Structure, Function, and Diagnostic Approach to Skin Disease 1
Margaret A. Bobonich
Primary and nondermatology specialty care clinicians see the majority of patients with skin complaints on a daily basis. While patients make appointments to see their provider for a physical or blood pressure management, they commonly add an “Oh, by the way ” skin complaint. In contrast, many patients call the office or central scheduling and cite their reason for seeking treatment as a “rash.” This common, catch-all term reported by so many patients can leave the provider wondering what kind of eruption is really on the other side of the examination room door. Clinicians must be knowledgeable in evaluating skin lesions, which could range from skin cancer to a sexually transmitted infection.
Cutaneous lesions may represent more than just a skin disease and can be a manifestation of an underlying systemic process. Conversely, cutaneous conditions can cause systemic disease, dysfunction, and death. Psychosocial conditions can also be the cause or sequelae of skin conditions but are often negated. So in addition to maintaining competency in a primary specialty, clinicians need to acquire the essential knowledge and skills in dermatology—a daunting task given that there are almost 3,000 dermatology diagnoses.
The best approach for acquiring basic competency in the recognition and initial management of dermatologic disease (dermatoses) is to focus on conditions that are:
• High volume—the most common skin conditions seen in clinical practice;
• High morbidity—skin disease that is contagious or can impact quality of life or the community; and
• High mortality—life-threatening conditions that require prompt recognition.
This chapter outlines essential dermatology concepts, including anatomy and physiology, morphology of skin lesions and algorithmic approach for the assessment of any skin condition. This will enable clinicians to develop the knowledge and decision making skills for far more than the 50 most common skin conditions. Subsequent chapters provide a comprehensive review of hundreds of skin conditions that MUST be considered in a differential diagnosis, ensuring an accurate diagnosis and optimal patient outcome.
STRUCTURE AND FUNCTION
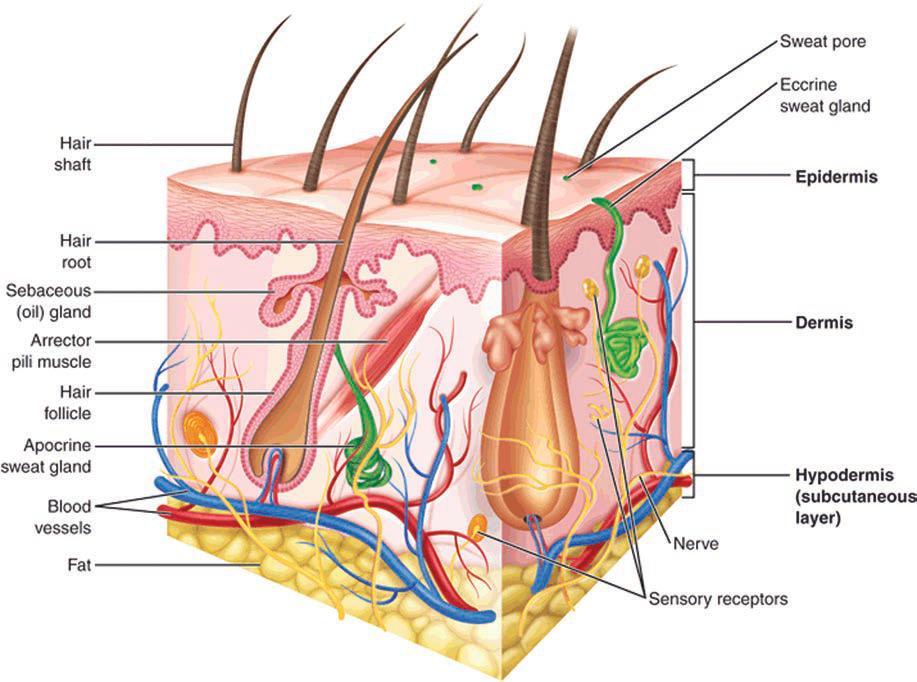
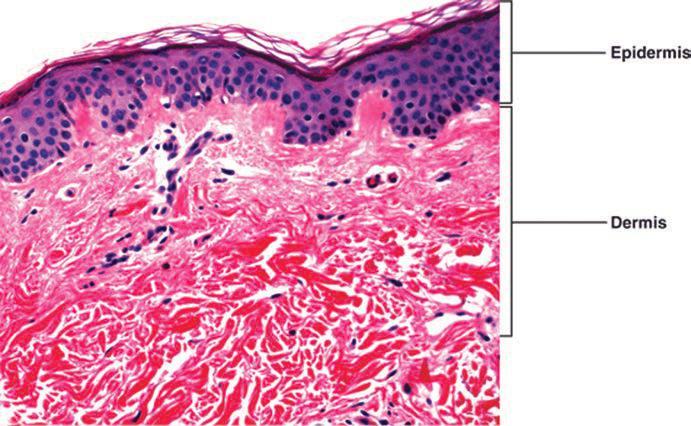
Understanding the normal structure and function of the skin enhances your ability to correlate clinical and histologic findings associated with skin lesions (Figure 1-1). The skin is not only the largest organ but also the most visible, allowing both patients and clinicians the opportunity to observe changes and symptoms.
The skin is complex and dynamic and provides a physical barrier against the environment; an innate and adaptive immunity that protects the body from pathogens; and thermoregulation. The skin is also responsible for vitamin D synthesis and protection from ultraviolet radiation on non-hair-bearing skin. It is a reservoir for medication administration and is a sensory organ (pain, pressure, itch, temperature,
touch). It comprises the epidermis, dermis, subcutaneous tissue, and adnexa or skin appendages and has regional variability in its thickness and structures. Glabrous skin does not have hair follicles or sebaceous glands, is located on the palms and soles, and is generally thick. In general, thin skin over the rest of the body houses a variable number of appendages, including the nails, hair, and sebaceous and sweat glands.
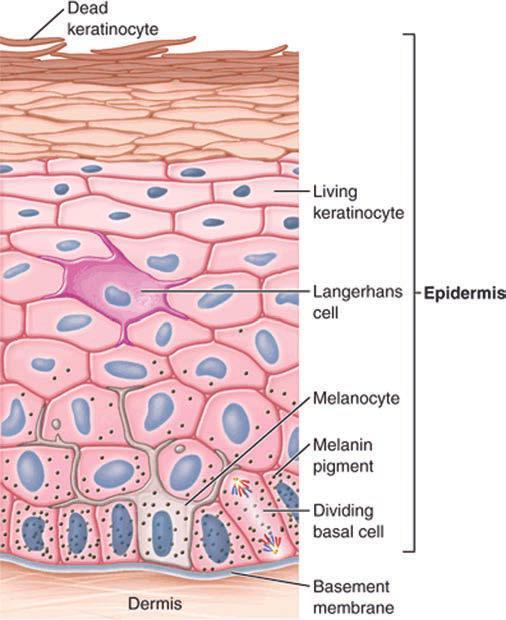
Epidermis
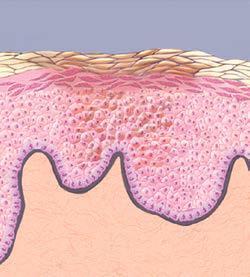
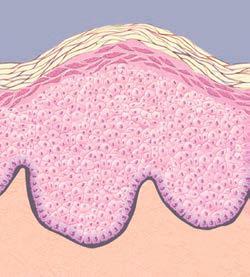
Commonly referred to as the “dead skin” layer, the epidermis is the locus of important structures and function (Figure 1-2). Cellular structures include keratinocytes, Langerhans cells, Merkel cells, and melanocytes. Nucleated keratinocytes differentiate as they ascend from the basal layer to the surface, filling with keratin and losing their nucleoproteins. Langerhans cells are intraepidermal macrophages responsible for phagocytosis of antigens and migration into the lymphatics and presentation to T cells. The immune function of the epidermis is paramount to our health. Merkel cells are believed to have a somatosensory function and are responsible for light touch and possible neuroendocrine function. Melanocytes synthesize the pigment which accounts for the variation in skin color among races. They are found in the dermis during fetal life and migrate to the basement membrane. The layers (strata) of the epidermis are responsible for protecting the body from the environment as both a mechanical and chemical barrier. Each strata has unique characteristics and functions (Table 1-1). Flattened keratinocytes with a thickened cell membrane create the stratified layer (shingles on a roof) in the stratum corneum, which is not capable of metabolic activity. This cornified layer saturated in a lipid complex provides a virtually impermeable barrier and minimizes water loss. Thus, any defect or impaired function of this layer can lead to pathologic changes and disease.
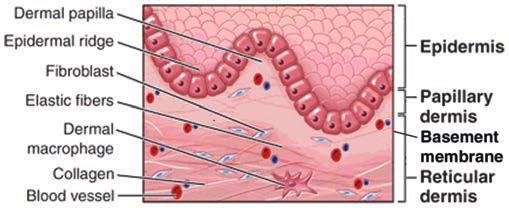
Dermis
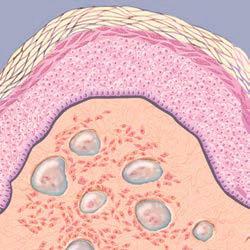
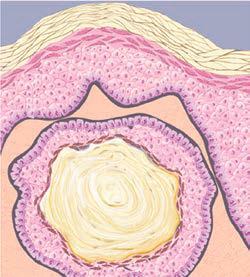
The dermis comprises fibroblasts, histiocytes, and mast cells, and is separated from the epidermis at the basement membrane (dermal–epidermal junction or DEJ). It adjoins with the papillary dermis (upper portion) Fibroblasts produce collagen (90% of the dermis), elastin, and ground substances, which comprise the majority of the dermis and are the supporting matrix of the skin (Figure 1-3). The dermis is also responsible for the continued immune response initiated in the epidermis by Langerhans cells, as well as neutrophils, lymphocytes, monocytes, and mast cells. Blood vessels, lymphatics, and sensory nerve endings for pain, itch, pressure, temperature, and touch are present. Arrector pili muscles in the dermis contract to make hair follicles stand up, creating the “goose bumps” effect. The reticular dermis (lower portion) joins with the subcutaneous or fat layer of the skin.
Subcutaneous Layer
The subcutaneous layer, also referred to as fatty tissue or hypodermis, comprises adipose cells and connective tissue, which varies in
1-1. Skin anatomy and histology. A: Anatomy of the skin. B: Corresponding photomicrograph of the skin showing the cellular distinction between the epidermis and dermis.
thickness according to the body location. The hypodermis provides a layer of protection for the body, thermoregulation, storage for metabolic energy, and mobility of the skin.
Adnexa
Adnexa or appendages of the skin include the hair, nails, and eccrine and apocrine glands. The structure of hair and nails is discussed in chapter 14.
Glands
Eccrine glands
Chiefly responsible for thermoregulation of the body, the eccrine or sweat glands are tubules that extend from the epidermis through the dermis and are triggered by thermal and emotional stimuli. Although they are diffusely spread over the body, most are located on the palms and soles, and can contribute to hyperhidrosis or
FIG.
1-2. Layers of the epidermis.
1-3. Dermis.
TABLE Strata of the epidermis 1-1
STRATUm (LAyER) CHARACTERISTIC
Corneum Brick and mortar layer
Lipid matrix and barrier Antimicrobial peptides
hypohidrosis. Eccrine glands maintain an important electrolyte and moisture balance of the palms and soles.
Apocrine glands
Found only in the axillae, external auditory canal, eyelids, mons pubis, anogenital surface, and areola, apocrine glands secrete a minute amount of an oily substance that is odorless. The role of these glands is not clearly understood.
ASSESSmENT OF THE SKIN
Clinicians should elicit a good patient history and perform a proper skin examination in order to generate a complete differential diagnosis.
