Get Ready For Our UPCOMING EVENTS

Registration Opens
September 1!
Register online or with enclosed form Visit sdds.org to view course offerings
September 9, 2025
General Membership CE Meeting
Tuesday • 5:45–9pm
Hilton Sacramento Arden West
Member Price: $89 early (ends 8/26)
$99 regular (begins 8/27) / $99 late (begins 9/7)
Non-Member Price: $218
Throwdown – Does CR Matter? (3 CEU, Core)
Presented by Paul Binon, DDS, MSD; Bryan Judd, DDS and Peter Worth, DDS
September 12, 2025
SDDS 14th Annual Shred Day
Friday • 10am–2pm • SDDS Office
Sponsored by CDA / TDIC Insurance Solutions
September 17, 2025
Business Forum
Wednesday • 6:30–8:30pm • SDDS Classroom
Member Price: Complimentary to SDDS Members
Staff of Member Price: $49 | Non-Member Price: $99
Navigating Year-End Planning and New Tax Regulations
Never Too Early, But Is It Too Late? (No CEU)
Presented by Brett LeMmon, CPA, MA; Earned (SDDS Vendor Member)
September 26, 2025
Continuing Education
Friday • 8:30am–3:30pm • SDDS Classroom
Member Price: $179 early (ends 9/5) / $199 regular (begins 9/6)
Non-Member Price: $398
Pearls in Our Backyard (6 CEU, Core)
Presented by Tim Mickiewicz, DDS; Nisha Manila, BDS, MS, PhD, FACD; Brandon Martin, DDS, MS; and Devan Dalla, DDS
October 2, 2025
Dentists Do Broadway - & Juliet
Thursday • 7:30pm show
October 8, 2025
Next Level Leadership Reception
Wednesday • 6:00pm • SDDS Office
October 14, 2025
General Membership CE Meeting
Tuesday • 5:45–9pm
Hilton Sacramento Arden West
Member Price: $89 early (ends 9/30)
$99 regular (begins 10/1) / $99 late (begins 10/12)
Non-Member Price: $218
The California Oral Health Plan: Partnering for Success (3 CEU, Core)
Presented by Shakalpi Pendurkar, DDS, MPH, State Dental Director
October 16, 2025
SDDS Member Mixer - Zócalo Folsom
Thursday • 6 –7:30pm
Sponsored by MUN CPAs and Dental & Medical Counsel PC
October 22, 2025
Continuing Education
Wednesday • 6 – 8:30pm • SDDS Classroom
Member Price: $99 early (ends 10/1) / $119 regular (begins 10/2)
Non-Member Price: $238
DIY Study Club – Bring Your Case! (2.5 CEU, 20%)
October 29, 2025
Licensure Renewal Webinar*
Wednesday • 5:30–7:30pm • Webinar
Member Price: $95 early (ends 10/8) / $115 regular (begins 10/9)
Non-Member Price: $230
Responsibilities and Requirements of Prescribing Schedule II Opioids (2 CEU, Core)
Presented by Ronni Brown, DDS, MPH, FADI
* Does not qualify for AGD credit

View all CE Courses & Events online with this QR code.

Carl
Ranna Alrabadi, DMD
Bryan Judd, DDS
Peter Yanni, DMD, MS • Idean Rezaei, Student Rep
James
William
Cyril
Peter Yanni, DMD,
Mohd Khalaf, DDS
Jeffrey

We’re excited to invite you to SDDS’ largest event of the year, taking place March 26-27, 2026, at the SAFE Credit Union Convention Center in Sacramento (1400 J Street). This two-day, in-person event offers exceptional continuing education (CE), an expo hall with all your favorite exhibitor partners and lots of opportunity to connect with colleagues.
42 Class Offerings
Larger Expo Hall
100 Exhibitors
28 Speakers Groovy Giveaways
Happy Hour Meals Included Team Building So Much More!
Attend both days and you could
Earn up to 13 CEU!
Great experience! I come from the Alameda County Dental Society and was impressed with how well everything was organized. The speakers were excellent, especially the food and camaraderie of everyone. I will attend next year!
– Dale Jeong, DMD (2025 attendee)


$425 Dentists | $345 Staff For full registrationone day pricing also available (ends 11/14/25)

ELEVATING OUR PROFESSION THROUGH
VALUABLE CE OFFERINGS
We are blessed to be part of a profession that is both dynamic and ever-evolving. Every day, new technologies, materials, and techniques are developed and brought to market, allowing us to be the best clinicians we can be. Dentistry continues to advance at an exponential rate, and staying ahead of these innovations requires us to be proactive in our continuing education and professional growth.
The past decade has seen an explosion of continuing education (C.E.) opportunities, ranging from traditional in-person courses to virtual offerings. Institutions such as Spear, Kois, Pankey, and Dawson continue to expand their programs, building legions of dentists who embrace their philosophies for treatment planning complex cases. At the same time, dental suppliers and manufacturers are hosting their own meetings and C.E. continuums, which raises questions about impartiality. Increasingly, the line between education and marketing has become “fuzzy,” requiring clinicians to approach the information they receive with a critical eye.
So where does the C.E. offered by SDDS and CDA fit into this landscape? With so many options available, I am often asked this question. How can we compete against these large companies and educational groups, whose
budgets dwarf ours? How do we continue to attract top talent and remain relevant?
Having served on the CDA Board of Managers for the past few years, and having been involved with programming at SDDS as well, I have seen firsthand the challenges organized dentistry faces in the continuing education space—and they are significant.
Yet one thing will always set us apart: our mission.
The volunteer leaders and staff who dedicate countless hours to creating programs for CDA and SDDS are not driven by profit or marketing dollars. They are motivated by a genuine desire to elevate our profession. These leaders are your colleagues, classmates, and friends—passionate about the future of dentistry. They carefully vet speakers to ensure presentations are engaging, scientifically accurate, and relevant. Biased content is avoided, and sponsored content is presented transparently.
While we may not have the financial power of large companies or institutions, we hold something even more valuable: the deep respect of the dental community. Speaking at SDDS or CDA is considered an honor—a recognition that often transcends monetary reward.

By Nima Aflatooni, DDS 2025 SDDS President
It is important that we, as members, continue to support the C.E. offered through SDDS and CDA. These are OUR organizations and OUR programs. I encourage you to contribute your ideas, suggest topics, and most importantly, get involved in leadership.
Our SDDS General Meetings continue to feature outstanding local speakers. The SDDS MidWinter Convention has grown into Northern California’s premier dental meeting. And CDA Presents—a member benefit— remains one of the nation’s leading dental meetings, attracting world-class speakers from across the country and around the globe.
Finally, the camaraderie found at SDDS and CDA programs is unmatched. The chance to reconnect with friends and colleagues, and to learn from one another as much as from the presentations themselves, is truly invaluable.
I look forward to seeing you all at our next SDDS General Meeting in the fall, the SDDS MidWinter Convention & Expo in March, and CDA Presents in May.

Mark Your Calendars - September 12, 10am-2pm SDDS 14th Annual Shred Day |
Sponsored by CDA and TDIC Insurance Solutions
An opportunity for SDDS members get rid of that pesky shredding for a fraction of the cost
Visit sdds.org to register or complete the registration form included in this issue.
Cost: Up to 5 bankers boxes free to SDDS Members. $10 per additional box. Payable to the SDDF.
Fall at SDDS: Events, Energy, & Engagement

By Caroll Badgley SDDS Executive Director
As summer winds down and we head into fall, I wanted to take a moment to connect with you not as just a member dentist, but as part of our closeknit SDDS community. This is the time of year when planning turns into action, and I’m so proud of what we’ve accomplished together and what’s still ahead.
One of the biggest things we’re preparing for is our 2026 MidWinter Convention, coming up March 26–27 at the SAFE Credit Union Convention Center. Registration is now open, and I hope you’ll consider attending. This event always feels like a reunion of colleagues, classmates, and friends, and we’ve worked hard to build a program that’s both relevant and refreshing. You’ll find all the details in the insert included in this issue of The Nugget
This year, we’d love your help in expanding our reach and encouraging even more participation. Watch for fun MidWinter posts on social media, and when you and your dental team register, tag us! Let’s build some energy around this event and show what makes SDDS so special. Together, we can make the 2026 convention our biggest and best yet.
Another opportunity to connect and clear out your office clutter is our 14th Annual Shred Day on Friday, September 12, from 10:00am to 2:00pm in the SDDS parking lot. It’s a simple, member benefit we look forward to each year. You can bring your documents for secure shredding and also drop off e-waste (check sdds.org for a full list of what’s accepted). We’ll have snacks and drinks on hand, so come by, say hello, and take a little break with us.
I also want to take a moment to recognize some of the great work happening right here at the SDDS office.
• Jessica Luther, our Graphic Designer, recently celebrated 10 years with SDDS. If you’ve ever admired a flyer, a Nugget cover, or any of our materials, Jessica had a hand in it.
• Sofia Gutierrez, who oversees Foundation projects and CPR, will be receiving the 2025 Oral Health Hero Award from the Center for Oral Health. Her dedication to access and outreach is inspiring, and we’re lucky to have her on our team.
The SDDS staff is small but mighty and incredibly committed to serving you. I’m grateful for the work they do every day, and even more grateful to do it alongside such a dedicated membership.
Thank you for being part of SDDS. Whether you’re actively involved, quietly supportive, or somewhere in between, you are an essential part of what makes this Society thrive. As always, I welcome your thoughts, questions, or just a friendly hello.
LEADERSHIP
President: Nima Aflatooni, DDS
President Elect/Treasurer: Jeffrey Sue, DDS
Secretary: Craig Alpha, DDS
SDDS BCR Rep: Volki Felahy, DDS
Editor-in-Chief: Carl Hillendahl, DDS
Executive Director: Caroll Badgley
Andrea Cervantes, DDS
Lisa Dobak, DDS
Diana Fat, DDS
Eric Grove, DDS
Michael Payne, DDS, MSD
Kart Raghuraman, DDS
Cherag Sarkari, DDS
Chirag Vaid, DDS
Guest of the Board: Rosemary Wu, DMD, MS
CNU Student Representative: Brandon Azali
UOP Student Representative: Resha Shah
CPR: Margaret Delmore, MD, DDS/ Brad Archibald, DDS
Membership/Engagement:
Jeffrey Delgadillo, DDS/Aneel Nath, DDS
Nominating/Leadership Development: Ash Vasanthan, DDS, MS
CSUS Pre-Dental:
Brian Orcutt, DDS/Jeremy A. Salvatierra, DMD
Budget & Finance Advisory: Jeffrey Sue, DDS
Bylaws Advisory: Ash Vasanthan, DDS, MS
CE Advisory: Ryan Wilgus, DDS
Strategic Planning Advisory: Jeffrey Sue, DDS/Craig Alpha, DDS
Foundation President: Carl Hillendahl, DDS
Caroll Badgley | Executive Director
Della Yee | Director of Operations
Sofia Gutierrez | Foundation Projects/CPR
Anne Rogerson | Office Manager
Jessica Luther | Graphic Designer
Jen Jackson | Member Liaison
is published bimonthly by the SDDS, 2035 Hurley Way, Ste 200, Sacramento, CA 95825 (916) 446-1211. Acceptance of advertising in The Nugget in no way constitutes approval or endorsement by Sacramento District Dental Society of products or services advertised. SDDS reserves the right to reject any advertisement.
Postmaster: Send address changes to SDDS, 2035 Hurley Way, Ste 200, Sacramento, CA 95825.
Oral Medicine:
The Intersection of Dentistry and General Health and a Pillar of Comprehensive Care
The ADA defines a dentist as someone who evaluates, diagnoses, and treats diseases, disorders, or conditions of the oral cavity, maxillofacial area, and the adjacent or associated structures and their impact on the human body. It is clear from this definition that our scope and ability to impact our patients go well beyond their teeth and gums. The ties between oral health and systemic health are well-documented, so it is important for us to keep this in mind, as it represents a key pillar in comprehensive dental care.
The field of oral medicine has rapidly evolved, and this reached a tipping point in 2020 when the National Commission on Recognition of Dental Specialties and Certifying Boards of the American Dental Association (ADA) reviewed and approved the American Academy of Oral Medicine’s application for specialty recognition and adopted a resolution recognizing oral medicine as a dental specialty.
The Growing Importance of Oral Medicine
The mouth is often the first place to show signs of broader health conditions. From oral manifestations of systemic diseases like diabetes and HIV/AIDS, to autoimmune conditions that present as oral lesions, or even more serious conditions such as leukemia and oral cancer itself, it’s crucial we adopt a more holistic, integrated approach in our care.
Diabetics often experience more severe gum disease, while untreated periodontal disease can exacerbate blood glucose levels, leading to a vicious cycle. Cases like this present us with a unique challenge of not only treating oral health issues but also collaborating with physicians to help manage the patient’s overall well-being. Oral medicine is in a unique position to bridge this gap.
Oral medicine also plays a critical role in identifying potentially life-threatening conditions like oral and systemic cancers, or autoimmune diseases such as mucous membrane pemphigoid, which can have wideranging systemic involvement. Early detection can make a world of difference in treatment outcomes, yet it requires a heightened awareness of subtle signs and symptoms, a key aspect of oral medicine.
Expanding the Role of the Dentist in Oral Medicine
So, what does this mean for us as practitioners? For starters, integrating oral medicine into our daily practice requires a deeper knowledge of how oral health ties into overall health. We need to become more adept at recognizing conditions that extend beyond what we typically address in a standard dental visit.
Beyond routine dental care, this means being vigilant about non-dental issues that present in the oral cavity. For example, oral manifestations of systemic diseases like lupus, Crohn’s disease, or even certain cancers can sometimes be missed if we aren’t specifically looking for them.
As we expand our role to include oral medicine in our practices, this does not necessarily mean we need to be an expert on oral disease, but it does mean that we need to recognize variations that extend beyond the acceptable parameters of normal. This will enable us to guide patients to seek proper care and treatment.
Interdisciplinary
Collaboration: A Necessity, Not a Luxury Oral medicine is inherently interdisciplinary. Our role often overlaps with other dental specialists and medical disciplines. Whether we’re working with other dental

