Living Well With Diabetes











The following resources can help you and the people close to you learn more about living a healthier life with diabetes.
American Diabetes Association www.diabetes.org
American Heart Association www.heart.org
Academy of Nutrition and Dietetics www.eatright.org
Centers for Disease Control and Prevention www.cdc.gov/diabetes
National Diabetes Education Program www.ndep.nih.gov
National Diabetes Information Clearinghouse www.diabetes.niddk.nih.gov
USDA MyPlate www.choosemyplate.gov smokefree.gov
American Lung Association www.lung.org http://betobaccofree.hhs.gov/ CDC www.cdc.gov/tobacco/quit_smoking/
American Cancer Society www.cancer.org

The groups listed on this page are only a few of many online resources. You can search for other sites using keywords on a specific topic, such as “A1C” or “insulin.” If you don’t have Internet access at home, many public libraries let you search online for free. Write the addresses (URLs) of your favorite sites here: www.diabetes.org/living

You’ve been given this workbook because you have diabetes. Diabetes is a chronic (lifelong) condition. Without treatment, it can result in serious health problems, including blindness, lower-limb amputation, heart disease, and stroke. But you can learn to manage diabetes. This workbook will help you understand what diabetes is and how it affects your health. It will also help you make daily decisions to manage your diabetes. Read on to find tips and tools you can use to live well with diabetes.
When you have diabetes, the glucose (sugar) level in your blood can become too high. (See page 8 to learn how this happens.) Over time, high blood glucose causes health problems, including damage to the heart, kidneys, eyes, and feet.
There is a way to keep track of how you’re managing diabetes and its complications, however. It’s called the ABC method: A for the A1C test, B for blood pressure, and C for cholesterol. By controlling your blood glucose, blood pressure, and cholesterol, you can better manage diabetes and reduce the risk of complications.
Anyone can develop diabetes. It can affect people of all ages and backgrounds. But there are some common risk factors for diabetes. These include:

• Family history of diabetes
• Lack of physical activity
• Being overweight
• Being over age 45
• Being African-American, Native American, Latino, Asian-American, Asian, Indian, or Pacific Islander
• History of gestational diabetes
The American Diabetes Association (ADA) gives target goals for blood glucose and blood pressure. Keep in mind that your goal numbers may be different. Talk to your health care provider about what your numbers should be. Then work together to fill out the Health Goals chart on page 61.
Blood glucose
A1C*
Pre-meal blood glucose
Post-meal blood glucose
Blood pressure
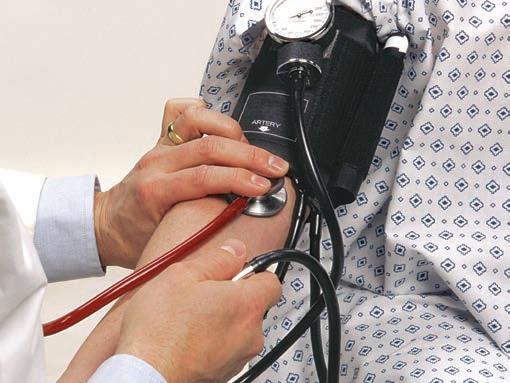
A test that checks the force of blood flow through vessels
LDL (“bad” cholesterol)
HDL (“good” cholesterol)
Triglycerides
<7%
80–130 mg/dL
<180 mg/dL
Postmeal glucose measurements should be made 1–2 hours after the beginning of the meal.
<140/90 mm Hg
A general goal for blood pressure of <140/90 mm Hg is appropriate for many adults with diabetes. A lower blood pressure target may be appropriate for some patients. Ask your health care provider about the blood pressure target that is right for you.
Cholesterol goals for LDL, HDL, and triglycerides are not the same for every patient with diabetes. Ask your health care provider about the cholesterol target that is right for you. If you have diabetes, you should have your cholesterol checked at the time of diagnosis, and every 5 years after that—or more often, if recommended by your health care provider.
*The general goal of <7% appears reasonable for many adults with diabetes. More or less stringent A1C goals may be appropriate for other patients.
Look for the following throughout the workbook:
Notes for Family and Friends: This appears in places that have advice for family members and friends of people with diabetes.
Tool Kit: You can find full-size charts for your own use in chapter 7 of the workbook.
Checkboxes and Fill-Ins: This is where you can write in your own goals and management plans.
Living with a chronic condition can be a challenge. Everyday life can distract you from diabetes management. But managing your diabetes is important. You don’t have to go it alone. You can work with health care providers who can support and advise you in creating a management plan that is best for you. Remember, you’re the expert on you. Make sure your plan is one that works for you.
This book is not homework. It’s full of tools to help you create a diabetes management plan you can stick with. Start by learning how eating healthy, being active, and taking medications as prescribed, if needed, can help you control your blood glucose, blood pressure, and cholesterol. Then use the tools you can download from this guide to write down your management plan and blood glucose, blood pressure, and cholesterol goals. Doing this will help you stay on top of your health. Keep this book handy so you can refer to it whenever you need to.

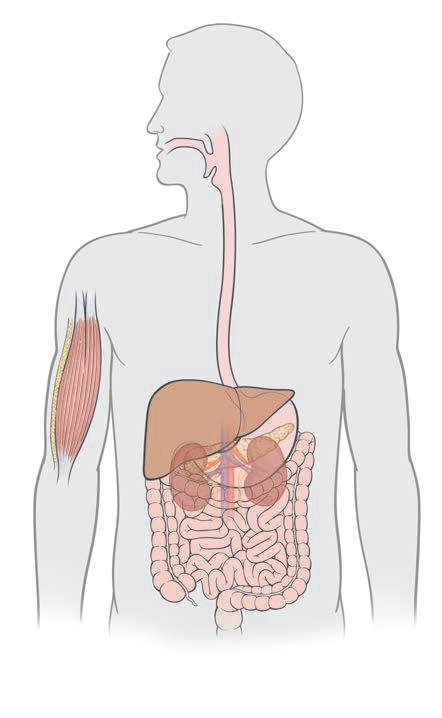
The body digests the food you eat to use as fuel. This fuel supplies energy to your body’s cells. When you have type 2 diabetes, the fuel has a hard time entering most cells.
The digestive system breaks down food, resulting in a variety of nutrients including sugar (glucose). Some of the glucose is stored in the liver. Most of it enters the bloodstream and travels to cells to be used as fuel. Glucose needs the help of a hormone called insulin to enter most cells. Insulin is made in the pancreas. It is released into the bloodstream in response to meals and also by the presence of glucose in the blood. Think of insulin as a key. When insulin reaches a cell, it unlocks a doorway in the cell wall. This creates an opening that allows glucose to enter the cell. Some cells do not need insulin and glucose can enter them without it.
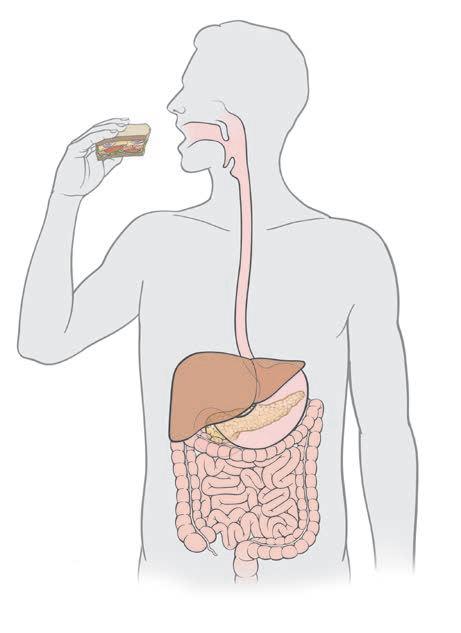
Your body breaks down the food you eat into glucose and other nutrients.
A healthy balance of insulin and glucose circulates in the bloodstream.
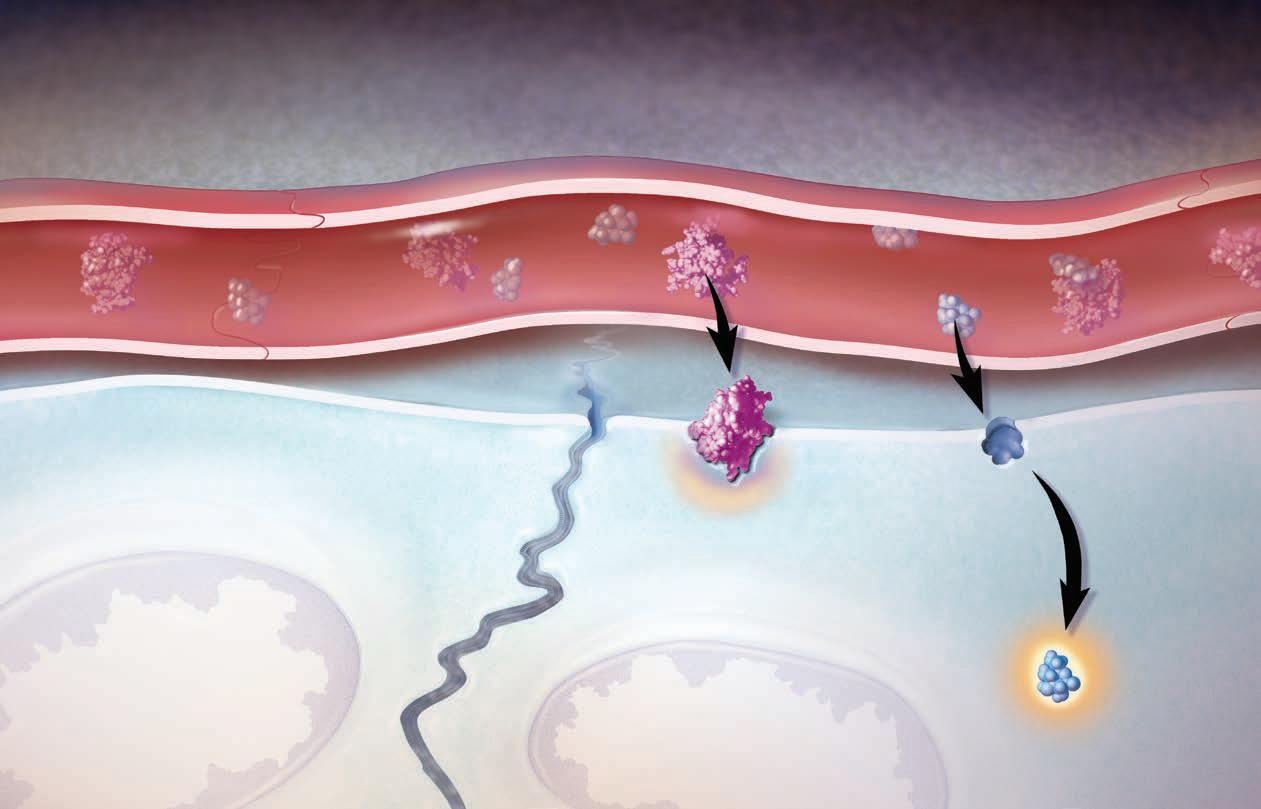
With type 2 diabetes, your body may not make enough insulin, and/or may not use insulin the right way. This means that glucose has trouble entering most cells. If it can’t enter the cells, glucose builds up to a harmful level in the bloodstream. This is called high blood glucose (hyperglycemia). There are two types of diabetes. Both are discussed below.

