International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 09 Issue: 11 | Nov 2022 www.irjet.net p-ISSN:2395-0072

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 09 Issue: 11 | Nov 2022 www.irjet.net p-ISSN:2395-0072
2
1Department of Computer Science, Cross River University of Technology, Calabar, Cross River State, Nigeria 2Department of Computer Science, University of Calabar, Calabar, Nigeria. ***
Abstract - Over the year’s studies have concentrated on causative factors for lack of quality care and treatment practices without much attention to the important role of healthcare providers such as community-based practitioners that contribute to high mortality rate including poor health seeking behaviours, and unavailability of health carefacilities or qualified health personnel. Community-based health practitioners’ knowledge and practice are crucial to the provision of quality care. Decision making in health care practice is a difficult task because of the uncertainties at different stages of interventions. Most times Patients are unable to explain the problems withdefinite detailsandhealth worker on the other hand are unable to accurately diagnose the presenting symptoms. Several CDSS have been develop but not so much has been considered in the area of Knowledge representation and inferences in CDSS under uncertainties. Using CDSS uncertainty handling can be achieved when designed in a manner to help in diagnosing the symptom and toassisttheCHWtohandlepatient’shealthrelatedproblems where patient’s specific records are not available. This research reviewed CDSS in relation on how it is usedinpatient diagnosis.
Key Words: eHealth, Telemedicine, Telehealth, Mhealth, MHAs,CBR,CDSS
The measure of quality of care is in This WHO in its guidelinesonhealthpolicyandsystemsupporttooptimize communityhealthworkerprogrammesin2016,articulates that shortages of health professionals remains a threat to realisingthehealth-relatedSustainableDevelopmentGoals (SDG)andUniversalHealthCoverage(UHC).Thesituation necessitated the endorsements to revise current health policiestoreflectasustainableandresponsiveskillsmixof available health professionals. Focus was made on communityhealthworkers(CHWs)asanimportantcadre within multidisciplinary primary healthcare teams since they are usually the first contact. CHWs are increasingly expected to take on additional tasks including identifying emergenciesandshouldbeabletostabilisepatientsbefore referraltotheright
The adherence to standardised clinical practice using approved guidelines, and the adherence by clinicians to evidence-based guidelines in which the end product is usually associated with better health outcomes [1]. And sometimes, it may also include the use of technology by
healthcareprofessionalsintheirclinicalpracticessuchas clinical decision support systems. Most CDSS combine individual’s health information in the form of Electronic Health record (EHR) with the health worker’s knowledge and clinical protocols to assist health workers in making diagnosisandtreatmentdecisions.Modernmedicalpractice usuallycombinestechnologyforthetreatmentofpatients, likeaCDSSwhichisacombinationofknowledge,algorithm and equipment. In recent times CDSS is gradually being adaptedinpracticeandissteadilyincreasinginsuchusage asa resultof the storageof electronichealthrecords. The implementationanduseofclinicaldecisionsupportwould influencetheoutcomeoftreatmentsinyearstocome
DSSapplicationsintegratesknowledge-basedintoclinical decision-makingprocess.Theideaistoprovideatthepoint ofcarerelevantinformationtothecaregiver.[2]describeda DSS implemented in PDAs in which a knowledge base is embedded to deliverthe requiredknowledge and monitor given therapy plans for physicians in making diagnostic decisionsatthepointofcare.Recentworkonmobileclinical supportsystemsaddressesdifferentdecisionsupportsuchas knowledge delivery on demand, medication consultant, therapy reminder [2], preliminary clinical assessment for classifyingtreatmentcategories[3]andprovidingalertsof potential drugs interactions and active linking to relevant medical conditions [4]. Studies has demonstrated that physicianworkstations,linkedtoacomprehensiveelectronic medical record, can be an efficient means for decreasing errors or omissions and improving adherence to practice guidelines.
