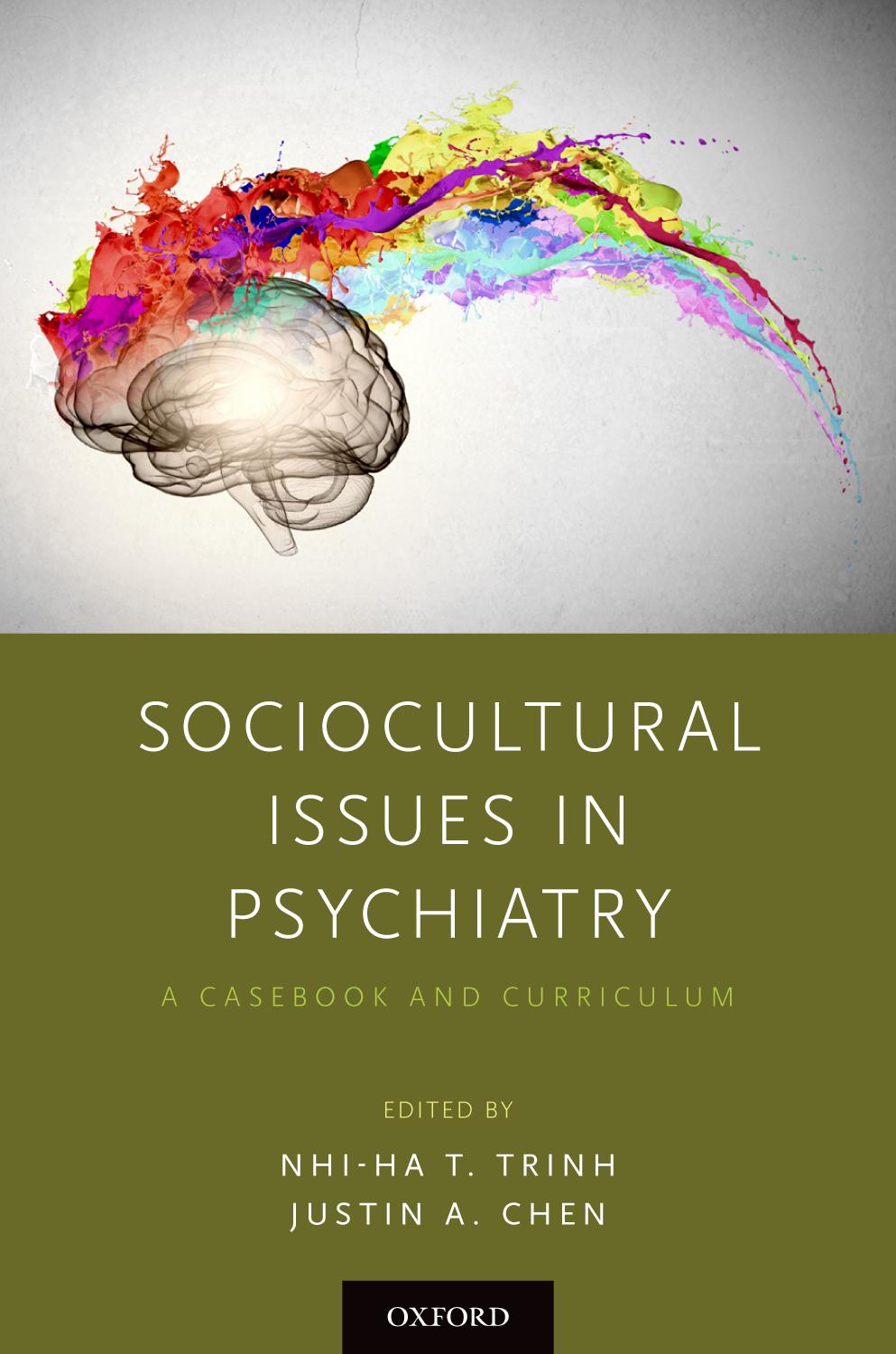
Sociocultural Issues in Psychiatry
A Casebook and Curriculum
EDITED BY NHI- HA T. TRINH AND JUSTIN A. CHEN
Oxford University Press is a department of the University of Oxford. It furthers the University’s objective of excellence in research, scholarship, and education by publishing worldwide. Oxford is a registered trade mark of Oxford University Press in the UK and certain other countries.
Published in the United States of America by Oxford University Press 198 Madison Avenue, New York, NY 10016, United States of America.
© Oxford University Press 2019
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Oxford University Press, or as expressly permitted by law, by license, or under terms agreed with the appropriate reproduction rights organization. Inquiries concerning reproduction outside the scope of the above should be sent to the Rights Department, Oxford University Press, at the address above.
You must not circulate this work in any other form and you must impose this same condition on any acquirer.
Library of Congress Cataloging-in-Publication Data
Names: Trinh, Nhi-Ha, editor. | Chen, Justin A., editor.
Title: Sociocultural issues in psychiatry : a casebook and curriculum / [edited by] Nhi-Ha T. Trinh, Justin A. Chen.
Description: Oxford ; New York : Oxford University Press, [2019] | Includes bibliographical references and index.
