasingly emerging, as dentists balance patient demands with business and administrative pressures. There is also limited engagement from banks and finance houses in providing lending for practice expansion. The increasing appeal of cosmetic dentistry is also attracting dental professionals, particularly younger dentists, away from general practice.
The Association is confident, however, that there are immediate steps that can be taken to stem the flow of dentists from general practice. This includes a dedicated national workforce plan, and the reintroduction of a structured mentorship programme.
The current landscape of general dental practice in Ireland is predominantly driven by private care delivery. However, crucial pathways for patient referrals from general practitioners to specialised secondary and tertiary care facilities remain underdeveloped. Furthermore, the specific needs and care of vulnerable patient populations are not formally recognised within the Register of Dental Specialists.
The Health Service Executive (HSE) and public service dental clinics face significant resource constraints and personnel shortages, impacting their capacity to provide essential services.There are now barely 600 dentists actively participating in the medical card scheme. This is equivalent to one dentist per 2,500 eligible patients.
A critical issue undermining the effective functioning of the dental sector is the low level of trust that exists between dental practitioners and policymakers. This lack of confidence is often exacerbated by the unpredictable modification or discontinuation of treatment-payment schemes, frequently occurring with little or no prior notification. Such instability discourages practitioners from participating in or renewing their involvement in these State-funded initiatives.
Finally, general dental practice in Ireland is clearly moving towards a mix of traditional dental care and cosmetic dentistry. This reflects changing patient demands and the increasing availability and appeal of aesthetic dental procedures.
6. Reintroduce an updated version of the discontinued one/two-year Vocational Training (VT) Programme for students graduating from dental schools in Ireland.
7. Consider incentives for private practitioners to support delivery of aspects of care traditionally provided by public service.
8. Introduce clear remuneration pathway or salary package for graduates entering general practice, providing clarity as to likely earning potential as one progresses in general practice; provide relocation grants to support rural practices.
9. Payment of exam fees and other incentives to retain the recent graduate on the academic pathway.
10. Inclusion of non-EEA dental nurses and dentists on the Critical Skills List for work permits as a matter of urgency.
Towards the future of care
A public health approach will require both co-operation and collaboration across a range of partners – with both public dental service and private practitioners working together, where appropriate, to ensure that preventive care and treatment in primary care dentistry is adequately resourced and delivered. The WHO recommends upstream, prevention-focused interventions. Ireland must prioritise prevention to reduce health disparities and long-term costs. The rollout of a prevention programme for our youngest is an obvious starting point. Prevention programmes should be funded across life courses. Private primary dental settings will remain the main centres for life-course oral healthcare provision. It is the view of the Association that an appropriately resourced public dental system is best placed to provide targeted, free oral healthcare to children from birth to the end of primary school education.
Post-primary school and onwards, all State schemes should be designed to provide people-centred care including, where appropriate, the provision of care for those with disabilities, special care adults and marginalised groups.
From time to time, GDPs should also be able to refer patients with challenging medical and dental histories to a reorientated public dental service, or to secondary or tertiary centres for episodic treatment. Future State schemes should fund additional skills acquired by GDPs to treat more challenging patients in primary care settings.
For many decades, the Dental Council and the IDA have advocated for further dental specialties to be recognised. The IDA supports the recognition of nine further specialties, similarly favoured by the Dental Council, in addition to the two in place: orthodontics and oral surgery.
Governance and regulation
The WHO and IDA both advocate for strong, accountable governance in oral health. Within the Department of Health, we believe it is essential that the role of Chief Dental Officer is provided with sufficient resources and authority to ensure that oral health is afforded the greatest priority in policy-making and resource allocation. The IDA has called for the role of the HSE National Oral Health Lead to report to the Office of the Chief Clinical Officer in the HSE. The IDA is also calling on the Government to establish an oversight group to ensure an effective roll-out of its new oral health policy. It is of great concern that the Government and the HSE could proceed with implementing Smile agus Sláinte without meaningful consultation and collaboration with the dental profession. There is, however, a strong welcome for the anticipated introduction of mandatory, structured CPD. The IDA recently welcomed the signing of a
The IDA is calling for the speedy establishment of both an implementation group and oversight group to support monitoring and more efficient implementation of Governmentled policy commitments. The Association is also advocating for the Minister and/or Dental Council to introduce new categories of dental healthcare professionals, and in particular a category for general practitioners specialising in the care of vulnerable patients.
Other actions we are calling for include:
1. Fostering public-private collaboration in prevention, health promotion and treatment delivery.
2. Delivering separate prevention programmes for children, adults, and older populations, tailored to life stages.
3. Dental home for children up to 12 years of age to be rooted in the public service. This dental home will then refer children, when it is safe and appropriate to do so, to private general dental and specialist practitioners for comprehensive oral healthcare provision.
4. Upskilling lower-grade dental personnel to deliver oral health promotion at community level.
commencement order by the Minister for Health for the Regulated Professions (Health and Social Care) (Amendment) Bill 2019, bringing into force a number of critical provisions to underpin patient safety.
There are still, however, gaps in the Dental Act that pose a significant risk to public and patient safety. Right now, legislation does not require dentists and dental auxiliary workers to maintain a professional competency. The Government’s commitment to introduce legislation this year providing for mandatory CPD is very welcome, and we urge the Minister to action this without delay.
1. Establish oversight and implementation groups with strong GP representation.
2. Appoint clinical leaders embedded in national healthcare governance structures.
3. Ensure independent mediation mechanisms are in place to resolve impasses.
4. Introduce mandatory CPD for all oral healthcare professionals to which patients have direct access.
5. Any CPD scheme should not rely solely on ‘self-certification’ but instead be supported or hosted by a recognised third-party provider; the Irish Dental Association, as the representative and advocate for best oral healthcare practice, would be the most relevant home for CPD provision and management.
6. CPD schemes must be subject to audit every c. five years.
7. The model employed for CPD by the pharmacy sector may provide an appropriate example to follow.
8. Recognise and regulate new roles within the dental team (e.g., dental therapists, expanded dental nurse/hygienist scope) with appropriate safeguards to protect patient care.
9. Enact a new Dental Act within the lifetime of this Government (2029).
The IDA promotes the interests of the dental profession and the overall well-being of Ireland’s population through advocating for and championing the delivery of fair, equitable and sustainable oral healthcare for all. In delivering a new vision for general practice dentistry, the IDA has identified specific actions for the Association.
5. Optimising the use of combined resources across private and public practice.
6. Establishing clearly defined referral pathways from general practice to a reorientated public dental service or to secondary/tertiary services.
7. Ensuring general practice is fully integrated into any new proposed universal healthcare model.
8. Consider incentives for private practitioners to support delivery of aspects of care, i.e., grant payment to support school visits for inspections.
9. Providing funding for the expansion of postgraduate training and the provision of consultant training.
10. Investing in secondary and tertiary care infrastructure.
1. Advocate for implementation of Smile agus Sláinte with appropriate stakeholder input.
2. Remain the ‘go-to’ authority and communicator on all matters relevant to the working lives of oral healthcare practitioners.
3. Copper-fasten the role and positioning of the IDA as the representative and negotiating body with Government and public bodies on schemes and payments relevant to dentists.
4. Call for speedy establishment of the implementation and oversight groups committed to as part of the 2019 oral health policy.
5. Serve as the provider of CPD and data infrastructure to provide confidence for the profession that such a scheme can be provided and managed efficiently, and accessed via a reliable system and proven provider.
6. Support new graduates through memberships, mentorship, training, and transition support.
7. Support the development of a data bank that profiles the make-up of the profession and enables strong evidence-based and informed decision-making.
8. Invest in a programme of marketing communications to communicate the opportunities available to new and recent graduates through a career in general dental practice.
9. Reinvigorate the Regional Committees to ensure an ear and voice for practitioners.
10. Engage with banks and relevant financial institutions to represent the dental profession from a financing perspective and the viability of the same.
Conclusion
A transformative model of general dental practice in Ireland is both necessary and achievable – but it requires urgent, co-ordinated implementation. This vision, shaped by the lived realities of general practitioners, outlines the steps needed to strengthen and underpin the delivery of sustainable oral healthcare in Ireland.
Read the full document at www.dentist.ie.
The IDA’s pre-Budget submission is prioritising investment in resourcing and legislative reforms.
The Irish Dental Association’s pre-Budget submission, ‘Fit for the Future: Resourcing, Regulation and Reform in Oral Health’, outlines a comprehensive and tenable pathway to address the critical challenges facing the profession that will improve access to dentistry for patients in Ireland and, critically, futureproof the delivery of care through strategic investment in a better-resourced public system, and an education structure that facilitates a greater number of dental graduates and new dentists practising in Ireland.
The current landscape: cracks in the system
Oral healthcare in Ireland is in crisis, suffering as a result of persistent underfunding amounting to a staggering ¤800m shortfall since 2007. Not surprisingly, this has had serious consequences—particularly for PRSI and medical card patients. In 2023, 104,000 schoolchildren missed HSE dental screening appointments due to a severe shortage of public-only dentists.
Our dental schools in Dublin and Cork are also underfunded, contributing to a shortage of new graduates. While we welcome the planned new dental school at RCSI, investment is still required at our existing schools. Moreover, we are increasingly out of step with our international colleagues in not having a mentoring programme for new graduates or newly arrived dentists to Ireland to gain experience in a mentored environment.
Additionally, the Dental Act of 1985 remains wholly outdated; that it does not require professional competency standards for dentists and auxiliaries – something now standard in all other healthcare professions – needs urgent address.
Six key recommendations for Budget 2026
To reverse this decline and ensure equitable access to care, the IDA urges the Government to invest in six critical areas:
1. Expand the Med 2 (dental tax relief) scheme
The Association is requesting amendments to existing tax relief available for dental care. It is outlining two proposals ranked in order of preference, as follows::
n extend the scope of tax relief at the standard rate of tax to routine dental treatment to cover preventive and rehabilitative treatments currently excluded, including direct restorations (fillings within the mouth), all extractions and dentures; and,

Roisín Farrelly Director of Advocacy & Communications
n restore tax relief at the marginal rate of tax for existing non-routine dental treatment for which income tax relief at the standard rate of tax is currently available.
2. Critical skills list inclusion for dentists and dental nurses
We call for the reversal of the decision to list dental nurses as ineligible for work permits and recommend adding dentists and dental nurses to the Critical Skills List. This would allow non-EEA professionals to access Stamp 4 status after two years, similar to doctors, and help address the significant recruitment challenges in the sector.
3. Restoring the ¤800m deficit
We seek Government commitment to restoring the ¤800m lost between 2009 and 2023 in dental supports for PRSI and medical card patients. With 800 fewer dentists contracted to the DTSS compared to 2012 – despite 15% population growth – this funding is critical to meet demand. The Government must hire an additional 920 dentists to strengthen the public dental system and support the delivery of the Smile agus Sláinte national oral healthcare policy.
4. Statutory continuous professional development
The Government’s commitment to introduce legislation this year providing for mandatory continuous professional development (CPD) is very welcome to bring dentistry in line with other regulated health professions. This can be implemented at minimal cost to the State, and we urge the Minister to do so without delay.
5. Structured mentoring scheme for new graduates
The IDA is calling for a budgetary allocation of ¤3m to reintroduce a structured mentoring scheme to facilitate new graduates in gaining experience in a mentored environment.
Such a scheme would help address the considerable unmet need of the Irish population, while also underpinning the continuing professional development of new graduates, mirroring best practice internationally.
6. Cap non-EEA student intake at 20%
Currently, approximately 40% of total dental student intake is from outside the EEA. While these students contribute significantly to funding, the vast majority do not remain in Ireland post graduation, impacting workforce planning. A 20% cap would ensure more opportunities for Irish and EEA students who are more likely to practise here after graduating.
A collaborative path forward
The IDA remains committed to working closely with the Government to ensure that programmes like Smile agus Sláinte succeed in delivering the best oral healthcare outcomes for all. We welcome the continued support of members as we advocate for these vital reforms.
Précis: This case report highlights the conservative management of non-syndromic multiple supernumerary teeth and emphasises the importance of vigilant radiographic monitoring, especially for future orthodontic considerations.
Abstract
This paper presents a case of metachronous supernumerary teeth in the mandibular premolar region, following previous removal of a supernumerary tooth and orthodontic treatment, in an adolescent patient following an interval of eight years.
Individual or multiple supernumerary teeth can develop anywhere in the jaws, although it is unusual for sequential supernumerary teeth to develop in late adolescence and after orthodontic treatment, particularly in non-syndromic patients.
The management of asymptomatic supernumerary teeth should fully consider the risks and benefits of surgical removal. Clinicians should remain aware of the possibility of subsequent supernumerary removal, and the presented case emphasises the importance of radiographic monitoring if subsequent orthodontic treatment is being considered following previous identification of supernumerary teeth.
Keywords: supernumerary; orthodontics; case report; multiple premolar supernumeraries; sequential supernumerary.
Journal of the Irish Dental Association 2024;71(4):185-189
Introduction
Supernumerary teeth are additional to the normal complement of 20 primary teeth and 32 permanent teeth. The presence of additional teeth can be referred to as ‘hyperdontia’, and supernumerary teeth can occur in 0.3-0.8% of primary dentitions and 1.2-3.5% of permanent dentitions.1 There may be under-reporting of primary dentition supernumerary teeth if they have erupted in an acceptable alignment or have exfoliated early. Supernumerary teeth are usually diagnosed at a single point in time and are referred to as non-sequential. In contrast, metachronous supernumerary teeth may develop and be identified at multiple time points throughout a patient’s lifetime.

