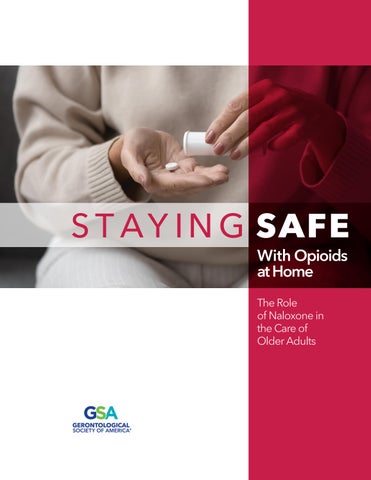
safe staying With Opioids at Home
The Role of Naloxone in the Care of Older Adults


With increasing age, older adults are more likely to encounter health conditions and injuries that may require opioid therapy for pain relief. This reality means that opioid overdoses are a concern for older adults as well as for their family members and other caregivers.
This decision aid serves as a guide to questions about pain management and opioid reversal that older adults and their caregivers can ask themselves and the older adult’s health care team. Caregivers should take the steps described in this guide if someone has signs and symptoms that indicate an apparent overdose.
Developed by

Key Points for Pain Therapy
1. Naloxone (also commonly known as the brand name Narcan) is a medication that can be used to restore breathing in people who have overdosed on opioids. When opioids are prescribed, the health care professional should also prescribe naloxone. Consumers can also purchase naloxone without a prescription.
2. To be prepared for a possible opioid overdose, naloxone should always be in the home if prescribed opioids are present or if any family members bring in opioids that were not purchased at a pharmacy.
3. Naloxone works by temporarily reversing the effects of opioids like heroin, fentanyl, and prescription painkillers.
4. When opioids are present in the home, they must be stored properly—safely away from pets, children, and drug-seeking adolescents and adults.
5. If someone appears to be unconscious and is not breathing normally, the life-saving medication naloxone should be administered.
6. Sedation and opioid overdoses are difficult to tell apart. When in doubt, act.
7. Even if a person has been safely taking opioids for a while, an overdose still can occur. The body’s responses to opioids can change, doses can be increased, or changes may be made to a different opioid or interacting drug.
8. Naloxone will not hurt a person even if it turns out there wasn’t an overdose.
9. Lay, spray, and stay are the basic steps in naloxone rescue.
10. First administer a dose of naloxone, and then call emergency services.
11. It is essential to act quickly, as minutes matter in opioid overdoses. Death or permanent brain damage can occur quickly in someone who is in respiratory failure.
12. A person may need multiple doses of naloxone, especially if fentanyl or other synthetic opioids are involved because these drugs can be stronger and longer-lasting.
13. A person who receives naloxone needs to be evaluated by medical professionals even when naloxone works initially. Additional naloxone doses may be needed to keep the person breathing.
14. This guide contains a decision tree for family members and caregivers, medical professionals, or bystanders in assessing whether an overdose is occurring and when to administer naloxone.
15. June 6 is National Naloxone Awareness Day. Plan activities in your community to promote naloxone awareness and proper ways of using it. Educational materials are available on many websites, including SafeProject.org

When opioids are needed, how can we monitor their effects, store them, and discard leftover medication?
Opioids are powerful and potentially addictive drugs that are sometimes needed for treating severe pain. When someone you live with or care for is interacting with opioids—to treat short- or long-term pain or for other reasons— family members, caregivers, friends, and other acquaintances must know about the adverse effects of these drugs and how to recognize and respond in cases of apparent overdoses.
Opioids must also be stored securely and discarded when they are no longer needed. As a patient, family member, or other caregiver, you should know what questions to ask during the evaluation and prescribing process and what to ask your pharmacist about methods for storing opioids securely and disposing of leftover products.
Safe Prescribing of Opioids
Physicians, dentists, and other health professionals grew accustomed over the years to prescribing opioids for a variety of relatively simple surgeries and minor conditions. Many of these situations are now recognized as responding well to nonopioid therapies. Always question the need for opioids when nonprescription drugs or other prescription medications could be strong enough to relieve pain.
If opioids are prescribed, the patient and caregivers should be sure they receive and fill a naloxone prescription. They can also purchase naloxone without a prescription by paying out-of-pocket. People often do not take all the opioid medication they are given, and these leftover medications lie forgotten in drawers and medication cabinets for long periods of time. Pets and children may discover and eat them.
?Questions to Ask Your Care Team
• Do I really need opioids?
• Would something with fewer side effects and problems be enough to stop my pain?
• If I need an opioid, why was this product chosen for me? Is it the best and the safest for me?
• How would my family members and care providers know if my dose is too high? What should they do if they are concerned that I’ve overdosed?
• So that my insurance covers it, could you prescribe naloxone in addition to the opioid?
Teenagers or adults who are experimenting with drugs or addicted to opioids may find and take these drugs. You never know when naloxone may be needed.
Patients, their families, and all caregivers should be educated about overdoses, how to recognize them, and what to do if they even suspect an overdose (for more, see page 11).
Safe Storage of Opioids
When opioids are present in the home, they must be stored properly—safely away from pets, children, and drug-seeking adolescents and adults. Recommended practices for the storage of opioids include the following:
• Use a locked cabinet or a medication lock box or drawer.
• Avoid storage in easily accessible areas such as bathrooms or kitchens.
• Keep opioids and other medications in their original containers with information on proper use and side effects.
• Keep track of the number of tablets or capsules remaining in the home.
• Educate all family members and caregivers on the risks associated with opioid use.
• Avoid storage in purses or bags to prevent theft or pilfering.
• Keep medications in locked containers when traveling and maintain a list of all transported medications.