When you have type 1 diabetes, the pancreas is usually not making any insulin at all. Type 1 diabetes most often develops in children. But people at any age can also get it. People with type 1 must take insulin every day.
When you have type 2 diabetes, your cells do not respond to insulin the way they should. This is called insulin resistance. The pancreas may try to overcome resistance by making more insulin. But, over time, the pancreas may not be able to provide enough insulin. People with type 2 diabetes may also need to take insulin. (But taking insulin does not mean that type 2 has become type 1.)
Over time, high blood glucose damages your blood vessels, both large and small. This damage can lead to complications that affect the whole body. Complications include heart attack, stroke, kidney disease, vision problems, blindness, nervous system problems, and risk of lower-limb loss (amputation). But, by controlling your blood glucose, blood pressure, and cholesterol according to your treatment plan, you can help reduce your risk of complications.
Brain
Stroke
Heart Heart attack
Female reproductive organs
Vaginal dryness
Nerves
Nerve damage (neuropathy)

Eyes
Eye disease (retinopathy)
Kidneys
Kidney problems (nephropathy)
Male reproductive organs
Erectile dysfunction (ED)
Legs and feet
Peripheral arterial disease (PAD)
Over time, diabetes can lead to cardiovascular (heart and blood vessel) disease, including heart attack and stroke. People with long-term very high blood glucose are especially at risk. High blood pressure and high cholesterol are conditions that also increase your risk of artery damage. The risk is even greater when combined with high blood glucose.
High blood pressure also raises your risk for eye problems and kidney disease. High blood pressure makes your heart work harder than it should. Your cholesterol numbers tell you about the amount of cholesterol, a fat-like substance, in your blood. Some kinds, like HDL cholesterol, help protect your heart. Others, like LDL cholesterol, can clog your arteries. High triglycerides raise your risk for a heart attack or a stroke.
Elevated levels of glucose in the blood affects the lining of artery walls. (An artery is a type of blood vessel. A vein is another type.) Arteries carry blood from the heart to the rest of the body. When arteries are healthy, the lining is smooth. But when you have diabetes, the artery lining becomes damaged over time by high blood glucose, high blood pressure, and cholesterol. This allows the buildup of plaque (fatty materials, such as cholesterol) in the arteries. Cigarette smoking can also damage the artery lining. People with diabetes who smoke have a higher risk for that damage than those who do not.
The buildup of plaque narrows arteries. This means that any blockage, such as a blood clot, can cut off blood flow. When this happens, heart attack or stroke can occur. Many people with diabetes need to control their blood pressure and/or cholesterol. By not smoking and controlling your blood glucose, blood pressure, and cholesterol, you can help reduce the risk of these problems.
If you smoke, quitting smoking is one of the most important changes you can make for your health. Talk with your health care provider about ways to stop smoking. Together, you can make a plan to quit. Quitting may be hard and take some time. But, the potential health benefits are worth it.
Smooth lining
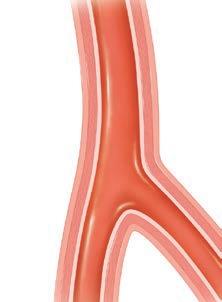
When the lining is smooth, blood flows easily through the arteries.
Damaged lining
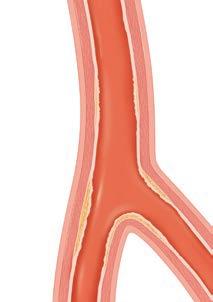
Over time, high blood glucose damages the lining.
Plaque
Blood clot
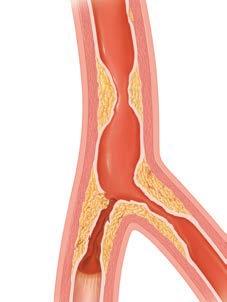
Plaque builds up in the artery walls, making it hard for blood to get through.
Controlling blood glucose, blood pressure, and cholesterol can help reduce the risk of long-term complications of diabetes. Talk to your health care provider to learn more, and keep track of your blood pressure and cholesterol levels with the charts on page 65.
Diabetes is itself a risk factor for heart disease and stroke. Heart attack and stroke affect people with diabetes more than twice as often as people without diabetes.
In fact, two out of three people with diabetes die from heart disease or stroke, which are together called cardiovascular disease. Clogged blood vessels can lead to heart attack, stroke, and other problems.
Coronary artery disease, sometimes called hardening of the arteries, is caused by narrowing or blocking of the blood vessels that go to your heart.
Your blood carries oxygen and other needed materials to your heart. If the blood vessels to your heart become partially or totally blocked by fatty deposits, then the blood supply is reduced or cut off. Then a heart attack, sometimes called a myocardial infarction or MI, can occur.
These are the signs of a heart attack:
• Chest pain or discomfort
• Pain or discomfort in your arms, back, jaw, neck, or stomach
• Shortness of breath
• Sweating
• Indigestion or nausea
• Light-headedness
• Tiredness or fatigue
You may not experience all of these symptoms, and they may come and go. Chest pain that doesn’t go away after resting may signal a heart attack. Diabetes can cause nerve damage that can make heart attacks painless or “silent.” If you have warning signs of a heart attack, call 911 immediately.
Heart failure doesn’t mean your heart has stopped working. It means that the heart is less able to pump the blood the body needs. Heart failure may be caused by a number of problems, such as heart attack, coronary artery disease, and high blood pressure. In congestive heart failure, fluid builds up inside body tissues such as the lungs. This makes breathing difficult.
The warning signs for heart failure can vary. These can include:
• Shortness of breath
• Weakness
• Nausea
• Fatigue
• Swelling of the feet and ankles (from fluid retention)
A stroke happens when the blood supply to part of your brain is suddenly cut off. This damages brain tissue. Strokes usually happen when a blood clot blocks a blood vessel in the brain or neck.
A stroke can cause movement problems, pain, numbness, and problems with thinking, remembering, or speaking. Sometimes people also experience emotional problems, such as depression, after a stroke.
People with diabetes are 1.5 times more likely to have a stroke than are people who don’t have diabetes. But people with diabetes can lower their risk of stroke by taking care of their health.
The warning signs for stroke can develop suddenly and can include:
• Weakness or numbness on one side of the body
• Sudden confusion or trouble understanding
• Trouble talking, dizziness, loss of balance, or trouble walking
• Trouble seeing out of one or both eyes
• Double vision
• Severe headache
You can help lower your risk for heart disease by doing the following:
• Control your blood sugar, blood pressure, and cholesterol.
• Be physically active for at least 30 minutes on most days of the week.
• Reach and stay at a healthy weight
• Eat foods high in fiber and low in fat.
• Stop smoking
Take medications as directed by your health care provider
Diabetes is a leading cause of nerve damage. About half of all people with diabetes have some form of nerve damage. Nerve damage is also called neuropathy. It can cause tingling, pain, or numbness in your feet and hands. It can also affect the nerves in your body that control your digestive system, urinary tract, sex organs, heart and blood vessels, sweat glands, and eyes. Keeping your blood sugar, blood pressure, and cholesterol levels in your target range can help prevent or delay nerve damage and other problems.
Your kidneys have millions of filters that remove waste from your blood. These filters keep protein in the blood. High blood glucose can damage these filters. When kidney disease starts, the filters in the kidneys do not work well. This causes protein to pass into the urine. Having protein in the urine is called albuminuria. You cannot see or feel this, but your health care provider can test your urine for it. Without treatment, the kidneys will get worse. Once this happens, the kidneys have a harder time controlling the body’s fluid levels. This can cause high blood pressure or make high blood pressure worse. When the kidneys do not work, a machine can be used to filter waste from the blood through a process called dialysis.
• Visit your health care provider regularly. Get screened for kidney disease to catch problems early. Your health care provider can check your blood pressure, urine (for protein), and blood (for waste products).
• Follow your health care provider’s advice. Sometimes exercise, changes to your diet, and medicine can help keep your kidneys healthy.
• Keep your blood glucose under control.
• Keep your blood pressure at goal. High blood pressure can lead to kidney disease or make it worse.
• Lose weight, if you are overweight
• Consume less salt
• Avoid drinking alcohol and smoking
• Be active every day. Talk to your health care provider before starting any physical activity.
You know that managing your diabetes can help you stay healthy and live your life. Still, some people find that daily diabetes management feels like a lot to handle. Diabetes affects your daily routine, at home, school, and work. Change isn’t always easy. But with practice, diabetes management can become a habit. As you get started, you’ll likely have questions or concerns. See the box below for some common questions about diabetes and where in this workbook to find answers.