Mobile technology shows potentials to improve the qualityofservicesprovidedbycommunityhealthworkers. Efforts in studies are increasing that could lead to robust positiveprogramoutcomes. Scientificgapswillneedtobe addressed as the advancement of the use of mobile technology tools for community health workers gain momentum.
[5]alludedthatMobiletechnologieshavethepotentialto bridgesystemicgapsneededtoimproveaccesstoanduseof healthservices,particularlyamongunderservedpopulations in resource poor countries. The use of mobile and/or electronic devices to support medical and public health practice and research is increasingly being appreciated worldwide.[6]concludedthatmobilepenetrationcoupled
2022, IRJET | Impact Factor value: 7.529 | ISO 9001:2008 Certified Journal

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 09 Issue: 11 | Nov 2022 www.irjet.net p-ISSN:2395-0072
with investments from technology companies can provide accessible platforms onto which innovations can establish andoffervalue-basedproducts,providesopportunityforits use in providing service at the point of care. [7] in their publicationareoftheviewthatmobilephoneinnovationsare cheap and so can provide fast solution especially in areas withpoorhealthcareinfrastructurelikeourruralareaswhich havethepotentialsofimprovementsinhealthoutcomes.
[8]intheirpaperCommunityHealthWorkersandMobile Technology:ASystematicReviewoftheLiteratureconcluded bysayingprogrammaticeffortstostrengthenhealthservice delivery focus on improving adherence to standards and guidelines, community education and training, and programmaticleadershipandmanagementpracticesshould beencouraged.Theyconcludedthatstudiesthatevaluated programoutcomesprovidedsomeevidencethatmobiletools help community health workers to improve the quality of careprovided,efficiencyofservices,andcapacityforprogram monitoringisencouraged,weagreecompletely.
In2020thelimitationstotelemedicinewasdemystifiedby theCOVID-19pandemicafterdecadesofresearch.COVID-19 imposed demands provided the motivation to solve regulatoryandinfrastructuredemandsthathadpreviously beenconceivedandthoughtasinsurmountable.Duringthe periodoflockdown,therewasurgencytoseepatientswhich wasverycrucialespeciallythosewithterminalailment,and in-personclinicalcare.
[9], in their part says CDSS are Systems that provide clinicianswithknowledge,intelligentlyfilteredorpresented at appropriate times, to enhance health and health care, offeringaneffectivepathwaytoimprovepatientsafetyand reduce errors of clinical practice. [10] defined CDSS as a systemprovidingdiagnosticdecisionsupportasacomputerbased algorithm that assists a clinician with one or more component steps of the diagnostic process. [11] defined CDSSsas“softwarethatdesignedtobeadirectaidtoclinical decision-making,inwhichthecharacteristicsofanindividual patient are matched to a computerized clinical knowledge baseandpatientspecificassessmentsorrecommendations are then presented to the clinician or the patient for a decision”
[12] noted that in the last decade, more mobile and electronicinformationtoolshavebeendeveloped,testedand implemented with CHWs to support their work roles. The toolshelptheCHWsinsurmountingchallengessuchaslack of appropriate work tools and inadequate supportive supervisionandtraining.[13]believesthattoolsinCDSSis instrumental in improving access to care by marginalised populationgroupssubjectedtostigmaandthoseinhard-toreachareasbyreducingbothtimeandcostoftravel.Assuch, researchonCHWs’useofmHealthtoolsisimportant.Several
pilot projects, using multiple designs and measures have been implemented. Several projects have reported improvementsinservicesrenderedbyCHWsandtherelated healthoutcomesforcommunities.Mostoftheinterventions demonstrated improvements in the CHWs’ delivery in maternal,new-bornandchildhealth,tuberculosisandsexual andreproductivehealthservices,amongothers.
