HEALTHCARE PLANNING, ARCHITECTURE, AND INTERIOR DESIGN SERVICES











Goodwyn Mills Cawood (GMC), established in 1947, has become one of the Southeast’s largest architecture and engineering firms, employing over 600 professionals. Our teams are dedicated to serving communities by designing schools, parks, hospitals, and commercial developments, as well as providing essential services like clean water and safe streets. GMC’s approach is rooted in the belief that communities are built by people, not companies, and we emphasize quality, integrity, creativity, and care in our projects.
GMC serves a diverse clientele, including government agencies, private corporations, and developers. Our national healthcare practice focuses on designing cost-effective spaces that enhance patient experiences, providing a competitive edge. Our success is reflected in our strong client retention, which is attributed to our expertise and a design process that targets measurable improvements.
Our process is designed to deliver spaces that:
• Enhance the total patient experience
• Provide a safe environment for patients, visitors and staff
• Increase operational efficiency through elimination of waste
• Reduce initial cost while providing a sustainable life-cycle
Healthcare Studio Services
• Acute Care Hospitals
• Academic Medical Centers/Research
• Ambulatory Surgery Centers
• Diagnostic Imaging Centers
• Master Planning
• Medical Office Buildings
• Outpatient Services
• Psychiatric Centers
• Specialty Hospitals
• Sports Medicine and Wellness
• Senior Living Facilities
• Promote wellness through the built environment
• Align the program, floor plan and budget early in the design process to avoid design changes that will impact the schedule
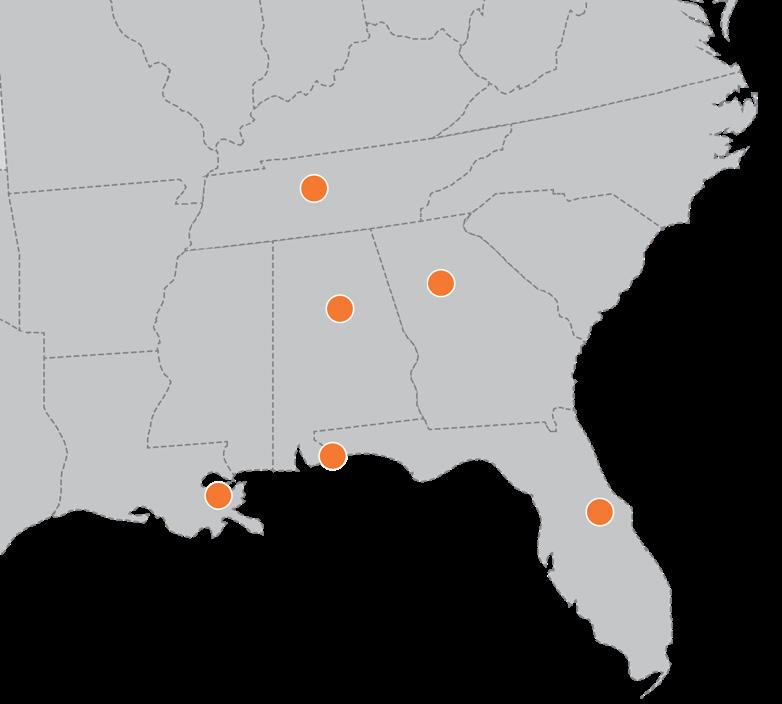
GMC has completed healthcare projects in 39 states. We have served a wide variety of clients, including federal, municipal, commercial, private developers, and hospital systems.

















