







9 Committee finds collapsed spy trial ‘beset by confusion’ and ‘shambolic’
9 Changing of expert opinion: when is it acceptable?
11 Lawyers united in opposing erosion of jury trial
11 Lawyers rely on independent experts in claims against police VIEWPOINT
13 When is an expert not an expert?
PROPERTY, CONSTRUCTION & ENGINEERING
15 Lords’ criticisms of BSR welcomed by law firm
15 How will new Cyber Security Bill impact on infrastructure sector?
17 RICS publishes guidance on flood risk management
17 When homes turn harmful: how expert evidence shapes damp, mould and disrepair claims
FIRE INVESTIGATION
18 Doubts raised over third-party fire certification
19 Insurer calls for mandatory fire suppression on farm machinery
DIGITAL FORENSICS
21 An expert’s perspective: document authenticity in disputes
FORENSIC ACCOUNTANCY
23 Bookkeepers’ body censured for AML failures
23 SFO publishes corporate compliance guidance
24 Govt reveals scale of fraudulent claims clawed back
25 Financial expertise can be a strategic asset for solicitors
26 Providing Part 35-compliant reports to the legal profession
TREE CARE
27 The benefits of a feasibility assessment can be applied throughout the legal process
ENVIRONMENTAL ISSUES
28 Litigation on climate change: the heat is on
30 Japanese knotweed: the legal responsibilities for UK property owners
AVIATION
31 The vital role of aviation experts in legal disputes and accident investigations
THE OIL & GAS INDUSTRY
32 Expert evidence in oil and gas disputes: navigating a changing energy landscape
MARITIME DISPUTES
33 The Devil’s in the detail when it comes to the Cancelling Date
TRANSLATING & INTERPRETING
35 Lost in translation: the crisis in UK court interpreting



45 Negligence costs come under renewed scrutiny
45 Woman jailed for fraudulent claim
47 CQC picks itself up and dusts itself off
47 Care home fined for ‘avoidable harm’ of resident
49 Patient alert issued over wrong name for allergy
49 Non-routine scan can predict heart failure
51 GMC consults on raising patient safety concerns
51 BMA reacts to Hallett’s Module 2 report
53 £1/2m-plus payout for missed skin cancer
53 New sepsis test has ‘potential to save lives’
55 Changes to ways patients contact GPs are affecting care, survey finds
ENT SURGERY
56 Surgeons’ body condemns ICBs’ ENT decision
56 ‘Lifelong damage’ fears for hearing loss kids
HAEMATOLOGY
57 Infected blood victims tell officials that compensation is ‘taking too long’
UROLOGY
59 No mass prostate screening, but charities take some comfort
MEDICO-LEGAL PRACTICE: THE CHANGING LANDSCAPE
61 How technology and transparency are reshaping medicolegal practice
OBSTETRICS & GYNAECOLOGY
63 RCOG welcomes Scottish abortion report
63 Investigation prompts call for better midwifery education
64 Is the continued use of the Bolam Test to assess the standard of intrapartum care in the UK acceptable?
67 What will yet another independent national inquiry into NHS maternity care achieve?
VASCULAR SURGERY
68 Nerve problems following varicose vein treatments
NEUROSURGERY
71 Persistent vegetative state: its medicolegal implications
BRAIN INJURY
73 Understanding the hidden impact of brain injury
PSYCHIATRIC & PSYCHOLOGICAL ISSUES
75 Psychiatrists’ lead comments on ADHD report
75 AI cannot solve all the issues which face the SEND system, says BPS
77 Would I lie to you?
78 Experts and AI: a helping hand or a gremlin in the system?
GERIATRIC & STROKE MEDICINE
79 Specialists make the connection between frailty and stroke
NURSING AND CARE
80 The value of expert evidence in care & case management claims
81 Quality, not quantity: the evolving role of the nursing expert witness
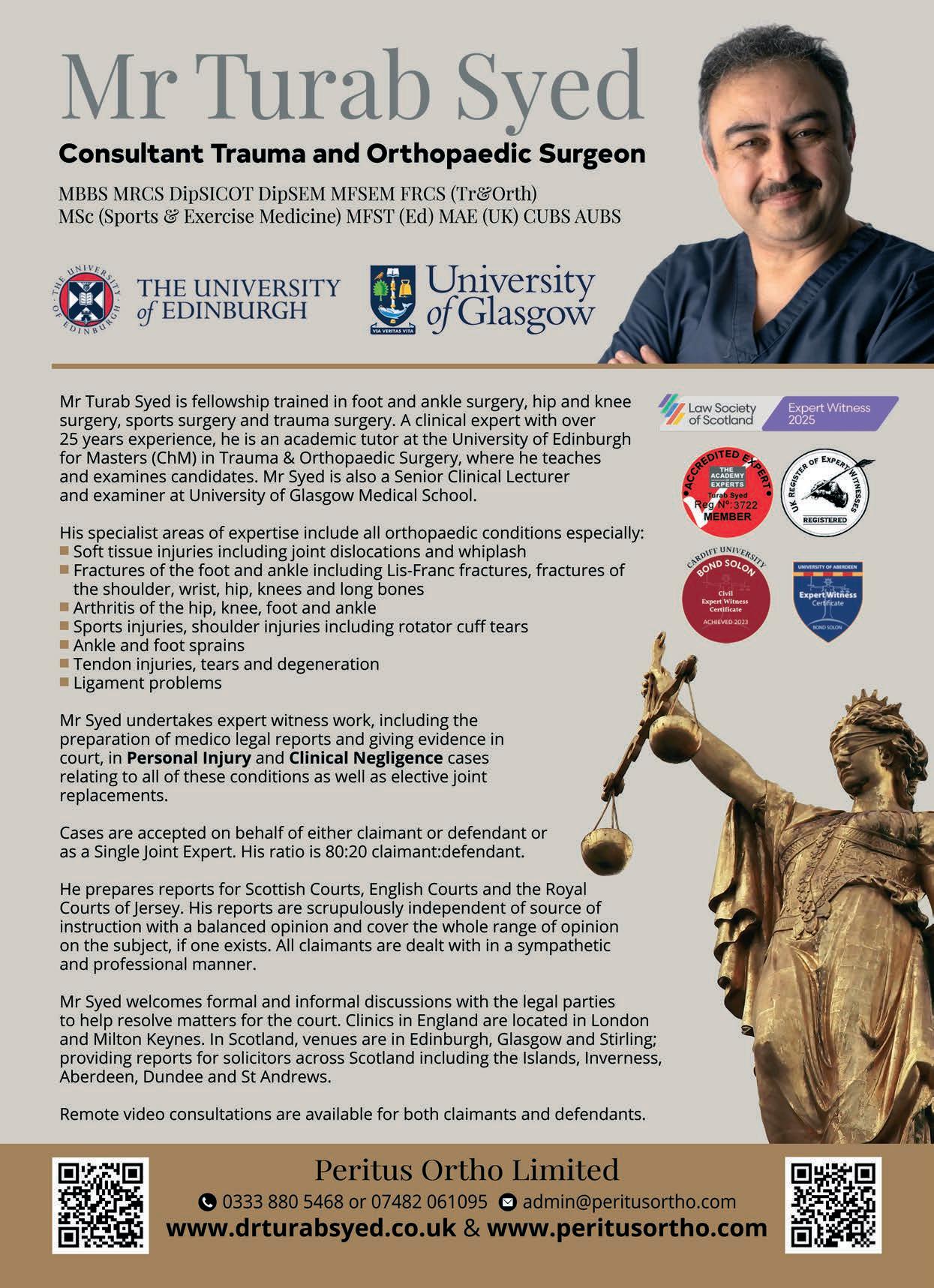
ORTHOPAEDICS
83 Review shows reduction in revision surgery
83 Documents set out best practice in orthopaedic surgery
85 From ‘acceptable’ to actionable: how biomechanical causation proves functional loss beyond doubt
87 Report reveals financial cost of arthritis

RESPIRATORY MEDICINE
90 Tis the season of goodwill…and pneumonia!
PHYSIOTHERAPY
91 Physiotherapy offers its views on the ‘left shift’
93 Physiotherapy and medico-legal practice
PLASTIC, RECONSTRUCTIVE & HAND SURGERY
95 Hand surgeons raise concerns over Cumberlege measures
95 Letter calls for fairer casting for visibly different people
OBESITY AND WEIGHT MANAGEMENT
96 Obesity, weight loss treatments and legal liability
DIABETES
97 Safety alert issued for blood sugar monitors
97 Top lawyer explains the risk of diabetes mismanagement
CARDIAC & THORACIC SURGERY
99 Heart of the matter: how cardiac & thoracic surgeons’ expert testimony can make or break a case
CARDIOLOGY
101 Royal College addresses issues around safety and collaborative working
OPHTHALMOLOGY & OPTOMETRY
103 Senedd report chimes with ophthalmologists’ wishes
103 Eye-Law Chambers offer specialist insight in ophthalmic expert reporting
103 Optical bodies urge drivers to have regular eyesight checks
105 When expert eyes matter: how expert witness evidence shapes cataract surgery claims
DENTISTRY & MAXILLOFACIAL SURGERY
107 Dentists’ body slams Reeves over CMA letter
107 GDC’s new strategy aims to build trust and transform dental regulation
INTENSIVE CARE
111 Postoperative intensive care: some medicolegal challenges
A & E MEDICINE
113 Budget announcement offers nothing to EDs, college says

[ LAWYERS ACROSS THE BOARD have been quick to lead the charge against David Lammy’s plans to scrap jury trials for all but the most serious crimes – together with what the MoJ describes as ‘particularly technical and lengthy fraud and financial offences’. The proposal, touted as being an effort to reduce the backlog of cases awaiting trial, has been critisised by both solicitors and barristers – not to mention judges and MPs in the Deputy Prime Minister’s own party. We wait to see whether the proposals progress to law.
• One trial that didn’t get off the ground, regardless of Mr Lammy’s proposals, was that of two people accused of spying on MPs on behalf of the Chinese government. The Joint Committee on the National Security Strategy has found it ‘did not find evidence of a co-ordinated high-level effort to collapse the prosecution, nor of deliberate efforts to obstruct it’. Instead it found a ‘shambolic’ approach on the part of officials.
• Still in the world of government and legislation, the Cyber Security Bill is currently creaking its way through Parliament. While that will mainly affect IT companies and consultancies, there are implications for other industries such as the architecture, engineering and construction (AEC) sector. A leading player in advising the sector on cyber resilience explains the ramifications.
• The construction industry has also drawn the attention of the upper house of Parliament; or rather the law brought in to ensure buildings are safe in the wake of the Grenfell disaster. The House of Lords Industry and Regulators Committee has criticised the Building Safety Regulator for dragging its feet over granting approvals. The delays are getting in the way of achieving housebuilding targets, the Committee says. At least one major law firm has praised the Committee.
• The Grenfell fire also highlighted failures in product testing and certification – failures that persist to this day, according to a leading fire testing specialist. They highlight the findings of a survey of those attending fire safety events, showing dissatisfaction with third-party certification schemes.
• A lack of fire suppression systems on agricultural vehicles has been decried by insurer NFU Mutual, following revelations that the bill for repairs to such plant as combine harvesters following fires came to £37m in 2024. Such devices not only reduce the costs associated with fires, but also save lives, the insurer says. Along with electrical faults, arson and lightning strikes remain the main causes of farm fires, which together cost the insurer nearly £102m last year.
• Flooding probably causes most people more cause to lose sleep than lightning or other natural risks. Assessing flood risk is one area of expertise that falls under the ambit of the RICS. That august body has published a new practice information paper for its members, stressing the need for surveyors ‘to integrate flood awareness and resilience thinking into every area of practice’.
• Whatever the area of expertise, some experts find that new revelations force them to change their minds over their evidence. In those cases the judge may look unfavourably on that expert’s evidence, although it is not necessarily the case. Bond Solon offer their customary thorough explanation of what can be a thorny issue.
• Changing your mind can also involve substantial cost: particularly if it concerns buying a ship, when it can run into millions of pounds. Deciding who is at fault for the cancellation of the sale was the subject of a recent Court of Appeal judgement. q
Ian Wild, Director of Business Development Your Expert Witness

[THE Joint Committee on the National Security Strategy has published its report on the circumstances surrounding the collapsed prosecution of two individuals accused of spying on Members of Parliament for China.
The decision to drop the case shortly before trial sparked widespread public concern. Key questions included whether there was improper influence at the highest levels of government – or efforts to allow the case to fail – alongside suggestions of questionable decision-making, failures of process and errors of judgement.
The report examines the timeline, actions and decisions from the Government and the Crown Prosecution Service. The Committee noted that the sequence of some events has raised eyebrows – in particular the number of times the Crown Prosecution Service engaged with the Government to obtain the evidence it required (ultimately unsuccessfully), and fact that the prosecution was dropped two days after a group of senior
[THE RECENT High Court decision in Patricia Andrews & Ors v Kronospan Limited [2025] EWHC 2429 (TCC) offers clear direction to experts as to when a change of approach or opinion is likely to be permitted by the courts, and when it is likely to be looked at ‘particularly critically’.
Expert witness training specialists Bond Solon have offered a breakdown of what the implications are.
“The case in point was a class action whereby the claimants – a group of residents from a large village – sought damages and other relief against the defendant, the UK arm of a group of companies operating a local factor, alleging environmental nuisance caused by dust particles, odour and noise.
“All four experts had initially agreed a common approach. However, at a later stage, the claimant experts attempted to add to and refine their approach based upon different criteria, which impacted the common approach.
“Whilst the judge did not question the conduct of the claimant experts, he concluded that their change of approach was subjective – in that it was ‘at least partially influenced by their desire to see whether or not further analysis would benefit their clients’ case more than their existing analysis’.”
To read the full account of Bond Solon’s reporting of the judge’s decision visit www.bondsolon.com q
officials met to discuss the case. The process for obtaining the second witness statement took eight months, for reasons which remain obscure to the Committee.
The Committee did not find evidence of a co-ordinated high-level effort to collapse the prosecution, nor of deliberate efforts to obstruct it, circumvent constitutional safeguards or frustrate the Committee’s inquiry.
However, the Committee did find evidence of a process ‘beset by confusion and misaligned expectations’ that was at times ‘shambolic’. The report criticises ‘systemic failures’: communications were inadequate, while constitutional safeguards designed to protect the independence of criminal proceedings instead catalysed a crisis of public confidence and fuelled allegations of conspiracy at the highest levels of government.
The report concludes that some decisions were questionable, opportunities to correct course were missed, and that the episode reflects poorly on the otherwise commendable efforts across public servants to keep the UK safe.
Chair of the Joint Committee, Matt Western MP, said: “As the global security environment worsens, sensitive national security cases will arise more frequently. The government must show the public that it is confident in standing up to adversaries when required: failing to do so will corrode public trust in our institutions.
“The government must work with legal partners to think through what happens when such cases arrive. How will they be prosecuted and handled in a way that mitigates the risk of misunderstandings?
“The government should also consider whether more support can be offered to senior public officials, such as the NSAs [National Security Advisers], who may be simultaneously exposed and isolated, due to the limits on what they can discuss during a case.” q

[ LAWYERS’ PROFESSIONAL BODIES were swift to react to the Deputy Prime Minister’s much-heralded announcement of the removal of jury trials for all but the most serious of crimes. The reforms were announced in Parliament on 2 December by David Lammy, who is also Justice Secretary, with the aim of ‘bringing the system back from the brink of total collapse and regaining the trust of both victims and the public’.
The new ‘Swift Courts’ will see cases with a likely sentence of three years or less heard by a Judge alone - estimated to take 20% less time than a jury trial, meaning guaranteed jury trials will only be for the most serious and almost all indictable offences – including rape, murder, aggravated burglary, blackmail, people trafficking, grievous bodily harm and the most serious drug offences.
Judge-only trials for particularly technical and lengthy fraud and financial offences will ‘free up jurors who have to give up months of their lives to hear particularly burdensome cases’.
Mr Lammy said: “This government inherited a justice system in crisis – victims are waiting far too long to get their case to court, and even more are being let down by a system that allows nefarious defendants
to try and game the system.
“The crumbling system we inherited has resulted in a Crown Court backlog of nearly 80,000 and rising. Justice delayed is justice denied.”
Law Society of England and Wales vice president Brett Dixon reacted: “The government’s proposals go too far in eroding our fundamental right to be judged by a jury of our own peers.
“Sir Brian Leveson’s recommendations, including two magistrates sitting alongside a judge in the new court, retained an element of lay participation in determining a person’s guilt or innocence. The government’s proposals remove this.
“Allowing a single judge, operating in an under-resourced system, to decide guilt in a serious and potentially life-changing case is a dramatic departure from our shared values.
“The government cannot justify stripping away this fundamental right without publishing clear evidence that putting more cases in the hands of a single judge will tackle the horrendous backlogs in our courts.
“The Leveson proposals, while an uncomfortable compromise, were understandable given the extensive challenges the criminal justice system faces
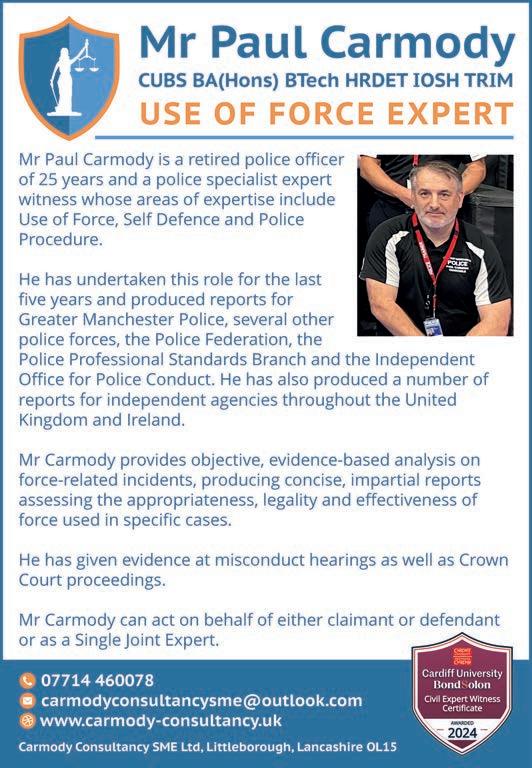
[ MR PAUL CARMODY is an expert in the increasingly prominent role of policing and use-of-force in civil claims, misconduct hearings and criminal proceedings. With growing public scrutiny, body-worn video now being standard, and forces facing rising volumes of complaints and IOPC referrals, legal teams are relying more than ever on independent experts who can analyse tactical decision-making, officer conduct and adherence to nationally recognised guidance.
As a consultant in this area of expertise, Mr Carmody can assist in interpreting operational decisions, assessing proportionality and necessity, and explaining the realities of dynamic incidents to courts and tribunals. He can also look at the challenges of reviewing evidence where accounts differ, where video footage does not show the full context, or where officers must justify split-second judgement in hindsight.
Mr Carmody can highlight the importance of balanced, CPR35compliant reporting, impartial analysis of force options and the clear explanation of police procedure – particularly in cases involving injury, restraint, non-compliance, mental health interventions or allegations of excessive force.
His extensive experience in police procedure, use-of-force evaluation, tactical decision-making and post-incident analysis puts Mr Carmody at the forefront in assessing and recording a clear, concise and professional report and analysis of police contact incidents, especially when instructed in misconduct hearings, civil actions against the police, criminal defence cases or IOPC matters. q
including unacceptable delays for victims, witnesses and defendants. Going beyond them is not.
“The criminal court backlogs are the result of decades of underinvestment in the criminal justice system, with justice spending down 24% since 2007/2008.”
The Bar Council was equally scathing. Removing the right to a jury trial ‘is not the answer’, the council said, and risks making the crisis facing the criminal justice system worse. Changing the fundamental structure of delivering criminal justice is not a principled response to a crisis which was not caused by that structure in the first place, the Bar argued.
Bar Council chair Barbara Mills KC said: “The current system is capable of working if sufficiently resourced. Funding for justice should be in line with the demands made of the system. We recognise that the present economic landscape is challenging, but that is not a justification for a total change to how some cases should be tried.
“We have put forward alternative approaches to increase efficiency. All of them should be tried before making structural changes that remove the right to trial by jury in some cases. An intermediate court is simply not the answer.” q

By Chris Makin chartered accountant, accredited civil mediator and accredited expert determiner
[AS ANY LITIGATOR in England and Wales knows, Part 35.3 of CPR states that the expert has an overriding duty ‘to help the court on matters within their expertise’ – and that expertise is measured by membership of appropriate professional bodies. I am typical: a fellow of the Institute of Chartered Accountants in England and Wales (ICAEW) and The Academy of Experts and a member of the Chartered Institute of Arbitrators, among others.
But what if an accountancy expert were to lose his qualification during preparation for a case? Let me tell you about Jeffrey Davidson.
Jeff, like me, was one of the early specialists in forensic accountancy. A Cambridge graduate, he was an affable chap who I met often at Institute events.
But about three years ago I was asked to help a businessman who had bought a business which had to go to expert determination, and Jeff was the accountant chosen to make a binding decision on value. The businessman was unhappy with the value, and my work quickly established that Jeff had committed a manifest error which caused my client to overpay by about £100,000.
I drew Jeff’s attention to this mistake and at first he said it was none of my business. When I pressed him, he said he would not alter his finding.
My client wanted to sell the business, and would find that difficult with ongoing litigation, so he swallowed the £100,000 and did not take the case to law.
But whilst this was being considered, both the client and I took a close look at Jeff, and we discovered two things. One was that something irregular may have happened with a charitable trust in which Jeff and his wife were the sole trustees, and that was to be investigated by the Charity Commission. I have not seen the outcome.
The other is that a client had lodged complaints which were being investigated by the ICAEW. They asked Jeff to disclose certain documents to aid their enquiry but he pleaded client confidentiality (not valid in these circumstances) and then that the documents had to be redacted, which for some reason was taking several months.
It is against our Royal Charter to refuse to supply documents in an enquiry, and Jeff was brought before the Disciplinary Committee. He was given a severe reprimand, a fine of £5,000, costs of £8,125 and an order to provide the documents within four weeks. When those documents were still not provided, he automatically lost his membership of ICAEW and was no longer a chartered accountant.
Interestingly, this was going on as a major trial approached in which Jeff was one of the forensic accountant expert witnesses. This was JSC Commercial Bank Privatbank v Igor Valeryevich Kolomoisky & Ors [2025]
EWHC 1987 (Ch) which concerned the alleged theft of £1.9 billion (yes, £1,900,000,000) from a Ukrainian bank just before it was nationalised. There were eight defendants including Ukrainian, English and Cypriot companies. The bank as claimants had four KCs and four junior counsel, and the various defendants fielded six KCs and five junior counsel. It must have been quite a jamboree and the courtroom must have been very crowded.
The hearing was over 43 days in 2023 and the judgment, by Trower J, was a heavy piece of work issued on 30 July 2025. It ran to 490 pages, with the contents page alone running to four pages. I confess I have not read it all.
The interesting part for us is at paragraphs 305 to 314 (there were 2,025 paragraphs in all!). The learned judge assessed the work of the forensic accountant for the bank and for the first two defendants. Jeff was expert for the first defendant.
After commenting on the work of the three expert accountants, Trower J turned to the status of Jeff at paragraph 311, which I quote in full:
“At the time of their reports, each of the experts was a fellow of the Institute of Chartered Accountants in England and Wales (ICAEW). During the course of July 2023, after the trial had commenced but before he was
called to give evidence, it came to the attention of the Bank’s solicitors that Mr Davidson’s status as a member of ICAEW was now recorded as Ceased with a sub-status recorded as Cessated. They wrote to Mr Kolomansky’s solicitors drawing attention to the cessation and attaching a copy of his disciplinary record which disclosed that he had been the subject of a severe reprimand in relation to two disciplinary matters in respect of which there had been hearings on 8 March 2023. None of this information had been disclosed by Mr Davidson either to the Bank or to the court.”

Trower J goes on at paragraphs 312 to 314 which are lengthy. I will quote parts of these:
“Mr Davidson’s explanation for what had occurred was eventually revealed on 29 September 2023, five days before he was due to give evidence.
“He also disclosed that the Charity Commission had removed him as trustee of two charities and that those charities had been the subject of statutory enquiries…” (One allegation was that funds of £500,000 were missing.)
“In his witness statement, Mr Davidson also gave notice that he would rely on his privilege against self-incrimination to justify his refusal to answer any questions about the August 2021 complaint to the ICAEW and the Charity Commission enquiry.
“In light of the position adopted by Mr Davidson, it was not possible for the court to obtain a full picture of what had occurred or the extent to which the matters in respect of which he had been investigated or criticised might have been relevant to the quality of his evidence.
“In my view, where an expert presents his evidence as a member of a professional organisation, which is expected by him to give the court assurance as to his ability to act in the case, he is under a duty to inform the court if his membership has ceased, more particularly where the cessation is linked to disciplinary proceedings against him.
“Mr Davidson also failed to disclose that he has been the subject of a finding in another case that his opinion was based on wholly unsupported and fanciful assumptions, which ignored the objective facts and undermined his credibility as an independent expert (per Leggat LJ in Al Neheyan v Kent [2018] EWHC 333 (Comm) at [1951]).”
I draw two morals: firstly, experts must inform the court if they have been drummed out of the regiment and if they have been criticised as experts in other cases; secondly, as I’ve said many times before, solicitors must choose their experts with care. q
[ CHRIS MAKIN was one of the first 30 or so chartered accountants to become an Accredited Forensic Accountant and Expert Witness – see www. icaew.com/about-icaew/find-achartered-accountant/find-anaccredited-forensic-expert

He is also an accredited civil and commercial mediator and an accredited expert determiner. Over the last 30 years he has given expert evidence at least 100 times and worked on a vast range of cases.
For CV, war stories and much more go to the website at www.chrismakin.co.uk – now with videos! q
[LAW FIRM IRWIN MITCHELL has welcomed the findings and recommendations from the House of Lords Industry and Regulators Committee around delays caused by the Building Safety Regulator (BSR).
The cross-party Committee, chaired by Baroness Taylor of Bolton, emphasised that while the creation of the Building Safety Regulator was a necessary step following the Grenfell Tower tragedy, the current level of delays in the approval process is ‘unacceptable’.
It highlighted that the delays are causing unnecessary anxiety and frustration for residents and businesses and stressed the need for urgent action from both the government and the regulator to ensure that essential safety work and new housing can progress more swiftly, without compromising on safety.
The report also found that the delays are significantly slowing the delivery of new homes, particularly in cities where high-rise buildings are
crucial to meeting government housebuilding targets. The Committee concluded that resolving the delays is essential if the country is to make progress towards building 1.5 million new homes in this Parliament. The report calls on:
• The BSR to give greater guidance to its multi-disciplinary teams (MDTs) on how compliance with the Building Regulations should be evidenced and assessed to ensure greater consistency
• The government to remove smaller works from the BSR’s building control approval processes, or introduce a streamlined approval process for them
• The BSR to allocate the same MDTs to similar buildings or projects built by the same organisation, which could improve efficiency and consistency
• The government to provide long-term funding for the training of new building and fire inspectors

Alex Delin, construction partner at the firm, said: “Following publication of the report, hopefully we will see better guidance for applicants to demonstrate their buildings are safe and less delay due to erroneous applications which the report finds can easily be resolved, together with building inspectors and planning authorities working in tandem with applicants as applications progress.” q
[ON 12 NOVEMBER the government introduced the Cyber Security and Resilience Bill to Parliament, with the aim of strengthening national security and protecting growth by boosting cyber protections for the services that people and businesses rely on every day.
Introducing the Bill, the government said: “In the face of increasing cyber threats, it will prevent disruption – keeping the taps running, the lights on and the UK’s transport services moving – while making sure those who supply our vital services have tougher cyber protections.”
While the architecture, engineering and construction (AEC) industries aren’t named directly in the Bill, many firms that work on projects linked to national infrastructure will be impacted.
Dave Adamson, solutions director at Creative ITC, advises AEC organisations on how to strengthen their cyber resilience and work with trusted partners to ensure long-term protection.
Commenting on the implications for the AEC sector, Dave said: “With the introduction of the Cyber Security and Resilience Bill to Parliament, the UK Government has highlighted cyber security as a national priority.
For AEC organisations, especially those delivering critical national infrastructure projects, this is a wake-up call to reinforce defences and embed resilience for the long term.
“Cyber risk must be a board-level issue, integrated into strategic

planning and governance. Leaders should follow the Cyber Governance Code of Practice and ensure their IT security teams sign up for the NCSC’s free Early Warning service to receive malicious activity alerts for their organisation.
“AEC firms need a culture of continuous monitoring. Complementing stretched IT and cyber teams and partnering with specialists ensures effective, round-the-clock defence measures. This should include 24/7, enterprise-wide IT visibility with expert insight to reduce false positives and minimise disruption. Known vulnerabilities should also be tracked and patched promptly to close gaps before attackers exploit them. Implementing robust multi-factor authentication across all access points will also limit exposure to risk.
“Cyber resilience doesn’t stop at your own network. The Bill recognises that supply chains are often the weakest link. Enforce strong security standards across partners, setting Cyber Essentials certification as a minimum requirement for all suppliers. Third-party risk management solutions further strengthen resilience, monitoring risks across supply chains for rapid remediation.” q
• To find out more about what Dave Adamson and his colleagues can offer visit www.creative-itc.com

