Department of Ophthalmology


Message From the Department of Ophthalmology Leadership
Breakthrough Light Wave Therapy for AMD Catapults
One Patient From Despair to Hope
A New Ophthalmic AI Fellowship Underscores Our Role as a Technology Leader
Groundbreaking Surgery to Remove Rare Retinal Tumor Saves 15-Year-Old Boy’s Eye
Exploring a Metabolic Resilience Factor for People at High Genetic Risk of Glaucoma
New Services and Facilities Confirm Our Focus on Growth
Painting a Clearer Picture of Blood Flow Dynamics With Doppler Holography
A Postcard From Jamaica
NYEE’s Longest-Serving Voluntary Faculty Member Embarks Upon a New Teaching Project at Age 99
AI Is Opening a Powerful New Window on Predicting Glaucoma Through Vascular Risk
Message From the Department of Ophthalmology Leadership
Unwavering in our 205-year commitment to patients and community, New York Eye and Ear Infirmary of Mount Sinai (NYEE) continues to expand and improve services across a wide range of ophthalmic medical fronts as well as our new 24/7 full-service urgent care.
At a time of exciting change within the field of ophthalmology, we remain on the cutting edge of technology in vital areas like treatment of adult macular degeneration (AMD) through a promising new form of light therapy, and in clinical practice by resecting a complex retinal tumor from a young patient through a rarely used surgical technique.
The formal opening of our Center for Refractive Solutions in the spring of 2025 underscores the progress we have made. The new Center is unrivaled in its ability to provide patients who seek refractive correction with the latest technologies, advanced corneal and anterior segment imaging, and staff of experienced specialists who confer with patients to carefully craft a surgical plan that complements their everyday ocular and lifestyle needs.
Mount Sinai-Urgent Care, East 14th Street, also builds on our unstinting commitment to growth and community service by bringing 24/7 access to skilled professional care for both medical and eye emergencies back to the New York metropolitan area. Our recently opened, fully equipped walk-in facility at NYEE’s East Village campus is prepared to respond in the middle of the night to all types of urgent eye needs through our team of on-call residents, fellows, and faculty specialists. Less severe medical conditions requiring immediate attention can also be managed by an on-site ER-trained physician.
When it comes to innovation and technology, there is no better example of how we remain in the vanguard than our role in the clinical development and introduction of noninvasive light therapy for dry AMD. Richard B. Rosen, MD, FARVO, Vice Chair of Ophthalmic Research at NYEE and Chief of the Retina Service for the Mount Sinai Health System, recently offered the breakthrough
light wave therapy known as photobiomodulation to his patients and immediately noticed improved visual acuity and slower disease progression—welcome developments for a serious condition with very few approved treatments.
We made further inroads in research through a novel study that used artificial intelligence (AI) and optical coherence tomography angiography to provide the strongest scientific evidence to date that vascular parameters should be considered along with the traditional structural variables in characterizing and assessing the risk of primary open-angle glaucoma in humans. At the same time, in the summer of 2025, we launched one of the first ophthalmic AI clinical and research fellowship programs in the country. The advanced education curriculum, under the umbrella of the newly launched Barry Family Center for Ophthalmic Artificial Intelligence and Human Health, is training a new generation of digitally skilled ophthalmologists who will pioneer new ophthalmic diagnostics and research approaches using AI to help close knowledge gaps in clinical care.
Finally, one of our longstanding voluntary teaching faculty members brought home to us the real meaning of dedicated service. Seymour Fradin, MD, former Associate Director of the Retina Service, continues to instruct residents and fellows at age 99. And this January, just for good measure, he published an instructional handbook for trainees on mastering the often-challenging art of indirect ophthalmoscopy and fundus exam techniques.
“For the past 60 years, Dr. Fradin has been an ingrained and valuable part of our professional community,” observes Dr. Tsai. “He has remained true to our mission of integrating clinical care, research, and education into everything we do, and stands out as an enduring model of the values and principles we are all working so hard to preserve at NYEE.”

James C. Tsai, MD, MBA
President, New York Eye and Ear Infirmary of Mount Sinai
Chair, Department of Ophthalmology
Icahn School of Medicine at Mount Sinai and Mount Sinai Health System

Paul A. Sidoti, MD
Chair, Department of Ophthalmology
New York Eye and Ear Infirmary of Mount Sinai

Louis R. Pasquale, MD, FARVO
Louis R. Pasquale, MD, FARVO
Chair, Department of Ophthalmology,
Chair, Department of Ophthalmology
The Mount Sinai Hospital and Mount Sinai Queens
The Mount Sinai Hospital and Mount Sinai Queens
Breakthrough Light Wave Therapy for AMD Catapults One Patient From Despair to Hope
Susan Baum felt trapped by her family’s bleak history with age-related macular degeneration (AMD).
“My father was diagnosed with AMD in his 50s, and I watched it slowly rob my younger sister of her independence, just like it had my dad,” she recalls.
“I thought I beat the odds…after all, my 50s and 60s went by with no major eye problems, and then I was diagnosed with the condition in 2023, the next step in what seemed like a doomsday scenario for me.”

Susan Baum
The doomsday feeling lifted in March 2025 thanks to the introduction of a breakthrough, noninvasive form of light therapy for dry AMD, which she began using in the office of Richard B. Rosen, MD, FARVO, Chief of the Retina Service for the Mount Sinai Health System. Within weeks of Ms. Baum’s first series of light wave treatments, her visual acuity began to improve—well beyond her expectations—and she was eagerly signing up for the next round of therapy in four months.
“Patients have responded well to it,” says Dr. Rosen, referring to the LumiThera Light Delivery System from Valeda � , “reporting noticeable improvements in their ability to see details they couldn’t before and generally feeling more confident in how they navigate visually. Those improvements have been modest, but any improvements when it comes to AMD are welcome.”
Dr. Rosen was co-author of a study, LIGHTSITE III, that paved the way for approval of the light delivery system by the U.S. Food and Drug Administration in November 2024. New York Eye and Ear Infirmary of Mount Sinai (NYEE) was one of 10 clinical centers around the country that participated in the study of 100 patients with early and intermediate dry AMD. After 13 months, 55 percent of treated eyes experienced a significant increase in vision of at least one line of letters on the standard eye chart. Of that group, 20 percent had a gain of two lines and nearly 6 percent had a gain of three lines.
“The study not only showed an improvement in vision, but also in the stabilization of metabolic function, reduction in drusen, and reduced risk for progression to geographic atrophy, which is latestage AMD affecting central vision,” notes Dr. Rosen, who is also the Vice Chair of Ophthalmic Research at NYEE. His interest in light therapy, also known as photobiomodulation, began in the 1990s with scattered reports of its use in treating dry macular degeneration. The science took a quantum leap years later with the

Photobiomodulation helps to activate the photoacceptors in the mitochondria at a cellular level by stimulating metabolic activity of ATP, preventing inflammation and cell death.
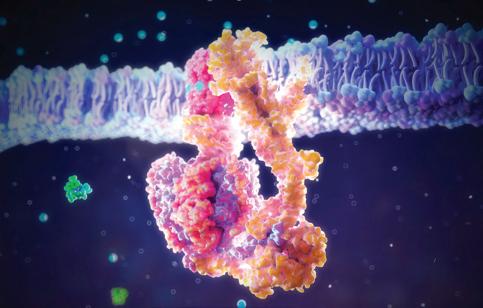
Improvements in cell function via increased enzymatic activity at two separate sites on cytochrome c oxidase (CuA and CuB) help drive the production of the proton gradient required by ATP synthase to produce energy. By restoring the production of energy and signaling molecules, a secondary effect is triggered that sustains improved cell function.
development and approval of the LumiThera system, the first treatment for dry AMD to show improved visual acuity and to slow progression of the disease. AMD afflicts an estimated 20 million people in the United States and there are no approved treatments for dry AMD in its early or intermediate stages beyond antioxidant supplementation, which delays progression in only 20 to 25 percent of eyes.
The newly approved light wave therapy involves a series of treatments over three to five weeks with three specific wavelengths (590 nm yellow, 660 nm red, and 850 nm infrared), which act by stimulating improvements in mitochondrial function in retinal cells. This photobiomodulation process occurs when the chain of proteins in the mitochondria responsible for
Even going down subway stairs to catch a train, I noticed that the lip of the steps was more clearly defined, reducing the chance of a dreaded fall.
—Susan Baum

generating adenosine triphosphate (ATP)—the universal energy source of cells—absorbs the wavelengths, enhancing the production of ATP and improving the energy of retinal cells.
Ms. Baum was among the earliest beneficiaries of this newly approved technology. A voice teacher with a busy practice in New York City, she realized that the job she loved doing for so long was suddenly in jeopardy due to her growing inability to read the notations in sheet music and to see the faces of her students. “Music is my life…and the thought of not being able to follow my passion sent me into a serious depression,” Ms. Baum recalls. She began studying the literature on AMD with the zeal of a research fellow in hopes of finding a treatment and sought out Dr. Rosen with new hope around this new treatment.
She started a course of nine sessions at NYEE, peering into the sleek machine with its programmed sequences of low-intensity light, and quickly started to see results. Back in her studio after the third week of treatment, she looked at the same sheet music from a few days earlier and noticed that the staff lines were less wavy, the G and C chord notations more differentiated. “I almost couldn’t believe it,” she exults. “Even going down
subway stairs to catch a train, I noticed that the lip of the steps was more clearly defined, reducing the chance of a dreaded fall.”
At a follow-up visit in May, Ms. Baum reported the encouraging news to Dr. Rosen; it was consistent with comments he was hearing from other patients using the device. Meanwhile, Dr. Rosen, who has been at the forefront of studying mitochondrial dysfunction in retinal disease for the past 13 years, is involved in other studies investigating the application of light therapy to retinal disorders that include diabetic retinopathy, central serous chorioretinopathy, and glaucoma. A recent grant from the Leon Lowenstein Foundation will further allow his lab to study the oxidative stress on the mitochondria in patients both before and after LumiThera treatment.
For now, though, anecdotal evidence from highly motivated patients like Ms. Baum are as meaningful to Dr. Rosen as the findings of any multi-site, placebocontrolled trial. “You’ve given me hope,” she wrote to her ophthalmologist in April, “that I might retain my vision and maybe even improve it, despite facing a hereditary and seemingly inevitable loss.”
A New Ophthalmic AI Fellowship
Underscores Our Role as a Technology Leader

