PREFACE
In the past 2 decades, diagnostics and therapeutics in neuroimmunology have rapidly evolved and increased in complexity. Diagnosis is assisted by various laboratory and advanced imaging techniques. Randomized clinical trials in multiple sclerosis (MS) and neuromyelitis optica (NMO), and smaller studies for rarer autoimmune diseases, have led to distinct immune molecule–targeted and mechanism-specific therapies. The fields of cerebrovascular medicine, neurooncology, and neuroinfectious diseases have not remained static either. All of these gains present a challenge, however, in that early and accurate neurologic diagnosis is more important than ever. In our experience, some diagnostic pitfalls lie in the interpretation of test results and images without reference to the nuances of the clinical history and examination. Although some things change (eg, technology), other things never change (eg, clinical common sense).
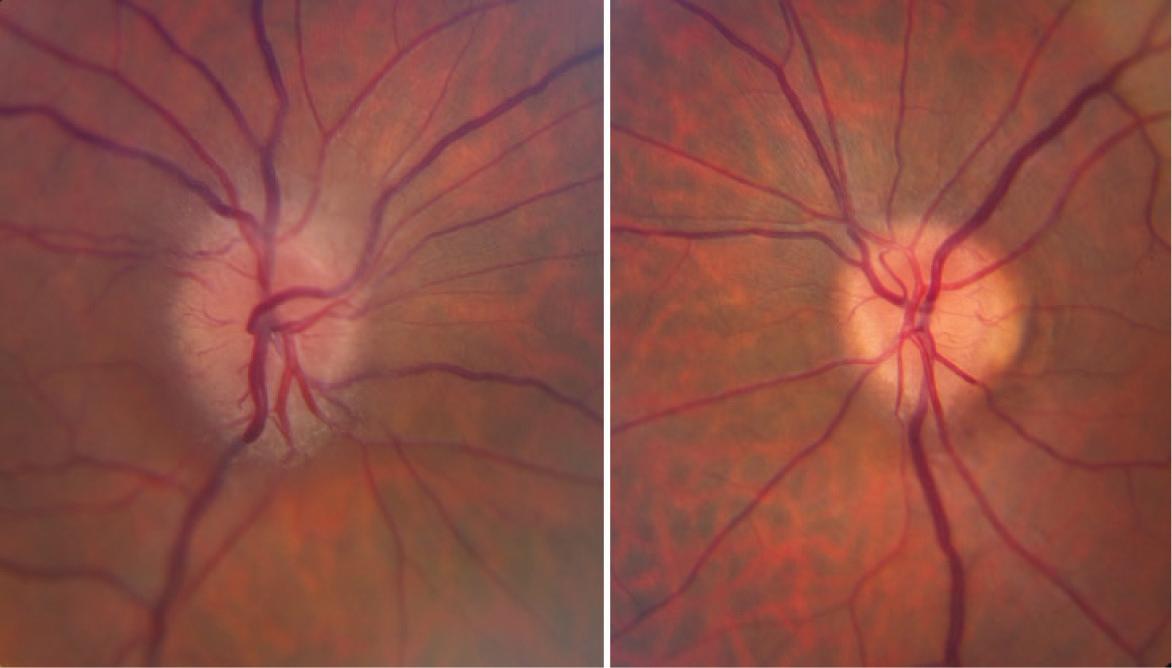
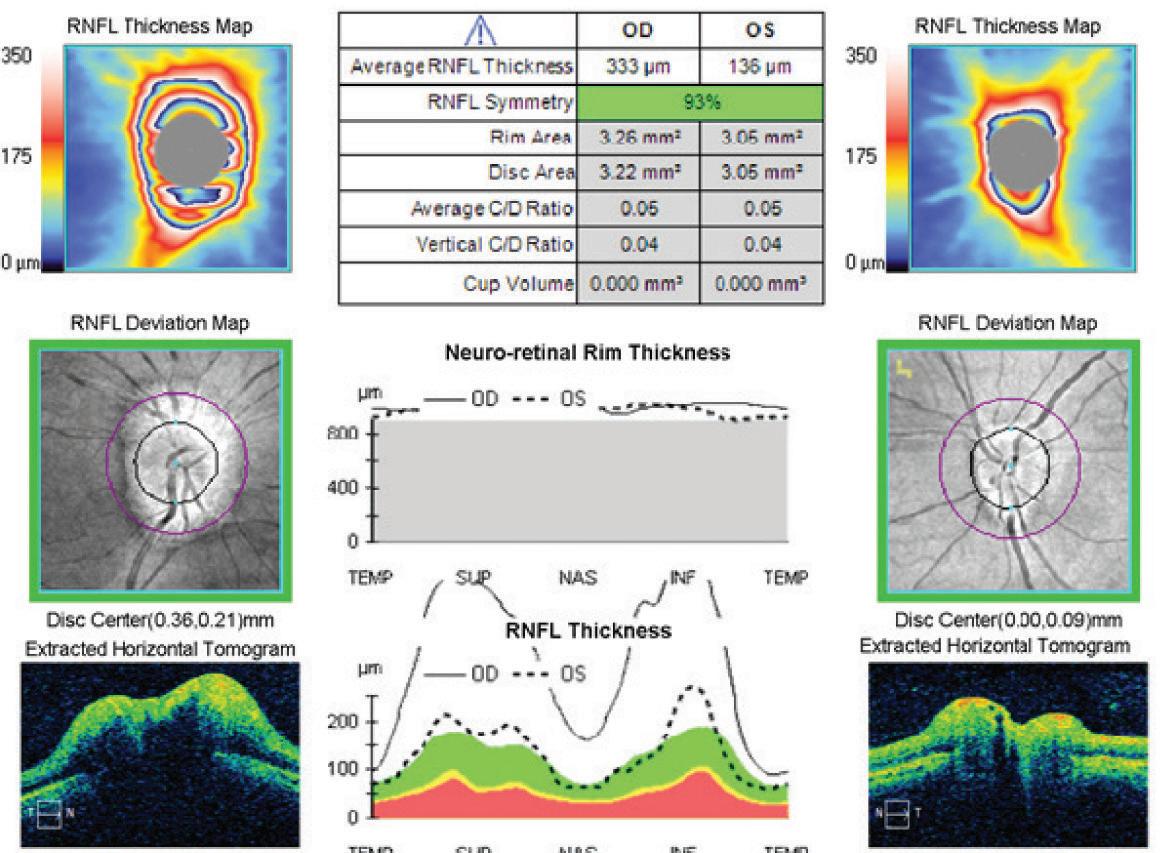
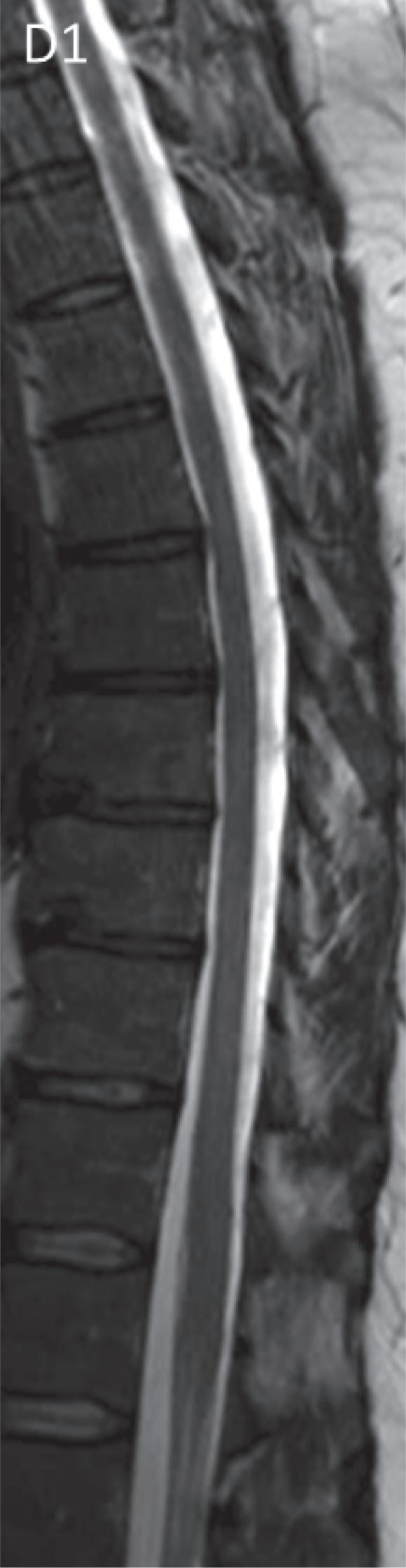
The 83 case-based chapters of Mayo Clinic Cases in Neuroimmunology are intended to provide a sampling of our clinical experiences across our Division of Multiple Sclerosis and Autoimmune Neurology at Mayo Clinic in Minnesota, Arizona, and Florida. These cases focus on key components of the history, examination and test findings, and differential diagnosis, although we also reference treatment approaches extensively throughout. To bring some form to this extensive repertoire of cases, we have divided the book into 3 sections covering central nervous system (CNS) demyelinating disease (MS, NMO, and limited forms of
those disorders), autoimmune neurologic disorders (usually defined by immunoglobulin G antibody biomarkers), and others (CNS inflammatory disorders not fitting into the first 2 categories, along with neuroimmunologic mimics). We have illustrated the cases extensively with imaging and, where relevant, pathologic images and video material. The book will be useful to all clinicians who evaluate patients with neurologic disorders, both generalists and neuroimmunology subspecialists. The book will also be useful to medical students and resident and fellow trainees in neurology, medicine, and psychiatry. Board review–style questions are also provided.
We wish to thank Kenna Atherton, LeAnn Stee, Jane Craig, Ann Ihrke, and Alyssa B. Quiggle, PhD, for their conscientious help in editing and preparing the manuscript for publication. We also thank Collette Justin for her expert help in preparing the figures. We are indebted to our patients and also to our Department of Neurology colleagues outside our subspecialty division (several of whom have authored chapters herein), without whom we never would have encountered many of the patients described. Finally, we wish to express our humble gratitude to our respective partners, Jen, Jenny, and Mairead, and our children, for their enduring patience and love.