History
Practitioners are afforded very limited time to assess, diagnose, treat, and document patient care. The patient history is sometimes slighted in view of time spent on the physical examination or patient education. However, the importance of an appropriate history relative to the skin complaint should not be overlooked. The history should begin with the patient’s general health and proceed with a focused or complete history relative to the skin complaint and presence of systemic symptoms (Box 1-1). Be aware that patients may be very cursory with details about their health history as they perceive that it is inconsequential to their skin condition. For example, a female seeking treatment for acne may fail to omit oral contraceptives on her medication list or her medical history of polycystic ovarian syndrome. Both can impact the clinician’s ability to adequately assess, diagnose, and manage her skin condition.
Medications are one of the most significant aspects of a history, receive the least attention, and yet have the greatest risk of impacting the patient’s skin condition. Medication history should not only include prescription drugs, but over-the-counter and illicit drugs, supplements, herbals, and “borrowed” medications. Chapter 17 provides tips on taking a medication history. The elderly and adolescents are known for sharing drugs and may be sheepish about admitting to it. NSAIDs are one of the most common causes of drug eruptions, but often omitted from their medication list. Oral contraceptives, which can have a significant impact on the skin, are commonly omitted from the patient’s list of medications.
FUNCTION
Mechanical protection; limits transepidermal water loss; limits penetration of pathogens (bacterial, viral, and fungal) or allergens
Lucidium Only on soles and palms protection
Granulosum
Keratin and fillagrin >80% of mass of epidermis profillagrin cleved into fillagrin, and loricin forming cornified envelop
Spinosum Lamellar granules (containing ceramides)
Langerhans cells
Basale
Cuboidal basal cells with nucleus and integrins
Scattered melanocytes
Found intracellularly in upper layer but migrate to corneum where most effect, responsible for lipid barrier function
Defends against microbial pathogens
Integrins responsible for adhesion to dermis
Initiation of keratinocyte differentiation
Migration upward to stratum corneum takes 2–4 wk
FIG.
FIG.
BOX 1-1 Complete History for the Assessment of Skin Lesions
Demographic Data
Age, sex, race—predilection in some diseases/conditions
Allergies
Drug, environmental, food (possible cross-reactivity)
medications
See chapter 17 (if drug-related eruption is suspected) prescription, over-the-counter, birth control, herbal supplements, illegal drugs
medical and Surgical History
personal (birth history for children), including skin cancer
Family (hereditary disease association or genodermatoses) pregnancy or lactation
History of Lesion or Eruption
Onset, circumstances, and duration
Spread and/or course of the skin condition
Aggravating or relieving factors
Associated symptoms—itching, pain, drainage, blisters, or odor previous episodes, treatment and response
Impact on sleep, eating, social activities, work, and school
Social History
Occupation and hobbies
Sunscreen use, tanning behaviors, and UVr exposure
Alcohol intake and smoking exposures (infectious or environmental)
Sexual behavior and orientation travel
Living conditions or household (especially important for infectious diseases)
Family structure
Psychological History
etiology or complication of skin conditions
Before concluding the history intake, it is recommended that clinicians inquire (an open-ended question) about any other specifics that the patient believes might be important about their skin condition. This invites communication and acknowledges the important role of the patient, family, and care givers in their patient-centered care. Patients may express grave concerns that their symptoms are similar to a disease discussed on a television talk show or health information discovered on an Internet search engine. Transparency in the patient’s perception and expectations at the beginning of the office visit will enable the clinician to personalize care for a better patient experience.
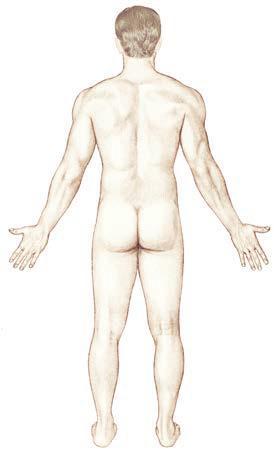
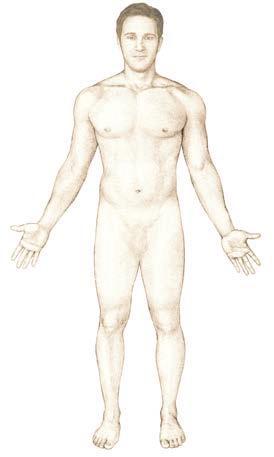
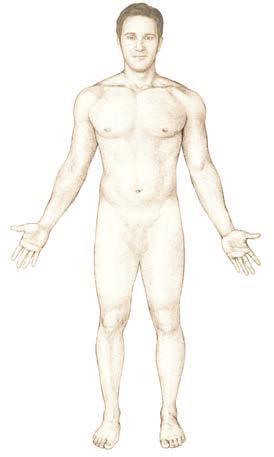
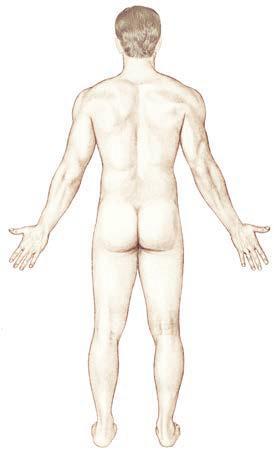
Physical Examination
Physical examination of the skin is a skill that is developed through repeated and systematic evaluations of your patients. The extent of the examination is determined by the patient’s symptoms and willingness to reveal their body. A complete skin examination is recommended for skin cancer screenings, with the patient completely disrobed and in a patient gown. It is also preferred for patients who come in with complaints of a skin eruption or those with systemic symptoms. In contrast, a focused examination from the waist up may be adequate for a chief complaint of acne that may require exposure
of the back and chest. Clinicians should encourage patients to allow maximum visualization for a thorough examination while respecting their modesty and rights to limit their physical exposure.
A helpful guide is provided to aid in developing a systematic approach for a skin examination for either the entire body or regional areas (Box 1-2). It is not necessary to wear gloves for a skin examination, allowing the clinician to use touch to optimize their assessment. All providers should clean their hands prior to and after examining a patient. Patients, and our society in general, have become increasingly aware of infection control and appreciate seeing the clinician cleanse their hands while in their presence. Yet, universal precautions should always be observed when preforming cutaneous procedures, exposed to body fluids, or examining skin that is not intact. They should also be worn when infection is suspected or touching the anogenital area and then immediately discarded.
Diagnostics
While the history and physical examination are the foundation for developing differential diagnosis, diagnostic tests may be necessary to rule out disease or support a definitive diagnosis. Each chapter in this text identifies recommended tests relative to the disease, and chapter 24 describes common procedures in detail. In-office diagnostic tools that can easily be used by nondermatology clinicians include the Wood’s light, KOH, or mineral prep. Diagnostic tests such as patch testing or tools such as dermoscopy should be reserved for dermatology clinicians trained in application and indications for practice.
One of the most important diagnostics used in the evaluation of cutaneous lesions is histopathology. Clinicians trained to perform shave and punch biopsies can send specimens for hematoxylin and eosin (H&E) staining, which provides microscopic analysis and reports on the pathologic changes in the skin. When indicated, immunohistology on patient tissue or sera utilizes various immunostaining techniques with light microscopy to identify antibodies. This is especially helpful in cutaneous manifestations with autoimmune diseases and is discussed in further detail in those chapters.
Clinicians should learn to competently interpret histopathology reports to ensure that clinicopathologic correlation exists, especially in inflammatory skin conditions. When there are questions regarding the report or interpretation, the clinician should discuss the biopsy with the pathologist. Most dermatology specialists send tissue biopsies to dermatopathologists who are specialty trained and board certified in dermatology with a fellowship in dermatopathology. They can provide a superior histologic analysis and opinion about possible diagnoses, especially when the clinician provides pertinent history, clinical findings, and their list of differential diagnoses.
ASSESSmENT OF SKIN LESIONS
Clinicians simply cannot know about every dermatosis, but they can develop assessment skills that will be the key to a timely and accurate diagnosis. Skin lesions can be described in a variety of ways and categorized by morphology, distribution, configuration, and arrangement. While some experienced dermatologists may use various approaches to diagnosis, these authors suggest that nondermatology and less experienced dermatology providers develop an algorithmic approach to diagnosis based on morphology of the primary lesion.
morphology
The characteristics or structure of a skin lesion is referred to as morphology. Once the clinician has identified the morphology of the primary lesion or eruption, they can generate a differential diagnoses.
BOX 1-2
Complete Skin Examination
How to Perform a Skin Examination
the two most important aspects of a complete skin examination are exposure and lighting.
patient must be properly gowned so that each part of the body can be visualized.
extra lighting may be needed for examination rooms without windows.
Always encourage the patient to undress completely; no peek-a-boo examinations!
Develop a systematic approach and use it for every skin examination. Begin with the patient seated in front of you and slightly lower.
Gently use your fingers to glide across the skin—your touch can identify lesions and comfort the patient.
Scalp
part the hair in various sections to visualize the scalp.
Look for papules, nodules, redness, scale, pustules, and scarring.
Hair
and Nails
Note hair color, pattern, and texture (see chapter 14).
Look for hair thinning or loss and patterns; note the presence/ absence of follicles.
Observe nails and periungual areas for discoloration, thickening, dystrophy, debris, or signs of infection. pigmented lesions can be found in unsuspecting places like beneath the nail.
Face
Get an overall view of the face.
Note the presence of scars and evidence of photodamage.
Look for redness, scaling, papules, pustules, comedones, skin tags, milia, keratoses, and pigmentation.
mouth
Look for any brown or red spots on the lips.
Dryness and scale on the lips in the elderly may be caused by photodamage.
Chapped lips in children or adolescents may be contact dermatitis. examine the mouth for lesions on the palate, buccal mucosa, and tongue.
patients on isotretinoin may have extreme dryness of facial skin and mucus membranes.
Eyes
examine the inner and outer canthi, orbital area, and lid margins for papules.
Note scale, erythema, or plaques in the brows or lids.
Check for erythema, erosions, or drainage of the conjunctiva.
Often, dermatology textbooks and online resources use a morphologybased approach to categorize diseases. Therefore, clinicians who lack the ability to correctly identify the morphology of the primary lesion must resort to fanning through the color atlas of dermatologic conditions, hoping that they will see a similar lesion or rash.
