5 minute read
Wireless and an Evolving Healthcare Environment
John Hancock, Editor
A monitoring system that matches patient, clinician and healthcare priorities
WE’VE LOOKED at the importance not just of monitoring but also of how it is carried out; and we’ve looked at some of the pressures challenging healthcare systems and, broadly, what sort of changes might help to tackle those challenges. Those challenges are summed up by The Health Foundation 31 , “With the older population growing rapidly, along with the numbers suffering chronic health problems, and a growing pay and drugs bill, demands on the health service will only continue to grow. Just to keep the NHS providing the level of service it does today will require us to increase spending by an average 3.3% a year for the next 15 years [which] would take health spending from 7.3% of national income today to 8.9% of national income by 2033/34.” In this article, we’ll look at one developments and how it might be useful in helping to address the challenges outlined above.
Clinical and Best Practice Guidelines The NICE (National Institute for Health and Care Excellence) Guidance, ‘Improving the detection and response to patient deterioration’ 32 , “requires that all adult patients in hospital have (i) a clear written monitoring plan specifying which vital signs should be recorded (and at what frequency), (ii) their severity of illness measured using a physiological early warning score (EWS) and (iii) a graded response strategy.” As long ago as 2012, a group of senior clinicians in the NHS 33 called for the standardization of monitoring vital signs across the system which led to the establishment of the National Early Warning Score (NEWS). NHS England 34 recorded that implementation of NEWS had, “significantly improved patient safety and outcomes, improved staff experience, and streamlined and standardized handovers which has increased time spent caring for patients.”
Wireless Vital Signs Monitoring One area where the NHS has shown interest in order to be able to match those clinical best practice guidelines has been the use of wireless vital signs monitoring. In 2015, The Telegraph reported the, ‘End of the thermometer as first NHS hospital trials wireless monitoring.’ 35 The article opened with, “The era of a nurse diligently making the rounds with a thermometer may be coming to an end after a British hospital began trialing new technology which monitors vital signs remotely.” and continued to set out the benefits of such a system. Those benefits include the frequency with which a wireless system can ‘report’ to a nurse, thus minimizing the risk of a patient’s deterioration between vital signs monitoring events going unnoticed until too much time has passed. It can also free the nurse to spend more time on treatment with less time needed to conduct vital signs monitoring than would have been the case with traditional methods.
Remote and wireless vital signs monitoring can also allow some patients to be discharged earlier with monitoring able to continue in their home environment. That is a good outcome for the patient and for the budget at the healthcare facility. As such possibilities for wireless monitoring of vital signs become possible, the requirements for viable and cost-effective solutions are evolving to take advantage of improving capabilities.