Andrew McKeon, MB, BCh, MD
B. Mark Keegan, MD
W. Oliver Tobin, MB, BCh, BAO, PhD
CONTENTS
Contributors xv
SECTION I
CNS DEMYELINATING DISEASE
Case 1 A Woman With Subacute Painful Vision Loss 3
Jiraporn Jitprapaikulsan, MD, M. Tariq Bhatti, MD, Eric R. Eggenberger, DO, Marie D. Acierno, MD, and John J. Chen, MD, PhD
Case 2 Rapidly Progressive Numbness and Weakness After Soft-Tissue Abscess 7
Elia Sechi, MD, and Dean M. Wingerchuk, MD
Case 3 Weakness With Neck Flexion 10
Brian G. Weinshenker, MD
Case 4 New-Onset Right-Sided Numbness and Double Vision 14
W. Oliver Tobin, MB, BCh, BAO, PhD
Case 5 Progressive Left Lower Extremity Weakness and Thoracic Spinal Cord Lesion 17
B. Mark Keegan, MD
Case 6 Progressive Spasticity With a Single Magnetic Resonance Imaging Lesion 20
Samantha A. Banks, MD, and Eoin P. Flanagan, MB, BCh
Case 7 Fluctuating Vision Loss, Seizures, and Left Parieto-Occipital Mass 22
Alicja Kalinowska-Lyszczarz, MD, PhD, W. Oliver Tobin, MB, BCh, BAO, PhD, Yong Guo, MD, PhD, and Claudia F. Lucchinetti, MD
Case 8 Diffuse Pain and Abnormal Brain MRI Findings 26
Andrew McKeon, MB, BCh, MD
Case 9 Lesions Found by Chance 29
Dean M. Wingerchuk, MD
Case 10 Encephalopathy and Quadriparesis After an Upper Respiratory Tract Infection 32
A. Sebastian Lopez Chiriboga, MD
Case 11 Severe Monocular Vision Loss Followed by Gait Difficulty 35
Brian G. Weinshenker, MD
Case 12 Multiple Sclerosis and Cognitive Impairment 39
Cristina Valencia-Sanchez, MD, PhD, and Jonathan L. Carter, MD
Case 13 New-Onset Gait Difficulty With Kappa Free Light Chains in Cerebrospinal Fluid 42
Maria Alice V. Willrich, PhD, and Ruba S. Saadeh
Case 14 A Girl With Back Pain, Paresthesias, and Painful Vision Loss 44
Cecilia Zivelonghi, MD, and Andrew McKeon, MB, BCh, MD
Case 15 A Septuagenarian With Progressive Hemiparesis 48
Roman Kassa, MD, and B. Mark Keegan, MD
Case 16 Recurrent Demyelinating Episodes 51
I. Vanessa Marin Collazo, MD
Case 17 Breakthrough Disease While on Multiple Sclerosis Immunomodulatory Therapy 55
Jonathan L. Carter, MD
Case 18 Highly Active Multiple Sclerosis 57
Roman Kassa, MD, and W. Oliver Tobin, MB, BCh, BAO, PhD
Case 19 Progressive Gait Difficulties 62
I. Vanessa Marin Collazo, MD
Case 20 Progressive Cerebellar Ataxia After Natalizumab Treatment 65
Michel Toledano, MD
Case 21 Weakness and Dysarthria After Radiosurgery 69
Andrew McKeon, MB, BCh, MD
SECTION II AUTOIMMUNE NEUROLOGIC DISORDERS
Case 22 Fatigue, Blurry Vision, and Swollen Optic Nerves 75
Marie D. Acierno, MD, M. Tariq Bhatti, MD,
John J. Chen, MD, PhD, and Eric R. Eggenberger, DO
Case 23 Progressive, Symmetrical, Painless Visual Loss 77
Eric R. Eggenberger, DO, Marie D. Acierno, MD, M. Tariq Bhatti, MD, and John J. Chen, MD, PhD
