
LEARN. DISCOVER.






EDITORS-IN-CHIEF:
Kristen Ashworth
Kyla Demkiv
Nayaab Punjani
EXECUTIVE EDITORS:
Beatrice Acheson
Jasmine Amini
Alyona Ivanova
Lizabeth Teshler
DESIGN EDITORS:
Ravneet Jaura (Co-Director)
Jinny Moon (Co-Director)
Qingyue Guo
Athena Li
Vicky Lin
Josip Petrusa
Raymond Zhang
SOCIAL MEDIA TEAM:
Lizabeth Teshler (Director)
Lielle Ronen
Abigail Wolfensohn
JOURNALISTS & EDITORS:
Aria Afsharian
Vicky Lin,
Mya Chronopoulos
Sara Corvinelli
Anthaea-Grace Patricia Dennis
Clarize Donato
Ysabel Fine
Grace Gibson
Katherine Guo
Rachel Lebovic
Jino Lim
Eryn Lonnee
Josephine Machado
Sabeeka Malik
Caroline Marr
Eliza McCann
Areej Mir
Anna Mouzenian
Gharaza Nasir
Kinjal Parekh
Karan Patel
Ana Piric
Anita Rajkumar
Gisany Ravichandran
Ankit Ray
Angenelle Eve Rosal
Steven Shen
Rebecca Smythe
Omer Syed
Alicia Tran
Tesam Ahmed
Regina Annirood
Gabriela Blaszczyk
Yalda Champiri
Carmen Chan
Michellie Choi
Serena Trang
Priya van Oosterhout
Shreya Vasudeva
Emily Wiljer
Abigail Wolfensohn
Saleena Zedan

By Qingyue Guo, MScBMC
Happy 2026, IMS!
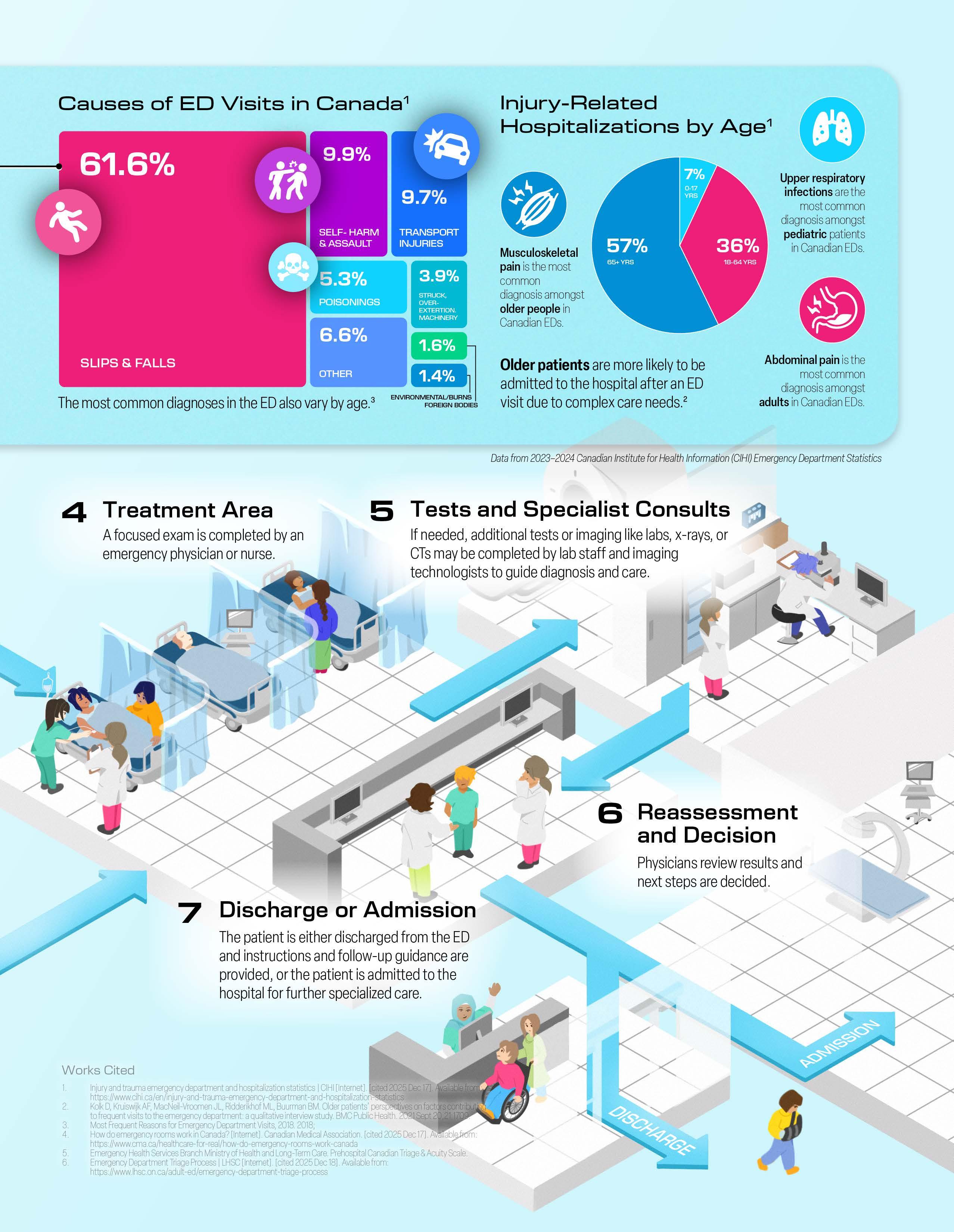
As we settle in for the winter months and gather momentum for the new year ahead, our Winter Issue of the magazine is doing the same, turning its focus toward a field that never slows down: Emergency Medicine.
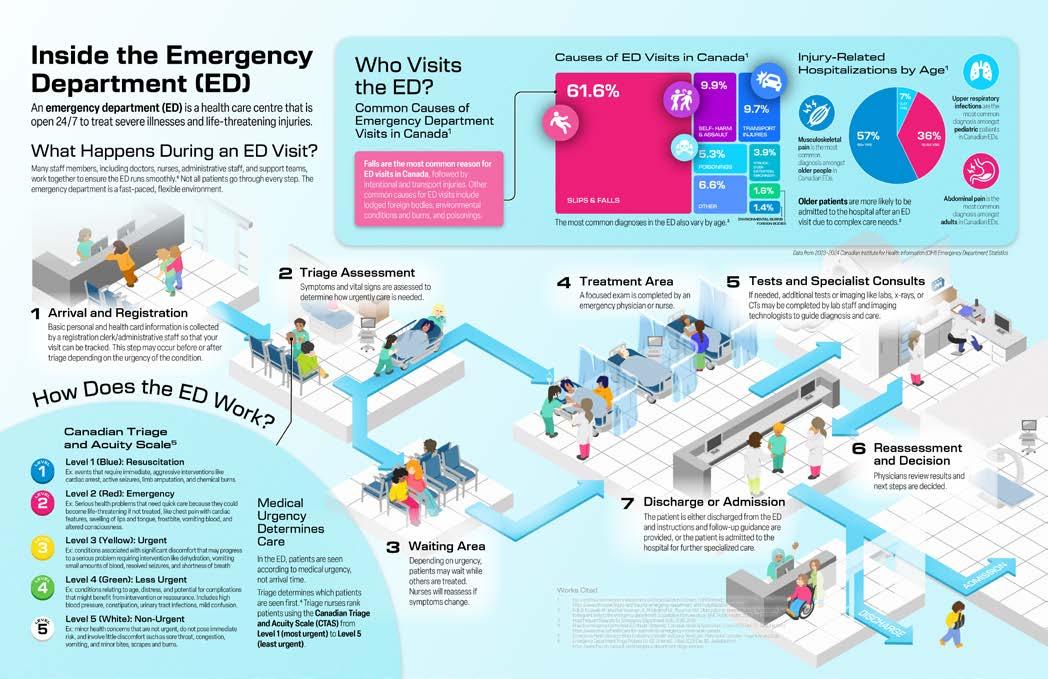
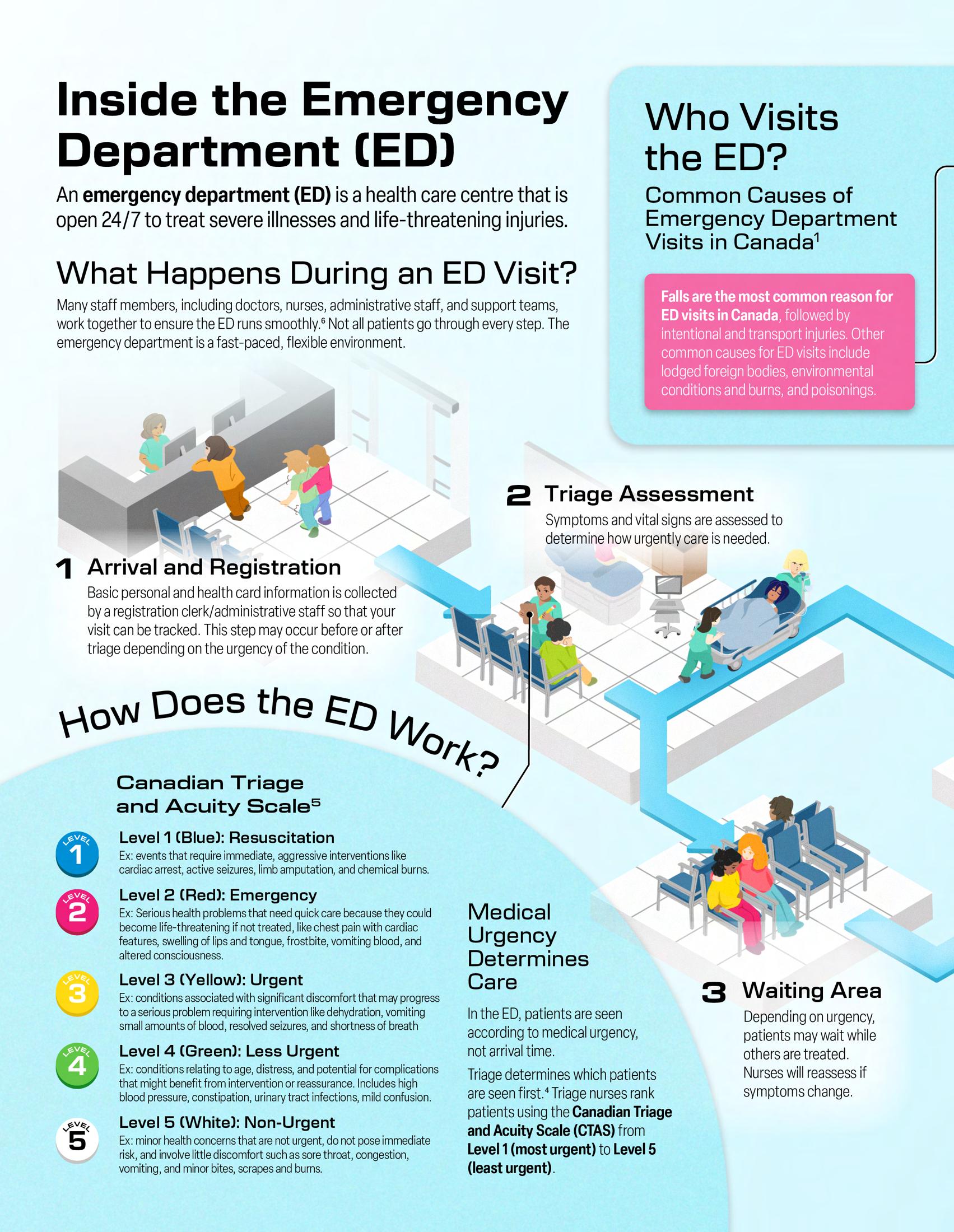
Emergency Medicine spans a remarkable breadth of clinical fields and, in tandem, a remarkable breadth of challenges. These challenges–some of which we are all too familiar with here in Canada–include accessibility to an emergency department (ED), efficient patient triage, prolonged wait times, accurate acute diagnostics, and the delivery of precise care under pressure.
Within the IMS, many of our faculty, whether in research, in clinical practice, or both, are navigating these complexities every day to improve evidence-based outcomes for patients of all backgrounds coming through the ED.
In this issue, we feature faculty whose work spans many different avenues of Emergency Medicine research. Dr. Jacques Lee is investigating the impacts of delirium and loneliness on the geriatric population in the ED; Dr. Muhammad Mamdani is harnessing the power of AI to improve wait times and system-wide efficiency in the ED; and, Dr. Brodie Nolan is studying the use of prehospital and transfusion protocols to improve trauma survival.
Our viewpoint articles broaden the conversation even further, covering important and diverse topics that are relevant and growing in the field of Emergency Medicine today: pain management in the ED; the use of synthetic platelets for trauma healing; the rural emergency care crisis across Canada; the impact of the youth mental health crisis on EDs; worsening emergency wait times; the ethical integration of AI in the ED; and even featuring a new ED peer-support program right here at Mount Sinai Hospital in Toronto.
In addition, this issue’s spotlight pieces highlight the achievements of some outstanding members of the IMS community–including faculty member Dr. Liisa Galea; students Mariam Elsaway and Shannen Kyte; alumnus Dr. Aravin Sukumar; and staff member Caroline Ruvio.
As always, we are grateful for our journalists, editors, and designers for bringing this issue, like every issue, to life. We hope this Winter Issue inspires deeper curiosity and reflection with the pressing questions and fast-moving world that define Emergency Medicine today.
Sincerely,
Kristen is a PhD student studying the use of a human-based retinal organoid model to investigate cell therapies for genetic eye disease under the supervision of Dr. Brian Ballios at the Krembil Research Institute.
@K_Ashworth01

Kyla Demkiv
Kyla is a PhD student studying the mechanism of action of novel therapies for lymphoma under the supervision of Dr. Armand Keating, Dr. John Kuruvilla, and Dr. Rob Laister.
@kylatrkulja




Nayaab Punjani
Nayaab is a PhD student examining a neuroprotective drug therapy for cervical-level traumatic spinal cord injury at the Krembil Research Institute under the supervision of Dr. Michael Fehlings.
@nayaab_punjani



Dear IMS Community,
I hope you were all able to have a restful holiday. On behalf of all the core staff at IMS, I would like to warmly welcome you to 2026! This IMS Magazine issue on Emergency Medicine pays tribute to the physicians and scientists who are working tirelessly to improve front-line access to care across various patient populations and research areas.
This issue features three faculty examining various facets of emergency care delivery to enhance patient-centred care. Dr. Jacques Lee is moving beyond the stigma to enhance care within the field of geriatric emergency medicine through better screening for delirium and loneliness. Dr. Muhammad Mamdani is navigating ethical and practical implications for implementing artificial intelligence within the emergency department— developing tools that include improving triage, nurse scheduling, and vital signs monitoring. Finally, Dr. Brodie Nolan is optimizing early-access transfusion protocols to improve trauma survival.
In addition to faculty, this issue places a spotlight on multiple IMS community members. The faculty spotlight is Dr. Liisa Galea who speaks about her journey as a researcher and her advocacy work within the field of women’s health. Mariam Elsawy and Shannen Kyte, co-recipients of the Jay Keystone Award, share the student spotlight for their initiative MedComics Con which will occur in Spring 2026, and Dr. Aravin Sukumar, alumnus of IMS, explains his transition to the field of scientific communications from academia. This issue also places a special staff spotlight on Caroline Ruivo, Executive Assistant to the Director and Faculty Affairs Administrator, speaking about the intersection of art and science and showcasing her own artwork. Finally, this issue highlights the 2025 Ori Rotstein Lecture in Translational Research by Dr. Karen Reue, which focused on how sex chromosomes and hormones shape health and disease in different ways.
I am extremely proud of the tremendous work the IMS Magazine team of journalists, editors, photographers, and designers contribute to prepare each iteration of the IMS Magazine. I would like to particularly commend the Editors-in-Chief Kristen, Kyla, and Nayaab, as well as Design Team Co-Directors Jinny and Ravneet for their collaborative guidance and leadership in putting this issue together.
Wishing everyone the very best in the New Year, and I hope that the articles in this issue will serve as inspiration as we work towards improving patient care within translational emergency medicine.
Sincerely,
Dr. Lucy Osborne Interim Director, Institute of Medical Science


Beatrice Acheson is a second-year MSc student working under the supervision of Dr. Peter St George-Hyslop at the Tanz Centre for Research in Neurodegenerative Disease, where she investigates the genetic and molecular mechanisms underlying microglial dysfunction in Alzheimer’s Disease. In addition to her research, Beatrice enjoys trivia and solving the New York Times Crossword Puzzle.
@bea.acheson

Jasmine Amini is a second-year MSc student working under the supervision of Drs. Daphne Korczak and Samantha Anthony at the Hospital for Sick Children. Her research interests lie in social media use and family functioning among youth with an acute self-harm or suicide-related concern. Outside of academia, Jasmine enjoys reading, volunteering, and exploring Toronto.
@Jasmine_amini9

Regina Annirood is a PhD student working under the supervision of Dr. Robert Chen at Toronto Western Hospital. Her research focuses on how transcranial ultrasound stimulation can modulate brain circuits to improve symptoms in people with Parkinson’s disease, contributing to advances in the understanding and treatment of movement disorders. Outside the lab, she enjoys travelling, pilates, reading, and spending time with family and friends.

Michellie Choi is a firstyear MSc student working under the supervision of Dr. Kazuhiro Yasufuku at the Latner Thoracic Research Laboratories and Toronto General Hospital (UHN). Her research focuses on AI applications for minimally invasive thoracic surgery and surgical guidance.

Mya Chronopoulos is a first-year MSc student supervised by Dr. Caleb Browne at the Centre for Addiction and Mental Health where she is exploring how serotonin and dopamine coordinate in the mesolimbic dopamine system to shape motivation/rewardseeking behaviour. Outside of the lab, she enjoys early morning pilates classes, spending time with family, and traveling.
@myachronopoulos

Sara Corvinelli is a PhD student supervised by Dr. Jacques Lee at the Schwartz/Reisman Emergency Medicine Institute. Her thesis is exploring innovative ways to improve delirium recognition for older people who seek emergency care. When she’s not researching, Sara enjoys ballet, nature walks, and spending time with loved ones.