Weaving artificial intelligence (AI) into the complex fabric of New York Eye and Ear Infirmary of Mount Sinai (NYEE) is undeniably a tall order. The process, which began in earnest several years ago, is now expected to pick up considerable steam with the creation of an Ophthalmic AI Clinical and Research Fellowship—among the first of its kind in the country—under the umbrella of the renamed Barry Family Center for Ophthalmic Artificial Intelligence and Human Health at the Icahn School of Medicine at Mount Sinai.
“The fellowship is a critical step in advancing NYEE’s strategic goals around AI and machine learning,” says Tak Yee Tania Tai, MD, Clinical Advisory Director of the Center, whose longtime relationship with the Barry family led to their generous gift in support of the fellowship and the new Center.
“The one-year fellowship will help cultivate the next generation of clinician-researchers who can harness AI to improve diagnosis, streamline clinical workflows, and develop more personalized approaches to care. It also reinforces our institution’s role as a leader in innovation.”
As Co-Director of the Ophthalmic AI Fellowship, Dr. Tai will help direct its efforts, in part, toward the diagnosis and treatment of glaucoma, a strong interest of the Barry family. She also serves as a mentor to the inaugural AI fellow, Gal Jacob Cohen, MD, who recently finished a five-year residency at Sheba Tel HaShomer Medical Center in Israel. In this supportive role, Dr. Tai plans to help shape the fellowship into a robust learning experience through hands-on collaboration and research guidance.
Dr. Cohen, for his part, couldn’t be more anxious to start.
“I knew early in my career I wanted to work at the intersection of technology and medicine,” he says. When he learned from colleagues that NYEE had created a dedicated center for AI in ophthalmology, followed by a fellowship, he leapt at the opportunity. “I felt like it was a calling, something I really needed to do,” he recalls. “And I was only too willing to take a break in my surgical training at home to devote a year to the fellowship.”
Having arrived in New York in July with his wife and children, he is now getting his feet wet in what promises to be a very busy and challenging year
ahead, combining clinical practice with cutting-edge research. One project he may take an active role in, for example, is leveraging AI to detect patients who progress rapidly to glaucoma, losing much of their visual field in a relatively short period and thus increasing their risk of blindness.
“Our new fellow will be working with others, including a bioinformatics specialist at The Charles Bronfman Institute for Personalized Medicine at the Icahn School of Medicine, to see if there are differences in the charts of a short list we have of fast glaucoma progressors versus those who are not,” says Louis R. Pasquale, MD, FARVO, Deputy Chair for Research and Co-Director of the Ophthalmic AI Fellowship and the Barry Family Center. “By using large language models, we may be able to discover, from chart information, patterns of glaucoma progression that are not evident to humans.”
Other potential projects for the fellow include developing AI algorithms for NYEE’s central retinal artery occlusion program, which identifies eye stroke from optical coherence tomography (OCT) images of patients who present at emergency rooms of Mount Sinai hospitals, and for its tele-retina program, where primary care providers use high-quality portable digital cameras to capture retinal images during annual patient exams.
In the year ahead, Dr. Cohen will also find himself many days in NYEE’s Retina Center and the David E. Marrus Adaptive Optics Imaging Laboratory under the guidance of Richard B. Rosen, MD, FARVO, Vice Chair of Ophthalmic Research at NYEE. As part of that learning experience, Dr. Rosen hopes to have the fellow collaborate with a group at the Joan and Irwin Jacobs Technion-Cornell Institute that is looking to deploy the power of OCT angiography together with AI to shorten the time it takes researchers to identify the minute changes that occur in the microvasculature of the retina.
In terms of education, the new AI fellow will have abundant opportunities to serve as both a trainee and trainer. “AI literacy is something all of us need to learn, and we hope that the fellow will present a lecture to our staff on AI and its growing role within ophthalmology,” explains Dr. Pasquale. “AI has the potential to teach our doctors how to be better observers of pathologies that are often easy for us to miss, and that’s a message our AI fellow can hopefully drive home.”
Groundbreaking Surgery to Remove Rare Retinal Tumor Saves 15-Year-Old
Boy’s Eye
When conventional treatments failed to stop the progression of a rare, benign retinal tumor that was damaging vision in a 15-year-old boy’s left eye, surgeons at New York Eye and Ear Infirmary of Mount Sinai (NYEE) took a bold and innovative step that they believed offered the best chance of avoiding a catastrophic loss of the eye.
Gennady Landa, MD Director of the Retina Service at NYEE and Associate Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai

