2 Understanding Breakthroughs in Brain Health
A compilation of the insights and implications of key scientific articles from January through May 2025 with important impact on primary care for brain health.

advisory board
Soo Borson, MD
Deputy Editor, Journal of the American Geriatrics Society
Co-Lead, BOLD Center of Excellence on Early Detection of Dementia
Professor of Clinical Family Medicine, USC Keck School of Medicine
Professor Emerita, Psychiatry and Behavioral Sciences, University of Washington School of Medicine
Barak Gaster, MD
Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine
Frederick Ketchum, MD, PhD
Assistant Professor, Department of Neurology, University of Wisconsin School of Medicine and Public Health
Anna Pendrey, MD, DABOM
Assistant Professor, Clinical Family Medicine–Geriatrics–Obesity Medicine
Associate Director, Indiana University Student Outreach Clinic School of Medicine, Indiana University
Kemi Reeves, DNP, MBA, GNP-BC
Associate Director, UCLA Alzheimer’s and Dementia Care Program, Division of Geriatrics, David Geffen School of Medicine at UCLA
Director of Nursing Health Care Equity, Office of Health Equity and Inclusive Excellence, UCLA Health System
Understanding Breakthroughs in Brain Health
Introduction
Welcome to the second issue of Insights & Implications: Understanding Breakthroughs in Brain Health! This series from the Gerontological Society of America (GSA) is designed to support clinicians in their efforts to gather recent research and implement relevant findings regarding brain health in primary care practice.
The emergence of new approaches for detecting and treating dementia, combined with a growing aging population, has renewed the emphasis on brain health in primary care practice. New tools make it easier to diagnose dementia early and intervene, giving primary care providers opportunities to improve care for their patients. However, remaining abreast of new literature about the rapidly expanding science behind the care of patients with dementia remains an ongoing challenge for busy clinicians.
This second issue of Insights & Implications summarizes key articles from the first five months of 2025 that may

have an important impact on primary care for brain health. Articles address new guidelines to inform diagnostic strategies, identification of risk factors for the development of dementias, current statistics related to dementias, the impact of various dosing strategies on the risks and benefits of donanemab treatment, and a new measure for assessing treatment outcomes.
The article selection process, guided by an expert advisory board, has identified scientific articles published in the first five months of 2025 with actionable implications for primary care providers. Stay tuned for future issues.


geron.org/brainhealth
contents
Introduction
5 6 7 3 2
4
Article 1.
The Alzheimer’s Association clinical practice guideline for the diagnostic evaluation, testing, counseling, and disclosure of suspected Alzheimer’s disease and related disorders (DETeCD-ADRD): Validated clinical assessment instruments.
Article 2. Modified titration of donanemab reduces ARIA risk and maintains amyloid reduction.
Article 3.
2025 Alzheimer’s disease facts and figures.
Article 4. Modifiable risk factors for stroke, dementia and late-life depression: a systematic review and DALY-weighted risk factors for a composite outcome.
Article 5. Defining benefit: clinically and biologically meaningful outcomes in the next-generation Alzheimer’s disease clinical care pathway
Article 1.
The Alzheimer’s Association clinical practice guideline for the diagnostic evaluation, testing, counseling, and disclosure of suspected Alzheimer’s disease and related disorders
(DETeCD-ADRD): Validated clinical assessment instruments.
insights
This guideline was developed by an expert workgroup that identified validated clinical instruments to support an evidence-based, patient-centered diagnostic evaluation for patients with symptoms suggestive of Alzheimer’s disease and related dementias (ADRD).
Although history taking (cognition, mood, behavior, daily function), examination of mental status, and neurological examinations are central to the diagnosis of ADRD, using validated assessments increases diagnostic accuracy, enables earlier detection, and improves patient outcomes. The guideline includes assessments that can be self- or informant-reported, clinician-administered, or adapted for telemedicine. They assess several domains:
• Cognitive symptoms (for example, Montreal Cognitive Assessment, or MoCA; Mini-Mental State Examination, or MMSE; General Practitioner Assessment of Cognition, or GPCOG; clock-drawing test).
• Functional impairment (for example, Functional Activities Questionnaire, or FAQ; Disability Assessment for Dementia).
• Mood and behavioral symptoms (for example, Neuropsychiatric Inventory; Mild Behavioral Impairment Checklist).