By Peter Yanni, DMD, MS Associate Editor
specialists, oncologists, endocrinologists, or rheumatologists, our ability to communicate effectively with these specialists is vital. This collaboration ensures that patients receive comprehensive care and that oral health issues don’t go unnoticed or untreated— potentially exacerbating other health problems.
Embracing the Full Scope of Oral Medicine
As we move forward in our practices, it’s essential that we view the mouth as a window to overall health and adopt a comprehensive, multidisciplinary approach, to improve our patients’ oral health but also contribute to their overall well-being.
For us as clinicians, staying informed about the latest developments in oral medicine— whether through continued education, collaboration with other healthcare providers, or patient management strategies—ensures that we remain at the forefront of modern dental practice. We are guardians of the oral cavity, and my hope is that the articles in the issue help us accomplish just that.
In this issue, Dr. Nisha Manila, an oral and maxillofacial radiologist, takes us through an overview of incidental findings of CBCT imaging. Dr. Cyril Pandarakalam, an oral medicine specialist, provides an overview of a thorough oral cancer screening. I contributed an article providing information regarding desquamative gingival diseases. Dr. Mohd Khalaf, a local oral medicine specialist, outlines burning mouth syndrome, an issue he receives a lot of inquiries about. Finally, Dr. Jeffrey Delgadillo, an oral and maxillofacial surgeon, outlines the most up-to-date guidelines for identifying and managing MRONJ.


R EPAI R SUP P LI ES

s





LARGE & SMALL EQUIPMENT
Operating lights, patient chairs, doctor & assistant seating
Handpieces, air driver & electric delivery systems, customized to fit any practice needs
Lab (lathes, model trimmers, etc )
Intraoral X-rays, 3D X-rays, panoramic and cephalometric extraoral X-rays.
Vacuum systems, classic wet-ring pumps, dry blowers, (HVE) high volume extraction systems, & variable waterless systems are available in sizes for single offices or entire medical buildings
Compressors, sterilizers, and more!
R ENOVATION S, P RACTICE OP EN I NG & CLOS
W h et h er you ' re remodeli n g an existi n g practice or bui ldi n g a n ew office from t h e grou n d u p, we can h elp you achieve your vision t hroug h out t h e pro ject From tradition al to bold an d moder n looks
We wor k closely wit h architects, desig n er s, contractor s, an d you, to ensure your pro ject r u ns smoot h ly an d t h a t ever y detai l of your dream office is addressed. We can also assist wit h practice h an doffs an d closi n gs Let us assist i n taki n g i nventor y of your equi pment!
FINANCING OPTIONS
Get fi nanci ng for new and used equi pment or technology for your practice Up to $150,000 is avai lable wit h an application only, or up to $1 mi llion wit h i ncluded fi nancials Loan and lease options are avai lable Recei ve f undi ng as fast as one day! 30 day to 72 mont h ter ms
S ERV ICE & SUP P LI ES
Yaeger Dental Supply Inc. provides general and specialty dentists in all nine San Francisco Bay Area counties, now ser vicing the Sacramento region, with the best ser vice, equipment and supplies.
Our exper ienced and trained technicians have the knowledge to keep doctors’ practices r unning smoothly to deliver top-tie r patient care.

YOU SHOULD KNOW
UOP’S PDS HEALTH CARE COLLABORATIVE CLINIC IS OPEN!
The UOP clinic is open and they are accepting new patients! They do hygiene and treatment. They accept most private dental insurance and take straight Medi-Cal dental and GMC MediCal. The clinic is located on University of the Pacific’s Sacramento Campus in Oak Park.
MEMBER BENEFITHR HOTLINE AVAILABLE FOR SDDS MEMBERS
The SDDS HR Hotline is an exclusive benefit to SDDS Members. It's powered by the California Employers Association and they are ready for your call.
SDDS HR HOTLINE
FREE TO SDDS MEMBERS!
888.784.4031
2024 SALARY SURVEY
AVAILABLE - VISIT SDDS.ORG OR EMAIL SDDS@SDDS.ORG TO ORDER YOURS
PAST WEBINARS AVAILABLE AS RECORDINGS
Email sdds@sdds.org to find out which courses are available as recordings.
HAVE YOU CHANGED YOUR ADDRESS IN THE LAST 12 MONTHS? LET US KNOW SO WE CAN UPDATE OUR RECORDS! EMAIL US AT SDDS@SDDS.ORG
NEW LOCATION & DATE FOR THE HOLIDAY PARTY THURSDAY, DECEMBER 11, 2025 6:00PM-9:30PM SUTTER CLUB, DOWNTOWN SACRAMENTO
The evening will be celebrating Dr. Nima Aflatooni’s outstanding year as President and welcome Dr. Jeffrey Sue as our incoming President, along with the installation of the 2026 Board of Directors.
We’re looking for auction items, please consider donating an auction item to help us create the most fabulous Silent Auction ever! Your contributions make our silent auction unforgettable! Here are some items that went for high bids in the past:
• Private chef dinner in your home
• Local artwork or hand-crafted items
• Jewelry from your favorite jeweler
• Your favorite wines or make a wine basket
• Sports tickets (i.e. your King’s seats)
• Unique experiences
Anything you’d like to donate - we appreciate the contributions. See page 36 for more details.
SFK SCREENERS NEEDED
By enrolling in the Dedicated Monthly Dentist (DMD) Program, you can …
Prepay for all 7 and Save … on the General Membership Meetings for 2025–2026 with one check or credit card charge. Just $589 for all 7 meetings.
Easily Register for Each Meeting … by responding to a simple email sent to you each month.
Help with SDDS recruitment!
If you are unable to attend a particular meeting, call SDDS and we’ll arrange for a new member to attend in your place.
Sign up with the enclosed insert and attend these great General Meetings!
Smiles for Kids (SFK) is looking for volunteers to screen kids at area schools in the Fall. Please contact the SDDS office at (916) 4461227 or email smilesforkids@sdds.org if you are interested in volunteering.
2026 MIDWINTER CONVENTION & EXPO REGISTRATION IS OPEN
Register your team and save!

By Nisha Manila BDS, MS, PhD, FACD SDDS Member
Dr. Manila received her dental degree from Rajiv Gandhi University of Health Sciences India and Ph.D. in Oral Radiation Oncology from Institute of Science Tokyo, Japan (Former Tokyo Medical and Dental University). To further specialize, she completed Oral and Maxillofacial Radiology residency at Texas A&M School of Dentistry. Dr. Manila holds a certification in Artificial Intelligence from Harvard T.H. Chan School of Public Health and a Master’s degree in the field. A Fellow of the American College of Dentists, Dr. Manila brings a valuable combination of clinical experience and research focus. She also serves as Adjucnt Professor at Manipal College of Dental Sciences, Karnataka, India and Saveetha Institute of Medical and Technological Sciences, Chennai, India. She actively presents research and explores the use of Artificial Intelligence to improve both healthcare education and patient outcomes.
CONE BEAM COMPUTED TOMOGRAPHY: BASICS AND INCIDENTAL FINDINGS
Cone Beam Computed Tomography (CBCT) is commonly used in dentistry and Otolaryngology for 3D imaging of anatomical structures. Undoubtedly, one of the greatest additions to the dentist’s diagnostic and treatment planning toolbox has been CBCT imaging. Analyzing CBCT scans requires a systematic approach to ensure accurate diagnosis of pathologies1 While analyzing CBCT scans, it is important to use the same approach every time to avoid missing details2. Reorientation with preliminary assessment is the first step, where you verify correct patient positioning and assess the image quality. When evaluating radiographs, our eyes naturally focus on the area of interest, especially the teeth, which often draw the most attention. However, consciously and purposefully avoiding the area of interest assists us in systematically evaluating images that are reproducible on every single patient scan. After reviewing all other structures, proceed to examine the teeth systematically. Analyze axial, coronal, and sagittal slices for a comprehensive assessment. Compare with normal anatomy or previous scans if available. A comprehensive evaluation is the next step, where you inspect the craniofacial structures, check for cortical integrity, lesions, and bone density. This demands a thorough understanding of head and neck anatomy, and familiarity with craniofacial disease processes is equally important. The approach is made easier by reorienting the scan and employing a structured method of evaluation. In the next focused examination step, you will evaluate root morphology, periapical pathology, and endodontic conditions starting from the upper right and then across and around to the lower right. Localization and characterization
of abnormalities is the final step. Try to identify the exact location, size, and shape of the lesion in the maxillofacial region. Check the periphery of the lesion. Is it welldefined or poorly defined? Can you easily trace its borders with a pencil, or is it hard to outline? Look at the internal structure. Is it completely radiolucent, completely radiopaque, or of mixed density? Assess how the lesion affects surrounding structures. This helps us understand its behavior. The pattern of behavior may give clues to the type of disease. These observations are key to forming a diagnosis. Finally, place the lesion into the correct category of diseases and narrow it down to a possible differential diagnosis3. This last step needs further knowledge of pathology and some practice.
CBCT scans often reveal incidental findings, not related to the primary purpose of imaging. Studies have shown that a significant percentage of CBCT scans reveal such findings. A systematic review reported incidental findings in 24.6% to 93.4% of scans 4. Another study found incidental findings in 78.6% of CBCT examinations, with 38.6% requiring treatment and 25.2% necessitating follow-up 5. These findings underscore the necessity for clinicians to thoroughly examine the entire CBCT scan, not just the area of immediate interest. Effective CBCT interpretation necessitates a structured, systematic approach and a comprehensive knowledge of craniofacial anatomy. Clinicians must be vigilant in recognizing incidental findings to ensure accurate diagnoses and optimal patient care. When in doubt, consulting with or referring to an oral and maxillofacial radiologist is advisable to mitigate risks and enhance diagnostic accuracy.
Cone Beam Computed Tomography: Basics and Incidental Findings




General category Findings
Soft tissue
References:
1. Ganguly, R., & Ramesh, A. (2014). Systematic interpretation of CBCT scans: Why do it? Journal of the Massachusetts Dental Society, 62(4), 68–70. PMID: 24624595
2. Scarfe, W., Li, Z., Aboelmaaty, W., Scott, S., & Farman, A. (2012). Maxillofacial cone beam computed tomography: Essence, elements and steps to interpretation. Australian Dental Journal, 57(Suppl 1), 46–60. https://doi.org/10.1111/j.1834-7819.2011.01657.x
3. Baghdady, M. (2014). Chapter 17 - Principles of radiographic interpretation. In S. C. White & M. J. Pharoah (Eds.), Oral radiology (7th ed., pp. 271–284). Mosby. https://doi.org/10.1016/ B978-0-323-09633-1.00017-1
4. Dief, S., Veitz-Keenan, A., Amintavakoli, N., & McGowan, R. (2019). A systematic review on incidental findings in cone beam computed tomography (CBCT) scans. Dentomaxillofacial Radiology, 48(7), 20180396. https://doi.org/10.1259/dmfr.20180396
5. Braun, M. J., Rauneker, T., Dreyhaupt, J., Hoffmann, T. K., Luthardt, R. G., Schmitz, B., Dammann, F., & Beer, M. (2022). Dental and maxillofacial cone beam CT—High number of incidental findings and their impact on follow-up and therapy management. Diagnostics, 12(5), 1036. https://doi.org/10.3390/diagnostics12051036
6. Barghan, S., Tahmasbi Arashlow, M., & Nair, M. K. (2016). Incidental findings on cone beam computed tomography studies outside of the maxillofacial skeleton. International Journal of Dentistry, 2016, 9196503. https://doi.org/10.1155/2016/9196503
7. Biel, P., Jurt, A., Chappuis, V., Buser, D., & Bornstein, M. M. (2024). Incidental findings in cone beam computed tomography (CBCT) scans for implant treatment planning: A retrospective study of 404 CBCT scans. Oral Radiology, 40, 207–218. https://doi. org/10.1007/s11282-023-00723-5
Thyroid/triticeous calcification
Tonsilloliths
Stylohyoid ligament/ stylomandibular ligament
Intracranial Pineal gland
Intracranial vascular calcification
Choroid plexus
Petroclinoid
Cervical vertebrae
Osteoarthritis
Lytic lesion
Vertebral misalignment (antero/posterolisthesis)
Fusion
Prior surgery
Suspected hemangioma/ pneumatocysts
Skull base Post. comm. artery aneurysm
Suspected clivus lesion
Airway and sinuses Narrowing of pharyngeal airway
Adenoidal hypertrophy
Asymmetry of pharyngeal airway
Hypoplastic paranasal sinuses
Blocked osteomeatal complex
Iatrogenic bone defect, oroantral communication
Concha bullosa
Deviated Nasal septum
TMJ
Osteophytes
Flattening condyle
Condylar erosion, degenerative change
Subcondylar cyst
Bifid condyle
Other Carotid artery calcification
Lymph node calcification
Calcification in subcutaneous tissue
Calcific tendonitis of the longus colli muscle