Neal Patel, MD Senior Vitreoretinal Surgery Fellow
They turned to a complex and rarely performed intraocular surgical procedure in a final attempt to save the eye and prevent permanent and complete vision loss. Only recently described in medical literature, the groundbreaking surgery involved using microscopic instruments and ultrafine sutures to meticulously ligate the blood vessels feeding the tumor before carefully resecting the tumor itself.
“We chose to attempt a technique we had never performed before,” says Gennady Landa, MD, Director of the Retina Service at NYEE and Associate Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai. “But we were confident this approach offered the most definitive treatment for such a complex case, while sparing the patient the side effects of repeated surgeries, radiation, or chemotherapy that are often required for treatment of tumors of this type.”
Dr. Landa was joined by Neal Patel, MD, Senior Vitreoretinal Surgery Fellow, in performing the surgery in February 2025.
Over the prior year, two attempts to treat the tumor through conventional laser surgery were undertaken by Ekaterina Semenova, MD, an ocular oncologist and Director of Pediatric Ocular Oncology at NYEE and The Mount Sinai Hospital. The retinal damage from this rare tumor, known as a retinal capillary hemangioblastoma, was found to be already considerable when Dr. Semenova first saw the patient. Though noncancerous, it had led to the development
of a large retinal detachment that had been slowly growing over the years and had gone unnoticed until it resulted in severe loss of vision in the affected eye.
“At first, we opted to start with a more conservative approach by trying to attach the retina and to prevent further growth of the tumor with two separate laser procedures and by injecting into the eye a medicine that aimed to stop leakage from the abnormal blood vessels. However, despite our efforts, the detachment only increased over time,” notes Dr. Semenova, who has treated her fair share of benign and malignant ocular tumors in children and adults over the years. “We knew the patient’s risk of completely losing the eye was high, so we began looking at other approaches.”
Dr. Landa, a seasoned retina surgeon used to handling the most complex retinal, macula, and vitreous surgical cases referred to him from across the New York metropolitan area, was an integral part of that conversation. He mapped out a unique and bold surgical strategy with Dr. Patel for their young patient that could accomplish three critical goals within the same procedure: ligate the feeder blood vessels, resect the tumor, and attach the retina.
The two-hour surgery began with removing vitreous gel from the center and from the edges of the eyeball to access the fragile retina and the tumor’s dilated feeder vessels. Dr. Landa and Dr. Patel then moved on to the most challenging part of the surgery—isolating and ligating the two abnormal vessels. Using intraocular forceps and the finest available sutures, they gently
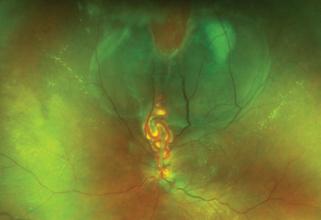
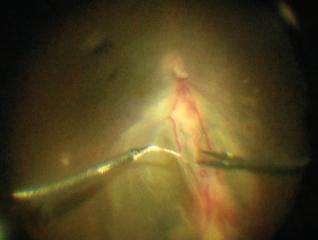
Fundus image of the tumor with a retinal detachment and the dilated feeder blood vessels
Ligation of the two abnormal vessels using intraocular forceps and sutures
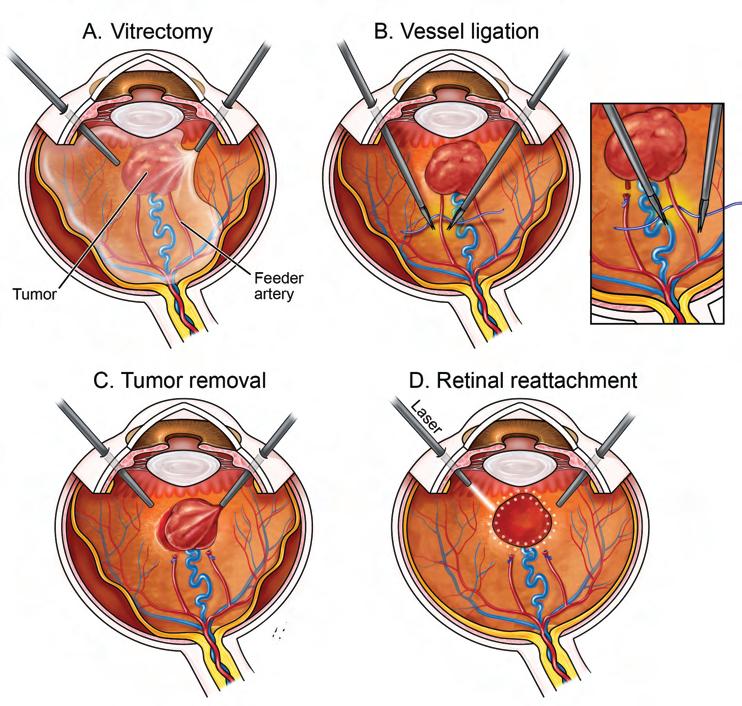
tied off the vessels from within the eye to prevent potentially devastating bleeding.
“The vessels were unusually large and dilated,” says Dr. Patel. “We couldn’t simply use traditional cautery and cut them without causing severe bleeding. They had to be carefully tied off with sutures, all within the tight confines of the eye.” A bimanual surgical technique with micro forceps and ultrafine sutures allowed the surgeons to complete this challenging task.
With the feeder vessels sealed, the team proceeded to remove the tumor, which measured approximately 3 mm thick and 8 mm in diameter. The retina around the tumor was treated with additional diathermy to prevent bleeding, and both the tumor and surrounding retina were excised with minimal blood loss. The detached retina was repositioned and secured using laser
Surgical diagram showing key steps performed by Dr. Landa and Dr. Patel, including tumor removal, vessel ligation, and laser therapy to repair the retinal detachment
therapy, and a gas bubble was inserted into the eye to maintain retinal attachment during healing.
Within two weeks, the teen had returned to his normal daily routine. The retina has remained attached, with no signs of tumor recurrence. While complete visual recovery is limited due to damage from longstanding retinal detachment, the eye appears healthy, functional, and cosmetically normal.
“We applied every bit of knowledge and surgical precision to execute this highly challenging, first-ofits-kind operation for our team, and we absolutely met our goals,” sums up Dr. Landa. “The tumor is out of the boy’s eye, the feeding blood vessels are sealed, and the retina is attached. Given the complexity and stakes, this was a major success and a testament to our collaborative efforts.”
JGregory
Exploring a Metabolic Resilience Factor for People at High Genetic Risk of Glaucoma
A team of researchers led by New York Eye and Ear Infirmary of Mount Sinai (NYEE) was intrigued by a statistical fact while investigating new approaches to accurately predict the risk of acquiring glaucoma. They learned from their observational study involving a large biobank that only 20 percent of people in the highest risk category for glaucoma based on their genetic scores had the disease.
Which begged the question: How had the other 80 percent managed not to have glaucoma? Just as critically, was there a resilience factor at play with significant implications for not just detection, but treatment, of a progressive neurodegenerative condition with no available cure?
The team’s findings, published in the April 2025 issue of eLife, made a strong and fascinating case for metabolites—the end products of biological processes that drive cellular growth and reproduction—as the molecular ingredient possibly providing a valuable buffer against genetic predisposition to glaucoma. More specifically, they suggest that a key member of that class of metabolites known as pyruvate may confer protective capability and, therefore, needs to be the focus of much additional research.
“We didn’t just stop at reporting that pyruvate could be a resilience biomarker against developing glaucoma in people with a high genetic predisposition,” says senior author Louis R. Pasquale, MD, FARVO, Deputy Chair for Research, and Director of the Mount Sinai/NYEE Eye and Vision Research Institute at the Icahn School of Medicine at Mount Sinai.
“We showed that integrating metabolites with genetics allowed us to come up with much stronger prediction models for glaucoma, and possibly better ways of treating and monitoring the disease down the road.”
To determine if metabolites enhanced glaucoma detection, scientists studied 4,658 glaucoma cases from the UK Biobank, a widely researched dataset with more than half a million participants from the United Kingdom. While it is widely known that glaucoma risk is influenced by both genetic and metabolic factors, investigators in the NYEE
study learned that metabolites by themselves were weak predictors of glaucoma. They were surprised to discover, however, that when they statistically combined people who had the highest metabolic risk scores with those with the highest genetic scores, the group showed a 25-fold increased risk of glaucoma over those at the bottom rung of both risk categories.
“Whenever we see results like that in epidemiology,” acknowledges Dr. Pasquale, “we know we are potentially on to something that must be seriously explored.”
To be sure, recent advances in metabolomic science have opened new avenues for investigating these small molecules as possible biomarkers for glaucoma and intraocular pressure (IOP), which is typically elevated in glaucoma patients. The new study is the first, however, to examine the utility of incorporating metabolic data into glaucoma genetic prediction algorithms. Furthermore, working in conjunction with Simon John, PhD, at Columbia University, the researchers validated pyruvate as a metabolite that could mitigate genetic risk of glaucoma in a human-relevant mouse model. Pyruvate use in mice with a strong genetic predisposition to glaucoma lowered IOP and protected against optic nerve damage.
“The statistical interaction we demonstrated between metabolite and genetic risk scores helped to identify individuals who, despite high genetic risk, are less likely to develop glaucoma due to favorable metabolic profiles,” sums up Dr. Pasquale, who is also Professor of Ophthalmology, and Artificial Intelligence and Human Health at the Icahn School of Medicine.
The next step for Dr. Pasquale is to conduct a small study to determine if pyruvate might affect intraocular pressure. And beyond that, the possibility of oral pyruvate supplementation for those with a high predisposition to glaucoma could appear on the radar screen of researchers.
“Though much work remains,” he says, “we’ve opened up important new therapeutic avenues using pyruvate as a resilience factor against glaucoma.”
Integrating the study of small organic molecules and large genetic datasets will help researchers develop better prediction models for glaucoma.
New Services and Facilities
Confirm Our Focus on Growth

