INSPIRE heads to Regional, Rural, Remote and Very Remote Australia.
There is no reason why people living in Regional, Rural, Remote or very Remote (RRRvR) communities shouldn’t have the same health outcomes as those in metropolitan areas. However, this remains one of Australia’s most pressing challenges.
The dedicated, incredible work that health and medical researchers and innovators do to address this challenge is worthy of elevating, and this is why we’ve decided to revisit this theme for INSPIRE three years on. While it’s not all sorted and solved, there is some good news!
RRRvR communities are characteristically tightknit with deep connections to the land, which fosters a distinctive sense of belonging and resilience. However, RRRvR communities face unique barriers to healthcare: lack of available services, long distances, workforce shortages, and higher costs. These challenges contribute to higher burdens of chronic disease, poorer mental health outcomes and preventable deaths. More broadly, Australians living in RRRvR communities are navigating an unprecedented period of change driven by an ageing population, economic uncertainty and rising climate risks.
Despite the challenges, RRRvR communities offer valuable lessons for Australia’s health and medical research and innovation landscape — from strong community partnerships to adaptive workforce models and culturally responsive services. Investing in RRRvR health and medical research and innovation isn’t just a way to improve health outcomes; it also enriches local economies and our overall national research capability.
RRRvR health and medical research and innovation is fundamental to addressing the diverse systemic issues to equitable health outcomes – whether its digital health, regional clinical trials, or supporting remote cancer patients - all require more than goodwill and passion. It demands sustained investment, innovation and collaboration. This issue of INSPIRE highlights the inspiring work being done to improve healthcare access and outcomes for Australians in RRRvR communities, and to showcase their research and innovation excellence.
In this edition you’ll read about a semitrailer converted into a mobile lung cancer screening platform bringing biomarker testing to rural and Indigenous communities; a digital care model that monitors inflammatory bowel disease; and a homebased hearthealth kit. We also feature community paramedics delivering primary care, telehealth specialists helping clinicians in the bush, and assistive
technologies for people with acquired brain injuries. Other articles explore genomic research into unexplained kidney disease, AI driven mental health interventions and teledentistry projects tackling childhood tooth decay. Each project is grounded in partnership, from researchers and local health workers to industry and communities.
What ties these stories together is a shared commitment to equity and a belief that geography should not determine health outcomes. Through these articles you will see how data and digital tools can complement on country care, how community led approaches can amplify impact, and how a focus on prevention and early intervention can ease the burden of chronic disease. Collectively, they remind us that improving health in regional, rural and remote Australia is not just a moral imperative but a practical strategy to learn what works in different settings, lift productivity and strengthen communities.
Research Australia is working closely with the Chair of the National Health and Medical Research Strategy and we wanted to make sure that RRRvR communities are firmly represented in this national direction for our country’s culture.
There is more on this topic from our latest University Roundtable, hosted by Charles Sturt University, and our recent Health Economics Symposium on the theme “Building a Sustainable Health Economics and Health Services Research Sector”. Both events highlighted the importance of investing in RRRvR research and health services.
We are grateful to all the researchers, clinicians, community leaders and participants who have contributed their knowledge, their stories and their time to this collection. Their efforts are paving the way for a healthier future for all Australians. We hope this publication sparks conversations, inspires new collaborations and reinforces the importance of investing in rural and remote health and medical research. Together, we can ensure that every Australian, no matter where they live, has the opportunity to lead a healthy and fulfilling life.
Best wishes
Nadia and your Research Australia Team

ADVISORY SERVICES
Research Australia has provided specialist consulting and advisory services for many years. Our consultancy services continue to expand each year, driven by our unique expertise, reputation for high quality work, and strong relationships to drive outcomes and influence system change.
Most recently we have worked with state and federal governments, patient groups, industry, hospitals, and aged care. Some of the consulting services Research Australia provides are:
Market scanning – detailed analysis of who is undertaking what research to inform project planning and ensure projects target the right health and medical research stakeholders.
Policy advice – on the funding streams, government policy landscape and political interests that impact your projects’ success.

Sector consultation – facilitating engagement with the health and medical research community and the consumers who can best inform approaches to health and medical research.
Grants guidance – evaluating and reviewing grants opportunities and funding programs. m +61 2 9295 8546
k admin@researchaustralia.org

Australian Health & Medical Research & Innovation












Publisher Research Australia Ltd
Art Direction Matthew Ware p +61 403 844 763 e matt@objktive.com
For Advertising enquiries please contact the Research Australia office on p 02 9295 8546 or e admin@researchaustralia.org researchaustralia.org
INSPIRE ONLINE issuu.com/researchaustralia
INSPIRE is a publication of Research Australia Ltd ABN 28 095 324 379 384 Victoria Street Darlinghurst NSW 2010
Who can submit articles?
Any current member of Research Australia who would like to share a relevant story that affects their organisation including, philanthropic donations and their outcomes, research findings, and any other related health and medical research topic that affects the Australian population.
Submission guidelines & deadlines For information regarding how to submit and publishing deadlines visit the Research Australia website
Disclaimer
The opinions expressed in INSPIRE do not necessarily represent the views of Research Australia. Whilst every effort has been made to ensure accuracy, no responsibility can be accepted by Research Australia for omissions, typographical or inaccuracies that may have taken place after publication. All rights reserved.
The editorial material published in INSPIRE is copyright. No part of the editorial contents may be reproduced or copied in any form without the prior permission from Research Australia. © Research Australia 2025.

CHRISTOPHE KEREBEL
My Twitter : @chriskere CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
My Twitter : @chriskere
LA TROBE UNIVERSITY
Australian Health & Medical Research & Innovation CONTENTS

38 New Heart Health Check Kit Brings Lifesaving Screening to Rural Communities
LA TROBE UNIVERSITY

48
“I don’t think I’m hearing things”
CENTRAL QUEENSLAND UNIVERSITY

50
Restacking the Odds for children and families
MURDOCH CHILDREN’S RESEARCH INSTITUTE

40 Research, Discovery, Translation and Kidney Failure JAMES COOK UNIVERSITY

44
Innovative musculoskeletal program heads to the Australian bush
UNIVERSITY



Closing the Rural Care Gap

Strengthening cancer care in rural and remote australia through partnerships and innovation
DEAKIN UNIVERSITY

The National Health and Medical Research Strategy
DEPARTMENT OF HEALTH, DISABILITY AND AGEING


Bolstering regional, rural, remote and very remote health and medical research and innovation


CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CROHN’S COLITIS CURE
EVENTS OVERVIEW
UNIVERSITY ROUNDTABLE
On 3 July 2025 Research Australia and Charles Sturt University hosted a University Roundtable in Orange, NSW. 53 representatives from 32 universities attended the meeting. Chaired by Board Director Professor Russell Gruen, the session focused on elevating the national conversation about health and medical research and innovation in regional, rural, remote and very remote communities. Professor Jenny May AM, the National Rural Health Commissioner, spoke about the challenges and opportunities facing researchers outside metropolitan centres, highlighting the need for long-term funding and workforce development as well as the strengths of community connectivity and integrated models of care. Ms Rosemary Huxtable AO PSM, chair of the National Health and Medical Research Strategy, acknowledged the unique needs of these communities and outlined next steps for the Strategy’s development.
A draft discussion paper, ‘Advancing Health and Medical Research and Innovation Across Regional, Rural, Remote and Very Remote Communities in Australia’, was tabled for discussion. Participants emphasised the importance
of co-design and local priority setting but noted ongoing systemic challenges in workforce, funding and infrastructure, particularly for leadership roles, and early- and mid- career clinician researchers. Following the Roundtable we hosted a virtual showcase of regional health and medical research and innovation in partnership with Charles Sturt University.

A LONG-TERM STRATEGIC GUIDANCE OF AUSTRALIA’S DIGITAL AND DATA INFRASTRUCTURE
Research Australia and the Digital Health CRC co-hosted a virtual workshop with 25 representatives from 18 organisations across government, academia and industry to explore how a coordinated national approach to health and medical data could strengthen data driven healthcare, research and innovation. Facilitated by Research Australia's Dr Talia Avrahamzon and introduced by Adjunct Professor Annette Schmiede, CEO of the Digital
Health CRC, the session considered how a unified data capability could be structured, where it should sit, and how it might align with current reforms such as the National Health and Medical Research Strategy, the Strategic Examination of R&D and the National Research Infrastructure Roadmap. Speakers from these initiatives highlighted gaps in leadership, fragmentation, barriers to access and the need for person centred infrastructure. Participants
agreed that no single entity can address these challenges and called for a bipartisan national framework with sustainable investment, clear governance, inclusive stewardship and ethical, community driven data practices. Research Australia, the Digital Health CRC and their partners committed to pursuing this opportunity to unlock the full value of health data for Australia’s health and economic prosperity.
University Roundtable participants online and in person at Charles Sturt University.
HEALTH ECONOMICS SYMPOSIUM
Research Australia’s recent Health Economics Symposium at the National Press Club of Australia drew more than a hundred leaders from government, academia, industry and consumer groups to tackle a pressing question: how do we build a sustainable health economics and health services research sector? With Australia’s productivity at a 60-year low and chronic diseases imposing a heavy economic burden, the conversations centred on the need for coordinated national investment, smarter evaluation of research and new models of government support. Delegates heard from the Hon Mark Butler MP the Minister for Health and Aged Care and Minister for the National Disability Insurance Scheme, Australia’s Chief Health Economist, Professor Emily Lancsar and other leading thinkers and agreed that health economics must sit at the heart of policy if we are to drive better health outcomes and lift national prosperity. A suite of outputs including a communiqué capturing the day’s insights and calls to action is now in preparation, underscoring Research Australia’s commitment to turning discussion into lasting impact.





Above: Professor Henry Cutler, Inaugural Director, Centre for the Health Economy, Macquarie University and Co-Chair of Research Australia's Health Economics Working Group, addressing the audience.
Below: Professor Emily Lancsar, Australia's Chief Health Economist, in conversation with Nadia Levin, CEO & Managing Director, Research Australia
Left: Panel discussion facilitated by Dr Lisa Higgins, Senior Research Fellow and Lead, Health Economics Program, ANZIC-RC, Monash University with Lane Carrandi, Dr Elisabeth Huynh and Associate Professor Alison Pearce
Below: Audience participation in Q&A

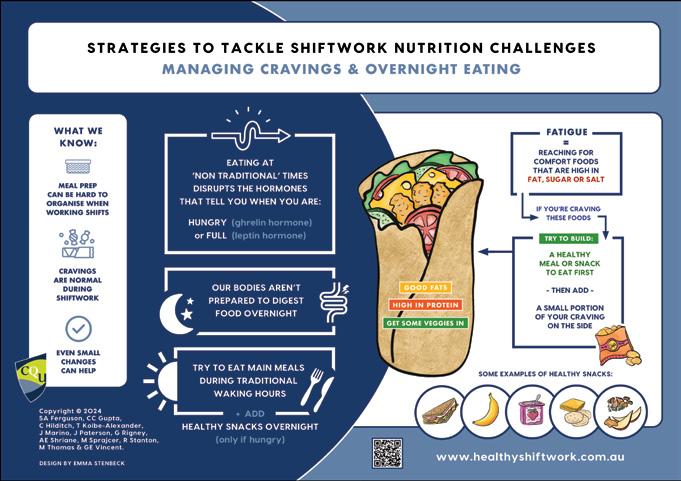
‘NO ONE TOLD US HOW TO MANAGE SHIFTWORK’
Practical Health Resources for Regional, Rural and Remote Shiftworkers.


Shiftworkers in regional, rural, and remote areas face major challenges in maintaining their health due to irregular hours, high demands, staffing shortages, and limited services. The Healthy Shiftwork resources offer free, co-designed, evidence-based strategies to support better sleep, nutrition, and physical activity, empowering shiftworkers and workplaces to improve health.
THE HEALTH BURDEN OF SHIFTWORK IN REGIONAL, RURAL AND REMOTE AUSTRALIA

Shiftwork is essential to keeping regional, rural, and remote Australia running. From around-the-clock patient care in hospitals to control room monitoring, supply chain logistics, emergency response, and farm work — there is work to be done 24 hours a day. Despite their vital roles, shiftworkers face serious health challenges from their schedules — including poor sleep, inadequate nutrition, and limited opportunities for physical activity
These health issues have wide-reaching consequences. These challenges also create a considerable economic burden, not only in healthcare costs, from chronic disease to fatigue-related errors and burnout, but also in staff turnover, reduced productivity, and safety risks.
In regional, rural, and remote areas, workers face shiftwork-related health challenges on top of staff shortages and stretched services. Healthcare workers, for example, often face high workloads, chronic understaffing, and limited support. Despite the Rural Health Strategy’s aim to recruit 6,000 more clinicians by 2028, retention remains a significant challenge — almost 1 in 8 healthcare workers are considering leaving within a year, often due to burnout. Without targeted, practical support to handle the demands of shiftwork, regional, rural, and remote workers will keep facing serious

Lead Associate
Professor Grace Vincent
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
health challenges — and regional, rural, and remote communities will pay the price.
SHIFTWORKERS WANT A SOLUTION
Our consultations with shiftworkers revealed a clear message. Existing health resources do not reflect the realities of working shiftwork, let alone shiftwork in the regional, rural or remote areas. ‘I love my job,’ one rural nurse said, ‘but the night shifts, travel and lack of support mean staying healthy feels impossible.’ A rural midwife shared, ‘Poor rest between shifts makes for potential errors the next day, poor judgement, and difficulty resting when you finally make it to your days off.’
Another shiftworker reflected on the lack of foundational training ‘When I started, I wasn’t told anything – there was no education. So, there’s this attitude of working aroundthe-clock, and a real lack of respect for your health.’
These insights made it clear that shiftworkers needed a tailored solution to support their health, yet few resources speak directly to their needs. The solution needed to be simple, practical, and developed by shiftworkers for shiftworkers.
INTRODUCING HEALTHY SHIFTWORK
Researchers at CQUniversity’s Appleton Institute ran multiple workshops with shiftworkers (some working in regional, remote, and rural communities), science communication experts, and world leading scientists to find out what advice shiftworkers need about sleep, nutrition, and physical activity. From this, we created Healthy
Shiftwork, a free suite of evidence-based tools to help shiftworkers manage sleep, nutrition, and physical activity. Hosted at www.healthyshiftwork.com.au , the free resources include website content, animated videos, infographics, and social media. From tips on napping effectively, when to consume caffeine on shift, to choosing what to eat on night shift, the resources are grounded in scientific evidence but designed specifically by shiftworkers for shiftworkers.
The goal of the project is to connect our world-leading shiftwork research with the reality of life as a shiftworker. Providing these evidence-based resources to shiftworkers early in their career, and having workplaces integrate them into organisational systems, creates the opportunity for workers to get into healthy habits early. In regional, rural and remote settings, this approach is critical to supporting recruitment and improving long-term retention of shiftworkers.
EARLY IMPACT AND WHERE TO FROM HERE?
Workers and workplace leaders have welcomed the Healthy Shiftwork resources. ‘This is the first time we’ve had something that actually speaks to our reality,’ noted an emergency services manager. The simplicity, flexibility and relevance of the tools have contributed to their initial uptake across diverse shiftwork settings.
Providing free access to Healthy Shiftwork is just the first step — success depends on uptake and integration into



routine practice. While we had input from shiftworkers from regional, remote, and rural communities into the development of the resources, there is room to further tailor the resources to these communities. Our next goal is to extend Healthy Shiftwork with input from more regional, rural, and remote shiftworkers — tailoring resources to local realities and improving workforce health.
Importantly, we also want to examine the individual and organisational barriers and enablers to implementation given the unique constraints of regional, rural and remote areas. This work would lead to a Healthy Shiftwork Implementation Toolkit for regional, remote and rural communities featuring onboarding templates, toolbox talks, and health and wellbeing planning guides. Given these toolkits do not require significant infrastructure, making them ideal for resource-stretched workplaces.
As Australia continues to strengthen its regional, rural and remote workforce, practical solutions like Healthy Shiftwork will be essential for improving health and keeping regional, rural, and remote shiftworkers safe, supported, and on the job.
Authors: Lead Associate Professor
Grace Vincent is an Associate Professor at CQUniversity’s Appleton Institute and the Centre of Health Equity in Regional and Remote Communities..
Co-author Dr Madeline Sprajcer is a Senior Lecturer at CQUniversity’s Appleton Institute and the Centre of Health Equity in Regional and Remote Communities.
Co-author Dr Charlotte Gupta Postdoctoral Research Fellow at CQUniversity’s Appleton Institute and the Centre of Health Equity in Regional and Remote Communities.
Co-author Dr Gabrielle Rigney is a Senior Lecturer at CQUniversity’s Appleton Institute and the Centre of Health Equity in Regional and Remote Communities.
The Healthy Shiftwork Team: Professor Sally Ferguson, A/Professor Matthew Thomas, Dr Cassie Hilditch, Dr Tracy Kolbe-Alexander, A/ Professor Rob Stanton, A/Professor Jessica Paterson, Ms Alexandra Shriane.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
FARMERS MATTER –DON’T THEY?