Case 24 Personality Changes, Cognitive Decline, and Jerking Movements 80
A. Sebastian Lopez Chiriboga, MD
Case 25 Rapidly Progressive Memory Loss, Mood Change, Mutism, and Abnormal Movements 83
Shailee S. Shah, MD, and Marie F. Grill, MD
Case 26 Behavioral and Cognitive Changes Followed by Coma 86
Anastasia Zekeridou, MD, PhD
Case 27 Episodic Hemiparesis, Cognitive Decline, and Seizures in a Woman With Pernicious Anemia 90
Cristina Valencia-Sanchez, MD, PhD, and Andrew McKeon, MB, BCh, MD
Case 28 Rapidly Progressive Dementia and Thyroid Antibodies 93
Amy C. Kunchok, MBBS, and Eoin P. Flanagan, MB, BCh
Case 29 Goose Bumps and Memory Loss 96
Jeffrey W. Britton, MD, Bhavya Narapureddy, MBBS, and Divyanshu Dubey, MBBS
Case 30 A Patient With Headache and Progressive Tremor 98
Anastasia Zekeridou, MD
Case 31 A Man With Flulike Symptoms and Hemorrhagic Brain Lesions 101
Michel Toledano, MD
Case 32 Hearing Loss, Imbalance, and Diplopia in a 44-Year-Old Man 105
Michelle F. Devine, MD, Divyanshu Dubey, MBBS, and Sean J. Pittock, MD
Case 33 Chorea, Ataxia, and Disturbed Sleep 108
John C. Feemster, and Erik K. St. Louis, MD, MS
Case 34 Rapidly Progressive Gait and Coordination Difficulties 111
Andrew McKeon, MB, BCh, MD
Case 35 Dancelike Movements in a Patient With a History of Rash 113
Andrew McKeon, MB, BCh, MD
Case 36 Body Spasms in a Woman With Thyroid Disease 116
Andrew McKeon, MB, BCh, MD
Case 37 Stiffness, Spasms, and Frequent Falls in a 41-Year-Old Man 118
Michelle F. Devine, MD, and A. Sebastian Lopez Chiriboga, MD
Case 38 Rapid-Onset Weakness and Numbness in a Patient With Systemic Lupus Erythematosus 120
Floranne C. Ernste, MD
Case 39 Progressive Quadriparesis and Cancer 122
Elia Sechi, MD, and Eoin P. Flanagan, MB, BCh
Case 40 Progressive Numbness, Burning Pain, Imbalance, and Dryness 125
Shahar Shelly, MD, and Divyanshu Dubey, MBBS
Case 41 Ascending Painful Paresthesias, Progressive Ataxia, and Bilateral Foot Drop 128
Rocio Vazquez Do Campo, MD, and Divyanshu Dubey, MBBS
Case 42 Painless, Symmetric, Ascending Weakness and Sensory Loss 131
Christopher J. Klein, MD
Case 43 Difficult-to-Treat Polyradiculoneuropathy 135
Marcus V. R. Pinto, MD, MS, and P. James B. Dyck, MD
Case 44 Autoimmune Peripheral Nervous System Hyperexcitability 138
Christopher J. Klein, MD
Case 45 Orthostatism, Constipation, and Early Satiety 140
Kamal Shouman, MD, and Eduardo E. Benarroch, MD
Case 46 Constipation and Syncope 143
Michelle F. Devine, MD, and Sean J. Pittock, MD
Case 47 Bulbar-Predominant Weakness 146
Jennifer A. Tracy, MD, and Vanda A. Lennon, MD, PhD
Case 48 Difficulty Climbing the Stairs 149
Anastasia Zekeridou, MD, PhD, and Vanda A. Lennon, MD, PhD
Case 49 Rapidly Progressive Proximal Weakness 152
Teerin Liewluck, MD, and Margherita Milone, MD, PhD
Case 50 Progressive Weakness and Rash 154
Margherita Milone, MD, PhD, and Teerin Liewluck, MD
