Collaborative Healthcare in Northern Ireland: Delivering the services children need in the community
Published June 2025
Royal College of Paediatrics and Child Healt h Ireland
Leading the way in Children’s Healt h


Collaborative Healthcare in Northern Ireland: Delivering the services children need in the community
Published June 2025
Royal College of Paediatrics and Child Healt h Ireland
Leading the way in Children’s Healt h

As a Paediatrician, it worries me deeply that the HSC system does not currently appear capable of providing consistent timely health care for our children and young people in the community. Community Paediatricians and the teams they work with face unsustainable service delivery pressures. We must acknowledge the crucial role paediatric community services play and resource accordingly if we are to give this vulnerable cohort the childhood and future they deserve.
Long waiting lists to access care and subsequent lengthy delays for ongoing support and therapy are unacceptable for any patient, but for children and young people these delays can be catastrophic. Early intervention is key in most developmental conditions and has the biggest impact on improving educational outcomes, wellbeing and family life. If the right window to treat a child is missed or a child waits too long for treatment the consequences may endure for years or become irreversible. The impact of delays in care can be seen beyond child health; an individual’s social development, school attendance and future economic contribution can all be impacted and it can lead to future pressure on adult HSC services.
The demands on community paediatrics have increased significantly in recent times and services have responded and evolved to meet the needs of local populations and the requirements of strategic directives. However, these responses were, by necessity, highly dependent on the available workforce in individual Trusts and have led to variations in the provision of services, diagnostic pathways and interventions across NI. Organisationally, community paediatrics has aligned differently with secondary care and with social services as well as other community and primary care services. Given competing demands in these systems, the strategic development of community paediatrics has the potential to be overlooked. A strategic delivery must acknowledge the collaborative nature of community paediatrics and the individual interfaces and be commissioned in a way that supports delivering care in the right place at the right time.
Delivering care to scale regionally and closer to home has long been a NI Executive ambition, particularly since Prof. Bengoa’s Systems not Structures Report1 which made clear that shifting from hospital-based care to community-based care was the way forward. Large increases in waiting times are a grim yardstick indicating a failure to prioritise or develop child health services in the community. For instance, region-wide data shows that Outpatient community paediatric waiters in NI alone grew by 85.9% between September 2020 – September 2023.
The staff in the NHS are really nice and can be helpful and understanding. The fact its free and everyone gets the same baseline opportunity from the start is good. But the waiting lists and times are long, and the staff seem worn out.
RCPCH &Us Voice Bank, Northern Ireland 2025
Maintaining this trajectory will continue to have detrimental effect on children in the here and now, stifling their rights and potential as well as having a broader societal and economic impact. Indeed, the NHS Confederation found higher spend on primary and community care could have significantly increased economic outputs.2 It’s time to recognise that investment is urgently needed in children’s community services. The NI Executive must support the Department of Health to be able to direct Trusts, Area Integrated Partnership Boards (AIPBs) and partners to focus on providing early years intervention and support throughout children’s life-course via holistic needs-led services in the community. The draft Children’s and Young People’s Emotional Health and Wellbeing Framework (CYP EHW Framework)3 embodies an ambition to provide ‘community health’ more holistically. The iThrive approach to modelling and the neuro-affirmative approach to practice and delivery is an ideal. It is imperative that funding and coordination across systems enables the principles and objectives to be achieved.
Inequity in children’s services affects all areas of society - school performance, housing prices, social class, economic performance, mental health, adult offending, substance abuse and others…
Community Paediatrics in NI is chronically underfunded with each Trust area working with different pathways, different types of delivery.
RCPCH Members, Northern Ireland Survey (May 2025)
Community Child Health (CCH) is the largest paediatric sub-specialty focussing on the care of vulnerable children and families, children with long-term conditions and child public health. This includes children with:
• developmental disorders and disabilities,
• complex health needs (including end of life care)
• behavioural presentations of neurodevelopmental disorders (e.g. Autism, ADHD)
• safeguarding concerns, who are “Looked After” or being adopted.
Community paediatricians usually work in multidisciplinary teams and across agencies with therapists, nurses and colleagues from schools, social services, the voluntary sector and local authorities. They have a vital role in planning and implementing local strategies to improve the health of all children in their area including safeguarding policy, universal and targeted lifestyle programmes and tackling local social determinants of health. A number of statutory roles are also usually provided by community paediatricians relating to child protection and child deaths, looked after children and those with special educational needs and disability (SEND).