Dr David Meredith and Associate Professor Marcus Cattani

Australian farmers are top of the workplace fatality league table. Why is this the case, and how can we give our famers what they need to stay safe at work?
Did you know that farmers have the highest rate of workplace injuries in Australia? The Inquiry into the agricultural industry in Western Australia (2023), initiated after the 12th fatality in Western Australia in 12 months, summarised that:
‘Many farmers are very conscious of the risks inherent in their operations and actively work towards overcoming those risks and keeping their workers safe. Others treat risks and incidents, injuries and deaths that arise as being inevitable.’‘This Inquiry found many examples of polaropposite views:
1. of industry leaders who view the need to take the time and effort to keep their people safe as a nuisance, an impediment to productivity and a reduction in profitability; and
2. of industry leaders and farmers consistently working towards education and training and better methods of keeping their people safe.’The Farmers Matter Project is currently being developed to address the issues contributing to this poor health and safety performance. Central to the project’s development is engagement with farmers and other key stakeholders.
LISTEN TO THE FARMERS: COMMUNITY OF PRACTICE
Using a methodology adopted from the SafeHabitus European program, farmers and other stakeholders will discuss issues and barriers in the implementation of existing and new injury prevention resources. These Communities of Practice will discuss matters such as priority-setting and program delivery preferences, and discuss key themes including leadership, mental health, workplace hazards and fitness for work. The SafeHabitus Community of Practice approach has successfully engaged with farmers to provide useful information to prompt action. The Australian project will use this essential information to update existing resources, translate resources from other industries, and commission new resources.
WORKPLACE HAZARDS: POOR EQUIPMENT AND/OR RISK-TAKING BEHAVIOUR?
Many government agencies and research organisations have high-quality publications and resources available on their websites, but there is insufficient uptake of these resources by farmers. For example, SafeWork Australia reports that most injuries (62% in 2022-23) occur during the use of vehicles. Since the 1990s, a wide range of reports and other resources have been published on this topic. Recently, side-by-side vehicles have been recommended because they are designed to be safer. However, in response to ongoing incidents, the Chair of FarmSafe Australia commented to the ABC that: ‘Farm safety advocates say while “the vehicle itself is a very safe
product”, vehicle users need to take the manufacturers’ safety advice more seriously.’The Community of Practice discussions will address the use of vehicles and other workplace hazards, to identify how farmers, manufacturers, maintainers and other stakeholders can improve the management the risk of these injuries.
LEADERSHIP COMMITMENT: THE RISKBASED APPROACH
The prevention of workplace injuries uses a risk management approach, which starts with leadership commitment, and subsequently a partnership with workers, to design and implement controls to achieve improved performance. If a leader does not commit to this approach and perceives workplace incidents and injury as inevitable, then, particularly when there are highrisk tasks taking place, injuries are more likely to occur as the necessary controls have not been put in place. The Community of Practice will inform systems designers, researchers and trainers how to develop leadership materials to assist farmers improve their risk management performance. It is expected that there will be an initiative to train farmers in a wide range of skills, including risk management, which can be applied across all disciplines on the farm, and not just health and safety.

GOVERNANCE AND SUSTAINABILITY: ADDRESSING INDUSTRY DIVERSITY
There is agriculture in every state and territory, and the industry comprises crops and livestock which each have diversity, made more complex due to local soil type and the environment. The industry comprises large to small organisations, with associated resources and organisational culture. In 2024, the Rural Health and Safety Alliance created a stakeholder map of around 50 research organisations, and around 50 commodity agencies who have a role in many aspects of their commodity, including health and safety.
This project includes a management structure to engage and collaborate with all organisations and agencies who are working for the common goal of preventing harm to farmers.
COORDINATE: FARMERS MATTER: AN ONLINE COMMUNITY AND RESOURCE
Farmers Matter will provide farmers with a customised approach to the management of injury risk on their farms. Subject to funding, it is planned to provide selfhelp resources, peer support and other injury prevention resources freely to farmers on the website.
Author: Associate Professor Marcus Cattani has worked for Edith Cowan University in Perth for 10 years. Marcus is leading the Farmers Matter project in Australia. Marcus was hosted in Dublin in July 2025 by Dr David Meredith and his team at SafeHabitus, a European program to improve farmer health and safety across 11 countries.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
Examples of community paramedic clinic in action
CAN IT BE THIS EASY?
How community paramedicine is transforming rural health care.


In rural Australia, access to quality health care is often a daily challenge. Clinics and doctors can be hours away, leaving many residents with limited options for managing ongoing health issues.
At the same time, thousands of trained paramedics across the country struggle to find roles within traditional ambulance services. What if there was a way to solve both problems with one innovative solution?
Community Paramedicine is gaining momentum thanks to a partnership between La Trobe University’s Violet Vines Marshman Centre for Rural Health Research, Safer Care Victoria and the Alliance of Rural and Regional Community
Health (ARRCH). This collaboration is pioneering a fresh way to deliver health care directly to rural communities by expanding the role of paramedics beyond emergency response.
THE PROMISE OF COMMUNITY PARAMEDICINE
Unlike traditional paramedics who respond primarily to emergencies, Community Paramedics provide routine health care within the community. They offer services such as health checks, chronic disease monitoring, and health advice at local hubs like town halls, libraries, and seniors’ centres. This model focuses on prevention, early intervention, and connecting people to the care they need before emergencies arise.
Originating over 15 years ago in Canada, the Community Paramedicine program has been hugely successful, reducing emergency ambulance call-outs by about 20% and saving healthcare systems significant costs. Inspired by these results, Australia has begun trials in rural Victoria, supported by organisations including Sunraysia Community Health Services, La Trobe University, and Safer Care Victoria.
A successful pilot of a Community Paramedic Clinic took place in Mildura in 2022-2023. Over 10 months, the program grew from one clinic and 8 attendees to 5 clinics servicing 111 people. Most participants were older, had 3 or more chronic diseases and a high diabetes risk score. Over a third of attendees had no regular GP. Paramedics and participants were unanimously enthusiastic about the program, which continues to be well supported by the community.
BRIDGING THE RURAL HEALTH GAP
In a recent La Trobe University Partner Showcase 2025, Professor Leigh Kinsman and Professor Evelien Spelten from La Trobe’s Violet Vines Marshman Centre joined Dr Louise Reynolds from Safer Care Victoria to highlight the impact of this program. Their collaborative work addresses a pressing issue: the healthcare gap between urban and rural areas.
Professor Evelien Spelten emphasised the unique opportunity Community Paramedicine offers: ‘There is an opportunity to use paramedics - a large, skilled but underutilised workforce - to ease pressure on hospitals and clinics while delivering care designed for the unique needs of rural communities. This approach is already making a difference in towns where trial clinics offer free, accessible health services to people who might otherwise go without.’
WHY IT MATTERS
Rural Australians face a disproportionate burden of chronic illnesses such as diabetes, heart disease, and

respiratory conditions. Managing these diseases requires regular monitoring and timely interventions — services often unavailable nearby. By integrating Community Paramedics into primary care, these challenges become easier to overcome.
Moreover, for paramedics, this model opens new career pathways outside traditional ambulance work, making better use of their extensive training and skills. It’s a solution that benefits everyone: communities get better care, paramedics find meaningful employment, and the health system reduces costly emergency visits.

OVERCOMING CHALLENGES
Despite its promise, rolling out Community Paramedicine is not without hurdles. Funding systems for these roles are not yet fully developed, and there are legal and regulatory barriers that limit paramedics’ scope of practice outside emergency response.
The partnership between La Trobe University, Safer Care Victoria and ARRCH is crucial in tackling these challenges. Together, they are working to clarify job roles, advocate for appropriate funding, and influence policy changes to make community paramedicine a sustainable part of rural health care.
WHAT’S NEXT?
The program is currently trialling in four rural Victorian towns, gathering vital data to demonstrate its effectiveness locally. The hope is to expand to many more communities, helping to close the health access gap for rural Australians.
For rural towns and health services interested in joining these trials, this is an exciting opportunity to be part of a pioneering healthcare innovation that could change the way care is delivered across the country.
A HEALTHIER FUTURE WITHIN REACH
Community Paramedicine shows that sometimes, the simplest solutions can have the biggest impact. By reimagining the role of paramedics and bringing health care directly to rural communities, Violet Vines Marshman Centre for Rural Health Research, La Trobe University, Safer Care Victoria, ARRCH and their partners are helping to build a future where quality health care is within everyone’s reach — no matter where they live.
Learn more about the project: CP@Clinic - IMOCSunraysia Community Health Services
Author: Professor Evelien Spelten is a Professor with La Trobe University Rural Health School, and is affiliated with the Violet Vines Marshman Research Centre.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
REMOTE WOMEN YARN FOR HEALTH
The inaugural Western CapeHER women’s health forum was abuzz over two days in Napranum, Cape York Peninsula, with researchers, experts and local women yarning about health. Organisers said it was the first time a gathering like this has happened on Country.
On day two of CapeHER, one speech made an enormous impact. Professor Sandra Creamer AM explained that in Queensland, health care without discrimination is a legislated human right.
Olivia Milsom, a Graduate Policy Officer with the Queensland Women and Girls Health Promotion Program at Queensland Health, was among the researchers there.
‘An Indigenous woman from Napranum said to me afterwards, “I had no idea my health was a human right. I’m going back to the community and telling people about this,’”’ said Ms Milsom.
‘That was when I knew Western CapeHER had made an impact.’
FROM STRONG FOUNDATIONS
Western CapeHER brought together almost 30 researchers and health experts to speak about remote women’s health, in Napranum in the Western Cape York Peninsula.
Minnie King , a Kaiwalagal, Umaii, and Kiwai and successful businesswoman from Weipa, was the creative force behind the forum. Ms King had had health concerns of her own but was also tired of the inequities experienced by Indigenous and other remote-living women in the Western Cape.
When Minnie King wants something, she makes it happen.


‘My dream was also based on need. We’d already done work around menstrual health with UQ,’ said Ms King, whose successful ‘Mind Your Body’ program for schools, created in collaboration with the University of Queensland, is free online and coveted by multiple state governments.
‘The women were saying, “We need to talk about health our way,”’ said Ms King.
Women from the Western Cape wanted health discussions to happen on Country, not in Cairns or Brisbane. King and her team created a local Community Advisory Committee comprising women from each represented community, which had the final decision about everything that happened at Western CapeHER.
‘I didn’t want someone coming in and telling us what’s important. That’s why we had a local Community Advisory Committee, with women from Mapoon, Napranum, Weipa, Aurukun. The women told us what mattered,’ explained King.
Ms Maria Pitt, a traditional owner and Tjungundji woman from Mapoon, said that events such as these need to be community based.
CapeHER Local Advisory Committee, L-R, Jessica Rex (Weipa) Minnie King (Weipa), Geraldine Mamoose (Mapoon).
Western CapeHER attendees


‘Everything is built from the roof down, until you allow the community to take responsibility, take ownership, and say to the rightful people, “Why aren’t you allowing us to have a seat and have a voice?”’ said Ms Pitt.
EXPERTS FROM AROUND AUSTRALIA
Speakers and experts at the forum had a variety of perspectives. They included Hylda Poi Poi, First Nations Assistant Director of Nursing Workforce Designs at Torres and Cape Hospital and Health Service, Keri Tamwoy, a local woman and former mayor of Aurukun; Professor Sandra Creamer AM, CEO of Australian Women’s Health Alliance; Bianca Blackmore and other specialists from Women’s Health Equity Queensland; and Professor Gail Garvey, head of First Nations Cancer and Wellbeing Research at The University of Queensland.
Michelle O’Connor spoke about the new birthing program at Weipa Hospital; Dr Jemma Nokes, Senior Medical Officer at the Hospital was one of many speakers that threw away their slides and spoke from the heart.
Linda McLachlan, a Mapoon woman, entitled her talk, ‘I yelled, but nobody heard me,’ a personal perspective on the effects of colonisation on health. Other topics included cancer and chronic disease, birthing and maternity, justice, oral health, and climate health.
The common feeling emerging from the collection of women was one of shared power, and of being heard.
‘People said they felt safe. Like they could finally talk about cancer, or grief, or their bodies, without shame,’ shared Ms King.
‘The moment that got me was one of the Elders saying: “This is the first time Country heard us speak like this.”’
A GOOD COLLABORATION
Minnie worked with Associate Professor Nina Lansbury, from the University of Queensland School of Public Health to create the forum. They received funding from partner Queensland Health, from Apunipima communitycontrolled health as a sponsor, and brought on Ms Milsom and the team at the Queensland Women and Girls’ Health Promotion Program.