Case 51 “Restlessness” After Cancer Diagnosis and Treatment 157
Anastasia Zekeridou, MD, PhD
Case 52 Sudden Onset of Diplopia and a Skeletal Muscle Antibody 160
John R. Mills, PhD
SECTION III
OTHER INFLAMMATORY CNS DISORDERS AND NEUROIMMUNOLOGIC MIMICS
Case 53 Diplopia, Orbital Pain, and Vision Loss in a Middle-Aged Woman 165
Lauren M. Webb, and Eoin P. Flanagan, MB, BCh
Case 54 A Young Man With Visual Field Loss, Decreased Hearing, and Confusion 168
M. Tariq Bhatti, MD, Eric R. Eggenberger, DO, Marie D. Acierno, MD, and John J. Chen, MD, PhD
Case 55 A Woman With Progressive Gait Difficulty and White Matter Abnormalities 171
Adrian Budhram, MD, and Ralitza H. Gavrilova, MD
Case 56 Progressive Asymmetrical Limb Impairment and Cognitive Decline With Leukoencephalopathy 174
B. Mark Keegan, MD
Case 57 A Woman With Fever, Confusion, and Seizures 177
Michel Toledano, MD
Case 58 Encephalopathy With Alternating Hemispheric MRI Abnormalities 181
Andrew McKeon, MB, BCh, MD
Case 59 Rapid-Onset Hemibody Sensory Loss, Incoordination, and Muscle Jerking 184
Andrew McKeon, MB, BCh, MD, and Nicholas L. Zalewski, MD
Case 60 A History of Sarcoidosis and a New Brain Lesion 187
Andrew McKeon, MB, BCh, MD, and Julie E. Hammack, MD
Case 61 Headache and Hemiparesis in Middle Age 189
Catalina Sanchez Alvarez, MD, and Kenneth J. Warrington, MD
Case 62 Subacute Cognitive Decline in an 86-Year-Old Woman With Prior Lobar Intracerebral Hemorrhage 192
Stephen W. English Jr, MD, MBA, and James P. Klaas, MD
Case 63 A 75-Year-Old Man With 5 Days of Progressive Gait Difficulties and Confusion 195
Julie E. Hammack, MD
Case 64 Night Sweats and Paraparesis 199
David N. Abarbanel, MD, and Ivan D. Carabenciov, MD
Case 65 A Woman With Headaches and a Tumefactive Brain Lesion 202
Andrew McKeon, MB, BCh, MD
Case 66 Behavioral Change, Seizures, and Temporal Lobe Lesion 204
Stuart J. McCarter, MD, and Andrew McKeon, MB, BCh, MD
Case 67 A Young Woman With Vessel Dissection and Brainstem Lesions 207
Burcu Zeydan, MD, and Orhun H. Kantarci, MD
Case 68 Headache, Uveitis, and Leptomeningeal Enhancement 210
Orhun H. Kantarci, MD
Case 69 Weakness and Punctate Enhancement 213
W. Oliver Tobin, MB, BCh, BAO, PhD
Case 70 Bilateral Paresthesias in Crohn Disease 216
Amy C. Kunchok, MBBS, and Andrew McKeon, MB, BCh, MD
Case 71 Seizures and Enhancing Brain Lesions 219
Josephe Archie Honorat, MD, PhD, and Andrew McKeon, MB, BCh, MD
Case 72 A Man With Recurrent Headache and Focal Neurologic Deficits 222
Jaclyn R. Duvall, MD, and Jerry W. Swanson, MD, MHPE
Case 73 Headache, Radicular Pain, and Enhancing Lesions 225
W. Oliver Tobin, MB, BCh, BAO, PhD
Case 74 Seizures 3 Months After Endarterectomy 228
Andrew McKeon, MB, BCh, MD, and
Robert D. Brown Jr, MD, MPH
Case 75 Progressive Bilateral Arm Pain, Gait Disturbance, Constipation, and Urinary Retention 231
