






By Paul Hegyi
CALPAC, the California Medical Association Political Action Committee, works to elect candidates who share our vision for the future of health care in California, as well as to maintain relationships with these legislators once in office.
Please donate today by scanning the code with your smartphone or visiting: calpac.org/donate.

CALPAC is a voluntary political organization that contributes to candidates for state and federal office who share our philosophy and vision of the future of medicine. Contributions are not deductible for state or federal income tax purposes. More information available at CALPAC.org
Editor: William T–C Tseng, MD, MPH
Editorial Board: James Santiago Grisolia, MD; David E.J. Bazzo, MD; William T-C Tseng, MD; Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
Marketing & Production Manager: Jennifer Rohr
Art Director: Lisa Williams
Copy Editor: Adam Elder
OFFICERS
President: Preeti S. Mehta, MD
President–Elect: Maria T. Carriedo-Ceniceros, MD
Immediate Past President: Steve H. Koh, MD
Secretary: Karrar H. Ali, DO, MPH
Treasurer: Rakesh R. Patel, MD, FAAFP, MBA
GEOGRAPHIC DIRECTORS
East County #2: Rachel B. Van Hollebeke, MD
Hillcrest #1: Vikant Gulati, MD
Hillcrest #2: Stephen R. Hayden, MD (Delegation Chair)
Kearny Mesa #1: Anthony E. Magit, MD, MPH
Kearny Mesa #2: Dustin H. Wailes, MD
La Jolla #1: Toluwalase (Lase) A. Ajayi, MD
La Jolla #2: Audra R. Meadows, MD
La Jolla #3: Emily A. Nagler, MD
North County #1: Arlene J. Morales, MD (Board Representative to the Executive Committee)
North County #2: Phil E. Yphantides, MD
North County #3: Nina Chaya, MD
South Bay #1: Paul J. Manos, DO
South Bay #2: Latisa S. Carson, MD
AT–LARGE DIRECTORS
#1: Steven L.W. Chen, MD, FACS, MBA (Board Representative to the Executive Committee)
#2: Kelly C. Motadel, MD, MPH #3: Kyle P. Edmonds, MD #5: Daniel D. Klaristenfeld, MD
#6: Alexander K. Quick, MD
#7: Karl E. Steinberg, MD, FAAFP #8: Alejandra Postlethwaite, MD
ADDITIONAL VOTING DIRECTORS
Young Physician: Quinne C. Sember, MD
Retired Physician: Mitsuo Tomita, MD
Medical Student: Christina Noravian
CMA OFFICERS AND TRUSTEES
Trustee: Sergio R. Flores, MD
Trustee: Timothy A. Murphy, MD
Trustee: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
AMA DELEGATES AND ALTERNATE DELEGATES
District I: Mihir Y. Parikh, MD
District I Alternate: William T–C Tseng, MD, MPH
At–Large: Kyle P. Edmonds, MD
At–Large: Sergio R. Flores, MD
At–Large: Robert E. Hertzka, MD
At–Large: Theodore M. Mazer, MD
At–Large: Albert Ray, MD
At–Large: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
CMA DELEGATES
District I: Christopher M. Bergeron, MD, FACS
District I: Corrie D. Broudy, MD
District I: Mojgan Hosseini, MD
District I: Quinn K. Lippmann, MD
District I: Yolanda Marzan, MD
District I: Bijal V. Patel, MD
District I: Eric L. Rafla-Yuan, MD
District I: Ran Regev, MD
District I: Kristen N. Rice, MD
District I: Kosala Samarasinghe, MD
District I: Mark W. Sornson, MD
District I: Wynnshang (Wayne) C. Sun, MD
District I: Patrick A. Tellez, MD, MHSA, MPH
District I: Randy J. Young, MD
District I: Nicholas (dr. Nick) J. Yphantides, MD, MPH
RFS Delegate: Shawn A. Ali, MD
Opinions expressed by authors are their own and not necessarily those of SanDiegoPhysician or SDCMS. SanDiegoPhysicianreserves the right to edit all contributions for clarity and length as well as to reject any material submitted. Not responsible for unsolicited manuscripts. Advertising rates and information sent upon request. Acceptance of advertising in SanDiegoPhysicianin no way constitutes approval or endorsement by SDCMS of products or services advertised. SanDiegoPhysicianand SDCMS reserve the right to reject any advertising. Address all editorial communications to Editor@SDCMS.org. All advertising inquiries can be sent to DPebdani@SDCMS.org. SanDiegoPhysicianis published monthly on the first of the month. Subscription rates are $35.00 per year. For subscriptions, email Editor@SDCMS.org. [San Diego County Medical Society (SDCMS) Printed in the U.S.A.]


FEATURE


4 SDCMS and Healthcare: Year in Review By Paul Hegyi, MBA
DEPARTMENTS
2 Briefly Noted: Vaccines • SDCMS • Practice Management

10
Report From the AMA Meeting: Change and Challenges By Kyle P. Edmonds, MD, FAAHPM


12
8 Proven: Systemic Training on Best Practices Improves Dementia Screening By Daniel Sewell, MD

How Come Biden’s Staffers Couldn’t See What America Saw? A Case Study in Presidential Fitness and Staff Loyalty By James Santiago Grisolia, MD
14
Lap Swimming With the Chlorinated Merpeople By Daniel J. Bressler, MD, FACP
16
Medical and Dental Record Issues By Richard Cahill, JD
20
Classifieds
THE ADVISORY COMMITTEE ON Immunization Practices (ACIP) voted in December to end the universal hepatitis B birth dose.
California neonatologist Dr. Valencia Walker says since CDC started recommending the vaccine in 1991, Hep B infections in kids dropped from approximately 18,000 cases per year to roughly 20 cases per year.
California Medical Association (CMA) President Rene Bravo, MD issued the following statement on this disappointing change in policy:
“Today’s ACIP vote is a profound setback for child health in America. As a pediatrician and on behalf of the California Medical Association, I am deeply concerned that abandoning the uni-
THE SAN DIEGO COUNTY MEDICAL Society’s board of directors held its annual holiday party at Tom Ham’s Lighthouse in early December. We had a wonderful turnout and everyone enjoyed the delicious spread while getting into the holiday spirit.


versal hepatitis B birth-dose recommendation and recommending new tests before receiving all doses dismantles a policy that has protected infants for more than 30 years — with no new evidence to justify the change.
“Before universal vaccination began in 1991, nearly 18,000 U.S. children were infected with hepatitis B each year, half during childbirth; since then, we have seen a 99% reduction in childhood infections because the vaccine is safe, effective, and reliably delivered at birth. This decision ignores how devastating — and entirely preventable — hepatitis B truly is, and it threatens infants whose mothers’ screening is incomplete or delayed, and children who may be exposed in their communities. It also casts a pall over good science and sound public-health policy, sowing more doubt and fear among parents who look to their physicians for trustworthy guidance. We are, in effect, dismantling an intervention that has worked for decades and could help us eradicate hepatitis B — and we are doing so for no legitimate reason.”



AS THE NEW YEAR BEGINS, practices should verify patients’ eligibility, benefits, and deductibles to avoid denials and unexpected coverage gaps — especially with deductible resets, payer changes, and the loss of federal exchange plan subsidies.
Physicians are reminded to be diligent in verifying patients’ eligibility and benefits to ensure they will be paid for services rendered. The start of a new calendar year brings reset deductibles and renewed visit frequency limitations, and open enrollment may mean patients are now covered by a new payer. Additionally, the recent loss of federal subsidies for exchange plans may cause unexpected coverage changes for some patients, making eligibility verification more important than ever.
Do your homework before patients arrive by obtaining updated insurance information and verifying eligibility at the time of scheduling, if possible. It is also best practice to remind patients when they make an appointment that their plan has a de-
ductible that may be resetting on Jan. 1 and, if that is the case, that payment will be due at the time of service. It is also important to make copies of insurance cards when patients come in for their first visits of the new year. Failure to collect deductibles, copays and coinsurance at the time of service can be very costly for a practice, as your ability to collect can decrease significantly after the patient leaves the office.
Taking proactive steps to protect your practice by preventing denials, delays in payment, and disgruntled patients goes a long way toward ultimately saving time and money.
Please note: For 2026 the annual deductible for all Medicare Part B beneficiaries is $283, an increase of $26 from the 2025 annual deductible of $257. For Medicare Part A, the inpatient hospital deductible per benefit period is $1,736 in 2026, an increase of $60 from $1,676 in 2025.
Practices that serve Medi-Cal patients should also review upcoming 2026 eligibility changes that may affect adult immigrants.