A/Prof. Lansbury has collaborated with Ms King for almost a decade.
‘Our role at the University is to listen, support and help amplify what’s already happening in community,’ said A/ Prof. Lansbury.
‘This was never about dropping in a project. It’s about a relationship, and Minnie has been guiding this project for years.’Ms Milsom conducted her Honours thesis via interviews with local women on the challenges of living remotely, with a focus on solutions.
Similarly, the forum was solutions focused. Each session was followed by group discussions about challenges, and possible solutions to the issues discussed, which were facilitated and recorded.
COMMUNITY FIRST, WORKS
The team will be presenting several results from Western CapeHER.
‘Within a couple of months, we hope to have a clear report written intentionally for government. There will be journal articles in the literature so that will extrapolate beyond just the Western Cape, to other remote and Indigenous women’s situations,’ said A/Prof Lansbury.
‘The dream is that this becomes a model for other places—but only if it stays grounded,’ said Ms King.
‘I’d love to see this happen again next year. But we need funding, recognition, and to keep the power where it belongs: with the women.’
Author: Rebecca Whitehead is a freelance health writer contributing regularly to the Medical Journal of Australia’s InSight+. Ms. Whitehead attended the inaugural Western CapeHER women’s health forum as the guest of organiser Ms. Minnie King. Western CapeHER was created, organised and funded by Ms. King and Prof. Lansbury at Queensland University, and Queensland Health.
at Western CapeHER in discussion
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
AI-ENHANCED INTERVENTIONS
Promoting
climate change disaster event preparedness in individuals with self-reported climate change-related
anxiety, worry, and stress.
Climate change is no longer a distant environmental concern. For many, especially those living in rural, regional, and remote areas, it is already a harsh reality, constantly experienced through climate-related disasters.
This has become increasingly clear in Australia, with the psychological impacts of climate change becoming more evident nationwide. A 2022 national poll by the Climate Council revealed that 63% of Australians had experienced heatwaves, 47% had faced flooding, 42% had encountered bushfires, and 36% had endured drought, with many having experienced multiple climate events during their lifetime. Over half of those surveyed said these events affected their mental health, with 21% describing the impacts as significant or moderate. These figures highlight a silent, worsening mental health crisis that current care systems are not equipped to handle, especially in Australia’s remote and rural communities.
Vulnerabilities in rural and remote Australian communities grow considerably due to a combination of factors, including increased exposure to climate events and related stressors, limited access to healthcare services, socioeconomic disadvantages, and, in some cases, unreliable digital connectivity. While the physical impacts of climate change are well understood, a clear gap remains in our understanding and response to its psychological effects. Emerging innovations—especially those involving digital artificial intelligence (AI)-driven solutions—are being called on to support existing infrastructure and provide early, personalised, and scalable mental health care.
BARRIERS TO EFFECTIVE MENTAL HEALTH RESPONSE IN RURAL AUSTRALIA
Even with growing awareness, several interlinked factors and barriers limit an effective mental health response to climate change in rural areas:
• Service Inaccessibility: Rural and remote communities often lack local mental health professionals and services, relying more heavily on flyin, fly-out options. This creates barriers to accessing
timely and consistent care, especially during and after a climate disaster when demand peaks.
• Scalability of Conventional Interventions: Psychological care, such as counselling and therapy, is labour-intensive and difficult to scale up. It can be resource-intensive and challenging to deliver across widespread communities in the event of mass trauma, like a bushfire or flood.
• Stigma and Help-seeking Barriers: Mental health stigma in rural Australia acts as a significant obstacle to accessing support. People are often hesitant to seek help, especially in close-knit communities where concerns about being seen or judged, or worries about confidentiality being breached, are common.
• Lack of Tailored, Preventive Support: Most assistance is offered after issues arise rather than focused on prevention, and it is seldom customised to the specific climate stressors or the socioenvironmental circumstances of regional and rural communities.
User input
Text preprocessing (Tokenisation & Cleaning)
Topic Classification
Sentiment Analysis
Intervention Suggestion (CBT-based) Response

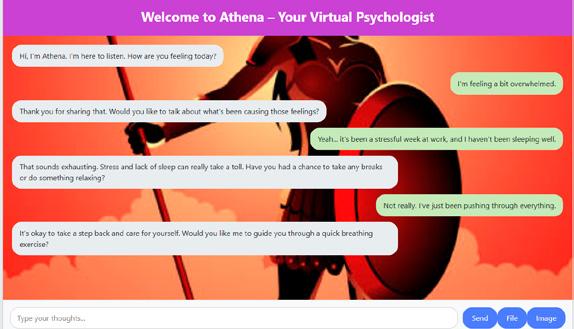
VIRTUAL PSYCHOLOGIST: A DIGITAL LIFELINE WITH ATHENAOS
The Virtual Psychologist, known as AthenaOS, is a nextgeneration Therapeutic AI Agent designed to deliver open, scalable, and personalised mental health support using Generative Artificial Intelligence (GenAI). Inspired by Athena, the Greek goddess of wisdom and strategy, this advanced platform combines open-source GenAI with evidence-based psychological methods to offer innovative, responsive, and contextually aware mental health assistance. AthenaOS aims to complement existing mental health services, providing 24/7 access through natural language conversations. This enables individuals to develop their coping strategies, conduct emotional checkins, and access personalised resources. Its capacity to learn and improve over time allows for continual refinement of responses, making it especially well-suited to support people in rural, regional, and remote communities where mental health services may be limited or hard to reach.
AthenaOS is designed with a multi-layered architecture to facilitate seamless and secure interactions. The topmost layer is the interaction interface, offering a straightforward chat or voice communication platform for users on a secure web-based system. Behind the scenes, the communication engine interprets and processes user input to ensure a natural and supportive conversation flow, utilising NLP for more human-like engagement. AI features are supported by an underlying AI analysis layer that categorises topics, analyses sentiment and severity, and understands context to customise responses. A cognitive behavioural therapy (CBT) response engine produces compassionate, clinically informed replies. At the same time, a safety filter continually monitors for high-risk language or behaviour, flagging issues for immediate escalation if needed.

KEY FEATURES
• Intelligent Therapeutic Conversations: Engages users in meaningful dialogue using advanced natural language processing
• Evidence-Based Methodology: Implements recognised therapeutic techniques like CBT
• Accessibility: Available 24/7 for users regardless of location
• Privacy-Focused: Ensures all user data is encrypted and stored securely
• Complementary Care: Designed to work alongside traditional therapy, not replace it
FUTURE VISION
AthenaOS is an AI-inspired project dedicated to supporting mental health in rural and remote communities across Australia. Leveraging the power of generative AI and large language models, AthenaOS aims to deliver accessible, scalable, and personalised mental health support to residents of Australia’s rural and remote areas, who often face higher risks of mental health issues and limited access to services. In many rural and remote locations, access to mental health care is hampered by workforce shortages, long distances to facilities, and a lack of local specialised care. AthenaOS could provide essential early intervention, emotional support, and crisis triage to anyone through a mobile or online app, complementing existing services and addressing gaps in care. It will support the national goal of reducing digital health inequities. It may help diminish mental health disparities in rural and remote Australia by offering timely, culturally appropriate, and ongoing support.
Author: Dr. Ahsan Morshed is a lecturer and Discipline Leader of Information Systems and Analysis at Central Queensland University.
AthenaOS Chatbot
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
SAFE WATER, HEALTHY COMMUNITIES
Addressing Drinking Water Quality in Australian Homelands Communities

Many rural and remote communities in Australia face ongoing challenges with access to safe and reliable drinking water. Homelands communities are especially affected, with water insecurity impacting everyday health and wellbeing. What practical steps can be taken to support fair and lasting solutions?
WATER SECURITY IN AUSTRALIA
Australia falls short of the Sustainable Development Goal of ‘Safe Drinking Water for All.’ Available data suggests that nearly 200,000 people in remote regions lack consistent access to potable water that meets health standards, while an additional 400,000 receive water that fails basic aesthetic benchmarks. Alarmingly, over 40% of affected localities are Homelands communities. Water insecurity not only compromises daily wellbeing, it entrenches health inequities and poses a serious challenge to improving rural and remote health outcomes.
WHAT’S IN THE WATER?
Household water supply in Australian Homelands Communities is predominantly sourced from groundwater. While this can be a dependable source of potable water, groundwater can have naturally elevated solute concentrations, which, along with challenges in infrastructure and treatment, can lead to exceedances of health-based Australian Drinking Water Guidelines (ADWG). Key concerns include elevated levels of trihalomethanes, nitrate, E. coli, fluoride, uranium, manganese, lead, chlorine, and bromate.
SAFE DRINKING WATER IS ESSENTIAL FOR HEALTH
Access to safe drinking water is fundamental to health and wellbeing, with poor drinking water quality linked to both chronic and acute health issues including kidney disease and gastrointestinal illness. Health risks associated with water-borne contaminants can be heightened in
The authors. Main photo (L-R): Caitlin Wyrwoll, Christine Jeffries-Stokes, Annette Stokes, Sarah Bourke, Leaf Kardol on Wongatha Country. Inset: Mara West (L), Roz Walker (R).

communities with limited water quality monitoring or management solutions.
Emerging research highlights that certain populations— particularly pregnant people and children—are more vulnerable to adverse health effects from drinking water contaminants. For example, while the Australian Drinking Water Guidelines (ADWG) set nitrate thresholds based on the risk of methemoglobinemia in formula-fed infants, recent studies suggest that even lower levels may be associated with increased risks of preterm birth, stillbirth, and foetal growth restriction . However, the causal evidence is not yet fully established, and these outcomes may be linked with broader water quality and health concerns.
Beyond consumption, poor water quality also affects household washing, sanitation and hygiene practices. Hard water limits the efficacy of soaps for washing clothes and skin, and can contribute to skin infections and other preventable health conditions. Hard water and chemical residues can also damage plumbing infrastructure, compromising sanitation systems such as toilets, showers, and food preparation areas.
Unpalatable water also influences hydration behaviours, leading some individuals to consume sugary drinks instead, which can exacerbate chronic health issues. In some cases, households may resort to purchasing bottled water, adding financial strain.
The psychological burden of living with unsafe and unreliable water—especially in communities where residents are aware of the risks but lack the means to address them—can contribute to stress and mental health challenges. The uncertainty and frustration of navigating complex service delivery systems to resolve water issues further compound these impacts.
DRIVING CHANGE: COMMUNITY CODESIGN AND PARTNERSHIPS
Water insecurity in Australian Homelands Communities is a national policy issue, yet consistent and adequate service provision remains a persistent challenge. Addressing this requires more than technical fixes, it demands genuine partnerships and co-designed solutions that centre the voices of those most affected.
Community co-participation, alongside collaboration with service providers, government, industry, and researchers, is essential to ensure that solutions are culturally appropriate, locally relevant, and sustainable. Empowering communities with agency to advocate for their own water security is not only ethical, it is effective.

Research plays a critical role in identifying contaminant exposures and their health impacts, which is vital for informing updates to the ADWG. Equally important is the need for transparent, accessible drinking water quality data, along with culturally appropriate health context to support community understanding. Improving data transparency and cross-cultural water literacy will support community advocacy, inform infrastructure planning, and help drive sustainable solutions. Community-led water testing and culturally appropriate real-time water quality screening tools can empower residents to manage potential health risks.
However, these efforts require sustained financial investment as well as ongoing relationship and capacity building efforts. It is estimated that at least $2.2 billion is required to ensure Australian Homelands Communities receive drinking water meeting the Australian Drinking Water Guidelines. This will take decades. While targeted funding is available to support infrastructure upgrades, more investment is required to support communityled initiatives and partnerships. Targeted, culturally appropriate training and employment programs in water quality and service delivery will be vital to support Community independence and long-term solutions. Without adequate resourcing, the cycle of water insecurity and its health consequences in Australian Homelands Communities will persist.
Authors: Annette Stokes is a senior Wongutha, Mulba-Ngadu, and Anangu woman based at the University of Western Australia’s School of Earth Sciences. Mara West is a Yamatji Elder with the Kids Research Institute Australia and Chair of the Homelands Advocacy Hub at the Coolamon Centre, Ngangk Yira Institute, Murdoch University. Sarah Bourke is a hydrogeologist at the University of Western Australia’s School of Earth Sciences.
Christine Jeffries-Stokes is a Kalgoorlie-based paediatrician affiliated with the Rural Clinical School WA at the University of Western Australia. Leaf Kardol is a PhD candidate at the University of Western Australia’s School of Human Sciences. Roz Walker is Director of the Coolamon Centre, Ngangk Yira Institute, Murdoch University.
Caitlin Wyrwoll is a reproductive physiologist at the University of Western Australia’s School of Human Sciences.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

BRIDGING THE GAP
Bringing Assistive Technology to Rural and Regional Communities
Living with Brain Injury



Ingham Institute for Applied Medical Research has established the Assistive Technology Hub (AT Hub)—a research and service initiative aimed at unlocking the power of technology for people with cognitive impairments, especially those beyond the metropolitan fringe.
Acquired Brain Injury (ABI) is more than a single moment of trauma — it’s a life-changing journey that continues long after the initial injury. The ongoing effects, like changes in memory, judgement, and thinking, can deeply affect how someone connects with the world and those around them. For people living in rural and regional areas, these everyday challenges can be even harder, with fewer specialised rehabilitation services close to home.
THE PROMISE OF ASSISTIVE TECHNOLOGY IN REGIONAL RECOVERY
Assistive Technology (AT) is emerging as a vital tool to support people with ABI by enhancing independence, aiding communication, and helping with cognitive rehabilitation. Recognising this potential, Ingham Institute for Applied Medical Research established the Assistive Technology Hub (AT Hub). Under the leadership of A/ Prof Grahame Simpson and management of Mr Brendan Worne, the AT Hub is focused on making assistive technology more accessible, relevant, and practical for people living in the community—wherever that community may be.
EXPANDING THE REACH: THE AT-WRAP PROJECT
A major step forward in closing the rural care gap is the AT Hub’s latest project, AT-wRAP (Assistive TechnologyRural Access Project). This three-year initiative, funded by icare NSW and delivered in collaboration with Ingham Institute, the University of Sydney, Charles Sturt University, and Monash University, aims to build local capability by supporting regional clinicians in delivering technologyenabled cognitive care.
With eight regional ‘spokes’ supported by two project officers living in those communities, AT-wRAP offers faceto-face training, live technology demonstrations, and personalised clinical guidance. This approach ensures that clinicians in rural towns—from Albury to Ballina— are equipped with both the tools and the knowledge to support individuals with ABI in their own communities.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

‘By delivering local training and showcasing assistive technologies, we’re building real capability where it’s needed most—outside the city,’ says project manager Brendan Worne – a physiotherapist by training and member of Ingham Institute’s Brain Injury Rehabilitation Research Group.
‘This is about empowering clinicians and their clients in rural areas to take advantage of smart, affordable solutions that support independence.’
SMARTHOME RESEARCH: TECHNOLOGY IN EVERYDAY LIFE
The AT Hub has also pioneered smart technology research through the SMARThome trial, a collaborative study with partners including Monash University, South Western Sydney Local Health District, and Royal Rehab
Group. Funded by the Transport Accident Commission Victoria and icare NSW, the study has explored how everyday technologies—like mobile apps, wearables, and smart home devices—can help people with ABI manage daily routines and improve executive functioning.
Using personalised goals and in-home assessments, the research team implemented tailored technology setups for each participant. The outcomes were promising; participants showed significant improvements in managing tasks like medication, daily routines, and social engagement—all in their own homes.
Importantly, SMARThome used mainstream, affordable technologies that many people already own, making the intervention both cost-effective and scalable for rural and remote populations.