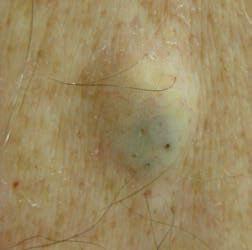
Primary lesions
The morphology of a primary skin lesion can provide important information about the depth of the process and the location of the
Ears
Look for scale or lesions on the helix
examine posterior earlobes for keloids and postauricular sulcus for redness and scale
Check conchal bowl for open comedones, hyperpigmented plaques, scale, and scarring
Nose
Look and feel the bridge, sides, creases, and nasal rims
Note telangiectasias, ulcerations, and abnormal pigmentation
Dilated blood vessels may signify sun exposure and possibly rosacea
Look for papules, pustules, and rhinophyma
Neck
Note the color, texture and distribution, especially anterior and lateral aspect, and inferior chin (photoprotected areas)
Trunk
Visualize the trunk with the patient sitting, standing, or lying down
Be sure to examine the buttocks, hips, and perianal area
If patients defer an examination of their genitals, inquire about new lesions or changes
Check the often forgotten umbilicus for psoriasis, nevi, and melanoma
Arms and Hands
Inspect arms separately and raise to inspect the axilla and lateral trunk
Look for discoloration or depigmentation in the axillae the antecubital fossa is a classic location for atopic eczema, whereas psoriasis and rheumatoid nodules favor the elbows. examine the dorsal and palmar surfaces of the hands, the fingers, and interdigital areas
Legs and Feet
examine the legs individually and thoroughly
Socks must be removed, to examine the feet, toes, and interdigital spaces
Don’t forget the plantar surface, which is a common place for pigmented lesions
Lymphadenopathy
Note occipital, posterior, and anterior cervical nodes with scalp lesions and infections
Check for regional and supraclavicular lymphadenopathy, as well as hepatosplenomegaly, in patients with a history of melanoma or squamous cell carcinoma
Use all the tools available to assess the “ABCDe” of melanoma. If in doubt, ask for help or refer to a dermatology specialist.
pathology, that is, the epidermis, dermis, and/or subcutaneous tissue. A thorough understanding of the structure and function of the skin will then allow the clinician to envision the underlying pathologic process and assist in making the clinicopathologic correlation. Flat lesions often represent disease located in the epidermis, while raised lesions usually involve the dermis and/or subcutis. All clinicians should be able to identify these basic morphological types that provide the foundation for the assessment and diagnosis of any skin condition (Figure 1-4).
macule < 1 cm
Patch ≥ 1 cm
Flat, discoloration
Nodule < 1 cm
Tumor ≥ 1 cm
Solid, circumscribed, dermal
Papule < 1 cm
Plaque ≥ 1 cm
raised, solid, well-defined
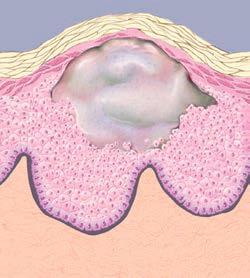
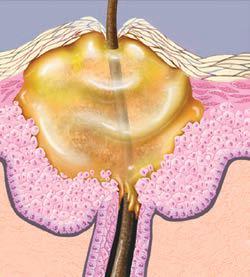
Cyst
Fluid/semisolid-filled nodule, maybe fluctuant
Vesicle < 1 cm
Bulla ≥ 1 cm
Fluid-filled, transparent
Fluid-filled, purulent
FIG. 1-4. Morphology of primary lesions.
Pustule
Secondary lesions
Secondary changes (scale, ulceration, lichenification, etc.) in the primary lesion can occur as the result of external factors, the process of healing, or complications from treatment (crusts, atrophy, purpura, scar, etc.). The characteristics of the secondary skin lesions provide further description (an adjective) about the primary lesion (noun). There are many descriptors, but several are commonly used in everyday practice (Figure 1-5).
Characteristics
The configuration of a lesion describes the shape, which can provide valuable clues. Annular plaques are characteristic of tinea and granuloma annulare. The arrangement is the location of lesions relative to each other. Lesions can be solitary, satellite (set apart from the body of the eruption), or clustered. While a red cherry angioma is typically a solitary lesion, the eruption of vesicles and pustules in herpes zoster is usually clustered and follows dermatomal arrangement.
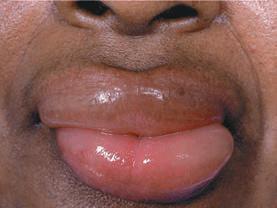
Distribution
When observed, the distribution of skin lesions can provide valuable diagnostic clues. Lesions may be generalized or localized, or may favor particular areas of the body such as the interdigital spaces, acral areas, or mucous membranes. Many cutaneous and systemic diseases have hallmark clinical presentations based on the distribution of lesions (Figure 1-6). For example, lesions on the palms are characteristic of conditions like erythema multiforme, dyshidrotic eczema, secondary syphilis, and palmar-plantar psoriasis. Chronic scaly and erythematous patches or plaques on the extensor aspects of the extremities would favor a diagnosis of psoriasis compared to atopic dermatitis that usually affects the flexural surfaces. Care should be taken to note lesions involving the hair, nails, and mucous membrane which can be unique for some diseases. And lastly, the clinician should remember that the distribution of the lesions may change as a skin eruption progresses. Drug rashes typically start on the trunk and spread to the extremities (centrifugal). In contrast, erythema multiforme starts on the hands and feet, and advances to the trunk (centripetal).
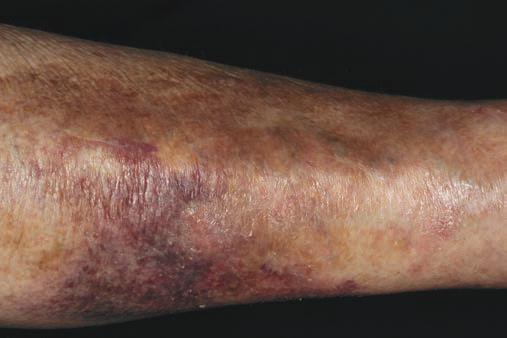
Color
For most clinicians, the color of lesions is given little consideration and usually categorized as red or brown. But next time, take a closer look and use tangential lighting. Colors can provide insight into the underlying pathophysiology of the lesion. Red, purple, and blue lesions usually have a vascular etiology. Yellow and orange colors are typically the result of lipid, chemical, or protein deposition. Brown, black, and blue colors are associated with melanin or hemosiderin. White lesions can be associated with a lack of pigment and a “fleshcolor” lesion refers to the patient’s natural skin color.
Associated Symptoms
Symptoms such as pruritus, pain, and burning can be helpful in discerning a diagnosis. For example, pruritus is a classic symptom in urticaria compared to the burning sensation associated with angioedema. Other lesion symptoms reported may include
tenderness, drainage, and odor. Clinicians should always be alert to systemic symptoms that may have proceeded or accompanied the cutaneous lesions. This should prompt a complete review of systems and detailed physical examination. Most importantly, patients presenting with red flag symptoms warrant immediate referral for further evaluation and management. Red flag signs and symptoms are febrile patients with a rash; altered levels of consciousness; facial edema or angioedema; purpura; oral or ocular mucosal ulcerations; bullae with mucosal involvement; chest pain or dyspnea; positive Nikolsky sign; and erythroderma ( >80% body with erythema).
mORPHOLOGy-BASED APPROACH TO DIFFERENTIAL DIAGNOSIS
The foundation for a diagnosis of any skin lesion begins with a thorough history and physical examination. We suggest that the morphology of the primary lesion provide the first step in a systematic approach for generating a differential diagnosis. After the primary morphology is identified, the clinician can incorporate other lesion characteristics and associated findings to narrow the differential to arrive at the correct diagnosis.
Use of algorithms can be helpful (Figures 1-7 and 1-8). Algorithms are intended as adjunctive tools accompanied by critical thinking Once the category of dermatoses is identified, key characteristics such as distribution, associated symptoms, and diagnostics studies are used to rule out or support the final diagnosis. Tables 1-2 to 1-5 provide abbreviated lists of differential diagnoses, including the most common skin conditions seen in primary care. More extensive lists of differential diagnosis can be found online, manuals, or tools such as Habif’s Differential Diagnosis Deck (2012).
Ultimately, success with diagnostic tools like these algorithms requires routine use, good clinical judgment, and individualized patient care. Yet there are always uncommon diseases and atypical presentation that will challenge even the most experienced dermatology clinician. When the clinician is perplexed by the lesion or eruption, he or she should always consult with another experienced colleague or dermatology specialist.
CLINICAL PEARLS
j When there is a change in the surface of the skin, it usually indicates an epidermal process.
j Always perform a punch technique for the biopsy of any inflammatory lesion.
j Vesicles can be from an immune response or infectious process. pustules are most often associated with infection.
j Consider the possibility of immunosuppression in patients with chronic or recurrent skin infections or atypical presentations.
j pathologic processes occurring deep in the dermis or subcutaneous can leave the surface of the skin smooth but result in larger plaques that are not as circumscribed (wheals/hives compared to angioedema).
j Be aware of some of the great mimickers of skin disease: lupus erythematosus, tuberculosis (mycobacterium), cutaneous t-cell lymphoma, secondary syphilis, sarcoidosis, and amelanotic melanoma.
j Diffuse eruptions involving large BSA can overwhelm the clinician. Always start with the basics: the morphology of the primary lesion.
Annular round plaque with raised border and central clearing
Reticular Lacy or network-like pattern
Perifollicular Arising from hair follicles, papules
Pedunculate On a stalk or stem
1-5. Common characteristics of skin lesions.
Umbilicated
Central depression or dell
Linear Straight lines, like scratching
Guttate Small, red, separate tear drop
Filiform Finger-like projections
Targetoid “Iris” shape, concentric rings with central bull’s-eye
Nummular “Discoid” or coin-shaped plaque
Collarette ring of scale around border
Serpiginous Wavy or creeping
FIG.
Desquamation
Shedding or peeling of epidermis
Wheal or Hives
Circumscribed, flat-topped plaques lasting < 24 hr
Ulceration
Focal loss of epidermis and dermis
Purpura
palpable and nonpalpable extravasation of blood into tissues
Crust
Dried serum, often honey-color exudate
Angioedema
edema in the dermis and cutis, not well circumscribed
Excoriation
Neurotic type, irregular shape
Petechiae
Nonpalpable, extravasation of blood into tissues, <3 mm
morbilliform
Small macules, measles-like appearance, usually red
Fissure
Deep tears through the epidermis and into dermis
Excoriation
Linear wounds from scratching
Lichenification thickened, exaggerated lines
FIG. 1-5. Common characteristics of skin lesions (continued)
Extensor areasFlexural areasAcral Symmetrical
Spares anterior neck
If patient wears shorts
Photodistributed Bilateral, asymmetrical
1-6. DIStrIBUtION OF LeSIONS. Bilateral, present on both sides of the body. Symmetrical, same location on both sides. Zosteriform/herpetiform, along one or more dermatomes, unilateral. Acral, ears, nose, feet/soles, hands/palms. Seborrheic, hair-bearing, and sebaceous glands; scalp, forehead, moustache/ beard, and chest. Diffuse/generalized, scattered over large area; localized, specific to one particular area.
FIG.
Morphology of primary lesion
Fluid-fillled vesicle/bulla pustule cyst* (Table 1-2)
Clear fluid
Purulent
Pustular dermatoses
Vesiclular dermatoses
Bullous dermatoses
Solid macule/patch papule/plaque nodule/tumor
Color of lesion (Table 1-3)
Flesh/skin
Brown
White/ yellow
Red color
Go to Figure 1-8
Differential diagnosis lists Further examination of characteristics
FIG. 1-7. Morphology-based approach to diagnosis of skin lesions. *Semisolid material and often nodular.
TABLE Fluid-Filled Dermatoses 1-2
VESICLES
(<1 Cm)
Dyshidrotic eczema
herpes simplex
Impetigo
Varicella/zoster
tinea pedis
Scabies
Contact dermatitis
hand-foot-andmouth disease polymorphic light eruption
Grover disease
Arthropod assaults erythema multiforme
Dermatitis herpetiformis
Id reaction
BULLAE (≥1 Cm)
Bullous impetigo
Bullous tinea trauma/thermal
Bullous erythema multiforme
SSSS
SJS/teN
Autoimmune blistering disease
Bullous drug eruption
Lichen planus porphyria cutanea tarda
Diabetic bullae
PUSTULAR
Acne vulgaris rosacea
Drug-induced pustular
acne
Folliculitis–bacterial, candidiasis, pityrosporum
Scabies
pustular psoriasis (especially palmar-plantar)
perioral dermatitis
Subcorneal pustulosis
TABLE Lesions with Color 1-3
FLESH COLOR BROWN WHITE
Rough
Skin tags
Verruca
Open comedones
Actinic keratosis
Corns/callus
epidermal nevus
Smooth
Molluscum
contagiosum
Basal cell carcinoma
Verruca/hpV epidermoid cysts
Lipomas
Keloids/ hypertrophic scar
Granuloma annulare
Neurofibromas
pearly penile papules
Adnexal tumors
Freckles
Skin tags
Lentigines
Nevi (intradermal, compound, junctional)
Seborrheic keratosis
tinea versicolor (pinkish)
postinflammatory hyperpigmentation
erythrasma
Dermatofibroma
Café au lait
Mongolian spot
Melanoma pigmented basal cell
Dysplastic nevus
Congenital nevus
Fixed drug eruption (purple)
Becker nevus
pityriasis alba
Idiopathic guttate hypomelanosis
tinea versicolor
Ash leaf macule
Milia
Keratosis pilaris postinflammatory hypopigmentation
Nevus anemicus
Morpheaform basal cell carcinoma
Vitiligo
piebaldism
Lichen sclerosus et atrophicus
Morphea tuberous sclerosis
Yellow
Xanthelasma
Sebaceous hyperplasia
Necrobiosis
lipoidica
Morphea
SSSS, Staphylococcal scalded skin syndrome
SJS/teN, Stevens–Johnson syndrome/toxic epidermal necrolysis.
hpV, human papilloma virus.