[IN OCTOBER The Royal Institution of Chartered Surveyors (RICS) published a landmark practice information paper, Flooding and its implications for property professionals, providing the profession with a comprehensive overview of the growing challenges and responsibilities associated with flood risk across the United Kingdom.
Authored by Charles Cowap from Harper Adams University, with contributions from Michael Chichester, James Ginley and Ben Sharp, and a cross-profession expert working group, the paper examines how surveyors across all disciplines are being called upon to help clients, communities and policymakers manage the escalating risks and consequences of flooding.
With the UK Climate Change Risk Assessment identifying flooding as ‘one of the most severe climate hazards’, RICS stresses the need for surveyors to integrate flood awareness and resilience thinking into every area of practice – from valuation and planning to land management, construction and property management.
The 2025 RICS practice paper brings together knowledge on:
• Types and sources of flooding – including fluvial, coastal, surface, groundwater and infrastructure-related flooding
• Economic, environmental and social impacts – with flood damage and management costs estimated at £2.2bn annually
• Climate trends – UK properties at high flood risk could double by 2050 without adaptation
• Planning, design and construction standards – including BS 85500:2025 and the wider adoption of sustainable drainage systems (SuDS)
• Property flood resilience – practical measures for both resistance and recoverability in residential, commercial and rural contexts
• Professional implications – covering valuation, insurance, mortgage lending, estate management and occupier guidance
The paper highlights how flooding intersects with key areas of

professional responsibility. Surveyors may be involved in:
• Providing flood risk assessments and resilience advice for clients and lenders
• Advising on drainage and flood adaptation in design and construction projects
• Assessing flood risk implications in valuation and due diligence
• Supporting clients in flood recovery, insurance and reinstatement
• Promoting collaboration across the surveying, engineering, planning and insurance professions
Fiona Mannix, the RICS senior specialist for land and development, said: “Flooding affects every part of the property lifecycle, and surveyors are uniquely placed to interpret its implications for value, safety, design and long-term resilience.
“This paper equips members with a broad understanding of the issues and encourages cross-disciplinary collaboration to meet this growing professional challenge.” q
[IN THE UK, tenants who find their homes afflicted with damp or mould often turn to the law – but success usually hinges on proving the root cause of the problem. Legal obligations mean that landlords are responsible for maintaining the structure and safety of properties, and expert evidence is frequently the deciding factor when disputes about disrepair reach court.
Landlords’ duties stem from the Landlord and Tenant Act 1985 and other housing safety legislation: they must keep the structure, exterior, heating, water and sanitation systems in proper repair. When damp or mould result from structural defects – a leaking roof, broken guttering, defective plumbing or a failed damp proof course – the landlord must act. Likewise, serious damp or mould that risks occupants’ health may trigger obligations under the housing safety regime, especially when the home becomes unfit for habitation.
At the same time, damp and mould can be caused by everyday living conditions – condensation from cooking or bathing, poor ventilation or heating habits. In those situations, liability becomes more complex, and landlords may not automatically be to blame.
Because the causes are often disputed or unclear, courts usually rely on expert evidence supplied by professional surveyors or environmental health specialists. Under the Civil Procedure Rules (CPR Part 35 and Practice Direction 35) such evidence must be necessary, properly instructed and approved by the court. In many cases, the court expects the parties to agree a single joint expert to inspect the property, identify causes, describe necessary works and estimate their cost – ensuring clarity, reducing conflict and preventing ‘expert duels’.
Expert reports help establish important facts: whether defects lie in structure or fittings –roof, damp proof-course, plumbing – whether mould stems from poor maintenance or tenant behaviour, such as inadequate ventilation, and what remedial works are needed to make the property safe again. Without such expert evidence, claims are more likely to fail –particularly where the landlord disputes liability.
If the claim succeeds, remedies can include ordering the landlord to carry out permanent repairs, compensate tenants for damaged belongings, reimburse health-related costs and provide compensation for loss of amenity
or enjoyment of the home. In cases where landlords belong to the social housing sector, rules under Awaab’s Law, enacted in England in October 2025, impose statutory timescales for investigating and remedying serious damp or mould hazards – underlining that expertled inspections and prompt action are now mandatory.
In practice, tenants pursuing disrepair claims should document their circumstances carefully: keep a record of all complaints and communications with the landlord, photograph or video damp and mould, and seek a professional survey. These actions build a robust factual record that courts or housing authorities can rely on when making judgments.
When conditions deteriorate to the point where homes become harmful due to damp or mould, expert evidence is often the difference between a stalled complaint and meaningful legal remedy. By clarifying the cause, identifying necessary repairs and underpinning claims for compensation, expert reports serve as a critical safeguard – helping to ensure tenants’ homes are safe, habitable and legally compliant. q
[A COMPREHENSIVE SURVEY of fire safety professionals has revealed significant shortcomings in current third-party certification schemes, with 60% of respondents reporting issues with their existing providers and 82% demanding greater transparency in certification processes.
The findings, published in a new whitepaper by fire testing specialists United Kingdom Testing & Certification Ltd. (UKTC), highlights persistent problems in the construction industry, eight years after the Grenfell Tower tragedy that claimed 72 lives and exposed systemic failures in product certification and safety assurance.
A survey of those attending fire safety events in 2024 uncovered troubling feedback about legacy certification schemes, with professionals describing them as having ‘inconsistent positions’ or ‘lack of transparency’ and providing ‘poor value-for-money service’. Three quarters of respondents indicated they assess certification body credibility primarily through UKAS accreditation status and regulatory compliance.
The whitepaper’s author, Andrew Hutchison, operations director at UKTC, said: “Despite the proliferation of third-party certification schemes, the sector still suffers from dangerous opacity. Field of Application reports, classification reports and test data are routinely withheld from the public, forcing specifiers and contractors to make critical safety decisions in the dark.”
In response to challenges highlighted within the survey, UKTC, which was acquired by the SOCOTEC Group earlier in 2025, has launched its UKTC ensure scheme.
The scheme is the first third-party certification programme designed explicitly around the principles of the Golden Thread framework, recommended by Dame Judith Hackitt’s Building a Safer Future report. Backed by UKAS accreditation under ISO 17065, UKTC ensure makes sure every performance claim is traceable and every certificate is verifiable.
Further innovative features of UKTC ensure include the complete publication of supporting documentation, such as Field of Application reports and classification reports, real-time updates with robust version control,

a secure digital vault serving as a single source of truth for all certification documents and unambiguous product marking with QR code access to performance data.
The whitepaper highlights the fact that the mandate for change is clear and non-negotiable
Andrew Hutchison added: “The lessons of Grenfell and subsequent inquiries cannot be ignored. Too often, critical voices and concerns were missed or dismissed, which cannot continue. Real change is long overdue, and change starts with transparent certification.”
The scheme represents a fundamental shift toward the digital, accessible and version-controlled evidence framework outlined in numerous government reports and British Standards, including BS 8644-1:2022 for managing fire safety information throughout a product's lifecycle.
Matthew Marriott, CEO of SOCOTEC UK and Ireland, said: “The release of this whitepaper highlights several concerning shortcomings in the thirdparty certification market at present. There’s a clear requirement for radical change, and we look forward to seeing UKTC ensure have a real positive change on the sector.” q

[THE ESTIMATED COST of farm fires reported to insurers NFU Mutual in 2024 has been revealed at almost £102m, according to the firm’s latest Farm Fires report.
The main causes of farm fires identified by the report were arson, lightning strikes and electrical faults, although the number of fire claims involving crops, buildings and farm equipment had dropped 18% since 2024.
In addition to the cost of farm fires, the insurance bill to repair and replace agricultural vehicles such as tractors and combine harvesters totalled an additional £37m in 2024. Despite that being lower for some vehicle types than recent years, Louise Nicholls, underwriting specialist at NFU Mutual, said that it was ‘vital that rural communities aren’t complacent’.
The report also set out NFU Mutual’s position on vehicle fire suppression: “NFU Mutual strongly recommends fitting fire suppression systems to high-risk kit, such as combine harvesters. These systems, commonplace in other industries like forestry, are highly effective at stopping small fires spreading and engulfing the entire machine.
“Fire suppression kits can save lives and prevent damage and disruption, and there are ways government can support. Introducing legislation requiring manufacturers to fit suppression kits as standard, or providing grants to farmers to allow them to purchase these kits, would be an effective way of making farms safer – while minimising the risk of damaging local infrastructure and disrupting the wider community.”
Highlighting the issues facing the agricultural sector, Hannah Binns, NFU Mutual’s rural affairs specialist, said: “Fire remains a constant risk to UK farms, with dangerous and devastating farm fires becoming all too common.
“To minimise the risk of a farm blaze it’s vital that farmers develop a detailed fire plan, outlining how to evacuate safely, ensuring buildings are secure, managing livestock and keeping machinery properly serviced and clean.” q

By Ryan Shields, digital forensics expert witness at S-RM
[IN MODERN LITIGATION the importance of digital documents cannot be understated. Whether in a multimillion-pound commercial dispute or an investigation into alleged misconduct, questions of authenticity can make or break a case. Was that spreadsheet truly created when it claims to have been? Was that email altered before disclosure? Can a screenshot of a WhatsApp chat be trusted as a genuine record of communication?
In a recent article for Your Expert Witness, I discussed the dilemma of deepfakes through a digital forensics lens. The rise of sophisticated editing tools and generative technologies has elevated authenticity disputes from rare exceptions to routine challenges. From ‘deepfake’ media to AI-generated text, the boundaries between genuine and fabricated digital content are increasingly blurred.
As a digital forensics expert, I have acted in several matters where the authenticity of disclosed documents was disputed. These cases span an increasingly diverse range of digital documents – from Microsoft Office documents such as Word or Excel files, to PDFs, text files and exported messages from instant messaging platforms including Skype, WhatsApp and Telegram.
Each format carries its own evidential nuances and pitfalls, and each demands a careful balance of forensic rigour and interpretive caution.
versions of a disputed document, emails or messages referencing its creation and modification, or usage of software to create and/ or modify the document. On mobile devices, message database records can corroborate or challenge the authenticity of messages produced as screenshots.

A recurring challenge in such disputes is the quality and provenance of the evidence presented for analysis. It is common for experts to be instructed to assess documents not in their native form – such as the original digital file complete with metadata – but as secondary copies, printouts or screenshots. These documents may contain the visible content, but often lack the underlying data that allows a forensics expert to verify when, how and by whom a document was created or altered.
Take, for example, a dispute centred on a contract document allegedly backdated to an earlier period. The original native file, if available, would typically contain metadata revealing timestamps of creation, last modification and author information. It might also include embedded metadata that could indicate tampering.
However, if that same document is only produced as a scanned PDF, those critical metadata fields are often stripped away. In such cases, the expert’s ability to reach definitive conclusions on authenticity is significantly limited.
The most meaningful forensic opportunities emerge not from derivative copies but from source evidence – the original devices, systems and/or accounts on which the documents were created, stored or otherwise handled. A computer, mobile phone or cloud account can retain a valuable digital footprint of user actions, timestamps and contextual artefacts that collectively tell the story behind a document.
For instance, forensic imaging of a laptop can reveal previous

Metadata alone can be spoofed, misinterpreted and inadvertently removed or overwritten; access to source evidence provides an expert with the opportunity to thoroughly investigate the facts with context. Building a comprehensive timeline of events around the document’s lifecycle enables corroboration against witness statements describing how and when documents were produced, and allows an expert to provide confident conclusions as to their authenticity.
The case for early expert involvement In high-stakes disputes, digital evidence is often no longer taken at face value. The change in landscape emphasises the requirement for authenticity considerations to be proactive, not reactive. By anticipating the challenge of authenticity early, legal teams can engage experts early ensuring that original evidence can be preserved.
Legal teams and investigators are best served by engaging forensic experts early in the disclosure process, ideally before documents are collected, converted or shared. Too often, by the time experts are engaged following allegations of tampering, key sources of evidence have already been lost – devices have been wiped, repurposed or replaced; online accounts deactivated; and critical contextual data irretrievably gone. Early intervention minimises the risk that key evidence is lost through well-meaning but destructive handling.
As digital evidence continues to underpin an ever-growing proportion of disputes, the question of document authenticity will continue to be raised to digital forensics experts.
Legal teams can engage experts early ensuring that original evidence can be preserved at the disclosure stage. This ensures that any authenticity challenges are met with confidence rather than conjecture. In a landscape where data can be easily copied, altered or fabricated, disciplined forensic methods and independent expert analysis remain the most reliable means of uncovering the truth and defending the issue of authenticity. q
• If you require the support of an expert where document authenticity is disputed, please don’t hesitate to contact me by emailing r.shields@s-rminform.com
[ THE FINANCIAL CONDUCT AUTHORITY (FCA) has censured the Institute of Certified Bookkeepers (ICB) for serious deficiencies in its anti-money laundering (AML) supervision. ICB is a professional body supervisor responsible for overseeing the AML compliance of over 3,000 bookkeepers under the Money Laundering Regulations 2017.
Between January 2022 and July 2023, ICB breached key AML regulations relating to its role as an AML supervisor, thereby increasing the risks of financial crime among members, said the FCA.
The FCA found that ICB failed to adopt an adequate risk-based approach to its supervisory functions and did not effectively monitor its members. The most serious breaches were caused or made worse by ICB’s decision to suspend all inspections – both onsite and virtual – for nine months. During that period ICB’s ability to scrutinise members’ compliance with AML regulations was seriously undermined. The failings exposed the sector to greater money laundering risks.
Therese Chambers, joint executive director of enforcement and market oversight at the FCA, said: “Anti-money laundering rules stop criminals from exploiting the financial system and help protect people, businesses and wider market trust. Strong AML supervision matters because it ensures these safeguards work in practice.

“This outcome demonstrates that the FCA is prepared to take enforcement action against professional body supervisors where their oversight of member organisations falls below the high standards we expect.”
[ THE SERIOUS FRAUD OFFICE (SFO) has published updated guidance on evaluating corporate compliance programmes, providing organisations with greater clarity on how their compliance arrangements will be assessed across a range of enforcement scenarios.
The refreshed guidance outlines the six scenarios in which the SFO may need to evaluate an organisation’s compliance programme, including when considering prosecutions, deferred prosecution agreements, compliance terms and monitorships, potential defences to corporate offences and sentencing considerations.
A key update to the guidance incorporates evaluation criteria for the new offence of failure to prevent fraud under the Economic Crime and Corporate Transparency Act 2023, including assessment of any potential defences of reasonable procedures.
The guidance emphasises that the SFO’s assessment will be based on an organisation’s individual circumstances. It stresses that having policies, procedures and controls in place does not automatically mean a compliance programme is effective. The SFO will examine how policies translate into conduct on the ground.
The new publication marks the latest step in the SFO’s refreshed approach to working with cooperating businesses to encourage best practice. It follows the release of the updated Corporate Cooperation Guidance in April this year and the Joint SFO-CPS Corporate Prosecution Guidance published in August.
Matthew Wagstaff, director of legal services at the SFO, said: “This updated guidance provides organisations with clear expectations and demonstrates our transparent approach to working with organisations that demonstrate best practice. Effective compliance is not a tick-box exercise – it’s about creating genuine cultures that prevent fraud, bribery and corruption.”
The guidance is available on the SFO website at www.gov.uk. q
The government has recently announced planned reforms to make the FCA the Single Professional Services Supervisor, aiming to deliver a more effective approach to combatting illicit finance. The reforms will take time to implement. In the interim, OPBAS – the Office for Professional Body Anti-Money Laundering Supervision, a unit within the FCA – will continue to work with professional body supervisors to ensure compliance with AML regulations. q
[ FRAUDSTERS HAVE BEEN STOPPED from stealing a record £480m from the taxpayer in the government’s biggest ever fraud crackdown, the government has revealed. The figure relates to the year from April 2024 to March this year.
Over a third of the money saved – £186m – comes from identifying and recovering fraud committed during the COVID-19 pandemic. Government efforts to date have blocked hundreds of thousands of companies with outstanding or potentially fraudulent Bounce Back Loans from dissolving before they would have to pay anything back. Millions of pounds have also been clawed back from companies that took out COVID loans they were not entitled to, or took out several loans when only entitled to one.
It builds on successful convictions in recent months to crack down on opportunists who exploited the Bounce Back Loan Scheme for their own gain, including a woman who invented a company and then sent the loan money to Poland.
Alongside COVID fraud, the record savings achieved include clamping down on people unlawfully claiming single person’s council tax discount and removing people from social housing waitlists who wanted to
illegally sublet their discounted homes at the taxpayers’ expense.
Announcing the record figures at an antifraud Five Eyes summit in London, Cabinet Office Minister Josh Simons said: “Working people expect their taxes to go towards schools, hospitals, roads and the services they and their families use. That money going into the hands of fraudsters is a betrayal of their hard work and the system of paying your fair share. It has to stop. That’s why this government has delivered the toughest ever crackdown on fraud, protecting almost half a billion pounds in under 12 months.
“We’re using cutting-edge AI and data tools to stay one step ahead of fraudsters, making sure public funds are protected and used to deliver public services for those who need them most – not line the pockets of scammers and swindlers.”
The AI system scans new policies and procedures for weaknesses before they can be exploited, helping make new policies fraudproof when they are drafting them. The tool could be essential in stopping fraudsters from taking advantage of government efforts to help people in need amid future emergencies. The high-tech push brought around £110m more than the year before back to the exchequer. It has been designed to prevent the scale of
criminality seen through the COVID pandemic, where millions were lost to people falsely taking advantage of furlough, COVID Grants and Bounce Back Loans.
The summit brought together key allies and showcased the government’s unprecedented use of artificial intelligence, data-matching and specialist investigators to target fraud across more than a thousand different schemes.
Over £68m of wrongful pension payments were prevented across major public sector pension schemes, including the Local Government Pension Scheme, NHS Pension Scheme, Civil Service Pensions and Armed Forces pension schemes. The savings were achieved by identifying cases where pension payments continued after the individual had died, often with relatives continuing to claim benefits they were not entitled to.
More than 2,600 people were removed from housing waiting lists they weren’t entitled to be on, including individuals who were subletting or had several tenancies unlawfully.
Over 37,000 fraudulent single-person council tax discount claims were stopped, saving £36m for local councils and taxpayers. The false claims, often made by individuals misrepresenting their household size to secure a 25% discount, were uncovered using advanced data-matching. q
[IN THE EVOLVING LANDSCAPE of personal injury and clinical negligence litigation, the role of independent financial experts has become increasingly pivotal. For solicitors navigating complex claims, the integration of financial insight is not just beneficial; it is essential.
At the core of personal injury and clinical negligence claims lies the principle of restitutio in integrum – restoring the claimant to the financial position they would have occupied but for the injury. This principle is underpinned by:
• OgdenTables (8th Edition): used to calculate future losses, including earnings and pension impacts.
• Damages Act 1996: governs the statutory discount rate applied to future loss calculations as amended by the Civil Liabilities Act 2018.
• Civil Procedure Rules (CPR Part 35): sets out the requirements for expert evidence, including independence and objectivity.
• Mental Capacity Act 2005 & Court of Protection Rules 2017: regulate the management of settlements for protected parties.
• Pre-Action Protocol for the resolution of clinical disputes: encourages early expert involvement and collaborative resolution. Solicitors increasingly instruct independent financial advisers to:
• Model future financial needs in catastrophic injury cases, including care costs and housing adaptations.
• Advise on the suitability of lump sum awards versus Periodical Payment Orders (PPOs).
• Establish and manage Personal Injury Trusts to protect means tested benefits.
• Provide post-settlement investment strategies and ongoing financial planning.
Nick Leech, independent financial adviser at Chase de Vere IFA Group plc, is widely recognised for his expertise in personal injury and clinical negligence claims. He works closely with solicitors,
barristers and forensic accountants; and together with the wider Personal Injury and Court of Protection (PICOP) team, Chase de Vere delivers:
• Settlement planning: tailored advice on structuring awards to meet long-term needs.
• Trust establishment and compliance: ensuring funds are protected and managed in line with legal requirements.
• Court-ready financial evidence: clear, objective and credible reports that support litigation and settlement negotiations.
Nick’s work is particularly valued in cases involving children, individuals lacking capacity and those with lifelong care needs. His work is further strengthened by the specialist skills within Chase de Vere PICOP.
PICOP combines technical financial planning expertise with a deep understanding of the legal and welfare frameworks that govern vulnerable clients. This specialist team ensures that every recommendation is tailored, compliant and aligned with the long-term interests of the claimant.
Chase de Vere operates as a secure UK-based independent advice firm, offering truly impartial guidance. This independence is underpinned by the strength and stability of its parent company Swiss Life – an independent global insurer providing clients and solicitors with confidence in the continuity and security of advice and service.
For solicitors handling high-stakes personal injury and clinical negligence claims, partnering with a trusted financial expert is a strategic advantage. The ability to quantify complex financial losses and present them with clarity and authority strengthens the legal case and improves outcomes for claimants.
As litigation becomes more multidisciplinary, the role of the independent financial adviser is not just supportive; it is indispensable. q
[WITH OVER THIRTY YEARS of experience in the financial services sector, Paxen Group Limited offers clear, independent and authoritative expert witness reports for civil litigation cases involving regulated financial activities.
The firm’s CEO, Andrew Smith, brings a rare blend of practical experience and regulatory insight, ensuring that each opinion provided is firmly grounded in both the letter and spirit of FCA regulation.
Mr Smith’s extensive background as a practitioner within regulated financial services – spanning compliance, risk and operational leadership – allows Paxen Group to interpret complex regulatory matters through the lens of real-world application. This ensures reports are not merely academic but reflect how firms, brokers and lenders operate in practice.
His specialist areas of expertise include:
• Regulatory compliance and governance – oversight failings, systems and controls, and senior management accountability.
• Consumer credit and motor finance – suitability, affordability and responsible lending assessments.
• Regulated mortgage contracts – advice suitability, disclosure obligations and post-completion conduct.
• Insurance distribution – compliance with FCA, IDD and Conduct of Business requirements.
• Conduct risk and consumer duty – fair value, transparency and customer outcome analysis.
All reports are fully compliant with the Civil Procedure Rules (CPR) Part 35 and the Expert Witness Protocol, offering a transparent

separation of fact, assumption and opinion. Paxen Group acts with complete independence, ensuring that findings are objective, defensible and withstand scrutiny under cross-examination.
Ethics and integrity underpin all work undertaken by Paxen Group. The firm accepts instructions solely within its field of competence and applies rigorous internal quality assurance to ensure evidence traceability, methodological consistency and impartiality.
As financial services litigation becomes increasingly complex and regulated, Paxen Group provides solicitors and barristers with expert analysis that combines technical precision with decades of practical experience. q
• For enquiries or instructions contact Andrew Smith, Chief Executive Officer, Paxen Group Limited on 07942 862185 or via email at andrew@paxen.co.uk

By Mark Chester, of Cedarwood Tree Consultants
[AS AN EXPERT WITNESS my starting point with most instructions is an appraisal of the evidence via a desk top assessment and a site visit where appropriate. The feasibility assessment is the basis for advising the client on the merits of their case. As I review the various cases I have worked on over the past few years, I am appreciating, more than ever before, how important that exercise is.
Often, evidence is presented to the courts, or is considered as part of a claim, without it being independently assessed. This can include witness statements. The process is more than simply proof reading. A key member of my team reads through each of my reports before they are issued, to ensure they are clear, follow a logical flow, and that there is no ambiguity. This is not a task for the author; it is very hard to proof read one’s own work.
The simple question: ‘What do you mean by this statement?’ can lead the witness to ensure clarity, without compromising integrity.
One case I was involved with several years ago, where the claimant led on the compilation of evidence, involved a hedgerow, which had been damaged, and the exact position of a boundary and rights of access. The claimant presented me with the statement of a key witness, confident that it supported the case. As I read it, it soon became apparent that this was a first draft document which was vague and presented me with more questions than answers. It didn’t appear to have been checked by a legal specialist.
I shared my observations with the claimant who, on re-reading it, now appreciated the limitations. Apparently, it was too late in the process for the witness to review and the case proceeded to court weakened. That case taught me much about the importance of the pre-trial team meeting to discuss the case – and the value of a good barrister.
Much of my work as an expert witness consists of assessing existing evidence and advising on it. However, I have found it fascinating over the past couple of years to work on cases that were developing in the gathering of evidence. It is interesting to observe, as the merits of a claim may be significantly changed by new material. There is the caveat, for any party, that new evidence may not be beneficial for their case. That is a reality which some choose not to pursue.
In one claim, where a number of trees being grown for timber had been felled and removed from a site in error during utility works, the landowner was seeking compensation, to which they were entitled. The party responsible for paying the compensation wished to ensure that the sum was reasonable and proportionate.
It was evident in that case that the claim had merit in principle but lacked evidence to justify. The claimant commissioned a specialist to advise on a value. It did not match their own claim, being notably lower, but resulted in a sensible settlement. The key issue here was that the original claim was based on assumption, and the defendant was unwilling to settle without evidence.
Two cases I have been involved with have turned dramatically based on new evidence. In one, during a conference call to review the merits and evaluate, I was presented with new material. The instructing barrister asked if, having reviewed this, I would need to update my report and reach a very different conclusion. This was, indeed, the case. He observed: “I think we will need a new report, and I do not think I will like the conclusions this time.” Is this beneficial for that party, in that their case no longer has merit? No. But in terms of proceeding in an informed basis, yes. In another case, where I had been advising the claimant, the new evidence supported the claim.
Appraising the evidence can enable parties to make timely adjustments to their response. For one party, facing enforcement action for allegedly pruning a protected tree beyond what was approved, my counsel resulted in a change of plea and no need for

a formal hearing. For another client, they were able to proceed with confidence in a not guilty plea. In that case, I remember meeting the client and their barrister on site ahead of a planned hearing. The barrister had been surprised at his client’s confidence. Then, having read my report, we finally we met on site. The basis for the confidence, based on my feasibility assessment, was soon apparent.
When I begin to assess the merits of a case, and the evidence provided, I am looking for what I call the ‘smoking gun’ – the piece of evidence that really supports the instructing party’s view; or the claimant’s if I am reviewing a case for loss adjusters seeking an independent view to enable them to resolve a claim. This may be at the top of the pile. It may be missing initially. It may not exist yet and need to be commissioned. Its absence may be sufficient evidence itself that the party does not have a strong case.
Having the evidence accessible and clearly presented is really important. In one case I was involved with, which went to a hearing, two items which supported the defendant’s case were not presented to the court. Both demonstrated errors in the prosecution case which I was aware of. For one, the absence limited the scope of my being cross-examined. For the other, there was the moment when the defendant’s barrister realised that a document was not in the building and, without it, he was unable to back up his argument.
Most of my work requiring feasibility described here is for legal cases. However, I also use it for surveying trees in connection with development sites. In most cases, the proposals are feasible with an appropriate structure of protection measures. Sometimes, challenges present themselves which require specific measures.
Occasionally, what is proposed is unrealistic and I have to deliver that reality to the instructing party. What can be additionally difficult is when the issues were evident at the start and the client has already spent money on an architect, designs and other specialist surveys. My advice, in such cases, is to instruct for the feasibility element at the earliest opportunity. It may save money and enable an informed approach on how to proceed. One client observed, as I explained that he was unlikely to be successful with his dream home due to the constraints present: “I wouldn’t have bought the site if I’d known.”
Feasibility ensures that the merits of a case are evaluated, including the strength of evidence. It allows opportunity for reviews and for swift resolution where possible. New evidence may require a re-evaluation of a previous position. For me, however, it is the basis for providing a truly professional service to my client. q
By Mark Hinnells, director of Susenco Consulting Ltd
[
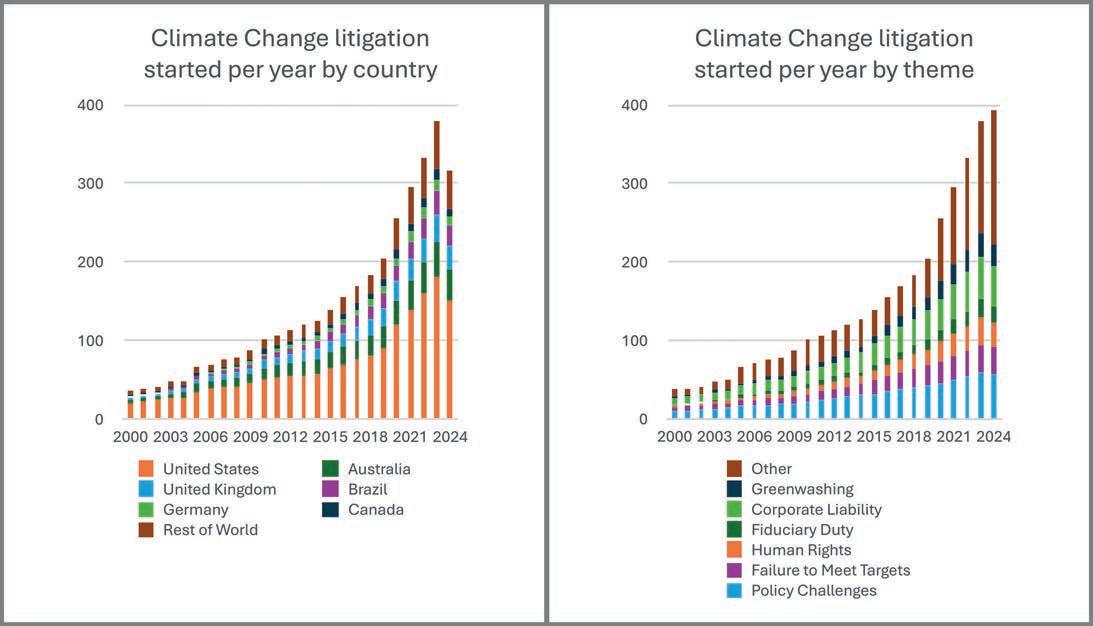
LITIGATION ON CLIMATE CHANGE IS, quite literally, heating up! In the past few months there have been two reviews of climate change and litigation: the UNEP Global Climate Litigation Report: 2025 Status Review was published in October, and the Grantham Research Institute at the London School of Economics published a review in June. Both reviews rely on data from the Sabin Center for Climate Change Law at Columbia University, which maintains a database of US and global litigation.
Since 1986, when the first climate case was recorded, there has been a steady rise in the number of cases and jurisdictions involved, with a broadening range of legal arguments used, and increasingly diverse groups turning to law. As of 30 June 2025 a cumulative 3,099 climate-related cases have been filed in 55 national jurisdictions or 24 international or regional courts, tribunals or quasi-judicial bodies.
Cases fall into three main types:
• Cases against governments
• Cases against corporations
• As pro-climate litigation grows, so anti-climate cases are also on
• the rise, particularly in the US.
To unpack those themes
Climate rights and policy failures
Courts are holding governments accountable for failing to meet statutory climate targets. For example, UK courts have twice ruled that the government’s climate strategies breach the Climate Change Act (Client Earth and Friends of the Earth v UK Government 2024). Similar challenges are emerging in other jurisdictions.
Climate and planning policy, much of which is in a quasi-judicial setting like public inquiries or planning appeals Climate change is now a material factor in major planning

decisions in the UK. Courts have required downstream emissions in environmental impact assessments: in the UK Finch v Surrey County Council 2024 and in Europe via Föreningen Greenpeace Norden and Natur og Ungdom v State of Norway (EFTA Court Advisory Opinion, May 25).
Climate and human rights
Cases are increasingly being brought by groups who feel themselves under pressure, for example youth, indigenous peoples and the elderly. Courts recognise the link between climate inaction and violations of rights to life, health and a healthy environment (KlimaSeniorinnen v Switzerland in the European Court of Human Rights in 2024, and Held v Montan, upheld in the Montana Supreme Court in 2024).
Climate, fiduciary duty and investing
Trustees in some jurisdictions face a lack of guidance, or conflicting perspectives, on the extent to which climate risks fall within fiduciary duty, though increasingly climate risks are seen as integral to both risk management and fiduciary duty. The Paris Agreement targets are written into Pensions legislation in the UK (Pensions Schemes Act 2021 S124).
Previously I have explored how, in the UK, in McGaughey v USS 2023 in the Court of Appeal, the Universities Superannuation Scheme faced a challenge in court on grounds of failing to perform fiduciary duty, but avoided being challenged on longer-term plans. In Canada the Supreme Court found that ‘climate change poses an existential threat’. As such, the duty of prudence requires a forward view, and duty of loyalty highlights a need to consider climate risk across generations.
Following that, four young people who will retire after 2050 are suing the Canada Pensions Plan Investment Board for failing to protect their pensions from climate risk.
Shareholders are testing directors’ duties (including fiduciary duty) through climate-related claims. However, it seems corporate law is more laissez-faire than human rights law, and gives more freedom to directors to steer between conflicting interests of different stakeholders. I have previously reported on how courts are reluctant to impose specific climate strategies on directors, though directors are under increasing scrutiny to align corporate strategy with climate goals, for example ClientEarth v Shell, UK High Court 2023 Climate and greenwashing
NGOs and consumers are increasingly using consumer protection and securities laws to challenge greenwashing. TotalEnergies in the Paris Court of Justice 2025 was perhaps the first major firm found guilty in France of misleading the public about its climate pledges. Anti-climate cases
Including cases brought forward to delay or dismantle climaterelated measures or actions, or to intimidate or silence climate advocates. For example, in 2024 Exxon sued climate activist investors in a bid to stop climate resolution from going to a vote at its annual investor conference.
Key conclusions include:
• The use of human rights law to frame state obligations on
• climate change is becoming common.
• Human rights law seems to be more in favour of the plaintiff
• than corporate law, which seems reluctant to interfere with the
• balancing act that directors have to perform to satisfy various
• stakeholders. I have previously explored how the use of human
• rights law will be aided by the recent influential but not binding
• judgements from the ICJ Advisory Opinion on Obligations Of
• States In Respect Of Climate Change in July 2025 and the Inter
• American Court of Human Rights (Advisory Opinion 32, July 2025).
• Courts and other adjudicatory bodies often require a clear,
• individualised and imminent harm to confer victim status – a
• threshold that is often difficult to meet given the nature of
• impacts of climate change. Climate attribution studies, such
• as exploring the likelihood of particular extreme weather events
• to emissions, will become increasingly important.
• The effectiveness of climate litigation depends on the remedy
• available. While lawsuits, even before a final decision, can
• exert pressure on legislatures and companies to change, the
• absence of strong enforcement frameworks or institutions,
• especially transnationally, limit the practical impact of climate
• rulings.
• Cases have increased by close to an order of magnitude since
• 2000. The US accounts for half of cases, representing the
• polarised nature of the debate in the US, as well as the litigious
• nature of the society. The UK accounts for 10% of cases,
• showing the importance of climate as a policy issue. Policy
• challenges or failure to meet targets account for 45% of cases,
• human rights 12% and cases aimed at the private sector
• (fiduciary duty, corporate liability and greenwashing) account
• for 43%.
In conclusion, climate change is increasingly a point of dispute and friction between stakeholders, ranging from NGOs and campaigners through to shareholders, private citizens, directors, regulators and government ministers. Within the client base of every large legal firm will be a larger client who, if they don’t have a case right now, will have one brewing, either in their own business or within their upstream supply chain or downstream customer base.
The preferred route, when there is friction between stakeholders, is clearly to reach a solution together through collaboration or arbitration. However, the risk of litigation is clearly heating up. Susenco would be very pleased to help with finding a resolution – or failing that, supporting litigation. q