Question
Answer
Does having diabetes mean I can’t have any sugar? All foods can fit into a healthy meal plan. See page 25.
Do I have to join a gym?
You don’t have to spend money to be active. See page 34.
Will I have to give myself shots every day? Not necessarily. See page 41.
What if I feel overwhelmed?
Taking care of your emotional health is a priority, too. See page 48.
Managing your diabetes is mostly up to you. But you don’t have to go it alone. A team of health care experts will teach you how to manage diabetes and the health risks it brings. Your family and friends can also provide support. Think about what kind of help you will need. Then decide whom to ask for that support.
Your diabetes health care team will work with you to create a management plan. Team members may include:
• A primary care provider, such as a general practitioner, internist, nurse practitioner, or physician assistant. This is the person whom you probably see most often and who can refer you to specialists as needed.
• An endocrinologist, a doctor who specializes in diabetes.
• A registered dietitian, an expert in food and nutrition, to teach you how food affects your blood glucose and how to plan meals.
• A diabetes educator, often a nurse, to teach you to manage and live with diabetes.

• A health psychologist or social worker, to help you with the emotional aspects of managing your condition.
• A pharmacist, who fills your prescriptions and explains your medications.
Family and friends can help support your efforts to take care of your health. They may be concerned about your condition and worried about complications. Or, it may be hard for them to understand all the changes you are making. But the important people in your life can help you succeed. People who care about you want to help. Think about the people who can support you, and the specific ways they can help. Then ask for the support you need. Your family and friends can help you stay focused and confident as you learn to manage diabetes.
Your health care team may be experts on diabetes, but you are the expert on you. No one else can manage your diabetes for you. So work closely with your health care team to create a management plan that you can stick with. Remember: As your life changes, your plan may need to change too. In fact, anytime your plan isn’t working as intended, it may be time to change the plan. This can help to protect your health, now and in the future.
The rest of this workbook focuses on what you’ll need to create your diabetes management plan. Each section gives you information and tips you can use every day. Use the fill-ins and checkboxes to mark ideas that you would like to try. In chapter 7, you’ll find an example of your diabetes tool kit. You’ll also find a glossary of diabetes terms and resources for learning more about diabetes management.

Diabetes can take a toll on your body and lifestyle. Here are just a few of the benefits you gain by creating and sticking with a management plan:
• May help reduce your risk of serious complications such as heart attack, stroke, blindness, or lower limb loss
• Have more energy and a better sense of well-being
• Miss fewer days of work, school, or other regular activities
Add a few of your own reasons here:

In this section, you will learn:
✓ The importance of checking your blood glucose
✓ How to know if your treatment plan is keeping your blood glucose where you want it to be
✓ What to do when your blood glucose is too high or too low
The first step in managing diabetes is learning to check (monitor) the level of glucose (sugar) in your blood. This will help you make daily decisions about blood glucose control. Monitoring isn’t hard to do. Your diabetes team will show you how. You will also learn how to keep a record of your numbers (readings). Your readings show you how food, activity, stress, and medication affect your blood glucose every day.
You can check your blood glucose at home, at work, or anywhere else. Your diabetes team will help you select a blood glucose meter. A meter measures the amount of glucose in your blood. You’ll use a lancet to prick your finger for a tiny drop of blood. The meter then gives you a reading that tells you the level of your blood glucose. With today’s meters, you can test just about anywhere you go.
Your blood glucose should be in your target range as often as possible. This means not too high and not too low. Staying in this range as often as possible helps reduce your risk of complications. Your diabetes team will help you figure out your ideal target range. Fill in the numbers for your target range in the box below.
Fill in your numbers here. My Target Range

Every time you check your blood glucose, use a log to keep track of your readings (see below, and use the full-size chart on page 62). You may check in the morning, at bedtime, and before and after meals. Be sure to write down all your numbers. Use your log to record things that might have affected your blood glucose. This may include being sick, being very active, stressed, or eating special foods on a holiday.