Identifiers: LCCN 2018028701 | ISBN 9780190849986 (pbk. : alk. paper)
Subjects: | MESH: Community Psychiatry | Ethnopsychology |
Sociological Factors | Models, Psychological | Professional-Patient Relations
Classification: LCC RC455 | NLM WM 31 | DDC 616.89—dc23 LC record available at https://lccn.loc.gov/2018028701
This material is not intended to be, and should not be considered, a substitute for medical or other professional advice. Treatment for the conditions described in this material is highly dependent on the individual circumstances. And, while this material is designed to offer accurate information with respect to the subject matter covered and to be current as of the time it was written, research and knowledge about medical and health issues is constantly evolving and dose schedules for medications are being revised continually, with new side effects recognized and accounted for regularly. Readers must therefore always check the product information and clinical procedures with the most up-to-date published product information and data sheets provided by the manufacturers and the most recent codes of conduct and safety regulation. The publisher and the authors make no representations or warranties to readers, express or implied, as to the accuracy or completeness of this material. Without limiting the foregoing, the publisher and the authors make no representations or warranties as to the accuracy or efficacy of the drug dosages mentioned in the material. The authors and the publisher do not accept, and expressly disclaim, any responsibility for any liability, loss or risk that may be claimed or incurred as a consequence of the use and/or application of any of the contents of this material.
9 8 7 6 5 4 3 2 1
Printed by WebCom, Inc., Canada
CONTENTS
Foreword vii
Contributors ix
1. Introduction to Sociocultural Psychiatry 1
Nhi-Ha T. Trinh, Chun-Yi Joey Cheung, and Justin A. Chen
2. Culture as a Multidimensional Construct 13
Anne Emmerich and Leslie Tarver
3. Culture in the DSM-5 37
Nhi-Ha T. Trinh, Maya Son, and Justin A. Chen
4. Global Psychiatric Epidemiology 51
Maria C. Prom and Alexander C. Tsai
5. Social Determinants of Psychiatric Illness 69
Kristen Nishimi, Esther Howe, and Erin C. Dunn
6. Psychiatry and Its Checkered Past: Perspectives on Current Practice 87
Judith Puckett and David Shumway Jones
7. Minority Stress Theory and Internalized Prejudice: Links to Clinical Psychiatric Practice 103
Christine Crawford, Lisa Sangermano, and Nhi-Ha T. Trinh
8. Identifying and Working with Diverse Explanatory Models of Mental Illness 127
Tony B. Benning and Justin A. Chen
9. Religion and Spirituality in Psychiatric Care: An Experiential Seminar Model
Addressing Barriers to Discussing Religion and Spirituality 145
Siobhan M. O’Neill, Jiaying Ding, and Gowri G. Aragam
10. Gender and Sexuality: Shame and Safety in the Psychiatric Encounter 165
Andrew Cruz, Julianne Torrence, and Christopher M. Palmer
11. Implicit Bias in Mental Health Care 185
Andrea S. Heberlein, Justin A. Chen, and Nhi-Ha T. Trinh
12. Responding to Patients’ Provider Preferences 203
Kimberly L. Reynolds, Kira Knight Rodriguez, Loucresie Rupert, and Michaela Owusu
13. Navigating Cultural Challenges in Patient–Clinician Dyads 227
Josepha A. Immanuel, Chun-Yi Joey Cheung, and Nhi-Ha T. Trinh
14. Teaching Sociocultural Psychiatry Throughout the Lifespan 245
Priya Sehgal, Maya Nauphal, and Justin A. Chen
About the Editors 261
Index 263
FOREWORD
The American Psychiatric Association (APA) has four strategic priorities: advancing psychiatry, supporting research, educating about mental disorders, and supporting and increasing diversity. While diversity stands as a separate pillar, it is also a common thread across all the priorities, especially education.
Since its inception in 1974, APA’s Division of Diversity and Health Equity has primarily focused on developing and educating a culturally competent workforce to meet the needs of minority and underserved populations. As early as 1969, APA’s official policies included the “Position Statement on the Delineation of Transcultural Psychiatry as a Specialized Field of Study,” and in 2013, APA’s Board of Trustees reaffirmed the 1969 policy regarding the importance of cultural teaching with its “Position Statement on Cultural Psychiatry as a Specific Field of Study Relevant to the Assessment and Care of All Patients.” Through many policies, strategies, and bylaws, the world’s largest psychiatric organization executes its mission of providing cultural education to its 38,000 members.
In their textbook, Drs. Nhi-Ha Trinh and Justin Chen spotlight the importance and challenges of teaching cultural and social issues in medicine today. As the U.S. population continues to become more culturally diverse, “cultural psychiatry” will soon be synonymous with “U.S. psychiatry.” Additionally, these ethnographic changes add complexity and numbers to people at the intersection of minority statuses or who have multiple social identities.
This textbook demonstrates that mental health providers can no longer understand culture as a unidimensional construct. Similarly, the latest Diagnostic and Statistical Manual (DSM) deepens our understanding of cultural psychiatry. DSM5 provides greater utility than its predecessors by introducing a focus on cultural concepts of distress.
Today’s generation of educators and mental health providers are required to be lifelong learners. They must commit to understanding many evolving areas relevant to cultural psychiatry, including social determinants of mental health, structural competency, cultural humility, minority stress theory, implicit bias, religion and sexuality, and the impact of patient–physician concordance. Sociocultural Issues in Psychiatry is timely for the well-prepared psychiatrist of today who is, at the same time, both culturally competent and curious.