By Cyril Pandarakalam, BDS, MDS
Dr. Cyril Pandarakalam is a board-certified specialist in Orofacial Pain, Oral Medicine, and Dental Sleep Medicine. He earned his BDS from Bangalore University, completed an internship in Germany, and received his MDS in Oral Pathology and Microbiology from Calicut University. After teaching in India, he moved to the U.S. in 2008 to complete specialty training at the University of Southern California, where he later served as an Assistant Professor.
He joined Southern Illinois University as a tenure-track faculty member and was promoted to Associate Professor in 2017. Since 2020, Dr. Pandarakalam has been practicing at Kaiser Permanente Medical Center in Santa Clara, California. He has published multiple peer-reviewed articles and frequently lectures on topics in oral health.
ORAL CANCER SCREENING
The American Cancer Society estimates that in 2025, approximately 59,660 new cases of oral cavity and pharyngeal cancers will be diagnosed in the United States, with about 12,770 deaths expected from these cancers (1). Regular dental visits provide a critical opportunity for oral cancer screening, enabling the early detection of oral cancer and precancerous lesions, which can significantly improve patient outcomes through timely intervention (2).
In a dental practice, oral cancer screening involves a thorough visual and tactile examination of intraoral and extraoral regions to detect abnormal tissue changes. This process involves carefully inspecting and palpating the face, neck, and oral cavity to identify any visible or palpable irregularities (3). Essential tools for conducting an effective oral cancer screening include a reliable light source, disposable gloves, a dental mirror, a tongue blade, and gauze (4).
Extraoral Examination
The extraoral examination begins with a careful visual inspection of the face to detect any asymmetries, swellings, or other unusual findings. Special attention should be given to the vermilion zone and its border, assessing for changes in color, texture, or the presence of lesions (Figure 1). The submandibular region should be palpated to evaluate lymph nodes for abnormalities, determining whether they are normal, enlarged, rubbery, tender, or fixed. Palpation can be performed externally or using a bimanual technique, with one finger placed intraorally and the other externally beneath the mandible (Figure 2). Additionally, a quick assessment of the anterior cervical lymph nodes, located anterior to the sternocleidomastoid muscle, may provide further diagnostic insight.


Intraoral Examination
Before beginning the intraoral examination, ensure adequate lighting to allow for a clear and comprehensive visual assessment. The patient should remove any removable dental appliances, such as dentures, retainers, or mouthguards, to facilitate unobstructed inspection of all oral structures. This allows for accurate evaluation of the teeth, mucosa, tongue, floor of the mouth, hard and soft palate, and oropharynx.
Labial Mucosa
Ask the patient to slightly open their mouth. Gently retract the upper and lower lips separately to allow for thorough inspection of the labial mucosa, vestibule, and the frenum of both the upper and lower lips. Examine these areas for any changes in color, texture, swelling, ulceration, or other visible abnormalities (Figure 3a and 3b). Palpate the tissues as needed to assess for underlying masses or tenderness. During this examination, minor salivary glands may be palpated, and ductal openings may be observed.


Buccal mucosa
Gently retract the buccal mucosa, beginning on one side and then repeating on the other, to inspect for any signs of abnormalities (Figure 4a and 4b). During this examination, be aware that the parotid papilla, located opposite the maxillary second molar, can vary in appearance. Also, note the possible presence of normal anatomical features such as the linea alba and Fordyce granules, which are common and typically benign findings in this area.


Gingiva
Examine the gingiva systematically by starting on one side and progressing to the other, addressing both the upper and lower jaws (Figure 5). It is recommended to follow a structured protocol: start with the upper right, move to the upper left, and then shift from the lower left to the lower right. This organized method helps ensure that no areas are overlooked.

A vendor member of the Sacramento District Dental Society
Torch Dental is the all-in-one platform to manage, order and budget for dental supplies. Torch Dental negotiates with 50+ authorized vendors across 100,000+ products on your behalf, so you can be confident you’re getting the best value on what you need. Simplify your finances, gain complete control over your spending and free up valuable time today.














...Continued from page 13
Tongue
To thoroughly examine the tongue, start by inspecting the dorsum (Figure 6a) and palpating the lateral borders (Figure 6b and 6c). Use gauze to gently move the tongue side to side to view the posterior lateral borders, where lingual tonsils may appear enlarged or inflamed but are typically benign unless other symptoms are present. Then, have the patient raise their tongue to the roof of the mouth to assess the ventral surface and floor of the mouth (Figure 6d). The plica fimbriata—normal folds under the tongue—can sometimes be mistaken for abnormal findings.




Floor of the mouth
Inspect the floor of the mouth for any abnormalities (Figure 7a). Bimanual palpation is performed bilaterally to assess the submandibular region for abnormalities such as swelling or nodules (Figure 7b). This allows for evaluating both the submandibular glands and the surrounding lymph nodes, aiding in the early detection of infections, salivary stones, or other pathologies.


Roof of the mouth
Ask the patient to open their mouth wide. If needed, use a mouth mirror or tongue blade to gently press down the tongue to improve visualization. Examine the hard palate, soft palate, and uvula carefully using good lighting (Figure 8). Look for any abnormalities such as redness, swelling, lesions, ulcers, discoloration, or asymmetry.

Oropharynx
To view the oropharynx, gently depress the tongue slightly toward its posterior using a mouth mirror or tongue blade (Figure 9). Adjust the tool as needed to avoid resistance from the tongue, ensuring patient comfort. Ask the patient to say “ahh.” This action elevates the soft palate, providing optimal visualization of the oropharynx.

Conclusion
Oral cancer screening should be performed routinely on all adult patients during comprehensive exams. Clinicians should remain vigilant and ensure that any lesions persisting beyond two weeks are either biopsied or referred promptly to an appropriate specialist for further management.
References
1. Siegel RL, Kratzer TB, Giaquinto AN, Sung H, Jemal A. Cancer statistics, 2025. CA: A Cancer Journal for Clinicians. 2025;75(1):10-45.
2. https://www.cancer.gov/types/head-and-neck/ hp/oral-screening-pdq
3. Lingen MW, Abt E, Agrawal N, Chaturvedi AK, Cohen E, D’Souza G, et al. Evidence-based clinical practice guideline for the evaluation of potentially malignant disorders in the oral cavity: A report of the American Dental Association. The Journal of the American Dental Association. 2017;148(10):712-27.e10.
4. https://oralcancerfoundation.org/discoverydiagnosis/cancer-screening-protocols/
Legends
1. Lips. Observe the vermilion zone and its border, assessing for changes in color, texture, or the presence of lesions
2. Submandibular region. Evaluate lymph nodes for any abnormalities
3. Labial mucosa
a. Upper labial mucosa
b. Lower labial mucosa
Inspect labial mucosa, vestibule, and the frenum of both the upper and lower lips and examine these areas for any changes in color, texture, swelling, ulceration, or other visible abnormalities
4. Buccal mucosa
a. Right buccal mucosa
b. Left buccal mucosa
Inspect buccal mucosa on either side for any signs of abnormalities. Note the presence of normal structures such as linea alba, Fordyce granules and parotid papilla
5. Gingiva. Examine the gingiva systematically by starting on one side and progressing to the other, addressing both the upper and lower jaws
6. Tongue
a. Dorsal surface
b. Right lateral border
c. Left lateral border
d. Ventral surface
Inspect dorsum and ventral surfaces of tongue.
Inspect and palpate lateral borders of tongue
7. Floor of mouth
a. Inspection
b. Bimanual palpation
Inspect the floor of the mouth. Bimanually palpate to assess the submandibular region for abnormalities
8. Roof of the mouth. Examine the hard palate, soft palate, and uvula and look for abnormalities
9. Oropharynx. Gently depress the tongue using a tongue blade. Ask the patient to say “ahh”, providing optimal visualization of the oropharynx.


By Peter Yanni, DMD, MS SDDS Member
Dr. Yanni earned both his masters degree in Medical Sciences as well as his dental degree at Western University of Health Sciences. Afterwards, he earned his masters in Oral and Craniofacial Sciences as well as his certificate in Periodontology at the University of California San Francisco. Dr. Yanni has recently joined Dr. Yi and Dr. Vasanthan at the Perio Specialist office is Roseville. He is a member of ADA, CDA, AAP, and SDDS.
DESQUAMATIVE GINGIVAL DISEASES
A vital part of every comprehensive patient exam is a review of their periodontal health. During these exams, we will subconsciously take notice of the general appearance of the patient’s gingiva, including the tone, texture and firmness before even picking up a periodontal probe. Understandably, our initial focus is to identify signs of periodontal disease, but as dentists, we are fine-tuned to identify when other abnormalities are present.
Sometimes, patients will present with nonplaque induced gingival diseases, and it is important to identify these, as they can potentially affect a patient’s quality of life as well as have systemic implications. Desquamative gingivitis is an umbrella term used to refer to chronic inflammatory gingival diseases characterized by gingival erythema, gingival sloughing, and erosion of gingival tissues. The three main diseases that fall in this category are lichen planus (LP), pemphigus vulgaris (PV), and mucous membrane pemphigoid (MMP).
Lichen Planus
Lichen planus is an inflammatory disease characterized by a T-cell-mediated immune response. Lichen planus can be divided into two different types, reticular or erosive. While a biopsy is needed to confirm a diagnosis of lichen planus, the results will not differentiate between the two types. Clinical findings and symptoms are critical for differentiating between the two. Reticular lichen planus is by far the most common type and is characterized by raised, thin, white lines that have a reticular pattern (Wickham’s striae). It is most commonly found on the buccal mucosa, tongue, and gingiva. Reticular lichen planus typically does not have any symptoms or require any treatment. The second type is erosive lichen planus and is characterized by erythematous or white pseudomembranous areas. It is also most commonly found on the buccal mucosa, tongue,
and gingiva. Patients will typically report related symptoms such as pain or a burning sensation within their gingiva. It is important to note that erosive lichen planus has 0.4% to 2% chance of malignant transformation, so annual biopsies are recommended if symptoms continue to persist.


Pemphigus Vulgaris and Mucous Membrane Pemphigoid
Both Pemphigus vulgaris (PV) and Mucous membrane pemphigoid (MMP) are autoimmune blistering diseases, where autoantibodies attack adhesion proteins within epithelial cells, resulting in a loss of adhesion. One of the key differences is the level of blister formation. PV causes blistering within the dermis in the intraepithelial layer, while MMP has deeper blister formation within the subepithelial layer and therefore does not rupture as easily.
Pemphigus vulgaris is particularly relevant to dentists as oral lesions are both the most common presentation and the earliest. These lesions typically appear before skin lesions and can be the only presentation of the disease. They are characterized by painful and slow-healing ulcers on the buccal mucosa, palate, and tongue. If pemphigus is expected, you can apply gentle friction to the gingiva and check for blistering and peeling, known as a positive Nikolsky’s sign. Mucous membrane pemphigoid clinically presents similarly to PV with painful blisters and erosions on the gingiva, buccal mucosa, palate, and tongue. MMP is typically characterized by a negative Nikolsky’s sign, so applying light friction to the gingiva should not cause blistering. Identifying MMP early is critical because a serious complication that can arise is ocular involvement. Ocular pemphigoid can lead to conjunctival scarring and vision loss. Both PV and MMP require a biopsy and analysis under both H&E staining and direct immunofluorescence for an accurate diagnosis.


Patients with a history of autoimmune and inflammatory conditions are at higher risk of developing desquamative gingival diseases, and it should raise a flag if you see these types of conditions mentioned on a patient’s health history questionnaire. These diseases cannot be cured and are typically treated with topical corticosteroids, but severe cases can require systemic corticosteroids or immunomodulators. Because of the side effects of chronic steroid use, it is important that these diseases are managed in conjunction with a patient’s primary care physician and an oral medicine specialist.