O ENCAPSULATE A YEAR IN A FEW WORDS (OR even pages) can be challenging. I’m still overwhelmed by the impact of H.R. 1 and the reckless damage that will indiscriminately be done to healthcare in the name of extending some tax cuts.
And while that was the headline of 2025 in healthcare, it was not the only story.
A highlight of the year was AMA’s then President-Elect (President as of June) Dr. Bobby Mukkamala joining the SDCMS Board at our annual retreat in February. Just months earlier Dr. Mukkamala had received devastating news: He was diagnosed in November 2024 with an 8cm tumor, an astrocytoma, on the left side of his brain. He underwent surgery a month later. He acknowledged the advantages he has as a physician to get expert advice on treatment, and even being in his hometown of Flint, Mich., where he could get swift access to an MRI. For those who don’t live close to health systems, they can see much longer waits for the tests they need.
The visit not only allowed SDCMS’s leadership to hear Dr. Mukkamala’s story and his plans as the soon-to-be leader of AMA, it was an opportunity for him to learn firsthand about the concerns and priorities San Diego physicians have for our community. We highlighted the need to protect Medicaid (Medi-Cal here in California.)
Dr. Robert Hertzka and I joined CMA President Dr. Shannon Udovic-Constant and CMA CEO Dustin Corcoran in Washington, DC last spring as H.R. 1 was being taken up for initial committee vote. In a whirlwind trip we met with more than 20 members of the House and Senate, highlighting the dangers present in the legislation to patients and our healthcare system. While disappointed in the final results of the legislation, it is critical we keep sharing stories with our elected officials and help them understand the impacts of their policy.
We also strongly supported extending patient subsidies for the Affordable Care Act later in the year, with Dr. William Tseng taking a leading public role representing SDCMS and the California Medical Association.








Dr. Preeti Sonni Mehta took office as our 155th president in June at our annual Gala: Lighting the Way to Health. The event had the largest attendance of any gala in at least the last decade and raised critical funding for our charity, Champions for Health (CFH). During the evening we recognized Dr. Steve Koh for his service as the 154th president; Dr. William Tseng received the James T. Hay, MD Award; the Nursing and Wellness Department at San Diego Unified School District
By Paul Hegyi



Vargas.



















Investigation on Your Practice,” and “Anatomy of a Lawsuit on Your Practice,” with nearly 300 participants across the series. These educational opportunities were complemented by a series of physician socials, free to members and a guest, gathering more than 250 participants.
California wrapped up its 2025 legislative session on Oct. 12, sending 1,247 bills to the governor’s desk — just over half of the 2,416 that were introduced last year. Amid shifting political priorities and an ever-changing policy landscape, each year feels more chaotic and frenetic than the last, and 2025 was no exception. After years of roadblocks to prior authorization reform, CMA introduced four bills to reform the state’s prior authorization systems. CMA’s prior authorization reform package included common-sense reforms to streamline prior authorization processes, expedite critical care for patients, and free up physicians’ time to focus on patients, not paperwork. Ultimately, we were successful in sending two bills to the governor’s desk, SB 306 and AB 512, with the former signed and the latter vetoed. SB 306 gives the administration the authority to remove prior authorizations on a code-by-code basis, as well as to require reporting from the health plans to give us a better picture of how prior authorization is being deployed at the ground level.
After months of delay, California has finally begun moving forward with implementation of Proposition 35, the voter-approved measure to increase Medi-Cal payments and expand access to care. While the 2025–26 state budget included budget allocations that were contrary to those

required under Proposition 35, California Medical Association (CMA) advocacy and sustained pressure are now beginning to yield progress across four key areas, with the expectation of more to come. These include emergency department physician payments, family planning, an additional $75 million for graduate medical education expansion, and supplemental payments for emergency transportation services.
In the fall, Andrew Gonzalez joined the medical society leading our Physician Pathway Program. SDCMS is working to highlight and connect students and early-
Building.

Right: Dr. William Tseng speaks out on behalf of SDCMS and the California Medical Association calling for an extension of ACA patient subsidies. He joined U.S. Senator Adam Schiff and U.S. Representative Mike Levin at a press conference at TrueCare in Oceanside.

career learners with pre-health and health-career opportunities across San Diego County and beyond. We kicked off the effort with a new webpage (www.sdcms.org/pathway) featuring a curated list of programs, internships, academies, and enrichment opportunities designed to support individuals interested in becoming physicians or pursuing other health professions. Opportunities may include clinical exposure, mentorship, research, academic enrichment, or stipends, and eligibility varies by program.
We’re excited for a lot more from the Physician Pathway Program in 2026 as we seek to coordinate existing pathway programs; expand promotion and participation; help participants navigate appropriate entry and development opportunities; engage in structured mentorship within medicine; and seek ways to expand pathway programs within San Diego County.
This looks to be an intensive year of statewide ballot measures, with three ballot initiatives already placed on the November 2026 ballot by the legislature and another two dozen or so are at various stages of the qualifications process.

Included among those are:
• Compensation Limits for Healthcare Executives: Proposed by Service Employees International Union-United Health Care Workers West (SEIU-UHW), this would limit total annual pay for healthcare executives (excluding physicians who are currently seeing patients) at $450,000.
• Restrictions on Health Clinic Spending: Also by SEIUUHW, this would require clinics to spend 90% of total revenue on a vaguely defined “mission-related program expenses” and impose hefty fees on clinics that fail to meet the requirement.
• Billionaires Tax: Just introduced and backed by SEIUUHW and Jim Mangia (St. John’s Community Health), it would impose a one-time tax on California billionaires to fund healthcare programs. Governor Newsom has already come out against it — and rumor has it that Mangia wants his name off it.
• Healthcare Union Transparency: Another brand-new measure, brought forward by the California Hospital Association (CHA), this initiative would require large unions in the healthcare industry (namely SEIU-UHW and the California Nurses Association) to report yearly spending on political activities, including ballot measures. SEIU has pushed multiple ballot measures that impact CHA over the years, including the aforementioned “Compensation Limits for Healthcare Executives.”
We will be following these measures closely and be certain to keep you informed.
Paul Hegyi is the chief executive officer of the San Diego County Medical Society.


