

football medicine & performance
In this issue
Pectoral Major Ruptures in Professional Football
Tom Whittamore
Gaps & Our Knowledge: HighGrade Hamstring Rehabilitation in Elite Football
Dr. Fearghal Kerin
How Manual Therapy Can Form Part of a Holistic Management Approach
Alex Ng
Establishing Team Match Physical Performance Reference Values at UEFA EURO 2024 Germany
Professor Paul S. Bradley
Tackling Football’s Achilles Heel
Dr. Colin Griffin
Chronic Pain in Football - the Unseen Struggle
Richmond Stace
The Connection Edge - How Psychological Safety & Belonging Can Unlock Performance, Engagement & Player Availability in Football
Ronan Conway
A Practical Approach to the Skeletal Muscle Morphology & Its Importance in Sports-Related Skeletal Muscle Injuries
Dr. Carles Pedret
Enigma Legal provides legal services and advice to managers, coaches and professionals working within the sports industry, its unique structure utilising a panel of expert barristers all with extensive experience of the sports industry, most notably their work with the League Managers Association.
Enigma Legal lawyers are tried and trusted to work in a flexible, agile and responsive way, demonstrating their understanding of the unique demands of the sports industry. A creative and pragmatic approach will ensure that Enigma Legal offers real value to the FMPA Membership.

www.enigmalegal.com
admin@fmpa.co.uk

CEO MESSAGE
Among the many support mechanisms available, member welfare remains our foremost priority. As the season progresses, it is important to emphasize the significance of well-being for every member of our association. While the initial stages of a campaign may bring energy and enthusiasm, the sustained demands of a long season—extended hours, pressure, stress, and fatigue— can have a considerable impact. Safeguarding welfare is not only vital to individual success but also essential to the effectiveness of the wider team.
Support within our industry exists at every level, whether through Human Resources, Heads of Department, colleagues, family, or friends. Beyond this, the FMPA plays a leading role in promoting and protecting member welfare, often working discreetly to provide assistance when it is needed most. This independent support is a valuable resource that responsible Club leaders should ensure is accessible to all staff.
The FMPA serves as the first point of contact for matters including contract issues, confidential concerns, conflict resolution, and periods of stress. Our team is available seven days a week, throughout the year, and our confidential mental health helpline remains open to anyone seeking guidance or advice. In addition, we provide legal support (contract evaluations and settlement agreements), education, recruitment services, member profiles, and financial guidance to complement this framework of care.
Together, these provisions form the independent, member-focused structure that underpins the association’s welfare strategy—a framework that is indispensable to all medical and performance practitioners within the game and one that consolidates our unique interpersonal relationship with members.
Salmon Eamonn Chief Executive Officer
Football Medicine & Performance Association
ONLINE COURSE MPA DIPLOMA
PREPARATION FOR WORK IN PROFESSIONAL FOOTBALL
✓ Health and safety
✓ Safeguarding
✓ Equality/Diversity
✓ Mental Health/wellbeing
✓ Confidentiality
✓ Record keeping
✓ Media TV
✓ Social Media
✓ Expectations of behaviour/general professionalism
✓ Integration within the MDT environment
✓ Insight into the working week
✓ Awareness of un-clinical skills
✓ From `Theory to Practice’
✓ How the science sits in the working environment
✓ What an employer is looking for – Employability, CPD, Reflective Practice, CV
✓ Portfolio design
Includes FREE FMPA membership access for 6 months:
• FMPA resources
• FMPA publication
• Free access to BJSM
• FMPA podcasts
• FMPA education
• Latest Jobs

• Sports Scientists
• Physiotherapists
• Doctors
• Analysts
• Sports Therapists
• S & C Coaches
• Fitness Coaches
• Soft Tissue Therapists
• Sports Rehabilitators
• Sports Psychologists
• Nutritionists
• Podiatrists
Contact us at:
admin@fmpa.co.uk 0333 4567897 www.fmpa.co.uk/courses/mpa-diploma

FROM THE EDITORS
As the 2025/2026 season gets underway, we are pleased to present a new edition of Football Medicine and Performance, featuring a diverse range of articles designed to inform and support your clinical and performance practice.
Reflecting on the 2023/2024 season, Professor Paul S. Bradley, Dr. Piotr Zmijewski, Shuyao Chen and examine team match physical performance reference values from UEFA EURO 2024. Dr. Carles Pedret, Dr. Ramon Balius, Dr. José Peña-Amaro and Dr. Tero Järvinen offer a practical overview of skeletal muscle morphology and its significance in sports-related muscle injuries.
Hamstring injuries are always a hot topic in the sports and rehab world, especially when it comes to high-grade hamstring strains (HSI), which can often lead to prolonged recovery and require careful management to avoid re-injury.
Dr. Fearghal Kerin explores current knowledge and gaps in the rehabilitation of high-grade hamstring injuries in elite football, while Alexander Ng discusses the role of manual therapy within a holistic management framework.
Chronic pain in football is addressed by pain and rehabilitation specialist Richmond Stace, who offers valuable insights and strategies for supporting elite players in managing pain effectively. Performance consultant Ronan Conway contributes a thought-provoking piece on how fostering psychological safety and a sense of belonging can enhance performance, engagement, and player availability. On the other hand, physiotherapist Tom Whittamore examines a topic that not much has been discussed in football medicine, the incidence and management of pectoralis major ruptures in professional football.
In addition, Dr. Colin Griffin, a lower limb rehabilitation specialist, provides an in-depth analysis of Achilles tendon injuries within the sport.
We hope you find this edition insightful and relevant to your practice. On behalf of the editorial team, we wish you a successful and fulfilling season.



Dr. Fadi Hassan Editor, FMP Magazine
Dr. Andrew Shafik Editor, FMP Magazine Fadi Hassan Andrew Shafik
Dr. Daniela Mifsud Editor, FMP Magazine Daniela Mifsud
ASSOCIATE EDITORS

Ian Horsley Lead Physiotherapist

Dr. Jon Power Director of Sport & Exercise Medicine
REVIEWERS

Matthew Brown Academy Sports Scientist

Lisa Edwards Sports Therapist

Dr. Danyaal Khan Academy Doctor

Mike Brown Head of Physical Performance

Jake Heath Elite Sports Specialist Podiatrist

Dr. Dáire Rooney Doctor

Dr. Manroy Sahni Medical Doctor

Dr. Andrew Butterworth Senior Lecturer Frankie Hunter Lead Sports Scientist


Dr. Jose Padilla MD Sports Medicine Specialist

Dr. Eleanor Trezise Doctor

Dr. Avinash Chandran Director

Callum Innes Medical Doctor

Kevin Paxton Strength & Conditioning Coach
Medicine And Performance Association t/a Football Medicine & Performance Association Office 5, Bank House, King St, Clitheroe, Lancs, BB7 2EL T: 0333 4567 897 E: info@fmpa.co.uk W: www.fmpa.co.uk
FMPA_Official Officialfmpa fmpa_official LinkedIn: Football Medicine & Performance Association
FMPA_Register FMPARegister fmpa_register
Chief Executive Officer Eamonn Salmon eamonn.salmon@fmpa.co.uk
Commercial Manager Angela Walton angela.walton@fmpa.co.uk
Design Oporto Sports www.oportosports.com
Photography Alamy, FMPA, Unsplash
Cover Image Rangers’ Ianis Hagi is injured after a tackle by Callum McGregor during the Old Firm Derby, at Ibrox Stadium. 4 May, 2025.
Photo: Alamy
© Football Medicine & Performance Association. All rights reserved.
The views and opinions of contributors expressed in Football Medicine & Performance are their own and not necessarily of the FMPA Members, FMPA employees or of the association. No part of this publication may be reproduced or transmitted in any form or by any means, or stored in a retrieval system without prior permission except as permitted under the Copyright Designs Patents Act 1988. Application for permission for use of copyright material shall be made to FMPA. For permissions contact admin@fmpa.co.uk
Carles Pedret,
Tero Järvinen



Ramon Balius, Dr. José Peña-Amaro,







BTL INDUSTRIES JOINS FMPA AS OFFICIAL BUSINESS PARTNER
FOR THE 2025/26 SEASON
With more than 30 years of ongoing innovation and a direct presence in over 80 countries, BTL is a global leader in non-invasive rehabilitation technologies, trusted by sports medicine teams, physiotherapists, and high-performance centres worldwide.
“We’re proud to partner with the FMPA to bring cutting-edge rehabilitation technology to the forefront of football medicine. At BTL, our mission is to support clinicians with innovative, evidence-based solutions that accelerate recovery, enhance performance, and help grow high-performing practices. This collaboration marks an exciting step forward in delivering smarter, non-invasive care across the professional sports landscape.”
– BTL Industries UK
“We are delighted to announce BTL Industries partnership with the FMPA. BTL Industries are one of the worlds leading manufacturers of medical equipment and have become a market leader in non invasive treatments, offering a range of products and services to the medical and performance sector in elite sports and clinical practice. We look forward to working together and engaging with BTL for the benefit of all our members and the wider sports industry”.
– Eamonn Salmon, FMPA CEO
BTL’s clinically proven device portfolio helps practitioners accelerate recovery, enhance functional performance, and grow their medical services, providing measurable value for both patients and practices. www.fmpa.co.uk/partner/btl-industries/




SPORTING EDGE (UK) LTD CONTINUE BUSINESS PARTNERSHIP WITH FMPA
Sporting Edge is a UK based manufacturing company with an expanding global reputation as the leader in the design and provision of Altitude & Environmental Facilities.
Sporting Edge systems deliver measurable fitness and performance improvements in as little as three weeks, with the added benefit of allowing fitness levels to be retained during injury repair – speeding up return to play.
Since 2005, Sporting Edge has consistently set the benchmark for performance, safety, reliability and control for Simulated Altitude, Temperature & Relative Humidity, supported by a number of patents and innovations. Endorsed by the UK Sports Institute (EIS) and with a client list including many UK Universities, Olympic facilities, Professional Sports Teams and Commercial Physical Performance Centres, Sporting Edge have more installations, delivering completely unmatched performance and control, than any other sector company.
If you would like to learn more, visit www.sportingedgeuk.com and maybe take a look at the research library section to see how you could benefit from a class leading, Altitude and/or Environmental chamber for you and your team. Beneficial to general squad fitness or return to play protocols, adding one of our chambers may be enough to give you the EDGE this season.
Contact info@sportingedgeuk.com for a free, consultation and quote for your altitude/environmental chamber today.
SWIMEX EXTEND THEIR BUSINESS PARTNERSHIP
INTO THE 2025/26 SEASON
SwimEx Sports Performance Pools and Accelerated recovery hot and cold deep water plunge pools.
SwimEx Sports Fitness, Hydrotherapy Pools and Plunge Pools have delivered Sports Wellbeing since 1986. SwimEx’s unique paddlewheel delivers fantastic laminar flow water resistance for sports peak performance training and rehabilitation. Athletes can also commence recovery exercises much earlier due to the buoyancy of the SwimEx variable depth deep water wells alleviating their bodyweight, accelerating their return to action and helping prevent future injuries.
SwimEx also offer motorised underwater treadmills for aqua running which can be included in a new pool or a drop in self propelled resistance version for existing pools.
In the UK and Ireland we have installations at Help For Heroes Recovery Centre and Headquarters at Tedworth House, British Military Special Forces, Manchester City FC, Wolverhampton Wanderers FC, Stoke City FC, Reading FC along with several installations across Europe football teams.
We recently installed two SwimEx pools at Queens Park Rangers FC including a recovery deep water cold plunge pool with an energy efficient heat pump chilling system.
You can contact Richard Bishop MISPE direct if you would like to discuss a health check on your existing facilities or considering a future hydrotherapy project. richard@aquathermae.co.uk www.aquathermae.co.uk



WORKING







To discuss the commercial opportunities available please contact the Commercial Team on 0333 4567897 or


PECTORAL MAJOR RUPTURES IN PROFESSIONAL FOOTBALL
FEATURE / TOM WHITTAMORE
Introduction
Pectoralis major injuries are a rare phenomenon in professional football. These injuries typically occur in upper limb sports such as american football, rugby and powerlifting (Kakwani et al, 2007). This is the second pectoralis major rupture I have seen in professional football within the past couple of years and both have been interesting cases to manage.
Anatomy
The pectoralis major muscle is situated on the anterior aspect of the chest wall, it is separated into two heads, one being the clavicular head, and the other the sternocostal head whilst its insertion point is on the proximal aspect of the humerus into the greater tubercle (Solari and Burns, 2023). It has two nerve supplies, one being the lateral pectoral nerve which innervates the clavicular aspect, whilst the medial pectoral nerve innervates the sternocostal head. Its blood supply is from the pectoral artery.
Its function is to medially rotate, flex, extension and adduct the arm (Solari and Burns, 2023).
Injury
There are four injury sites for where the pectoralis major can be torn. Most commonly it occurs at the humeral insertion, followed by the musculotendinous junction, then the muscle belly itself and finally the sternal aspect though this is considered rare (Shoulder Doc, 2024).
The injury likely happens when there is a sudden eccentric force during activities such as a bench press motion or when there is a sudden eccentric to concentric force produced in positions such as abduction and external rotation.
A typical presentation is hearing a tearing or ripping sensation. In both cases I have been involved in, the player report feeling a ‘rip’. In the first case the player fell into
the shoulder loose pack position with his opponent on top of him. Whilst assessing the player on the pitch, I was expecting to be told there was a ‘pop’ and deformity of the shoulder possibly indicating a dislocation. However, I was informed by the player that he had felt a ‘rip’ and knew he had torn his pectoral muscle. In most cases there is pain, swelling, loss of function and a palpable deficit. Both cases presented with these findings acutely.
Imaging
The gold standard investigation for a suspected pectoralis major rupture is an MRI scan to determine the extent of the injury including the length of tendon retraction from the insertion site. Along with the retraction, it will show fluid/ oedema around the tendon.
Ultrasound may show hypoechoic areas due to the collection of fluid around the injury site such as a haematoma;
Head Physiotherapist Mansfield Town Football Club
ultrasound may also detect tendon disruption.
Both players underwent MRI scans which reported ‘complete pectoralis major tendon rupture with 5cm gap’ and ‘the injury involves the free tendon and is completely torn/ disrupted (Grade 3)’. ‘There appears to be an approximate 2cm gap between the retracted tendon and a small stub of tendon which remains attached to the proximal humerus’ respectively’.
Management
There are two management methods for these types of injuries: surgical or conservative.
Conservative management isn’t considered ideal for those wanting to return to contact sports due to the risk of reduction in strength (Long et al, 2022). Given the risks of conservative rehabilitation (namely strength deficits), both players opted for surgical management.
The second case will be discussed in more detail below, with some of the discussion relating back to the first case.
Consent
Both players provided consent for their case to be shared. Details of the first case can be found here
Case
A 22-year-old professional footballer sustained a left pectoralis major rupture at the
proximal humeral origin during a game whilst out on loan. The player reported their arm becoming caught in the ground in horizontal abduction whilst performing a slide tackle and hearing a ripping sensation. The player got up and tried to get back into position due to his team facing an attacking threat. Once the threat subsided, the player was removed from the field of play and immobilised in a sling.
The player returned to the club to be assessed two days later. Upon examination, there was very little movement due to player’s reluctance to move due to pain.
Palpation of the gleno-humeral joint and acromioclavicular joint provided no pain. However, on the proximal anterior aspect of the humerus there was pain, swelling and bruising evident.
Pattern recognition determined that the player had likely sustained a pectoralis major rupture, having seen this injury prior two years ago. Both the first and second player presented in the same way clinically despite their mechanisms: - player 1) being in the loose pack position and an opponent falling on them respectively, and player 2) horizontal abduction and their arm caught in the ground. It was felt unlikely to be a dislocation of the glenohumeral joint or acromioclavicular region due to no reported dislocation/deformity or pain evident around the respective site.
It was confirmed through an MRI scan that there was a pectoralis major rupture, and the player was therefore sent to a surgical
specialist. At the consultation the player was given the option of either conservative or surgical management for this case. The information provided showed the pros and cons of each pathway. It is considered that 3 weeks or less to undergo surgery is an appropriate timeframe for good outcomes of this injury. A discussion prior to the consultation, with the medical team had prepared the player for the eventuality that to return to contact and high intensity sports, a surgical pathway would be advisable. The player agreed to the surgical treatment and underwent the procedure a couple of days later.
Surgery
The incision was via the low anterior axillary fold with a deltopectoral approach, and the player positioned in supine with arm supported using a Trimano holder. Upon examination there was a 3cm retraction from the humeral insertion. Two anchors of 2.6 FibreTak with suture tape were used for the repair. Surgical time was 1 hour, and the wound was closed with glue.
Initial post-surgical advice was 6 weeks in a shoulder immobiliser however this was modified at the 3 week follow up to wean off the sling completely by 4 weeks. Safe zones were implemented for weeks 0-3, and 3-6 to protect the repair which initially were abduction and flexion restricted to 45 degrees with no rotation to be performed. No adverse events were reported from the surgery and the player was discharged from hospital and arrived home on the same day.

Safe Zones (Shoulder Doc, 2024)
Rehabilitation
Rehabilitation was split into 3 phases:
Weeks 0-3
The purpose of this stage of recovery is to allow the repair to heal. During this time the player was immobilised in a sling and was reviewed once per week at the training ground. The player was unable to drive during this time therefore was given time off to recover. From week 0-3 active assisted movements into flexion, abduction, early scapula activation and neuromuscular electrical stimulation of the rhomboids and trapezius (disuse atrophy setting) were performed. The first 2 weeks did not include any conditioning to avoid sweating and the associated risk of wound infection.
Week 4-6
The player could now begin to progress their range of motion into Zone B. This is up to 90 degrees flexion and abduction initially as well as 0-10 degrees lateral rotation. Once the player had demonstrated good scapula control and shoulder movement, they were allowed
Example programme in Phase 2: Day 1 – Strength
Example programme in Phase 1:
to begin working past these restricted ranges under the guidance of the physiotherapist. Phase 2 reintroduced upper limb weights including shoulder and bench press. The player also received scar tissue massage daily, this was the same for the first player.
2 - Isometrics
The player began running at 6 weeks post-surgery. This was an appropriate time for the player to return to running having demonstrated a sufficient range of motion progression and completion of running mechanics exercises in the gym.
Week 6+
This phase starts working towards return to training with controlled contact work and tailored conditioning. The 6-week block of running started with running mechanics and volume running.
Running was initially linear, then progressed to controlled change of direction before then completing unrestricted conditioning drills. Towards the end stage of rehabilitation at around
An example of the player’s gym programme in Phase 3: Day 1 – Posterior Chain
Day 2 - Anterior Chain
week 9, contact drills were introduced starting with early pushing and holding, progressing to learning to fall, wrestling and grappling in the box with the use of a tackle pad.

