Smart Prevention: Utilizing Design Thinking and IoT Technology to Prevent Pressure Ulcers in Healthcare
Dr. B. Sivasankari 1 , S. Sathish 2 , Sasikumar. S 3 , Mohit. S 4 , Santhosh Kumar. R 5ABSTRACT: - This paper aims to address the prevalent issue of hospital-acquired pressure ulcers (HAPUs) in India, which affects a significant proportion of hospitalized patients. HAPUs commonly occur in patients who are immobile and unable to shift positions independently, leading to pressure sores. Although repositioning patients everytwohoursandusingpressure-relievingmattressescan prevent HAPUs, the compliance of caregivers with these guidelines is often inadequate in healthcare facilities. In addition, there are challenges in continuously monitoring patient positions and alerting caregivers of necessary turns. The proposed solution involves a Design Thinking method that tracks the patient's position by means measuring their Temperature, Pressure, Sensory perception, Mobility, Activity and communicates wirelessly with a tablet to alert caregivers of necessary turns, following hospital policies. The IoT technology allows for centralized monitoring, recording and updating of patient positions and turning operations. In a controlled environment, the system successfullytrackedpatientpositionsandidentifiedcommon poses an IoT-based approach to prevent HAPUs is a promising solution that can significantly improve compliance with turning guidelines, reduce the workload on caregivers,offercentralizedmonitoring,minimizetheriskof HAPUs, and offer a non-invasive and patient-friendly solutiontoHAPUprevention
Keywords: Pressure Sores, Pressure Ulcers, Repositioning,Prevention,DesignThinking,Internetof Things
1. Introduction: -

Apressureulcer,alsoknownasapressuresore,decubitus ulcer, or a bedsore, is a type of injury to the skin and underlying tissue caused by pressure, shear, or friction. Theapplicationofpressuretoaparticularareaofthebody canresultinreducedbloodflowandoxygensupplytothe tissues, leading to tissue ischemia and cellular damage. Elderly individuals with reduced mobility, impaired mental capacity, and increased skin friction and shear are atahigherriskofdevelopingpressureulcers.
According to a study conducted by the Agency for Healthcare Research and Quality (AHRQ), pressure ulcers are a significant problem in U.S. hospitals, affecting approximately 2.5 million patients each year. The study found that pressure ulcers were associated with longer hospital stays and increased healthcare costs, with an estimated cost of $9.1 to $11.6 billion per year. The study also noted that certain patient populations, such as older adults,thosewithlimitedmobility,andthosewithchronic medical conditions, were at higher risk for developing pressureulcers.TheAHRQrecommendsseveralstrategies to prevent pressure ulcers, including implementing a pressure ulcer prevention program, using pressurereducing support surfaces, and training staff on proper patientpositioningandturning.
To prevent pressure ulcers, healthcare providers employ various strategies, such as repositioning the patient or using pressure-relieving pillows or mattresses to reduce thedurationormagnitudeofpressureattheskin'ssurface. Intrinsicfactors,suchasthepatient'sskin'sabilitytoresist damage and remain intact, also play a role in pressure ulcerprevention.
In addition to pressure ulcer prevention, maintaining adequate nutrition, circulation, and hydration can help reduce the risk of pressure injury. Malnutrition has been found to be positively correlated with the frequency and severity of pressure ulcers. Reduced calorie intake, dehydration, and decreased serum albumin levels can make the skin and underlying tissues less resistant to pressure,friction,andshearingforce,increasingtheriskof skindisintegrationanddelayingwoundhealing.
Pressureulcersareassociatedwithpoorhealthoutcomes, high treatment costs, and future legal judgments. Therefore, the use of appropriate support surfaces and repositioning schedules are crucial preventive strategies forpressureulcers.Traditionally,hospitalshaveemployed a2-hourlyscheduleforrepositioningpatients,butpatients in a prolonged state of unconsciousness may not move positions independently, making it challenging for caregiverstoadheretothisschedule.