Keeping track of your blood glucose readings helps you identify patterns. These patterns tell you how your actions affect your blood glucose. For example, you may notice high or low numbers after eating certain foods. Use these patterns to make decisions about steps you can take to keep your blood glucose in your target range. Be sure to take your log book with you every time you see your health care provider. And be honest! There are no “good” or “bad” numbers. The readings just tell you if you need to make changes to your treatment plan.
You use a meter to track your blood glucose every day. But you also need to know if your treatment plan is working for you over time. An A1C (glycated hemoglobin) test can help. This test measures your average blood glucose level over 2 or 3 months. If your A1C number stays too high, your treatment plan may need changes.
An A1C result often is shown as a percentage. Your health care provider will help you figure out your target A1C. Many people aim for an A1C of 7% or lower. The general goal of <7% appears reasonable for many adults with diabetes. Higher or lower A1C goals may be appropriate. Ask your health care provider what A1C goal is right for you. Your target A1C number will depend on your age, general health, and other factors. Achieving your A1C goals may help lower your risk of complications
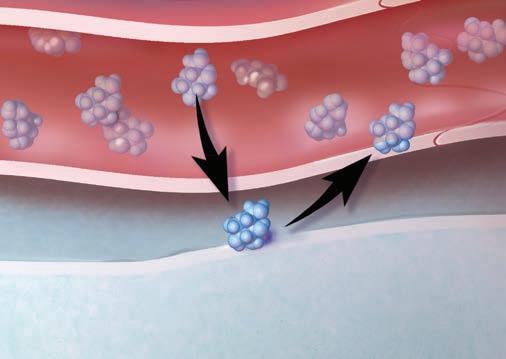
The A1C is a blood test. It measures how much glucose is connected to a protein (called hemoglobin) inside the red blood cells over the prior 2 to 3 months. You will likely have an A1C test every 3 to 6 months. Your health care provider may have your A1C tested 2 times a year (ie, every 6 months) if you are meeting your treatment goals and have stable blood glucose control. However, your health care provider may have your A1C tested more frequently (eg, every 3 months) if your therapy has changed or if you are not meeting your blood glucose target. Talk with your health care provider to schedule an A1C. And don’t forget to follow up on the results.
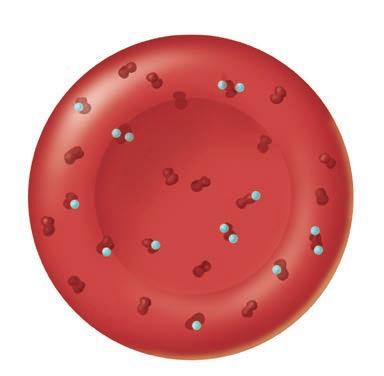
Healthy red blood cells have some glucose connected to them.

A high A1C means that too much glucose is connected to the cells.
Many things (including food, physical activity, and medication) can raise or lower blood glucose. Extreme highs and lows can be dangerous! Some people connect how they feel with having a high or low blood glucose. Others may not. That’s why you have to check using a blood glucose meter. Ask your health care provider which numbers outside your target range are dangerous for you.
Hyperglycemia means that your blood glucose is too high (for example, 200 mg/ dL). You might experience:
• Increased thirst
• Increased need to urinate
• Increased tiredness
• Blurred vision
Ask your health care provider when to call in case of emergency.
Always check your blood glucose right away.
If it’s too high:
1. Drink water or other sugar-free liquids to stay hydrated.
2. If you take insulin, you may need to take an extra dose. Ask your health care provider for instructions about taking extra insulin.
3. Check at least every 4 hours to make sure your blood glucose is going down. Call your health care provider if it doesn’t go down after two checks, or if symptoms get worse.
Hypoglycemia means that your blood glucose is too low (for example, 70 mg/dL or lower). A drop in blood glucose can happen very quickly. You might have:
• Sweating or cold, clammy skin
• Dizziness, shakiness, or tingling feeling
• Hard, fast heartbeat, or headache
• Confusion or irritability
If you don’t notice symptoms of low blood glucose or if you have had episodes of severe hypoglycemia, your health care provider may tell you to raise your target blood glucose.
Always check your blood glucose right away. If it’s too low:
1. Eat or drink 15 grams of fast-acting carbohydrate. This could be 3 or 4 glucose tablets or ½ cup (4 oz) of fruit juice.
2. Check your blood glucose again after 15 minutes. If it’s still low, repeat step 1. Check again after another 15 minutes. If it’s still too low, call your health care provider right away.
3. Once your blood glucose rises, eat a small snack if your next planned meal is over half an hour away.
It’s important that you learn to recognize the signs of hypoglycemia (low blood glucose), which can come on quickly. You may need to be prepared to provide glucose tablets or another fast-acting carbohydrate. In some cases, a special injection (of a hormone called glucagon) is needed if severe hypoglycemia occurs in a person who uses insulin. You may need to learn how to inject this medication in an emergency.

You can’t always have perfect blood glucose control. But make the effort to keep your blood glucose in your target range as often as possible. Check your blood glucose as directed. And make sure you get an A1C test every 3 to 6 months. This will help you decide if you need to change your management plan to reach your blood glucose goals.
Are you remembering to check your blood glucose as often as you planned? If not, what’s stopping you? Write down your barriers. Be specific. For each barrier, think of a solution that you can stick with. Write it down in the space provided. Then refer back to this chart whenever you need a reminder.
Example: Change I want to make: Remember to test my blood glucose 2 hours after eating. What’s stopping me: I forget when I get too busy at work.
Solutions: Set an alarm to go off when I need to check my blood glucose. Or, pick an activity I do every day and always check at that time, such as during a break.
Change I want to make:
What’s stopping me:
Solutions: Change I want to make:
What’s stopping me:
Solutions: Change I want to make:
What’s stopping me:
Solutions:

Eating healthy foods every day is key to controlling your blood glucose. In this section, you will learn:
✓ How different foods affect blood glucose levels
✓ How to create a diabetes-friendly meal plan and put it into action
✓ How to stick to your meal plan away from home
A key part of controlling blood glucose is eating healthy foods every day. You don’t have to stop eating the foods you like. But you do need to know how food affects your blood glucose. Ask to meet with a registered dietitian (an expert on food and nutrition). The dietitian will teach you the skills you need to plan healthy, diabetes-friendly meals.
Before you see the dietitian, you may be asked to keep a food diary for a few days. Write down all the foods you eat and when you eat them. Bring this list with you when you see the dietitian. It will help the dietitian get to know your eating habits.
The dietitian will work with you to design a meal plan. The meal plan will be based on your likes and dislikes. The dietitian will teach you how the foods you eat affect blood glucose. You’ll learn how to judge serving and portion sizes of the foods you eat. Creating a plan you can live with will help you keep your blood glucose in your target range.

You may work with the dietitian one-on-one or in a group class.
Often, when people are diagnosed with diabetes, they don’t know where to begin. One way is to adjust the portions you are already eating. It’s an easy way to get started with managing blood glucose levels.
Focus more on filling a 9-inch plate with nonstarchy vegetables and having smaller portions of starchy and protein foods. You don’t need any special tools or have to do any counting. It’s simple and effective — draw an imaginary line on your plate, select your foods, and enjoy your meal! You may have heard of this as the “Plate Method.”
Once you’ve changed your portion sizes, you can work on making healthier choices for each food group.

1/2
1/4
1/4
Just as a car needs the right type of fuel (gas) to run, you need the right kind of fuel (food) to function. To sustain energy, your body needs food that contains carbohydrates. But carbohydrates raise blood glucose levels higher and faster than other kinds of food.
You need to eat carbohydrates every day. But the more you eat, the higher your blood glucose may rise. To help keep your blood glucose in your target range, learn which foods contain carbohydrates. Then decide how much of these foods fit into your meal plan. The main types of carbohydrates are: starches, sugars, and fiber (a type of carbohydrate that doesn’t raise blood glucose).

Starches are found in grains, some vegetables, and beans. Grain products include bread, pasta, cereal, and tortillas. Starchy vegetables include potatoes, peas, corn, lima beans, yams, and squash. Kidney beans, pinto beans, black beans, garbanzo beans, and lentils also contain starches.

Sugars are found naturally in many foods. Or sugar can be added. Foods that contain natural sugar include fruits and dairy products. Added sugars are found in most desserts, processed foods, candy, regular soda, and fruit drinks. You can find added sugars in the ingredient list on food labels. Limit foods with added sugar.

Fiber comes from plant foods. Most fiber isn’t digested by the body, so it doesn’t raise blood glucose like other carbohydrates. Fiber is found in fruits, vegetables, whole grains, beans, peas, and many nuts.
You can learn to figure out how much carbohydrate you are eating every day. Ask your dietitian to teach you a technique called “carb counting.” This system helps you keep track of the carbohydrates you eat at each meal. There are different ways to do carb counting. See the chart below to learn more.