The nature and relative volumes of childhood illness have changed in recent decades with more mental health and neurodevelopmental disorders such as autism and ADHD being diagnosed, greater reporting and awareness of safeguarding issues and more emphasis on children in public care. These, together with additional statutory duties in recent years, have added to the volume and complexity of community paediatric roles.
The data sets in the figures below represent region-wide aggregated ‘outpatient community paediatric waiters in Northern Ireland’ waiting times between 2020 and 2023. This data was provided via Freedom of Information submission to the Department of Health requesting data held on all children and young people waiting to access a community paediatric service whether medically led, Allied Health professional (AHP) led or otherwise.
However, it should be noted that the lack of disaggregation or clarity on what the category ‘outpatient community paediatric waiter’ means, leaves space for ambiguity in estimates waiting for access to all children’s community health services. In April 2022 a NI Children’s Commissioner monitoring review estimated that approximately 34,278 children were waiting to access services with significant numbers noted in community paediatric medical services (regional total in 2022: 8014), speech and language therapy (regional total in 2022: 4574), orthoptics (regional total in 2022: 3086) dietetics (regional total in 2022: 2526) and occupational therapy (regional total in 2022: 2231).4 The data shown may be more indicative of a community paediatric medically led service as opposed to all services.
Nonetheless, a marked increase in waiting times volume may be observed between September 2020 and September 2023. A further notable increase may be seen in those waiting more than 104 weeks during the same period.
Nonetheless, a marked increase in waiting times volume may be observed between September 2020 and September 2023. A further notable increase may be seen in those waiting more than 104 weeks during the same period.
Outpatient community
paediatric waiters in NI
Sept 2020: 5397
Outpatient community paediatric waiters in Northern Ireland
Sept 2023: 10,035
5,397 10,035
Sept 2020 Sept 2023
Outpatient community paediatric waiters in NI waiting >104 weeks
Sept 2020: 676
Outpatient community paediatric waiters in Northern Ireland >104 weeks
Sept 2023: 2,223
676 2,223
Sept 2020 Sept 2023
In anticipation of datasets from all HSC Trusts in NI post-digitisation departmental quarterly reporting, we looked to Table 1 as an indication of numbers waiting in 2024 Given the combined total of 10,035 across all of NI in 2023, a sum of 2097 community waiters in one, albeit the largest Trust, remains worrying.
In anticipation of datasets from all HSC Trusts in NI post-digitisation departmental quarterly reporting, we looked to Table 1 as an indication of numbers waiting in 2024. Given the combined total of 10,035 across all of NI in 2023, a sum of 2097 community waiters in one, albeit the largest Trust, remains worrying.
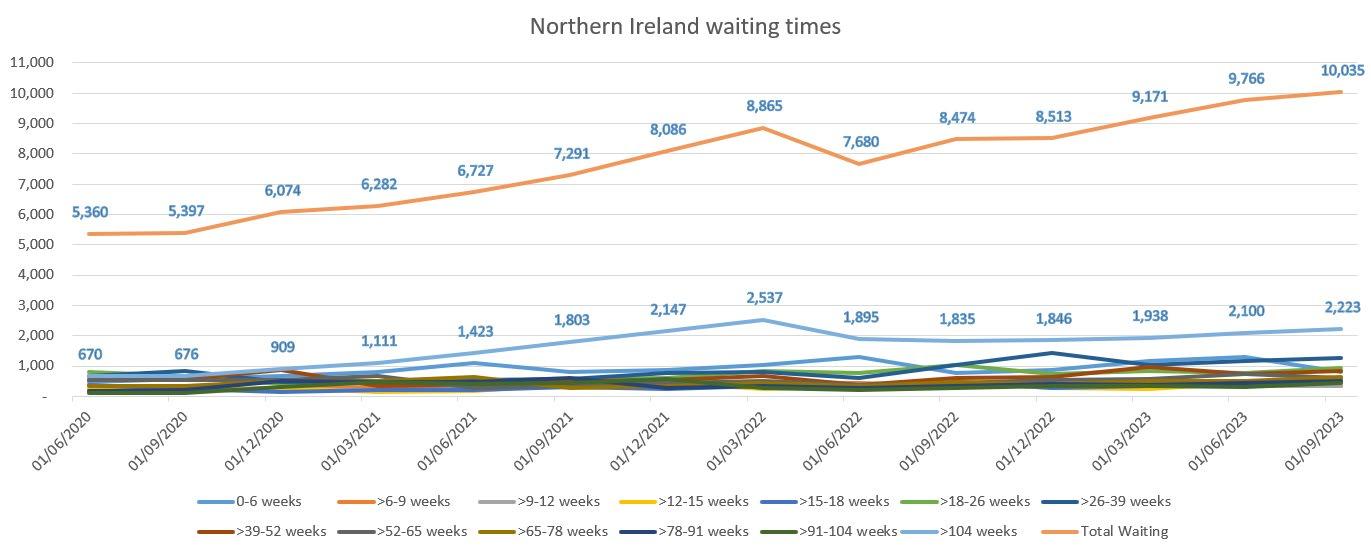
Figure 1: ‘Outpatient Community Paediatrics’ waiting times in NI as [cohorts as published in official statistics] produced from Department of Health FoI – March 2025
Figure 1: ‘Outpatient Community Paediatrics’ waiting times in NI as [cohorts as published in official statistics] produced from Department of Health FoI – March 2025.