Testing
Criteria for both players was taken from different contact sports and shoulder rehabilitation protocols that involve impact and throwing activities. It was felt that this would be appropriate given some of
these sports (american football, rugby and baseball) use both contact and throwing activities therefore increasing our confidence in returning the player to the training pitch. A modified SIRSI questionnaire was used to
test the psychological aspect of returning to training, this is a shortened version of the SIRSI questionnaire (Pasqualini et al, 2023). Both are validated return to training tools for returning to play from a psychological point of view.
Outcome
The player successfully returned to full contact training 83 days post-surgery. In comparison the first player returned at 87 days post injury.
Player compliance
The 22-year-old was a full-time professional footballer. Compliance and progressions were determined by how the player presented on the day and the following day which was gauged by any adverse reaction such as swelling and soreness. During the rehabilitation the player did not report any adverse event to the pectoralis major repair which enabled the player to return to training at 3 months safely.
Complications
The player had no adverse events to the pectoralis major repair. However, it was noted that the player developed a right-side potential long thoracic nerve palsy having presented with a winging scapula, it was unclear what caused this. This was rehabilitated in conjunction with the left side with the focus on scapula stability work. This issue resolved by the time the player returned to training. However, this could have had implications on the limb symmetry index for return to play especially given no baseline testing was available for the player.
Clinical Relevance
Player one helped tailor player two’s rehabilitation which on reflection ensured overemphasis of the importance of scapula stability work in the early stages due to the slight issue player one developed.
Both case studies demonstrate that this injury can return safely within 3 months post-surgery in contrast to research of 4 months plus (Yu et al, 2019). Football been a predominately lower limb sport helped reduce the time frame
compared to the rehabilitation of a player from a upper limb dominant sports which may necessitate more time within this process.
No reoccurrence or return to play issue was reported by either player suggesting that the rehabilitation approach in both case studies was appropriate for returning to play
The case studies showed the importance of utilising other sports and shoulder rehabilitation research to help facilitate return to play given the lack of research of pectoralis major injuries.
Given the mechanism of injury it is important to consider a pectoralis rupture in the differential diagnosis of shoulder injuries.
References
Conclusion
In conclusion the pectoralis major rupture is a challenging injury to manage in football given its rare occurrence, however both case studies may help inform clinicians on appropriate rehabilitation strategies to facilitate return to play. Surgical repair for those wanting to get back to professional football with a typical return to play in around 3 months is advisable.
Background
Tom Whittamore is a physiotherapist who has worked within professional football for 11 years. Starting out at Derby County Academy before leaving to work with the first team at Mansfield Town where he has been for the past 6.5 years.
Funk, L. Pectoralis major rupture. Available at: -www.shoulderdoc.co.uk/article/1033. Date accessed: March 29, 2025
Kakwani, R.G., Matthews, J.J., Kumar, K.M., Pimpalnerkar, A., Mohtadi, N., (2007). Rupture of the pectoralis major muscle: surgical treatment in athletes. Int. Orthop. 31 (2), 159–163. Long, MK., Ward, T., DiVella, M., Enders, T., Ruotolo, C. (2022) Injuries of the Pectoralis Major: Diagnosis and Management. Orthopaedic Review. 14(4)
Pasqualini, I., Andres Rossi, L., Brandariz, R., Tanoira, I., Fuentes, N., Ranalletta, M. (2023)
The Short, 5-Item Shoulder Instability–Return to Sport After Injury Score Performs as Well as the Longer Version in Predicting Psychological Readiness to Return to Sport, Arthroscopy: The Journal of Arthroscopic & Related Surgery 39(5) 1131-1138.
Solari, F. and Burns, B. (2023) Anatomy, Thorax, Pectoralis Major. Available at: - www. ncbi.nlm.nih.gov/books/NBK525991/ Date accessed March 20, 2025
Whittamore, T., and Funk., L (2023) Surgical repair and rehabilitation of a ruptured pectoralis major muscle in a professional footballer – A case report. Journal of Bodywork and Movement Therapies 36(2). 291-299
Yu, J., Chang, C., Horner, N., Ayeni, O.R., Leroux, T., Alolabi, B., Khan, M., (2019). Outcomes and return to sport after pectoralis major tendon repair: a systematic review. Sport Health 11 (2), 134–141.



GAPS AND OUR KNOWLEDGE: HIGH-GRADE HAMSTRING REHABILITATION IN ELITE FOOTBALL
FEATURE / DR FEARGHAL KERIN, B.SC, M.SC, PH.D
The changing face of hamstring injuries
There appears to be a shift in the profile of hamstring injuries in elite football. The injuries being sustained in 2025 seem to be not only more frequent, but also increasingly severe than previously (Middleton, 2025). Whether this reflects changes in athletic profiles, increasing fixture congestion, the extended periods of additional time at the end of halves or simply the evolving physical demands with changes in game models is unclear.
What is widely accepted though is that the nature of injury is changing — moving away from the traditional sprint-type strains at the musculotendinous junction, associated with short return-to-play timelines, and towards more high-grade injuries involving the intramuscular tendon — the
central scaffold within the muscle belly, continuous with the proximal and distal free tendons (Kerin et al., 2023). These are typically classified as BAMIC ‘c’ type injuries (Pollock et al., 2014).
This has created several new challenges: how do we structure rehabilitation for these higher-grade injuries to prevent recurrence — particularly when managing them non-operatively and aiming to optimise the environment for tendon healing?
Mind the gap – managing 4C injuries
Despite the increase in severity, we now have a stronger knowledge base for managing these injuries. The BAMIC cohort showed that bespoke rehabilitation approaches for 3c injuries led to excellent outcomes, with no reinjuries (Macdonald
et al., 2019). Their approach involved delaying the introduction of eccentrics, sprinting, and hip-dominant loading for approximately 3 weeks. Notably, the timelines for 2c and 3c injuries were not significantly longer than those previously reported for lower grades — a marked contrast to earlier data showing reinjury rates of up to 60% for intramuscular tendon injuries (Pollock et al., 2022; Pollock et al., 2016). This suggests that how we load these injuries is more important than how long we wait, and that the tendon can adapt well to conservative loading if managed appropriately.
It’s worth noting, however, that the BAMIC data did not include any 4c injuries. Vermeulen et al. (2020) work suggests that even in cases of persistent tendon discontinuity and loss of tension on
imaging, athletes can return successfully and remain asymptomatic. In many cases, players returned with a tendon that had not fully regained anatomical integrity. Whether this is acceptable in elite football, where demands are higher and margins are smaller, is unclear. The transferability of this evidence to Premier League or Champions League-level competition remains uncertain.
We do now have more guidance around risk at the point of return. Isern-Kebschull et al. (2022) have shown that when two or more of five specific MRI signs are present at the time of return to play, the athlete is significantly more likely to reinjure. These signs include persistent tendon gapping, loss of tension, intermuscular oedema, residual high signal, and callus separation. This provides a helpful framework for decision-making in complex tendoninvolved cases, particularly 4c injuries. Rather than a binary, time-based approach, it becomes a case of weighing
total risk — imaging, clinical signs, exposure, and athletic profile.
Creating the environment for healing
Since moving from a club environment to consultancy, my caseload is now almost entirely made up of high-grade and recurrent hamstring strain injuries. The aims of the clients in both groups tend to overlap — to stop recurrences from continuing to recur and prevent highgrade injuries from becoming recurrent. As a result, with complex or persistent presentations, having a structured framework is critical (Figure 1).
Recurrent injuries also need to feel like they’re being managed differently than previously, and that the practitioner understands their problem. That doesn’t always mean a radically different plan, but repeating the same process that’s already failed is rarely effective. Something must change — whether that’s timeline, communication, loading strategy, or onward referral — and that shift often
helps the athlete build confidence that this time might be different.
The first step is always getting clarity on the anatomical diagnosis. This is where a strong relationship with sports medicine and radiology is essential for the rehabilitation practitioner. Anatomical diagnosis includes the precise site of injury, the structure involved, and the severity — all of which will influence loading decisions.
In practice, this means matching the diagnosis to a clear set of loading principles. While delaying certain loading characteristics is often necessary, it’s still critical to begin rehabilitation early and meaningfully. This early mechanical input to direct collagen alignment, maintain muscle architecture, and kick-start the remodelling process (Kerin, 2025; Lauf et al., 2025). If the injury is recurrent, the first question is whether previous rehab genuinely addressed the underlying contributors. If not, that becomes the focus of the current rehabilitation.
Figure 1: Dual classification model outlining anatomical injury type and functional contributors to guide targeted rehab.


Figure 2: Asymmetry in hamstring muscle volumes post-injury, showing long head atrophy and compensatory hypertrophy (Springbok Analytics).
Culprit or victim
I then work off a simple model: is the hamstring the culprit, or the victim? The culprit model — where dysfunction within the hamstring itself is seen as the root cause — is well described by Fyfe et al. (2013). Strength and fascicle length are the two most commonly cited factors, but in practice, I rarely come across elite male athletes who aren’t already strong, even following a high-grade injury. I also don’t routinely assess fascicle length, because the intervention most likely to help — lengthened-state eccentrics — forms a central part of my approach even without an objective measurement (Bourne et al., 2018).
What’s often missed is the third pillar: activation. Fyfe et al. (2013) has highlighted the neuromuscular inhibition that typically follows injury — particularly affecting the long head of biceps femoris. This can lead to compensatory hypertrophy in surrounding structures, most commonly the short head. The issue is that standard strength tests won’t detect this. Total output may look normal, but how the athlete produces that force may vary. A Nordbord test or isokinetic profile might suggest they’re ready — even when they’ve developed maladaptive recruitment patterns (Figure 2).


Figure 3: Stepwise priority hierarchy for high-grade hamstring rehabilitation, guiding intervention timing and focus.
Atrophy, activation and adaptation
This is where I find early activation work for the long head particularly useful (Figure 3). That might involve EMG biofeedback or simply targeted positional coaching. The long head tends to respond well to lower load work in the early stages, but athletes can also lose muscle volume quickly during this phase — so while the load may need to be reduced, it’s important to maintain either time under tension or proximity to failure.
While we typically train the biceps femoris as either knee- or hip-dominant, it’s often overlooked that it also acts as a rotator. I’ve found that introducing isometric or eccentric rotational activities can be an effective way to bias the long head and drive local adaptation. The Springbok Analytics example in Figure 2 illustrates this clearly — marked atrophy in the long head with compensatory hypertrophy in surrounding tissue.
Targeting this area early is critical. In many of these cases, unless the long head is isolated and reactivated from the outset, the athlete restores strength through other parts of the hamstring complex — but not at the injured site. That ultimately leads to failure when exposed to higher-demand activities later in the process.
Intramuscular tendon hypertrophy and remodeling
A return of tension at the intramuscular tendon

Figure 4: Example loading progressions across rehab phases, with emphasis on contraction type, joint focus, and range.
on MRI typically occurs at around four weeks. This tends to be an appropriate point to begin reintroducing outer range eccentric work. Until then, I delay heavy eccentrics, modify hipdominant loading, and hold off on fast running.
Exercise selection across the phases of rehabilitation is outlined in Figure 4. A key objective is to prepare the athlete to tolerate a dedicated block of lengthened-state eccentric training. This type of loading has been shown to drive adaptation within the intramuscular tendon itself. The work of Lazarczuk et al. (2024), and more recently Maeo et al. (2024), suggests that this influences both tendon structure and muscle architecture — as well as increasing eccentric strength and improving fascicle length. This becomes particularly important in strong athletes, where force production is likely to be the most helpful adaptation, but where improving force transmission may be worthwhile. It’s also likely helpful in creating the mechanical conditions needed for tendon remodeling during healing. As the athlete progresses toward higherend, end-stage activities, Isern-Kebschull et
al. (2024) model can be a useful tool for monitoring scar maturation and gauging reinjury risk.
Shifting focus – the pelvis, the ankle and the hamstring as a victim
A primary cause of hamstring injury or recurrence is the presence of deficits remote from the hamstring itself. The influence of motor control at the pelvis on the attaching musculature is well established. King et al. (2018) have shown that by focusing on intersegmental control and mobility — rather than direct tissue loading — longstanding groin pain can be resolved in under 10 weeks. Mendiguchia et al. (2024) have demonstrated that every 5 degrees of anterior pelvic tilt adds roughly 1cm of strain to the proximal hamstrings, and that targeted intervention focused on mobility and strength can reduce anterior tilt during gait, altering load and modifying injury risk (Mendiguchia et al., 2022). This makes lumbo-pelvic mechanics a central consideration in high-grade hamstring rehabilitation to modify strain during running and reduce load, both acute and chronic.
Having worked in football and the Gaelic sports more recently, I now feel that the influence of the ankle is also frequently overlooked. It’s not uncommon to find previous ankle injury or arthropathy, limited dorsiflexion, reduced plantarflexor strength, or altered push-off mechanics (Green et al., 2020). This matters because during acceleration, where the ankle is the primary contributor to force production (Schache et al., 2012). If the ankle underperforms, load will shift proximally —to the hip and hamstring – which may explain the proliferation of this mechanism.
When planning rehabilitation, one of the early priorities is to establish the relevant contributing factors and build a clear problem list: what needs to change, how are we going to do it, and how will we know when it’s done? This often allows us to prioritise key issues early and make meaningful changes quickly — even if the hamstring itself isn’t the primary focus of loading in those initial phases. This is illustrated in an example model of a high-grade proximal hamstring rehabilitation (Figure 5).
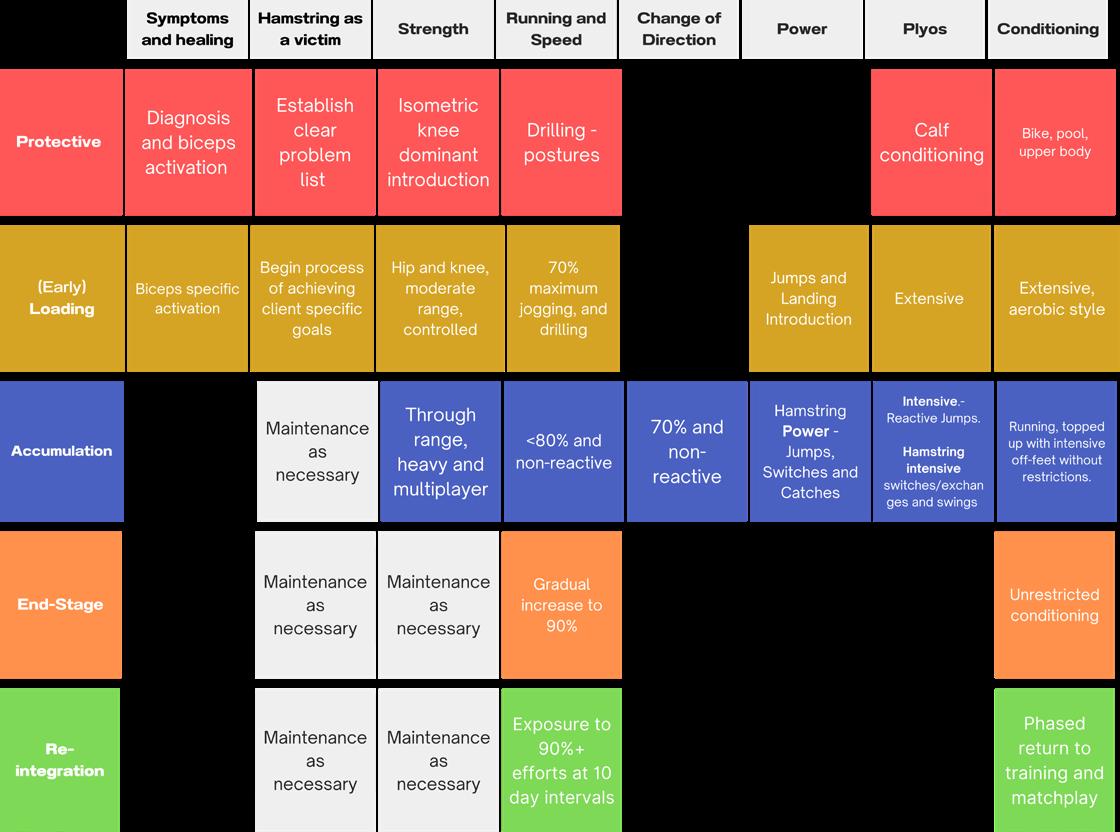
Figure 5 Rehabilitation framework across key domains and phases following high-grade hamstring injury.
This can be assessed through a combination of history taking, clinical testing and movement profiling — including strength, power and plyometric qualities. In many cases, the primary focus of rehabilitation may be on a remote area, with smaller top-ups applied to the hamstring simply to promote remodeling and maintain baseline strength. In this model, the hamstring isn’t the central focus if the athlete is already above certain critical thresholds.
Conclusion: What It Means in Practice
Rehabilitation for high-grade and recurrent
References
hamstring injuries starts with respecting the diagnosis — knowing exactly what structure is involved, where it is, and how severe it is. From there, the challenge becomes figuring out the maximum we can do at each stage while influencing adaptation and preparing the athlete for return to their sport.
There is much to learn from recurrent injuries – they often show us what wasn’t addressed the first time. For high-grade injuries, early reactivation of the long head is key. If we want to maintain volume and avoid compensatory patterns, this should be
targeted early to maintain cross-sectional area and output through the rehabilitation.
These injuries also offer an opportunity. In many cases, they’re the signal that something else is influencing overload of the hamstring muscle— whether it’s pelvic mechanics, poor ankle function, or another element of the kinetic chain. Identifying and addressing these contributory factors can be critical in turning the tide on complex injuries and modifying these should be a critical focus during the early stages of high-grade hamstring rehabilitation.
Bourne, M. N., Timmins, R. G., Opar, D. A., Pizzari, T., Ruddy, J. D., Sims, C., Williams, M. D., & Shield, A. J. (2018). An Evidence-Based Framework for Strengthening Exercises to Prevent Hamstring Injury [journal article]. Sports Med, 48(2), 251-267. https://doi.org/10.1007/s40279-017-0796-x
Fyfe, J. J., Opar, D. A., Williams, M. D., & Shield, A. J. (2013). The role of neuromuscular inhibition in hamstring strain injury recurrence. J Electromyogr Kinesiol, 23(3), 523-530. https://doi.org/10.1016/j.jelekin.2012.12.006
Green, B., Bourne, M. N., van Dyk, N., & Pizzari, T. (2020). Recalibrating the risk of hamstring strain injury (HSI): A 2020 systematic review and meta-analysis of risk factors for index and recurrent hamstring strain injury in sport. Br J Sports Med, 54(18), 1081-1088. https://doi.org/10.1136/bjsports-2019-100983
Isern-Kebschull, J., Mecho, S., Pedret, C., Pruna, R., Alomar, X., Kassarjian, A., Luna, A., Martinez, J., Tomas, X., & Rodas, G. (2024). Muscle Healing in Sports Injuries: MRI Findings and Proposed Classification Based on a Single Institutional Experience and Clinical Observation. Radiographics, 44(8), e230147. https://doi. org/10.1148/rg.230147
Isern-Kebschull, J., Pedret, C., Mecho, S., Pruna, R., Alomar, X., Yanguas, X., Valle, X., Kassarjian, A., Martinez, J., Tomas, X., & Rodas, G. (2022). MRI findings prior to return to play as predictors of reinjury in professional athletes: a novel decision-making tool. Insights Imaging, 13(1), 203. https://doi.org/10.1186/s13244-02201341-1
Kerin, F. (2025). Non-surgical rehab and outcomes for complete hamstring tendon tears. SportSmith. Retrieved May 24 from https://www.sportsmith.co/ articles/non-surgical-rehab-and-outcomes-for-complete-hamstring-tendon-tears/ Kerin, F., O’Flanagan, S., Coyle, J., Farrell, G., Curley, D., McCarthy Persson, U., De Vito, G., & Delahunt, E. (2023). Intramuscular Tendon Injuries of the Hamstring Muscles: A More Severe Variant? A Narrative Review. Sports Med Open, 9(1), 75. https://doi.org/10.1186/s40798-023-00621-4
King, E., Franklyn-Miller, A., Richter, C., O’Reilly, E., Doolan, M., Moran, K., Strike, S., & Falvey, E. (2018). Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: prospective cohort of 205 patients. Br J Sports Med, 52(16), 1054-1062. https://doi.org/10.1136/ bjsports-2016-097089
Lauf, K., van der Made, A. D., Jaspers, R., Tacken, R., Maas, M., & Kerkhoffs, G. (2025). Successful rapid return to performance following non-operative treatment of proximal hamstring tendon avulsion in elite athletes. BMJ Open Sport & Exercise Medicine, 11(2). https://doi.org/10.1136/bmjsem-2025-002468
Lazarczuk, Stephanie L., Collings, Tyler J., Hams, Andrea H., Timmins, Ryan G., Shield, Anthony J., Barrett, Rod S., & Bourne, Matthew N. (2024). Hamstring Muscle‐Tendon Geometric Adaptations to Resistance Training Using the Hip Extension and Nordic Hamstring Exercises. Scandinavian Journal of Medicine & Science in Sports, 34(9). https://doi.org/10.1111/sms.14728
Macdonald, B., McAleer, S., Kelly, S., Chakraverty, R., Johnston, M., & Pollock, N. (2019). Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice. Br J Sports Med, 53(23), 1464-1473. https://doi.org/10.1136/bjsports-2017-098971
Maeo, S., Balshaw, T. G., Nin, D. Z., Mc Dermott, E. J., Osborne, T., Cooper, N. B., Massey, G. J., Kong, P. W., Pain, M. T. G., & Folland, J. P. (2024). Hamstrings Hypertrophy Is Specific to the Training Exercise: Nordic Hamstring versus Lengthened State Eccentric Training. Medicine & Science in Sports & Exercise, 56(10), 1893-1905. https://doi.org/10.1249/mss.0000000000003490
Mendiguchia, J., Castaño-Zambudio, A., Jiménez-Reyes, P., Morin, J. B., Edouard, P., Conceição, F., Tawiah-Dodoo, J., & Colyer, S. L. (2022). Can We Modify Maximal Speed Running Posture? Implications for Performance and Hamstring Injury Management. Int J Sports Physiol Perform, 17(3), 374-383. https://doi.org/10.1123/ ijspp.2021-0107
Mendiguchia, J., Garrues, M. A., Schilders, E., Myer, G. D., & Dalmau-Pastor, M. (2024). Anterior pelvic tilt increases hamstring strain and is a key factor to target for injury prevention and rehabilitation. Knee Surg Sports Traumatol Arthrosc, 32(3), 573-582. https://doi.org/10.1002/ksa.12045
Middleton, E. (2025). Are hamstring injuries getting worse in the Premier League? BBC. Retrieved May 24 from https://www.bbc.com/sport/football/articles/ cjr7g54n319o
Pollock, N., James, S. L., Lee, J. C., & Chakraverty, R. (2014). British athletics muscle injury classification: a new grading system. Br J Sports Med, 48(18), 1347-1351. https://doi.org/10.1136/bjsports-2013-093302
Pollock, N., Kelly, S., Lee, J., Stone, B., Giakoumis, M., Polglass, G., Brown, J., & MacDonald, B. (2022). A 4-year study of hamstring injury outcomes in elite track and field using the British Athletics rehabilitation approach. Br J Sports Med, 56(5), 257-263. https://doi.org/10.1136/bjsports-2020-103791
Pollock, N., Patel, A., Chakraverty, J., Suokas, A., James, S. L., & Chakraverty, R. (2016). Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med, 50(5), 305-310. https://doi.org/10.1136/bjsports-2015-094657
Schache, A. G., Dorn, T. W., Blanch, P. D., Brown, N. A., & Pandy, M. G. (2012). Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc, 44(4), 647-658. https://doi.org/10.1249/MSS.0b013e318236a3d2
Vermeulen, R., Almusa, E., Buckens, S., Six, W., Whiteley, R., Reurink, G., Weir, A., Moen, M., Kerkhoffs, G., & Tol, J. L. (2020). Complete resolution of a hamstring intramuscular tendon injury on MRI is not necessary for a clinically successful return to play. Br J Sports Med. https://doi.org/10.1136/bjsports-2019-101808
Adjustable Cold Therapy
Intermittent Compression
One Easy Application
Monthly Rental*
£250 ex VAT / £300 inc VAT

Accelerate Recovery from Injury or Surgery
Used by surgeons, healthcare professionals, athletes and rehabilitation units around the world, Game Ready now offers monthly Rental Systems to allow everyone the opportunity to recover like an elite athlete.