CARMICHAEL/FAIR OAKS AREA: 4 Ops, 19+ Yrs Goodwill, 1,310 Sq. Ft., Open Dental PMS, Paperless, Digital, 55% Delta Premier 2024 GR $516K #CA4300
FRESNO METRO AREA: New Listing! 6 Ops, GP, 33+ Yrs Goodwill, Eaglesoft PMS, Digital, 3 5 days/wk Hygiene 2024 GR $1 46M #CA4240
GREATER STOCKTON METRO & SURROUNDING AREA: New Listing! 6 Ops, GP, 55+ Yrs Goodwill, FFS, 8 days/wk Hygiene, 1,880 sq ft 2024 GR $1 4M #CA4533
MODESTO: GP, 5 Ops, 14+ Yrs Goodwill, 1,950 Sq Ft , 1 25 days/wk Hygiene, Dentrix PMS 2023 GR $405K. #CA4340
REDDING/RED BLUFF AREA: GP, 4 Ops, 22+ Yrs Goodwill, Dentrix PMS, 2,100 Sq Ft , Paperless, Desirable Location! 2024 thru September GR $313K #CA4266
REDDING/RED BLUFF/SHASTA COUNTY AREA: $1 73M 2024 Collections GP Practice with Real Estate available, 6 Ops, Hi Tech (Dentrix, CEREC, 3D Conebeam), Seller to work back 3 to 5 years #CA3790
REDDING/RED BLUFF NORTHERN CA VALLEY AREA: 5 Ops+RE, GP, 36+ Yrs Goodwill, High-Traffic Location, 9 days/wk Hygiene, 2,138 sq ft 2024 GR $1 39M #CA3954
SACRAMENTO: $1 1M Collections GP in perfect Sacramento Metro Location for High Traffic 5 Ops (could be 8 total Ops) on 7 days/week Hygiene, with Seller multi-year Workback offered #CA4459
SOLANO COUNTY AREA: 8 Ops, GP, 45+ Yrs Goodwill, 3,800 sq ft Paperless, Dentrix PMS, Digital 2024 GR $1 535M #CA3586


By Mohd Khalaf, DDS SDDS Member
Dr. Mohd Khalaf is specialized in the areas of Orofacial Pain and Oral Medicine. He completed his training in Orofacial Pain and Oral Medicine at the University of Kentucky and the University of Southern California, Los Angeles. Dr. Khalaf is Board certified by the American Board of Orofacial Pain (ABOP), and a Fellow of the American Academy of Orofacial Pain (FAAOP). He taught at postgraduate level in both Orofacial Pain and Oral Medicine, at the University of Kentucky. He is also published in both fields of Orofacial Pain and Oral Medicine. Dr. Khalaf founded the Head & Neck pain and Oral Medicine services at Kaiser Permanente in Northern California. He is the founder & President of The Head Pain Center in Roseville California.
OVERVIEW OF BURNING MOUTH SYNDROME
Burning Mouth Syndrome (BMS) is a chronic oral pain condition. It is characterized by an oral burning sensation and may be associated with dysgeusia, paresthesia, dysesthesia, and dry mouth. The etiology of the disease process is not very clear, but it is believed to be neuropathic in origin if other local and systemic factors are ruled out. BMS is a diagnosis of exclusion, and local and systemic factors must be ruled out. According to the International Headache Society, BMS is defined as “an intraoral burning or dysaesthetic sensation, recurring daily for more than 2 hours per day over more than 3 months, without clinically evident causative lesions.”
Clinical features of BMS:
The clinical features of BMS are burning and/or pain sensation, Dysgeusia, and Xerostomia are three symptoms that characterize BMS. These symptoms may be associated with or aggravated by parafunctional habits, see Fig.1.
Patients may further report feeling a burning sensation in affected sites. This symptom is usually localized in the tip or the anterior two-thirds of the tongue but can also affect the lips, palate, gingiva, buccal mucosa, and oropharynx.
Other reported symptoms by BMS patients included numbness, tingling, prickling, or simply vague discomfort sensations in the mouth. These symptoms typically present bilaterally. The intensity of the pain ranges and can fluctuate from mild to severe.

Fig. 1. Tongue Scalloping can be seen in some BMS patients. https://pmc.ncbi.nlm.nih.gov/articles/ PMC6459460/
Patients may further report feeling a burning sensation in affected sites. This symptom is usually localized in the tip or the anterior two-thirds of the tongue but can also affect the lips, palate, gingiva, buccal mucosa, and oropharynx.
Types of BMS - Primary BMS:
If no causative factors are identified, it is defined as primary (or idiopathic) BMS.
BMS occurs spontaneously and without any specific precipitating factor in more than 50% of patients. Nearly one-third of patients report that their burning pain is related to a dental procedure, medical illness, or medication use. However, a cause-and-effect relationship between these incidents has not been identified.
Examination findings in patients with BMS show no evidence of oral lesions or other oral mucosal abnormalities.
Secondary BMS:
When BMS is associated with underlying causative factors, it is defined as secondary BMS.
Secondary BMS has multiple causative local and systemic factors.
The most common oral disease that can present with burning pain in the mouth is oral candidiasis, see Fig.2. as an example of such presentation. A fungal culture should be taken to confirm the diagnosis, and if the oral candidiasis diagnosis is confirmed, then a prescription of antifungal medication should be discussed with the patient. In addition, oral mucosal lesions like erosive lichen planus, recurrent aphthous stomatitis, or other vesiculobullous diseases may present with burning mouth symptoms. However, these disorders usually present with characteristic lesions affecting the oral mucosa.
Some of the systemic diseases associated with burning pain in the mouth include:
• Hematologic deficiencies
• Nutritional deficiencies
• Hypothyroidism
• Diabetes mellitus
• Autoimmune disorders
The following tests can help in the diagnosis of secondary BMS:
• Complete blood count with differential
• Fasting blood glucose
• Hemoglobin A1c
• Serum Iron Test
• Ferritin
• Vitamins B1, B2, B6, and B12
• Folate
• Serum Zinc Test
• Thyroid panel
• Autoantibodies (i.e., antinuclear antibody, rheumatoid factor, and anti–Sjögren syndrome antigens A and B.
Xerostomia is another key contributing factor that needs to be evaluated and addressed in BMS patients.

Fig. 2.
https://pmc.ncbi.nlm.nih.gov/articles/ PMC6459460/
Management:
Managing BMS can be challenging. Differentiating between primary and secondary BMS is the first step in aiding the diagnosis and management of BMS.
Secondary BMS is treated by managing the underlying etiology. Primary BMS can be more challenging to manage.
In the management of primary BMS, patients must be educated and assured about the benign nature of primary BMS. The provider needs to set realistic treatment expectations; BMS is a chronic pain condition. As such, symptoms can be managed, but complete resolution may not be achieved.
Evidence suggests that primary BMS can be neuropathic in nature; the pharmacologic management of BMS is similar to the management of other neuropathic pain conditions. Studies have evaluated the efficacy of various medications, categorized as anxiolytics, anticonvulsants, antidepressants, and analgesics, for the management of primary BMS. Dietary supplements, physical barriers, capsaicin, low-level laser therapy, acupuncture, electromagnetic radiation, and cognitive behavioral therapy (CBT) have also been studied. First-line pharmacologic agents include clonazepam and the antioxidant α-lipoic acid (ALA). Anticonvulsants, such as gabapentin, and antidepressants are second-line medications. Topical anesthetics, such as 20% benzocaine, may provide temporary relief.
Conclusion:
BMS is a chronic orofacial pain. To accurately diagnose BMS, the clinician must first rule out and address any possible underlying local or systemic factors. Increasing evidence indicates that BMS may be a neuropathic pain condition and needs to be managed as such. Appropriate referral of patients with BMS to an orofacial pain specialist is necessary to establish the correct diagnosis and provide the appropriate management.

By Jeffrey Delgadillo, DDS SDDS Member
Dr. Delgadillo practices full scope Oral & Maxillofacial Surgery as partner at Drs. Heise, Alpha & Delgadillo. Born and raised in Sacramento he is committed to carrying on the practice’s 75 year legacy of patient centered care and support of organized dentistry.
PRACTICAL GUIDE TO MEDICATION RELATED OSTEONECROSIS OF THE JAW (MRONJ)
What Is MRONJ?
MRONJ is defined as:
• Exposed bone or bone that can be probed through a fistula lasting ≥8 weeks.
• Occurs in patients treated with antiresorptive (i.e. bisphosphonates, RANKL inhibitors) or antiangiogenic agents.
• No history of radiation therapy to the jaws or obvious jaw metastasis.
How to Identify Patients at Risk for MRONJ?
When obtaining patient medical history, you can identify patients potentially at risk for MRONJ when they report osteoporosis, osteopenia, and current/or previous cancer treatment. You should ask further questions or request a medication list to review.
It is important to understand the differences in mechanism of action between the different classes of medications: bisphosphonates/RANKL inhibitors/antiangiogenic agents. Knowing the dosage and frequency of prescribed medications is important.
*Note: Common medications generic names that end in -dronate, -mab, -nib
High-Risk Medications Associated with MRONJ
Medication Name Drug Type Indication
Zoledronic acid (Zometa®) IV bisphosphonate
Cancer-related bone disease
Pamidronate (Aredia®) IV bisphosphonate Cancer-related bone disease
Denosumab (Xgeva®) RANKL inhibitor (high dose) Cancer-related bone disease
Bevacizumab (Avastin®) Antiangiogenic agent Solid tumors
Sunitinib (Sutent®) Multi-kinase angiogenesis inhibitor Renal cell carcinoma
Moderate/Low Risk Medications Associated with MRONJ
Medication Name Drug Type Indication
Alendronate (Fosamax®) Oral bisphosphonate Osteoporosis
Risedronate (Actonel®), Ibandronate (Boniva®) Oral bisphosphonates Osteoporosis
Denosumab (Prolia®) RANKL inhibitor (low dose) Osteoporosis
Romosozumab (Evenity®) Sclerostin inhibitor with antiresorptive effect Osteoporosis
MRONJ Staging and Management (AAOMS 2022)
AAOMS now includes Stage 0 MRONJ, which presents without exposed bone but may involve pain, radiographic changes, or swelling.
Stage Presentation Treatment
0 Non-exposed bone + symptoms or imaging changes Monitor, analgesics, +/- antibiotics
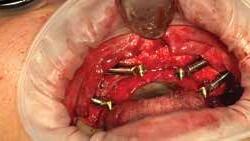
1 Exposed bone, asymptomatic Antibacterial rinse, monitor See Fig 1
2 Exposed bone with pain/infection Rinse, antibiotics, superficial debridement, OMFS referral See Fig 2
3 Extensive bone necrosis or fracture Surgery, antibiotics, OMFS referral See Fig 3


Recommended Antibiotics for MRONJ Management
Situation First-Line Option

Alternatives (Penicillin Allergy)
Mild to moderate infection Amoxicillin Azithromycin, Doxycycline
Moderate to severe infection
Adjunct therapy for all cases
Clindamycin or Amoxicillin/ clavulanate (Augmentin®)
0.12% chlorhexidine gluconate rinse
When to Consider a Drug Holiday
Clindamycin or azithromycin + metronidazole
Same
A drug holiday is a temporary pause in antiresorptive therapy considered prior to invasive dental procedures like extractions or implant placement.
Medication When to Consider Drug Holiday Typical Duration
Oral bisphosphonates (e.g., Fosamax®)
Denosumab (Prolia®)
• Quarterly Tax and Business Planning
• QuickBooks setup, Training and Consulting
• Work with over 100 Dental Practices
• Assistance with Practice Purchases
• Review of Proper Business Structures
• Business Valuation
• Real Estate and LLC’s
≥4 years or ≥2 years + additional risks (e.g., steroids)
≥2 years of therapy
IV bisphosphonates (e.g., Zometa®) Not routinely advised; consider only with OMFS and oncology input
Cancer meds (Xgeva®, Avastin®, etc.) Not advised; avoid elective procedures during treatment
2 months before and after procedure
Schedule surgery at end of 6-month cycle
Case-by-case basis
Requires specialist coordination