• When you count carbohydrate grams, you use the “Nutrition Facts” label on packaged foods. The label tells you the actual carbohydrate amount (in grams) in a food.
• To give you an idea of how much carbohydrate is in food:
1 slice of bread = 15 grams of carbohydrate
1 apple = 15 grams of carbohydrate
1 cup milk = 12 grams of carbohydrate
• A dietitian can help you determine how many grams of carbohydrate to have at each meal. (If you take insulin, you will also learn how to adjust your mealtime insulin based on your carbohydrate intake.)
• The dietitian will help you determine how many carbohydrate servings to have at each meal and snack.
• This method is a good way to get started with carb counting.
The “Nutrition Facts” label on packaged food tells you how many grams of carbohydrate are in the food. (See page 29 to learn about reading food labels.) But some foods, such as fresh vegetables, don’t have labels. Or you may be eating away from home, where food is already removed from its packaging. If you are counting carbs, learn the serving sizes of carbohydratecontaining foods that you eat often. Use the chart on page 63 to look up the serving sizes of many common foods.
You’ll work with a dietitian to design a meal plan. Your plan needs to fit with your eating habits and schedule. Planning what and when you eat helps keep your blood glucose in your target range. Aim to eat foods from all the food groups every day.
Eating from all the food groups gives your body the nutrients it needs to work properly. The six food groups are: grains, vegetables, fruits, proteins, dairy, and oils. Work with the dietitian to include a variety (many types) of foods from each group. Variety can keep you from getting bored with your plan.
If you want to lose some weight, reduce the amount of calories you take in. Reducing your portion sizes will help (review the plate method on page 25). Two more ways to cut calories are eating less fat and drinking fewer sugary beverages:
• Cut fat by using only small amounts of liquid oil for cooking (instead of butter, shortening, or lard). Avoid packaged foods with trans fats.
• Reduce the amount of regular soda, sports drinks, and fruit juice that you drink. Instead, drink plenty of water and other sugar-free liquids.

When it comes to blood glucose control, when you eat is as important as what you eat. You may want to eat several small meals spaced evenly through the day to stay in your target range. Pay attention to what keeps your blood glucose steady. And don’t eat most of your food at one time. Doing so can cause your blood glucose to rise too high or fall too low.
Consult your meal plan before you go to the store. Decide ahead of time what you want to cook and make a list. This helps you stay on track while you shop. At the grocery store, read food labels to help you make the healthiest choices. If you don’t do the shopping, be sure the person who does understands your needs.
Look for the “Nutrition Facts” label on packaged foods. It tells you how much of the food makes up one serving. It also tells you how much carbohydrate and fat are in each serving. This will help you decide if the food fits into your meal plan.
• Look for brightly colored fruits and vegetables.
• Buy lean meats, such as chicken, turkey, and fish.
• Avoid high-fat snack food aisles.
• Look for whole-grain foods and low-fat dairy products.
Use the following tips to help you prepare healthier, diabetesfriendly meals at home:
• Trim fat off meats before cooking.
• Broil, steam, bake, or grill meats and vegetables instead of frying.
• Use olive or canola oil instead of butter or lard for cooking.
• Don’t cook meat and vegetables in cream- or butter-based sauces.
This tells you how much of the food makes up one serving. If you eat more than one serving, all the other values increase.
This is the total amount of saturated fat in each serving. Limit saturated fats and avoid trans fats. Both are bad for your health.
A healthy meal plan with less salt can help you control your blood pressure. Limit your salt to no more than 2,300 mg each day if you have diabetes. For people with both diabetes and high blood pressure, a further reduction in sodium may be necessary.
This tells you how many grams of carbohydrate are in one serving. If you do carb counting, this number helps you fit the food into your meal plan.
You may not always have control over what is available to eat or how it’s prepared. But you can choose which foods to eat and how much to eat at once. You can follow your meal plan, even when you eat away from home.

At restaurants, use the following tips to help you stick to your meal plan:
• Ask how food is prepared. Avoid fried or breaded foods, or ones sautéed in butter or cream.
• Ask if sauces and dressings can be served on the side, and use them sparingly.
• Most restaurants serve large portions. Eat half your meal and take the rest home.
• At a buffet, remember the portion-size plate diagram on page 25. Devote at least half your plate to vegetables and green salad, and ¼ each to starch and protein.
• Split a dish or dessert with a friend or family member.
• Skip the bread or chips basket before the main meal.
Drinking alcohol can lower your blood glucose level. It can affect you up to 24 hours after drinking. Never drink when your blood glucose is low or on an empty stomach! And be aware that alcohol adds calories. You may have to adjust your meal plan if you decide to have a drink. Ask your health care provider or pharmacist if any of the medications you take interact with alcohol.
Parties and holidays often involve special or traditional foods and drinks. Eating foods that aren’t normally part of your meal plan can affect your blood glucose. But you can adjust your meal plan or insulin dose to allow for these foods. (Ask your health care provider to show you how.) Remember to check your blood glucose often to see how different foods affect you. And talk to your health care provider and clergy about safer ways to fast during religious holidays.
Well-meaning family and friends may not always understand your meal choices. This can be especially true at parties or other social gatherings. But you don’t have to eat or drink something that affects your blood glucose just to be polite. If you find yourself eating or cooking to please others, try the tips below:
• You can accept any food and drink that is offered. But you don’t have to eat or drink it. Just holding a drink or small plate of food is often enough. This will usually keep people from insisting that you have another helping or another drink.
• Plan ahead. Bring a dish to share that you know you will enjoy. Then you won’t have to feel deprived if most of the offered food doesn’t fit into your meal plan.
• At home, you can cook different side dishes or prepare traditional foods in healthier ways. Talk with your family about the benefits these changes can bring.
Are there other ways to stick with your meal plan at social gatherings? Write in your ideas:
A family member with diabetes may choose to make changes in his or her eating habits. Your support during this time is very important. You can encourage him or her to explore new ways of cooking and eating. Ask how involved your family member wants you to be. And remember: Change can be difficult! The person with diabetes needs to be the one to decide on making changes for him- or herself. Your job is to be supportive.
You may choose to change your own eating habits, too. This is a great way to offer your support. Eating healthier is better for the whole family. For more ways you can support your family member with diabetes, see the box below. Check off one or two things you would like to try.

Ask if your family member wants to be reminded about his or her meal plan. If not, don’t nag.
Buy and keep healthier foods in the house. Eat these foods yourself, too.
Remember that eating and food can be very emotional topics! Believe in your loved one’s ability to make changes. Saying “I know you can do it” goes a long way.
Write in your own methods of support here:

Getting active is a great way to help manage your blood glucose. In this section, you will learn:
✓ How losing even a little weight can lower your blood glucose
✓ Why just getting out and walking helps your cells use glucose
✓ Ways to overcome barriers that are keeping you from meeting your activity goals
Being physically active every day can help you manage your blood glucose, blood pressure, and cholesterol. That’s because an active lifestyle can improve your body’s ability to use insulin. Daily activity can help reduce the risk of complications of diabetes. And it’s a great way to relieve stress. If you aren’t normally active, be sure to consult your health care provider before getting started.
If daily activity is new to you, start slow and steady. Try to do a total of at least 150 minutes per week of aerobic exercise, such as brisk walking, spread over 3 or more days a week. If you are just starting out, start with 5 minutes a day and gradually add more time. Do this by adding a few minutes each week. It doesn’t have to be done all at once. Each active period throughout the day adds up.
Prolonged periods of sitting are not good for anyone, especially people with type 2 diabetes. Get up and walk around at least every half-hour if you sit for lengthy periods of time, such as at work or at home.

If you are overweight, work up to 60 minutes of daily activity. Weight loss can help improve your ability to keep your blood glucose in your target range. Even a modest loss of 5 to 10 pounds can help you meet your blood glucose goals. Other potential benefits of weight loss include increased energy and improved mood. Talk with your health care team before starting any exercise program and about setting a weight-loss goal that is right for you.

You don’t have to join a gym or own pricey sports equipment. Just get out and walk. Walking makes your heart beat faster. The more you walk, the easier it gets. Make it part of each day. Walk with a friend or a group to keep it interesting and fun. Try taking several short walks to meet your daily activity goal. And to track how many steps you take daily, you might want to use a pedometer or digital activity tracker. Either one will keep a running tally of the steps you take. Remember: With every step, you’re doing a little more to help you manage your diabetes.