Red lesions
Scaly epidermis and possibly dermis pathology (Table 1-4)
Papulosquamous dermatoses no epidermal interruption
Eczematous dermatoses
epidermal interruption
Smooth dermal and/or subcutaneous pathology (Table 1-5)
Vascular reactions multiple lesions polymorphic
Inflammatory lesions solitary lesions monomorphic
FIG. 1-8. Morphology-based approach to diagnosis of red skin lesions.
T ABLE red and Scaly Dermatoses 1-4
ECZEmATOUS PAPULOSqUAmOUS
epithelial disruption, pruritus, and excoriations often prominent. Morphology may vary in acute and chronic stages.
Atopic dermatitis
Irritant contact dermatitis
Allergic contact dermatitis
Dyshidrotic eczema
Nummular eczema
Stasis dermatitis
Scabies
Secondary lesions (dermatitis herpetiformis, tinea, psoriasis, etc.)
Seborrheic dermatitis
polymorphic light eruption
Drug eruption
Lichen planus
Xerotic eczema
exfoliative erythroderma
T ABLE red and Smooth Lesions 1-5
Inflammatory lesions
Monomorphic (same size and shape), usually solitary
papules and dome-shaped
macules and papules
Arthropod assaults
Spider and cherry angiomas
Scabies
Acne
Keratosis pilaris
Candidiasis
pyogenic granulomas
Granuloma annulare
Viral exanthems
early psoriasis lesions
pityriasis rosea (w/o scale)
Secondary syphilis
pityriasis lichenoides
Grover disease
Nodules
Furuncles/carbuncles
epidermoid cysts
Cellulitis
erythema nodosum
Acne vulgaris
Mycosis fungoides
READINGS
No epithelial disruption, raised and scaly
Papules
pityriasis rosea
Keratosis pilaris
tinea
Lichen planus
Secondary syphilis
Guttate psoriasis
Prominent plaques
psoriasis
tinea
Lupus erythematosus
DLe
CtCL (mycosis fungoides) pityriasis rubra pilaris
Vascular reactions
polymorphic (varied size and shape)
Multiple, often confluent
Flat-topped
Transient rosacea
Urticaria
Persistent/blanchable
Kawasaki disease
SSSS
toxic shock syndrome
red man syndrome
Angioedema
Autoimmune blistering diseases
erythema multiforme
erythema nodosum
Drug eruption
Urticarial vasculitis
Ackerman, A. B. (1975). Structure and function of the skin. Section I. Development, morphology and physiology In S. L. Moschella, D. M. Pillsbury, & H. J. Hurley (Eds.), Dermatology. Philadelphia, PA: Saunders. Bolognia, J. L., Jorizzo, J. L., & Schaffer, J. Y. (2012). Dermatology. Philadelphia, PA: Elsevier.
Purpuric/nonblanchable petechiae
Coagulation disorders
Leukocytoclastic vasculitis
henoch–Schönlein purpura
ecchymoses
Meningococcemia
rocky Mountain spotted fever
Vascular ulcers
Calonje, E., Brenn, T., & Lazar, A. (2012). McKee’s pathology of the skin (4th ed.). St. Louis, MO: Elsevier. Habif, T. P. (2012). Dermatology DDX deck (2nd ed.). St. Louis, MO: Mosby. Habif, T. P. (2009). Clinical dermatology (5th ed.). St. Louis, MO: Mosby. Lynch, P. J. (1994). Dermatology (3rd ed.). Baltimore, MD: Williams & Wilkins.
CtCL, cutaneous t-cell lymphoma: DLe, Discoid lupus erythematosus.
CHAPTER
Corticosteroids and Topical Therapies 2
The skin is a large and complex organ that performs multiple functions allowing us to maintain a state of homogeneity. As a barrier, it protects against chemicals, microorganisms, ultraviolet radiation (UVR), and the loss of bodily fluids. It is a nutritive organ supplied by a network of superficial vessels that nourish and repair the skin. Constant vasodilation and constriction of blood vessels, along with the cooling response of sweat glands, accomplishes temperature regulation.
These functions can alter the moisture content in the skin and subsequently affect the penetration and efficacy of topical preparations. Percutaneous absorption (PCA) of topical treatments also varies depending on the thickness of the skin on different areas of the body. For instance, eyelid, antecubital, axillae, and genital skin are very thin and medication is quickly absorbed. The skin of the palms, soles, knees, and elbows is thicker, decreasing the rate of the absorption of medications applied. The presence or absence of occlusion also affects product permeability, rate, and potency of medications used.
This chapter will explore various topical formulations and the most appropriate use of each in the treatment of common dermatologic conditions. Sunscreens and their proper use will be presented, and an overview of botanical products will be outlined.
Systemic agents, specifically corticosteroids, are often used in dermatology, and we will review their optimum indications and usage. At times, oral agents may seem to be a more convenient option; however, topical therapies are often the better choice. With the correct usage of topical corticosteroid (TCS) therapies, side effects will be minimized.
SKIN HEALTH
Patients often ask about proper skin care. They are besieged with advertisements about the best and latest “miracle cream” and often believe that cost is equated with efficacy. For some, it is merely a factor of cosmesis, but many seek help because of uncomfortable and sometimes disfiguring skin conditions. Providing accurate information regarding product ingredients will help patients make better, more informed choices when faced with the myriad of options.
Cleansing
Everyone can benefit from a good skin care regimen. Recommendations regarding bathing and hand washing vary depending on a person’s age, activity, environment, culture, and skin condition. Cleansing the skin too often can contribute to worsening of certain skin conditions such as acne and eczema. The use of antibacterial soaps, abrasive materials, and gadgets are not necessary, and can be harmful to the skin by contributing to antibiotic resistance, irritation, or allergic reactions.
Environment
Protecting the skin from all types of weather is important. Sun, wind, cold, and humidity can hinder the skin’s protective function. In dryer climates, moisturizers should be applied within minutes of bathing to help prevent water evaporation and skin cracking, which can predispose patients with certain skin conditions to infection. Oil-free and noncomedogenic products are recommended for the skin of the face, while thicker moisturizers and those containing urea or lactic acid are more effective in treating hyperkeratotic skin commonly seen on the feet. Lactic acid, an α-hydroxy acid, is useful for softening dry, thick skin. This ingredient can also cause skin irritation and should not be used on delicate or inflamed skin.
In very cold climates, dry air from heating systems enhances water evaporation and contributes to the overall dryness of the skin. In humid climates, light-weight breathable clothing can help skin to remain dry. In all climates, sunscreen should be applied to exposed areas in the morning and reapplied every 2 hours when staying in the sun.
Healthy lifestyles also help maintain a person’s youthful skin appearance. Incorporating regular exercise, maintaining a proper diet, minimizing alcohol intake, and avoiding smoking and excessive stress are key factors in protecting the skin from aging prematurely.
Irritants and Allergens
Individuals with sensitive skin should choose products less likely to include common allergens such as fragrances, dyes, lanolin, propylene glycol, and parabens. If there is a suspected allergy, referral to a dermatologist can help the patient identify the allergens through patch testing (see chapter 3). Furthermore, dermatologists can provide patients with lists of personal hygiene products (a “safe” list) that they should avoid and those that are free of specific allergens. Patients are still warned to check the ingredient list of all products; even those on the safe list can change ingredients without any notice. Otherwise, primary care clinicians can provide some general guidance on widely available moisturizers that are free of the most common allergens (Table 2-1). Patients should be warned that the label “hypoallergenic” does not mean that the product does not contain common sensitizers. This is a marketing claim used by manufacturers and is not standardized or monitored. It only means that the product may cause fewer allergic reactions or has lower amounts of common sensitizers compared to other brands.
Yet not all dermatitis is caused by allergens. Frequent hand washing with soap and water is sometimes necessary, but can aggravate skin that is already affected by dermatitis. Hand dermatitis may be due to allergens in cleansers or irritation from the harsh chemical ingredients that can damage the epidermis and trigger inflammation. Water itself is the most common irritant in hand dermatitis and
Susan Busch and Gail Batissa Lenahan
TABLE Brand-Name Products Free of the Most Common Allergens* 2-1
CATEGORYPRODUCT†
Wipes7th Generation Free & Clear Baby Wipes
CleansersAveeno Baby Cleanser Moisturizing Wash
Eucerin Skin Calming Dry Skin Body Wash
Free & Clear Liquid Cleanser for Sensitive Skin
Vanicream Gentle Facial Cleanser
VML Hypoallergenics Essence Skin-Saving Clear & Natural Soap
Spring Cleaning Purifying Facial Wash for Oily Skin
MoisturizersAveeno Eczema Therapy Moisturizing Cream Baby
Eczema Therapy Moisturizing Cream
Cetaphil Oil Control Moisturizer SPF
Eucerin Professional Repair for Extremely Dry Skin
Lotion
Vaniply Ointment for Sensitive Skin
VML Hypoallergenics Red Better Daily Therapy
Moisturizer
LubricantsFragrance- and preservative-free: Aquaphor
Fragrance-, lanolin-, and preservative-free: white petrolatum or petroleum jelly
*Formaldehyde, fragrance (including botanicals), paraben mix/parabens, and propylene glycol.
†Retailers may sell old formulations of the brand. Manufacturers may change the formulation at any time and without warning or notice to consumers.
is often seen in health care workers. The use of a mild cleanser or a gel sanitizer made with at least 60% alcohol provides a less drying alternative. Alcohol gel sanitizers can prevent cracking and drying of the skin and should be used only on intact skin when hands are not visibly soiled.
TOPICAL THERAPIES
Moisturizers
Throughout this text, we will discuss skin conditions which involve, among other factors, a loss of the skin’s barrier function. When the skin is dry, the epidermis cannot perform its protective function, allowing microbes and allergens easy access to stimulate inflammation and/or infection. To maintain hydration and proper barrier function, the skin should be cleansed daily with lukewarm water and dried with a patting motion (not rubbed vigorously) to preserve the oils in the skin. Within 3 minutes of a shower or bath, a moisturizer or emollient should be applied to the entire body. This helps to “seal” in the water and increase moisture in the stratum corneum.
Moisturizer is a term commonly used when referring to any topical that is applied to treat dry skin. Products that are actually moisturizers hydrate the skin by drawing water into the stratum corneum through the use of humectants such as urea, glycerin, lactic acid, or glycolic acid. Emollients soften the skin and can offer a protective barrier with a layer of oil or another occlusive agent. Products may have one or both properties, and selection of the topical is an individual preference based on texture, odor, and location of the application. Moisturizers are available as ointments, creams, and lotions. Ointments offer the most hydration and greatest barrier and are especially effective for thick, dry, and scaly areas.
Moisturizers are also used for cosmetic purposes and can be applied several times a day, particularly after hand washing. Many
contain sunscreen, fragrances, alcohol, preservatives, and other chemicals mentioned above that are known to cause contact dermatitis. Patients with allergies should be instructed to apply the best agent for their dry skin but to avoid known agents that can trigger contact dermatitis.