New York Eye and Ear Infirmary of Mount Sinai (NYEE) significantly grew its campus footprint over the past year, bringing to patients and the community at large an array of enhanced, premium-quality services encompassing not just ophthalmology, but urgent care for most minor illnesses and injuries as well as primary care.
Center for Refractive Solutions
With the ribbon cutting in June 2025 for the Center for Refractive Solutions (CRS), NYEE became one of the most comprehensive and innovative centers in the nation for individuals desiring to improve their vision and requiring refractive correction. That includes cataract and intraocular lens surgery, as well as refractive
procedures like laser vision correction (LASIK) and the EVO Implantable Collamer Lens (ICL).
“With cataract and lens surgery, there are many options available today depending on the individual’s visual needs, lifestyles, and long-term goals,” says Paul A. Sidoti, MD, Chair of the Department of Ophthalmology at NYEE. “Our specialists at CRS are prepared to sit down with patients to discuss those options and work closely with them to tailor the type of surgery and lens implant that assures the best possible outcomes.”
The Center—made possible by a generous donation from Toni and Martin T. Sosnoff—assembled a team of
Ribbon-cutting ceremony held on June 4, 2025, to celebrate the opening of the Center for Refractive Solutions. From left to right: Anna Guller, James C. Tsai, MD, Kira Manusis, MD, Toni and Martin T. Sosnoff, Paul A. Sidoti, MD, Gennady Landa, MD, Salvatore Loiacono, and Sangyoon Jason Shin, DO
highly experienced ophthalmic surgeons and houses state-of-the-art corneal and ocular imaging equipment. This provides a unique opportunity for advanced imaging with more precise calculations and diagnostics. With this information, they are able to develop and customize a surgical plan that may include the latest intraocular lens platforms, such as trifocal and extended depth-offocus lenses, as well as the new light-adjustable lens. For patients who don’t have cataracts, the best route might be LASIK, a refractive lens exchange, or an EVO ICL, which corrects vision without the need to remove any corneal tissue.
Patients also benefit from a streamlined service under a single roof at the newly renovated space at 310 East 14th Street in Lower Manhattan. “By centralizing all the necessary equipment, services, and staff, we’re able to ensure patients an efficient and thorough evaluation in just one day,” emphasizes Kira Manusis, MD, Director of CRS and Co-Director of the Cataract Service at NYEE. “And that’s a huge advantage for our many patients who lead busy lives. Today, patients have more choices than ever and we’re here to help them design their vision to fit their lifestyle.”
Mount Sinai-Urgent Care
The opening in April 2025 of Mount Sinai-Urgent Care, East 14th Street, on the ground floor of our main building at Second Avenue and East 14th Street also offers major advantages to lower Manhattan patients in need of urgent care.
Adults and children can now walk right in—no appointment is needed—and obtain treatment from a professional team for less serious injuries and conditions such as allergy and asthma attacks, cuts that need stitches, earaches and sinus infections, sprains and strains, urinary tract infections, and sudden eye emergencies. Individuals who require more extensive care are seamlessly referred to other specialists or facilities across the Mount Sinai Health System, including its hospital emergency departments.
The Urgent Care clinical team is closely integrated with NYEE’s Eye Clinic, allowing patients with urgent and emergent eye conditions that require immediate attention to receive specialty care any time of the day or night. “Mount Sinai-Urgent Care is a great example of how we’re listening to the needs of the community by offering a service that people told us was critically needed,” notes James C. Tsai, MD, MBA, President of NYEE. “We’re now one of a few centers nationwide able to provide this level of eye triage and urgent care
Today, patients have more choices than ever and we’re here to help them design their vision to fit their lifestyle.
Kira Manusis, MD
at virtually all hours. Our subspecialists are always on call and now accessible after regular hours through the Urgent Care center.”
Mount Sinai-Adult Primary Care
In another effort to ensure community access to quality-based medical care—particularly for those underserved—Mount Sinai-Adult Primary Care (formerly General Medicine Associates) relocated its internal medicine specialists to NYEE’s downtown campus in April.
The resident-run program, originally housed at the nowclosed Mount Sinai Beth Israel hospital, will continue to help patients manage and treat chronic illnesses and maintain healthy lifestyles from its new home at NYEE. The co-location of Adult Primary Care with the NYEE ophthalmology clinics will also help our efforts to ensure that all NYEE patients have an established primary care provider. A key step in early detection and management of diseases, this effort bridges the current gap with a new referral pathway for eye clinic patients to general medicine physicians and clinics on-site—a welcome addition to the medical practices at Mount Sinai-Union Square and throughout the Health System.
Painting a Clearer Picture of Blood Flow Dynamics With Doppler Holography
As science has begun to demonstrate, measuring retinal and choroidal blood flow to the eye can provide extraordinary clues not only to ocular diseases like glaucoma, but to systemic abnormalities that include diabetes and cardiovascular, sickle cell, and Alzheimer’s diseases. The hitch is that measuring localized blood perfusion has for years presented a real challenge, with no device providing the level of precision scientists and clinicians need.
That could soon be changing thanks to new technology known as Doppler holography, which New York Eye and Ear Infirmary of Mount Sinai (NYEE) is clinically developing in partnership with a handful of research centers around the world. Over the past year, NYEE has assembled a Doppler holography imaging system on-site and started using it to acquire data from patients that will be pivotal to seminal studies of the sophisticated technology now getting underway. Helping to propel the work is a $100,000 grant from the New York Eye and Ear Infirmary Research Foundation.
“We’ve been getting very exciting images from Doppler holography thanks to its ability to accurately measure total flow of blood into and out of the optic nerve,” says Richard B. Rosen, MD, FARVO, Vice Chair of Ophthalmic Research at NYEE, who is spearheading the hospital’s research in this field. “It will provide us with an important metric for diagnosing many diseases by offering clues about a variety of perfusion deficits to the eye that are characteristic of conditions like glaucoma and retinal vascular diseases. We are particularly interested in using the technology to detect early changes that occur in our patients with diabetes and sickle cell disease.”
Dr. Rosen, who is also the Belinda Bingham Pierce and Gerald G. Pierce, MD, Distinguished Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, has looked at many different approaches
to measuring blood flow in the retina over the years, including scanning laser ophthalmoscopy, stroboscopic fundus angiography, and most recently OCT Doppler imaging. The latest device being tested is a noninvasive holographic imaging technique fixed to a chin rest, like a slit lamp. However, unlike handheld Doppler ultrasound, it is more repeatable and less operator-dependent, producing whole-volume images of blood flow with the ability to focus on specific vessels within the retina. The system is powered by highperformance software that is consistently updated by the creator of Doppler holography—research investigator Michael Atlan, PhD, at the Institut Langevin Ondes et Images in Paris.
NYEE is now part of a global collaboration with Dr. Atlan and academic research centers in Europe, as well as a second U.S. site at the University of Pittsburgh, to clinically test the Doppler microscopy system. “We will all benefit from sharing our findings among the research partners,” acknowledges Dr. Rosen. “Our role now is to determine how we can best use Doppler holography to enhance patient care. To that end, we have been collecting normative data from healthy subjects in the lab and are now expanding our studies to patients with clinical problems.”
In addition to Dr. Rosen, Alon Harris, MS, PhD, FARVO, Professor of Ophthalmology, and Artificial Intelligence and Human Health and Co-Director of the Barry Family Center for Ophthalmic Artificial Intelligence and Human Health at the Icahn School of Medicine, will figure prominently in the unfolding investigation into Doppler holography. The project is a perfect fit for Dr. Harris, who has focused his 25-year research career on the relationship between glaucoma prevalence and progression and vascular abnormalities. Dr. Harris is one of the pioneers worldwide to apply an ultrasound device called color Doppler imaging to measure blood flow dynamics in the human eye.
Holographic Doppler Imaging
Doppler imaging provides detailed, real-time information about blood flow dynamics within the microvasculature of the eye, including retinal blood flow and arterial resistivity index. The below examples in a healthy control show the impact of intraocular pressure on retinal perfusion.
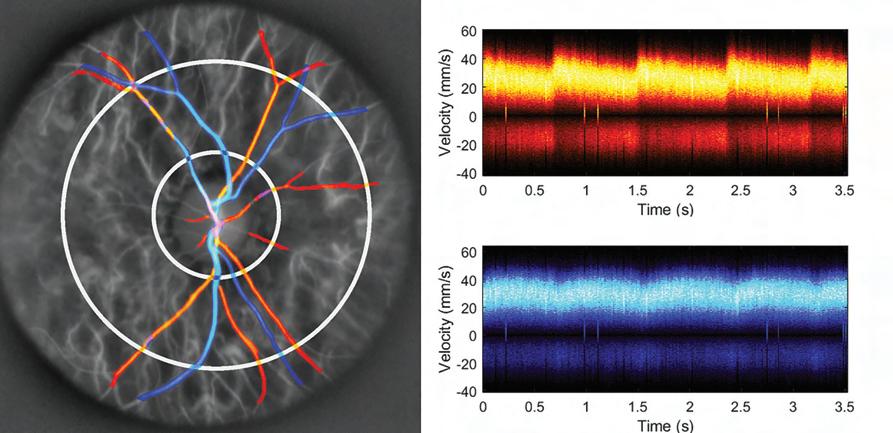
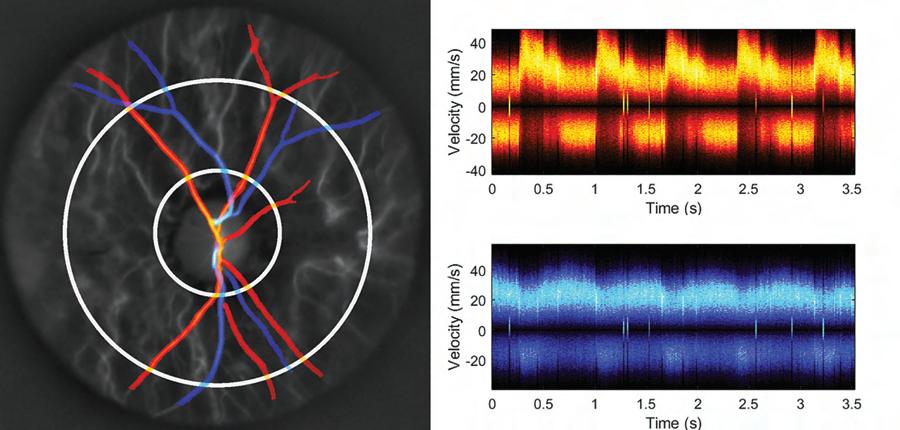
“Doppler holography could be useful in detecting many vascular-related diseases, and help identify their potential risk to patients,” says Dr. Harris. “It has many potential applications within the expanding field of oculomics, where we’re using powerful imaging techniques along with machine learning to identify the early presence of systemic pathologies including cardiovascular disease, hypertension, and diabetes.”
Dr. Rosen is equally bullish on the vast potential of Doppler holography. “We believe it could become an important tool for ophthalmologists, cardiologists, and other physicians in a couple of years,” he predicts. “By combining advanced optical imaging and computing, it will allow us to detect a wide range of diseases earlier in order to improve longterm outcomes.”
Healthy control, with normal intraocular pressure
Arterial
Venous
Same healthy control, exhibiting digitally elevated intraocular pressure
Arterial
Venous
A Postcard From Jamaica
As ophthalmology plays an increasingly important role in public health programs around the world, residents at New York Eye and Ear Infirmary of Mount Sinai (NYEE) are eagerly stepping up as ambassadors.
Two second-year residents are traveling to Jamaica in 2025 as part of a new Ophthalmic Global Health Program designed to help citizens—in countries with few ophthalmic specialists— address serious issues like cataracts, glaucoma, and chronic vision loss while advancing their own education.
“Many of the people we helped hadn’t been able to see for months or even years, and they had no idea what their underlying conditions were,” says Michael Lai, MD, who spent a week in Jamaica in November 2024 as the program’s first resident, examining some 70 patients a day in a makeshift clinic tucked inside a local church. “Giving them care on the spot and providing guidance on how to follow up was very meaningful.”
Harsha S. Reddy, MD, Associate Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, and Director of the Ophthalmology Residency Program at NYEE, is a stalwart believer in global service by doctors and was an animating force behind creation of the Ophthalmic Global Health Program. “As a residency program, we wanted to ensure we were offering a strong educational experience in other countries, and that we were selecting trainees for the program who could support our mission of providing the best possible care in a culturally compassionate way,” says Dr. Reddy, an oculoplastic surgeon who has donated his time over the years to working in countries as far-flung as India, Nepal, Rwanda, and Ethiopia.
Dr. Lai was more than equal to the task. As a second-year resident, he was used to treating a very diverse community of patients, many of them immigrants, at NYEE’s walk-in Eye Clinic in downtown Manhattan and NYC Health + Hospitals/ Elmhurst, an affiliate teaching institution in Queens.
“A lot of our patients present with advanced pathologies due to their lack of continuity of care,” he explains. “I found similar
advanced pathology in Jamaica, and my visit was an opportunity to bring what I had learned at our own clinic to patients in another country. It was also the chance to gain a better appreciation for the different cultures and backgrounds of people we treat, which is critical to ensuring them the best outcomes.”
Upon arriving in Jamaica on a Sunday, Dr. Lai was immediately swept up in preparations for the weeklong ophthalmology clinic, which included moving furniture and setting up his own private space for full ocular examinations of patients with a desk-mounted slit lamp in a tiny corner of the church. Around him was a team of nearly 30 optometrists, opticians, and nurses, all part of Great Shape! Inc., a charitable nonprofit organization empowering the children and families of Jamaica and the Caribbean by providing access to education and health care. The group worked closely with a local eye hospital and ophthalmologist to expand services. Team members funneled patients whose vision could not be refracted to better than 20/40 after an initial visual acuity screening at the clinic to Dr. Lai.
“People looked to me for guidance, particularly the optometrists, and it could get pretty chaotic at times,” Dr. Lai acknowledges. “I saw a lot of patients with retinal diseases like retinal detachment, diabetic retinopathy, and macular degeneration, and we referred them to a local retina specialist. We also handed out a lot of eye drops to a population known to have a high rate of glaucoma.”
One woman complaining of sharp eye pain was diagnosed by Dr. Lai with optic neuritis and urged to go to the local hospital for imaging and specialized treatment. During two days of his visit, Dr. Lai was at Cornwall Regional Hospital, assisting the ophthalmologist on duty, Dr. Charmaine Scarlett, with panretinal photocoagulation laser procedures.
On Dr. Lai’s agenda was another task outside the usual domain of providing patient care. Working with