[14]saidthatclinicaldecisionsupportsystem(CDSS)is intended to improve healthcare delivery by enhancing medicaldecisionswithtargetedclinicalknowledge,patient information,andotherhealthinformation.ACDSScomprises of software designed to be a direct aid to clinical-decision making. Usually, the characteristics or symptoms of an individual patient are matched to a computerized clinical knowledge base and patient-specific assessments or recommendationsare thenpresented totheclinicianfor a decision.TheintendedCDSStobedevelopedwillprimarily beusedatthepoint-of-care,forthecliniciantocombinetheir knowledgewithinformationorsuggestionstobeprovidedby theCDSS.
[15]outlinedaspectsofCDSSformodelsandframeworks, summarizing the literature. These aspects include the adaptationofCDSStohospitalworkflow,constructionofits components, interoperability and sharing of data, considerationsofreasoning,healthsystemspriorities,quality improvementoutcomes,andCDSeffectivenessevaluation.It is recognize that these aspects address several different layers of data, analysis, and decisions, including organizational,interoperability,andmodellingaspects.
[16]saidtheoptimaluseofCDSSshavethepotentialto improve healthcare processes and outcomes by ensuring compliance with the most up to date guidelines, reduce clinicalerrors,andreducecostwithoutcompromisingcare.A CDSS should be viewed as supportive tool available to the clinician to facilitate their task, and definitely not as her substitute.
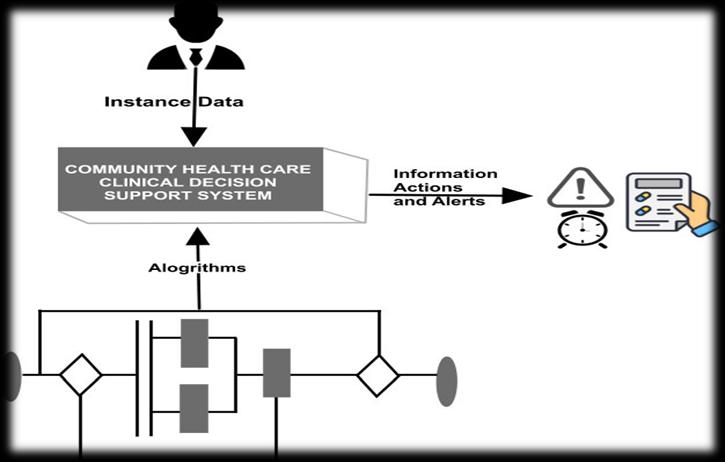
Fig1depictsthethreeprincipleelementsgenerallyrequired for a CDSS, which are: the knowledge base contains in a computer interpretable format the rules, associations, and clinical know-how for the task at hand (e.g. screening, diagnosis,treatment,prognosis);thealgorithmsdetermine howtocombinetheknowledgebasetoaninstanceofpatient specific data, which is supplied to the system in order to generateanactionablerecommendationorassessmentofthe patient; the communication mechanism is the manner in whichthesysteminputsthepatientspecificdataandoutputs therecommendationsorassessmentstotheclinician.
© 2022, IRJET | Impact Factor value: 7.529 | ISO 9001:2008 Certified Journal | Page704

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 09 Issue: 11 | Nov 2022 www.irjet.net p-ISSN:2395-0072
users,andeffectonrelationshipsbetweenprofessionalsin theclinics.Itisparticularlyimportantforuserstobevigilant andnotexcessivelyrelyontheCDSS,buttoalsomakesure theyusetheirowncommonsenseandcritical-thinkingskills duringtheearlystagesofimplementation.Usersareexpected to be competent and knowledgeable in their fields and be capableofmakinglogicalandsafedecisionsthatprioritize patientsafety.