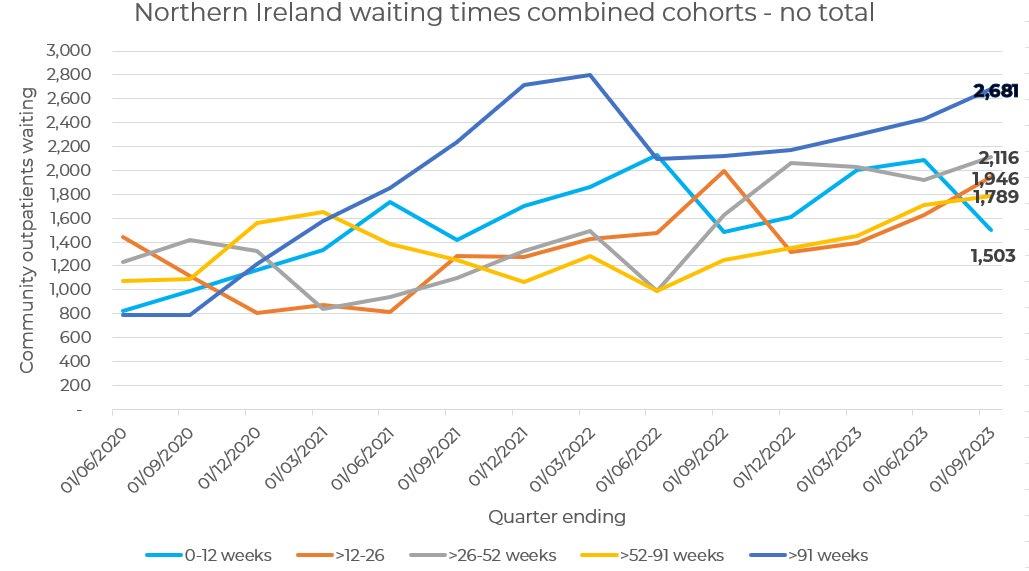
Figure 2: Combined cohorts of ‘Outpatient Community Paediatrics’ in NI waiting times 2020-23 – produced from Department of Health FoI – March 2025.
Figure 2: Combined cohorts of ‘Outpatient Community Paediatrics’ in NI waiting times 2020-23 –produced from Department of Health FoI – March 2025. Belfast Health & Social Care Trust – Community Paediatric waiting times at December 2024
Belfast Health & Social Care Trust – Community Paediatric waiting times at December 2024
0 - 6
Total: 2097
Total: 2097
Table 1: Post-encompass ‘community paediatric waiters’ in Belfast HSC Trust at December 2024 (Official statistics in development), available at: https://www.health-ni.gov.uk/publications/northernireland-waiting-time-statistics-outpatient-waiting-times-december-2024
Table 1: Post-encompass ‘community paediatric waiters’ in Belfast HSC Trust at December 2024 (Official statistics in development), available at: https://www.health-ni.gov.uk/publications/northern-ireland-waiting-time-statisticsoutpatient-waiting-times-december-2024)
In addition to the data, we issued a survey to all levels of community paediatrician across Northern Ireland to assess their experiences of the current service, as well as their thoughts on approaches to service improvement. Returns represented approximately one third (lack of clarity due to combined rotas and other factors) of community paediatricians across all five NI Trusts from consultant and Staff grade and Associate Specialist (SaS) doctor cohorts. The findings of the survey are illustrated through the recommendations, quotes and statistic boxes which follow. We thank all those who contributed their time and expertise.