Ranna Parekh, MD, MPH Deputy Medical Director Director, Diversity and Health Equity
American Psychiatric Association
Gowri G. Aragam, MD
Resident, Adult Psychiatry
Adult Psychiatry Residency Training Program
Massachusetts General Hospital/ McLean Hospital (MGH/McLean)
Boston, Massachusetts
Tony B. Benning, MBChB, MSC, PGDIP, MRCPsych (UK), FRCPC, PhD
Clinical Instructor in Psychiatry
Department of Medicine, University of British Columbia
Consultant Psychiatrist
Maple Ridge Mental Health Center and Ridge Meadows Hospital
Vancouver, British Columbia, Canada
Justin A. Chen, MD, MPH
Assistant Professor of Psychiatry
Harvard Medical School
Medical Director, Ambulatory Psychiatry Services
Massachusetts General Hospital
Boston, Massachusetts
Chun-Yi Joey Cheung, BS
Research Coordinator
Depression Clinical and Research Program
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
CONTRIBUTORS
Christine Crawford, MD, MPH
Fellow, Child and Adolescent Psychiatry
Division of Child and Adolescent Psychiatry
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Andrew Cruz, MD
Resident, Adult Psychiatry
Adult Psychiatry Residency Training Program
Massachusetts General Hospital/ McLean Hospital (MGH/McLean) Boston, Massachusetts
Jiaying Ding, MDiv
Graduate Student
Harvard Divinity School
Cambridge, Massachusetts
Erin C. Dunn, ScD, MPH
Assistant Professor of Psychiatry
Harvard Medical School
Psychiatric and Neurodevelopmental Genetics Unit
Center for Genomic Medicine
Massachusetts General Hospital Boston, Massachusetts
Anne Emmerich, MD
Instructor of Psychiatry
Harvard Medical School
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Andrea S. Heberlein, PhD
Senior Lecturer
Boston College
Chestnut Hill, Massachusetts
Esther Howe, BA Program Coordinator
Depression Clinical and Research Program
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Josepha A. Immanuel, MD Clinical Faculty
Baylor College of Medicine
Child, Adolescent and Adult Psychiatrist
Legacy Community Health
Houston, Texas
David Shumway Jones, MD, PhD
A. Bernard Ackerman Professor of the Culture of Medicine
Harvard University Cambridge, Massachusetts
Maya Nauphal, BA Research Coordinator
Depression Clinical and Research Program
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Kristen Nishimi, MPH PhD Candidate
Department of Social and Behavioral Sciences
Harvard T.H. Chan School of Public Health
Psychiatric and Neurodevelopmental Genetics Unit
Center for Genomic Medicine
Massachusetts General Hospital Boston, Massachusetts
Siobhan M. O’Neill, MD Assistant Professor of Psychiatry (Part-Time)
Department of Psychiatry
Massachusetts General Hospital Harvard Medical School Boston, Massachusetts
Michaela Owusu, MD, MSc Fellow, Child and Adolescent Psychiatry Division of Child and Adolescent Psychiatry
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Christopher M. Palmer, MD
Assistant Professor of Psychiatry
Harvard Medical School
Director, Department of Postgraduate and Continuing Education McLean Hospital Belmont, Massachusetts
Ranna Parekh, MD, MPH Deputy Medical Director Director, Diversity and Health Equity
American Psychiatric Association Washington, DC
Maria C. Prom, MD
Resident, Adult Psychiatry
Adult Psychiatry Residency Training Program
Massachusetts General Hospital/ McLean Hospital (MGH/McLean) Boston, Massachusetts
Judith Puckett, MD
Resident, Adult Psychiatry
Adult Psychiatry Residency Training Program
Massachusetts General Hospital/ McLean Hospital (MGH/McLean) Boston, Massachusetts
Contributors
Kimberly L. Reynolds, MD
Assistant Professor of Clinical Pediatrics
University of Miami Miller School of Medicine
Pediatric Hospitalist
Holtz Children’s Hospital at Jackson Memorial Medical Center
Miami, Florida
Kira Knight Rodriguez, MD, MS
Association of University Centers on Disabilities (AUCD) Diversity Fellow
Mailman Center for Child Development
University of Miami Miller School of Medicine
Miami, Florida
Loucresie Rupert, MD
Medical Director of Psychiatry
Winona Health
Adult, Child and Adolescent Psychiatrist
Insightful Consultant, LLC
Winona, Minnesota
Lisa Sangermano, BA
Research Coordinator
Depression Clinical and Research Program
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Priya Sehgal, MD, MA
Child and Adolescent Psychiatry Fellow
Cambridge Health Alliance/Harvard Medical School
Cambridge, Massachusetts
Maya Son, MD
Resident, Adult Psychiatry
Adult Psychiatry Residency Training Program
Massachusetts General Hospital/ McLean Hospital (MGH/McLean)
Boston, Massachusetts
Leslie Tarver, MD, MPH
Resident, Adult Psychiatry
Adult Psychiatry Residency Training Program
Massachusetts General Hospital/ McLean Hospital (MGH/McLean) Boston, Massachusetts
Julianne Torrence, LICSW Director
Department of Performance and Quality Improvement
Connecticut Junior Republic Litchfield, Connecticut
Nhi-Ha T. Trinh, MD, MPH
Assistant Professor of Psychiatry
Harvard Medical School
Director, Psychiatry Center for Diversity
Director of Multicultural Studies and of Clinical Services
Depression Clinical and Research Program
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Alexander C. Tsai, MD, PhD
Associate Professor of Psychiatry
Harvard Medical School
Department of Psychiatry
Massachusetts General Hospital Boston, Massachusetts
Introduction to Sociocultural Psychiatry
NHI- HA T. TRINH, CHUN-YI JOEY CHEUNG, AND JUSTIN A. CHEN ■
Psychiatry must learn from anthropology that culture does considerably more than shape illness as an experience, it shapes the very way we conceive of illness.
Arthur Kleinman1
From its founding, the United States has been a country composed of people from diverse racial, ethnic, and cultural backgrounds. Furthermore, demographic shifts in the United States have recently accelerated; in the past 20 years, racial and ethnic minorities have increased from 19% to 27% of the U.S. population.2–4 According to the U.S. Census Bureau, this growth is projected to continue; by 2044 the United States will become a “majority minority” nation, with the largest growth occurring among Hispanic and Asian populations.2
Race, ethnicity, and culture may all exert a tremendous impact on medical diagnosis, treatment, and outcomes. This is especially true in psychiatry, given the prominent role that culture plays in patients’ interpretation and management of symptoms that fall within the affective, behavioral, and cognitive domains. Although an in-depth understanding of every culture is impossible, familiarity with some basic principles will help minimize cultural clashes and reduce the risk of compromised medical care.