By Steven Alby / Special to Healthcare Facilities Today
May 22,
2020
Now, more than ever, it may seem difficult to identify time to address major planning goals, but a widespread industry challenge such as the COVID-19 pandemic exposes opportunities for improvement as infrastructure is tested.
Simultaneously, there is also time to pause infrastructure development efforts as non-essential activities grind to a halt, making way for strategic efforts such as master planning.
As healthcare transitions to a value-based model with an increasing focus on wellness and preventative care, healthcare organizations are seeking opportunities to tailor their services to the communities they serve. To support these services, the facilities being planned are evolving as well, making the planning process more complex and involved than it has been historically.
and specialties. Below are insights for navigating and mastering the master planning process.
Participation Is key. The positioning and “evolution” of an organization’s total real estate holdings must be in alignment with their high-level mission and strategic direction. Because of this organic connection, the master planning must be developed internally and not as a passive activity outsourced to consultants and then presented to senior leadership at
patients and their families. This ensures that multiple viewpoints are considered and contributes to consensus building that gives participants ownership of the master plan and empowers them to implement it.
Every hospital is different. Many healthcare organizations use metrics and benchmarking to streamline the master planning process, but it is important to account for unique demographics that drive different service lines and use rates. For example, a patient population in Florida, which has the highest percentage of residents over 65 in the country, will require different service lines and different ratios of high acuity and outpatient spaces than one in Colorado, where the median age is 37.6 years.

Traditionally, master planning has focused on the acute care hospital campus by identifying ideal locations for expansion and addressing both infrastructure deficiencies and building obsolescence through a lens of future growth. In today’s competitive healthcare industry, the process must also address how to leverage an organization’s physical plant to support the full continuum of care and develop an ambulatory strategy that deploys wellness, primary care,
the end of the engagement. Successful master plans are the result of a robust, collaborative process involving hospital leaders at multiple levels.
While the facilities manager may be responsible for coordinating the process, diverse stakeholder input is critical. Seek to engage and obtain input from all levels of the organization, including C-suite decision makers, physicians, nursing staff, board members, and community representatives, involving
Data. Data. Data. Often healthcare organizations take a Field of Dreams approach to adding new service lines, assuming an “if you build it, they will come” strategy based on potential high profit margins for certain service lines like orthopedics and oncology. Incorporating specific data based on the communities served in the master planning process mitigates the potential for an overbuild – for example, a cancer center with 40 infusion bays when the market catchment area will only support 20.
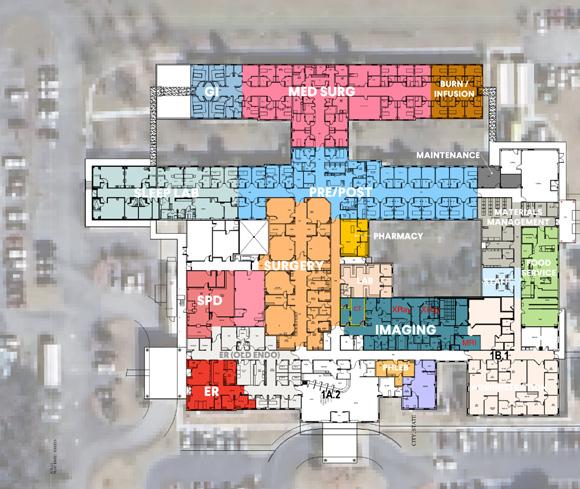
Operationalize your strategy. Use the master planning process to better understand how each service line works: The patient flow, volume, and caregiverto-patient ratio can vary significantly from one service to another. As a starting point, planning teams want to understand how each service line currently operates in its existing space, creating a foundation for Current State vs Future State workshops to identify potential space saving efficiencies.
It is also worth considering a department’s current location relative to other departments and whether they could be collocated more effectively to optimize efficiency. For example, perhaps a department that appears to have outgrown its space could simply move, rather than grow. Getting an accurate picture of their day to day operations and how they use their existing space is crucial in developing strategies for growth and future flexibility.
Factor in financials. At the core of planning, budget drives implementation. A master plan that does not reflect the financial realities of the healthcare organization will only sit on the shelf. A cost estimator who has specific experience in pricing healthcare projects can be an important member of the master planning team, aligning strategy with financial capability.
When planning budgets, remember that the costs for a new facility or expansion into a new service line include more than the cost of the physical assets of building and equipment. There are costs for staff and the operation of the facility that are key to the budget planning as
well as costs associated with physician recruitment, training, and marketing.