In addition to the data, we issued a survey to all levels of community paediatrician across Northern Ireland to assess their experiences of the current service as well as their thoughts on approaches to service improvement. Returns represented approximately one third (lack of clarity due to combined rotas and other factors) of community paediatricians across all five NI Trusts from consultant and Staff grade and Associate Specialist (SaS) doctor cohorts. The findings of the survey are illustrated through the recommendations, quotes and statistic boxes which follow. We thank all those who contributed their time and expertise.
88% of survey respondents reported growing complexity in their routine work
of survey respondents reported long-term demand outstripping
- 53% of those stated this pressure predated the COVID pandemic
of survey respondents reported significant increases in numbers waiting to access community paediatric services
1 Strategic models of care and system improvement
88% of survey respondents reported growing complexity in their routine work
100% of survey respondents reported long-term demand outstripping capacity. 53% of those stated this pressure pre-dated the COVID pandemic
94% of survey respondents reported significant increases in numbers waiting to access community paediatric services
There are several existing policies and strategies that reference and/or impact the work carried out in community paediatrics. These include but are not limited to: a Strategy for Paediatric Healthcare Services Provided in Hospitals and in the Community (2016-2026)5 the Autism Strategy 2023-20286, the Children & Young People’s Emotional Health and Wellbeing in Education Framework (2021)7 the Mental Health Strategy (2021-2031),8 the Special Educational Needs Framework9 (and associated strategies) and the Safeguarding Board for Northern Ireland Strategic Plan 2022 – 2026.10
It follows that, as a service, community paediatrics is influenced by changes in various departments and strategic areas. Despite growing need and awareness of the impact of failure to support vulnerable children early, community paediatrics does not have a fully developed overarching regional development plan. As such, by necessity, services across Trusts have evolved organically in different areas to meet local need often without regional alignment.
Talk to people with experience of the NHS. Go round to student areas to capture voices. RCPCH &Us Voice Bank, Northern Ireland 2025
Children have good ideas. Everyone deserves a chance to speak. We are going to be the future, our voice should be heard as everyone else’s.
RCPCH &Us Voice Bank, Northern Ireland 2024
Despite sustained effort, service capacity simply cannot keep up with demand. This matters because delays in accessing community child health services can have a significant long-term impact on children and their families. Many interventions need to be given by a particular developmental stage and missing that window to intervene can have a lifelong impact, not only on the individual, but ripples throughout society in emotional and economic cost.
The need to deliver on the proposals within the draft CYP EHW Framework must be prioritised through funding and meaningful structural change. Refreshing ‘Working Together: A Pathway for Children and Young People through CAMHS (2018)’ 11 with a view toward ‘bringing all existing emotional and mental health and wellbeing services together to provide a seamless service for children, young people and their families’ at a service and planning level is welcome. However, the role of community paediatrics – wherever delivered and through whichever commissioning line – must be captured within this Framework’s development and delivery and be prioritised in all related policy making and resource allocation.
The current variation between trusts is challenging. However, it would be difficult to regionalise the triage journey when service arrangements are also different by trust. I would support a regional approach to service provision, structures and patient journey.
Equity - there are big differences in structure and delivery of community paeds services between trusts because they have evolved separately in a mostly non-commissioned fashion.
In my opinion, Trust based triage works well however a regional approach to waiting lists and data analytics around this would be useful for planning and commissioning purposes.
Regional guidelines and agreed pathways could be useful.
RCPCH Members, Northern Ireland Survey (May 2025)
We asked Community Paediatricians what they thought the key outputs of a renewed Strategy for Paediatric Healthcare Services Provided in Hospitals and in the Community should be in terms of community paediatric services. Respondents reported similar themes illustrating a need for a more cohesive, streamlined and, in most cases, regionalised approaches to the delivery of the broad spectrum of services and clarification of the paediatrician’s role therein. Respondents told us that the specialty itself required robust inclusion in any follow-on Strategy because the role and extent of need in community child health services is not recognised in the current iteration.