THE FUTURE: RURAL ACCESS TO CLINICAL SERVICES
Looking ahead, the AT Hub is set to expand its services by embedding within the Perich Centre for Robotics & Health Technology at the Ingham Institute. The Perich Centre is driven by ‘tech-quity’ – advancing global health equity through technology in areas as diverse as AI in stroke imaging, pre-hospital cardiac treatments, remote intervention and therapeutics, and surgical robotics. By being based in the Perich Centre, the AT Hub team will be able to offer telehealth and hybrid services, extending the reach of specialist support into regional and rural communities.
‘We’re not just researching—we’re building a system that rural communities can access and trust,’ says Brendan. ‘The AT Hub is here to help people in Dubbo or Wagga just as much as someone in Sydney.’Empowering Recovery, Wherever You Live
With a firm commitment to equity in healthcare, the Assistive Technology Hub is transforming the rehabilitation
journey for people with ABI, no matter their postcode. Through projects like SMARThome and AT-wRAP, and the upcoming expansion into clinical services, the AT Hub is driving innovation that ensures rural and regional Australians don’t get left behind.
These efforts are already delivering meaningful results: better health outcomes, reduced reliance on carers, and greater community participation. Most importantly, they’re restoring dignity, autonomy, and hope to people living with brain injury—right across the state.
Authors: Professor Grahame Simpson: Lead, Brain Injury Rehabilitation Research
Mr Brendan Worne: Lead, Brain Injury and Assistive Technology Hub Ingham Institute for Applied Medical Research
Examples of Assistive Technology at the AT Hub
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
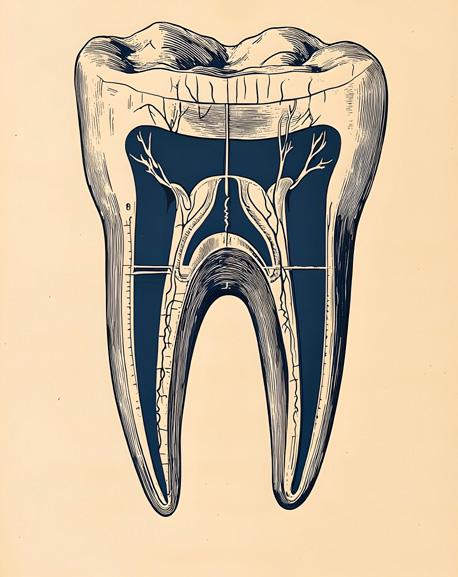
THE ROOT OF THE PROBLEM
Tackling Tooth Health in Regional WA.
Using biological samples, tele-dentistry and community-led models, ORIGINS sub-projects are uncovering hidden risks and delivering practical, evidence-based care to families in rural and remote regions — driving new approaches to oral health from the earliest stages of life.
Two pioneering sub-projects from the ORIGINS longitudinal study are transforming dental care and hygiene in remote and Indigenous communities across Western Australia.
ORIGINS is Australia’s largest longitudinal cohort study of its kind, following 10,000 WA children and their families from conception through early childhood to support research aimed at preventing and treating noncommunicable diseases in the early years of life.
The study, a 10-year collaboration between The Kids Research Institute Australia and Joondalup Health Campus in Perth, has built an extensive data platform with more than 16 million data points, linked health records, and 400,000 biological samples — including children’s teeth.
This last collection has paved the way for The Heavy Metal Tooth Fairy Project and The Dental Screening Study. With the teeth of ORIGINS participants available for use as control and pilot samples, the researchers have been able to build two efficient, cost-effective projects focused on dental health in rural and Indigenous communities.
THE HEAVY METAL TOOTH FAIRY PROJECT
The Heavy Metal Tooth Fairy Project addresses a crucial gap in understanding around whether groundwater contaminants, particularly heavy metals, are accumulating in children living in remote Australia.
Led by Chief Investigator Dr Christine Jeffries-Stokes and Dr Anette Stokes, both from The University of Western Australia (UWA), the project team is analysing 125 baby teeth from remote WA communities alongside 125 teeth from ORIGINS participants to compare the presence of heavy metals in children’s teeth from regional and metropolitan areas.
Heavy metals such as arsenic, lead, copper, mercury and zinc occur naturally in the environment and are more common in resource-rich regions like WA.
While low exposure to some of these elements is harmless, or even necessary, long-term exposure — even at low levels — can result in toxic accumulation and adverse health effects.
Babies and young children are especially vulnerable due to their developing tissues and organs being more susceptible to environmental influences.
In children, heavy metal toxicity has been linked to intellectual disability, neurocognitive and behavioural disorders, and cardiovascular and respiratory issues.
In addition to identifying exposure levels, the project is helping remote communities build skills in monitoring water quality, STEM education and dental hygiene.
Dr Jeffries-Stokes said empowering Aboriginal and remote communities to assess their own water quality allowed them to advocate for improvements.
‘Building awareness, skills and knowledge of environmental health, dental hygiene and STEM in remote communities is vital to bridging the gap in health and education outcomes between Indigenous and regional Australians and those living in urban areas,’ Dr JeffriesStokes said.
THE DENTAL SCREENING STUDY
During the COVID-19 pandemic, Principal Investigator and Honorary Research Fellow at UWA’s School of Allied Health, Dr Somayyeh Azimi, championed the idea of teledentistry to improve access to paediatric dental care.
This concept led to the Dental Screening Study: a pilot program launched within ORIGINS to maintain dental care during lockdowns and reduce children’s anxiety by enabling dental screenings at home.
Dr Azimi’s team conducted dental checks during routine ORIGINS three-year Kids Check appointments and trained parents to take photos of their child’s teeth.
The images were securely uploaded via a cloud-based system accessible only to authorised professionals and, when assessed by an external dental therapist, were found to closely match in-person exams — proving the method both reliable and simple for families to adopt.


Following the pilot, the team extended the program into regional and Indigenous communities to address significantly higher rates of tooth decay among children in remote areas compared to those in metropolitan regions.
In the central Great Southern region, the team developed a step-by-step guide for parents, while dental students, child health nurses and community partners visited familiar settings like daycare centres and playgroups to train staff and parents, conduct screenings and triage children.
The project helps parents recognise when and where to seek help, facilitating early identification of oral health problems. The project also supports health professionals — including emergency doctors, speech pathologists and neonatal nurses — in assessing severity and expediting referrals to specialists.

The program has since gained international interest — notably from a dentist in Saudi Arabia, where it has now been adopted across parts of the country and translated into Arabic, extending access to quality dental care for even more families worldwide.

Authors: Dr Christine Jeffries-Stokes is a paediatrician from UWA’s Rural Clinical School of WA. Her ground-breaking research as co-lead investigator of the Western Desert Kidney Health Project (WDKHP) found that nitrate contaminated drinking water was a contributing factor to higher-than-expected rates of kidney disease and type 2 diabetes in the Goldfields.
Dr Somayyeh Azimi is a highly skilled professional with specialty training in oral and maxillofacial diseases. As an Honorary Research Fellow of the International Research Collaborative — Oral Health and Equity at UWA, Dr Azimi is affiliated with a renowned oral health research and development group with a global reputation for addressing oral health disparities. Article submitted by the The Kids Research Institute Australia
The Heavy Metal Tooth Fairies. From left, Dr Christine Jeffries-Stokes, Dr Annette Stokes, Dr Sarah Bourke, and Prof Yulia Shiikha at UWA Perth. Image courtesy of UWA.
This image reveals the need for urgent surgical extraction. With early identification, the family could act immediately, avoiding worsening complications.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
BUILDING DIGITAL HEALTH TECHNOLOGIES THAT WORK FOR REMOTE COMMUNITIES
How trust, technology, culture, and care must come together to support a digital health shift across remote Australia.
Aboriginal and Torres Strait Islander peoples living in remote and very remote communities of the Northern Territory (NT) continue to face barriers to accessing timely and appropriate healthcare.
In these communities, service delivery is typically anchored by local primary health care clinics staffed primarily by Remote Area Nurses (RAN), with intermittent visits from general practitioners (GPs) and specialist outreach teams. When more advanced care is required, patients often are required to travel long distances to access care in regional centres such as Garramilla (Darwin), Mparntwe (Alice Springs), and even interstate.
As digital health technologies (DHTs) (such as videoenabled telehealth, remote monitoring devices and online appointment systems) reshape the Australian healthcare landscape, they offer promising resources to bridge geographic and systemic barriers to care in remote regions. The question isn’t just whether DHTs work, but whether these technologies work for the people they intend to serve.
To answer this, a large research project led by the Menzies School of Health Research and the University of Sydney is investigating remote community and providers’ experiences of, and preferences for using DHTs, and opportunities to co-design, implement, and evaluate the impact of DHTs in the Northern Territory (NT). Through conversations with health workers, GPs, and residents, we found that concerns about internet connectivity and technical difficulties were just the start. Beneath the surface, a deeper story about trust, culture, and the complex realities of navigating technology-enabled models of care emerged.
A CASE STUDY OF TELEHEALTH IN REMOTE COMMUNITIES
In a remote island community of the NT, a locally governed Aboriginal Health Service provides care to thousands of First Nations people across the region. For both healthcare providers and residents, delivering and accessing care
often requires extensive travel. Many health professionals rely on fly-in, fly-out (FIFO) models, while community members often face long waits for visiting specialists.
For many First Nations people, travelling to Darwin for care is not just logistically difficult; it is mentally and socially disruptive. Being away from community and family, even temporarily, can cause distress. For residents, healthcare needs and priorities often look different. As one GP noted, ‘Our locals are not always consistent in their attendance. They’ve got other priorities and responsibilities. They need to hunt, feed their families, and attend funerals…’
Our early findings confirm that when thoughtfully implemented, DHTs can provide meaningful benefits, but they must be shaped to and support everyday life. This means using locally appropriate language, offering culturally safe telehealth spaces within communities, and integrating support from primary care clinics. When done well, DHTs go beyond convenience to enhance deliver of quality care closer to home. Community-based telehealth enables patients to involve family if so desired by the patient, reduce unnecessary travel, and engage more fully in their care. For health professionals, it improves work-life balance, offers timely clinical support and eases professional isolation, especially for those working remotely. As one RAN shared: ‘I had a patient with cellulitis, and I was a bit worried - can I send them home with oral antibiotics, or do they need IV antibiotics? I needed a second opinion. If someone were always there on telehealth, it would be easier to get that help.’
CHALLENGES THAT CAN’T BE IGNORED
Trust plays a critical role. ‘Our people don’t trust very easily,’ another health worker said. ‘They don’t come to the clinic because they don’t know people.’ Familiarity with providers who know the local community builds comfort and credibility. The therapeutic relationship is just as important as the treatment itself. As a GP noted, ‘50% at least’ of the impact in patient care stems not from treatment, but from trust and connection. In remote communities, where cultural safety, continuity of care, and communication barriers affect outcomes, trust is critical. Health professionals in remote areas are not just delivering clinical services; they are building relationships that influence whether patients feel safe, respected, and willing to engage in ongoing care.
It’s impossible to ignore the challenges for the staff behind the screen. Telehealth only works as well as the people who make it possible. In many remote communities,


healthcare workers are often overextended due to staff shortages in remote areas. ‘We’re bombarded. On weekends, we’re covering morning and evening alone,’ a nurse said. However, it is not only staff shortages that create challenges, but also high staff turnover rates that impact the continuity of care and maintaining operational knowledge, including around digital tools. A GP recalled the challenges of using an earlier telehealth setup that involved a portable computer: ‘No one knew how to use the machine properly due to the staff changeover’.
LOOKING AHEAD
Despite progress, there’s still a long road ahead to make DHTs truly work for person-centred care, in remote communities. Getting there means more than just tech — it demands real investment in culturally safe care models, rock-solid digital infrastructure, and strong local workforces.
Success hinges on deep partnerships between communities and health services. That’s why our project team is working shoulder-to-shoulder with key partners — including the NT Department of Health, the Australian Government Department of Health, Disability & Ageing, Aboriginal Medical Services Alliance NT, NT Primary Health Network, the Australian Digital Health Agency and Healthdirect - to turn our findings into action that matters.
Workshops are underway to chart practical, respectful pathways for applying what we’ve learned. As more remote health services roll out tech-enabled hybrid

models of care utilising a combination of in-person and telehealth consultations, the opportunity is clear: balance the value of face-to-face relationships with the convenience of timely, remote support, ensuring continuity of care and care that remains close to culture, community, and country.
Authors: This article was prepared by Nicki Newton, Josielli Comachio, Vishnu Khanal, Kureisha Wilson, Emily Saurman, Amy Von Huben, John Wakerman, Bronwyn Rossingh, Lou Sanderson, Julia Coshan, Timothy Shaw and Deborah Russell on behalf of the project team. The project team includes researchers from the Menzies School of Health Research and the University of Sydney, in collaboration with policy makers, administrators and health professionals from Australian Government Department of Health, Disability and Ageing, Northern Territory Department of Health, Aboriginal Medical Services Alliance Northern Territory, Northern Territory Primary Health Network, Australian Digital Health Agency, and Healthdirect Australia. The project is supported by the Digital Health CRC Limited (DHCRC). DHCRC is funded under the Australian Commonwealth's Cooperative Research Centres (CRC) Program.
Aerial view of a remote island community in Australia’s Northern Territory
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CROHN’S & COLITIS
AUSTRALIA LAUNCHES LANDMARK REPORT
ON IBD
Highlighting the Human Cost Behind the Statistics

In February 2025, Crohn’s & Colitis Australia (CCA) released its State of the Nation in Inflammatory Bowel Disease (IBD) in Australia report at Parliament House, with the Hon Mark Butler MP, Minister for Health and Aged Care, officially launching the findings.
The report presents the most comprehensive picture to date of how Crohn’s disease and ulcerative colitis affect Australians—socially, economically, physically and mentally. It highlights the unique challenges faced by people living with IBD in regional Australia and underscores the need for equitable access to timely diagnosis and effective treatment.
Led by Associate Professor Greg Moore and Leanne Raven from CCA, the report combines in-depth research, economic modelling, and patient perspectives to highlight the growing urgency for a national response.

INCIDENCE OF IBD IN AUSTRALIA
An estimated 180,000 Australians are currently living with IBD, with more than 91,000 experiencing active symptoms. While IBD rates are rising globally, Australia is seeing one of the fastest increases. The projected growth in IBD prevalence here is expected to outpace that of Canada, the UK and New Zealand. Young people aged 15–29 are most affected, disrupting key life milestones like study, work and relationships.
THE IMPACTS OF LIVING WITH IBD
The journey to an IBD diagnosis is often long and complex, over one in three people experience symptoms for more than a year before being diagnosed. Delays in diagnosis lead to delayed treatment, with more than 40% of patients reporting it took over five years to bring their condition under control, despite an average remission time of three years.
Crohn's & Colitis CEO Leanne Raven with the Hon mark Butler MP
People with IBD are among the most frequent users of hospital services, with higher rates of hospitalisation and emergency department visits per case than cancer. Many experience symptoms beyond the gut, including joint pain, skin conditions, eye disease and increased risk of colorectal cancer.
The mental health burden is high: one in two experience anxiety, one in three report depression, along with fatigue, brain fog and insomnia. Up to 22% of children with IBD miss school due to symptoms.
IBD places a major financial strain on patients, families and the health system, costing Australia an estimated $7.8 billion in 2025 and $77.9 billion over the next decade.

PUTTING A FACE TO IBD: LUKE ESCOMBE’S STORY
At the launch, CCA Ambassador and performer Luke Escombe shared a moving personal story, offering a powerful reminder that statistics don’t tell the full truth.
“I once heard a quote: ‘Statistics are just human beings with the tears wiped off.’ Today, I want to put the tears back on.”
Diagnosed with Crohn’s disease at 14, Luke spoke of the pain and isolation he experienced before getting the help he needed.
“I remember the pain sitting on hard benches at school. It was sharp and dull all at once. I was terrified to tell anyone. When I finally did, the GP told my mum I was faking it.”
That pain turned out to be a tennis-ball-sized abscess—a common complication in Crohn’s disease. Though Luke was diagnosed within six weeks, he urged listeners not to be misled by timelines alone.
“Six weeks sounds fast. But it was six weeks of intense pain, fear, and self-doubt. That’s what each data point in this report really represents—real people suffering in silence.”

The emotional toll lasted much longer. Luke described losing friendships, confidence, and his sense of self.
“By 18, I was a shadow of who I’d been at 13. IBD didn’t just affect my body—it changed the course of my life.”
His story also reflected the broader family impact:
“I remember my mum breaking down on the eve of my 15th birthday because I was back in hospital. I had to be the one to comfort her. IBD affects the whole family, not just the person living with it.”