Grace Gibson is a second-year MSc student in the Biomedical Communications program studying to become a medical illustrator. She aims to work in patientfacing media and outreach focused on the LGBTQ community. In her free time, Grace enjoys reading books and painting.

Alyona Ivanova is a PhD student investigating the molecular signature of glioblastoma using spatial -omics technologies at the Hospital for Sick Children under the supervision of Dr. Sunit Das. Alyona is a professional figure skater and a model. Alyona is a Creative Director of Panoramics - A Vision Inc. She enjoys traveling, cooking, and reading.
@_alyonaivanova_

Rachel Lebovic is a second-year PhD student at Sunnybrook Health Sciences Centre under the supervision of Dr. Mark Sinyor. She is studying suicide prevention through popular media as a tool to teach mental health literacy to youth. Outside of research, Rachel enjoys cooking, going for walks, and building Lego.
@rachel.lebovic

Josephine Machado is a second-year MSc student working under the supervision of Dr. Andrea Knight at The Hospital for Sick Children. Her research is focused on examining the neuropsychiatric impacts of childhoodonset systemic lupus erythematosus (cSLE) through the study of brain-aging in children with the condition. Outside of research, Josephine enjoys reading, playing the piano, nature walks, and volunteering.


Sabeeka Malik is a second-year MSc student at the SickKids Research Institute, working under the supervision of Dr. Andreas Schulze. Her research aims to determine effective substrate reduction therapy drug candidates for Mucopolysaccharidosis III (Sanfilippo Syndrome), a lysosomal storage disease. Outside of the lab, Sabeeka enjoys reading and playing card games with her friends.

Areej Mir is a first-year MSc student at Women’s College Hospital. Her research focuses on studying disparities in breast cancer treatment and care among immigrants in Ontario. She has a strong passion for health-equity focused research. She is thrilled to be a part of the IMS Magazine, helping to share stories that make health research more accessible and engaging for all audiences. Outside of academics, she enjoys volunteering in her community, exploring Toronto’s food scene, and curating creative content online.

Anna Mouzenian is a second-year MSc student working under the supervision of Dr. Victor Tang and Dr. Daniel Felsky at the Centre for Addiction and Mental Health. Anna is investigating the use of wearable devices to predict outcomes for substance use disorders. In her free time, she enjoys dancing, hiking and pilates.

Gharaza Nasir is a second-year MSc student at the Toronto General Hospital Research Institute, working under the supervision of Dr. Arndt Vogel. Her research utilizes patient-derived xenograft (PDX) models to investigate tumour dynamics and evaluate potential therapeutic strategies for Cholangiocarcinoma. In her free time, Gharaza enjoys working out, playing video games, and spending time with friends and family.
@g.harazanasir

Kinjal Parekh is a firstyear MSc student at St. Michael’s Hospital, working under the supervision of Dr. Andras Kapus. Her research is focused on uncovering the mechanism of a novel inhibitor targeting the YAP/TAZ transcription factors, central regulators whose overactivation drive cancer and fibrosis. Outside of research, she enjoys cooking, playing badminton, and nature walks.
@kinjalparekh09

Ana Piric is a secondyear MSc student at the Princess Margaret Cancer Research Tower working under the supervision of Dr. Aaron Schimmer. Her research is focused on the molecular targeting of the mitochondrial protease LONP1 in cellular and mouse models of acute myeloid leukemia (AML). In her free time Ana enjoys yoga, reading, and exploring the food scene in Toronto!
@anapiric18


Anita Rajkumar is a second-year MSc student at Women’s College Hospital, working under the supervision of Dr. Joanne Kotsopoulos. Her research aims to understand hormonal contraceptive use and breast cancer risk among BRCA carriers. In her free time, Anita enjoys reading, running, and trying new restaurants.
@anita.raj_

Rebecca Smythe is a first-year MSc student at Women’s College Hospital working under the supervision of Dr. David Lim. Her research aims to better understand the lived experiences of transgender and gender diverse (TGD) individuals navigating breast cancer care, across the entire care continuum from screening to survivorship. Outside of her work Rebecca enjoys reading, travelling, and spending time with loved ones.
@beckyysmythe

Alicia Tran is a first-year MSc student working under the supervision of Dr. Lihi Eder at Women’s College Hospital. Her research explores sex differences in response to advanced therapies in patients with psoriatic arthritis. Outside of the lab, she enjoys exploring Toronto with her sister, vintage shopping, and baking new recipes for the holiday season.
@aliciaxtran

Shreya Vasudeva is a first-year MSc student at the Poul Hansen Family Centre for Depression under the supervision of Dr. Joshua Rosenblat. Her research focuses on investigating the abuse liability of ketamine when prescribed for treatment-resistant mood disorders. Outside of research, Shreya loves movies, spending time with family and friends, trying new cafes around the city!

Saleena Zedan is a second-year MSc student at the Centre for Addiction and Mental Health, being supervised by Dr. George Foussias. Her research is focused on investigating the role of gender-identity and socioenvironmental variables in predicting recovery outcomes for individuals with psychosis. Saleena enjoys spending time with her family, friends, and dog outside of her work.
Aria Afsharian
Tesam Ahmed
Gabriela Blaszczyk
Yalda Champiri
Carmen Chan
Anthaea-Grace Patricia Dennis
Clarize Donato
Ysabel Fine
Katherine Guo
Jino Lim
Eryn Lonnee
Caroline Marr
Eliza McCann
Karan Patel
Gisany Ravichandran
Ankit Ray
Angenelle Eve Rosal
Steven Shen
Omer Syed
Serena Trang
Priya van Oosterhout
Emily Wiljer
Abigail Wolfensohn

Lizabeth Teshler (Lead) is a PhD student supervised by Dr. Brian Feldman at The Hospital for Sick Children. Her research investigates how to improve the clinical examination of musculoskeletal health for people with Hemophilia. Outside of research, she loves biking, spending time outdoors, and exploring new cities.

Lielle Ronen is a secondyear MSc student in Dr. Andrew Sage’s Lab at the Latner Thoracic Surgery Research Labs in PMCRT. Her research investigates smoking damage in donor lungs to improve post-transplant outcomes using Ex-Vivo Lung Perfusion (EVLP). Aside from research, she loves painting, baking, running and trying local restaurants in Toronto.
Abigail Wolfensohn is a second-year MSc student in Dr. Mojgan Hodaie’s lab at Toronto Western Hospital. She is researching how the brain’s waste-clearance system functions in people with trigeminal neuralgia, a chronic facial pain condition. In her free time, she enjoys outdoor activities, puzzles, trying new restaurants, and playing the piano.
@abbywolfen
The IMS Design Team is a group of 2nd-year MSc students in the Biomedical Communications (BMC) program. Turning scientific research into compelling visualizations is their shared passion, and they are thrilled to contribute to the IMS Magazine.

Ravneet Jaura (Co-Director) ravneetjaura.com

Jinny Moon (Co-Director) jinnymoon.ca
@artby_reetu @jmoon.vis

@athna.stomosis @qiy_o_0 liathena101.wixsite.com/portfolio

@viyxlin @jpetrusavisuals
Josip Petrusa josippetrusa.com
Raymond Zhang helloimraymond.github.io
@rayz_the_roof
By Sara Corvinelli
“Unless you’re a paediatrician or an obstetrician, you’re a geriatrician,” says Dr. Jacques Lee, an emergency physician at Mount Sinai Hospital and Research Chair in Geriatric Emergency Medicine (GEM) at Schwartz/Reisman Emergency Medicine Institute (SREMI). The field of GEM aims to address the unique and unmet needs of older people who seek emergency care.1 With a growing aging population, patients 65 years and older account for over 25% of all Emergency Department (ED) visits in Canada as of 2014.2 The future of emergency medicine demands attention to how well we care for this older population.
Older people are especially vulnerable to complex care challenges, including falls, delirium, and loneliness, but they are often overlooked in a fast-paced ED. While our population continues to age, the significant demographic shift termed the “Silver Tsunami” is imminent in emergency care. To address this, leaders in GEM are working towards novel solutions and advocacy for age-friendly practices in the ED. Dr. Lee’s research program encourages slowing down and recognizing the person behind the patient.
Dr. Lee’s path to improving emergency care for older people was shaped by clinical insight and research training. He pursued his medical education at the University of Alberta and completed a residency in emergency medicine at McGill University. Following this, Dr. Lee
began his scientific career at Sunnybrook Hospital, where he conducted research in management and measurement of acute pain. In his clinical practice, he noticed the shifting demographics in the ED—a rising number of seniors—and recognized a growing need to further optimize the merging of emergency and geriatric care. In 2018, he joined Sinai Health and was named the Inaugural Research Chair in GEM at SREMI.
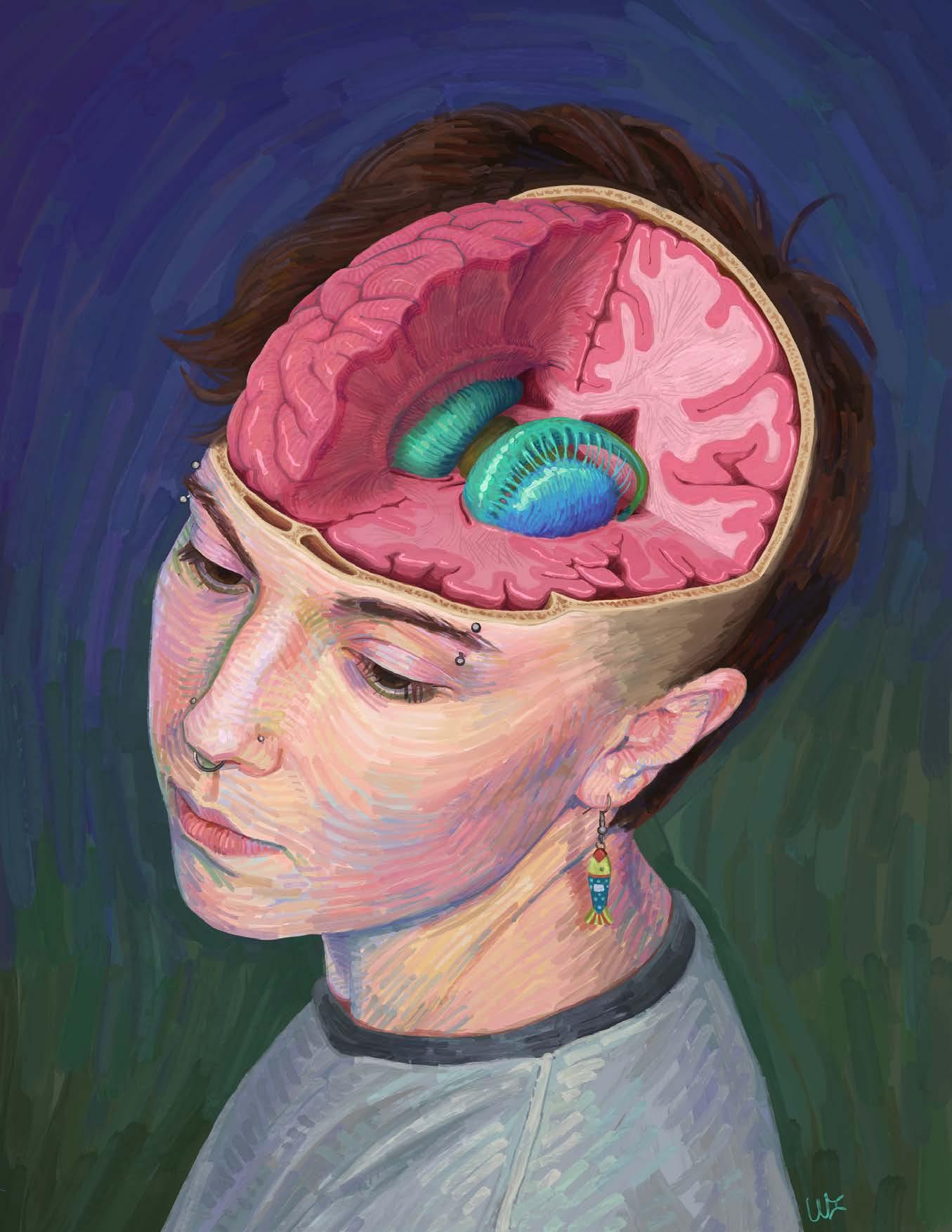
Dr. Lee’s research stands on two key pillars, both of which are rooted in the context of caring for aging adults in the ED. The first explores delirium, a serious and common condition characterized by a sudden change in mental state. Delirium is underrecognized by ED staff despite its association with a three-fold increased risk of death.3 The second examines social isolation and loneliness, a crisis that impacts both mental and physical health of older adults, as loneliness is “just as bad for you as smoking a pack of cigarettes a day,” Dr. Lee says.4 Delirium and loneliness can be lethal, but are often overlooked as they present with less obvious, more insidious symptoms than other afflictions in the ED.
Delirium affects around 12% of older people who seek care at Canadian EDs.3 It is associated with prolonged hospitalization, loss of independence, and increased risk of cognitive decline and mortality.3 However, delirium remains poorly understood by researchers and
clinicians. “After 400 years, no one knows what’s actually going on in the brain when you have delirium,” Dr. Lee says. The real breakthrough lies in understanding what causes delirium, and finding a test that provides an objective diagnosis, thereby increasing recognition rates.
In pursuit of this breakthrough, Dr. Lee is investigating biomarkers and measurable changes in the body that provide insights into a person’s health. To do so, Dr. Lee and his team are analyzing urine samples of older adults with hip fractures who are at risk of delirium. Urine samples were collected in the ED at baseline, then twice daily to track delirium development. Dr. Lee aims to identify changes in metabolites associated with the onset of delirium in hopes of enhancing our current understanding of the underlying pathophysiology. Discovery of biomarkers associated with delirium onset may enable the development of diagnostic tools for earlier recognition of delirium in the ED.
In parallel to understanding what causes delirium, there is a dire need to improve its prompt recognition. “The best delirium recognition rate in the emergency department is 50%. If your child brings that report card home, you don’t put it up on the fridge,” says Dr. Lee. To address this, his research team is conducting a multi-centre prospective cohort study, called Better ED Delirium Recognition (BEDDeR), which will compare innovative


Dr. Jacques Lee MD, MSc, FRCPC Emergency Physician, Mount Sinai Hospital Schwartz/Reisman Emergency Medicine (SREMI) Research Chair, Geriatric Emergency Medicine Associate Professor, University of Toronto
strategies to recognize delirium in the ED, including the use of tablet games and hospital volunteers administering a simple screening tool. The findings will support the creation of solutions to improve delirium recognition rates. “We must move past, ‘delirium recognition is terrible,’ to, ‘let’s start improving it’,” Dr. Lee emphasizes.
In addition to Dr. Lee’s research on delirium, while at the frontlines of the COVID-19 pandemic, he witnessed the emerging crisis of loneliness in elderly patients. Dr. Lee recounts the story of
We know how to measure blood pressure and pain, but not loneliness. “ “
an older patient who was brought to the ED by ambulance from an assisted living home. He vividly recalls the patient’s stark words: “He looked at me and said, ‘Don’t send me back, doctor. I’m dying of loneliness.’” Dr. Lee realized that social isolation and loneliness are profoundly underappreciated social determinants of health. This inspired the formation of his “How-RU” program of research. Patients recently discharged from the ED that experience social isolation in their current living situation are connected with hospital volunteers for weekly conversations on the phone or via video call. The program addresses loneliness among older patients, and through sub-studies Dr. Lee hopes to advance the development of evidencebased, practical tools to identify social isolation and loneliness.
Whether screening for delirium or loneliness, it is crucial to recognize that older patients are people with stories, not just medical conditions. The ED is prone to the “blue gown effect”, where “[…] an older person shows up, they’re wearing a blue gown, and they all look the same. You don’t know this person is a retired CEO and still active on their board of directors. You lose all that context. That’s what leads to mistakes,” Dr. Lee says. He looks forward to ushering in a new era of person-centred care for older people in the ED.
Dr. Lee is working toward a future where loneliness screening is routine and
delirium recognition rates improve with the use of new tools and cultural change. He hopes, “In the future, asking about loneliness in the ED will be as normal as asking [older patients] if they smoke.” The possibilities are in reach, and Dr. Lee believes that someday, we will “reach a point where we can just dip a urine test strip and know a patient has delirium or is about to get it. That would be a huge step forward.”
To ensure lasting progress, Dr. Lee is passing the torch to the next generation and encouraging more physicians to participate in GEM research. His mission is to make compassionate, evidence-based care for older adults the norm, not the exception. He envisions people saying, “Of course we needed to improve care for older people. It was horrible what we did before.” There may be resistance to change, but the evidence is clear. Dr. Lee hopes for a turning point when screening for delirium, asking about loneliness, and recognizing the person behind the patient become “so obvious that nobody even thinks twice— like washing your hands.”
References
1. Melady D, Schumacher JG. Developing a Geriatric Emergency Department: People, Processes, and Place. Clin Geriatr Med. 2023;39(4):647-58.
2. Latham LP, Ackroyd-Stolarz S. Emergency department utilization by older adults: a descriptive study. Can Geriatr J. 2014;17(4):118-25.
3. Kakuma R, du Fort GG, Arsenault L, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51(4):443-50.
4. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-37.