We also asked Community Paediatricians for views on how community paediatrics can be delivered in a more equitable, accessible and integrated way in a region the size of NI. Agreed care pathways, a clear view of need identified with commensurate commissioning and robust workforce planning, as well as an action plan driven by a community paediatric network were recurring response returns.
1.1. The Child Health Partnership should be empowered to develop and deliver a community paediatrics regional action plan to run consecutively with related frameworks and follow-on Strategy for Paediatric Healthcare Services Provided in Hospitals and in the Community. This should ensure community paediatrics is acknowledged within broader policy and commissioning. Establishment of a bespoke community paediatric network should also be considered for better alignment and continuity of care.
1.2. The Department of Health should drive the development of models of joint working between primary care and paediatric teams as well as closer working with education and Child & Adolescent Mental Health (CAMHS). Every Area Integrated Partnership Board (AIPB) within the NI Integrated Care System should be supported to do this, using examples of best practice such as the Child Health GP Hub model.
1.3 In addition to the service standards that community paediatrics operate under, the Department of Health should mandate regional and Trust agreement on service provision as well as central reporting mechanisms for referral data and waiting lists. Coordination and management of waiting lists regionally should be capable of identifying children with significant needs are not waiting excessively or are on multiple lists.
88% of survey respondents reported staffing shortages in their service
75.5% of those reporting staff shortages reported an inability to recruit in response to planned leave, ad hoc leave and / or retirements
Community paediatrics encompasses a broad range of services and systems, each tailored to the unique needs of children and young people. In preparation for this report, our members shared the current challenges faced in community paediatrics including growing demand and persistent understaffing, which significantly impacts the ability to deliver equitable and timely services.
To understand the support needed by both staff and patients toward creating a sustainable child health workforce, it is crucial to conduct a comprehensive review of the breadth of community child health services and staffing levels delivering them. Effective service delivery remains dependent on adequate staffing which includes staff wellbeing. Our members report a variable picture of unfilled posts and patchy recruitment where cover for absences has simply not been forthcoming. Not only that, but a majority also alluded to a need for enhanced staffing levels and training opportunities in these services beyond that which is currently funded regionally and locally.
Addressing workforce issues in Community Paediatrics is a constant challenge. ‘Workforce’ has been number one concern on our monthly team meeting agenda for over 10 years and while we have experienced short periods of a fuller team these are not sustained.
Since I have worked in Community Paediatrics for the last 10 years we have always had 1.5 less Consultants than we should have and at least less than 1 Specialty Doctor.
Development of a regional Community Paediatric network to develop regional resources and support Understanding of the pressures on current workforce and forward-thinking workforce planning
Understanding and recognition that currently services are provided differently across the different Trusts and that each Trust has adapted organically to the needs of its population with the workforce available.
RCPCH Members, Northern Ireland Survey (May 2025)
The Department of Health’s most recent active recruitment statistics paint a worrying picture. The data is not disaggregated in a manner that allows an insight into community paediatrics: vacancies of 111 in OT, 99 in Physiotherapy, 30 in SLT, 55 in paediatric nursing in the context of an overall 10.3% shortfall in SAS doctors and 6% in consultant posts, expose concerning gaps.12 We wholly welcome the uplift in AHPs announced by the Department of Health in May 2025, and are hopeful that community child health will benefit from these allocations. However, the community paediatric medical workforce is under significant pressure, as evidenced by this review and recent NI Children’s Commissioner Reports, and results in a delay of time-dependent interventions for children. It is therefore imperative that the medical workforce is adequately supported to deliver timely and effective care.
There are systematic issues for doctors linked with resources. There needs to be more staff, more funding and to cut down the waiting times.
RCPCH &Us Voice Bank, Northern Ireland 2025
2.1. The Department of Health should conduct a scoping review of the current community child health workforce, including paediatrician per Trust and per capita (Whole Time Equivalent).
2.2. The NI Executive should support the Department of Health to invest in the community child health workforce. This includes addressing workforce gaps for community paediatricians, Allied Health Professionals, nursing and beyond.
2.3. The Department of Health should consider the modelling of children’s health within longerterm HSC Workforce Plans. Investment in the workforce should be evidence-based and align with the five principles of public budgeting for children’s rights: effectiveness, efficiency, equity, transparency and sustainability while taking account of increased demand and complexity in child health.
