UnderstandingPsychopharmacology:TheBasics
Partoneofthisbookbrieflycoversthedevelopmentofpsychopharmacologyfromahistoricalandsociological perspectiveandthengoesontoprovideanoverviewofneurobiologyandpharmacology Thepurposeofthese chaptersisnottoprovideacomprehensivediscussionofthefieldsofpharmacologyorneurophysiology,butis simplytofamiliarizeyouwiththebasicterminologyandmodelsofpharmacokinetics.
Introduction
This book is intended primarily for mental health professionals and those in graduate training in psychology, social work, psychiatric nursing, and counseling The professional goal of most readers will be to provide services that aim to reduce emotional pain, to promote psychological growth and healing, and to foster the development of personal autonomy. To these ends, we in the field are trained in various theoretical approaches that attempt to explain the development of maladaptive lifestyles and subjectively painful psychiatric symptoms These theories serve to give meaning and coherence to what we do in clinical practice and, most importantly, lay a foundation of understanding so that interventions make sense and further the goalofreducingsufferinginwaysthatareeffective
Many schools of thought exist regarding the origins of mental health problems. As has been well documented in the history of psychiatry, as schools of thought evolve, controversy, dogma, and empassioned belief systems emerge It may be inherent to the development and maturation of science that these emotionallytonedbeliefsystemsandtheresultingdebatesoccur.
Fromthemid-1960sthroughthe1970s,polarizationoccurredwithinpsychiatrybetweenthoseadvocating psychological theories (primarily psychodynamic and behavioral models) and those on the other side of the fence using biological and medical models The disagreements that emerged were more than differences of opinion or dry debate Each school attracted followers who had strong emotional investments in their perspective.
For many years this division resulted in the development of barriers between groups of mental health clinicians andattimesinfragmentationincare.Fortunately,duringthepastdecadesomethinghaschanged. We are beginning to witness a shift in thinking, as increasing numbers of practitioners and training institutes move away from egocentric and dogmatic positions and begin to embrace a more integrated approach with regardtoboththeoriesofetiologyandmethodsoftreatment.
New discoveries in the neurosciences, refined technical advances in psychotherapy, and a large number of outcome studies in both pharmacotherapy and psychotherapy have made it abundantly clear: People are complex Mental health problems spring from many sources; and reductionist, unidimensional models are simply inadequate to explain the wide array of mental and emotional problems people experience. Likewise, no single approach to treatment works for all problems Certain disorders clearly respond better to certain interventions,whereasothersrequirealternativeapproaches
In writing this book, although our primary focus is on psychopharmacology, we share a strong respect for what will be termed integrative approaches to treatment: recognition of the importance of varied treatments andcollaborationamongprofessionalsfromdifferentdisciplines
We hope that you will find this book helpful as you engage in this most important profession and work towardthegoalofreducingemotionalpain
HistoryofBiologicalPsychiatry
Inunderstandingpsychopharmacology,itmaybehelpfulifyouareabletoplaceitinahistoricalcontext Let’s takeabrieflookatthishistoryasitunfolded
Inthelateeighteenhundreds,psychiatrywasclearlyrootedinthemedicalmodelandtheneurologyofthe day Psychiatrists believed, almost exclusively, that mental illness could be attributed to some sort of biologic disturbance. The earliest attempts to approach the understanding of mental illness in this era involved two mainareasofinvestigation
On one front was the development of the first systematic nosologic system by Emil Kraepelin. This pioneering work laid the foundation for all later diagnostic schema (such as the Diagnostic and Statistical Manual of Mental Disorders, or DSM). And many of Kraepelin’s original notions about the classification of major mental illness have stood the test of time. He was a brilliant investigator and the one most responsible forusheringindescriptiveclinicalpsychiatry However,hisendeavorsmusthavebeenaccompaniedbyagood deal of frustration and impotence, since, despite the development of a systematic approach to diagnosis, Kraepelinandotherpsychiatristsofhistimehadfew,ifany,methodsoftreatment.
At the same time, the hunt was on for evidence of brain pathology, which was presumed to underlie mental illness Research was conducted in neuroanatomy labs but yielded few concrete results For example, the famous French neurologist Jean-Martin Charcot believed that hysterical conversation symptoms were undoubtedly due to some type of central nervous system lesion. He explained the fact that no demonstrable pathology could be isolated on autopsy by saying it simply suggested that somehow the lesion mysteriously disappearedatthetimeofdeath Wemustbearinmind,however,thatinalllikelihood,theseresearchersand clinicians were desperate to find causes and cures and went at it by the means best known to them (biology) andusingthescanttechnologyavailableatthetime
Biologicalpsychiatrygotashotinthearminthelateeighteenhundreds,astwodiscoveriesweremade.At the time, probably one half of those housed in asylums suffered from a type of psychotic-organic brain syndromethatultimatelywasfoundtobecausedbytheTreponemapallidumbacteria(acentralnervoussystem infection seen in the late stages of syphilis). It was also eventually discovered that some organic mental syndromes were due to pellagra (a disease associated with niacin and protein deficiency) These were important discoveries, and they fueled enthusiasm in biological psychiatry It was just a matter of time, it was felt, before other biologic causes would be isolated and medical treatments developed. However, such discoveries did not occur until the middle of the twentieth century For practical purposes, biological psychiatrycametoahaltasitenteredthenineteenhundreds
The disappointments stemming from medical research on mental illness and the failure to develop any effectivetreatmentprobablyincreasedthereceptivityofpsychiatrytodivergentapproaches Atthissametime Sigmund Freud was assembling the basic notions of psychoanalysis. Freud’s initial theory was strongly influenced by his own medical and neurological training (for example, his “Project for a Scientific Psychology,” 1895), and many of his prevailing ideas continued to have their roots in biology, including drive theory, instincts, and psychosexual development. However, his newly emerging theory and techniques of
treatmentsparkedinterestintheuseofnovel,nonmedicalapproachestotreatment
By the 1920s psychological (rather than biological) explanations for the development and treatment of psychopathology had found their place in clinical psychiatry, and by the 1940s psychodynamic thinking had permeated American psychiatry and become the dominant theoretical model Yet these newly developed approaches proved to be inadequate in the treatment of the more serious forms of mental illness, such as schizophrenia and manic-depressive psychosis In one of his last manuscripts, Freud himself admitted his disappointment in psychoanalytic methods for treating schizophrenia He hypothesized that eventually it would be discovered that these grave mental disorders were due to some form of biologic abnormality, and thatperhapsdrugswouldeventuallybefoundtotreattheseillnesses
SomaticTherapies
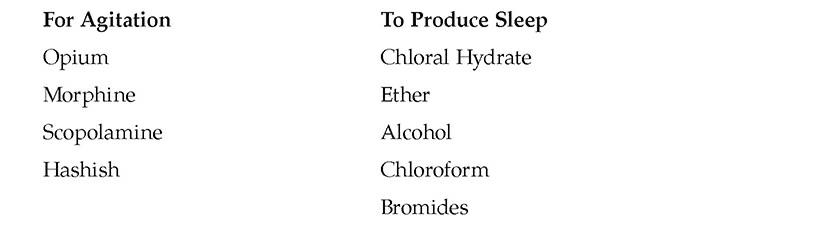
In the days of Kraepelin, pharmaceuticals were used to treat mentally ill patients Generally, the drugs were prescribed to sedate wildly agitated psychotic patients For example, Kraepelin listed in one of his textbooksthefollowinggroupofrecommendedmedications(SpiegelandAebi1989):
Kraepelin noted, however, that none of these preparations cured mental illness, that they were for shortterm use, and that a number of them could lead to problems with addiction All of these drugs achieved behavioral control by sedating patients; none really affected psychotic symptoms per se, nor did they have any impactonactivatingpatientswhowerestuporousorclinicallydepressed
Other somatic therapies were developed in the first half of the twentieth century, with variable results Malaria therapy was conceived in 1917, insulin shock in 1927, psychosurgery in 1936, and electroconvulsive treatment (ECT) in 1938. All of these methods, as originally conceived, carried serious risks, and most demonstrated marginal effectiveness Psychosurgeries were carried out by the thousands in the 1940s, resultinginrathereffectivebehavioralcontroloveragitatedpsychoticpatientsbutatgreathumancost Many, ifnotmost,lobotomizedpatientswerereducedtoanergic,passive,andemotionallydeadhumanbeings.