Wet Dressings
When skin integrity has been altered and the skin becomes weepy or wet, several wet dressing options are available over the counter. Aluminum acetate powder (Domebero) is a medication that can be mixed with water for its antiseptic and drying properties. Acetic acid solution can be prepared by adding a half cup of household white vinegar to a pint of water for its bactericidal quality. Patients should be instructed to soak clean facecloths in the liquid and wring them out before placing on the weeping rash. These hypertonic treatments are effective in drying blisters and are commonly used for severe sunburns, poison ivy rashes, or moist intertrigo, but must only be used until the wet aspect of the condition has resolved.
Application is recommended two to four times per day for no longer than 30 to 60 minutes. Cool temperature water is used to decrease inflammation, while lukewarm water may be used to stimulate circulation in an infectious process.
In the pediatric population, especially those children with atopic dermatitis, plain wet dressings are recommended to help with the itch. In these cases, an emollient or TCS ointment (if prescribed) is applied first, followed by plain-water-soaked gauze, and covered with dry dressings or cotton pajamas and left on overnight. Wet dressings should never be occluded with plastic wrap as this increases the risk for maceration and increases bacterial growth.
Bleach Baths
Bleach baths can also be used for patients who are at higher risk for superficial skin infections. Patients with atopic dermatitis or recurrent skin and soft tissue infections from methicillin-resistant staphylococcus aureus (MRSA) can benefit from sitting in a warm bleach bath once to twice weekly for 10 minutes to reduce the bacteria count on their skin, and reduce the itching experienced by these patients. The bath is made from one quarter of a cup of unscented household bleach in a full bathtub. This dilutes the bleach to avoid any harmful effects. The skin is then treated with an emollient immediately after exiting the bath.
Cosmetic Botanicals
Clinicians are often asked about skin care products, specifically those containing natural ingredients (Table 2-2). There is some evidence to suggest that botanical products may be useful, but the scientific data are lacking. For patients with sensitive skin, eczema, atopic dermatitis, inflammatory or pruritic conditions, products containing feverfew, colloidal oatmeal, or sunflower seed oil may provide some soothing relief. Patients with rosacea and pigmented lesions may benefit from products containing licorice root extract, which has skin lightening and anti-inflammatory properties.
Botanical extracts are being used with increased frequency in the cosmetic industry, and the future of antiaging products, in particular, appears to be promising. Today many cosmetic formulations are made of botanical extracts and may improve the health, texture, and integrity of the skin, hair, and nails. Botanicals are also being used in cleansers, moisturizers, and astringents. Therefore, it is important to have an understanding of the expected benefit of these products.
Table 2-2 includes a synopsis of the more popular botanical ingredients used in skin care products today, but does not represent
TABLE Common Botanicals
NAME ORIGIN
Aloe Leaves of Aloe vera
Arnica Flowers of Arnica montana
CalendulaFlowers of Calendula officinalis (pot marigold)
Cayenne Fruit of Capsicum annuum
ChamomileDried flower heads and oil from Matricaria chamomilla
ChocolateSeeds of Theobroma cacao
DandelionLeaves, flowers, or root of Taraxacum officinale
EucalyptusLeaves, oil from Eucalyptus globulus
Feverfew Leaves, flowering tops of Tanacetum parthenium
Green TeaLeaves, buds from Camellia sinensis
Lavender Flowers, essential oil from Lavandula angustifolia
LemongrassLeaves, young stems, and oil of Cymbopogon citratus
Licorice root extract * Underground stem of Glycyrrhiza glabra
PatchouliLeaf, stem of Pogostemon cablin
ResveratrolSkin and seeds of grapes, berries, peanuts, and other foods
RosemaryLeaves, twigs from Rosmarinus officinalis
Soy Seeds from Glycine max
Tea tree oilLeaves from Melaleuca alternifolia
Witch hazelLeaves, bark, twigs of Hamamelis virginiana
EFFECT
Emollient, preventing infection
Anti-inflammatory
Antifungal, anti-inflammatory
Analgesic, warming stimulant
Antioxidant, antimicrobial, analgesic, anti-inflammatory
Antioxidant
Anti-inflammatory, antioxidant, antibacterial, possible antitumor activity
Antiseptic, astringent
Antioxidant, anti-inflammatory, anti-irritant, and anticancer properties. Orally, chewing leaves can cause ulceration and oral edema
Anti-inflammatory, antioxidant
Fragrance, antimicrobial,antianxiety
Antiseptic, antibacterial, antifungal
antioxidant, anti-inflammatory, antiviral and antimicrobial
Antibacterial, antifungal
antioxidant, anti-inflammatory, and antiproliferative agent
USE
Eczema, wound care, ringworm, burns, insect bites
Wound care, bruising, eczema, blisters (Avoid use on broken skin), acne, chapped lips
Radiation induced burns, decubitus ulcers, bruising
Neuropathic pain from shingles, massage oils, psoriasis
Wound care, burns
Cocoa butter for chapped skin, burns, irritants
Eczema, psoriasis, acne
Skin abscesses, minor wounds, bruises
Rosacea, antiaging, atopic dermatitis
Healing wounds and photoprotection
Fragrance, sleep inducer, sunburn, fungal infection, as rub form circulatory and rheumatic ailments
Athlete’s foot, ringworm
Skin lightening, healing for herpes blisters, canker sores, sunburn, insect bites
Eczema, seborrhea, acne, eczema, mosquito repellent
Antiaging, wrinkle reduction
Anti-inflammatory, antioxidant, analgesicSeborrhea, alopecia
Antioxidant, anticarcinogenic, anti-inflammatory
Skin lightening, improve skin elasticity, moisturizer
Antifungal, antimicrobial, anti-inflamamtoryAcne, onychomycosis, ringworm, dandruff eczema, insect bites
Astringent, antioxidant, anti-inflamamtoryAcne, contact dermatitis, bites, burns
*The oral form of licorice root extract can interact with angiotensin-converting enzyme inhibitors, aspirin, oral contraceptives, oral corticosteroids, diuretics, insulin, and stimulant laxatives.
Adapted from Foster, S., & Johnson, R. L. (2006). Desk reference to nature’s medicine. Washington, DC: National Geographic Society.
all botanicals on the market and is not an endorsement. Patients with skin disorders should always use caution before using any new topical products, as they may include ingredients that can cause contact dermatitis. Providers can guide patients away from allergens included in these products that can initiate an irritant or an allergic response, no matter how “natural” the ingredients.
CORTICOSTEROIDS
Corticosteroids play a significant role in the treatment of dermatologic disorders. The fact that they can be used topically, intralesionally, and systemically provides the clinician numerous options for patient management. Corticosteroids are a synthetic derivative of the natural steroid, cortisol, which is produced by the adrenal cortex. There are two types of corticosteroids, glucocorticoids and mineralocorticoids. Glucocorticoids are the drugs most often used in dermatology and will be the focus of discussion in this chapter. In general, regardless of the method of administration, these drugs act as anti-inflammatory, immunosuppressive, and antiproliferative agents. When they are used topically, their vasoconstrictive properties determine their potency, and they are used to treat a wide range of disorders from acute allergic dermatitis to chronic immunobullous disorders. We will look more closely at these frequently used medications in the next two sections and will discuss their mode of administration, indications, and side effects and will make recommendations for use depending on the severity of the disorder.
Topical Corticosteroids
Many conditions seen in primary care and dermatology can be appropriately treated with a TCS. They penetrate the skin and work by decreasing the inflammatory pathways that cause the skin to become red and inflamed. Within days of use, however, the production of new skin cells is suppressed, creating the risk of atrophy and striae with long-term usage. The following factors can have an effect on treatment success and should be considered when prescribing any topical medication.
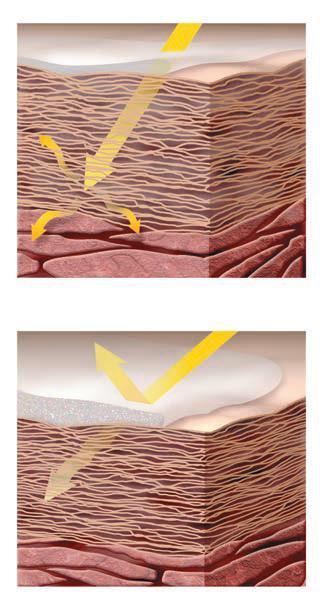
Percutaneous absorption
The ability of a topical medication to be effective is dependent on the transdermal delivery of the active ingredients from the stratum corneum of the epidermis to the underlying capillaries. There are many variables which can promote or impede PCA, including drug concentration, frequency of administration, occlusion, surface area involved, the vehicle, age and weight of patient, location on the body, and amount of time the topical is left on the skin. PCA is increased with hydrated (moist) skin, heat or elevated temperature, and the condition of skin barrier.
Vehicles
Topical agents are prepared in a variety of vehicles or bases that constitute the inactive portion of the medication, allowing the drug to be delivered into or through the skin (Table 2-3). Generic formulations of TCS may vary in the contents of the vehicle. Contact allergies may worsen if a generic product is substituted for a brand-name prescription. Vehicles can also alter the potency of the corticosteroid itself, which is why a drug may be class 1 in an ointment form but a different class in a cream or lotion vehicle. Additionally, consistency of the vehicle can be important.
Strength/frequency
A concentration of 1% indicates 1 g of drug will be contained in 100 g of the formulation. Efficacy of a topically applied drug is usually
TABLE Vehicles for Topical Preparations 2-3
VEHICLEDEFINITION
SolutionHomogenous mixture of two or more substances
LotionLiquid preparation, thicker than solution
Likely to contain oil, water, and/or alcohol
CreamThicker than lotion Requires preservatives to extend shelf life Greater potential for allergic reactions
OintmentSemisolid, mostly water-free
Petrolatum-based product Spreads easily, penetrates better than creams
GelAqueous, semisolid emulsion
Liquefies when in contact with skin
FoamLiquid comprised of oil, solvents, and water packaged under pressure in aluminum cans
SprayLiquid dispensed through an aerosol container or atomizer
PREFERENCES
Excellent for scalp/ hair-bearing areas
Lotions spread easily. Use in large areas
Use when skin is moist or exudative. Can be used in any area
Well tolerated
Choose when skin is dry or for increased penetration (thick skin). Messy in hairy areas
Great for hairy areas
Avoid on blistered skin, may sting
Great for scalp and thick plaques
Penetrates well without mess
Helpful for hard to reach places
And scalp or hairy areas
not proportionate to the concentration. Doubling or halving the concentration often has a surprisingly modest effect on the response. Occlusion increases the penetration and ultimately the effectiveness of the product. Compounding of proprietary products with other ingredients may alter the stability of the drugs and should be done with caution if at all.
The common recommendation is to use the least potent TCS that is effective; however, using a TCS that is too weak may be ineffective and decrease compliance and patient confidence in the provider. Low-potency corticosteroid preparations can be used safely when needed on thinner skin. The common risks that apply to all TCS still exist when overused.
Ultrapotent or high-potency TCS should be used on a rotation schedule, with two or three daily applications for a 2-week period, followed by 1 or 2 weeks without TCS. Some clinicians advocate use of nonsteroidal agents or emollients during this break period. Paradoxically, stronger TCS (groups I and II) are commonly used in skin disorders such as lichen sclerosis and lichen planus that may involve mucosal skin without concern for atrophy.