2.4 The Department of Health should develop an overarching child health workforce strategy. This should take a whole system, long-term approach to recruitment and retention including consideration of expanding training places for paediatricians. Given the pressures on the medical workforce, community child health should be a core focus. This is essential for delivery of services which can safely meet children’s health needs now and into the future.
At time of publication, a full data set for community waiters for all paediatric services was not available. However, the region-wide data set provided for ‘Outpatient community paediatric’ waiters via Department of Health Freedom of Information return, showed a growth of 85.9% between September 2020 and September 2023. We welcome the capability of all Trusts to publish community paediatric regional data post-Encompass. However, data disaggregation and the ability to share information more widely is crucial. The dataset presented in this report upon request from the Department of Health illustrates growing demand yet omits a clear picture of that demand. Families and community paediatricians alike are in support of improved data collection, as evidenced in the following quotes.
Outpatient community paediatric waiters in NI grew by 85.9%
September 2020 – September 2023
Tell us what the expected timeline is – like a link to a countdown to your appointment.
RCPCH &Us Voice Bank, Northern Ireland 2024
You could have an app to see how long of a wait you have left.
RCPCH &Us Voice Bank, Northern Ireland 2024
…a regional approach to waiting lists and data analytics around this would be useful for planning and commissioning purposes.’
‘Collation of local and regional waiting list data to inform service requirements…’
‘Sharing of information and resources - building on the good practice and ideas that are in every Trust area … Embracing the benefits of Encompass.
RCPCH Members, Northern Ireland Survey (May 2025)
3.1. The Department of Health should support Trusts and ICS structures to standardise data collection and sharing between community health services across secondary, primary, community services toward a greater understanding of need and streamlining care.
3.2 Mandatory data reporting from all Trusts should be forthcoming to ensure a full and accurate picture of the number of children on waiting lists.
3.3. The Department of Health should support the development of a high-quality data source to support community child health services which enables inequalities in waiting times to be explored at system, area, trust and specialty level. Data coding could include information on income, ethnicity and deprivation to understand at what point people are experiencing barriers to accessing services.
3.4. The Department of Health should break down and clarify the different services and interfaces that fall into the category ‘Outpatient community paediatric’ waits and combine with datasets for all community child health services. We welcome the capability to publish outpatient community paediatric waiting data going forward, however, disaggregating this data to clarify which service line applies while adding detail on waiters for all other community child health services will enhance understanding for service providers as well as build a better overview for benchmarking and service alignment.
Community paediatrics necessitates extensive collaboration across various staff groups and sectors. Primary care, Child and Adolescent Mental Health Services (CAMHS), nursing, Allied Health Professionals (AHPs), education providers, and social services all play a crucial role in this collaborative effort. Adjacent to statutory services, colleagues in the voluntary and community sector provide key support to many patients of community paediatrics.
Secondary care is often considered as taking place in hospital settings, however many aspects of paediatric care are provided in communities and delivered by teams of clinicians, nurses, allied health professionals, child health assistants and psychologists supported by dedicated referral co-ordinating
teams and clinical administrative staff. Community paediatricians provide medical knowledge and skills within these teams. They are integral to the examination, investigation, diagnosis and ongoing medical management of children and young people in community settings, yet demand for medically led community child health services remains exceptionally high. Our members also report a growing demand on their time toward supporting more multi-agency work.
There is definitely an increased number of children with social communication difficulties and learning disabilities since COVID. In 5 years, the demand for special school has skyrocketed...
Stronger links between health and Education Authority- being able to raise concerns early to help ensure appropriate and timely support for education.
…Children are waiting for SLT/OT/PT services. Children cannot access services in a timely manner for social work. Children are not being allowed to access the learning disability service if they are not given a formal LD diagnosis which is not possible in the younger children.
There is also very long waiting lists for the services we refer to: OT 3 years, SLT 10 months, ADHD 3-5 years, ASD 3 years, LD up to 5 years so these patients do not get the timely early support andintervention they need with Community Paediatrics being the main support for these families.
The most vulnerable families are often the ones who don’t access services or fail to attend appointments. Local links who know the children, AHPs, schools and families are often their support network which might be lost somewhat in a regional plan.
…adolescents should not be forgotten and they are often stuck between child and adult services. More clarity on who the right services are for them should be given. Transition to adult services for children with complex needs is also done variably across the region. Children who have well known medical conditions should not have to wait on an adult new patient waiting list to be seen. That is not a transition, that is a new referral...