By Anna Mouzenian
When Dr. Muhammad Mamdani reflects on what first drew him to artificial intelligence, he recalls a simple but powerful thought: Wouldn’t it be great if a computer could look at 100,000 patients and based on learnings from these patients, tell me what to do for the one patient sitting in front of me? It’s a question that resonates strongly in the emergency department (ED), where real-time decision-making is essential.
A pharmacist by training with degrees in econometric theory and statistics, Dr. Mamdani has built a career around turning this thought into reality. As Director of the Temerty Centre for Artificial Intelligence Research and Education in Medicine (T-CAIREM) and Clinical Lead – AI for Ontario Health, he is helping to redefine evidence-based medicine for the era of big data and bringing artificial intelligence (AI) out of the lab and into clinical spaces like the ED.
Dr. Mamdani’s journey in AI began when he realized that the evidence supporting conventional clinical decision making often reflects an idealized patient sample rather than the people physicians actually treat, leaving doctors to apply sample-level averages to unique individuals. With the rise of AI, the possibility to draw on largescale clinical data to support individualised decision-making is within reach.
Few places illustrate the potential of AI more clearly than the fast-paced and complex world of emergency medicine,
where even small gains in speed or accuracy can save lives. The pace of the ED, he says, demands systems that operate in real time. “In trauma care, you can’t have an algorithm that runs every hour. It has to run every second,” Dr. Mamdani says. Previously, Dr. Mamdani was the Vice President of Data Science and Advanced Analytics at Unity Health Toronto. St. Michael’s Hospital, part of Unity Health Toronto, provides an ideal setting for these AI solutions, given its commitment to advancing artificial intelligence in healthcare and its status as one of only two Level I trauma centres in Toronto.
Several AI technologies are already reshaping the clinical space. Dr. Mamdani and his multidisciplinary team have developed over 50 AI-driven tools designed to make hospitals safer and more efficient. One of the best-known is CHARTWatch, an AI tool at St. Michael’s Hospital which continuously monitors patient data such as vital signs, lab results, and nursing notes, assessing between 150 and 170 parameters every hour to flag those at risk of unexpected death or transfer to an intensive care unit (ICU).1 Though currently used in the General Internal Medicine Ward as well as the General Surgery unit, tools like CHARTWatch hold great promise for the ED, where delayed transfer of critically injured patients to the ICU results in higher hospital length of stay and increased mortality.2
Additionally, AI scribes, now being tested in Canada and abroad, generate automated medical notes by listening
to clinician–patient conversations. At Michael Garron Hospital, for example, the introduction of an AI transcribing tool enabled emergency physicians to see 10 to 13 percent more patients per shift and spend up to two fewer hours per shift on documentation, contributing to shorter wait times and reduced administrative burden.3 Tools like these could solve massive problems facing Canadian EDs, which are plagued by overcrowding, long wait times, and physician burnout.4,5
The impact of these tools is also evident in a nurse-assignment system developed at St. Michael’s Hospital. The system reduced the time from 3 hours per day to under 15 minutes, while cutting error rates from over 20 percent to under 5 percent. Another project, ASIST-TBI6, which is currently deployed in the St. Michael’s ED, is an AI algorithm that analyzes CT scans in under 2 minutes to identify whether there is need for immediate surgical intervention as opposed to medical management, with accuracy comparable to that of neurosurgeons. In suspected stroke or traumatic brain injury, delays in identifying brain bleeds may mean the difference between recovery and death.7 Such rapid and reliable tools represent a transformational shift in care.
Though in the early phases of deployment, technologies like these could elevate emergency care by enabling AI-assisted triage, flagging urgent cases, or ordering imaging before a physician even arrives. These innovations succeed, he says, because


clinicians help build them. Instead of delivering ready-made software, his group begins by asking front-line teams, like ED physicians, what problems they most want solved. “Everybody buys in because we built the solution together,” he says.
As AI tools become increasingly prevalent in clinical care, they introduce ethical tensions that are especially acute in the ED, where decisions must be made quickly, and often without complete information. The reach and ability of these tools necessitate responsibility, and Dr. Mamdani is candid about the gray zones that accompany medical AI. One algorithm designed by his team, which identifies structurally vulnerable people who use intravenous drugs and are at high risk of death, has never been deployed despite achieving over 80 percent accuracy. Patient interviews revealed discomfort with being flagged without consent and concerns
about the stigma associated with addiction, underscoring the importance of trust and patient autonomy in AI-supported care.
Bias in AI decision-making presents another major challenge. Race data is rarely collected in Canadian hospitals, but omitting it limits the ability to meaningfully address bias. “When we ask for race information, some find it offensive,” Dr. Mamdani explains, adding that “when we don’t [ask for that information], others say it’s unethical. You can’t have it both ways.”
Clinical AI presents a difficult tradeoff between ethical idealism and lives saved. CHARTWatch, which does not include race data and has faced criticism for this limitation has nevertheless been associated with a 26% reduction in unexpected in-hospital mortality.1 He asks, “If a tool saves lives, is it ethical not to use it while we wait for perfect data?” At Unity Health, ensuring the responsible use of AI is a central priority. Projects undergo ethics review and bias assessment, and then enter a “silent testing” phase, during which models run without influencing patient care. CHARTWatch underwent nine months of silent testing before its official rollout. Rigorous evaluation and ongoing performance monitoring are essential to minimizing bias and ensuring responsible AI use in clinical practice. These frameworks reflect a serious commitment to ethical use of AI in clinical care and enable the safe, responsible integration
of AI tools into high-stakes clinical environments like the ED.
Dr. Mamdani emphasizes that training the next generation of AI researchers is critical for its continued success. For students eager to enter the field, Dr. Mamdani offers practical advice: identify what you enjoy and what you excel at and let that guide your path. “If you love math and you’re good at it, learn to code. If you’re more interested in people and processes, focus on change management or ethics. There’s a role for everyone in AI.” Dr. Mamdani’s vision is both ambitious and humanistic. His work reflects a future where AI strengthens, rather than replaces, the human connection at the heart of medicine. It’s a vision that holds promise for the ED, reshaping care by equipping clinicians with real-time insights when they matter most.
1. Verma AA, Stukel TA, Colacci M, et al. Clinical evaluation of a machine learning–based early warning system for patient deterioration. CMAJ. 2024 Sept 16;196(30):E1027–37.
2. Gregory CJ, Marcin JP. Golden hours wasted: The human cost of intensive care unit and emergency department inefficiency*. Crit Care Med. 2007 June;35(6):1614.
3. Michael Garron Hospital. MGH’s Stavro Emergency Department adopts AI transcribing tool to reduce patient wait times and address physician burnout [Internet]. Toronto (ON): Michael Garron Hospital; 2024 Nov 6 [cited 2025 Dec 16]. Available from: https://www.tehn.ca/about-us/newsroom/mghs-stavro-emergency-department-adopts-ai-transcribing-tool-reduce-patient-wait
4. de Wit K, Tran A, Clayton N, et al. A Longitudinal Survey on Canadian Emergency Physician Burnout. Ann Emerg Med. 2024 June;83(6):576–84.
5. Emergency Department Overcrowding in Canada: CADTH Health Technology Review Recommendation [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2023 [cited 2025 Dec 16]. (CADTH Health Technology Review). Available from: http://www.ncbi.nlm.nih.gov/books/NBK599980/
6. Smith CW, Malhotra AK, Hammill C, et al. Vision Transformer-based Decision Support for Neurosurgical Intervention in Acute Traumatic Brain Injury: Automated Surgical Intervention Support Tool. Radiol Artif Intell. 2024 Mar;6(2):e230088.
7. Kwon H, Kim YJ, Lee JH, et al. Incidence and outcomes of delayed intracranial hemorrhage: a population-based cohort study. Sci Rep. 2024 Aug 22;14(1):19502.

By Mya Chronopoulos and Michellie Choi
Sirens fade as the doors to the hospital swing open. Before the wheels of the stretcher even lock, a physician is already at work—glancing at monitors, issuing orders, and making split-second decisions that leave no room for hesitation. In these moments, one minute may be the difference between life and death. This is the image that comes to mind when one imagines emergency medicine. The moments preceding what happens in the trauma bay are critical—but often overlooked. These moments are the ones that Dr. Brodie Nolan aims to optimize to promote better outcomes in trauma care.
Dr. Nolan is an emergency and trauma team leader at St. Michael’s Hospital, as well as a transport physician with Ornge, Ontario’s air ambulance service. Initially uncertain of his career path, Dr. Nolan enrolled at Wilfred Laurier University for his undergraduate studies. During orientation, he witnessed a student collapse a few rows in front of him, and the coordinated response of first responders immediately drew his attention. Inspired, he began volunteering across campus, assisting first responders by supplying oxygen and medical equipment—an experience that provided early exposure to the intensity of emergency care. Dr. Nolan later attended medical school at the University of Toronto, where he gravitated towards emergency and trauma medicine. “In trauma, you’re dealing with some of the sickest patients in the country, but this allows more time to get to know one patient and their family,” Dr. Nolan says.
As a researcher, Dr. Nolan focuses on optimizing care in the first hour after traumatic injury–what trauma physicians call “the golden hour”. For trauma patients, such as those experiencing massive bleeding, timely care within this small window of time is critical for ensuring good outcomes. “In studies looking at patients with massive bleeding, for every one-minute delay in getting a blood transfusion, their odds of death go up by five percent,” Dr. Nolan says.
Speed and efficiency in trauma care depend largely on the location of the incident. As Dr. Nolan explains, “If you can’t change where people live, then you need to be able to bring the hospital to them—a challenge known as the “tyranny of distance.” While downtown Toronto is minutes away from two level I trauma facilities, many rural regions of Ontario are hours from specialized care. Through his work, Dr. Nolan hopes to eliminate this barrier to timely care.
Bridging this gap in access to timely trauma cases is the mission of Ornge, Ontario’s air ambulance service. Ornge provides rapid air and land medical transport for critically ill or injured patients across the province. Working with Ornge gave Dr. Nolan firsthand insight into how delays in trauma care occur. In one instance, Ornge was dispatched to transport an unconscious motorcyclist on the side of the highway who was struggling to breathe. After takeoff to retrieve the patient, on-site paramedics cancelled the helicopter, deeming it unnecessary. Hours later, Ornge was called again for the same patient as a transfer from a community hospital. The patient was now
unstable and severely injured. “By then, you’re well outside of that first hour,” he said. Unfortunately, the patient arrived at the trauma centre too late and died. This case highlights how miscommunication and decentralized decision-making can contribute to preventable delays in trauma care.
Such experiences encouraged him to investigate and optimize the logistics of transport medicine. Although delays in prehospital trauma care are widely acknowledged, there is limited systematic data documenting how often they occur and their consequences. Dr. Nolan and colleagues conducted an analysis of air ambulance transports to identify common sources of delay—including inclement weather, waiting for documentation, delay to intubate, among others.1 His ongoing work aims to document these patterns and help systems better identify patients that require expedited transportation to trauma centres.
Dr. Nolan is also working to improve trauma care on the ground, not just in the air. The Trauma Black Box is an educational quality improvement tool that allows for the capturing of every aspect of trauma resuscitation, including patient data and the procedural environment, allowing teams to review what flowed well, where delays happened, and how future performance can improve.2 Dr. Nolan describes this technology as “reviewing game footage after a big sports game. It’s not for blame, but rather for learning.”
Beyond improving logistics and team performance, Dr. Nolan’s research also centres around how and when blood is given to trauma


Institute of Medical Science, Institute of Health Policy, Management and Evaluation
patients experiencing severe bleeding. Prior to World War I, bleeding patients were given intravenous saline. While this temporarily restored blood pressure, saline is insufficient given its lack of oxygen and clotting factors. During the war, battlefield surgeons realized that delivery of whole blood—containing red blood cells, plasma, and platelets—is more effective, as it has crucial features that saline lacks.3 By the 1960s and 1970s, however, trauma care shifted to component therapy, in which donated blood is separated into its individual parts—red blood cells, plasma, and platelets. With this method, a single donation could help multiple patients—for example, someone with chronic anemia (low red blood cell count) could use a transfusion of just red blood cells, without the other components. This approach improved safety, efficiency,
and resource management, reducing adverse reactions by moving away from the one-sizefits-all model of whole blood transfusion.3
Although component therapy has become the most popular method of blood transfusion, a 2015 study suggested that trauma patients did better when given blood products in a 1:1:1 ratio (plasma:platelets:red blood cells), effectively recreating whole blood.4 More recent advances, like leukoreduction filters that safely remove white blood cells—which are responsible for many transfusion adverse reactions, including fevers, inflammation and immune complications—have made whole blood transfusion safer. It still remains uncertain which approach, component therapy or the new methods of whole blood transfusion, offers the best outcomes in trauma care.
These uncertainties prompted the development of the Study of Whole Blood in Frontline Trauma Canada (SWiFT), a national prehospital transfusion trial, co-led by Dr. Nolan, that investigates the efficacy of whole blood transfusion for patients experiencing severe bleeding.5 The study is currently recruiting patients and is still ongoing to develop conclusive results, but Dr. Nolan notes that while component therapy may be advantageous in classical care settings, whole blood transfusion has many potential advantages in high-pressure settings. “In a helicopter, you have two paramedics, a critically injured patient, and a lot going on,” he says. “Being able to administer a single bag [of whole blood], as opposed to two or three bags [separated into components], simplifies a lot.”
In a trauma bay with 30 people and endless resources, these logistics aren’t as daunting, but in the air, where space, time, and hands are limited, simplicity matters.
Dr. Nolan is pursuing multiple avenues to make great strides in trauma care. He is sustained in large part by his gratitude and the opportunity to work three different jobs that he loves: emergency shifts, trauma team leadership, and transport medicine. Each demand something different but still reinforce the others. “Emergency medicine is such a team sport,” he says. “There’s not that hierarchy that sometimes exists within medicine, everyone’s kind of just moving and doing what they can for the best of patients.” Whether he is at the bedside, in the trauma bay, or guiding paramedics from hundreds of kilometres away, his philosophy is grounded in urgency: acting early, decisively, and doing everything possible to keep patients within the critical window of timely care is essential to ensuring better outcomes in trauma care.
1. Nolan B, Haas B, Tien H, et al. Causes of Delay During Interfacility Transports of Injured Patients Transported by Air Ambulance. Prehosp Emerg Care. 2019;24(5):625-33. doi:10.1080/10903127.2 019.1683662
2. Nolan B, Hicks CM, Petrosoniak A, et al. Pushing boundaries of video review in trauma: using comprehensive data to improve the safety of trauma care. Trauma Surgery & Acute Care Open. 2020;5(1):e000510. doi: 10.1136/tsaco-2020-000510
3. Nolan B, Schellenberg M, Ball CG, et al. Evidence Based Reviews in Surgery: a critical appraisal of whole blood resuscitation in injured patients. Canadian Journal of Surgery. 2025; 68(3):E271-3. doi: 10.1503/cjs.009924
4. Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of Plasma, Platelets, and Red Blood Cells in a 1:1:1 vs a 1:1:2 Ratio and Mortality in Patients With Severe Trauma: The PROPPR Randomized Clinical Trial. JAMA. 2015;313(5):471-82. doi:10.1001/jama.2015.12
5. Antonacci G, Williams A, Smith J, et al. Study of Whole blood in Frontline Trauma (SWiFT): implementation study protocol. BMJ open. 2023;14(2):e078953. doi:10.1136/bmjopen-2023-078953

Winter is a medical illustrator with an interest in 2SLGBTQ+ health communication. He specializes in creating educational pieces for gender-affirming care. Style and aesthetics are just as important as accuracy in his work, as seen by his unique use of fine arts techniques in digital work.


Chloe Friesen is a first year MSc student in the biomedical communications program at the University of Toronto. She is passionate about the value of clear, high quality visuals for facilitating communication, especially in a healthcare setting.


Yvonne Ma is a first-year MSc student in the Biomedical Communications program, training to become a medical illustrator. With a strong background in art, she is passionate about integrating medical knowledge with visual storytelling. Yvonne aims to bridge art and science by making complex concepts accessible to diverse audiences through clear and engaging visuals.

Ravneet Jaura is a biomedical communicator in her 2nd year studies at the Master of Science in Biomedical Communications. Combining her unique experience as a scientist and researcher, she aims to communicate science with accuracy. Ravneet is particulary interested in storytelling through infographic visualization and animation. More of Ravneet’s work can be found at: www.ravneetjaura.com.
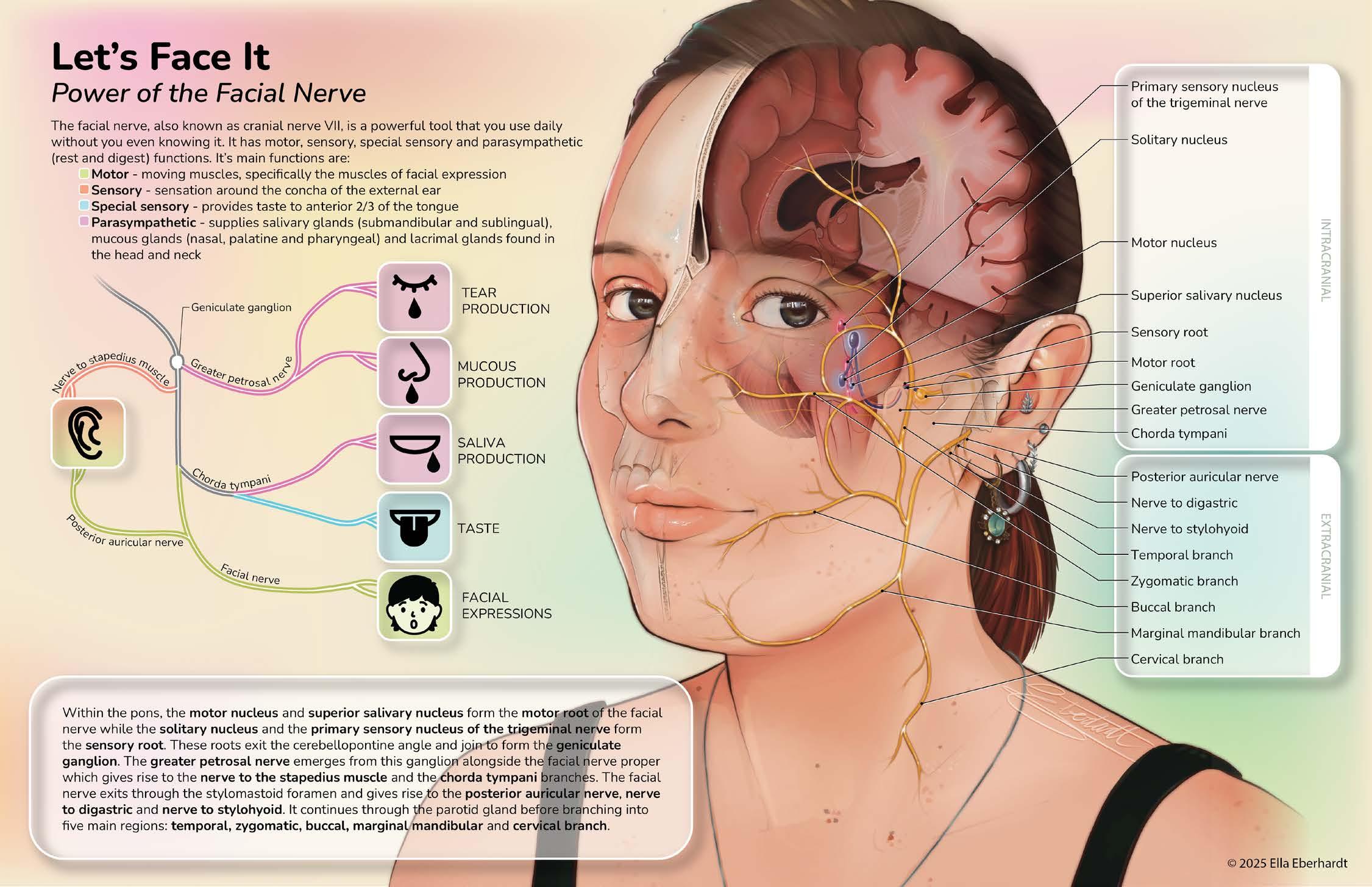

Ella is currently a second year MScBMC student at the University of Toronto. Her thesis is focused on creating patient education material for people experiencing facial palsy (paralysis) whether that be due to Bell’s palsy, congenital or otherwise. The goal is to create work that inspires people to understand more about their bodies.


