


Patient with long-standing urinary issues highlights her life-changing experience with sacral neuromodulation, a minimally invasive therapy used to treat bladder and bowel dysfunction.

While many people feel embarrassed or uncomfortable speaking about symptoms of urinary incontinence, urgency, frequency or frequent nighttime urination (nocturia), Rebecca King, a patient who once struggled with severe bladder symptoms, hopes to empower others with her story of successful treatment.
“I started experiencing symptoms in my late teens, and it soon began to take over my life,” explains King. “I was physically exhausted; it affected my hobbies, my social life, travel and even just going to the shop.” King experienced extremely severe symptoms, which dominated her life, including using the bathroom not only frequently, but for long periods of time to fully void her bladder, often getting up multiple times a night to go to the toilet.
Exploring treatment options
With symptoms so severe, she attended her local GP for assessment, but was not advised of any tangible treatment options and was not referred for specialist assessment. Sadly, this situation is all too common in clinical practice, as a lack of awareness and associated stigma can delay access to effective treatment methods.
“I felt so deflated because I was so young, and I knew something was wrong,” explains King. “I decided to move practice, and was eventually referred for urology assessment and given a range of options based on my specific case.”

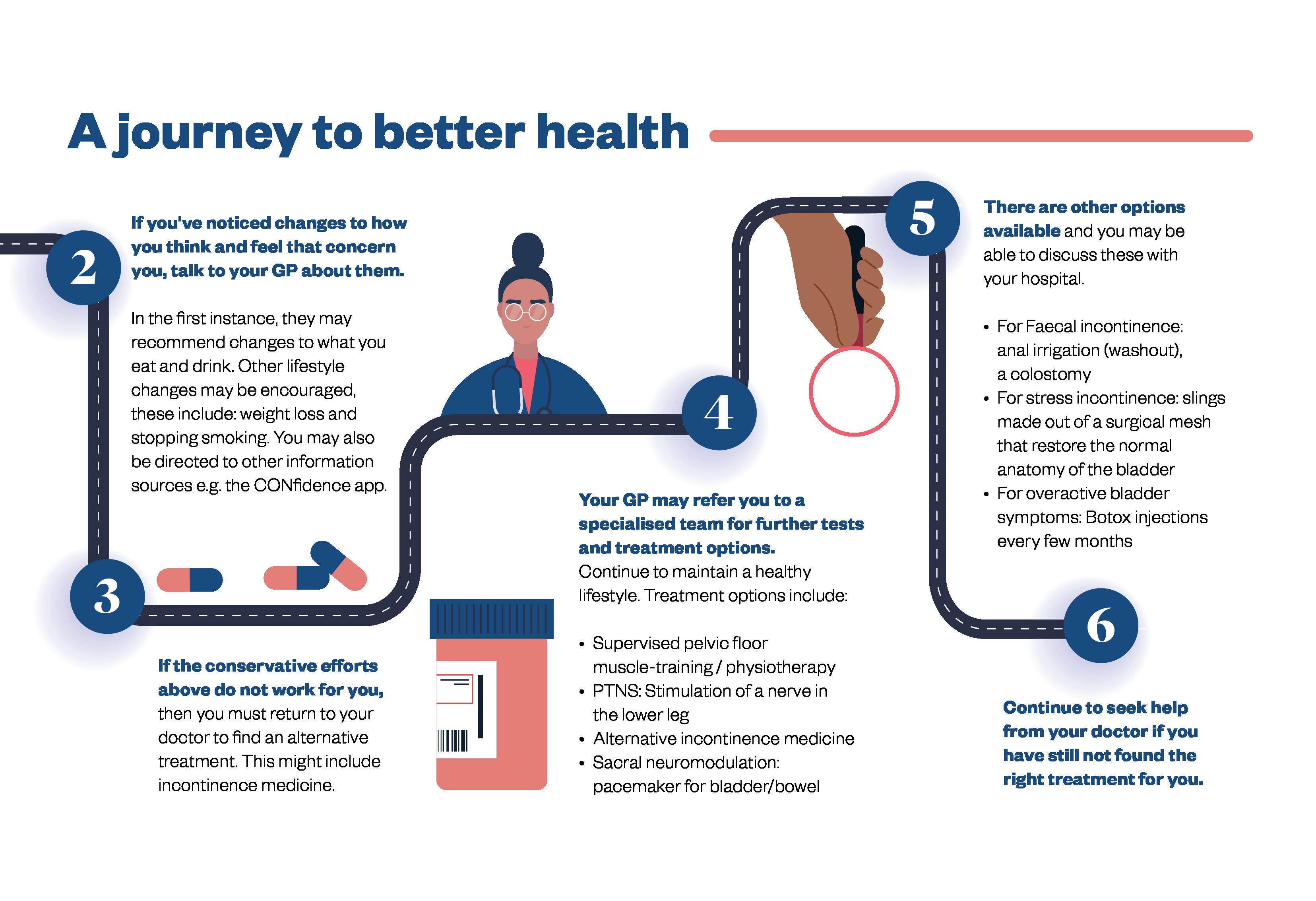
Treatment typically depends on the symptoms, their severity and the patient’s preferences and characteristics. First-line treatments include lifestyle adjustments, such as pelvic floor exercise, followed by medications and several minimally invasive treatments, such as Botox injections, can also be considered.
Patients are often required to complete a bladder diary to track symptoms and treatment effects, which helps to inform clinical and shared decision-making.
“Being taken seriously changed everything — to hear you have options and a potential solution gives you hope, and to feel understood is truly life-changing.”
Sacral neuromodulation
Sacral neuromodulation (SNM) is a minimally invasive therapy that uses a small implanted device to send gentle electrical pulses to the nerves controlling the bladder and bowels.
For patients like Rebecca, it can restore communication between the bladder or bowel and the brain, regulating normal function.
“I was finally told I was a candidate for SNM due to an overactive bladder, and after years of monitoring and considering a life of selfcatheterisation or lifelong medication, the InterSim device seemed like a no-brainer to me,” explains King. “I was sent for Urodynamic testing under Dr Forde and his team at Beaumont Hospital, following which I received a test device for two weeks to check it was going to work for me before the permanent device was fitted.”
“Getting the device isn’t as scary as you’d imagine. And when it works, you get your life back,” explains King. “While some steps can be quite intrusive, Hannah Graham, an advanced nurse practitioner at the Beaumont Hospital, made the process feel so easy and comfortable.”
Looking back, King notes that the treatment has resulted in far more than just physical symptom relief, but the emotional and social benefits have allowed her to regain her life.
“There is a stigma around urinary issues, which makes it extremely isolating, and it can be very depressing,” says King. “Not being offered options is incredibly diminishing to people’s wellbeing and hope. When you are finally taken seriously and shown a treatment pathway, it changes your whole life. I can finally go horse riding again, play with my children, go to the shops and travel, things most people take for granted.”