Rental Systems include:
࢚ Control unit, AC adapter, connector hose, carry bag & one fully assembled anatomical wrap from range available.
࢚ UK delivery within 24-48 hours & Return Shipping*
࢚ Information pack with easy-to-follow instructions & treatment guidelines.
࢚ Equipment cleaned to hospital infection control standards.
࢚ New fabric sleeve applied to every wrap.
For further information: Email ukrental@gameready.co.uk or call 01344 379797
HOW MANUAL THERAPY CAN FORM PART OF A HOLISTIC MANAGEMENT APPROACH
FEATURE / ALEX NG, MSC ADV. MANIP, BSC (HONS), MCSP
Introduction
According to CIES Football Observatory, an average of 50.8 matches were being played in the 2023/24 season, by clubs competing in the five major European leagues and UEFA Champions League, which averages a game every 7.18 days all year round (CIES, 2024). Alongside with international fixtures, which was not included in the report, player workload and wellbeing is a constant topic of discussion. As performance and medical teams, balancing risk and player availability remains a challenge within the football medicine world (Read & Rosenbloom, 2024).
Manual therapy is a low risk, non-invasive modality that is widely used across various football environments, it is “a specialized area of physiotherapy that manages neuro-musculoskeletal conditions using clinical reasoning and highly specific manual techniques” (IFOMPT), including joint and tissue mobilisation, manipulation, passive physiological movement and muscle energy technique (Claret al, 2014). Despite being an integral part of many professional athletes’ care, there is a lack of high-quality evidence on how it contributes towards availability, performance and injury management (Short et al, 2023). This editorial aims to explore the clinical reasoning for incorporating manual therapy into multidisciplinary holistic care.
“Can I have some anti-inflams please?” - Management of pain Despite the potential side effects on tissue healing and the exercise recovery process,

the F-MARC have found a high prevalence of NSAIDS usage (Male: 77%; Female: 85%) across major tournaments over a 12 year period (Tscholl et al, 2015). Analgesic medications, when appropriately used, can manage symptoms to allow participation, they can however mask the injury and can be perceived as increasing the risk of causing further tissue damage (Read & Rosenbloom, 2024). Other potential side effects such as increasing cardiovascular risk, gastrointestinal and renal issues are also noted in literatures (Tscholl et al, 2015; Fitzpatrick et al, 2024).
Targeted manual therapy can provide a safe alternative to manage pain and
improve function through complex neurophysiological pathways (Bialosky et al, 2018). It can complement the effect of other treatment modalities or substitute more invasive interventions and reduce the minimal effective dosage of medication needed to provide pain relief. Other non-invasive modalities such as isometric exercises, mobility, cryotherapy and electrotherapy have also shown moderate to good efficacy in reducing pain across different pathologies, a more holistic approach in pain management should be considered (Clifford et al, 2020; Silva et al, 2020; Caneiro et al, 2021; de Sire et al, 2024; Fitzpatrick et al, 2024).
In the presence of pain, player may not be able to participate or perform at their maximal potential. When considering player development, pain can be a limiting factor for athletic development and adaptative training. Well-reasoned treatment and exercise selection, informed by pain mechanism allow effective modulation of symptoms and increase activity tolerance.
“Player is flagging but what next?” –Proactive management of injury risk Screening tools such as wellness, objective testing and player load data provide us with numerous of insights and should no doubt form the basis of risk assessment. Where possible, performance and medical staff can influence external risk factors such as training exposure,
Loans and Emerging Talent Performance Physiotherapist, Tottenham Hotspur Football Club
Figure 1: Clinical reasoning of treatment focus in relation to pain generating source


match day involvement and travel arrangement, however, context does not always allow our recommendations to follow through (Read & Rosenbloom, 2024). The challenge often is on how to act on the findings effectively to lower the risk within a short window before training.
For many players, manual therapy is an essential part of their daily routine preparation and recovery. While manual therapy can meet players’ expectation to provide short term improvements, it also provides a regular window for practitioners to assess for any
potential causes of physiological change and treat to modify internal risks. Kinesiopathological approaches such as symptoms modification procedures (diagnostic mini treatment), not only provide symptoms relief, more importantly, allow practitioners to identify contributing factors and inform a targeted treatment and exercises to address the issue there and then (Lewis et al, 2018; Ludewig et al; 2022). Acknowledging the role of manual therapy in providing short term neurophysiological improvements can be useful for a team to action on findings under strict time constrain. Alongside other strategies such as
motor control exercises and post activation potentiation, practitioners can be proactive in their approach in pre-training preparation to mitigate injury risk and performance (Li et al, 2023). At times when players are reporting poorly on wellness, changing symptoms of their perceived impairment can reinforce their confidence and positively influence team performance (Short et al, 2023).
Example of kinesiopathological approach hip symptom modification framework (Images reproduced from Sports Map article “How to modulate hip pain to maximise performance”, 2025) in Figure 2.
Figure 2: Hip Symptom Modification Framework (Ng, 2025)
“Control the controllables”Management of physiological and mechanical risk factors
Acute injuries
It is no secret that professional footballers play through pain and injuries (Hammond et al, 2014). Research have shown that uniqueness of the changing room environment, psychological and other sociocultural factors, can influence players’ playing decisions, despite having underlying physiological concerns (Hammond et al, 2014). The competitive nature of professional football demands a team of supporting staff with wide range of expertise, with a ‘can do’ mentality to proactively improve players’ readiness and team availability (Read & Rosenbloom, 2024). A clinically structured holistic approach allow practitioners to “think wide and act specific”.
Case study to demonstrate the use of manual therapy in a holistic approach:
Player history:
• > 3 years history of bilateral chronic Achilles tendinopathy
• Right side being managed throughout the season while playing
Load profile:
• A box to box midfielder
• Averages 2.3 matches/14 days (43 matches in 252 days) 9.1km per match throughout the season
• An increase in load following an international break
• Recent 4 matches in 14 days recorded 8.5km, 10.6km, 8.6km and 7.3km
Sociocultural context:
• Key player of the team
• The team is fighting for promotion and is short in central midfielder selection
• Upcoming matches scheduled within 48 hours and 126 hours from the time of assessment
• Manager very keen on player to start both matches
Psychological context:
• Keen to play but unsure if he will be ready given his functional limitation and pain

Figure 3: Holistic multimodal management framework
• Believe that this flare up is worse than previous episodes, as the Achilles tendon is not responding by “doing the same as he has been, icing regularly”, described it as “never felt like this before with the right side”
• A motivated character, willing to “push” if he can functionally jump and hop
Clinical presentation:
• Acute flare up of left sided Achilles tendinopathy
• No acute mechanism, gradual build up of symptoms throughout the last three matches.
• Reported morning stiffness 7/10 VAS
• Subjectively reported 7/10 VAS sharp pain on every step he takes in the past 72 hours, since the last match.
• Objectively compensates with an obvious reduction in push off and hip extension with walking. Reduction in knee to wall range and calf raise height compare to baseline, unable to jump and hop, limited by pain.
• Unable to train
General considerations:
• Targeted intervention informed by subjective and objective findings on mechanism of symptoms
• Appropriate dosage of therapeutic exercises to avoid any flare ups considering recent increase in load and the proximity of upcoming matches

Intervention:
Mechanism Multimodal agents and exercises
Nociceptive (Inflammatory) Circulation circuit:
10’ Cryotherapy > 10’ Mobility Spin > (10s:10s) x2’x2 Elevation ankle pumps ^
2’ every 2 hours foam roll plantar fascia for lymphatic return^
Oral medication: NSAID (Naproxen 250mg) 4/day
Lifestyle:
Selection of anti-inflammatory food
Sleep advice
Nociceptive (Mechanical) Local analgesics:
10’ Cryotherapy ^
20’ Electroacupuncture pain setting 30Hz (BL60, KI3)
Analgesic isometric: (Low volume due to ↑SIN)
Loop banded mid-range isometric hold 3x5x5
Central (Affective) Autonomic, endocrine & non-specific pain modulation:
20’ Electroacupuncture pain setting 30Hz (SP6, SP9)
Yoga/Reformer:
Posterior chain focus including downward dog/bridges/bird dog
Pain education:
Pain vs structure, positive reinforcement
Neurogenic (Segmental)
Glider/Tensioner:
Sciatic nerve floss with tibial bias (10s:10s) x2’x2 ^
Sciatic nerve floss common peroneal nerve bias (10s:10s) x2’x2 ^
Spinal control and mobility:
Spinal dissociation and mobility exercises ^
Biomechanical (Kinetic chain)
Mobility/movement control: (Low volume due to ↑SIN)
Forward lunge rotation into reverse overhead lunge 1x5*
Curtsy lunge rotation into overhead side lunge 1x5*
Single leg Romanian deadlift rotation into hip drive with side trunk flex 1x5*
Sub maximal pain free run specific isometric 3x5x5*
Movement variability:
Big toe-little toe taps in 20° plantar flexion 6x8x8 (forefoot supination-pronation/rearfoot inversion- eversion)
Biomechanical (Local) Load management: (reduce compressive force)
0.5cm heel raise
Motor control/Proprioception:
1x10mx5 Eyes closed banded mid-range tip toe crab walks*
1x10mx5 Eyes closed banded mid-range tip toe monster walks*
Muscle activity: NMES FHL/AbHB 4’ Warm up setting*
Manual Therapy:
Circulation and anti-inflammatory response:
Lymphatic drainage with topic anti-inflammatory agent, magnesium cream ^
Passive physiological movements * Passive accessory movements *
Local neurophysiological response: Lateral to medial transverse mobilisation *
Fascial lifting, desensitise oscillation ^
Autonomic, endocrine & non-specific pain modulation:
Combined effect of nociceptive and neurogenic treatment
Nerve mobility:
Tibial nerve mobilisation
Segmental manipulation:
Proximal and distal tibiofibular glide
L4/L5/S1
Innominate posterior tilt
Regional interdependence:
Ipsilateral hip rotators and posterior capsule manipulation *
Ipsilateral Quadratus lumborum and latissimus dorsi tissue release *
Manipulation:
Talar AP/Talocalcaneal lateral glide/ Cuboid eversion/Mid tarsal joint pronation eversion/1st metatarsal extension/1st MPJ distraction & extension *
Manual diathermic electrotherapy on calf complex 10’ ^
Figure 4: Example of holistic approach in an acute Achilles tendinopathy (NMES: neuromuscular electrical stimulation; SIN: Severity, irritability and nature; MPJ: Metatarsophalangeal joint)
*Part of pre-training preparation upon return to training
^Part of post-training recovery upon return to training
Outcome:
• Participated in the following matches recorded 10km and 9.65km
• Subjectively reported ‘feeling very good’ pre and post both match
• Objectively knee to wall returned to baseline, asymptomatic on walking, jumps and hops
• Functionally returned to within 10% of baseline on countermovement jump height, concentric peak force and eccentric breaking impulse metric (Case study written retrospectively, as repeated hop testing does not form part of the team routine screening and therefore no data was collected)
• Participated in every match rest of the season with a 6.52 performance rating (Season average 6.72)
Degenerative conditions
In progressive degenerative conditions, chronic adaptations such as thickening of capsule and ligaments affect articular joint force vector (Grimaldi et al, 2009). Compromised joint space, repetitive shearing and suboptimal mechanical loading pattern, alongside with the high rate, volume and force of loading, can therefore progressively cause damage and contribute to deformities, such as labral damage associating with CAM morphology in the hip and osteochondral lesions in the knee and talus (Shaw et al, 2022; Fermín et al 2022).
In season, having options to manage joint load and health becomes key in performance and availability contexts, as surgical options such as hip arthroscopy and osteochondral allograft transplantation often comes with a lengthy period of time loss. Alongside pathophysiological diagnosis, assessing specific
contributing factors functionally, such as tissue tension and movement patterns, can provide practically meaningful findings for treatment (Lewis et al, 2018; Ludewig et al 2022).
Effective use of manual therapy improves function and arthrokinematics, which enhances therapeutic effects of other interventions such as exercises, orthoses and hyaluronic acid injection (Short et al, 2023).
Conclusion
This editorial provides insights on the considerations to incorporate manual therapy in the context of pain modulation, injury risk management and performance. The value of manual therapy in holistic athlete management should not be overlooked. Further research exploring evidence informed practice of manual therapy, individual and team benefits, can encourage discussions around optimising the use of manual therapy in professional football.
References
Caneiro, J.P., Alaiti, R.K., Fukusawa, L., Hespanhol, L., Brukner, P. and O’sullivan, P.P., 2021. There is more to pain than tissue damage: eight principles to guide care of acute non-traumatic pain in sport. British journal of sports medicine, 55(2), pp.75-77.
CIES Football Observatory, 2024, Match calendar and player workload.
Clar, C., Tsertsvadze, A., Court, R., Hundt, G.L., Clarke, A. and Sutcliffe, P., 2014. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & manual therapies, 22, pp.1-34.
Clifford, C., Challoumas, D., Paul, L., Syme, G. and Millar, N.L., 2020. Effectiveness of isometric exercise in the management of tendinopathy: a systematic review and meta-analysis of randomised trials. BMJ open sport & exercise medicine, 6(1).
de Sire, A., Marotta, N., Prestifilippo, E., Parente, A., Lippi, L., Invernizzi, M., Longo, U.G. and Ammendolia, A., 2024. Effectiveness of physical agent modalities for pain relief in injured athletes: A systematic review. Journal of Back and Musculoskeletal Rehabilitation, p.10538127251314711.
Grimaldi, A., Richardson, C., Durbridge, G., Donnelly, W., Darnell, R. and Hides, J., 2009. The association between degenerative hip joint pathology and size of the gluteus maximus and tensor fascia lata muscles. Manual therapy, 14(6), pp.611-617.
Hainline, B., Derman, W., Vernec, A., Budgett, R., Deie, M., Dvo ák, J., Harle, C., Herring, S.A., McNamee, M., Meeuwisse, W. and Moseley, G.L., 2017. International Olympic Committee consensus statement on pain management in elite athletes. British Journal of Sports Medicine, 51(17), pp.1245-1258.
Hammond, L.E., Lilley, J.M., Pope, G.D., Ribbans, W.J. and Walker, N.C., 2014. ‘We’ve just learnt to put up with it’: an exploration of attitudes and decision-making surrounding playing with injury in English professional football. Qualitative Research in Sport, Exercise and Health, 6(2), pp.161-181.
Fermín, T.M., Macchiarola, L., Zampeli, F., Maskalo, G., Olory, B., Papakostas, E., Murawski, C.D., Hogan, M.V., Kennedy, J.G. and D’Hooghe, P., 2022. Osteochondral lesions of the talar dome in the athlete: what evidence leads to which treatment. Journal of Cartilage & Joint Preservation, 2(2), p.100065.
Fitzpatrick, D., Leckie, T., Heine, G. and Hodgson, L., 2024. The use of pain killers (NSAIDs) in athletes: How large is the risk?. Journal of Science and Medicine in Sport.
Lewis, J., Mintken, P.E. and McDevitt, A.W., 2025. Treating musculoskeletal conditions with a bit of exercise and manual therapy: are you kidding me? It’s time for us to evolve again. Journal of Manual & Manipulative Therapy, pp.1-6.
Ludewig, P.M., Saini, G., Hellem, A., Kahnert, E.K., Rezvanifar, S.C., Braman, J.P., Staker, J.L. Changing our Diagnostic Paradigm Part II: Movement System Diagnostic Classification, 2022. Int J Sports Phys Ther. 17(1):7-17.
Read, D. and Rosenbloom, C., 2024. What contextual factors influence pain management decision making concerning player availability in professional men’s football? A qualitative analysis of practitioner perceptions. Science and Medicine in Football, pp.1-12.
Short, S., Tuttle, M. and Youngman, D., 2023. A clinically-reasoned approach to manual therapy in sports physical therapy. International journal of sports physical therapy, 18(1), p.262.
Silva, F.P.D., Severo-Silveira, L., Plentz, R.D.M., Durigan, J.L.Q. and Baroni, B.M., 2020. Electrophysical agents in clinical practice of orthopedic and sports physical therapists in Brazil. Fisioterapia e Pesquisa, 27, pp.202-209. Tscholl, P.M., Vaso, M., Weber, A. and Dvorak, J., 2015. High prevalence of medication use in professional football tournaments including the World Cups between 2002 and 2014: a narrative review with a focus on NSAIDs. British journal of sports medicine, 49(9), pp.580-582.