Reanna Craig
BDS MFDS RCS(Eng) FHEA
School of Dentistry
Belfast Health and Social Care Trust
In the permanent dentition, supernumeraries have been reported to be more common in males.1,2 This sex-related pattern is not observed in primary teeth. Patients who develop primary supernumerary teeth may exhibit a higher likelihood of presenting with this anomaly in the permanent dentition.3 Supernumerary teeth can be categorised by shape, including conical, tuberculate, supplemental and odontomas.4 Conical supernumeraries often exhibit a ‘pegshaped’ appearance and typically manifest palatal to, or erupted between, the maxillary central incisors, often referred to as a mesiodens. Tuberculate supernumerary teeth are often located in the maxillary midline, are barrel-
Andrew McBride
BDS MFDS MOrth
MDSc FDS(Orth)
Consultant Orthodontist and Honorary Lecturer
School of Dentistry
Queen’s University Belfast
Prof. John Marley
BSC BDS PhD FDSRCS(Eng) FDS(Oral Surg) RCS(Eng)
FFDRCSI
Consultant Oral Surgeon and Honorary Professor
School of Dentistry
Queen’s University Belfast
Corresponding author: Reanna Craig E: rcraig19@qub.ac.uk
Chris Johnston
BSC BDS FDS MOrth FDS(Orth) RCSEd PhD
Consultant Orthodontist and Clinical Reader
School of Dentistry
Queen’s University Belfast


shaped, generally larger in size, and display incomplete root formation.4 The term ‘supplemental’ is used to describe well-formed additional teeth, commonly found in the upper lateral incisor region and also the premolar or molar region.1
Odontomas include ‘compound odontomas’ for tooth-like structures and ‘complex odontomas,’ for hamartomatous tooth-like formations.1
Supernumerary teeth can present as single or multiple teeth, unilateral or bilateral. Although supernumerary teeth can be located in any region of the maxilla or mandible, they are most commonly located in the premaxilla.2,3,5-7 The second most common location for multiple supernumeraries is the mandibular premolar region.5,6 Supernumerary teeth in the premolar region account for 810% of cases, with 75% presenting in the mandibular arch.5,6 Among supernumerary teeth in the mandibular premolar region, 75% are reported to be unerupted and asymptomatic.8 The mandibular premolar region has been reported as the most common site for multiple supernumeraries in non-syndromic patients.9 Yousof found that 44.8% of non-syndromic multiple supernumerary teeth occurred within the mandibular premolar area.9 Erupted supernumerary teeth can be identified through clinical examination. Unerupted supernumerary teeth are normally identified by radiographic examination. Various theories have been proposed to explain the aetiology of supernumerary tooth development. The atavism theory, which proposes a connection to the evolution of the dentition, has been discredited by Primosch10 due to the high incidence of single supernumerary teeth and their ectopic position. Another theory, dichotomy, postulates that the tooth bud splits in two.11 Hyperactivity of the dental lamina is now the widely accepted aetiology of excessive tooth development.7 Primosch theorised that supplemental supernumeraries develop from an accessory tooth bud,7 and more poorly formed supernumerary teeth develop from the epithelial remnants of the hyperactive dental lamina.7 A positive family history is often observed with supernumerary teeth.5 There is no simple genetic pattern that has been identified, and the complex interactions of genetic/environmental interfaces have led to theories of the influence of environmental factors and the possibility of sporadic genetic mutations.12 Supernumerary teeth can adopt various orientations, either remaining impacted or erupting into the oral cavity. Studies by Stafne5 and Brook,13 have reported that around 25% of permanent supernumerary teeth have the potential to erupt.
Supernumerary teeth can contribute to delayed eruption of permanent teeth. Non-eruption of permanent central incisors has been reported to be associated with supernumerary teeth in 26-57% of cases.7 Supernumerary teeth can also result in median diastemas, rotations, periodontal defects or crowding, and have also been associated with dilaceration, abnormal permanent root development, cystic formation,1,6 and resorption of adjacent teeth with pulpal necrosis.12 During orthodontic treatment, unerupted supernumerary teeth can prevent space closure.13
Disorders that have been reported to exhibit an increased prevalence of supernumerary teeth include: cleft lip and palate (CLP); Gardner’s syndrome (GS); and, cleidocranial dysplasia (CCD).10,14,15 Multiple supernumerary formation is strongly linked to GS and CCD. Other less common syndromes associated with supernumerary teeth are: Fabry Anderson syndrome;16 Ellis-Van Creveld syndrome;17 Ehlers-Danlos syndrome;18 incontinentia pigmenti; and, trico-rhinophalangeal syndrome.19 CCD is a rare autosomal dominant disorder, characterised by skeletal and dental anomalies. Classic CCD presents with a triad of symptoms considered to be pathognomonic of the condition: absent or hypoplastic clavicles; multiple supernumerary teeth; and, open cranial sutures.20 Patients with CCD often present with delayed eruption of permanent teeth, root abnormalities, ectopic teeth, prolonged retention of deciduous teeth, supernumerary teeth, and an underdeveloped maxilla resulting in a Class III malocclusion.19
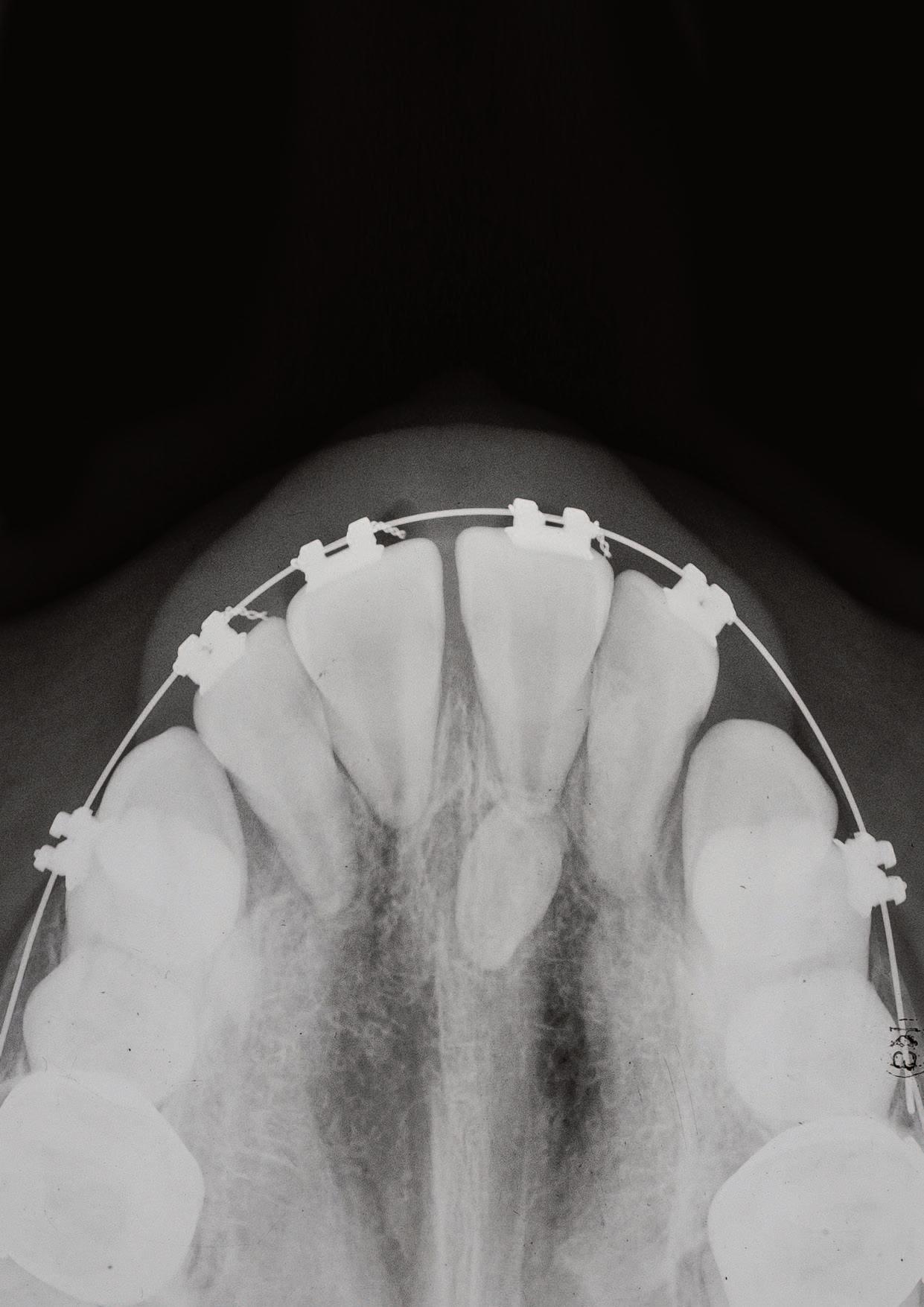
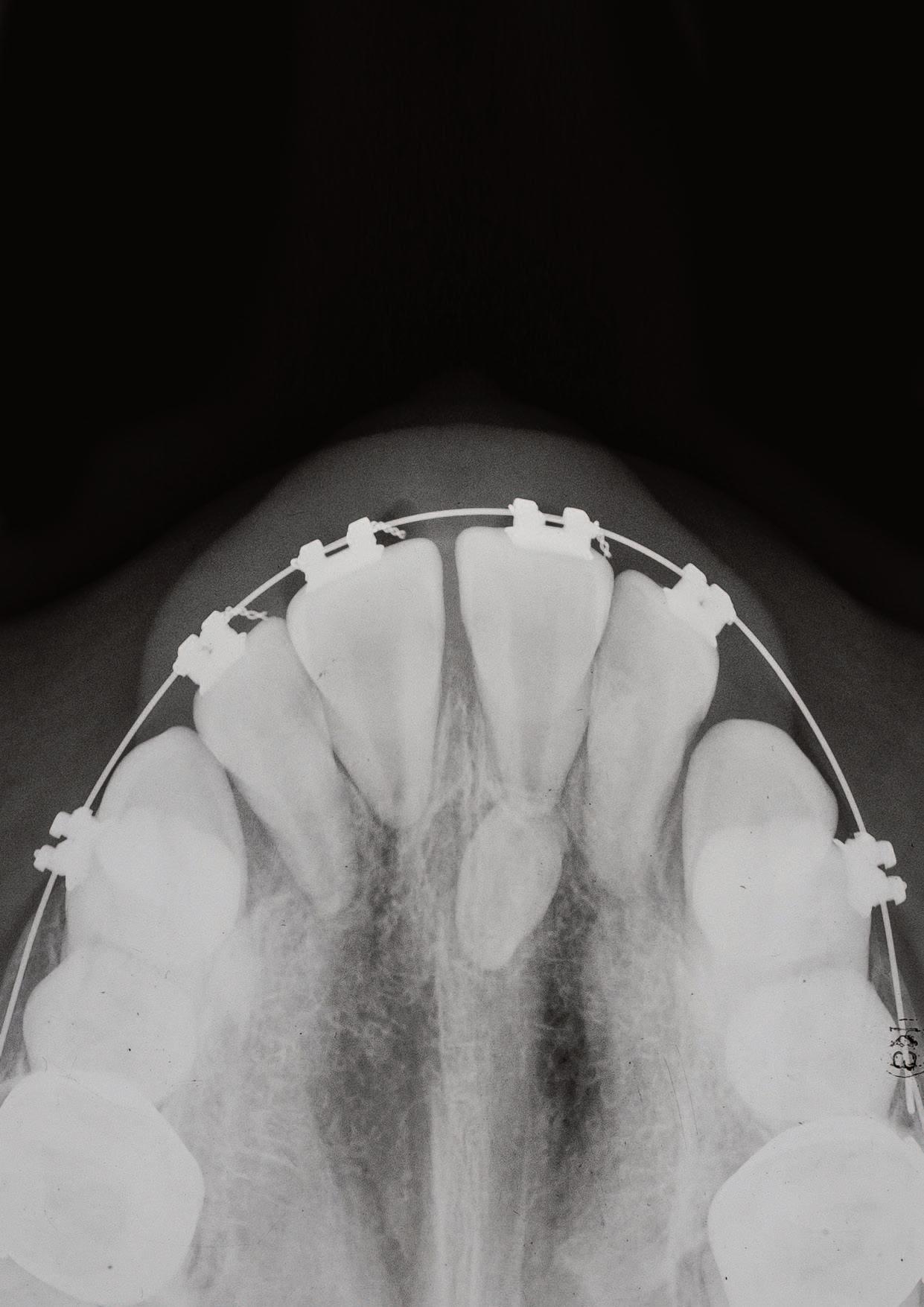
This patient first attended the Oral Surgery Department of Royal School of Dentistry Belfast for removal of a compound odontome in the right mandibular premolar region. This was an incidental finding discovered during assessment for orthodontic treatment (Figure 1). There was no evidence at that time of any other supernumerary teeth elsewhere in the jaws. This compound odontome tooth was surgically removed at that time following the informed consent process. The patient subsequently completed orthodontic treatment. Eight years later, at the age of 21, the patient was referred to the Oral Surgery Department for a second time due to the incidental finding of another supernumerary tooth on the contralateral side (Figure 2). The patient reported no relevant medical or genetic conditions. There was no reported family history




of supernumerary teeth. Clinical examination at age 21 years revealed a wellaligned dentition with a maxillary bonded retainer in place (Figure 2). No symptoms were reported related to the supernumerary teeth. None of the teeth were tender to percussion and all adjacent teeth exhibited a positive response to ethyl chloride. There was a palpable lingual bulge in the alveolar region of the lower left second premolar and first permanent molar. The panoramic radiograph indicated the presence of a radiopaque lesion and a radiolucent lesion in the left mandibular premolar region (Figure 3). A conebeam computed tomography scan was recorded to further characterise the lesion and surrounding area to aid surgical planning (Figure 4).