Less is sometimes more. Many healthcare organizations approach master planning as an exercise in understanding how best to expand and build new on their campus. With healthcare becoming increasingly focused on population health management and wellness initiatives, a robust ambulatory strategy is often needed to complement the inpatient campus strategy. The acute care campus is naturally a transition to smaller, more compact, higher-acuity facilities that deploy growth in the form of lean operations strategies and other creative means rather than strict physical expansion.
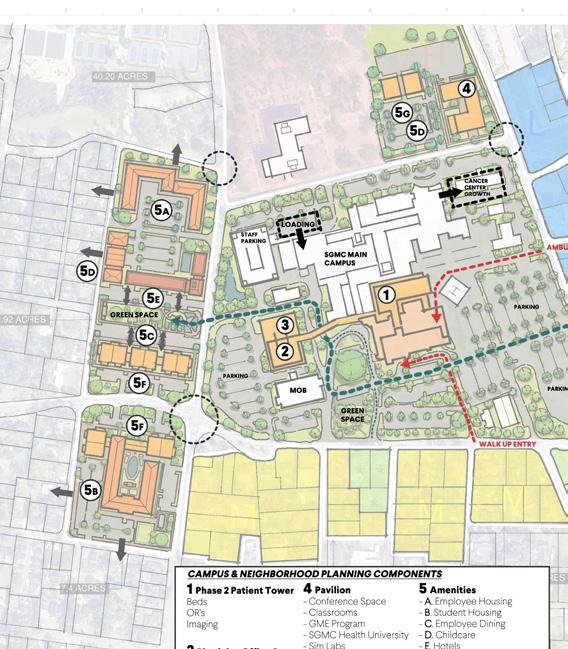
Effective hospital master plans have expanded to address community care and an ambulatory strategy. Ambulatory overlay strategies examine how outpatient buildings might be deployed into the community to improve access to care at lower costs. The master planning process can be a tool to scrutinize the utilization of existing buildings and investigate options for repurposing them to support priorities such as outpatient services. While examining renovation options, be sure to include estimates for new construction, which can often be less expensive than retrofitting.
New projects continually break the mold as the care model shifts from treatment to wellness. The ultimate manifestation of this is a migration to active, retailoriented community spaces that have multiple wellness-related offerings that forma “wellness village.” These could include open park settings with walking
trails, farmer’s markets, or yoga classes. The surrounding facades include medical offices interspersed with fitness centers and health eateries, offering visitors a robust and appealing wellness solution that promotes the idea of keeping people healthy over treating them when they are sick.
Mastering master planning. The master planning process can be complex and difficult to navigate. When done correctly, a successful master plan provides a “living document” that functions as a framework and clear directive for decision-making.
Involving diverse stakeholders in the process ensures that the master plan establishes a uniform vision that is shared among all members of the organization. That ownership fosters an increased level of commitment to the organization and its goals, improved quality of service, and a pathway for future growth.
By the end of the planning process the master plan becomes your master plan. Because of their hands-on role, stakeholders understand the decisions that led to the final plan and how those visions inform its implementation. They’ll also understand what not to do thanks to the detailing in the plan itself. Leaders who have taken the time to participate in the plan’s creation not only understand it, they own it, having mastered the master planning process.
Steven Alby, NCARB, LEED AP, is vice president, healthcare, with GMC. He can be reached at steve.alby@ gmcnetwork.com.


Scope of Services
TASK 1 - Project Initiation Kick-Off
TASK 2 - Assess Site, Infrastructure, Facilities and Departmental Operations
TASK 3 - Conduct Space Benchmark Analysis
TASK 4 - Develop/ Evaluate Facility Planning Options
TASK 5 - Select and Refine Preferred Facility Master Planning Options
TASK 6 - Document Facility