ESTABLISHING TEAM MATCH PHYSICAL
PERFORMANCE REFERENCE VALUES AT UEFA EURO 2024 GERMANY
FEATURE / SHUYAO CHEN1, DR PIOTR ZMIJEWSKI2,3, PROFESSOR PAUL S. BRADLEY4,5
Introduction
The UEFA European Championships 2024 was the 17th instalment of Europe’s flagship quadrennial international tournament. This tournament did not disappoint on a team level, with breath-taking performances from Luis de la Fuente’s Spain who become the first nation to win it four times. In fact, La Roja set a new tournament scoring record with 15 goals, therefore surpassed the 14 goals France scored in 1984. Moreover, the avid football fan was completely absorbed by the performances of debutantes Georgia, as they reached the knockout stage. On an individual level, numerous players excelled but Spain’s dynamic wing duo of Lamine Yamal and Nico Williams were fearless and exquisite at creating penetrating width. This was despite Yamal being the youngest player to ever appear at the tournament and Williams the youngest to score at a European Championship final since 1968.
This tournament showcased some fascinating tactical trends ranging from player-for-player defending to unique attacking interplay between wide defenders and wingers.1 Another feature of UEFA Euro 2024 was the elevated intensity of matchplay for selected teams. From a collective perspective, Austria’s aggressive counterpressing after losing the ball exhibited the switching up of intensity for some teams in the tournament. Pertinent examples of individual physicality varied from the tireless work rate of Portugal’s Bernardo Silva to the lighting fast sprints of France’s Kylian Mbappé. As a comprehensive tactical overview of this tournament has already been presented,1 and the current authors have also examined the demands across position,2 a more detailed analysis was needed on the collective physicality of match-play. The UEFA report1 has not standardised team physical data (e.g., it
did not exclude extra time) and thus these averages cannot be used as benchmarks. The scientific literature typically homogenises analyses by only quantifying physical metrics across normal time plus added time.3 Thus, this piece will examine the team physical demands at UEFA Euro 2024 using a similar filtering method to previous work. This essentially means that the data presented below excluded extra time and goalkeepers. This information may provide a snapshot into the basic physical benchmarks of international teams. Documenting this is especially important given the intensification of modern match demands at international competitions.3 Thus, the findings from this piece could provide valuable information about the match demands at recent tournaments, which could be useful for teams to optimise their physical preparations.
1. Typewind Ltd, UK
Jozef Pilsudski University of Physical Education, Warsaw, Poland
Research & Development Centre Legia Lab, Legia Warszawa, Poland
Football Science Consultant, UK
German Sport University Cologne, Germany
Benchmarking the Match Demands at Team Level
The UEFA Euro 2024 tournament showcased some diverse tactical philosophies and physical approaches across the 24 nations competing. This analysis provides a detailed examination of the interplay between tactical systems, match context, opponent styles and physical performances.
All games were analysed during the competition using a multi-camera optical tracking system. Data were then separated into three main physical metrics: total, high-intensity running and sprinting distance (e.g., presented as absolute values). Total distance represented the overall ground covered during match-play. High-intensity running consisted of the distance covered ≥20 km·h −1, while sprinting included the distance covered ≥25 km ·h −1. As previously noted, the trends below analysed match data that excluded extra time and goalkeepers. This was unlike previously published trends 1 that included some of those elements. Thus, some differences would be expected between the two sources.
Total Distance Covered Team total distance is commonly reported to highlight the overall collective activity of all outfield players. This is generally informative for a practitioner as it gives a snapshot into the volume of activity a team has undertaken. No previously standardised team benchmarks have been reported for this specific UEFA tournament and therefore the insights below are extremely novel. Figure 1A demonstrates that the average total distance covered at UEFA Euro 2024 was 112.7 km. This value was slightly higher than the benchmark reported at the FIFA World Cup 2022. 3 Interestingly, Croatia, Germany and Czechia were in the top three and Belgium, Netherlands and France were in the bottom three teams for the overall ground covered during matches (Figure 1A). Regarding individual game context, Germany covered the most distance at the tournament in their draw against Switzerland (124.2 km). As Germany controlled this game, their high overall work rate was associated with collective movement going forward to be an offensive threat. For instance, German attackers regularly ran in behind or between the lines more in this game than any other. These offensive sequences were regularly followed by supporting runners. Although Germany generally dominated possession, they still worked hard collectively to press and track back regularly when out of possession. In
contrast, Scotland covered the lowest overall distance of the tournament against Germany in their heavy 5-1 defeat (103.6 km). As Scotland were without the ball for long periods in that game, they defended in a compact lowto mid-block and used a direct approach in build-up when occasionally regaining possession. Similar match physical performance trends were reported at the FIFA World Cup 2022 for teams that employed a similar deep lying defensive style. 3
High-Intensity and Sprinting Distance
Although team total distance quantifies collective volume, the ground covered at higher speeds provides an indication of intensity. This is incredibly important as intensity is linked to key moments in games (e.g., goal scoring opportunities). Regarding intense collective movement, Figures 1B-1C demonstrated average team high-intensity and sprinting distances, respectively. On average, teams covered approximately 8.0 km and 2.1 km in the high-intensity and sprinting speed zones (≥20 km·h -1 and ≥25 km·h -1). Although fairly similar averages were attained for team total distance covered at the UEFA Euro 2024 tournament (Figure 1A) compared to those at the FIFA World Cup 2022, 3 this was not the case for intense metrics. Despite the upper speed thresholds being identical at both competitions (≥20.0 km·h −1 and ≥25.0 km·h -1), the average distances covered were lower at UEFA Euro 2024. This disparity could be due to differences in the optical tracking systems employed, the filtering and dwell times applied to the raw data, in addition to varying match durations across both tournaments. 4,5 Austria were positioned first and second respectively for the distances covered at the upper speed zones (≥20 km·h -1 and ≥25 km·h -1). Although Romania were placed ninth for team high-intensity distance, they were ranked first for team sprinting distance. Interestingly, Slovenia, Serbia and Albania were placed within the bottom three at the tournament for the upper speed zones.
Match Variation
Each team’s variation in match physical performance can be subjectively observed in Figures 1A-1C by viewing the scatter of the dots around each bar (e.g., each dot represents an individual match). For instance, greater scatter equates to more performance variation from game to game. To improve objectivity, each team’s coefficient of variation (CV) was calculated to determine the data spread across each
metric. Team match-to-match CV’s at the tournament for the distance covered in total and also that covered at higher intensities (≥20.0 km·h -1 and ≥25.0 km·h -1) were 3.0%,11.8% and 17.2%, respectively. Although striking similarities were found for the variation in total distance between UEFA Euro 2024 compared to the FIFA World Cup 2022 (3.0% vs 3.2%), 3 the spread for the distances covered at the upper speed zones were greater at UEFA Euro 2024 (≥20 km·h -1: 11.8% vs 9.1% and ≥25 km·h -1: 17.2% vs 13.9%). Positional variability for high-intensity metrics across both tournaments also corroborated this trend. 2,6
Team physical performance variability at UEFA Euro 2024 was highly dependent upon each team and metric. The lowest variability was evident for the Netherlands, Hungry and Croatia for the distances covered in total (CV: 0.9%), high-intensity (CV: 3.3%) and sprinting (CV: 3.2%), respectively. Alternatively, Scotland (6.2%), Romania (17.9%) and Denmark (30.5%) exhibited the most variation from match-to-match for the distance covered in total, highintensity and sprinting, respectively. To understand Denmark’s considerable match to match sprinting variation, it can be helpful to observe the nature of the games at the extremes. For instance, Denmark covered their greatest sprint distance in their round of 16 defeat against the hosts Germany. While their lowest sprint distance was in their draw against Serbia in the last group game. This substantial range was not the result of a large mismatch in match duration, as both games were played over a similar duration. Research has demonstrated that a powerful influencing factor of a team’s work-rate is the opposition they play against. 7 Thus, this trend was understandable as Germany were one of the top four sprinting teams, while Serbia were in the bottom two sprinting teams at UEFA Euro 2024. Although it is important the reader is aware that numerous factors may also influence collective performance variability (see final section of this piece on the various contexts and tactics that could impact match demands).The maximum and minimum team values reported here for UEFA Euro 2024 were roughly in the region to that documented at the FIFA World Cup 2022 for the distances covered in total (max: 124.2 vs 121.2 km; min: 103.6 vs 97.7 km), high-intensity (max: 11.1 vs 12.0 km; min: 5.6 vs 6.0 km) and sprinting (max: 3.2 vs 3.6 km; min:1.2 vs 1.1 km). 3



Figure 1: Average team distance in: (A) total, (B) high-intensity, (C) sprinting and match-to-match variation at UEFA Euro 2024. Normalised for 90 min plus added time (excludes goalkeepers and extra time).
B.
C.
Quadrant Plots: Team Volume Versus Intensity
Identifying how teams physically perform across key dimensions could aid preparations (e.g., volume and intensity). For instance, verifying your teams’ characteristics enables training specificity to occur and knowing your oppositions profile prior to a match helps you scout them. Although only a moderate association was found between the total and high-intensity distance covered (≥20.0 km·h-1) across all UEFA Euro 2024 matches (r=0.54; P<0.01), each team revealed a distinctive profile (Figure 2A). Thus, using quadrant plots enabled team comparisons to be made and this could facilitate the strategic formulation of opposition plans. For instance, playing against high volume and intensity teams such as Austria, Croatia, Germany or Czechia in the upper-right quadrant may require a greater work rate throughout the game to physically compete against them. In contrast, a more sedate activity profile could be expected against low volume and intensity teams in the lower-left quadrant such as Albania, Belgium, England and the Netherlands. The most fascinating information can be gleaned from the upper-left and lower-right quadrants as these are teams high on one physical dimension but low on another. The reader should be cognisant that these quadrants usually have fewer extreme instances. Romania were an interesting upper-left quadrant exemplar, as their volume was lower than the tournament average but they performed at an above average intensity. Slovenia were the reverse of this, with above average volume but their intensity was below tournament benchmarks.
A weak association was found between the total and sprint distance covered (≥25.0 km·h-1) across all UEFA Euro 2024 matches (r=0.26; P>0.05). The quadrant plot revealed sprinting trends were reasonably similar to that demonstrated for high-intensity running, with a few notable exceptions (Figure 2B). A noteworthy difference
was the number of teams that fall around the tournament average for sprinting distance as opposed to high-intensity distance (Figures 2A and 2B). Romania’s prominent sprinting performances at the tournament resulted in them being positioned even higher in the upper-left quadrant compared to their highintensity distances. The reverse trend was true for Italy as their much lower sprinting distances positioned them further down in the lower-right quadrant. Croatia also demonstrated a lower position in sprint distance versus high-intensity distance. Finally, in the bottom-left quadrant it was evident that Georgia moved up and Albania moved further down.
Additional Tactical and Contextual Considerations Related to the Collective Match Demands at UEFA Euro 2024
In accordance with previous tournments,3,7 tactics and contextual factors emerged as potential determinants of a teams’ physical output at UEFA Euro 2024. The authors have used video and/or event data in an attempt to highlight ‘why’ the demands across teams were potentially different. Teams employing proactive pressing strategies such as Austria, Spain and Portugal seemed to record notably greater high-intensity distances (Figure 1B). Austria exemplified this relationship, registering the maximum high-intensity distance at the tournament (11.1 km). Their tactical commitment to relentless pressing may have elevated their running demands. A recent study demonstrated that ball recoveries were positive predictors of winning at UEFA Euro 2024.8 Thus, intense pressing in selected pitch areas may increase the likelihood of a ball recovery via an interception or tackle, which may then progress to offensive play. Austria’s high match demands may have also been influenced by their 4-2-2-2 formation, that emphasised vertical passing and dribbling to directly penetrate the opponent’s defensive line. This

approach allowed them to maintain a high pitch position, which also facilitated their highpressing tactics when a turn-over in possession occurred. When opposition teams beat their high press, this required Austrian players to cover long intense recovery runs to get into a better tactical position. Research highlights that recovery running accounts for one of the greatest proportions of a team’s high-intensity distance3,9 and could be a contributory factor linked to Austria’s high match demands.
Spain’s energetic 4-3-3 system, characterised by quick wing play and passing in addition to intense off the ball movement in the final third was consistently associated with elevated physical outputs. Interestingly, passing in the final third was found to be strong predictor of winning at the tournament,8 and Spain excelled at this quality. Conversely, teams that adopted a more conservative approach by prioritising defensive compactness and positional discipline (e.g., France, Serbia, Albania) seemed to consistently register lower total distances. For instance, France averaged the lowest total distance at the tournament (107.6 km), and this could be due to their tactical approach that was geared towards efficient positioning. However, their physical outputs notably increased in the knockout stages or when trailing in games, indicating an ability to adapt their physicality based on the match context.
Match importance and game state may have also influenced match physical performances at the tournament. For instance, matches with decisive outcomes such as the Croatia vs Italy group encounter and the Germany vs Denmark knockout clash, were associated with heightened match intensity. Conversely, matches with mutually beneficial outcomes such as the Slovakia vs Romania game resulted in reductions in physical outputs as teams strategically conserved energy. In agreement with the findings from the FIFA World Cup 2022,3,7 the opponent’s style and quality may have also affected match running performances at UEFA Euro 2024. For instance, encounters between possession-oriented teams (e.g., Germany) and defensive teams (e.g., Scotland) resulted in physical outputs that were opposing, with possession dominant teams typically running more. Conversely, matches featuring two high-intensity teams such as Spain and Georgia, mutually elevated running outputs, reflecting reciprocal intensity.
Czechia maintained a high overall work-rate with players interchanging roles regularly and this resulted in extensive movement during match-play. This could be attributed to their top three position at the tournament for the total and high-intensity distance covered in matches. While Croatian players’ on-field responsibilities did not vary as dramatically as the Czechs (hence their lower match-to-variability across


Figure 2: Average team distances in: (A) total versus high-intensity and (B) total versus sprinting at UEFA Euro 2024. Normalised for 90 min plus added time (excludes goalkeepers and extra time).
all physical metrics), but multiple midfielders were responsible for large coverage areas, thus providing effective linking functions for the team. In fact, a recent study benchmarking specialised positions at UEFA Euro 2024 demonstrated that Croatian midfielders Marcelo Brozovic and Lovro Majer covered some of the highest overall distances at the tournament.2 Croatia notably recorded the highest average total distance (118.8 km) and ranked second for high-intensity running distance (9.4 km) at UEFA Euro 2024. These outputs are indicative of their aggressive pressing and particularly their high defensive line that required players to track back when turn-overs occurred. Despite Croatia’s physicality, their limited tactical efficiency in front of goal ultimately undermined their competitive standing (only two goals in three matches). This highlights that physicality alone is insufficient without precise tactical execution. Portugal’s midfield approach was similar but with the key difference being their younger squad. As research has found a clear link between age and physical match performance,10 it could highlight that Portugal’s youthful squad were able to combine patient build-up play with explosive transitions, thus achieving high team sprinting outputs at the competition.
Despite Italy’s high overall distance covered, they struggled to establish a clear tactical identity resulting in lower-than-average highintensity and sprinting distances. The Azzurri couldn’t raise their game tempo as evidenced by their opening match against Albania. This game was one of the slowest of the tournament and resulted in Italy recording the lowest (1.2 km)
References
and Albania the third (1.4 km) lowest sprinting distance at the tournament. Although Italy and Germany’s requirements for midfield coverage areas cannot compare with Croatia and Portugal, they still maintained a high overall work-rate during UEFA Euro 2024. The disparity between these two teams lies in their additional positional responsibilities. For example, Italy’s centre-backs were tasked with ball progression during build up play (e.g., Riccardo Calafiori covered ~12.0 km in total in certain games), while Germany’s forwards frequently dropped back to get involved with play (e.g., Kai Havertz covered ~1200 m at high-intensity in selected games).2 These additional duties further increased both teams’ movement demands.
Conclusion
This is the first time that the physical demands of international teams competing at the UEFA Euro 2024 tournament have been benchmarked in a standardised manner (e.g., full game data minus extra time). As this piece will be read by both performance and medical practitioners within elite football, it is imperative that they are aware of the current demands of the game. The data presented in this piece clearly demonstrate the high physical demands of contemporary international football. Accordingly, performance and medical practitioners should be cognisant of the fact that a team’s physical demands are shaped by a myriad of factors and this makes interpretations challenging (e.g., demands are influenced by tactics, score, opposition standard, environment etc). It is important to be aware that large variations in
the demands will occur from game to game. Ideally, these demands should be viewed from an individual (each game) and collective (all games) perspective to gain a more rounded view of the physicality of match play. Moreover, adding context to the physical trends creates a much-needed narrative to the data that can be used from a practical perspective (e.g., insights and/or training application). These findings are important to medical and performance practitioners as they prepare players to not only perform intensely during games but ideally be robust enough to repeatedly compete without injury. Thus, high-intensity training is essential to enable players to compete and remain on the pitch during such tournaments. For instance, high-intensity training interventions over just a four-week period were found to have a favourable impact on players endurance and repeated sprint abilities.11 Furthermore, targeted and appropriately loaded high-speed running interventions at selected times during the training week may reduce hamstring injuries.12
Corresponding author:
Shuyao Chen, Typewind Ltd, UK E-mail: shuyao.chen@typewind.co.uk
Conflict of Interest:
No conflict of interest was reported by authors. Shuyao Chen was responsible for all data presented (e.g., ownership, permission, cleaning, filtering, analysing, quality control and visualising), conceptualising in addition to writing aspects of the study. Professor Paul Bradley and Dr Piotr Zmijewski were only responsible for writing parts of the study.
1. UEFA Euro 2024 Germany. Technical Report. 2024, Nyon: UEFA. Available from: https://uefatechnicalreports.com/pdf-euro-2024technical-report. 1-53. [Accessed February 2025].
2. Chen S, Zmijewski P, Bradley PS. Establishing reference values for the match running performances of thirteen specific positional roles at UEFA Euro 2024. Biol Sport. 2025;42(3).
3. Bradley PS. ‘Setting the Benchmark’ Part 2: Contextualising the Physical Demands of Teams in the FIFA World Cup Qatar 2022. Biol Sport. 2024 Jan;41(1):271-278.
4. Randers MB, Mujika I, Hewitt A, Santisteban J, Bischoff R, Solano R, Zubillaga A, Peltola E, Krustrup P, Mohr M. Application of four different football match analysis systems: a comparative study. J Sports Sci. 2010 Jan;28(2):171-82.
5. Varley MC, Jaspers A, Helsen WF, Malone JJ. Methodological Considerations When Quantifying High-Intensity Efforts in Team Sport Using Global Positioning System Technology. Int J Sports Physiol Perform. 2017 Sep;12(8):1059-1068.
6. Bradley PS. ‘Setting the Benchmark’ Part 1: The Contextualised Physical Demands of Positional Roles in the FIFA World Cup Qatar 2022. Biol Sport. 2024 Jan;41(1):261-270.
7. Bradley PS. ‘Setting the Benchmark’ Part 5: The Contextual and Tactical Factors that Influenced the Physical Match Demands at the FIFA Men’s and Women’s World Cups. Footb Med & Perf Assoc Magazine. 2025 Jan; 48:19-25.
8. Stafylidis A, Mandroukas A, Michailidis Y, Metaxas TI. Decoding Success: Predictive Analysis of UEFA Euro 2024 to Uncover Key Factors Influencing Soccer Match Outcomes. Appl. Sci. 2024 Sept; 14: 1-13.
9. Bradley PS. The Premier League Way: Contextualising the Demands of the World’s Most Intense League. 2022; Amazon, UK.
10. Rey E, Costa PB, Corredoira FJ, Sal de Rellán Guerra A. Effects of Age on Physical Match Performance in Professional Soccer Players. J Strength Cond Res. 2023 Jun 1;37(6):1244-1249.
11. Fransson D, Nielsen TS, Olsson K, Christensson T, Bradley PS, Fatouros IG, Krustrup P, Nordsborg NB, Mohr M. Skeletal muscle and performance adaptations to high-intensity training in elite male soccer players: speed endurance runs versus small-sided game training. Eur J Appl Physiol. 2018 Jan;118(1):111-121.
12. Gómez-Piqueras P, Alcaraz PE. If You Want to Prevent Hamstring Injuries in Soccer, Run Fast: A Narrative Review about Practical Considerations of Sprint Training. Sports (Basel). 2024 May 15;12(5):134-150.