...Continued from page 21
Current Debate: Is a Drug Holiday Effective?
Implants and Bone Grafting?
While drug holidays are often recommended for osteoporosis patients on long-term therapy, their efficacy in preventing MRONJ remains controversial. The oral surgery community cautiously supports drug holidays for certain low-risk patients, while emphasizing medical consultation and shared decision-making with our medical colleagues for our mutual patients after properly evaluating risks vs. benefits.
For patient safety as well as interprofessional etiquette you should not recommend a patient to discontinue use of a medication to treat a medical disease that is not prescribed by you.
There is also the question of whether or not these patients are good candidates for bone graft and implant placement. This is based on understanding of the medications and what they are treating correlated with clinical experience.
Clinical Summary for General Dentists
• Ask about antiresorptive/antiangiogenic medications at every exam.
• Document drug name, dose, and treatment duration.
• Avoid extractions in high-risk patients unless necessary.
• Consider drug holiday in long-term osteoporosis patients, but only after medical consultation.
• Refer to oral surgery/coordinate care with physicians.
• Educate patients on hygiene, caries control, and implant risks.
Final Takeaways
• MRONJ is rare but can be serious, especially with Zometa®, Xgeva®, and Avastin®.
• The 2022 AAOMS guidelines emphasize conservative treatment with escalation by stage.
• Drug holidays are selectively beneficial in patients on longterm oral therapy or Prolia®- evidence is evolving.
• Dentists play a key role in risk prevention, early detection, and interdisciplinary care. Treatment planning strategies should be more aggressive for poor, questionable and hopeless teeth prior to initiation of treatment with known high-risk medications.
The oral surgery community admits there is still much we do not understand, and that more research is required to refine guidelines and our understanding of the risks associated with these medications. Let patient-centered care always lead the way and never be afraid to ask for help.
References:
Marx, R. E. (2022). Drug - Induced Osteonecrosis of the Jaws: How to Diagnose, Prevent, and Treat It (3rd ed.). Quintessence Publishing. ISBN 978 -1- 64724 - 089 - 9. (quintessence-publishing.com)
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F. American Association of Oral and Maxillofacial Surgeons Position Paper on Medication-Related Osteonecrosis of the Jaw—2022 Update. Journal of Oral and Maxillofacial Surgery. 2022;80(5):920-943. https://doi. org/10.1016/j.joms.2022.01.008


Let's have a conversation about your goals and timeline today.
Mobile: (805) 714-2115
Email: brian@integritypracticesales.com
Brian's DRE#: 01947466 IPS DRE#: 01911548
With over 20 years of customer service and sales experience, Brian Flanagan has become a resource for dentists up the down the state. He has eight years’ experience in the industry, five of them with Integrity Practice Sales. During his time at IPS, he has partnered with many doctors to help them transition successfully and achieve their financial goals. As a Davis native, Brian has a special place in his heart for Northern California and is our area specialist.
As an Insurance Broker, Brian is also able to help dentists with their insurance needs


A Closer Look at the Smiles for Kids Program Process and Timeline
The Sacramento District Dental Foundation (SDDF) is excited to announce that planning is already underway for the 2026 Smiles for Kids Day (SFK), taking place on Saturday, February 7, 2026! Now in its 25th year, this annual event provides free dental care to children in need throughout the region, made possible through the incredible generosity of our SDDS member dentists and their dental teams.
Mark your calendars and get involved! Here’s what’s ahead for this year’s Smiles for Kids program:
• September 16, 2025: We kick off the program with our School Nurse Meeting at the SDDS office. Nurses and staff from participating schools will receive detailed information about how to get involved and prepare for school dental screenings, which run from September through the end of November.



• Participating schools will receive toothbrushes, toothpaste, floss, bookmarks, and pencils to distribute to each child screened.
• Throughout the year, the SDDS team works closely with school nurses and staff to navigate children with a dental home and ensure those with urgent dental needs receive timely care.
• As part of the program, SDDS offers schools interactive puppet shows by The Puppet Art Theater! Children will learn the importance of the basics in maintaining their oral health from Sir Enamel, who teaches them how to fight off the infamous Sugar Bugs and Plackey!
All of this is made possible through your generous support of the SDDS Foundation through membership and donations. If you would like to volunteer for the SFK program, here are ways you can help:
• Volunteer to do school screenings (September–November 2025)
• Open your office as a site on Smiles for Kids Day (February 7, 2026)
• Volunteer to assist at one of our Smiles for Kids Day sites

• Volunteer to Adopt-a-Kid (for children who need immediate care or children who need additional care after SFK Day).
Stay tuned for more updates as we prepare for a day of giving back and promoting healthy smiles across our community!



Does Your Practice Own You or Do You Own a Business?
Understanding the difference – BPE Law works with you to ensure that you have the best opportunity to be successful and build a thriving business. Offering efficient, professional and cost-effective representation for our clients.
Our Dental Law Services Include:
• Corporate Law
• Contract Law
• Employment Law
• Practice Transitions
• Finance
• Real Estate
• Estate Planning (916) 966-2260 | info@bpelaw.com | bpelaw.com
Volunteer OPPORTUNITIES
Ways to volunteer and support the SDDS Foundation:
Become a member of the Foundation –it’s only $75 per year
Donate to the programs of the Foundation –donations help provide screening supplies, toothbrushes and fund the puppet shows Smiles for Kids Day – February 7, 2026 –Save the Date!
Opportunities include:
• Host an SFK site
• Adopt a child, post SFK Day
• Volunteer to be a specialty provider for adopt-a-child
• Volunteer to screen kids at schools
To volunteer, Contact: SDDS office 916.446.1227 • smilesforkids@sdds.org
Smiles for Big Kids is ongoing all year long –we need volunteers to adopt the BIG kids too (especially vets and the elderly)
Volunteers Needed: Dentists willing to “adopt” patients for immediate/emergency needs in their office.
To volunteer, Contact: SDDS office 916.446.1227 • sdds@sdds.org
Willow Dental Clinic
One Saturday every other month Contact dental@willowclinic.org for more information. You can check out their website here: www.willowclinic.org/services/dental
CCMP (Coalition for Concerned Medical Professionals) Volunteers needed: General Dentists, Specialists, Dental Assistants and Hygienists.
To volunteer, Contact: 916.925.9379 • ccmp.pa@juno.com
Everyone for Veterans
To volunteer, Contact: SDDS office 916.446.1227 • sdds@sdds.org everyoneforveterans.org/for-dentists.html
California CareForce
2025 Sacramento Valley Clinic
October 10-12, 2025 • 7am • CalExpo To volunteer, visit: www.californiacareforce.org/

YOU
THE DENTIST, THE EMPLOYER
Holiday HR Starts Now
By Mari Bradford; California Employers Association (SDDS Vendor Member)
Ah, the holiday season! A magical time of year when office coffee mysteriously becomes pumpkin and then peppermintflavored, leftovers are brought to the office, Secret Santa gifts are exchanged, and you have to juggle the fine line between festive fun and California labor law compliance. But don’t worry—we’re here to help you navigate bonuses, gifts, and celebrations while keeping your team feeling merry and bright (and keep you out of trouble).
Holiday Pay: The Great Debate
First things first: Do employees in California have to get extra pay for working on holidays? The short answer? Nope! Unless your company policy states otherwise, holiday pay isn’t legally required.
Bonuses: Generosity with a Side of Compliance
Bonuses are a fan favorite, but in California, you’ve got to know your “discretionary” from your “non-discretionary.”
• Discretionary Bonuses: These are like surprise holiday cookies— completely unexpected and with no strings attached. They’re not tied to performance metrics and don’t affect overtime calculations. These are not considered part of the employee’s regular rate of pay.
• Non-Discretionary Bonuses: These are more like the fruitcake of bonuses—deliberate and full of ingredients. If bonuses are tied to measurable performance (like sales goals) they must be included in overtime calculations, or the labor board may hand you a lump of coal.
Pro tip: To avoid confusion, be crystal clear when announcing the nature of the bonuses to your team.
Holiday Gifts: It’s the Thought (and Budget) That Counts
You don’t need to break the bank to spread holiday cheer. A little thoughtfulness can go a long way in making your employees feel valued:
• Self Care Packages: Who doesn’t love unwrapping a box of snacks, candles, or a cozy blanket? Curate gifts that cater to employees’ interests or regional preferences, such as locally sourced treats.
• Gift Cards: They’re the Swiss Army knife of gifts—practical, flexible, and guaranteed to not end up re-gifted at next year’s white elephant exchange.
• Extra Time Off: The holy grail of employee gifts. Nothing says “We appreciate you” like a bonus day to sleep in or tackle that Netflix backlog.
Parties and Celebrations: Keeping It Jolly (and Inclusive)
Holiday celebrations are the ultimate team-building opportunity—or at least an excuse to wear that reindeer sweater you love. But holidays also mean different things to different people, so inclusivity is the name of the game:
• Neutral Themes: Instead of Christmas-specific décor, consider going with winter wonderland vibes. Everyone loves twinkly lights and hot chocolate, right?
DO YOU USE THE HR
The SDDS HR Hotline is an exclusive benefit to SDDS Members. It's powered by the California Employers Association and they are ready for your call.
• Team Activities: Host a fun, lowpressure event like trivia, cookie decorating, or a “guess the ugly sweater” contest. Virtual or inperson, keep it light and full of laughs.
• Charity Initiatives: Nothing warms the heart like giving back. Partner with your team to support a local cause or charity—it’s a win for everyone.
Wrapping It All Up
The holidays are a time to show your team how much you appreciate their hard work—without accidentally stepping on a compliance landmine. They’re also an opportunity to reinforce a culture of recognition and care. Bonuses, gifts, or just a heartfelt thank-you can go a long way in ending the year on a high note. So, grab your Santa hat, double-check your payroll policies, and spread some joy that would make even the Grinch crack a smile. After all, happy employees are the best gift of all!
Questions on this or any other HR issue? Give CEA a call at the SDDS HR Hotline at 888-784-4031.












By Idean Rezaei CNU Dental Student (D4)
Originally from Florida, Idean is now in his fourth year of dental school. His future career goals after school include working as an associate for a private practice or a DSO while also taking on CE courses in implants. Outside of dentistry Idean enjoys most outdoor activities, and is looking forward to continuing to enjoy all that California has to offer.
The Softer Side of Dentistry
Coming into the field of dentistry, I had a clear understanding of what would be expected in terms of the hard sciences and clinical skills. These competencies can be built through coursework, shadowing, and assisting. However, what is much harder to prepare for and arguably just as critical is the development of soft skills required to interact with patients, especially those in vulnerable states. Whether due to acute pain, aesthetic concerns, or general dental anxiety, patients often present with emotions that require sensitivity and careful navigation. Building trust and establishing rapport are essential for helping patients understand and value the treatment being proposed.
A key starting point in patient management is case selection. Beyond evaluating whether a case falls within our clinical capabilities, we must also assess the patient’s emotional state and determine whether we, as providers, are equipped to manage it. While some emotional complexity can and should be managed with empathy and professionalism, hostile or verbally abusive behavior especially when directed at auxiliary staff should not be tolerated under any circumstance.
During my time in the field, I have observed a wide range of responses from providers when patients present with heightened emotions. What stands out most is the importance of not feeding into negative emotions like frustration or fear. I’ve found it helpful to remain calm and composed, sometimes expressionless, while allowing the patient space to express themselves. Emotional outbursts shouldn’t be ignored, but they must be addressed constructively. I aim to gently redirect the conversation toward the patient’s primary reason for seeking care, acknowledging their concerns and then outlining what I can do to help them in that moment and how it ties into their broader
treatment goals. Given the time constraints of a busy clinical day, we must be both empathetic and efficient in these interactions.
Although we are not mental health professionals, we must remain mindful of how mental health intersects with oral health. Dental anxiety is a common example, one that causes many patients to avoid care until their issues become urgent, which only worsens their experience. Understanding the root of a patient’s anxiety, whether from a past negative experience or a physical trigger like a strong gag reflex enables us to adjust our communication and techniques accordingly. For some patients, this might mean detailed explanations at every step; for others, minimizing discussion may be more effective.
Clear, honest communication of expectations is essential, especially during the more uncomfortable parts of treatment, such as local anesthesia or impressions. It is equally important to establish a way for patients to assert control such as raising a hand to pause treatment and to honor that agreement without dismissing their needs with comments like, “just one more second.” Trust is built not only through words but by consistently following through on what we promise.
While technical proficiency is fundamental in dentistry, it is our ability to listen, empathize, and adapt that often defines the patient’s experience. Developing these interpersonal skills requires ongoing reflection and practice but makes us more effective and compassionate providers.

