6 minute read
Bringing the Hospital ER into the Field
Signs of Life and Changes
John Hancock, Editor
Vital signs are a means for a clinician not only to discover a patient’s condition but also how it develops
VITAL SIGNS might be described as a catch-all term for a range of indicators as to whether the body is performing normally or not and/or is in danger or not, and how a condition or treatment is progressing.
What Are Vital Signs? Those who are familiar with hospitals will also be familiar with the charts, often at the end of the bed, recording a patient’s vital signs: but vital signs have a much broader application than only on end-of-bed charts. Any clinician will, if possible, ask the patient how they feel but, as well as the possibility that they might not be able to respond through injury or concussion, there is also the consideration that what different patients feel with identical injuries or conditions will vary according to their pain threshold or nature or other outside factors. Clinicians need something constant against which to measure a patient’s condition: UK Essays 1 explains that, “The measurement and recording of the vital signs is the first step in the process of physically examining a patient. This step involves collecting objective data.” That word ‘objective’ is critical and is supported by the fact that there are established parameters for vital sign measurements in healthy adults. The main vital signs used and their healthy levels or measurements are listed in the UK Essays article as…
VITAL SIGN HEALTHY RANGE Blood pressure (BP) 120/80 mmHg Pulse or heart rate (HR) 60-100 beats per minute Temperature (T°) 36.5°C to 37.5° Celsius Respiratory rate (RR) 10 to 16 breaths per minute Blood oxygen saturation (SpO2) 98%-100%
Monitoring Vital Signs As we’ve already noted, there other factors to take into account. The Milton S. Hershey Medical Center 2 explains that, “Some medical problems can cause changes in one or more vital signs.” and that medication and age can also have their effects. But, generally, readings that fall outside of these parameters might indicate that something is wrong and changes between periodic readings might indicate a rate of change in the patient’s condition. The Lippincott Nursing Center 3 recommends that, when dealing with patients in an Accident and Emergency department, vital signs should be monitored, “Every 5 to 15 minutes as needed based on clinical presentation and no less frequently than every hour for the first 4 hours, then every 2 hours if clinically stable.” The article continues to outline changing frequencies as the patient progresses.
Vital signs are an important component in patient care. They determine which treatment protocols to follow, provide critical information needed to make life-saving decisions, and confirm feedback on treatments performed. Accurate, documented vital signs are a very important part of a managed treatment program. But they also can save lives. The Telegraph 4 reported in May 2019 that, “Six thousand patients are dying every year because hospital staff are not properly monitoring vital signs.” The article continues to highlight The Royal College of Physicians proposal of a National Early Warning Score to standardize the monitoring of and reading of vital signs (temperature, pulse, blood pressure, breathing rate, level of consciousness, and oxygen saturation) across all UK healthcare facilities. That last sign, oxygen saturation, is a measure of how much oxygen is in the blood and has only recently been adopted by hospitals. A low score can indicate heart and lung problems.
While vital signs are often used in cases where rapid and unpredictable change is a feature of the patient’s condition – trauma, rapid onset of infection, during transport to hospital – they are also very useful in more controlled clinical and surgical situations such as on the general ward, in the critical or intensive care ward and during anesthesia. Monitoring vital signs is a key factor in determining the development and outcome of most clinical conditions and procedures. Perhaps a last word on this can come from the Patient Safety Network (PSN) 5 , “… vital sign monitoring leads to early identification of patient deterioration and rapid response activation.”