By Daniel Sewell, MD
IT SHOULD COME AS NO SURPRISE TO ANY PHYSICIAN that training on best practices followed by EMR support in applying these practices will improve patient outcomes and provider competence. But in order to affect systemic change in San Diego County’s healthcare systems, we felt we had to prove it. And we did.
The Alzheimer’s Project Clinical Roundtable (APCR) has been working since 2014 to develop, establish and update standards of practice for the screening, evaluation and diagnosis, and care management of individuals with cognitive concerns and dementia. Physicians from every health system in our county contributed to their development and are now advocating for the broad application of these standards. The Clinical Roundtable’s efforts have been noticed and adapted at the state level and by organized medicine throughout the country.
A major reason for creating these clinical guidelines was the rapidly increasing number of individuals 65-plus, and particularly 85-plus, resulting in a rapidly growing number
consistent way to screen for potential dementia that would fit into their busy clinical practices.
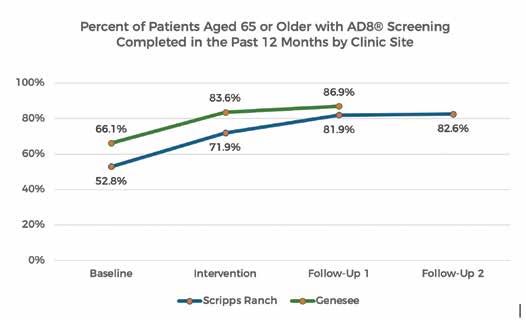
To build a case for the benefits of dementia care best-practice standards, we launched a small-scale research study at two UC San Diego family medicine clinics, resulting in statistically significant improvements in physician comfort and competence in their clinical practice, and a significant increase in the number of patients with cognitive concerns who were appropriately screened and provided follow-up care.
of individuals with cognitive decline alongside the inadequate number of specialists to whom primary care providers (PCPs) might refer these individuals. PCPs daily see older adults with high blood pressure, diabetes, and other chronic diseases, and are best able to spot cognitive changes. Likewise, they will be the providers caring for the behavioral issues that may ensue over the 10 to 15 years of disease progression. So the guidelines were created to provide PCPs a quick and
As we had conducted numerous grand rounds and virtual trainings for physicians in San Diego County since 2017 when the guidelines were initially published, the use of a truly pure “control group” composed of physicians with no prior exposure to the educational programs and dementia care best practices created by APCR was not possible. So instead, the study was designed using a comparison group of clinicians who did not receive the training provided to physicians who were in the study (the intervention group). We were pleased to see that at four different time points over the course of the study the subjective assessment of the comfort and competence of clinicians in working with patients with cognitive complaints increased and that comfort and confidence was higher for intervention group PCPs than the comparison group PCPs. Dementia screening at both clinics
increased from baseline to post-intervention: 52.85 to 82.6% for clinic 1 and 66.1% to 86.9% for clinic 2.
The APCR created and subsequently updated eight on-demand webinar trainings on screening, evaluation, behavioral management, medications, and care planning; these units are all credentialled for both AMA and ANCC continuing education credits. PCPs in the intervention group were required to view these webinars and rated them highly. One-hundred percent said they were satisfied with the level of training they received. (These modules are available to all providers throughout the county at no cost, thanks to the partnership between Champions for Health and The Doctors Company.)
In addition to building comfort and competence on dementia screening and evaluation, the training also increased communications skills with patients and family caregivers, and statistically increased comfort in referring patients and families to community resources. In prior surveys of primary care providers, lack of information on community resources was a consistent concern of physicians.
One important component of the study was building enhancements into the electronic medical record system to prompt providers on the step-bystep evaluation process. Many health systems have not been able to track easily whether a screening
has been done or disease progression has occurred based on changes in serial patient screening scores.
At the two UC San Diego Family Medicine clinics, all screening and evaluation instruments are now included as smartphrases with specific fields for scores; physicians no longer have to hunt through notes to find the information they need. Banners were added to alert providers if their Medicare Annual Wellness Visit patient-completed AD8 results require follow-up. Smart order sets make follow-up significantly easier. For example, providers are able to quickly click for caregiver information and lists of community resources to be added to the after-visit summaries. Relatively limited time for care provision continues to be an issue in primary care practice as most physicians can relate. It is challenging to address all the needs of older adult patients, particularly those with com-
munication or cognitive deficits, in short appointment slots. It is recommended that a separate appointment for cognitive screening, and particularly evaluation, be established, however we recognize that getting patients to return for follow-up appointments can also be challenging. The current Medicare billing standards for cognitive assessment and care planning do allow for billable one-hour visits and encourage progressive appointments. The billing code can be used twice each year, which should assist with these time concerns.
We are hopeful the results of the study will create urgency at both the clinician and system levels to utilize these bestpractice guidelines to insure optimal screening, evaluation and diagnosis, and care management for our rapidly growing population of older adults facing memory concerns. While we are not advocating for annual universal screening of everyone 65 and older, the increasing number of individuals and their family members expressing concerns about memory and cognition is sufficient to keep primary care providers busy.
All of the resources created for providers and for patients and their family caregivers are available on the ChampionsforHealth.org/alzheimers website. We hope you will download information, include handouts in your after-visit summaries, and avail yourselves of the rich educational content developed through the SDCR for your benefit.
Dr. Sewell is a retired geriatric psy chiatrist, professor emeritus in the Department of Psychiatry at UC San Diego, former medical director of the UC San Diego Health Senior Behavioral Health Program, and a member of the Alzheimer’s Project Clinical Roundtable Executive Committee.

By Kyle P. Edmonds, MD, FAAHPM

I don’t go to AMA meetings to be surrounded by people who agree with me. I go to sit shoulder-to-shoulder with the sometimes unruly family of medicine — because that’s how we move forward, a little at a time. Progress isn’t loud or flashy; it’s incremental, forged in debate and compromise. This year’s Interim Meeting in National Harbor, Md., reminded me why that work matters.
The meeting opened with a milestone: welcoming John J. Whyte, MD, MPH, as the new CEO of the AMA. In his first address to the House of Delegates, Dr. Whyte struck a tone of urgency and unity: “The future of the AMA is not something we wait for,” he said. “It’s something we shape — with urgency and unity.”
Dr. Whyte acknowledged the headwinds physicians face: administrative burdens, burnout, workforce shortages, and the disruptive rise of generative AI. His blueprint for the AMA centers on three pillars:
• Cutting Red Tape: Strengthening advocacy to reduce prior authorization and restore physician autonomy.
• Defending Science and Trust: Elevating evidence-based policy and combating misinformation in an era of politicized healthcare.
• Investing in Physician Wellbeing: Treating burnout not as an afterthought but as a moral and strategic priority. “We are not bystanders. We are architects,” Dr. Whyte told delegates, pledging to make the AMA a beacon of integrity and a powerful ally for physicians.
What could you do with $50,000? The AMA’s Community Health Impact Lab is betting that small, strategic investments can spark big change. Through its new micro-grant program, the AMA will fund physician-led projects tackling urgent local health challenges — from food insecurity and maternal health to caregiver support and chronic disease management.
The goal is simple: empower physicians to innovate where they live and work. These grants aren’t about bureaucracy; they’re about agility, creativity, and impact. For physicians frustrated by systemic barriers, this is an opportunity to lead solutions that matter.
Learn more and apply here: https://www.amaassn.org/amaone/community-health-impact-labmicro-grants.
Healers and Warriors: Bobby Mukkamala’s Call to Action
AMA President Bobby Mukkamala, MD, framed his remarks around a challenge: “Let us be healers, yes, but let us be warriors when necessary. Warriors when we need to fight — for our patients, for our colleagues, for the future of medicine.”
Dr. Mukkamala celebrated the diversity and unity of the House — nearly a thousand physicians from every state and specialty — and highlighted advocacy wins since June:
• Medicare Payment Reform: Amplifying calls to fix a system plagued by 25 years of declining rates.
• Standing Against Intrusion: Opposing government interference in exam rooms and reaffirming the importance of immunization.
• Championing International Medical Graduates: Fighting exorbitant H-1B visa fees that threaten an already strained workforce.
He reminded us that advocacy is not just about resistance — it’s about collaboration and progress. Recent successes include modernizing e-prescribing and pushing for ethical, physician-led integration of AI into care delivery.
Beyond speeches, the House advanced policies that matter across specialties:
• Prior Authorization Reform: Eliminating requirements for low-cost medications and procedures.
• Rural Health Sustainability: New payment models to keep hospitals viable in underserved areas.
• Community Health Innovation Grants: $1 million in micro-grants for physician-led projects addressing local health challenges.
• Digital Health and AI Leadership: Launching a Center for Digital Health and AI to ensure technology serves — not supplants — the physician-patient relationship.
The Interim Meeting drew significant attention for the keynote address by CMS Administrator Mehmet Oz. His remarks emphasized reducing bureaucracy and restoring physician autonomy, framing these issues as central to revitalizing the profession. However, the presentation included assertions about Medicaid utilization, the One Big Beautiful Bill Act, and ACA subsidies that were widely viewed as lacking nuance and context.
While the speech was positioned as a call to action, it employed a rapid-fire sequence of loosely connected assertions — overwhelming the audience with volume rather than depth. This approach, combined with selective framing of facts, appeared designed to divert attention from areas of substantive policy disagreement and to recast the narrative in terms more favorable to the Administration’s agenda. He made assertions regarding patient behavior — such as television viewing habits among Medicaid beneficiaries — that risked reinforcing stereotypes rather than advancing constructive dialogue on systemic reform.
The AMA responded promptly, clarifying its commitment to evidence-based policy and rejecting proposals that would reduce coverage or access for vulnerable populations. Dr. Mukkama’s statement included, “we will remain engaged where we have differences: opposing Medicaid cuts, advocating for a permanent Medicare payment fix that reflects the cost of running a practice, and preventing coverage loss while rooting out fraud.” I hope this underscores the AMA’s role as a stabilizing force amid rhetoric that can polarize rather than unite.
In many ways, the AMA House of Delegates feels like a family meeting I might have in the hospital — messy, passionate, and full of competing priorities. Anyone who has ever sat with a family struggling to make decisions knows this dynamic well. It’s not about winning every argument; it’s about listening, finding common ground, and moving forward together. That’s how we move forward — one conversation, one compromise, one patient at a time.
Dr. Edmonds is an inpatient palliative physician in the UC San Diego Palliative Care Program and has been active at the AMA since he was a first-year medical student. He is a delegate to the AMA House of Delegates from California. He offers his usual disclosure that he’s not impartial when it comes to AMA Trustee Dr. Lasé Ajayi, since the two have been married for many years.