Side effects
Common side effects with TCS or their vehicle’s include contact dermatitis, acne-like eruptions, skin atrophy, hypopigmentation, telangiectasia, purpura, and striae, as well as ocular effects of increased
intraocular pressure, cataract formation, and glaucoma. When using corticosteroids under occlusion, there is also a risk for folliculitis and maceration of the skin. In addition to patient education, providers can help reduce these risks by ordering only enough medication to achieve clearing. Refills may be given; however, follow-up appointments should be provided. Prescriptions given to poorly compliant patients should not be refilled indefinitely, and nonsteroidal alternatives may be a better option for some individuals.
Due to variability in generic formulations and the common addition of propylene glycol, a common allergen, allergic reactions from TCS can be a conundrum. If a corticosteroid allergy is suspected, desoximetasone ointment 0.05% is the treatment of choice until the allergen is confirmed. Referral to dermatology can identify specific allergens through patch testing with Thin-layer Rapid Use Epicutaneous Test (TRUE Test). This company has recently added tixocortol pivalate and budesonide, which can help identify TCS allergies. These products are widely used in dermatology and allergy practices. Testing for propylene glycol, however, requires a more comprehensive patch series such as the North American Series, which is usually provided only at larger academic or occupationally focused clinics. Any patient who is not improving on TCS should be reevaluated, and the provider should consider the following:
• Contact dermatitis due to the corticosteroid or preservative in the corticosteroid;
• Noncompliance;
• Tachyphylaxis (a decrease in the pharmacologic response after repeated administration of a topical agent); and
• Incorrect diagnosis: alternate diagnoses to consider include but are not limited to cutaneous T-cell lymphoma, drug reaction, or fungal infection.
Atrophy or thinning of the skin from the application of TCS can occur within a fairly short period of time with potentially permanent results. Atrophy can be manifested by fragile skin and stretch marks (Figure 2-1). Labeling on the tubes of TCS rather than on their outer boxes may help patients follow instructions on how much and where medications are to be applied, thereby reinforcing instructions given during the office visit.
Superficial staphylococcal folliculitis is a possible side effect of TCS, especially when using with occlusion. If noticed early, this can sometimes be reversed by drying out the skin with aluminum acetate compresses (i.e., Dombero); however, folliculitis often requires oral antibiotics to clear.
Adrenal suppression is a possible side effect of the stronger TCS, especially if used on a large surface area. This side effect is generally
TABLE Estimated Amounts for Topical Medication 2-4
Conversions: Adult: 30 g covers entire adult body in one application; children: ½ of the adult amount; infants (6–12 months): only ¼ of the adult amount; 1 FTU = 0.5 g per application.
FTU, fingertip unit.
reversible and frequently associated with long-term oral corticosteroid therapy.
Avascular necrosis (AVN) is another very rare side effect that can be caused by either topical or systemic corticosteroids. AVN has been documented with long-term use of TCS. Magnetic resonance imaging (MRI) of the hip may be ordered in the investigation of AVN symptoms, which include pain in the groin, hip, buttock, or knee that increases with activity and is relieved with rest.
Quantity
How much medication is needed to achieve the desired effect is always a question (Table 2-4). The fingertip unit (FTU) and rule of hand are two measurements used to determine how much product is needed and how much to prescribe. The FTU is the amount of topical medication that comes out of a tube with a 5 mm diameter and covers the area from the distal crease of the forefinger to the ventral aspect of an adult fingertip (Figure 2-2). For an adult, 2.5 FTU is needed to cover the entire neck and face. For a child (ages 1–5), one half of this amount would be needed to cover the same area. For an infant, quarter of the adult amount would be sufficient. One FTU
FIG. 2-1. Steroid atrophy.
FIG. 2-2. Fingertip units.
weighs approximately 0.5 g. Therefore, an adult face and neck would require a 35-g tube of cream for a 2-week course of treatment. The “rule of hand” describes the area to be treated. An area the size of four adult hands (including the digits) can be treated with 1 g of ointment or two FTU.
Occlusion
For increased penetration of very thick skin plaques or to treat a full body rash, occlusion may be used for a period of 2 hours twice daily. Medication is applied, and plastic wrap is used to cover the entire area where it is practical, such as an arm or leg. Alternatively, corticosteroid-impregnated tape such as Cordran Tape is available and useful for small, thickened areas. If the entire body surface is involved, a plastic suit, known as a sauna suit, can be worn for a few hours in the day after applying the corticosteroid to all areas. Occlusive plastic suits are inexpensive and can be found at most sporting goods stores.
Brand versus generic
Insurance companies often require that providers use generic in place of brand-name topical preparations. While generic products contain the same active ingredient, the product’s vehicle often differs, altering the efficacy of the drug as well as contributing to the induction of contact dermatitis. The choice of a generic versus a brand-name drug is dependent on many patient-specific factors, but is often unfortunately determined by the insurance company’s formulary.
Combination drugs
Commercially prepared TCS may be combined with drugs from a different class such as antifungal or antiyeast agents and are not generally recommended by dermatologist. They may provide some symptomatic relief, but may obscure the correct diagnosis. In addition, they can promote development of microbial resistance to antibiotics and may increase sensitization to ingredients. TCS have been successfully paired, however, with a vitamin D analog, calcipotriene (Dovonex, Vectical), in the treatment of psoriasis. Likewise, acne preparations are often combined, offer ease of use, and assist with the compliance of the younger patient.
Patient education and follow-up
The patient’s ability and willingness to comprehend and comply with treatment recommendations can be influenced by a variety of factors, including the patient’s relationship with their provider, the belief that the treatment will work, comprehension of directions provided, financial or time constraints, as well as the cosmetic elegance, or “feel” of the prescribed products. Patients are more likely to adhere to simple dosing schedules. It is helpful to provide them with clear verbal and written instructions.
Acne patients should be advised to avoid skin trauma by using minimal friction when cleansing skin and avoiding picking at their skin. When discussing topical retinoids, providers should refer to a “pea-sized” dab for the correct amount to apply to the face. Using the demonstration of a pea-sized emollient cream during an office visit may help patients better understand application instructions. For patients with psoriasis, demonstrating the application of emollients into thickened plaques can increase compliance and prescription efficacy. Recommending that all patients bring remaining tubes of products to their follow-up visits can help determine usage. Providers can consider creative options for patients to help them follow the agreed upon treatment plan. Smart phone features such as alarms and calendars can remind patients when to use their medications and return for follow-up appointments.
Systemic Corticosteroids
Many providers of dermatology services are extremely comfortable managing patients on TCS. It is instinctual to choose the proper dose, vehicle, and quantity for the patient. Those same practitioners, however, are far less comfortable when the patient requires additional and specifically systemic therapy. While there are numerous conditions which respond well to systemic corticosteroids and in fact may be essential, fear of side effects and rebound disease prevail. Oral administration usually takes preference over the intramuscular (IM) route although IM injection guarantees the proper dose and can be helpful if gastrointestinal side effects exist.
Systemic corticosteroids are classified as short, intermediate, and long acting. Prednisone, which is the corticosteroid of choice in dermatology, is an intermediate acting medication. Prednisone is actually the inactive form of the drug and must be converted to the active form, prednisolone, by the liver. It is generally given as a single daily, oral dose because it most closely approximates the body’s natural diurnal variation. Divided doses are generally reserved for acute, lifethreatening conditions and in general have an increased effect despite the same total daily dosage. In liver impaired patients, prednisolone is the drug of choice. The length of a treatment course depends entirely on the condition. In acute dermatoses such as contact dermatitis, a short 2- to 3-week tapering course or “burst” is suggested. In severe conditions which will require more than 4 weeks of treatment, an alternate day dosing schedule can be used. Once the skin condition has cleared, the dose will be carefully decreased in increments until the patient maintains improvement on a minimal dose.
Prednisone dosing
There are little data in the literature comparing or recommending the duration of therapy for corticosteroid use, and many practitioners are confused by the correct way to prescribe and taper the corticosteroids when needed. For example, when treating allergic contact dermatitis with oral corticosteroids, many experienced clinicians will treat with 40 to 60 mg per day for 2 weeks and will discontinue without taper. The risk involved with short-course therapy is rebound of the condition and not adrenal suppression. Some clinicians experienced in treating a widespread contact dermatitis for an adult prescribe prednisone 20 to 60 mg daily (depending on the extensiveness of rash and patient’s weight) for 7 days followed by a tapering dose for an additional 7 to 14 days.
If the rash affects more than 20% of the body surface area, oral prednisone at a dose of 0.5 to 1 mg/kg/day for 7 days is given, then the dose may be reduced by 50% in the next 5 to 7 days and then tapered and discontinued over the following 2 weeks (Basow, 2013). See Box 2-1 for considerations in systemic corticosteroid selection and Table 2-5 for corticosteroid tapering suggestions.
BOX 2-1 Considerations for Systemic Corticosteroid Selection
Age and weight of patient
Comorbidities: diabetes mellitus, hypertension, peptic ulcer disease, osteoporosis
Systemic infections: fungal
Short term (2–3 weeks) versus long term (months)
Need for vitamin D and calcium supplementation
Biphosphonates if on oral corticosteroids for more than 4 weeks
Known hypersensitivities
Drug interactions
Frequency of dosing: b.i.d. dosing has a more potent effect than QD dosing but should only be used for acute therapy of life-threatening illness.
TABLE Prednisone Taper Suggestions (Alternative to Medrol Pack) 2-5
DURATION OF TAPER DOSE AND AMOUNTPATIENT INSTRUCTIONS*
2 wk in decreasing daily doses 5-mg tabs, dispense #114
3 wk 10-mg tabs, dispense #70
4 wk (simplified)10-mg tabs, dispense #70
Day 1: Take 14 pills (70 mg), then decrease by 1 pill each day for 14 days
Week 1: 6 tabs QAM
Week 2: 3 tabs QAM
Week 3: 1 tab QAM
Week 1: 4 tabs QAM
Week 2: 3 tabs QAM
Week 3: 2 tabs QAM
Week 4: 1 tab QAM
Note: Calculations based on dosing 0.5–1 mg/kg for 150-lb (68 kg) adult.
*In addition to dosing, patient instructions should include: “To avoid recurrence of symptoms, do not stop taking pills without being instructed by your provider.”
Side effects
Side effects associated with oral corticosteroid therapy are usually dose and duration dependent. Some preexisting conditions are associated with increased risk, including diabetes, hypertension, dyslipidemia, heart failure, cataracts or glaucoma, peptic ulcer disease, concurrent use of nonsteroidal anti-inflammatory drugs, presence of infection, low bone density, and osteoporosis.
Consider the patient’s risk of fracture when prescribing oral prednisone. Bone loss is a serious, potential side effect of glucocorticoid therapy and needs to be monitored closely. To minimize bone loss, the following general principles should be kept in mind:
• The glucocorticoid dose and duration of therapy should be as low as possible.
• Topical therapy is preferred over systemic and should be used whenever possible.
• Weight-bearing exercises are recommended to prevent bone loss.
• Patients should avoid excess alcohol and smoking.
The American College of Rheumatology Task Force Osteoporosis Guidelines offer suggestions for patients taking any dose of glucocorticoids for greater than 3 months:
• Patients should maintain a total calcium intake of 1,200 mg per day and vitamin D intake of 800 IU per day through either diet and/or supplements.
• Bisphosphonates may be added based on the individual risks, which include gender, age, and fracture risk especially if the course of corticosteroids is intended for several months.
• Bone mineral density (BMD) testing is recommended at the initiation of glucocorticoid therapy and after 1 year for patients receiving any dose of glucocorticoids for greater than 3 months.
Avascular necrosis is a rare side effect that can be caused by either topical or systemic corticosteroids. As mentioned in the TCS section, a MRI scan may be ordered in the investigation of AVN symptoms. Patients should be advised that should signs and symptoms of AVN develop they should call their medical provider immediately.
Patient education and follow-up
When prescribing systemic corticosteroids, clinicians should educate patients for maximum outcomes and minimal side effects:
• Take prednisone with food.