[ JAPANESE KNOTWEED is one of the UK’s most problematic invasive plants – and its impact has extended far beyond gardens and development sites into property law and litigation. Introduced in the 19th century as an ornamental species, it now represents a legal risk for landowners because it spreads aggressively underground, is difficult to eradicate and can affect property use and value. It is not illegal simply to have Japanese knotweed growing on your property. The key legal point is that you must not cause it to spread. Japanese knotweed is listed under Schedule 9 of the Wildlife and
Countryside Act 1981, which makes it a criminal offence to plant it or otherwise cause it to grow in the wild. That includes actions that might unintentionally spread it, such as moving contaminated soil off site or disposing of it improperly. In addition, the Environmental Protection Act 1990 classifies knotweed material as controlled waste. Any plant fragments, roots or soil that contain knotweed must be handled by a licensed waste carrier and disposed of at an approved facility. Homeowners, developers and contractors have a legal duty of care to ensure disposal is compliant.
Civil law has also developed around knotweed, particularly in relation to private nuisance. A landmark Court of Appeal judgment in 2018, Network Rail Infrastructure Ltd v Williams , confirmed that allowing knotweed to encroach from one property onto another can amount to a legal nuisance, even if no physical structural damage has occurred.
The court held that knotweed’s presence creates a ‘natural hazard’ affecting the amenity and value of neighbouring land. As a result, affected homeowners may seek compensation for treatment costs and losses, and they can apply for injunctions requiring the responsible landowner to control or eradicate the plant. The important principle established is that landowners must take reasonable steps once they are aware of knotweed on their land, especially near boundaries.
The presence of knotweed can also influence property transactions. Sellers are expected to disclose whether the property is affected through the Law Society’s standard inquiries form. Failing to disclose known knotweed can lead to legal action for misrepresentation if a buyer later discovers it. Many mortgage lenders require evidence of a professional knotweed management plan before approving lending on affected properties. Those plans typically include long-term herbicide treatment or excavation undertaken by a specialist contractor, as well as an insurance-backed guarantee to protect the buyer and lender.
While enforcement varies, local authorities and agencies have powers to require action where knotweed is causing ongoing problems. Under anti-social behaviour legislation, councils can issue notices compelling owners to control the plant where its spread is having a detrimental impact on the community.
The consistent message in UK law is that knotweed creates responsibilities, not automatic criminal liability. Owners are expected to manage it properly, prevent its spread and follow strict disposal rules. Taking early professional advice, keeping clear records of treatment and acting promptly if there is a risk of encroachment are the safest ways to protect both property and legal position. q
[ IN THE FAST-PACED WORLD of modern air travel, aviation relies on a complex network of engineering, regulatory oversight and asset management. When disputes arise – whether commercial, contractual or following accidents – courts and arbitration panels often face challenges in understanding highly technical issues. That is where aviation professionals acting as expert witnesses make an indispensable contribution.
Expert witnesses with aviation backgrounds bring clarity and authority to matters that would otherwise be opaque to legal decision makers. Their expertise spans aircraft maintenance, airworthiness, regulatory compliance, engine performance and operational safety.
In commercial disputes, such experts help determine whether parties have met contractual obligations, adhered to maintenance schedules or complied with safety standards. They also assess the condition and performance of aircraft and components, providing independent and objective evaluations that underpin the resolution of high-value claims.
In accident investigations, aviation experts play a crucial role in reconstructing events, analysing system failures and interpreting flight data. Their assessments can identify the root causes of incidents, distinguishing between human error, mechanical malfunction or procedural lapses. Courts and tribunals rely heavily on their reports to understand the interplay of technical and operational factors, ensuring decisions are based on evidence rather than speculation.
Beyond technical analysis, the ability of aviation experts to communicate complex information in clear, concise terms is vital. Judges, arbitrators and juries often lack specialist knowledge, making the expert’s skill in translating engineering, maintenance and regulatory concepts into understandable evidence – a cornerstone of effective dispute resolution.
As the aviation industry continues to evolve, with increasingly sophisticated aircraft and tighter regulatory frameworks, the role of the expert witness remains critical. Their insights not only inform legal outcomes but also uphold safety standards, reinforce compliance and provide confidence to parties navigating high-stakes disputes.
In essence, aviation professionals serving as expert witnesses bridge the gap between technical complexity and legal scrutiny, ensuring that decisions in the sector are fair, informed and technically sound. q

[ THE OIL AND GAS SECTOR is undergoing profound change. As energy markets shift towards decarbonisation, regulatory frameworks evolve and commodity prices fluctuate, disputes in the industry are becoming increasingly complex. Expert witnesses in petroleum engineering, geoscience, health and safety, environmental impact, valuation and energy economics play a critical role in helping courts, tribunals and arbitration panels make sense of these challenges. Their analyses are essential across the full spectrum of oil and gas operations from exploration and production to transportation and decommissioning.
In disputes concerning exploration and production, petroleum engineers and geoscientists provide technical insight into reservoir performance, drilling operations and the interpretation of seismic and subsurface data. Their evidence can determine whether operational decisions were consistent with industry standards and whether any deviations contributed to financial loss or project delays.
Environmental experts, meanwhile, assess the impact of exploration and production activities on surrounding ecosystems, ensuring that regulatory compliance and sustainable practices are considered in claims of liability.
Transportation and decommissioning also generate contentious issues. Experts may be called upon to evaluate pipeline integrity, shipping risk or offshore platform decommissioning strategies. Their analyses help establish whether operators met safety and regulatory obligations, whether costs and timelines were reasonable and whether environmental or operational risks were appropriately managed. Health and safety specialists often focus on procedural compliance and risk mitigation, translating complex operational practices into clear evidence for non-technical decision-makers.
Contract performance and joint venture disputes are another major area where expert evidence is pivotal. Valuation experts and energy economists can model financial outcomes, assess the reasonableness of investment decisions and quantify damages arising from project underperformance or partner disagreements. Those assessments often require consideration of market volatility, regulatory changes and broader energy transition dynamics, highlighting the commercial as well as technical dimensions of the dispute.
Environmental liability and operational safety claims increasingly rely on a multidisciplinary input. Experts interpret evolving regulations, assess the adequacy of mitigation measures and evaluate the consequences of operational failures. Their evidence can determine whether harm was foreseeable, whether risk management adhered to industry norms and how potential damages should be calculated.
Ultimately, expert witnesses serve as a bridge between complex technical realities and legal scrutiny. In an industry defined by high stakes, evolving standards and rapid innovation, their evidence provides tribunals with the clarity, context and technical rigour required to resolve disputes fairly. q

[ DOES A SELLER’S FAILURE to deliver a ship by the agreed Cancelling Date under a ship sale Memorandum of Agreement (MOA) on the Norwegian Saleform 2012 (NSF 2012) – resulting in the cancellation of the MOA – entitle the buyer to recover ‘loss of bargain’ damages under Clause 14 of the NSF 2012, where that failure did not amount to a repudiatory breach by the seller?
That was the thorny problem addressed by the Court of Appeal recently when it was asked to overturn a previous decision of the High Court in the case of Orion Shipping & Trading LLC v Great Asia Maritime Ltd (The LILA LISBON) [2025] EWCA Civ 1210.
Sebastian Lea and Maria Kaperoni of Baltic Exchange members Clyde & Co explained the complexities of the case: “In this case, the seller (Orion Shipping and Trading LLC) had agreed to sell the Lila Lisbon, a capesize bulk carrier, to the buyer (Great Asia Maritime Ltd) for $15m under a Memorandum of Agreement made on the Norwegian Saleform 2012, dated June 4, 2021.
“Following the seller’s failure to serve the Notice of Readiness by the (extended) Cancelling Date, the buyer proceeded to cancel the sale contract in accordance with its terms and commence arbitration proceedings. The buyer sought to recover from the seller $1.85m; this amount representing the difference between the market price of the vessel at the date of cancellation ($16.85m) and the sale contract price ($15m).
The Tribunal found that the seller’s failure to deliver by the Cancelling Date was due to proven negligence on their part and concluded that the buyer was entitled to loss of bargain damages under Clause 14.”
Under the terms of the MOA, Clause 14 of the NSF 2012 provided that, “should the Sellers fail to give Notice of Readiness…or fail to be ready to complete a legal transfer by the Cancelling Date the Buyers shall have the option of cancelling this Agreement…In the event that the Buyers elect to cancel this Agreement, the Deposit together with interest earned, if any, shall be released to them immediately.”
Lea and Kaperoni related that the Arbitration Tribunal found in favour of the buyer and awarded them $1.85m by way of damages for ‘loss of bargain’, together with compound interest at 5% per annum. The Tribunal found that the seller’s failure to deliver by the Cancelling Date was due to proven negligence on their part and concluded that the buyer was entitled to loss of bargain damages under Clause 14.
Following an appeal by the seller to the High Court, the judge reversed the Tribunal’s award, holding that the buyer was not entitled to damages for ‘loss of bargain’ under Clause 14 and that, furthermore, the seller was under no obligation to provide Notice of Readiness by the Cancelling Date.
Importantly, the Court did not find the seller’s conduct to be a repudiatory breach.
“The buyer proceeded to appeal to the Court of Appeal which held that a buyer was entitled to ‘loss of bargain’ damages where the seller’s failure to deliver the vessel by the Cancelling Date was caused by ‘proven negligence’ as contemplated by Clause 14 of the NSF 2012.
“Furthermore, the Court found that, under the NSF 2012, a seller is under an obligation to use reasonable diligence to deliver the vessel by the Cancelling Date. It held that the Judge was wrong to conclude that there was no obligation on sellers to tender Notice of Readiness, nor to be ready to validly complete a legal transfer, by the Cancelling Date.”
Importantly, the Court did not find the seller’s conduct to be a repudiatory breach. Typically, under English law, ‘loss of bargain’ damages are only recoverable where a contract is terminated following such a breach. However, Clause 14 of the NSF 2012 creates a distinct contractual mechanism: if the seller fails to deliver due to proven negligence, the buyer may cancel and claim compensation for losses and expenses, including the ‘loss of bargain’.
So, what was the ‘proven negligence’ in the Lila Lisbon?
Lea and Kaperoni explained: “The seller’s failure to deliver by the original Cancelling Date of 20 August 2021, derived from regulations at Qingdao which required the departing crew to leave mainland China on the day of disembarkation. The seller’s failure to arrange the necessary flights in time, resulting in the loss of the berthing slot, constituted ‘proven negligence’ on the part of the seller.” q

















COLLISION INVESTIGATION & RECONSTRUCTION

COMPLIANCE CONSULTANTS


COMPUTER & MOBILE FORENSICS


DIGITAL TECHNOLOGY

ENERGY CONSULTANTS


EQUESTRIANS
ERGONOMICS

FINANCIAL SERVICES
















Andrew F Acquier BA FRICS
Chartered Art & Antiques Surveyor
Expert witness reports and representation at court for matters involving:
• Divorce settlements • Insurance valuation disputes • Arts litigation
• Contentious Probate • Associate member of Resolution for many years
www.andrewacquier.co.uk
Clarke Gammon
Chartered Surveyors with experience in All Aspects of Property • Residential property values
• Asset valuations • Land values and more www.clarkegammon.co.uk
Crowe Expert Witness Services
Forensic and Tax Resolutions Specialists Audit / Tax / Advisory / Consulting Smart decisions. Lasting value. www.crowe.co.uk
DRC Forensics Limited




DRC Forensics Limited offers the complete range of forensic accounting & litigation support: • Fraud • Money laundering
• Partnership disputes • Loss of profit • Professional negligence www.drcforensics.co.uk
FHDI - Kathryn Thorndycraft-Pope

Formedecon Ltd
Forensic & Investigative Services to the Legal Profession
• All Aspects of Forensic Work Undertaken
• LAA and Privately Funded • Free Estimates www.Formedecon.com
Dr Dan Jones PhD MSc BSc MA MEWI Cert

Ecological Consultant – Japanese Knotweed. Undertakes expert witness instructions, including the preparation of expert reports and giving evidence in court, in civil claims relating to the growth and spread of all invasive plants.
www.advancedinvasives.com
Mr Chris Makin
• Chartered Accountant • Accredited Civil Mediator

Mr Roger Flaxman ACII MAE
Chartered Insurance Practitioner with more than two decade’s experience serving as an expert witness in matters of insurance practice, broker’s duty of care, insurance market procedure and as an advocate in the resolution of disputed insurance claims.
Examining documents & handwriting • to determine authenticity • to expose forgery • to reveal aspects of origin. Electro Static Detection Apparatus and Mi-Scope used. www.forensichandwriting.co.uk www.flaxmanpartners.co.uk

Forensic Collision Investigation & Reconstruction Ltd
Specialists in the analysis of road traffic collisions
• Collision Reconstruction • Expert Witness
• Vehicle Examinations www.FCIR.co.uk

Simon Quinton Smith BSc FRICS MI Hort
Expert Witness to the Garden Centre & Horticultural Industry
• Rent Reviews • Lease Renewals
• Accredited Expert Determiner www.chrismakin.co.uk www.quintonedwards.co.uk
Valuation
Planning

Compensation
Tax Issues
Colin Todd – Fire Safety Expert
• Fire safety management
Fire risk assessment
• Means of escape • Fire protection of buildings
• Fire engineering • Application of fire safety legislation
• Fire detection and alarm systems www.cstodd.co.uk



www.woodexperts.com WOODEXPERTS
Timber Consultancy and Training since 1991 • Site visits & investigations • Structural surveys
Desktop analysis & review of documents
Species identification

[A MAJOR CONCERN for practically as long as this publication has been covering medical negligence issues has been the cost to the NHS of settling claims. The latest perfect storm to beset NHS Resolution – the body that is tasked with settling claims, formerly the NHS Litigation Authority – is made up of the National Audit Office and the House of Commons Public Accounts Committee. The former has revealed that the current liability of the NHS is £60bn – up from £14.4bn in 2006/7. That represents a more than trebling in two decades.
The House of Commons Public Accounts Committee has described the lack of a plan to address the level of claims as ‘unacceptable’. In its defence, NHS Resolution points to the number of claims settled without going to court.
• Not ones to normally jump to the defence of NHS Resolution, we can point to the fact that it does prosecute when it comes across cases of people attempting to defraud the NHS. One such case occurred in Lincolnshire, where a woman attempted to claim over £3m for damages concerning a cauda equina case – despite the fact she had made a good recovery. She has been sentenced to 26 weeks in prison.
• Another NHS organisation that has come in for a buffeting of late is the Care Quality Commission (CQC). That body has grasped the nettle and set about reorganising its processes and procedures. It is looking to carry out much more inspections, by inspectors with qualifications more attuned to the task in hand.
• It is, it seems, the season to relaunch strategies. The General Dental Council (GDC) has also published a new strategy for the forthcoming three years, during which it will ‘champion a model of regulation that supports professionalism, enables learning and resolves issues quickly and proportionately’. It has recognised previously that fitness to practise cases can have a devastating effect on dentists, often for minor infringements if any. Restructuring should ensure only the most serious failings result in full-blown investigations.
• All of these bodies have as their main concern the safety of patients. That is also the stated main aim of all medicine’s professional bodies – although, as the Society for Cardiothoracic Surgery points out, surgeons must not shy away from risk, but manage it effectively. Recently, however, inquiry after inquiry has revealed a climate of fear to speak out among medical staff.
That problem has been addressed by the General Medical Council, which has stated that not only should clinicians speak out when they encounter patients safety issues, but management must act on those concerns.
• The BIG ISSUE when it comes to patient safety, particularly as winter sets in, is that of patients being stacked up in A&E departments and treated in corridors. The Royal College of Emergency Medicine has complained that the issue has been ‘forgotten’ in Rachel Reeves’s Budget – lost in the rhetoric around community care and reducing waiting lists.
• Another group of patients who are feeling ‘forgotten’ is the multitude of victims of the infected blood scandal. Despite the outcome of the Infected Blood Inquiry, a group of organisations representing victims have made their feelings known to the government on the length of time it is taking to receive compensation – too late for some.
• As a lay patient of the NHS it sometimes feels that the medical community can’t make up its mind about who we should turn to. We are urged on one side to avoid going to A&E except in the most dire emergency, yet GPs are complaining that a contract clause requiring them to make online contacts available is leading them to field enquiries that should be referred to A&E. Sometimes they are not addressed until the situation has deteriorated. q


[ NOW AT £60bn, the government’s liability for clinical negligence claims has increased in real terms from £14.4bn since 2006-07 and is the second largest liability on the government balance sheet, a report by the National Audit Office (NAO) has found. Cost increases in the past 10 years were largely due to a small number of highvalue claims.
Although NHS Resolution has taken significant steps to control costs, the NAO has advised that even more can be done to manage cost pressures, including building on the use of analytics and DHSC reviewing the approach to claims in cases where the legal costs exceed the amount of compensation.
NHS Resolution (NHSR) is responsible for handling clinical negligence claims against the NHS in England. The Department of Health and Social Care (DHSC) oversees NHSR and develops policy to manage the costs of clinical negligence cases. Between 2006-07 and 2016-17, the number of settled clinical negligence cases more than doubled, from 5,625 to 11,397. Most claims related to hospital activity, but volumes have been relatively stable since they peaked in 2016-17.
The NAO said: “Since 2016-17 increases in costs are due to rising amounts of compensation paid out on claims. This is primarily due to a small number of very high-value claims. Reasons for increased compensation include advancements in medicine and treatments, and people needing more care as they live for longer. Damages on very-high value cases (with awards of £1m or more) accounted for 68% of all costs in 2024-25, despite only constituting 2% of claims by volume.”
The NAO points to a rising tendency to settle claims at private healthcare cost, while claimants may be entitled to NHS treatment.
“There is also a risk that government may be paying twice in some cases: first by settling a claim, and then again by paying for further treatment as patients could go on
to use publicly funded health or social care services, despite the settlement being paid with the assumption that they will use the private sector.”
The level of claims is once more being investigated by the House of Commons Public Accounts Committee (PAC), which has found it ‘unacceptable’ that the DHSC has yet to develop a plan to deal with the cost of clinical negligence claims, with so much taxpayers’ money being spent on legal fees. It found that £58.2bn had been set aside to cover the potential cost of clinical negligence events in the 2023-24 accounts – the second largest liability across government after nuclear decommissioning.
The PAC last scrutinised the topic of clinical negligence in 2017, saying at the time that bold action was required to address the impact of claims on resources
available for frontline care and patients. Its report urged government at the time to end its complacency over the cost of clinical negligence, with the annual amount paid out having quadrupled over the preceding decade from £0.4 billion in 2006-07 to £1.6 billion in 2016-17.
NHS Resolution points to its efforts in settling claims without going to court. In its response to the NAO report it said:
“The proportion of claims resolved without litigation has increased from 67% in 2006-07 to 83% in 2024-25. In addition, most clinical negligence cases (99.8%) did not proceed to trial in 2024-25, reducing both costs and emotional distress for patients and healthcare staff.
“The report highlights NHS Resolution’s innovation in dispute resolution and learning from claims such as the Early Notification Scheme for maternity.” q
[ A WOMAN from Lincolnshire has been jailed for contempt of court after being found to have deliberately misrepresented a claim for damages against the NHS of over £3m.
On 15 October she received a 26-week custodial sentence, of which she will serve a minimum of half, and was ordered to pay £135,000 towards legal costs.
Kae Burnell-Chambers brought a clinical negligence claim against Northern Lincolnshire and Goole NHS Foundation Trust in November 2019 for an alleged delay in diagnosis and treatment of cauda equina syndrome. However, surveillance footage and extracts of social media entries and videos obtained by NHS Resolution revealed significant discrepancies in Burnell-Chambers’s account of her condition and capabilities. Following disclosure of the evidence, Burnell-Chambers accepted her clinical negligence claim was fundamentally dishonest and discontinued her claim.
On 25 July 2025, almost two years after proceedings were issued against her, BurnellChambers provided a written guilty plea in which she accepted she had deliberately misled the legal teams and medical experts instructed during the clinical negligence claim, with the intention of seeking to receive more compensation.
Helen Vernon, chief executive of NHS Resolution, said: “All aspects of the clinical negligence claim were based on a dishonestly exaggerated claim. The truth was that [she] had made a good recovery. She lied about her symptoms to make a substantial claim. The trust found you out…taking all into account and mitigation evidence, it is appropriate to impose an immediate custodial sentence.” q


[
FOLLOWING A NUMBER of critical reviews of its operations, the Care Quality Commission (CQC) has reported how it has been working to rebuild itself, getting it back to its purpose of providing effective regulation of health and adult social care services.