By James Santiago Grisolia, MD
KARINE JEAN-PIERRE, PRESIDENT BIDEN’S FORMER press secretary, is suffering in the midst of a famously blinkered1 promotion tour for her memoir, Independent: A Look Inside the Broken White House. Her confused defense of former President Biden’s cognitive status echoes other Biden staffers’ defenses, ranging from “he was just fine” to “normal aging.” Yet the American people saw a very different Joe Biden in his CNN debate with Donald Trump on June 27, 2024. Rapid-fire accusations, even prevarications, completely overwhelmed Biden’s ability to defend or counter-attack, and the American public clearly saw a president who could not deliver the quick responses of political debate. This abject performance crystallized prior concerns about his evident frailty, the tectonic shift trig-
gering the rising wave that forced him to step down as his party’s nominee. So why couldn’t JeanPierre and his other staffers see what America could see so plainly? Republicans quickly advanced conspiracy theories, protecting Biden from exposure out of personal loyalty or baser motives.2 Certainly many other American presi-
dents have had important health conditions which were covered up: strokes for Woodrow Wilson, polio for Franklin Roosevelt, heart attack for Dwight Eisenhower, Addison’s and chronic pain for John F. Kennedy, and Alzheimer’s for Ronald Reagan.3 Accusations of lack of medical transparency also surround the Trump White House.4
Normal aging in the human brain affects many functions, changes which vary in intensity among normals, but are intensified in neurodegenerative conditions. Most importantly, healthy oldsters begin to lose spontaneity and ability to generate rapid, inventive, and multiple responses. Processing speed declines, as does mental flexibility. In contrast, long-term knowledge and habit patterns remain relatively preserved, so-called “crystallized intelligence” in neuropsychological parlance.5
In the case of Joe Biden, we have no detailed medical information, only video evidence of his increasing frailty and physical instability, as well as White House records of visits by a Parkinson’s specialist.6 Nevertheless, Biden’s successes and even some perceived failures can be readily explained by a long career archived in crystallized intelligence.
When Russia attacked Ukraine, Biden immediately perceived the threat to European and American security and rapidly rallied Western governments to support Ukraine. His alac-
rity was reasonably explained by long experience with Putin, with Western and Eastern Europe, and personal experience with many foreign leaders. His success in passing the Inflation Reduction Act, as well as landmark environmental and infrastructure legislation, depended on crystallized knowledge of the workings of Congress and personal relationships with many members. Even the chaotic U.S. withdrawal from Afghanistan, among the greatest failures of the Biden administration, may be considered a failure of crystallized intelligence, in Biden and his administration’s uncritical acceptance of the prior administration’s flawed 2020 Doha Agreement with the Taliban without considering new conditions on the ground or rethinking diplomatic and military alternatives.7
Clearly, at least some Biden staffers viewed his mental changes as part of normal aging. For example, in a New Yorker interview, Jean-Pierre said the following: “No one is saying that he didn’t age, but he is someone that I engaged with. I saw him every single day as his White House press secretary, and he was someone that was engaged, on top of policy, challenging his staff.”8
When queried about his debate performance, she replied, “The debate for me was one time. I had never seen him like that before.”
Apart from concerns about his lack of sleep or a possible viral syndrome9, the debate with Donald Trump savagely exposed Biden’s weaknesses. Rapid verbal responses were needed, often to unexpected or even counterfactual assertions from Trump. Viewers expected a rapid, fluent delivery, while Biden’s lifelong stammer was now hampered by reduced verbal fluency and slower processing speed. The debate forced Biden to play verbal speed chess, with every word and gesture scanned by millions of viewers.
Normal aging of the human brain happens at different rates in different persons, with potential acceleration by any neurodegenerative condition. White House staff, personally loyal to Biden and untrained in medicine, appreciated his daily judgements in unhurried meetings, while dismissing his public frailties as normal aging. A lifetime’s experience in foreign and domestic policy informed his daily judgements. The American public, little exposed to his private deliberations, saw him as frail and inarticulate under pressure of timely responses on the public stage. Any accentuation by Parkinson’s or related conditions will await eventual disclosure of specific medical records.
Personal loyalty and keeping a united front against opponents, both domestic and international, warred in the hearts of Biden’s staffers with providing optimal leadership for the nation. This conflict doubtless informed the other presidential cover-ups cited earlier. Our 25th amendment to the U.S.
Constitution was passed in the wake of the JFK assassination and was poorly designed to deal with mental infirmity.10 Both the vice president and a majority of the cabinet must approve removal, and a complex Congressional process ensues if that removal is contested by the sitting president. Now that President Trump is also aging, these questions demand our continued concern.11
References
1. Karine Jean-Pierre and a Book Tour Most Authors Would Not Dream Of, NY Times, Oct 29, 2025
2. Original Sin: President Biden’s Decline, Its Cover-Up, and His Disastrous Choice to Run Again Hardcover. Jake Tapper, Alex Thompson. Penguin. May 20, 2025
3. 5 Presidents Who Hid Their Health Issues. Ryan Mattimore. History.com. https://www.history.com/articles/5presidents-who-hid-their-health-issues
4. Rep Crockett Launches Investigation into the Administration’s Cover-Up of President Trump’s Failing Health. https://crockett.house.gov/media/press-releases/repcrockett-launches-investigation-administrations-coverpresident-trumps
5. The Impact of Age on Cognition. Daniel Murman. Semin Hear 2015; 36(03): 111-121
6. Parkinson’s Expert Visited the White House 8 Times in 8 Months. Emily Baumgaertner and Peter Baker. https:// www.nytimes.com/2024/07/08/us/politics/parkinsonsexpert-white-house.html
7. U.S. Review of chaotic Afghanistan withdrawal blames Trump. Zeke Miller and Norman Merchant, Associated Press, reported in PBS News, Apr 6, 2023.
8. Why Biden’s White House Press Secretary is Leaving the Democratic Party. Isaac Chotiner. New Yorker. October 27, 2025.
9. Biden Has a Cold, Sources Say. Alex Gangitano. The Hill https://thehill.com/homenews/campaign/4744889-joebiden-has-a-cold-debate/
10. 25th Amendment unlikely to be invoked over Trump’s mental health. Josh Gerstein. Politico, Jan 7, 2018. https:// www.politico.com/story/2018/01/07/trump-25th-amendment-mental-health-327503
11. ‘He has trouble completing a thought’: bizarre public appearances again cast doubt on Trump’s mental acuity. Adam Gabbatt. The Guardian Aug 3, 2025. https://www.theguardian.com/us-news/2025/aug/03/ donald-trump-mental-fitness
Dr. Grisolia is a general neurologist at Scripps Mercy Hospital. He is a longstanding member of the San Diego County Medical Society, a former SDCMS Communications Committee chair, former editor of San Diego Physician , and a former California Medical Association Trustee.