KEY DEFINITIONS
Race is defined as a category of humankind that shares certain distinctive physical traits,5 such as skin color, facial features, and stature. Most people think of race in biological terms; for more than 300 years, or since the era of white European
colonialization of populations of color in the world, race has indeed served as the “premier source of human identity.”6 Anthropologists, sociologists, and many biologists now question the value of these categories and thus the value of race as a helpful biological concept.7,8 Indeed, DNA studies have debunked race as a biological construct and more of a social construct, as less than 0.1% of all our DNA accounts for physical differences among people associated with racial differences.8 However, because society has valued these physical differences, the classification of individuals based on physical characteristics has led societies to treat them differently—and unequally.
In contrast, ethnicity refers to a particular ethnic affiliation or group,9 with the term ethnic relating to large groups of people classed according to common racial, national, tribal, religious, linguistic, or cultural origin or background ethnic minorities.10 Thus, ethnic groups also are a social construct and have shared social, cultural, and historical experiences stemming from common national or regional backgrounds.
The term culture has multiple meanings. Culture can describe the beliefs, customs, and arts, of a particular society, group, place, or time; culture can be used as a synonym for a particular society that has its own beliefs, ways of life, and art, for example ; finally, culture can refer to a specific way of thinking, behaving, or working that exists in a place or organization.11 Clearly certain ethnic or racial groups can have their own cultures, but the association is not always one to one; in addition, groups or organizations made up of multiple races or ethnicities can create their own culture, such as, for example, “American culture” or the culture of medicine.
Culture can thus be thought of as the collected body of beliefs, customs, and behaviors that a group of people acquire socially and transmit from one generation to another through symbols and shared meanings. It provides the tools by which members of a given society adapt to their physical environment, to their social environment, and to one another. It organizes groups of ready-made solutions to the problems and challenges that people often face. There are two levels of culture: physical and ideological.
Physical culture—including art, literature, architecture, tools, machines, food, clothing, and means of transportation—can be directly observed through the five senses and/or through items collected in a museum or recorded on film. The physical level of culture yields more easily to change and to adaptation than does the ideological level.
Ideological culture refers to aspects of culture that must be observed indirectly, usually through behaviors, including beliefs and values; reasons for holding some things sacred and others ordinary; the events and characteristics of which a society is proud or ashamed; and the sentiments that underlie patriotism or chauvinism. Religion, philosophy, psychology, literature, and the meanings that people give to symbols are all part of the ideological aspect of culture. Without some understanding of the ideological aspect of culture, it is difficult to understand the meaning of a group purely at the physical level.
One level above culture, sociocultural encompasses the combination of the cultural with the social, and hence a broader focus not just on race, ethnicity, or even a cultural group, but all of society and its structures, including, for instance, the institution of medicine, or the historical and political systems of the United States.
In this sociocultural context, a minority group is a part of a population differing from others in some characteristics and often subjected to different treatment.12 Minority groups are differentiated from the social majority, defined as those who hold major positions of social power in a society. The differentiation can be based on one or more observable human characteristics, including ethnicity, race, religion, disability, gender, wealth, health, or sexual orientation, and may be enforced by law. The term is applied to various situations and civilizations within history despite its association with a numerical, statistical minority.13
SOCIOCULTURAL CHALLENGES IN CLINICAL PRACTICE
Understanding a patient’s sociocultural background will aid in the delivery of highquality care. However, a little knowledge can also be a dangerous thing. Variability among individuals is inevitable; a particular patient may not fit into a clinician’s preconceived notion of his or her culture. Thus, the clinician must probe for clues regarding the patient’s background while remaining flexible enough to recognize when a patient’s behaviors and clinical presentation do not necessarily match what is expected. The clinician should be aware of his or her own feelings, biases, and preconceptions about other cultures. In addition, clinicians must assess the social context, including the impact of the hospital environment, the attitudes of the medical and ancillary care teams, and the patient’s experience within the health care system. Mistrust of the health care system is common and may influence a patient’s behavior, level of cooperation, and adherence to treatment.