According to a statement by CQC: “We have made progress on addressing some of the most urgent challenges that affect the way we work. This includes improving the experience for providers when registering with us and tackling our backlog of applications.
[MILKWOOD CARE LTD, the provider of Ganarew House Care Home in Herefordshire, has been ordered to pay £33,230 at Kidderminster Magistrates’ Court, following a prosecution brought by the Care Quality Commission.
The provider pleaded guilty to one offence of failing to provide safe care and treatment to Mrs Eva Cox, thereby resulting in avoidable harm. That is an offence contrary to Regulations 12 and 22 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014. It was fined £6,000 and also ordered to pay £27,040 costs to CQC, and a victim surcharge of £190.
Eva was admitted to Ganarew House on 9 March 2020. She was 98 years old and had mixed vascular and Alzheimer ’s type dementia.
She was known to staff to have a desire to leave the care home and return to her own home. Between 10 January 2020 and 24 May 2021 Eva attempted to leave the care home on seven occasions; five were via windows. Then, on 1 June 2021, Eva entered the firstfloor shower room and got out through the window onto a flat roof, which was around eight feet off the ground. In attempting to lower herself from the roof, Eva fell and sustained a serious injury, which resulted in her being unable to walk.
The window which Eva went out of had a built-in restricted hinge; however it was not fitted with a window restrictor that complied with national guidance.
An investigation by CQC found Milkwood Care Ltd failed to ensure Ganarew House Care Home was safe and that adequate window restrictors were fitted.
Amanda Lyndon, CQC’s deputy director of operations in the midlands, said: “This was an awful, preventable incident, and our sympathies are with Eva’s family. The provider failed in its duty to protect her in a place she should have been safe and receiving the best possible care.
“It’s unacceptable that staff were aware of Eva’s attempts to leave the care home on several occasions prior to the incident; however she was still able to leave the property and come to harm, which should have never happened.
“I hope this prosecution reminds all care providers they must always ensure people’s safety and manage risks to their health and wellbeing.
“The majority of providers do a good job; however, where we find someone has been put at risk of harm, we will use our regulatory enforcement powers to protect people.” q
We are testing a simpler registration form and improving our online guidance to help make the process quicker and clearer.
“Under our four Chief Inspectors we have moved into operational inspectorates focused around areas of sector expertise. Making these changes means we are now delivering more assessments and are on track to meet our target of 9,000 assessments by the end of September 2026. We have also recruited more registration inspectors, and are seeing a steady increase in the volume of registrations completed each month.”
Alongside immediate improvements, CQC has been looking to the long-term: “The changes we are making include reviewing our assessment framework and methodology and making sure we provide effective guidance to support providers. There is also a significant amount of work needed to improve our digital platforms and how we manage, use and store data. To manage these changes effectively while not hindering our ability to inspect, this work needs to be planned and scheduled.
“Learning from previous experience, we will move forward in a planned way with clear points to pause and review progress before continuing. We will be guided by a clear plan that sets out the direction, priorities, and capabilities we need as we rebuild our regulatory services. This plan represents our shared view of where we’re going and how we’ll get there together.”
CQC says its immediate focus is on actions until the end of 2026, with longer-term planning for delivering the changes up to the end of 2028. q
[ A JOINT National Patient Safety Alert has been issued by the NHS England National Patient Safety team, in collaboration with the Royal Pharmaceutical Society, Royal College of Physicians and Royal College of General Practitioners, about the risk of harm from inadvertently recording patients’ penicillin allergies as penicillamine allergies in electronic prescribing and medicines administration (EPMA) systems.
According to NHS England: “There are reports of healthcare staff incorrectly recording a patient’s penicillin allergy as a penicillamine allergy in electronic prescribing systems. This error risks a patient with a known penicillin allergy being administered a penicillin-based antibiotic and having a potentially fatal anaphylactic reaction.”
The release explains: “Penicillin describes a group of broadspectrum penicillin-based antibiotics. Penicillamine is a drug used to treat Wilson’s disease and severe active rheumatoid arthritis.”
The alert requires primary and secondary care organisations to form working groups to identify affected patients, clinically review and correct allergy records, implement additional safeguards in training and processes and work with digital system suppliers to develop technical mitigations.
All actions must be completed within 12 months.
Patients do not need to take any immediate action, the report says. Healthcare staff should always check a patient’s allergy status before prescribing or administering medication as part of routine safety procedures. Affected patients may be contacted directly by a healthcare professional.
The NHS England National Patient Safety team was the first national body to be accredited to issue National Patient Safety Alerts by the National Patient Safety Alerting Committee (NaPSAC), whose responsibilities now come under the National Patient Safety Committee.
All National Patient Safety Alerts are required to meet NaPSAC’s thresholds and standards. Those thresholds and standards include working with patients, frontline staff and experts to ensure alerts provide clear, effective actions for safety-critical issues.
The National Patient Safety Committee requires providers to introduce new systems for planning and co-ordinating the actions required by any National Patient Safety Alert across their organisation, with executive oversight.
Failure to take the actions required under any National Patient Safety Alert may lead to the Care Quality Commission taking regulatory action. National Patient Safety Alerts are shared rapidly with healthcare providers via the Central Alerting System (CAS). q
[ A SIMPLE NECK SCAN can identify men with double the risk of heart failure compared to their peers, according to research led by University College London.
A carotid ultrasound, like the ultrasound for pregnant women, is quick and painless, using a small handheld device moved gently over the neck to scan the arteries underneath. When around 1,600 men over the age of 70 received the scan, it showed the ‘flexibility’ of their carotid arteries: how much they stretch and expand with each heartbeat.
The quarter of men with the least flexible carotid arteries were 2.5 times more likely to develop heart failure than those with the most flexible carotid arteries.
The researchers, funded by the British Heart Foundation and the National Institute for Health and Care Research, say people at risk of heart failure could be encouraged by doctors to eat more healthily, do more exercise and take medications, if needed, to help reduce their risk.
GPs do not currently routinely carry out the cheap and easy scan on healthy patients without symptoms. But where GP surgeries have the capacity, offering a neck scan to older people to measure the flexibility of their arteries could help them better understand their risk of future heart failure, according to the researchers.
Having relied upon data from the British Regional Heart Study, which began in the 1970s and only involved men, researchers highlight that the findings next need to be looked at in women. q
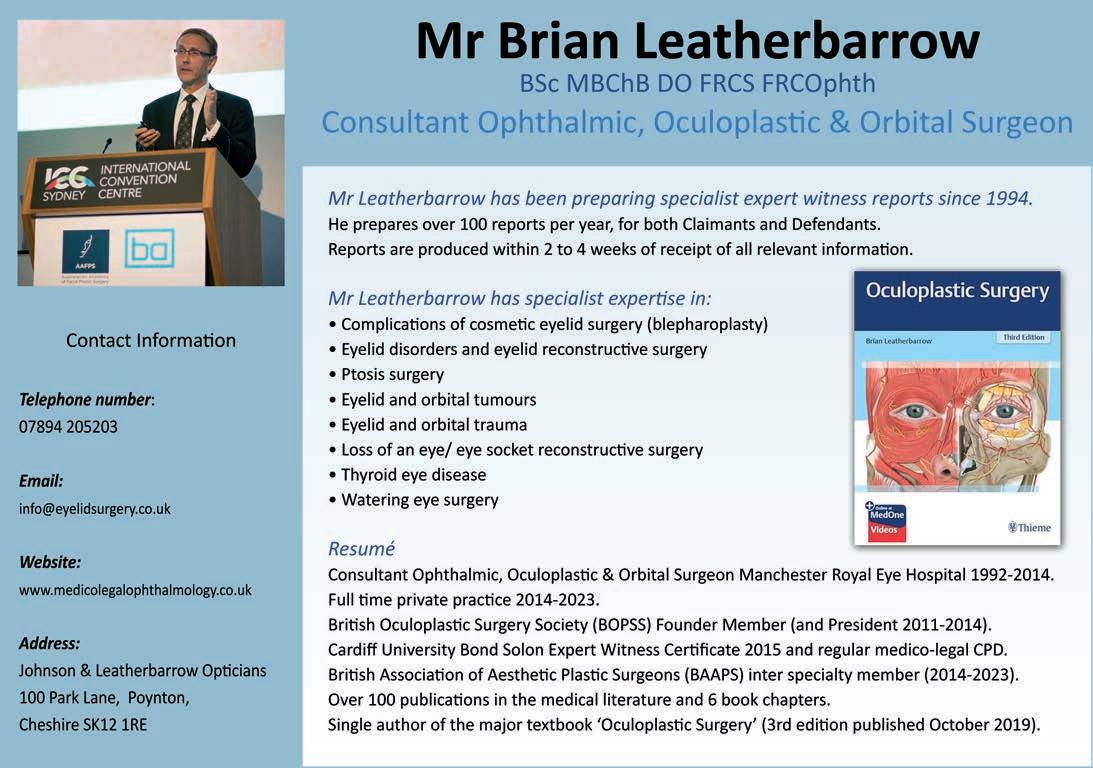
[DOCTORS, physician associates (PAs) and anaesthesia associates (AAs) must speak up if they spot patient safety concerns, and healthcare leaders must act when issues are raised with them, the General Medical Council (GMC) said as it launched a review of key guidance.
The GMC is seeking views on two pieces of its guidance, Raising and acting on concerns about patient safety and Leadership and management Both pieces of guidance play crucial roles in setting positive workplace culture standards that prioritise patient safety. They make clear the regulator’s expectations on when and how concerns should be raised, as well as how those in management positions should respond.
The regulator is ensuring the guidance reflects developments across the UK’s healthcare systems, and wider social changes, while remaining
[
THE BMA, which is a core participant in the UK COVID-19 inquiry, says the Module 2 report of the inquiry “lays bare the catastrophic impact” of the national governments’ “lack of urgency and collective complacency”. Agreeing with Baroness Hallett’s view, the association says governments did “far too little, too late” in the first few weeks of the pandemic.
Tom Dolphin, chair of BMA council, said: “As doctors who were looking after the sickest patients, my colleagues and I will recognise the report's findings as a terrible indictment of the government’s almost incomprehensible failings and incompetence.
“The government told the country and NHS workers that the measures they were putting in place would stop the NHS becoming overwhelmed: the report says otherwise. It also talks of ‘misleading assurances from the Department of Health and Social Care that the UK was well prepared for a pandemic’. On the front line, doctors and nurses could see the tidal wave of sick patients coming our way as we scrambled to be ready, even while the then Prime Minister was talking about shaking hands with patients.”
The Module 2 report said the lockdowns in 2020 and 2021 “undoubtedly saved lives” but “only became inevitable because of the acts and omissions of the four governments” – none of which, it said, had adequately prepared for a lockdown or had a strategy for when or how they would exit lockdown.
The inquiry rejected criticism that governments were wrong to impose a mandatory lockdown on 23 March 2020, saying they each “received clear and compelling advice to do so” – adding that “without it, the growth in transmission would have led to an unacceptable loss of life. However, their failure to act promptly and effectively had put them in this position”.
The report said there was “a toxic and chaotic culture” at the centre of the UK Government during the pandemic.
It noted that politicians “did not take the pandemic seriously enough until it was too late”, describing February 2020 as a “lost month” where little action was taken despite “clear warning signs” such as the virus spreading to Italy.
There was no COBRA meeting chaired by the Prime Minister until 2 March 2020. Neither COBRA nor cabinet meetings were held in the February 2020 half-term holiday. q
clear, relevant and helpful. It will be the first significant updates since they were published in 2012.
Earlier this year results from the GMC’s annual national training survey revealed that more than one in five trainee doctors were hesitant about escalating concerns about patient care, and GMC chief executive Charlie Massey warned in a speech in September that maternity services were at risk from harmful cultures that put ‘cover-up over candour’ and ‘obfuscation over honesty’.
Professor Pushpinder Mangat, medical director and director of education and standards at the GMC, said: “Our guidance is there to provide support and confidence, as well as practical help, for people to speak up when necessary. But speaking up is no good in isolation. Leaders and managers have a duty to act when concerns are raised with them.
“Whenever we update guidance, it is important we hear views from a range of respondents. Their voices and real-life experiences will be instrumental in ensuring our guidance is clear, relevant and helpful, and reflects the needs of everyone it affects.”
The GMC’s consultation runs until midnight on 22 January. It is seeking input from doctors, PAs and AAs, patients, healthcare bodies and stakeholder organisations, as well as other individuals working in healthcare.
The two pieces of guidance are being reviewed together due to their close connections and because they share key issues the regulator wants to explore around positive workplace cultures, leadership and raising concerns without fear of negative consequences.
Following the consultation, the GMC expects to publish updated versions of the guidance during 2026. q
[IN 2001, when he was 31, ‘David’ was referred to Homerton University Hospital in Hackney, East London for what was thought to be a minor sebaceous cyst on his upper thigh. Sebaceous glands are microscopic glands in hair follicles that secrete oil to protect the skin. In 2002, the cyst was found to be a benign tumour with a risk of recurrence, and was removed. The hospital failed to arrange any follow-up appointments.
The lump returned in 2004 and David went for another removal. A further microscopic study found the tumour had not been fully removed, but records show that information was not shared with David or his GP. Over the next several years David repeatedly sought help from his GP as the lump reappeared and worsened. Between 2014 and 2018 he reported pain and bleeding, but those concerns were not acted upon.
In 2018 David was referred back to Homerton University Hospital. He was diagnosed with adnexal carcinoma, a rare and aggressive skin cancer. His treatment involved multiple surgeries, radiotherapy, the management of serious complications including pulmonary embolism, and a blood clot in his lungs. David says his recovery was slow and painful.
Following a relapse in 2022 he had further surgery, and a 2023 scan raised concerns about remaining cancer cells.
Now, aged 55, David lives with lymphoedema, a condition that causes swelling and limits his mobility. This has left him with chronic discomfort. As a self-employed technician, David’s ability to work has been severely impacted. The injuries have also taken a toll on his mental health.
David instructed Nandi Jordan, a partner in the medical negligence team at law firm Leigh Day, to investigate his case and was successful in his claim for damages. Homerton Healthcare NHS Foundation Trust admitted liability and agreed to pay a settlement of £575,000.
David said: “I am grateful that the case has finally been resolved and that justice has been served. Although no outcome can erase the hardship and emotional weight of what happened, I take comfort in knowing the truth has been acknowledged. My heartfelt thanks go to Nandi and her team for their strength, guidance and unwavering support throughout this difficult journey.”
Nandi Jordan added: “This was an awful case where there were basic and avoidable errors during treatment. Nothing can make right the impact on my client’s health, but I hope that the award of damages goes some way in restoring the financial losses he has suffered and providing financial security to my client in the future.” q
[ EVERY YEAR , children and young people across the UK die from sepsis, often in situations where it is treatable but is not recognised quickly enough in hospital settings, according to law firm Fieldfisher.
Despite clear warning signs, too many families are left grieving because of delays in diagnosis and treatment. In some cases antibiotics are not administered until it is far too late. These are not rare or isolated incidents; they are systemic failings, and they are costing lives.
Fieldfisher represent many families whose lives have been devastated by a failure to spot and treat signs of sepsis or meningococcal meningitis in time. Too often we hear how parents' concerns that something is seriously wrong with their child are dismissed by medical staff.
That is why the news that the NHS is trialling a new 15-minute blood test to rapidly detect lifethreatening infections in children is so important. The test has the potential to save lives by helping doctors distinguish between viral and bacterial infections in minutes, not hours.
The MeMed BV test is currently being trialled in three major children’s hospitals: Alder Hey Children’s NHS Foundation Trust, St Mary’s Hospital in London and the Great North Children’s Hospital in Newcastle. It works by analysing the body’s immune response to infection, providing a result in just 15 minutes.

Fieldfisher’s Deborah Nadel said: “I represented the family of Mia Ginever, a 19-year-old university student who died after being admitted to Frimley Park Hospital with suspected sepsis. Despite clear signs of deterioration, she was not given antibiotics for over eight hours. The coroner concluded that her death was avoidable and described the care she received as ‘lamentable’.
“At Fieldfisher, we continue to support families affected by delayed or inadequate medical care. We welcome this trial as a vital step toward improving patient safety and preventing avoidable deaths from sepsis.” q
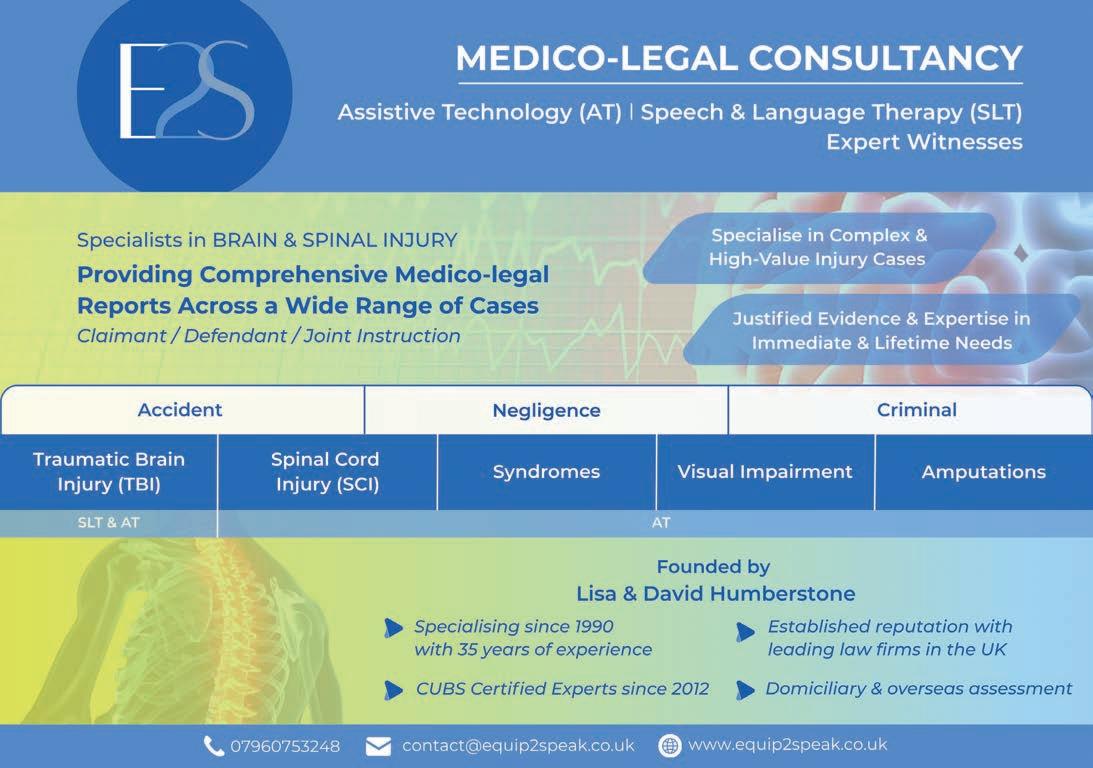

[ GP CONTRACT CHANGES that dictate how patients are able to contact their practice have negatively impacted patient care and practice staff, an extensive new survey of over 1,300 practices published by the BMA has revealed. More than one in five practices in England responded and over 1,300 unique practice responses were recorded. Of those, the majority (73%) had to change their ways of working due to the contract change.
On 1 October 2025, the government introduced changes to how patients contact their GP practice via online platforms. In what it says was an attempt to ‘end the 8am scramble’, the government imposed the requirement for all practices to provide continuous online, telephone and in-person access throughout core hours –8am to 6.30pm, Monday to Friday – without delivering the promised necessary safeguards to prevent urgent requests and queries being accidentally submitted online by patients.
GPs have confirmed in their survey responses that urgent and emergency requests have been submitted online, risking patient harm and staff stress/anxiety, which compounds the existing workforce pressures felt across GP practices in England.
Nearly half (42%) of practices have had to reduce face-to-face appointments: all reducing the time patients spend with their family doctor. Over half (55%) of those practices had seen a negative effect on patient care. Despite GPs warning of the risk of patient harm, 74% of the practices said they’d seen an increase in workload, 68% reported an increase in stress and 54% said there was an increase in working hours.
The general practitioner committee's (GPC England) current dispute with the government includes that issue, after it failed to meaningfully engage with GPC England to deliver the necessary safeguards prior to 1 October 2025, as per GPC England’s conditions to agreeing the terms of the 2025/26 contract.
GPC England has repeatedly said that patient access must be clinically safe. To ensure that happens, practices must retain the ability to manage their consultation systems safely, including when demand exceeds safe capacity, rather than being forced to prioritise convenience over patient need in a woefully underresourced environment.
Over half of practices implementing the change reported that there had been a negative effect on patient care, and 70% revealed that their practice had received requests that are medically inappropriate –mostly urgent requests coming through as routine/non-urgent, and an increase in requests that should not come to a GP practice at all.
Practices have been sharing their experiences with the BMA since the change came into effect on 1 October: urgent requests have been

coming through as routine or admin requests; patients deliberately bypass the triaging systems by marking an urgent query as nonurgent, and issues have specifically worsened because of the 1 October changes. GP services are now easier to contact than other services, increasing the volume of requests.
BMA GP committee chair Dr Katie Bramall said: “Government is right that GP is the front door to the NHS, but they are wrong in refusing to understand how it works. To have over 1,000 practices respond as quickly as they did shows the impact of how badly government have chosen to embed these changes, with six in 10 remaining extremely unsupportive, and two in 10 somewhat unsupportive. Over four in 10 are having to reduce the number of GP appointments they can offer to their patients so they can manage or triage online requests and queries instead. If government had chosen to listen to us and work with us, we could have made this so much more of a success.
“There is still ample opportunity for Wes Streeting to engage with us and help rebuild general practice, which would transform the NHS experience for the 1.5 million patients who use it every day The public want more GPs delivering more appointments to fix the NHS.
“We will continue to comply with the changes brought in on 1 October 2025 under protest, while exploring all options on how best to deliver transformative and safe change for general practice in England. Any action we take will be measured, informed and undertaken only to defend GP partnerships and the safe, GP-led community-based care patients and their families rely upon.” q
[
ENT UK, the professional membership body representing ear, nose and throat surgery and head, neck and thyroid surgery in the UK, has issued a statement condemning the recent decision made by South East England ICBs to suspend funding for septoplasty, turbinate surgery and functional septorhinoplasty.

The statement says: “We firmly believe that this decision will have a significantly detrimental impact on patients in numerous ways, including:
Harming patients : This policy threatens the wellbeing of individuals, in particular people who suffer from asthma or sleep disorders, who rely on these procedures for improved health and quality of life.
Increasing ENT waiting times : The suspension of funding will inevitably lead to longer waiting lists, exacerbating the distress and discomfort of those in need of timely treatment.
Contradicting evidence-based medicine : This decision stands in stark contrast to established medical research and practices, undermining the principles of effective healthcare delivery.”
Alongside co-signatories the British Rhinological Society, the Association of Otolaryngologists in Training, the British Society for Facial Plastic Surgery and the patient charities SmellTaste and Sinus UK, ENT UK has written to Health and Social Care Secretary Wes Streeting, asking for “immediate intervention from the Department of Health to reverse this policy for the sake of patients’ health and wellbeing, and we have offered to work with decision makers to
develop more effective solutions to the challenges they face while continuing to provide the best possible service to patients.”
They are urging all those affected by the decision to “raise their voices by contacting their local MP or Integrated Care Board”. q
[ THE PARENTS of a boy whose severe hearing loss went undetected by doctors for three-and-a-half years, despite repeated tests, say they fear hundreds of other children’s lives will have been ‘forever affected’ by failing testing centres.
Ronke Bain, associate chartered legal executive at Hudgell’s Solicitors, tells his story: “Tommie’s parents were repeatedly reassured by numerous specialists at Northern Lincolnshire and Goole NHS Foundation Trust that his hearing was fine from birth. Doctors maintained his lack of development was more likely a result of being born prematurely.
“Despite raising repeated concerns over Tommie’s hearing, his parents say specialists even told them not to worry as ‘boys are lazy’ and often take longer to develop compared with girls.
“The trust has now admitted that Tommie was born with hearing loss and was displaying ‘red flag’ signs which should have been picked up in testing. Despite that, it was not until his eighth hearing test, when he was three and a half, that Tommie was diagnosed as being profoundly deaf. Even then, he was not immediately fitted with cochlear implants. Instead, he was given hearing aids which fitted poorly and made little impact.
“Such was the level of failings, Tommie’s parents were advised to seek legal advice. They have now instructed our medical negligence specialists, who will help Tommie to access the continued therapy and support he needs.” q
[
REPRESENTATIVES from the Cabinet Office and the Infected Blood Compensation Authority were told directly that compensation payments were ‘taking too long’ at a special session for the infected blood community, at a Big Get-Together (BGT) conference on 22 November.
A panel including David Foley, interim chief executive of the Infected Blood Compensation Authority, and Ellie Nicolson, director of the Cabinet Office’s Public Inquiry Response Unit, faced questions from the BGT audience. Ms Nicolson said that there was unlikely to be a significant update until the current consultation on the government’s proposed changes to the compensation scheme ended on 22 January.
She said there would be a government response to the consultation within 12 weeks of it closing, with related legislation laid in Parliament before the summer recess.
Ms Nicholson was asked about emerging concerns that some compensation payments are liable for Inheritance Tax, despite government assurances that the payments are exempt from the tax. She said she was ‘aware of the strength of feeling’ around this issue. She also acknowledged criticism that compensation payments to affected people were ‘taking far too long’.
Also on the panel were Clive Smith, chair of the Infected Blood Memorial Committee, independent financial adviser Sam Richards and Victoria Miller, professional lead of the Infected Blood Psychological Service.
Clive Smith announced that a National Service of Remembrance will take place at St Paul’s Cathedral in London on 19 May 2026 for the infected blood community. He said the Infected Blood Inquiry’s memorial, which is a large rack of messages from loved ones contained

in medical specimen jars that was previously located at the inquiry, has found a new permanent home at the University of Manchester.
Ms Miller told BGT that 460 people had been in contact with IBPS since it was set up earlier this year. She urged people to use the service, which is open to those infected and affected in England. There is psychological support for people in Northern Ireland, Wales and Scotland which can be accessed through the infected blood support schemes.
Sam Richards outlined what financial guidance is available to people going through the compensation process and emphasised that, even if people have completed their claim, they can still access the free service. He said that temporarily high bank balances are covered by the Financial Services Compensation Scheme for up to six months and urged people not to rush into a decision without getting trusted, expert financial advice. q
[ THE UK National Screening Committee (UK NSC) is running a public consultation on prostate cancer screening. It is consulting on its 2025 review of updated evidence and a draft updated recommendation. The consultation runs for 12 weeks from 28 November.
As widely reported, the NSC’s draft recommendation is to offer a targeted national prostate cancer screening programme to men with confirmed BRCA1 or BRCA2 gene variants every two years from age 45 to age 61. It does not recommend population screening, targeted screening of black men or targeted screening of men with a family history of the disease.
The committee commissioned the Sheffield Centre for Health and Related Research (SCHARR) to develop the updated 2025 prostate cancer screening modelling study. The SCHARR report predicts the potential impact of various screening strategies, including population screening and targeted approaches aimed at high-risk groups including black men, men with a family history and men with a BRCA gene variation.

The response from cancer charities to the announcement has been mixed. Prostate Cancer UK said: “It’s a deeply disappointing decision. And it means prostate cancer remains the only major cancer without a mass screening programme in the UK.”
Its chief executive Laura Kerby added: “The committee’s decision will come as a blow to the tens of thousands of men, loved ones and families who’ve fought for a screening programme.”
Cancer Research UK was more positive in its response. It said: “We support this recommendation for men with BRCA mutations, who are more likely to develop aggressive prostate cancer than men without BRCA mutations, but there’s more to do before screening can be rolled out.”
The draft recommendation is also to collaborate with the TRANSFORM screening research trial team to answer outstanding questions on screening effectiveness for black men and men with a family history – as soon as trial data becomes available.
The TRANSFORM trial – the biggest prostate cancer screening study for 20 years – is being funded by Prostate Cancer UK and aims to provide definitive answers to the questions that remain, paving the way to a screening programme for every man.
Spearheaded by six of the world’s leading prostate cancer experts, TRANSFORM will test a number of screening options – including blood tests, fast MRI scans and genetic testing – to find the safest and most accurate method.
The charity continued: “Today, the committee has decided we don’t yet have enough evidence that the benefits of screening for all high-risk men would outweigh the possible harms of unnecessary biopsies and treatments. But it has recommended screening for a specific group of men who have a high risk of prostate cancer due to variations in their BRCA genes.
“This is an important step forward, which opens the door to the first prostate cancer screening of any kind in the UK and shows we’re moving in the right direction.” q
[ THE ROLE of the medico-legal expert witness is undergoing a significant and accelerating transformation. Once shaped largely by clinical reputation, a steady courtroom presence and the quiet authority of detailed written opinions, the profession is being redefined by technology, commercial pressures and heightened expectations from the legal sector. For clinicians working in medicolegal practice, the shift presents both valuable opportunities and some disruption.
Technology is the most visible driver of change. Remote hearings, widely adopted during the pandemic, have now become a standard feature in many jurisdictions. Virtual testimony, electronic bundles and real-time screen-shared imaging mean that medico-legal experts must be as skilled in digital presentation as they are in clinical reasoning.
Similarly, cases involving significant medical records, monitoring data, imaging archives and digital correspondence demand fluency in analysing large datasets. Experts who can translate complex clinical information into clear visual formats – timelines, risk stratification charts and imaging interpretation summaries – are increasingly valued by legal teams.
Artificial intelligence and machine-assisted analysis are also reshaping the evidential landscape. AI tools are now used to scan vast volumes of clinical documentation, highlight anomalies in medical imaging and model treatment scenarios. However, their use raises questions of transparency, bias and scientific validity.
An expert who draws on computer-assisted findings must be prepared to explain model selection, data limitations and the methodology underpinning the conclusions. Courts are rightly cautious of ‘black box’ outputs; and credibility increasingly depends on a demonstrable chain of reasoning rather than the technology employed.
Newer clinicians with strong technical and analytical capability are entering medico-legal practice earlier in their careers. This has altered how medico-legal teams are composed: senior consultants provide strategic opinion and courtroom presence, while junior specialists support with evidence synthesis, literature analysis and digital modelling.
Regulatory and professional bodies have tightened guidance around conflicts of interest, funding arrangements and independence. The court expects full transparency regarding the basis of an opinion: what evidence was relied upon, what assumptions were made and where uncertainty remains. Detailed records, traceable methodologies and careful drafting of joint statements are no longer simply good practice – they are essential to admissibility and expert integrity.
The expectations of instructing solicitors have also changed. Cost pressures, budgeting requirements and the need for efficient case preparation mean experts are increasingly asked to provide targeted

reports. Collaborative workflows – for example, clinicians working alongside statisticians, radiologists or human factors specialists –allow for depth without unnecessary duplication.
The adversarial nature of medico-legal proceedings has likewise evolved. Cross-examination is more rigorous, with particular scrutiny on methodology rather than purely clinical judgement. Experts are expected to communicate complex medical concepts in plain language, supported by robust evidence.
Regulation and accreditation are becoming more structured. Courses in expert witness practice, medico-legal report writing, courtroom skills and ethical duties are now widely available, and formal expert panels or court-approved lists are growing in significance. In many jurisdictions, credibility is no longer based solely on clinical reputation, but on recognised competence in medico-legal practice itself.
For practitioners, the message is one of adaptation and professional evolution. The most effective medico-legal experts will combine deep clinical experience with digital fluency, rigorous methodology and a transparent approach to opinion formation. For instructing lawyers, the challenge is to leverage these evolving skills while safeguarding fairness, impartiality and the integrity of the judicial process.
The medico-legal expert witness profession is now richer in tools, talent and analytical capability than ever before – but also more exacting. Those who embrace innovation, invest in their medicolegal skills and maintain absolute independence will not only thrive in this changing landscape, but will help define the future standards of clinical evidence in the twenty-first-century courtroom. q

[THE Royal College of Obstetricians and Gynaecologists (RCOG) has welcomed the publication of an independent report by the expert group established to review Scotland’s abortion law. The Abortion Law Expert Group was commissioned as part of the Scottish Government’s 2023–24 Programme for Government to undertake an independent review of the current law and to consider how abortion can be regulated as a safe, modern healthcare service for women.
In response to the report, RCOG President Professor Ranee Thakar said: “We welcome this report – the proposed changes in Scotland represent an important step towards ensuring that women can access abortion care safely, confidentially and without fear of investigation or prosecution.
“These recommendations also reflect a positive trend across all four nations of the UK towards treating abortion as essential healthcare rather than a criminal issue. In England and Wales, MPs have already sent a clear message by voting to remove women from the criminal law – reflecting public opinion that reproductive rights matter. We now urge Peers in the House of Lords to follow suit and back this vital amendment to see abortion decriminalised.
“Abortion is healthcare that around one in three women will need in their lifetime, and it should be regulated and delivered to the same professional standards as any other medical procedure, not through the criminal law.” q
[ THE Royal College of Midwives (RCM) has reiterated its calls for more investment in the education of the next generation of midwives and those working in the university sector. The call came in response to a Sunday Times investigation into midwifery education.
The RCM said the Sunday Times’ findings reflect long-standing issues it has raised repeatedly about inadequate investment in midwifery education and the educators themselves. Those educators are being let down by the increased student numbers, against a backdrop of falling lecturer numbers and a lack of access to postgraduate education opportunities.
It also identifies weaknesses in the Nursing and Midwifery Council (NMC), which has responsibility for both the setting of the undergraduate curriculum and regulatory oversight of universities delivering those programmes.
Gill Walton, chief executive of the RCM, said: “Midwifery students should be supported by a system that prepares them for the realities of modern maternity care. Right now weak and inconsistent oversight from the NMC is failing midwifery education – for those who are delivering it, for students and for women and families.