TACKLING FOOTBALL’S ACHILLES HEEL
FEATURE / DR COLIN GRIFFIN, PHD, ASCC
Introduction
Every professional football team can anticipate at least one Achilles tendon injury per season, and, if fortunate, a rupture every few years. Achilles tendinopathies account for 2.5% of all injuries in professional football, with initial injuries resulting in an average absence of 18-23 days1 and 22% of cases with symptoms lasting more than 4 weeks.2 However, the recurrence rate is 27%, with an elevated risk if recovery from the initial injury is less than 10 days with older players particularly susceptible.1 Recurrent Achilles tendinopathies can extend absence times to more than 30 days.1
Achilles Tendon Injuries
A tendinopathy is the most prevalent type of Achilles tendon injury in football, occurring at the mid-portion (2-7cm above the heel insertion) and at the heel insertion.2 Other common midportion Achilles tendon injuries include paratenonitis – inflammation of the paratenon – and plantaris-related Achilles tendon pain, which may necessitate additional interventions; the latter accounts for 20% of all cases of midportion Achilles pain and often requires
surgical removal.3 In cases of insertional Achilles pain, contributing factors such as retrocalcaneal bursitis, a Haglund’s deformity, or enthesitis (inflammation of the bone tissue at the tendon insertion) may also be present. An Achilles tendon rupture typically occurs at the midportion, often with evidence of pre-clinical tendinopathy coupled with an inciting event involving an explosive action and poor control of rapid dorsiflexion.4,5
Achilles Tendinopathy
Over the past few decades, the understanding of tendinopathy has evolved from viewing it as an acute inflammatory issue (tendinitis) to recognising it as a tissue degeneration issue (tendinosis). It is now understood to involve a complex interaction between immune cells, tenocytes, and the extracellular matrix, typically resulting from overload or an inability to adapt to regular stress.6 Some athletes may exhibit a heightened inflammatory response and should be assessed for potential underlying health conditions that could contribute to this injury. Pain at multiple tendon insertion sites may suggest an underlying inflammatory condition, warranting a more holistic treatment plan.7 Other systemic health factors impacting
tendon health include metabolic disorders such as diabetes, cardiovascular disease, hypertension, and haemochromatosis8 Medications such as fluoroquinolone antibiotics, statins, and corticosteroids may also affect tendon health.6
The pain experienced by patients does not always correlate with structural findings on imaging or functional impairments. It is widely accepted that the release of neuropeptides, such as Substance P and glutamate, stimulates the sprouting of unmyelinated nerve endings, resulting in amplified nociceptive feedback.6 Biopsychosocial factors may also be present in some patient subgroups;9 given the stresses of professional sport and the impact of injury, appropriate supplementary support should be considered.
Individual Anatomy Matters
The Achilles tendon comprises subtendon fibres from the soleus, medial, and lateral gastrocnemius muscles. These fibres form a spiral orientation, rotating at the midportion to insert at the calcaneus as illustrated in Figure 1. The deeper fibres from the soleus insert on the anteromedial aspect of the calcaneal tuberosity, while the superficial layers from the lateral gastrocnemius insert
Lower-limb Rehabilitation Specialist, Sports Medicine Department UPMC Sports Surgery Clinic, Dublin

Figure 1: An illustration of the spiral anatomy of the subtendon fibres from the individual triceps surae muscles. Image designed by Vicky Earle. Reproduced with permission from Merry, K., Napier, C., Waugh, C. M., & Scott, A. (2022)17
on the medial aspect, and the medial gastrocnemius on the posterior aspect, with some individual variations.10,11 The soleus has the largest muscle volume and force contribution to the Achilles tendon and its deep subtendon fascicles experience the greatest displacement.12–14 Given the slightly medialised orientation of the AT around the subtalar joint axis, the triceps surae provides an inversion moment.15 However, variable anatomy at an individual muscle level and torsion of the AT subtendon fascicles, as well as foot posture, may impact this joint moment and AT strain.16
Given the anatomical variation of the individual triceps surae muscles and classifications of torsion among the subtendon fibres, muscle coordination, foot shape, and rotation will impact tendon strain and stress distributions. During the stance phase, when the tibia internally rotates, the subtendon fibres externally rotate18 – a mechanism that may be compromised in a stiff cavus foot type. In young, healthy tendons, there is variable sliding between the deep and superficial layers of the tendon, a characteristic that diminishes in older tendons and following tendinopathy.19 Reduced neural drive and atrophy of the lateral gastrocnemius are commonly observed in Achilles tendinopathy, resulting in altered triceps surae coordination.20,21 When assessing a patient, it is important to consider the shape of the triceps surae and foot posture.
A Muscle Needs a Good Tendon
The Achilles tendon acts interchangeably to facilitate efficiency, amplify force, or dissipate energy, depending on the task. A tendon with optimal stiffness (the ability to resist elongation in response to applied force) enables the muscle fascicles to operate on their preferred region of the force-length-velocity curve, thus promoting efficient muscle contractions during repetitive movements like running,22 or effective force transmission and energy return during explosive actions such as jumping or accelerating.23,24 Therefore an injury to a region of the tendon can alter the function of its muscle origin – more likely due to loss of tension of the subtendon fascicle resulting in reduced neural drive and altered architecture to the muscle.25,26
Tendons Like Routine
Tendons are metabolically active and mechanosensitive organs. Some individuals are more sensitive to acute and accumulative changes in training and match loads. When fatigue accumulates, musculotendinous unit (MTU) capacity reduces. The addition of travel, disrupted sleep quality, altered circadian rhythm, and added stress creates an environment conducive to Achilles tendon injuries. This poses a challenge in professional football, where congested match schedules and some high-risk players may require careful monitoring and individualised programming.
Assessments
Diagnostics
Clinical tests can aid in differentiating between Achilles tendinopathy and paratenonitis, as well as other differential diagnoses, but where feasible, imaging provides greater clarity. MRI is the gold standard imaging technique for muscle or tendon injuries, but point-of-care ultrasound (POCUS) can be provide good diagnostic clarity in tendons. Common features of Achilles tendinopathy include fusiform swelling in the anterior-posterior plane. Oedema on the peripheral aspects of the Achilles tendon indicates paratenonitis or plantaris involvement if oedema is visible between the two structures in close proximity. Dynamic ultrasound imaging may be useful to verify plantaris interference and to detect Haglund’s deformity or retrocalcaneal bursitis contributing to irritation at the insertion. Other features, such as power Doppler, may suggest regionalised neovascularisation and inflammatory activity. Ultrasound tissue characterisation (UTC) is used to classify tissue quality within the tendon based on echo type, providing a useful screening tool for tendon health and detecting early degeneration in regions of tissue. Other differentials to exclude include sural nerve irritation if the pain is on the lateral side, as well as posterior ankle impingement.

Figure 2: A screening framework for Achilles tendon injuries

Anatomy and Muscle Morphology
It is important to develop a comprehensive understanding of the player and identify all plausible factors that may be impacting the injury. This begins with assessing their foot shape and tibia alignment. A rigid cavus foot type can prove challenging for players with a Haglund’s deformity, where a calcaneal varus with limited ability to rotate may exacerbate the issue. In these cases, it is worth assessing ankle eversion strength and addressing any deficiencies in the peroneal muscles. Muscle morphology may also suggest patterns of loading and de-conditioning. Football players
often exhibit external rotation of the foot when kicking and passing, favouring the medial gastrocnemius muscle. Reduced neural drive to the lateral gastrocnemius muscle and increased demand on the soleus muscle is a common pattern detected in Achilles tendinopathy. These features may influence regional strains within the Achilles tendon due to an imbalance in individual muscle recruitment.25
Strength and Capacity
Assessing peak strength from the calf complex and muscle endurance provides
a comprehensive profile the athlete’s calf capacity (see Figure 4). Isokinetic dynamometry, isometric force plate testing, or repetition maximum testing using external loads lifted on a Smith machine or leg press will provide a measure of peak strength. The most widely used test is a seated calf isometric test, where a peak force of around twice bodyweight is a target. An isokinetic strength test with the knee extended at slower speeds of 30º/sec enables relative torque values of more than 100% bodyweight to be produced, with values in excess of 160% bodyweight desirable. A single leg heel raise test on a 10º incline board or off a step to a metronome of 60 beats per minute to fatigue or technical failure is a simple clinical test to measure calf endurance. This can be objectified by using the Calf Raise app, where total work done or decline in output can be measured.27 If time allows, including a measure of kinetic chain and synergist muscle strength may be useful. The synergist muscles should include the ankle invertors, evertors, and toe flexors, which can be measured with a handheld dynamometer or on the ForceFrame. Surface EMG can be used to measure activation patterns among the individual triceps surae muscles, and in vivo ultrasound can measure tendon strain in response to external load on calf strength exercises to individualise exercise prescription. A full battery of performance assessments are outlined in Figure 3.

Figure 3: Performance assessments
Figure 4: A calf capacity quadrant to profile an athlete based on their calf peak strength and endurance

5: Tendon strain of between 4.5-6.5% with at least 3 seconds time under tension has been found to be the sweet spot to improve tendon mechanical properties
Power and Reactive Strength
While calf muscle strength and capacity, as well as synergists and kinetic chain function, are critical, it is also important to measure stretch-shortening cycle (SSC) capacity through jumping and hop testing. The tendon tensile loading rates in these tasks closely replicate the demands of moderate-to-high speed running. 28–30 These tests can include double and single leg drop jumps, a single leg horizontal plyometric task, a repeated hop test such as a 10-5, and a countermovement jump. Aside from performance outcome metrics such as RSI and jump height or hop distance, it is useful to assess the player’s strategy by looking at the force trace and using complementary video analysis to identify any relevant kinematic features. Relative symmetry in performance metrics and a smooth force trace with sound kinematics are key targets.
Rehab
Tendons require tension and adequate strain (4.5-6.5%) to adapt and minimise negative adaptations 31–34 as illustrated in figure 5. Therefore, complete rest should be avoided when managing a tendinopathy without co-existing partial tears or paratenonitis. In the presence of paratenonitis, it is important to offload movements that cause friction in the tendon until the oedema subsides, often requiring anti-inflammatory
medication. The objective is to identify the appropriate entry level of calf and Achilles loading exercises and progress through a graded rehabilitation pathway. For a player with a very painful tendinopathy, this may involve low load, long duration isometrics or a modified calf raise that does not provoke symptoms beyond a tolerable level. Others may enter at more advanced calf exercises and include plyometric exercises early on. 35 An individualised approach is key, informed by initial assessments. Many players will present with calf muscle strength deficiencies, and often the lateral gastrocnemius experiences reduced neural drive and appears atrophied. As well as building global calf strength and capacity, targeting individual muscles such as the lateral gastrocnemius may be prudent. A healthy tendon experiences non-uniform strain between the subtendons from the individual muscles and between the deep and superficial layers – a mechanism that is compromised in older tendons and in tendinopathies. 19,36 Therefore, targeting the individual muscles may help restore that nonuniformity to ensure stresses are more evenly distributed across the tendon.
37
Plyometric exercises should initially focus on smooth ground contacts through active dorsiflexion during the flight phase to generate pre-tensioning of the
MTU and more favourable tendon loading during the early stance phase. 38 Once skill and capacity have been developed bilaterally and unilaterally, and in multiple planes, plyometric exercises can be intensified. For players who are naturally plyometric and less robust, caution needs to be applied with their plyometric loading. Players who fit this profile may benefit from keeping their plyometric loading submaximal and focusing more on building capacity and robustness.
Running can be introduced or progressed when a player is tolerant to consecutive plyometric sessions and demonstrates minimally acceptable calf strength and capacity, such as >1.6 x BW on a seated calf isometric test and >25 single leg calf raises through range. For players with milder symptoms and timely intervention at the reactive stage, removing running from their program may not be necessary. This may also provide an opportunity to work on running technique and coordination. Running can be progressed to the point where the player covers consecutive sessions of >3000m volume at moderate speeds, 400m of high-tomaximal speed running, and a club-agreed number of accelerations, decelerations, tackles, and other game-specific tasks. Once the player is pain-free, maintaining some calf and Achilles loading in their program and treating it like an ongoing injury is important.
Figure
Address neuromuscular inhibition & atrophy to individual TS muscles
If reduced EMG activity or atrophy to LG
Calf raises with feet turned BFR and/or NMES can be added on injured leg
e.g. 4 x 10-15 reps @ 2 RIR
SL calf long ISO holds
e.g. 4 x 30-45s e/s @ BW>30% BW
Progress to single-leg working into ↑ TUT in dorsiflexion

Conclusion
Develop synergist muscles & kinetic chain strength
If inhibition/strength deficits in ankle invertors/ evertors/ intrinsic foot muscles
Band/cable resisted inversion/eversion
Assess hip abduction and extension strength and include targeted exercises if there are deficiencies
Maintain/develop kinetic chain strength with squats/deadlifts and single leg exercises such as step-ups and lunge variations
• Effective management of Achilles tendinopathies require a thorough assessment of individual anatomy, muscle morphology, strength, capacity, and biomechanics, as well as medical history to identify contributing factors and guide personalised rehabilitation.
• Rehabilitation should be tailored to the specific needs of the player, considering the severity of the tendinopathy and individual deficiencies. A graded
References
Build calf strength & capacity Develop AT stiffness
Use calf endurance test and maximal strength test to determine volume
SL calf raises working into dorsiflexion.
Regress with heel on floor or on a wedge if painful tendon or insertional tendon pain and progress when tolerable
e.g. 4 x 8-12 reps e/s @ 2 RIR
Progress to 4 x 6 reps e/s @ 2RIR aiming for >65% BW external load on a smith machine
Determine optimal calf loading to achieve 5% AT strain SL calf ISOs on smith machine/leg press in slight dorsiflexion
e.g. 4 x 5 x 3-5s holds
For most athletes this will be 100-150% BW external load on a smith machine or 200-250% BW on a leg press
Supramaximal eccentric training

approach that incorporates appropriate loading on the tendon and plyometric exercises is essential for optimal recovery.
• Due to the high recurrence rate, ongoing monitoring of training loads, fatigue, and biomechanics is necessary to prevent future injuries. Maintaining calf and Achilles loading in the player’s program, even after they are pain-free, is crucial for long-term tendon health and performance.
Develop explosive & reactive strength Optimal MTU function
Begin with low-level hopping/skipping as symptoms permit
DL pogo hops
e.g. 4 x 15-20 reps
Progress to SL multi-planar hops and ultimately high-intensity plyometric exercises such as drop

Abbreviations
MTU: musculotendinous unit
TUT: time-under-tension
SL: single-leg
DL: double-leg
e/s: each side
SSC: stretch-shortening cycle
EMG: electromyography
TS: Triceps surae
1. Gajhede-Knudsen M, Ekstrand J, Magnusson H, Maffulli N. Recurrence of Achilles tendon injuries in elite male football players is more common after early return to play: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013 Aug 1;47(12):763–8.
2. Waldén M, Gajhede Knudsen M, Ekstrand J, Hägglund M, D’Hooghe P, Alfredson H, et al. Achilles Tendon Pain in Male Professional Football Players - A Prospective Five-Season Study of 88 Injuries from the UEFA Elite Club Injury Study. Open Access J Sports Med. 2024 Nov 9;15:171–9.
3. Alfredson H, Waldén M, Roberts D, Spang C. Tendinopathic Plantaris but Normal Achilles Tendon Found in About One-Fifth of Patients Not Responding to Conservative Achilles Tendon Management - Results from a Prospective WALANT Surgical Case Series on 105 Tendons. Open Access J Sports Med. 2024;15:41–5.
4. Cramer A, Højfeldt G, Schjerling P, Agergaard J, van Hall G, Olsen J, et al. Achilles Tendon Tissue Turnover Before and Immediately After an Acute Rupture. Am J Sports Med. 2023 Jul 1;51(9):2396–403.
5. Villa FD, Buckthorpe M, Tosarelli F, Zago M, Zaffagnini S, Grassi A. Video analysis of Achilles tendon rupture in male professional football (soccer) players: injury mechanisms, patterns and biomechanics. BMJ Open Sport & Exercise Medicine. 2022 Sep 1;8(3):e001419.
6. Millar NL, Silbernagel KG, Thorborg K, Kirwan PD, Galatz LM, Abrams GD, et al. Tendinopathy. Nat Rev Dis Primers. 2021 Dec;7(1):1.
7. Crowe LAN, Akbar M, de Vos RJ, Kirwan PD, Kjaer M, Pedret C, et al. Pathways driving tendinopathy and enthesitis: siblings or distant cousins in musculoskeletal medicine? The Lancet Rheumatology. 2023 May 1;5(5):e293–304.
8. Lai C, Li R, Tang W, Liu J, Duan XDXF, Bao D, et al. Metabolic Syndrome and Tendon Disease: A Comprehensive Review. Diabetes Metab Syndr Obes. 2024;17:1597–609.
9. Edgar N, Clifford C, O’Neill S, Pedret C, Kirwan P, Millar NL. Biopsychosocial approach to tendinopathy. BMJ Open Sport & Exercise Medicine. 2022 Aug 1;8(3):e001326.
Figure 6: A rehab framework for Achilles tendinopathy
10. Ballal MS, Walker CR, Molloy AP. The anatomical footprint of the Achilles tendon: a cadaveric study. The Bone & Joint Journal. 2014 Oct;96-B(10):1344–8.
11. Edama M, Kubo M, Onishi H, Takabayashi T, Inai T, Yokoyama E, et al. The twisted structure of the human Achilles tendon. Scandinavian Journal of Medicine and Science in Sports. 2015;25(5):e497–503.
12. Albracht K, Arampatzis A, Baltzopoulos V. Assessment of muscle volume and physiological cross-sectional area of the human triceps surae muscle in vivo. Journal of Biomechanics. 2008 Jul 19;41(10):2211–8.
13. Fukunaga T, Roy RR, Shellock FG, Hodgson JA, Edgerton VR. Specific tension of human plantar flexors and dorsiflexors. Journal of Applied Physiology. 1996 Jan;80(1):158–65.
14. Stenroth L, Thelen D, Franz J. Biplanar ultrasound investigation of in vivo Achilles tendon displacement non-uniformity. Transl Sports Med. 2019 Mar;2(2):73–81.
15. Wang R, Gutierrez-Farewik EM. The effect of subtalar inversion/eversion on the dynamic function of the tibialis anterior, soleus, and gastrocnemius during the stance phase of gait. Gait & Posture. 2011 May;34(1):29–35.
16. Edama M, Takabayashi T, Inai T, Kikumoto T, Ito W, Nakamura E, et al. Differences in the strain applied to Achilles tendon fibers when the subtalar joint is overpronated: a simulation study. Surg Radiol Anat. 2019 May 1;41(5):595–9.
17. Merry K, Napier C, Waugh CM, Scott A. Foundational Principles and Adaptation of the Healthy and Pathological Achilles Tendon in Response to Resistance Exercise: A Narrative Review and Clinical Implications. Journal of Clinical Medicine. 2022 Jan;11(16):4722.
18. Prosenz J, Rath C, Hadrovic-Avdic M, Hirtler L. The Twist of the Achilles Tendon – Associations of Torsions in the Lower Extremity. Clinical Anatomy. 2018;31(7):1085–91.
19. Slane LC, Thelen DG. Non-uniform displacements within the Achilles tendon observed during passive and eccentric loading | Elsevier Enhanced Reader [Internet]. 2014 [cited 2023 Jan 4]. Available from: https://reader.elsevier.com/reader/sd/pii/S0021929014004242?token=2CE30FDFB B4A330A7CB680C7146544E5D9ECE69672BDFEDE63576D8A0830AF398647C2D3A973EC2BFF91AA62A9D5AF9B&originRegion=eu-west-1&originCreation=20230104171336
20. Crouzier M, Tucker K, Lacourpaille L, Doguet V, Fayet G, Dauty M, et al. . . . Published ahead of Print Force-sharing within the Triceps Surae : An Achilles Heel in Achilles Tendinopathy. 2019.
21. Fernandes GL, Orssatto LBR, Sakugawa RL, Trajano GS. Reduced motor unit discharge rates in gastrocnemius lateralis, but not in gastrocnemius medialis or soleus, in runners with Achilles tendinopathy [Internet]. Sports Medicine; 2022 May [cited 2022 Sep 22]. Available from: http://medrxiv. org/lookup/doi/10.1101/2022.05.05.22274750
22. Bohm S, Mersmann F, Santuz A, Arampatzis A. The force–length–velocity potential of the human soleus muscle is related to the energetic cost of running. Proceedings of the Royal Society B: Biological Sciences. 2019 Dec 18;286(1917):20192560.
23. Farris DJ, Lichtwark GA, Brown NAT, Cresswell AG. The role of human ankle plantar flexor muscle-tendon interaction and architecture in maximal vertical jumping examined in vivo. Journal of Experimental Biology. 2016;219(4):528–34.
24. Lai A, Brown N, Lai A, Schache AG, Brown NAT, Pandy MG, et al. Human ankle plantar flexor muscle – tendon mechanics and energetics during maximum acceleration sprinting Human ankle plantar flexor muscle – tendon mechanics and energetics during maximum acceleration sprinting Author for correspondence : 2016;(August).
25. Crouzier M, Baudry S, Vanwanseele B. Achilles Subtendons Stiffness Differ in People with and without Achilles Tendinopathy. Medicine and science in sports and exercise. 2025 Apr 3;
26. Hullfish TJ, O’Connor KM, Baxter JR. Medial gastrocnemius muscle remodeling correlates with reduced plantarflexor kinetics 14 weeks following Achilles tendon rupture. Journal of Applied Physiology. 2019 Oct 1;127(4):1005–11.
27. Hébert-Losier K, Ngawhika TM, Gill N, Balsalobre-Fernandez C. Validity, reliability, and normative data on calf muscle function in rugby union players from the Calf Raise application. Sports Biomechanics. 2022 Sep 19;1–22.
28. Komi PV, Fukashiro S, Järvinen M. Biomechanical loading of Achilles tendon during normal locomotion. Clinics in sports medicine. 1992 Jul;11(3):521–31.
29. Gheidi N, Kernozek TW, Willson JD, Revak A, Diers K. Achilles tendon loading during weight bearing exercises. Physical Therapy in Sport. 2018;32:260–8.
30. Baxter JR, Corrigan P, Hullfish TJ, O’Rourke P, Silbernagel KG. Exercise Progression to Incrementally Load the Achilles Tendon. Medicine and Science in Sports and Exercise. 2021;53(1):124–30.
31. Lazarczuk SL, Maniar N, Opar DA, Duhig SJ, Shield A, Barrett RS, et al. Mechanical, Material and Morphological Adaptations of Healthy Lower Limb Tendons to Mechanical Loading: A Systematic Review and Meta-Analysis. Sports Medicine 2022. 2022 Jun 3;1–25.
32. Arampatzis A, Mersmann F, Bohm S. Individualized Muscle-Tendon Assessment and Training. Frontiers in Physiology. 2020 Jun 26;11:723.
33. McMahon G. No Strain, No Gain? The Role of Strain and Load Magnitude in Human Tendon Responses and Adaptation to Loading. Journal of Strength and Conditioning Research [Internet]. 2022 Jul 7 [cited 2022 Jul 11];Publish Ahead of Print. Available from: https://journals.lww.com/10.1519/ JSC.0000000000004288
34. Devaprakash D, Graham DF, Barrett RS, Lloyd DG, Obst SJ, Kennedy B, et al. Free Achilles tendon strain during selected rehabilitation, locomotor, jumping, and landing tasks. Journal of Applied Physiology [Internet]. 2022 Mar 29 [cited 2022 Jul 15]; Available from: https://journals.physiology.org/ doi/10.1152/japplphysiol.00662.2021
35. Griffin C, Daniels K, Hill C, Franklyn-Miller A, Morin JB. A criteria-based rehabilitation program for chronic mid-portion Achilles tendinopathy: study protocol for a randomised controlled trial. BMC Musculoskeletal Disorders. 2021 Dec 14;22(1):695.
36. Arndt A, Bengtsson AS, Peolsson M, Thorstensson A, Movin T. Non-uniform displacement within the Achilles tendon during passive ankle joint motion. Knee Surg Sports Traumatol Arthrosc. 2012 Sep 1;20(9):1868–74.
37. Crouzier M, Dandois F, Sarcher A, Bogaerts S, Scheys L, Vanwanseele B. External rotation of the foot position during plantarflexion increases nonuniform motions of the Achilles tendon. Journal of Biomechanics. 2022 Aug;141:111232.
38. Muraoka T, Muramatsu T, Fukunaga T, Kanehisa H. Influence of tendon slack on electromechanical delay in the human medial gastrocnemius in vivo. Journal of Applied Physiology. 2004 Feb;96(2):540–4.
CHRONIC PAIN IN FOOTBALL —THE UNSEEN STRUGGLE
BSC (HONS) PGDN
Chronic pain is an often hidden, misunderstood reality in football.
Beneath the surface of performance and professionalism, many players are stuck— still in pain despite rest, rehab, or even surgery.
Terms like “chronic” or “persistent” pain can feel discouraging, especially when the focus remains solely on damaged tissue. But pain is more than a body part—it’s shaped by stress, history, expectations, and identity.
In football, where pressure is high and vulnerability is rare, pain becomes something players push through—until they can’t.
We know pain can change. It’s not a fixed condition but an experience shaped by many factors. The key isn’t just treating the body—it’s helping and guiding the person.
Chronic pain can be eased and transformed when we listen deeply, work with the whole individual, and support their journey with care, science, and compassion.
There is pain — but there is also real hope.
How does chronic pain show up in football?
Chronic pain in football often hides in plain sight. It rarely announces itself clearly.
Instead, it emerges through subtle patterns and ongoing struggles that can be misunderstood or overlooked. Here are common ways it shows up:
• A player doesn’t recover from an injury within expected timelines
• Ongoing aches and pains that affect mood, confidence, and performance
• Regular requests for pain relief or treatment, even when tests show “nothing wrong”
• Frequent visits to the medical room, often with shifting symptoms
• Difficulty returning to full training or competitive play
• A frustrating stop-start pattern: returning to action, then flaring up again
• Recurrent injuries, often in the same area, despite good rehab
These signs reflect the bigger picture of the player and their life.
What is pain?
Pain is a deeply personal and private experience. You can’t see it, measure it, or
fully understand it from the outside.
It’s real—but it’s not just in the body. It’s in the person.
Think of pain like thirst or hunger: a need state. But unlike thirst, we often misunderstand pain as something that simply comes from damaged tissues. That’s not the full picture.
Pain doesn’t come from the tissues—they have no ability to generate a conscious experience. It is about the person. Tissues don’t feel; people do.
The current science points toward pain being a protective experience generated by your body systems—nervous, immune, hormonal, cognitive—all working together to keep you safe (Kiverstein et al., 2022).
According to predictive processing models, pain is your body’s best guess about what’s happening, based on past experiences, expectations, and sensory data. If things don’t match up, you feel something—pain, fatigue, tension, or other symptoms.
You can watch neuroscientist Anil Seth talk about it here