Tasks 1, 2, & 3 (8 Weeks)
• Departmental Tours and Interviews
• Building Ages
• Infrastructure Condition & Capacity
• Parking and Access
• Departmental Benchmarking
Task 4 (8 Weeks)
• Key Planning Units
• Development Zones
• Circulation Diagrams
• Infrastructure Planning
• Parking and Access
• Cost & Phasing Implications
Tasks 5 & 6 (8 Weeks)
• Select Preferred Option
• Site and Department Block Plans
• Massing Diagrams
• Infrastructure Diagrams
• Parking and Access
• Cost & Phasing Charts
• High-level Schedule Document

With 3-4 system-wide master plans completed annually across the U.S., our team delivers fresh insight and proven innovation in healthcare design.
We believe success is defined by design excellence and a creative client/firm partnership that enhances accountability, efficiency, and sustainability. Our integrated approach results in enhanced environments, flexible and innovative spaces, and efficient and environmentally sensitive healthcare buildings. Our performance history on these types of projects is exemplary.
The GMC Healthcare practice focuses on programming, planning and designs that:
• Enhance the total patient experience
• Provide a safe environment for patients, visitors and staff
• Increase operational efficiency through elimination of waste
• Reduce initial cost while providing a sustainable building lifecycle
• Promote wellness through the built environment
Utilizing a patient-centered care approach that combines expertise and national experience, GMC’s team of healthcare architects can assist you with speed-to-market solutions for new construction and renovation projects, from outpatient facilities and greenfield hospitals, to complex diagnostic and interventional platforms.







“ GMC has completed
Surgery Centers in states 100+ 37
Surgery partners has been working with GMC on healthcare projects across the country for over a decade. Our continued relationship speaks volumes to our level of trust and confidence we have in their healthcare team and the quality of design in which they produce. Our project types range from complicated phases renovation and addition projects to freestanding surgery centers, medical office buildings, and surgical hospitals. It is without hesitation that I would recommend GMC as a healthcare design partner.”
-
Michael Kump , VP of Facility Development, Surgery Partners

Ambulatory Surgery Centers must be designed to foster efficient workflow, flexibility, future growth, security, ergonomics, safety, and comfort for both patients and staff.





Committed to designing patient-focused environments, GMC collaborates to build better, healthier, and thriving communities.
Creating cost-effective, accessible spaces is essential for efficient care delivery. When these spaces also enhance the patient experience, they become a competitive advantage. The GMC team designs environments that prioritize safety, operational efficiency, and sustainability. Our process ensures spaces that improve patient experiences, provide a secure setting for all, eliminate waste, and lower initial costs while supporting long-term sustainability. By integrating wellness-focused design, we create spaces that foster both care and comfort.


HEALTH FIRST PLANS $230 MILLION EXPANSION OF PALM BAY HOSPITAL, WHICH COULD DOUBLE CAPACITY.

“AS WE HAVE FOR OVER 30 YEARS, HEALTH FIRST IS COMMITTED TO GROWING WITH AND MEETING THE NEEDS OF OUR COMMUNITY. THIS PALM BAY HOSPITAL EXPANSION PROJECT IS ONE OF MANY AMBITIOUS INVESTMENTS WE HAVE LONG PLANNED, AND WE’RE VERY PROUD AND EXCITED TO SEE THESE PLANS QUICKLY BECOMING A REALITY.”
- TERRY FORDE, HEALTH FIRST PRESIDENT AND CEO
‘TRANSFORMATIVE’ EXPANSION PROJECT
“PALM BAY IS A CITY ON THE RISE, AND THIS TRANSFORMATIVE EXPANSION BY HEALTH FIRST REFLECTS THAT MOMENTUM. IT BRINGS MORE JOBS, MORE PHYSICIANS AND MORE PEACE OF MINDS TO OUR RESIDENTS. WE ARE GRATEFUL FOR THIS INVESTMENT IN THE HEALTH AND FUTURE.”
- ROB MEDINA, MAYOR OF PALM BAY