implications
Until recently, guidelines for diagnosing cognitive impairment in ADRD were decades old and targeted to specialists. This evidence-based guideline, in contrast, is developed for primary care providers and offers a structured approach for evaluating patients with cognitive impairment that includes the domains of cognitive symptoms, functional impairment, and mood and behavioral symptoms. Validated ADRD assessments should be interpreted along with history, risk factors, and clinical judgment, not used in isolation.
Validated ADRD assessments should be interpreted along with history, risk factors, and clinical judgment, not used in isolation.
Atri A, Dickerson BC, Clevenger C, et al. The Alzheimer’s Association clinical practice guideline for the diagnostic evaluation, testing, counseling, and disclosure of suspected Alzheimer’s disease and related disorders (DETeCD-ADRD): Validated clinical assessment instruments. Alzheimers Dement. 2025;21(1):e14335. doi: 10.1002/alz.14335.
Article 2.
Modified titration of donanemab reduces ARIA risk and maintains amyloid reduction.
insights
Removing amyloid from the brain using targeted monoclonal antibodies such as donanemab has been shown to slow the progression of Alzheimer’s disease (AD). However, monoclonal antibodies can be associated with adverse events, including amyloid-related imaging abnormalities with edema or effusions (ARIA-E), which are transient changes seen on imaging. ARIA-E is most likely to occur in earlier stages of treatment. Thus, researchers have explored whether modifying the initial regimen for treating AD reduces the risk for ARIA-E.
TRAILBLAZER-ALZ 6, a multicenter, double-blind, ongoing phase 3b study of 843 participants with early symptomatic Alzheimer’s disease, investigated the impact of various dosing regimens for donanemab on the occurrence of ARIA-E. It employed a standard regimen—three doses of 700 mg monthly followed by 1,400 mg monthly—and three alternate approaches. One alternate approach, a modified titration schedule, involved a gradual increase from 350 to 700 to 1,050 and then 1400 mg. The other alternate approaches involved dose skipping and more frequent but smaller doses. The primary outcome was a relative reduction

of the risk of ARIA-E at 24 weeks in all three alternate approaches. ARIA-E frequency was 13.7% in the modified titration regimen compared with 23.7% in the standard regimen at week 24, and there were no severe ARIA-E events under the modified regimen. (Rates of ARIA-E for the other two modified approaches fell between those for the standard and modified titration regimens.) The risk of ARIA-E was reduced from 57.1% to 19.0% in individuals at high genetic risk (those who are homozygotes for the apolipoprotein E, or APOE, ε4 allele).
Aside from the incidence of ARIA-E, the modified titration and standard regimens showed comparable safety profiles, amyloid reduction, plasma phosphorylated tau217 reduction, cumulative exposure, and pharmacokinetics. Data at week 52 were consistent with week 24 results.
implications
A modified donanemab dosing schedule using gradual increases in titration reduced the frequency and severity of ARIA-E events. The modified schedule did not affect efficacy of amyloid plaque clearance or biomarker improvement. These findings suggest that the modified titration schedule may be a safer alternative, especially for those who are at higher genetic risk, without compromising efficacy.
Wang H, Nery ESM, Ardayfio P, et al. Modified titration of donanemab reduces ARIA risk and maintains amyloid reduction. Alzheimers Dement. 2025;21(4):e70062. doi: 10.1002/alz.70062
Article 3.
2025 Alzheimer’s disease facts and figures.
This article, a report from the Alzheimer’s Association, provides the latest statistics on Alzheimer’s disease (AD) and other dementias in the United States, including data regarding prevalence, mortality, caregiving, workforce issues, and costs of care.
Topics covered in this year’s report include the following:
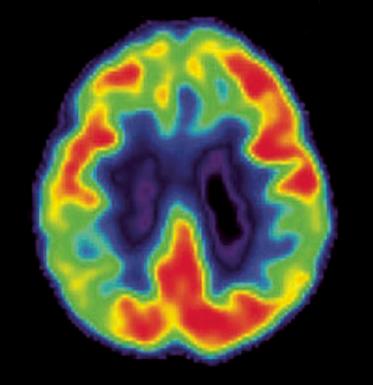
• Brain changes that occur with AD.
• Risk factors for AD.
• Incidence of AD nationally and for each state.
• Gender, racial, and ethnic differences in the prevalence and risk of dementias.
• Number of deaths due to AD nationally and for each state, as well as death rates by age.
• Number of family caregivers, hours of care provided, and economic value of unpaid care nationally and for each state.
• The impact of caregiving on caregivers.
• The impact of COVID-19 on dementia caregiving.
• The roles of the paid workforce involved in diagnosing, treating, and caring for people with AD or other dementias.
• Costs of care for individuals with AD or other dementias.
• Medicare payments for people with dementias compared with those for people without dementias.
models are urgently needed. Furthermore, approximately 11 million family caregivers provide more than 16 billion hours of unpaid care annually.
The 2025 report includes a special report with results of a survey of adults in the United States, 45 years of age and older, about their perspectives on early detection of AD in the era of treatment.
implications insights
The report reveals that, in 2025, approximately 7.3 million people ages 65 years and older are living with AD in the United States. Women and people of Black and Hispanic race and ethnicity are disproportionately affected. Age is the strongest risk factor for AD and other dementias, but genetics; family history; conditions such as hypertension, diabetes, and obesity; and behaviors such as smoking also increase risk.
In 2025, total payments for health care, long-term care, and hospice for people with dementias were estimated to be more than $400 billion. Medicare and Medicaid cover most of the costs due to dementias; however, families pay high out-of-pocket expenses. Importantly, there are significant shortages in the paid workforce for dementia care, particularly with rising demand, and collaborative multidisciplinary care
Most people surveyed for the report support early detection of AD, particularly as new treatments (for example, lecanemab and donanemab) that can slow progression of the disease in people with mild cognitive impairment or mild dementia have emerged. Blood-based biomarker tests can enable more timely, widespread diagnosis and can facilitate early detection.