Fig -1:Elementsofclinicaldecisionsupportsystem
Clinical decision support systems have the potential to improve patient care in a many ways. A CDSS help in the reducingmedicalerrorsandreducingofadversedrugeffects onpatients,itensurescomprehensivetreatmentforpatient illnesses and conditions, It encourage adherence to guidelines, and shorten the length of stay of patient. A successful CDSS that can effectively operate and achieve outcomeswillpotentiallydecreasetheexpenses.Studieson CDSS confirm its use with medication administration and healthpreventiondecisionsupportwillresultsinimproved quality of patient care. Clinical decision support systems provide enhanced communication across disciplines, it improves accessibility to references on best practice, improvesadherencetocareguidelines,andamoreconsistent qualityofpatientcareresultinginbetterpatientoutcomes.A CDSSalertsandremindersencouragescontinuouslearning for CHW at the novice level and reinforce already known knowledgeinnurseswhoareexperts.Thepromptdeliveryof care options to the users aids in expediting the decisionmakingprocessregardingpatientcare[17].
Issuesborderingonethicsareofgreatconcernwhenit comes to CDSSs, the risk ofpatient harm if the tool is not developedorusedcorrectlyisveryimportantandcaremust betakeninmakingsurethatitworkscorrectlyeverytime [18].TheSoftwareEngineerCodeofEthicsandProfessional Practiceguaranteesthatthesystembeingdevelopedshould bebeneficialtotheuserandshouldcausenoharm.Greatcare mustbetakenindevelopingCDSSsbecauseanyerrorsthat are not caught prior to implementation can become a detrimentalerrorsthatcanaffectapatient.
TheethicalconsiderationthatrelatestoCDSSsincludes the standards of care, the proper utilization, suitability to
Foradditional protectionand safetyofthe patient, itis expectedthatthedevelopmentofCDSS shouldbedonebyall members of the clinical team that will be using it. No one specialityshouldprofoundlyinfluencethedesign.TheCDSS should encourage multi-disciplineusage. Theusersshould feel comfortable with the design as it has incorporated all disciplines,thesewillleadtothesafedeliveryofqualitycare. The usersshould be well-trained ontheCDSSso that they take appropriate actions to preserve patient safety when prompted
Amajorconcerninthedecreaseofprofessionalrelationships maybetracedtotheoverdependenceonCDSSs.Theresulting qualityofcarethatthepatientreceivesbecomesanethical concern. To overcome this it is important for the users to haveregularmeetingstosharetheirexperiencesontheuse oftheCDSSforfutureimprovementandtoincorporatenew ideasthiswouldinturnprovidethepatientswiththebestof care.
TheaimofCDSSistobetterthesafetyandqualityofpatient care, improve patient treatments and quality of care, decrease the over dependence on memory, reduce error rates, and improve response time. It is a software that interpretsspecificpatientinformationthatisenteredinto thesysteminordertoprovideassistanceinmakingthemost appropriateandsafedecisionwhenprovidingpatientcare.It supportsuserswiththedetectionandpreventionofpossible riskstopatientsafetyandencouragestheappropriateusage of evidence-based practice and guidelines. It support caregiversinmakingthebestdecisionregardingpatientcare bygatheringallpertinentdataandinformationneededso thatitiseasilyaccessibleto theuserin oneplace.ACDSS takes the information entered and processes it with the utilizationoforganizationalmodels,algorithms,inorderto achieve a variety of potential action options based on the unique circumstances of the individual patient. The information that is gathered by a CDSS about a specific patient is presented with prompts, alerts, or recommendations to the correct user at the most appropriatetime[19],[20]and[21].
CDSS’saredesignedtobeofdirectaidtoclinicaldecisionmaking [22], [23] in which the characteristics of an individualpatient(symptom)arematchedtoacomputerized clinicalknowledgebase,andpatient-specificassessmentsor
© 2022, IRJET | Impact Factor value: 7.529 | ISO 9001:2008 Certified Journal | Page705

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 09 Issue: 11 | Nov 2022 www.irjet.net p-ISSN:2395-0072
recommendationsarethenpresentedtotheclinicianand/or thepatientforadecision“[24],[25].Itcanalsobesaidthata CDSSislikeajobaidthathelpscliniciansatthepointofcare tomaketherightdecisions.