• b.i.d. dosing will have a more potent effect than once per day dosing, but is not recommended for short-term treatment.
• Taking prednisone early in the morning helps diminish the possible side effects of hyperactivity or sleep disruption and decreases risk of adrenal suppression.
• Patients should be advised against stopping prednisone dosing abruptly and to continue medication until the entire taper course is complete to prevent rebound dermatitis.
All patients on long-term oral corticosteroids should be monitored for elevated blood sugar, hypertension, and weight gain after 1 month and then every 2 to 3 months. Complaints of eye pain, blurry vision, or halos may be indicative of increased intraocular pressures, and patient suffering from these complaints should be seen by an ophthalmologist. The provider should be most cautious in prescribing prednisone to patients who have the comorbidities of hypertension, diabetes, and obesity or to those who abuse alcohol or tobacco as these patients are already at high risk for developing infections, ulcers, and glaucoma. As long-term prednisone use is also associated with possible gastrointestinal perforation, an upper gastrointestinal series may be ordered if the patient has a history of peptic ulcer disease.
Patients who are on long-term prednisone therapy should be seen at least every 1 to 2 months for evaluation and more frequently if symptoms of possible complications arise. Close monitoring for possible side effects may be done in collaboration with the patient’s dermatologist.
Special Considerations
Corticosteroids in pregnancy
Practitioners will inevitably encounter pregnant women in their practice and must be familiar with medication safety when providing care to this group of patients. Prescribing medication during pregnancy can be particularly challenging given the insufficient data and research on the safety of medications during this period. Some skin conditions of the pregnant woman require topical and systemic treatment. The Food and Drug Administration (FDA) pregnancy categories (Table 2-6) should always be considered.
Topical corticosteroids. During pregnancy, women are generally advised to avoid the TCS treatments that they have come to rely on during flares. In general, topical medications are often considered first-line therapy for most; however, there are times when systemic agents may be more appropriate.
The data on the effects of TCS used during pregnancy are limited; however, the current available data on the safety of mildto-moderate TCS during pregnancy suggest a lack of association between their use by the mother and oral clefts, preterm delivery and fetal death as previously postulated. Therefore, the following recommendations for TCS use in the pregnant patient are as follows:
• Mild- to moderate-potency TCS should be preferred to more potent corticosteroids during pregnancy.
• Potent to very potent TCS should be used as second-line therapy for as short a time as possible.
• There is a small risk for fetal growth restriction when using potent/ very potent TCS during pregnancy.
• There is a theoretically higher risk of adverse events with use of TCS when used in high-absorption areas such as eyelids, genitals, and flexures.
Systemic corticosteroids. There are limited data on the potential teratogenic effects on the fetus, mainly because of the ethical issues
TABLE FDA Pregnancy Categories 2-6
CATEGORY DEFINITION
A Adequate and well-controlled studies have failed to demonstrate a risk to the fetus in the first trimester of pregnancy, and there is no evidence of risk in later trimesters.
B Animal reproduction studies have failed to demonstrate a risk to the fetus, and there are no adequate and well-controlled studies in pregnant women.
C Animal reproduction studies have shown an adverse effect on the fetus, and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
D There is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
X Studies in animals or humans have demonstrated fetal abnormalities, and/or there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience, and the risks involved in use of the drug in pregnant women clearly outweigh potential benefits.
involved in testing corticosteroids drugs in pregnancy. As mentioned previously, TCS are often considered the first line of therapy; however, when topical agents aren’t enough, the provider and patient must weigh the risk versus benefit of oral agents.
With oral glucocorticosteroids, there is a potential for increased risk of premature rupture of the membranes (PROM) and intrauterine growth restriction. There may also be an increased risk of pregnancy-induced hypertension, gestational diabetes, osteoporosis, and infection. They should be avoided during the first trimester when the hard palate is forming. When necessary, the lowest effective dose should be used.
Glucocorticosteroids are excreted in breast milk, but their use during lactation is deemed compatible by the American Academy of Pediatrics (AAP) if justified by the potential benefit to the health of the mother. An alternative is to discard the breast milk for the first 4 hours following ingestion of a dose of prednisone >20 mg.
CLINICAL PEARLS
j Avoid prescribing Lotrisone for diaper dermatitis. The high potency TCS in this product is not FDA approved for children and is too strong for the diaper area. In addition, the antifungal is too weak to be effective.
j When prescribing a potent or ultrapotent corticosteroid, patients should not use more than one 45-g tube per week. Pharmacists will not usually refill ahead of time, so calculate correctly for best results.
j The popular and conveniently packaged Medrol dose pack (methylprednisolone) is an insufficient short-term remedy that tends to prolong patients’ suffering due to rebound flaring.
j Mild- to moderate-strength TCS appear to be safe during pregnancy for short-term use. Avoid high-potency TCS if possible, especially during the first trimester. If high-potency corticosteroids are needed, as always, they should be used for the shortest amount of time.
ULTRAVIOLET LIGHT
Photobiology
In discussing the impact of the environment on skin health, UVR must be at the forefront to address the favorable benefits and negative impact of exposure. The basic concepts of photobiology are fundamental when assessing risks and benefits, and educating your patients (also see Chapter 23 Aging Skin). UV light is a form of radiation not visible to the human eye and is composed of three wavelengths: UVA, UVB, and UVC. These wavelengths differ primarily in the depth to which they penetrate the skin. The effects of UVB radiation can be immediate such as in sunburn or allergic skin reaction. UVA and UVB cause more long-term effects as in photoaging and skin cancer. UVC wavelengths are filtered by the ozone, do not reach the earth’s surface and do not contribute to skin damage.
It is understood that the ozone layer around the earth is trapping less UVR than ever before and allowing more harmful light to penetrate the earth. This is especially important to think about when in high altitudes, as less ozone means less filtering of UV light, making one more susceptible to sun damage. According to statistics from the Denver Visitors Bureau, at 6,280 ft or approximately 1 mile above sea level, there is 25% less protection from UVR. Thin ozone linked with increased outdoor leisure activities puts the population at higher risk. Unfortunately, tanning is still considered fashionable and desired by many despite the fact that it is a primary cause of melanoma and nonmelanoma skin cancers.
UVR is measured in wavelengths. UVA accounts for 95% of the sun’s UVR that reaches the earth and has two spectrums: UVA1 (340-400nm) and UVA2 (320-340nm). UVA1 has a longer wavelength and penetrates deeper in the dermis, resulting in greater biologic effect and DNA damage than UVA2. Interestingly, while UVA1 increases the risk for skin cancer and photoaging, it can also be utilized for therapeutic treatment of atopic dermatitis and other skin diseases. UVA rays also penetrate glass and clouds, increasing the risk for individuals who drive frequently for work or recreation and for those who do not use sunscreen as directed.
UVB rays are the middle-range wavelengths between 290 and 320 nm. They are found in combination with UVA in some tanning beds that contribute to the risk of this practice. Not only is UVB responsible for photoaging, sun tanning, and sunburns, it also causes ocular diseases such as cataracts, glaucoma, and macular degeneration. Paradoxically, specialized narrowband UVB is used in many dermatology settings to treat skin conditions such as psoriasis and can increase the risk of nonmelanoma skin cancers. Sun-protective measures are provided for eyes and noninvolved skin and are encouraged during all phototherapy treatments in dermatology offices.
UV Index
The UV Index (Figure 2-3) is a means of predicting the expected risk of overexposure to UVR from the sun. The National Weather Service calculates the UV Index forecast for most ZIP codes across the United States, and the Environmental Protection Agency (EPA) publishes this information. The UV Index is then accompanied by recommendations for sun protection and is a useful tool for planning sun-safe outdoor activities.
Ozone depletion, as well as seasonal and weather variations, causes different amounts of UVR to reach the earth at any given time. Taking these factors into account, the UV Index predicts the level of solar UVR and indicates the risk of overexposure on a scale from 0 (low) to 11 or more (extremely high). A special “UV alert” may be issued for a particular area, if the UV Index is forecast to be higher than normal.
Sun Protection
Public education regarding skin cancers and the photodamaging effects of the sun has led to increased use of sunscreens in many populations. Australia is one country that has made great strides in educating the public about sun-protective measures. In 1980, it launched one of the most successful health campaigns in its history. The Slip Slop Slap Seek and Slide campaign is credited as playing a key role in the dramatic shift in sun protection attitudes and behaviors over the past two decades. Basal cell and squamous cell carcinomas have also decreased in Australia as well. Unfortunately, melanoma incidences continued to increase despite the attitude and behavioral change which may stress the importance of the multifactorial dimensions of UV sun exposure.
Sun avoidance during the hours of 10 a.m. and 4 p.m. is recommended. UVR is magnified by 85% when it is reflected off snow. Cloud cover only minimally decreases the intensity of the sun. Loose-fitting clothes and tightly woven fabrics in long pants and long shirts offer the best source of sun protection. Although we have made advances in educating patients regarding the use of sunscreen in the United States, more efforts are needed to encourage patients to use sun-protective clothing and sunglasses and to seek shade more often. Providing the public with outdoor tents in gathering places such as parks and beaches is one example of such an effort.
Sunscreen
Sunscreens are topical agents that lessen the effects of UV light by reflecting, scattering, or absorbing the light (Figure 2-4). Their efficacy is determined by their ability to protect against the erythema caused by both UVA and UVB. Sun-protective factor (SPF) is the unit of measure used to describe how well a sunscreen can protect the skin from the harmful effects of the sun. The SPF for each sunscreen is determined in a laboratory by comparing an individual’s response to sun with and without sunscreen use. Dermatologists recommend patients choose sunscreen with an SPF of 30 or higher. The average adult should apply at least 2 tablespoons or a “shot glass full” on sun exposed areas of the body whenever outdoors for any length of time. Sunscreen should be reapplied every 2 hours or after sweating or swimming regardless of latitude.
On June 14, 2011, the U.S. FDA announced new requirements for sunscreens currently sold. Previously, there was no standard applied for SPF designation. Currently, the FDA requires the use of the term broad spectrum to be included on any sunscreen packaging which claims to prevent sun damage. This means that the product provides both UVA and UVB protection for the skin. Only broad-spectrum
Chemical sunscreens
Chemical sunscreens act to weaken ultraviolet radiation before it causes damage to DNA in the nuclei of skin cells. Chemical sunscreens absorb ultraviolet radiation within the spaces between the skin cells, convert it into specific chemicals, and release the energy as insignificant amounts of heat. The higher the SPF rating of the chemical sunscreen, the longer it takes for sunlight to damage the skin.
Physical sunscreens
Physical sunscreens prevent ultraviolet radiation from entering the skin at all. Physical sunscreens form a thin film of inert metal particles (zinc oxide, etc.) that reflect back into the atmosphere.
sunscreens with an SPF value of 15 or higher can claim to reduce the risk of skin cancer and early skin aging if used as directed with other sun protection measures. Non-broad-spectrum sunscreens and broad-spectrum sunscreens with an SPF between 2 and 14 can only claim to help prevent sunburn.
Manufacturers cannot label sunscreens as “waterproof” or “sweatproof,” because these claims overstate their effectiveness. Water resistance claims on the front label must indicate whether the sunscreen remains effective for 40 minutes or 80 minutes while swimming or sweating, based on standard testing.
Sunscreens also cannot identify their products as “sunblock” (Figure 2-4) or claim to provide sun protection for more than 2 hours without reapplication. The product’s label must not claim to provide protection immediately after application.