Safe Disposal of Opioids
Just as safe storage is important, opioids should also be disposed of properly.
The best way to dispose of opioids safely is by taking them to a collection site registered by the U.S. Drug Enforcement Administration (DEA). These drop-off locations are usually pharmacies or law enforcement agencies. Twice each year, the DEA sponsors National Prescription Drug Take-Back Days with numerous locations available to receive unneeded medications, including opioids. Consumers can also ask pharmacists for preaddressed envelopes to mail unneeded opioids back to the pharmacies.
When those options are not available, the next best choice is making the drug products unpalatable or impossible to use before disposing of them in household trash. One method is mixing crushed-up drug products with coffee grounds, cat litter, or dirt. Another is to dissolve the products in water mixed with vinegar or dish soap and then soak up the solution using paper towels. Either way, the unusable drugs can be discarded in household trash.
High-risk products such as hydrocodone and fentanyl can be flushed down the toilet when other options are not feasible. Check the U.S. Food and Drug Administration (FDA) drug disposal flush list to determine whether a product can be safely flushed.

?Questions to Ask Your Care Team
• Is there a medication take-back option readily available?
• If not, is the medication on the FDA “flush list”?
• What is the best way to dispose of this medication in the household trash?
What are the most common and the most serious side effects of opioids?
The most common side effects of opioids are sedation, constipation, euphoria, and mood changes. Prevention is the first step in managing these side effects. When these red-flag side effects occur, patients and caregivers must monitor the patient and be prepared to take prompt action. Sedation is the focus of this guide, but constipation, euphoria, and mood changes are also important to recognize and treat.
Sleepiness and sedation are difficult to distinguish from opioid overdose. Family members and other caregivers can take these actions to detect and manage sedation during opioid therapy:
• Watch diligently for signs of excessive sedation, such as difficulty waking the patient, dizziness, or confusion.
• Take and record vital signs (pulse and respiratory rates, and, when possible, blood pressure and oxygen saturation).
• Report to the patient’s health care professionals all current therapy with medications, supplements, and nonprescription drugs as well as any recreational drug use.
• Ensure that the patient follows the prescribed dosing instructions and does not take extra doses.
• Encourage the older adult to avoid alcohol and other sedating drugs, including benzodiazepines such as diazepam (Valium) and alprazolam (Xanax).
Has the older adult ever used illicit drugs, or might the person be currently using recreational drugs?
Three-fourths of the Baby Boom generation are now in the over-65-year-old population. Some of these older adults have been around—or participated in—drug use at some point during their adult lives. Caregivers need to consider the possibility that an older adult could be using other drugs, sometimes secretly, when opioids are added to their drug regimen. In addition, drug use in past years can change the way older adults respond to opioids and other drugs that affect the brain.


