Acknowledgements
The development and publication of the book was substantially supported by a grant from the German Research Foundation provided to the first author (DFG; No. 470515295). This support is gratefully acknowledged. The Faculty of Medicine, Heinrich-Heine-University, offered an ideal work environment to the first author. Both authors are deeply grateful to Pia Schneider who with her excellent skills contributed to the preparation of the manuscript during several stages of development. Draft versions of chapters were sent to colleagues for informal review, and their comments were highly appreciated. Our special thanks go to Peter Angerer, Chantal Brisson, Nico Dragano, Christine Fekete, Siegfried Geyer, Timothy A. Matthews, Mariann Rigó, Wendie Robbins, Reiner Rugulies, Andrew Steptoe, Töres Theorell, Pablo Verde, and Morten Wahrendorf. Furthermore, we thank the team at Oxford University Press, in particular Rachel Goldsworthy and Janine Fisher, for a most productive collaboration.
Düsseldorf and Los Angeles Johannes Siegrist and Jian Li
PART I: GENERAL BACKGROUND
1 Psychosocial occupational health: A new perspective
The psychosocial dimension of work and its relationship with health
Scientific disciplines and challenges of psychosocial occupational health
Summary
Relevant questions
2 The changing nature of work and employment in modern societies
Historical background
The process of economic globalization
Digitization, automation, and artificial intelligence
The growth of nonstandard employment
Tensions between economy and ecology
Summary
Relevant questions
PART
II:
ASSESSING PSYCHOSOCIAL WORK ENVIRONMENTS AND THEIR RELAT IONSHIP WITH HEALTH
3 Theoretical concepts of psychosocial work
The role of theory in psychosocial occupational health
Main theoretical models and new developments
Stress-theoretical and behavioural pathways
Summary
Relevant questions
4 Measurement, methods, data collection, and study designs
Measuring psychosocial work environments
Data collection and study designs
Summary
Relevant questions
5 Data analysis and statistical modelling
Regression analysis, structural equation, and multilevel modelling
Causal analysis
Systematic review and meta-analysis
The ethical dimension of scientific research
Summary
Relevant questions
PART III: EFFECTS OF WORK ON HEALTH
6 Evidence from cohort studies
Social distribution of psychosocial work environments
Effects on major chronic diseases
Effects on other health outcomes
Work and unequal health: mediation and moderation
Summary
Relevant questions
7 Evidence on psychobiological pathways
Study designs with stress-related biomarkers
Psychosocial work environments and stress-related biomarkers
Future directions
Summary
Relevant questions
PART IV: EFFECTS OF HEALTH ON WORK
8 Working with a disease or disability
Health and work trajectories
Return to work with chronic disease or disability
Summary
Relevant questions
9 Organizational contexts and social change in rehabilitation
Legal and structural conditions
Empowering people with chronic disease or disability
Some suggestions for further development
Summary
Relevant questions
PART V: PREVENTION: THE POLICY DIMENSION
10 Prevention and health promotion at work: the organizational level
From risk assessment to workplace health promotion
Health-related intervention effects
Summary
Relevant questions
11 Healthy work in a national and international perspective
Impact of labour and social policies on occupational health
The Global South as a future challenge
Summary
Relevant questions
Psychosocial occupational health
A
new perspective
1.1 The psychosocial dimension of work and its relationsh ip with health
In the twenty-first century, paid work performed by humans continues to play a crucial role. Despite far-reaching technological progress, large parts of the adult population globally are engaged in recurrent economic activity by participating in the labour market. While pronounced levels of long-term unemployment and informal employment are still a serious concern, especially so in low- and middle-income countries, formal employment involving an occupational position or job is the predominant pattern in economically advanced and some rapidly developing countries. For instance, in OECD countries, around seventy-seven per cent of the work age population (15–64 years) were participating in the labour market in 2020 (OECD 2021). Overall, access to an occupational position mainly depends on qualification and training. The primary significance of paid work is due to its capacity of producing a double benefit. For the working person, participation in the labour market offers a continuous income and basic social protection: it confers social status; it promotes the development of skills and achievements; and despite its strenuous demands, it often generates experiences of control, reward, meaning, and satisfaction. Notably, these benefits vary substantially according to the quality of work and employment. For society, the benefits of work consist in a general advancement of welfare and social progress, economic growth, and improvement in tangible living conditions. Again, these benefits vary substantially and most markedly according to the degree of wealth distribution across society. It is this combination of personal and societal benefit that accords a unique primacy to the work role in modern societies, thus structuring and determining the adult life-course over several decades. Given their significant role and long-term impact, work and employment matter for human health and well-being in rather substantial ways. To analyse the associations of modern work with the health of working people and to discuss the practical implications of this knowledge is the main aim of this book.