Angela is a first year MScBMC student and a former high school biology/visual arts teacher. Her background in education and instructional design has shaped her commitment towards dismantling scientific illiteracy and student apathy.
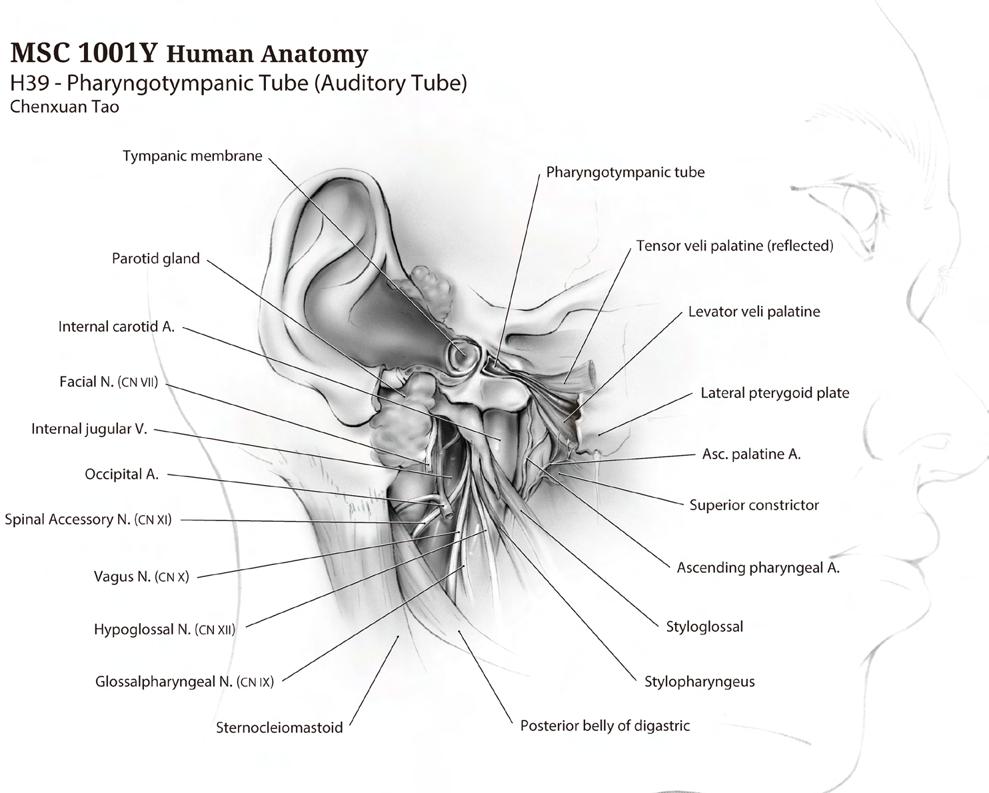

Chenxuan Tao is currently enrolled as a first year MScBMC student. His works aim to explore the balance of aesthetic attraction and scientific accuracy, making knowledge more accessible and interesting.

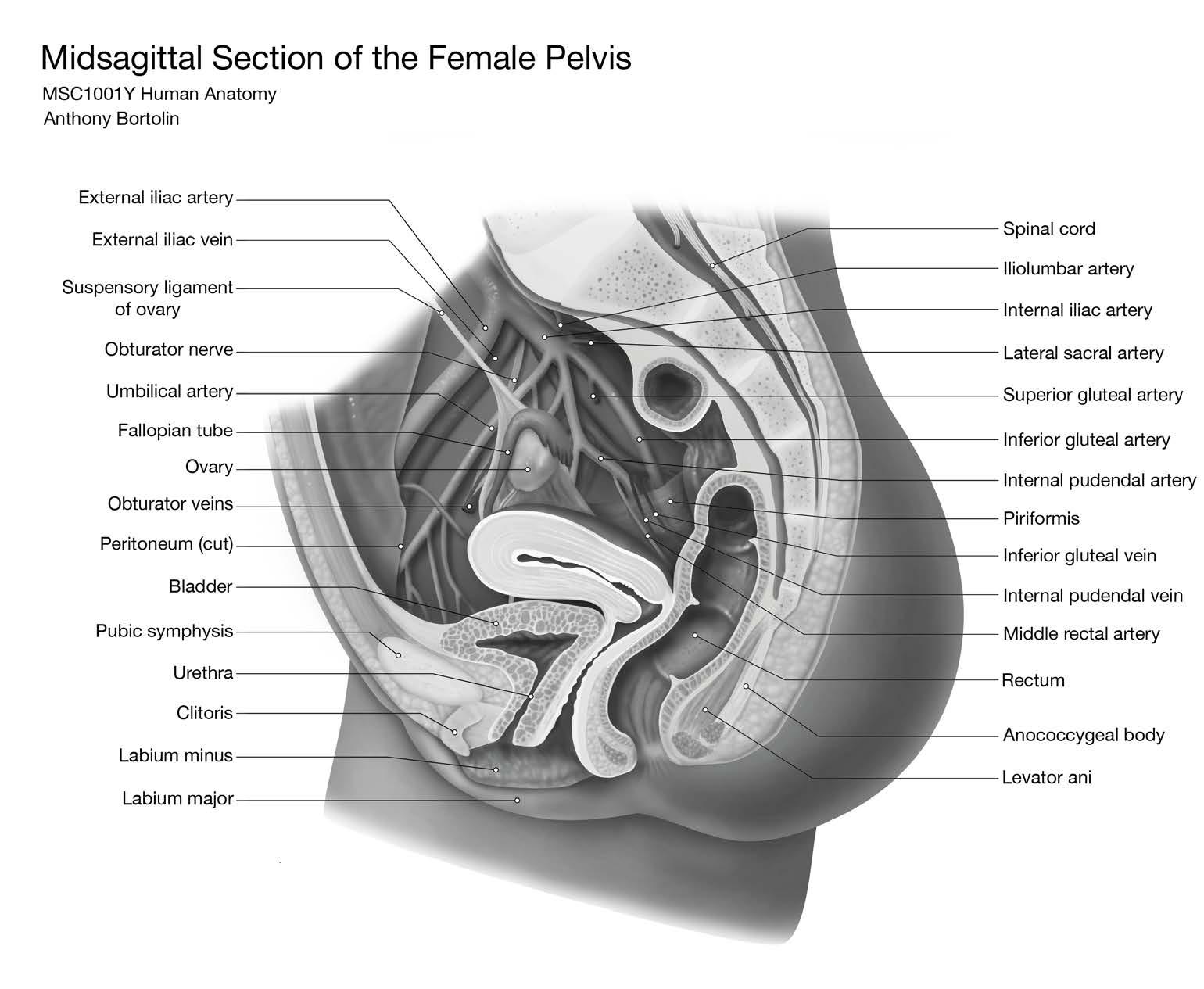
Anthony Bortolin is a first-year Biomedical Communications student at the University of Toronto with a passion for 3D scientific communication. He focuses on anatomydriven visuals that bridge accuracy and clarity.

By Saleena Zedan
“Can I please have more medication? I’m still in a lot of pain,” I asked my doctor in the emergency department (ED) after suffering excruciating pain from two slipped discs in my lower spine. I was denied an increased dose due to concerns about developing an opioid addiction from the ED—a prevalent issue across North America.1 Although I posed no risk for addiction, it did not matter; I had to persevere through the pain.
My experience is not unique—up to 94% of patients report feeling dismissed across all medical settings by their physicians.2 This feeling can be especially difficult in the ED, where patients often arrive in acute pain and distress. This demonstrates how easily pain can be minimized in emergency settings and highlights the need for change in the ED that places care at the forefront.
In Canada, pain management in the ED is suboptimal. Increasingly, patients are reporting longer wait times for pain relief, often exceeding two hours after initial contact.3,4 These prolonged delays may result in limited opportunities for physicians to conduct thorough assessments with their patients. This may contribute to decisions regarding prescription of pain medication being made quickly, without fully understanding patients’ pain or risk of addiction. As a result, pain management may become shaped by quick judgements based on
previous experiences with other patients rather than individualized care.
These are not the only concerns, as research shows inequity in pain management. Older adults often wait longer in the ED for pain-relieving medication compared to younger adults.4 While 70% of ED physicians report that patient age influences their prescribing practices, the extent to which this affects actual prescribing remains unclear.5 Race and ethnicity have also been found to negatively impact pain-management and wait times in the ED.6 Specifically, patients belonging to minority groups in the ED are less likely to receive adequate pain management and more likely to endure longer wait times before assessment or treatment. A scoping review found that in 11 (91%) out of 12 studies on ED wait times, minority groups waited longer than White patients to be seen.6 Meanwhile, in terms of pain treatment, six (35%) of 17 studies found that minority groups were less likely to receive any analgesics and 11 (85%) of 13 studies found that they were less likely to receive opioids.6 Another study using data from 2013–2017 found that Black and Hispanic patients had significantly longer wait times than White patients, waiting 47-50 minutes for pain medication compared to 36-40 minutes.7 This difference was seen even after controlling for triage level and hospital factors, once more raising concerns about delayed access to timely pain relief in the ED. Together, these findings demonstrate
that inequitable pain management in the ED may be shaped by unconscious assumptions that influence patient’s care.
Inequities in the pain management process are exacerbated by the history of opioid overprescription in the ED. Opioid overprescription in the ED began as a result of Purdue Pharma marketing the opioid oxycontin as safe and effective with little chance of developing an addiction in the 1990s.8 Consequently, between 2001-2010, prescribing opioids in the ED increased by approximately 10%.9 This history continues to influence practice today, creating a complex landscape in which physicians must balance the risk of undertreating pain with concerns about opioid-related harm. Although best practices recommend trying non-opioid options first,10 these alternatives are often limited and may be insufficient for severe pain. While new non-opioid medications such as Suzetrigine offer promise, they are not yet widely available and therefore do not meaningfully expand current ED treatment options.11,12 This lack of accessible, non-opioid treatments makes it challenging for physicians to balance two competing priorities of relieving patients’ pain while minimizing the potential for long-term opioid use.
Recent evidence illustrates this tension: a recent study found that most ED opioid prescriptions do not lead to persistent use, although small increases in use were observed in some patients, which helps explain why healthcare providers

remain careful when contemplating a prescription.13 However, at the same time, several patients in the ED still received opioid prescriptions even when they reported low pain ratings.14 Prescribing also varies widely across hospitals. A study that compared opioid prescriptions across three Canadian hospitals found that patients presenting to one ED were roughly 3.5 times more likely to be prescribed an opioid than patients at the other two, suggesting that the practices that are in place are not routinely followed across hospitals.10 These inconsistencies, paired with documented inequities in treatment, reveal how both caution and bias can shape management decisions in the ED.
It is unclear whether there is a relationship between opioid overprescription in the ED and the current opioid epidemic in Canada. To better understand whether ED opioid prescriptions play a role in Canada’s opioid crisis, future research could investigate long-term patient outcomes or examine how hospital-level prescribing practices may affect community-level harm. Regardless if there is a link between opioid prescription and the epidemic, overprescription of opioids remains an issue if individuals are being prescribed opioids unnecessarily and their core concerns are being overlooked.
In my case, as a young woman requesting additional medication, I may have been perceived as someone at a higher risk for opioid misuse, which resulted in the denial
of the treatment I needed. My experience reflects the broader patterns described, that pain management in the ED can be influenced by assumptions. These biases contribute to the documented inequities of longer wait times, undertreatment, and limited access to non-opioid medications in the ED. Addressing these issues requires greater awareness of how these assumptions shape clinical decisions and a commitment to providing equitable pain care across patients entering the ED.

1. Canada PHA of. Opioid- and stimulant-related harms in Canada: Key findings [Internet]. 2025 [cited 2025]. Available from: https:// health-infobase.canada.ca/substance-relatedharms/opioids-stimulants/
2. Kennedy LP, Quimby D. What you told us about medical gaslighting [Internet]. HealthCentral; 2023 [cited 2025 Dec 6]. Available from: https://www.healthcentral.com/chronic-health/what-you-told-usabout-medical-gaslighting
3. Woolner V, Ahluwalia R, Lum H, et al. Improving timely analgesia administration for musculoskeletal pain in the emergency department. BMJ open quality. 2020;9(1):e000797.
4. Mills AM, Edwards JM, Shofer FS, et al. Analgesia for older adults with abdominal or back pain in emergency department. The western journal of emergency medicine. 2011;12(1):43–50.
5. Varney SM, Bebarta VS, Mannina LM, et al. Emergency medicine providers’ opioid prescribing practices stratified by gender, age, and years in practice. World Journal of Emergency Medicine. 2016;7(2):106. doi:10.5847/wjem.j.1920-8642.2016.02.004
6. Owens A, Holroyd BR, McLane P. Patient race, ethnicity, and care in the emergency department: A scoping review. Canadian journal of emergency medicine. 2020;22(2):245–53.
7. Lu FQ, Hanchate AD, Paasche-Orlow MK. Racial/ethnic disparities in emergency department wait times in the United States, 2013–2017. The American Journal of Emergency Medicine. 2021 Sept;47:138–44. doi:10.1016/j.ajem.2021.03.051
8. Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy. American Journal of Public Health. 2009;99(2):221-227.
9. Mazer‐Amirshahi M, Mullins PM, Rasooly I, et al. Rising Opioid Prescribing in Adult U.S. Emergency Department Visits: 2001–2010. Academic emergency medicine. 2014;21(3):236–43.
10. Gomes T., Hamzat B, Holton A, et al. Trends in Opioid Prescribing in Canada, 2018 to 2022 [Analysis in brief on the Internet]. Canada’s Drug Agency; 2025 [cited 2025]. 15 p. Available from: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.cda-amc. ca/sites/default/files/hta-he/HC0071_Summary%20Report_EN.pdf
11. Mohiuddin AL, Ahmed Z. Suzetrigine – a novel fda‐approved analgesic – opportunities, challenges and future perspectives: A perspective review. Health Science Reports. 2025 Nov;8(11). doi:10.1002/hsr2.71545
12. Commissioner O of the. FDA approves novel non-opioid treatment for moderate to severe acute pain [Internet]. FDA; 2025 [cited 2025 Nov 29]. Available from: https://www.fda.gov/news-events/ press-announcements/fda-approves-novel-non-opioid-treatmentmoderate-severe-acute-pain
13. Hayward J, Rosychuk RJ, McRae AD, Sinnarajah A, Dong K, Tanguay R, et al. Effect of emergency department opioid prescribing on Health Outcomes. Canadian Medical Association Journal. 2025 Feb 9;197(5). doi:10.1503/cmaj.241542
14. McNeil CL, Habib A, Okut H, et al. Administration and Prescription of Opioids in Emergency Departments: A Retrospective Study. Kansas journal of medicine. 2021; 14:1–4.