FEATURE / RICHMOND STACE, MSC (PAIN) BSC (PHYSIO)
That’s why chronic pain can exist even when scans are clear or injuries have healed. It’s not about faking or weakness— it’s about how the body systems have reset themselves to protect. There are needs to be met and goals to work towards.
Pain is asking for a shift, not a fix. A shift in thinking, understanding and living.
Understanding this changes everything. It opens the door to new ways of helping players transform their pain—not by fixing tissues, but by supporting the whole person: their biology, beliefs, behaviours, and goals.
Reflection moment: think of a player who has been struggling with pain. What other symptoms and behaviours did they demonstrate?
Pain and injury are poorly related
The simple fact is this: pain and injury are not the same—and they’re not even closely linked much of the time. Professor Pat Wall, one of the founding figures of modern pain science, was already saying this in the 1970s (Wall, 1979). He lay the groundwork for a new understanding of pain—not just as a body problem, but as a whole-person experience, a need state.
Sadly, this wisdom didn’t take root as it should have. The old biomedical model— focused on fixing tissues—continued to dominate. But it misses the mark. It doesn’t explain why pain persists long after healing, or why some players struggle deeply when nothing obvious appears “wrong.”
We now know better. And that opens up new, more hopeful paths for recovery—by listening to the whole person, not just looking at the injured part.
Pain ‘types’
To help guide assessment and management, pain is commonly described using three categories: nociceptive, neuropathic, and nociplastic
It’s important to remember that these are conceptual tools—labels to support understanding and communication. They are not the lived experience itself. As practitioners, we aim to support and transform that experience.
While categories can help, they are not the whole truth. Our knowledge will evolve, and so must we—this is the spirit of the beginner’s mind.
To truly understand a player’s pain, we must go beyond tissues and tests. We must understand them—their story, their context, and the conditions that shape their experience.
Here are the current IASP definitions:
Nociceptive pain: Arises from actual or potential tissue damage due to activation of nociceptors.
Neuropathic pain: Caused by damage or disease affecting the somatosensory nervous system.
Nociplastic pain: Arises from altered nociceptive function without clear evidence of tissue damage or nerve injury.
These types often overlap. This is why listening deeply to the player’s story is as essential as any examination or scan.
Using the predictive processing model, we can keep sight of the whole picture— subjective and objective—both essential, and both true.
To help someone with their pain, you need to know the person.
Pain but no obvious pathology or injury
You now know that pain and injury are not the same—and often, they’re not even well related. Where pain is felt is not where it is generated.
To truly understand a player’s pain, we must go beyond tissues and tests. We must understand them—their story, their context, and the conditions that shape their experience.
In chronic pain, it’s common to find no clear pathology. Imaging may show ageexpected changes or mild inflammation— nothing to explain the level of suffering.
Yet the pain is real.
Why? Because pain emerges from many influences:
• Beliefs
• Expectations
• Attention
• Context
• Environment
These shape perception.
Footballers expect some aches and soreness— it comes with the territory. But when pain lingers, disrupts performance, or leads to suffering, it’s time to pay closer attention.
Pain is a whole-person experience—a best guess the body systems create based on available information: past experiences, present context, and predicted needs.
The opportunity? To change the sensory information. To help the player gather new sensory evidence—through new movements, new thoughts, new patterns—that reshape their experience.
Habit formation is at the heart of it.
That’s the essence of getting better, going beyond the training ground.
How players get stuck with pain
At first, there’s usually hope of recovery.
A player feels pain, seeks advice, follows treatment, and expects to get better. That expectation is reasonable. Often, it’s what happens.
But sometimes, things don’t improve as expected.

When recovery stalls, there’s a gap between what the player believed would happen and what actually does. There is a mismatch between expectations and reality.
Over time, as this mismatch continues, the body systems recalibrate.
Now, pain becomes the new expectation. The system predicts pain in certain situations, and so it produces pain in those situations. Gradually, the range of those situations can expand.
This is how players get stuck.
It’s essential to explore the biology, of course—but never in isolation. We must always listen to the lived experience.
And remember, nothing is fixed.
Each moment is new. This is the principle of impermanence. The body and brain are always changing.
The question is—in which direction is the change going?
This is where we come in. Through caring collaboration, we help guide the player toward their picture of success—step by step, moment by moment.
How can we help?
The first step is simple—but vital: connect and listen deeply.
Before anything else, the player needs to feel heard and understood. Their story matters. Their experience matters. Validation is not optional—it’s foundational.
In fact, in therapeutic work, it’s often how we are with someone that makes the difference, not just what we do.
Helping a player with chronic pain is not just an extension of treating acute pain. The two are very different.
Yes, all experiences arise from the body’s systems. But persistent pain reflects deeper patterns, often shaped by past experiences, beliefs, context, and more. Recovery requires more than rest or rehab— it asks for something active, personal, and transformative. It’s like learning a musical instrument.
The player must learn the skills to live themselves better. With the right guidance, support, and environment, this is entirely possible.
And that’s where we come in.
A personalised programme
Personalised means more than just a set of instructions—it’s about meeting the player where they are and working together toward their unique goals.
This approach is flexible and responsive, evolving as the player progresses.
The first step is to help the player truly understand their pain.
This means explaining:
1. Why the pain persists.
2. How pain is generated in different circumstances.
3. The key influences that shape their pain experience.
These insights provide clarity and help make sense of the player’s journey. When the experience is understood, the way forward becomes clearer.
With this understanding, a range of skills and practices opens up—each tailored to the player’s needs.
Chronic pain is not about a one-size-fits-all solution. Instead, it’s about fostering a caring collaboration, with shared goals, a clear strategy, and practical skills that the player can integrate into their daily life.
This is how transformation happens.
Strategy, skills and rehabilitation ~ a guide
Bringing a personalised programme to life means combining a clear strategy, practical skills, and a caring collaboration.
The practitioner’s role is that of a guide—a coach. Over 20 years ago, I coined the term Pain Coach for this very reason.
Transforming chronic pain is a learning process. Treatments can help, but lasting change comes from new beliefs, fresh thinking, and different actions.
We begin by clarifying the player’s picture of success—their personal goals—so we understand their direction.
Next, we design a strategy: a practical, realistic route from where they are to where they want to be. This includes personalised rehabilitation, the skills of being well, self-care, and tools to navigate challenging moments.
The strategy then becomes active as the player learns and practices their skills in real life. For example:
• How to get the best from an exercise by preparing mind and body (priming with breathwork, imagery, and intention),
• Staying focused during practice (mindfulness), and
• Finishing with recovery and reflection (recharge).
Underpinning every step is meaningful coaching—knowledge, insights, and knowhow—so the player understands why and how the practices help, and how to apply them in their world.
Key insights to repeat and reinforce:
• Focus on the process, not just the prize
• Move toward what you want—not away from what you fear
• It’s not just what happens, but how you relate to it that matters
Each of these insights returns attention to what the player can control.
While the details of a rehabilitation programme are always tailored, it’s the principles that make it truly personal.
Once players understand and embody these principles, they become their own coach— guiding themselves toward their goals, with you walking alongside.
Concluding words
“My teaching is like a finger pointing to the moon. Do not mistake the finger for the moon”
~ Buddha
Chronic pain exists in football. It exists in players—real people—who need understanding, guidance, and support to move through it and beyond it.
Our way of helping is grounded in science, enriched by care, and powered by compassion.
We build a caring collaboration. Together, we guide the player to focus on what they can do—to concentrate on the daily practice of living themselves better. Return to training. Return to play. Or some other picture of success they have chosen. But always onwards.
Pain is real. So is change. So is hope. We guide. Onwards. —RS
Three takeaways
1. Seek to understand pain and its purpose by building your knowledge, but not getting attached to any particular model. Knowledge is not truth. It will change.
2. Examine your way of being— what is your approach and style? The caring collaboration and environment you create matters.
3. Practice your listening skills and notice how this merges with acceptance of the person you are working with, and in turn how this is the basis of positive change.
References and resources
Kiverstein et al. (2022). An Embodied Predictive Processing Theory of Pain Experience. Review of Philosophy and Psychology 13:973–998.
Wall PD (1979). On the relation of injury to pain. The John J. Bonica lecture. Pain. Jun;6(3):253-264.
Learning area on my website for videos, podcast episodes and reading: https://richmondstace.com/learning/


THE CONNECTION EDGE
- HOW PSYCHOLOGICAL SAFETY & BELONGING CAN UNLOCK PERFORMANCE, ENGAGEMENT & PLAYER AVAILABILITY IN FOOTBALL
FEATURE / RONAN CONWAY, B.COMM, MIMAS, HDIP PSYCH, CERTIFIED
Introduction
‘Connection’. A term often used by players and managers reflecting on a successful season. But, what exactly is meant by this? As a felt experience, it’s tricky to put your finger on what it actually is. Yet when it’s alive in an environment, the impacts are real and profound. Connection transforms who we are, how we relate, and how we perform.
Since 2019, I’ve facilitated connection building programs in elite sporting setups - working across levels from player groups, to medical, backroom and coaching staff. I’m continually amazed by the genuine alchemy that takes place in these spaces. Yet, it surprises me how relatively unexplored this field is in the world of high-performance. In this article, I’ll explore the following:
1. Connection building spaces in elite sport.
2. Psychological safety and belonging at the core of connection.
3. How both can impact performance, engagement and player availability.
4. Measure how connected your team environment is.
Connection Building Spaces
‘We shape our buildings, therefore they shape us’
Winston Churchill.
Tribes and communities have gathered to connect long before the days of ‘high performance’. The Polynesian Navigators had a sacred ritual of gathering before every epic voyage they embarked on. Around a fire the tribe would remind themselves of who they were, where they were going, and what inspired their journey.1 Na Fianna, a band of Irish ‘warrior-hunter-poets’ were known to gather around a fire underneath the stars. Here they would tell stories, celebrate their heroism and the bonds they shared.2
Countless cultures and communities across time mirror such rituals. It’s like a magnetic pull toward gathering in a circle is hardwired into us as humans. Not merely for the sake of it, but with the intention to nourish, unify and fortify. Similar practices live on in elite sports, packaged in the form of ‘connection building’ programs.
In the lead up to the 2023 Ryder Cup, Rory McIlroy described an “amazing experience” around a fire pit where they delved into their
backstories, family and why they played golf. Delving deeper into who they were and their motivations unified them into a team unit. “I got to know something different about them,” McIlroy said, “and I think that really galvanised us.”3
In the lead up to Chicago Bulls Last Dance, Phil Jackson (below, centre) gathered his players. He invited Michael Jordan, Scottie Pippen and co to write about what the team meant to them, before reading aloud. ‘Everyone had an emotional word to say’, Steve Kerr recounted. To finish, Jackson turned out the lights and set fire to their answers in a tin cup. “One of the most powerful things I’ve ever seen”, Kerr said.4
Usually, at certain points in a workshop, a deep calm envelopes the room. It feels like the group is breathing in sync. The depth of attunement feels ancient. What is it about a group ‘connecting’ with purpose that creates such palpable shifts? For me, it boils down to people’s core human needs for safety, belonging and purpose being met on a heightened level. With those moments, beliefs about themselves, their place in the group, and the meaning behind their journey transform profoundly.

Core Human Needs
‘Invisible threads are the strongest ties’ Friedrich Nietzsche
Believe it or not, footballers are human beings too. Like anyone, they scan their workplace to determine ‘am I safe?’, and ‘do I belong?’
When we feel psychologically safe, we believe we can contribute as ourselves without fear of judgement, repercussions or punishment. The fight, flight or freeze response goes offline, and ‘social engagement mode’5 comes online. Here we are open to engaging or taking ‘interpersonal risks’ with the group humans.6 Dr. Gabor Mate says, ‘safety isn’t the absence of threat, but the presence of connection’.
This ‘presence of connection’ lies at the heart of belonging too. Belonging is characterised by supportive ties with teammates. The environment has a community feel, if not a family feel to it. It feels like we matter, and what we add to the mix is valued - no matter our age, position, culture or personality.
In the next section, I will break down how a combination of psychological safety and belonging can significantly enhance performance both on and off the field. Furthermore, supporting your people to keep well and available for selection.