Furthermore, disparities in health care delivery have been well documented and are influenced by factors such as gender, race, ethnicity, and culture. The 2001 Surgeon General’s report “Culture, Race, and Ethnicity” documented the existence of striking disparities for racial, ethnic, and other minorities as compared to white populations in mental health care. In sum, the report found that compared to whites, racial and ethnic minorities have reduced access to mental health services, are less likely to receive needed care, and receive lesser-quality care—if they were to receive mental health care at all. The supplement to the Surgeon General’s report suggested multiple reasons for these disparities on various levels—structural, financial, and individual. Rather than operating independently, these factors may intersect, resulting in minorities’ failing to receive adequate screening and care for mental health diagnoses and, therefore, presenting for treatment only at later or more severe stages. The Federal Collaborative for Health Disparities Research listed mental health disparities as one of its top research priorities in 2006, underscoring the gravity of the problem.14
NEED FOR SOCIOCULTURAL EDUCATION
To meet the needs of the growing minority and underserved populations, clinicians must be educated and well versed in the skills and strategies needed to provide culturally respectful and relevant care for their patients. While the demographic profile of patients is changing rapidly, the demographic profile of mental health professionals is changing more slowly.15 For instance, a 2013 survey found that a
majority of psychologists were white and female (83% and 68.3%). Between 2005 and 2013, the percentage of racial and ethnic minority groups within the psychology workforce grew from 8.9% to 16.4%; this is significantly behind the 39.6% of the overall workforce from racial/ethnic minority backgrounds, and the 25.8% in the general doctoral/professional workforce.16 Despite these advances, rates of Asian American, Black, and Latino American psychologists have continued to remain low (4.3%, 5.3%, and 5% respectively in 2016).17 Similarly, in 2013, the racial and ethnic breakdown of U.S. physicians in practice was non-Hispanic white (43.0%), Hispanic or Latino (4.0%), Black or African American (3.7%), Asian (10.9%), and Native American/Alaskan Native (0.3%).18 For U.S.-trained psychiatrists, the numbers of minorities are even lower than those in the overall U.S. physician workforce.19,20 For social workers, the situation is slightly less dire; in 2015, 67.3% of social workers were white, 23.3% were Black, and 5.3% were Asian Americans.21
In a survey of 689 psychologists, the majority of whom were white, more than 80% reported discussing racial or ethnic differences in at least one cross-racial therapeutic encounter in the previous two years.22 Yet they also reported that racial or ethnic differences were discussed in less than half of all cross-racial clinical sessions, a finding that is particularly surprising because racial and ethnic identity is central to an individual’s experience in the world, similar to sexual or gender identity. Understanding a racial or ethnic minority individual’s cultural identity may be crucial to developing a therapeutic alliance and treatment plan. Indeed, with the demographic composition of the United States rapidly evolving, ongoing efforts should be made to increase both the diversity of the physician workforce and the capacity and skill of providers to deliver quality health care for diverse patient populations. Training focused on fostering an attitude of cultural respect will help equip providers for this challenge. Efforts to create and recruit a diverse psychiatric workforce should proceed in tandem with efforts to cultivate a culturally respectful psychiatric workforce.20
FROM CULTURAL COMPETENCE TO CULTURAL HUMILITY
Because of this, the term “cultural competence” has become au courant, as a clinical solution to bridge the disparities in access and treatment for depression for racial and ethnic minorities specifically, given how central racial and ethnic minority status may inform one’s cultural identity. And yet individuals can belong to several cultural groups based on their racial, ethnic, religious, or family backgrounds.11 Thus cultural competency can be defined as “a set of congruent behaviors, attitudes, and policies that come together in a system, agency or among professionals and enable that system, agency or those professions to work effectively in cross-cultural situations.”23
Cultural competency encompasses systems as well as individual therapeutic encounters. Betancourt and colleagues24 define three levels for cultural competence interventions: organizational (leadership/workforce), structural (processes of care), and clinical (provider–patient encounter). They note that at the clinical level, training has often focused on a categorical approach that involves ascribing attitudes, values, beliefs, and behaviors to broad cultural groups, which may lead to stereotyping. Combining knowledge-based training with training in cross-cultural
communication allows for a more nuanced understanding of how cultural content may or may not be relevant to individuals. There is some evidence that cultural competence training can lead to increased knowledge and awareness among providers, but it is unclear at this point whether training also improves patient outcomes, and more research is needed in this area.
Cultural competence is not uniformly accepted as a core competency in therapy. Sue and colleagues25 summarize debates on the utility of cultural competence through a series of questions. These include whether cultural competence stereotypes minorities, discriminates against other types of diverse identities such as social class or sexual orientation, overemphasizes external factors such as discrimination at the expense of intrapsychic factors, and creates pressure on therapists to ascribe to cultural competency in order to be viewed as nonracist. The authors respond to these debates by noting that the debates tend to oversimplify the concept of cultural competence and ignore a more nuanced perspective, which includes a focus on multiple intersecting identities and an acknowledgment of intrapersonal, interpersonal, and societal influences on the lives of our patients. Ultimately, the authors argue that cultural competence is necessary as a response to a historical context that has resulted in systematic bias against the inclusion of culturally specific experiences in therapy.
At the same time, however, research has been limited on how such interventions improve patient outcomes in racial and ethnic minority groups. In one review article, which aimed to evaluate the effect of cultural competence trainings on patient, professional, and organizational outcomes, researchers found no evidence of improved treatment outcomes or evaluations of care based on cultural competence interventions.26 In addition, they found that none of the studies evaluated potential adverse events of such interventions. Therefore, while there have been initiatives to address these issues of clinician bias and discriminatory behavior within the health care system through education, the efficacy of these interventions is yet to be determined. Future research must focus on how to better design and evaluate cultural competence interventions.
Qureshi and colleagues27 note that the term “cultural competence” itself may obscure important distinctions in the types of barriers faced by racial, ethnic, and other minority patients. A focus on culture may pertain to differences in understanding and expressing symptoms, as well as how preferences for treatment are developed and communicated. However, the authors also argue that racial and ethnic bias, discrimination, financial or structural barriers presented by poverty, immigrant status, and other experiences linked to minority status are not “cultural” but rather structural challenges disproportionately experienced by members of nonwhite racial and ethnic groups.
Clinicians must therefore be prepared to address a wide range of possible experiences impacting their patients; however, many current training models focus primarily on acquiring knowledge rather than on developing skills or examining attitudes, which ultimately may prove more useful. Thus “cultural humility” is the “ability to maintain an interpersonal stance that is open in relation to aspects of cultural identity that are most important to the patient.”28 Culturally humble clinicians can express respect and a lack of superiority with regard to the patient’s culture; they do not assume competence in terms of working with a particular patient simply based on prior experience with other patients from similar backgrounds.
Indeed, providers who self-identify as being of a minority background may understand their own personal culture but may not understand every culture, or even that of an individual patient sharing their same cultural background. Therefore, it is equally fundamental for providers, regardless of identity or background, to cultivate cultural humility as a lifelong practice.