By Kinjal Parekh
Imagine being a paramedic treating a trauma patient who’s bleeding uncontrollably. Every second feels like a countdown, yet your options are limited. The patient needs platelets to survive, but those lifesaving cells are stored within hospital blood banks, far from the scene of the crisis. Severe hemorrhage is the leading cause of death among trauma patients before they reach the hospital, and it accounts for up to 40% of in-hospital trauma fatalities.1 Given this reality, what if synthetic platelets were readily available to quickly reach the site of injury and stop bleeding?
Though this may sound like science fiction, it could soon become a reality, thanks to synthetic platelets which are designed to mimic the wound-healing functions of natural platelet and hold immense potential to transform trauma medicine.2 If proven safe and effective, they could one day become a routine treatment for first responders and clinicians to control blood loss and save countless lives.2 For now, however, further testing and careful clinical translation remain essential.
Platelets play a critical role in the body’s defense against blood loss. When a blood vessel is injured, they sense the damage, travel to the site, and trigger the coagulation cascade, a chain reaction that forms a stable clot and stops bleeding. Without them, even minor injuries could become fatal.3
The current standard of treatment for severe bleeding is the transfusion of blood products, such as platelets.2 While lifesaving, these donated platelets have notable limitations. They have a short shelf life of five days and must be stored at room temperature while constantly being shaken to prevent clumping, making them difficult to transport and maintain.2 They can also trigger immune reactions in recipients and carry a risk of bacterial contamination, making them the blood component most frequently associated with transfusion-related sepsis.4
These clinical challenges are compounded by supply shortages. In 2022, the American Red Cross declared its first-ever national blood crisis, reporting the worst shortage in over a decade. Hospitals were forced to delay vital transfusions, and platelet donations were in particularly short supply,5 underscoring the urgent need for sustainable, alternative ways to manage bleeding emergencies.
Efforts to improve bleeding management have led to several alternative approaches. Recombinant clotting factors, which are lab-produced versions of the body’s natural clotting proteins, can help restore coagulation in certain conditions, but their high cost limits widespread use, particularly in low-resource or emergency settings.6 Another option is topical sealants, often used in surgery, which can help control external bleeding by forming a physical barrier over wounds.7 However, they are ineffective against internal bleeding, which remains one of the leading
causes of preventable death in trauma.7 These limitations have driven scientists to explore a new frontier: artificial plateletmimetic materials that can work with the body’s own repair mechanisms. Such technologies could one day bridge the gap between current treatments and the urgent need for safe, shelf-stable, and rapidly deployable solutions.
A promising advance comes from the lab of Dr. Ashley Brown, an associate professor in the Joint Department of Biomedical Engineering at North Carolina State University and the University of North Carolina at Chapel Hill. Her team has developed platelet-like particles (PLPs), synthetic materials designed to replicate the key behaviours of natural platelets.2
These PLPs are made from ultrasoft hydrogels, which are soft, water-based polymers that can deform and respond dynamically to their environment. What makes them remarkable is their ability to recognize and bind to fibrin, a protein that naturally forms at injury sites to stabilize blood clots. This fibrin-targeting mechanism acts as a biological “homing signal,” guiding the synthetic platelets directly to the wound.7 Once attached, the PLPs change shape and contribute to clot retraction, a critical process that pulls the wound edges together and strengthens the clot, just as real platelets do. This helps seal the injury and may also accelerate tissue repair and recovery.7

In preclinical studies, these synthetic platelets have shown highly encouraging results. In mouse models of liver injury, PLPs rapidly localized to the site of bleeding and significantly reduced blood loss compared to natural platelet transfusions. Treated animals displayed smaller wounds, more stable clots, and faster recovery. Similar outcomes were observed in rat and pig models, where PLP treatment led to reduced bleeding and effective clot formation.7
Importantly, the particles did not accumulate in major organs like the liver, a common concern for nanoparticlebased therapies. Instead, they were safely filtered and cleared by the kidneys within hours. Even in healthy animals without injury, PLPs circulated harmlessly without triggering unwanted clotting elsewhere. This selective, injury-dependent activity is a major step forward in ensuring both safety and precision.7
In addition to their safety profile and efficient wound healing, synthetic platelets offer another key benefit: their availability. These platelets can be produced in laboratories, making them readily available to patients regardless of blood type, which is a major advantage in emergencies where time is critical. Because their production does not rely on blood donations, they could help overcome ongoing platelet shortages and ensure a consistent, highquality supply.8
Dr. Ronald Warren, a program director in the Division of Blood Diseases and
Resources at the National Heart, Lung, and Blood Institute, explains, “By developing a new generation of treatment options for emergency medicine, this research may help improve patient outcomes while potentially reducing healthcare costs.”2
Dr. Brown’s team is now exploring how best to store these particles. Early findings show they can be freeze-dried, making them ideal for ambulances, military settings, and remote areas, or kept in liquid form for hospital use. With continued refinement and testing, synthetic platelets could soon offer a safe, scalable, and lifesaving tool for controlling bleeding.2
While the results are exciting, innovation in medicine always requires careful testing. These synthetic platelets, though impressive, do not yet replicate all the complex functions of natural ones, including how real platelets work together to build and strengthen a clot. So far, they have only been tested in experimental settings, where they were given as a single treatment and not in combination with other therapies. In the future, researchers will need to evaluate how well they work alongside regular platelets or other bleeding treatments, and whether repeated doses are safe and effective.7 Most importantly, there have been no in-human clinical trials yet, which is critical for these synthetic platelets to become a reality.7
Nonetheless, even in these early stages, the potential of synthetic platelets is undeniable. Representing a new generation of trauma care, these engineered particles, with continued research, collaboration, and cautious optimism, could one day become a standard treatment in trauma settings, transforming how we save lives when every second counts.

1. Raykar NP, Makin J, Khajanchi M, et al. Assessing the global burden of hemorrhage: The global blood supply, deficits, and potential solutions. SAGE Open Medicine. 2021 Jan;9:205031212110549.
2. A potential game-changer for emergency medicine: synthetic platelets. National Heart, Lung, and Blood Institute. 2024. Available from: https://www.nhlbi.nih.gov/news/2024/potential-game-changer-emergency-medicine-synthetic-platelets
3. Holinstat M. Normal Platelet Function. Cancer and Metastasis Reviews. 2017 Jun;36(2):195–8. Available from: https://www.ncbi. nlm.nih.gov/pmc/articles/PMC5709181/
4. Levy JH, Neal MD, Herman JH. Bacterial contamination of platelets for transfusion: strategies for prevention. Critical Care. 2018 Oct 27;22(1).
5. American Red Cross. Red Cross Declares First-ever Blood Crisis amid Omicron Surge. Redcross.org. 2022. Available from: https:// www.redcross.org/about-us/news-and-events/press-release/2022/ blood-donors-needed-now-as-omicron-intensifies.html
6. Blankenship C. To manage costs of hemophilia, patients need more than clotting factor. Biotechnology Healthcare. 2008 Nov 1;37–40.
7. Nellenbach K, Mihalko E, Nandi S, et al. Ultrasoft platelet-like particles stop bleeding in rodent and porcine models of trauma. Science translational medicine. 2024 Apr 10;16(742).
8. Synthetic platelets stanch bleeding, promote healing using advanced materials. National Science Foundation. 2024. Available from: https://www.nsf.gov/news/synthetic-platelets-stanch-bleeding-promote-healing.

By Ana Piric
No one expected emergency departments’ 24/7 availability to come to an end. Many rural towns across Canada are experiencing reduced emergency department hours, operating only during daylight and with planned evening and weekend closures.1 In Chesley, a small community in Bruce County, Ontario, the emergency room (ER) has been open only on weekdays from 7a.m. to 5p.m. since 2022.2,3 In addition, countless unplanned closures have left patients stranded with no option besides travelling to the closest town with an open emergency department.1 Even according to Natalie Mehra, the Executive Director of the Ontario Health Coalition, ER closures have become so severe that “it’s at the point that if a hospital ER is closed in one place, there’s no guarantee the one at the next-closest hospital is open.”2 Similarly, The Globe and Mail reports that 34% of Canadian ERs have experienced a closure since 2019, collectively totalling 1.14 million hours or 47,500 days.1
While the pandemic deepened discrepancies in rural emergency care, unequal access to care is nothing new. In 2015, just 11.8% of Canadian nurses served rural or remote communities, despite these areas representing approximately 17.8% of the population. 4 Even recent data from 2024 demonstrated only 7% of physicians in Canada practiced in rural areas.5 Recruitment and retention of healthcare workers has long been imbalanced in rural compared to urban
communities across Canada due to challenges with attracting healthcare workers. 6,7 Contributing factors include limited hospital financial resources and infrastructure, the geographic isolation of communities resulting in reduced access to transit and schools, and increased burnout in overworked hospitals. 7,8 These recruitment challenges contribute to a snowball effect of reduced access to primary and emergency care, ER closures, and ultimately, poorer health outcomes for patients in rural areas.6 Furthermore, generations of residents are faced with the difficult choice of leaving their smaller hometowns due to limited healthcare access. 1,2 With over 350 physician vacancies in Northern Ontario alone, 7 it’s clear that this already concerning issue will worsen if effective solutions are not implemented.
The cycle of instability in emergency care systems causes further problems, as unpredictable closures deter new healthcare workers from accepting positions at rural ERs.2 One solution is hiring locum physicians and nurses who temporarily step in and fill desperatelyneeded positions that would otherwise be offered as permanent roles.6,7 While this approach bridges the staffing gap, several other issues have emerged. Locum physicians and nurses are compensated by the provincial government, but hospitals often provide incentives by topping up their salary and paying for expenses such as accommodations, flights, and car
rentals.7 These financial benefits hinder long-term solutions by de-incentivizing healthcare workers from accepting permanent positions.6 Top-up practices also lead to competition for emergency care between hospitals in neighbouring towns, further contributing to poor health care outcomes.7
The Ontario and municipal governments have additionally proposed that some ERs be reclassified as urgent care centers to redistribute resources and healthcare staff based on the level of care patients require. 1 In contrast to ERs, urgent care centers (UCCs) provide same-day care for pressing, yet non-life-threatening concerns; UCCs often operate later than walk-in clinics, but close nightly. It is possible that reclassifying ERs into UCCs could lead to shorter wait times and less crowding, ensuring more timely care and improved patient outcomes.1 Conversely, the issue with reclassifying ERs into UCCs lies in the fact that round-the-clock access is no longer the status quo. Without improvements in accessing emergency care in ERs, reclassification is not a long-term solution, and inequities in accessing emergency care will be deepened. 6,9
Systemic solutions aimed at achieving long-term impacts are being implemented. As of September 2024, there has been increased funding from the Ontario government to enhance physician compensation in ERs and standardise pay for physicians in rural
areas.10 In August 2025, the Ontario government aimed to address nursing shortages by expanding the number of nursing training and education seats at Ontario colleges and universities.11 To alleviate physician shortages, the Northern Ontario School of Medicine has established a social accountability mandate to promote medical school enrollment from students in rural, Francophone, and Aboriginal communities in Northern Ontario and to encourage graduating physicians to practice in their home communities.12 This program has successfully retained 50% of physicians in independent practice within Northern communities; however, more physicians continue to settle in larger centres across Northern Ontario rather than rural communities.12 As a parallel effort, initiatives like the Ontario government’s Learn and Stay grant and the Canadian government’s Canada Student Loan Forgiveness program aim to encourage healthcare program graduates to provide care in underserved rural or remote communities.13,14 Ontario’s Learn and Stay grant covers educational costs for students enrolled in priority programs such as nursing, paramedic, and laboratory technologist programs in underserved communities as long as they work a term in the same community after graduation.13 Similarly, through the Canada Student Loan Forgiveness program, family medicine physicians and residents are eligible for $60,000 in loan forgiveness while nurses are eligible for $30,000 in loan forgiveness
for five years of work in underserved or rural communities.14 It is only through continued targeted actions such as these, which address the underlying issues in attracting and retaining healthcare workers, that ERs can return to providing reliable 24/7 care.
Rural ERs are in crisis. Patients requiring immediate care are considered lucky if their local ERs are open and often have to travel to neighbouring ERs, which may or may not be open.2 Consequently, healthcare staff are discouraged from working in rural ERs, perpetuating a cycle of instability.2 Addressing discrepancies in emergency care in rural communities requires urgent, intentional decisionmaking that reflects the underlying issues in rural health care to ensure long-term impacts. While progress has been made in the right direction, continued efforts are needed to eliminate emergency care inequities in rural areas across Canada.
1. Raman-Wilims M, Thanh Ha T, Grant K. Canada’s emergency room crisis is worse than we thought. The Decibel: A Daily News podcast from the Globe and Mail [Internet podcast]. 2025 [cited 2025 Oct 25]. Available from: https://www.theglobeandmail.com/podcasts/ the-decibel/
2. Kerr P. Ontario Health Coalition warns that Chesley Hospital most at risk of closure in the province. Ontario Health Coalition [Internet]. 2023 [cited 2025 Oct 25]. Available from: https://www.ontariohealthcoalition.ca/index.php/ontario-health-coalition-warns-that-chesleyhospital-most-at-risk-of-closure-in-the-province-2/
3. Bhargava I. Rural Ontario residents offer solutions amid emergency room closures at local hospitals. CBC News [Internet]. 2024 [cited 2025 Oct 25]. Available from: https://www.cbc.ca/news/canada/ london/rural-ontario-residents-offer-solutions-amid-emergency-room-closures-at-local-hospitals-1.7383545
4. Macleod MLP, Stewart NJ, Kulig JC, et al. Nurses who work in rural and remote communities in Canada: a national survey. Human
Resources for Health [Internet] 2017;15(1). Available from: https:// dx.doi.org/10.1186/s12960-017-0209-0
5. A profile of physicians in Canada. Canada Institute for Health Sciences [Internet]. 2025 [cited 2025 November 5]. Available from: https:// www.cihi.ca/en/a-profile-of-physicians-in-canada
6. Ireton J, Ouellet V. 2024 Worst Year for Ontario ER closures, CBC analysis finds. CBC News [Internet]. 2024 [cited 2025 Oct 25]. Available from: https://www.cbc.ca/news/canada/ottawa/data-analysis-er-closures-three-years-2024-worst-year-for-scheduled-closures-1.7396789
7. Hassan S. Rural Ontario hospitals offering hefty incentives for traveling doctors amid shortage. Global News [Internet]. 2025 [cited 2025 Oct 25]. Available from: https://globalnews.ca/news/11312973/ rural-ontario-hospitals-offering-hefty-incentives-for-traveling-doctors-amid-shortage/
8. Challenges and Opportunities in Recruiting Rural Healthcare Workers. Supplemental Health Centre [Internet]. 2024 [cited 2025 Nov 10]. Available from: https://shccares.com/blog/workforce-solutions/ rural-healthcare-recruiting-challenges/
9. Ireton J. Should some rural ERs close permanently if better supports are in place? CBC News [Internet]. 2024 [cited 2025 Oct 25]. Available from: https://www.cbc.ca/news/canada/ottawa/rural-er-issuesshould-some-close-permanently-1.7402517
10. Ontario Government and Ontario Medical Association Confirm Funding Increase That Will Protect Provincial Health Care. Ontario Newsroom [Internet]. 2025 [cited 2025 Oct 25]. Available from: https://news.ontario.ca/en/release/1005805/ontario-government-and-ontario-medical-association-confirm-funding-increase-that-will-protect-provincial-health-care
11. Ontario Government and Ontario Medical Association Confirm Funding Increase That Will Protect Provincial Health Care. Ontario Newsroom [Internet]. 2025 [cited 2025 Oct 25]. Available from: https://news.ontario.ca/en/release/1006278/ontario-investing-568-million-to-expand-nursing-enrollment
12. Ross B, Newbery S, Cameron E, et al. Rurally focussed undergraduate medical education at the Northern Ontario School of Medicine University. Canadian Journal of Rural Medicine. [Internet] 2025;30(2):101-102. Available from: https://journals.lww.com/cjrm/ fulltext/2025/04000/rurally_focussed_undergraduate_medical_education.10.aspx
13. Ontario Expanding Learn and Stay Grant to Train More Health Care Workers. Ontario Newsroom [Internet]. 2023. [cited 2025 Oct 25]. Available from: https://news.ontario.ca/en/release/1002652/ontarioexpanding-learn-and-stay-grant-to-train-more-health-care-workers
14. Drawing more doctors and nurses to rural and remote communities through Canada Student Loan forgiveness. Government of Canada [Internet]. 2025. [cited 2025 Oct 25]. Available from: https://www. canada.ca/en/employment-social-development/news/2025/03/drawing-more-doctors-and-nurses-to-rural-and-remote-communitiesthrough-canada-student-loan-forgiveness.html

By Rachel Lebovic
“Hi there. My name is Rachel, and I’m with the peer support team. We check in on anyone who comes into the department between the ages of 16 and 29 because we know the emergency department can be an overwhelming and uncomfortable environment, especially for young adults, so our job is to check in, see how you are doing, and see if there is anything we can do to make your time here a little easier”. As a peer support worker, this is how I introduce myself to patients at the Mount Sinai Hospital (MSH) emergency department (ED).
Soon after starting my PhD at the Institute of Medical Science (IMS) studying suicide prevention, I was looking for a hands-on opportunity to complement my research, allowing me to better understand the systems and serve the populations I hope to work with in my future. Given that my research and career aspirations are largely driven by my lived experience navigating mental health care, peer support felt like the perfect option.
The RBC Pathway to Peers (P2P) program1,2 launched at MSH in May 2020. In his work as an emergency medicine physician, Dr. Bjug Borgundvaag, Director of the Schwartz/Reisman Emergency Medicine Institute (SREMI), noticed an increasing number of young patients were presenting to the MSH ED with mental health and substance use concerns. Dr. Borgundvaag was likely not the only ED physician across the province who noticed this, as from 2006 to 2017,
there was an almost 90% increase in ED visits for mental health reasons in youth.3 Recognizing the limitations of what the ED could offer these patients, yet wanting to better meet their needs, the RBC P2P program was created. Dr. Borgundvaag and Dr. Shelley McLeod, both researchers at SREMI and faculty members in the Department of Family and Community Medicine at the University of Toronto, have led the development, implementation,4 evaluation, and now expansion of the RBC P2P program to Michael Garron Hospital.
Peer Support Canada defines peer support as a “form of service provision, a philosophy, and a movement.”5 In simple terms, peer support refers to an individual with a lived experience providing support to another in a similar situation. Founded from the consumer/survivor and drug user activist movements, where those who were mistreated by the healthcare and criminal justice systems advocated for better mental health and substance use care, peer support is based on the core values of:
• Hope and recovery
• Self-determination
• Empathetic and equal relationships
• Dignity, respect, and social inclusion
• Integrity, authenticity, and trust
• Health and wellness
• Lifelong learning and personal growth
Through these values, peer support emphasizes person-centred, traumainformed, culturally sensitive, and harm reduction approaches informed by antiracism and anti-oppressive principles. In our interactions, we aim to reduce power imbalances and empower patients in a confusing, limited system, where trust is often lacking.
While peer support is not a new concept, it is believed that the RBC P2P program is the first of its kind in Canada in which peer support workers are fully embedded into the ED setting. As non-clinical members of clinical teams, peer support workers are uniquely positioned to enhance patient care. Due to the flexible nature of our role, we can spend extended periods of time with patients, providing them with much-needed emotional support. This can be as simple as getting them a sandwich and a blanket or engaging in a more in-depth conversation.
For patients presenting with a mental health or substance use health concern, support often centres around empathizing with a shared experience. For example, I had a patient who was a university student in the ED for stomach pains. From her chart, I could see she had a mental health history, but my experience guided me not to assume those were related. I introduced myself and asked if I could