Ivan D. Carabenciov, MD, and Michael W. Ruff, MD
Case 76 A Woman With Subacute Numbness of the Trunk, Arms, and Legs 233
Eoin P. Flanagan, MB, BCh
Case 77 A Septuagenarian With Progressive Lower Extremity Weakness and Pain 235
Nicholas L. Zalewski, MD
Case 78 Acute Quadriparesis in a Smoker 238
Nicholas L. Zalewski, MD
Case 79 A 25-Year-Old Man With Recurrent Back Pain and Rapid-Onset Paraplegia 242
Nicholas L. Zalewski, MD
Case 80 Progressive Myelopathy After Neck Pain 246
Eoin P. Flanagan, MB, BCh
Case 81 Progressive Imbalance and Visual Impairment in a Patient With Diabetes 248
Neeraj Kumar, MD
Case 82 Progressive Myelopathy After Spine Surgery 251
Andrew McKeon, MB, BCh, MD, and Nicholas L. Zalewski, MD
Case 83 Altered Mental Status During the COVID-19 Pandemic 254
Sara Mariotto, MD, Silvia Bozzetti, MD, Maria Elena De Rui, MD, Fulvia Mazzaferri, MD, PhD, Andrew McKeon, MB, BCh, MD, and Sergio Ferrari, MD
SECTION IV
QUESTIONS AND ANSWERS
Section I: CNS Demyelinating Disease Questions and Answers 259
Section II: Autoimmune Neurologic Disorders Questions and Answers 269
Section III: Other Inflammatory CNS Disorders and Neuroimmunologic Mimics Questions and Answers 285
Index 299
CONTRIBUTORS
David N. Abarbanel, MD
Resident in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Marie D. Acierno, MD
Senior Associate Consultant, Department of Ophthalmology, Mayo Clinic, Scottsdale, Arizona; Assistant Professor of Ophthalmology, Mayo Clinic College of Medicine and Science
Samantha A. Banks, MD
Resident in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Eduardo E. Benarroch, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
M. Tariq Bhatti, MD
Senior Associate Consultant, Department of Ophthalmology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology and of Ophthalmology, Mayo Clinic College of Medicine and Science
Silvia Bozzetti, MD
Department of Neuroscience, Biomedicine, and Movement Sciences, University of Verona, Verona, Italy
Jeffrey W. Britton, MD
Chair, Division of Epilepsy, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Robert D. Brown Jr, MD, MPH
Chair, Division of Stroke and Cerebrovascular Diseases, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Adrian Budhram, MD
Research Collaborator in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Ivan D. Carabenciov, MD
Senior Associate Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota
Jonathan L. Carter, MD
Consultant, Department of Neurology, Mayo Clinic, Scottsdale, Arizona; Associate Professor of Neurology, Mayo Clinic College of Medicine and Science
John J. Chen, MD, PhD
Consultant, Department of Ophthalmology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Neurology and of Ophthalmology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Maria Elena De Rui, MD
Infectious Diseases Section, Department of Diagnostic and Public Health, University of Verona, Verona, Italy