CDA Major Issues & Priorities 2025
1. Medi-Cal Funding
Medi-Cal currently provides medical and dental coverage to 15 million low-income Californians (one-third of all residents and half of all children), making it the largest dental plan in the state.
The 2025-26 state budget preserves Proposition 56 funding for Medi-Cal Dental services and dental coverage for undocumented adults in California through July 1, 2026. CDA is very appreciative that the state legislature rejected the governor’s proposal to eliminate this funding in this year’s budget.
Proposition 56, which voters approved in 2016 to raise the state’s tobacco tax and increase Medi-Cal reimbursement rates, has led to historic improvements in patient access to care and dentists’ participation in Medi-Cal:
• 27% increase in new dental office visits by Medi-Cal patients over the past five years, amounting to nearly one million more Californians getting dental care.
• 34% increase in the number of MediCal dental providers across the state.
• 40% of California dentists are now enrolled in Medi-Cal.
Unfortunately, the new federal budget signed in July slashes Medicaid spending by $1 trillion over the next ten years, which will amount to an estimated 20% reduction in federal funding for California. Among the most significant federal changes are new restrictions on provider taxes, such as the managed care organization tax that Proposition 35 is built on. California voters approved the CDA-sponsored ballot measure last November to protect the Medi-Cal budget, with 68% of voters supporting.
The state budget also diverted Proposition 35 funding this year to pay for already incurred Medi-Cal costs, rather than reimbursement
rates as the measure intended. Diverting these funds disregards the will of the voters and raises serious legal concerns.
CDA will continue advocating for budget actions that protect access to dental care and the progress we have made in recent years to improve the Medi-Cal Dental program.
2. SB 386: Virtual Credit Card Payments (CDA-Sponsored)
CDA is sponsoring SB 386, authored by Sen. Monique Limon (D-Santa Barbara), to address the use of virtual credit cards (VCCs) as a payment method by dental insurance companies. Dental plans are more frequently using third party companies to issue payments to dental offices through VCCs, which take a processing fee of 2-5%, plus the merchant transaction fee through their credit card terminal. These fees can take up to 10% off the top of the payment owed by the plan.
VCC payments in many cases become the default payment method. While dental practices can opt out of VCC services, the opt-out process is often difficult and not always permanent. VCC companies are known to reinstitute the payment method with its excessive fees after the provider opts out, even as soon as the very next payment. Furthermore, requesting an alternative payment method can delay receipt of that payment, waste administrative staff time and create challenges for office accounting. Ultimately, this trend is taking health care dollars away from patient care and reducing the value of dental coverage. SB 386 will address this by:
• Requiring that the default payment method must be one that does not include a fee. If a dentist would like to use VCCs as their primary payment method, they may do so, but only by written authorization – and they may opt out of VCCs again at any time.
Reprinted with permission from California Dental Association
• Requiring plans to notify dentists of alternative payment methods, how to select a payment method, and any fees associated with each payment method.
SB 386 continues last year’s work on SB 1369. To address concerns with the previous bill, SB 386 would not apply if a contract between a plan and dentist specifically addresses the type of payment methods for services rendered.
The bill passed in the Senate and is now under consideration in the Assembly.
3. AB 371: Dental Insurance –Access & Accountability (CDA-Sponsored)
Dental patients across California are facing increasing challenges with finding a dentist who is included in their dental plan’s network. CDA sponsored AB 371 this year, authored by Asm. Matt Haney (D-San Francisco), to address the growing inadequacy of dental plan networks and the resulting barriers to care. The bill does this in three ways:
• Requires dental insurance companies to report provider network information to the state for all dental plans they sell. Nearly half of Californians with commercial dental coverage are in plans governed by federal ERISA law, which are not included in the current network adequacy assessments conducted by the Dept. of Managed Health Care and Dept. of Insurance. As a result, the state has a very incomplete picture when assessing dental provider networks.
• Establishes new “time and distance” standards for dental plans to reduce the time patients must wait for an appointment or distance they must travel. The current required standards for dental plans are well below the standards for medical plans.
• Requires all dental plans to comply with a patient’s “assignment of benefits” (AOB) requests, so that patients can receive care from an out-of-network dentist and have the dental plan send payment directly to the dental office. Currently, many patients seeing an outof-network dentist must pay 100% of the treatment costs upfront and wait to be reimbursed, putting an unnecessary burden on patients and further restricting use of their already limited dental benefits.
AB 371 did not advance in the Assembly Appropriations Committee this year due to projected implementation costs. CDA will continue working to address those concerns and is committed to moving this proposal forward. Patients should not be penalized for seeing an out-of-network dentist when their dental plan is not ensuring an adequate provider network.
4.
AB 873: Dental Assistant Infection Control Training
(CDA-Sponsored)
Dental practices across California are struggling to hire and retain staff due to new statutory barriers impacting unlicensed dental assistants. Currently, newly hired unlicensed dental assistants must complete an 8-hour infection control course in person before beginning work in a dental office. However, the limited availability of in-person courses—especially in rural and underserved areas—causes significant hiring delays, leading some candidates to seek jobs in other industries. This workforce challenge reduces access to care for patients and exacerbates existing staffing shortages in dental practices.
CDA is sponsoring AB 873, authored by Asm. Juan Alanis (R-Modesto), to address these issues by:
• Repealing the immediate timing requirement and establishing a 90-day window for completing the eight-hour IC course.
• Directing the dental board to approve virtual course formats, making the training more accessible and flexible for new hires statewide.
This bill will help dental offices hire new staff more efficiently while maintaining patient safety and important infection control standards. These reforms ensure that unlicensed dental assistants can receive timely training without unnecessary delays that impact both dental teams and the patients they serve.
AB 873 passed in the Assembly and is now under consideration in the Senate.
5.
SB 351: Private Equity in Health Care (CDA Co-Sponsored)
Dentists are increasingly concerned with the ways private equity firms are interfering with their clinical judgement about what is best for their patients. This bill, authored by Senator Christopher Cabaldon (D-West Sacramento), addresses consolidation in the state’s health care system and the growing role of private equity interests that are not aligned with patient healthcare needs.
SB 351, co-sponsored by CDA, strengthens the existing ban on the corporate practice of dentistry and medicine by explicitly barring the specific ways private equity groups or hedge funds are influencing the clinical decisions of dentists and physicians. Under existing law, licensed dental professionals and dental corporations are subject to strict professional and ethical standards to ensure patient care remains in the hands of qualified practitioners. However, existing laws do not explicitly regulate the increasing involvement of private equity and hedge funds in dental practices. As a result, these entities can exert controls that allow corporate interests to influence clinical decision-making.
This bill prohibits, for example, patient quotas, limits on time spent with patients, and interference in treatment plans, referrals and selections of equipment or diagnostic tests. By unambiguously prohibiting controls over clinical decision-making, the bill provides regulators and dental practices with the necessary clarity to maintain professional integrity in dentistry. SB 351 fully preserves the ability to purchase or sell dental or other health care practices, while ensuring patient needs and dentists’ clinical judgment come first and that private equity interests are not influencing decisions about health care in pursuit of higher returns on investments.
SB 351 passed in the Senate and is now under consideration in the Assembly.
6. AB 350: Fluoride Varnish Coverage (CDA Co-Sponsored)
Tooth decay is one of the most common childhood health issues, yet it is largely preventable with early care. CDA is cosponsoring AB 350, authored by Asm. Mia Bonta (D-Oakland), to expand access to fluoride varnish treatments for children, ensuring they receive this critical preventive care in dental, primary care, community, and home-based settings.
Currently, fluoride treatments are covered for children and adults through Medi-Cal, but only when applied in specified settings. Many children, especially those in low-income communities, might more easily access these treatments in school-based programs or home visits by community health workers. By allowing fluoride varnish application to be applied under the direction of a Medi-Cal provider in a variety of additional settings and expanding coverage to all children under 21, AB 350 removes barriers to preventive dental care.
AB 350 will:
• Require health insurance plans and Medi-Cal to cover fluoride varnish application for children under 21.
• Expand Medi-Cal coverage for fluoride varnish treatments in a variety of settings, such as school-based programs and home visits.
• Direct the Medi-Cal Dental Program to establish clear billing and reimbursement policies so that providers can efficiently offer these treatments.
By making fluoride treatments more accessible, AB 350 helps protect children from cavities, reduces the need for costly dental procedures, and improves overall health outcomes.
AB 350 passed in the Assembly and is now under consideration in the Senate.
Updated July 8, 2025

YOU THE DENTIST, THE BUSINESS OWNER
Year-End Tax Moves for Dentists
Submitted by Brett LeMmon, CPA; Earned (SDDS Vendor Member)
As the year winds down, many dentists are focused on wrapping up patient care, hitting production goals, and juggling personal commitments before the holidays. But December is also a critical window to take proactive tax steps that can help you keep more of your hard-earned income — whether you own a practice or not. Here are 7 Earned strategies to consider before December 31:
1. Get Organized Early
Accurate records are the foundation of smart tax decisions. Waiting until January can lead to missed deductions and added stress.
• Reconcile bank, credit card, and loan accounts now.
• Gather receipts and invoices for deductible expenses.
• Review year-to-date pay stubs or payroll reports for accuracy.
Getting organized now means fewer headaches — and fewer missed opportunities — when it’s time to file.
2. Review Qualified Business Income (QBI) Deduction Eligibility
The recent “Big Beautiful Bill” extended provisions from the 2017 Tax Cuts and Jobs Act, including the Qualified Business Income Deduction (set to expire in 2026). This benefit gives practice owners and 1099 contractors a deduction equal to 20% of qualified business income.
For dentists, the deduction phases out once your taxable income reaches these limits:
• Single / Married Filing Separately
• Full deduction: ≤ $197,300
• Phase-out: $197,300–$247,300
• No deduction: > $247,300
• Married Filing Jointly
• Full deduction: ≤ $394,600
• Phase-out: $394,600–$494,600
• No deduction: > $494,600
If you’re near or above these thresholds, consider strategies like depreciation write-offs or retirement plan contributions to reduce taxable income and maintain eligibility.
3. Prepay Pass-Through Entity Tax (PTE)
California’s PTE tax deduction remains available under the new bill. If your practice is an S Corp or partnership and you elected to pay PTE tax by making your initial installment by June 15, 2025, you can prepay the remaining estimated amount before 12/31.
Doing so allows you to take the deduction for 2025 rather than waiting until next year — improving cash flow and lowering currentyear taxes.
4. Make Smart Year-End Purchases
For practice owners, equipment or technology placed in service by December 31 may qualify for Section 179 deductions or bonus depreciation. The new tax bill restores bonus depreciation to 100% for 2025.
If purchasing practice real estate or starting a buildout, consider a cost segregation study to accelerate depreciation.
For associates, deductible year-end investments might include replacing worn-out instruments, upgrading professional tools, or prepaying continuing education before January.
5. EV and Solar Credit Planning
If you’re considering an electric vehicle or solar installation, timing is critical:
YOU ARE A DENTIST. You’ve been to school, taken your Boards and settled into practice. End of story?
Not quite. Are you up to speed on tax laws, potential deductions and other important business issues?
In this monthly column, we will offer information pertinent to you, the dentist as the business owner.
• EV Tax Credits for new and used vehicles expire September 30, 2025. To qualify, the vehicle must be purchased and in service by that date.
• Income limits: $150,000 (single) / $300,000 (MFJ)
• Leased EVs are exempt from income limits, and dealerships often pass along the credit.
• Residential Clean Energy Credit (Section 25D) for solar and eligible battery systems ends December 31, 2025. Installation must be complete by midnight to qualify.
6. Prepare for Tax Forms and Reporting
• Practice Owners: Ensure you have W-9s for any contractors paid $600+ to simplify issuing 1099s in January.
• Associates: Confirm you’ll receive all necessary W-2s and 1099s from employers and other sources
7. Request a Year-End Tax Projection
A projection from your CPA — based on current income and deductions — can help you:
• Avoid underpayment penalties
• Identify last-minute adjustments
• Plan cash flow for April tax payments
Bottom line: Whether you’re running a practice or focusing on clinical work, year-end tax preparation is about getting organized, capturing every eligible deduction, and making intentional moves before December 31. A little effort now can mean lower stress, fewer surprises, and more control over your tax outcome when filing season arrives.
You’ve Earned It!
Professional Practice Sales of The Great West Your Trusted Advisor
PPS monetized dental practices when we pioneered this activity in 1966
Experience
PPS has faithfully served the members of the Sacramento District Dental Society since 1966 per their interest in entrusting their practices to the next caretaker. During this time, we have successfully concluded the sale of thousands of dental practices in California. We know the process from that first phone call to the closed escrow.
Customer Service
PPS incorporates a very strong risk management application in every engagement. This is paramount when in essence you are selling blue sky referred to as “goodwill.” You require this assurance that everything was done to cover your “assets!”
PPS’ Intangibles
We are phenomenal coaches throughout the entire process. When necessary, we put on our therapist hat as these journeys can be emotional. We are expert at controlling the entire process which includes getting a practice (and its owner) properly prepped prior to being placed “For Sale.” Once the “For Sale” door is opened, we manage the journey!
Why Choose Us

We have no interest in having an extensive inventory where many opportunities get little attention. It takes an enormous amount of time and focus to get this right and conclude an engagement. We are very selective regarding the practices we take on. We do not outsource valuations to third parties who will never set foot in your office. We are not a Fortune 500 company, a franchise, career changing bankers or previous dental reps. This is all we have ever done! We adhere to full disclosure on each listing. We know where to look, the questions to ask and the information to gather. When we take a practice to market, we have a complete toolbox! There are no surprises and we can immediately respond to inquiring parties and their advisors.
“
It was my time to step down. After talking to Ray and Edna, I knew they were best suited to handle this change. I received multiple offers. I am very pleased with how everything was handled.
- Bill Iliff, DDS; Sacramento
We graduated together, started practicing together and decided to retire together. We had two very busy practices. Ray got the job done including the sale of our large building!
- Steven Holm, DDS and Stacey Holm, DDS; Roseville & Auburn
Wanting to retire, I contacted PPS last year. Ray reviewed my data and made suggestions to best position my practice. Suggestions made and the practice was placed For Sale. I received multiple Offers. Practice and condo sold.
- Terri Speed, DDS; Elk Grove
“
Mid-Year Membership Engagement Update: Building Community, One Event at a Time
As we move into the latter half of 2025, the Sacramento District Dental Society’s Membership Engagement Committee is proud to share an update on our progress, priorities, and exciting opportunities still ahead. With a continued focus on recruitment, inclusivity, member satisfaction, and engagement, our mission remains clear: to help every SDDS member feel seen, supported, and truly part of our local dental family.
This year has been marked by meaningful action and genuine connection. The committee has worked diligently to organize events that foster community while keeping the unique needs of our members front and center. Whether you’re a new graduate, a seasoned practitioner, or somewhere in between, we want you to feel that SDDS is your professional home!
Our member mixers have proven to be a cornerstone of that effort. These informal, welcoming events provide the space to build

relationships beyond the clinical setting. Our member mixers at Centro and ZocaloRoseville were a great success! We enjoyed the energy and new faces that reflected the strength of our growing membership. We’re already looking ahead to the fall: the October 16, 2025 member mixer at Zocalo in Folsom. This will be another fantastic evening of food, drinks, and conversation.