Image 1: A montage of pictures from various connection sessions.
The Connected Environment
“The strength of the Pack is the Wolf, the strength of the Wolf is the Pack.”
Rudyard Kipling
On-Field Performance
• Strong, healthy relationships between team members are central to social cohesion. One study involving 36 football teams found that high levels of cohesion were linked to positive results in teams’ weekly games.7
• Communication is key in game time. There’s zero space for doubt, hesitation or insecurity. When communication flows freely on the field, teams experience fewer errors, along with greater coordination, teamwork and team resilience 8
• ‘Red Head Blue Head’ is a concept born out of a World Cup winning All Blacks camp. A Red Head refers to a player being overwhelmed, tight, inhibited or anxious. In contrast, Blue Head is when a player is in a present , calm , and clear state. 9 A regulated nervous system is the foundation for accessing this state, and indeed accessing the elusive flow state
Player Availability
• Poor communication between head coach, manager and medical staff was found to increase both the likelihood and severity of injury. Highlighting the importance of forging open, communicative dynamics amongst backroom, doctors and physios.10
• A change in the makeup of a backroom team typically disrupts established training and recovery protocols. A UEFA study found that such changes are linked with an increased rate of hamstring injury. Specifically, when a team doctor or fitness coach changed, it resulted in an 81% and 63% increase in hamstring injury, respectively.11 Underscoring the need for stable, consistent dynamics.
• Safety and belonging are like natural coolants for the nervous system. When we are regulated, we have greater cognitive functioning, better decision-making and motor control. In this state, athletes are found to have reduced risk of injury 12
• Teams with low communication levels reported 5% less training attendance, and also 4% lower player availability on match-day.16 A cohesive team tends to have higher attendance levels, less lateness or absenteeism from training and games.17
• When psychological safety is high, athletes are less likely to experience distress18 or athlete burnout, 19 and
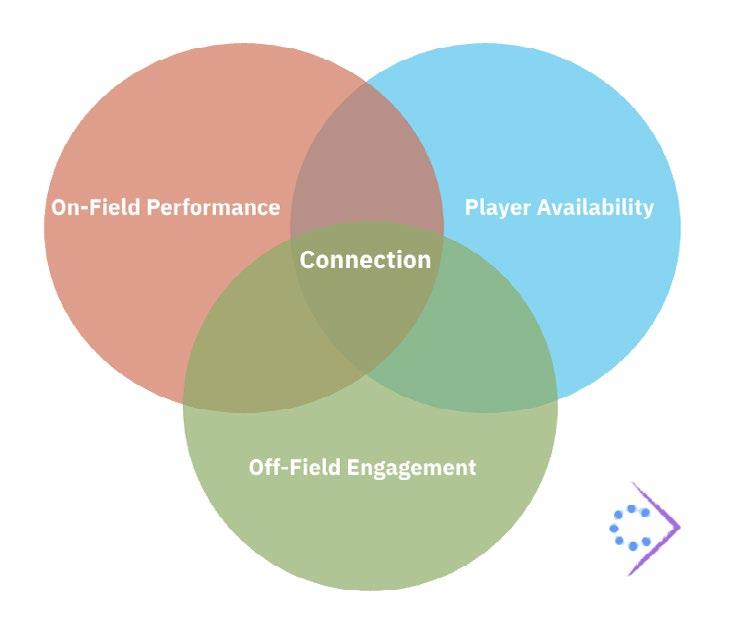
more capable of dealing with setbacks and uncertainty.20 A footballer who feels supported by teammates and coaches, they’ll be better equipped to handle pressure21 and sustain performance 22 Trusting and cooperative ties between athlete and coach have been shown to enhance players psychological well-being and self-confidence 23

Off-Field Engagement
• Post-game reviews, department and medical meetings have the potential to be goldmines. Valuable insights about performance, opponents, injuries and nutrition are there waiting to be tapped into. A psychological safe dynamic ‘takes the handbrake off’, letting the wisdom and knowledge flow more effortlessly. In a landmark study of their workplace teams, Google identified psychological safety as being the top predictor of team effectiveness.24
• ‘Feedback is the breakfast of champions’, they say. But, the quality of the relationship will determine how well the feedback is received. When there is trust or respect lacking, the receiver will likely hear the feedback as a threat, and will then become guarded or defensive. When the relationship is grounded in safety, the feedback is heard as supportive and constructive.25
• Keeping a squad of differing ages, cultures and personalities satisfied can be a challenge. When players come to training or match-day feeling valued, accepted and they can be themselves, it’s a huge step toward keeping people engaged and bought in. A Harvard Business Review study found that belonging in the workplace is linked to a 56% increase in performance, 50% less risk of turnover, and 75% reduction in sick days 26
• Belonging and safety are natural mood enhancers. Feel good chemicals like serotonin, oxytocin, and dopamine create healthy shifts in our physiology, supporting our mental and emotional wellbeing. Positive energy and emotions are ‘contagious’,27 and will ripple out to positively impact levels of morale and camaraderie
3 Take-Aways
Connection as a need: Connection is more than a nice feeling, it’s a human need. Players, coaches and staff are searching for it on the daily, whether they know it or not. When met, wellbeing and performance spiral upwards together.
Sacred team spaces: Connection sessions may appear like a modern sports psychology technique, but they are in fact age-old human rituals. When these spaces are held with skill, care and integrity, they have the potential to transform.
How connected is your team?

The butterfly effect: A football club is an interrelated ecosystem. When safety and belonging are alive in the dynamic, the effects filter into the dressing room, postgame reviews, medical consultations, to the white heat of battle.
Now’s a chance for you to check the temperature of your environment - be it the players group, coaches, backroom, to medical departments. The following survey will help you to pinpoint how connected your team really is. *This tool has been designed and refined by myself for various clients in elite sport and multinationals alike.

If you scored 50/50, that’s awesome. For those who scored anywhere below, consider this: Imagine what could be unlocked if your team’s connection was dialled up another level, or five. What ripple effects might you see on the field, in team meetings, and with the availability of your athletes?
Conclusion
Connection is a potent force in elite football. When people can be themselves and feel truly valued in the environment, it’s like taking the handbrake off. Energy flows into what matters - game-plans, team meetings, medical consultations, training drills and ultimately, performance. The group serves as a wellspring of wellbeing and resilience, a buffer against stress and dis-regulation.
Connection is like a fire. It takes care, attention and tending. Connection sessions are a potent and intentional way to keep the fire stoked and burning bright throughout the season. The beautiful thing is, safety and belonging are inherent in who we are as people. They’re always there - waiting for the right conditions to come to life.
Author Affiliations:
• Performance Consultant who has worked with elite sports teams, like the Ireland Rugby Team, Leinster Rugby Team, Shelbourne Football Club, Dublin’s historic 5-in-a-row winning gaelic football team.
• Facilitates The Circle, a self development program for the prison population.
• Runs team development programs for multinationals and corporate leadership teams.

References
1. Eastwood, O. (2021). Belonging: The ancient code of togetherness. Quercus Books – Belonging by Owen Eastwood
2. The Brehon Academy. https://brehonacademy.org/by-the-chase-the-hunt-and-the-song-the-linguistic-origins-of-na-fianna-irelands-elite-bandof-warrior-hunter-poets/?utm_source=chatgpt.com
3. Morfit, C. (2023, October 1). Rory McIlroy proves himself to be the heartbeat of this Ryder Cup. PGA Tour. Article here
4. Thanawalla, A. (2020, May 18). NBC Sports Bay Area. Steve Kerr recalls ‘powerful’ end of Michael Jordan, Bulls’ ‘Last Dance’. See article here.
5. Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. W. W. Norton & Company
6. Google. (2015). Re:Work guide: Understanding team effectiveness. Article here
7. Tziner, A., Nicola, N., & Rizac, A. (2003). Relation between social cohesion and team performance in soccer teams. Perceptual and Motor Skills, 96(1), 145–148. https://doi.org/10.2466/pms.2003.96.1.145
8. LeCouteur, A., & Feo, R. (2011). Real-time communication during play: Analysis of team-mates’ talk and interaction. Psychology of Sport and Exercise, 12(2), 124–134.
9. Evans, C. (2017). Perform under pressure: The science of doing your best when it matters most. Penguin Life.
10. Ekstrand, J., Lundqvist, D., Davison, M., D’Hooghe, M., & Pensgaard, A. M. (2019). Communication quality between the medical team and the head coach/manager is associated with injury burden and player availability in elite football clubs. British Journal of Sports Medicine, 53(5), 304–308.
11. Ekstrand, J., Van Zoest, W., & Gauffin, H. (2023). Changes in head staff members in male elite-level football teams are associated with increased hamstring injury burden for that season: the UEFA Elite Club
12. Grooms, D. R., Appelbaum, G., & Onate, J. A. (2021). Lower Kinetic Chain, Meet the Thinking Brain: A Scoping Review of Cognitive Function and Lower Extremity Injury Risk. International Journal of Sports Physical Therapy, 16(3), 648–663.
13. Ekstrand, J., Lundqvist, D., Lagerbäck, L., & Hägglund, M. (2019). Communication quality between the medical team and the head coach/manager is associated with injury burden and player availability in elite football clubs. British Journal of Sports Medicine, 53(5), 304–308.
14. Burke, S. M., Davies, K. M., and Carron, A. V. 2014. “Group cohesion in sport and exercise settings,” in Group Dynamics in Exercise and Sport Psychology, 2nd Edn, eds M.R. Beauchamp and M. A. Eys (New York, NY: Routledge). p. 147–63.
15. Nicholls, A. R., Madigan, D. J., & Levy, A. R. (2022). Psychological safety in elite sport settings: A psychometric study of the psychological safety scale for elite athletes. BMJ Open Sport & Exercise Medicine, 8(2), e001251.
16. Fransen, K., McEwan, D., & Sarkar, M. (2020). The impact of identity leadership on team functioning and well-being in team sport: Is psychological safety the missing link?
17. Kristiansen, E., Halvari, H., & Roberts, G. C. (2012). Organizational and media stress among professional football players: Testing an achievement goal theory model. Scandinavian Journal of Medicine & Science in Sports, 22(4), 569–579.
18. Kristiansen, E., Halvari, H., & Roberts, G. C. (2012). Organizational and media stress among professional football players: Testing an achievement goal theory model. Scandinavian Journal of Medicine & Science in Sports, 22(4), 569–579.
19. Morris, R., Tod, D., & Oliver, E. (2017). Performance and organizational stressors in the junior-to-senior transition in football. Qualitative Research in Sport, Exercise and Health, 9(4), 477–494.
20. Coussens, A. H., Stone, M. J., & Donachie, T. C. (2024). Coach–athlete relationships, self-confidence, and psychological wellbeing: The role of perceived and received coach support. European Journal of Sport Science, 25(1), e12226
21. Edmondson, A. C. (2018). The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth. John Wiley & Sons.
22. Patterson, K., Grenny, J., McMillan, R., & Switzler, A. (2011). Crucial conversations: Tools for talking when stakes are high (2nd ed.). McGraw-Hill.
23. Carr, E. W., Reece, A., Rosen Kellerman, G., & Robichaux, A. (2019, December 16). The value of belonging at work. Harvard Business Review.
24. Christakis, N. A., & Fowler, J. H. (2009). Connected: The surprising power of our social networks and how they shape our lives. Little, Brown and Company.


A PRACTICAL APPROACH TO THE SKELETAL MUSCLE MORPHOLOGY AND ITS IMPORTANCE IN SPORTS-RELATED SKELETAL MUSCLE INJURIES
Introduction
Cells and tissue morphology seem to be very far from our daily practice, but it is very important to notice that if we want to understand in the best possible return-toplay from a myoaponeurotic injury in our players, skeletal muscle morphology plays a crucial role.
Several classification systems for muscle injuries have been proposed in recent years.1,2,3 They take into consideration the location of the injury and the injured structures as a key point for the diagnosis and prognosis. The problem is that, despite significant amount of research invested in the topic, disagreement persists among healthcare practitioners regarding the proper application/use of such basic anatomical terms such as tendon, aponeurosis, and fascia. To achieve clarity on this issue, specifically ensuring uniformity in our terminology, it is essential to first comprehend the unique properties of each anatomical component.
Let’s try to think about a very simple example. We are facing an injury in a player that has been classified as a BAMIC 2B. By definition, this is a moderate muscle/myoaponeurotic tear. But the key question remains: do we really understand what exactly an aponeurosis is? Which type of connective tissue is it and what are its functional characteristics?
There is a need to include a histoarchitectural definition4 in muscle injuries, which describes both the damage to connective tissue structures and the connective tissue itself, not only the topographic classification. Consequently, any clinically meaningful injury nomenclature should highlight the injury’s histoarchitectural features along with its macroscopic anatomy.
In the skeletal muscle structure are, as said before, three major connective tissue structures: Tendon, aponeurosis and fascia. Whilst all three are fibrous
structures surrounding the skeletal muscle fibres, they differ in their morphological composition, macroscopic connections and how they interact with other elements.
Morphological definitions
Although all three structures are composed of dense connective tissue, histologically speaking, the orientation of the collagen fibres in each of the three structures remains distinct. This is, probably, the most important concept to understand from this article.
Fascia contains collagen fibres that are compact, but unlike those found in the epimysium, they are not orientated or organised in the same way. This is because the primary function of fascia is to cover the muscle.5 The collagen fibres that are found in tendons and aponeuroses, on the other hand, are aligned with the direction that traction is being applied.6
Structure-wise, tendons and aponeuroses are distinct from one because they are subjected to different directions of traction. In tendons, all collagen fibres are aligned in the same direction forming longitudinal fascicles, allowing longitudinal traction. Aponeuroses are arranged in overlapping planes; it is possible for them to exhibit both longitudinal and transverse traction. This is because all the fibres in aponeuroses are parallel to each other, whilst their orientation is oblique or perpendicular with respect to the adjacent plane.7
Tendon:
The tendon is histologically defined as dense connective tissue with oriented collagen fibres (Fig. 1). That is, all collagen fibres are oriented in the same direction of traction. The same orientation of collagen fibres in tendons allows large number of cross-links between identically oriented collagen fibres to form. It is the number of these cross-links between the collagen fibres that ultimately define the mechanical strength of the connective tissue.8,9,10 Due to the identical orientation of all collagen fibres in tendons, it is easy to understand why the Achilles tendon has the highest concentration of cross-links between its collagen fibres and is the strongest tendon in the human body.10 This anatomical arrangement is critical as it enables the tendon to withstand high tensile forces, transferring the contraction forces from the muscle to the bone to produce movement. Injuries to tendons are often a result of overuse, leading to conditions such as painful tendinopathy or traumatic, acute ruptures due to excessive tension. The tendons are relatively avascular and have a high tensile strength, with collagen fibres forming longitudinal fascicles that support longitudinal traction. The only elasticity they have is in the crimps (that can be straightened) the collagen fibres form.11
Aponeurosis:
Aponeuroses are like tendons in that they are also made of dense connective tissue, but they differ in their structure (Fig. 2). They have layers of collagen fibres arranged in a flattened sheet, with the fibres of successive layer-oriented perpendicular to those in the previous layer. This arrangement allows for the dispersal of force over a wider area and supports both longitudinal and transverse traction, thereby reducing the risk of injury.
Fascia:
A fascia is a fibrous connective tissue sheath that surrounds a skeletal muscle or muscle group (Fig. 3). It does not have the same regular, organised structure of collagen fibres as tendons or aponeuroses. Instead, its fibres are loosely organised, allowing for more flexibility and movement between internal body structures. From a histological perspective, it presents two well-defined layers: The outermost layer presents non-oriented collagen fibres with blood vessels and nerves, whilst in the inner layer the collagen fibres are more compacted and oriented.12

1: A) Tendon. Histological section at the level of a MTJ showing the parallel arrangement of collagen fibres in the tendon. Among them are the nuclei of the tenocytes (fibroblasts). B) Tendon histological section labelled with arrows. The blue arrows indicate the muscle fibres. The black arrows indicate the tendon. Hematoxylin-eosin dye, 40x.

Figure 2: A) Aponeurosis. Histological section clearly shows layered organization, with collagen fibres sections running in various directions within the aponeurosis. Between the collagen layers are the nuclei of fibroblasts. B) The same Histological section of aponeurosis labelled with arrows. The blue arrows indicate the muscle fibres. Hematoxylin-eosin dye, 40x. Black arrows indicate the distribution of the collagen fibers running to different directions.

Figure 3: A) Fascia. Histological tissue section without labeling. B) Fascia histological tissue section labelled with arrows. Fascia display up to three different connective tissue layers (thin black arrows). The first two (a and b) correspond to the fascia, while the deepest connective tissue structure(c) corresponds to the epimysium, which continues into the actual skeletal muscle forming perimysial septa between the skeletal muscle fibres (thick black arrows). The blue arrows indicate the skeletal muscle. In layer (a) a large vascular structure is observed (arrowhead). Hematoxyline-eosine dye, 20x.
Figure
Continuity of connective musculotendinous frameworks
Histologically, we currently understand that the epimysium is clearly continuous with the epitenon and the perimysium clearly continuous with the tendon, but the endomysium is not continuous with the epitenon.13 We consider this anatomical detail very important for understanding why injuries are more frequent at the musculotendinous junction (MTJ) than in the tendon itself. In this context, the lack of continuity between the endomysium and the endotenon and the elastic nature of the MTJ act as safety valves against the functional stress of the muscle: before a tendon rupture occurs, it is preferable to have a rupture at the MTJ, as it is easier to manage or heals better and faster than the tendon rupture. Furthermore, the ruptured skeletal muscle fibres always adhere to the connective tissue with it is a scar or fascia by forming new MTJs at the end of adhering skeletal muscle fibres.
It is probable that this pattern may vary depending on the muscle and its relationship with the tendon or aponeurosis. The characteristics of structural continuity between skeletal muscle and tendon are an important component of skeletal muscle physiology.
We want to emphasise that it is important to remember that both the amount of intramuscular connective tissue and its morphological distribution is highly variable between different skeletal muscles with different functions,14 just as variability is important in form, size and location (intra- or extra-muscular) of tendons.
This variability may also complicate or hinder the diagnosis of lesions which occur in these regions in sports. A myoconnective junction is always involved in a muscular lesion,13 whether this be at myotendinous or myofascial level. The extent of injury extending to the connective tissue structure in any given
location within a skeletal muscle-tendonunit is the crucial factor that needs to be defined in all injuries.15 Due to this, the characterisation and systematisation of the different histoarchitectural patterns in the muscle-tendon relationship is essential for classifying or being familiar with the clinical characteristics, correct diagnosis, prognosis and physiotherapy for the different lesions.16
How can we apply this to our daily practice?
In the context of sports injuries, these differences influence the diagnosis, prognosis and treatment of each injury. It was recently demonstrated in hamstring injuries that injuries affecting the “free tendon”, i.e. the proximal tendon, can take almost two and a half times longer to heal than the injuries occurring in intramuscular aponeuroses.15 Furthermore, in relation to hamstrings, the involvement of the MTJ in the hamstring injury, in turn, increased the risk of re-injury significantly.17 These recent scientific findings highlight the clinical significance of identifying the exact connective tissue structure that had been injured within the skeletal muscle.
In addition, the most important consideration when planning a return-toplay process in an injured athlete are:
- injury mechanism.
- athlete’s characteristics.
- type of sport and position he/she plays.
- the histological/anatomical structures affected by the injury.
- the degree (classification) of this specific injury.
- clinical exploration.
Consequently, a precise understanding of these structures helps tailor rehabilitation strategies and helps athletes return to their sport safely.18,19
So, when it comes to accurately describing and diagnosing skeletal muscle and tendon injuries in sports, it is crucial to use the same nomenclature regarding the histological structures20,21 as well
as with the classification systems that we normally use. If not, the confusion amongst all the specialists that participate in the RTP process can lead to miscommunication and an incorrect RTP plans.
It is well known that each of the structures have different functions, collagen density and strength, and thus, a different resistance and tendency for certain types of injuries (Table 1).
Tendons are designed for high tensile strength in the load direction, so they have a huge density in terms of collagen organisation and thickness. This makes it almost impossible to have an acute rupture in a healthy tendon but, when there is some degeneration in the tendon structure, they’re prone to either acute, traumatic tears or chronic, painful degeneration (tendinopathy) from overloading.
The collagen distribution of the aponeurosis is probably one of the most important points that we need to understand, because it is designed to disperse force in all directions and might be more resilient because of this. It can be said that aponeuroses are structures that are mainly an intramuscular continuum of the tendon, this increases the length of the MTJ and increases risk of injury due to excessive multi-directional stress from the skeletal muscle attachments
One of the first things that we look at after an acute injury is the injury mechanism. It is known that a highenergy injury mechanism normally leads to severe injuries.22 Even here, the histological structures help in determining the mechanism of injury. Tendinous, aponeurotic or myotendinous injury occurs from a sudden explosive movement, whilst fascial tissue doesn’t require a high-energy mechanism for rupture to occur. This is due to fasciae and myofascial junctions being inherently weaker than aponeuroses and tendons.3,4
Table 1: Generalized comparison of different properties of connective tissue structures in skeletal muscle-tendon-unit and the characteristic RTP time after the injury for every type of tissue.