To feel your best, your health care provider may suggest adding strengthening exercises to your routine. Exercises such as lifting weights, working with resistance bands, and swimming are good choices. When done at least three times a week, resistance exercises help build muscle and increase endurance. They may also help improve heart health and help you manage your weight.
Make daily activity a lifelong habit. Once you feel good about being active, look for ways to stick with your new active lifestyle. The key is finding activities that you enjoy. Vary your routine from day to day to keep from getting bored. See the box below for ways to add activity to your day. Check off at least two ideas that you would like to try.
Physical activity doesn’t have to be hard to do to help you manage your blood glucose. Choose activities that fit into your everyday routine, such as:
Yardwork (gardening, mowing the lawn, or raking leaves).
Riding a bike to go shopping or run errands.
Walking the dog around the neighborhood after dinner.
Parking farther away from store entrances.
Taking the stairs instead of the elevator whenever possible.
Plan activities you enjoy. The more fun you have, the more likely you’ll stick with it. Here are some ideas to get started:
Join a social group that walks or does another activity.
Bowl or golf with friends.
Put on your favorite music and dance at home.
Find interesting places to walk, such as museums, parks, malls, or the zoo.
Hike, bike, or go to the park with kids or grandkids.

Being active may cause blood glucose to drop faster than usual. This is especially true if you take certain medications to help control your blood glucose. But there are things you can do to help reduce the risk of low blood glucose levels.
• Include friends and family in your activities. Being active with a “buddy” is safer than being alone.
• Wear a medical ID bracelet that says you have diabetes.
• Always carry identification. Carry a cell phone in case of emergency.
• Use the right safety equipment (such as a bicycle helmet).
• Be sure to wear closed-toed shoes that fit your feet.
• Drink plenty of water before and during activity.
• Keep a fast-acting carbohydrate (or glucose tablets) on hand in case of low blood glucose.
• Dress for the weather.
• Avoid being active for long periods in very hot or very cold weather. For instance, go out in the evening if it’s too hot during the day.
• Skip activity if you’re sick.


Physical activity is important when you have diabetes. But you need to keep an eye on your blood glucose level. Check often if you have been active for longer than usual, or if the activity was unplanned. Make it a habit to check your blood glucose before being active. Check again several hours later (blood glucose may decrease for a few hours after activity). Use your log book to write down how activity affected your numbers. If you take insulin, you may be able to adjust your dose before a planned activity. This can help prevent low blood glucose. Talk to your health care provider to learn more.
Many people want to be as active as possible. But being active every day can be a challenge. You may find yourself making excuses or getting distracted. If so, what’s keeping you from reaching your activity goals? Copy the chart below to write down your specific roadblocks. Then fill in ideas that can help you stay on track.
“I don’t want to walk in my neighborhood after dark.”
“I’m too tired to be active when I get home from work.”
“In the winter, it’s too cold to walk outside!”

Walk inside the house! Dance to your favorite music, or pop in a workout video or DVD.
Take breaks for short walks during the day. Three 10-minute walks will boost your energy and help you meet a 30-minute goal.
Find an indoor mall near you. Take a friend or family member window shopping. Or, walk up and down the stairs at home.

Most people with diabetes need medication. In this section, you will learn:
✓ How different medications work
✓ How to develop a daily medication routine
Like healthy eating and physical activity, taking medication can help you manage your blood glucose, blood pressure, and cholesterol. Glucose-lowering medications improve your ability to keep your blood glucose in your target range. Similarly, blood pressure and cholesterol medications help keep those levels within your target ranges.
The next three pages will tell you about the different types of glucose-lowering medications and how they work. Many people take one or more medications to help manage their diabetes. Talk with your health care provider, diabetes educator, nurse, or pharmacist and learn the names of your medications. Then have him or her help you fill out the chart on page 64.
Talk to your health care provider about your medications. Medications affect different parts of the body. For instance, some medications increase insulin sensitivity in cells. Some prevent the liver from making and releasing too much glucose. Some cause carbohydrates to break down more slowly in the digestive tract. Some stimulate the pancreas to produce and release more insulin. Some cause excess glucose to be eliminated in the urine. The diagram at right shows where different glucose-lowering medications work. Talk to your health care provider about the medications you are taking and how they work.

There are many kinds of medications. Some medications can be swallowed. Others have to be injected, or else they would be broken down in the stomach before reaching the bloodstream. Some are inhaled. The main ways of taking medication for diabetes are shown below.

Oral medications
Pills

Shots given using a syringe or pen-like device


Insulin pumps
Devices that can deliver a steady amount of insulin 24 hours a day
Many people with type 2 diabetes end up needing insulin. Taking insulin can give you greater flexibility in your daily blood glucose management. You will learn how to adjust your dosage based on your blood glucose goals, meal plan, and activity level. Talk with your health care provider about the types of insulin. You may need to use more than one type.
Insulin and certain other medications are given by injection. Giving yourself shots every day might seem overwhelming at first. But they can help you feel better and improve your blood glucose control.

Your diabetes educator will help you practice giving yourself shots until you feel more comfortable. You may find that giving yourself shots is easier than you thought. And with practice, it can become part of your everyday routine.
You won’t always be at home when it’s time for insulin shots. You’ll need to inject insulin no matter where you are. You might have concerns about giving yourself injections in public. But managing diabetes means taking care of yourself, not worrying about what people might think. Most injection devices can be used quickly and quietly, even at the dinner table. And you can choose more private locations to perform injections, such as public restrooms or your parked car. Be prepared to give yourself shots anywhere you go.
High blood pressure and high cholesterol can increase your risk of artery damage. The risk is even greater when combined with high blood glucose. You may also need to take medications for high blood pressure and high cholesterol to help prevent serious health problems.
Your blood pressure checks how hard your heart has to work to pump blood to your body. Cholesterol is a fat-like substance in the blood. Everyone’s body makes cholesterol. Cholesterol also comes from the foods you eat. Many people with diabetes will also need to take medications for high blood pressure and high cholesterol. Keep track of your blood pressure and cholesterol levels with the charts on page 65.
Use a chart to keep track of your medications. (There’s a full-size chart on page 64 that you can copy and carry with you.) Be sure to keep this list up-to-date. Bring a copy with you every time you see a health care provider or pharmacist.
Taking daily medications may seem like a big step. But medications work best when you take them as prescribed. Talk to your health care provider or pharmacist if you have questions or concerns about how to take your medications.
Vitamins, herbal supplements, and some prescription and over-thecounter drugs can interfere with other prescribed medications. Be sure to tell your health care provider about all the medications you’re taking. This includes remedies for headaches, allergies, colds, and even constipation. Ask your health care provider or pharmacist if there are any medications you need to avoid. Always read the warning labels and directions on everything you take. Show your medication list to the pharmacist every time you get a new medication or if you change pharmacies.
Taking glucose-lowering medications as directed by your health care provider will help control your blood glucose. Like a meal routine, a medication routine can help you stay in your target range. Use a daily schedule to keep you on track. If you are having trouble, ask a family member or friend to help. And be sure to ask your health care provider or pharmacist what to do if you miss a dose.

The tips below can help you stick with your medication routine.
• Don’t change your dosage or stop taking any of your medications, even if you are feeling better! Always talk to your health care provider first.
• Refill your prescriptions before they run out. Check the brand and dosage to make sure they are correct.
• Prepare a small travel kit (see page 60) so you can take your medications with you everywhere you go.
• Call your health care provider right away if you notice any side effects. But don’t stop taking your medications unless told to do so.
• Ask family or friends for help if you are having trouble remembering to take your medications.
• Make filling out your daily schedule part of your routine. Ask a family member to help you stay organized.

Starting to take medication for diabetes can be a big step. Your family member with diabetes might feel sad or angry about having to take medication. You can make this change easier by helping with the tips above.
Taking medications every day may require some changes to your lifestyle. But change doesn’t always happen right away. The box below has tips that can help you adjust to taking medication. These tips can help you manage a smoother transition to your medication routine.
Everyone handles change a little differently. The following tips can help if you are having trouble adjusting to taking diabetes medications.
• Prepare yourself for slow, steady progress. Taking medication won’t cure diabetes. Change doesn’t happen overnight, but small changes add up. You may not see the benefits of treatment right away. Contact your health care provider if your medications aren’t working or if you’re having side effects.
• Establish a daily routine. Taking your medications in the same way and at the same time every day is crucial. When your daily routine is disrupted, it’s easy to forget. To make your medication routine work for you, plan ahead. And don’t get discouraged if you slip up a few times. You’ll get better at sticking with your routine with daily practice.
• Ask for support. Taking medications for diabetes can have a big impact on your life. Tell the people close to you how they can help you stay on track. You might want to join a diabetes support group. There, you can talk with people who have many of the same concerns, fears, and goals.