Electroconvulsive treatment, conversely, was quite effective in certain groups of patients, such as those with psychotic depressive disorders. However, early methods of administration were fraught with dangerous complications and side effects, and ECT was used on a widespread basis, indiscriminately Many patients were treated with it inappropriately and did not respond (As shall be discussed later, in recent years significantadvanceshavebeenmadeinECT,anditnowaffordsahighlyeffective,safetreatmentforselected typesofpatients)
Most severely ill patients in the late nineteenth and early twentieth centuries continued to be housed in
overcrowded state mental hospitals and were “treated” using tried and true methods of the day: seclusion, restraint,andwet-sheetpacks Althoughseeminglyinhumaneprocedureswereemployed,itmaybeimportant to consider that the psychiatrists of that era were relatively helpless in the face of very severe mental illnesses and that these approaches (although certainly misused at times) reflected their attempt to reduce the horrendoushumansufferingseeninthousandsofseverelyillpeople
NewDiscoveries
In the 1950s, three new discoveries heralded the beginnings of a new interest in biological psychiatry Interestingly, these three areas of investigation were conducted by separate groups of researchers, each with littleknowledgeoftheworkbeingdonebytheircolleagues(Kety1975).
THORAZINEANDOTHEREARLYPSYCHOTROPICDRUGS
ImmediatelyafterWorldWarII,medicalresearchersandchemistsworkingforpharmaceuticalcompanies were trying to develop a drug that would reduce the complications associated with shock following major surgery In early 1951, a compound initially labeled #4560 RP was developed and testing with surgical patients was begun (Spiegel and Aebi 1989). The initial results were encouraging. Given preoperatively, it relaxed patients, somewhat reduced postoperative shock, and proved to be a good antiemetic (preventing postsurgical nausea) The finding that it produced noticeable sedation came as a surprise In the aftermath of field trials with surgical patients, the pharmaceutical company Laborit decided to try this medication with restless, agitated psychiatric patients to help improve sleep, totally unaware that the drug would prove to have morewidespreadeffectsonthepsychiatricpatientswhoweretested
Initialclinicaltrialsfirstreportedin1952resultedinmarkedbehavioralchangeswhengiventomanicand schizophrenicpatients Notonlydiditproduceacalmingeffect,butafteraperiodoftimeitactuallyappeared to reduce psychotic symptoms, such as delusions and hallucinations. Additional studies were carried out the following year, and by 1954 the drug was approved for use The new medication was given the generic name chlorpromazine;intheUnitedStatesitwasmarketedunderthebrandnameThorazine Itreceivedimmediate acceptance, and by the end of 1954, for the first time ever, there was a marked decrease in the number of patientsincarceratedinstatementalhospitals:thefirstmajorbreakthroughinpsychopharmacology
Otherpsychotropicmedicationswerediscoveredduringthe1950s.Thefirstantidepressantwasdeveloped in 1952 (iproniazid, an MAO inhibitor), although clinical studies in humans did not take place until 1956 The first tricyclic antidepressant, imipramine (Tofranil), was developed in 1954 and entered the market in 1957. The first minor tranquilizer, meprobamate, was released in 1955, followed shortly by the safer benzodiazepine, chlordiazepoxide (Librium), in 1958 Finally, lithium carbonate, originally used as a sedative by J. Cade in 1948, began to be used to treat bipolar disorder (formerly called manic-depressive illness) in the early1960s.
It is interesting to note that most of these psychopharmacological discoveries were accidental; that is, the drug companies were developing medications to treat other medical illnesses and just happened to find that the drugs could affect psychiatric symptoms Also, these discoveries were made empirically; they were not developed as an outgrowth of a particular theory of neurochemical dysfunction, nor was the mechanism of
actionatallknown Whatwasevidentwasthatthemedicationsworkedandwerefarsuperiortoanyprevious treatmentsforseverementalillness
THESYNAPSEANDNEUROCHEMICALTRANSMISSION
Although C S Sherrington inferred the existence of the synapse (the small space separating individual nerve cells) as early as 1906, the specific details of synaptic transmission were not fully understood for many decades thereafter Sherrington’s ideas involved a sort of telephone switchboard model of the nervous system, and neuronal messages were assumed to be transmitted via electrical stimulation It was not until the 1950s that neuroscientists realized that communication between nerve cells, although partially electrochemical in nature, is largely due to the release of chemical substances These chemicals, which transmit messages from one nerve cell to another, are referred to as neurotransmitters; other chemicals that play an indirect role in neurotransmissionarecalledneuromodulators.