By Daniel J. Bressler, MD, FACP
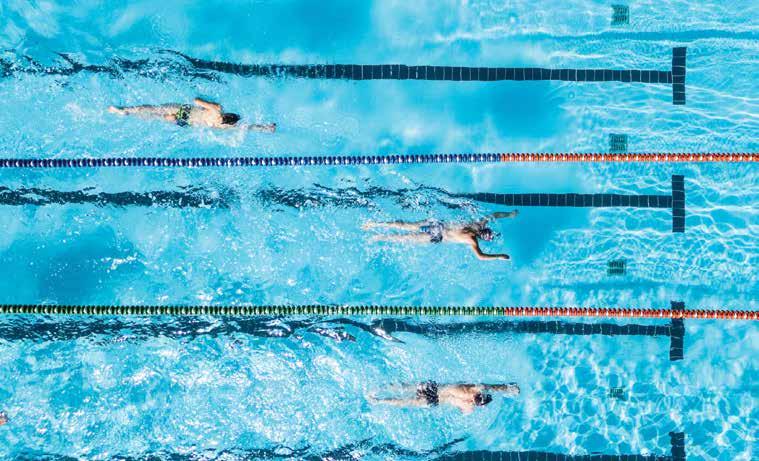
WHEN I GRADUATED FROM USING A WALKER TO A hard external knee brace after the deftly delivered intra-articular steroid given to me by Dr. M, I still had remarkable pain and an obvious gait deformity. I could bear enough weight to ambulate using only a cane. The shot allowed my acutely torn menisci to stop releasing inflammatory cytokines and permitted the knee to bear more of its assigned weight. I no longer had to be driven to the office by my dutiful nurse and the walker could be folded away.
I wish I had a better “war story” for this injury. It was due to pickleball + stubbornness + a missed hose + a gopher hole. The pickleball is the most defensible: playing doubles with my 31-year-old son as my partner at a pickup court near the harbor. We had a streak of luck defeating a run of worthy opponents (mostly my son’s doing) which allowed us to stay on the court for about six straight matches. I felt fine going home but the next day the knee was both stiff and sore. There was no swelling or redness, and no extreme joint tenderness, so I figured I should just lay off the pickleball but keep walking the 2-mile roundtrip to work and back. No “rest and ice.” Just “walk and wait.” My inflated ego wouldn’t allow me to baby the knee. So when it didn’t get better (or rather got gradually worse) over the next few weeks, I again insisted it would just take more time and more walking. Then there was the frontyard hose I tripped over in the twilight (acute exacerbation No. 1) and then a head-in-the-clouds misstep into a gopher
hole while walking Vanna, our Tibetan terrier (acute exacerbation No. 2). By now, the knee was howling, swollen, and wouldn’t allow me to bear weight. Maximum dose Tylenol plus celecoxib kept me barely functioning.
The MRI unsurprisingly showed tears in both my lateral and medial menisci. Dr. M’s steroid shot gave me about 50% relief within 24 hours. We discussed getting surgery in the next few weeks to prevent accelerated joint degeneration. In the meantime I had to get some exercise so as to not go crazier. That’s how my investigations brought me to learn about The Bud Kearns Municipal Pool in Balboa Park.
William A. “Bud” Kearns had been the recreation
Lap swimming is part meditation and part marathon. In the first few minutes, my mind darts between the day’s patients, my to-do list, family matters and news of the world. Over the course of the swim, thoughts tend to slow down and simplify to the here and now.”
director for the City of San Diego in the 1920s and ’30s. He was especially keen on expanding aquatic sports for our citizens. The pool that now bears his name was constructed at its current site in Morley Field in 1933. It is open every day except Sunday. Two dollars and twenty-five cents, the cost of admission for those over 60, buys me access to this gem, this resource,
this conduit. The shallow end is reserved for kids getting lessons. The deep end most afternoons is home to water polo practice happening under the gaze and scolding bullhorn direction of a no-nonsense coach. Between these two ends are the 15 lanes, roped off with stringed buoys, for me and the other lap-swimming chlorinated merpeople.
In myths from around the seafaring world there exists a fabled species that is half-human and half-fish. Mermaids are the female and mermen the male version of this creature. In some stories (particularly Celtic and Norse), seductive mermaids lure sailors to their watery deaths. In others, including African and Japanese, the merpeople
can be either benevolent or dangerous. In the antiquated outdoor locker room, the mermen with whom I change from street clothes into swim gear come in every age, shape, size, and color. Some are stout and have come to burn calories and drop weight. Some are trim and have all the cool gear that mark them as former competitive swimmers, there to maintain their skill and times. Some — like me — are the limping-wounded, removing our knee and ankle braces and stashing our canes before doffing our swimsuits. Undoubtedly, a similar scene happens in the women’s locker room.
After the mandatory preswim shower, we merpeople make our way up the concrete ramp to the pool area. We then enter the water in a variety of telling ways. Some tentatively descend at the shallow end using steps and the hand rails (as I did for the first months so as to offload my bad knee). Some squat, sit and twist their way directly into their claimed lane. Others jump or dive in from the smooth coping of the concrete border. All of us arrive into a lane that is temporarily our private and sequestered aquatic habitat. The former competitive swimmers propel themselves with more speed than do the rehabilitating lame and the weight-loss seekers, but, remarkably, once in the water all the merpeople possess a kind of similar grace. All of us find ourselves in a world of relative weightlessness and frictionlessness compared to our terrestrial
lives. The forgiving water supports us and transforms us, for a while, into this other version of ourselves.
The water is heated to a Goldilocks-level 81 degrees Fahrenheit, the temperature used in Olympic and NCAA competitions and the same temperature recommended by the American Red Cross for exercise swimming to minimize both stress and overheating. It is a level that is at once enlivening and comfortable. And while swimming laps, the fewer distractions the better. The focus is on breathing, form, and adjusting intensity to ambition and stamina. By trial and error, I’ve acquired my own hacks to help that focus: short haircut, tight-fitting goggles, truncated flippers, and a tight rubber finger cot to keep my wedding ring from sliding off.
Lap swimming is part meditation and part marathon. In the first few minutes, my mind darts between the day’s patients, my to-do list, family matters and news of the world. Over the course of the swim, thoughts tend to slow down and simplify to the here and now. How are my shoulders holding up? How is the balance of propulsion between my legs and my arms? Am I hyperventilating or underbreathing? Ultimately I aim for the simplicity of a machine tasked with conveying my animal consciousness back and forth across this waterpath for no reason whatsoever. At some point either my tired muscles or the numbers on my diver’s watch tell me I’m done for the day.
Exiting the pool is not as easy as I remember as a kid growing up in Southern California. But after a lap session (which has grown over the course of my adventure from 10 minutes to 60) I somehow push my body high enough to tuck my good knee onto the concrete deck, and eventually rise to standing as my body reacquaints itself with standard gravity. From there I shuffle in my sandals down the ramp, rinse off in the blessedly-warm shower, and then change back into my landlubber clothes.
My endorphins stay high for at least an hour after each session. My knee is slowly healing. After a few months of swimming twice a week, I have been able to ditch the knee brace. I have decided to hold off on surgery for now. I have also decided to continue to incorporate swimming into my life. The water is kept at 81 degrees during both summer and winter. It is obviously more of a challenge getting in and out during a chilly winter than it was in July — but I’m thinking a regular, temporary transformation into a lap-swimming chlorinated merman that has been so good for my knee will be good for the rest of me as well.
Dr. Bressler has been practicing internal medicine in San Diego since 1984. During his career he has taught medical students and residents and also chaired various hospital commit tees. He is currently affiliated with Scripps Mercy Hospital and Mission Hills Post Acute Care.


Frequently Asked Questions
By Richard Cahill, JD
Medical and dental records are essential to the delivery of care and play a crucial role in all clinical operations, including communicating vital information to other treating practitioners. The following information provides answers to questions that we frequently receive from members.
Does the patient record include financial information, such as billing and insurance data?
Financial information, including medical and billing records, is part of the designated record set as defined by HIPAA (45 CFR § 164.501). Such materials are often requested by CMS as well as third-party private payers when auditing documentation submitted to request reimbursement. Financial information, which should be kept separate from patient care entries, is not part of the legal health record (a subset of the designated record set). Follow a consistent policy on what is released as part of the legal health record for all patients who request a copy of their medical or dental record. Healthcare providers should periodically review their internal policies and procedures to ensure that they are current and consistent with existing rules and regulations and third-party payer agreements.
How long should patient records be kept?
You must follow federal and state-specific laws, administrative code regulations, and guidelines. Failure to follow these requirements and guidelines may negatively affect your ability to defend yourself in a civil action or administrative investigation if an adverse event occurs.
Professional licensing boards, professional associations, and specialty societies may also be able to provide information on state statutes, administrative code provisions, policies, or recommendations on patient record retention. If no federal or state statutory requirements exist and reference to secondary resources is not sufficiently instructive, The Doctors Company recommends the following:
• Adult patients: 10 years from the date the patient was last seen
• Minor patients: 28 years from the patient’s birth
• Deceased patients: Five years from the date of death
For a more detailed discussion of record retention, see The Doctors Company’s article “Medical and Dental Record Retention.”
Is information stored in other formats — such as videos, X-ray films, ECG recordings, fetal monitoring strips, photos, paraffin tissue blocks, and dental models/casts — part of the patient record?
Yes. Regardless of the format, any and all data collected at the time of a patient encounter is part of the healthcare legal document. Retain computerized and physical 3D models used for surgical and dental treatment plans according to the same retention schedule.
It is recommended that you check with your business attorney or state professional licensing board for details regarding retention laws on billing and insurance records—especially as the laws may relate to Medicare or Medicaid patients. For example, CMS requires Medicare managed care providers to retain records for 10 years, and the Internal Revenue Service requires billing records to be retained for seven years.
How long should patient telephone calls and messages, email or text messages, and scheduling records be kept?
Electronic messages play an important role in evaluating patient care and helping to achieve optimum clinical results. For these materials, The Doctors Company recommends the following:
• Document in the patient record all telephone calls and messages and email or text messages that pertain to patient care, and keep the documentation according to the above-referenced record retention guidelines.
• Keep patient scheduling records for one year.
If I obtain copies of records from a patient or another practitioner, am I required to maintain them?
Review, extract, and copy any information that might be needed from that record for accurate patient diagnosis or treatment. The retained information or documentation is then incorporated into the patient’s permanent office record. Be aware that keeping all of the patient’s records could make the healthcare professional inadvertently liable for information related to other specialties. If the information is not used for patient care, promptly and timely destroy it or return it to the source.
How should patient records and other associated media (such as photos, digital images, CDs, paraffin tissue blocks, and films) be destroyed?
Any destruction method must maintain the confidentiality of the information, and the methodology must be consistently applied by the practice. The only safe methods for destroying
paper records are incineration and shredding. A destruction method for electronic media must render the information unreadable. Professionals must be mindful that metadata can often be retrieved and reproduced for inspection by IT experts. Simply deleting the record is not sufficient. Use a reputable company to destroy paper and electronic information, models/casts, and equipment, such as computers and copiers. Keep a log of the records destroyed, when, and by whom.
What are considerations for the long-term storage of inactive patient records?
Inactive records that have been kept for the required or recommended time may be thinned from the active patient cases. Take the following factors into consideration when arranging long-term storage:
• Privacy. Will the records be protected from unauthorized disclosures in a manner that is consistent with federal and state privacy laws?
• Safety. Will the records be physically secure and protected from fire, flood, or other damage, and from unauthorized access or theft?
• Accessibility. Will the records be easy to retrieve and copy?
May I transfer paper records to an electronic format?
Yes. The factors in the previous question on privacy, safety, and accessibility can also guide you on transferring records to an electronic format. Any protected health information (PHI) transferred or stored electronically must be encrypted. Back up computer data at regular intervals and store it offsite.
Is it sufficient to back up a copy of an EHR onto an external storage device or in the cloud?
Yes, best practice is to perform a backup every evening to the cloud or to a separate server stored in another physical location. Establish a schedule and periodically assess the backup function to help ensure compliance with federal and state requirements. All PHI stored electronically must be encrypted. If you use an application service provider — where your data is stored by the EHR vendor and you access it online — confirm that your contract includes terms that guarantee your data will be available to you when you are ready to arrange for longterm storage or in connection with legal proceedings.
May I thin and purge patient records prior to storage?
Yes. Copies of other healthcare practitioners’ records that are not directly related to your care, such as hospital records, may be purged because the originals will be maintained by the hospital. Keep records from other practitioners that are directly related to your care and are maintained as a regular part of your record for the same period that you retain your own records.