Michelle F. Devine, MD
Research Collaborator in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Divyanshu Dubey, MBBS
Senior Associate Consultant, Department of Laboratory Medicine & Pathology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Laboratory Medicine & Pathology and of Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Jaclyn R. Duvall, MD
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with Utica Park Headache Clinic, Tulsa, Oklahoma
P. James B. Dyck, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Eric R. Eggenberger, DO
Consultant, Department of Ophthalmology, Mayo Clinic, Jacksonville, Florida; Professor of Neurology and of Ophthalmology, Mayo Clinic College of Medicine and Science
Stephen W. English Jr, MD, MBA
Senior Associate Consultant, Department of Neurology, Mayo Clinic, Jacksonville, Florida
Floranne C. Ernste, MD
Consultant, Division of Rheumatology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Medicine, Mayo Clinic College of Medicine and Science
John C. Feemster
Graduate Research Employment Program, Center for Sleep Medicine, Mayo Clinic, Rochester, Minnesota; Medical College of Wisconsin, Central-Wisconsin, Wausau, Wisconsin
Sergio Ferrari, MD
Department of Neuroscience, Biomedicine, and Movement Sciences, University of Verona, Verona, Italy
Eoin P. Flanagan, MB, BCh
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Neurology, Mayo Clinic College of Medicine and Science
Ralitza H. Gavrilova, MD
Consultant, Departments of Clinical Genomics and Neurology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Medical Genetics and of Neurology, Mayo Clinic College of Medicine and Science
Marie F. Grill, MD
Consultant, Department of Neurology, Mayo Clinic Hospital, Phoenix, Arizona; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Yong Guo, MD, PhD
Research Associate, Department of Neurology, Mayo Clinic, Rochester, Minnesota
Julie E. Hammack, MD
Consultant, Department of Neurology, Mayo Clinic, Jacksonville, Florida; Associate Professor of Neurology, Mayo Clinic College of Medicine and Science
Josephe Archie Honorat, MD, PhD
Research Fellow in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with SUNY Downstate Health Sciences University, Brooklyn, New York
Jiraporn Jitprapaikulsan, MD
Research Collaborator, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with Siriraj Hospital, Bangkok Noi, Thailand
Alicja Kalinowska-Lyszczarz, MD, PhD
Research Collaborator in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Orhun H. Kantarci, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Roman Kassa, MD, PhD
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with University of Cincinnati College of Medicine, Cincinnati, Ohio
B. Mark Keegan, MD
Chair, Division of Multiple Sclerosis & Autoimmune Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