ORIGIN AND DEVELOPMENT OF THE SOCIOCULTURAL CURRICULUM
The Massachusetts General Hospital (MGH)/McLean Hospital Adult Psychiatry Residency’s Sociocultural Psychiatry Curriculum had its origins in 1992 under the leadership of Dr. David Henderson, who sought to create a residency didactics curriculum to focus on social and cultural issues with the goal that these aspects would be integrated into every residency lecture—for example, on bipolar disorder, schizophrenia, and anxiety disorders. Dr. Henderson found that most teaching faculty were reluctant to address these topics themselves due to their feeling of not being “experts” on culture. As a result, this curriculum continued, with subsequent course directors adding their specific focus to the series. Dr. Anne Becker, trained in both anthropology and psychiatry, brought an additional focus on global psychiatry; Dr. Siobhan O’Neill meanwhile incorporated her own interest in religion and spirituality. By the time Dr. Nhi-Ha Trinh took the series as a resident in 2002–2006 and then became course director in 2008, the series had grown both unwieldy as well as somewhat “tokenist”—although there was a robust series on religion and spirituality, “cultural issues” writ large were relegated to two lectures on ethnopsychopharmacology by Dr. Henderson as well as three lectures on Asian American, Latino American, and African American mental health. Dr. Trinh was interested in adding a focus on resident self-reflection in the spirit of developing attitudes of cultural humility; she was also interested in making the series more clinically relevant by adding opportunities for resident case discussion.
As part of a curriculum overhaul for the entire residency didactic curriculum in 2013, “content teams” of teaching faculty and interested trainees were formed to reexamine the content, depth, and breadth of residency education. Dr. Trinh was joined by Dr. Justin Chen and Dr. Chris Palmer, as well as trainees at the time, such as Drs. Mimi Owusu, Christine Crawford, and Maithri Amereskere, to critically examine the scope of the series. The content team recommended expanding the scope of the series to become longitudinal, spanning postgraduate year 1 (PGY-1) through PGY-3, and more than doubling the number of hours from 9 to 19. In addition, the arc of the curriculum was developmentally tailored to budding psychiatry residents as they progressed through training.
Box 1.1 lists the course objectives and Box 1.2 lists the lectures for the series. Both course directors (NHT and JC) teach the four PGY-1 lectures, which occur back to back, in order to develop a relationship with residents early on and to foster trust by creating a safe, confidential space where respect for diversity of opinions is encouraged. The course directors attempt to model the type of introspection and vulnerability they hope the residents themselves will demonstrate by using hefty doses of self-disclosure, humor, and validation. The course directors also lead certain PGY-2 and PGY-3 discussions, and one course director endeavors to be present at
Box 1.1.
MGH-McLean Adult Psychiatry Program, Sociocultural Series: Course Objectives
Course Directors: Nhi-Ha Trinh, MD, MPH, and Justin Chen, MD, MPH
PGY-1 Course Objectives, Sociocultural Series
By the end of the PGY-1 series, residents will be able to recognize personal cultural influences and how these might impact the psychiatric clinical encounter by:
1) Defining the concepts of culture, minority status, and privilege.
2) Describing their multidimensional cultural identity.
3) Applying a multidimensional cultural perspective in clinical encounters.
PGY-2 Course Objectives, Sociocultural Series
By the end of the PGY-2 series, residents will be able to demonstrate the influence of “culture,” broadly conceived, on psychiatric practice by:
1) Identifying three challenges of defining psychiatric illness using global psychiatric epidemiology techniques.
2) Listing three social determinants of psychiatric illness in the United States.
3) Understanding and applying the DSM-5’s approach to culture, including specific tools such as the Cultural Formulation Interview.
PGY-3 Course Objectives, Sociocultural Series
By the end of the PGY-3 series, residents will be able to reflect on how psychiatry has been impacted by larger systems (historical precedent, medical practice), and the impact of categories of race, ethnicity, sexuality, socioeconomic status, gender, et cetera by:
1) Describing two historical controversies and two current critiques of psychiatry.
2) Defining minority stress theory, internalized prejudice, and their links to psychiatric illness and practice.
3) Utilizing advanced interviewing techniques to address cultural clinical impasses.
each of the sessions led by other faculty in an attempt to “keep a pulse” on the series for any given class.
In PGY-1, the focus is on grounding residents in an attitude of cultural humility and self-reflection. In PGY-2, the series focus shifts to grounding residents in the broader base of sociocultural psychiatry knowledge and key concepts in crosscultural psychiatry, including social determinants of mental health, global psychiatric epidemiology, defining the line between psychiatric health and illness, and a description of how culture is addressed in the Diagnostic and Statistical Manual of Mental Disorders (DSM). A final interactive lecture based on the residents’ own clinical cases rounds out this year of the series and serves to bring the preceding topics together. As residents become more clinically advanced and sophisticated in their
Box 1.2.