• Acknowledge new emotions. It’s common to resist or feel angry or scared about having to take medications. You’re not alone. Share your feelings with your health care team and people close to you. Acknowledging new emotions is the first step toward accepting them.

Living well with a chronic condition means taking care of your whole body. In this section, you will learn:
✓ How to help maintain your emotional health
✓ How to help maintain your physical health
✓ How to manage changes in your daily routine, such as sick days and travel
Managing your emotional health is just as important as managing your physical health. You can’t change the fact that you have diabetes. But you can choose to make your emotional health a priority. Think about ways you can take care of your whole self, not just your diabetes. The tips on these pages can help.
Everyone feels stressed at times. But for people with diabetes, managing stress is even more important. This is because stress can increase or decrease blood glucose. So, think about what causes stressful feelings. Then, find ways to limit or avoid stressful situations. To combat stress, try:
• Physical activity, a natural stress reliever.
• Making time to do things you enjoy, such as hobbies or spending time with family and friends.
• Talking to a counselor or a close friend.
Living with a chronic condition takes focus and concentration every day. You don’t get “days off” from diabetes management. This may leave you feeling tired or “burned out.” Some days will be harder than others. To help fight burnout, take care of yourself as a whole person, not just a person with diabetes. See the next page for tips on avoiding burnout.

Many people feel sad or down when they first hear that they have diabetes. Feelings like these are normal. But frequent feelings of helplessness or hopelessness are a symptom of depression. Depression is a serious problem, but it can be treated. If you feel overwhelmed, or if you are having trouble sleeping or eating, talk to your health care provider. Don’t wait!
Thinking about your blood glucose all the time can make you feel stressed or depressed. To fight stress, take time out every day to relax your body and clear your mind. Relaxation techniques include the following:
• Yoga, tai chi, meditation, and prayer all ways to relax the mind and body
• Deep breathing to release physical tension
• Visualization (picturing a relaxing scene in your mind) to recharge your mental batteries.
Getting plenty of good-quality sleep (not too little or too much) is important to help keep blood glucose under control. Talk with your health care provider about how much sleep is right for you.
To keep from feeling overwhelmed, set your priorities. Focus on doing the things that are the most important. Make decisions about what needs to be done and when. Ask yourself: “Do I really need to do this today?” If the answer is no, don’t worry about it! Don’t forget to ask those close to you for help. Also, look for ways to do tasks with less effort.

Having diabetes means making some changes. But you can still do things you enjoy. Don’t forget to have fun! Make time every week for at least one activity you like to do. Here are some suggestions:
• Watch a ball game with a friend.
• Spend time playing with kids or grandkids.
• Go to a movie.
• Read a new or favorite book.
• Have a friend over for coffee.
• Window shop with friends or family in a local mall.
• Take your dog for a long walk in a new part of town.
• Go on a day or weekend trip.
• Ask someone else to take a turn making dinner.
Managing your blood glucose every day helps reduce your risk of complications. You also need regular checkups with your health care provider to monitor risk factors for diabetes complications. Keep up-to-date on the tests listed below. Ask what other tests you might need based on your age, health, and gender (such as cancer screenings).
The American Diabetes Association recommends having the following tests done to help reduce your risk of complications (especially from comorbidities):
• Blood pressure (every time you visit the health care provider)
• A1C (at first, every 3 to 6 months)

• Cholesterol and blood lipids (at the time of diagnosis, and every 5 years after that—or more often, if recommended by your health care provider)
• Foot exam (a thorough examination once a year. Have your feet looked at during every visit.)
• Vaccinations (as directed by your health care provider)*
*Ask your health care provider which immunizations would help you.
If you smoke, quitting smoking is one of the most important changes you can make for your health. Talk with your health care provider about ways to stop smoking. Together, you can make a plan to quit. Quitting may be hard and take some time. But, the potential health benefits are worth it.
Forming a “quit plan” can improve your chances of success. First, ask your health care provider about quit aids and medications, such as nicotine gum or patches. Plan when you’ll quit and what method you’ll use. Decide ahead of time how you will deal with the urge to smoke. Let your family and friends know how they can support you. Start by setting a quit date.
Over time, diabetes can affect nerves and blood vessels that supply the legs and feet. This means you may not be able to feel if you have a cut or infection. Wounds on your feet may be slow to heal, and may infect easily. Because of this, you need to pay close attention to your feet. Check them daily. Ask a family member for help if you have trouble seeing your feet, especially the bottoms. If you have problems with your feet, you should have your feet examined every time you see your health care provider.
Here’s what you can do to help prevent serious health problems with your feet:
• Inspect your feet every day for cuts, cracks, sores, redness, or swelling. Watch for cuts and scrapes that are slow to heal, itch, feel warm, ooze fluid, or smell bad. If you notice any of these problems, contact your health care provider right away. He or she may refer you to a podiatrist (a specialist in foot health).
• Keep your feet clean and protect them from injury. Wash your feet in warm (not hot) water and dry thoroughly, especially between toes.
• Don’t soak your feet.
• Do not go barefoot, and always wear clean socks and comfortable shoes that protect your feet.
• Do not trim any corns or calluses. Talk to your health care provider if you need help cutting and filing your toenails safely.
• Look for color changes in your feet (redness with streaks can signal a severe infection).
• The American Diabetes Association recommends that you have a thorough foot exam at least once a year. Anyone who has diabetes should have their feet inspected at every office visit.

Diabetes can lead to retinopathy. This is a condition caused by changes in the retina, the part of the eye that senses light. If not treated, retinopathy can lead to blindness. To help monitor your eyes for changes (such as changes to the retina), see an eye care specialist (ophthalmologist or optometrist) at least once a year. Do this even if your eyes feel fine and you aren’t having trouble seeing. Call the health care provider if you notice any of the following:
• Any new dark spots in your vision
• Poor vision in dim light
• Eye pain or pressure

People with diabetes are at risk of periodontal (gum) disease. This is an infection that destroys gums and the bones that hold the teeth. The infection can also enter the bloodstream, affecting the heart and other organs. To help prevent gum disease, brush your teeth at least twice a day. Don’t forget to floss! And see a dentist at least twice a year. Be sure to tell anyone who works on your teeth that you have diabetes. Call your dentist if you notice any of the following:
• Bleeding gums
• Red, swollen, or tender gums
• Gums that have pulled away from teeth
• Loose teeth, or permanent teeth that have shifted position

Intimacy and sexual function are an important part of life. But over time, high blood glucose can contribute to physical problems that affect intimacy, such as erectile dysfunction (ED). The good news is that ED can be treated.
If you are experiencing ED, talk to your health care provider. It may be that your diabetes management plan needs changes. Your health care provider might also prescribe a medication specifically for ED.

Vaginal dryness is twice as common in women with diabetes as it is in women without diabetes and is one of the main reasons women with diabetes have discomfort during sex.
It’s also a result of aging and is very common among women who are menopausal or postmenopausal. In the cases of vaginal dryness resulting from menopause, a lack of estrogen can be the cause of dryness, and problems may be treated with medications prescribed by your health care provider. Better lubrication may be one solution. However, researchers don’t understand exactly why women’s bodies lose the ability to self-lubricate when menopause isn’t the cause. Each woman’s individual medical situation needs to be carefully discussed with her health care provider to make the best decision for her.
Diabetes can also increase risk to a mother and baby during pregnancy, so be sure to talk with your health care provider any time you have concerns about your blood glucose and its impact on your health and quality of life.