The Continence Foundation of Ireland brings together experts from multiple disciplines to improve the lives of all affected by urinary and faecal incontinence. CFI coordinates efforts, raises awareness and provides education and support for patients, families and professionals. Learn more or get involved at continence.ie.


Consultant urologist Dr Bianca Barea discusses the importance of shared decision-making for bladder dysfunction and the life-changing intervention of sacral neuromodulation.

Urinary and faecal incontinence affect millions, yet stigma and embarrassment mean many never seek help or discuss their symptoms,” says Bianca Barea, consultant urologist at Beaumont Hospital. “Patients need to know that treatment options are available, empowering them to take that first step to initial assessment.”
Raising awareness of sacral neuromodulation
Sacral neuromodulation (SNM) is a minimally invasive procedure in which an implanted device sends mild electric impulses to stimulate the nerves that control your bowel and bladder. “Alternative treatments for bladder control often require repeat procedures, but the SNM device can last for many years, providing long-term relief, giving patients their quality of life back,” explains Barea.
Beaumont Hospital has a comprehensive SNM service, including a highly experienced team — Dr Barea, Dr Forde, Dr McCawley and advanced nurse practitioner Hannah Graham — equipped to provide patients with expert assessment, individualised treatment planning and seamless management of both trial and permanent SNM implants. “We also run workshops for GPs to ensure they know that SNM is an option for patients in practice.”
Importance of shared decision-making
Alternative treatments for bladder control often require repeat procedures, but the SNM device can last for many years
“SNM is typically a third-line option for patients who haven’t responded to conservative or medication-based treatments, but it can be life-changing, helping patients regain normal bladder or bowel function. Patients who undergo the SNM procedure often report dramatic improvements; some go from waking five times a night to not waking at all, or from being unable to void to emptying normally again.”
Shared decision-making is important, aligning treatment discussions with the expertise of the healthcare professional and the patient’s preferences. “Making patients aware of their treatment options is one of the most important parts of the consultation,” explains Barea. “Each treatment option has its pros and cons, and what’s right depends on the patient’s age, gender, lifestyle and the specific characteristics of their condition. Patient preferences are key, and treatment should be tailored to everyone’s needs.”
Raising awareness of potential treatment options can influence patient outcomes, whether through information aids such as leaflets or via online resources such as BAUS or BBUK, which ensure that patients fully understand their choices, feel supported in decision-making and can access the most appropriate therapies for their individual needs.