LIVING WITH IBD IN REGIONAL AUSTRALIA
Around 73,000 Australians with IBD live in regional areas, where access to care is often limited. People in rural and remote communities face higher rates of hospitalisation and poorer access to primary healthcare than those in major cities. Specialist care is scarce, meaning many patients must travel long distances for appointments, tests or treatment, often during painful flare-ups.
Limited access to multi-disciplinary care can lead to fragmented treatment, with patients seeing only one or two specialists rather than a coordinated team. While essential medications like biologics are subsidised through the PBS, delays in mail delivery, stock shortages at local pharmacies, and the need to travel for infusions all add to the burden.
These challenges, combined with the physical and emotional toll of the disease, highlight the need for improved, locally accessible, high-quality IBD care across regional and remote Australia.
IMPROVING IBD OUTCOMES FOR AUSTRALIANS
CCA has submitted a national IBD strategy to the federal government calling for:
• A National IBD Clinical Standard
• A “Living Well with IBD” support program
• A comprehensive IBD patient registry
• Targeted research funding through the Medical Research Future Fund
“We need to act now,” said Leanne Raven. “This report is not just about numbers—it’s a call to improve quality, equity, and access for the tens of thousands of Australians living fearlessly with IBD.”
Explore the full report and proposed solutions: IBD State of the Nation
Author: Leanne Raven is the CEO of Crohn’s and Colitis Australia
Luke Escombe, CCA Ambassador
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

ROTAVIRUS RESEARCH WITH WORLDWIDE IMPACT
A collaborative research initiative underway in communities across the Northern Territory aims to reduce the global burden of diarrhoeal disease in young children.
REDUCED ROTAVIRUS EFFECTIVENESS IN REMOTE AREAS
Each year, diarrhoea kills more than half a million children, predominantly in the world’s resource-poor, remote settings. Almost one-third of these deaths is attributed to rotavirus, despite the availability of an effective vaccine used widely throughout the globe.
Here in Australia, routine rotavirus vaccination coverage is high, yet vaccine effectiveness is lower among Aboriginal and Torres Strait Islander populations.
Professor Tom Snelling, from The University of Sydney and The Sydney Children’s Hospitals Network, with an honorary affiliation with the Wesfarmers Centre of Vaccines and Infectious Diseases, based at The Kids Research Institute Australia, said diarrhoeal disease remained an important cause of hospitalisation and health inequity among Aboriginal babies living in remote Northern Australia.
‘Our research has shown us that rotavirus hospitalisations in remote communities are significantly higher for Aboriginal and Torres Strait Islander children, with evidence showing waning protection from the rotavirus vaccine after the first year of life,’ Professor Snelling said.
‘We needed to work out why this is the case, and what can be done to optimise the effectiveness of the rotavirus vaccine - not just for children living Australia’s rural and remote communities, but also for populations affected by diarrhoeal disease around the world.’
NATION-WIDE COLLABORATIVE APPROACH
Professor Snelling is leading the Optimising Rotavirus
Cultural Advisors Nolene Dungun and Ada Parry with Aboriginal Health Practitioner Gregoriana Parker in Wadeye, NT
Vaccine in Aboriginal Children (ORVAC) Study, which aims to investigate if administering an additional booster dose of oral rotavirus vaccine to Aboriginal babies aged six to 12 months could provide stronger, longer-lasting protection against rotavirus.
Developed as a Bayesian, double-blind, randomised, placebo-controlled trial, the design provides the unique benefit of allowing frequent analysis of data and permits the study to stop as soon as a valid conclusion can be made.
‘Using the Bayesian platform trial design really makes this study stand out – there is no unnecessary burden on families or time wasted in order to meet a pre-determined number of participants, plus the data can be analysed quicker and resulting policy changes can be made significantly earlier,’ Professor Snelling said.
Funded by the National Health and Medical Research Council and conducted in partnership with Aboriginal health services across the Northern Territory, ORVAC involves researchers from The University of Sydney, Menzies School of Health Research, Murdoch Children’s Research Institute, The Kids Research Institute Australia and The University of Western Australia.
ORVAC began recruitment in 2018 and has now enrolled 871 Aboriginal babies across remote Northern Territory communities.
Dr Bianca Middleton, paediatrician and Senior Research Fellow at Menzies School of Health Research in Darwin, said early findings have already indicated enhanced immune response from a booster dose oral rotavirus vaccine.
‘ORVAC is made up of two stages – the initial stage focusing on the immunological response, followed by an on-going follow-up period looking at clinical responses,’ Dr Middleton said.
‘We are now in the second stage, checking in on the families to see if a booster dose of oral rotavirus vaccine led to decreased medical attendance due to diarrhoea.
‘If successful, we expect that the findings will inform updates to the National Immunisation Schedule for children living in rural and remote areas, as well as influence global recommendations for settings where rotavirus vaccine effectiveness is suboptimal.
‘We also hope that ORVAC demonstrates that highquality, complex research is achievable in remote settings, paving the way for future trials in similar geographical and logistical contexts,’ Dr Middleton said.

BUILDING COMMUNITY PARTNERSHIPS
Conducting research in Australia’s top end comes with significant challenges, including managing the logistics around the movement of samples, access to infrastructure and equipment and difficult weather conditions.

Culturally appropriate involvement of communities and families is also essential, and this has been achieved thanks to guidance from Aboriginal health services and capacity building opportunities provided to develop a skilled, locally engaged workforce.
This includes Aboriginal Health Practitioner Gregoriana Parker, who joined the ORVAC team when the study began and attended the community visits alongside the team’s study nurse.
‘This work is very important because it helps children have better health and gives families knowledge they can use to care for their babies and stop sickness,’ Gregoriana said.
‘The families talked about how worrying it is when their little ones get sick, and they appreciated having the chance to sit down with us, to talk, and to listen to what’s good for their babies’ health.
‘They were very happy to be in involved in the study and interested to learn more about how to stop this diarrhoeal disease,’ Gregoriana said.
Results from the first stage of ORVAC were published in the Journal of Infectious Diseases in 2022, and final results are expected to be available in mid-2026.
Authors: Professor Tom Snelling is a paediatric infectious diseases physician and clinical researcher based at The University of Sydney and the Sydney Children’s Hospitals Network, with an honorary affiliation with the Wesfarmers Centre of Vaccines and Infectious Diseases, based at The Kids Research Institute Australia. As Chief Investigator of ORVAC, he provides scientific leadership for the trial.
Dr Bianca Middleton is a paediatrician and Senior Research Fellow at Menzies School of Health Research in Darwin. She works clinically at Royal Darwin Hospital. In the ORVAC Study, she plays a key coordinating role, bringing together her clinical, research, and community engagement expertise to support trial delivery in remote Northern Territory communities.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
REVOLUTIONISING RURAL PAEDIATRIC CARE

PARIS on Country Brings
Lifesaving
Respiratory Treatment Home
PARIS on Country is transforming paediatric respiratory care across Far North and NorthWest Queensland by helping more children receive advanced treatment close to home.
When a young child in remote Queensland becomes seriously ill with respiratory distress, the difference between stabilisation and escalation can hinge on how quickly they access effective care. For some families, that has traditionally meant airlifting their child hundreds of kilometres away to tertiary hospitals.
Now, a pioneering research initiative— PARIS on Country—is changing the trajectory of paediatric emergency care across remote Australia. Led by Associate Professor Donna Franklin, Paediatric Acute Respiratory Intervention Study (PARIS) on Country is empowering clinicians in 14 rural and remote hospitals to treat acute paediatric respiratory illness locally, using proven interventions and tailored training that reflect the realities of care in remote Australia.
‘We want to see more families supported close to home and country,’ says A/Prof Franklin, a paediatric research fellow and nurse with over 30 years of clinical experience. ‘When a child is unwell, it affects the whole family. The emotional, cultural and financial toll of transfers, especially for Indigenous families, can be immense.’

RESPONDING TO GAPS IN RURAL AND REMOTE HOSPITALS
Co-funded by EMF and the Medical Research Future Fund (MRFF), PARIS on Country builds on over a decade of research. It all began with the original PARIS trials, funded by EMF, that demonstrated the effectiveness of nasal high flow oxygen therapy, a simple, non-invasive method of delivering breathing support. This reduced the need to escalate care for infants and young children with bronchiolitis and other respiratory conditions. The initial trials involved hospitals across Australia and New Zealand, both tertiary and regional, and resulted in widespread practice change, with findings published in journals including The New England Journal of Medicine and JAMA.
Yet despite the demonstrated effectiveness of high flow therapy, rural and remote hospitals remained underserved. Recognising this gap, a follow-up study known as PARIS Remote, led by PhD candidate and nurse researcher Ms Sally West, successfully introduced the therapy to remote Queensland sites including Cooktown, Weipa and Thursday Island. This project not only trained local clinicians, but also developed clinical guidelines and educational materials - laying the foundation for the broader, more ambitious PARIS on Country.
PARIS on Country has taken this model further. With 14 participating sites, including Innisfail, Mareeba, Bamaga, Cloncurry and other remote communities across three Queensland Hospital and Health services, the program introduces a respiratory care bundle for children under five, ensuring that local hospitals are equipped and educated to provide timely, evidence-based treatment. Crucially, the research responds to direct feedback from Indigenous parents who voiced a strong belief that care could, and should, be delivered locally, close to family and community. The program is a direct response to this call for equity, cultural safety and respect.
‘Some people questioned whether high flow could ever be used safely outside intensive care, let alone in rural or remote settings,’ A/Prof Franklin recalls. ‘We were told we were cowboys. But now, thanks to years of work and clear outcomes, regional centres are often outperforming tertiary hospitals when it comes to early respiratory intervention.’


CREATING A SKILLED AND RESILIENT REMOTE HEALTH SERVICE
A vital component of the program is its ‘Train the Trainer’ model. Local nurses, including researchers and clinicians, are upskilled to educate their peers, ensuring clinical knowledge and practical capability remain within the community. This peer-led approach not only builds confidence - it fosters resilience within remote health services, which are often the only line of care in regions where transfers can be delayed by extreme weather, flooding or even camel crossings.
PARIS on Country aims to halve the current paediatric transfer rate, reducing it from 25% to 12.5%, and an accompanying economic evaluation will assess the costeffectiveness of the model based on air medical transports avoided.
‘This is about equity,’ says A/Prof Franklin. ‘All children deserve the same timely access to life-saving care, regardless of where they live.’For EMF, this project underscores the value of investing in clinician-led research that is grounded in local needs. Supporting research like PARIS on Country reflects EMF’s commitment to funding projects led by clinicians across a range of disciplines and experience levels, from first-time investigators to established researchers, with a strong focus on improving care in rural, remote, and regional settings.
As the latest chapter in the PARIS story unfolds, it’s clear that the vision behind PARIS on Country, that healthcare that is responsive, local and culturally safe, is already transforming outcomes for some of Queensland’s most vulnerable children.
Author: Associate Professor Donna Franklin is a paediatric nurse, researcher and educator with over 30 years’ clinical experience. Based at Gold Coast University Hospital and Griffith University, she leads the PARIS on Country project, focused on improving paediatric respiratory care for children in rural and remote communities.
Article submitted by Emergency Medicine Foundation
A/Prof Donna Franklin with a family in Weipa
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
RURAL COMMUNITIES


Associate Professor Simon Edgerton
Heart
disease remains
a leading cause
of death in many rural and remote parts of Australia. Incidence rates, relative to metropolitan areas, increase by 40% in outer regional areas and by 300% in remote areas, with co-occurring levels of disease burden.
For people living in these areas, getting early checks and treatment can be a real challenge. Long travel distances, lengthy wait times, and high costs often make accessing care difficult.
THE NEW INNOVATION SUPPORTING RURAL COMMUNITIES
To address this, a team of La Trobe researchers have collaborated with the rural communities of Mildura and local clinicians to create an easy-to-use Heart Health Check Kit designed specifically for rural communities. This innovative kit allows individuals to check key heart health indicators right at home or at their local pharmacy - no need for a doctor’s visit.
Associate Professor Simon Egerton from La Trobe University, who is leading the project, explains:
‘Rural communities face significant barriers to the standard model of care, including lengthy waits, long distances to travel, and high out-of-pocket expenses. Our goal with this Heart Health Check Kit is to remove those barriers and make it easier for people to know their heart health status early.’Katrina Umback, rural and remote heart health advocate is part of the research team. She was named the 2025 Mildura Rural City council Citizen of the Year in recognition of her efforts to raise awareness about heart disease risks following the death of her husband.
‘In 2019, heart disease stole my 42-year-old husband’s life while we waited for care that was located 600kms from us and that never arrived in time. That should never happen in a country like Australia. After losing Scott to heart disease, I made a promise that no one in my community should ever be left behind like that again. This research gives me hope because the Heart Health Check Kit brings lifesaving prevention right to our doorsteps.’ she said.
‘It is more than data and devices; it’s about health equity. It’s about recognising that people in rural and regional communities deserve the same chance to live long, healthy lives as anyone else.’The kit includes portable devices to measure blood pressure, blood sugar, and cholesterol-critical factors in assessing heart disease risk. Once the test is done, results are sent back to individuals by phone or mail, along with clear guidance on next steps if any risks are detected.
Currently, the project is being piloted in the communities of Mildura, Lockington, Wentworth Shire, and Broken Hill.
‘If successful, this project will help us reach more people in rural and remote communities, enabling early detection


and better management of heart disease risks,” Associate Professor Egerton says. “This has the potential to save lives and improve health outcomes for some of Australia’s most underserved populations.’
WHAT DOES SUCCESS LOOK LIKE?
Success means more people in remote areas getting timely heart health checks - breaking down the barriers of distance, cost, and complexity. The H2Check-Kit is designed to fit seamlessly into everyday health services, helping doctors and health workers provide faster, smarter care. This leads to earlier detection, better treatment, and ultimately healthier lives.
Brooke Shelly is a GP Pharmacist at Ontario Medical Clinic in Mildura and project partner. As a rural clinician she sees the success of this project overcoming the greatest barrier to care in regional areas like Mildura.
‘By delivering care into people’s homes and local community pharmacies, it removes the single greatest barrier we face, access. These pharmacies are often the most accessible healthcare touchpoints we have, and the cornerstones of many rural communities. This is what place-based innovation looks like: designed with rural people, for rural people.’ she said.
The project team will gather strong evidence to refine the kit and prepare for larger clinical trials.
‘We hope to influence heart health policies across Australia, especially in underserved rural areas. This proactive, community-driven approach might even serve as a blueprint for tackling other health conditions,’ adds Associate Professor Egerton.
Working closely with partners like the Australian Heart Foundation, rural health networks, pharmacies, community health centres and local community, the team is ensuring the project meets real community needs and makes a lasting impact.
On completion of the feasibility study in 2027, findings will be shared with key policy makers to help inform and shape heart health care across the country.
Author: Associate Professor Simon Edgerton is the leader of the Regional Rural Remote Digital Health Research Group, as well as the director of the Technology Innovation Lab, at La Trobe University
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

RESEARCH, DISCOVERY, TRANSLATION AND KIDNEY FAILURE
Using genomics to get to the bottom of kidney disease for those who need it most


Connecting research, translation and kidney health in regional settings is critical to providing answers and minimising kidney disease and failure.