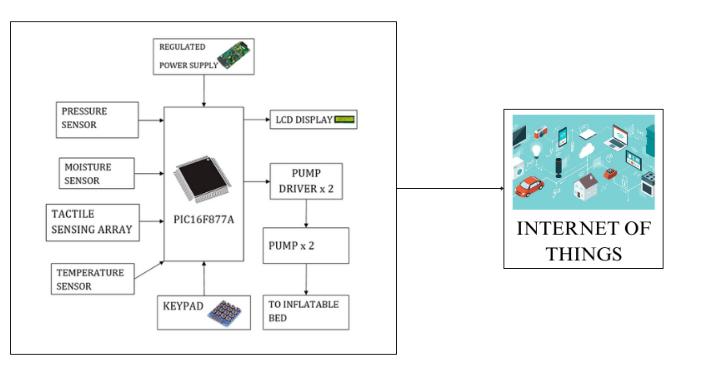
To address this issue, the proposed solution involves a wearable device that continuously monitors the patient's sensory perception, moisture, activity, mobility, nutrition, friction, and shear. The system wirelessly communicates with a tablet to notify caregivers when it is time for the patient to be turned, in accordance with hospital policies. The use of cloud technology allows for centralized monitoringand recordingofpatientpositionsandturning operations, offering a promising solution to the need for effectiveHAPUprevention
2. LITERATURE SURVEY: -
"Preventionofpressureulcersintheelderlythroughthe use of intelligent assistive technology: A systematic review." This literature survey conducted a systematic review of studies related to the use of intelligent assistive technology in preventing pressure ulcers in elderly patients. The authors found that while the use of such technologywaspromising,furtherresearchwasneededto assessitseffectivenessandcost-effectiveness.
"The effectiveness of different support surfaces for preventing pressure ulcers in patients: A systematic reviewandnetwork meta-analysis."Thisliteraturesurvey focused on comparing the effectiveness of different types of support surfaces in preventing pressure ulcers in patients. The authors found that while there was limited evidence to support the superiority of any one type of support surface, some surfaces such as alternating pressure mattresses and high-specification foam mattressesmaybemoreeffectivethanothers.
"Asystematicreviewofrepositioninginterventionsforthe prevention of pressure ulcers." This literature survey focused on examining the effectiveness of repositioning interventions in preventing pressure ulcers. The authors found that repositioning interventions, particularly those that were more frequent and involved a greater range of positions, were more effective in preventing pressure ulcersthanlessfrequentorlessvariedinterventions.
"Barriers and facilitators to implementing pressure ulcer prevention strategies in nursing homes: A systematic review." This literature survey examined the barriers and facilitators to implementing pressure ulcer prevention strategies in nursing homes. The authors found that factorssuchasstafftraining,communicationbetweenstaff and residents, and the availability of resources and equipment could all impact the effectiveness of pressure ulcerpreventionstrategiesinthissetting.
"Theimpactofnutritional interventionsonpressureulcer healing: A systematic review." This literature survey
focused on examining the impact of nutritional interventions on the healing of pressure ulcers. The authors found that while there was limited evidence to support the effectiveness of any one nutritional intervention, interventions such as protein supplementation and multivitamin supplements may be beneficialinpromotinghealingofpressureulcers.
3. EXISTING METHOD: -
The existing methods for preventing pressure ulcers includerepositioningthepatientregularly,usingpressurerelieving mattresses, and addressing the intrinsic factors affecting skin resistance, such as nutrition and hydration. Repositioning the patient every two hours can help redistributethepressureattheskin'ssurfaceandprevent the development of pressure ulcers. The use of pressurerelievingmattressescanalsohelpreducethedurationand magnitude of pressure at the skin's surface. In addition, addressing intrinsic factors such as nutrition and hydrationcanhelpimproveskinresistanceandreducethe risk of developing pressure ulcers. Malnutrition and dehydration have been linked to increased frequency and severity of pressure ulcers. Therefore, it is important to ensure patients receive adequate nutrition and hydration. Other interventions may include the use of skin moisturizers, pressure-relieving dressings, and education ofpatientsandcaregiversonproperskincaretechniques.
The development of the proposed system, which utilizes IoT technology, aims to continuously monitor and assess thehealthstatusofpatientsinhealthcaresettings.Theuse of IoT in healthcare has proven to be a game-changer, allowingforbetterpatientcare,earlydetectionofdiseases, and real-time monitoring of health status. The system assesses several critical parameters, including Sensory Perception,Moisture,Activity,Mobility,Nutrition,Friction, and Shear. Sensory Perception is crucial in evaluating the patient's capacity to recognize and respond to discomfort or pain resulting from pressure on specific areas of the

body. This parameter includes the patient's pain perception as well as their level of consciousness and cognitiveresponsetopressure-relateddiscomfort.