Changes in your normal routine might make it harder to follow your meal plan and medication schedule. But with a little planning, you can manage diabetes anywhere you go. A diabetes “tool kit” can help you stay organized. See page 60 for a list of supplies to include.
Medications that can cause low blood glucose may affect driving safety. Always check your blood glucose before you get started. If it’s low, eat or drink a snack to raise your blood glucose to above 70 mg/dL. If you feel symptoms of low blood glucose while driving, pull over so you can take action. Keep your diabetes supplies where you can reach them, not in the back seat, glove compartment, or trunk. Store medications, especially insulin, out of direct heat, such as sunlight. In case of emergency, always carry identification that says you have diabetes.
About 1 month before your trip, ask your health care provider if you should have a checkup to make sure your diabetes is under control. Go over your schedule and talk about the medicines you take. Get any needed vaccines at least 1 month before your trip. Be prepared to manage your blood glucose everywhere you go. If you are flying, check with the airline for guidelines for traveling with supplies and medication, or contact the Transportation Security Administration (TSA). Carry your travel kit, with your supplies clearly labeled. Keep it with you at all times, not inside checked baggage! Make sure you have identification with you that says you have diabetes. Remember to drink plenty of water to stay hydrated. Check your blood glucose often. And ask your diabetes team for advice if you are traveling across time zones.
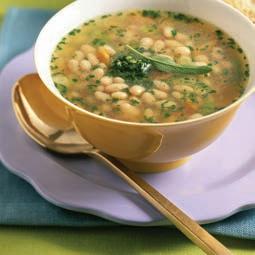
Having the flu, or even a cold, can make it hard to keep your blood glucose in your target range. You may not feel well enough to be active or eat regular food. Your diabetes health care team can help you develop an action plan for sick days. Follow all instructions from your health care provider closely.
Your blood glucose can rise quickly when you are sick. High blood glucose may also be a sign of infection. So it’s important to check your blood glucose often. Try to stick to your meal plan. If you have trouble eating solid foods, try soup, applesauce, or yogurt. And be sure to drink plenty of water and other sugar-free fluids to stay hydrated.
Your body needs carbohydrates in order to function. If you can’t eat at all, you will need to drink liquids with sugar or carbohydrates. This includes fruit juice, regular soda, and sports drinks. Talk to your diabetes team about the right amount of liquid carbohydrates. This will help keep your blood glucose from going too high or too low. Continue to drink water to stay hydrated.
Even if you can’t eat, don’t stop taking insulin when you are sick. If your blood glucose is high, you may need to adjust your dosage. If you adjust your insulin dosage, be sure to check your blood glucose often. This is to make sure your blood glucose doesn’t go too low. If your blood glucose falls below 70, take action! Eat or drink 15 grams of a fast-acting carbohydrate, such as glucose tablets or juice. Follow the directions on page 21 for treating low blood glucose.

When you’re sick, try to get plenty of rest. Only do as much as you comfortably can. You may need to ask family or friends for help with daily tasks. This may include cooking and cleaning, running errands, or picking up medications if you’re almost out of them. Those close to you should learn to recognize the signs of high and low blood glucose. Make sure family and friends know how to treat high and/or low blood glucose if needed.


Call the health care provider right away if:
• You can’t keep liquids down for more than 4 hours.
• You have vomiting or diarrhea for more than 6 hours.
• Your blood glucose stays over 240 mg/dL or under 70 mg/dL, even though you have taken your medication as directed in your sick-day plan.
• You have not eaten normally for more than 24 hours.
• You have a fever of 100.4˚F (38˚C) or higher.
• You have trouble breathing.
• You can’t stay awake or think clearly.
• Your chest hurts.
• You aren’t certain what to do to take care of yourself.
When someone you love has diabetes, it can mean big changes in your life. It’s likely that you will be called on as a helper, caregiver, or source of emotional support. Diabetes can be stressful for the whole family. Remember, taking care of yourself is just as important as taking care of your loved one.

It may be hard to watch someone you love cope with a chronic condition every day. You can help by:
• Learning as much as you can about diabetes. This will help you understand why your family member is making so many changes.
• Learning the signs of high and low blood glucose and how to treat them. Know when to call the health care provider in an emergency.
• Learning to be patient. At first, diabetes management can be confusing or frustrating. Ask how you can be most helpful.
Caring for someone else can take an emotional toll on you. Don’t forget to make time to focus on yourself. This is not selfish! Your emotional health is important. Some of these suggestions may help:
• Understand that some things are out of your control. You can be supportive, but you can’t manage your family member’s condition for them.
• Take time to relax. See page 49 for techniques that you can use.
• Ask for and accept help from others when you need to take breaks. Don’t feel guilty—we all need time to ourselves.
• Be aware of how you react to stress. If you become easily upset, stop for a moment. Take deep breaths, count to 10, or go for a walk to calm down.
• Look for support groups for caregivers. Some of the resources listed on page 67 may help.
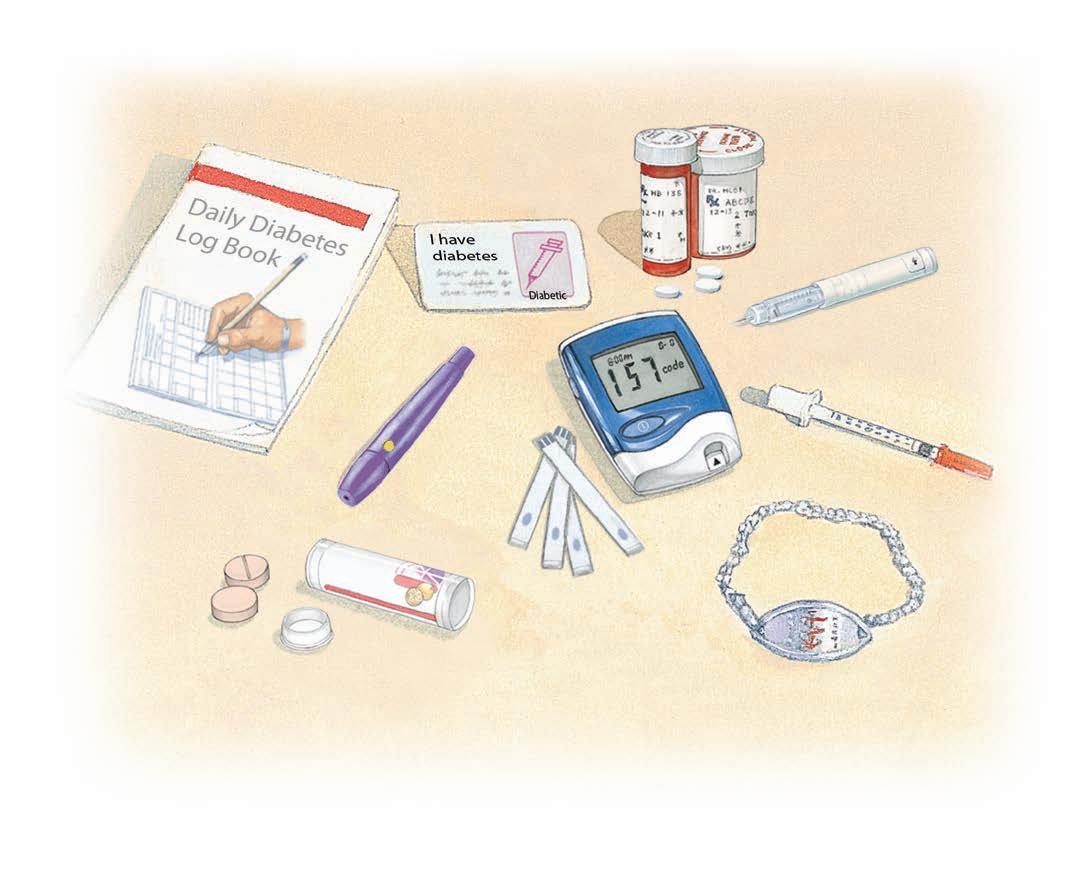
Keep track of your blood glucose supplies and medications by creating a diabetes kit. A small makeup or travel bag makes an ideal “diabetes tool kit.” Include the supplies shown below, as needed. And don’t forget to include any other medications you take for diabetes-related conditions.
Don’t forget any other medications you take!
Be prepared for an emergency. Keep an insulated, waterproof diabetes disaster kit ready. Include all the same items as in your diabetes tool kit. A disaster kit should also contain prescription numbers, medication lists, and photocopies of recent lab results. Be sure to update this kit at least twice a year.