“The NMC’s fundamental duty is to protect the public through regulation of midwifery education and practice. We are increasingly concerned that they are not fulfilling this duty adequately.”
The college said that the NMC has failed to keep pace with the increased demands on, and expectations of, midwives, including understanding complexities, mental health awareness and assessment, and vital skills and competencies such as supporting home and water births. Those are essential to the safe delivery of maternity care, and midwives should be competent to deliver that care.
Gill Walton added: “The needs of the women and families in our care must always be the priority. Our expectation
is that universities support midwives to advocate for women and support them to make informed choices based on evidence. Midwifery education must focus on personalised and safe care for each woman, whatever her choices, from day one of registration.”
The RCM’s own research has shown that midwifery departments are facing cuts, shrinking teams and fewer experienced educators at a time when women’s health needs are becoming more complex.
“We have some of the most robust midwifery education standards in the world,” added Gill Walton. “But standards alone are not enough, particularly if they are not being regularly assessed by the regulator. We need investment in the education workforce and in the seniority, skill and experience of the educators who train future midwives.”
The RCM said it supports Health and Social Care Secretary Wes Streeting’s call for an overhaul of regulators, including the NMC, to ensure training keeps pace with modern maternity care.
“This is a moment for the NMC to show it can provide dependable, transparent and consistent regulation.” said Gill Walton.
“Educators, students, midwives and families need a regulatory system they can trust.” q

By Edwin Chandraharan
[THE BOLAM TEST is widely used in clinical negligence cases to determine the standard of care provided by individual healthcare professionals for their patients in the United Kingdom. This legal test is based on the principle that the healthcare professional is not deemed guilty of medical malpractice or clinical negligence if they have acted in accordance with clinical practice accepted as proper by a responsible body of medical professionals within their field of practice.
The Bolam Test was introduced into the civil justice system to recognise the fact that there is a wide variation in individual patient circumstances and the clinical context, and therefore healthcare providers cannot be expected to provide the same care or treatment for every patient. It was designed to allow for the variation in clinical practice, provided such practice which may be seen as deviation from the expected standard of care is accepted by a responsible body of healthcare practitioners within the same field of practice as ‘proper’.
However, it is important to appreciate that the ‘responsible body’ referred to in the Bolam Test must be ‘reasonable and logical’, which is crucial to ensure justice for patients who have been harmed in the UK healthcare system, as well as to the clinicians providing care. Fortunately, most clinical specialties in the UK follow evidence-based clinical guidelines, and clinical care based on logic and basic scientific principles.
However, in UK maternity services, except for antenatal care and the fetal medicine service which are based on sound scientific principles and evidence-based clinical care, guidelines on intrapartum care are often riddled with historical (mal)practices which are not based on scientific evidence and often contrary to the basic scientific principles taught in medical schools.
Repetitive Each Baby Counts reports published by the Royal College of Obstetricians & Gynaecologists (RCOG) have highlighted substandard care contributing to more than 70% of intrapartum-related severe hypoxic-ischaemic encephalopathy (HIE) leading to cerebral palsy and perinatal deaths, and misinterpretation of cardiotocographs (CTG) contributing to approximately 50% of those poor perinatal outcomes.
In addition, confidential enquiries into maternal deaths in the UK have highlighted a near doubling of deaths due to postpartum haemorrhage in the UK – the vast majority due to placenta accreta spectrum (PAS): a serious complication of previous caesarean sections, and more recently there were concerns regarding birth trauma.
Maternal and perinatal outcomes in the UK have been found to be among the worst compared to our European peers. Although the competencies of frontline midwives and obstetricians, as well as ‘lack of funding’, are often blamed for these unacceptable

poor outcomes, it is important to appreciate the role played by unscientific and illogical national guidelines in causing these poor maternal and perinatal outcomes.
Therefore, it is vital to understand the root causes of poor maternal and perinatal outcomes in the UK and to ask the question: “Is the continued use of the Bolam Test in the UK to determine the standard of care fair and justifiable, if the ‘responsible’ body of medical opinion (ie the national guidelines) which are used both by the defence and the prosecution in clinical negligence cases are not based on robust scientific evidence, and do not withstand logical scrutiny?”
Cardiotocograph misinterpretation: the role of illogical and unscientific national recommendations
The National Institute of Health and Care Excellence (NICE) guideline on CTG interpretation erroneously increased the upper limit of the baseline fetal heart rate (FHR) to define abnormal FHR to 180 bpm for UK fetuses, based purely on the personal opinions of the guideline development group, as stated within the guideline. That was contrary to scientific evidence and all recognised international guidelines.
That potentially very dangerous error resulted in fetuses who are unable to mount sufficient compensatory responses to hypoxic stress, such as fetal growth restriction, chorioamnionitis and chronic hypoxia, being misclassified as ‘normal or suspicious’ in the UK. Similarly, the UK guideline defined baseline FHR variability of more than 5 bpm as normal, instead of the internationally accepted 5-25 bpm, leading to fetuses with excessive variability (greater than 25 bpm or the ‘ZigZag Pattern’) due to rapidly evolving hypoxic stress being misclassified as ‘normal’ – increasing the risk of poor outcomes. In the UK, unlike other European countries, CTG guideline ‘stickers’ were printed with exactly the same parameters and were used in every fetus, stipulating the same time limit to become suspicious or pathological irrespective of their individual reserves.
The UK guideline also illogically and erroneously recommended administration of oral or intravenous fluids to the wrong person (the mother) to treat CTG abnormalities, despite the reported risks of maternal fluid overload and neonatal convulsions in a report from NHS Resolution. Similarly, the UK guideline recommended that the skin of the fetal scalp be sampled because it was illogically thought to be close to the fetal brain, increasing the risks of emergency caesarean sections and poor perinatal outcomes in fetuses with chorioamnionitis.
Although fetal scalp blood sampling (FBS) was discontinued in the USA approximately 30 years ago, it continued to be
recommended in the UK despite scientific publications highlighting the potential dangers to both mothers and their fetuses. These illogical and potentially dangerous historical, unscientific obstetric practices, which were repetitively promoted by UK national guidelines from 2001, were only stopped in 2022.
FHR decelerations which were physiological fetal responses to hypoxic stress were erroneously classified as ‘pathological’ after 30 minutes, leading to an increase in unnecessary caesarean sections and their resultant complications – including maternal and fetal trauma due to an impacted fetal head. Moreover, illogically the guideline on operative vaginal births recommended a maximum three pulls in the UK, leading to the likelihood of excessive force in an attempt to complete the procedure ‘within three pulls’. That may lead to an increased likelihood of perineal trauma and fetal trauma, as well as second stage caesarean sections and the resultant complications such as postpartum haemorrhage and maternal and fetal trauma. That erroneous guideline was only rectified in 2020, which increased the number of pulls to six.
However, even this recommendation of ‘six pulls’ was illogical because the number of pulls would depend on the station of the presenting part, position, rotation and the degree of deflection of the fetal head, as well as the resistance offered by the birth passage. If there was no evidence of any progress within the first two pulls, then the procedure must be abandoned, instead of pulling six times. Conversely, if there is evidence of progress (ie flexion, rotation or descent) with each pull, then ‘gentle pulls’ should be continued until birth is achieved, instead of stopping after six pulls, because performing an emergency caesarean section may increase the likelihood of maternal and fetal trauma.
The role of a national guideline in increasing the risk of emergency caesarean section rates
Fetal heart rate decelerations are physiological fetal compensatory responses to protect the myocardial workload in response to repetitive and intermittent umbilical cord compression or interruption of placental blood supply by on-going uterine contractions. They are similar to increases in the rate and depth of respiration observed in adults undertaking physical exercise. FHR decelerations do not need any intervention if there is evidence of good central organ oxygenation on the CTG trace.
It has been well known from 1996 that classification of CTG traces into ‘suspicious and pathological’ based on the observed morphology of decelerations has a false positive of more than 90%. However, despite the knowledge that approximately 90% of emergency caesarean sections would be potentially unnecessary, the UK CTG guidelines from 2001 classified CTG traces as ‘pathological’, based on the observed morphology of decelerations – despite scientific evidence from 1996.
That erroneous approach very likely contributed to an exponential increase in the rate of emergency caesarean sections and resultant complications, such as postpartum haemorrhage, wound infections, placental accreta spectrum and uterine ruptures. Despite FBS not being performed in the USA, the UK guidelines erroneously recommended FBS to reduce the caesarean section rates when a pathological CTG trace was encountered. That was against medical school teaching, which forbids taking a sample from the skin of the scalp to determine the oxygenation of the brain as the blood supply to the skin is different to that to the brain.
As expected, FBS was shown to increase the rates of emergency caesarean section rates from 2015, but NICE CTG guidelines did not only not stop their recommendation to perform FBS until 2022, they unfairly advised frontline clinicians to ‘advise women that FBS would reduce further interventions’, despite concluding in the same guideline that, based on scientific evidence, FBS increased the rate of emergency caesarean sections and instrumental vaginal births. Therefore, women were provided with this incorrect
information which may have potentially invalidated their informed consent for FBS.
In conclusion, the errors outlined above by the national CTG guidelines in the UK have probably contributed to significant harm to both mothers and babies. That is evidenced by the fact that hospitals that have stopped NICE CTG guideline have shown demonstrable improvements in perinatal outcomes. The continuation of the error-producing NICE CTG guideline, and the resultant avoidable harm to mothers and babies, has necessitated the first-ever national maternal enquiry, and significant financial burden to the UK taxpayer from medico-legal claims against the maternity service.
Therefore, the key question for the legal profession is this: should the error-producing national guidelines in the UK be continued to be considered as the basis of the Bolam Test to determine the standard of clinical care in our maternity service?
That is because the cardinal principle of the Bolam Test is that the ‘responsible body’ must be ‘reasonable and logical’ to deliver justice to our patients as well as to our frontline healthcare providers. Any guideline that is not based on basic scientific principles and contemporary scientific evidence is unlikely to fulfil the criteria for being considered as ‘reasonable or logical’. q

Edwin Chandraharan has worked as a consultant obstetrician and gynaecologist, and was the lead consultant for the labour ward with special interests in FHR monitoring, massive PPH, placenta accreta, operative vaginal births and acute gynaecology and early pregnancy scanning at a large teaching hospital in London for 15 years. He holds the Bond Solon Cardiff University Expert Witness Certificate and has appeared as an obstetric expert witness in the Coroner’s, Magistrate’s and the High Court.
Contact Mr Chandraharan on 07824 338 787 or via email at edwin.c@sky.com .

By Lorin Lakasing,
author of ‘Delivering the truth: Why NHS maternity care is broken and how we can fix it together’
[ IN JUNE 2025, Health Secretary Wes Streeting announced a rapid inquiry into NHS maternity services, with preliminary findings due in December. It’s the latest in a series of investigations stretching back twenty-two years.
In my book, Delivering the Truth, I argue that the inquiries themselves have become part of the problem. Not through malice or incompetence, but through a fundamental misunderstanding of what’s actually wrong with maternity services.
The recommendations they produce make perfect sense in theory. More training. Better protocols. Enhanced oversight. Increased transparency. However, on the ground, these translate into more boxes to tick, more time away from patients, more fear of getting something wrong. Each layer of bureaucracy added to ‘improve’ care actually makes providing good care harder.
The carrot and stick problem

The way these recommendations get implemented reveals another fundamental misunderstanding and a perverse dynamic.
Managers become experts at chasing carrots, developing vast teams devoted to meeting targets and improving ratings. Meanwhile, clinicians become adept at dodging sticks, following protocols defensively rather than using clinical judgement while avoiding difficult conversations that might lead to complaints.
Actual patient outcomes become almost incidental. A unit can tick every box, meet every target, achieve an ‘Outstanding’ rating, yet have clinical outcomes no better that another rated ‘Inadequate’. Conversely, a unit providing excellent clinical care might be rated ‘Inadequate’ because they prioritised patients over paperwork.
National inquiries, by their nature, seek national solutions. But maternity services face vastly different challenges depending on location, demographics and resources. What works in rural Gloucestershire won't necessarily work in inner London, yet inquiries produce one-size-fits-all recommendations.
When Streeting selected underperforming units for special attention in his rapid inquiry, it was widely reported that many served deprived areas. The assumption was that these units are failing due to poor practice rather than considering what deprivation truly means for maternity services. These units might actually be performing miracles given their starting point, but that nuance is invisible when you’re only looking at standardised outcomes.
The transparency paradox
Prompted by patient complaints about concealment and collusion, most recent inquiries have emphasised ‘transparency’ and ‘openness’. The idea is compelling: if we’re honest about problems, we can address them. If we involve patients more, we’ll build trust. In practice, this well-intentioned approach has created new problems.
A recurring theme across NHS trusts is senior managers placing reputational damage limitation ahead of patient and staff safety. The pressure for transparency, paradoxically, incentivises hiding or whitewashing problems until they become undeniable crises. Staff learn quickly that raising concerns brings scrutiny, blame, and career consequences. Rather than building trust with patients, quite the reverse happens.
Patients arrive hypervigilant, looking for fault, expecting to be let down and all too ready to seek information from alternative online groups. Staff cannot provide confident reassurance without fear of reprisals or accusations of failing to listen to patients. Ultimately, these factors combine to create an environment where clinicians are squeezed into impossible situations and end up in either adversarial relationships with patients or disengaging with them. No one wins.
The solutions aren’t rocket-science. Whilst the patient voice is clearly important, it is frontline staff who know what would improve care. But they’re rarely asked, and when they are, their answers don’t fit the inquiry framework.
First, we need clinicians, practising professionals who understand current realities, involved in designing and implementing solutions.
Second, we must reform the incentive structure completely. We need to reward clinical excellence, staff retention, and team stability rather than tick-box compliance.
Third, recognise that different areas need different solutions. Stop pretending universal protocols solve local problems.
Fourth, NHS maternity units already track comprehensive metrics through various software systems. We should use this wealth of data to understand performance holistically. Trust that clinicians want the best outcomes for patients – they don't need carrots and sticks, they need respect, appropriate resources, and pay that recognises their expertise and incentivises continuation in clinical work.
Fifth, address why clinical work is undervalued. When moving into management or investigation work pays significantly more than delivering babies, we’re telling our best clinicians their expertise is worth less than bureaucracy.
Sixth, create psychological safety for staff. Staff need to know they can raise concerns without destroying their careers, make clinical judgements without defensive documentation, and learn from mistakes without punishment.
Without fundamental changes in approach, this current inquiry will likely produce similar recommendations to its predecessors. More transparency. More patient involvement. More oversight. More protocols. More training. More targets. The cycle will continue.
However, if this inquiry did something revolutionary – genuinely listened to frontline staff, recognised local contexts, addressed perverse incentives, valued clinical work appropriately, it could begin real change. q
• Dr Lorin Lakasing is an NHS consultant in obstetrics and fetal medicine. She draws on her 30 years of clinical experience in maternity care to give an insider’s view of the current worrying situation and its development, and suggests how we might move towards the safe, effective NHS maternity service that everyone deserves.
Her latest book, ‘Delivering the truth: Why NHS maternity care is broken and how we can fix it together’ is about the stories behind the headlines, revealing the reasons why major stakeholders in this vital service have inadvertently been encouraged to pursue different agendas, and how that has made effective, collaborative working towards optimal clinical outcomes almost impossible.
Web: lorinlakasing.com or Amazon: amzn.eu/d/g1dX9rh
By Philip Coleridge Smith DM MA BCh FRCS, Consultant Vascular Surgeon, Medical Director of the
[ VARICOSE VEIN SURGERY was the traditional way of removing varicose veins. Treatment was performed under general anaesthesia and led to significant post-operative pain and a recovery period of about one month. The long-term outcome of treatment was satisfactory.
In the last 20 years minimally invasive treatments under local anaesthetic have been introduced. These include thermal ablation methods where a tube is passed along the diseased vein for a distance of 20-50cm. The tube is used to contain a heating method which may be a laser fibreoptic or an electrically heated catheter. The vein is anaesthetised by injecting local anaesthetic around the vein and heat is applied to destroy it without removing the vein.
An improved method of injecting varicose veins known as ‘ultrasound-guided foam sclerotherapy’ has been popularised. In this method, injections of foam created from a sclerosant drug are made into the diseased saphenous veins and associated varices under ultrasound guidance. Local anaesthesia is not required for this treatment except at the site of injection.
Surgery

In general, the frequency of adverse events arising from modern treatments are substantially reduced compared to those which were caused by surgical techniques. Since large incisions in the leg are usually avoided, wound healing problems are minimised but a number of additional problems may arise.
Thermal injuries : The veins on the surface of the leg may lie close to the skin and to cutaneous nerves. Both of these structures may be damaged by heating the adjacent vein leading to undesirable outcomes. One of the methods used to abolish pain during treatment is to inject a large volume of dilute local anaesthetic around the varicose vein. This allows the vein to be heated painlessly if the anaesthetic is injected correctly under ultrasound guidance. The anaesthetic fluid thermally insulates the surrounding tissues from the heat applied to the vein and affords protection against skin burns.
Care must be taken to separate the skin and the nearby vein. Failure to observe good practice may lead to a linear burn in the leg 10 or 20cm in length. I have advised in a case where such a burn arose necessitating excision of affected skin, leaving a long scar in the leg. The claimant settled a claim against the surgeon following my advice.
Sensory nerves lie close to the saphenous veins, especially below the knee in the calf. Inadvertent heating of a sensory nerve may lead to loss of sensation in the affected region of the leg but may also produce long-lasting neuropathic pain. The nerve regenerates to some extent but then causes pain or unpleasant sensations in the innervated region that are very troublesome.
The medical literature on this complication is very limited but patients should be made aware that heating treatments for varicose vein may lead to loss of nerve function or neuropathic pain. Failure to warn of this complication could comprise substandard management.
I have also advised in a case where thermal treatment of a varicose vein on the back of the calf led to injury to components of the sciatic nerve. This is an unusual injury although a few published case reports
show that damage to motor nerves may occur following treatment of the varicose veins in this region. These veins pass up the back of the calf and join the main vein in the leg at the back of the knee, lying immediately next to the sciatic nerve. Under normal circumstances, the heating catheter is positioned under ultrasound guidance so that it lies about 2cm from the main vein and sciatic nerve.
Local anaesthetic is then infiltrated around the vein to insulate the heated region from the sciatic nerve and its branches. Damage to the nerve is very unlikely unless the heating catheter has been positioned incorrectly arising from incorrect interpretation of ultrasound images. In general, where motor nerve injury arises from varicose vein treatment it is likely to give rise to litigation which will be difficulty to defend.
Problems with phlebectomies : Thermal methods of treatment only destroy the main longitudinal veins on the surface of the leg, whereas the varicose veins usually arise in tributaries of these veins. Additional treatment can be provided by sclerotherapy or foam sclerotherapy (injection treatments for varicose veins) in order to destroy the varicose veins themselves.
Some surgeons like to use phlebectomy to treat residual varicose veins after thermal ablation. This treatment involves making a small incision in the skin and using a vein hook to pull out the troublesome veins. Wound healing problems are uncommon since the incisions are small but damage may also arise to nerves and lymphatic vessels lying close to the veins. Reported rates of damage to cutaneous nerves after this treatment range from 5-30% in published medical literature.
I have advised in one case where a long section of cutaneous nerve was removed at the ankle, leading to a large area of loss of sensation on the top of the foot combined with neuropathic pain in the leg. In a further case, damage to lymphatic vessels arose in the calf leading to the accumulation of lymphatic fluid in a cyst. This reached about 5cm in diameter at one stage, much to the dismay of the patient. The cyst was successfully managed by ultrasoundguided sclerotherapy.
The use of phlebectomies is still regarded as acceptable medical
practice despite the alternative of sclerotherapy being just as effective and much less likely to lead to nerve injury. Patients should be made aware of the possible complications of phlebectomy as part of the consent process. Failure to complete this step may comprise substandard medical practice.
Foam sclerotherapy : The modern vein treatment of ultrasoundguided foam sclerotherapy in which the main surface vein is injected with a sclerosant foam that immediately destroys the vein has become standard practice. This is a very effective treatment in skilled hands and requires no surgical incision. The main structure which should be avoided in such treatment is any artery in the leg. Ultrasound imaging is used to guide the injections and vascular surgeons should be able to identify and avoid the arteries. Inadvertent intra-arterial injection can cause severe damage to the skin and subcutaneous tissues.
I have advised in one case where a major artery at the ankle was injected, leading to a below-knee amputation. The defendants admitted liability having reviewed my report. Lesser damage may be done to skin by injecting excessively strong solutions or excessive volumes. The consent process should include mention of these potential problems which only occur on rare occasions.
In the UK there has been a change in practice towards minimally invasive methods of treatment for varicose veins as advocated by NICE. Data from the NHS Hospital Episode Statistics show that minimally invasive treatments have almost completely replaced varicose vein surgery. These treatments lead to more rapid recovery with equivalent efficacy to surgical treatment
The complications seen following surgical treatments are usually avoided, but a new selection of adverse events may arise. Surgeons undertaking the newer treatments should be aware of the potential post-operative problems and discuss these with their patients. q


By Professor Upendra Chowdhary, Emeritus Professor of Neurosurgery and presently medicolegal neurosurgical expert witness
[THE DEFINITION and an accurate clinical diagnosis of persistent vegetative state (PVS) remains difficult and controversial. There are further problems with several alternative names given to the state. The rate of misdiagnosis has been 37-43% on a long-term basis. The foundation of an accurate diagnosis is still careful, repeated clinical examinations.
There has been research going on to find out whether a sophisticated protocol of MRI scanning, such as functional MRI and/or a special protocol of prolonged EEG recording, will increase the accuracy of the diagnosis.

The short and long-term prognosis of severe damage to the brain, where the patient survives, is at its worst a state of coma, where there is no response even to pain, to almost complete recovery of consciousness. The state above coma is persistent vegetative state, where the patient has a sleep-wake cycle with intermittent spontaneous opening of the eyes, but has no awareness of self, surrounding or environment and no reproducible, purposeful or voluntary sensory or motor response.
The next best state is minimally conscious state, in which the patient has visual fixation, ocular pursuit movements and an occasional ability to follow simple commands.
There are two main aetiologies for PVS: severe traumatic brain injury and severe hypoxic/anoxic episode. Such patients initially undergo intensive treatment. Those who survive and regain spontaneous respiration have variable recovery, with some falling into PVS. The dilemma at this stage is when a physician should diagnose that patient to have developed PVS.
The prognosis of such patients will vary according to time-line, age and aetiology. Those with severe head and brain injury have a better prognosis than the hypoxic group. The younger the patient is, the better is the prognosis. The recommended criteria about the time-span when the diagnosis of PVS should be made is minimum of three months of the PVS persisting. But a certain percentage of patients with PVS diagnosed at that time-line – and even a small percentage of patients in PVS for 12 months –show improvement to minimally conscious state or even better awareness.
It is likely, according to some studies, that up to 24% of patients who were diagnosed as being in PVS for six months have recovered at least to minimally conscious state.
There are various ethical dilemmas in the long-term management of patients with PVS. They include practical aspects of clinical management which require a great amount of nursing and ancillary support. A particular society’s perceived norms and tradition, as well as religious beliefs, will also have an impact.
It is difficult to answer whether all forms of management, including that of hydration and nutrition, must be maintained while the patient is alive but has no voluntary response and no awareness. Such questions have been debated at the highest level in society, politics and in religious spheres and even gone into judicial reviews.
From a medicolegal point of view, we should concentrate upon the question of when should the diagnosis of PVS be accepted by both
parties in a litigation; and what will be the decision in the case of a particular patient in PVS regarding whether to continue full supportive management, which is very time consuming, costly and must be continued till the patient dies. Such decisions will be influenced by the patient’s closest relatives, their outlook about sanctity of life, their religious beliefs, the societal outlook and the physician’s opinion. It ultimately may have to be decided in a court of law, as has happened in the United Kingdom in quite a few cases.
The other medicolegal question in such a case is the effect on longevity. Patients with PVS would have a shortened life-span as they are prone to repeated chest infection, urinary infection, pressure sore problems and problems with nutrition. How much reduction in life-span will happen in a particular patient will have to be determined by a medical expert in that speciality. q
[WHEN SOMEONE sustains an acquired brain injury, develops cognitive impairment or experiences post-traumatic stress following trauma, the consequences can extend far beyond what is visible on imaging.
Memory loss, difficulties with attention and executive function, emotional dysregulation and a reduced ability to manage daily tasks can profoundly affect an individual’s independence, employability and quality of life.
In litigation, these often invisible impairments can be central to claims for compensation; yet assessing and communicating them requires highly specialised expertise. That is where neuropsychologists, in collaboration with occupational therapists, play a crucial role.
Occupational therapists (OTs) are integral in evaluating the practical implications of cognitive and psychological deficits identified by neuropsychologists. While neuropsychologists assess cognitive domains such as memory, attention, problem-solving and emotional regulation through structured testing. OTs translate those findings into an understanding of how the deficits manifest in everyday life. They consider a patient’s ability to manage self-care, household tasks, work responsibilities and social interactions. Together, neuropsychologists and occupational therapists provide courts, solicitors and insurers with a comprehensive picture of the individual’s functional limitations and needs.
The assessment process begins with detailed neuropsychological testing, including interviews, review of medical records and standardised cognitive assessments.
Neuropsychologists evaluate the extent of cognitive and emotional impairment, distinguishing between pre-existing conditions, situational stressors and the direct impact of injury. Occupational therapists then apply this insight to assess functional capacity in realworld contexts, observing how cognitive and psychological challenges affect daily routines, work performance and social engagement. This collaboration ensures that litigation assessments are both clinically rigorous

and practically meaningful.
In cases involving traumatic brain injury (TBI), stroke or post-traumatic stress, the combination of neuropsychological evaluation and occupational therapy insight can be decisive. A client may present with subtle memory deficits or difficulty planning multi-step tasks that significantly impair their ability to return to work.
While these issues might not be immediately apparent in standard medical assessments, the OT can demonstrate through structured functional testing and real-life observation how these deficits affect independent living, vocational performance and social participation. Such information is critical for courts to understand the full impact of the injury and to determine appropriate compensation.
Neuropsychologists provide objective evaluation of cognitive capacity, while occupational therapists can assess whether an individual is able to understand, retain and act upon information in everyday contexts.
For instance, in cases of mild TBI where cognitive deficits are subtle, OTs can show how memory lapses or impaired concentration interfere with the patient’s ability to manage finances, adhere to medication schedules or follow work protocols. That evidence bridges

the gap between cognitive assessment scores and real-world functioning, providing clarity for legal proceedings.
Expert testimony is a key element of litigation. Neuropsychologists prepare detailed reports outlining cognitive deficits, prognosis and the likely trajectory of recovery, while OTs provide evidence of functional limitations, rehabilitation needs and the practical impact of injuries on daily life. Together, their reports present a coherent picture of the claimant’s abilities and challenges. In court, their testimony reflects not only the medical facts but also the lived experience of injury, clarifying the degree of impairment and the support required.
Real-world examples illustrate the value of this collaborative approach. Consider a client who sustains a moderate TBI in a workplace accident. Neuropsychological assessment can reveal deficits in attention and executive function, while occupational therapy evaluation will demonstrate difficulties in planning and completing tasks. The combined evidence can directly influence the outcome of the compensation awarded.
The growing complexity of litigation involving brain injury and psychological trauma has led the courts to increasingly value the joint insights of neuropsychologists and occupational therapists. This collaboration ensures that compensation claims reflect the true impact of injury, encompassing both the invisible cognitive effects and their practical implications for everyday life.
In cases where the consequences of brain injury are not immediately visible, that combined expertise illuminates the full scope of impairment. By bridging clinical assessment and functional analysis, they provide the courts with evidence that is both scientifically rigorous and practically meaningful.
Their work ensures that legal outcomes are informed, fair and based on a comprehensive understanding of how injuries affect both cognition and daily living, reinforcing the indispensable role of specialist assessment in modern litigation. q


[ON 6 NOVEMBER the independent ADHD Taskforce published its final report, which aims to address challenges in ADHD care. Part Two of the report looks at ways of implementing the recommendations made in Part One, which was published in June.
That part of the report highlighted that ADHD is associated with higher risks of educational failure, not being in education, employment or training, long-term unemployment, welfare costs, early entry into the criminal justice system, family breakdown, chronic mental health problems, self-harm, suicide, substance misuse, obesity, physical illhealth and premature mortality.
Responding to the final report, Dr Ulrich Müller-Sedgwick, ADHD Champion at the Royal College of Psychiatrists, said: “There has been a profound increase in the number of people with ADHD struggling to access an accurate diagnosis and treatment in recent years. This often has serious consequences for their health, education, ability to work and wider society.
“While the report outlines challenges facing the whole of the UK, current models for delivering services differ across each nation, and therefore must be addressed through specific provisions in Scotland,
[NEW GOVERNMENT-BACKED RESEARCH could help identify children with special educational needs sooner. The Special Educational Needs in the Accelerator Programme will trial the creation of new AI tools which could result in earlier intervention and improved support for pupils.
Responding to the news, Dr Helena Bunn, the chair of the British Psychological Society’s Division of Education and Child Psychology, said: “The government’s renewed focus on early intervention and prevention for children with possible special educational needs is welcome news. It is vital that children who require SEND support have their needs identified in a timely manner. This has the potential to trigger early support, which is key to preventing problems becoming entrenched.
“Although AI can help to an extent, it is also important to acknowledge that its capabilities should continue to be treated as assisting the identification of SEND needs and supporting decision making. AI cannot, and will not, solve all the issues which currently face the SEND system, most obviously in provision, where significant gaps are widely acknowledged.
“This trial needs to explore, and acknowledge, both the capabilities and the limitations of using AI in a complex system such as SEND. It must not, however, be perceived as a ‘quick fix’ to the current financial and staffing pressures via the promotion of AI-led apps as a direct replacement of current operations within SEND.
“It is imperative that such initiatives involve important stakeholders in their development, including schools, parents and parent groups. Most essentially of all, it must include professionals involved in current delivery, most notably educational psychologists.
“Given that it is widely acknowledged that the SEND system is unsustainable in its current form, these initiatives must form part of a wider long-term strategy from government, fundamentally based on human-led identification. The government must urgently produce a new and costed plan, which should include the appropriate use of AI apps and programmes as a tool used by professionals, in the identification of SEND requirements. Careful and targeted investment is needed to ensure that the educational psychology profession continues to grow to meet ever-increasing demand.” q
Wales, Northern Ireland and the Crown Dependencies (Jersey, Isle of Man and Guernsey). The Royal College of Psychiatrists in Scotland is currently working with Scottish policymakers on a 10-point plan for change in its new report: Multi-system solutions for meeting the needs of autistic people and people with ADHD in Scotland
“Priority must be given to addressing the shameful waiting lists that leave many people without vital support for years at a time. The introduction of waiting time standards that are on par with those for physical illnesses would be a crucial first step in addressing this.
“We know that untreated ADHD has a significant impact on the economy and that investing in appropriate care and support can help ease pressure on the NHS while also keeping people in work. It is therefore vital that the appropriate funding is made available to implement the recommendations of the report in England. Progress must also be supported in other sectors such as education, employment and criminal justice.” q

A fascinating webinar hosted by Expert in Mind and Dr Laura Pipon-Young, Clinical and Chartered Psychologist (pictured), addressing the question of validity in psychological assessments – how can we tell if someone is lying? Here we give you a breakdown of the key questions
Spotting malingering in psychological assessments: an insightful guide for practitioners
In psychological and neuropsychological assessments, accuracy hinges on one crucial assumption: that the individual being assessed is providing a genuine, consistent and unmanipulated account of their symptoms and abilities. When this assumption is compromised, the validity of the assessment is at risk, potentially leading to false positives, false negatives, misdiagnosis or misguided interventions. Understanding how to detect malingering – intentional fabrication or exaggeration of symptoms for external gain – is therefore not only a clinical skill but an ethical necessity.
What affects the validity of an assessment?
Human behaviour is complex, and there are countless reasons why a person may appear to be underperforming or exaggerating during a psychological assessment. Some of these reasons are genuine: mental illness, fatigue, pain, trauma, cognitive impairment, cultural differences, distractibility or poor rapport can all affect performance or reporting. However, deliberate attempts to mislead – whether by inventing symptoms, exaggerating existing ones or presenting old symptoms as current – also occur, particularly when external incentives are at play. Malingering for financial gain, legal advantage, access to services or avoidance of responsibility remains a significant concern across medicolegal contexts.
The consequences of invalid performance are wide-reaching. Invalid data can lead to inappropriate treatments, financial loss, unnecessary referrals or misallocated health and social-care resources. In legal cases, malingering can distort child protection decisions, sentencing or access to disability benefits. Conversely, failing to recognise genuine impairment can result in denying rightful support or misinterpreting symptoms. In short, validity issues affect fairness, justice and clinical integrity at every level of assessment.
There is no single tell-tale sign of deception. Instead, psychologists use a formulation-driven, multi-method approach to evaluate whether an individual’s presentation is credible.
PVTs assess whether a person’s performance on cognitive tasks is consistent with known patterns of genuine impairment. These tests are designed so that even individuals with significant cognitive difficulties usually perform above certain thresholds. Failing multiple PVTs greatly increases the likelihood of deliberate underperformance: for example, failing three PVTs is associated with a 99% likelihood of performance invalidity. Importantly, psychologists do not infer intent from PVT failure –only that the test data cannot be interpreted with confidence.
In contrast, SVTs examine the plausibility and consistency of symptom reporting. They help identify over-endorsement, improbable symptoms or symptom combinations that rarely occur together. SVTs may be embedded within personality measures or used as stand-alone tools, and they are particularly useful when assessing psychiatric symptoms rather than cognitive ability.