[1] Huang, M., Gibson, C., & Terry, A. (2018). Measuring electronichealthrecorduseinprimarycare:Ascoping review. Applied Clinical Informatics, 09(01), 015-033. doi:10.1055/s-0037-1615807
[2] Spreckelsen, C., Lethen, C., Heeskens, I., Pfeil, K., & Spitzer, K. (2000). The roles of an intelligent mobile decisionsupportsystemintheclinicalworkflow.IFAC Proceedings Volumes, 33(12), 93-96. doi:10.1016/s1474-6670(17)37284-1
[3] Berner, E. S., & Lande, T. L. (2004). Clinical decision support systems: Impacting the future of clinical decisionmaking.HealthcareInformationManagement Systems,463-477.Doi:10.1007/978-1-4757-4041-7_36
[4] Smith,D.H.,Perrin,N.,Feldstein,A.,Yang,X.,Kuang,D., Simon, S. R., Soumerai, S. B. (2006). The impact of prescribing safety alerts for elderly persons in an electronicmedicalrecord.ArchivesofInternalMedicine, 166(10),1098.doi:10.1001/archinte.166.10.1098
[5] NkrumahGordon,A.,&EboHinson,R.(2007).Towards a sustainable framework for computer based health information systems (CHIS) for Least Developed Countries(LDCs).InternationalJournalofHealthCare Quality Assurance, 20(6), 532-544. Doi:10.1108/09526860710819468
[6] Luna,D.,Almerares,A.,Mayan,J.C.,GonzálezBernaldo deQuirós,F.,&Otero,C.(2014).Healthinformaticsin developing countries: Going beyond pilot practices to sustainable implementations: A review of the current challenges. Healthcare Informatics Research, 20(1), 3. doi:10.4258/hir.2014.20.1.3
[7] Oluoch,T.,Santas,X.,Kwaro,D.,Were,M.,Biondich,P., Bailey,C.,DeKeizer,N.(2012).Theeffectofelectronic medicalrecord-basedclinicaldecisionsupportonHIV care in resource-constrained settings: A systematic review. International Journal of Medical Informatics, 81(10),e83-e92.doi:10.1016/j.ijmedinf.2012.07.010
[8] Braun,R.,Catalani,C.,Wimbush,J.,&Israelski,D.(2013). Community health workers and mobile technology: A systematic review of the literature. PLoS ONE, 8(6), e65772.doi:10.1371/journal.pone.0065772
[9] Jao, C. S., Hier, D. B., & Galanter, W. L. (2008). Using clinical decision support to maintain medication and problemlistsapilotstudytoyieldhigherpatientsafety.
2008 IEEE International Conference on Systems, Man andCybernetics.doi:10.1109/icsmc.2008.4811366
[10] Miller,R.A.,&Geissbuhler,A.(1999).Clinicaldiagnostic decision support systems An overview. Health Informatics,3-34.Doi:10.1007/978-1-4757-3903-9_1
[11] Sim,I.,Gorman,P.,Greenes,R.A.,Haynes,R.B.,Kaplan, B.,Lehmann,H.,&Tang,P.C.(2001).Clinicaldecision support systems for the practice of evidence-based medicine.JournaloftheAmericanMedicalInformatics Association, 8(6), 527-534. doi:10.1136/jamia.2001.0080527
[12] Fraser,H.S.,Thomas,D.,Tomaylla,J.,Garcia,N.,Lecca,L., Murray, M., & Becerra, M. C. (2012). Adaptation of a web-based, open source electronic medical record systemplatformtosupportalargestudyoftuberculosis epidemiology. BMC Medical Informatics and Decision Making,12(1).Doi:10.1186/1472-6947-12-125
[13] Graven,M.,Allen,P.,Smith,I.,&MacDonald,N.E.(2013). DeclineinmortalitywiththeBelizeintegratedpatientcentredcountrywidehealthinformationsystem(BHIS) with embedded program management. International Journal of Medical Informatics, 82(10), 954-963. doi:10.1016/j.ijmedinf.2013.06.003
[14] Osheroff, J. (2012). Improving outcomes with clinical decisionsupport.doi:10.4324/9781498757461
[15] Greenes, R. A. (2014). Looking ahead. Clinical Decision Support,851-864.doi:10.1016/b978-0-12-398476-0.000300
[16] ReisWC,BonettiAF,BottacinWE,ReisASJr,SouzaTT, PontaroloR,CorrerCJ,Fernandez-LlimosF.Impacton process results of clinical decision support systems (CDSSs) applied to medication use: overview of systematicreviews.PharmPract(Granada).2017OctDec;15(4):1036. doi: 10.18549/PharmPract.2017.04.1036. Epub 2017 Dec 18.PMID:29317919;PMCID:PMC5741996.