Alexander Pinhas, MD, and Dr. Reddy, he initiated a smallscale research project based on the pathologies he observed over his weeklong tour to highlight areas in greatest need of specialized ophthalmic care within the community.
The goal is to track this information longitudinally with the support of other residents in the future to help Jamaican health authorities allocate resources in the most effective way. Dr. Lai has provided the project with a strong launchpad, compiling the detailed information he gathered into a poster that was presented at the recent annual meeting of the Association for Research in Vision and Ophthalmology.
“Understanding the breadth of pathology in any country is a different way of seeing the big picture, and that’s one of the things we hope to accomplish with our Ophthalmic Global Health Program,” emphasizes Dr. Reddy, who hopes to eventually double the number of participants.
“We want to track information about the kinds of eye disease that exist within communities and use it as the basis for long-term relationships with those countries where our residents are both learning from local collaborators and providing valuable support.”
NYEE’s Longest-Serving Voluntary Faculty Member Embarks Upon a New Teaching Project at Age 99
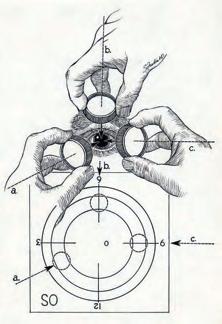
Seymour Fradin, MD, knows a good opportunity when he sees one. When the COVID-19 pandemic forced him to suspend his longstanding voluntary teaching faculty duties at The Bendheim Family Retina Center at New York Eye and Ear Infirmary of Mount Sinai (NYEE), Dr. Fradin did what anyone else in their mid-nineties and with a lot of time suddenly on their hands would have done: He decided to write a medical handbook.
The book is a compendium of lectures and tutorials he has given on performing fundus examinations on patients with the indirect ophthalmoscope, among the most challenging diagnostic techniques young ophthalmologists are asked to master. Rounding out the edifying prose are sprightly illustrations throughout the book, also the handiwork of Dr. Fradin, a brilliant retina specialist and accomplished medical artist who graduated from the Johns Hopkins University Department of Art before becoming, in 1959, the third clinical fellow (and later associate director) of NYEE’s Retina Service.
Richard B. Rosen, MD, FARVO, the current Chief of the Retina Service for the Mount Sinai Health System, has been a student, mentee, colleague, friend, and collaborator of Dr. Fradin over the years. As he so aptly put it in the book’s preface: “His own experience as a World War II veteran, engineer, aviator, scientist, medical artist, retinal surgeon, and teacher has provided him with a rare combination of perspectives into the optics, mechanics, medical science, and bedside manner that few enjoy.”
Dr. Fradin retired in 1996 but never left NYEE. He has continued to instruct first-year residents and fellows to this day, earning the distinction of being the longest-serving voluntary teaching faculty member in NYEE’s history. This dedication to teaching has been a hallmark of many voluntary teaching faculty members at NYEE who believe in the mission to integrate education, research, and clinical care into trainees’ teaching curriculum.
Still active, perceptive, and productive at age 99, Dr. Fradin
takes exception to the prevailing view of indirect ophthalmoscopy as a difficult discipline to learn. “People make it into such a difficult thing when anyone can really master it if you’re given the essential steps to follow,” he is quick to observe. “That’s why I wrote this book and called it ‘The Essential Guide.’”
Available for purchase on Amazon, the handbook has also been given to graduating fellows. The project is actually an extension of a prior collaboration between Dr. Fradin and Dr. Rosen that resulted in the 1997 release of the first digital ophthalmoscopy simulation, “Techniques of Indirect Ophthalmoscopy and Fundus Drawing,” a highly animated and fully interactive learning tool that can be accessed by trainees from a web browser or a mobile device app. It was incorporated into the American Academy of Ophthalmology’s ONE® Network, a global platform for ophthalmic education.
“He really wanted to keep the learning process as simple as possible for the effective training of residents and fellows,” acknowledges Dr. Rosen. “It just shows how young, agile, and even playful his mind has remained over the years. He’s always thinking outside the box, always inventing new things. He’s been a great role model for me.”
Dr. Fradin began cultivating his own love for ophthalmic medicine—and the retina in particular— nearly 70 years ago. His teacher was his childhood friend, Morton Rosenthal, MD, a highly esteemed authority in the field of retinal surgery who founded and was director of the New York metropolitan area’s first retinal service at NYEE in 1960. Dr. Fradin followed in his mentor’s very large footsteps, serving as associate director of the service from 1963 to 1968. From 1970 until his retirement in 1996, he maintained a busy private retinal practice on Park Avenue while volunteering countless hours teaching the next generation of ophthalmologists at NYEE.

A practical guide to mastering indirect ophthalmoscopy and fundus exams, featuring Dr. Fradin’s medical illustrations, step-by-step techniques, and clinical insights for students, trainees, and eye specialists

From his extraordinary vantage point, Dr. Fradin is more than eager to comment on the seismic change ophthalmology has undergone since he took up the craft.
“Above all, it’s become more technical—we do things today that were unheard of back then,” he says. And ophthalmic imaging, he continues, is the linchpin of that transformation.
From right to left: Seymour Fradin, MD, and Richard B. Rosen, MD, standing in front of the portrait of Thomas O. Muldoon, MD. A vitreoretinal surgeon, Dr. Muldoon trained under Dr. Fradin, becoming the Surgeon Director of the RetinaVitreous Service at NYEE. Under his leadership, The Bendheim Family Retina Center attained international and national renown as a leading center for medical and surgical management of complex retina diseases.