MGH-McLean Adult Psychiatry Program, Sociocultural Series: Lectures
Course Directors: Nhi-Ha Trinh, MD, MPH, and Justin Chen, MD, MPH
PGY-1 lectures (4 hours) (Nhi-Ha Trinh, MD, MPH, and Justin Chen, MD, MPH)
1. Introduction to the Sociocultural Psychiatry Lecture Series: What’s in a name?
2. Culture as multidimensional construct
3. Cultural self-reflection
4. Addressing culture through clinical cases
PGY-2 lectures (6 hours)
1. The other side of normal (Jordan Smoller, MD, ScD)
2. Global psychiatric epidemiology (Alexander Tsai, MD, PhD)
3. Social determinants of psychiatric illness (Erin Dunn, ScD)
4. Culture and psychiatry (Justin Chen, MD, MPH)
5. Disparities in mental health: A case for the DSM-5 Outline for Cultural Formulation and Cultural Formulation Interview (Nhi-Ha Trinh, MD, MPH)
6. Clinical cases through the lens of culture (Justin Chen, MD, MPH, and NhiHa Trinh, MD, MPH)
PGY-3 (9 hours, including three 2-hour workshops)
1–2. Religion and spirituality seminar (2-hour workshop) (Siobhan O’Neill, MD)
3. History of mistakes in psychiatry (Harrison Pope, MD, MPH)
4. Criticisms of psychiatry (David Jones, MD, PhD)
5. Minority stress theory and internalized prejudice (Christine Crawford, MD, MPH)
6–7. When race gets personal in the hospital (2-hour workshop) (Nhi-Ha Trinh, MD, MPH, and Justin Chen, MD, MPH)
8–9. Credibility vs. over-identification in the psychiatric encounter, a.k.a. “You don’t know my life” (2-hour workshop) (Chris Palmer, MD, and Nhi-Ha Trinh, MD, MPH)
understanding during PGY-3, the series once again shifts to address clinical and ethical challenges through experiential workshops that focus on religion and spirituality, cultural dilemmas between clinicians and patients, and discussions on the impact of the checkered history of psychiatry as well as critics of the field—the latter emphasizing the fact that psychiatry itself represents its own culture, with unique historical influences, thought patterns, and behaviors. Taken together, the series endeavors to fulfill the course objectives outlined while providing opportunity for interactive discussion and self-reflection.
Mirroring the structure of the longitudinal sociocultural psychiatry curriculum used in this program, this textbook is designed to take the reader along an arc from more conceptual topics at the beginning to more specific exploration of clinical issues and dilemmas toward the end. The opening chapters focus on big-picture concepts: defining culture as a multidimensional construct, reviewing the role of culture in DSM-5, exploring the principles of global psychiatric epidemiology, and providing an overview of the social determinants of mental health. While some of these topics may seem basic, the editors have previously been frustrated by a lack of engaging, accessible, and succinct articles or publications that summarize these key concepts in a manner that can be used among mental health trainees and clinicians in a practical manner. The current textbook attempts to remedy this deficit.
The next several chapters dive into somewhat more controversial and complex territory, with a consideration of the field of psychiatry as a culture unto itself, an introduction to the concepts of minority stress theory and intersectionality, and an overview and practical guide for working with diverse patient explanatory models of illness. This section of the textbook benefits greatly from the traditions of other disciplines such as history of medicine, sociology, and anthropology to expand the understanding and worldview of learners, while still remaining firmly grounded within the context and practice of psychiatry through the use of real-world clinical examples.
Following these discussions, the important sociocultural concepts of religion/spirituality and gender/sexuality are highlighted with their own chapters. In both cases, concepts of “normal vs. abnormal” and the often blurry line between pathology and culturally acceptable behavior are explored. The next chapter delves further into the influential and expanding knowledge base surrounding implicit bias, with a specific emphasis on the role of clinicians’ unconscious stereotyping in the care they provide.
The textbook’s two penultimate chapters dive headlong into trickier clinical territory. Dr. Reynolds and colleagues explore the challenges that arise when patients request providers of a specific race, religion, gender, or language, and discuss the various historical, ethical, patient-related, and organizational factors that must be considered when deciding whether to accommodate such requests. Meanwhile, Dr. Immanuel and colleagues take a deeper dive into three more in-depth clinical cases that highlight the difficulty of navigating cultural challenges within patient–clinician dyads.
The textbook closes with a chapter that describes sociocultural psychiatry curricula nationwide and proposes a framework for incorporating this important topic into lifelong learning. While this textbook’s chapters roughly correspond to the lectures in the MGH/McLean psychiatry residency’s longitudinal curriculum, it is by no means meant to serve as the only possible template for educators wishing to establish their own curricula on this topic. Due to the very nature of sociocultural issues in psychiatry, any curriculum on the subject should ideally be tailored to the particular knowledge/readiness of residents, patient populations, community needs, and local context, as well as of course the availability of faculty to facilitate these often confronting and challenging conversations.
FINAL NOTES: STRUCTURAL COMPETENCY AND TERMINOLOGY
Emerging trends in the fields of medical education have increasingly focused on “structural competency” of clinicians as an important framework for addressing disparities in clinical care. Structural competency is defined as “the ability for health professionals to recognize and respond with self-reflexive humility and community engagement to the ways negative health outcomes and lifestyle practices are shaped by larger socioeconomic, cultural, political, and economic forces.”29 This represents a recent shift in medical education “toward attention to forces that influence health outcomes at levels above individual interactions.”30 More work will be needed to fully develop curricula to address structural competency for trainees, as well as continuing education for clinicians in practice. The editors of this volume wholeheartedly agree with and support the emphasis on structural competency; at the same time, this volume intentionally focuses on the enhancement of clinical care and practice through honing skills and attitudes relevant to care of individual patients of diverse cultural backgrounds. While this book does touch upon on some of the social determinants of health, as well as historical, social, and global forces shaping psychiatry, it does not primarily focus on structures. The editors believe this is a case of “both/and” rather than “either/or”; mental health trainees can and should understand both structural and cultural contributions to health and illness.
Finally, although key concepts are defined, some variation in terminology may occur from chapter to chapter, reflecting the diversity of the field and the academic orientations of the chapter authors. For instance, terms such as provider, clinician, or psychiatrist may be used; similarly, Black versus African American, or Hispanic versus Latino may appear in the chapters. As much as possible, chapter authors have been asked to define terms used and to be consistent throughout. As reflected in the diverse terminology and perspectives presented, the field of sociocultural psychiatry is filled with both lively discussion and often fractious commentary. The intent of this volume is to highlight for the reader overarching themes in sociocultural psychiatry to enrich clinical practice, with the intent of illuminating the full spectrum of human experience.