May I sell my records when I sell my practice?
Yes. We suggest that you include the recommended retention time and access capability as part of your sales agreement. For more information, see The Doctors Company’s guide Closing or Relocating a Healthcare Practice.
If I move to another state, may I take my records with me?
Yes, with the same conditions for retention and accessibility that prevail in a sale. It is reasonable to alert the patients in your active/current caseload — through individual letters or emails, electronic notification in the patient portal, reference on your website, or an advertisement in a publication of general circulation in the community — about your move, in order to give them ample opportunity to request a copy of their records.
If a patient requests a copy before I move or close my practice, may I hand over the original record?
No. The original documentation is the property of the healthcare professional, who has a legal duty to maintain
the record. The patient should be given a copy upon written request, preferably using a HIPAA-compliant authorization signed by the patient or their legal representative. The practitioner should never relinquish custody of the original record.
Are healthcare professionals permitted to complete record documentation from home?
The only time an active, original paper patient record should be out of an office is when it is required to be present in a judicial proceeding or pursuant to a lawful court order. Any access to electronic records while away from the office must be through an encrypted, HIPAA-compliant format.
What should I do if someone claiming to be a representative of a deceased patient’s estate requests a copy of the record?
You must first verify through your own records or from a certified death certificate issued by the appropriate public entity that the patient has expired. Then, ensure that the individual requesting the record is a qualified representative of the decedent’s estate (for example, the executor). The individual should provide a copy of an official document from the state
as proof, and the record request should be in writing and signed by the individual acting as the estate’s qualified representative. Additionally, the person requesting the records should present proof of identity through a valid passport or government-issued REAL ID.







The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each healthcare provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Reprinted with permission. ©2025 The Doctors Company (thedoctors.com)
Richard Cahill is vice president and associate general counsel at The Doctors Company.