A maxillofacial radiology report confirmed the presence of fused supernumerary teeth with abnormal crown forms, with an inferiorly located mixed density lesion. The circular mixed density lesion had a radiodense periphery and a radiolucent core superimposed by the inferior alveolar canal. The follicle of the fused supernumeraries and that of the mixed density lesion were confluent. The mixed density lesion was consistent with an invaginated (dilated) odontome. Minor root resorption was reported into the outer dentine of the lower left premolar and lower left first molar.
The patient was happy with the outcome of their previous orthodontic treatment and no further orthodontic treatment was planned. The risks and
benefits of surgical removal of the supernumerary teeth were discussed with the patient, including consideration of the proximity of the roots of adjacent teeth, and the inferior alveolar canal. It was agreed that a further radiographic reassessment would be carried out in 18 months to monitor for the possibility of cystic change or resorption. The possibility of further supernumerary development was discussed with the patient.
Discussion
We have described the case of metachronous development of supernumerary teeth and odontome in the right mandibular premolar region, eight years following removal of a supernumerary in the right mandibular premolar region.
Multiple supernumerary teeth can be associated with a developmental genetic aetiology and associated syndromes such as GS and CCD.10,15 While supernumerary teeth are a common clinical phenomenon, metachronous supernumerary teeth are rare.21 Non-syndromic multiple supernumerary teeth have been reported to have a predilection for the mandibular premolar region. 9 A review of the literature did not reveal any case reports of metachronous supernumerary formation in syndromic patients. Multiple supernumerary teeth are defined as more than three or five. The reported prevalence of multiple supernumeraries varies within the literature, with some studies reporting less than 1% of cases while others indicate a prevalence of 14% in certain populations.6,7
The timing of supernumerary development in this case is atypical, and presented at 21 years. It is generally agreed that supernumeraries develop later than the normal dentition, attributed to delayed root development observed radiographically It is estimated that supernumerary premolars exhibit a delayed development of 7-11 years compared to normal premolars. 22 Case studies documenting late developing supernumerary premolars consistently indicate that these supernumeraries tend to appear later than supernumeraries in other locations.23 Oehlers reported continued supernumerary premolar root growth in a 23-year-old man. Due to their delayed development, supernumerary premolars have been postulated to be part of a third series of teeth, supporting the post-permanent dentition theory as an explanation for this phenomenon.24
Treatment planning requires consideration of various tooth factors, including angulation and proximity to the cortical bone, inferior alveolar nerve, mental nerve, blood vessels, and neighbouring teeth. Moreover, management is significantly influenced by patient-specific factors, including their capacity to withstand interventions, aesthetic considerations, the current symptoms and medical background.
Two approaches are available for the management of supernumerary teeth. The first is proactive removal. Theoretically, this approach offers the advantage of removing further risk of root resorption of adjacent teeth. Supernumeraries do not usually cause resorption, although if they develop roots, they may have the eruptive potential to cause resorption of adjacent teeth.7 Removal of a supernumerary may reduce the risk of cystic formation and ankylosis.6,7 Timely removal can also harness the eruptive potential of obstructed teeth and has been described to provide an improved prognosis.7 The bone quality in younger patients may make removal easier, although this must be weighed against the increased likelihood of requiring a general anaesthetic. This was the approach taken to manage the right mandibular supernumerary at age 13 in this patient to facilitate orthodontic tooth movement and to reduce the risk of root resorption of adjacent teeth.
An alternative approach involves radiographic monitoring in the absence of symptoms or planned orthodontic treatment. The advantages of radiographic monitoring include the lack of postoperative pain and discomfort, infection, bruising, and swelling, and avoidance of potential nerve trauma. Avoidance of a general anaesthetic also removes risk of mortality or morbidity. Leaving the supernumerary in situ can remove the risk of post-surgical permanent numbness or devitalisation of adjacent teeth. If the supernumerary is located near immature roots, delaying treatment until these have fully developed can minimise potential growth disruption.25 Garvey et al supported this approach in patients with the absence of symptoms or pathology, where all permanent teeth have erupted unimpeded and where no orthodontics is planned, and that approach was adopted in this case. Radiographic evaluation prior to orthodontic treatment – including in cases of retreatment – remains essential. Clinicians should maintain an index of awareness that additional supernumerary teeth can emerge over time even if this is exceedingly rare.21
This case report demonstrates an uncommon presentation of supernumerary teeth. It is unusual for multiple supernumerary teeth to present in the absence of an associated syndrome. Nevertheless, there are previous reports of supernumerary teeth developing in the mandibular premolar region in late adolescence and early adulthood. Clinicians should make patients aware of the possibility of the future development of additional supernumerary teeth. Supernumerary teeth can often be managed conservatively in the absence of complications, with appropriate longitudinal radiographic examination. This is particularly important in patients who are subsequently considering orthodontic treatment. Careful consideration should be given to their removal in relation to the risks to adjacent structures and the benefits of removal. In cases with additional clinical features, consideration should be given to a genetic aetiology.
References
1. Rajab LD, Hamdan MA. Supernumerary teeth: review of the literature and a survey of 152 cases. Int J Paediatr Dent. 2002;12(4):244-254.
2. Sharma A, Singh VP. Supernumerary teeth in Indian children: A survey of 300 cases. Int J Dent. 2012;2012:745265.
3. Lu X, Yu F, Liu J, Cai W, Zhao Y, Zhao S, et al. The epidemiology of supernumerary teeth and the associated molecular mechanism. Organogenesis. 2017;13(2):7182.
4. Meade M. Supernumerary teeth: an overview for the general dental practitioner. Dent Update. 2020;47(9):729-738.
5. Stafne EC. Supernumerary teeth. Dent Cosm. 1932;74:653-659.
6. Nazif MM, Ruffalo RC, Zullo T. Impacted supernumerary teeth: a survey of 50 cases. J Am Dent Assoc. 1983;106(8):201-204.
7. Primosch R. Anterior supernumerary teeth: assessment and surgical intervention in children. Pediatr Dent. 1981;3(2):204-215.
8. Breckon JJW, Jones SP. Late-forming supernumeraries in the mandibular premolar region. Br J Orthod. 1991;18:329-331.
9. Yousof WZ. Non-syndromal multiple supernumerary teeth: Literature review. J Can Dent Assoc. 1990;56:147-149.
10. Golan I, Baumert U, Hrala BP, Mussig D. Dento-maxillofacial variability of cleidocranial dysplasia: clinicoradiological presentation and systematic review. Dentomaxillofac Radiol. 2003;32:347-354.
11. Taylor GS. Characteristics of supernumerary teeth in the primary and permanent dentition. Dent Pract Dent Rec. 1972;22:203-208.
12. Sian JS. Root resorption of first permanent molar by a supernumerary premolar. Dent Update. 1999;26:210-211.
13. Brook AH. Dental anomalies of number, form, and size: their prevalence in British schoolchildren. J Int Assoc Dent Child. 1974;5:37-43.
14. Bohn A. Dental anomalies in harelip and cleft palate. Acta Odontol Scand. 1963;21:1-114.
15. D’Agostino S, Dell’Olio F, Tempesta A, Cervinara F, D’Amati A, Dolci M, et al. Osteoma of the jaw as first clinical sign of Gardner’s syndrome: the experience of two Italian centers and review. J Clin Med. 2023;12(4):1496.
16. Regattieri LR, Parker JL. Supernumerary teeth associated with Fabry-Anderson’s syndrome. Oral Surg Oral Med Oral Pathol. 1973;35:432-433.
17. Hattab FN, Yassin OM, Sasa IS. Oral manifestations of Ellis-Van Creveld syndrome: report of two siblings with unusual dental anomalies. J Clin Pediatr Dent. 1998;22:159-165.
18. Melamed Y, Barkai G, Frydman M. Multiple supernumerary teeth (MSNT) and EhlersDanlos syndrome (EDS): a case report. J Oral Pathol Med. 1994;23(2):88-91.
To claim CPD points, go to the MEMBERS’ SECTION of www.dentist.ie and answer the following questions:
1. What is the most common location for supernumerary teeth?
l A. Lower premolar region
l B. Upper premolar region
l C. Premaxilla
19. Gorlin RJ, Cohen MM, Wolfson J. Tricho-rhino-phalangeal syndrome. Am J Dis Child. 1969;118(4):595-599.
20. Tanaka JL, Ono E, Filho EM, Castilho JC, Moraes LC, Moraes ME. Cleidocranial dysplasia: importance of radiographic images in diagnosis of the condition. J Oral Sci. 2006;48:161166.
21. Moore SR, Wilson DF, Kibble J. Sequential development of multiple supernumerary teeth in the mandibular premolar region: a radiographic case report. Int J Paediatr Dent. 2002;12(2):143-145.
22. Rubenstein LK, Lindauer SJ, Isaacson RJ, Germane N. Development of supernumerary premolars in an orthodontic population. Oral Surg Oral Med Oral Pathol. 1991;71:392-395.
23. Cochrane SM, Clark JR, Hunt NP. Late developing supernumerary teeth in the mandible. Br J Orthod. 1997;24(4):293-296.
24. Oehlers FA. Postpermanent premolars. Br Dent J. 1952;93:157-158.
25. Garvey MT, Barry HJ, Blake M. Supernumerary teeth: an overview of classification, diagnosis, and management. J Can Dent Assoc. 1999;65:612-616.
2. What orthodontic concerns are not associated with supernumerary teeth?
l A. Cystic formation
l B. Rotations
l C. Class III malocclusion
l D. Delayed eruption
Submitted by Dr Niamh Coffey, Royal College of Surgeons in Ireland.
A 30-year-old woman, currently 23 weeks pregnant, attends for routine dental examination. She complains of bleeding gums, exacerbated by brushing. Apart from current pregnancy, there is no relevant medical history. On examination, gingivae are erythematous, swollen and bleed easily on probing. Localised plaque and calculus deposits are visible, particularly in the anterior region. However, there is no clinical attachment loss or mobility.
3. Which disorders are associated with an increased prevalence of supernumerary teeth?
l A. Gardner’s syndrome
l B. Turner syndrome
l C. Down syndrome
Questions
1. What is the most likely diagnosis?
2. What is the current evidence linking periodontal health and pregnancy outcomes?
3. What management is appropriate for this patient during pregnancy, based on current guidelines?
4. What precautions should be taken when providing dental care during pregnancy?
Answers on page 201.
Précis: Facial infiltrating lipomatosis is associated with dental developmental anomalies and medical complications of the affected side, requiring multidisciplinary care.
Abstract
Introduction: Facial infiltrating lipomatosis (FIL) is a rare congenital and benign condition, resulting from mature non-encapsulated adipocytes penetrating into neighbouring structures. Individuals with FIL present with unilateral facial and craniofacial hemihypertrophy, alongside various medical and dental complications of the affected side.
Case report: At birth, the infant had an evident right-sided facial swelling, which remained asymptomatic but continued to increase in size. Mild right-sided hearing and visual impairments were also present, with an epidermal naevus evident on the right cheek Magnetic resonance imaging confirmed right-sided lipomatous hyperplasia and genetic testing confirmed a somatic mutation to PIK3CA – the cause of cell hyperproliferation, often identified in FIL cases. A multidisciplinary team (paediatric medicine and dentistry, dermatology, ear, nose and throat (ENT), and plastics at Great Ormond Street Hospital) has contributed to managing the complex condition. At 12 months old, paediatric dentistry observed premature eruption of teeth 53, 54 and 84, and hyperplasia of the upper right alveolar arch. At five years old, the child presented with premature exfoliation of primary teeth and premature eruption of permanent teeth 14, 16, 41, 42 and 46, with bilateral crossbites.
Management: A dental prevention regime has been implemented and the child remains caries free. The developing dentition will continue to be monitored with consideration of orthodontic management. As the child remains stable, a conservative approach without surgical or medical intervention has been adopted. His vision has been corrected with glasses.
Conclusion: FIL is associated with dental developmental anomalies and medical complications of the affected side, requiring multidisciplinary care.
Keywords: FIL; facial infiltrating lipomatosis; swelling; unilateral swelling; multidisciplinary; congenital; genetic mutation; PIK3CA.
Journal of the Irish Dental Association 2025;71(4):190-193
Introduction
Facial infiltrating lipomatosis (FIL) is a rare congenital condition first described by Slavin in 1983.1 The major morphohistological characteristics of FIL include: mature non-encapsulated adipocytes penetrating neighbouring structures (e.g., masseter muscle, parotid); 2 benign proliferation of adipocytes; absence of lipoblasts; increase in numbers of vessels and nerves; and, adjacent bone hypertrophy. Facial asymmetry is typically observed at birth and progresses with growth.3