get her anything. She said she was ok, but looking nervous, I asked if she would like a stress ball to play with while waiting. Upon return, I explained that while we check on everyone who comes into the ED in our age range, we have expertise when it comes to mental health, driven by lived experience, and if she wanted to talk about anything, I would be more than happy to listen. This started a conversation that lasted close to two hours. She shared that she had never spoken to someone before who had been through it too, someone who gets it. She got emotional as I told her how proud of her I was and how confident I am that she has a bright future ahead.
While we prioritize seeing patients who present with mental health and substance use health concerns, we understand that any young person presenting to the ED may need support, and I have often found myself spending significant time with patients in the ED for reasons relating to
chronic illness. One patient I saw had been struggling with neurological symptoms for a significant period and had not had success with treatment. She explained how living in a rural area, it is very difficult to get appointments with specialists and many of the providers she has seen have dismissed her symptoms as psychosomatic. I could see the fear and desperation on her face as she described how her symptoms have impacted her day-to-day life and wondered if they would ever get better. I asked how I could best support her. At the patient’s request, I spoke with the neurology resident before she assessed her, providing a brief overview of the situation and explaining that the patient’s biggest fear at the moment is being dismissed. The patient also asked me to stay in the room while the resident did their consultation for moral support. After the resident left, I asked the patient how she felt it went. She shared that having me there, even though I didn’t say or do anything during the consultation, gave her confidence. Just knowing that someone in the room was on her side empowered her to advocate for herself, which she did amazingly.
The interaction that I believe has been my most impactful was with a patient who was in the ED for domestic violence and sexual assault. We spoke for hours. At times the conversation centred on her relationship and what happened, while at other times we focused on distractions, talking about school and life goals. We discussed what comes next, collaborating with social workers to ensure she had
somewhere to go and resources for support after leaving the ED. I spent my entire shift with her that day; she didn’t want to be alone. In the structured chaos of an ED, a nurse, physician, or social worker has very limited time they can spend with a single patient. As a peer support worker, I was able to spend hours with her keeping her company, helping her process what happened, and making her feel safe.
I have seen firsthand the impact the RBC P2P program has on young adult patients in the ED. Yet while I may be impacting these patients, they are also impacting me. Each interaction I have, every story I hear, contributes to my understanding of healthcare that I will take with me throughout my education and into my career.
1. RBC Pathway to Peers [Internet]. [cited 2025 Oct 22]. Available from: https://sremi.ca/rbc-pathway-peers
2. Peer support program supports youth through mental health and addictions crises in the ED [Internet]. [cited 2025 Oct 22]. Available from: https://dfcm.utoronto.ca/news/peer-support-program-supports-youth-through-mental-health-and-addictions-crises-ed
3. Chiu M, Gatov E, Fung K, Kurdyak P, Guttmann A. Deconstructing The Rise In Mental Health–Related ED Visits Among Children And Youth In Ontario, Canada: Study examines the rise in mental health-related emergency department visits among children and youth in Ontario. Health Aff (Millwood). 2020 Oct 1;39(10):1728–36.
4. McLeod SL, Thomas R, Dunning A, Chalmers C, Figueiredo S, Nikoo M, et al. Implementation of a patient-centered, peer support model of care for young adults presenting to the emergency department with mental health and substance use challenges. Can J Emerg Med. 2025 Sept 4;s43678-025-00978–3.
5. National Peer Supporter Certification Handbook [Internet]. Peer Support Canada; [cited 2025 Oct 22]. Available from: https:// pscportal.ca/wp-content/uploads/2023/12/National_Peer_Support_Certification_Handbook.pdf

By Josephine Machado
Imagine this scenario: It’s 4 a.m. in a Toronto emergency department (ED), and you’re left sitting under the harsh fluorescent lights of an echoing waiting room wondering if you’ve made the right decision dragging your 14-yearold daughter to the ED. Upon triage, she is placed on a Form 1 hold under Ontario’s Mental Health Act and admitted to the psychiatric floor. She is just one of thousands of children whose initial encounter with a mental health professional was not in a clinic or counsellor’s office as you had hoped, but in an ED designed for everything but emotional trauma.
A recent Canadian-based study evaluating transitions in care for children and youth found that over 50% had used the ED as the first contact for mental health concerns without previously seeking outpatient care.1 This comes as no surprise given that there are 28 000 Ontario youth and children waiting for mental health services; for some families, this wait is up to 2.5 years long.2 This is in addition to an estimated 200 000 children and youth requiring mental health care that do not reach the front door of specialized centres.2 Long-term trends in Ontario have shown the impact this unmet need has had on EDs, as mental health-related ED visits doubled from 11.7 per 1000 citizens in 2003 to 24.1 per 1000 citizens by 2017.3
Currently, there is limited information regarding the reasons behind the surge in mental health-related ED visits for
Canadian youth; however, the Centre for Addiction and Mental Health (CAMH)’s Ontario Student Drug Use and Health Survey (OSDUHS) indicates significant mental health-related stressors among Ontario youth in its 2023 report. Of the 10145 grade 7 to 12 students surveyed, 51% of students indicated moderate-to-severe psychological distress, including symptoms of anxiety and depression.4 Additionally, one-in-five students reported engaging in intentional self-harm, and one-in-six students reported experiencing some form of suicidal ideation over the past year.4 Overall, indicators of psychological stress have significantly increased since monitoring began a decade ago in 2013, when students reporting moderate-to-serious levels were just above 20%.4 When investigating overarching trends in youth mental health, Statistics Canada (2023) reports that suicide is the second-leading cause of death among individuals aged 10-24; a pattern underscoring the impact of severe mental health crises across the spectrum of adolescence.5
The Provincial Council for Maternal and Child Health’s Implementation Toolkit indicates the process for patients reporting mental health concerns upon intake to the ED.6 First, staff triage and evaluate whether resuscitation or emergency care is required. Once patients are deemed medically stable, mental health screening is done using survey-based screening
tools. Clinical assessment is then done by an ED physician and/or a child and youth mental health clinician. High risk patients can be reviewed for admission with consultation from other members of the healthcare team such as a psychiatrist, pediatrician, or family physician. Outcomes of a mental-health related ED visit can range from immediate referral to a mental health specialist with possible admission, to outpatient referral to the community with clinical follow-up. EDs can also simply recommend that patients follow-up with a primary care provider and provide information on mental health resources that the patient can opt to pursue.6
The rising demand for youth mental health care, in addition to the lack of resources and frequent use of EDs as a first point of contact, creates the perfect storm for disaster. The increasing number of adolescents who access the ED following self-harm or for mental disorders is of significant concern. Additionally, the ED can be an overstimulating setting for delivery of mental health care or for care of adolescents, particularly those who have engaged in self-injury.3 Furthermore, there are a substantial number of individuals who present to the ED who do not require institutional emergency services or hospital admission. They are instead retained in the ED or are admitted due to a lack of available community-based services and support.7
28 000 Ontario youth and children [are]waiting for mental health services. “ “

It is imperative that we continue to advocate for improvements in the realm of youth mental health aimed at bettering the ED experience and reducing the load of patients requiring emergency care. In 2008, the Canadian Mental Health Association presented a policy submission addressing ED wait times and enabling access to community mental health and addictions services.7 The submission was prepared by a partnership inclusive of six mental health organizations representing patients and service-providers. Primary recommendations point to the development and investment in 24-hour crisis response systems in communities, so patients have places to go outside of the ED. Other suggestions include expanding peer-run phone/text support, peer-support worker involvement in discharge planning, and the strengthening of communitymental health services that are directly linked to hospitals to help divert people out of the ED when possible. Successful solutions require shifting investments from EDs to community-based systems that can respond before crises escalate. A promising model to execute this reform is the Integrated Youth Services Approach (IYS), which brings together mental health, substance use, primary care, and peer, family and social supports under one roof. A CAMH-led study explored the model between 2016-2020 and showed that youth in the IYS model accessed services nearly three times faster and required fewer hospital-based psychiatry resources than those in traditional care or a hospital outpatient program.8
Improving ED staff training and implementing dedicated emergency mental health teams should also be prioritized. A systematic review of 18 studies conducted between 2013-2023 had found that installing collaborative care models (CCMs) resulted in a 20% reduction in the percentage of patients requiring readmission within 30 days of release.9 Moreover, telepsychiatry has drastically improved patient outcomes in rural and underserved areas by providing timely psychiatric consultations, resulting in reduced ED overcrowding and improved patient satisfaction.9 Other approaches can include pushing for school-based mental health programs. Children spend a significant amount of time at school, thus educational institutions are well-positioned for working towards mental health promotion, early identification, and suicide prevention. Finally, we must prioritize funding reform, Canadian provinces and territories spend just 6.3% of overall healthcare budgets on mental health; this remains below what many peer countries are spending and is also well short of the recommended 12%.7
Despite the concerning trends, there is power in in the possibility for change of how youth mental health is addressed in the ED. Structural changes are necessary to provide care for youth mental health crises and support high patient loads. These changes must be precipitated by an increase in available resources and the initiation of significantly more research to
better understand key factors underlying trends in youth mental health. Youth turning to emergency departments for mental-health care is a clear sign of a chronic shortage of accessible services that cannot be ignored.
References
1. Tucci A, Cloutier P, Polihronis C, et al. Improving transitions in care for children and youth with mental health concerns: implementation and evaluation of an emergency department mental health clinical pathway. BMC Health Serv Res. 2025; 25(1): 475. https:// bmchealthservres.biomedcentral.com/articles/10.1186/s12913025-12524-z
2. Children’s mental health ontario. Children’s Mental Health Ontario - CMHO. [cited 2025 Nov 9]. https://cmho.org/
3. Gardner W, Pajer K, Cloutier P, et al. Changing rates of self-harm and mental disorders by sex in youths presenting to ontario emergency departments: repeated cross-sectional study. Can J Psychiatry. 2019; 64(11):789–97.https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6882075/
4. The ontario student drug use and mental health survey(Osduhs).CAMH. [cited 2025 Nov 9]. https://www.camh.ca/en/ science-and-research/institutes-and-centres/institute-for-mental-health-policy-research/ontario-student-drug-use-and-healthsurvey---osduhs
5. Government of Canada SC. Leading causes of death, total population, by age group [Internet]. 2023 [cited 2025 Nov 9. https:// www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039401
6. Emergency department clinical pathway for children and youth with mental health conditions – pcmch. [cited 2025 Nov 9]. https://www.pcmch.on.ca/emergency-department-clinical-pathway-for-children-and-youth-with-mental-health-conditions/
7. In Canada, mental health is a privilege. It should be a right. CMHA National. [cited 2025 Nov 9].https://cmha.ca/what-we-do/state-ofmental-health-in-canada/
8. New study shows integrated collaborative care helps youth access mental health and substance use supports faster. CAMH. [cited 2025 Nov 9]. https://www.camh.ca/en/camh-news-and-stories/ new-study-shows-integrated-collaborative-care-helps-youth-access-supports-faster
9. Katiki C, Ponnapalli VJS, Desai KJ, et al. NYA. Enhancing emergency room mental health crisis response: a systematic review of integrated models. Cureus. 2024. https://www.cureus.com/ articles/312677-enhancing-emergency-room-mental-health-crisis-response-a-systematic-review-of-integrated-models

By Grace Gibson
As a rapidly advancing field, there are many proposed applications for artificial intelligence (AI) in healthcare settings. In high-stress specialties like emergency medicine, AI-based solutions have the potential to transform patient experiences by increasing the standard of care and ensuring faster emergency response times.1,2 However, AI solutions have their limitations, raising numerous concerns if introduced into healthcare settings.1,3
“AI” has become an umbrella term for many different technologies, but as a general description, AI tools integrate and process data to produce an output. The subset of AI discussed here, generative AI (GenAI), uses input data to produce new text or images.4 These tools, many of which fall under the category of large language models (LLMs), process huge volumes of information from past cases so that they may output reasonable predictions for similar scenarios in the future.1
In ER environments that demand immediate and accurate decisionmaking, AI solutions may augment the capabilities of healthcare providers, improving their ability to care for patients. 3,4 In one possible use, AI tools can improve initial triage performed when a patient enters the ER. These assessments often use the emergency severity index (ESI) to standardize evaluations, but ESI values may be inaccurate due to provider fatigue or limited time.1 Additionally, demographic
factors like race and gender can impact perceptions of a patient’s condition. 5
Theoretically, an AI model could replace human-directed ESI assessment, as healthcare providers could input the patient’s health records and physiological data to generate a suggested ESI value. 1,3
AI models can also be used in the diagnostic process. An AI tool that can compare a patient’s scans to a comprehensive dataset could identify potentially concerning indications without the need for human evaluation.1 Alternatively, a tool trained to identify the common presentations of specific conditions, such as different types of stroke, could recognize medical emergencies in their early stages based on a patient’s test results. Some emergency departments already use this type of AI tool for early stroke detection, with applications to cardiac arrhythmias and traumatic brain injuries in development.2 In the future, LLMs may also play a role in directing ambulance dispatch to patients and transcribing doctor-patient interactions as they occur, though these uses have not yet been implemented.1,2,3,4
When presented in examples like this, AI tools appear to be wholly positive for emergency medicine; however, institutions should remain cautious about AI for many reasons.4 As an example, if a model is trained on inaccurate or biased datasets, the outputs will mirror the deficiencies in the original data.3 This may be the case for LLMs trained on data from a particular
set of institutions—data that might not be representative of other healthcare settings, which differ in institutional policies, patient demographics, and more.3 Additionally, human error and prejudice may be present in AI training data, introducing the possibility of inaccurate or biased output.1,3,4
Healthcare AI tools can also raise questions of privacy and security for patients. In some cases, LLM training involves the release of personal health information to third-party companies that develop AI tools, something that patients might want to avoid, especially given the limited regulation of the use of personal data in training LLMs. 6 In-house development and training can ensure that patient data is not released to third-party companies, but this fact may not assuage patients’ perceived security concerns about new AI tools. 3,6
The lack of AI legislation also presents liability challenges. Just as any human physician can make mistakes, AI tools can produce incorrect results or provide substandard information; however, medical malpractice legislation does not account for AI applications, and an AI can’t be held liable for harm it may cause. Until there are significant developments in legislation over GenAI tools and healthcare, implementing tools like these introduces the risk that patients who are harmed by an inaccurate AI output may not be able to pursue legal action. 7
There are steps institutions can take to address these issues before introducing GenAI tools: training datasets can be carefully selected to ensure generalizability, data protection measures can be strengthened, and LLMs can be developed internally. 8 However, beyond the specific concerns around introducing AI into healthcare settings, there are additional ethical questions around any application of GenAI.
One concern is the impact of AI on the job market. Expanding the use of AI fuels widespread worker displacement, leaving many people jobless across industries.9 However, the implementation of AI does not appear to balance this job loss with either equivalent productivity gains or generation of high-quality jobs.10 Furthermore, replacement of skilled human work contributes to a general decline in worker skill levels. Increased automation of the workforce may improve performance in some sectors, but this comes at the cost of permanent worker displacement and decay of skilled human labor, hurdles that may not be overcome with the projected benefits of automation.9,10
Another concern about increasing GenAI use is the associated environmental damage. The high computing power required by AI data centres has driven a global increase in electricity use, negating previous goals in improving efficiency and reducing emissions.11,12 AI’s increasing energy demands have additionally necessitated the rapid construction of
new data centres, a process that can have serious consequences for communities in which they’re established.12 Residents living near these centers face higher electricity costs, lower air quality, and exposure to hazardous waste products.13
Emergency departments looking to implement AI solutions therefore must grapple with overarching ethical questions: do the benefits of using an AI tool outweigh the economic and environmental costs associated with widespread GenAI adoption? For some situations, the answer might be “yes”—there are significant, datavalidated benefits to some applications of GenAI in the ER, including improvements to triage and early stroke detection.1,2 However, healthcare institutions should avoid indiscriminately promoting AI solutions, especially if they’re unable to rectify issues like inaccurate training data or violation of patient privacy. Moreover, developing new GenAI tools without sufficient justification for their use contributes to an unnecessary AI saturation, a trend with potentially disastrous consequences for our society, our environment, and, by extension, our health.11 As we envision how GenAI might impact emergency medicine, we should aim to embrace its transformative and lifesaving uses, but we should remain wary of introducing AI solutions without weighing their wider ethical implications.
1. Kachman MM, Brennan I, Oskvarek JJ, et al. How artificial intelligence could transform emergency care. Am J Emerg Med. 2024 Jul;81:40-46.
2. Piliuk K, Tomforde S. Artificial intelligence in emergency medicine. A systematic literature review. Int J Med Inform. 2023 Dec;180:105274.
3. Chenais G, Lagarde E, Gil-Jardiné C. Artificial Intelligence in Emergency Medicine: Viewpoint of Current Applications and Foreseeable Opportunities and Challenges. J Med Internet Res. 2023 May 23;25:e40031.
4. Zhang K, Meng X, Yan X, et al. Revolutionizing Health Care: The Transformative Impact of Large Language Models in Medicine. J Med Internet Res. 2025 Jan 7;27:e59069.
5. Sax DR, Warton EM, Mark DG, et al. Evaluation of Version 4 of the Emergency Severity Index in US Emergency Departments for the Rate of Mistriage. JAMA. 2023;6(3):e233404.
6. Da Silva M, Flood CM, Goldenberg A, et al. Regulating the Safety of Health-Related Artificial Intelligence. Healthc Policy. 2022 May;17(4):63-77.
7. Shumway DO, Hartman HJ. Medical malpractice liability in large language model artificial intelligence: legal review and policy recommendations. J Osteopath Med. 2024 Jan 31;124(7):287-290.
8. Labkoff S, Oladimeji B, Kannry J, et al. Toward a responsible future: recommendations for AI-enabled clinical decision support. J Am Med Inform Assoc. 2024 Nov 1;31(11):2730-2739.
9. Holzer HJ. Job Loss, Displacement, and AI: Anticipating and Preventing Their Costs. In: Orrell B, editor. New Approaches to Characterize Industries: AI as a Framework and a Use Case. Washington, DC: American Enterprise Institute; 2025. p. 59–62.
10. Tyson LD, Zysman J. Automation, AI & Work. Daedalus. 2022;151(2):256–271.
11. Bashir N, Donti P, Cuff J, Sroka S, Ilic M, Sze V, et al. The Climate