All sunscreens must include standard “Drug Facts” information on the back and/or side of the container. The FDA also mandates that sunscreen labels recommend reapplying sunscreen at least every 2 hours. (Cong. Rec., 2011)
Broad-spectrum sunscreens include at least one of the following ingredients: zinc oxide, titanium dioxide, avobenzone, or ecamsule to provide adequate UVA protection (Table 2-7). Helioplex is the name brand of a sunscreen stabilizer owned by Neutrogena. A stabilizer ensures the sunscreen ingredients are more photostable, preventing chemical breakdown when exposed to the sun. Only Loreal has the rights to the chemical ecamsule that is sold as Mexoryl sunscreen. Europe has several other sunscreen ingredients available that are not FDA approved.
FIG. 2-3. The ultraviolet index forecasts the strength of the sun’s harmful rays. The higher the number, the greater the chance of sun damage.
FIG. 2-4. Illustration showing how sunscreens work.
TABLE Sunscreen Ingredients 2-7
INGREDIENT
Physical agents
Titanium dioxide
Zinc oxide
Chemical absorbers
Aminobenzoic acid (PABA) •
Butyl methoxydibenzoylmethane (Avobenzone) • Dioxybenzone
Ecamsule (Mexoryl SX) • Ethoxyethyl p-methoxycinnamate (cinoxate) • Homomenthyl salicylate (homosalate)
• Octyl methoxycinnamate (octinoxate) •
Oxybenzone
Octocrylene ••
••
Sulisonbenzone
Ethoxyethyl p-methoxycinnamate (cinoxate)
UVA, ultraviolet A; UVB, ultraviolet B.
Allergies to sunscreens
Practitioners often hear from patients that they are allergic to sunscreens. The most common reactions reported with the use of sunscreens are allergic contact dermatitis, photoallergic contact dermatitis, irritant contact dermatitis, and acne. There are two categories of sunscreens, “inorganic” or “physical” sunscreens, which include zinc oxide- and titanium dioxide-based products, and “organic” or “chemical” sunscreens, which include 15 different chemicals, including para-aminobenzoic acid (PABA) and benzophenones. PABA is no longer used in the manufacturing of most sunscreens today due to the incidence of allergic reactions. Oxybenzone, a type of benzophenone, is frequently used in sunscreens today and is now also known to cause contact dermatitis. Photoallergy has not been reported with the inorganic sunscreens; therefore, allergy-prone patients should be advised to choose these products. Examples of sunscreen brands that contain zinc and titanium dioxide as either the sole ingredient or main ingredient are Badger, Vanicream, Solbar zinc, Neutrogena Sensitive Skin, and Blue Lizard.
Sunscreen controversies
Oxybenzone, Retinyl Palmitate. Sunscreens have been approved by the FDA since 1978 and now cannot be sold without extensive testing. There has been controversy over several sunscreen ingredients,
including both oxybenzone and retinyl palmitate. It has been claimed by some groups that oxybenzone accumulates in the body and can interfere with hormone levels. Other studies have demonstrated that no appreciable risk exists. Retinyl palmitate has been accused of causing free radicals, therefore increasing cancer risk. There are no published studies proving that sunscreen or their ingredients are toxic to humans or hazardous to human health.
Vitamin D. With improved sunscreens, there is now increased media attention and concern in the rise of vitamin D deficiencies resulting from sunscreen use. Much of this controversy is fueled by the very powerful tanning industry, who extols the benefits of tanning booths as a source of vitamin D. In fact, most individuals do not apply their sunscreen adequately or frequently enough to prevent sunburn or block the synthesis of vitamin D.
Given the risk of DNA damage to the skin and photocarcinogenesis from overexposure to UV light, it is advised that people focus on acquiring their daily recommendation of vitamin D from food or supplements. Vitamin D3 (cholecalciferol/colecalciferol) is made by the body when UVB radiation interacts with 7-dehydrocholesterol that is present in skin. The amount of sun exposure required for this interaction is minimal, and can be satisfied by less than 15 minutes of exposing the face, hands, and neck during nonpeak hours daily. Vitamin D3 is also found in some food products such as meat, oily fish, and fortified processed foods. It is also found as a dietary supplement. Vitamin D3 is converted into its active form, calcitriol, by the kidneys and liver and helps form and maintain bone. Patients who are concerned about their vitamin D levels should discuss their options with their primary care provider.
Oral photoprotection
Polypodium leucotomos is the most studied form of oral photoprotection. Polypodium leucotomos is an extract from a fern grown in Central America. It has been shown to decrease erythema, DNA damage, UV-induced epidermal hyperproliferation, and mast cell infiltration in humans. However, one study suggested that Polypodium leucotomos only offered an SPF of 3, which is insufficient for most people. There may be a role for this oral product for patients with photosensitivity from lupus or other photoinduced conditions as a supplement to sunscreens. It should not to be used as a replacement for sun-protective clothing and sunscreen. This dietary supplement is sold as brand names Heliocare and FernCarePLE.
Clothing
Loose-fitting clothes and tightly woven fabrics in long pants and long sleeved shirts offer the best source of sun protection. A typical cotton T-shirt offers an SPF of about 5, and a wet T-shirt offers much less protection than a dry one. Darker colors may add a bit more protection than lighter ones. Hats with wide brims are highly recommended. Fashionable sun-protective clothing with the minimum standard ultraviolet protection factor (UPF) of 40 to 50+ is available by several companies such as Coolibar, Radicool Australia, Sunday Afternoons, Sun Precautions, Tilley Endurables, Tuga sun protective sunwear, and Wallaroo hat company.
Sunglasses
UV damage to the eyes is cumulative just as it is for the skin, so it is important to begin wearing sunglasses at an early age. Children’s eyes are still developing and at higher risk for damage. Choose sunglasses that provide full protection against UV light. The coating used for UV protection is clear; so a tinted sunglass will not necessarily be more protective. Patients should look for a label or a sticker as follows:
• Lenses block 99% or 100% of UVB and UVA rays;
• Lenses meet ANSI Z80.3 blocking requirements. (This refers to standards set by The American National Standards Institute); and/or
• UV 400 protection (blocks light rays with wavelengths up to 400 nm, which means that your eyes are shielded from even the tiniest UV rays).
Sunless Tanning
There are no FDA regulations regarding sunless tanners and bronzers. These terms typically refer to products that provide a tanned appearance without exposure to the sun or other sources of UVR. The most common ingredient in sunless tanners is dihydroxyacetone (DHA), a color additive that darkens the skin by reacting with amino acids in the skin’s surface. Bronzers are made from color additives approved by the FDA for cosmetic use. They stain the skin for a short time when applied and can be washed off with soap and water. DHA is being used commonly in salons and advertised as Spray Tan, but “misting” application has not been approved for use by the FDA. DHA is restricted to external application and should not be applied to the lips or any surface covered by mucous membranes. When using DHA containing products, it may be difficult to avoid exposure to the eyes, lips, or mucous membranes. Those who choose to use spray-tanning booths should then be sure to protect their eyes, lips, and mucous membranes from the spray.
CLINICAL PEARL
j Previously unseen seborrheic keratoses will become more visible as the keratotic cells absorb the sunless tanning chemical.
Tanning pills
Tanning pills contain canthaxanthin, a color additive similar to β-carotene, the substance that gives carrots their orange-like color. The FDA has approved some additives for coloring but they are not approved for use in tanning agents. Canthaxanthin, at high levels, can appear in the eyes as yellow crystals, which may cause injury and impair vision. There have also been reports of liver and skin problems.
Patient Education and Follow-up
It is important to teach patients that UVA and UVB light cause photoaging and is a known risk factor for melanoma, nonmelanoma skin cancers, and eye damage. UVR, from the sun and from tanning beds, is classified as a human carcinogen, according to the U.S. Department of Health and Human Services and the World Health Organization. Daily sunscreen application and UV-protective clothing and sunglass usage should be recommended to all patients. General UV protection advice should include the following (see Sun Safety tips for patients in Chapter 8):
• Emphasize choosing SPF 30 or greater.
• If acne prone, advise oil-free and noncomedogenic products. Most brand-name products marketed for the face are safe.
• Apply at least 20 minutes before exposure and reapply every 2 hours, or after swimming or excessive sweating.
• Sunscreens are not recommended for babies under 6 months of age as they have a larger body surface area and may absorb more active chemicals that are in sunscreens than is safe. Instead, emphasize sun avoidance and sun-protective clothing.
• Sunscreen spray should not be inhaled as the safety of the effects on mucous membranes and the lungs have not been determined. When sprayed, sunscreen may not afford adequate protection as much of the product escapes into the air.
• The expiration of sunscreens is 3 years after the purchase date. Discard before the expiration date if it has been exposed to extreme heat.
• Avoid tanning and tanning booths.
• Use extra caution near water, snow, and sand.
• Get vitamin D safely.
READINGS
Basow, D. S. (Ed.). (2013). Management of Contact Dermatitis. www.UpToDate Berth-Jones, J. (Ed.). (2010). Topical therapy. Rook’s textbook of dermatology (8th ed., pp. 73.1–73.52). Chichester, England: Wiley-Blackwell.
Chi, C., Wang, S., Mayon-White, R., & Wojnarowska, F. (2013, September 4). Pregnancy outcomes after maternal expsosure to topical corticosteroids; A UK population-based cohort study. Journal of the American Medical Association, E1–E7.
Craig, K., & Meadows, S. E. What is the best duration of steroid therapy for contact dermatitis (rhus)? The Journal of Family Practice, 55, 166–167.
Cong. Rec. (2011). FDA Sunscreen drug products for over the counter use.
DelRosso, J. Q., & Kircik, L. H. (2012, December). Not all topical corticosteroids are created equal! Optimizing therapeutic outcomes through better understanding of vehicle formulations, compound selection, and methods of application. Journal of Drugs in Dermatology, 11, 5–8.
FDA: FDA Sheds Light on Sunscreens. www.fda.gov/forconsumers/consumerupdates/ ucm258416.htm
Ference, J. D., & Last, A. R. (2009, January 15). Choosing topical steroids. American Family Physician, 79, 135–140.
Gilchrest, B. (2008). Sun exposure and vitamin D sufficiency. American Journal of Clinical Nutrition, 88(suppl), 570S–577S.
Grossman, J. M., Gordon, R., Ranganath, V. K., Deal, C., Caplan, L., Chen, W., & Saag, K. G. (2010). Recommendations for the prevention and treatment of glucosteoid induced osteoporosis [Arthritis Care Res]. American College of Rheumatology, 62, 1515–1526.
Gupta, R., High, W. A., Butler, D., & Murase, J. E. (2013). Medicolegal aspects of prescribing dermatological medications in pregnancy. Seminars in Cutaneous Medical Surgery, 32(4), 209–216.
Habif, T. P. (2010). Topical therapy and topical corticosteroids. In clinical dermatology. A color guide to diagnosis and therapy (5th ed., pp. 75–90). China: Elsevier.
Kelly IV, J. D., & Wald, D. (2012). Femoral head avascular necrosis. Medscape http://emedicine.medscape.com/article/86568-overview
Lebwohl, M., Heymann, W., Berth-Jones, J., & Coulson, I. (2006). Treatment of skin desease. Comprehensie therapeutic strategies (2nd ed.). London: Mosby.
Middelkamp-Hup, M. A., Pathak, M. A., Parrado, C., Goukassian, D., & Riuz-Diaz, F. (2004, December). Oral Polypodium leucotomas extract decreases ultraviolet induced damage of the human skin. Journal of the American Academy of Dermatology, 51, 910–918.
Romain, P. L. (Ed.). (2013). Use of anti-inflammatory and immunosuppressive drugs in rheumatic diseases during pregnancy and lactation. UpToDate. March 4, 2014.
Skin Cancer Foundation, Skin Cancer Prevention. www.skincancer.org/prevention/ sun-protection/prevention-guidelines
Zirwas, M. (2012, December). Allergy to topical steroids. Journal of Drugs in Dermatology, 11, 9.
CHAPTER