Dr Ayoola Bode
BDS MFDS RCS Eng Paediatric Dental Core Trainee
Royal Belfast Hospital for Sick Children/School of Dentistry, Queen’s Belfast
Dr Fawad Aslam
MBBS MRCP
Dermatology Trainee
Royal Belfast Hospital for Sick Children
Dermatological features are often the first to be noticed and include: unilateral facial swelling with ipsilateral epidermal naevi of varying length; hypertrichosis; thickened lips; and, capillary blush.4 Oral features include:
Dr Donal O’Kane
MB BCh BAO MRCP PhD
Consultant Dermatologist
Royal Belfast Hospital for Sick Children
Corresponding author: Dr Ayoola Bode E: Ayoola.bode@hotmail.com
Dr Angela McIntosh MBChB MRCPCH
Consultant Paediatrician
Department of Paediatrics
Altnagelvin Hospital Londonderry
Dr A. Karen Humphreys
BDS MFDS FDS(Paed Dent) RCSEd Paediatric Dental Consultant
Royal Belfast Hospital for Sick Children/School of Dentistry, Queen’s Belfast

ipsilateral hemimacroglossia; unerupted teeth; hypodontia; mucosal neuromas; and, macrodontia.2,3,5 Advances in sequencing technology have demonstrated the link between somatic phosphatidylinositol 3-kinase catalytic subunit alpha (PIK3CA) pathogenic variants and numerous overgrowth disorders (PIK3CA-related overgrowth spectrum or PROS). 5 PIK3CA mutations result in cell hyperproliferation6 and have been identified in FIL patients.7 Localised and segmental lesions like FIL are associated with hotspot PIK3CA variants, whereas systemic disorders that would be the main differentials, such as CLOVES syndrome (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and skeletal/scoliosis and spinal abnormalities) and MCAP (megalencephaly-capillary malformation-polymicrogyria) are more likely to be caused by non-hotspot and rare PIK3CA variants.2
Medical background
We present the case of a male infant born at full term by elective caesarean section at 39 weeks’ gestation who exhibited a right-sided facial swelling soon after birth. The swelling appeared to be asymptomatic and there were no associated feeding difficulties. An increase in size of the swelling was noted at a four-week assessment by the paediatric medical team.
Dermatological features
In addition to the right cheek swelling, a faint linear hyperpigmentation of the right cheek was noted by the paediatric dermatology team. This was initially localised to the pre-auricular skin but with time became more prominent on the cheek and forehead, and developed the classical appearance of an epidermal neavus. Subtle telangiectasia and mild hypertrichosis of the involved cheek also became more obvious over the first two years (Figure 1).
Investigations
An ultrasound of the right cheek on day six post birth demonstrated a diffuse increase in subcutaneous fat within the cheek. No abnormal Doppler blood flow or cystic component was identified. A repeat ultrasound after eight weeks demonstrated an increase in size of the abnormality but with a similar radiological appearance. Magnetic resonance imaging (Figures 2 and 3) at 11 weeks demonstrated lipomatous hyperplasia of the right head and neck soft tissues including the buccal, pre-auricular and submandibular regions (Figures 2 and 3). Imaging supported the clinical diagnosis of unilateral FIL, prompting genetic testing for a PIK3CA mutation. A sample from the right buccal mucosa confirmed a somatic mutation to PIK3CA (Figure 4).



4: Frontal view showing increase in size of right-sided unilateral swelling involving the buccal, pre-auricular and submandibular regions (age: five years and seven months).
In addition to the cutaneous presentation, the presented case has mild right-sided hearing impairment secondary to the surrounding tissue overgrowth and also anisometrophic hypermetropia and astigmatism in the right eye (managed by corrective glasses). He is otherwise doing well with no concerns of developmental delay. Now aged six, he is doing well at school following appropriate adjustments to his classroom environment for his mild hearing impairment. Due to the rare, complex nature of his diagnosis, he remains under the care of a number of medical specialties including dermatology, ear, nose and throat (ENT), and a plastic surgery team at a tertiary centre (Great Ormond Street Hospital). Surgical and medical (systemic PIK3 inhibitors) interventions may be required in the future; however, as he has remained relatively stable in recent years, a conservative approach is currently being taken.


Dental progress
This child has always presented with a clinically caries-free dentition, and healthy intraoral soft tissues with no obvious ulceration. The dental anomalies are coincident with the right side, where infiltrating lipomatosis is present.
At age 12 months, the child presented with hyperplasia of the upper right alveolar arch and premature eruption of the upper right primary canine, upper right first primary molar and lower right first primary molar (53, 54 and 84).
At age three years and seven months, the child presented with early loss of the lower right primary lateral incisor (LRB), mild midline discrepancy, right buccal crossbite and left lingual crossbite (Figure 5).
At age five years and seven months, the child presented with early mixed dentition, i.e., premature eruption of the upper right first premolar, upper right first permanent molar, lower right permanent central incisor, lower right permanent lateral incisor, and lower right first permanent molar (14, 16, 41, 42 and 46), mild hypoplasia upper right first premolar (14), moderate midline discrepancy – right centreline shift, incisal class III – edge to edge, right-sided buccal crossbite, and left-sided lingual crossbite (Figure 6).
Dental management of the child at present
Over 4.5 years, a prevention regime was implemented:
n six-monthly attendance with the local community dentist; n 22,600 fluoride varnish application every six months; n 1,450ppm fluoride toothpaste with supervised brushing twice a day; n fissure sealants of the premature permanent dentition;
n clinical photography to document occlusion;
n annual review at the paediatric dental hospital for close monitoring; and,
n an assessment in the hospital’s orthodontic department will be conducted around age nine, following further growth and development of the permanent dentition, to determine if orthodontic intervention is necessary.
No active dental treatment has been required as the child remains caries free.
Discussion
FIL is a unilateral congenital craniofacial deformity caused by adipocytes infiltrating surrounding facial structures. The most frequently affected structures are the parotid, tongue and masseter.8
Radiological investigations involve magnetic resonance imaging to demonstrate diffuse fatty infiltration and increased thickness of subcutaneous fat on the affected side, as a bright signal.8 Computed tomography typically shows a non-encapsulated diffusely infiltrating low-attenuation mass and changes to the facial bones.9
A case reported by Hongrui et al 2 describes a patient who had computed tomography reconstruction, which showed considerable zygomatic and mandibular enlargement and misalignment of teeth, resulting in an overbite and malocclusion. This case also describes ipsilateral hemimacroglossia with some unerupted teeth on the affected side.2 Also, observed features of the affected side include: abnormal root formation; early eruption of deciduous and permanent teeth;9 hemimacroglossia; erythema; and, mucosal neuroma.3 FIL is predominantly asymptomatic but as it affects a patient’s appearance, it often impacts psychosocial well-being and facial functionality such as chewing, swallowing and vision.10
Genetic testing of samples obtained from FIL show PIK3CA to be the cause of soft tissue and bone overgrowth, as in this case report. The pathophysiology is not fully understood, especially why various cells, e.g., fat, bone, and endothelial cells with different embryonic origins, are affected.2 One theory is that the mutation occurs early in embryonic development before cell differentiation.2 Another theory is whether the mutated cells are affecting the surrounding cells through cell contact, cytokines or via other unknown mechanisms.2
Surgical resection is the main form of proposed treatment, involving the resection of infiltration of adjacent tissue and osteotomy of skeletal hyperplasia.2 However, due to the complexity of FIL presentations, surgery is
not always possible and pharmacological approaches are sought.2 Surgery carries the risk of recurrence and damage to vital anatomical structures.9 Surgery should ideally be performed at the end of the facial growth period. 11 Facial growth typically concludes around the age of 17 for females and around 21 for males.12 Parents of children with FIL may request early surgery for aesthetic and selfesteem issues that may become evident during the school years. However, due to the increased activity of the growth hormone prior to facial growth completion, the recurrence rate is likely to be increased.3 The delay of definitive surgery has advantages such as minimising the chance of damage to the facial nerve, decreasing the total number of procedures, and having a mature contralateral cheek contour to match.11 Liposuction can be attempted depending on the size of the lesion. Drug approaches utilise PIK3K-targeted inhibitors, which aim to reduce the lesion volume, thus improving function. Alpelisib is a PI3K-selective inhibitor 13 and studies have shown a significant reduction in volume of facial soft tissues after one month. Notably, the drug does not affect skeletal deformities. 10 Further prospective studies are required to investigate side effects, optimal treatment duration and dosage for age groups, and the possibility of relapse after drug withdrawal.2
Conclusion
FIL presents as a unilateral facial swelling that often presents at birth and slowly grows with age. Dermatological manifestations are the first noticeable signs and such patients need a thorough dermatological assessment to rule out systemic or syndromic associations. It is important that these patients are seen promptly and referred to other specialties appropriately and early. The associated dental anomalies require close monitoring and intense prevention advice to prevent decay to the prematurely developing dentition or the limited dentition if hypodontia is observed. Clinical examination, radiographical imaging and genetic testing aid diagnosis. The medical management is multifaceted with regular bi-annual or annual reviews depending on the specialty due to the potential involvement of several organs. Paediatric dentistry conducts an annual review of the child, in collaboration with the community dental services, to ensure comprehensive shared care. Multidisciplinary management is therefore crucial. Surgical and medical (PIK3 inhibition) treatment may be required in individual cases depending on the severity of overgrowth and associated complications.
To claim CPD points, go to the MEMBERS’ SECTION of www.dentist.ie and answer the following questions:
1. Which is not an oral feature of facial infiltration lipomatosis?
l A. Hemimacroglossia
l B. Mucosal neuroma
l C. Premature eruption of teeth
l D. Lichen planus
References
1. Slavin SA, Baker DC, McCarthy JG, et al. Congenital infiltrating lipomatosis of the face: clinicopathologic evaluation and treatment. Plast Reconstr Surg. 1983;72(2):158-164.
2. Hongrui Chen, Bin Sun, Wei Gao, et al. Facial infiltrating lipomatosis with hemimegalencephaly and lymphatic malformations caused by nonhotspot phosphatidylinositol 3-kinase catalytic subunit alpha mutation. Paediatr Dermatol. 2023;40(6):1115-1119.
3. Padwa BL, Mulliken JB. Facial infiltrating lipomatosis. Plast Reconstr Surg. 2001;108(6):1544-1554.
4. Chen H, Sun B, Gao W, et al. Delineation of the phenotypes and genotypes of facial infiltrating lipomatosis associated with PIK3CA mutations. Orphanet J Rare Dis. 2023;18(1):189.
5. Keppler-Noreuil KM, Rios JJ, Parker VE, et al. PIK3CA-related overgrowth spectrum (PROS): diagnostic and testing eligibility criteria, differential diagnosis, and evaluation. Am J Med Genet A. 2015;167A(2):287-295.
6. Fruman DA, Chiu H, Hopkins BD, et al. The PI3K pathway in human disease. Cell. 2017;170(4):605-635.
7. Maclellan RA, Luks VL, Vivero MP, et al. PIK3CA activating mutations in facial infiltrating lipomatosis. Plast Reconstr Surg. 2014;133(1):12e-19e.
8. Sun R, Sun L, Li G, et al. Congenital infiltrating lipomatosis of the face: a subtype of hemifacial hyperplasia. Int J Pediatr Otorhinolaryngol. 2019;125:107-112.
9. Harouna MS, Belgadir H, Fadoul A, et al. Facial infiltrating lipomatosis, a rare cause of facial asymmetry to be known: case report and literature review. Ann Med Surg (Lond). 2021;73:103118.
10. Wenger TL, Ganti S, Bull C, et al. Alpelisib for the treatment of PIK3CA-related head and neck lymphatic malformations and overgrowth. Genet Med. 2022;24(11):23182328.
11. Kamal D, Breton P, Bouletreau P. Congenital infiltrating lipomatosis of the face: report of three cases and review of the literature. J Craniomaxillofac Surg. 2010;38(8):610-614.
12. Hardin AM, Knigge RP, Oh HS, et al. Estimating craniofacial growth cessation: comparison of asymptote- and rate-based methods. Cleft Palate Craniofac J. 2022;59(2):230-238.
13. Venot Q, Blanc T, Rabia SH, et al. Targeted therapy in patients with PIK3CA-related overgrowth syndrome. Nature. 2018;558(7711):540-546.
2. Which mutated gene has been identified as the cause of facial infiltrating lipomatosis?
l A. ZNF469
l B. PIK3CA
l C. COL5A1
l D. B4GALT7
3. Which is not a dermatological feature of facial infiltrating lipomatosis?
l A. Unilateral facial swelling
l B. Epidermal naevi
l C. Cyanosis
l D. Thickened lips
Learning outcomes
On reading this paper, individuals should be able to:
n identify features of anterior and posterior crossbite amenable to interceptive orthodontics;
n design upper removable orthodontic appliances for anterior or posterior crossbite correction;
n understand component adjustment for anterior and posterior crossbite correction; and,
n recognise the value of typodont teaching for correction of these occlusal anomalies.
Introduction
Anterior or posterior crossbite may be first identified in the mixed dentition. The reported prevalence of anterior crossbite is 2.2% to 11.9%, depending on the age at assessment,1 whereas posterior crossbite is reported to affect 4% of European children and adolescents.2 Timely interceptive correction is advised for these occlusal anomalies when associated with mandibular displacement to avert the crossbite being perpetuated to the permanent dentition. In the case of a forward mandibular displacement associated with an anterior crossbite, correction also removes occlusal trauma, which, if left untreated, may lead to incisal wear and compromise periodontal support, with resultant mobility of the opposing lower incisor.3 On the other hand, a posterior crossbite with displacement has been associated, although weakly, with temporomandibular joint dysfunction.2,3 Where mandibular displacement remains untreated, a posturing habit may ensue and muscular activity may become asymmetric.3
Correction of anterior or posterior crossbite may be undertaken using either removable or fixed appliances.1,2 Features that make an anterior or posterior crossbite amenable to correction by orthodontic means are given in Table 1. The Dental Council of Ireland Accreditation Manual (2022)4 and the Graduating European Dentist (GED) resource of the Association for Dental Education in Europe (ADEE)5 indicate or recommend, respectively, that a graduating dentist must be able to design, insert and adjust active removable appliances to manage simple malocclusions. These would include correction of a single tooth anterior crossbite or a unilateral posterior crossbite, with associated mandibular displacement. With the reported prevalence of these anomalies, it is difficult in the undergraduate curriculum to provide sufficient clinical exposure to meet these requirements.