By Regina Annirood
Visiting the hospital when sick is an experience most people dread. After arriving, whether on your own or by ambulance, you register with a triage nurse who asks pointed questions, records your vitals, and assigns a level of urgency. You hope to be seen quickly, but instead wait for hours with little communication, anxious and hungry among others in varying states of illness. This is the reality for many patients in Canadian emergency departments, and it is time to ask what must change.
Arriving at an emergency department follows a predictable process. After registering with personal details, a triage nurse assesses the patient using the Canadian Triage and Acuity Scale (CTAS), recording vital signs, main complaints, and medical history.¹ Implemented in 1999, the CTAS was designed to identify patients’ needs for timely care and to standardize emergency department operations.¹ Yet, despite advances in technology and rising patient volumes, it has changed little over the past 25 years and now struggles to keep pace with the complexity, data demands, and technological possibilities of 2025.¹ After triage, patients wait to see a physician or healthcare provider, with urgent cases prioritized.¹ Many then undergo tests, imaging, or consultations, necessary parts of care that nonetheless add to overall delays.¹ These delays often stem not from the assessments themselves but from limited staffing and
high clinician workloads, which slow both the completion of tests and the response to results.2 The final step, known as disposition, determines whether the patient is discharged, admitted to the hospital, or referred elsewhere. Each stage in the process depends on staffing, bed availability, and system flow, so delays at any point extend wait times for everyone.2
Across Canada, median wait times and total length of stay have risen in almost every province over the past five years, with the largest increases in Ontario and Alberta.3 Emergency room wait times in Ontario have worsened over the past decade. Health Quality Ontario (2024) reports an average two-hour wait from registration to initial assessment, about three hours for low-urgency non-admitted patients, five hours for high-urgency cases requiring more extensive testing or assessment and 19.2 hours for those eventually admitted.4 In 2017–18, the average emergency department stay for admitted patients was nearly 16 hours, which is two hours longer than in 2015–16 4 The prolonged effects of pandemic-related staffing shortages, delays in elective care, and elevated patient volumes have further strained emergency departments, pushing wait times to record highs. In Ontario, a projected shortfall of 33,000 nurses and personal support workers by 2027 to 2028 is expected to further strain the system,
worsening wait times and causing more temporary closures.⁵ Together, these statistics reflect a system in which long waits are no longer the exception, but the expectation.
One of the hardest parts of visiting the emergency room is not just the wait, but the lack of communication. Patients often do not know how many people are ahead of them, what stage of care they are in, or what they are waiting for. A 2021 study explored patients’information needs while waiting in emergency departments and found strong demand for real-time updates on wait times and care progress.⁶ The research revealed that most patients wanted transparent, continuously updated information about expected delays and the sequence of care but noted that few hospitals provide such systems.⁶ This finding wasn’t specific to a single study – in fact, a 2024 review of 29 studies examining patient experiences of emergency department triage identified communication as a key determinant of perceived quality of care, highlighting that clear, compassionate, and timely communication during triage and waiting periods significantly shapes patient satisfaction, trust, and overall experience.7 These growing concerns suggest that the system needs to shift towards treating patients as active participants in their care.

While delays in receiving clinical care are concerning, the side effects of long wait times should also be recognized. Many hospitals have cafés or food courts, but few operate around the clock, leaving vending machines as the only accessible option during overnight hours. These machines rarely offer nutritious choices, as an INFORMAS Canada survey found that only 3% of hospitals provided exclusively healthier food options, with an average of 4.7 less healthy items out of every 10 available.8 This prolonged waiting and lack of nourishment contribute to growing fatigue and discomfort. Beyond physical needs, the environment itself adds to the strain. Crowded waiting rooms filled with patients of varying conditions heighten noise, stress, and discomfort for everyone. Research shows that noise levels in emergency departments frequently exceed World Health Organization recommendations, contributing to increased patient anxiety and dissatisfaction with care.9 Similarly, studies on emergency department environments have found that overcrowding and constant activity negatively affect patients’ sense of safety and overall experience.10
While structural reforms are essential to address the root causes of prolonged wait times, there are also opportunities
to improve patient experience within the existing system. Patients could be grouped by severity of their condition, creating quieter and lower stress areas for those needing urgent attention.9 Hospital staff should clearly explain the process during triage by informing patients of their status, such as, “You have been assigned CTAS Level 3; expect to wait about X hours; here is what comes next.” Even approximate updates can ease anxiety.7
Digital tools can also improve transparency. Many clinics already use text notifications and queue tracking apps; similar systems could show patients their place in line or send alerts when they are next. Studies show strong patient support for access to real-time wait information.6 Further, small quality-oflife changes such as healthier vending options, extended cafeteria hours, comfortable seating, quieter areas, and charging outlets also make a difference by signaling respect and care.
Many of these solutions do not require reinventing care. Instead, they involve small, practical changes in how waiting is treated as part of the care process, how communication is handled, and how time and space are managed. Waiting in an emergency department should not feel like being left in limbo. While medical urgency differs, the need for clarity, dignity, and timely care remains universal. As we work to address structural issues underlying long emergency room wait times, we must also work to make waiting itself a
transparent, humane, and intentional part of the care experience.
1. Kayuni J, Dordunoo D, Mallidou A, Mohan M, Marquard P. Exploring delay points at the emergency department.Can J Emerg Nurs. 2024;47(1):14–19.
2. Calder-Sprackman S, Kwok ES, Bradley R, Calder LA. Availability of emergency department wait times information: A patient-centered needs assessment. Emerg Med Int. 2021;2021:8883933.
3. Health Quality Ontario. Time spent in emergency departments. 2024 [Internet]. Available from: https://www.hqontario.ca
4. Canadian Medical Association. Why are ER times so long in Canada? CMA Health Care for Real [Internet]. Ottawa (ON): Canadian Medical Association; [cited 2025 Oct 29]. Available from: https:// www.cma.ca
5. Financial Accountability Office of Ontario. Expenditure Monitor 2023–24: Q3—Health sector. Toronto (ON): Financial Accountability Office of Ontario; 2024.
6. Afilalo M, Lapointe L, Lavoie J, Léger R, Pomey M-P. Availability of emergency department wait times and the patients’ information needs: A mixed-methods study. Int J Emerg Med. 2021;14(1):37.
7. Janerka C, Jordan Z, Tran DT, Crawford T, Carter B. Patient experience of emergency department triage: An integrative review. Int Emerg Nurs. 2024;78:102353.
8. INFORMAS Canada. An in-depth look at Canadian food environments. Toronto (ON): INFORMAS Canada; 2025.
9. Adams C, Short A, Johnstone M. Noise levels in the emergency department: Are we meeting World Health Organization standards? Int Emerg Nurs. 2024;73:102242.
10. Rowe A, Zaremba L, Goldmann E, Doran K. The impact of the healthcare environment on patient experience in the emergency department. J Patient Exp. 2022;9:23743735221086545.
By Rebecca Smythe & Areej Mir
Dr. Liisa Galea grew up in a time when girls had to wear skirts to school. “It sounds strange now, but that was normal,” she recalls. “I remember being told, ‘Oh, you can’t do that, you’re a girl.’ And that really bothered me.” Her parents, though, refused to accept those limits. “They always told me, ‘You can do whatever you want. Don’t listen to them.’” That message became the foundation of her worldview. “It really set me up to always be inquisitive,” she says. “If someone told me something, I wanted to find out if it was actually true.”
That curiosity first led her to Queen’s University to study Engineering. However, in her second year, a Psychology elective with Dr. Susan Lederman changed her direction. Dr. Lederman told the class that she was the first woman, psychologist, and Canadian asked to join a NASA committee to design better space gloves. “I was hooked,” Dr. Galea says. Not long after, Dr. Galea took a course called “The Biology of Sex” in which, the professor, Dr. Laurene Ratcliffe, taught that the prevailing understanding of the development of male sex as “active” while the female sex development was “passive” was likely due to not enough research attention paid to female development. This message piqued her interest as she noticed how often women were missing from data. This realization grounded her focus in women’s health and led her to pursue graduate work on sex differences in the brain with experts such as Dr. Doreen Kimura at Western University (UWO), Dr. Martin Kavaliers
(UWO), and then her postdoctoral work with Dr. Bruce McEwen at Rockefeller University. Following this, she then joined the University of British Columbia (UBC) in the department of psychology. The Centre for Addiction and Mental Health (CAMH) is now her lab home.
Since joining CAMH, Dr. Galea’s role has supported broader advocacy for women’s health while continuing her research. The Galea lab investigates many fascinating topics, such as how estrogens influence hippocampal plasticity and memory, or stress resilience in animal models. Recently, the Galea lab found some supporting evidence that the route of hormonal therapy administration matters and that certain estrogens can be more advantageous than others. In clinical practice, women often take menopause hormone therapy as an oral pill, as opposed to transdermal gels or patches, however, this has implications for metabolism. “When you take estradiol orally, it can change into a weaker and less beneficial estrogen, but if you take it transdermally or subcutaneously, it doesn’t go through that hepatic conversion and remains the more beneficial form, estradiol,” Dr. Galea explained. This has been confirmed through her work with rodents and similar trends have been observed in Canadian databases with human data.
Dr. Galea considered taking on some studies working with human data, but quickly learned that many databases
lack critical metadata, like the type of prescribed hormone used, the dose or duration, as well as a woman’s age at first pregnancy or hormonal contraceptive use. Without these critical parameters, it is hard to accurately assess women’s health. This underscores the broader issue that federal funding often fails to prioritize women’s health, a point Dr. Galea emphasized in our interview. She explains, “In one of our studies, about seven percent of research funding over fifteen years went to [women’s health studies].1 We need people and organizations who recognize that women’s health deserves that extra attention.” She credits philanthropist Sandi Treliving for providing her a platform to advocate for women’s health at a national level, as the Treliving Family Chair in Women’s Mental Health. Taking on this role has allowed her “to bring everything together— research, mentorship, and advocacy.” As the comprehensiveness of human data available improves, Dr. Galea hopes to be able to focus more on menopause. Since menopause presents differently across individuals, its manifestations can offer valuable indicators of broader health patterns. Dr. Galea’s lab aims to be able to leverage human data and machine learning to create a menopausal precision risk calculator for clinical applications.
The road had its challenges. When asked about the obstacles she faced, Dr. Galea laughed and replied, “All of them.” Early on, expectations for women in her Master’s lab were strict: no makeup,
I remember being told, ‘Oh, you can’t do that, you’re a girl.’ And that really bothered me. “ “

“Science fills my cup, but it doesn’t hug me at night,” she says with a smile. Her two children, currently pursuing PhDs, share her passion for discovery. “Now we talk science at the dinner table,” she laughs, “It’s the best kind of full circle.”
She conveys an insightful message by saying “there’s many roads to success, just because it worked for Person A doesn’t mean it will work for you.” So, if you believe in something, keep trying!
no hair down, no partners, and twelvehour workdays. “It was incredibly rigid,” she says. “I almost dropped out.” With her mother’s support, she turned that experience into a guide for how to lead. She wanted to create spaces where people feel supported and can be themselves regardless of gender. The culture, she notes, can still be unforgiving. You need to be resilient, “whether it’s reviewer comments or the color of your skin, whether you have breasts, wear a dress, or use makeup. You can’t let negative comments stop you from doing the science you love.”
Despite her many accomplishments, her proudest achievements remain at home.
Juggling her roles as a mother, scientist, and advocate, Dr. Galea speaks frankly, “There is no balance.” Early in her career, neuroanatomist Dr. Joanne Weinberg, advised her not to chase an unrealistic ideal. While life may have its ups and downs, she emphasizes the importance of taking time to recharge. “I think it’s really important to just get your mind completely out of your day-to-day, however you do it, reducing stress is really important.” An easy way to disconnect while on the go is through podcasts. Dr. Galea recommends Women’s Health Interrupted, which she’s hosting, and encourages readers to check it out. You can find it and other free content on women’s health at the Women’s Health Research Cluster, led by Dr. Galea. The cluster is a community of trainees, investigators, clinicians, and community members interested in learning more about women’s health and advocating for more research (https:// womenshealthresearchcluster.com/).
As we finished up, Dr. Galea imparted some advice for early trainees. “Develop a thick skin because you’re going to need it,” she said with a smile. “We’re always going to have stumbling blocks,” which is true of any stage, but learning to persevere and problem-solve is key.
Before signing off, Dr. Galea took a moment to say, “Not a Bikini.” She explained that people often think of women’s health as just what’s under their swimwear, but it’s so much more. She pointed out that biological sex is present in every nucleated cell in the body, across all organs. Women’s health covers more than our reproductive organs. Women’s health, she stressed is not limited to what’s under the bikini. Her words reflected the curiosity, courage, and commitment that have made her a lasting inspiration to women in science everywhere.
References
By Shreya Vasudeva
“This is the most random email you’re ever going to get.”
It all began with a spontaneous message that sparked a collaboration between Institute of Medical Science (IMS) students Mariam Elsawy and Shannen Kyte. This correspondence eventually grew into the Medical Science Comic Conference (MedComics Con), a creative initiative connecting IMS and Biomedical Communications (BMC) students to turn research into visual stories, earning them the 2025 Jay Keystone Memorial Award for Innovation in Scientific Communication.
For Mariam, the journey to IMS began after completing her undergraduate degree in Health Sciences with a minor in Psychology at Carleton University. After graduating during the pandemic, she moved to Toronto and worked at SickKids in administrative roles but her interest in public health and policy led her to Dr. Ahmed Bayoumi at the MAP Centre for Urban Health Solutions at Unity Health Toronto. Now, her work focuses on alternatives to drug criminalization and the lived experiences of people who use drugs.
Shannen graduated from the University of Toronto Scarborough (UTSC) with a specialist in Psychology and a minor in English Literature. Shannen discovered IMS through what he fondly calls “the wonders of LinkedIn” when a UTSC alumnus reached out with an opportunity and introduced him to the program. He now works with Dr. Philip Gerretsen at the Centre for
Addiction and Mental Health, researching illness awareness in schizophrenia and substance use disorders, neural correlates, and interventions including deep brain stimulation and virtual reality.
Mariam and Shannen first met in their Graduate Professional Development class, designed to help students explore communication and professional growth. Mariam recalls connecting with Shannen, who “mentioned that he is passionate about education and making it accessible.”
Months later, Mariam returned to a childhood passion—drawing. “I drew things I was learning about. It was always a way I was learning things. I missed that in grad school, and I remember thinking I wish there was a way I could implement this into my research or a part of IMS and share it with others.”
That week, emails about the Jay Keystone Award went out. Mariam had “an epiphany that this was the perfect time to apply to this award.” She reached out to Shannen with the now-famous line. Shannen, chuckling as he recalled the email, was immediately interested.
The pair connected with Dr. Shelley Wall, a professor in Biomedical Communications known for her work in graphic medicine who opened their eyes to the field. The resulting concept was simple but innovative: to create a science-focused event that combines research and visual storytelling. On developing the basis for the project,
Mariam explains, “I think the idea of comics itself was how I imagined the easiest way to really understand something, having pictures along with words makes things so much easier.” Shannen adds that many people are visual learners and noted that around the same time, he also saw a realworld example in Marvel’s Moon Knight, whose depiction of dissociative identity disorder fascinated him.
Developing the award-winning proposal was at times challenging, but the support from their collaborators was incredibly encouraging. Mariam notes that it was sometimes difficult “to balance the ambition of what they wanted the event to be with what was realistic time- and budget-wise.” Together with IMSMagazine and BMC students, they figured out what was feasible, managed the budget, and anticipated logistical challenges.
At its core, MedComics Con is about accessibility, creativity, and engagement. Shannen’s hope for MedComics Con is two-fold; “[Grad school] can be frustrating at times, so it’s a good time for students to explore the creative side of science and think about their research at a much simpler level.” He also hopes to “make science easy to understand for anyone and everyone.”
MedComics Con provides IMS students with an opportunity to get involved with their community outside their labs. Mariam points out that despite being part of large research sites, students “can also
MedComics Con is helping to remind people that there is room to think outside the box in science. “ “