Figure 4. Imaging composition of a Rectus femoris (RF) conjoint tendon rupture: (A) Histological sample of a tendinous structure. (B) Sagittal view of a cadaveric sample (E) of the human RF. Different connective tissue structures are identified and marked: PT (proximal tendons); AA (anterior aponeurosis); CA (central aponeurosis); PF (posterior fascia); PA (posterior aponeurosis); DT (distal tendon). (C) MRI Axial T2 sequence showing the normal appearance of the proximal tendons of the RF when they conform the conjoint tendon (red bracket). (D) Tranversal ultrasound scan showing the normal appearance of the conjoint tendon (red arrow). (E) Axial T2 sequence showing a complete rupture of the conjoint tendon (red bracket). (F) Transversal ultrasound scan where it can be seen the complete absence of the conjoint tendon (red arrow).
Ruptures in the dense connective tissue structures have the worst prognosis.15,23,24,25,2 6,27,28This statement correlates perfectly with the histo-anatomical knowledge to design RTP programmes according to the structure affected by the injury.
Tendons and aponeuroses, being less vascular than skeletal muscle fibres, heal slower, and may benefit from interventions that enhance blood flow to the area surrounding the injured region.29 They may also benefit from a more conservative approach in the early stages after the injury to allow granulation and scar tissue formation, i.e. creating a better “scaffold” for the healing process.24,27,30 By allowing extra recovery time in the acute phase after the injury, the high re-injury risk that is associated with these injuries can be potentially avoided.31 After all, it is re-ruptures that are is the severest complication of injury to the muscle-tendon unit; they have substantially longer RTP times than primary ruptures.
Fascial injuries are associated with the best prognosis due to their different structural properties. They might also respond better to manual therapy and stretching exercises.15,31 Myofascial and fascial injuries can be managed a bit more aggressively in terms of
the RTP as their re-injuries are not as severe as tendinous or myotendinous ones.
Due to their different healing times (tendon being the slowest, followed by the aponeurosis and both also being the most prone for re-injuries) and properties, the prognosis will differ according to the structure affected.32,33
Recently, there has been some controversy regarding injury prevention programmes and their utility. If we want to design an appropriate prevention programme, we need to consider each specific structure that we want to work on. For instance, fascia requires multi-directional flexibility. Training can incorporate mobility work to prevent fascial restrictions that can lead to an injury. The same concepts can be applied when designing a programme for a proximal hamstring enthesopathy, or to gain strength in the hamstring muscle group.
Beyond the concepts described above, we also need to consider that all muscles are different in terms of their architecture, and inter-personal differences can be found due to large anatomical variabilities between individuals.
Another important point to consider is that, if we use the same nomenclature and we can apply these concepts properly, the separation between the three main histological components can also be seen in imaging techniques like ultrasound or, especially, in magnetic resonance imaging (MRI). This would allow us to use the correct nomenclature not just when reporting scans (which is key for having an accurate initial diagnosis (Figure 4, Figure 5, Figure 6)), but also for the reproducibility of formal academic research on these injuries.
Conclusions
Uniform nomenclature for skeletal muscle ruptures involving the connective tissue structures based on histological differences of the connective tissues allows for clear communication between athletes, coaches, and healthcare providers, ensuring an accurate understanding of the injury’s nature, which is essential for effective treatment and for optimal rehabilitation strategies.
Understanding the structure and function of every type of connective tissue will allow us to prescribe the most appropriate exercise according to the tissue’s characteristics and the RTP evolution.

Figure 5. Imaging composition of a Rectus femoris (RF) central aponeurosis rupture. (A) Histological sample of an aponeurosis structure. (B) Sagittal view of a cadaveric sample (E) of the human RF. Different connective tissue structures are identified and marked: PT (proximal tendons); AA (anterior aponeurosis); CA (central aponeurosis); PF (posterior fascia); PA (posterior aponeurosis); DT (distal tendon). (C) MRI Axial T1 sequence showing the normal appearance of the central aponeurosis of the RF (orange bracket). (D) Tranversal ultrasound scan showing the normal appearance of the central aponeurosis of the RF (orange bracket). (E) Axial T2 sequence showing a complete rupture of the central aponeurosis of the RF (orange bracket). (F) Transversal ultrasound scan where it can be seen the complete rupture of the central aponeurosis of the RF (orange bracket).

Figure 6. Imaging composition of a Rectus femoris (RF) myofascial injury. (A) Histological sample of a fascial structure. (B) Sagittal view of a cadaveric sample (E) of the human RF. Different connective tissue structures are identified and marked: PT (proximal tendons); AA (anterior aponeurosis); CA (central aponeurosis); PF (posterior fascia); PA (posterior aponeurosis); DT (distal tendon). (C) MRI Axial T1 sequence showing the normal appearance of the posterior fascial tissue of the RF which is located proximal and lateral (green bracket). (D) Tranversal ultrasound scan showing the normal appearance of the posterior fascial tissue of the RF (green bracket). (E) Axial T2 sequence showing a myofascial rupture of the posterior fascial tissue of the RF (green bracket). (F) Transversal ultrasound scan where it can be seen the myofascial rupture of the posterior fascial tissue of the RF (green bracket).
By focusing on the histological characteristics, there is a layer of specificity added that can significantly refine the approach to diagnosis, prognosis, and treatment of sports-related muscle and tendon injuries, not only for the treatment of athletes, but also for the reproducibility of the academic research on these injuries.
References
Author Affiliations:
Carles Pedret MD, PhD: Clinica Diagonal. Sports Medicine and imaging department. Esplugues de Llobregat. Spain.
Ramon Balius MD, PhD: Sport Catalan Council. Generalitat de Catalunya. Barcelona. José Peña-Amaro MD, PhD: Department of Morphological Sciences (Section of Histology), Faculty of Medicine and Nursing, Maimonides. Biomedical Research Institute of Cordoba (IMIBIC), University of Cordoba, Spain
Tero Järvinen MD, PhD: Tampere University and Tampere University Hospital. Finland.
1. H.-W. Mueller-Wohlfahrt et al., “Terminology and classification of muscle injuries in sport: The Munich consensus statement,” Br J Sports Med, vol. 47, no. 6, pp. 342 LP –350, Apr. 2013, doi: 10.1136/bjsports-2012-091448.
2. N. Pollock, S. L. J. James, J. C. Lee, and R. Chakraverty, “British athletics muscle injury classification: a new grading system,” Br J Sports Med, vol. 48, no. 18, pp. 1347 LP –1351, Sep. 2014, doi: 10.1136/bjsports-2013-093302.
3. X. Valle et al., “Muscle Injuries in Sports: A New Evidence-Informed and Expert Consensus-Based Classification with Clinical Application,” Sports Medicine, vol. 47, no. 7, pp. 1241–1253, 2017, doi: 10.1007/s40279-016-0647-1.
4. R. Balius et al., “Role of the Extracellular Matrix in Muscle Injuries: Histoarchitectural Considerations for Muscle Injuries,” Orthop J Sports Med, vol. 6, no. 9, pp. 4–6, 2018, doi: 10.1177/2325967118795863.
5. R. P. Wohlgemuth, S. Sriram, K. E. Henricson, D. T. Dinh, S. E. Brashear, and L. R. Smith, “Strain-dependent dynamic re-alignment of collagen fibers in skeletal muscle extracellular matrix,” Acta Biomater, Aug. 2024, doi: 10.1016/j.actbio.2024.08.035.
6. A. R. Gillies and R. L. Lieber, “Structure and function of the skeletal muscle extracellular matrix.,” Muscle Nerve, vol. 44, no. 3, pp. 318–331, Sep. 2011, doi: 10.1002/ mus.22094.
7. B. B. Wheatley, O. L. Dyer, E. E. Tully, and M. A. Seeley, “Aponeurosis structure-function properties: Evidence of heterogeneity and implications for muscle function.,” Acta Biomater, vol. 168, pp. 298–308, Sep. 2023, doi: 10.1016/j.actbio.2023.06.035.
8. M. Lehto, T. J. Sims, and A. J. Bailey, “Skeletal muscle injury--molecular changes in the collagen during healing.,” Res Exp Med (Berl), vol. 185, no. 2, pp. 95–106, 1985, doi: 10.1007/BF01854894.
9. M. Järvinen, L. Józsa, P. Kannus, T. L. Järvinen, M. Kvist, and W. Leadbetter, “Histopathological findings in chronic tendon disorders.,” Scand J Med Sci Sports, vol. 7, no. 2, pp. 86–95, Apr. 1997, doi: 10.1111/j.1600-0838.1997.tb00124.x.
10. R. B. Svensson, S. T. Smith, P. J. Moyer, and S. P. Magnusson, “Effects of maturation and advanced glycation on tensile mechanics of collagen fibrils from rat tail and Achilles tendons.,” Acta Biomater, vol. 70, pp. 270–280, Apr. 2018, doi: 10.1016/j.actbio.2018.02.005.
11. T. A. H. Järvinen, T. L. N. Järvinen, P. Kannus, L. Józsa, and M. Järvinen, “Collagen fibres of the spontaneously ruptured human tendons display decreased thickness and crimp angle.,” J Orthop Res, vol. 22, no. 6, pp. 1303–9, Nov. 2004, doi: 10.1016/j.orthres.2004.04.003.
12. M. H. M. Langevin and P. P. A. Huijing, “Communicating About Fascia: History, Pitfalls, and Recommendations,” International Journal of Therapeutic Massage & Bodywork: Research, Education, & Practice, vol. 2, no. 4, Dec. 2009, doi: 10.3822/ijtmb.v2i4.63.
13. J. Peña-Amaro, “The musculotendinous transition of the extracellular matrix,” Apunts Sports Medicine, vol. 56, no. 210, 2021, doi: 10.1016/j.apunsm.2021.100350.
14. P. P. Purslow, “The structure and functional significance of variations in the connective tissue within muscle.,” Comp Biochem Physiol A Mol Integr Physiol, vol. 133, no. 4, pp. 947–66, Dec. 2002, doi: 10.1016/s1095-6433(02)00141-1.
15. X. Valle et al., “Return to Play Prediction Accuracy of the MLG-R Classification System for Hamstring Injuries in Football Players: A Machine Learning Approach.,” Sports Med, vol. 52, no. 9, pp. 2271–2282, Sep. 2022, doi: 10.1007/s40279-022-01672-5.
16. S. G. of the M. and T. S. from the S. S. of S. Traumatology et al., “A Histoarchitectural Approach to Skeletal Muscle Injury: Searching for a Common Nomenclature,” Orthop J Sports Med, vol. 8, no. 3, pp. 2325967120909090–2325967120909090, Mar. 2020, doi: 10.1177/2325967120909090.
17. M. I. Zein et al., “Baseline clinical and MRI risk factors for hamstring reinjury showing the value of performing baseline MRI and delaying return to play: a multicentre, prospective cohort of 330 acute hamstring injuries.,” Br J Sports Med, May 2024, doi: 10.1136/bjsports-2023-107878.
18. B. Macdonald, S. Mcaleer, S. Kelly, R. Chakraverty, M. Johnston, and N. Pollock, “Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice,” Br J Sports Med, p. bjsports-2017-098971, 2019, doi: 10.1136/bjsports-2017-098971.
19. B. Hamilton, J. M. Alonso, and T. M. Best, “Time for a paradigm shift in the classification of muscle injuries,” J Sport Health Sci, vol. 6, no. 3, pp. 255–261, 2017, doi: 10.1016/j.jshs.2017.04.011.
20. M. Zügel et al., “Fascial tissue research in sports medicine: From molecules to tissue adaptation, injury and diagnostics: Consensus statement,” Br J Sports Med, vol. 52, no. 23, p. 1497, 2018, doi: 10.1136/bjsports-2018-099308.
21. R. Schleip, G. Hedley, and C. A. Yucesoy, “Fascial nomenclature: Update on related consensus process,” Clinical Anatomy, vol. 32, no. 7, pp. 929–933, 2019, doi: 10.1002/ ca.23423.
22. N. Maffulli et al., “Muscle Injuries: A Brief Guide to Classification and Management.,” Transl Med UniSa, vol. 12, pp. 14–8, 2015.
23. D. W. Creighton, I. Shrier, R. Shultz, W. H. Meeuwisse, and G. O. Matheson, “Return-to-play in sport: a decision-based model.,” Clin J Sport Med, vol. 20, no. 5, pp. 379–85, Sep. 2010, doi: 10.1097/JSM.0b013e3181f3c0fe.
24. J. Isern-Kebschull et al., “Muscle Healing in Sports Injuries: MRI Findings and Proposed Classification Based on a Single Institutional Experience and Clinical Observation.,” Radiographics, vol. 44, no. 8, p. e230147, Aug. 2024, doi: 10.1148/rg.230147.
25. J. Doege et al., “Defining Return to Sport: A Systematic Review.,” Orthop J Sports Med, vol. 9, no. 7, p. 23259671211009588, Jul. 2021, doi: 10.1177/23259671211009589.
26. B. M. Paton et al., “London International Consensus and Delphi study on hamstring injuries part 3: rehabilitation, running and return to sport.,” Br J Sports Med, vol. 57, no. 5, pp. 278–291, Mar. 2023, doi: 10.1136/bjsports-2021-105384.
27. T. A. H. Järvinen et al., “Muscle injuries: optimising recovery.,” Best Pract Res Clin Rheumatol, vol. 21, no. 2, pp. 317–31, Apr. 2007, doi: 10.1016/j.berh.2006.12.004.
28. R. Shamji, S. L. J. James, R. Botchu, K. A. Khurniawan, G. Bhogal, and A. Rushton, “Association of the British Athletic Muscle Injury Classification and anatomic location with return to full training and reinjury following hamstring injury in elite football,” BMJ Open Sport Exerc Med, vol. 7, no. 2, May 2021, doi: 10.1136/bmjsem-2020-001010.
29. T. A. H. Järvinen, “Neovascularisation in tendinopathy: from eradication to stabilisation?,” Br J Sports Med, vol. 54, no. 1, p. 1, Jan. 2020, doi: 10.1136/ bjsports-2019-100608.
30. C. Pedret, J. Peña-Amaro, R. Balius, and T. Järvinen, “Histological Definition of Skeletal Muscle Injury: A Guide to Nomenclature Along the Connective Tissue Sheath/ Structure.,” Sports Med, Dec. 2024, doi: 10.1007/s40279-024-02165-3.
31. D. Pieters, E. Wezenbeek, J. Schuermans, and E. Witvrouw, “Return to Play After a Hamstring Strain Injury: It is Time to Consider Natural Healing.,” Sports Med, vol. 51, no. 10, pp. 2067–2077, Oct. 2021, doi: 10.1007/s40279-021-01494-x.
32. J. Isern-Kebschull et al., “MRI findings prior to return to play as predictors of reinjury in professional athletes: a novel decision-making tool.,” Insights Imaging, vol. 13, no. 1, p. 203, Dec. 2022, doi: 10.1186/s13244-022-01341-1.
33. T. A. Järvinen, M. Järvinen, and H. Kalimo, “Regeneration of injured skeletal muscle after the injury.,” Muscles Ligaments Tendons J, vol. 3, no. 4, pp. 337–45, Oct. 2013.


SWIMEX HYDROTHERAPY, CONTRAST
PLUNGE
POOLS & HYDROTHERAPY SUITE DESIGN GUIDANCE
Aqua Thermae are specialists in professional sports and medical hydrotherapy, distribute the world class SwimEx pool range across the UK, Ireland and the rest of Europe, whilst also managing projects further afield in the Middle East.
Our clients include Warner Brothers film studios, The UK Sports Institute, The Ministry of Defence - Special Forces Hereford, Plymouth University extreme climate research pools, Wolves FC, as well as specialist medical clinics and hospitals. Recent projects include Queens Park Rangers’ training ground, installing a SwimEx 600T performance and recovery pool, and a deep water plunge cold recovery pool with energy efficient heat pump chiller. We also Installed the SwimEx 600T at the Strive Elite Sports Academy in jersey which has hosted the World champions South Africa squad, the British & Irish Lions, England Rugby, Leicester Tigers, Sale and Bath rugby.
The success and delivery of elite sports performance and recovery aquatic-based solutions is founded on experienced design
specification and selection of premium quality equipment designed to exceed the industry guidance. Richard Bishop M.P.W.T.A.G. Technical Design Director, has 38 years industry experience and composed the award winning technical paper for the institute of Swimming Pool Engineers, and presented talks on Sports Hydrotherapy Design to the Institute.
Previously we refurbished the filtration system at Bisham Abbey to help Team GB’s build-up to the Paris Olympics. We were honoured to work with The UK Sports Institute and Team GB, and proud in receiving wonderful first-hand feedback from the athletes and the medical team.
Whether you are looking for a brand new hydrotherapy suite from ice bath to physiotherapy pool to a sauna, or seeking to upgrade your existing filtration and water treatment facilities to enhance and look after your existing pool equipment, Aqua Thermae are available to support your project across the UK and Europe. We can provide a simple health check with guidance on your existing facilities,
design consultation and supply Internet monitored management systems and planned maintenance services for the ultimate peace of mind after-care.
Well maintained hydrotherapy resources will protect your athletes and, in many cases, help deliver accelerated recovery outcomes, ensuring the players return to the field sooner with more resilience, to help prevent repeat injuries.
As we proudly say “Aqua Thermae strives to design well and deliver far more”.
SwimEx Performance and Physiotherapy Pools are handcrafted, custom-built marine grade pools, similar to an ocean racing yacht. They are custom built to order for each client and can be emblazoned to reflect the sports teams colours and branding.
SwimEx was designed over 40 years ago to deliver a unique laminar smooth resistance flow experience from its patented paddlewheel water drive system, which can be enhanced with custom deep wells, physiotherapy stations and underwater motorised treadmills.
Recovery Pools
We also install SwimEx hot and cold deep water recovery pools for accelerated recovery and prevention of D.O.M.S. post-training and between matches. We can supply self-contained individual ice baths through to full team recovery pools.
Filtration
We minimise chemical inputs into the pool water for a better bathing experience and lower running costs by hyper filtration screening the water more efficiently with advanced filter medias and deep bed filters. By removing the particulate matter more effectively we reduce or replace the amount of traditional chlorine required to keep the pool water safe. Energy saving control on the water flow further enhances the operation of the system.
Water Treatment
Our water treatment systems are specified for each pool and include advanced UV systems and accurate ph, chlorine monitoring and control, all inked to the internet so we can provide monitoring which allow for rapid remote technical support, 24/7.
This year we have launched a new natural sea salt hydrolysis system to deliver a better bathing experience for the players and medical team and reduce operational costs for the club.


Climate Control
One of the largest cost factors operating an Indoor hydrotherapy suite will be the heating energy costs. We can help design and enhance your heating system to ensure the pool water, air temperature and humidity are maintained in harmony and balance. This will lead to substantial savings in operational costs.
Training
We offer a comprehensive planned maintenance service schedule along with professional training of on-site staff to ensure the pools are operated efficiently and deliver safe bathing water.
MEMBERSHIP OFFER
We are pleased to offer a free initial pool plant health check and guidance report for existing pools to all UK and Ireland FMPA members. Contact Richard Bishop direct to discuss: Email richard@aquathermae.co.uk Tel 07484 070765
www.aquathermae.co.uk www.swimex.com




It is well understood that the physical demands in football centre on the ability to sprint fast and the ability to repeat these sprints (RSA) throughout the 90-plus minutes. Players who can maintain a high proportion of this RSA over the duration of a match are generally those who can also maintain their technical skill level and avoid injury. However, developing this ability in the pre-season and maintaining it throughout the season is challenging. In the unfortunate circumstance of an injury, returning players to match-ready fitness is a constant challenge, and methods to accelerate this process are valuable.
More detailed analysis of the research in the use of Intermittent Hypoxic Training (IHT) using altitude chambers over the last 10 years or so, shows convincing evidence of the effectiveness of this mode of training – when used correctly.
When using an altitude chamber, players
ALTITUDE : HEAT : HUMIDITY
OUTSTANDING FACILITIES FROM THE WORLD LEADER, BASED HERE IN THE UK


can train at lower intensities, requiring less muscular and joint loads, for the same or higher cardiovascular demands. When blood oxygen levels are very low, which can only be achieved for long periods when hypoxia is combined with exercise, several hypoxia-sensitive genes are stimulated which initiate a series of downstream events that lead to adaptations throughout the muscle bundle using protein in the diet to build and construct a series of new structures and organelles, as well as improve the efficiency and rates of energy production. These changes improve both aerobic and anaerobic energy production, and are what create, and explain, the improvements in high intensity exercise and repeat sprint ability.
A number of papers also point to the effectiveness of heat as an effective stressor for endurance, and the ability to investigate and mitigate the effects of Exertional Heat Illness is increasingly
important as players have to deal with playing in ever increasing temperatures.
Recent research shows that regular short exposures to hypoxia, such as those during IHT, also causes an increase in EPO, which not only drives an increase in oxygen carrying capacity of the blood, but also plays a much wider role in enhancing aspects of metabolism, oxidative function and muscle tissue repair.
For this reason, the use of hypoxia has a particular benefit in injury rehabilitation. The same hypoxiasensitive mechanisms described above that increase aerobic and anaerobic ability, may play a role in accelerating the repair and re-organisation of damaged muscle tissue and bone. It allows the post-injured player to receive a larger metabolic challenge at a lower load and intensity, facilitating a faster increase in fitness and return to play.


FMPA MEMBERSHIP
Expert legal support and representation across employment medico legal and regulatory law
All the benefits of Union membership through the FMPA
Priority member only access to job listings and email alerts 24/7 support from the FMPA and much more…
“I believe FMPA membership is now essential and should be a pre-requisite for any member of staff within our sector.”
Head of Sport Science & Medicine, Premier League