Beyond formal testing, behavioural inconsistencies often provide valuable clues. Rare or bizarre symptoms, improbable severity, vague but wide-ranging complaints, inconsistencies between reported and observed behaviour or an overfocus on stereotypical symptoms can all raise concerns about validity. These patterns, described as ‘The Magnificent Seven’, help clinicians evaluate the plausibility of an individual's account.
Psychologists also consider medical records, school reports, witness interviews, behavioural observation and daily functioning. Often, inconsistencies between self-report and collateral data suggest performance management issues. Understanding motivations – such as financial settlement, access to services, avoidance of prosecution or desire for diagnosis – is essential, though never the sole basis for determining malingering.
The challenge of deception and self-deception
Detecting intentional dishonesty is notoriously difficult. Contrary to popular belief, there are no reliable behavioural markers of lying. Some individuals use sophisticated strategies, while others deceive themselves as much as others. Psychological mechanisms such as rationalisation, emotional memory bias or selective omission blur the line between deception and genuine misunderstanding of one’s own experience.
Symptoms arising from functional neurological disorders, factitious disorder or dissociation may appear inconsistent or exaggerated but are not rooted in intentional deception. Distinguishing these from malingering requires careful formulation, attention to trauma history and an understanding that both external and internal motivations may coexist. Already-marginalised groups are disproportionately labelled as ‘faking’, so clinicians must approach the assessment with cultural sensitivity and humility.
Ultimately, psychologists do not determine intent – that is the role of the court or tribunal. Instead, they provide expert opinion on whether assessment data are valid, consistent and interpretable. PVTs and SVTs are powerful tools, but they must be embedded within a broader clinical picture that includes history, behaviour, context, comorbidity and collateral data. Overreliance on psychometric tests alone risks misinterpretation and legal challenge, especially where test security restricts transparency in court settings.
Spotting malingering is not about catching people out – it is about protecting the integrity of psychological assessment and ensuring that conclusions are safe, fair and evidence-based. By combining structured validity testing with nuanced clinical judgement, psychologists can navigate the complex interplay of symptoms, motivation, deception and genuine distress to provide clear, balanced and ethically-grounded opinions. q
• If you would like the link to watch this informative webinar on demand, or be notified of future CPD registered webinars, please contact office@expertinmind.co.uk
By Lisa Crowther of Carter Brown
[ AI IS PERHAPS already reshaping how expert evidence is prepared and presented in UK courts, offering speed and new analytical power, while forcing courts and practitioners to confront questions of reliability, disclosure and ethics.
In practice, experts use AI to automate repetitive tasks: extracting facts from large document sets, converting unstructured data into timelines, running statistical models, and producing visualisations that make complex technical evidence accessible to judges and juries.
Experts report gains in efficiency that can reduce costs and speed case preparation. In recent months, a number of experts have approached me about the potential use of AI in their work, which has led me to explore this further. It perhaps comes as a result of changes within their day-to-day work, where AI tools are being used for discrete purposes, for example, within healthcare settings.
Recently updated guidance for Judicial Office holders (Courts and Tribunals Judiciary, 2025) warns of AI-generated fake case citations and the potential for sanctions where AI is misused. The judiciary’s evolving guidance underlines that human responsibility and verification remain essential, ultimately advising that conducting legal analysis and legal research using AI tools is not recommended.
Regulatory and institutional responses are moving quickly. The Bar Council, Law Society and government initiatives have issued guidance emphasising professional duties: lawyers and experts must verify

AI outputs, protect confidentiality when using cloud-based tools and remain transparent to the court. The Ministry of Justice’s broader AI action plan signals an appetite to embed AI for triage and access-tojustice improvements – but always with human adjudication at the centre, being clear ‘AI should support, not substitute, human judgment’. Procedural rules also frame AI’s role. Part 25 of the Family Procedure Rules continues to require that expert evidence be limited to what is necessary to resolve the proceedings. Practice Direction 25B makes it clear that experts should ‘provide advice to the court that conforms to the best practice of the expert’s profession’. The expert in the family proceedings also needs to ensure that the manner in which an assessment has been completed is as transparent as it can be, outlining how interviews, testing and analysis have been undertaken. The term ‘AI’ does not yet appear in the relevant Practice Direction in family, criminal or civil proceedings.
Guidance from professional bodies, specific to expert witness work, is scant. Having reviewed the joint guidance from The British Psychological Society and the Family Justice Council, AI is not mentioned. In the most recent version of Good Medical Practice – the General Medical Council’s guidance for doctors, updated in December 2024 – a change has been made to the wording to reflect the use of new technologies: “To help keep patients safe you must report adverse incidents involving medical devices (including software, diagnostic tests and digital tools) that put the safety of a patient or another person at risk, or have the potential to do so.”
The Law Society Gazette reported, at this year’s Bond Solon conference: “The proportion of experts who use it [AI] has doubled from last year, to 20%, but this is considerably lower than usage elsewhere. According to KPMG’s UK attitudes to AI study, 65% of workers in the UK intentionally use AI for work.” There is a paucity of specific guidance relating to the use of AI and experts – and this statistic clearly reflects experts’ reticence to incorporate AI into their work in the absence of a clear position on this.
For expert witnesses, AI has the potential to increase efficiency in some aspects of the expert’s role, but only if its limits are managed. Without clear directives in place, experts should continue to document methods, validate results, be transparent in their communication to instructing parties and the court, and prepared to explain – under oath –how outputs were generated and checked. The expert remains entirely accountable for the delivery of a service and ultimately the contents of their written report. q
[THE RELATIONSHIP between stroke medicine and geriatrics has been recognised by clinicians for many years.
In 2020 Dr Nicholas Evans, clinical lecturer in geriatric and stroke medicine at the University of Cambridge and Honorary Specialist Registrar in Geriatric and Stroke Medicine at Addenbrooke’s Hospital, wrote on the website of the British Geriatric Society: “Geriatricians play a key role in stroke medicine. Alongside neurologists and rehabilitation physicians, geriatricians bring a vital skill to the management of stroke: an understanding of frailty.
“Frailty, the decreased physiological reserve to withstand a stressor event, is widely recognised to influence morbidity and mortality across a range of medical conditions.”
Dr Evans separates the concepts of ageing and frailty, arguing that frailty is a more accurate concomitant of stroke: “Recognition that the role of frailty is independently associated with stroke outcomes reflects a core tenet of the geriatrician; that age and frailty are not synonymous.
“Our results support the holistic approach
of the geriatrician in considering how the individual’s state before their stroke affects the individual they are after it, and how this must be considered as distinct from chronological age. There may also be implications for the use of frailty, rather than age, as a variable in research, as well as its incorporation into routine clinical assessment of acute stroke.
“As geriatricians, it is important that we advocate this message and combat nihilistic ageism. There is little we can do about the number of times an individual has gone round the sun, but frailty represents an important target to promote healthy ageing and improve outcomes after stroke.”
Five years later, on 5 December this year, a new report from the National Audit Office (NAO) looked at how the NHS identifies and supports people living with or at risk of frailty before they reach the point of medical crisis or hospital admission. With the population ageing, the NAO found that GPs are not providing the required support and follow-up for people diagnosed with frailty.
“Frailty is a clinically recognised medical
syndrome related to the ageing process in which multiple body systems gradually lose their in-built reserves,” the NAO states. The report specifically pinpoints GPs as the first point of contact for people living with frailty. However, that is not happening.
The NAO says: “The GP contract requires GPs to identify any registered patient aged 65 years or over who is living with moderate to severe frailty. However, in 2024-25 GPs only assessed one in six patients aged 65 or over for frailty (1.9 million people). This is well below the one in four assessed when the requirement was introduced in 2017-18.”
Gareth Davies, head of the NAO, said: “With the need for health and social care services set to increase in our aging population, it is crucial that people with frailty are supported effectively and consistently across the country. Our report shows that many older people are not getting the support they need.
“The NHS needs to seize the opportunity of the 10-year health plan to build the more effective and sustainable service that it recognises older people need.” q
[ IN PERSONAL INJURY and clinical negligence litigation, the question of future care can lie at the heart of the damages assessment. Where a claimant has sustained a life-changing injury, the court must understand not only the nature of the disability, but the level of care, rehabilitation and professional support required over a lifetime. It is experts specialising in care and case management who provide the detailed evidence that enables those decisions to be made.
Their reports translate complex clinical information into clear, costed support packages that reflect the claimant’s prognosis, functional ability and potential for rehabilitation. In high-value claims involving acquired brain injury, spinal injury, cerebral palsy, amputation and loss of mental capacity, this evidence is critical. Without it, courts are left to make assumptions in an area where precision is essential and the consequences of error can be profound.
A care and case management report must provide a balanced and defensible opinion. The expert is required to analyse medical records, therapy notes, neuropsychological assessments and social circumstances, before forming a view on the claimant’s needs. It is not an exercise in advocacy, but a professional judgment based on experience of managing similar cases and knowledge of the standards of good practice in long-term rehabilitation.
The report will typically set out the nature and extent of the support required: whether the claimant needs 24-hour care,
waking night cover, specialist nursing input, behavioural support or assistance from trained support workers. It will consider the frequency and duration of therapies, the likely trajectory of the rehabilitation plan, the necessity for adapted accommodation and the ongoing involvement of a professional case manager. Each recommendation must be costed and its rationale explained, so that the court can understand both the need identified and the calculation used to reflect that need in damages.
Small differences in clinical presentation can have a significant impact on the valuation of a claim. The distinction between parttime and full-time care, for example, or between sleeping-night and waking-night supervision, will alter the calculation of damages over decades. It is for this reason that experienced expert evidence is so valuable. A well-reasoned report provides a clear evidential pathway from diagnosis to costed provision, allowing the court to reach a proportionate outcome.
The question of care is often interlinked with the claimant’s ability to work or re-enter education. Expert witnesses are frequently asked to comment on the extent to which the injury has affected independence, daily living and vocational potential. Assessments may address the feasibility of a phased return to work, the need for workplace adjustments or the likelihood of permanent loss of earnings. These opinions help the court to determine not only the cost of care, but the wider consequences of injury on the claimant’s life.
Contemporary rehabilitation is inherently multidisciplinary and expert reports will reflect this. Rather than focusing on isolated interventions, they describe a coordinated model of support involving physiotherapy, occupational therapy, speech and language therapy, neuropsychology and specialist medical oversight. Assistive technology and home adaptations are now central components of many care plans, and the expert must consider both their therapeutic value and their cost implications.
Digital health tools are increasingly relevant. Remote monitoring, virtual rehabilitation sessions and technology to support communication and safety are now part of the landscape in longterm care. Expert witnesses must be able to comment on whether such tools are appropriate, cost-effective and sustainable, and whether they reduce staffing needs or supplement existing support.
Litigation reforms in recent years have also influenced expectations of expert evidence. Courts now emphasise clarity of reasoning, transparency of assumptions and concise presentation. While reports must still be thorough, judges expect structured opinions supported by data rather than narrative description alone.
Scenario modelling is increasingly common, particularly in claims involving children or young adults where needs will evolve over time.
Despite these developments, the essential value of care and case management evidence remains the same: it allows the court to understand the real costs and practical demands of living with serious injury. The expert provides a bridge between medical complexity and legal decision-making, allowing damages to be assessed on the basis of professional judgement rather than conjecture. Their reports provide the blueprint for future care, supporting sustainable, appropriate and evidence-based provision.
In a field where accuracy can change a person’s quality of life for decades, the importance of experienced, impartial expert evidence is undeniable. For legal teams navigating complex claims, the contribution of care and case management experts remains central to achieving outcomes that are fair, well-grounded and truly reflective of the injured person’s needs. q
By Lena Walliman, care expert, practising case manager, advanced nurse practitioner and independent prescriber
[ AS HEALTHCARE becomes more complex across both the NHS and the private sector, the role of the nursing and care expert witness is shifting rapidly. Litigation demands expertise that goes beyond task lists; beyond rotas; and far beyond the simple calculation of care hours. What is required is skilled reasoning, a deep understanding of governance and patient safety, and a realistic awareness of how care is actually delivered in today’s overstretched system.
When care is misunderstood, mis-specified or poorly designed, the consequences can be profound. There is a significant risk that, when the nuance, complexity and clinical reality of care delivery is overlooked, packages will fail in ways that cause harm to the client, to their family and to the financial sustainability of the package itself.
I have seen situations where the amount of care mattered far less than the quality of it. In several cases I have been instructed on, or taken over as a care provider, the wrong care, despite being wellfunded, has caused more damage than benefit.
Care experts are central, and our assessments should go far deeper than describing what support someone may need. When considering short and long-term needs, the approach must be holistic. Care can either restore function or quietly undermine it: not simply through physical support, but through social, emotional and personalised support. The role of meaningful social interaction is often underestimated.
Care Is not a rota: it’s a recipe
Poorly matched or loosely governed support can be actively harmful and risks:
• Undermining confidence
• Increasing dependence
• Placing increased and unsustainable pressure on families
• Eroding trust
• Wasting time and funding
• Stalling or compromising rehabilitation
Having spent years as the owner and director of complex care provisions for adults and children across the UK, I became known for stabilising and turning around failing care packages. My experience taught me that quality of support outweighs quantity every time. Hours alone do not rehabilitate a person: skill, personality compatibility, training, boundaries, communication and clinical leadership do. If the match is wrong or the assessment incomplete, the support package will ultimately fail.
My on-going work within The Silverlining Brain Injury Charity reinforces the importance of community, connection and meaningful interactions. I see first-hand how positive social engagement can complement clinical care and restore a sense of belonging, identity and hope: key components of long-term recovery that too often fall outside traditional care planning.
Independence, objectivity and realistic expectations
Maintaining independence is not simply a procedural requirement under CPR Part 35; it is a safeguard. Whether instructed by claimants or defendants, a care expert and NMC registered nurse’s responsibility is the same: to recommend care that is proportionate, evidence-based, safe and deliverable.

Deliverability is one of the biggest challenges in healthcare today. Workforce shortages, recruitment difficulties, inflationary pressure, agency instability and rising complexity in community practice all affect what is possible. An expert who is disconnected from real-world practice may recommend provision that looks reasonable on paper but is impossible to implement.
To remain objective, it is essential to stay closely connected to the delivery of care: maintaining contact with providers, directly employed teams, treating teams, case managers and regulatory change.
Another important consideration is the hidden burden of care on families. When care is poorly structured, insufficiently skilled or inconsistently delivered, families quietly step in. They become the untrained safety net: often at great personal cost – physically, emotionally and socially.
The right care is not the most care; it is the care that:
• Restores dignity
• Supports identity
• Prevents deterioration
• Protects family relationships
• Rebuilds a person’s life, not just their routine
What differentiates care experts is more than qualifications and titles; it is the ability to see and understand the full picture –clinical, emotional, realistic, practical and operational: quality over quantity; evidence over assumption; independence over optimism; and, above all, care that repairs. q



[ THE NATIONAL JOINT REGISTRY (NJR) has published its 22nd Annual Report. It was launched at the annual congress for the British Orthopaedic Association in September.
The aim of the NJR Annual Report is to increase the availability of evidence-based information on joint replacement surgery to all NJR stakeholders by providing a year-on-year view of clinical activity and outcomes. The report also provides a summary of the work and progress of the registry, including management and funding.
The full published report, along with associated appendices, infographics and updates on NJR activity and committees, can be found on the NJR’s dedicated Annual Report website at reports.njrcentre.org.uk
Having collected data since April 2003, with the purpose of improving patient outcomes following hip, knee, ankle, elbow and shoulder replacement, the registry has now recorded over 4.5 million
[THE British Limb Reconstruction Society (BLRS) and British Orthopaedic Association (BOA) have collaborated to define best practice for patients being considered for limb reconstruction surgery.
The document – Best Practice in Limb Reconstruction Surgery in the United Kingdom – addresses the configuration of services, describes best practice and provides recommendations for consultant competency, collaborative working and professional standards.
It is part of a suite of documents, which includes a position statement released on 31st July 2025 and the BOA are confident that it will provide a framework to ensure that the highest quality care is available to all patients.
According to the guidance: “Limb reconstruction surgery involves the management of a diverse group of congenital and acquired conditions. The goal of treatment is to improve limb function and quality of life by correcting limb deformity, reconstructing skeletal defects, managing long bone and fracture related infection, and fracture non-union. It may also involve ablative reconstruction or amputation surgery. Limb reconstruction is generally undertaken in specialist units, typically located in elective surgical sites and major trauma centres and with suitable support within a district general hospital.”
The document was published in December.
Earlier, in November, a further document outlines Best Practice in Children’s Trauma & Orthopaedics in the UK, in this case produced as a collaboration between the BOA and the British Society of Children’s Orthopaedic Surgery.
According to the BOA: “This document addresses the configuration of elective services, describes best practice in children’s fracture management, and provides recommendations for consultant competency, collaborative working and professional standards in paediatric orthopaedic surgery. This is part of a suite of documents, which includes a position statement released on 20th March 2025 and we are confident that this will provide a framework to ensure that the highest quality care is available to all patients.” q
procedures. Everyone with an interest in joint replacement will be delighted to see that it shows even more widespread and up-to-date analyses of the outcomes of the many implant brands available.
As a result of the increasing volume and quality of data, it is possible to make more accurate analysis available to all stakeholders. It is essential that as much good quality data as possible is captured to continue to improve clinical outcomes and patient safety – the report has also been prepared in separate joint sections again this year. A key message is that patient safety and clinical outcomes continue to improve, as identified through the year-on-year reduction of joint revision surgery.
According to the British Orthopaedic Association, the report ‘shows a continued reduction in joint revision surgery – evidence that implants are lasting longer, and that outcomes for patients have improved year-on-year’.
Annual Clinical Reports (ACRs) for hospitals are also now available on NJR Connect. The reports show NJR data for the most recent complete financial year and cover:
• Indicators of data quality: rates of compliance, patient consent and linkability
• Hip and knee replacement outcomes data (funnel plots), for revision for all hospitals and surgeons (anonymised) across procedure types
• Hospital outcomes data for hip and knee replacement (funnel plots) for mortality. q
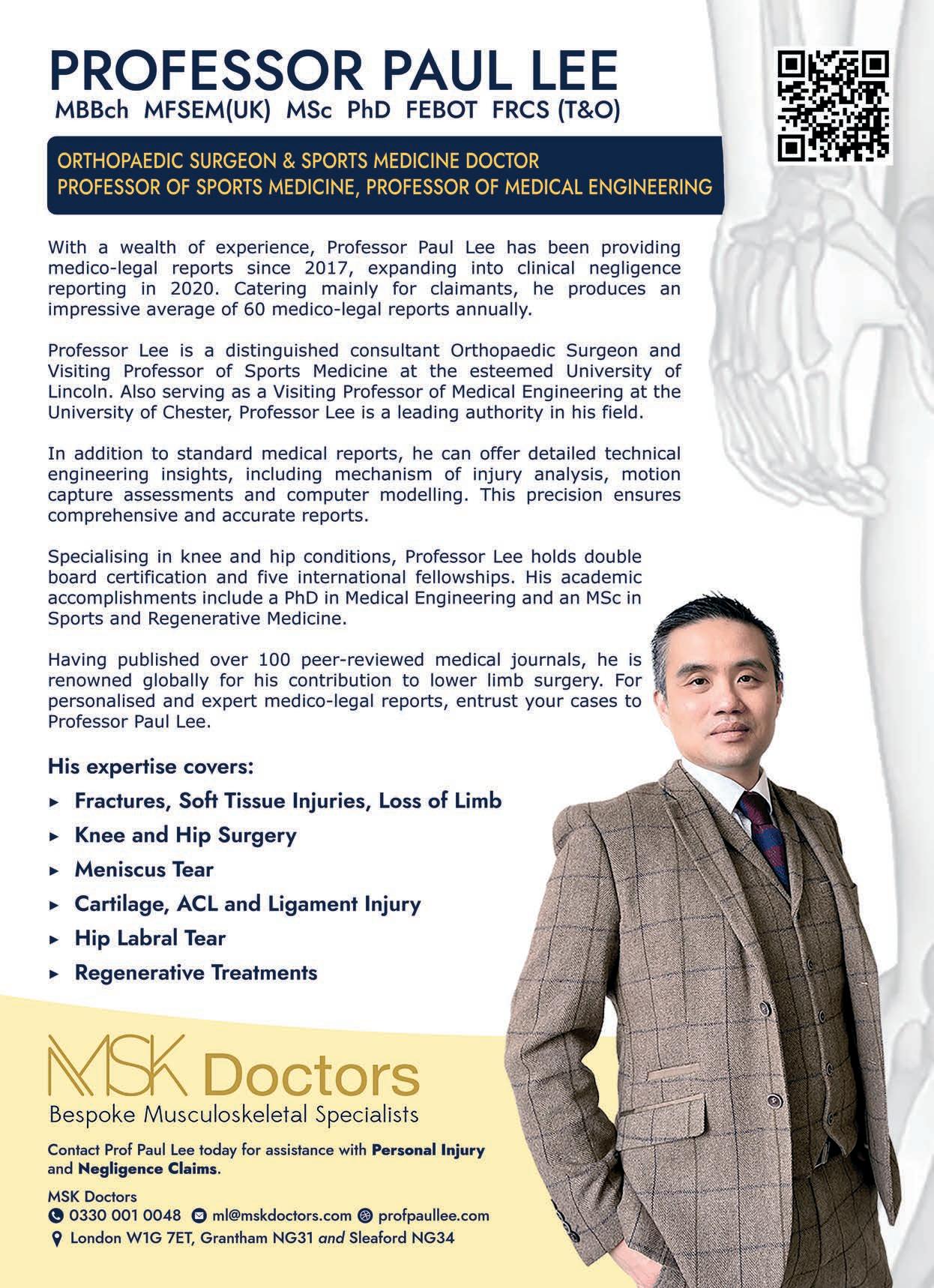
By Professor Paul Y F Lee, consultant orthopaedic surgeon, Honorary Professor of Sports Medicine and expert witness
[IN PERSONAL INJURY and clinical negligence work, one scenario appears time and again. The radiology looks ‘acceptable’; the bone has ‘healed’ – yet the client still limps, fatigues easily or cannot return to work.
Traditional reports often stop there: two experts presenting two opinions. But when we apply biomechanics and engineering we move from opinion to objective proof.
Beyond the X-ray: seeing the truth in 3D
A plain film may confirm union, but it cannot reveal the mechanical reality of how that limb now functions. A joint or fracture may appear anatomically aligned, yet subtle rotational errors, limb shortening or changes in offset alter how force travels through the body. Those changes are often invisible on twodimensional imaging, but unmistakable in three-dimensional reconstruction.
As both a consultant orthopaedic surgeon and a researcher with a PhD in Medical Engineering, I combine clinical insight with computer-aided modelling. By converting CT or MRI data into precise 3D representations (pictured), we can mirror the uninjured side and directly compare it with the repaired anatomy.
That exposes any geometric deviation – however small – and, more importantly, allows us to understand what that deviation means in daily life.

The legal tests of breach of duty and causation both benefit from this approach.
• Breach of duty: Did the surgical reconstruction, fixation or alignment meet accepted biomechanical standards?
• Causation: Can we prove that a measurable deviation led directly to functional disadvantage?
By framing the argument in measurable, mechanical terms we supply the missing link between radiological appearance and lived reality. It is particularly valuable in cases where the defence relies on the phrase ‘within acceptable limits’. Acceptable to whom – and by what metric? Biomechanics provides that metric.
The modern courtroom demands clarity and objectivity: biomechanical analysis delivers both. It bridges the gap between a radiological ‘healing’ and a functional ‘recovery’: proving that the two are not always the same. It explains why a client continues to limp, how muscle demand has changed and what that means for their capacity to work or enjoy normal life.
The result is testimony grounded not in conjecture but in measurable, reproducible science. It transforms a borderline case into one supported by demonstrable facts: facts that can withstand the highest level of scrutiny.
Once the 3D model is created, the analysis moves from observation to calculation. We assess how far the repair has restored the body’s natural lines of force and how mechanical efficiency has changed. In practical terms, a few millimetres of shortening or a few degrees of rotation can shift the body’s centre of gravity, forcing muscles to compensate. What looks perfectly fine on an X-ray can translate into an altered gait, quicker fatigue or pain after ordinary activities such as climbing stairs, walking on uneven ground or standing for long periods.
Across thousands of steps each day, that small imperfection becomes a continual energy drain: an unseen cost the patient pays with every movement.
That is the real strength of biomechanical causation analysis: it turns opinions into facts; a picture is worth 1,000 words. It converts abstract geometry into consequences that anyone can understand.
We can demonstrate that the leg is working harder to keep the pelvis level, that balance strategies have changed, or that joint loading has shifted toward areas not designed to bear that stress.
In court, that means we are no longer debating subjective complaints but showing a clear, mechanical chain of cause and effect. The injury is not merely painful: it is physically inefficient, and that inefficiency can be demonstrated, visualised and explained.
Orthopaedic surgery and engineering share a single purpose: restoring structure and function. When that restoration falls short – even slightly – the consequences ripple through the body’s mechanics and the patient’s life.
By applying engineering principles to clinical data, we can now reveal those effects with precision: helping the court to see not just that a fracture healed, but whether it healed right. That is how we move from ‘acceptable’ to actionable: from shadows on a scan to proof beyond reasonable doubt.
• Objective causation: 3D biomechanical reconstruction transforms subjective symptoms into measurable proof – demonstrating how even small misalignments cause real functional loss.
• Breach of duty defined by physics: By quantifying deviation from normal mechanics, it becomes clear whether a surgical outcome or fracture alignment truly meets acceptable biomechanical standards.
• Evidence that stands up in court: Visual models and reproducible calculations provide persuasive, court-ready evidence that strengthens arguments on causation, breach and quantum. q
• Professor Paul Y F Lee is a consultant orthopaedic surgeon, Honorary Professor of Sports Medicine and expert witness specialising in biomechanics, imaging and causation analysis. He and his team at MSK Doctors operate across London and Lincolnshire, with offices in London, Marylebone and near Liverpool Street Station. Urgent expert opinion can be provided by prior agreement

[
MILLIONS OF PEOPLE with arthritis are not receiving timely diagnoses or adequate treatment, are left to face avoidable pain and are often unable to work, according to a report by the charity Arthritis UK – formerly known as Versus Arthritis.
Arthritis affects one in six people and is a leading cause of disability, yet the condition remains largely misunderstood and many with the condition are not receiving the care and support they urgently need. As a result, people with arthritis are living with high levels of pain, fatigue, mental health challenges and financial strain, according to the report.
Arthritis UK has worked with YouGov to survey around 8,000 people representative of the population affected by the condition. It has revealed that, of the people surveyed, one in two (50%) said that arthritis had impacted on their ability to work. Of those, nearly four in 10 (39%) have stopped work due to their arthritis and over a third of retired people (35%) said arthritis played a part in their decision to retire.
Left Waiting, Left Behind: The Reality of Living with Arthritis presents the reality of living with the condition through lived experiences and personal stories, and shows that the impact of arthritis is unequal, with people from lower social grades reporting worse experiences from all areas of life. It concludes that people with arthritis face widespread challenges in accessing effective treatment and support, long delays to secure a diagnosis and lack of treatment options once a diagnosis is made.
More investment, improved services and better training for frontline healthcare professionals are urgently needed to avoid further adversely impacting the lives, relationships and work opportunities of this large group, Arthritis UK says.
The report’s other key findings include:
• Nearly one in three people (32%) surveyed say arthritis severely or very severely impacted their life in the past year.
• Six in 10 people (60%) are living in pain most or all the time due to their arthritis.
• Over one in three people (36%) surveyed felt their condition was not well managed.
• Nearly one in two people (48%) who have seen a healthcare professional felt their symptoms were not taken seriously or were underplayed when they were trying to identify their arthritis.
• Nearly one in two people (46%) reported their ability to exercise was affected severely or very severely by their arthritis symptoms – even though being active can be important in preventing other long-term conditions.
• Seven in ten (71%) younger adults (those aged 18 – 44) felt other people didn’t understand the impact arthritis has on their life.
People in lower social grades, younger adults and those with autoimmune inflammatory conditions are disproportionately impacted by arthritis, facing greater challenges across all areas of life and more frequent barriers.
The survey found of those who reported arthritis having an impact on their ability to work, 28% of those in higher social grades reported stopping work due to arthritis compared to nearly half (49%) of respondents from lower social grades.
People with arthritis are being financially squeezed, as the condition can increase the personal cost of living while impacting the ability to earn. Arthritis affects every aspect of life, from physical health to relationships and mental health, with barriers to effective care preventing people from living the lives they want to lead, the report concludes.
Deborah Alsina MBE, chief executive of Arthritis UK, commented: “Too many of the 10 million people with arthritis are being left unsupported and left to face daily pain, without timely diagnosis and adequate treatment. This erodes their quality of life and damages the prospect of economic growth. This report shows us that huge numbers of people with arthritis are falling out of work and risk being pushed into poverty. The further tragedy is that much of this is avoidable.
“Arthritis is grossly misunderstood, with diagnoses too often delayed or absent. We must tackle the misconception that arthritis is an inevitable part of ageing and improve the diagnosis rates and the treatment available, especially as the number of people with arthritis increases. We are sitting on a ticking timebomb of costs that the country will struggle with if it is not properly identified as a major risk to public health.
“One of the many reasons arthritis must be considered a major risk to public health is it is a gateway condition, increasing the risk of other serious diseases like cardiovascular disease and depression. We cannot afford to miss or mistreat arthritis as it can be a warning sign that patients could accumulate other conditions, and with more rapid progression.“q

David Berry PhD FRC Path MFSSoc MRSC
Independent Toxicology Consultant Specialist in Clinical and Forensic Toxicology with particular emphasis on drugs (both illicit and therapeutic) and alcohol. www.toxicologyservices.co.uk
Mr Timothy Burge MBChB FRCS FRCS(Plast) DMCC MSc
Consultant Burns & Plastic Surgeon
• Cosmetic and aesthetic surgery of the breast and trunk
• Burns • Trauma • Scars
Clinics in Birmingham, Bristol, Cardiff, London and Salisbury. www.clifton-plastic-surgery.co.uk


Professor Paul J Ciclitira MB PhD FRCP MRCS FRCP AGAF
Dr Lance N. Forbat BSc (Hons) MD FRCP FRCP (Glasgow)
Consultant Cardiologist
Experienced in writing medico-legal reports on all aspects of adult cardiology – specialising in angina, heart failure, arrhythmias and pacing.
www.heartattacksymptoms.co.uk
Mr Kim Hakin FRCS FRCOphth
Consultant Ophthalmic Surgeon and Expert Witness on ophthalmological matters
www.kimhakin.com


•
Dr Sarah Cockbill Expert Pharmaceutical Witness
PhD BPharm MPharm LLM DAgVetPharm FRPharmS FVPA
• Pharmacology
• Drug Interactions • Formulation
• Appropriate Dosage • Veterinary Pharmacy • Drug Licensing Instructions for claimant, defendant or as Single Joint Expert
Professor of Gastroenterology with particular interest in food allergy, including Coeliac disease, peptic ulcer, inflammatory bowel disorder and hepatology. www.profpaulciclitira.co.uk E: cockbills1@gmail.com
Mr Philip Coleridge Smith DM MA BCh FRCS
Consultant Vascular Surgeon
20 years of:
• Defendant instructions • Claimant instructions
• Single joint expert • Court experience



www.adsummedicolegal.com & www.britishveininstitute.com
Dr Sam Creavin MPhil MBChB MRCP(UK) MRCGP PhD CUBS General Medical Practitioner

• Delayed diagnosis: cancer, sepsis, spinal disorders, ectopic pregnancy, diabetes, heart disease • Instructed by GMC and NHS resolutions 60/40 split • Quick turnaround. Authoritative, logical and reasoned reports. www.gpexpertwitness.com
Chris Dawson MS FRCS LLDip
Consultant Urologist with 20 years experience of medico legal report writing and expert witness work and has completed over 1,850 reports. He also regularly completes Fitness to Practice reports for the General Medical Council.
www.chrisdawson.org.uk
Mr Mark Duxbury MA (Oxon) DM FRCSEd (Gen Surg)
Consultant Hepatobiliary, Pancreatic & General Surgeon
• General & emergency surgery • Hernia surgery
• Liver & pancreatic surgery • Gallbladder & biliary surgery
• Laparoscopic surgery • Hepatobiliary surgery www.markduxbury.info/medicolegal
and