Declan Millett BDSc DDS FDS DOrth MOrth FHEA
Professor of Orthodontics, Oral Health and Development
Cork University Dental School and Hospital, University College Cork
Table 1: Features that make an anterior or posterior crossbite suitable for interceptive correction.
Anterior crossbite
n Class I/mild Class III skeletal pattern with average facial proportions
n Single upper incisor in crossbite with associated mandibular displacement
n Upright or slightly retroclined upper incisor
n Uncrowded or mildly crowded upper arch
n Average to increased overbite on the incisor in crossbite
Posterior crossbite
n Class I/mild Class II/III skeletal pattern with average facial proportions and no skeletal asymmetry
n Unilateral buccal crossbite with associated mandibular displacement
n Upright or palatal inclination of upper buccal segment teeth
n Uncrowded or mildly crowded upper arch
n Well interdigitating buccal occlusion
Indeed, the challenges of imparting competency in orthodontic treatment during undergraduate education have been clearly acknowledged.6 Final-year undergraduate dental students at four UK-based dental institutes reported a preference for case-based and practical teaching sessions in orthodontics, with less interest in lectures or problem-based learning approaches.7 Of those open to additional teaching, 30% requested supplementary practical sessions.7 Overall, more than 60% were interested in further teaching in interceptive orthodontics.7
Another UK survey of final-year dental students at Cardiff University, six months prior to graduation, identified that the lowest confidence was reported in relation to design, fit and adjustment of orthodontic appliances.8
This paper describes two typodont models to assist in teaching design, insertion and adjustment of upper removable appliances for two cases, one for correction of a single tooth anterior crossbite and the other for correction of a unilateral posterior crossbite, both amenable to interception in the mixed dentition.
Case descriptions
Case 1
n An eight-and-a-half-year-old child with a Class I malocclusion on a Class I skeletal base, with average facial proportions and no facial asymmetry; n upper and lower arches were uncrowded;
Keith Evans MATLHE RDT LOTA
Senior Instructor, Dental Technician (Orthodontics)
Cork University Dental School and Hospital, University College Cork
John Brown = MSc
PGCTLHE RDT LOTA
Late Emeritus Lecturer in Dental Technology (Orthodontics), Cork University Dental School and Hospital, University College Cork
Claire Laide BSc MSc 3D Imaging Technical Assistant Cork University Dental School and Hospital, University College Cork
Corresponding author: Declan T. Millett, Professor of Orthodontics, Oral Health and Development, Cork University Dental School and Hospital, University College Cork. E: d.millett@ucc.ie
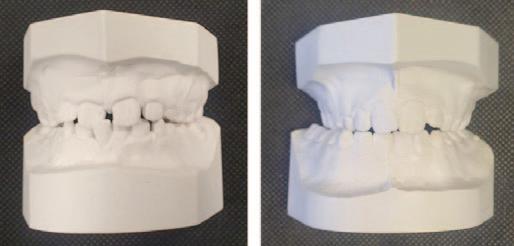
Table 2: Details of the upper removable appliance (URA) design* for correction of each crossbite.
Anterior crossbite
Activation:
Z spring (0.5mm hard stainless steel wire) to procline UR1
Retention:***
Adams clasps URD and ULD (0.6mm hard stainless steel wire)
Adams clasps UR6 and UL6 (0.7mm hard stainless steel wire)
Anchorage:****
Posterior teeth and supporting baseplate
Baseplate:
Posterior acrylic capping approximately 2mm to disengage the incisors
Posterior crossbite
Activation:
Midline expansion screw**
Retention:***
Adams clasps URD and ULD (0.6mm hard stainless steel wire)
Adams clasps UR6 and UL6 (0.7mm hard stainless steel wire)
Anchorage:****
Posterior teeth and supporting baseplate
Baseplate:
Posterior acrylic capping approximately 2mm to disengage the posterior teeth
*An upper removable appliance is designed as per the acronym ARAB: A = Activation; R = Retention; A = Anchorage; and, B = Baseplate.
**Note that a midline expansion screw, rather than a screw offset to the right buccal segment, is required for symmetrical upper arch expansion, as on initial occlusal contact the upper and lower midlines were coincident, but became discrepant on closure into maximum intercuspation.
***Retention near to the site of proclination (clasping URD and ULD) is required to counteract the displacing effect produced on activation of the Z spring. Using a midline screw for arch expansion affords the option of clasping the teeth that need to be moved (the upper right and left buccal segments).
****Anchorage (resistance to the force of reaction generated by the active components) requirements are minimal where one upper incisor is being proclined with a force of 30-50g. The resultant reactionary force is dissipated via the baseplate to the other teeth and the supporting alveolus. Upper arch expansion with a midline screw uses reciprocal anchorage as the teeth being moved are also the anchor teeth.
n UR1 was in crossbite with just over a 2mm anterior mandibular displacement from initial occlusal contact on the mesio-incisal edge of UR1; and, n LR1 was in traumatic occlusion displaced labially and mobile.
Case 2
n A nine-year-old child with a mild Class II division 1 malocclusion on a Class I skeletal base, with average facial proportions and no facial asymmetry;

Table 3: Adjustment of the active components for each appliance and subsequent appliance management.
Anterior crossbite
Active component:
Z spring (0.5mm hard stainless steel wire) to procline UR1
Adjustment for the typodont:
Pull the Z spring forward 1-2 mm, ensuring that it is still resting on the mid-palatal surface of the upper incisor. Repeat activation until the crossbite is corrected.
Clinically, reactivation of the z-spring would be on a monthly basis until the requisite tooth movement is achieved. Then, the buccal blocks should be reduced to half their height at one visit and removed completely at the following visit.
Wear of the URA should be maintained until the posterior occlusion settles. Provided adequate overbite is present (one-third to half coverage of the lower incisor), wear may then be discontinued and the developing occlusion monitored.
Posterior crossbite
Active component:
Midline expansion screw
Adjustment for the typodont:
With the 'key' provided, turn the midline screw forward one turn (this gives 0.25mm activation). Repeat adjustment until the crossbite is corrected.
Clinically, the screw would usually be turned twice weekly until crossbite correction is achieved. Then, the buccal blocks should be reduced to half their height at one visit and removed completely at the following visit.
Wear of the URA should be maintained until the posterior occlusion settles. Provided there is good buccal segment interdigitation, wear of the URA may be discontinued and the developing occlusion monitored.
n the upper right buccal segment was in crossbite with an associated right lateral mandibular displacement on closure of 2.5mm from initial occlusal contact on the upper right and lower right primary canines; and, n upper and lower arches were minimally crowded.
Removable appliance typodonts
Pre-treatment study models of these two cases (Figure 1) were duplicated in acrylic resin to produce two typodont models. For the anterior crossbite typodont model, the incisor in crossbite and associated acrylic were sectioned from the model; a 0.7mm stainless steel wire was inserted in a hole created two-thirds of the way down the incisor root, and the wire/tooth combination repositioned in the model with wax to replace the acrylic deficit. For the posterior crossbite typodont model, the model was sectioned in the midline and a 4mm wide trough of acrylic removed and replaced with wax.