Family-friendly events have also played a vital role in engaging our members and their loved ones. The June outing to the River Cats game is a yearly highlight. What a great evening filled with sunshine, baseball, and community spirit. It was exciting to see so many SDDS families relaxing together and enjoying America’s pastime from the comfort of our group section. Not to mention the thrilling finish with a walk off homerun for the River Cats to win the game!
Similarly, our summer Ice Cream Social was another sweet success, bringing together members of all ages for an evening

By Jeffrey Delgadillo, DDS 2025 Membership/Engagement Committee Co-Chair
of treats and connection. It was nice to bring our community together under our very own roof. We are excited for a new growing tradition to keep cool during the Summer months.
Looking ahead, the second half of the year is full of opportunities to get involved. The beloved Polar Express event returns this winter, offering a festive experience for families to kick off the holiday season. And of course, our Annual Holiday Party is just around the corner—always a highlight and a wonderful way to close out the year with colleagues and friends.
In addition to social events, we encourage all members to take advantage of the continuing education programs offered through SDDS. These courses provide not only valuable CE units, but also a chance to learn alongside peers and stay up to date with the latest in clinical practice and dental leadership.
If you’ve been inspired by the events and energy of this year, we invite you to take the next step: consider joining the Membership Engagement Committee in 2026. It’s a rewarding opportunity to help shape the member experience and give back to the dental community that supports us all.
Thank you for being part of what makes the Sacramento dental community so special. Here’s to an exciting second half of the year— we hope to see you at the next event!
Member MIXERS
OCTOBER 16 - Zocalo, Folsom
Join your fellow SDDS Members for a fantastic evening of networking, laughter, and great company at SDDS’ Member Mixer! Whether you’re looking to make new connections or catch up with familiar faces, this is the perfect opportunity to relax and enjoy a casual NON-CE atmosphere. Don’t miss out!
$20 if registered by 10/1/25
Co-sponsored by MUN CPAs and Dental & Medical Counsel PC THURSDAY, 6:00-7:30pm
Visit sdds.org for more details


What We Do
We provide reliable dental hiring solutions for practices across Northern California. Whether you need temporary coverage or are hiring for a permanent role, we specialize in placing experienced front-office and back-office professionals, including DAs, RDAs, RDHs, and administrative staff.
With over 20 years of industry experience, we understand the fast pace and evolving needs of dental offices. Our goal is to help you stay fully staffed and focused on delivering exceptional patient care.

Dental Day with the River Cats EVENT HIGHLIGHTS










We had a blast at the River Cats game last week. A special highlight—our very own President, Dr. Aflatooni, kicked things off by throwing out the first pitch! It was great to see so many familiar faces return and to welcome all our first-time attendees—thank you for making it such a memorable day!
TICKETS FOR FAMILY, TEAMS & FRIENDS
1,971
TOTAL NEW MEMBERS FOR 2025: 77 TOTAL MEMBERSHIP (as of 8/7/25)
New Members
Nazanin Abdehoo, DMD
General Practice
• New Grad from California Northstate University
Zahraa Abdulabbas, DMD
General Practice
• New Grad from California Northstate University
MARKET SHARE: 78.5%
RETENTION RATE: 94%
ENGAGEMENT RATE: 79% active / 58% retired
TOTAL ACTIVE MEMBERS: 1,380
TOTAL RETIRED MEMBERS: 359
TOTAL DUAL MEMBERS: 10
TOTAL AFFILIATE MEMBERS: 1
TOTAL STUDENT MEMBERS: 218
TOTAL CURRENT APPLICANTS: 2
TOTAL DHP MEMBERS: 55
Alejandro Albarran Montoya, DDS
General Practice
• New Grad from UOP Arthur A. Dugoni School of Dentistry
Ranna Alrabadi, DMD
General Practice
• New Grad from California Northstate University
• Practices at The Art of Dentistry in Roseville and Monica Crooks, DDS in Sacramento
Antonina Borisov, DMD
General Practice
• New Grad from California Northstate University
Nandini Braganza, DDS – Transfer
General Practice
• UCLA School of Dentistry in 2024
Nathan Chan, DMD
General Practice
• New Grad from California Northstate University
Owen Chen, DMD
General Practice
• New Grad from California Northstate University
Devan Cruz, DMD
General Practice
• New Grad from University of Colorado
Joseph Danna, DDS
General Practice
• Graduated Nicolae Testemițanu State University of Medicine and Pharmacy, Moldova in 2022
Tai Dang, DMD
General Practice
• New Grad from California Northstate University
Allison Dietze, DDS – Transfer
General Practice
• USC Herman Ostrow School of Dentistry in 2021
Sukhpreet Dosanjh, DMD
General Practice
• New Grad from California Northstate University
Bridget Faltas, DDS
Periodontics
• Touro College of Dental Medicine at NYMC in 2022
• University of Kentucky in 2025 for Periodontics school
• Practices at Clifton Nakatani, DDS in Sacramento
Rakan Fawakhiri, DMD
General Practice
• New Grad from California Northstate University
Aidan Flynn, DDS
General Practice
• New Grad from UOP Arthur A. Dugoni School of Dentistry
Samantha Gallia, DDS
Oral Radiology
• UOP Arthur A. Dugoni School of Dentistry in 2022
• Washington University in 2024 for Oral Radiology specialty
Athens Graves, DMD
General Practice
• New Grad from Arizona Midwestern University
Jalmeen Jhaj, DMD
General Practice
• New Grad from California Northstate University
Simranjit Kaur, DMD
General Practice
• New Grad from California Northstate University
Aleena Khan, DMD
General Practice
• New Grad from California Northstate University
Eliana Kim, DDS
General Practice
• New Grad from USC Herman Ostrow School of Dentistry
Conrad Lemon, DMD
General Practice
• New Grad from California Northstate University
Youssef Mahmoud, DDS
General Practice
• New Grad from UOP Arthur A. Dugoni School of Dentistry
Mahgol Mehranpour, DMD
General Practice
• New Grad from California Northstate University
Wisam Morrar, DDS
General Practice
• New Grad from USC Herman Ostrow School of Dentistry
Jaskiran Nat, DMD
General Practice
• New Grad from California Northstate University
Ryan Ngo, DMD
General Practice
• New Grad from California Northstate University
Tanjeet Nijjar, DDS
General Practice
• New Grad from USC Herman Ostrow School of Dentistry
Sang Park, DMD
General Practice
• New Grad from California Northstate University
Harshini Paruchuru, DDS
General Practice
• New Grad from UOP Arthur A. Dugoni School of Dentistry
Jordan Phen, DDS
General Practice
• New Grad from UCLA School of Dentistry
Mary Quilici, DDS
General Practice
• New Grad from UOP Arthur A. Dugoni School of Dentistry
Namrata Rana, BDS – Transfer
Pediatric Dentistry
• International School in 2017
• University of Alabama in 2023 for specialty of Pediatric Dentistry
Jasraj Sandhu, DMD
General Practice
• New Grad from California Northstate University
• Practices at Arden Oaks Dental Care in Sacramento
Ali Shahcheraghi, DMD
General Practice
• New Grad from California Northstate University
Elaha Shaur, DDS
General Practice
• New Grad from UCSF School of Dentistry
Navdit Sidhu, DMD
General Practice
• New Grad from California Northstate University
Justin Sue, DMD
General Practice
• New Grad from California Northstate University
• Post Grad Student at University of Nebraska Medical Center
Bohkyeong Suh, DMD
General Practice
• New Grad from California Northstate University
Allison Suzuki, DDS
General Practice
• New Grad from UCLA School of Dentistry
Dara Taghvaei Sourouei, DMD
General Practice
• New Grad from California Northstate University
Kevin Tang, DMD
General Practice
• New Grad from California Northstate University
Dianne Torres, DDS
General Practice
• New Grad from Loma Linda University
Dan Truong, DDS – Transfer
General Practice
• New York College of Dentistry in 2017
Adam Wong, DDS
General Practice
• New Grad from UCLA School of Dentistry
In Memoriam
Dr. Premjeet Brar
Dr. Premjeet Brar passed away suddenly from a car accident on July 11, 2025. She graduated from dental school in 2012 at New York College of Dentistry. She then went on to specialty school in 2018 at Howard University, where she earned her specialty degree in Pediatric Dentistry.
Dr. Brar was an active member of SDDS since 2020 and a devoted pediatric dentist in Rocklin. Tragically, she and her husband passed away in the accident on July 11. They are survived by two young children who now face a long and difficult path ahead.
A fundraiser has been organized by a trusted friend and family member to help support the children and provide for their needs during this incredibly challenging time.
www.gofundme.com/f/aid-puneet-andveenus-4yr-and-8yr-olds

Dr. Roger Kingston
Dr. Roger Kingston passed away on July 12, 2025. He graduated from dental school in 1971 from UCLA School of Dentistry. He then went on to earn his specialty degree in Oral and Maxillofacial Surgery from UCLA Medical Center in 1975. He was a member for 13 years.
Dr. Robert Shimada
Dr. Robert Shimada passed away February 9, 2025. He graduated from dental school in 1959 from UCSF School of Dentistry and was a member for over 65 years.
We’re Blowingyour horn! Congratulations to...
Dr. Estella Kim welcomed baby Noah Riley Kim to their family. (1)
Dr. Jeff Sue was on Fox40, July 22, for a TV segment all about keeping those smiles shining bright! Watch it at www.sdds.org/resource/hotnews/ (2)
Dr. Viren Patel is a first-time grandpa – Luka Davis Schimchak, born 7/4/2025, 8:17am, 7 lbs, 1 oz, 19 inches.
#
CNU class of 2029 Orientation, Caroll (SDDS) and Medelyn (CDA). (4)
CNU’s Inaugural class of 2025 for graduating in May! (5)
UOP’s IDS class of 2027, they had orientation in June







Have you heard of the Dedicated Monthly Dentist (DMD) Program?
By enrolling in the Dedicated Monthly Dentist (DMD) Program, you can …
Prepay for all 7 and Save … on the General Membership Meetings for 2025–2026 with one check or credit card charge
Easily Register for Each Meeting … by responding to a simple email sent to you each month.
Help with SDDS recruitment!
If you are unable to attend a particular meeting, call SDDS and we’ll arrange for a new member to attend in your place.
Sign up with the enclosed insert and attend these great General Meetings!
SEPTEMBER 9, 2025 3 CEU, Core
Does CR Matter?
Paul Binon, DDS, MSD, Bryan Judd, DDS and Peter Worth, DDS
OCTOBER 14, 2025 3 CEU, Core
Working Together to Improve Oral Health in California
Shakalpi Pendurkar, DDS, MPH, State Dental Director
NOVEMBER 11, 2025 3 CEU, Core
Tooth Be Told! Drilling Down on Office-based Anesthesia
Samuel Seiden, MD, FAAP
JANUARY 13, 2026 3 CEU, Core 15 on 15: Multi-Topic Pearls – Technology in Dentistry (15 Minutes, 15 Slides, 5 Speakers/Topics) SDDS Member Speakers TBA
MARCH 10, 2026 3 CEU, Core Mental Health & Wellness
Eric Johnson, DDS
Sponsored by Heise, Alpha and Delgadillo OMS
APRIL 14, 2026 3 CEU, Core Non-Odontogenic Tooth Pain
Mohd Khalaf, DDS
MAY 12, 2026 3 CEU, Core
$589 FOR ALL 7 MEETINGS!
Drugs, Bugs and Dental Products, What to Prescribe!
Peter Jacobsen, DDS
Sponsored by Capitol Periodontal Group
Banking to build your legacy
Take control of your future as a dental practice owner with our comprehensive suite of financial products.
• Acquisition
• Startup
• Equipment
• Refinance
• SBA loans
• Jumpstart Plus
• Commercial real estate
• Tenant improvements
• Ground-up construction
• Equity Cash-out
• Provide Card®
• Banking


Christine Carvalho
Regional Director of Practice Finance 408-981-2524 christine.carvalho@getprovide.com
Jason Schneller
Senior Regional Director of Practice Finance 818-561-8106 jason.schneller@getprovide.com
© 2025 Fifth Third Bank, National Association. All Rights Reserved.
Provide is a division of Fifth Third Bank, National Association. Member FDIC. All lending is subject to credit review and approval.