Mr Vijay Joshi MBChB, LL.B (Hons), FRCSEd (C-Th), PGCert (Medical Law)
Consultant Thoracic Surgeon
Personal injury and clinical negligence cases relating to diseases and injuries of the chest. Preparation of medicolegal reports and giving evidence in court. www.thoracicexpertwitness.co.uk
Atul Khanna FRCS (Plast)
Consultant Plastic, Reconstructive and Hand Surgeon
• Hand surgery • Soft tissue injury • Burns management
• Medical negligence in cosmetic surgery www.atulkhanna.co.uk/expert-witness/
Dr Raj Kumar – Dental Expert
Causation and Liability and Condition and Prognosis Reports
• General dentistry • Cosmetic dentistry • Patient consent
• Dental implantology • Orthodontics • Facial aesthetics 07802 456 804 | info@dentalexpert.me | www.dentalexpert.me
Kulvinder Lall Consultant Cardiothoracic Surgeon Instructions taken in cases relating to cardiac and thoracic surgery, including aspects relating to surgical care and those following trauma to the structures of the chest. www.kulvinderlall.com
Mr Brian Leatherbarrow BSc MBChB DO FRCS FRCOphth




Consultant Ophthalmic, Oculoplastic & Orbital Surgeon • Complications of cosmetic eyelid surgery • Eyelid reconstructive surgery • Eyelid and orbital tumours and trauma • Loss of an eye / socket reconstructive surgery • Thyroid eye disease • Ptosis surgery
www.medicolegalophthalmology.co.uk
Mr Richard Matthews MB BS FRCS FRCSE MAE PLASTIC & HAND SURGEON
Mr Matthews is well versed in the provision of Medical Reports relating to Personal Injury ranging from scarring through trauma, including burns and scalds, to non-bony hand injuries.
www.richardmatthewsmedicolegal.uk
Mr Lindsay Muir MB MCh(Orth) FRCS(Orth)
Consultant Hand Surgeon
• Amputation • Nerve injury • Dupuytren’s disease
• Scaphoid fracture • Finger fracture • Tendon injury
• Hand surgery • Wrist fracture www.tmhc.co.uk



Mr Abraham Odumala
MBBS M.MedSci FWACS FRCS FRCS(Tr & Orth)
Consultant Orthopaedic Surgeon – Upper Limb Specialist. Expertise in all upper limb conditions and treatment. Shoulder, elbow, wristand hand injuries. www.yorkshire-upperlimb.co.uk
Dr Shanthi Paramothayan
BSc PhD MBBS LLM MScMedEd FHEA FCCP FRCP
Consultant Respiratory Physician specialising in negligence cases relating to all aspects of respiratory medicine. www.paramothayan.com
Jonathan Park Consultant Ophthalmologist
MB ChB (Hons) BSc (Hons) FRCOphth
Clinical negligence (ophthalmology) and personal injury (non-surgical ocular trauma) cases. Can act on behalf of either claimant or defendant or as a Single Joint Expert. www.jonathan-park.co.uk
Dr Nick Plowman MA MD FRCP FRCR
Consultant in Clinical Oncology
Specialist areas of expertise include radiation therapy, chemotherapy, immunotherapy and genomics as well as delay in diagnosis. This applies to adults and children. drnickplowman.com
Dr Stuart Porter Chartered Physiotherapist
PhD MCSP HCPC BSc Hons Grad Dip Phys MLACP PgCAP Cert.MHS SFHEA
Specialist areas of expertise include: • Clinical negligence
• Breach of duty • Allegations of inappropriate contact
• Assessment of adults and children • HCPC investigations. stuartbporter@aol.com
Dr Samy Sadek MBBS BSc MCEM FCEM
Consultant in Emergency Medicine & Pre-Hospital Care
• Minor injuries • Major trauma
• Medical emergencies • Criminal and forensic cases





Prof. Elizabeth J. Soilleux MA MB BChir PhD FRCPath PGDipMedEd
Expert Witness Pathologist with a particular interest in haematopathology. Short reports on specimens, full court compliant reports and expert biopsy reporting. www.expertwitnesspathologist.co.uk

Mr Bernard Speculand MDS FDS FFD FRACDS (OMS) Consultant Oral and Maxillofacial Surgeon. Personal injury and clinical negligence cases for claimant, defendant and as Single Joint Expert. Special interest is TMJ Surgery.
Yvette Young (Secretary) T: 0121 605 1884 E: info@medsecadmin.co.uk www.birminghamtmj.co.uk
Dr Ian Starke MSc MD FRCP
Stroke Medicine and Medicine for the Elderly Reports and examinations for clinical negligence and personal injury cases in stroke medicine and geriatric medicine www.expertwitnessinstrokes.co.uk
Mr. William E G Thomas Bsc, MBBS, FRCS, MS
Consultant Surgeon specialising in general surgery, hernia surgery, gastrointestinal surgery, hepatobiliary-pancreatic surgery, laparoscopic surgery and endocrine surgery T: 0114 262 0852 E: wegthomas@btinternet.com W: www.wegthomas.com
UK Ophthalmology Experts
UK Ophthalmology Experts are a team of leading, independent ophthalmology experts covering all aspects of ophthalmology. www.ukophthalmologyexperts.co.uk




DR S V MEDICALS (Mr Sen Venkat)
MSc Ortho (London) FRCS Consultant Orthopaedic Surgeon • Whiplash injuries • General trauma • Sports injuries
Mr Sameer Singh MBBS BSc FRCS Orth Consultant Orthopaedic Surgeon • All aspects of trauma – soft tissue and bone injuries • Upper and lower limb disorders and injuries
• Whiplash injuries • Expert Witness for defence and claimant Clinic locations – London, Milton Keynes and Bedford
• Reports on survivability and cause of death. www.drsamysadek.com www.orthopaedicexpertwitness.net


• Clinical negligence work • Joint replacement surgery of hip and knee • Hand, shoulder, elbow and wrist injury www.drsvmedicals.co.uk
Ms Leyla Ziyal MPhil AFBPsS CPsychol
HCPC Registered clinical Neuropsychologist
• Neuropsychological assessment and rehabilitation
• Depression • Occupational stress • PTSD • Anxiety www.accentpsychology.co.uk



[
LUNG CHARITY Asthma + Lung UK, has warned that hospitals are hurtling towards a respiratory catastrophe this winter, as new analysis shows there has been a 23% rise in the number of emergency admissions for respiratory issues in England in the three years since 2022/23. NHS England data show that the crisis reached an alarming high in December last year, when over 220,000 people were rushed to hospital in respiratory distress across England.
With this year’s flu season starting earlier and looking significantly worse than last year, the charity is concerned emergency admissions will rise even higher this winter, putting further strain on an already stretched NHS. In addition, a lack of access to care is creating a revolving door crisis with the number of readmissions for respiratory illness back into A&E within 30 days of discharge going up by almost 30%; between April 2024 and March 2025 there were more than 405,000 ‘bounce-back’ admissions.
Respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD) are the UK’s third biggest killer next to cancer and cardiovascular disease, and are the main drivers of winter pressures on the NHS – influenced by factors like colder weather and increased winter viruses. They are also identified as the leading cause of annual emergency admissions.
Sarah Sleet, chief executive at Asthma + Lung UK, said: “Winter is the worst time of year for people with lung conditions and hospitals are at risk of becoming overwhelmed as a result with flu levels already higher than expected – and this year it is predicted to be the worst outbreak for a decade.”
Alongside asthma and COPD, a major reason for hospitalisation, particularly among older people, is pneumonia. Older people’s insurer SAGA has published an alert around pneumonia, including what it terms ‘walking pneumonia’ – wherein a person can be suffering from

the disease yet not realise it because the infection is not severe enough to incapacitate them.
SAGA’s alert also points out the growing instance of hospital-acquired pneumonia (HAP), or nosocomial pneumonia. Described by the BMJ as “an acute lower respiratory tract infection that is by definition acquired after at least 48 hours of admission to hospital and is not incubating at the time of admission”, HAP has a higher death rate and results in a longer hospital stay than community-acquired pneumonia (CAP).
In certain circumstances the infection could be the result of poor hygiene during a hospital stay and may lead to a negligence claim. According to Manchester-based advice.co.uk: “You can sue for hospital-acquired pneumonia if it developed due to the negligent care and treatment you received, as this would constitute medical negligence. This applies whether you suffered negligence in an NHS hospital or a private healthcare setting.” q
[ PHYSIOTHERAPY was one of four allied health profession (AHP) groups invited to provide evidence to the Select Committee on Health and Social Care to inform the government’s 10-year workforce plan for the NHS in England. Karen Poole, AHP rehab consultant and clinical lead for rehab and reablement, represented the Chartered Society of Physiotherapy (CSP).
Questions from parliamentarians were focused on challenges and opportunities facing AHP professions when considering the 'left shift' from hospitals to communities.
Karen, an AHP rehabilitation consultant for East Sussex Healthcare NHS Trust and strategic clinical lead for rehabilitation and reablement at NHS Sussex, said: “We have a glass ceiling with allied health professions and I think we need to break through that glass ceiling.
“In order for us to help the government achieve the ambitions of the shift into neighbourhood health and into community we need to have those voices at those levels, being able to inform, bring along those kind of skills. Ensuring that we've got that visibility of AHP leadership there, who can advocate and can also describe the opportunities around how we start to deliver care within the community.”
The witness panel also included representatives from occupational therapy, dietetics and radiography. Across all AHP contributions, several common themes emerged:
• The need for stronger career progression pathways
• The challenges of delivering care in community settings
• The importance of AHP leadership at system level
• The development of advanced practice routes.
They also highlighted the significant opportunities AHPs offer in supporting the shift from hospital-based care to communityfocused services.

The panel was asked about having the right amount of workforce in acute therapy versus in the community, to which Karen explained: “This is about working across that pathway. And it's not an either/or.”
She said that community services have been ‘under-resourced for a very long period of time’ but that at the same time: “We [also] need to make sure that we have the right investment into our acute therapy staffing.”
When asked about community services, Karen put forward that we don’t have a supply problem with physiotherapy: we have an issue with career progression: “It’s about putting in some of those advanced practice roles; seeing the career progression, as well as seeing some of those diverse, support worker roles, which also have career progressions between bands.”
The CSP is calling for a workforce plan that fully recognises physiotherapy and rehabilitation as central to achieving the NHS’s goals for prevention, community care and productivity. For that to happen, the plan must ensure that the physiotherapy workforce is considered as a core pillar of neighbourhood working, with rehabilitation and AHP leadership embedded at system, place and neighbourhood levels within ICB and provider structures.
The CSP is calling for investment in career development and leadership, including advanced practice and consultant-level rehab roles.
Ash James, director of practice and development at the CSP, said: “The CSP is taking the voice and experience of our members to the heart of power to speak up for physiotherapy. This was a huge opportunity to share experiences and help shape the decisions that define the future of care.
“We are very grateful to Karen for speaking out with such passion and experience, particularly raising importance of leadership roles for physios as we move from hospital to community.” q

[ THE British Society for Surgery of the Hand (BSSH) has produced a report detailing its reaction to the introduction of sterile pre-packed implants. The mandatory introduction of individually pre-packed screws and plates has raised significant clinical concerns among hand surgeons in the UK. Those concerns include the safety and efficiency of surgery, prolonged tourniquet time, infection risk, significant

[ THE CHARITY Changing Faces has addressed an open letter to casting agents, asking them to work towards positive change by ensuring fair and inclusive casting practices for people with visible differences.
Visible difference continues to be used as a sign of evil and villainy on stage and screen, the charity notes, negatively impacting on the visible difference community, especially around Halloween, when the letter was posted.
“This damaging stereotype is often seen in Halloween costumes, not only through the characters people dress as – eg Joker and Freddy Krueger – but also in the fake scars, burns and other prosthetics sold in shops.
“That’s why we’re asking casting agents to do their bit towards positive change by diversifying the actors they hire and breaking down stereotypes in the media.”
The letter reads in part: “Visible differences – scars, marks, burns and conditions that affect one’s appearance – should never define a character. Yet far too often, film and TV cast people with visible differences as villains, reinforcing harmful stereotypes that shape how society views the visible difference community.
“This isn’t just lazy storytelling; it has real-world consequences that influence how people with a visible difference are treated. And that can impact on people’s mental health and wellbeing.”
The letter continued: “It’s time for hurtful comments that associate difference with evil to end. We hope you’ll play your part.
“People with a visible difference can play villains. They can also play the hero, the love interest or the family member. But we rarely see that.”
The letter points out that, in a recent survey by Focaldata, just 17% of respondents had seen someone with a visible difference cast as the hero. And over half of those surveyed feel people with visible differences are inaccurately represented in film and TV, showing a persistent lack of range and opportunity.
“We want more roles to be open to people with a visible difference, reflecting the reality of their lives and breaking the damaging link between difference and evil.” q
environmental issues and increased financial burden to the NHS.
According to the report: “To better regulate surgical implant use and mitigate unrecognised harm, the Cumberlege Report recommended that all implants should be traceable from point of manufacture to implantation and beyond. This robust monitoring could facilitate early identification of poorly performing or dangerous implants.”
Historically, the report says, plates and screws used in orthopaedic trauma surgery have been sterilised on an implant and instrument tray and replenished with new implants on this tray as required. While that had numerous surgical benefits – immediate availability of screws, ability to template precisely and technical ease for scrub teams and surgeons alike – those implants are not traceable and thus not supported by the recommendations made by Baroness Cumberlege.
“Fixation of hand fractures involves use of micro-screws and plates. These are more difficult to handle when packed to allow full traceability, impairing the surgeon’s ability to safely treat injuries. Many similar implants have been excluded from the traceability legislation on the basis of their small size.
“However, there is increasing pressure from regulatory bodies for hand surgeons to adopt the use of single item sterile trauma implants. Hand surgeons throughout the UK are of the opinion that this would compromise care of hand surgery patients and would contradict the principles of Values Based Healthcare. This has been echoed by hand surgeons in Scotland, where PPIs have been enforced for the past few years.
“Hand surgeons throughout the UK are of the opinion that a move to using sterile packed implants is neither indicated nor clinically practical. It would be to the detriment of the environment, add significant financial burden to the NHS, and most importantly would result in worse outcomes for patients.” q

By Professor Jonathan Pinkney
[OBESITY, a condition once neglected and widely stigmatised by society and doctors, has become an important field of medicine.
Contrary to popular misconceptions, obesity is not simply a matter of choice, but the outcome of a complex interplay of genetics, upbringing and social environment. Severe obesity is a leading cause of ill-health and impacts on life expectancy to a similar extent as many common cancers and heart disease. Until recently, however, effective treatments remained elusive, although that is changing.
Important advances in treatment have fuelled demand. An increasing range of commercial weight loss services are available, especially providing ‘remote’ consultations and ‘digital’ delivery, which has both advantages and potential pitfalls. Weight loss surgery (bariatric surgery) has also become a widespread and valuable treatment for selected people. In general, however, the NHS has neglected obesity medicine. However, the advent of powerful new weight loss drugs – the
glucagon-like peptide-1 receptor agonists, often called GLP1s for short – has heralded a new era, offering much improved prospects for weight loss. These treatment advances have brought new hope for many people; although, not unexpectedly, there are always unfulfilled expectations, unsuccessful treatments, unforeseen side effects and occasionally medical errors.
The rise of obesity gives rise to increasing litigation and claims in both the health and occupational settings. Common reasons for solicitors and patients to seek expert assistance in the field include the generic concerns like inadequate clinical assessment and judgement, side-effects and errors. The arms-length nature of remote consultation and monitoring can also limit the quality of the assessment.
In the headlong rush for drug treatments, the risk of adverse effects is sometimes overlooked and patients can be exposed to unintended consequences. Failure to address
underlying dietary problems and eating disorders, excessive weight loss with difficulty in weight stabilisation, and vitamin and mineral deficiencies, are also among common pitfalls. Severe obesity particularly impacts upon people’s ability to maintain their independence and undertake day-to-day tasks both at home and in the workplace.
Finally, many people who are not technically obese also now seek drug treatment, which is sometimes prescribed with few questions asked, exposing some people to danger and leaving practitioners open to criticism. q
• Professor Pinkney is a consultant in endocrinology and diabetes and has a special interest in the medicolegal aspects of obesity. He has worked in the field of obesity medicine and been an active researcher for over 25 years. His professional affiliations include the Pituitary Foundation, Endocrine Society and the Association for the Study of Obesity.
He has advised NICE on obesity treatments, NIHR on obesity research and speaks and lectures on the subject
[PEOPLE ACROSS THE UK with diabetes who use the FreeStyle Libre 3 (pictured) or FreeStyle Libre 3 Plus sensors have been warned that some sensors are giving incorrect readings showing low glucose levels, which if undetected may pose a potential health risk for people living with diabetes.
The alert was reported by Diabetes UK, who advised: “If you use either of these sensors, you’ll need to see if your sensors are affected.”

Abbott, the company that makes the FreeStyle Libre 3 and FreeStyle
[ THERE ARE A NUMBER of serious complications linked to diabetes which, if not identified and treated, can lead to a claim for clinical negligence. Leigh Day’s medical negligence partner Julia Reynolds offered a number of examples from her own casebook.
For those who suffer with type 1 diabetes there can sometimes be a failure to recognise the symptoms, and patients can suffer diabetic ketoacidosis, which can be life-threatening if not managed correctly.
“I was instructed by the mother of a child with type 1 diabetes,” Julia Reynolds writes, “who died from diabetic ketoacidosis. Guidelines from the National Institute for Health and Care Excellence (NICE) requires immediate referral for suspected type 1 diabetes. When these guidelines are not adhered to, they can have devastating consequences for families.”
Regarding type 2 diabetes, she writes: “I have seen a number of patients with type 2 over the years who suffer life changing foot and leg injuries. About 10% of diabetics will suffer a foot ulcer at some point and 7,000 diabetes related amputations are performed each year in the UK.
“A very minor injury, such as a blister or ulcer, can become quite serious very quickly. NICE recommend that people with diabetic foot ulcers see multi-disciplinary teams to ensure any issues are treated quickly and appropriately. However, in my experience the reality is often sadly very different. The process can take weeks, allowing ulcers to progress and become necrotic. This can result in amputation – a life changing surgery that can often be avoided if they have timely medical treatment.”
She also explained what happens when gestational diabetes is mismanaged: “Gestational diabetes can develop in anyone during pregnancy – typically diagnosed between 24 and 28 weeks – and is caused by hormonal changes. There are certain risk factors, such as being overweight or obese, belonging to certain ethnic groups, family history or being over 40 years old. If gestational diabetes is diagnosed, the pregnancy should be monitored very closely to manage blood sugar.”
The consequences of mismanaging gestational diabetes can be severe, causing complications such as:
• Larger than average baby – increasing the risk of complications during labour and delivery
• Pre-eclampsia – high blood pressure in pregnancy
• Low blood sugar in newborn after birth
• Respiratory and metabolic issues in the newborn
“When a baby is larger than average, there may be a need for an induction or planned caesarean section to avoid birth injuries to both mother and baby.” q
Libre 3 Plus, is contacting people who use these sensors through their app and by email to ask them to check the serial number of their sensors. They may also be contacted by their diabetes team.
There are different ways to locate the serial number. If the sensor is still in its package, the serial number can be found on the bottom of the sensor carton packaging and on the sensor applicator label. For sensors in use or already used, the serial number can be found in the FreeStyle Libre 3 reader or app.
For those using a sensor with a connected insulin delivery device, they should refer to the connected insulin delivery device user manual on how to locate the sensor serial number.
Diabetes UK advises: “Once you have reported an affected serial number, you will then be asked to provide your contact information so Abbott can send you a replacement sensor at no extra cost. This applies whether you get your sensors on prescription or you self-fund them. If you’re wearing a sensor that has been affected, you should immediately remove the sensor and dispose of it as you usually would.
“If your sensor is affected, and you do not have a replacement, you can use the built-in meter in the FreeStyle Libre 3 reader, or an alternative blood glucose meter, to check your glucose levels while you await your replacement. You can continue to use your FreeStyle Libre 3 or FreeStyle Libre 3 Plus sensors if they are not impacted.
“If your sensor is not impacted, but your sensor readings don’t match your symptoms or expectations (such as symptoms of low or high blood sugar), then you should test your blood glucose levels using a blood glucose monitor before making treatment decisions.” q


[
MEDICO-LEGAL DISPUTES over cardiac and thoracic surgery represent some of the most demanding, technically intricate challenges in clinical litigation. Whether a case centres on coronary artery bypass grafting, valve repair or replacement, aortic aneurysm repair, thoracic oncology surgery, minimally invasive chest procedures, chest-wall reconstruction or the aftermath of major trauma, courts frequently rely on specialist surgeons to cut through the complexity.
Such experts don’t merely recount medical events – they translate dense clinical detail into objective, evidence-based opinions that help courts understand what constitutes reasonable care, accepted practice and where potential fault may lie.
Cardiac and thoracic surgery always carries risk. Even when performed to the highest standards, serious complications can occur: stroke, myocardial infarction, bleeding, graft failure, infection, respiratory collapse or arrhythmia. In litigation, the critical question typically is not whether something went wrong; it is whether the adverse outcome was a foreseeable risk that had been properly managed or rather resulted from a breach of duty, a deviation from accepted practice, omission or error.
That is where the expert witness becomes pivotal. By reviewing surgical technique, peri-operative care, post-operative management and consent documentation, the expert provides the court with the context necessary to distinguish between an inherent surgical risk and a substandard outcome that was preventable.
Advances in surgical technique bring additional complexity to medico-legal cases. Minimally invasive valve repairs, robotic-assisted thoracic operations, hybrid procedures and complex chest-wall reconstructions have not only expanded what is clinically possible – but also what could be scrutinised in court. Expert witnesses must explain what constituted the standard of care at the time of the surgery, whether the surgical choice was reasonable and defensible and whether innovation was appropriate or experimental.
When unexpected complications arise, having a credible, contemporaneous clinical benchmark is essential in evaluating whether the surgeon’s actions were within acceptable standards.
The matter rarely ends in the operating theatre. Good outcomes depend on the entire continuum of care: intensive monitoring in critical care units, appropriate anticoagulation, rigorous infection control, vigilant post-operative observation, respiratory support and timely physiotherapy. In many cases, it is systemic factors – delayed recognition of deterioration, inadequate monitoring or miscommunication between teams – rather than flawed surgical technique that determine outcome.
Expert testimony frequently adopts a multidisciplinary approach, considering anaesthesia, critical care, nursing, rehabilitation and communication failures, as well as the surgery itself, to assess causation and liability fairly.
Consent and communication with the patient are also critical. Courts carefully examine whether patients were made aware of material risks, complications and realistic alternatives before proceeding with surgery – especially when high-risk or novel procedures were proposed. Experts evaluate consent documentation and discussion notes, assess whether explanations were adequate, and consider whether the patient’s comprehension mattered in light of their condition. Poorly documented consent or insufficient explanation of risks can turn a recognised complication into a viable negligence claim.
In one High Court decision, a young adult with congenital heart disease underwent elective open-heart surgery. During the procedure, a saw slipped, damaging the aorta and causing catastrophic bleeding and prolonged cerebral hypoxia.
The court found that the surgical team had failed to obtain proper informed consent and had not adequately planned for the foreseeable risk of vascular injury. Preoperative preparation of femoral vessels for rapid cardiopulmonary bypass – a reasonable contingency – had been omitted. That failure, coupled with delayed intervention, led directly to permanent brain injury.
Expert evidence was crucial in highlighting failures in both consent and surgical planning, establishing breach of duty rather than an unavoidable complication.
Expert witnesses in cardiac and thoracic surgery litigation serve as more than medical commentators – they are interpreters between life-saving medicine and the legal system.

Their value lies in clarifying what is acceptable risk, what constitutes reasonable care, and whether a deviation has caused harm. They help courts appreciate the pressures, split-second decisions and systemic complexity that define major surgery, grounding legal judgment in medical reality rather than assumption or emotion.
As surgical practice evolves – with minimally invasive, robotic-assisted and hybrid procedures becoming more common – the role of the expert witness remains indispensable. Those with current clinical expertise, rigorous methodology and the ability to communicate clearly and impartially enable courts to navigate even the most complex cases with confidence.
In disputes where lives, livelihoods and serious injury claims hang in the balance, expert testimony ensures that fairness, clarity and justice prevail, connecting clinical complexity with informed legal outcomes. q
[THE Society for Cardiothoracic Surgery in Great Britain & Ireland (SCTS) has issued a statement to its membership addressing issues that were raised at a recent representatives meeting regarding patient safety, complex case management, consultant collaboration and teamwork. The statement was issued by the society’s president Aman S Coonar.
The statement read: “As your professional society, we reaffirm that patient safety is, and must always remain, our highest priority. Every element of our practice and culture, from the operating theatre to the ward and clinic, from training to service design, must be guided by this fundamental duty to safeguard our patients.
“At the same time, we recognise that the greatest benefits in cardiothoracic surgery are often achieved in patients with higher risk profiles or more complex needs. Our role is not to avoid these cases, but to ensure that robust systems are in place to manage them safely, consistently and transparently.”
The statement outlined seven priorities:
• Safety above all
“All decisions should be tested against one simple question: does this maximise safety and minimise avoidable harm? Efficiency and innovation are important, and they must always serve, not compromise, patient welfare.”
• Risk reduction, not risk avoidance
“Our philosophy must be risk reduction, not risk avoidance. Systems should be designed to minimise variation and eliminate single points of failure, while still enabling patients with complex disease to be offered safe surgery where the potential benefit can be greatest.”
• The role of the safety net
“Structured safety nets such as checklists, multidisciplinary team decision-making, active peer review, transparent morbidity and mortality processes, and clear escalation protocols are essential.
“These mechanisms protect patients, strengthen professional practice, and give teams more confidence to undertake high-risk or complex work within a controlled and safe environment.”
• Dual and multiple consultant operating and anaesthesia
“For high-risk or complex procedures, dual or multiple consultant operating is a proven model of care. It enhances decision-making, reduces individual cognitive and physical burden, and ensures oversight at critical phases. Mentoring and proctoring are encouraged and essential in the introduction of new procedures.”
• Organisational culture and team-working
“We are highly-trained individuals with very specialised skills working in intensely pressured situations. Healthy team dynamics relies on calm professionalism and a culture that values different opinions.


“Structures and working patterns should actively encourage collaboration and team-working across all professional groups. A culture that promotes mutual respect, shared responsibility and open communication is critical to ensuring safety, supporting learning and delivering high-quality outcomes for patients.”
• Transparency and improvement
“Continuous data collection, outcome monitoring and open discussion are fundamental to progress. Sharing results, including complications and near-miss events, is vital for collective learning and ongoing improvement. Transparency also includes shared decision making with patients, including being open with data on outcomes to allow fully informed consent.”
• The role of administration and system leadership
“While consultant surgeons and anaesthetists provide clinical direction and care, hospital administrations, commissioners and system leaders must ensure the necessary resources, staffing and organisational structures.
“This includes job planning for safe dual consultant operating, resilient rotas, protected time for audit, education, service improvement, peer review and other core safety activities.
“Job planning must be realistic, remunerated and support these essential processes. Without these sustained commitments, our profession cannot consistently deliver the standard of safety and excellence that patients deserve.”
The statement goes on to affirm that the SCTS will continue to support its members in embedding those principles to make heart, chest and lung surgery better, on behalf of patients.
“We call on administrators and healthcare leaders to provide the structures and resources required to deliver the safest and best possible care.” q

[ THE Royal College of Ophthalmologists (RCOphth) has welcomed the report by the Welsh Senedd’s Health and Social Care Committee of its inquiry into ophthalmology services in Wales – to which it contributed. The report makes far-reaching recommendations to policymakers that could help tackle challenges around workforce, estates and IT infrastructure, the RCOphth says.
The report’s key recommendations include:
• Health Education and Improvement Wales to provide the Welsh Government with an update on how it will improve the recruitment, retention and training capacity of the ophthalmic workforce, developing a professional workforce plan for ophthalmology to identify workforce needs and improve retention.
• Establishing a cross-sector oversight board for ophthalmology to monitor implementation of the National Clinical Strategy for Ophthalmology, with representation from the college.
• Record waiting list data for ophthalmology at a sub-specialty level
[
EYE-LAW CHAMBERS is one of the UK’s leading providers of specialist ophthalmic medicolegal expertise. Founded by Professor Charles Claoué over 10 years ago, the Chambers brings together a distinguished group of consultant ophthalmologists covering every major ophthalmic subspecialty, ensuring that instructing solicitors receive reports of the highest clinical accuracy, clarity and relevance.
Their experts benefit from Chambers organising on-boarding, marketing and invoicing, thus taking all the administrative burden away from them. This frees up time for both medicolegal and clinical work.
The team encompasses recognised expertise across the full spectrum of eye-related medicolegal work, including personal injury, medical negligence, criminal and employment tribunal cases.
With specialists in paediatrics, cornea and anterior segment, refractive surgery and laser vision correction, glaucoma, retina (medical and surgical), oculoplastics and general ophthalmology, EYE-LAW CHAMBERS is uniquely positioned to handle cases ranging from the straightforward to the exceptionally complex. This means that solicitors have access to experts in precisely the right areas for their cases.
The Chambers recognise the pressures faced within the legal system and the importance of timely, well-reasoned expert evidence. To support this, they operate with a four-week standard turnaround for reports, complemented by two fast-track options for more urgent matters: a five-working-day service and an enhanced premium service delivering reports within two working days. They also offer domiciliary visits for claimants who are unable to travel.
Every report is prepared by a consultant actively practising within their subspecialty – they are all in active clinical practice, ensuring insight grounded in contemporary clinical practice. All experts combine academic credibility, surgical experience and clear, decisive communication; qualities essential for instructing parties seeking robust, court-ready evidence. q
• For enquiries or to discuss a case, please contact our dedicated medicolegal coordinator, Ms Nadia Bouras, on 0208 852 8522 or eyes@dbcg.co.uk. Further information is available at www.eyelawchambers.com
so that service planning can be better aligned to patient need.
• Report on the progress of making OpenEyes, the electronic health record system, accessible across all parts of the eye care sector by the target date of March 2026.
The recommendations reflect many of the key issues raised by the college in its written evidence, and through the evidence its Llywydd (Presiding Officer), Rhianon Reynolds, gave in-person to the committee in March.
Commenting on the report, Rhianon Reynolds said: “It is really positive that the committee has listened to our evidence and has made important recommendations to help tackle the serious issues facing ophthalmology services in Wales. Underpinning this is the effective implementation of the National Clinical Strategy for Ophthalmology.
“The onus is now on the Welsh Government to implement the recommendations. We look forward to working with policymakers to do that, and ultimately ensure patients have better access to services and we cut waiting lists and reduce avoidable sight loss.” q
[THE College of Optometrists and Association of Optometrists are urging all drivers to ensure they have regular eye tests to check their vision still meets UK driving standards.
Routine eye tests, recommended every two years or as advised by your optometrist, are vital to maintaining good eye health and helping to keep all road users safe. Many common conditions, including glaucoma, cataracts and diabetic retinopathy, can progress silently in the early stages, meaning drivers may not realise their eyesight has deteriorated.