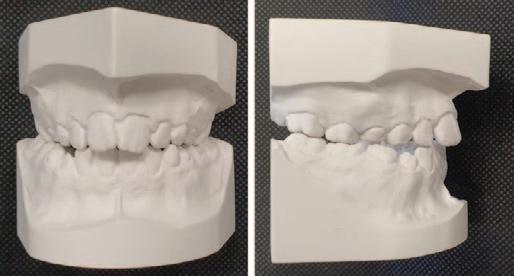
For posterior crossbite correction (Case 2), the midline screw was activated one turn (0.25mm) and the typodont placed in a hot water bath (50°C) for 10 minutes and then removed to monitor tooth movement. Reactivation of the midline screw was undertaken until the crossbite was corrected (Figure 6 ). This took 12 adjustments. The interdigitation of the buccal segment occlusion maintained crossbite correction (Figure 7). The adjustment of the active components and subsequent appliance management are described in Table 3
Appliances to the descriptions outlined in Table 2 were fabricated and fitted to each model (Figure 2). For anterior crossbite correction (Case 1) the Z spring was adjusted and the force measured with a Correx gauge (Table 3, Figure 3), and the appliance placed on the acrylic model, which was then placed in a hot water bath (50°C). After 10 minutes, the model was removed to assess tooth movement. Following further adjustment of the Z spring, the typodont was then replaced in the hot water bath and movement monitored until UR1 had been moved forward out of crossbite ( Figure 4 ). This took four adjustments. Simultaneous lingual movement of the labially displaced lower incisor occurred clinically with disengagement of the occlusion and soft tissue pressure from the lower lip ( Figure 5 ). The positive overbite on UR1 maintained crossbite correction.
Early orthodontic intervention in an undergraduate orthodontic clinic with removable appliances, or removable and fixed appliances for limited treatment outcomes, has been shown to be successful and cost effective. 9 With the current teaching objectives of the undergraduate curricula, 4,5 the high expectations of orthodontic patients,10 and the complexity of cases eligible for treatment within the publicly funded orthodontic services in the Republic of Ireland,11 cases suitable for upper removable appliance treatment alone are limited. 12 Apart from current use in clear aligner treatment, 13,14 removable orthodontic appliances constructed of wire and acrylic may at present be used effectively in carefully selected cases for anterior or posterior crossbite correction in the mixed dentition.
Aside from their use as an aid in undergraduate orthodontic teaching, the simulation exercises described here may also be useful for continuing professional development of dentists involved in primary care. Within the publicly funded orthodontic service, they would also allow instruction in the
provision of limited interceptive treatment for correction of some crossbite anomalies following consultant advice, and thereby reduce in part the burden placed on orthodontic treatment waiting lists.
The benefits of the simulation exercises described in this paper are that they:
n provide experience in the fitting of two standard removable appliances for anterior and posterior crossbite correction;
n give an opportunity to adjust active and retentive components on these appliances;
n allow tooth movement to be monitored following adjustment of the active components;
n simulate a course of orthodontic treatment in a condensed timeframe;
n provide a ‘hands-on’ learning opportunity, which can be repeated until the desired outcome is achieved;
n facilitate timely and constructive feedback; and,
n have a modest cost.
The limitations include:
n the time required to construct the models;
n the need for a hot water bath;
n wax does not mimic alveolar bone;
n settling of the occlusion cannot be reproduced; and,
n wax needs to be replaced following successful completion of each exercise.
Various types of typodont models have been used in undergraduate orthodontic programmes to assist with teaching adjustment of removable appliance components.15,16 Recently, there have been developments in virtual reality technology, haptics (enabling a sense of touch), and robotics in dental simulation.17 Haptic simulation has been shown to be a useful adjunct to phantom head teaching,18 providing real-time sensory feedback and a more optimal sense of a clinical procedure, which enhances the student learning experience.17 It would appear that such a system has not been developed for orthodontic simulation of the case types outlined in this paper, but in the future this may be produced. As curricula in orthodontic undergraduate education evolve,6,19 with a likely greater emphasis on acquisition of diagnostic rather than therapeutic skills, the simulation exercises described here and similar may be useful in provision of a brief exposure to what limited interceptive measures can achieve with targeted case selection.
Conclusions
n Anterior or posterior crossbite may be amenable to correction in the mixed dentition by removable orthodontic appliances; and, n instruction in appliance design, as well as fitting and component adjustment of these appliances, is afforded by typodont models.
Acknowledgements
Prof. Mairead Harding, Professor in Dental Public Health and Preventive Dentistry, University College Cork, and Mr Paul Lyons, Education Officer, Dental Council of Ireland, are thanked for their helpful comments.
References
1. Borrie F, Bearn D. Early correction of anterior crossbites: a systematic review. J Orthod. 2011;38(3):175-184.
2. Ugolini A, Agostino P, Silvestrini-Biavati A, Harrison JE, Batista KB. Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev. 2021;12(12):CD000979.
3. Fleming PS, Johal A, DiBiase AT. Managing malocclusion in the mixed dentition: six keys to success. Part 1. Dent Update. 2008;35(9):607-610, 612-613.
4 Dental Council of Ireland. Dental Council Accreditation Manual – January 2022. Dental-Council-Accreditation-Manual-2022_to-Schools.pdf (dentalcouncil.ie) Accessed August 15, 2024.
5. Association for Dental Education in Europe. Graduating European Dentist Curriculum. Published April 21, 2020. https://adee.org/graduating-europeandentist/graduating-european-dentist-curriculum. Accessed August 15, 2024.
6. Raghavan S, Abu Alhaija E, Ali K. Orthodontic curricula in undergraduate dental education—a scoping review. Int J Environ Res Public Health. 2023;20(6):4914.
7. Jauhar P, Mossey PA, Popat H, Seehra J, Fleming PS. A survey of undergraduate orthodontic teaching and factors affecting pursuit of postgraduate training. Br Dent J. 2016;221(8):487-492.
8. Gilmour ASM, Welply A, Cowpe JG, Bullock AD, Jones RJ. The undergraduate preparation of dentists: confidence levels of final year dental students at the School of Dentistry in Cardiff. Br Dent J. 2016;221(6):349-354.
9. Bernas AJ, Banting DW, Short LL. Effectiveness of phase 1 orthodontic treatment in an undergraduate teaching clinic. J Dent Educ. 2007;71(9):1179-1186.
10. Sayers MS, Cunningham SJ, Newton JT. How do you identify the patient with ‘high expectations’ of orthodontic treatment: an empirical approach. J Orthod. 2020;47(4):289-293.
11. Scott C. Understanding the IOTN. J Irish Dent Assoc. 2015;61(5):236-239.
12. Littlewood SJ, Tait AG, Mandall NA, Lewis DH. The role of removable appliances in contemporary orthodontics. Br Dent J. 2001;191(6):304-306, 309-310.
13. d’Apuzzo F, Perillo L, Carrico CK, et al. Clear aligner treatment: different perspectives between orthodontists and general dentists. Prog Orthod. 2019;20(1):10.
14. Johal A, Bondemark L. Clear aligner orthodontic treatment: Angle Society of Europe consensus viewpoint. J Orthod. 2021;48(3):300-304.
15. Jones ML, Volp C. A ‘mini-typodont’ for removable appliance teaching. Br J Orthod. 1989;16(4):277-279.
16. Mirmoghtadaie Z, Seifi M, Namdari M, Eskandarloo F, Amdjadi P. Effectiveness of educational intervention with non-wax and virtual typodont methods in practical orthodontic course of dental students, Shahid Beheshti University of Medical Sciences. J Dent School, SBUMS. 2023;40(2):67-72.
17. Farag A, Hashem D. Impact of the haptic virtual reality simulator on dental students’ psychomotor skills in preclinical operative dentistry. Clin Pract. 2021;12(1):17-26.
18. Huang Y, Huang S, Liu Y, Lin Z, Hong Y, Li X. Application of virtual reality and haptics system Simodont in Chinese dental education: a scoping review. Eur J Dent Ed. 2023:10.1111/eje.12984.
19. Agou S, Alansari R. Defining orthodontic learning outcomes for general dentists: a modified Delphi process-based curricular modification. Semin Orthod. 2024;30(4):413-421.
Impact of pulpectomy versus extraction of primary teeth on patient-centred outcomes: a systematic review of clinical studies
Vitali FC, Kominami PAA, Andrada AC, Takeshita EM, Massignan C.
Objectives: Although pulpectomy is recommended as the choice treatment for primary teeth with pulpal involvement, some clinicians and parents consider tooth extraction a viable option. This systematic review aimed to assess the impact of pulpectomy versus extraction of primary teeth on patient-centred outcomes.
Methods: Seven electronic databases and grey literature were searched on April 5, 2024. Two independent reviewers selected clinical trials comparing the impact of pulpectomy versus extraction of primary teeth on patient-centred outcomes. Studies not directly comparing pulpectomy versus tooth extraction were excluded. Critical data were summarised following the Synthesis Without Meta-analysis guideline. The risk of bias was assessed using the Version 2 Cochrane risk-of-bias tool for randomised clinical trials and the Risk Of Bias In Nonrandomized Studies of Interventions tool for non-randomised clinical trials. The certainty of evidence was assessed using the GRADE approach.
Results: A total of 1,228 studies were retrieved in the search. After the screening process, two studies were included. The outcomes evaluated were oral healthrelated quality of life (OHRQoL), dental anxiety, postoperative pain, and behaviour. Qualitative synthesis indicated that children treated with pulpectomy exhibited improved OHRQoL and lower dental anxiety than those treated with tooth extraction. The treatment modality did not influence behaviour and postoperative pain. Included studies present potential bias in specific domains. The certainty of evidence was low.
Conclusion: Pulpectomy demonstrated superior patient-centred outcomes, suggesting that it is a more favourable choice for treating primary teeth than tooth extraction.
J Evid Based Dent Pract. 2025;25(1):102072.
The role of hydroxyapatite-based, fluoride-free toothpastes on the prevention and the remineralisation of initial caries lesions: a systematic review and meta-analysis
Chatzidimitriou K, Theodorou K, Seremidi K, Kloukos D, Gizani S, Papaioannou W.
Objectives: he aim of the present systematic review and meta-analysis was to critically appraise all evidence available on the effectiveness of biomimetic hydroxyapatite (HAP) toothpastes in promoting remineralisation and inhibiting demineralisation.
Data: A literature search was conducted in electronic databases to identify in situ randomised controlled trials in children, adolescents, and young adults aged <25 years evaluating the effectiveness of fluoride-free HAP compared to conventional fluoride toothpastes.
Sources: Medline (via Pubmed), Embase, Scopus, Cochrane Central Register of Controlled Trials, Dentistry & Oral Sciences Source, and LILACS database were searched. Additional search of the grey literature, abstracts of conferences and meetings, and manual search of the reference lists of retrieved studies, were also performed.
Study selection: The search retrieved 68 studies, of which four were considered eligible.
Conclusions: Development of new and progression of existing lesions, recorded using DMFS/ICDAS indices, showed no significant differences between HAP and fluoride toothpastes. Significant differences were recorded in lesion size (p<0.0001) and fluorescence value (p=0.01) after six months. Meta-analysis showed non-significant risk ratio (0.98, p=0.61; 95 % CIs 0.85, 1.12) and odds ratio (0.90, p=0.68; 95 % CIs 0.57, 1.42) for HAP and fluoride toothpastes.
Clinical significance: HAP toothpaste could be an effective alternative to fluoride-containing toothpaste in preventing caries progression and promoting enamel remineralisation. The comparable performance of HAP to fluoride, coupled with its superior biocompatibility and lack of toxicity, positions it as a promising option for individuals seeking fluoride-free oral care solutions.
J Dent. 2025;156:105691.
Cleansing efficacy of the electric toothbrush Oral-B iO compared to conventional oscillating-rotating technology: a randomised-controlled study
Polak AL, Wiesmüller V, Sigwart L, Nemec N, Niederegger L, Kapferer-Seebacher I.
Objectives: This study aimed to compare the cleansing efficacy of the Oral-B iO electric toothbrush incorporating oscillating-rotating technology with microvibrations – with a traditional oscillating-rotating toothbrush.
Materials and methods: Thirty adult participants were randomly assigned to use the iO electric toothbrush with the brush head iO Ultimate Clean or the traditional oscillating-rotating toothbrush Oral-B Genius with the cross-action brush head. Oral hygiene indices (Rustogi Modified Navy Plaque Index and Gingival Bleeding Index) were assessed before and after 28 days of home use of the assigned product. Participants were instructed to refrain from interdental hygiene during the study period. After a two-week washout period, the clinical investigation was repeated in a crossover design.
Results: All 30 participants completed the study with no dropouts. After 28 days of use, the iO showed statistically significantly lower plaque levels than the conventional oscillating-rotating toothbrush (25.09% vs. 30.60%, p=0.029). This difference was particularly noticeable in marginal and approximal areas. There were no significant distinctions in gingival bleeding indices.
Conclusions: The Oral-B iO electric toothbrush displayed enhanced plaque removal efficiency compared to a conventional oscillating-rotating technology. Clinical relevance: This study highlights the potential benefits of advanced toothbrush technologies for plaque reduction and encourages further research.
Clin Oral Investig. 2024;28(9):493.
The 6C Clinic Conversion Framework can optimise the patient journey and boost profits.

Having worked in the dental sector for nearly two decades, I’ve had the privilege of visiting countless clinics and supporting practice owners on their journey to success. Over the years, I’ve gained valuable insights into what truly drives sustainable growth. But in the last two years, one recurring theme has emerged time and time again: “Our revenue doesn’t reflect our effort”, with rising running costs, increased wage bills, and lower treatment acceptance rates being the main offenders. This is not just frustrating, it’s disheartening. Over time, it can drain team morale, affect the owner’s selfesteem, and put financial pressure on a business that otherwise has so much potential. The good news? It can be fixed. And the solution lies in building a clinic that converts. Too often, I see dentists invest in marketing – whether through social media, ads, or new websites – hoping to raise their profile and attract new patients. But what happens after a patient enquires? That’s where the real conversion journey begins. If this journey isn’t supported by the right systems and strategies, then clinics risk throwing good money after bad. A converting clinic is one where every patient touchpoint – from first click to final follow-up – is optimised to build trust, communicate clearly, and inspire action. It’s not always about adding more – it’s about improving what’s
already there. That’s why I developed the ‘6C Clinic Conversion Framework’. It helps identify the gaps, align your systems, and ultimately increase your return, making you feel more in control of your business and its success.
1. Content that converts
Your online presence is often your first impression, and it needs to do more than just look good – it needs to connect. Dental websites typically have a conversion rate of 2-3%, 1 which is considered below optimal. Yet, many dental websites and social media pages are filled with jargon-heavy posts that fail to connect emotionally. Top-performing dental practices can achieve conversion rates as high as 23.1%.2 When I work with a clinic, we start by getting granular with the detail. Often this is an eye-opening exercise for the practice owner and means they can make the necessary changes based on evidence-based figures bespoke to their clinic. That is how you build the foundations for a clinic that converts, as everything that follows will be led by this process.
Lisa Grogan
Lisa Grogan Coaching

Conversion blocker: clinics post about treatments without explaining the benefits and why they matter to the patient. There’s little storytelling, no emotional hooks, and no clear call to action (CTA). The content is generic and does not inspire the onlooker to take action.
2. Contact that converts
Once a potential patient reaches out, the conversion clock starts ticking. Clinics that respond to enquiries within one hour are seven times more likely to secure a booking. But response times are just part of it – how your team communicates is everything.3
Conversion blocker: front of desk staff who quote prices without building rapport, give vague answers, or delay follow-ups. Any hesitation or shying away from discussing treatment options and pricing can break down a patient’s trust, and you risk them not converting into an appointment. Patients are not as loyal as the used to be and often call two to three clinics to see which one they feel more confident in attending. This is why equipping your reception team with the tools they need to handle these conversations with confidence is essential to the success of a clinic.
An online booking system on your website makes it very convenient for a patient to make a booking while they are in work. It can make the difference between a patient attending your clinic or going somewhere else. Approximately 77% of patients prefer providers that offer online booking and scheduling services.4
3. Conversations that convert Consultations are where connection and confidence create conversions. Studies show that 70% of patients go ahead with treatment when they feel heard, informed, and involved.5
Conversion blocker : talking through treatment options too quickly, not asking enough questions, or making the conversation overly clinical. Shying