CRANIO/MAXILLOFACIAL AND HEAD & NECK
SURGERY: Accepting new adolescent and adult patients seeking evaluation and management of head and neck masses, multidisciplinary assessment of oral/ facial cancers and reconstruction, nasal airway assessment and functional rhinoplasty, corrective jaw surgery including jaw advancement for obstructive sleep apnea, cleft and craniofacial reconstruction, maxillofacial fracture management and secondary facial and jaw reconstruction. We work with Medicare, Tricare, most PPO insurance plans, and some HMO plans. Referrals may be called in to (619) 452-7332, or emailed to jaw@ scrippshealth.org. [2887-0808]
VIRTUAL SPEECH THERAPY AVAILABLE: Accepting new pediatrics and adult patients. We accept FSA/ HSA, Private pay, Medicare, Medi-Cal, and several commercial insurance plans pending credentialing. Visit virtualspeechtherapyllc.org or call (888) 855-1309.
PSYCHIATRIST AVAILABLE: Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla & San Diego. Visit hylermed.com or call (619) 707-1554.
PHYSICIAN OPPORTUNITIES
PULMONOLOGY PHYSICIAN | PHMG NORTH COUNTY: Palomar Health Medical Group is seeking a board–certified Pulmonology/Critical Care Physician to join our multi–specialty, not–for–profit practice in North San Diego County. The ideal candidate will offer expert pulmonary care in a comprehensive outpatient and inpatient setting, supported by advanced facilities at Palomar Medical Center Escondido and Poway. Responsibilities include diagnosing and treating a wide range of pulmonary conditions, performing both inpatient and outpatient procedures, and collaborating with specialists across the Palomar Health network. Candidates must hold a valid California medical license, be board–certified in Pulmonology, and preferably have at least two years of clinical experience. Per diem roles are also available, offering competitive pay and flexible scheduling. Join us in reimagining healthcare with compassion and excellence. To apply, send your application and CV to clayton.trosclair@palomarhealth. org. [2893-1015]
UCSD DEPARTMENT OF FAMILY MEDICINE | FACULTY POSITIONS AVAILABLE: UCSD Department of Family Medicine seeks motivated faculty to join our team in clinical, teaching, and scholarly roles. Faculty participate in comprehensive patient care, resident and fellow education, and research or quality improvement initiatives. We welcome candidates with diverse experiences and a passion for family medicine, community engagement, and academic medicine. Opportunities are available at various academic ranks, with salary commensurate with experience, rank, and step. Join a collaborative, supportive environment committed to excellence in primary care and education. Apply here: https://apol-recruit.ucsd.edu/JPF04341. [2889-0822]
OB/GYN PHYSICIAN | PHMG ESCONDIDO: Palomar Health Medical Group is seeking a full–time, board–certified/eligible Obstetrics and Gynecology Physician to deliver comprehensive reproductive care, including labor and delivery management, gynecologic surgeries, and OB call rotations. The ideal candidate will possess strong surgical skills, California licensure, and a commitment to maternal health. We offer competitive compensation, performance–based incentives, and a collaborative team environment. Please email CV to clayton.trosclair@palomarhealth.org or phil. yphantides@phmg.org. [2882-0626]
FAMILY MEDICINE/INTERNAL MEDICINE PHYSICIAN | PHMG RANCHO PENASQUITOS: Palomar Health Medical Group is seeking a Family Medicine or Internal Medicine Physician (MD/DO) to join our multi–specialty practice at our Rancho Penasquitos clinic location. Experienced physicians and new graduates
are encouraged to apply. Clinic schedule is Mon–Fri, outpatient only, no weekends or holidays. We offer competitive salary of $300k/year or more depending on experience. In addition, we offer productivity and other bonuses, PTO, CME reimbursement, health, dental, vision insurance, participation in 401K with partial employer match, short and long–term disability, and life insurance. Student loan repayment assistance is also available. Join Palomar Health Medical Group, where we’re reimagining healthcare with compassion, excellence, and integrity. Please email CV to clayton. trosclair@palomarhealth.org or phil.yphantides@phmg. org. [2881-0626]
FAMILY PRACTICE | INTERNAL MEDICINE PHYSICIAN: La Jolla Village Family Medical Group is seeking a PT/FT primary care physician to join our well–established private practice. We’ve been caring for our La Jolla/UTC area neighbors for 35+ years providing comprehensive, longitudinal care to patients of all ages. Call responsibilities are minor; hours consistent with a healthy work/life balance. Our office is new, clean, modern, and well–appointed. Our clinical team is collegial, passionate, and close–knit, with a supportive, cohesive support staff. A true private practice where physicians practice artfully and build enduring relationships with patients and colleagues. Seeking a Board–certified, California–licensed MD/DO physician, passionate about medicine and looking to establish roots in a practice dedicated to the art of good medicine. Competitive salary and excellent benefits including medical, dental, vision, and retirement. Send a cover letter and CV to jcataluna@lajollafamilymedical. com. [2880-0520]
CLINICAL DIRECTOR | BEHAVIORAL HEALTH SCIENCES | COUNTY OF SAN DIEGO: The County of San Diego is seeking a dynamic physician with a passion for building healthy communities. This is an exceptional opportunity for a California licensed, board–certified physician to help transform the local behavioral health continuum of care and lead important work within the Health and Human Services Agency’s Behavioral Health Services department. CLICK HERE to view a detailed brochure outlining the duties and responsibilities of the position. Anticipated Hiring Range: $310,000 to $320,000 annually. In addition to the base salary, the incumbent may receive a 10 % premium for Board Certification or a 15 % premium for Board Certification and Sub–specialty. CLICK HERE to file your application. [2877-0225]
VENOUS DISEASE SPECIALIST | NORTH
COUNTY: La Jolla Vein & Vascular, the premier vein care provider in San Diego, is seeking a highly skilled and experienced Venous Disease Specialist to join our team at our newest location in Vista, CA, nestled in the stunning coastal region of North County San Diego. This full–time position offers competitive salary and benefits, including profit-sharing and a 401(k). Our state–of–the–art facility operates Monday through Friday, with no weekend or night shifts, promoting an excellent work–life balance. Ideal candidates may also consider a locum or locum–to–hire arrangement. Join us in making a difference in our patients’ lives while enjoying your dream location! Email cv to jobs@ljvascular. com. [2875-1030]
PART–TIME PRIMARY CARE PHYSICIAN: Primary Care Clinic in San Diego searching for part–time physician for 1 to 2 days a week, no afterhours calls. Please send CV to medclinic1@yahoo.com. [2872-0909]
OB/GYN POSITION AVAILABE | EL CENTRO: A successful Private OBGYN practice in El Centro, CA seeking a board eligible/certified OB/GYN. Competitive salary and benefits package is available with a tract of partnership. J-1 Visa applicants are welcome. Send CV to feminacareo@gmail.com or call Katia M. at (760) 352-4103 for more information. [2865-0809]
COUNTY OF SAN DIEGO PROBATION DEPT.
MEDICAL DIRECTOR: The County of San Diego is seeking dynamic physician leaders with a passion for building healthy communities. This is an exceptional opportunity for a California licensed, Board-certified, physician to help transform our continuum of care and
lead essential medical initiatives within the County’s Probation Department. Anticipated Hiring Range: Depends on Qualifications Full Salary Range: $181,417.60 - $297,960.00 annually. As part of the Probation Administrative team, the Medical Director is responsible for the clinical oversight and leadership of daily operations amongst Probation facilities’ correctional healthcare programs and services. As the Medical Director, you will have significant responsibilities for formulating and implementing medical policies, protocols, and procedures for the Probation Department. Medical Director.
PART–TIME CARDIOLOGIST POSITION AVAILABLE: Cardiology office in San Marcos seeking part–time cardiologist. Please send resume to Dr. Keith Brady at uabresearchdoc@yahoo.com. [2873-0713]
INTERNAL MEDICINE PHYSICIAN: Federally
Qualified Health Center located in San Diego County has an opening for an Internal Medicine Physician. This position reports to the chief medical officer and provides the full scope of primary care services, including diagnosis, treatment, and coordination of care to its patients. The candidate should be board eligible and working toward certification in Internal Medicine. Competitive base salary, CME education, four weeks paid vacation, year one, 401K plan, No evenings and weekends, Monday through Friday 8:00am to 5:00pm. For more information or to apply, please contact Dr. Keith Brady at: uabresearchdoc@yahoo.com. [2874-0713]
FAMILY MEDICINE/INTERNAL MEDICINE PHYSICIAN: San Diego Family Care is seeking a Family Medicine/Internal Medicine Physician (MD/DO) at its Linda Vista location to provide outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care and participating in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@sdfamilycare.org or call us at (858) 810-8700.
PHYSICIAN POSITIONS WANTED
PART–TIME CARDIOLOGIST AVAILABLE: Dr. Durgadas Narla, MD, FACC is a noninvasive cardiologist looking to work 1-2 days/week or cover an office during vacation coverage in the metro San Diego area. He retired from private practice in Michigan in 2016 and has worked in a San Marcos cardiologist office for the last 5 years, through March 2023. Board certified in cardiology and internal medicine. Active CA license with DEA, ACLS, and BCLS certification. If interested, please call (586) 206-0988 or email dasnarla@gmail.com.
OFFICE SPACE / REAL ESTATE AVAILABLE
RECENTLY UPDATED MEDICAL OFFICE SPACE TO SUBLEASE IN VISTA: Recently updated and wellappointed medical office space for partial or full sublease in Vista, CA. This approximately 6,000 square foot clinic is located at 2067 West Vista Way, within a prime medical office building. The space is equipped with 16 exam rooms, 3 restrooms, and ample dedicated office and lab space. The building itself is ADA compliant and offers several amenities, including ample parking, an outdoor atrium, elevators, and public restrooms on all floors .For more information or to discuss sublease terms, please contact Denise @ dporter@tpirc.org.
MEDICAL OFFICE AVAILABLE TO RENT | MID–CITY: Practice for sale, medical office available for rent. Centrally located in San Diego’s Mid–City community at 3250 El Cajon Blvd, San Diego, CA 92104. Contact Miguel Losada, MD at (619) 282-2178 or by fax at (619) 282-2179.
AVAILABILITY OF UTC MEDICAL OFFICE: Office in UTC area. 2–3 exam rooms, ample waiting room, 2 private offices. Ground floor location. Just one block from 805 exit. Close to Genesee Ave, all major shopping and restaurants in UTC. Parking available. Ground floor office, handicapped accessible. Six month–one
year lease available with possibility to renew. Call (619) 585-0476. Ask for Alisha. [2890-0825]
OFFICE SPACE FOR LEASE | AESTHETIC SET-