Long waits for child development clinics, neurodevelopmental services, complex child development services … impacted by waits for other services, such as CAMHS and transition services such as adult ADHD services.
More awareness in general public that being seen by a community paediatrician is only part of helping the family and that engagement with other services is essential.
RCPCH Members, Northern Ireland Survey (May 2025)
Have an advocate or a point of contact to clear up, misunderstandings between departments for children and young people.
RCPCH &Us Voice Bank, Northern Ireland 2024
Have a relationship with the pharmacy so you can get your medication straight from them instead of having to go to the GP first which will cut down waiting times
RCPCH &Us Voice Bank, Northern Ireland 2025
We need to help children with their troubles if they’re struggling at home school or is depressed it would help child feel better if there is quicker mental health help and they won’t always be feeling sad, down or over thinking
RCPCH &Us Voice Bank, Northern Ireland 2024
4.1. The NI Executive must support the Department of Health to invest in understanding the complex care caseload community paediatricians are tasked with. They should be situated in the right place utilising their unique skills and training within Multi-Disciplinary Teams to focus on medical intervention and advice.
4.2. The Department of Health and Education should work collaboratively through the CYP EHW Framework, 10-year CYP Strategy and legislative vehicles such as the Children’s Services Cooperation Act (NI) 2015 to drive coordinated working practices which wrap around vulnerable children.
4.3. The Department of Health should enable processes for closer working with and access to CAMHs and mental health practitioners within community paediatric services to ensure better coordinated workplans and patient care plans.
4.4. The Department of Health should enable the scoping of onward transitions from community child health services to commensurate adult services – looking to other jurisdictions for best practice.13 The draft CYP EHW Framework provides a basis for continuous care which must be pushed forward through sustained action.
4.5. Regional plans and strategies pertaining to community paediatrics must pay cognisance to local support to vulnerable families whose needs may be complex and require enhanced provision
A comprehensive overview of the number of children diagnosed with specific neurodevelopmental conditions, and those currently awaiting assessment, is not publicly available. However, we do know that approximately 5% of school age children have an autism diagnosis, representing 1 in every 17 school age children.14 Robust neurodevelopmental processes and triage take time and should involve clinicians who understand the range of presenting problems. There is a need for mapping pre-referral and referral processes to ensure that children are seen in the right service for their needs.
There needs to be signposting to groups to learn about Autism and ADHD, as well as support for the parents of children with neurodiversity.
RCPCH &Us Voice Bank, Northern Ireland 2024
When we come in to services, it would be good to have fidget spinners and sensory toys.
RCPCH &Us Voice Bank, Northern Ireland 2024
All Community Paediatricians responding to our survey expressed a level of concern around inequitable access and lengthy waits for neurodiversity assessment and support services. Our members recommended that in order to offer the neurodevelopmental assessment approach recommended in
the draft CYP EHW Framework, a hub and spoke regional system could be optimal. Pooling resources across Northern Ireland to develop one region-wide waiting list for assessment with follow up, therapy and reviews carried out by local Trust teams.
These children and families cannot be parcelled onto the same conveyor belt with the end point being a label on their head with a diagnosis then discharge. Our service is more than making a diagnosis or onward referrals - the ideal would be good quality & timely multidisciplinary care especially for the most vulnerable families and good support until they get their wings to fly.
Increased complexity probably compared to pre-Covid. We are seeing more patients with multiple diagnoses of ASD/ADHD/DCD/Tourette’s etc.
Certainly increased numbers of ASD children and many with anxiety or behaviour issues who cannot access a therapeutic service so come to Community Paediatrics as GP do not know where to refer or get referrals rejected by other services.
More social communication difficulties and attentional difficulties. Increase in ASD/ADHD presentation. Also increase in level of need, previously would have seen children with mild-moderate learning difficulties in CDC, now seeing SLD (severe learning difficulty) level - mainly non-verbal children with significant issues with behaviour/transition.
RCPCH Members, Northern Ireland Survey (May 2025)
5.1. The NI Executive should support the Department of Health to fully implement the draft CYP EHW Framework alongside enabling policies, ensuring adequate resource and coordination to develop a roadmap for the delivery of uniform ND pathways and support services prior to any diagnosis. For example, children’s ADHD services are provided by Community Child Health, CAMHS and Intellectual Disability Services. Collaboration between different parts of the service is crucial as is the support provided by the VCS.