THE BURDEN OF KIDNEY DISEASE IN REGIONAL AUSTRALIA
Chronic kidney disease (CKD) presents a significant public health challenge in Australia, particularly in North Queensland, where prevalence rates are notably high across regional, rural and remote communities. The Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) reports an end-stage kidney disease (ESKD) prevalence of 1,586 cases per million people in this region, which is more than three times the state average for Queensland. Approximately 10% of ESKD cases remain unexplained despite the use of standard diagnostic tests, such as serology, imaging, and kidney biopsy, as highlighted in studies, including that by Robert and colleagues in 2023. This underscores the pressing need for regionally focused research to uncover the causes of kidney failure and improve outcomes for these underserved communities.
UNEXPLAINED KIDNEY FAILURE: A REGIONAL CHALLENGE
In North Queensland, unexplained kidney failure is a pressing issue, particularly in regional and remote settings where access to advanced diagnostics is limited. Patients often present late, at ESKD, with inconclusive kidney biopsy results showing nonspecific patterns like interstitial fibrosis or glomerulosclerosis. This diagnostic uncertainty complicates treatment, prognosis, and transplant planning, placing a significant burden on patients and healthcare systems. Conventional diagnostic tools often lack clarity, emphasising the need for innovative approaches to identify the drivers of kidney disease in this region.
GENOMIC MEDICINE: A REGIONAL SOLUTION
Genomic medicine is ideally positioned to clarify the high rates of kidney failure in North Queensland by identifying genetic variants associated with kidney disease. This approach enhances diagnostic accuracy, facilitates personalised treatment plans, and encourages family screening to prevent disease progression in individuals at risk. The KidGen Collaborative, a national leader in kidney genomics, has showcased the effectiveness of this strategy through a decade of innovative research and successful clinical application, whilst now being based in regional North Queensland.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

KIDGEN: PIONEERING REGIONAL GENOMIC RESEARCH
Over the past decade, KidGen has established a national network of 20 multidisciplinary kidney genetics clinics (MD-KGCs), as detailed in our study published in Kidney International Reports in 2024. This network has provided genomic testing for over 1,500 patients suspected of having monogenic kidney disease, achieving an overall diagnostic yield of 45.8%. Frequently diagnosed conditions included Alport syndrome (61.7% yield), cystic kidney disease (50.6% yield), and glomerular disease (38.0% yield), delivering actionable insights that impacted clinical management, including treatment and transplant decisions. This success culminated in a major achievement in 2022: the inclusion of genomic testing for kidney disease in Australia’s Medicare Benefits Schedule (MBS), ensuring sustainable funding and broader access to this essential healthcare service.
THE HIDDEN STUDY
KidGen’s national HIDDEN study focused on patients with unexplained kidney failure, which is particularly relevant to the challenges faced in North Queensland. In this prospective study of 100 patients under 50 with unexplained advanced kidney disease or kidney failure, whole-genome sequencing (WGS) achieved a diagnostic rate of 25%, identifying conditions such as autosomal dominant tubulointerstitial kidney disease and Alport syndrome. Notably, 13% of those without a family history received a genetic diagnosis, underscoring the utility of WGS in sporadic cases. Unlike kidney biopsy, which proved inconclusive in 24 out of 25 stage 5 patients, wholegenome sequencing was safer and more informative.
GENESIS: A REGIONAL TAILORED RESPONSE
To address the challenges of kidney failure in North Queensland, we are launching the GENESIS (Genomic Exploration for Navigating Chronic and End-Stage Kidney Disease and Shaping Innovative Solutions) Program, a transformative initiative integrating advanced genomics with a culturally safe and community-focused approach. GENESIS plans to enrol 1,000 patients across all stages of CKD at five health services across North Queensland, utilising both short-read and long-read WGS to identify genetic risk factors, including complex structural variants often overlooked by standard sequencing. The program’s multidisciplinary team, comprising nephrologists, geneticists, scientists, community leaders, and health economists, merges research with medicine to enhance diagnostic yield, personalise treatment, and reduce health disparities. The program seeks to bring the transformative power of translational genomic research and healthcare to regional, rural and remote Australia to identify answers to health issues, such as kidney disease, where they are arguably experienced the most.
CULTURALLY SENSITIVE REGIONAL DESIGN
GENESIS goes beyond monogenic concepts to examine social determinants, pharmacogenomics, and polygenic risk scores that predict CKD progression and its severe cardiovascular complications. By analysing hundreds of kidney-related genes and conducting annual data reanalyses, the program aims to uncover novel genetic associations and refine clinical pathways. Its culturally sensitive design, developed in partnership with local



communities, ensures ethical conduct and equitable outcomes, fostering trust and community ownership of health solutions.
IMPACT AND FUTURE DIRECTIONS
The GENESIS Program promises to reshape kidney health in North Queensland and serve as a model for regional research globally. By clarifying the genetic and social drivers of kidney failure, it will improve diagnostic rates, customise therapies, and inform policies to address CKD disparities. Its findings could reduce the incidence and mortality of ESKD while advancing the field of genomic medicine. Rooted in regional research, GENESIS demonstrates how place-based innovation can drive equitable healthcare delivery.
Through advanced genomics, regional expertise, and respectful community engagement, we aim to improve kidney health in North Queensland, fostering hope and equity in the fight against chronic kidney disease.
Authors: Professor Andrew Mallett is a leading expert in kidney medicine, clinical genomics and translation within these fields. He is a Professor of Medicine and Head of Discipline for Internal Medicine at James Cook University (JCU), and heads Australia’s first and largest renal genetics clinical service.
Dr Erik Biros is a distinguished medical researcher specialising in the molecular and genomic foundations of chronic diseases. Dr Biros leads national efforts to improve kidney health outcomes at the KidGen Collaborative, and is affiliated with JCU’s College of Medicine and Dentistry, and Townsville University Hospital.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

INNOVATIVE MUSCULOSKELETAL PROGRAM HEADS TO THE AUSTRALIAN BUSH
With musculoskeletal conditions the leading cause of disability burden, the PACERURAL trial will provide rural health professionals with virtual access to musculoskeletal specialists to create supportive professional relationships and improve patient outcomes for their most complex pain patients.
CQUniversity Associate Professor Katie de Luca is part of a national, multidisciplinary team who are tackling health inequalities in regional, rural and remote Australia.
Under the guidance of physiotherapists Professor Trudy Rebbeck and Associate Professor Kerrie Evans, both from The University of Sydney, a team of experts will implement a new model of care for musculoskeletal (MSK) conditions in rural and regional Australia.
MUSCULOSKELETAL
CONDITIONS ARE THE LEADING CAUSE OF DISABILITY BURDEN
Musculoskeletal conditions are the leading cause of disability globally, and access to high-value care remains inequitable. Traditional MSK care pathways contribute to the burden by following a fragmented, biomedical model. Few people are offered evidence-based care, and patients are quickly ‘stepped up’ to higher-costing and often unnecessary care such as imaging, surgery and preventable hospitalisations. People in regional, rural and remote Australia often face additional challenges such as geographic isolation, poor access to specialist allied health services and a higher prevalence of risk factors.
The team of clinician-researchers, who have secured $2.5 million from the Medical Research Future Fund, will implement and evaluate a pathway of care for people with MSK conditions in eight regions across Queensland, New South Wales, Victoria and Western Australia. The hybrid type II effectiveness-implementation trial involves a simple online tool at the point of care to identify people who may recover well and those who may not. People with back, neck, knee and hip pain who are likely to recover well can be guided by the online resource, mypainhub.com, which provides evidenced based advice to aid recovery.
EARLY ACCESS TO VIRTUAL CARE
People at risk of poor outcomes will receive timely virtual access to an expert allied health specialist. Using telehealth, the local health professional will work closely with an allied health specialist through an advanced assessment of risk factors to develop an individualised

treatment plan. Together, clinicians in the bush will be supported with telehealth to provide appropriate care for their most complex pain patients.
‘Telehealth provides a great way for patients and clinicians to connect and explore management strategies together,’ explains A/Prof Kerrie Evans FACP, from The University of Sydney and Healthia Limited.
‘This model enables real-time clinical reasoning and collaboration, with the aim of improving outcomes for people living with musculoskeletal pain.’
COLLABORATIVE CARE FOR PEOPLE WITH COMPLEX MUSCULOSKELETAL PAIN
PACE-RURAL offers a great opportunity for rural allied health professionals to be involved in a study that aims to ensure efficient and appropriate use of medical and allied health services. They will be provided with hybrid education (online and in person) and, importantly, PACERURAL will facilitate collaborative care for their patients at risk of poor outcome.
‘Many rural clinicians tell us they feel isolated when managing people with complex presentations,’ notes Dr Darren Beales FACP from Curtin University. ‘PACERURAL creates supportive professional relationships while enhancing clinical skills and improving patient outcomes.’
A/Prof de Luca adds, ‘Chiropractors, and all health care professionals, need to work within multidisciplinary teams to decrease the burden of musculoskeletal conditions. Here, chiropractors can partner with allied health specialists to improve health outcomes for high-risk individuals in rural and remote Australia.’

The PACE-RURAL team live and work in the regions where this project takes place. As a regional chiropractor located in South West Rocks in NSW, A/Prof de Luca understands the everyday challenges of regional clinicians.
‘Living and working as a chiropractor in regional Australia, my own musculoskeletal management plans are often limited by access to and communications with specialists and a limited rural workforce. We are usually short on time, and resources. However, our rural patients are resilient, often living with chronic pain and traveling for hours to receive treatment. This large-scale program, PACE-RURAL, will be offered across the country for the first time, providing a high quality and yet low-cost solution to managing complex musculoskeletal pain.’

Professor Rebbeck adds, ‘For many people living in rural and remote parts of Australia, one of the biggest challenges is access to specialised healthcare, so we hope that through this program, we will broaden access to evidenced-based, effective care and importantly, improve long-term musculoskeletal health.’
The PACE-RURAL project has been funded as part of a $20 million boost for improved primary care and chronic pain treatment. Working across several Universities and endorsed by key stakeholders, this project places CQUniversity at the forefront of finding health solutions for regional Australians.
GET INVOLVED IN PACE RURAL!
Would you like to participate? If you are a chiropractor, physiotherapist, general practitioner, osteopath or exercise physiologist, working in regional, rural or remote settings and regularly treat people with MSK conditions, you can join the PACE-RURAL study.
For more information, email the research team directly at pace.study@sydney.edu.au and visit the team’s LinkedIn page for updates.
Author: Katie de Luca is a registered chiropractor at South West Rocks in NSW and Associate Professor in the School of Health, Medical and Applied Sciences at CQUniversity. Her research focuses on the epidemiology and management of musculoskeletal conditions, with a particular interest in rural health and healthy ageing. She is the current Chair of the World Federation of Chiropractic Disability and Rehabilitation Committee and is a member of WHO World Rehabilitation Alliance research workstream. The PACE-RURAL trial is led by Prof Trudy Rebbeck, Conjoint Professor of Allied Health and Professor of Clinical Translation in Allied Health at The University of Sydney and Northern Sydney Local Health District.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

CLOSING THE RURAL CARE GAP


With inflammatory bowel disease (IBD) on the rise in Australia and rural patients facing the greatest barriers to care, a new digital care model is under trial in regional Queensland.
Combining real-time monitoring and remote clinical oversight, this innovation offers a scalable, cost-effective approach to improving quality of life and reducing pressure on hospital-based services.
A GROWING BURDEN, UNEVENLY CARRIED
IBD affects almost ~1% of Australians and is increasing at one of the fastest rates in the world. The recently released State of the Nation in IBD report highlighted an urgent need for systemic reform—placing the national economic burden of IBD at $7.8 billion in 2025, including direct healthcare costs, lost productivity, and reduced quality of life.
The impact of these costs is disproportionately felt by the 1 in 3 Australian IBD patients that live in rural, regional and remote communities. Rural Australians are faced with challenges of limited access to specialists, and fragmented follow-up care, leading to delayed diagnoses, increased time to remission, and suboptimal disease management. However, much of the personal, social and economic impact is avoidable.
FROM DATA TO ACTION – THE CCCURE DIGITAL MODEL
Crohn’s Colitis Cure (CCCure), in partnership with Royal Brisbane and Women’s Hospital, is piloting a digitally integrated care model in Rockhampton, Queensland. The study combines three innovative tools:
• CCCare : A web-based clinical platform that links an electronic medical record (EMR) with a clinical quality registry (CQR), enabling real-time disease management and tracking, as well as longitudinal data capture.
• IBDSmart: A mobile app that empowers patients to monitor and report their symptoms.
• IBDoc: A home self-test kit that measures faecal calprotectin, a key biomarker of gut inflammation. Together, these tools deliver a data-driven, patient-centred model of care that supports earlier intervention and
continuous monitoring. CCCare can also function as a guided practice tool, allowing specialists to support large regional patient cohorts by working alongside local clinical teams. This “one-to-many” model makes specialist input more scalable and sustainable—especially critical in areas with workforce shortages.
The 15-month randomised controlled trial involves up to 200 patients. Participants in the intervention arm use the digital tools from home, while a control group receives standard care. Researchers will assess quality of life, symptom control, disease activity, usability, and healthcare costs.
SHIFTING THE MODEL, LIFTING THE SYSTEM
This project offers more than convenience—it signals a fundamental shift in the delivery of chronic disease care in Australia. By leveraging real-time data and enabling a coordinated, distributed model of care, the approach simultaneously improves outcomes, advances equity of access, and drives greater affordability across the system.
Reducing reliance on face-to-face appointments and unnecessary reviews frees up clinical capacity for urgent needs. More importantly, it empowers patients with timely information and ongoing engagement. These are the hallmarks of modern, person-centred care.
CCCure’s goal is to transform care in IBD. This project is a clear example of that mission in action. This project is designed for scale and is already primed for broader application across the country. As the State of the Nation report made clear, modernising chronic care means more than adding services—it requires restructuring how care is accessed, delivered, and paid for. CCCare offers a powerful platform to do just that.
Author: Bill Petch is CEO of Crohn’s Colitis Cure (CCCure), a not-for-profit Medtech committed to transforming IBD care. CCCure is driving practical data led solutions to ensure timely diagnosis, consistent care, and better outcomes for people living with IBD, regardless of where they live.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
“I DON’T THINK I’M HEARING THINGS”
Tackling Hidden Hearing Loss in Regional, Rural and Remote Australian children.

Barriers like long wait times and limited access mean many Australian children miss out on hearing assessments—putting their development at risk.
In Australia, 75% of children with hearing loss have mild to moderate loss, yet these children are often missed by current hearing screening systems designed to pick up more severe hearing losses. Children with mild to moderate hearing loss may be starting life at a disadvantage, which can lead to delays in areas like speech and language. These delays can affect academic performance, social development, and opportunities later in life. For families living in regional, rural and remote communities, accessing health services to treat hearing loss and overcome speech and language delays can be difficult.
WHY SO MANY CHILDREN ARE BEING MISSED
Since 2001, Australia’s Universal Newborn Hearing Screen (UNHS) has improved the lives of millions of Australian children by identifying more severe hearing losses, and allowing children to access earlier assistance. For children who are not identified at birth, there are no consistent systems of follow up or re-assessment of hearing Consequently, many children with mild to moderate hearing loss can go undiagnosed until they are much older – often when they are already experiencing speech and language delays.
A recent PhD project explored this issue from the perspectives of parents, speech pathologists and clinical service leaders across Australia. It found that access to hearing services is strongly influenced by a family’s circumstances and understanding of the health system. Findings showed not all parents fully understand how hearing supports speech and language development. One parent said “I was just worried about his speech. I don’t even really think about hearing. And then the doctor recommended that before we look into speech therapy, to get his hearing tested.” Other parents didn’t realise that hearing loss might occur at any time in childhood so didn’t know to continue to monitor their child for signs of hearing loss. Often, those parents who struggle to understand the health system, are also the parents who need the services the most.
EXTRA CHALLENGES IN REGIONAL, RURAL AND REMOTE COMMUNITIES
Many of the barriers shared by stakeholders were unique to regional, rural and remote communities, particularly the shortage of trained audiologists. The Hearing Health Workforce Audit 2021 suggests the number of audiologists will increase exponentially by 2030, but it is unclear whether regional, rural and remote communities will benefit from this increase.
A coordinated, national plan, like the Roadmap for Hearing Health, a strategic plan by the Australian Government aimed at improving hearing health, needs to do more to support training and incentives for regional, rural and remote health professionals. For instance, government policy needs to reflect the importance of promoting work for health professionals in these areas, by offering incentives such as financial assistance, housing allowances, and professional support and mentoring. Targeting students at universities

through offering regional and rural placements and basing campuses outside of major cities can encourage health professionals to seek jobs in such communities.
INNOVATIVE SOLUTIONS FOR A LONGSTANDING PROBLEM
Audiology is currently identified as a skill shortage in Australia. Scholarships and financial incentives are already available for students who work in regional, rural and remote areas, but could be more strategically applied to healthcare professionals with known shortages. Australia’s new migration policies could prioritise skilled audiologists who want to live and work in regional, rural and remote communities, and consider offering a smoother path to permanent residency.