Inflammatory Bowel Disease (IBD), the umbrella term for Crohn’s Disease and Ulcerative Colitis, affects around 50,000 people in Ireland, yet remains one of the most misunderstood chronic illnesses.
These conditions cause persistent inflammation of the digestive tract, leading to symptoms such as severe abdominal pain, diarrhoea, fatigue, joint pain and weight loss.
IBD doesn’t discriminate by age. While most diagnoses occur between ages 15 and 35, we also see a second peak in later adulthood, and cases in children are rising. This means IBD can impact anyone at any stage of life, often striking during critical periods for education, career and family.
Hidden costs and stigma of living with IBD
Despite advances in treatment, there’s no cure for IBD, and its impact extends beyond physical health. A recent survey by Crohn’s & Colitis Ireland revealed that 52% of patients experienced a flare in the past year, and 35% reported stigma or unfair treatment. Alarmingly, 60% face financial hardship, spending over €3,000 annually on care, while nearly half delayed treatment due to cost. These figures underscore the urgent need for systemic change — from expanding medical card eligibility to recognising IBD under the Long-Term Illness Scheme.
The burden on our healthcare system is significant. Delays in diagnosis remain common, with 14% waiting more than a year for confirmation, and almost half presenting to A&E before being diagnosed. Beyond clinical care, mental health support and workplace accommodations are lacking, leaving many patients isolated and struggling to maintain wellbeing and employment.
Policymakers must prioritise IBD in national health strategies, employers must create inclusive workplaces and the public must stand with us to break the stigma. Strategic Account Manager: Lucy Harris lucy.harris@mediaplanet.com Managing Director Ellie
Media Manager: Jonni Asfaha All images supplied by Getty Images, unless otherwise specified
Call for urgent action and inclusive support
This week marks Crohn’s and Colitis Awareness Week (December 1–7), an opportunity to challenge misconceptions and advocate for better supports. Crohn’s & Colitis Ireland is leading the charge with education campaigns, peer support groups and resources for patients and families. We’re calling for investment in specialist services, equitable access to healthcare and public facilities that accommodate hidden disabilities. Policymakers must prioritise IBD in national health strategies, employers must create inclusive workplaces and the public must stand with us to break the stigma. Together, we can ensure that living well with IBD becomes the norm — not the exception
Urinary incontinence is the unintentional leak of urine and is a common problem affecting people of all ages. People should not suffer in silence, as healthcare professionals are there to help.

There are three types of urinary incontinence.
The first is called stress incontinence; this is the leakage of urine with exertion such as coughing, sneezing or exercise. This is more common in women and can especially be an issue after pregnancy or post-menopause. Urge incontinence is the second type; you might leak on your way to the bathroom or have the need to pass urine. This can be associated with an overactive bladder. Finally, there is mixed incontinence, which is a mixture of both types.
Who can I talk to about urinary incontinence?
A lot of people suffer in silence and can feel embarrassed or upset about their symptoms. However, it is important to know there are treatments that can help, and healthcare professionals are used to talking about this problem. If you are suffering from incontinence, discuss it with your general practitioner, see a urologist or urogynaecologist or see a chartered physiotherapist who specialises in pelvic health and continence. The Continence Foundation of Ireland
website contains helpful information and links to other websites and resources.
Incontinence management options
Management of incontinence usually starts with small lifestyle changes, such as reducing caffeine intake, fizzy drinks and alcohol, as these can irritate the bladder. It is important to see a healthcare professional, so any conditions that may worsen incontinence can be ruled out or managed, such as infections. Physiotherapy can also be helpful to re-train the bladder, strengthen the pelvic floor and reduce urinary symptoms. If these management options are not improving symptoms enough, some people may need medication or surgery to help. There are well-established guidelines with safe and effective treatments available to help with symptoms. Anyone who thinks they may have incontinence or urinary problems should not be embarrassed about asking for advice or treatment.