Moisture is another parameter that is monitored and recorded by the system. The excessive and continuous moisture of the skin can lead to maceration of skin tissue, putting the skin's integrity at risk. The Activity parameter revealsthelevelofphysicalactivityofthepatient,whichis critical as inactivity can promote tissue breakdown and muscular atrophy. Mobility parameter evaluates the patient's ability to change their body position independently, including their willingness to move and theirphysicalabilitytodoso.Apatient'snutritionalstatus is also assessed by examining their daily eating habits, whereasmallnumberofmealsoranimbalanceddietmay indicate a higher risk. The proposed system's objective is to monitor patients' health status continuously, allowing for early detection of potential health risks, particularly pressure ulcers. Pressure ulcers are a severe problem in healthcare, particularly in patients who are immobile or havelimitedmobility.Earlydetectionofpressureulcersis crucial as they can lead to severe complications such as infection and sepsis. The proposed system, utilizing IoT technology, provides an effective solution to prevent pressureulcersfromdeveloping,makingita valuabletool in healthcare. The system's continuous monitoring and assessment of the patients' health status will provide healthcare providers with real-time information, enabling them to provide better patient care and improve patient outcomes.
5. RESULT: -
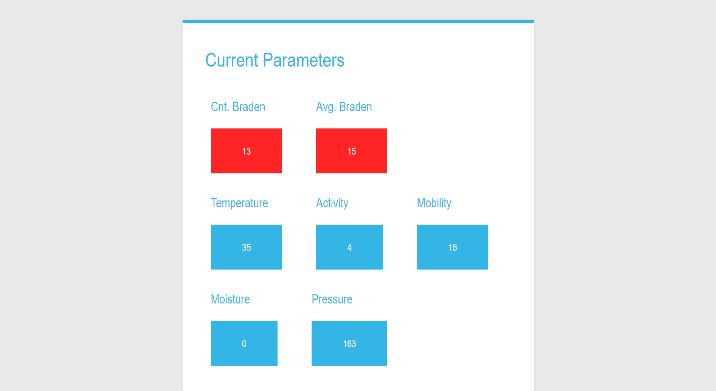
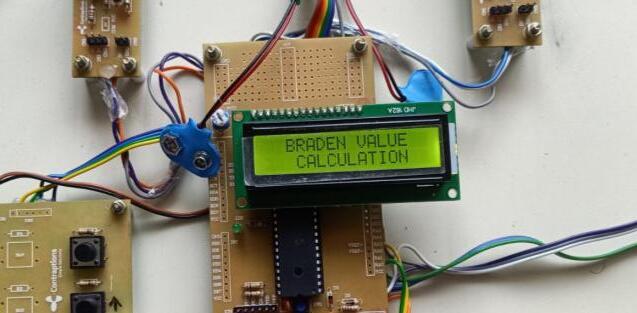
The results can be displayed in the LCD First it displaysthe Braden Scale for Predicting Pressure Ulcer Risk.


The above figure shows the Parameters such as Temperature,Pressure,Mobility,Activity,Moistureetc.
6. CONCLUSION: -
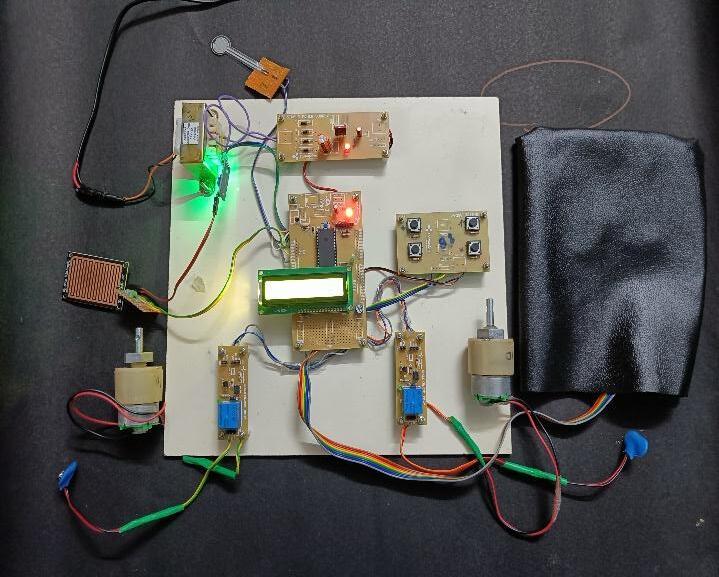
The proposed method for preventing and monitoring pressure ulcers and various health parameters involves theuseofadvancedtechnology.Thesystemisdesignedto automatically inflate the bed to assist patients who are unable to move and change positions independently. This not only helps to prevent the development of pressure ulcersbutalsoaidsinthecontinuousmonitoringofseveral important parameters such as Sensory Perception, Moisture,Activity,Mobility,Nutrition,Friction,andShear.