James P. Klaas, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Christopher J. Klein, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Neeraj Kumar, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Amy C. Kunchok, MBBS
Research Collaborator, Mayo Clinic School of Graduate Medical Education and Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Vanda A. Lennon, MD, PhD
Consultant, Department of Laboratory Medicine & Pathology, Mayo Clinic, Rochester, Minnesota; Professor of Immunology and of Neurology, Mayo Clinic College of Medicine and Science
Teerin Liewluck, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Neurology, Mayo Clinic College of Medicine and Science
A. Sebastian Lopez Chiriboga, MD
Senior Associate Consultant, Department of Neurology, Mayo Clinic, Jacksonville, Florida; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science, Jacksonville, Florida
Claudia F. Lucchinetti, MD
Chair, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
I. Vanessa Marin Collazo, MD
Consultant, Department of Neurology, Mayo Clinic, Jacksonville, Florida; Instructor in Neurology, Mayo Clinic College of Medicine and Science
Sara Mariotto, MD
Department of Neuroscience, Biomedicine, and Movement Sciences, University of Verona, Verona, Italy
Fulvia Mazzaferri, MD, PhD
Infectious Diseases Section, Department of Diagnostic and Public Health, University of Verona, Verona, Italy
Stuart J. McCarter, MD
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education and Instructor in Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Andrew McKeon, MB, BCh, MD
Consultant, Departments of Laboratory Medicine & Pathology, and Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Laboratory Medicine & Pathology and of Neurology, Mayo Clinic College of Medicine and Science
John R. Mills, PhD
Consultant, Department of Laboratory Medicine & Pathology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Laboratory Medicine & Pathology, Mayo Clinic College of Medicine and Science
Margherita Milone, MD, PhD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Bhavya Narapureddy, MBBS
Research Assistant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; now with Upstate Medical University, Syracuse, New York
Marcus V. R. Pinto, MD, MS
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education and Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Sean J. Pittock, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Michael W. Ruff, MD
Senior Associate Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Ruba S. Saadeh
Clinical Research Assistant, Department of Neurology, Mayo Clinic, Rochester, Minnesota
Catalina Sanchez Alvarez, MD
Fellow in Rheumatology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Jacksonville, Florida; now with University of Florida Health, Gainesville, Florida
Elia Sechi, MD