Withthisdiscovery,itbecamepossibletoimaginethatcertainneurologicdysfunctionsmightbecausedby chemical irregularities, and that therefore it might be possible to develop drugs that could influence or alter neurotransmitterfunction
GENETICSTUDIES
The third line of investigation involved both genetics and studies of familial patterns of mental illness The earliest research in this direction was ultimately criticized for numerous methodological flaws Yet some of the basic findings proved to be fundamentally correct. There is a strong genetic loading for certain mental illnesses, in particular for schizophrenia and bipolar disorder. (In recent times evidence has been obtained revealing genetic loadings for a number of mental disorders, although clearly the strongest evidence exists for bipolardisorder,attention-deficit/hyperactivitydisorder,andsometypesofschizophrenia.)
Controversy
By the early 1960s then, it had been discovered that synaptic activation is chemical in nature; certain illnesses seem to be genetically passed on from generation to generation (and genetic factors are expressed biochemically); and newer drugs could significantly reduce psychiatric symptoms The triangulation of this data provided rather strong support for a renewed interest in biological psychiatry. There was new hope for the millions of patients suffering from serious mental illness, and psychiatry had begun to step back into “real medicine”again
However, despite the advances, these new treatments were plagued by a host of side effects some unpleasant, some actually dangerous These potent drugs were also often overused or were misused in certain treatment settings. Consequently, controversy began to arise, both among professionals, and in the lay public andmassmedia
Research studies and clinical experience certainly influence prescribing practices. However, in recent years the media has had a profound effect on publicopinionandultimatelyonclinicalpractice
In the late 1980s, negative attention was focused on the drug Ritalin (methylphenidate), a widely prescribed stimulant used in the treatment of attention-deficit/hyperactivity disorder (ADHD). Andrew Brotman, summarizing the work of Safer and Krager (1992), states, “The media attack was led by major national television talk show hosts and in the opinion of the authors, allowed anecdotal and unsubstantiated allegations concerning Ritalin to be aired There were also over twenty lawsuits initiated throughout the country,mostbyalawyerlinkedtotheChurchofScientology”(Brotman1992, audiotape).
In a study of the effects of this negative media and litigation blitz, conductedinBaltimoreCounty,Maryland,SaferandKrager(1992)foundthat the use of Ritalin had dropped significantly From 1981 through 1987, the use of Ritalin had increased fivefold However, in the two-year period during and just following the negative media attention, there was a 40 percent decrease in prescriptionsforRitalin Andthisdecreaseoccurredatatimewhenresearchon ADHD and stimulant treatment continued to strongly support the safety and efficacy of such medications. The authors go on to state that 36 percent of children who discontinued Ritalin experienced major academic maladjustment (such as failing grades or being suspended), and an additional 47 percent who discontinued encountered mild to moderate academic problems. Concurrently, as Ritalin use (especially new prescriptions) decreased, there was a significant (fourfold) increase in the prescription of tricyclic antidepressants among ADHD children. It is important to note that tricyclics, although often used to treat ADHD, tend to have more troublesome side effects than Ritalin, and have been implicated in six reports of cardiac fatalities Brotman (1992) concludes,“Whentherearereportsinthemediathatleadtostigmatizationofa certain drug there tends to be a move to other medications which have less notoriety,eveniftheymay,infact,bemoreproblematic”
More recently, following wide acclaim as a new “breakthrough drug for depression” (Cowley et al 1990), Prozac (fluoxetine) came under attack by consumergroupsand,again,theChurchofScientology Thenegativeattention was sparked by a single article (Teicher, Glod, and Cole 1990) documenting the emergence or reemergence of suicidal ideas in six patients treated with Prozac Thesixpatientshadbeendiagnosedassufferingfromseveredepressive disorders, and in no case were there actual suicide attempts following the onset of treatment with Prozac But suddenly Prozac was thrust into a very unfavorable light and was the next drug in line to find itself the topic of televisiontalkshows.
Subsequent studies have failed to find any evidence that Prozac is more likelytobeassociatedwithsuicidalfeelingsthananyotherantidepressant(Fava and Rosenbaum 1991; Beasley and Dornseif 1991) In fact, in one study the incidence of suicidal ideations was greater in patients treated by placebo or imipramine (a tricyclic antidepressant) than by Prozac (Beasley and Dornseif 1991)
The Church of Scientology attempted to convince the Federal Drug Administration (FDA) to pull Prozac from the market However, the FDA ruled against taking such action because there was no scientific evidence to supporttheclaimsmadebytheChurchofScientology(Burton1991)
All medications produce some side effects Reports of adverse effects, even if very infrequent, must be taken seriously and investigated systematically There is a place for skepticism and scrutiny. However, one must consider the negative effect of unsubstantiated reports in the lay press For example, the risk of Prozac-induced suicide appears to be extremely low, and the suicide rate in untreated major depression is reported to be 9 percent. Clearly, failure to treat carriesthegraverrisk
ItisverylikelythatmanyseriouslydepressedpeopleandparentsofADHD children have been understandably, and unnecessarily, frightened by negative, sensationalistic reports in the media To quote Brotman (1992) again,
“Pharmacotherapydoesnotexistinasocialandpoliticalvacuum.”
PROFESSIONALDISSENTION
Within professional ranks, debate issued from two fairly discrete theoretical camps: those who were promedication and those who were pro-psychotherapy Each group amassed impassioned arguments not only infavorofitsownpointofview,butalsoagainsttheotherschoolofthought,assetoutbelow.
PROMEDICATION (ANTIPSYCHOTHERAPY) ARGUMENTS IN FAVOR OF MEDICATION TREATMENT AS THE TREATMENTOFCHOICE:
Because of its quantifiable nature that is, the ability to monitor dosage medication treatment can bestudiedmuchmoresystematicallythanpsychotherapy.
Medicationsactquicklytoreducepainfulanddebilitatingsymptoms
Thequickerresponseseenwithmedicationscanhelptorestorehopeandreducedemoralization
Treatment with medications can be conducted in a much more systematic and standardized fashion, whereaspsychotherapyreliesheavilyontheindividualskillofthepsychotherapist.
Rapid and effective symptom relief can potentially reduce suffering to such an extent that the patient is better able to engage productively in psychotherapy Likewise, the reductions of drive strength afforded by some psychotropic medications may operate to free up more psychic energy, which could thenbechanneledintoadaptiveegofunctions.
Medicationscanprovidehelptopatientswhohavelimitedintellectualcapacity,pooregostrength,or both;thatis,drugsmaybeeffectivewithpeopleforwhompsychotherapyisinappropriate
Psychotherapy is often prolonged and expensive, may be unavailable to many people, and is of unproveneffectiveness(thiswasthecaseespeciallyinlightoftheverylimitedpsychotherapyoutcome studies available in the 1950s and 1960s) Thus medications are much more cost-effective and more readilyavailabletothegeneralpublic.