REFERENCES
1. Kleinman, A. (1977). Depression, somatization, and the new cross-cultural psychiatry. Social Science and Medicine, 11, 3–10.
2. Colby, S. L., & Ortman, J. M. (2017). Projections of the size and composition of the U.S. population: 2014 to 2060. U.S. Census Bureau. Retrieved from: http://wedocs. unep.org/bitstream/handle/20.500.11822/20152/colby_population.pdf?sequence=1
3. U.S. Census Bureau. (2012). Section 1. Population. In Statistical abstract of the United States. Retrieved from: https://www.census.gov/library/publications/2011/ compendia/statab/131ed/population.html
4. U.S. Census Bureau. (2018). QuickFacts: United States. Retrieved from: https://www. census.gov/quickfacts/fact/table/US/PST045217
5. Race. (n.d.). In Merriam-Webster dictionary. Retrieved from: https://www.merriamwebster.com/dictionary/race
6. Smedley, A. (2008). “Race” and the construction of human identity. American Anthropologist, 100(3), 690–702.
7. Barkan, S. E. (2011). 10.2. The meaning of race and ethnicity. In Sociology: Understanding and changing the social world. Retrieved from: http://open.lib.umn.edu/sociology/ chapter/10-2-the-meaning-of-race-and-ethnicity/
8. Begley, S. (2008, Feb. 29). Race and DNA. Newsweek. Retrieved from: http://www. newsweek.com/race-and-dna-221706
9. Ethnicity. (n.d.). In Merriam-Webster dictionary. Retrieved from: https://www. merriam-webster.com/dictionary/ethnicity
10. Smedley, B. D., Stith, A. Y., & Nelson, A. R.; Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press, 191.
11. Culture. (n.d.). In Merriam-Webster dictionary. Retrieved from: https://www. merriam-webster.com/dictionary/culture
12. Minority. (n.d.). In Merriam-Webster dictionary. Retrieved from: https://www. merriam-webster.com/dictionary/minority
13. Barzilai, G. (2010). Communities and law: Politics and cultures of legal identities. Ann Arbor: University of Michigan Press.
14. Safran, M. A., Mays Jr, R. A., Huang, L. N., McCuan, R., Pham, P. K., Fisher, S. K., . . . Trachtenberg, A. (2009). Mental health disparities. American Journal of Public Health, 99(11), 1962–1966.
15. U.S. Census Bureau. (2010). Census 2010 News. Retrieved from: https://www.census. gov/2010census/news/press-kits/demographic-profiles.html
16. American Psychiatric Association. (2018, January 11). 2005–13: Demographics of the U.S. psychology workforce. Retrieved from: http://www.apa.org/workforce/ publications/13-demographics/index.aspx
17. American Psychiatric Association. (2018, March 26). CWS Data Tool: Demographics of the U.S. psychology workforce. Retrieved from: http://www.apa.org/workforce/ data-tools/demographics.aspx
18. Nivet, M. A., & Castillo-Page, L. (2014). Diversity in the physician workforce: Facts & figures 2014. Association of American Medical Colleges. Retrieved from: https:// www.aamc.org/data/workforce/reports/439214/workforcediversity.html
19. Brotherton, S. E., Rockey, P. H., & Etzel, S. I. (2005). US graduate medical education, 2004-2005: Trends in primary care specialties. Journal of American Medical Association, 294(9), 1075–1082.
20. Lokko, H. N., Chen, J. A., Parekh, R. I., & Stern, T. A. (2016). Racial and ethnic diversity in the US psychiatric workforce: A perspective and recommendations. Academic Psychiatry, 40(6), 898–904.
21. Data USA. (2018, March 26). Social workers. Retrieved from: https://datausa.io/profile/soc/211020/#demographics
22. Maxie, A. C., Arnold, D. H., & Stephenson, M. (2006). Do therapists address ethnic and racial differences in cross-cultural psychotherapy? Psychotherapy: Theory, Research, Practice, Training, 43(1), 85.
23. NCCC. (2018, March 26). Curricula enhancement module series. Retrieved from: https://nccc.georgetown.edu/curricula/culturalcompetence.html
24. Betancourt, J. R., Green, A. R., Carrillo, J. E., & Ananeh-Firempong, O. (2003). Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports, 118(4), 293–302.
25. Sue, D. W. (1994). Asian-American mental health and help seeking behavior: Comments on Solberg et al. (1994), Tata and Leong (1994), and Lin (1994). Journal of Counselling Psychology, 41, 280–287.
26. Horvat, L., Horey, D., Romios, P., & Kis-Rigo, J. (2014). Cultural competence education for health professionals. Cochrane Database Systematic Reviews, 5, CD009405.
27. Qureshi, A., Collazos, F., Ramos, M., & Casas, M. (2008). Cultural competency training in psychiatry. European Psychiatry, 23, 49–58.
28. Hook, J. N., Davis, D. E., Owen, J., Worthington, E. L., & Utsey, S. O. (2013). Cultural humility: Measuring openness to culturally diverse clients. Journal of Counselling Psychology, 60(3), 353–366.
29. Bourgois, P., Holmes, S. M., Sue, K., & Quesada, J. (2017). Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Academic Medicine, 92(3), 299–307.
30. Neff, J., Knight, K. R., Satterwhite, S., Nelson, N., Matthews, J., & Holmes, S. M. (2017). Teaching structure: A qualitative evaluation of a structural competency training for resident physicians. Journal of General Internal Medicine, 32(4), 430–433.