TING: Take your practice to the next level with this beautifully appointed office space available in a modern, fully equipped clinical environment. Whether you’re already in aesthetics or starting an aesthetic practice, we offer flexible, high–end rental options. Rentals include use of PicoSure Pro Laser and Potenza Microneedling with Radiofrequency, two private treatment rooms and staff breakroom in a professional, clean and serene setting. Available Mondays, Tuesdays, Thursdays and Fridays at $1,000/day between the hours of 8:30am–5:00pm. Ideal for dermatologists/ plastic surgeons, cosmetic physicians, nurse injectors or other licensed professionals in the aesthetic field. Must see to appreciate the quality and atmosphere. Contact us today at Vivian@sandiegomobiledoctor. com to schedule an in–person tour of this great opportunity. [2886-0804]
OFFICE SPACE FOR LEASE | MEDICAL SETTING:
Take your practice to the next level with this beautifully appointed office space available in a modern, fully equipped clinical environment. Whether you’re in primary care or specialty medicine, we offer flexible, high–end rental options. Rentals include use of two medical exam rooms and waiting (lobby) area in a clean, professional setting. Available Mondays, Tuesdays, Thursdays and Fridays at $350/half day or $600/day between the hours of 8:30am–5:00pm. Ideal for primary care physicians and specialists seeking flexible space. Must see to appreciate the quality and atmosphere. Contact us today at Vivian@sandiegomobiledoctor.com to schedule an in–person tour of this great opportunity. [2885-0804]
LA JOLLA/XIMED OFFICE TO SUBLEASE: Modern upscale office on the campus of Scripps Hospital — part or full time. Can accommodate any specialty. Multiple days per week and full use of the office is available. If interested please email kochariann@yahoo. com or call (818) 319-5139. [2866-0904]
SUBLEASE AVAILABLE: Sublease available in modern, upscale Medical Office Building equidistant from Scripps and Sharp CV. Ample free parking. Class A+ office space/medical use with high-end updates. A unique opportunity for specialist to expand reach into the South Bay area without breaking the bank. Specialists can be accommodated in this first floor high-end turnkey office consisting of 1670 sq ft. Located in South Bay near Interstate 805. Half day or full day/week available. South Bay is the fastest growing area of San Diego. Successful sublease candidates will qualify to participate in ongoing exclusive quarterly networking events in the area. Call Alicia, (619) 585-0476.
MEDICAL OFFICE FOR SALE OR SUBLEASE: A newly remodeled and fully built-out primary care clinic in a highly visible Medical Mall on Mira Mesa Blvd. at corner of Camino Ruiz. The office is approximately 1000 sq ft with 2 fully equipped exam rooms, 1 office, 1 nurse station, spacious and welcoming waiting room, spacious reception area, and ADA accessible restroom. All the furniture and equipment are new and modern design. Ample parking. Perfect for primary care or any specialty clinic. Please contact Nox at (619) 776-5295 or noxwins@hotmail.com. Available immediately.
| EL CAJON: Recently renovated, turnkey medical office in freestanding single-story unit available in El Cajon. Seven exam rooms, spacious waiting area with floor-to-ceiling windows, staff break room, doctor’s private office, multiple admin areas, manager’s office all in lovely, drought-resistant garden setting. Ample free patient parking with close access to freeways and Sharp Grossmont and Alvarado Hospitals. Safe and secure with round-the-clock monitored property, patrol, and cameras. Available March 1. Call 24/7 on-call property manager Michelle at the Avocado Professional Center (619) 916-8393 or email help@ avocadoprofessionalcenter.com.
OPERATING ROOM FOR RENT: State of the Art AAAASF Certified Operating Rooms for Rent at Outpatient Surgery of Sorrento. 5445 Oberlin Drive, San Diego 92121. Ideally located and newly built 5 star facility located with easy freeway access in the heart of San Diego in Sorrento Mesa. Facility includes two operating rooms and two recovery bays, waiting area, State of the Art UPC02 Laser, Endoscopic Equipment with easy parking. Ideal for cosmetic surgery. Competitive Rates. Call Cyndy for more information (858) 658-0595 or email Cyndy@roydavidmd.com.
PRIME LOCATION | MEDICAL BUILDING LEASE OR OWN OPPORTUNITY IN LA MESA: Extraordinary opportunity to lease or lease-to-own a highly visible, freeway-oriented medical building in La Mesa, on Interstate 8 at the 70th Street on-ramp. Immaculate 2-story, 7.5k square foot property with elevator and ample free on-site parking (45 spaces). Already built out and equipped with MRI/CAT machine. Easy access to both Alvarado and Sharp Grossmont Hospitals, SDSU, restaurants, and walking distance to 70th St Trolley Station. Perfect for owner-user or investor. Please contact Tracy Giordano [Coldwell Banker West, DRE# 02052571] for more information at (619) 987-5498.
KEARNY MESA OFFICE TO SUBLEASE/SHARE: 5643 Copley Dr., Suite 300, San Diego, CA 92111. Perfectly centrally situated within San Diego County. Equidistant to flagship hospitals of Sharp and Scripps healthcare systems. Ample free parking. Newly constructed Class A+ medical office space/medical use building. 12 exam rooms per half day available for use at fair market value rates. Basic communal medical supplies available for use (including splint/cast materials). Injectable medications and durable medical equipment (DME) and all staff to be supplied by individual physicians’ practices. 1 large exam room doubles as a minor procedure room. Ample waiting room area. In office x-ray with additional waiting area outside of the x-ray room. Orthopedic surgery centric office space. Includes access to a kitchenette/indoor break room, exterior break room and private physician workspace. Open to other MSK physician specialties and subspecialties. Building occupancy includes specialty physicians, physical therapy/occupational therapy (2nd floor), urgent care, and 5 OR ambulatory surgery center (1st floor). For inquiries contact kdowning79@gmail.com and scurry@ortho1.com for more information. Available for immediate occupancy.
LA JOLLA/UTC OFFICE TO SUBLEASE OR SHARE: Modern upscale office near Scripps Memorial, UCSD hospital, and the UTC mall. One large exam/procedure room and one regular-sized exam room. Large physician office for consults as well. Ample waiting room area. Can accommodate any specialty or Internal Medicine. Multiple days per week and full use of the office is available. If interested please email drphilipw@ gmail.com.
ENCINITAS MEDICAL SPACE AVAILABLE: Newly updated office space located in a medical office building. Two large exam rooms are available M-F and suitable for all types of practice, including subspecialties needing equipment space. Building consists of primary and specialist physicians, great for networking and referrals. Includes access to the break room, bathroom and reception. Large parking lot with free parking for patients. Possibility to share receptionist or bring your own. Please contact coastdocgroup@gmail.com for more information.
NORTH COUNTY MEDICAL SPACE AVAILABLE: 2023 W. Vista Way, Suite C, Vista CA 92082. Newly renovated, large office space located in an upscale medical office with ample free parking. Furnishings, decor, and atmosphere are upscale and inviting. It is a great place to build your practice, network and clientele. Just a few blocks from Tri-City Medical Center and across from the urgent care. Includes: multiple exam rooms, access to a kitchenette/break room, two bathrooms, and spacious reception area all located on the property. Wi-Fi is not included. For inquiries contact hosalkarofficeas-
sist@gmail.com or call/text (858) 740-1928.
MEDICAL EQUIPMENT / FURNITURE FOR SALE
FRIDGE & FREEZER EQUIPMENT AVAILABLE |
MINT CONDITION: Pristine medical cold storage refrigeration equipment available for purchase by Champions for Health, SDCMS’ philanthropic 501(c)3. Used to store vaccines. Includes 2 (two) commercial–grade Accucold ARG49ML 49 cu ft upright pharmacy refrigerators each with two glass doors, automatic defrost, digital thermostat and stainless steel cabinets (83.75” H x 55.25” W x 31.0” D), plus 1 (one) pharmaceutical–grade TempArmour BFFV15 compact freezer built to ensure stable temperatures and virtually eliminate supply losses (26.5” H x 25.0” W x 31.0” D). All units were acquired new, in use between 2-4 years and in very gently used condition. Units meet all CDC guidelines for vaccine storage. Asking price for each fridge is $4,000 OBO and $2,500 OBO for the freezer. Purchase individually or as a set. Contact Adama at (858) 300–2780 or adama.dyoniziak@championsfh.org. [2879-0502]
NURSE PRACTITIONER | PHYSICIAN ASSISTANT: Open position for Nurse Practitioner/Physician Assistant for an outpatient adult medicine clinic in Chula Vista. Low volume of patients. No call or weekends. Please send resumes to medclinic1@yahoo.com. [2876-1121]
POSTDOCTORAL SCHOLARS: The Office of Research Affairs, at the University of California, San Diego, in support of the campus, multidisciplinary Organized Research Units (ORUs) https://research.ucsd.edu/ ORU/index.html is conducting an open search for Postdoctoral Scholars in various academic disciplines. View this position online: https://apol-recruit.ucsd.edu/ JPF03803. The postdoctoral experience emphasizes scholarship and continued research training. UC’s postdoctoral scholars bring expertise and creativity that enrich the research environment for all members of the UC community, including graduate and undergraduate students. Postdocs are often expected to complete research objectives, publishing results, and may support and/or contribute expertise to writing grant applications https://apol-recruit.ucsd.edu/JPF03803/ apply. [2864-0808]
RESEARCH SCIENTISTS (NON–TENURED, ASSISTANT, ASSOCIATE OR FULL LEVEL): The University of California, San Diego campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd. edu/ORU/index.html is conducting an open search for Research Scientists (non–tenured, assistant, associate or full level). Research Scientists are extramurally funded, academic researchers who develop and lead independent research and creative programs similar to Ladder Rank Professors. They are expected to serve as Principal Investigators on extramural grants, generate high caliber publications and research products, engage in university and public service, continuously demonstrate independent, high quality, significant research activity and scholarly reputation. Appointments and duration vary depending on the length of the research project and availability of funding. Apply now at https://apol-recruit.ucsd.edu/JPF04188/apply. [2867-0904]
PROJECT SCIENTISTS: Project Scientists (nontenured, Assistant, Associate or Full level): The University of California, San Diego, Office of Research and Innovation https://research.ucsd.edu/, in support of the Campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd.edu/ORU/index. html is conducting an open search. Project Scientists are academic researchers who are expected to make significant and creative contributions to a research team, are not required to carry out independent research but will publish and carry out research or creative programs with supervision. Appointments and duration vary depending on the length of the research project and availability of funding: https://apol-recruit. ucsd.edu/JPF04189/apply. [2868-0904]