Vendor Member SPOTLIGHT
Based in Folsom, CA, Emergency Dental Kit: Meds 2U Pharmacy specializes in providing dental offices the essentials needed for your offices emergency dental situations. We offer affordable and customizable emergency dental kit options. We can save you the hassle of worrying about expiration dates and auto-replenish items in your emergency dental kit. Benefits, Services, Special Pricing and/or Discounts Extended to SDDS Members: Emergency Dental Kits starting at $269.99
ph: (916) 221-7789 www.meds2urx.com/emergency-dental-kit
William Huynh william@meds2urx.com
LIBERTY Dental Plan (LIBERTY) is a California-based dental plan, founded and run by a dentist, and a leadership team offering a combined 300 years of dental and healthcare industry experience. LIBERTY is one of the nation’s fastest growing dental plans and we now administer dental benefits to over 4.5 million members nationwide on behalf of states, health plans, and commercial clients. We have almost 20 years of experience administering dental benefits in California and as one of the Dental Geographic Managed Care plans in Sacramento County, we are proud to make our members shine one smile at a time. ph: (800) 268-9012 | www.libertydentalplan.com
Gisel Simington, Provider Relations Manager (949) 246-9482 | gsimington@libertydentalplan.com

Neo Dental Laboratory is a Mid-Sized full service crown and bridge lab specializing in dental Implants and digital work flow. We are committed to delivering consistent quality and service at a fair price.
Benefits, Services, Special Pricing and/or Discounts Extended to SDDS Members: Neo offers discount vouchers to new accounts, and quarterly promotions for all SDDS members. Please contact Frank Sanchez for more information and send your first case today.
ph: (916) 271-7536 | neodentallab.com
Frank Sanchez
franksanchez@neodentallab.com

Global leader in implant, restorative and regenerative dentistry. Implant, Restorative, and Regenerative products for both conventional and digital workflows. Contact Todd Allington for current specials.
ph: (800) 448-8168
www.straumann.com/group/en/home/customers-and-solutions/professional-dentistry.html
Todd Allington (916) 508-9218 | todd.allington@straumann.com

Analgesic Services, Inc. offers comprehensive and prompt medical gas services, from installation and system upgrades to reliable deliveries and repairs. For over thirty years, we have been Sacramento’s only full service medical gas provider who guarantees unparalleled technical experience, unequalled product quality and unrivaled customer service.
Benefits, Services, Special Pricing and/or Discounts Extended to SDDS Members: SDDS members using Analgesic Services, Inc. as their medical gas provider receive highest priority service response, loaner equipment (if repairs are needed), product and labor discounts, all from a team of dedicated medical gas professionals.
ph: (916) 928-1068 | www.asimedical.com
Ron Andres info@asimedical.com

SD Dental Solutions is the leading IT and Dental Billing company in the Sacramento area. We specialize in dental billing services such as Insurance aging, patient accounting and AR services, insurance eligibility and verification, and even practice sales and transitions. Our dynamic and experienced IT services offer a full suite of IT support, malware protection, network services and consulting.
Benefits, Services, Special Pricing and/or Discounts Extended to SDDS Members: Please call us today for a free practice evaluation and discover what SD Dental Solutions can do for you and your practice!
ph: (916) 367-4244 | sddentalsolutions.com
Dennis Krohn Jr., President/Partner dennis@sdreliance.com
We strive to be your single source for all your dental office needs and to provide you with the best customer experience and personalized service available.
ph: (800) 736-4688 | www.pattersondental.com
Cara Montoya Operations Manager ph: (916) 780-5129
cara.montoya@pattersondental.com
We provide service and maintenance of all types of dental equipment, but our scope of work also includes: new equipment sales, office design and construction, relocations and remodels. The equipment we service ranges from handpieces to digital x-ray and everything in between. Being a family owned business allows us the flexibility to personalize our sales and service to your needs. Our integrity and professionalism is what you remember of us and we never forget we are working for you.
ph: (916) 259-2838 www.descodentalequipment.com
Tony Vigil tony.desco@gmail.com
916.928.1068

Meds 2U Pharmacy: Emergency Dental Kit
William Huynh, Pharm D 916.221.7789 www.meds2urx.com/emergency-dental-kit
Jordyn Levitas 646.741.4816 torchdental.com/

Cara
Sarah
Regional General Manager 925.499.2919 henryschein.com

Todd Allington 916.508.9218 straumanngroup.us

Yaeger Dental Supply Inc.
Tim Yaeger 650.593.5100 yaeger.dentist

916.918.5752 ddsmatch.com

Amin Amirkhizi,
877.311.7373 supplydoc.com

Dr.

Jay Harter 916.812.0500 henryscheindpt.com







Wendie
916.993.4182 nwstaffing.com


CJ
614.560.5417
Forrest Wiederman
949.910.3343
bofa.com/practicesolutions

Brett
925.939.2500

Ashlee
866.232.7640
adamsdentalconsulting.com


Clint
Chris Llamas
916.317.6803
myavesis.com/access-dental/





Keith
Kim





Advertiser INDEX
Dental Supplies, Equipment, Repair
Analgesic Services Inc. 43, 44
Desco Dental Equipment. 43, 44
Henry Schein Dental. 44
LumaDent Inc. 44
Meds 2U Pharmacy 43, 44
Patterson Dental. 43, 44
Job Bank
The SDDS Job Bank is a service offered only to SDDS Members. It is for job seekers to reach other Society members who are looking for dentists to round out their practice, and vice versa. If you are a job seeker or associate seeker contact SDDS at (916) 446-1227 or by email at sdds@sdds.org, we can also provide contact information for the members listed below.
ASSOCIATE POSITIONS AVAILABLE
Sukhjeet Kaur, DDS • Jackson • FT/PT • GP
Amy Kiesselbach, DDS • Rocklin • PT • GP
Nahid Afshari, DDS • Fair Oaks • PT • GP
Dan Gustavson, DDS • Auburn • PT • GP
Gautam Dogra, DDS • Sacramento • PT/FT • GP
Harkeet Sappal, DDS • Sacramento • PT • Endo
Mugunth Nandagopal, DDS • Sacramento • FT/PT • GP
Andrea Cervantes, DDS • Elk Grove • PT • GP
Sean Roth, DDS • Folsom • FT • GP
Peter Kim, DDS • Sacramento • PT • GP
Hossein Kazemi, DDS • Roseville • PT/FT • GP/Perio
Arash Aghakhani, DDS • Sacramento • FT/PT • GP
Darryl Azouz, DDS • Lake Tahoe • FT/PT • GP
Oleg Oliferuk, DDS • Folsom • PT • GP
Siamak Okhovat, DDS • Roseville • PT/FT • GP
Monica Tavallaei, DDS • Sacramento • PT/FT • GP/PEDO
Sabrina Jang, DDS • Sacramento • PT/FT • GP
Albert Lee, DDS • Sacramento • PT • GP
Amandeep Behniwal, DDS • Roseville • PT/FT • GP
Elizabeth Johnson, DDS • Wellspace - various locations • FT/PT/Fill-In • GP
Amy Woo, DDS • Sacramento • PT 1 Day • Endo
David Park, DDS • several/multiple positions • FT/PT • GP
DOCS SEEKING EMPLOYMENT
Linda Zhu, DDS • open • PT • GP
Sara Baig (graduated NYU May 2025) • FT/PT • GP
Harshini Paruchuru (graduated UOP May 2025) • FT/PT • GP
Navneet Sehgal, DDS • FT • GP
Gaetan Tchamba, DDS • PT/locum tenans • GP
Classified Ads
Join Make A Smile Dental! We’re hiring dental assistants, hygienists, and general/specialty dentists. Competitive pay and a supportive team environment. Send your resume to resume@ makeasmile.com today! 11-12/24
Are you ready to take your career to the next level? We’re thrilled to invite you to apply to join one of Sacramento’s most respected and wellestablished private endodontic practices: Midtown Endodontics. Known for our exceptional patient care and commitment to quality, we are backed by a network of top-tier referring dentists who trust us to deliver outstanding results. Call (916) 446-6143 if interested. 5-6/25
ENDODONTIST: Seeking a Endodontist to join our professional dental team. We have been serving Sacramento for over 25 years and Voted Top Dentist by Sacramento Magazine. If you like to experience the many facets of dentistry, our practice consists of general, periodontist, endodontist, and orthodontist this practice is for you. For more information about us, please visit DrAmyWoo.com. 1-2/24
Kids Care Dental & Orthodontics seeks doctors to join our teams in the greater Sacramento and greater Stockton areas. We believe when kids grow up enjoying the dentist, healthy teeth and gums will follow. As the key drivers of our mission—to give every kid a healthy smile— our dentists, orthodontists and oral surgeons exhibit a genuine love of children and teeth. A good fit for our culture means you are also honest, playful, lighthearted, approachable, hardworking, and compassionate. Patients love us... come find out why! Send your CV to drtalent@kidscaredental.com. 6-7/17
WELLSPACE HEALTH
ORGANIZATION
(an FQHC) is taking applications for fill-in/part-time/ full-time dentists. Send your resume/CV to eljohnson@wellspacehealth.org. 1/15
Kids Care Dental & Orthodontics seeks orthodontists to join our teams in the greater Sacramento and greater Stockton areas. We believe when kids grow up enjoying the dentist, healthy teeth and gums will follow. As the key drivers of our mission—to give every kid a healthy smile—our dentists, orthodontists and oral surgeons exhibit a genuine love of children and teeth. A good fit for our culture means you are also honest, playful, lighthearted, approachable, hardworking, and compassionate. Patients love us... come find out why! Send your CV to drtalent@kidscaredental.com. 6-7/17
Price Reduced $729,000 Madison Avenue Dental Office for sale; Roseville New Construction/ Sacramento Dental/Orthodontic Offices for Lease; Ranga Pathak, Broker Associate, RE/MAX Gold, DRE01364897; Tel: (916) 201-9247; Email: ranga. pathak@norcalgold.com. 8-9/21
SACRAMENTO DENTAL COMPLEX has one 3 unit suite which is equipped for immediate occupancy. Two other suites total 1630 sq. ft which can be remodeled to your personal office design with generous tenant improvements. 2525 K Street. Please call for details: (916) 539-1516. 10/11
PRACTICE AND EQUIPMENT FOR SALE/LEASE Dental Office Condo for sale or lease. One story prime location corner opposite Kaiser Hospital. 2,743 square feet of NRA located at 1603 Eureka Rd., Roseville. Six operatories with equipment. Call (916) 797-7436 for details. 9-10/25c
Practice for sale in Mt. Shasta, CA. Refers out most endo, 3rds, ortho, some implants. FFS/ no insurance contracts, very busy and well known in the community. High visibility location in town, shares building with medical practice, real estate is also available. OpenDental, XDR, Sirona CBCT, Ergonomic Products delivery systems. 7-digit production and collections on 4d/week. Great schools and community, live where others vacation. Contact practice owner at 530-925-5900. 9-10/25
NEW Online “This Week” Classified Advertising for SDDS Members/Vendor Members only
SDDS’ weekly “This Week at SDDS” eblast reaches our entire membership every Sunday at 8:00am, with a circulation of 2,200 and an impressive open rate of 67% – contract due by noon on the Wednesday prior to the Sunday e-blast.
Guidelines for Online Classified Advertising:
• Members must place and pay for the ad themselves
• Non-Vendor Member companies and representatives cannot be listed in the ad
• Contact info in the ad must be direct to member/member’s office, non-member emails and phone numbers are prohibited
Visit www.sdds.org/publications-media/advertise/ to advertise
Selling your practice? Need an associate? Have office space to lease? SDDS member dentists get one complimentary, professionally related classified ad per year (30 word maximum). For more information on placing a classified ad, please call the SDDS office at 916.446.1227 or visit www.sdds.org/publications-media/advertise/
2035 Hurley Way, Suite 200 • Sacramento, CA 95825
916.446.1211 • www.sdds.org
ADDRESS SERVICE REQUESTED
SDDS CALENDAR OF EVENTS
SEPTEMBER
9 General Membership CE Meeting Throwdown - Does CR Matter?
Paul Binon, DDS, MSD; Bryan Judd, DDS and Peter Worth, DDS
12 SDDS 14th Annual Shred Day SDDS Office • 10am-2pm
17 Navigating Year-End Planning and New Tax Regulations
Brett LeMmon, CPA, MA; Earned Wednesday • 6:30–8:30pm
OCTOBER
2 Dentists Do Broadway & Juliet
8 Next Level Leadership Reception SDDS Office • 6pm
14 General Membership CE Meeting The California Oral Health Plan: Partnering for Success
Shakalpi Pendurkar, DDS, MPH, State Dental Director
22 DIY Study Club – Bring Your Case!
29 Licensure Renewal Webinar
Responsibilities and Requirements of Prescribing Schedule II Opioids Ronni Brown, DDS, MPH, FADI Wednesday • 5:30–7:30pm • 2 CEU, Core