Finally, those strongly wedded to a biochemical model of psychopathology contended that social, behavioral, and psychological approaches simply could not correct the underlying biologic abnormality responsibleformajormentalillnesses.Recentstudies,however,havecastdoubtonthishypothesis.
PRO-PSYCHOTHERAPY (ANTIMEDICATION) ARGUMENTS IN FAVOR OF PSYCHOTHERAPY AS THE TREATMENTOFCHOICE:
Only psychotherapy, not medications, can address the complexity of human psychological functioning Medicationsonlytreatsymptoms,whereaspsychotherapyfocusesonthewholepersonor
psyche.
Psychotherapy aims toward personal growth and autonomy, whereas drugs are likely to foster dependency,eitheronthedoctororonthedrugitself
Drugs can interfere with autonomy and expressions of free will, whereas psychotherapy honors these processes The prescription of medications may, at least at an unconscious level, communicate the message that the drug will do the work, you don’t have to (Numerous documented instances of overuseoftranquilizingmedicationstoachievebehavioralcontrolprovidedfodderforthisargument.)
Medicationsmayreduceanxietyandotherformsofsufferingtosuchanextentthatpeoplewillbeless motivatedtoengageinpsychotherapy
Manydrugshaveundesirableordangeroussideeffects,andsomecanleadtodependenceandabuse
Medications ultimately do not solve problems, teach adaptive coping skills, mend broken hearts, or fillemptylives(Menninger1963)
Althoughthisdebatecontinuedthroughoutthe1960sand1970s,clearlytherewerealsoanumberofwhat G L Klerman (Beitman and Klerman 1991) calls “pragmatic practitioners” those mental health professionals who used whatever approaches seemed to work. Certainly it was, and is, reasonable to consider thatsomedisordersarebesttreatedbypsychotropicmedications,othersbypsychotherapy,anditoftenmakes sensetouseacombinationofbothmodalities
PUBLICOPINION
A parallel to the professional debate began to occur within the general public. In institutes of higher education, the humanistic movement began to permeate not only departments of psychology but the global academic community as well The post-McCarthy social climate was ripe for new attitudes that challenged political and social control and applauded the expression of free will, self-expression, and self-actualization. Reports began to surface regarding the abuse of psychiatric medication by the medical profession Opponents to drug treatment accused the psychiatrists of using medications to achieve control The term “chemical straitjacket”becamepopularized.
The1970ssawtheproliferationofnewtranquilizers,andpharmaceuticalcompaniesreapedfortunesfrom thesaleofwell-knownpillssuchasValiumandLibrium.Thevastmajorityofprescriptionswrittenforminor tranquilizers (more than 90 percent) were written by family practice doctors, not psychiatric specialists The “drugged state” was the fastest growing state in the union (Bly 1990) The inappropriate use and abuse of tranquilizersgainedincreasingpublicattentionandevenfounditswayintopopularsongs(theRollingStones’ “Mother’sLittleHelper”)andmovies(I’mDancingasFastasICan)
Inthe1960s,theChurchofScientologywassuccessfullysuedbytheAmericanPsychiatricAssociation.In retaliation, it began a long, embittered assault on American psychiatry Initially the Church of Scientology launched a negative campaign against the use of Ritalin, a psychotropic medication used to treat attentiondeficit disorder. More recently it has orchestrated a move to shed negative light on the antidepressant Prozac
(seeboxonpage8).
Biological psychiatry was under attack. Although clearly there was a good deal of abuse and misuse of psychoactive drugs, there also continued to be decreasing numbers of people living in mental hospitals, and drug companies were at work developing newer and “cleaner” psychotropic medications, medications with fewersideeffects.
Rapprochement:BiologicalandPsychologicalPerspectives
During the 1980s, a shift began in which increasing numbers of mental health practitioners and researchers widened their previously narrow views on etiology and treatment of mental illness Increasingly, it became recognized that unidimensional models, whether psychological or biological, fell short of explaining the tremendous complexities of human psychological functioning and psychopathology. This transition to morecomplementaryandintegratedviewsofcauseandcurecanbeattributedtoseveralnewdevelopments:
Psychopharmacologyandthe“ManagedCare”Dilemma
Since the advent of newer-generation psychotropic medication, many millions of people are receiving more effective treatment for a host of psychiatric conditions. For this we are grateful. However, it also has become abundantlyclearthattheeffectsofpsychiatricdrugsarelimited Underthebest of all circumstances such treatments do not have an impact on all aspects of psychologicalsuffering.
In our view, successful psychiatric treatment should always include psychotherapy. Only in the context of a healing relationship may many aspects of psychological dysfunction be adequately addressed Numerous interpersonal, intrapsychic, spiritual, and existential dimensions of human functioning simply arenotamenabletopharmacologictreatment.
Inthisbookweacknowledgethemanybenefitsofdrugtreatment;however, we must also share a concern: In these days of cost containment and managed care, individual human lives and quality-of-life issues are often ignored It is a real concern that an automatic, knee-jerk reaction will be just to prescribe pills,
whensomuchmoreisneeded.Wearetreatingpeople,notjustnervecells.
However, given the rising cost of pharmaceuticals, the most recent costcontainmentstrategiesareaslikelytofocusontheuseofpsychiatricmedication as well as on psychotherapeutic interventions Paradoxically, perhaps as psychotropic drugs begin to account for an ever-increasing percentage of total health care expenditures, we will see best-practice guidelines influenced in a waythatwillsupportpsychotherapy
We hope that critical questions will be raised Are medication treatment failures completely an effect of the drugs not working? Or could the relative lack of psychotherapeutic modalities be a contributing factor? Similarly, as the prescribing of psychotropics has become the first step in treatment, has that firststepbeentakenbeforeanaccuratediagnosiswasmade?Arewemedicating out of habit, when it is not really indicated? If the patient would benefit more frompsychotherapy,arewedoingmoreharmthangood?
We remain hopeful that the pendulum will swing back to support what most practicing clinicians know to be true: the best outcomes result from appropriatelybalancedtreatmentthatincludestherapyandmedications.
Human beings and their life problems are enormously complex. And it is the highly trained clinician who must ultimately decide which combinations of treatments are best suited for each individual client (not insurance companies, treatmentmanuals,oruntrainedtechnicians)!
The side effects of medications historically resulted in very poor compliance rates among psychiatric patients, and the most effective medication available is useless if the patient doesn’t take the drug as prescribed Compounds introduced in the 1980s and early 1990s have yielded effective medications withmuchmoreuser-friendlyside-effectprofiles.
Discoveries have been made in which new medications and newer uses for existing medications
provide very good results in treating certain types of mental illnesses, such as panic disorder and obsessive-compulsive disorder This greatly increases the psychiatrist’s arsenal of effective medications.