For instance, along with wireless monitoring have come wearable sensors that can record vital signs information without the intrusive nature of traditional equipment and methods. Although not exclusively so, such technology is particularly applicable when dealing with older patients whose vital signs might well need to be monitored but whose health does not otherwise justify them being in a hospital bed. ‘Sensors’ 36 on NCBI explains, “Such systems equipped with non-invasive and unobtrusive wearable sensors can be viable diagnostic tools to the healthcare personnel for monitoring important physiological signs and activities of the patients in real-time…” And, of course, in all this, we mustn’t forget the patient. ResearchGate’s ‘Review of Vital Signs Monitoring Systems – Patient’s Acceptability Issues and Challenges’ 37 concludes, “… that despite some limitations commented by patients


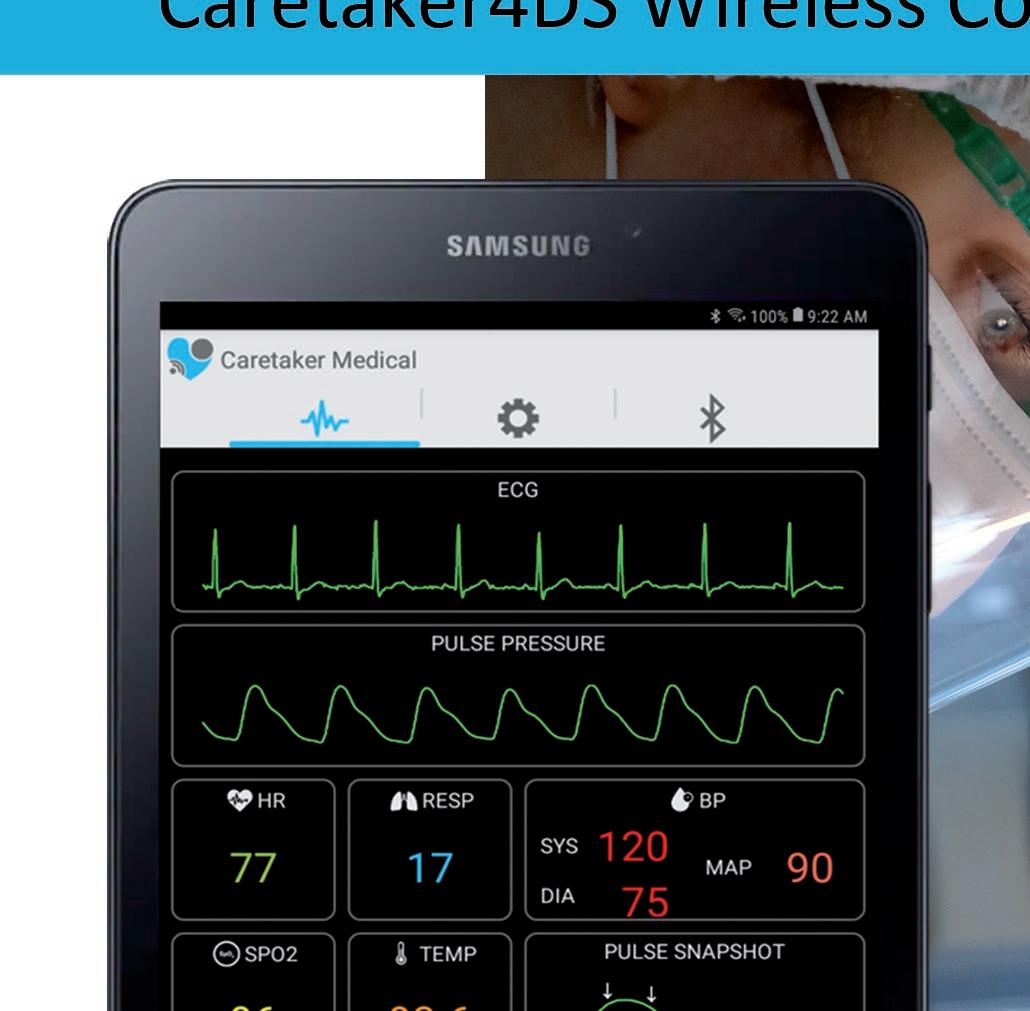
Focus On Your Patient Not Your Monitoring Equipment Caretaker4DS Wireless Continuous NIBP and Viatls Signs Monitor Caretaker 4 Wireless Continuous NIBP and Vitals Signs Monitor
and clinicians, these systems should be more compact and simple to operate and they should be available to healthcare professionals with minimum interruption to normal daily life activities (ADLs).”
Improving Patient Comfort, Safety and Outcomes Hopefully, by now it is clear what the advantages are for using wireless devices to deliver remote and continuous vital signs monitoring. Changes in the patient’s condition can be better responded to than if the monitoring is at intervals which, in turn, will improve patient care and safety. This is a critical advantage in those situations where speed of response will have literally life-ordeath consequences: patients whose condition could be subject to rapid change such as with trauma and for those whose condition might deteriorate rapidly and (with some conditions) catastrophically. Clinicians don’t have to invest time in monitoring and yet have the benefit of better monitoring results to support their professional efforts; hospitals will not only be better informed to improve care of any patients but might also be able to discharge patients earlier. All of this contributes to reduced costs for financially stretched healthcare systems. And one thing that we have not covered but will be true is that, for patients and their families, a single, digital wireless device will be a lot less alarming than the traditional array of monitoring equipment.
Events and developments are progressing rapidly in this field with devices such as the CareTaker ® finger-cuff wireless patient monitoring platform for continuous non-invasive blood pressure and vital signs. These types of devices can measure beat-by-beat blood pressure and heart rate in a non-invasive wearable form-factor. The best include features that enable clinicians to have a continuous and comprehensive view of patient’s physiological condition.
It also enables a clinician to manage several patients but with better levels of real-time information for each patient than if they had to rely on periodic vital signs monitoring. Let’s allow the last word on monitoring to Professor Sir Bruce Keogh, Medical Director of the NHS, “Catching deterioration in the early stages can mean huge improvements in patient safety and outcomes. This score offers an opportunity for the NHS to standardize how it monitors a patient’s condition across different healthcare settings.”

FDA and CE Certifi ed
● Integrated Cloud Portal
● LCD User Display
● Antibacterial materials
● Remote Monitoring
● OEM Integration
● Vitals Audible Alarms
● Vital Signs Platform