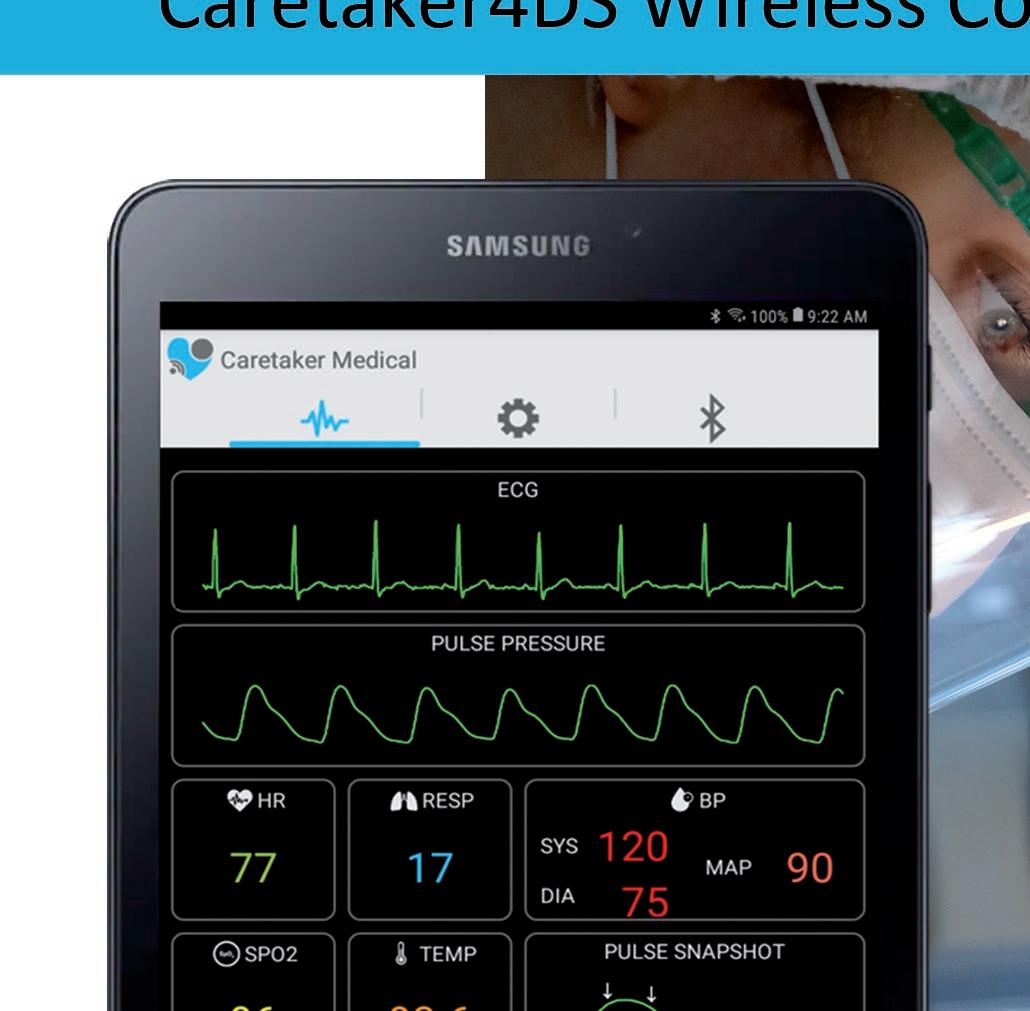
Focus On Your Patient Not Your Monitoring Equipment Caretaker4DS Wireless Continuous NIBP and Viatls Signs Monitor Caretaker 4 Wireless Continuous NIBP and Vitals Signs Monitor
The Value of Vital Signs A PLoS One article carried by NCBI 6 , tells us that, “… surprisingly few attempts have been made to quantify [vitals signs’] clinical performance [although] numerous studies have reported that changes in vital signs occur several hours prior to a serious adverse event.” The article adds, “Even though it is accurately predicted by vital sign changes, clinical deterioration often goes unnoticed, or is not detected until it is too late to treat. This is mainly caused by inadequate recording of vital signs or as a result of an inappropriate response to abnormal values. Among nurses and doctors there is insufficient knowledge and appreciation of vital sign changes and their implications for patient care.”
In the UK, the Royal College of Emergency Medicine 7 has recognized this challenge and, in 2010, published ‘The Vital Signs Standards’. In a 2018/19 update, the RCEM issued an information pack to help clinicians understand what could be learned from vital signs. As a first step, the pack confirmed that, in 2010/11, “[while] Pulse (97%), BP (97%), O2 saturation (96%) and respiratory rate (92%) were well recorded. Temperature (88%) and GCS or AVPU (77%) were less well recorded… [and] The percentage of audited notes where abnormal vital signs were observed varied greatly between EDs [Emergency Departments] (from 8% to 98%) which suggests considerable variation in patient acuity.”
An excellent source of information as to what clinicians can do with vital signs information is provided by Nursing Times, ‘How to measure and record vital signs to ensure detection of deteriorating patients’ 8 which focuses on patient deterioration and offers explanatory notes on each of the main vital signs, including what information can be gleaned from them and why regular monitoring can help a clinician detect even minor changes that, cumulatively, might point to a potentially more serious outcome. Further notes on ‘Assessing and Responding to Changes/ Abnormalities in Vital Signs’ are available from Registered Nursing 9 . What is clear from any source is that regular and systematic vital signs monitoring plus application of the results is a critical component in the receiving, assessing and continual monitoring of a patient’s condition and progress.

FDA and CE Certifi ed
● Integrated Cloud Portal
● LCD User Display
● Antibacterial materials
● Remote Monitoring
● OEM Integration
● Vitals Audible Alarms
● Vital Signs Platform