Illustration of a giant meridional fold with operculated hole
Hand and lens positioning during a fundus exam using a quadratic approach and a fundus drawing
“Remember, the eye is part of the brain, and if you look into the eye, you can learn about the basis for many diseases, no matter where they are in the human body,” he says.
“You can see the changes that occur, make diagnoses, and track the progress of the disease. For those reasons, I think ophthalmology will become in the years ahead an important diagnosis tool for all of medicine.”
AI Is Opening a Powerful New Window on Predicting Glaucoma Through Vascular Risk
Structural damage to the retina and optic nerve has long been the standard by which primary open-angle glaucoma (POAG) is diagnosed. But time has shown it to be an imperfect measurement that presents a sizable barrier to providing precision care to patients.
Alon Harris, MS, PhD, FARVO, Professor of Ophthalmology, and Artificial Intelligence and Human Health at the Icahn School of Medicine at Mount Sinai, has spent much of his career studying the impact of vascular and cardiovascular risk factors on the development and progression of glaucoma. A new study he helped pilot combines optical coherence tomography angiography (OCTA) and artificial intelligence (AI) to offer the strongest evidence yet for considering both vascular and structural variables in characterizing and assessing POAG risk in humans.
The novel study used neural network machine learning models trained on specific datasets to identify biomarkers that could prove most useful in understanding the etiology of the disease for which no gold standard, especially in its earliest stages, currently exists. Above all, the team learned that OCTA vascular parameters were equal to or better than OCT-assessed structural endpoints, including retinal nerve fiber layer, ganglion cell complex, and macular thickness for predicting risk for early-stage glaucoma.
“OCT structural measures, including retinal nerve fiber layer and ganglion cell complex thickness, have long been used for diagnosing and characterizing glaucoma, but our paper shows that OCTA vascular parameters may have the same diagnostic strength, and should therefore be actively investigated,” explains Dr. Harris, co-author of the study and Co-Director of the Barry Family Center for Ophthalmic Artificial Intelligence and Human Health at the Icahn School of Medicine. “Our data also suggest that POAG predictability may not only be enhanced through OCTA-identified biomarkers, but that these could be highly informative to clinicians at the earliest stages of the disease, before significant visual field loss occurs.”
The New York Eye and Ear Infirmary of Mount Sinai (NYEE) study, published in the September 2024 issue of Investigative Ophthalmology & Visual Science , used small artificial neural network models, also known as multi-layer perceptrons, that were trained on datasets comprising 144 POAG patient eyes and 149 controls without eye disease. The analysis showed that AI models trained with OCTA measurements performed similarly to models that used OCT structural markers for diagnosis. Interestingly, combining OCT and OCTA measurements into one model did not improve the results, suggesting to the team that both imaging modalities provide similar information about glaucoma through different formats.
According to lead author Nicholas Riina, a medical student for the past two years in Dr. Harris’s lab, the observational study was particularly successful in using AI and minimally invasive OCTA to explore where few researchers had been before: the hemodynamics, or blood flow, within the microvasculature of the eye. “Leveraging these technologies gave us a highresolution window on hemodynamic factors of the eye, such as changes to blood vessel density in the retina, allowing us to compare them to the more established structural parameters gathered through OCT,” Mr. Riina says.
The goal, Mr. Riina emphasizes, is to continue to train machine learning algorithms on larger and larger datasets that cross ethnic and population borders. That pursuit is well underway at NYEE through collaborations with other research centers around the world.
“We’re working toward developing an algorithm that could be combined with OCTA to enable clinicians to accurately diagnose patients for glaucoma right at their practices,” he notes. “We’re not quite there yet, but this could potentially be a game changer by opening the door to much earlier interventions and more tailored therapeutic approaches to patient care for glaucoma.”
From the Bench: Impact Publications
Each year, our vision researchers break new ground in our understanding of ocular diseases. Laboratory research highlights of note are:
Yu M, Hwang HH, Roberts AL, Koenen KC, Wiggs JL, Pasquale LR, Kang JH. Childhood or adolescent abuse and primary open-angle glaucoma in a longitudinal cohort of women. Eye (London). 2025 Apr 10. doi: 10.1038/s41433-02503785-3. Epub ahead of print. PMID: 40211014.
In the Nurses’ Health Study, there was positive association between early sexual abuse and primary open-angle glaucoma, particularly for participants who subsequently developed early paracentral visual field loss.
Hu DN, Zhang R, Iacob CE, Yao A, Yang SF, Chan CC, Rosen RB. Constitutive and hypoxiainduced VEGF production by cultured uveal melanocytes and retinal pigment epithelial cells. Exp Eye Res. 2025 May;254:110318. doi: 10.1016/j.exer.2025.110318. Epub 2025 Mar 1. PMID: 40032151.
Retinal pigment epithelial (RPE) cells constitutively produce more VEGF than uveal melanocytes (UM). However, UM respond more robustly to high hypoxia or chemical hypoxic stimulation. RPE cells are crucial for normal VEGF production, but UM may contribute to the pathological increase in VEGF under severe ocular hypoxia.
Otero-Marquez O, Haq A, Muncharaz Duran L, Bellis J, McCuskee S, Ahsanuddin S, Rosen RB, Glassberg J, Chui TYP. Preferential sites of retinal capillary occlusion in sickle cell disease. Invest Ophthalmol Vis Sci. 2025 Jan 2;66(1):57. doi: 10.1167/iovs.66.1.57. PMID: 39854010; PMCID: PMC11760755.
Optical coherence tomography angiography (OCTA) scans from 107 patients with sickle cell disease (SCD) and 51 controls were obtained using spectral-domain OCT. This study suggests that the periarteriolar aspect of the vascular bed is the preferential site of retinal capillary occlusion in patients with SCD, with more involvement of the temporal aspect of the parafovea.
Govindaiah A, Bhuiyan T, Smith RT, Dhamoon MS, Bhuiyan A. A machine learning prediction model to identify individuals at risk of fiveyear incident stroke based on retinal imaging. Sensors (Basel). 2025 Mar 19;25(6):1917. doi: 10.3390/s25061917. PMID: 40293071; PMCID: PMC11946667.
Drs. Smith and Bhuiyan developed and validated a stroke prediction model that incorporates retinal images in a multi-ethnic dataset.
Makovoz B, Eriksen AZ, Warrington RE, Williams D, Blenkinsop TA. Neuroectoderm-derived iris muscle characterization at the singlecell resolution in native human iris and a pluripotent stem cell eye model. Nat Comm. 2025, in press.
The signals that govern how the various cells in the iris (which contains heterogeneous cell types) develop from the neuroectoderm are not well understood. Dr. Blenkinsop and his team identified a gene signature that serves as the blueprint for iris development. Understanding this signature will help explain iris alterations in various ocular diseases.
Department of Ophthalmology at a Glance
New York Eye and Ear Infirmary of Mount Sinai (NYEE) and The Mount Sinai Hospital (MSH)/ Icahn School of Medicine at Mount Sinai
Combined 2024 numbers for NYEE and MSH
NYEE-East 102nd Street 17 East 102nd Street New York, NY 10029
NYEE-East 85th Street 234 East 85th Street New York, NY 10028
NYEE-Tribeca 77 Worth Street New York, NY 10013
NYEE-Midwood 1630
Street
NY 10010
Avenue
11102
FACULTY NEWS: AWARDS
AND HONORS, SEPTEMBER 2024-2025
Varun Kumar, PhD, Assistant Professor of Ophthalmology, and Pharmacological Sciences, was accepted to the National Alliance for Eye and Vision Research, 2025 Emerging Vision Scientist Program. A Capitol Hill fixture for a decade, the program strengthens the connection between emerging vision scientists and policymakers. During the two-day program, that took place in September in Washington, participants presented their cutting-edge research and educated members of Congress and staff about the importance of vision research.
Alon Harris, MS, PhD, FARVO, Co-Director of the Barry Family Center for Ophthalmic Artificial Intelligence and Human Health, was honored with The Glaucoma Foundation’s Robert Ritch Award for Innovation and Excellence in Glaucoma, June 2025, New York City. The award honors exceptional individuals who have made significant and lasting contributions to the science and medicine of glaucoma.
Richard B. Rosen, MD, FARVO, the Belinda Bingham Pierce and Gerald G. Pierce, MD, Distinguished Professor of Ophthalmology, presented the inaugural Peter Reed Pavan Lecture to the University of South Florida (USF) Department of Ophthalmology in May 2025. The lectureship, established in 2024 by an anonymous donor, honors the remarkable service and enduring legacy of Peter Reed Pavan, MD, a vitreoretinal specialist and professor emeritus of ophthalmology at USF Health, and celebrates his legacy of clinical excellence, research innovation, and educational leadership.
James C. Tsai, MD, President of NYEE and Chair of the Department of Ophthalmology at the Mount Sinai Health System, was appointed PresidentElect of the Association of University Professors of Ophthalmology (AUPO), April 2025, San Francisco. Considered the voice of academic ophthalmology, the mission of AUPO is to promote ophthalmology research, education, and patient care.
Dr. Tsai was also recognized with the Jacobi Medallion from the Mount Sinai Health System, March 2025, New York City. This prestigious award honors members of the Mount Sinai community who,
through long-term service, have made exceptional contributions to the fields of clinical medicine or biomedical research, or have exemplified extraordinary dedication to Mount Sinai.
Jost B. Jonas, MD, FARVO, Adjunct Professor at the Icahn School of Medicine at Mount Sinai and Chair of the Department of Ophthalmology at Ruprecht Karl University of Heidelberg in Germany, received the Kupfer Award from the Association for Research in Vision and Ophthalmology, May 2025, Salt Lake City. The award honors those who have demonstrated distinguished public service with national or global impact, on behalf of eye and vision research.
Tsontcho A. Ianchulev, MD, MPH, Director of Ophthalmic Innovation and Technology at NYEE, was a recipient of the Catalyst Award at the Glaucoma 360 Gala, February 2025, San Francisco. The annual event celebrates the scientists, advisors, donors, and volunteers who work together to advance the field of glaucoma and bring us closer to curing glaucoma and restoring vision.
Nisha Chadha, MD, Director of Medical Student Education in the Department of Ophthalmology, was recognized with the Women in Ophthalmology (WIO) Emerging Leader Award at a reception held during the American Academy of Ophthalmology, October 2024, Chicago. The award recognizes individuals who have made significant contributions to WIO and/or to the profession and who have demonstrated the potential for leadership and continuing service.
Avnish Deobhakta, MD, Associate Professor of Ophthalmology, won first prize in the Winning Pitch Challenge at Eyecelerator, held during the American Academy of Ophthalmology Annual Meeting, October 2024, Chicago. The Winning Pitch challenge offers ophthalmologists the opportunity to solve unmet needs in eye care through innovation, and a chance to compete for cash prizes in a Shark Tank–style competition.
FACULTY NEWS: RECRUITS