“THIS WORLD-CLASS FACILITY HAS CULMINATED FROM MONTHS OF PLANNING AND DESIGN EFFORTS. IT HAS TRULY BEEN A PLEASURE AND AN HONOR TO WORK WITH THIS TEAM, AND WE LOOK FORWARD TO CONTINUING OUR EFFORTS TO DEVELOP STATE-OF-THE-ART HEALTHCARE TOOLS AND RESOURCES THAT ADVANCE CARE ACROSS THE REGION.”
- JOE GORDY, ADAMS MANAGEMENT SERVICES VP
“THIS EXPANSION PROJECT IS A DIRECT RESULT OF OUR SGMC HEALTH PHYSICIANS’ DESIRE TO PROVIDE AN UNSURPASSED PATIENT EXPERIENCE AND UNEQUALED ACCESS TO ADVANCED CAPABILITIES AND THE HARD WORK AND DEDICATION OF OUR 3,200 HEALTH SYSTEM EMPLOYEES. IT TRULY REFLECTS THE COMMITMENT OF SO MANY THROUGHOUT THE REGION TO ADVANCE HEALTHCARE FOR THE PEOPLE WE SERVE FOR GENERATIONS TO COME.”
- RONALD E. DEAN, SGMC HEALTH PRESIDENT AND CEO




Committed to achieving outstanding patient-focused environments through high-quality design, GMC is driven by the power of building better, happier, healthier, thriving communities.
Through a design-build delivery method with Rabren General Contractors, the project consisted of selective demolition and partial renovation to an existing East Chase business. In partnership with Baptist Health, Southern Orthopaedic Surgeons LLC and Pro Impact Physical Therapy & Sports, the new physical therapy and orthopedic clinic provides diagnostic and treatment services related to physical rehabilitation. Connected with a shared waiting/lobby space, the orthopedic care side of the clinic provides six exam rooms, provider area and tech station alcoves, an x-ray room and cast room with four curtained areas. The physical therapy side of the clinic houses a large open gym, allowing sufficient space for multiple physical therapy sessions utilizing PT exercise equipment, treatment tables and five private treatment rooms adjacent from the open gym.
GMC provided architecture, interior design and civil engineering services.

8,100 square feet $2,635,000
Location: Montgomery, AL
Status: Completed 2021
Contact: Jake Dean Baptist Health System sjdean@baptistfirst.org



87,500 square feet $26,100,000
Location: Auburn, AL Status: Completed 2021
GMC designed the Auburn Medical Pavilion located in Auburn University’s Research and Technology Park. The three-story, 87,500 square-foot building includes a freestanding emergency department (FSED), ambulatory surgery center (ASC) and a women's outpatient imaging center. The project includes the following elements:
First Floor: Freestanding Emergency Department, 37,425 sf
• FSED with 12 patient rooms
• Retail pharmacy to serve the surgery center, FSED patients and the public.
• Outpatient imaging center comprised of a radiography/ fluoroscopy room, x-ray room, two CT rooms and two MRI rooms.
• Space for future growth up to 18 beds.
Second Floor: Ambulatory Surgery Center, 24,145 sf
• ASC with four operating rooms.
• GI Center with four procedure rooms.
• 22 pre/post recovery positions and required support.
Third Floor: Outpatient Imaging Center, 24,145 sf
• Women’s outpatient imaging center with mammography, ultrasound and dexa scan services.
• Physician offices are also included on the third floor.
David Fowler Development Solutions dfowler@dsfocus.com




16,700 square feet $8,000,000
Location: Viera, FL Status: Completed 2024
The Viera community has experienced a significant population increase of 58% from 2010 to 2022, with projections to double by 2050. The Birth Suites at Viera Hospital is a state-of-the-art labor and delivery unit designed to support this rapid growth in the central coastal region and is dedicated to providing advanced obstetrical and gynecological care to residents of Brevard County.
The unit is thoughtfully designed with 14 private suites that accommodate labor, delivery and post-care, ensuring families can stay in one comfortable space throughout their hospital visit. Each suite is equipped with a unique feature—a button that plays a lullaby over the intercom to celebrate the birth of a new baby. The facility also includes two operating rooms specifically for cesarean sections and a nursery.
This transformative interior project brought new life to the Health First Viera Hospital’s fifth floor. GMC led the architectural vision, with Gilbane managing construction as the general contractor. BCER provided mechanical, electrical and plumbing engineering, while Cripe Architects + Engineers contributed served as the medical equipment consultant.
Together, the team delivered a space that not only meets clinical needs but also elevates the patient experience. In recognition of their work, the HF Viera 5th Floor Labor and Delivery Buildout received the 2025 Build Florida Award from AGC for Best Medical Project under $99M.