his “fun and light spirit” through their initiative. Mariam says, “He felt like a friend who was talking to you at a coffee shop and explaining the things they do at the lab.”
MedComics Con will be a one-day event in Spring 2026, bringing together IMS and BMC students. Student pairs will be matched in late November 2025 to create comic-style research posters showcased at the event, which will feature guest speakers in graphic medicine and an interactive comic workshop. A poster competition will recognize top entries with certificates, cash prizes, and publication in the Fall 2026 issue of IMSMagazine .
“Sometimes we live in our own minds, and we limit ourselves, but push yourself to start on things and worry about the little things later. There are people out there who can help you make your idea possible.”
Looking forward, Mariam and Shannen hope MedComics Con becomes an annual event, offering a space for scientists, artists, and communicators to collaborate and learn; “If attendees and participants walk away having learned something new about graphic medicine and potentially implementing it in their future careers, I would personally feel like we did a really good job,” Mariam says.
become isolated or siloed.” She hopes that the event will encourage students to rediscover creativity, explore graphic medicine, and develop professional skills while sharing research. In addition, collaboration with BMC students is central to the project. Mariam says, “It’s mutually beneficial, BMC students get to build their portfolios by illustrating real-world projects, and IMS students learn a different way to represent their research.”
“MedComics Con is helping to remind people that there is room to think outside the box in science,” Mariam says. Shannen agrees, noting, “Science is vast and [it is] for all.” They also wanted to pay tribute to Dr. Jay Keystone and his legacy, aiming to embody
Receiving the Jay Keystone Award has been a validating experience for Mariam and Shannen. Shannen says it felt “reassuring” and emphasized that “even though science can sometimes feel rigid, there is a lot of room to grow and be creative.” Mariam adds, “Whenever you can’t find the specific thing you’re looking for, you can always make your own opportunities.” She also realized the importance of collaboration. “Wherever I go, even beyond IMS, I’ll always look around [myself] to see who around me has overlapping interests, take [the time] to speak to them, and see what comes of it.”
Mariam and Shannen both emphasize the importance of taking initiative and believing in your ideas, even when selfdoubt arises. They encourage students to seek out opportunities, share their ideas with others, and not be discouraged by the details early on. As Shannen puts it,
Mariam and Shannen want to thank the University of Toronto and IMS for having the Jay Keystone award, which made the initiative possible. They are currently launching social media channels and sharing updates through the IMS Student Association (IMSSA) newsletter and their Instagram: @medcomic.con. Mariam encourages students to get involved however they can, whether it is volunteering, sharing research, or illustrating.
By blending art and science, Mariam and Shannen’s initiative seeks to help researchers communicate complex ideas while inspiring the IMS community to explore new ways of thinking. Throughout it all, the spirit of Dr. Jay Keystone— playful, innovative, and committed to education—lives on.
By Alicia Tran
“Iwas always really interested in science and understanding the pathogenesis of diseases,” recalls Aravin, reflecting on the roots of his academic journey. “I thought doing a PhD would be a good way to develop skills in that area—and eventually work in industry.” This curiosity became a driving force behind a journey that has taken Aravin from the lab benches of St. Michael’s Hospital to a career at the intersection of science, strategy, and communication.
Choosing where to pursue a PhD was a pivotal decision. For Aravin, the Institute of Medical Science (IMS) stood out because of its research diversity in both basic science and clinical research. “IMS has so many different research programs—cancer, cardiovascular disease, psychiatry, and neuroscience,” he explains. As he navigated possible research avenues, he was drawn to the field of chronic disease and the work being conducted by Dr. Philip Marsden at St. Michael’s Hospital. Under Dr. Marsden’s mentorship, Aravin delved into the molecular mechanisms underlying endothelial cells, which form the inner lining of arteries, veins, and capillaries.1 His doctoral research focused on how these cells respond to stress in ways that mirror human blood flow. The experience didn’t just sharpen his technical skills—it helped shape how he solves problems and approaches collaboration across disciplines in his current work.
As his PhD progressed, Aravin began to think about what would come next. Like many graduate students, he admits that during the early days, he did not know what he wanted to do. While he once considered becoming a professor or working in pharmaceuticals, he was drawn to science communications—a field that combined his interest in research with the opportunity to collaborate with clinicians and industry professionals. “I never thought I would be in scientific communications—I was more curious about the business side of science at the time,” Aravin remarks. However, his growing curiosity of the field eventually led him toward a path he hadn’t initially considered.
Today, Aravin works as a Science Communications Specialist at Boston Scientific, a role that blends scientific knowledge with strategic impact. One of his favourite aspects of this role is tactically piecing together data and evidence as a story, while ensuring it aligns with the goals of the company. In many ways, this role fosters Aravin’s entrepreneurial spirit—shaping how scientific work is understood and how it can be best communicated to different stakeholders.
Aravin helps translate complex research findings into engaging narratives for various audiences including healthcare professionals, scientists, and internal teams. Aravin mentions that this is accomplished by wearing different hats
and adapting to each group’s priorities: clinicians want to understand how data affects patients and their workflow, marketing teams focus on how findings support the company’s strategy and values, and research and development teams emphasize device performance and operator needs. Aravin also highlighted that evidence is at the foundation of science communications, providing a comprehensive picture that allows him to communicate data in a way that fulfills the goals of each team. Together, his ability to adapt his evidence-based communication style to varying audiences has become a key strength to enhance understanding and engagement.
One recent project that Aravin is proud of was contributing to a pre-clinical study comparing the company’s cardiac device to a competitor product. He played a key role in planning and executing experiments, analyzing data, and working on the full manuscript, which earned recognition from colleagues and leadership teams. “What made that project special was the collaborative effort,” he says. “It involved people from engineering, marketing, legal, and other departments. Seeing how their input shaped the outcome was rewarding.” This experience reinforced the value of collaboration across disciplines to drive scientific innovation.
Despite common misconceptions, the field of science communications isn’t confined to a desk. Aravin has had several hands-on


within the clinic to improve patient care. These opportunities deepened his appreciation for how scientific communication connects directly to realworld clinical practice.
opportunities to engage with engineers and scientists directly to investigate device features that can impact operator handling and procedure outcomes. He also found interest in the clinical side of his work where he interacts frequently with physicians. For instance, he has had the chance to observe live simulated cases of surgical ablations and left atrial appendage occlusions. This has allowed him to gain firsthand insight into clinical workflow, as well as a deeper understanding for how specific devices may be implemented
When reflecting on how his doctoral training shapes his work today, Aravin highlights the cross-disciplinary mindset it instilled. His research allowed him to explore engineering principles through his work with modeling blood flow, providing him with a foundation that extended beyond traditional biomedical science. This blend of perspectives allowed Aravin to understand the interplay between engineering and science and appreciate how that intersection influences the way scientific information is generated and interpreted. He now applies this lens when adapting his communications material to the specific teams he supports. This interdisciplinary grounding continues to guide Aravin’s work, enabling him to translate data into formats that resonate across diverse fields.
Transitioning from academia to industry came with its challenges, however, Aravin considers every step a valuable experience. “I’m not using all of my scientific training in molecular biology in my current role, but I’ve added clinical and technical knowledge on top of what I did during my PhD,” Aravin reflects. “It’s given me a really interesting perspective for my future goals.” He encourages other graduate students to view every experience as a stepping stone,
even if it doesn’t perfectly align with their long-term interests. Developing soft skills— like communication, collaboration, and adaptability—can be just as important as subject-matter expertise in industry roles. In his view, these broader skills often shape fulfilling career paths.
For current IMS students, Aravin’s message is one of exploration and optimism. He encourages students to pursue opportunities both within and outside their research expertise, noting that each experience contributes to personal and professional growth. He also reminds students that career paths don’t always follow a linear path—interests can shift after a conversation, a new connection, or an unexpected opportunity. As for success, Aravin defines it by progress. “If you’re growing in your role, learning new things, developing new relationships, that should be the definition of success,” he says. Aravin’s journey from the lab to science communications is a reminder that research can lead to more than one career trajectory—with curiosity and adaptability, it can be the foundation for impactful work beyond the lab.
References

By Anita Rajkumar
Caroline Ruivo, the newly-appointed Executive Assistant to the Director of the Institute of Medical Science (IMS), has a deep understanding of how both academic experiences and personal interests can be combined within your professional career. With a natural inclination towards creative art from an early age—she has been a children’s Art Instructor for more than ten years— Caroline enrolled in an Art Illustration course at Seneca College after completing her undergraduate studies in Psychology at York University. Although the course provided an opportunity to explore her interests in creative art, she ultimately chose not to complete the program after realizing that she wanted to focus on furthering her academic studies and keep art as a personal passion instead.
Transitioning beyond her undergraduate studies, she wanted to try something new and see where it would take her, leading her to complete a Master’s degree in Developmental Psychology and Education at the University of Toronto. Caroline later worked as a Cognitive-Behavioural Therapy (CBT) Life Coach where she supported individuals experiencing anxiety, depression, and suicidal ideation. While she valued this work, she realized that studying Psychology and practicing it were very different experiences. This led her to her current position at IMS, where she could give back to the University of Toronto, a place she knows well and feels at home in as an alumna.
She found her previous roles and experiences acted as building blocks for the skills she uses in her current position. As an example, her tasks involve designing award announcements for students or welcome guides for faculty members, which allows her to incorporate her passion for creative art. She highlighted how “a lot of the times when something comes naturally to us or we have a specific talent such as art, we think we need to hone in on one specific career outcome, such as becoming an artist. However, you can incorporate art in any field or industry. You can find outlets to be creative.”
For Caroline, art is found in the quiet moments of everyday life, whether in the delicate swirl of cream in your morning coffee or the simple act of preparing a meal. When asked about her thoughts on the intersection of art and science, Caroline believes they are very similar: you don’t have all the answers at first, but you’re willing to explore and navigate challenges to reach them.
She recently came across virtual reality headsets that present different healthcare scenarios in real time which made her think of the possibilities and the lives that can be improved through art. It made her realize that curiosity is enough to lead you to a masterpiece, which can be a breakthrough in science or medical care.
When reflecting on her graduate studies, she wishes she was more precise and clearcut if she were to do it again. However, she

does see the beauty in not having a plan and going with the flow, allowing you to dip your toes into multiple roles to learn what you like and don’t like. Her greatest advice to students is to practice selfcompassion. “No matter what everyone is going through, just be kind to yourself,” she said. “It’s a very stressful time in life and giving yourself grace to navigate a new trajectory is really important.”


Artist Statement:
This piece illustrates the connection between vulnerability and strength within emergency care. The flowers symbolize hope and healing, while the anatomical heart and subtle ECG line evoke the urgency of needing medical assistance. My father has undergone emergency heart surgery and this illustration is a tribute to the compassion and precision that sustains life when every second counts. I wanted to capture the contrast between clinical and emotional, as they are both deeply intertwined in every patient’s experience.

By Jasmine Amini
Over 6 million Canadians do not have a family physician. 1 That’s nearly 1/6 of us without access to primary care. Beyond the personal impacts of not having a trusted health professional to turn to in times of need, it’s safe to say that insufficient primary care access has wreaked havoc on the Canadian health care system. From delayed diagnosis to worsening chronic conditions to ballooning emergency room wait times, every one of us is affected by our crumbling primary care system. How did we get here? More importantly, how do we recover, both literally and metaphorically?
Authored by former federal Minister of Health and primary care physician Jane Philpott, Health for All: A Doctor’s Prescription for a Healthier Canada 2 explores the antecedents underpinning the ongoing collapse of Canada’s primary care system. Moreover, the author outlines a multifaceted plan to address shortcomings in current health policy and practice, tying in her experiences as a clinician and policymaker. In just under 300 pages, Philpott explores the clinical, spiritual, social, and political factors that, she argues, will be necessary to facilitate systemic change.
Philpott advocates for the widespread introduction of “primary care homes,” (PCHs) which are comprehensive health hubs, equipped with “doctors, nurse practitioners (NPs), nurses, and
administrators, plus others according to the specific community needs” (pg. 17). Some may also include extended supports like physiotherapists, social workers, and dieticians, as well as additional health and social services, such as prenatal seminars and tax clinics, with the goal to serve as a “one-stop shop” for all things health. Critically, instead of the onus of clinical services resting solely on physicians, it would be apportioned among allied health professionals, which would ensure access to primary care for all Canadians when they need it.
Undoubtedly, this vision necessitates more than just funding to be realized. It requires a comprehensive framework that appreciates the various cultural and political factors that will ultimately govern its implementation. Philpott emphasizes the importance of unity in the goal of providing primary care access to all Canadians. From citizens rallying for change to leaders advocating for partnerships between stakeholders at the federal, provincial, and municipal levels, everyone has a role to play. These plans cannot come to fruition, the author stresses, without recognizing the need for systems of care that promote hope, belonging, meaning, and purpose. Although she highlights the First Nations Mental Wellness Continuum framework, which provides tangible steps to support individual wellbeing, this
section focuses on her personal experiences and religious beliefs, making it feel somewhat vague and conceptually detached from the rest of the book. Finally, Philpott turns her attention to various social and political issues related to health care access more broadly, including the legacy of residential schools on health policy and strategies to address Canada’s opioid use epidemic.
Health for All is an ambitious primer to the intricacies of the Canadian primary care system that straddles the line between memoir and policy paper. Philpott’s personal experiences as a primary care physician and former health minister offer engaging insights into how current shortcomings in health care policy and access impact patients. However, these experiences, at times, fail to comment on or advance the vision that she has described to universalize primary care access. As such, the book’s overall “goal” is somewhat muddled. Regardless of these drawbacks in structure, Health for All is an accessible, entertaining introductory text that empowers readers to advocate for our primary care system, a necessary step to enacting change.
References

By Anita Rajkumar
This summer I had the privilege of attending the Cancer Prevention Conference in London, United Kingdom hosted by Cancer Research UK and the American Cancer Society.
As one of three students selected from Toronto, I was honoured to share my research on hereditary breast cancer at an international level, while networking with leading clinicians and scientists in cancer prevention research.
The three-day conference was packed with various speaker sessions and networking events that explored the intersection of aging, genetics, and cancer development. It also provided insights into advances in pre-cancer biology, as well as inequalities that influence cancer risk and incidence. Each day began with a keynote address, followed by flash talks from emerging researchers, panel sessions, debates, and scientific poster presentations. Notable sessions included Dr. Elizabeth Jaffee

from Johns Hopkins University School of Medicine discussing the burden of cancer worldwide, Sir John Burn from Newcastle University highlighting the role of aspirin in the prevention of colorectal cancer, and Dr. Prabhat Jha from the University of Toronto discussing the global effects of smoking, quitting, and taxing tobacco. These sessions displayed high engagement due to their global relevance.
The unique aspect of this conference was that it was heavily trainee-focused, meaning that there were plenty of formal and informal networking sessions tied into the agenda. On the first night, there was a trainee dinner designed to connect early-career researchers with peers and senior leaders in the field based on an assigned table topic. I had the opportunity to chat with Dr. Sarah Blagden, a medical oncologist and clinician-scientist at the University of Oxford, about modifiable lifestyle factors in cancer prevention and learned about her road to research. The second night ended with a cocktail dinner at SEA LIFE London Aquarium nestled along the River Thames, where I further connected with other trainees while exploring aquatic exhibits.
One of the best parts about visiting London in the summer were the late sunsets at around 10 pm, which allowed me to squeeze in some sightseeing after conference activities. Major tourist attractions were within walking distance including Big Ben, Westminster Abbey, Tower Bridge, Tower of London, and national museums. I was lucky enough to see His Majesty King Charles III as he drove by in his royal motorcade from

Buckingham Palace! I also explored the vibrant streets of Notting Hill, which is the backdrop for the iconic film “Notting Hill,” starring Julia Roberts and Hugh Grant. Other stops included Hyde Park and Kensington Gardens, Covent Garden shopping district, and Windsor Castle, the official residence of the royal monarch.
The food scene and café options in London were spectacular! From British staples to Italian and Thai food, every bite was memorable. It was my first time trying a traditional British scone with clotted cream and strawberry jam at The Cheeky Scone which cannot be beat! Another must try is the slow-roasted pork sandwich from The Black Pig at Borough Market which was well worth the wait despite the long line!
I’m grateful to have had the opportunity to visit London and immerse myself in a new culture. The learning experiences and connections I gained were beyond what I expected and I’m excited to apply all the knowledge learned to my graduate research!

By Alicia Tran
Students, clinicians, and faculty members eagerly gathered at the Li Ka Shing Auditorium at St. Michael’s Hospital on Wednesday, November 19th, 2025, for the 15th Annual Ori Rotstein Lecture, one of the Institute of Medical Science’s most anticipated yearly events. The lecture delved into one of the most pressing frontiers in medical science: how sex and gender shape health and disease.
This year’s keynote speaker was Dr. Karen Reue, a distinguished professor in the Department of Human Genetics at the University of California, Los Angeles. Dr. Reue delivered a compelling lecture on biological sex and disease mechanisms in obesity, drug reactions, and cardiometabolic disease risk. Her research challenges the long-held assumption that sex chromosomes serve only to direct reproductive development. While these developmental roles are essential, she explained that sex chromosomes are also involved in more intricate processes within every cell of the human body and throughout the lifespan.
Presenting data from her lab’s genomic and metabolic studies, Dr. Reue illustrated how sex chromosomes drive differences in disease trajectories between males and females. One of her key findings was that fat distribution is strongly influenced by sex chromosomes, with female mouse models having higher fat mass and distinct fat depots under the skin. These findings have important implications for understanding differential obesity risk and cardiometabolic disease patterns between sexes.
Following the keynote lecture, the morning transitioned to an insightful panel discussion on the role of biological sex in disease mechanisms.
Moderated by Dr. Ori Rotstein (Unity Health Toronto), the panel brought together experts whose fields spanned neuroscience and cardiovascular health. Joining Dr. Reue onstage were Dr. Liisa Galea (Centre for Addictions and Mental Health), Dr. Tatyana Mollayeva (KITE Research Institute), Dr. Subodh Verma (St. Michael’s Hospital), and Dr. Jennifer Rabin (Sunnybrook Research Institute).
The panel unfolded as an interdisciplinary conversation highlighting the perils of overlooking sex and gender in health research. Panelists pointed to persistent disparities in clinical trials and diagnostic practices, noting that women often present with atypical or under-recognized symptoms in several disorders, including cardiovascular and neurological conditions. These gaps, they emphasized, can lead to delayed diagnoses and poorer treatment outcomes.
A recurring message throughout the discussion was the vast gap in funding and recognition for sex-specific research. Despite growing acknowledgement of the issue, only a small fraction of research funding addresses women’s health issues. The panelists underscored the importance of sustained investment in women’s health research to ensure scientific findings reflect biological diversity.
The discussion also highlighted the critical role of emerging scientists in driving change. Several speakers encouraged students and trainees to continue pushing for sex-inclusive and gender-responsive study designs, further emphasizing that advancing this field of research requires persistence as well as strong mentorship and institutional support.
This year’s Ori Rotstein lecture was a timely reminder for a more equitable approach to understanding human health. We extend our sincere gratitude to Dr. Rotstein for his dedication to promoting translational research with the IMS community. We also thank Dr. Reue and the panelists for their enlightening contributions. Lastly, we acknowledge the IMS Ori Rotstein Planning Committee for organizing another successful and impactful annual lecture!


Panel discussion on “The Role of Biological Sex in Disease Mechanisms: Insights from Neuroscience and Cardiovascular Research”, featuring experts in the field of neuroscience and cardiovascular health.
Author and Illustrator: Cathy Zhou


View the full comic here:


Cathy is a second-year MScBMC student in Toronto, Canada. She is particularly interested in pharmacology and toxicology, and new, inventive graphic design. You can find her on her website at cathyzhou.com

issuu.com/imsmagazine imsmagazine.com @IMSMagazine