A growing body of well-controlled research studies (double-blind, randomized, placebo-controlled) lendconvincingsupporttotheefficacyofpsychotropicdrugs
Neuroimaging techniques, such as PET and SPECT scans, allow researchers to view metabolic activity in the living brain. These technologies have been able to isolate localized brain abnormalities in certain mental disorders, including major depression, schizophrenia, ADHD, and obsessivecompulsive disorder They can provide data on particular sites of drug action or binding, and can illustrate changes between the pre- and post-treatment status of particular brain structures. Imaging techniqueshaveaddedconsiderable“harddata”tovarioustheoriesofbiochemicaletiologyinselected mentalillnesses
Neuroimaging techniques have been accompanied by a host of new laboratory procedures that allow neuroscientists to assay the neurochemical by-products found in spinal fluid. Although early psychopharmacology was implemented without any real knowledge of the underlying pathophysiology,inthepastdecade,biochemicaltheorieshavegainedscientificsupport
These new developments in psychiatry and the neurosciences have been hard to ignore. Many formerly hard-linepsychotherapistshavebeenwonoverbythefloodofresearchfindingsandtheirpersonalexperiences intreatingpeoplewithpsychoactivedrugs
During this same period, important advances were made in the theory and practice of psychotherapy During the late 1970s and 1980s the first truly well-controlled psychotherapy studies emerged (including the now popular meta-analyses). The results of these studies cast doubt on the findings of early research that had suggested that psychotherapy was ineffective (Eysenck 1965, for example) Of the many forms of psychotherapy that have been developed, the meta-analyses suggest that no single school of therapy is clearly superiorandthatpsychotherapiesacrosstheboardareoftenmuchmoreeffectivethannotreatment.
Also during this time we witnessed the development of novel treatment approaches, such as cognitive behavioral psychotherapy (Beck 1976) and interpersonal psychotherapy (Klerman et al. 1984) as a treatment forparticulardisorders,suchasdepressionandpanicdisorder Theseapproacheshaveappeal,inthattheycan be somewhat systematically applied (some even provide “canned” formats or “cookbooks”). Also, the methodology is a bit less reliant on the personal characteristics of the therapist. These approaches then lend themselves to a short-term format and can often be conducted in groups And, finally, these psychotherapies can be more easily studied. Both cognitive behavioral and interpersonal psychotherapies have a solid track recordofeffectiveness(asisdiscussedfurtherinthenextchapter).
Finally, both clinical-anecdotal and research studies have emerged that support the combined use of pharmacotherapy and psychotherapy in the treatment of particular disorders At times, the combined treatmentshavebeenshowntobesuperiortoeithersingletreatmentalone
For many in the mental health community, the writing on the wall has become far more legible: A single
modelforunderstandingandtreatingmentaldisordersistoonarrowandissimplyinadequate Asweshallbe discussing in subsequent chapters, current evidence suggests that particular disorders do respond best to certain medical treatments, and for these, medications are the treatment of choice. Other disorders have little to do with biochemical dysfunction, and medications play little or no role in their treatment. And still other disordersrequiretheskillfulintegrationofbiologicalandpsychotherapies
As the saying goes, when you only have a hammer, every problem looks like a nail Fortunately, at the present time, mental health professionals have access to a “toolbox” of approaches that can, if employed appropriately, dramatically increase our effectiveness in reducing emotional suffering and promoting mental health
WhyLearnAboutPsychopharmacology?
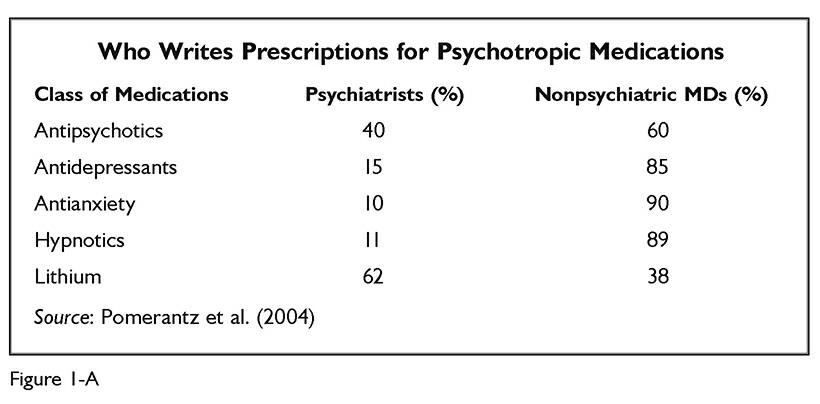
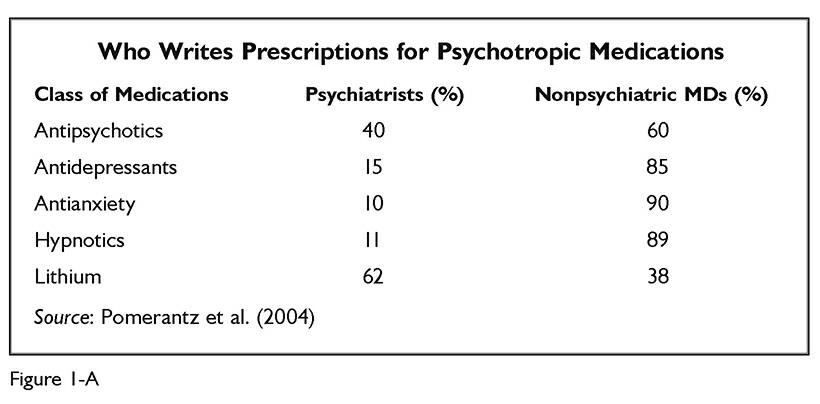
In the United States, the majority of mental health services are provided by nonmedical therapists Likewise, the majority of prescriptions for psychotropic medications are written by family practice and primary care physicians (see figure 1-A). Thus, even though psychiatrists represent the branch of medicine that specializes in psychopharmacology, they are directly responsible for providing only a fraction of professional services to the mentally ill Consequently, it is becoming increasingly important for all mental health clinicians to have a basicfamiliaritywithpsychiatricmedicationtreatment.