[17] Boxwala, A. A., Rocha, B. H., Maviglia, S., Kashyap, V., Meltzer,S.,Kim,J.,Middleton,B.(2011).Amulti-layered frameworkfordisseminatingknowledgeforcomputerbaseddecisionsupport.JournaloftheAmericanMedical InformaticsAssociation,18(Supplement1),i132-i139. Doi:10.1136/amiajnl-2011-000334
[18] Zhang,S.,&Goddard,S.(2007).Asoftwarearchitecture and framework for web-based distributed decision support systems. Decision Support Systems, 43(4), 1133-1150.doi:10.1016/j.dss.2005.06.001
[19] Hu,Y.,Wen,X.,Wang,F.,Yang,D.,Liu,S.,Li,P.,&Xu,J. (2018). Effect of telemedicine intervention on
© 2022, IRJET | Impact Factor value: 7.529 | ISO 9001:2008 Certified Journal | Page706

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 09 Issue: 11 | Nov 2022 www.irjet.net p-ISSN:2395-0072
hypoglycaemiaindiabetespatients:Asystematicreview and meta-analysis of randomised controlled trials. JournalofTelemedicineandTelecare,25(7),402-413. Doi:10.1177/1357633x18776823
[20] Gordon, W. J., Landman, A., Zhang, H., & Bates, D. W. (2020). Beyond validation: Getting health apps into clinical practice. npj Digital Medicine, 3(1). Doi: 10.1038/s41746-019-0212-z
[21] Hong,S.N.(2018).Clinicalusefulnessofremotepatient monitoringusinge-Healthtechnologiesinpatientswith inflammatory bowel diseases. The Korean Journal of Internal Medicine, 33(5), 876-878. doi:10.3904/kjim.2018.298
[22] Berner, E. S., & Lande, T. L. (2004). Clinical decision support systems: Impacting the future of clinical decisionmaking.HealthcareInformationManagement Systems,463-477.Doi:10.1007/978-1-4757-4041-7_36
[23] Berlin, A., Sorani, M., & Sim, I. (2006). A taxonomic descriptionofcomputer-basedclinicaldecisionsupport systems.JournalofBiomedicalInformatics,39(6),656667.doi:10.1016/j.jbi.2005.12.003
[24] Kong, G., Xu, D., & Yang, J. (2008). Clinical decision supportsystems:Areviewofknowledgerepresentation andinferenceunderuncertainties.InternationalJournal of Computational Intelligence Systems, 1(2), 159. doi:10.2991/ijcis.2008.1.2.6
[25] Fan, A., Lin, D., & Tang, Y. (2017). Clinical decision support systems for comorbidity: Architecture, algorithms, and applications. International Journal of Telemedicine and Applications, 2017, 1-10. doi:10.1155/2017/1562919
© 2022, IRJET | Impact Factor value: 7.529 | ISO 9001:2008 Certified Journal | Page707