Contact: Al Forbes Health First albert.forbes@hf.org
The strategic relocation of labor and delivery services from Cape Canaveral Hospital to Viera Hospital, a move of approximately 20 miles, is a response to the increasing demand for healthcare services in the area. Additionally, Health First is constructing a new hospital and medical office complex in Merritt Island to further support regional growth.
This project won AGC's Central Florida Best Medical Project in the "under $99 million" category and ABC Central Florida's Excellence in Construction Merit Award, $5 - $10 million category.


16,750 square feet $5,600,000
Location: Montgomery, AL
Status: Completed 2025
Contact: Jake Dean Baptist Health System sjdean@baptistfirst.org
This project involves the design and buildout of a state-of-the-art Neonatal Intensive Care Unit (NICU) within a 16,747-sf shell space on the 4th floor of Baptist East Hospital in Montgomery, Alabama. The new NICU is designed to provide advanced neonatal care in a modern, patient-centered environment that prioritizes both clinical efficiency and family support.
The NICU will feature 18 private patient rooms, ensuring a quiet and controlled environment that promotes healing and development. Of these, six rooms are designed to accommodate overnight stays for families, reinforcing Baptist East’s commitment to family-integrated care. The remaining 12 infant positions are organized in clusters, maximizing visibility for both staff and families, fostering efficient monitoring and seamless communication among the care team. In total, the unit will house 30 infant beds, providing a balanced approach between privacy and accessibility for neonatal care.
This NICU buildout at Baptist East Hospital represents a significant investment in neonatal healthcare, providing an environment where technology, compassionate care, and innovative design come together to support infants and their families during critical stages of development. Through private rooms, clustered infant care areas, natural light, and clear wayfinding, the new NICU ensures an optimal balance between clinical efficiency and family support, reinforcing Baptist East Hospital’s mission to deliver exceptional neonatal care.



22,400 square feet
$5,600,000
Location: Franklin, TN
Status: Completed 2022
Sleek metal panels, banded brick facades and open spaces inform the design of this two-story medical office building. The first floor combines a state-of-the-art sports training facility with all means of physical therapy. Turfed areas inside and out provide for a full regimen of exercise-centric activities. Specialized spaces provide for both public and private physical therapy as well as massage therapy. Well appointed locker rooms, showers and changing facilities are also provided. Management is provided with both open and private offices, a separate AV capable meeting room and a spacious break room.
The second floor houses an advanced sports medicine and orthopedics office with twenty exam rooms. An MRI, X-ray and casting rooms are provided for the treatment of all types of musculoskeletal issues in house. Large, open nurses’ stations, offices, breakroom and meeting rooms are included to provide staff with all the facilities required to perform their duties capably.
The project was a fast-tracked effort, designed with the contractor’s input for effective use of both time and resources. GMC provided full architectural services and coordinated mechanical, electrical, plumbing and fire protection through our contract. The civil design was provided through the developer as part of a separate contract. The resulting building provides an elegant design solution to house a unique program, allowing the owner to provide their services efficiently and effectively.
Contact: Ralph Knauss SouthStar rknauss@southstarco.com




900 square feet
$1,055,000
This project consists of the replacement of the existing Philips Biplane equipment with a new Siemens Biplane Machine at Kennestone Hospital in Marietta, GA. In addition to the replacement equipment, this project consists of new lead-lined entry doors, expansion of the lead-lined window for the control room, relocation of medical gases, new finishes throughout and other related mechanical, electrical and plumbing items. This project is currently proceeding through the design process, which was completed in July 2024. This project is began construction in late 2024 and was completed at the end of 2024.
Location: Marietta, GA Status: Completed 2024