5.2. The Department for Health should consider a hub and spoke approach to service modelling, enabling a more streamlined, equitable means to neurodevelopmental diagnosis at regional centre/s and local Trust review and therapeutic management.
5.3. A key component to the consideration of service modelling must include scoping the medical community child health workforce and placing them appropriately to utilise the unique skill they bring to services.
5.4. The NI Executive must work in conjunction to address the disproportionate prevalence of autism as in indicator of ND prevalence in children from disadvantaged backgrounds. The impact of deprivation on equity of access to diagnostic and therapeutic support must be addressed by all relevant policy makers.
1 Professor Rafael Bengoa (2016) Systems not Structures, available at: https://www.health-ni.gov.uk/topics/ systems-not-structures-changing-health-and-social-care
2 NHS Confederation, 2023. Creating better value: understanding the economic impact of NHS spending by setting. Available at: https://www.nhsconfed.org/publications/creating-better-health-value-economicimpact-care-setting
3 draft Children’s and Young People’s Emotional Health and Wellbeing Framework
4 One Year Post Publication Monitoring Report ‘More than a number’ – A rights based review of child health waiting lists October 2022 https://www.niccy.org/wp-content/uploads/2022/11/niccy-monitoringreport-more-than-a-number-one-yr-on-27-october-2022.pdf
5 NI Department of Health (2016) A Strategy for Paediatric Healthcare services provided in Hospitals and the Community (2016-16) available at: https://www.health-ni.gov.uk/publications/strategy-paediatrichealthcare-services-provided-hospitals-and-community-2016-2026
6 NI Department of Health (2023) Autism Strategy 2023-2028, available at: https://www.health-ni.gov.uk/ publications/autism-strategy-2023-2028
7 NI Department of Education (2021) Children & Young People’s Emotional Health and Wellbeing in Education Framework (2021) available at: https://www.education-ni.gov.uk/sites/default/files/ publications/education/Children%20%26%20Young%20People%20s%20Emotional%20Health%20 and%20Wellbeing%20in%20Education%20Framework%20%28final%20version%29.PDF
8 NI Department of Health (2021) Mental Health Strategy (2021-2031), available at: https://www.health-ni. gov.uk/publications/mental-health-strategy-2021-2031
9 NI Department of Education (2021) Special Educational Needs Framework, available at: https://www. education-ni.gov.uk/articles/new-sen-framework
10 SBNI (2022) Safeguarding Board for Northern Ireland Strategic Plan 2022 – 2026, available at: https:// www.safeguardingni.org/sites/default/files/2022-09/SBNI%20Strategic%20Plan%202022-2026%20 Final%20v1.0.pdf
11 NI Department of Health (2018) Working Together: A Pathway for Children and Young People through CAMHS (2018), available at: https://www.familysupportni.gov.uk/Content/uploads/userUploads/CAMHSPathway.pdf
12 most recent active recruitment statistics
13 RCPCH, Best Practice examples of health transition. Available at: https://www.rcpch.ac.uk/resources/ best-practice-examples-health-transition
14 NICCY (2022) One Year Post Publication Monitoring Report ‘More than a number’ – A rights based review of child health waiting lists October 2022 https://www.niccy.org/wp-content/uploads/2022/11/ niccy-monitoring-report-more-than-a-number-one-yr-on-27-october-2022.pdf
The Royal College of Paediatrics and Child Health is the membership body for paediatricians and we have over 24,000 members across the UK and internationally. We are responsible for education, training and setting professional standards and informing research and policy. We work to transform child health through knowledge, research and expertise, to improve the health and wellbeing of infants, children and young people across the world.
For further information, please contact Anna McDaid, Head of Policy and Public Affairs (Devolved Nations): anna.mcdaid@rcpch.ac.uk
Collaborative Healthcare in Northern Ireland: Delivering the services children need in the community
©RCPCH 2025
Incorporated by Royal Charter and registered as a Charity in England and Wales: 1057744 and in Scotland: SCO38299. Registered Office 5-11 Theobalds Road, London WC1X 8SH. Patron HRH The Princess Royal.
Royal College of Paediatrics and Child Healt h Ireland
Leading the way in Children’s Healt h