The system can be used to prevent and monitor pressure ulcers by ensuring that the patients are repositioned and relievedofpressureoncertainareasofthebody.Bydoing so, the risk of developing pressure ulcers is greatly reduced. Additionally, the system continuously monitors the patient's Sensory Perception, which evaluates their ability to recognize and respond to discomfort or pain causedby pressureoncertainareasof the body.Moisture levels are also monitored to prevent skin tissue from becoming macerated and at risk of erosion, while activity levels are assessed to ensure that patients remain physically active, which reduces the risk of tissue breakdownandmuscularatrophy.
Mobility is another important parameter that is continuously monitored by the system. It evaluates a patient's capacity to change their body position on their own, including their willingness to move and physical ability to do so. By monitoring mobility, the system can determine when it is necessary to inflate the bed to assist patientsinchangingpositions.
In addition to these parameters, the system also monitors the patient's nutritional status and friction and shear levels.Thenutritionalstatusisevaluatedbyexaminingthe patient'seatinghabitsandlookingforsignsofahigherrisk of developing pressure ulcers, such as eating only small amountsoffoodorhavinganunbalanceddiet.Frictionand shearlevelsarealsomonitoredtoensurethatthepatient's skin is not subjected to excessive friction or shear forces thatcancauseskinbreakdownandpressureulcers.
In conclusion, the proposed method is an advanced and effective way to prevent and monitor pressure ulcers and various important health parameters. By automatically inflating the bed and continuously monitoring these parameters, the system provides an essential tool for healthcare providers to ensure the well-being and health oftheirpatients.
7. REFERENCES: -
1) Levine JM. Historical perspective on pressure ulcers: the decubitus ominosus of Jean-Martin Charcot.J Am Geriatr Soc.2005 Jul;53(7):124851.[PubMed]
2) Anders J, Heinemann A, Leffmann C, Leutenegger M, Pröfener F, von Renteln-Kruse W. Decubitus ulcers: pathophysiology and primary prevention.Dtsch Arztebl Int.2010 May;107(21):371-81; quiz 382.[PMC free article] [PubMed]
3) Bansal C, Scott R, Stewart D, Cockerell CJ. Decubitus ulcers: a review of the literature.Int J Dermatol.2005Oct;44(10):805-10.[PubMed]

4) van Marum RJ, Meijer JH, Ribbe MW. The relationship between pressure ulcers and skin blood flow response after a local cold provocation.Arch Phys Med Rehabil.2002 Jan;83(1):40-3.[PubMed]
5) Leblebici B, Turhan N, Adam M, Akman MN. Clinical and epidemiologic evaluation of pressure ulcers in patients at a university hospital in Turkey.J Wound Ostomy Continence Nurs.2007 Jul-Aug;34(4):407-11.[PubMed]
6) GefenA. Reswick andRogerspressure-time curve for pressure ulcer risk. Part 1.Nurs Stand.2009 Jul15-21;23(45):64,66,68passim.[PubMed]
7) Witkowski JA, Parish LC. Histopathology of the decubitus ulcer.J Am Acad Dermatol.1982 Jun;6(6):1014-21.[PubMed]
8) Rhoads DD, Wolcott RD, Percival SL. Biofilms in wounds: management strategies.J Wound Care.2008Nov;17(11):502-8.[PubMed]
9) Pressure ulcer treatment. Agency for Health Care Policy and Research.Clin Pract Guidel Quick Ref GuideClin.1994Dec;(15):1-25.[PubMed]
10) McInnesE,Jammali-BlasiA,Bell-SyerSE,Dumville JC, Middleton V, Cullum N. Support surfaces for pressure ulcer prevention.Cochrane Database Syst Rev.2015 Sep 03;2015(9):CD001735.[PMC freearticle][PubMed]
11) BatraRK,AseejaV.VACTherapyinLargeInfected Sacral Pressure Ulcer Grade IV-Can Be an Alternative to Flap Reconstruction?Indian J
Surg.2014 Apr;76(2):162-4.[PMC free article]
[PubMed]
12) Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds.Cochrane Database Syst Rev.2015 Jun 24;2015(6):CD004123.[PMC free article]
[PubMed]

13) Langer, G., Knerr, A., Kuss, O., Behrens, J., & Schlömer, G. J. (2003).Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database of Systematic Reviews.doi:10.1002/14651858.cd003216
14) Jakobsen, T. B. T., Pittureri, C., Seganti, P., Borissova, E., Balzani, I., Fabbri, S., … Fabbri, E. (2020). Incidence and prevalence of pressure ulcers in cancer patients admitted to hospice: A multicentre prospective cohort study. International Wound Journal. doi:10.1111/iwj.13317