All these factors make it important for the caregiver to be alert to adverse effects or opioid overdose among older adults in their care. Older adults with past histories of substance abuse may be on treatments such as methadone or buprenorphine, and these can increase the risk of opioid overdose.
Safely using opioids requires attention to these instructions by everyone involved at all times:
• Never take more opioids than prescribed without first consulting the health care provider or pharmacist.
• Keep a record of any changes in signs and symptoms or reactions to the opioids during treatment.
• Ensure family members know the signs that indicate an emergency situation requiring immediate medical attention.
Exactly what do family members and other caregivers do if an older adult appears to have overdosed?
As shown in the decision tree on page 11, signs of potential opioid overdoses include excessive sleepiness or trouble staying awake, walking, or talking. Other signs of an overdose are slow or shallow breathing, snoring or gurgling sounds, pale or cold skin, blue lips or fingernails, or constricted (small) pupils. If these signs are present, call the person’s name loudly, shake them,and rub your knuckles on their sternum (center chest) to try and wake them up.
If the patient does not awaken, immediately administer naloxone. Lay the patient on their back and tilt their head up. Follow the instructions provided with the product you are using. For intranasal sprays, insert the nozzle into the nostril and press until the unit clicks to spray. For injectable naloxone, use the device as directed, injecting the medication into the outer thigh or upper arm (like an EpiPen).
Naloxone quickly reverses an overdose by blocking the effects of opioids. It can restore normal breathing within 2 to 3 minutes in a person whose breath has slowed, or even stopped, as a result of opioid overdose. After the naloxone dose is given, place the person on their side with the top leg bent to prevent choking if they vomit.
Call emergency medical services (911 in North America) after administering the first dose of naloxone. Tell emergency services where you are and describe the patient’s condition. If you have experience monitoring someone’s vital signs, record their heart rate, breathing rate, and when possible, oxygenation and/or blood pressure. When help does arrive, give them the patient’s vital signs if you were able to take them.
Stay with the person until help arrives. The effects of naloxone only last for up to 90 minutes, and the opioid still in the patient’s system could again suppress breathing. Continue to observe the patient. If breathing is not restored after 3 minutes, give additional doses of naloxone every 2 to 3 minutes until help arrives. Emergency services can help you determine when you need to administer another dose.
Questions to Ask Your Care Team
• What if I’m not sure whether the person has overdosed? What if they are just sleeping?
• Will naloxone hurt them if they didn’t really overdose?
• Do we need to take the naloxone everywhere we go?
minutes matter overdose act quickly lay, spray & stay emergency euphoriaprescription awareness confusion mood
sedation
opioids safet y
Conclusion
Opioids are powerful drugs that can control severe pain. However, overdoses still can occur even in patients who have been using opioids for a while. The body’s responses to opioids can change, doses can be increased, or therapy may be switched to a different opioid.
As shown in the decision tree (see page 11) and the information in this guide, family members and caregivers for older adults play an essential role in opioid safety. By knowing what signs and symptoms to watch for and what to do for opioid overdose, these individuals can protect the health and lives of older adults.
Decision Tree for Use of Naloxone for Possible Opioid Overdose
A decision tree (see page 11) for when to use naloxone (also commonly referred to by the brand name Narcan) for an opioid overdose can help guide family members and caregivers, medical professionals, or bystanders in assessing whether an overdose is occurring and when to administer this life-saving medication.
Key Points
When using the decision tree, remember these tips:
Always call emergency services immediately, even if you are trained to use naloxone and know rescue breathing techniques.
Naloxone works by temporarily reversing the effects of opioids like heroin, fentanyl, and prescription painkillers.
It is important to act quickly because opioid overdoses can lead to death from respiratory failure.
A person may need multiple doses of naloxone, especially if fentanyl or other synthetic opioids are involved because these drugs can be stronger and longer-lasting.
Even if naloxone revives the person, they still need to be evaluated by medical professionals because the effects of naloxone wear off faster than the opioids in the system.
Decision Tree: How to Use Naloxone for Management of Potential Opioid Overdose
LAY the person down in a safe position.
SPRAY the Naloxone into each nostril.
STAY with the person until help arrives.
• No need for naloxone.
• Observe for any changes
Step 1 Is the person responsive?
Step 3
Administer first dose of naloxone according to instructions.
Step 2 Are signs of opioid overdose present?
Step 4 Call EMS now!
• No need for naloxone.
• Observe for any changes
Signs of Overdose
• Unresponsiveness.
• No or shallow breathing.
• Blue lips or nails.
• Pinpoint pupils.
• Unusual drowsiness or inability to stay awake.
Step 5
• Monitor the person.
• Does the person regain consciousness or start breathing again?
NO
Step 6
Continue giving naloxone every 2 to 3 minutes until the person wakes up or EMS arrives.
Call MedicalEmergencyServices (EMS) NOW
Even if you have naloxone, you need to have EMS assess the person and likely transport them to a medical facility.
Naloxone can be administered by spraying an intranasal product into the person’s nose or using an injectable product as instructed (into the person’s thigh or upper arm)
Continue monitoring the person until EMS arrives.
2025 Gerontological Society of America • geron.org


geron.org/pain