away from discussing pricing can also break down patients’ trust. Lack of visual aids during the conversation can lead to lack of clarity for the patient – as the saying goes, ‘If you confuse, you lose!’
I see many practice owners invest in expensive equipment like scanners and attend courses to take on new treatment options. The reason behind this is to offer a better patient journey, raise the practice profile, and to attract more high-value work into the clinic. Both of these investments are a clever move to achieve those goals; however, too often these exercises are in vain as they are introduced into the clinic without a strategy. If the conversations with the patient are not centred around their scan it will never bring you the return on investment. If after attending a course you do not put your new skills into practice, your confidence dwindles by the day and that treatment risks never taking off (Figure 1). Both of these scenarios are unfortunately common. To make the most of these investments there needs to be a strategy that will ensure that you not only see the return but they also generate you a much higher income.
4. Connection that converts
Staying connected with patients after their initial consultation is key to longterm conversions. Patients who attend regular reviews are 40% more likely
to complete their full treatment plans. 6 Connecting with dental patients during treatment is essential for fostering trust, reducing anxiety, and enhancing overall patient satisfaction. Discussing goals and priorities ensures that both the dentist and patient are aligned, leading to increased satisfaction and better treatment outcomes. Use simple, clear language and visual aids to help patients understand their treatment options. Encouraging questions and ensuring comprehension can alleviate fears and promote informed decision-making.
Conversion blocker: clinics that don’t track appointment reviews may lose contact with patients who say ‘I’ll think about it’, or fail to follow-up with patients between stages of care. Not seeking feedback during a patient’s treatment can break down rapport and trust, which is essential to maintain a longstanding relationship with the patient.
5. Completion that converts
The final touchpoint in a patient’s treatment journey is often overlooked, but it’s one of the most powerful. Clinics that actively ask for reviews and referrals see up to 25% more new patient leads.7 Patients who come to a clinic through referrals are more trusting, positive, and are more willing to convert into treatment as they have a good understanding of costs and expectations. Patients who have had positive experiences are more likely to refer friends and family to your practice. In fact, 45% of dental patients are referred by friends, neighbours, or relative. Online reviews play a crucial role in attracting new patients.8 Approximately 90.4% of patients trust online reviews, and 73.6% read them to assess the quality of dental services.9
Conversion blocker: teams that forget to collect feedback, skip before and after photos, or assume patients will naturally refer others. By focusing on this final touchpoint, dental practices can transform satisfied patients into active promoters, driving growth and enhancing their reputation.
Questions on page 189.
Quiz answers:
1. Plaque-induced gingivitis, with pregnancy-associated exacerbation. Gingivitis is a plaque-induced inflammation of the gingivae. Pregnancy does not cause this condition, but hormonal changes, i.e., increased levels of oestrogen and progesterone, can increase the inflammatory response to existing plaque.
2. There is a substantial body of evidence demonstrating that periodontitis is associated with adverse pregnancy outcomes such as preterm birth, low birth weight and pre-eclampsia. Several hypotheses have been proposed, including inflammatory mediators or oral bacteria from the gums entering the bloodstream and affecting placental or foetal tissue.
3. Management during pregnancy, based on European Federation of Periodontology (EFP) guidelines:
n provide professional mechanical plaque removal (scaling) and oral hygiene instruction;
6. Clinics that convert
At the centre of it all is your clinic’s internal culture, systems, and leadership. Clinics with defined standard operating procedures, clear pricing, and strong teams grow 30% faster and retain more patients.10
There are lots of ways to optimise each of the 6Cs to ensure that you have a successful clinic that converts online views into satisfied patients who will return time and time again.
When you align your clinic around these six conversion points, you create a business that supports your patients, your team, and your future. You stop guessing and start growing – with clarity, confidence, and consistency. If you’re ready to turn potential into profit, and loyal patients into your best promotors, start building a clinic that converts.
References
1. https://www.ruleranalytics.com/blog/reporting/cosmetic-marketingstatistics/?utm_source=chatgpt.com
2. https://www.ruleranalytics.com/resources/dental-and-cosmeticconversion-benchmark-report/
3. https://www.calldrip.com/blog/speed-to-lead-statistics?utm
4. https://www.dentistrytoday.com/modernize-the-dental-patientexperience-via-automation/
5. https://www.mdpi.com/2227-9032/12/12/1195?utm/
6. https://www.arini.ai/blog/improve-appointment-to-show-attendancerate-dental-clinics?utm
7. https://onspirehealthmarketing.com/online-reputation/reviewsmanagement/lessons-learned-from-collecting-24587-patientreviews/?utm_source=chatgpt.com
8. https://pubmed.ncbi.nlm.nih.gov/10865345/
9. https://connectthedoc.com/blog/how-online-reviews-impact-dentalpractices-the-stats?ut
10. https://usewhale.io/blog/the-importance-of-sops/?utm
n emphasise home care with soft toothbrushes, interdental cleaning, and short-term chlorhexidine if needed
n schedule regular reviews throughout pregnancy;
n if patient develops signs of periodontitis (e.g., pocketing or attachment loss), begin non-surgical periodontal therapy; and, n offer advice on smoking cessation and diet if appropriate.
4. Routine dental care is safe and supported during all stages of pregnancy. Elective treatment is often scheduled in the second trimester, when nausea is reduced and positioning is more comfortable.
The EFP recommends that pregnant women diagnosed with gingivitis or periodontitis should be informed that “the risks of no treatment are significantly higher than the minimal trauma that might occur during therapy”:
n radiographs are safe when needed;
n local anaesthetics such as lidocaine with adrenaline are safe and well tolerated; and,
n in the later stages, position the patient semi-reclined to minimise the risk of dizziness or hypotension.
Associates
South Dublin. Join our growing practice! We’re seeking a passionate dental associate to provide exceptional care in a supportive environment. Competitive salary, flexible hours, and opportunities for growth. Apply today and make an impact! Contact dentalassoc993@gmail.com
Associate dentist and orthodontist positions are available in Dublin 9. Private/PRSI. Friendly working environment. Must be IDC registered. Reply with CV to dublinsmilecenter@gmail.com
Dental associate position available in large multidisciplinary practice in Dublin. Fully private, busy book. Flexible days available. Specialists working on site. Digital scanner, CBCT scanner. Mentoring available. Excellent remuneration. CPD organised. Free parking. DART a two-minute walk. Contact dentalassociatepositiondublin@gmail.com
Full-time associate for maternity cover, six months from October 2025. Also, permanent three-day per week associate position. 40 minutes north of Dublin Airport. Fully computerised. Digital X-rays, IO/CT scanners. www.blackrockdentist.com. CVs to dentistnortheast01@gmail.com
Part-time associate required for busy, modern dental practice in Athlone. Private/PRSI book. Great support staff, CBCT and intra-oral scanner. New grads welcome. Contact athlonedental@gmail.com
Classified advertisements are accepted via the IDA website –www.dentist.ie – only, and must be pre-paid. The deadline for receipt of advertisements for inclusion in the next edition is Friday, September 12, 2025. Classified ads placed in the Journal are also published on www.dentist.ie for 12 weeks.
Please note that all prices are inclusive of VAT.
Advert size Members Non-members up to 25 words ¤135.30 ¤270.60 26 to 40 words ¤161.70 ¤330.65
The maximum number of words for classified ads is 40. If the advert exceeds 40 words, then please contact: Think Media, The Malthouse, 537 North Circular Road, Dublin 1. Tel: 01-856 1166 Fax: 01-856 1169 Email: paul@thinkmedia.ie
Please note that all classified adverts MUST come under one of the following headings:
4 Situations wanted 4 Situations vacant
4 Practices for sale/to let 4 Practices wanted
4 Equipment for sale/to let
Classified adverts must not be of a commercial nature. Commercial adverts can be arranged by contacting Paul O’Grady at Think Media.
Greater Dublin. Experienced, part-time associate for a very busy, expanding practice. Supportive, progressive environment. Excellently equipped. Superb support staff. Endo/oral surgery experience helpful. Good long-term prospects for suitable candidate. Email tristanorthodontics@gmail.com
Dental associate position available in busy, long-established Cork City practice, four to five days, strong patient book, private/PRSI. Experienced clinical support team in place. Contact irwinnora@gmail.com
Full/part-time associate position available in a family-run, private practice in Galway City. A modern, fully digital practice with 3Shape/OPG/CBCT scanners. Excellent support team. Must reside in Ireland with IDC registration. Contact dentistgalway2022@gmail.com
Part-time dental associate required for a busy dental practice in Dublin 15. Scope to become full-time. In-house technician present. Flexible working hours. Fully computerised. Excellent support staff. Friendly atmosphere. Apply by email to shbak17@yahoo.co.kr
Associate dentist required for busy practice in west Cork. Full- or part-time. Fully computerised. Digital X-rays. Modern, fully equipped surgery. Full support given. Tel: 086-172 7064, or email harrycogswell7@gmail.com
Exciting opportunity for a part-time dental associate in an established practice. Suitable for an experienced or new graduate. Private/PRSI only. Enjoy a busy diary and a competitive salary with full support staff. Fully computerised practice. Contact info@goreydentalpractice.ie
Associate dentist position, part-time, flexible, in long-established practice in north Wicklow. Computerised, hygienist, supportive staff. New graduates welcome. Contact lumina1863@gmail.com
Associate dentist required to join our team at D15 Dental Care, Dublin 15. Flexible hours – full/part-time. All modern facilities including CBCT/intraoral scanner. Enjoy a busy diary, a competitive salary with full support staff. Fully computerised practice. Contact admin@d15dentist.ie
Smiles Wexford (Bupa) – part-time associate dentist opportunity in a wellestablished practice. Contact leah.hall@bupadentalcare.co.uk
Associate dentist required with interest to take over a busy private practice. Reason: principal retirement. CV and cover letter to crana.dental18@outlook.com
Part-time associate wanted to join a long-established, newly furbished practice in Dublin 18. Digital X-rays and intraoral scanner, friendly patients and staff, private and PRSI. Must be IDC registered. Email CV to d18dental@gmail.com
Part-time associate wanted to join a long-established newly furbished practice in Ballincollig, private and PRSI. Busy practice. Independently owned. Email CV to dentistcork24@gmail.com
Full-time associate position southwest Dublin. Busy mixed practice. High remuneration, easy-going with good staff and equipment, start August. Contact seanbearnais@gmail.com
Ennis Dental Health Centre, Co. Clare, seeks a part-time experienced dental associate, for two days per week. Busy, modern practice with excellent support staff, and high earning potential. 50% pay. Must have IDC registration and be living in Ireland. Contact gbrowne.ennis@gmail.com
We are a well-established and rapidly growing clinic in Galway City. We are looking to welcome a skilled and compassionate associate dentist to our team. A modern clinic with digital technology, with a strong and growing patient base. Contact ethna@galwaydentalgroup.ie
A well-established clinic in the centre of Dublin (Raheny) seeks a part/fulltime dentist. IDC registration, indemnity, permit to work required. Recent graduates will receive mentorship support. Please contact for further details. Contact soumandent@gmail.com
Dental Care Ireland Galway – full book on offer, high earnings, replacing departing colleague. We offer excellent, experienced clinical support. August 2025 start. Must reside in Ireland with IDC registration. Within modern, established practice. Contact careers@dentalcareireland.ie
Eden Medical Clinic seeks part-time dentists/doctors with 1+ year facial aesthetics experience preferably, and AWI training, for our clinics in Leinster. Contact hr@eden-medical.ie
Exciting full-time dentist position available in Galway City. Become part of our welcoming, multidisciplinary practice where patient care, mentorship, and modern technology come together. Enjoy a busy diary, competitive salary, and continuous learning in a collaborative, forward-thinking team. Contact galwaydentists2025@gmail.com
Passionate, patient-focused general dentist wanted to join our modern dental team in Blanchardstown Village, Dublin 15. Full/part-time available. https://www.beechview.ie
Dental Care Ireland north Dublin – part/full-time opportunity in our established, modern practice, strong patient book on offer, private/ PRSI, experienced clinical support team in place. Must have IDC registration, reside in Ireland, and have indemnity insurance. Contact: careers@dentalcareireland.ie
Dentist to replace experienced colleague in modern Cork practice. Full support, good aesthetic potential, hygienist. Two days going to full-time. CV to caringdentist97@gmail.com
Private dentist required to bring down patient waiting lists. One hour from Dublin/Newry. Fully private practice – any hours/days available as new modern third surgery just built. Fully digital. 50% remuneration. Great staff atmosphere! Flexible working. Contact kingscourtdentalpractice@gmail.com
Busy Sligo private clinic. Brand new suite. Belmont chair, I/O camera, Enbio silent autoclave, NSK U/S and EMS scalers. Computerised appointments. Full employee status. No weekends/evenings. Excellent remuneration. New grads welcome. We will help with accommodation. Contact newsmiledentalclinic@gmail.com
Dentist required to join our team at Westside Dental Athlone. Flexible hours. Modern, friendly practice. New chair and equipment. Excellent support staff. Contact info@westsidedental.ie