Many nonmedical psychotherapists are or will become strongly and rather directly involved in medication treatment. In some settings psychologists and social workers assume a major role in monitoring client responses to psychotropic medications As primary therapist, these practitioners are in most frequent contact withclientsandareinthebestpositiontoobservesymptomaticimprovement,side-effectproblems,andissues involvingmedicationadherence.Whenconsultingwithprimarycarephysicians,orasastaffmemberinsome HMO settings, nonmedical therapists who are well-versed in the use of psychiatric medications can play an active(albeitcollaborative)roleinrecommendingparticularmedicationsanddosageadjustments Inaddition, the Department of Defense, in response to an inadequate number of psychiatrists available in the military, implemented a program to train a small number of psychologists so that they are able to prescribe a limited formulary of psychiatric medications Currently, properly trained psychologists can become licensed to prescribepsychiatricmedicationsinthestatesofNewMexico,Illinois,andLouisiana.Thesevariousactivities reflectquitedirectinvolvementinmedicationtreatmentbynonmedicaltherapists
In contrast, many nonmedical therapists have little to do with drug treatment. In some cases this may be duetothenatureoftheirpositioninaparticulartreatmentsetting;inothersitmayhavemoretodowiththeir own preferences and biases, such as opposition to medication treatment However, we believe that, regardless of the degree of involvement and interest in medication treatment, it is increasingly important that all mental healththerapistsbecomeacquaintedwithsomebasicnotionsregardingpsychopharmacology.
Convincing evidence now exists that certain mental disorders are either caused or accompanied by
neurochemical abnormalities The failure to appropriately diagnose and medically treat such conditions can result in the use of ineffective or only partially effective treatments and hence in prolonged suffering Aside from the obvious cost in human terms, prolonged inappropriate treatment results in excessive financial burdensforclients,theirfamilies,andthehealthcaresystem.
In addition, to date there have been successful malpractice suits brought against therapists who failed to treat or refer for treatment patients suffering from particular disorders known to be generally responsive to medication
All mental health professionals must be able to, at the very least, diagnose mental disorders that require psychotropic medication treatment so that appropriate referrals can be made Differential diagnosis will be discussedindetailinthisbook.
In many cases, clients may not choose to see a psychiatrist, even when told by their therapists that medication treatment is indicated. This may be due to financial concerns or to the negative stigma some people believe is attached to psychiatric treatment A viable alternative, in some cases, is referral to the family practice doctor Many people suffering from emotional distress see their family physician first This doctor maybegintreatmentwithpsychotropicmedicationsandmayalsoreferthepatientforpsychotherapy.Insuch cases, the nonmedical therapist may be in a key position to supply information regarding diagnosis and treatment response Increasingly, family practice physicians and nonmedical therapists become partners collaborating on the treatment of many clients especially those suffering from fairly uncomplicated depressiveandanxietydisorders
Effective consultation with family practice doctors and psychiatrists alike is enhanced by the nonmedical therapist’s ability to accurately communicate and discuss diagnosis, target symptoms, presumed etiology, and possible treatments. We hope this book will provide a solid grounding in basic issues to help improve communicationandcooperationbetweenprofessionals.
Mental health treatment has moved increasingly toward greater acceptance of multidisciplinary and integrated treatment modalities As sophistication in the diagnosis and medical treatment of mental disorders continues to develop, it will be important that mental health professionals not take a step backward The polarization of models and professional “turf battles” of the 1960s and 1970s may have sparked useful and lively debate, but they also often resulted in a fragmentation of care Ongoing knowledge of and respect for diversemodelsandcollaborativeinvolvementholdpromiseforincreasinglyeffectiveeffortsintreatingmental illness. If you are an instructor interested in using this book in courses you teach, visit http://wwwnewharbingercom/39256forclassroomadoptionresources
IntegratedModels
The decision about whether to use psychotropic medications in the treatment of psychiatric disorders is influenced by a number of factors Unfortunately, often the decision is based largely on the clinician’s a priori viewtowardtreatment,derivingfromhisorhertheoreticalperspective Asweshallargue,thecriticalvariable in this decision is more appropriately based on the diagnosis, and in particular on the presence or absence of keytargetsymptomsthatsuggestthepatientisexperiencingsomeformofneurochemicaldisorder
Inbroadandextremelyheterogeneousgroupsofdisorders,suchasmooddisorders,somemaybelargelyor exclusively caused by biological factors Other disorders in such groups share some symptoms with biologicbased mental illness, yet their etiology stems largely or exclusively from nonbiologic sources, for example, emotional, psychosocial, or cognitive sources. Thus a very important question to address when making a diagnosis and subsequent decisions about treatment is, “Is there any evidence to suggest that this person ’ s problemsareduetosomeformofbiologicdisturbance?”However,alltoooftenthisquestionisframedoverly simplistically:“Isthedisorderbiologicalorisitpsychological?”
The distinction between what is psyche and what is soma is ambiguous at best Invariably, there is a complex interaction between psychological and biological factors in all cases of emotional disorder. This complexitywillbethefocusofthischapter
PsychologyandBiology:ATwo-WayStreet
Acomprehensivediscussionoftheclassicphilosophicalissue,mind-braindualism,isbeyondthescopeofthis book (The reader is referred to Goodman 1991; Young 1987) However, we would like to highlight a small numberofcasesandresearchstudiesthatillustratetheinteractiveeffectsofbiologicandpsychologicfactors.
BiologicalFactors’ImpactonPsychologicalFunctioning
Menoughttoknowthatfromthebrain,andfromthebrainonly,ariseourpleasures,joys,laughter,andjests,as wellasoursorrows,pains,griefs,andfears….Itisthesamethingwhichmakesusmadordelirious,inspiresuswith dreadandfear,whetherbynightorbyday,bringssleeplessness,inopportunemistakes,aimlessanxieties, absentmindedness,andactsthatarecontrarytohabit
Hippocrates
Forthepasttwothousandplusyears,therehasbeenatleastrudimentaryrecognitionofthebrainasthesiteof reasoningandemotions
Early physicians were keen to note that brain injuries could result in profound changes in personality, cognition, and emotional control. And, as noted in chapter 1, in the earliest days of modern psychiatry the fieldwasgroundedinbiologicalsciencesandthemedicalmodel
Twofairlycommonclinicalexamplesserveasillustrationsofhowdisorderedbrainfunctioningcanleadto markedpsychiatricsymptomatology
CASE1
RobertB isaforty-two-year-oldstockbroker Hehasalwaysbeenanambitious,bright,energeticman Despite normalstressesofdailylife,hehadneverexperiencedmajorpsychiatricproblemsuntilamonthago Forno apparentreasonhebegangraduallytoslipintoastateoflethargy,fatigue,andlowmotivation.Hisnormalzest forlifediminished,hisusualsharpnessofwitbecamedull,andhissenseofenthusiasmgavewaytoincreasing blandnessandemptiness Hewastotallyperplexedashesearchedhisrecentlifeexperiencestofindthecauseforhis malady.Nonewastobefound.
Intheensuingweekshelostweight,frequentlywokeat3:00AM andwasunabletogobacktosleep,and lostallsexualdesireforhiswife.