With an ageing population, the number of people living with common eye diseases that can impact drivers’ vision is set to increase over the coming decade. In particular, the number of people with glaucoma is forecast to increase by 10% over the next five years, with more than one million people in the UK expected to be living with the condition by 2030.
The number of people diagnosed with diabetic retinopathy is also projected to rise by more than 25,000 between 2025 and 2030 to over one million people: a 2.5% increase.
Drivers are reminded that they must meet the legal eyesight standard for driving and inform the Driver and Vehicle Licensing Agency (DVLA) if they have certain eye conditions.
Daniel Hardiman-McCartney MBE, clinical adviser at the College of Optometrists, explained: “Conditions like glaucoma and diabetic retinopathy can develop gradually and without obvious symptoms at first. Booking an eye test is one of the simplest and most effective actions drivers can take to see safely when driving. Your optometrist can help ensure your vision meets the required standard and that any problems are identified early, when treatment is most effective.”
Dr Peter Hampson, clinical and policy director at the Association of Optometrists, added: “We know that regular eye tests play a vital role in keeping drivers safe on the road for longer Having that routine check can keep eyes healthy and help protect drivers vision from sight threatening conditions that sometimes simply don’t present with obvious symptoms.
“Early detection of issues like glaucoma, cataracts or retinal disease allows for timely treatment that can preserve vision for many years, and by maintaining good eye health drivers can stay confident and independent.” q

[CATARACT SURGERY is one of the most commonly performed operations worldwide, restoring vision and quality of life for millions of patients each year. Despite its routine reputation, the procedure carries inherent risks and complications which, though uncommon, can have serious, life-altering consequences.
This is where expert witnesses play a critical role. Ophthalmic specialists provide courts and legal teams with impartial, evidence-based insight, helping to determine whether poor outcomes were an unfortunate risk or the result of negligence.

A medicolegal expert witness in ophthalmology is typically a consultant surgeon with extensive experience in cataract procedures. Their task is to translate complex clinical facts into clear, legally relevant analysis. In doing so, they review surgical records, consent forms, preoperative assessments, postoperative notes and imaging – assessing whether the care provided met the standard expected of a competent ophthalmic surgeon.
Expert evidence is often required when there are intraoperative complications such as posterior capsule rupture, vitreous loss or lens placement errors; and with post-operative complications such as infection, retinal detachment, lens dislocation or chronic inflammation. Issues around informed consent or postoperative care may also have contributed to harm.
Even though cataract surgery is generally successful – with over 95% of patients achieving improved vision without serious issues – complications do occur. One of the most serious is posterior capsule rupture, in which a tear in the lens capsule can lead to vitreous loss, retinal detachment or infection. While uncommon, posterior capsule rupture can have devastating consequences if not properly managed.
Experts examine whether such complications were foreseeable and whether the surgeon took reasonable precautions. The mere occurrence of a complication does not automatically indicate negligence, making expert analysis essential in distinguishing accepted risk from substandard care.
Informed consent is another area where expert opinion is critical. Surgeons must ensure that patients are fully aware of the risks, benefits and alternatives to surgery. If a patient was not adequately counselled –particularly if they had additional risk factors such as dense cataracts, prior ocular disease or small pupils – and a serious complication occurs, that can form the basis of a negligence claim. Postoperative care is equally important. Prompt recognition of complications such as elevated intraocular pressure, infection or lens instability can prevent permanent vision loss. Experts evaluate whether follow-up protocols, patient instructions and interventions met professional standards, helping the court understand where care may have fallen short.
A recent UK case illustrates how expert witnesses can be decisive. A patient scheduled for cataract surgery under general anaesthetic underwent the procedure under local anaesthetic instead. During surgery, the posterior capsule ruptured, no lens was implanted and retained lens fragments caused significant vision loss.
Ophthalmic experts concluded that if general anaesthesia had been used as planned, the surgery would likely have been uncomplicated. Their evidence established that deviations in anaesthetic choice and surgical technique directly caused the poor outcome, resulting in a successful settlement. This example demonstrates how experts clarify the standard of care, identify where deviations occurred and determine whether those deviations caused harm.
Expert evidence in cataract litigation transforms complex medical detail into accessible legal testimony. It ensures that courts can differentiate between known risks and lapses in care, and it provides a structured, objective assessment of causation. By combining clinical expertise with impartial communication, ophthalmic experts play a pivotal role in guiding courts toward fair and informed outcomes.
In cataract surgery claims, expert witnesses do more than illuminate technical facts; they often define the course and outcome of the case. Their input ensures that justice is informed by rigorous clinical understanding, not conjecture or emotion, highlighting the indispensable role of expert eyes in navigating the complexities of modern ophthalmic care. q
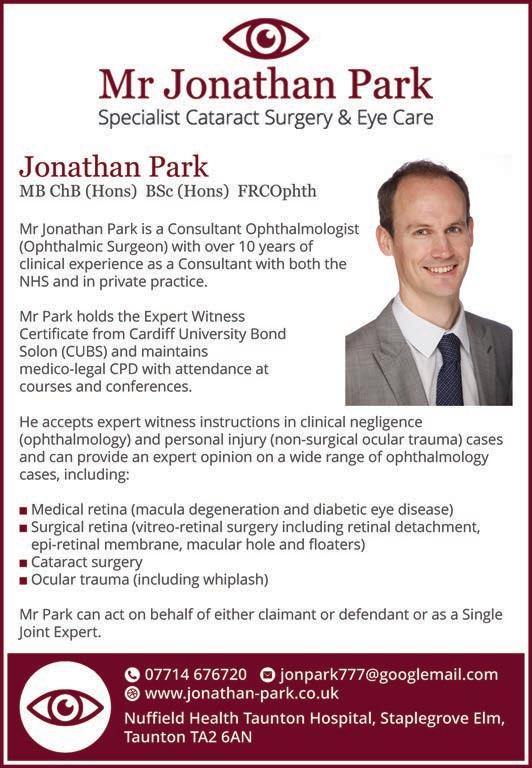
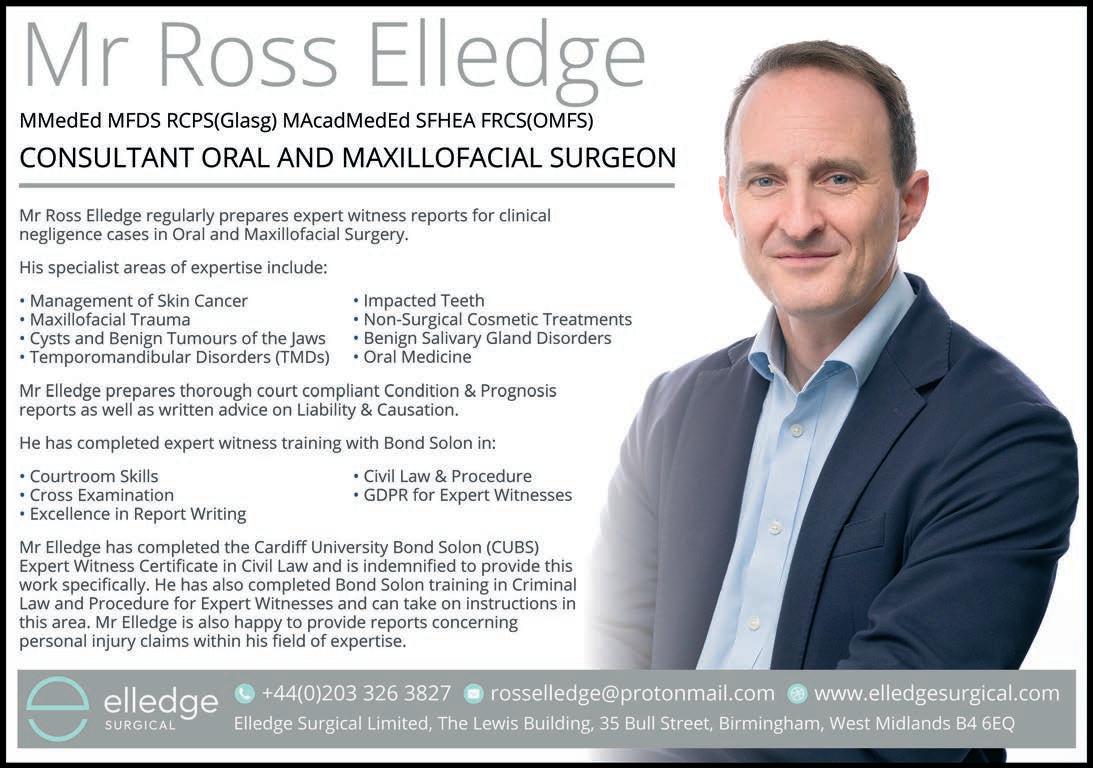
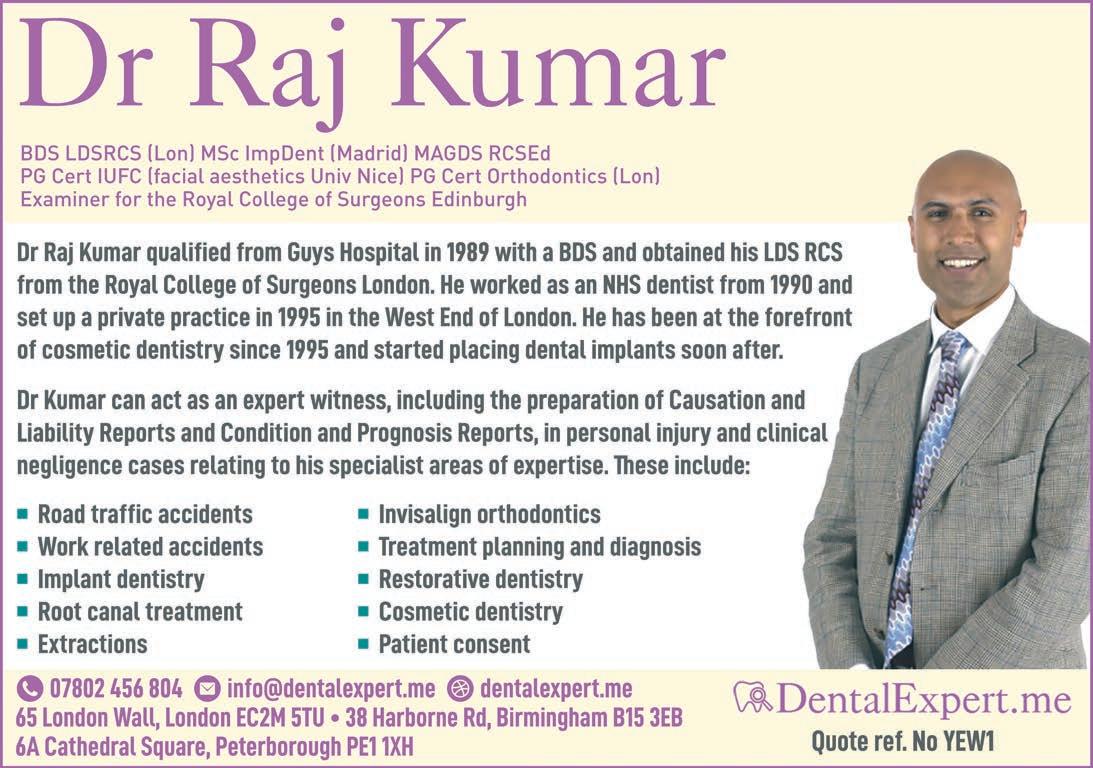
[THE BRITISH DENTAL ASSOCIATION (BDA) has hit out at Chancellor Rachel Reeves over her letter to the Competition and Markets Authority (CMA) urging it to launch an investigation into the pricing of private dentistry, saying: “We are determined to fight the corner for this profession.”
In the letter Rachel Reeves said: "…the scourge of hidden costs, lack of transparency and overtreatment has blighted families in need of dental treatment for too long. That’s why I want to see urgent action taken to help reduce prices, whilst the cost of living still puts pressure on families across the country.”
In response, the BDA says: “Private practices have had to cover significant increases in overheads following the Chancellor's first budget, with surging costs across the piece. Over the last four years we estimate private fees have increased at an average of 13.8% – when costs of delivering care have increased by as much in a single year. Cumulative inflation for the period 2021 to date stands at 24.5%.
“Private dentistry is never one size fits all, and there is clearly no scope for a ‘national tariff’. The reality is private dentistry
needs to operate to market forces, with prices that cover the costs of delivering treatment, often using techniques and materials unavailable on the NHS.
“A generation of savage cuts have left typical NHS practices delivering treatments like dentures and bridges at a financial loss. We told the Public Accounts Committee earlier this year that lossmaking NHS services were being kept afloat by a cross subsidy from private work of over £330m.”
The BDA’s chair Eddie Crouch commented: “This call for an investigation is utterly perverse. The Chancellor is singling out private dentists for doing what any business does: covering their costs, some of which are of the Chancellor's own making.
“At the same time, she’s very happy to starve NHS services of vital funding. We’d remind her that profits from private care are all that are keeping NHS dentistry afloat.”
The association says it has already written to the watchdog and will be closely monitoring developments.
“We will speak up for the many thousands of dentists in both private and mixed practice delivering high-quality care.” q
[ ON 18 NOVEMBER the General Dental Council (GDC) published its new strategy for 2026-2028, committing to significant change and improvement over the next three years – and towards 2030.
Announcing the launch of the document, the GDC said: “Our vision is to be a trusted and effective regulator, supporting dental professionals to provide safe and effective care for their patients. To do this, we will champion a model of regulation that supports professionalism, enables learning, and resolves issues quickly and proportionately.”
Central to the new approach is a commitment to tackling the climate of fear in dentistry, recognising that fear of fitness to practise (FtP) proceedings can impact on dental professionals’ mental health and wellbeing – ultimately impacting on patient access and care.
Tom Whiting, chief executive and registrar at the GDC, said: “We want to regulate in a way that promotes learning over fear –supporting the dental team to demonstrate professionalism. We want to provide regulation that fits the times we're in, anticipates future changes and tackles shared challenges.
“We want people to feel that we are easy to deal with, approachable and ready to listen and support. We will be transparent about our progress and performance, reporting regularly and keeping an open dialogue about what we are doing to build trust and effectiveness.”
A key aspect of the new strategy is to build an organisation that acts in line with the GDC’s values: respectful, transparent, inclusive and purposeful. The strategy responds to real challenges facing dentistry, including the strain on dental services, growing demand for international registration routes and outdated legislation. Key initiatives include:
• Doubling the number of dentists joining the register each year via the Overseas Registration Examination and developing new frameworks for international registration, including exploring mutual recognition of qualifications.
• Closing FtP cases earlier through less adversarial methods such as remediation, to reduce the punitive effect and stress on all parties involved.

• Launching a digital-first registration service in early 2026 to simplify applications and tracking progress.
GDC chair Dr Helen Phillips said: "Our strategy is very consciously titled ‘trusted and effective’. This is what we aim to be and how we want your experience of us to feel. It is different and ambitious.
“The council is determined to be recognised as a regulator that operates with greater effectiveness and works collaboratively as a valued partner. I am committed to nurturing relationships built on trust, using these to listen and learn so we support dental professionals to provide safe and effective care to patients.” q



By Dr Martin Stotz, consultant in intensive care and anaesthesia
[ MANY PATIENTS develop complications due to the physiological and inflammatory changes associated with surgery. Postoperative complications are one of the leading causes of patient mortality, leading to over three million deaths each year. Therefore, measures to prevent, identify and treat potentially fatal complications arising during the postoperative period are vital.
Consequently, admission of high-risk surgical patients to the intensive care unit (ICU) is often regarded as essential to minimise the risk of mortality. Around 10% of patients are at a higher risk of experiencing complications; but identifying those who would benefit from admission to the ICU remains a challenge.
For low-risk surgical patients, admission to the ICU makes little difference to the already low mortality rates experienced by that group. Instead, monitoring systems outside the ICU, coupled with rapid response teams, may be sufficient to identify complications. Some of those will be related to the patient’s comorbidities, such as heart failure, diabetes and chronic obstructive pulmonary disease, rather than the surgery itself, and so may be more predictable.
For patients undergoing high-risk operations, more precise management of fluid administration, haemodynamic balance, bleeding and coagulation control and pain management may be required, along with early detection of infection and prevention of venous thromboembolism and postoperative respiratory failure.

Infections are one of the commonest postoperative complications, affecting between 1% and 26% of patients. They may be superficial, affecting just the skin and subcutaneous tissue surrounding the surgical incision, or deeper, involving the fascia and muscle layers. Deep-seated infections can be difficult to treat and may require repeat surgery and a prolonged hospital stay. They can also lead to the death of the patient.
Venous thromboembolism (VTE) is a frequent and serious complication experienced by around 25% of patients after surgery. Pulmonary thromboembolism (PE) is much less common, occurring in around 1.6% of patients. Based on clinical factors, patients can be categorised according to their risk of VTE/PE but prophylactic measures are sometimes withheld due to a fear of excessive bleeding. Compression stockings are a safe and effective preventative measure, together with automatic calf compression devices; and the risk of VTE is also reduced by the administration of low molecular weight heparin and fondaparinux.

Enhanced Recovery After Surgery is a multimodal approach in which postoperative measures aim to reduce and proactively treat the response to surgical stress and speed patient recovery. The four key elements of that approach are comprehensive preoperative evaluation of the patient, optimum anaesthesia and minimally invasive surgery – with the aim of reducing patient response to surgical stress – adequate postoperative management of symptoms such as pain to allow early mobilisation, and prompt reintroduction of an adequate diet.
Postoperative monitoring of vital signs should be carried out in all patients, but for those with cardiovascular or respiratory comorbidities the use of semi-invasive monitoring – including pulse wave analysis, variations in systolic volume, transthoracic bioimpedance or oesophageal Doppler ultrasound – may be considered. Adequate pain relief is essential for early mobilisation, but can be difficult to monitor in patients who are not able to communicate.
When body tissues are injured, they release catabolic hormones and inflammatory mediators that encourage salt and water retention, so that circulating volume, blood pressure and vasoconstriction are all maintained. Therefore, patient fluid balance should be adequately preserved. Failure to do so can result in postoperative complications and an extended hospital stay.
Although it is recognised that a moderately liberal fluid intake is safer than a restrictive regimen, the amount required by each patient varies according to the type of surgery, blood loss and comorbidities. Initially, the aim should be to replace lost fluids and achieve a normal circulating volume. That is followed by a maintenance period wherein fluid therapy is lowered once the patient resumes normal oral intake.
Around 5% of patients undergoing noncardiac surgery will suffer a myocardial infarction, with around three-quarters of those occurring in the first 48 hours after surgery. Many affected patients do not show clinical signs; therefore, for patients at high risk, or who have a history of cardiovascular events, monitoring of troponin levels may be indicated. Acute ischaemic events – heart attack – may lead to heart failure, which may also be caused by inadequate fluid management, acute kidney or lung injury, or sepsis. Atrial fibrillation is also relatively common post-surgery and, again, many patients are asymptomatic. It may be caused by tissue trauma and pain-related catecholamine release, hypoxia or electrolyte disturbance.
Delirium occurs in over one-third of patients admitted to the ICU after surgery, although it is often underdiagnosed; so the incidence may be considerably higher. The presence of delirium is known to increase risk of mortality and the need for re-admission to hospital, and lengthens hospital stay. It also increases the likelihood of the patient developing post-intensive care syndrome (PICS): a constellation of physical, psychological and cognitive disorders that affect daily functioning and quality of life in survivors of critical illness.
Patients with PICS experience loss of muscle mass and function, persistent pain, fatigue and sleep disorders, anxiety, depression and post-traumatic stress symptoms, together with impaired memory, executive function and mental processing. PICS is extremely heterogeneous and the exact symptoms, and their intensity and duration, vary from patient to patient. As the risk of PICS can be mitigated by following the approach outlined in the Enhanced Recovery After Surgery regimen, that should always be adopted. q
• Dr Martin Stotz is the Airway Lead at St Mary’s Hospital, London – part of the Imperial College NHS Trust – where he leads a multidisciplinary team. St Mary’s is a major trauma centre and a tertiary vascular referral centre. Dr Stotz is an experienced expert witness, providing expert opinion on most aspects of anaesthesia, the care and management of patients pre, during and postoperatively, and the clinical management of critically ill patients
[IN ITS AUTUMN BUDGET the government has taken some positive steps to bolster the NHS, but the Budget doesn’t offer anything to address extremely long waiting times and so called ‘corridor care’ in Emergency Departments (EDs). That’s the message from the Royal College of Emergency Medicine (RCEM), in response to Chancellor Rachel Reeves’s statement on 26 November.
EDs are under extreme pressure, with additional stresses to come over winter. The emergency care system is in dire need of support from the government to continue providing safe and effective care, the RCEM says.
Its president Dr Ian Higginson commented: “Patients on trolleys in Emergency Department corridors have been forgotten in the Autumn Budget. It states the government is committed to protecting and strengthening the NHS. But this must include emergency care –something which hasn’t been mentioned a single time in the document.
“While we welcome any move to improve care in the community, as well as driving down waiting lists for planned care, patients needing emergency care must not be forgotten about. We cannot fix the health service without fixing one of the most important parts.
“Patients will still come through our doors, and the sickest and most vulnerable are more likely to wait incredibly long hours, often in trolleys in corridors and other inappropriate spaces. Long waits are degrading and dangerous for patients, and they are associated with excess deaths. Surely that’s worth investing in?
“Last month over 164,800 patients in England alone endured a wait of 12 hours or more to be admitted, discharged or transferred from major EDs. Last year 1,731,737 patients did. This is beyond unacceptable and is happening because the system is in crisis.
“Politicians must make sure there is still enough effort made towards improving patient safety and prevent skilled staff, who are fed up with the lack of investment and action, from leaving the profession.
“We are deeply concerned about the state of our EDs heading into winter and are left with little confidence that we can provide the high standard of care our patients deserve. With each successive failure to act by the government our confidence falls even further.
“RCEM urges the government to bear in mind how essential urgent and emergency care is to all our communities – now and into the future. Those of our members and their colleagues who are left standing will always be there for our patients – 24 hours a day, seven days a week; but they should be supported by the government in this.”
The statement followed the publication of figures which showed that, in Wales alone in October, 10,493 people waited more than 12 hours before being admitted, discharged or transferred: another record month. That is equivalent to one in every seven people enduring such an unacceptably long wait in a Welsh ED – an increase of 4% compared to last October, despite attendances only rising by 1.8%. The RCEM described the figure as ‘dismaying’ and demanded more support from policymakers.
Dr Rob Perry, RCEM vice president for Wales, said: “It is dismaying to see yet another worst month on record. With temperatures already starting to drop, today’s data is a reminder – if one was even needed –that politicians should listen to the alarm bells ringing from every ED in the country.
“Thousands of people – loved ones seeking help – found themselves waiting on trolleys or chairs for hours on end, in conditions we know put them at risk of further harm. This cannot continue.
“Meanwhile, our staff are working themselves to the bone to try and keep their patients safe. But without action from government, this will get harder and harder.
“This has been our reality all year, even in the warmer months when

we are supposed to get some respite. The winter surge is about to start, and I fear we are not ready for what’s to come.
“Minor improvements compared to September are welcome, but they are but a drop in the ocean compared to what we need to be seeing in order to escape the spiral we find ourselves in.
“The Welsh government must continue to address delayed discharges and flow. Its recent announcement of funding for social care was a good first step – but we need sustained support. EM staff will step up for their patients this winter. We will get through this, but, I fear, at what cost?” q
ACCIDENT & EMERGENCY MEDICINE


CARDIOLOGISTS & CARDIOTHORACIC SURGEONS


DENTAL & ORTHODONTIC EXPERTS






GASTROINTESTINAL & COLORECTAL SURGEONS
GENERAL SURGEONS

HAEMATOLOGY

MEDICAL NEGLIGENCE

NEUROLOGY

NEUROSURGEONS



















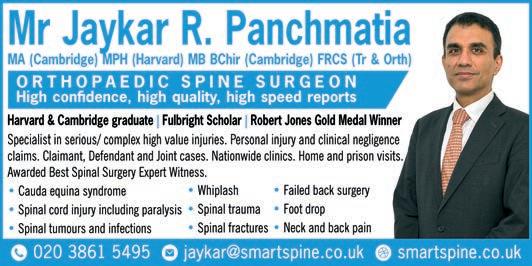

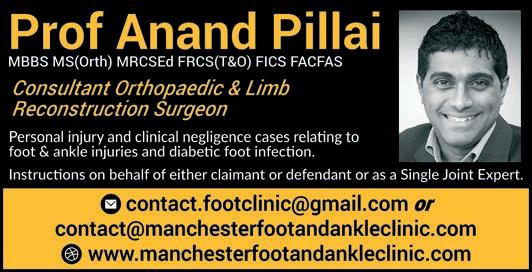

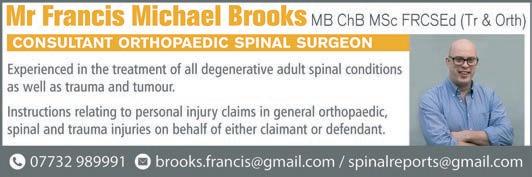
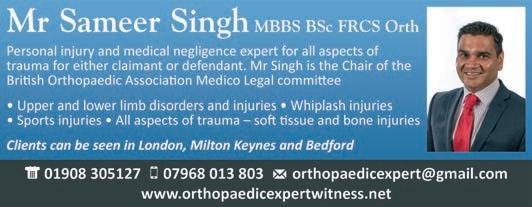











RADIOLOGISTS

SKIN CAMOUFLAGE CONSULTANTS

SPEECH & LANGUAGE THERAPY

THORACIC SURGEONS




VASCULAR SURGEONS

EXPERTS FOR MEDIA is a regular section in Your Expert Witness for experts who wish to offer their views and the benefit of their experience to the vast range of print and broadcast media.
Ever wondered how news teams find the experts they consult to explain the ramifications of breaking news stories, seemingly at the drop of a hat? Or how the producers of TV drama series ensure their stories are accurate and reflect the realities of the professions they portray?
The fact is that researchers consult registers of experts and expert periodicals just as lawyers do. In fact, Your Expert Witness is receiving an increasing number of enquiries from media researchers and public relations agencies looking to locate appropriate experts to inform their clients.
Experts for Media is therefore an ideal space to attract their attention. For prices and to book your space, contact Ian on 0161 710 3880 or via ian@dmmonline.co.uk .
Joanne Caffrey Expert Witness & Trainer
Ms Joanne Caffrey undertakes expert witness instructions in cases relating to the following police topics:
• Use of force
• Custody procedures
• Drink/drug driving
• Ligature deaths
T: 07528 800 720 E: joanne_caffrey@sky.com

Professor Paul J Ciclitira MB PhD FRCP MRCS FRCP AGAF Professor of Gastroenterology

Professor Ciclitira has a particular interest in food allergy, including Coeliac disease, peptic ulcer, inflammatory bowel disorder, hepatology and general internal medicine. He undertakes expert witness instructions in cases relating to all of these conditions, acting on behalf of either claimant or defendant or as a Single Joint Expert.
T: 0207 603 3594 E: gastropjc@gmail.com W: www.profpaulciclitira.co.uk
Mr Jeremy Crew MA MD BChir(Cantab) FRCS(Urol) Consultant Urological Surgeon

Mr Jeremy Crew has offered a medicolegal service for over sixteen years. He provides expert medical opinion, medico-legal reports and court attendance on all aspects of urology including clinical negligence, personal injury and criminal matters.
T: 01865 307433 or 07508 617949 E: jeremycrew@urologyoxford.com W: www.oxfordurology.co.uk


Dr Dan Jones
PhD MSc BSc MA MEWI Cert Ecological Consultant - Japanese Knotweed
Dr Dan Jones undertakes expert witness instructions, including the preparation of expert reports and giving evidence in court, in civil claims relating to the growth and spread of all invasive plants. He can act on behalf of either claimant or defendant or as a Single Joint Expert.
T: 07967 408844 E: daniel@advancedinvasives.com W: www.advancedinvasives.com
Laird Assessors Automotive Expert

Mr Robert Marston BSc(Hons) MBBS FRCS(Eng) FRCS(Edin) FRCS(ORTHO) Consultant Orthopaedic and Trauma Surgeon

Mr Marston has 25 years experience as an expert witness. His special interest is lower limb orthopaedics and trauma, particularly hip and knee arthroplasty, joint injuries and fractures. His main medico legal work is with alleged clinical negligence. He also takes on selected personal injury cases.
T: 07464 425 444 E: marstonmedicolegal@gmail.com W: www.marstonmedicalpractice.co.uk

Laird Assessors are the UK’s leading independent automotive expert witness firm supporting claimant, defendant and criminal solicitors – from instruction to court. Laird provide intelligence to the automotive world predominantly relating to crashed vehicles.
T: 0151 342 9961 E: enquiries@laird-assessors.com W: www.laird-assessors.com
Mr Jonathan Luck
FRCS FRCOphth Consultant Ophthalmologist
Mr Jonathan Luck has over 20 years of experience in medicolegal work. Experience of giving evidence in court including cross examination. Rapid turnaround of reports. Full consulting and diagnostic facility for Condition and Prognosis reports. Holder of the Bond Solon Cardiff University Civil Expert Witness Certificate.

E: jon.luck@nhs.net W: www.jonathanluckmedicolegal.org.uk
Chris Makin FCA FCMI FAE QDR MCIArb
Chartered Accountant • Accredited Civil Mediator
• Accredited Expert Determiner
Chris Makin was one of the first chartered accountants to become an Accredited Forensic Accountant and Expert Witness. He is also an accredited civil and commercial mediator and an accredited expert determiner. Over the last 30 years he has given expert evidence at least 100 times and worked on a vast range of cases.
T: 01924 495888 or 07887 660072 E: chris@chrismakin.co.uk W: www.chrismakin.co.uk

Mr Luke Meleagros BSc MBBS MD FRCS Consultant Surgeon
Mr Meleagros Completes 3-4 expert reports per month on medical negligence cases and abdominal injury/major abdominal trauma cases. He has reported extensively on cases involving abdominal laparoscopy surgery and hernia surgery.
T: 0208 527 0977 E: L.Meleagros@btinternet.com Sec: jawdobson@gmail.com

RSK
Materials and Structures
RSK offers impartial specialist materials and structures expertise in support of legal matters. Our team of consultants can act as expert witnesses on behalf of either claimant or defendant or as a Single Joint Expert in a range of construction disputes.

T: 01442 437500 E: info2@rsk.co.uk W: www.rskgroup.com
Kathryn Thorndycraft-Pope Examination of Documents and Handwriting

FHDI provides an independent document examination service, giving unbiased professional advice for criminal or civil litigation.
• Handwriting • Alterations • Indentations • Authenticity
T: 01569 764508 M: 07710 655838 E: fhdi@icloud.com W: www.forensichandwriting.co.uk