More people are living with AD and other dementias than ever before, and the costs for individuals, caregivers, family, and society are enormous. New treatments offer opportunities to delay the progression of AD but pose challenges regarding access, equity, and affordability. Early detection, better workforce training, and investment in care infrastructure are essential for the future.
2025 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2025;21:e70235. doi: 10.1002/alz.70235.
Article 4.
Modifiable risk factors for stroke, dementia and late-life depression: a systematic review and DALY-weighted risk factors for a composite outcome.
insights
Three major age-related brain diseases—stroke, late-life depression (LLD), and dementias—share similar underlying vascular pathology. This article reports findings from the first systematic review of meta-analyses of overlapping modifiable risk factors for these conditions. Researchers calculated the relative impact of each of these risk factors for these brain diseases. Effect sizes were adjusted using disability-adjusted life years (DALYs) to reflect each disease’s global burden.
Hypertension was found to be the risk factor increasing disease burden most strongly, followed by (ranked in descending order by size of increase) severe kidney disease, hyperglycemia, smoking, poor sleep, high body mass index, hearing loss, depressive symptoms, stress, and pain. The greatest protective factor was found to be leisure-time cognitive activity, followed by high levels of physical activity, large social networks, and healthy diet elements (fruits, vegetables, and nuts).

implications
It is estimated that at least 60% of strokes, 40% of dementias, and 35% of LLD could be prevented by addressing modifiable risk factors. This study generated a ranked list of risk factors that affect the development of these age-related brain diseases. These risk factors all involve health issues that can be addressed in primary care.
Primary care providers can use the list of risk and protective factors to guide preventive strategies and empower patients to reduce their risk of strokes, dementias, and LLD through lifestyle, psychosocial, and medical interventions.
Senff J, Tack RWP, Mallick A, et al. Modifiable risk factors for stroke, dementia and late-life depression: a systematic review and DALY-weighted risk factors for a composite outcome. J Neurol Neurosurg Psychiatry. 2025;96(6):515-527. doi: 10.1136/jnnp-2024-334925.
Article 5.
Defining benefit: clinically and biologically meaningful outcomes in the next-generation Alzheimer's disease clinical care pathway
To integrate biomarker test results with cognitive and functional assessments, the authors propose a Minimum Biologically and Clinically Important Difference (MBCID) measure. The measure would capture outcomes that are most important to patients and caregivers, including preserved memory, daily functioning, and quality of life and delayed loss of independence. In addition, the MBCID measure would account for changes in biomarkers that predict disease progression, and it can reflect therapeutic effects at earlier stages of AD.
implications insights
This article reviews current knowledge about the underlying biology of Alzheimer’s disease (AD), current staging practices for AD, biomarkers, and strategies for assessing treatment effects over time and presents a new framework for defining meaningful benefit in the management of AD.
The authors explain that AD treatments can affect clinical and functional outcomes as well as the underlying biology of AD. However, many cognitive and functional assessments in current use are not sensitive enough to detect biological changes in early stages of the disease, including preclinical AD and mild cognitive impairment (MCI). Furthermore, they may not capture key treatment outcomes of interest to patients, especially subtle early changes. Treatments that slow the progression of functional impairment and loss of independence in later stages may benefit patients with preclinical AD and MCI.
Patient-reported outcomes are particularly important in preclinical and early stages of AD, as patients are able to report changes that may be less noticeable to observers. Outcomes that patients and caregivers consider most meaningful include cognitive decline, compromised independence, reduced quality of life, and impaired physical health. Meaningful functional domains include complex activities of daily living (for example, financial planning, programming the television, and meal preparation) and interpersonal functioning (for example, conversational skills and comprehension of written material). Functional questionnaires that are sensitive to changes in these domains may be of particular relevance, given that not all functional outcomes are equally important to all patients.
At the same time, recently approved biomarker tests can detect biological changes associated with evolving pathophysiology before clinical symptoms emerge. These new tests also have a role in early detection and evaluation of responses to therapy.
...recently approved biomarker tests can detect biological changes associated with evolving pathophysiology before clinical symptoms emerge.
This article calls for a shift in how the benefits of AD therapies are evaluated, advocating outcome measures that integrate clinical symptoms, patient-reported experiences, and biological data.

The authors underscore the importance of shared decision making and incorporating patient priorities into AD care plans. Discussions about the outcomes patients value most should directly inform treatment choices. Sensitive clinical tools for outcome assessment, particularly in the preclinical and early stages of AD, can help ensure interventions align with patient goals. Primary care providers may also incorporate biomarker findings when assessing treatment effects.
Elhage A, Cohen S, Cummings J, et al. Defining benefit: Clinically and biologically meaningful outcomes in the next-generation Alzheimer’s disease clinical care pathway. Alzheimers Dement 2025;21:e14425. doi: 10.1002/alz.14425.