Senior Research Fellow in Neurology, Mayo Clinic School of Graduate Medical Education and Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with the University of Sassari, Sassari, Italy
Shailee S. Shah, MD
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Shahar Shelly, MD
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Kamal Shouman, MD
Senior Associate Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Erik K. St. Louis, MD, MS
Chair, Division of Sleep Neurology and Consultant, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota; Associate Professor of Neurology, Mayo Clinic College of Medicine and Science
Jerry W. Swanson, MD, MHPE
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
W. Oliver Tobin, MB, BCh, BAO, PhD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Neurology, Mayo Clinic College of Medicine and Science
Michel Toledano, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Jennifer A. Tracy, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Cristina Valencia-Sanchez, MD, PhD
Resident in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Rocio Vazquez Do Campo, MD
Fellow in Neurology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with UAB Medicine, Birmingham, Alabama
Kenneth J. Warrington, MD
Chair, Division of Rheumatology, Mayo Clinic, Rochester, Minnesota; Professor of Medicine, Mayo Clinic College of Medicine and Science
Lauren M. Webb
Medical Student, Mayo Clinic Alix School of Medicine, Mayo Clinic College of Medicine and Science, Rochester, Minnesota
Brian G. Weinshenker, MD
Consultant, Department of Neurology, Mayo Clinic, Rochester, Minnesota; Professor of Neurology, Mayo Clinic College of Medicine and Science
Maria Alice V. Willrich, PhD
Consultant, Department of Laboratory Medicine & Pathology, Mayo Clinic, Rochester, Minnesota; Associate Professor of Laboratory Medicine & Pathology, Mayo Clinic College of Medicine and Science
Dean M. Wingerchuk, MD
Chair, Department of Neurology, Mayo Clinic, Scottsdale, Arizona; Professor of Neurology, Mayo Clinic College of Medicine and Science
Nicholas L. Zalewski, MD
Senior Associate Consultant, Department of Neurology, Mayo Clinic, Scottsdale, Arizona; Assistant Professor of Neurology, Mayo Clinic College of Medicine and Science
Anastasia Zekeridou, MD, PhD
Associate Consultant, Departments of Laboratory Medicine & Pathology and Neurology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Laboratory Medicine & Pathology and of Neurology, Mayo Clinic College of Medicine and Science
Burcu Zeydan, MD
Associate Consultant, Department of Radiology, Mayo Clinic, Rochester, Minnesota; Assistant Professor of Neurology and of Radiology, Mayo Clinic College of Medicine and Science
Cecilia Zivelonghi, MD
Research Fellow in Neuroimmunology, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota; now with University of Verona, Verona, Italy