Douglas R. Fredrick, MD
The Department is excited to welcome back Dr. Fredrick. An academic leader with an international reputation in the treatment of complex strabismus, pediatric cataracts, cortical visual impairment, and modalities to slow the progression of childhood myopia, Dr. Fredrick rejoins the Department of Ophthalmology as System Chief of Pediatric Ophthalmology. He will also serve as Senior Associate Dean for Graduate Medical Education, and an Associate Designated Institutional Official for the Icahn School of Medicine at Mount Sinai. Prior to rejoining NYEE, he held a faculty post at Kaiser Permanente South San Francisco Medical Center, and a Clinical Professorship in the Department of Ophthalmology, University of California, San Francisco. Dr. Fredrick served as NYEE’s Deputy Chair for Education and System Chief of Pediatric Ophthalmology from 2018 to 2021.
Jiani S. Lin, OD
Dr. Lin joins NYEE as an Instructor, Department of Ophthalmology, Division of Optometry. She earned her Doctor of Optometry from Illinois College of Optometry, Chicago, and completed her residency in ocular disease and cornea and contact lens at Massachusetts Eye and Ear Infirmary, Boston. She has been recognized by her peers with the 2023 Cribb Leadership and Service Award, and in 2024, with the E. Richard Tennant Memorial Scholarship and the Cooper Vision 4th Year Contact Lens Clinical Excellence Award.
Anne Marie Mc Veigh, MD
A board certified comprehensive ophthalmologist, Dr. Mc Veigh joins the Department of Ophthalmology at NYEE as an Assistant Professor of Ophthalmology. Dr. Mc Veigh has been part of the Mount Sinai Health System since 2022 as an Assistant Professor of Ophthalmology and an Ophthalmology Attending at the Mount Sinai Doctors-West 23rd Street multispecialty practice. She received her medical degree from New York Medical College in Valhalla, NY, followed by an ophthalmology residency at St. Vincent’s Hospital and Medical Center of New York.
Nehali Nanti, MD
A fellowship-trained glaucoma specialist, Dr. Nanti earned her medical degree from Rutgers New Jersey Medical School, Newark, NJ, and completed her ophthalmology residency at SUNY Stony Brook University, Stony Brook, NY, where she served as chief resident at the Northport Veterans Affairs Medical Center. She then pursued a glaucoma fellowship at Manhattan Eye, Ear & Throat Hospital, New York City. A co-author of scientific papers and posters, Dr. Nanti is a vision researcher and presents her work at national conferences.
Kevin Y. Yan, MD
A board certified neurologist, Dr. Yan joins Mount Sinai as an Assistant Professor of Neurology, with secondary appointments in Ophthalmology and Neurosurgery. His clinical focus will be diagnosing and treating neuro-ophthalmologic conditions like optic neuropathy, optic neuritis, and abnormal vision. Dr. Yan received his medical degree from the University of Massachusetts Medical School, Worcester, MA, followed by a residency at Yale University School of Medicine, New Haven, CT, where he served as chief neurology resident. He completed his fellowship in neuro-ophthalmology at Emory University School of Medicine, Atlanta.
FACULTY LISTING
NYEE RESIDENTS
PGY-4
Jennifer Drechsler, MD
Jose Omar Garcia, MD
Catalina Garzon Vargas, MD
Andy Huang, MD
Claire Kim, MD
Michael Lai, MD
Oscar Otero, MD
Yash Shah, MD
Benjamin Steren, MD
Amanda Wong, MD
PGY-3
Aileen Arevalo, MD
Xiaoyu Cai, MD
Emily Duffner, MD
Jeff Huang, MD
Angela Kim, MD
Eliott Kim, MD
Sophia Lam, MD
Marissa Patel, MD
Jose Quiroz, MD
Dominic Williams, MD
PGY-2
Evan Bilsbury, MD
Spandana Jarmale, MD
Grace Lee, MD
Andy Medina, MD
Nicholas Moehringer, MD
David Qi, MD
Joshua Reyes, MD
Sagar Shah, MD
Liang Wang, MD
Stephanie Ying, MD
NYEE FELLOWS
Ahmad Abdel-Aty, MD
Aaron Brown, MD
Devin Cohen, MD
Gal Cohen, MD
Kevin Dahlan, MD
Neha Gupta, MD
Kimberly Jun, MD
ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI DEPARTMENTAL LEADERSHIP
James C. Tsai, MD, MBA
President, NYEE
Chair, Department of Ophthalmology
Director, BFCOAIHH
Icahn School of Medicine and MSHS
Louis R. Pasquale, MD, FARVO
Chair, Department of Ophthalmology
MSH and MSQ
Deputy Chair for Research Director, Mount Sinai/NYEE Eye and Vision Research Institute
Co-Director, BFCOAIHH
Icahn School of Medicine
Paul A. Sidoti, MD
Chair, Department of Ophthalmology
NYEE
Deputy Chair for Education Department of Ophthalmology
Icahn School of Medicine
Chief, Glaucoma Service, MSHS
Richard B. Rosen, MD, FARVO
Vice Chair of Ophthalmic Research, NYEE
Chief, Retina Service, MSHS
Douglas R. Fredrick, MD
Chief, Pediatric Ophthalmology Service, MSHS
Senior Associate Dean for Graduate Medical Education and Associate Designated Institutional Official Icahn School of Medicine
Salvatore Loiacono Jr., MPA
Deputy Chair, Finance and Administration, MSHS
Vice President, Ophthalmology Services, NYEE
Elizabeth Sellman
President and Chief Operating Officer
Mount Sinai Downtown
Tamiesha Frempong, MD, MPH
Vice Chair, Faculty Engagement
Department of Ophthalmology
Icahn School of Medicine
Sandra K. Masur, PhD
Vice Chair, Academic Development and Mentoring, Department of Ophthalmology
Icahn School of Medicine
Anita Gupta, MD
Vice Chair, Professional Development
Department of Ophthalmology
Icahn School of Medicine
Director, Cornea Service, NYEE
Alon Harris, MS, PhD, FARVO
Co-Director, BFCOAIHH
Director, Ophthalmic Vascular Diagnostic and Research Program, MSH
Vice Chair, International Research and Academic Affairs
Chair, Promotion and Tenure Committee Department of Ophthalmology
Icahn School of Medicine
Gareth M.C. Lema, MD, PhD
Vice Chair, Quality, Safety, and Experience Department of Ophthalmology, MSHS
Tak Yee Tania Tai, MD
Vice Chair, Clinical Operations Department of Ophthalmology, NYEE
Clinical Advisory Director, BFCOAIHH
Icahn School of Medicine
Director, Glaucoma Clinic, NYEE
Gennady Landa, MD
Vice Chair, Clinical Integration of Ophthalmology
Icahn School of Medicine and MSHS
Director, Retina Service, NYEE
Nisha Chadha, MD
Director, Medical Student Education Department of Ophthalmology
Icahn School of Medicine
Masako Chen, MD
Director, Comprehensive Ophthalmology Service, NYEE
Tsontcho A. Ianchulev, MD, MPH
Director, Ophthalmic Innovation and Technology, NYEE
FACULTY LISTING
RESIDENCY AND FELLOWSHIP
EDUCATION
CLINICAL DIVISIONS AT MOUNT SINAI HEALTH
SYSTEM FACULTY PRACTICES
Sumayya Ahmad, MD
Associate Director, Ophthalmology Residency Program, NYEE/ISMMS
Masako Chen, MD
Associate Director, Ophthalmology Residency Program, NYEE/ISMMS