Uponcloseinvestigationbyhisfamilyphysician,itwaseventuallydiscoveredthatthedepressivesymptoms beganseveralweeksafterhehadstartedtakinganantihypertensivedrugtotreathishighbloodpressure The medicationwassuspectandwaseventuallychanged Withinacoupleofweeks,thedepressionvanished
Thiscaseillustrateshowamedicationcan,attimes,dramaticallyalteraperson’sbrainchemistry,resulting in major psychiatric symptoms. In Robert’s case, there was no evidence of long-standing psychological problemsandnoclearpsychologicalstressors
Thebraincanbeseen,inasense,asatremendouslycomplexbiologicalecosystem.Asinotherecosystems, global functioning and survival depend on a large number of interrelated variables At times, small changes in oneaspectofthesysteminfluenceanumberofothervariables inessence,sendingarippleeffectthroughout the entire system. In the brain, often certain delicately balanced neurochemical systems can be altered (the term often used is dysregulated), resulting in a cascade of alterations affecting many other neurochemicals and thefunctioningofahostofbrainstructures.Adrug,asintheexampleabove,isbutoneofmanyvariablesthat can result in neurochemical dysregulation and resulting psychiatric symptoms. (More will be said about other causeslaterinthechapter)
CASE2
ElizabethM isasixty-eight-year-oldretiredaccountantwhosepassionisgardening However,duringthepast threemonthsshebecameunabletotendhergardenformorethanafewminutesatatime.Shewasalmost constantlyseizedbytremendousrestlessnessandagitation,fretting,wringingherhands,andpacingabouther house “IfeellikeIamgoingtocrawloutofmyskin,”shesaid Elizabethlosttwenty-fivepoundsoverthisthree-monthperiodandsufferedfitfulsleep Shealsobeganto contemplatesuicide Herhopesforawell-deserved,peacefulretirementseemedtohavebeenerased,asifshewere plaguedbysomekindofcurse.Shecouldpinpointabsolutelynopainfullifeeventsthatmightgivemeaningtoher condition
Fortunately,ultimatelyitwasdiscoveredthatshewassufferingfromhyperthyroidism.Followingsuccessful treatment,shehasbeenabletoreturntohergardenandherlife
In this case, a metabolic disorder was the culprit In the cases of both Robert and Elizabeth, neurochemical and hormonal factors grossly interfered with brain functioning. In both cases, the people were radically changed Their perceptions were altered (pessimism, hopelessness), their sense of self was shaken, their emotions were out of control, and their physiological functioning had been derailed Certainly they had strong emotional reactions to these changes (a phenomenon sometimes referred to as secondary emotional symptoms);however,inbothcasestheprimaryetiologywasbiological
Allmentalhealthclinicianswillencounterclientswhopresentfortreatmentwithpresumedpsychological problems but who, in fact, are suffering from biologically based disorders Such disorders fall into three categories:
Duetomedicalillnesses(suchashyperthyroidism)
Duetodrugs(prescribed,over-the-counter,orrecreational)
Endogenousmentalillnesses1
PsychologicalFactors’ImpactonBiologicalFunctioning
For a very long time there has been some vague notion that emotional stress can affect physiology. For example, for hundreds of years it has been noted that severe stress can lead to disease Family physicians have
long noted that in the wake of tragic losses, the bereaved easily fall prey to illness Yet not until this century did the psychology-biology interaction begin to be explored Psychosomatic medicine was ushered in by the pioneering work of Franz Alexander in the 1940s. And an explosion of interest and research has been seen in the 1980s and 1990s in the emerging field of psycho-neuro-immunology the study of the effects of emotionalfactorsondiseasesusceptibilityanddiseaseresistance
1. The term endogenous means “arises from within.” Certain psychiatric disorders have been found to be largely endogenous; that is, they arise spontaneously in the absence of provoking psychosocial stressors The disorders can be attributed to a biological abnormality or a predispositionorvulnerabilitytodysfunction Manyoftheso-calledendogenousdisordersappeartocarryageneticloading:theyarepassed from generation to generation and presumably can be linked to certain genetic factors More will be said about endogenous psychiatric disordersinsubsequentchapters
It would require several textbooks to even begin to review the literature in psychosomatics and psychoneuro-immunology Wewould,however,liketobrieflydiscussafewstudiesthatshedsomelightontheissue of the interaction of psychology and biology and its relationship to mental illnesses. The first two of these studiesinvolvedexperimentationwithanimals
E Kandel and colleagues have studied the effects of environmental experiences and learning on the nervous system in the Aplysia (a marine mollusk). This animal is well suited for such a study because its nerve cells are quite large and easy to visualize. Also, it does respond well to learning experiments suchashabituation,sensitization,andclassicalconditioning(Pinskeretal 1970)
The researchers were able to trace neural pathways from touch receptors in the mollusk’s gill and siphon, through its primitive nervous system, and out into corresponding motor neurons. Using repeated exposures to mild aversive stimuli, the investigators were able to document specific biochemical changes at the synapse, as well as structural changes in specific nerve cells. Conclusion: environmentaleventsandlearningareactuallyaccompaniedbymeasurablechangesinnervecells;the animal’sbiologyisaltered
Neurologic changes have similarly been demonstrated in studies of learned helplessness in rats In these classic studies, animals are exposed to extremely aversive conditions, from which they have no escape After a period of exposure, the animals begin to exhibit marked behavioral changes: They become passive and immobile And they fail to mount coping responses (escape) from later aversive situations from which escape is possible. In many respects, the animals have learned that they are helpless to respond, and then they come to take on characteristics that resemble major depression in humans Interestingly, not only do these helpless rats behave in a depressed manner, but their biochemical functioning is altered. Measures of brain chemistry reveal neurochemical alterations that are identical to those seen in humans suffering from severe grief reactions or clinical depression Again, environmental experiences have modified brain functioning (Weiss, Glazer, and Pohorecky 1976).
In very similar ways, in numerous studies the biochemistry of people with reactive depressions has been shown to be markedly altered For example, emotionally healthy individuals without a personal or family history of depression who encounter major psychosocial stressors (especially losses) can become depressed Presumably such people are not especially at risk (biologically or psychologically)
for depression, but nonetheless they become depressed in response to significant stressful events. Further, in the course of their reaction, some patients develop not only emotional symptoms (sadness, pessimism, low self-esteem) but also a host of biologic symptoms, such as sleep disturbances and marked biochemical abnormalities. The chemical dysfunctions include dysregulation of both neurotransmitters in the brain and hormones (for instance, adrenal hormones such as cortisol) Metabolic by-products of neurotransmitters have been measured in assays of spinal fluid and by way ofbrain-imagingtechniquessuchasPETandSPECTscanning.