A motivated, ambitious dentist with a passion for delivering high-quality dentistry required three to four days/week in Mallow, Co. Cork. Non-corporate position. Newly renovated practice with all modern facilities including CBCT. Amazing team and full clinical support. Contact suzannecurran@aol.com
Join our high-tech, growing practice! Intra-oral scanner and CBCT. We’re seeking an ambitious and motivated general dentist eager to enhance their clinical skills and advance their career. Enjoy a busy diary. Contact admin@hansfieldmedicalcentre.ie McMahon Dental Blackrock. Experienced part-time dentist required for busy family practice. Team includes endodontist, implantologist and hygienists. Fully digital, 15 years CEREC users, iTero, OPG, four-surgery clinic. Commencing September. Contact dentist@mcmahondental.ie
Dental Care Ireland – south Dublin. We have opportunities within some of our modern established practices. Offering strong patient books and high earning potential. Must be IDC registered and living in Ireland. Experienced and friendly clinical teams in place. Contact careers@dentalcareireland.com
Smiles Dun Laoghaire (Bupa) – part-time general dentist role in a supportive, experienced team. Contact leah.hall@bupadentalcare.co.uk
Raheny Dental Centre seeks part-time dentist for two days per week in our modern, well-equipped two surgeries, intra-oral scanner. Patient-focused, experienced
Will you still be smiling at the end of the year?
Make sure your practice is profitable in 2025
As Ireland’s only specialist dental accountants we’re here to help you control your practice costs


supportive team treating private, PRSI and medical card patients. IDC registration essential. Contact rahenydentalcentre@gmail.com
Dental Care Ireland Athenry – we have part-time flexible days/hours in our established Athenry practice. Strong patient books on offer, competitive hourly rate. IDC registration essential and must live in Ireland. Friendly and experienced clinical team already in place. Contact careers@dentalcareireland.ie
Dental Care Ireland Waterford – part/full-time days on offer in our established practice, high earnings due to busy patient books. Must have IDC registration and be living in Ireland. Experienced clinical team already in place. Contact careers@dentalcareireland.ie
Enthusiastic, experienced dentist required for a busy north Dublin practice on a locum or part-time basis. Independently owned. Excellent support staff including two hygienists. OPG, intra-oral scanner, full SprintRay 3D printing set-up, etc. Minimum two years’ experience. Contact reception@castlemilldental.ie
Experienced, permanent general dentist wanted for a busy, established practice in Rush, Co. Dublin. 50% pay offered, flexible hours, start as soon as possible. Contact info@rushdentalsurgery.ie
Fantastic opportunity in well-established clinic just 25 minutes from Galway City. Large patient base, excellent support staff, and principal dentist in place. Great opportunity in a busy, long-standing practice. Please email CV to jobs@cubedental.ie
General dentist to join a busy practice. Large patient base, modern digital surgeries. Location Navan, 30 minutes from M50. 50% pay offered, flexible hours, start asap. Must have IDC registration and be living in Ireland. CV to dentalreceptionnavan@gmail.com
Swords Dental seeks an experienced dentist on Saturdays (9.00am-3.00pm). Busy, modern practice with excellent support staff and high earning potential. Contact colinpatricklynam@hotmail.com
Specialist/limited practice

MedAccount offers a full range of specialist dental accounting support and advisory services for Associates, Principals, Expense Sharing Partners and Hygienists.

S20, The Pottery, Pottery Road, Dun Laoghaire, Co. Dublin. Tel: 01 280 6414
Email: info@medaccount.ie


Orthodontist required for a busy practice in Dublin 15. Apply with a CV to shbak17@yahoo.co.kr
Associate dentist and orthodontist positions are available in Dublin 9. Private/PRSI. Friendly working environment. Must be IDC registered. Reply with CV to dublinsmilecenter@gmail.com
Part-time endodontist needed to join our multi-special interest practice in Longford (perio, prostho and oral surgeon). Treatments under sedation and hygienist available. Professional, skilled and flexible team. Modern facilities. For details, contact admin@keystoneperio.net
Specialist orthodontist required for existing specialist practice off M50. Initially one day per week building within 12 months to three days. Motivated support staff.
Orthodontic practice situated within well-equipped, modern general practice. Positive, inclusive work environment. Contact embracespecialists@gmail.com
Dental Care Ireland south Dublin – we have an opportunity for an oral surgeon. Parttime, flexible days/hours. Specialist registration is essential. Due to company growth, come join us to work as part of a multidisciplinary team. Contact careers@dentalcareireland.ie
Dental Care Ireland orthodontist opportunities Meath and Dublin areas. Part-time flexible options, high earnings on offer with strong patient book within our established, modern practices. Opportunity is due to company growth. Please specify your preferred location, IDC registration essential. Contact careers@dentalcareireland.ie
Endodontist or dentist with special interest in endodontics required for our Naas practice. CBCT, microscope. Replies with CV to james@theclinicnaas.ie
Hygienists
Dental Care Ireland Meath, Dublin, west of Ireland – hygiene opportunities due to exciting company growth. Established modern practices, strong patient books on offer, part-time, flexible hours/days. Are you considering a new opportunity? Come join our team. Contact careers@dentalcareireland.ie
Mullingar! Registered hygienist required. We are expanding our team and moving into a state-of-the-art new dental clinic on the main street of Mullingar. This is a part/full-time role, flexibility and a very competitive salary! Contact info@lakelandsdental.ie
Step into a modern, multidisciplinary practice in Galway City as a dental hygienist. Provide meaningful care and education in a warm, progressive team. Enjoy tailored mentorship, real career development, and remuneration that quietly exceeds expectations. Contact galwaydentists2025@gmail.com
Dental hygienist – join our award-winning team committed to exceptional patient care. Full book available one day a week in Dublin. Flexible on day. Excellent remuneration. Nursing support available. State-of-the-art equipment. CPD provided. Periodontists working on site. Contact dentalassociatepositiondublin@gmail.com Waterford. Hygienist required part-time to replace departing colleague. Fully digital. Private/PRSI. Sea view from your surgery! Friendly team and motivated patients. Contact tramoredental@hotmail.com
Part-time dental hygienist position available in large, multidisciplinary, fully private dental practice. Flexible day(s) available. Nursing support provided. CPD provided. Free parking. Five-minute walk from the DART, 15-minute drive from Dublin city centre. Contact dublinhygienistposition@gmail.com
Hygienist position available part-time, Gorey, Co. Wexford. Employee status. No late nights or weekends. Choice of equipment. Digitalised and computerised. Nurse if requested. Large bright surgery. Dedicated free parking. Travel costs covered. Contact info@thebridgedentalsurgery.ie
Hygienist required (Tuesday/Friday) to join team in Mallow, Co. Cork. Modern practice with great facilities. High practising standards and team support. Contact suzannecurran@aol.com
Lucey Dental Greystones requires a hygienist to join our multidisciplinary team in our state-of-the-art practice. The hygienist will provide guided biofilm therapy to our patients. Mentoring provided and new grads welcome. Free parking on site. Contact manager@luceydental.ie
Castleknock Dublin 15: dental hygienist required for Tuesdays to work alongside periodontist. 7.00am to 3.00pm; however, hours are negotiable. ¤60 per hour. Modern practice. Contact roryperio@gmail.com
Shields Dental Clinic in Blackrock, Dublin, requires dental hygienist for maternity cover commencing in September 2025. Part-time position with flexible days. Contact jobs@shieldsdentalclinic.ie
Slievemore Dental in Stillorgan, Dublin, looking for a dental hygienist to take over from an experienced colleague. Great remuneration and room for growth. If interested, please submit CV to info@slievemoredental.ie
Hygienist wanted to replace departing colleague in a family-friendly practice. Three days (more in a neighbouring town if wanted). No weekends or late evenings. Full book in relaxed atmosphere. Good remuneration and support. Contact timlynchbds@hotmail.com
Locum dental hygienist wanted for a busy multi-surgery family practice in Oranmore, Galway, required immediately. Flexibility in days and hours. Email info@orantowndental.ie
Dental nurses/receptionists/practice managers/ treatment co-ordinators
Beaumont Dental in Dublin 9 seeks a full/part-time dental assistant to join a very wellmotivated team. Work ethic, attention to detail and great service mentality highly valued. Growth and learning opportunity. Happy work culture highly valued. Contact Bryan@beaumontdental.ie
Join our modern, efficient, and team-oriented dental practices in Navan, Dunshaughlin and Maynooth. We’re offering full- and part-time nursing positions. Enjoy a high-tech, supportive, friendly team with excellent career development opportunities. Contact Carol@boynedental.ie
We are seeking a qualified dental nurse to join our friendly team in Swords Orthodontics. This position is available immediately and a dental nursing qualification is required. We are looking for a reliable, enthusiastic, and friendly team member. Contact brenda@swordsortho.com
Qualified dental nurse required to join our friendly multidisciplinary team in north Dublin. We are looking for a dental nurse with excellent organisation skills and who is also a good team player. Potential for promotion. Beside DART. Free parking. Contact northdublindentalassociate@gmail.com
Join our state-of-the-art hi-tech dental practices in north Dublin. We have full- and part-time nursing positions available. CPD provided. Free parking. Beside DART. Enjoy a supportive and friendly team working environment. Contact dentalassociatepositiondublin@gmail.com
Dental practice for sale, midwest area, Clare, private PRSI. Dentist retiring, full book, good income, lots of room for expansion. Email rooneyniamh16@gmail.com
Southeast – Dublin 90 minutes. Very busy two-surgery practice with ample room to expand. Prime location. Excellent ground floor/dedicated parking. Strong new patient numbers. Computerised, digitalised, strong hygienist service. Potential for quick growth. Flexible transition – negotiable. Contact niall@innovativedental.com
Successor wanted for busy leasehold practice in attractive rural town, Co. Waterford. Long established. No capital required. Mainly private. Very profitable, low overheads. Scope for expansion. Principal retiring. Email dentalpracticesale21@gmail.com
Fully equipped surgery room to let. Blackrock, Co. Dublin. Dentist with a special interest only (no orthodontics/general). Use of common areas and OPG. Contact alex@whitesmiledental.ie
Modern two-surgery practice in prime Dublin 2 location. Stylish, fully digital, expansion ready. Flexible transition. Photos and details available by email. Contact modernsurgeryindublin2@gmail.com
Two-surgery, busy, long-established mixed practice for sale southwest Dublin. Free parking, high turnover. Available leasehold or freehold, principal can facilitate transition. Contact: fiachloir86@gmail.com
Digital Sensor Carestream RVG6200 Size 2 sensor. One year old, like new. Two available, ¤3,500 each. Retail price new ¤6,000. Contact conatyni@tcd.ie
Dr Madina Danishani was born in Baku, Azerbaijan, completed her undergraduate dental training both there and in Dublin, and now works in Oakland Dental in Leixlip, Co. Kildare.

Why did you choose dentistry?
The biggest influence in my life was my dad. He was a scientist – a geologist with an endlessly curious mind – and our conversations often wandered into the world of medicine and science. He had a surprising fascination with teeth, which became a recurring theme in our chats. Those early talks, filled with curiosity and wonder, quietly planted the seed that would one day shape my own path.
What was dental education like in Azerbaijan?
I began studying dentistry in Azerbaijan in 1992. The Soviet Union had just collapsed – one day we were part of one country, and the next, everything had changed. Despite the uncertainty, there was a real sense of excitement about the future and the rebirth of Azerbaijan. But the reality was tough. There was political instability, economic collapse, and high unemployment. And in the middle of all that, we were just students trying to study. It was hard to stay focused, but our teachers did their best to keep us on track. By the time we graduated, though, there was a gap – we were well-educated, but we didn’t have the hands-on skills. We had barely any clinical exposure. I could write a perfect essay on how to pull a tooth, but I couldn’t actually do it.
What encouraged you to move to Ireland?
I came here in 2001. It was a combination of personal and political circumstance. We chose Ireland because it was a welcoming place. It was a stable, growing economy. It was the right choice. It is a really beautiful place.
What was your dental education experience in Ireland?
When I arrived in Ireland, I spent the first few years focusing on improving my English. By 2006, I felt ready and applied to Trinity. I was shortlisted and invited for an interview – but ultimately, I was rejected. I applied again in 2007, and once more, I didn’t get in. As you can imagine, it was incredibly frustrating. But I’m not someone who gives up easily. In 2008, I applied for the third time. The interview lasted only five minutes because I walked in and told them: “You’re wasting my time and your own time, because I’ll be back next year, and the year after, and the year after that. I’m getting into this programme”. Half an hour later, they called to offer me the place.
The five years at Trinity were tough, but I’ve never regretted a moment of it – it shaped me into who I am today. From second year onwards, we were seeing patients, and by the time we graduated, we were well prepared for the real world.
Can you name a lecturer/mentor you admire and why?
Prof. Stephen Flint. He was the embodiment of what you imagine when you think of a true academic – a real gentleman. The way he spoke, the depth of his knowledge, the clarity with which he explained even the most complex concepts – it was remarkable. He had a calm authority about him, and he made things easy to understand without ever simplifying them. More than that, he was incredibly supportive. He made me feel seen, especially during moments when I was doubting myself.
Another person I deeply admired was Mr Kumara Ekanayake. The man is a legend. His surgical skill was extraordinary. The precision and artistry with which he operated was unlike anything I’ve ever seen.
I came here in 2001. It was a combination of personal and political circumstance. We chose Ireland because it was a welcoming place. It was a stable, growing economy. It was the right choice. It is a really beautiful place.
What do you think are the big issues for dentistry in Ireland right now? One of the biggest issues is the medical card scheme. I’m one of the very few dentists still participating in it. In my view, the core problem isn’t funding, it’s the management. It’s clear that it’s not being managed effectively. That’s why so many dentists are walking away from it.
Tell us about an interest you have outside dentistry. I love reading. I also have an interest in floristry. If I have an occasion, instead of just buying a bouquet of flowers, I will buy flowers and some greenery and make an arrangement myself.