Avnish Deobhakta, MD Director, Medical Retina Fellowship Program
Associate Director, Vitreo-Retinal Fellowship Program NYEE/ISMMS
Tamiesha Frempong, MD, MPH Assistant Director, Ophthalmology Residency Program, NYEE/ISMMS
Meenakashi Gupta, MD Director, Resident and Fellow Wellness, Department of Ophthalmology, NYEE/ISMMS
Alon Harris, MS, PhD, FARVO Co-Director, Ophthalmic AI Clinical and Research Fellowship, NYEE/ISMMS
Gautam Kamthan, MD
Assistant Director, Ophthalmic Innovation and Technology, NYEE Associate Director, Cataract Surgical Training, NYEE/ISMMS
Gennady Landa, MD
Associate Director, Vitreo-Retinal Fellowship Program, NYEE/ISMMS
Louis R. Pasquale, MD, FARVO Co-Director, Ophthalmic AI Clinical and Research Fellowship, NYEE/ISMMS
Harsha S. Reddy, MD Director, Ophthalmology Residency Program NYEE/ISMMS
Richard B. Rosen, MD, FARVO Director, Vitreo-Retinal Fellowship Program NYEE/ISMMS
Tak Yee Tania Tai, MD Director, Microsurgical Education Co-Director, Ophthalmic AI Clinical and Research Fellowship, NYEE/ISMMS
Kateki Vinod, MD Director, Glaucoma Fellowship Program, NYEE/ISMMS
Angie E. Wen, MD Director, Cornea and External Diseases Fellowship Program, NYEE/ISMMS
Cataract Surgery
Richard Koplin, MD Co-Director, Cataract Service NYEE
Kira Manusis, MD
Director, Center for Refractive Solutions
Co-Director, Cataract Service NYEE
Sumayya Ahmad, MD
Yandong Bian, MD
Nisha Chadha, MD
Masako Chen, MD
Anita Gupta, MD
Tsontcho A. Ianchulev, MD, MPH
Gennady Landa, MD
Tak Yee Tania Tai, MD
Angie E. Wen, MD
Cornea, External Diseases, and Refractive Surgery
Anita Gupta, MD Director, Cornea Service NYEE
Angie E. Wen, MD Director, Keratorefractive Surgery Division, NYEE
Sumayya Ahmad, MD
Yandong Bian, MD
Masako Chen, MD
Kira Manusis, MD
Eye Trauma
Ronald C. Gentile, MD
Director, Posterior Segment Trauma Service, NYEE
Harsha S. Reddy, MD
Director, Oculoplastic Trauma Service, NYEE
Sumayya Ahmad, MD
Masako Chen, MD
Mary-Abigail Craven, MD
Avnish Deobhakta, MD
Alberto G. Distefano, MD
Valerie I. Elmalem, MD
Robin N. Ginsburg, MD
Anita Gupta, MD
Meenakashi Gupta, MD
Gennady Landa, MD
Gareth M.C. Lema, MD, PhD
Kira Manusis, MD
Richard B. Rosen, MD, FARVO
Angie E. Wen, MD
Glaucoma
Paul A. Sidoti, MD
Chief, Glaucoma Service MSHS
Tak Yee Tania Tai, MD
Director, Glaucoma Clinic NYEE
Nisha Chadha, MD
Donna Gagliuso, MD
Tsontcho A. Ianchulev, MD, MPH
Paul S. Lee, MD
Nehali Nanti, MD
Louis R. Pasquale, MD, FARVO
James C. Tsai, MD, MBA
Kateki Vinod, MD
Neuro-Ophthalmology
Rudrani Banik, MD Co-Director
Neuro-Ophthalmology Clinic NYEE
Valerie I. Elmalem, MD Co-Director
Neuro-Ophthalmology Clinic NYEE
Mary-Abigail Craven, MD
Alberto G. Distefano, MD
Kevin Y. Yan, MD
FACULTY LISTING
Ocular Oncology
Paul T. Finger, MD Director, Ocular Oncology Service, NYEE
Ekaterina Semenova, MD Director, Pediatric Ocular Oncology, NYEE/MSH
Ophthalmic Pathology
Jodi Sassoon, MD Chair, Pathology, NYEE
Codrin E. Iacob, MD, FCAP
Oculoplastic, Orbital, and Reconstructive Surgery
Alberto G. Distefano, MD
Director, Oculoplastic, Orbital, and Reconstructive Surgery, MSH
Harsha S. Reddy, MD Director, Oculoplastic, Orbital, and Reconstructive Surgery, NYEE
Mary-Abigail Craven, MD
Valerie I. Elmalem, MD
Pediatric Ophthalmology and Strabismus
Douglas R. Fredrick, MD
Chief, Pediatric Ophthalmology Service, MSHS
Tamiesha Frempong, MD, MPH
Thomas J. Quehl, MD
Edward Raab, MD
Primary Care Ophthalmology/Optometry
Masako Chen, MD
Director, Comprehensive Ophthalmology Service, NYEE
Vivien Boniuk, MD
Phillip Braun, MD
Kristina Creadore, OD
Lisa Kingsly, OD
Jiani S. Lin, OD
Anne Marie Mc Veigh, MD
Niki Mizraei, OD
Retina
Richard B. Rosen, MD, FARVO Chief, Retina Service, MSHS
Robin N. Ginsburg, MD Director, Retina Service, MSH
Gennady Landa, MD Director, Retina Service, NYEE
Nazanin Barzideh, MD
Avnish Deobhakta, MD
Meenakashi Gupta, MD
Gareth M.C. Lema, MD, PhD
R. Theodore Smith, MD, PhD
Uveitis and Ocular Immunology
Varun K. Pawar, MD
Basic Science/Translational Research Faculty
Louis R. Pasquale, MD, FARVO Director, Mount Sinai/NYEE Eye and Vision Research Institute Co-Director, BFCOAIHH
Icahn School of Medicine
Timothy A. Blenkinsop, PhD
Bo Chen, PhD
Yuen Ping Toco Chui, PhD
Alon Harris, MS, PhD, FARVO
Varun Kumar, PhD
Jun Lin, MD, PhD
Sandra Masur, PhD
Richard B. Rosen, MD, FARVO
R. Theodore Smith, MD, PhD
Affiliated Leadership
Douglas F. Buxton, MD
President, Jorge N. Buxton, MD, and Douglas F. Buxton, MD, Microsurgical Education Fund
Paul S. Lee, MD
Chief, Department of Ophthalmology
James J. Peters VA Medical Center
President, NYEE/MSH Department of Ophthalmology Alumni Association
Theodore Lyu, MD Director, Department of Ophthalmology
Elmhurst Hospital Center
Michelle K. Rhee, MD Associate Director Department of Ophthalmology
Elmhurst Hospital Center
Voluntary Teaching Faculty NYEE
Ahmed Abdelhady, MD
Steven Agemy, MD
Rudrani Banik, MD
Alexander Barash, MD
Alessandra Bertolucci, MD
Brett Bielory, MD
Douglas F. Buxton, MD
Gaurav Chandra, MD
Alan Dayan, MD
Jonathan Ellant, MD
Julia Fallon, MD
Elizabeth Fang, MD
Paul T. Finger, MD
John Flanagan, MD
Donald Fox, MD
Seymour Fradin, MD
Ronald C. Gentile, MD
Robyn Horowitz, MD
Jimmy Hu, MD
Lawrence Jacobson, MD
Steven Kane, MD
Yogita Kashyap, MD
Stephen Kronenberg, MD
Kaushal Kulkarni, MD
Jessica Lee, MD
Marc Lustig, MD
Palak Majmudar, MD
Kerline Marcelin, MD
Sarah McCord, MD
Jeffrey Nightingale, MD
Jai Parekh, MD
Deep Parikh, MD
Alexander Pinhas, MD
Aryeh Pollack, MD
Alexander Rabinovich, MD
Allen Rubin, MD
Edwin Schottenstein, MD
Jonathan Shapiro, MD
Ahmed Sheikh, MD
FACULTY LISTING
Alan Sheyman, MD
Glenn Silbert, MD
Marc Sirota, MD
Mark Tannenbaum, MD
Theresa Tretter, MD
Cynthia Tung, MD
Eugene Weise, MD
Rebecca Weiss, MD
David Witzel, MD
Sze Wong, MD
MSH
Ahmed Abdelhady, MD
Alexander Barash, MD
Ben Cohen, MD
Peter Condax, MD
Stella Douros, MD
Edward Marcus, MD
Joseph Podhorzer, MD
Ravi Raharkrishnan, MD
Ahmed Sheikh, MD
Alan Sheyman, MD
VA Medical Center
Isaac Ezon, MD
Hope Garner, MD
Chandak Ghosh, MD, MPH
Doris Herzfeld, MD
Paul S. Lee, MD
Theodore Lyu, MD
Jonathan Schulhof, MD
Steven Teich, MD
Elmhurst Hospital Center
Robert Fischer, MD
Laiyin Ma, MD
Richard Most, MD
Andrew Schwartz, MD
Kevin Wu, MD
BFCOAIHH
Barry Family Center for Ophthalmic
Artificial Intelligence and Human Health
Icahn School of Medicine/ISMMS
Icahn School of Medicine at Mount Sinai
MSHS
Mount Sinai Health System
MSH
The Mount Sinai Hospital
MSM
Mount Sinai Morningside
MSQ
Mount Sinai Queens
MSW
Mount Sinai West
NYEE
New York Eye and Ear Infirmary of Mount Sinai