Currently, hearing screening and assessment postnewborn screening are not regulated, which means they are inconsistent, and at times non-existent, especially outside of major cities. This leads to children with mild to moderate hearing loss, particularly those living in regional, rural, and remote communities, slipping through the cracks, preventing access to early intervention that could help them thrive.
The Deadly Kids: Deadly Futures in Queensland exemplifies how ongoing monitoring for hearing loss and culturally responsive care can be effective. Expanding and adapting this framework nationally could improve access to necessary healthcare for all children with hearing loss.
A nationally coordinated, equitable approach to hearing services for all children would support access to early intervention, reducing speech and language delays. This approach should include regular hearing checks, especially for at-risk children, and be co-designed with families and communities to ensure that it is culturally appropriate, easy to navigate, and addresses the needs of each specific community.
WHAT’S NEXT?
Hearing loss – especially mild – can be invisible but its impact is not. Even mild hearing loss can result in speech and language delays meaning children are not reaching their full potential. This is particularly disheartening knowing some of those delays could have been avoided if needed healthcare was received. For all Australian children to have the best start to life, they need access to clear hearing. We need to come up with innovative solutions to overcome the barriers to hearing assessments for all children in Australia. We know what the barriers are. Now it’s time to remove them.
Author: This article was developed by Dr Jenna Zussino, a Speech Pathologist who completed her PhD at Central Queensland University. Her PhD project was supervised by Associate Professor Barbra Zupan and Dr Robyn Preston, both at Central Queensland University.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
RESTACKING THE ODDS FOR CHILDREN AND FAMILIES

Restacking The Odds (RSTO) is a collaboration between Murdoch Children’s Research Institute, Social Ventures Australia and Bain and Company. We’re empowering early years service providers, community initiatives and governments with the data and skills they need to improve
Australia’s early childhood services.
Experiences in the early years have a lasting impact on children’s health, development and wellbeing. High-quality, evidence-informed early childhood services are a vital piece of the puzzle –putting children on the path to fulfil their potential.
Currently in Australia, many children can’t access, participate in or make the most of high-quality early years services, causing them to fall behind their peers before they’ve even started school.
These inequities are more pronounced in rural, regional and remote areas, where services may be in short supply or families must travel a far distance to reach them.
To address this, Restacking the Odds (RSTO) is empowering local communities, service providers and governments with the data and skills they need to improve the quality, quantity and participation rates of Australia’s early years services.
Ebony Lee, Early Years and Engagement Leader at Gowrie Victoria, an early childhood education and care centre that is partnering with RSTO.
We’ve recently partnered with Minderoo Foundation to scale RSTO nationally and reach more children and families across Australia, particularly in rural, regional and remote communities.
By focusing on the early years and enabling locally led solutions, RSTO is creating the conditions that ensure all children can thrive.
DRIVING EQUITY THROUGH STACKING
Children’s health, development and wellbeing can be improved by ‘stacking’ or combining multiple early years services. RSTO focuses on strengthening five key services that we know support good outcomes for children: antenatal care, sustained nurse home visiting, early childhood education and care, parenting programs and the early years of school.
These five services have a profound impact on child health and development. They support children throughout early childhood, engage both children and their parents, and are backed by evidence. RSTO research shows that the positive effects of these services are amplified when they’re accessed together, or ‘stacked’, with children boosting their learning outcomes by participating in two or more high-quality, evidence-informed services simultaneously.
‘Instead of relying on a ‘silver bullet’ solution, stacking utilises more of what our system already offers and ensures it can meet the unique needs of Australian families,’ said Sharon Goldfeld, Director of the Centre for Community Child Health at Murdoch Children’s Research Institute.
RSTO supports communities, governments and service providers to strengthen and ‘stack’ early years services by offering a lead indicator framework, a data dashboard, and a training program that equips partners to collect, monitor and use data on quality, quantity and participation to inform action.
RSTO’s innovative use of evidence-informed lead indicator data enables front line workers to see how they’re doing and adjust in real-time – allowing them to make more effective and timely improvements.
OUR IMPACT
We currently partner with nine service provider organisations and 15 community sites, including two Child and Family Hubs and two place-based initiatives across Victoria, South Australia, NSW and Queensland.
For Ebony Lee – Early Years and Engagement Leader at Gowrie Victoria, an early childhood education and care

centre – RSTO has been pivotal in enabling her team to make more informed decisions about continuous improvement.
‘I’ve loved learning about the story stats can tell,’ said Ebony.

‘Over time, [the staff] really started to see the value [of RSTO] and could see, when they implemented something, a difference in the stats that RSTO is presenting.
‘Coming together to put a plan in place has great benefits and supports us to do the best we can for our community.’
Their efforts have led to notable increases in participation rates among children and families disproportionately affected by inequity in the early years.
REACHING MORE COMMUNITIES
RSTO is proud to have recently partnered with Minderoo Foundation to scale nationally, and place data, lead indicators and tools for action into the hands of early childhood service providers in more communities across Western Australia, Queensland, New South Wales and South Australia.
‘We know that community-driven solutions are often the most effective and sustainable solutions,’ said Penny Dakin, Communities Executive Director, Minderoo Foundation.
‘Restacking empowers local people with the information they need to deliver locally relevant and responsive services for children and their families.’
Minderoo’s investment of $8,550,000 over three years will support RSTO’s work equipping early years services and communities with the skills to use data for continuous improvement.
The partnership will contribute to Minderoo Foundation’s vision to see all children in Australia reach their full potential in thriving communities, and RSTO’s vision to tackle inequities in early childhood.
For more information about Restacking the Odds, visit rsto.org.au
Authors: Jasmine Lykissas, Communication and Engagement Lead, RSTO, Murdoch Children’s Research Institute; and Olivia Hilton, General Manager, RSTO, Murdoch Children’s Research Institute.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
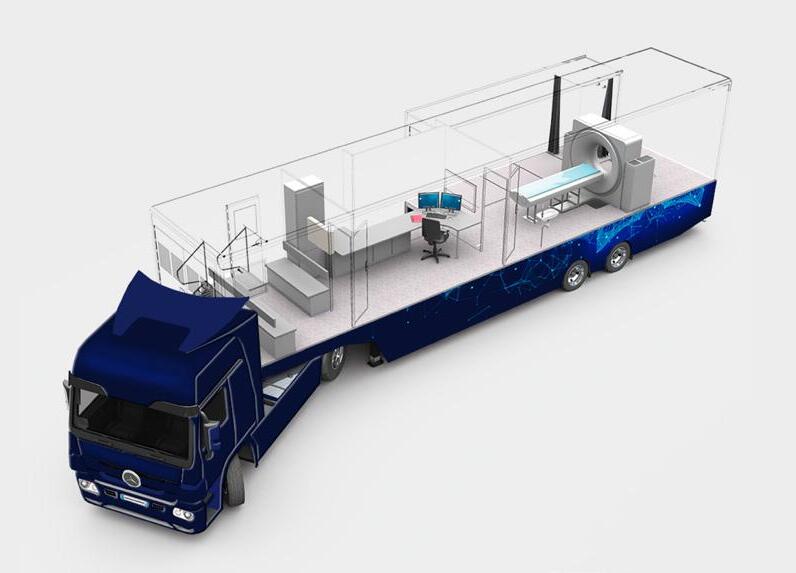
ON THE ROAD TO BETTER CARE FOR LUNG CANCER
A novel approach will hugely benefit Australians in rural, remote and Indigenous communities with limited access to cancer screening
Asemi-trailer will become the world’s first mobile lung cancer screening research platform integrating imaging and biomarker testing to help boost early detection and increase survival rates.
Construction of the ACRF Lung Cancer Screening Centre of Excellence (LUSCE) mobile facility will be completed this year and integrates imaging, breath and blood biomarker screening research. It is an initiative of The University of Queensland’s Thoracic Research Centre and funded by Australian Cancer Research Foundation (ACRF).
LUNG CANCER IN AUSTRALIA
Lung cancer has the highest mortality rate of all cancers, accounting for 1 in 5 deaths from cancer in Australia. The prognosis for lung cancer is poor, with a 5-year survival rate of only 21%, compared to 70.1% in all cancers combined. This is because lung cancer is typically diagnosed at an advanced stage after it has spread to other parts of the body.
University of Queensland (UQ) researcher and Prince Charles Hospital thoracic physician, Professor Kwun Fong said lung cancer has a high potential cure rate, 67 per cent, if detected early. ‘Unfortunately, two thirds of patients present with advanced disease, when five-year survival is less than four per cent.’
EQUITY
IN LUNG CANCER SCREENING ACCESS
While the potential success of early detection is clear, lung cancer screening is not easily accessible to people living in regional areas.
‘Lung cancer also has a greater proportional impact on Aboriginal and Torres Strait Islander people, people in regional and rural areas, and those in lower socioeconomic environments,’ Professor Fong said.
Aboriginal and Torres Strait Islander people living in remote communities, who are statistically two times more likely to be diagnosed with lung cancer, are one and a half times more likely to die from the disease than nonIndigenous Australians.
This program will develop and test a novel, mobile, multiplatform for lung cancer detection research to identify new ways to reduce health disparities by ensuring equitable access to effective screening for rural and remote communities and at-risk populations.
There is opportunity through research to increase survival

from lung cancer and remove health disparities, closing the gap through access to screening.
THE ACRF LUSCE MOBILE FACILITY— A NOVEL APPROACH
Professor Fong said the ACRF LUSCE mobile research facility will help identify how multi-platform lung cancer screening can identify cancers at a stage when a cure is possible.
‘Early-stage lung cancer can normally be cured with surgery and radiation therapy, but most lung cancers are typically diagnosed late when curative treatments are not able to be offered.
‘With effective lung cancer screening technology accessible to all, we can save lives,’ Professor Fong said.
There is a stigma associated with lung cancer, and while the majority of cases are linked to smoking, 10% of males and 30% of females with lung cancer have never smoked. Research into lung cancer in these individuals is just one example of an area where further work is needed and where improved diagnosis could help.
A $2M grant from Australian Cancer Research Foundation helped fund the technology and equipment required for the program, including a fit for purpose CT scanner.
‘ACRF is proud to enable this pilot study to provide more equitable access to effective screening technology for all Australians. Having supported Professor Fong’s visionary


research in the past, we are confident this project has the expertise behind it to really make an impact,’ said Kerry Styrdom, CEO of ACRF.
A central part of ACRF LUSCE is the Australian Lung Screen Trial (ALST). ALST will research lung cancer screening in populations Aboriginal and Torres Strait Islander peoples and people at risk of developing lung cancer across a range of communities.
The program has been co-designed with Aboriginal and Torres Strait Islander community members and organisations. ACRF LUSCE will provide CT scans for the ALST.
Professor Gail Garvey, Professor of Indigenous Health Research at UQ is establishing a program focused on cancer and wellbeing of Australia’s First Nations People. A $5 million grant has been provided by the Federal Government to test a one stop cancer screening shop for Aboriginal and Torres Strait Islander people. ACRF LUSCE will be used to support this project.
Professor Garvey is also co-designing activities to garner support for the ACRF LUSCE project from Aboriginal and Torres Strait Islander organisations. Active engagement is also underway with a range of organisations and health services across Queensland continues including Inala Indigenous Health, Townsville Aboriginal and Torres Strait Islander Health and Carbal Medical Services in Toowoomba.
National screening programs have been effectively employed for breast, bowel and cervical cancers, and the screening program for lung cancer will be launched in July. This research project will provide new data to help inform and enhance the upcoming national lung cancer screening program.
Projects like LUSCE are only possible thanks to the generous individuals and businesses across Australia who support Australian Cancer Research Foundation.
Author: Australian Cancer Research Foundation
Professor Kwun Fong
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
STRENGTHENING CANCER CARE IN RURAL AND REMOTE AUSTRALIA THROUGH PARTNERSHIPS AND INNOVATION
The ECORRA program’s collaborative approach to partnerships, consumer engagement, and place-based research offers a powerful framework for healthcare equity in rural and remote Australia.
When Sarah from remote Queensland received her cancer diagnosis, the nearest oncologist was 800 kilometres away. Her story mirrors thousands of Australians living in rural and remote areas who face the stark reality of having their postcode risk their cancer outcome.
But communities across rural and remote Australia are working together to change this narrative. They
are partnering to develop meaningful, strategic, and sustainable approaches to cancer care delivery. The Equitable Cancer Outcomes for Rural and Remote Australia (ECORRA) program is based on the principle that distance doesn’t have to mean disadvantage.
THE RURAL AND REMOTE REALITY CHECK
Rural and remote Australians consistently experience poorer cancer outcomes than their urban counterparts. Late diagnoses, delayed treatments, and limited access to specialist care create a storm of health inequity.
Yet within this challenge lies an unprecedented opportunity. Rural and remote communities bring unique strengths to healthcare challenges through their tight-knit networks, resourcefulness, and determination to look after their own.
ECORRA is a comprehensive research program supported by over $6.1 million in federal and state funding. Led by the Centre for Quality and Patient Safety Research within the Institute for Health Transformation at Deakin University,

Pictured (left to right): Dr Rebecca Bergin, Dr Charlene Wright, Dr Anna Chapman, A/Prof Skye Marshall, Prof Anna Ugalde, Sharina Riva, and Hannah Jongebloed from the ECORRA research group. Not pictured: Helena Rodi and Laura Sergeant.

the program addresses rural cancer care inequities by harnessing local strengths and dismantling structural barriers. The initiative comprises three complementary projects that generate evidence, develop solutions, and test real-world implementation:The ECORRA Trial is a fiveyear initiative working to reduce delays in cancer diagnosis and treatment across rural and remote Australia. Through co-design with communities and health services, the trial is developing and testing an implementation package that aligns local services with the Optimal Care Pathways.
• The ECORRA Optimal Care Pathways project responds to a key gap in the 2023 Australian Cancer Plan by developing a best-practice cancer care framework tailored to the rural and remote context.
• The ECORRA Vic project identifies factors associated with delayed diagnosis and treatment across Victoria and provides evidence-based recommendations through statewide surveys and broad stakeholder engagement.
Together, these projects inform a scalable, sustainable model for equitable cancer care.
FOUR GAME-CHANGING STRATEGIES
Four strategies underpin ECORRA’s success, each representing a fundamental shift in how rural healthcare challenges are approached.
Partnership Power: ECORRA’s foundation isn’t cuttingedge technology or million-dollar equipment. It’s a collaborative framework that brings together more than 100 stakeholders spanning health services, community organisations, government agencies, and universities. These partnerships pool resources and expertise in ways that multiply impact.
Complex problems require collaborative solutions. When organisations move beyond their silos and work towards shared goals, systemic problems can be improved.
Listening to Lived Experience: Seventeen rural and remote Australians form an essential element of the programECORRA’s National Consumer Program. These aren’t token representatives wheeled out for consultation meetings. ECORRA’s consumer members are integral to program development, conduct, and dissemination, bringing insights that no amount of research data can capture. A formal charter establishes clear roles, training, and fair compensation. Consumer co-chairs provide leadership to the group, ensuring that the consumer voice remains central to decision-making processes.
Place-Based Precision: One size doesn’t fit all in rural and remote health. ECORRA’s research team spend significant time in communities, conducting site visits, public consultations, and in-depth interviews. They understand that each rural and remote community has unique characteristics that require tailored healthcare solutions.
Evidence-Based Implementation: approach to building evidence whilst maintaining community connections underpins all of ECORRA’s work.
This systematic program demonstrates that sustainable healthcare improvement requires comprehensive research, genuine partnership with the communities being served, and sustained commitment to long-term change.
RECOGNITION AND PROMISE