Baxter et al (1992) have convincingly demonstrated that psychotherapy can affect brain functioning PET scans allow researchers to directly image living brain tissue and thus provide data on metabolic activityofspecificareasofthebrain.StudiesusingPETscansinsevereobsessive-compulsivedisorder reveal a localized brain abnormality: a metabolic disturbance in the head of the caudate nucleus, a brainstructurethatispartofthebasalganglia Inobsessive-compulsivedisorder,whenindividualsare symptomatic, this abnormality is visible on PET scans. Yet following successful behavioral treatment (exposureandresponse-preventiontreatments)thefunctioningofthisbrainareanormalizes
Evidence also exists supporting the theory that the earliest episodes of affective illnesses in bipolar patients are often “reactive” in nature; that is, the initial episode is not an endogenous, biologic event butratherisevokedbypsychologicalstressors Asaconsequenceoftheinitialepisode,neuronsinkey areas of the limbic system may undergo a process of modification (neurochemically and even structurally), whereby the brain is changed more or less permanently. The result of this is that, following the first one or two episodes, the altered brain functioning leaves the nervous system at much greater risk for subsequent episodes and sets in motion an endogenous process whereby affectiveepisodescanthenoccurspontaneously,evenintheabsenceofpsychologicalstress.Fromthat point on, if the disorder is not controlled, each episode further affects the nervous system; the threshold for recurring episodes becomes progressively lower This process is known as kindling It beginsasaresponsetoexternalstressorsandevolvesintoalargelybiologicalillness.
These are but a few of many studies and clinical findings that collectively provide strong support for the ideathatenvironmentalandpsychologicalfactorscansignificantlyaffectbiologicandneurologicfunctioning
Biological-PsychologicalInteractions
It is very likely that complex, interactive effects exist between biological and psychological factors It’s neveraquestionofallornone InthecaseofRobertB,hewassufferingfromanendogenousdepressionand experiencing marked lethargy, poor concentration, and low motivation. This eventually led to performance problemsatworkandanumberofcriticalremarksfromhisboss Theseeventsbegantofueltheflameoflow self-esteem Low self-esteem is generally not felt to be a primary symptom of biologically based depressive disorders,butitisalmostuniversallyseentoemergeaspatientslivewithongoingclinicaldepression.
Biologiceffectsmaysecondarilyaffectpsychologicalfunctioninginanumberofways,amongthem:
Altered perception. Biologic effects can contribute to the pessimistic thinking seen in depressive
disordersandthetendencytoanticipatefearfuloutcomesoftenseeninanxietydisorders.
Increased emotional sensitivity and reduced emotional controls Increased emotional arousal or pain may motivate a person to become more socially withdrawn and can often lead to a host of negative conclusionsregardingpersonalcompetency,asin,“What’swrongwithme?I’mcryinglikeababy.”
Decreased energy and arousal, poor concentration, and lowered motivation, which often leads to impairedperformanceinschoolandwork
Sexualdysfunction,whichcantranslateintointerpersonalproblemsinintimaterelationships.
Bizarre behavior enacted during a manic or a psychotic episode. Such behavior can continue to be a sourceoftremendouspersonalembarrassmentandshamelongafterthepsychoticepisodeisresolved
These consequences of a primarily biologically based mental disorder have an impact on the individual’s sense of self-worth and competency in the world. Conversely, this increased level of despair can, in itself, operatetointensifytheunderlyingbiologicalabnormality
PracticalImplications
As previously mentioned, the question “Is this disorder psychological or is it biological?” is too simplistic The more appropriate question is “To what extent is there evidence that biochemical factors may be contributing to a patient’s current symptomatology?” This is much more than an academic question. To the extent that we can determine biologic etiology (or at least a degree of biologic dysfunction as a part of the moreglobaldisorder),pharmacologictreatmentsmaybeindicated (Howabiologicetiologyandtheneedfor medicationaredeterminedisaddressedindetailinlaterchapters.)
Stimulus-ResponseSpecificity
Stimulus-response specificity is a concept describing conditions where a very specific response can be predicted with tremendous regularity when a stimulus is applied. One example would be that an electrical shock to muscle tissue evokes a contraction This model is appropriate for some types of medical interventions For example, for acute cardiac and respiratory arrest, the techniques of cardiopulmonary resuscitation (CPR) can be used with most victims, regardless of their age, socioeconomic status, sex, or religiousbeliefs Whenthereisanobstructedairway,performinganemergencytracheotomyisappropriatefor victimsregardlessoftheiremotionalstatus,personalitystyle,orlevelofpsychosocialmaturity Likewise,some medications have fairly universal effects on all people; for instance, sodium pentothal produces unconsciousness(Deckert1985)
Medical treatments in psychiatry generally do not follow the rule of stimulus-response specificity. Although the particular mechanism of drug action may be identified, the same medication given to two depressed patients, for example, may affect them very differently Some of these differences may be traced to variations in metabolism from individual to individual (see chapter 4). Or the underlying biochemical abnormalityinonedepressedpatientmaybedifferentthantheabnormalityinanotherdepressedpatient,and
thusthemedicationsaffectdifferentunderlyingdisorders
Beyondthesephysiologicaldifferences,however,thepatients’responsesmaybeinfluencedtoasignificant degree by a host of social, cognitive, and personality factors that have little or nothing to do with biology In the realm of psychiatric medication treatment, sociocultural experiences and beliefs, personality style, and a vast number of personal psychodynamic factors can, and do, dramatically influence patient response. Psychological functioning cannot be understood using the simple, reductionist notions implied in stimulusresponsespecificity
Thegoodclinicianalways treats the person, not just the disorder We may choose to influence nerve cells withpsychotropicdrugs,buttheresponsewillalwaysbewovenintothecomplexfabricofhighlyidiosyncratic personality factors. Therefore, successful pharmacologic treatment always requires a thorough knowledge of not only the diagnosis and pathology and the medications used, but the unique meaning of the treatment to the individual patient Assembly-line psychotropic treatment often fails, not because medications are ineffective,butbecausecliniciansdonottakethetimetounderstandtheirpatients.
Unfortunately, in many overcrowded mental health clinics, some clinicians act as if stimulus-response specificity is appropriate. The result is that often these attempts at treatment efficiency and cost containment backfire Many patients don’t respond well and either must demand further outpatient services or continue to decompensate until they require hospitalization And, of course, there is the human cost associated with prolongedsuffering.
In the remainder of the chapter, we explore a number of ideas regarding psychological factors that have directbearingontheoutcomeofmedicationtreatment