This research team is an Implementation Partner of the Australian Cancer Plan. Cancer Australia and Deakin University, via the Institute of Health Transformation, have come together in partnership to implement activities that support achieving the goals of the Australian Cancer Plan.
There is confidence in ECORRA’s methodology of genuine partnership, consumer engagement, and place-based research. The program’s systematic approach to building evidence whilst maintaining community connections positions it to deliver the coordinated care that Australians like Sarah need.
BEYOND CANCER CARE
ECORRA’s framework transcends cancer treatment. The principles of genuine partnership, consumer engagement, and place-based solutions offer a blueprint for addressing rural and remote health challenges.
As Australia grapples with workforce shortages, ageing populations, and increasing demand for health services, ECORRA demonstrates the potential for rural and remote communities to lead healthcare innovation.
THE PATH FORWARD
Launched in 2024, the program’s initial success has sparked new conversations. Are we genuinely engaging with the communities we aim to serve? Are our partnerships authentic or merely transactional? Do our solutions reflect real-world constraints and opportunities?
ECORRA provides more than a program, it provides a path. A path to equity, collaboration, and care that reflects the needs of all Australians. For Australians like Sarah, and thousands like her, it represents access to the care they deserve.
Authors: Dr Charlene Wright, Helena Rodi, A/ Prof Skye Marshall, Prof Anna Ugalde, and the ECORRA research group are part of the Institute for Health Transformation at Deakin University. They specialise in advancing meaningful and sustainable patient-centred, evidence-based cancer care for rural and remote Australians. For further information and a full list of ECORRA partners and collaborators please visit the ECORRA website
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

BOLSTERING REGIONAL, RURAL, REMOTE AND VERY REMOTE HEALTH AND MEDICAL RESEARCH AND INNOVATION
Charles Sturt University Orange Campus

Nearly 30% of Australians live in regional, rural, remote or very remote (RRRvR) communities –critical to the nation’s prosperity, culture, and identity, offering unique strengths shaping Australia’s economic and social fabric.
RRRvR research, researchers, and research institutions excel in connectivity and co-design, establishing research priorities led by local needs and impactful service delivery models. Infrastructure such as regional universities, rural health departments and research institutes are essential to local communities – contributing to both healthier communities and healthier local economies.
Despite the strengths of RRRvR communities and health and medical research and innovation, communities face unique challenges, including funding inequities, workforce gaps and research infrastructure gaps.
To address these issues, Research Australia convened a regional university steering committee to draft a discussion paper, ‘Advancing Health and Medical Research and Innovation Across Regional, Rural, Remote and Very Remote (RRRvR) Communities in Australia’1 – summarised for this edition of INSPIRE
RRRVR POLICY AND FUNDING LANDSCAPE
RRRvR health and medical research and innovation sits within a complex, fragmented policy and funding system and lacks dedicated strategic focus. There is an increased recognition of the disparities in health outcomes between RRRvR and non-RRRvR Australians. There is also a range of international frameworks (such as International Declaration on Rural Mental Health Research), national policy and funding policy statements (eg. MRFF and NHMRC or Closing the Gap National Agreement), and local declarations (eg. Orange Declaration on rural and remote mental health). However, national coordination remains absent.
The NHMRC (through the Medical Research Endowment Account, or MREA) and the MRFF are the main funding agencies; and both have expressed a commitment to funding research that improves health and wellbeing in RRRvR communities. Despite an increase in research activity since the MRFF began prioritising RRRvR in its grant opportunities, there remains a disproportionate number of applications received from lead or administering organisations located in RRRvR areas classified as Modified Monash Model 2 and above; and ongoing disproportionate investment; and the investment still does not match the need.
Based on publicly available NHMRC funding data between 2022 and now (post-covid), the Group of Eight
1 The Research Australia University Roundtable (the Roundtable), is a committee of Research Australia, providing a forum for discussion of matters of relevance to the University members of Research Australia which directly inform Research Australia’s policy and advocacy platforms.
universities received the highest share of NHMRC funding, accounting for over $1.27 billion, reflecting their dominant role in Australia’s research landscape. The Regional Universities Network received only $2.87 million, and all other universities and institutions received moderate funding. The concentration of funding in the Group of Eight suggests a strong preference for established research infrastructure and capacity.
ADDRESSING THE CHALLENGES

In order to address these systemic challenges, we have identified 6 key priority areas:
• Secure sustainable funding and increase RRRvR allocation via reforms to funding and governance processes
• Recognise diversity, addressing intersectional discrimination in funding and policy systems
• Strengthen RRRvR research capacity through national research infrastructure alignment, better digital connectivity, data systems, facility access, and workforce training
• Invest in comprehensive workforce models focused on early to mid-career and clinician researchers, as well as research leadership
• Build genuine community partnerships, embedding principles into policy, assessment, and reporting frameworks
• Elevate national coordination by making RRRvR a strategic priority in the National Health and Medical Research Strategy
Bolstering research investment and capacity in RRRvR communities will significantly benefit local communitiesimproving health outcomes, healthcare services, workforce, and local economies. However, this is not just about replicating non-RRRvR models. The strengths of RRRvR research lies in offering alternative, community-grounded approaches to health and medical research and innovation - approaches that could strengthen all health and medical research and innovation, even in non-RRRvR communities. By undertaking these systemic reforms and incorporating the recommendations into the National Health and Medical Research Strategy, we can elevate the strengths of regional, rural, remote and very remote communities, not only for equity but for the health of the nation.
Authors: Dr
Talia Avrahamzon, Head of Policy, Projects
and
Advocacy, Research Australia;
Max Chester, Policy
Officer,
Research Australia. We acknowledge the steering committee comprised of Research Australia’s regional university members that guided the original development of this paper.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
THE NATIONAL HEALTH AND MEDICAL RESEARCH STRATEGY
Considerations for rural, regional and remote research in Australia

Australia’s first National Health and Medical Research Strategy (National Strategy) is under development and on track to be delivered at the end of 2025.
My role as Chair of the National Strategy is to manage the consultation process and provide leadership as we develop the architecture, action areas and initiatives of the National Strategy. I am working closely with the Commonwealth Department of Health, Disability and Ageing and the National Health and Medical Research Council (NHMRC) and being supported by many individuals and organisations who have generously contributed their time and ideas.
To date, in a first phase of consultation I have been fortunate to engage with stakeholders from right across Australia’s diverse health and medical research ecosystem, including those who undertake and lead the translation of
research to improve the health of the 27% of Australians who reside in rural, regional and remote areas. The input I have received from these individuals and organisations has been invaluable in better understanding the issues faced by rural, regional and remote communities and the experience for clinician researchers.
WHAT WE ARE HEARING
At the outset it is clear that the populations of rural, regional and remote Australia face many unique health challenges including higher mortality rates, high levels of disease and injury and poorer access to and use of health services, compared to those living in major cities.
What we have heard to date is that solutions to remedy some of these significant health inequities will best be addressed by research that is designed and led by experts within those communities, and where there are specific implementation strategies to ensure that rural, regional


and remote communities benefit from the outcomes of research through appropriate implementation of practice, equitable access to advanced technologies and better leveraging of research translation centres and knowledge hubs.
The Australian Health and Medical Research Workforce Audit, undertaken to inform the National Strategy, identified some important barriers to developing the workforce in regional areas, including funding opportunities that are not aligned to regional working conditions, and limited access to supporting workforce (such as health economists and statisticians).
More broadly, there is significant disparity between the capacity for clinician engagement in research in rural, regional and remote areas compared to metropolitan locations, related to clinical workloads and restricted capacity to conduct clinical trials. We are considering

approaches that could better incentivise research, and manage workloads, in those clinical settings to directly benefit rural communities and create a nation-wide learning healthcare system.
Please stay up to date with opportunities to engage and provide feedback on our website
Author: Ms Rosemary Huxtable AO PSM is the Chair of the National Strategy. Ms Huxtable is the former Secretary of the Commonwealth Department of Finance and a former Deputy Secretary of the Department of Health, Disability and Ageing. Ms Huxtable has extensive experience in government policy development and implementation, financial management and strategic leadership.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL



EMERGENCY MEDICINE FOUNDATION
FUNDING INNOVATION TO IMPROVE EMERGENCY CARE
The Emergency Medicine Foundation (EMF) is a not-for-profit organisation improving patient care in Australian emergency departments by funding innovative, clinician-led research.
We are one of the only organisations in Australia dedicated solely to funding emergency medicine research. Our grants support projects led by a range of clinicians, including doctors, nurses, paramedics, allied health professionals, and rural and remote teams, working in hospitals as well as pre-hospital services such as ambulance and retrieval teams.
Since 2007, we have invested more than $24 million in over 290 research projects across Queensland and Australia. Our funding helps frontline clinicians drive real-world change by asking the questions relevant to their experiences and generating the evidence needed to deliver better care, whether that’s reducing unnecessary tests, shortening emergency department wait times or delivering culturally safe care to all communities.
“EMF offers a range of research grants for clinicians at all stages of their research journey, from small, early-stage investigations to large, multi-year studies. We fund research that builds local capacity, drives system-wide innovation and addresses critical gaps such as trauma care in rural and remote communities, areas that are often overlooked in traditional research funding,” says Dr Angie Nguyen Vu, EMF General Manager.
EMF research has led to tangible improvements in emergency care, including the use of bedside ultrasound to diagnose children’s fractures without X-rays, more effective treatment for asthma and anaphylaxis in rural hospitals, and the landmark Improving Patient Flow Study, which is helping futureproof Queensland’s healthcare system.
Beyond grant funding, EMF strengthens emergency care research by nurturing new researchers, supporting mentoring and promoting meaningful consumer engagement. We also host research symposiums and events to share knowledge, spark collaboration and celebrate impact.
“At EMF, we empower frontline clinicians who are uniquely positioned to identify and address healthcare challenges within their specific contexts and communities,” says Professor Hugh Grantham ASM, EMF Board Chair. “Whether delivering trauma care in low-resource settings, serving as the all-round expert in rural and remote areas, or addressing the unique healthcare needs of complex patients, our clinicianresearchers are equipped with the research skills and funding to develop solutions that are evidence-based and tailored to real-world needs.”
As the only organisation of its kind in Australia, EMF plays a vital role in supporting emergency clinicians to deliver research with real-world impact, research that is transforming care and making a lasting impact.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
THE LAST WORD

RESEARCH THAT REACHES
Bridging gaps in cancer control –
for every community, everywhere.
Every day, countless people, families and communities feel the profound impact of cancer, a disease that causes physical, psychological and financial hardship at scale.
Despite advancements in our understanding of cancer, diagnoses have increased by over 75% since 2000 and are projected to rise a further 26% by 2036. This is largely driven by our ageing population and modifiable lifestyle factors such as obesity.
As a paediatric oncologist, I’ve seen the devastation cancer can bring. The relentless treatment cycles, emotional exhaustion, mounting bills, lives of family members upended, and, for many living outside major cities, the burden of travel.
The challenge is clear - to support individuals, health systems and communities, so people not only survive but live well with and beyond cancer. That means ensuring all communities can access evidence-based, highquality care as close to home as safely as possible, while investing in solutions that reduce cancer’s future toll.
At a population level, NSW boasts some of the world’s highest cancer survival rates. However, closer examination of the local experience reveals stark disparities in outcomes across different communities.
For a range of complex, interrelated reasons, certain groups face a disproportionate burden. For example, Aboriginal people are 1.5 times more likely to be
diagnosed with cancer than non-Aboriginal people. Barriers to screening and care also impact people from multicultural backgrounds, the LGBTQI+ community, those with mental illness, people in the justice system, and individuals from socioeconomically disadvantaged areas.
WHERE YOU LIVE SHOULDN’T DETERMINE YOUR OUTCOMES
Unfortunately, geography still plays a significant role in cancer outcomes.
Rural, regional, and remote NSW has higher cancer incidence rates than major cities, with mortality increasing with remoteness.
The reasons are complex and interwoven – demographic trends, higher smoking rates, occupational sun exposure, lower access to screening and specialist care, and a higher proportion of Aboriginal populations.
Melanoma, for example, is more common in regional communities, with most of NSW’s melanoma hotspots found outside urban areas. Lung, head and neck cancers are also more prevalent in these areas, often reflecting historical tobacco use.
Add to that the tyranny of distance. NSW spans over 800,000km, and for many, accessing timely, appropriate care requires long journeys and personal sacrifice.
For some cancers, high-quality, centralised care is sometimes necessary, with sub-specialist expertise, multidisciplinary teams and research-informed pathways located at major centres.
However, when safe and feasible, care should be delivered closer to home. That’s why strengthening regional cancer

services, expanding outreach models and addressing increasing workforce challenges are core aims of the NSW Cancer Plan and the NSW Regional Health Strategic Plan.
BUILDING EQUITY THROUGH INNOVATION
At the Cancer Institute NSW, we’re working in partnership to reduce cancer’s burden and address inequities through connected, data-driven strategies. Collaborative efforts across government, health services and community partners are achieving progress.
• Over 95% of the NSW population now live within 100km of a cancer centre.
• Radiotherapy access has expanded significantly across regional NSW.
• Telehealth is helping bridge the distance between patients and specialists.
• Tele-trials and decentralised models are scaling through targeted investment, improving access to clinical trials for rural and regional patients.
• Capacity-building grants support research infrastructure and workforce development in regional centres.
• The Institute’s Patient Reported Outcomes Program allows patients to flag concerns in real time, helping clinicians respond promptly to what matters most.
• The Reporting for Better Cancer Outcomes Program is helping identify opportunities to link people to multidisciplinary care and improve outcomes.
• Culturally-appropriate care is improving through Aboriginal Cancer Care Coordinators embedded within services.



• Targeted health campaigns are tailored to regional communities, informed by behaviour change research, local data and lived experience.
• The latest Outpatient Cancer Clinics Patient Experience survey shows people in rural and remote NSW often rate their care more highly than metropolitan peers – a testament to the quality care delivered by local services.
THE UNTAPPED POWER OF PREVENTION
While we rightly focus on treating cancer better, we must not overlook the enormous potential of prevention.
Around 16,000 cancers and 5,000 deaths annually in NSW are potentially preventable through lifestyle changes – increased physical activity, improved diet, maintaining healthy weight, effective sun protection, reducing alcohol and stopping smoking/vaping.
Yet, when it comes to funding, prevention remains the poor cousin of cancer control. Despite proven return on investment, prevention programs are chronically underfunded and constrained by short-term grants. These time-limited cycles hinder the sustained, generational change needed to shift behaviours and environments that drive cancer risk.
To be effective, prevention must be viewed as a longterm, structural investment, integrated into education, urban design, taxation, regulation and health promotion in sustained, far-reaching ways.
The Cancer Institute NSW advocates for whole-of-system approaches that elevate prevention as a core pillar of cancer control and community wellbeing. This will reduce cancer’s burden on people, communities, and health systems – now and into the future.
Author: Professor Tracey O’Brien AM is the NSW Chief Cancer Officer and CEO of Cancer Institute NSW
Professor Tracey O’Brien AM
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

Image supplied by James Cook University (JCU)