1.1.1 The impact of work and employment on health
It is not easy to determine the impact of work and employment on health. One reason of this difficulty concerns the fact that the occupational sphere and the broader environmental sphere are intimately intertwined. Take for example the case of climate change and global warming. This broader environmental challenge can affect the health of workers by increasing exposure to heat at work with related adverse consequences. It can also contribute
to reduced health by causing redundancy and forced occupational mobility due to climateinduced migration and dislocation of companies and organizations (Kjellstrøm et al. 2020). Or remember the huge burden on workers’ health due to the COVID-19 pandemic, whereby infection risks at the workplace increased, resulting in an elevated burden of morbidity and mortality. In addition, poor mental health resulted from job loss and income reduction, social isolation, and distant work induced by lockdown measures and the pandemic’s economic consequences (International Labour Organization 2022).
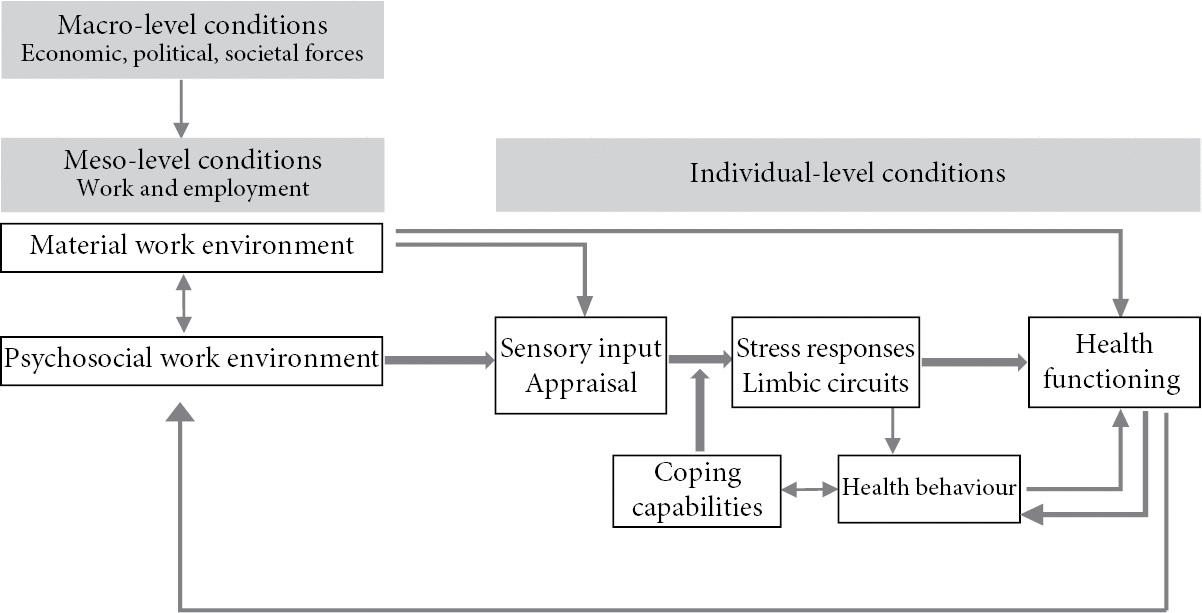
To disentangle these intimate links of the broader environment with the work environment and their impact on health, three different levels of analysis can be distinguished and examined: the macro-, meso-, and micro-level. At the macro-level of analysis, a broad range of large-scale, distant structural conditions is identified that exert their impact on intermediary factors operating in people’s more proximate living and working environments. Macro-level factors are generally defined in geographical, economic, epidemiologic, legal, or policy terms. Examples include climate change (geography), global financial crisis (economics), epidemic health risks (epidemiology), international trade agreements (law), or national labour market programmes (policy). Rather than acting directly on individuals’ behaviour, health, and well-being, they influence intermediate, proximate contextual conditions to which individuals are exposed. These conditions are located at the meso-level of analysis. Work environments, as defined by organizations, enterprises, other work settings or distinct employment groups, are the main category of meso-level conditions in our approach, and exposure to these conditions defines the main pathway to workers’ health risks and health gains. Indirect effects of macro-level factors on health via meso-level conditions were already illustrated in case of climate change and COVID-19. Similarly, the global financial crisis did not directly affect workers’ health, but it had deleterious effects on employment opportunities, increasing downsizing, redundancy, and income loss, and these latter factors increased workers’ risk of poor health (Riumallo-Herl et al. 2014). Or take the case of transnational supply chains. Improved legal regulations exert their beneficial effects on workers primarily through strengthening safety at work, reducing the number of unhealthy workplaces, or limiting excessive workload (Labonté et al. 2011). In conclusion, macro-level factors originating from the broader environment are important for health by exerting their adverse effects on intermediary, proximate conditions. These conditions are located at the meso-level of work environments within organizations, where they operate as risk factors or protective conditions of workers’ health. Conceptually, a micro-level aspect can be distinguished from meso-level work environments, focusing on individual workplaces with their specific features. However, research dealing with health effects on working populations is mainly concerned with macro- and meso-level environments. Importantly, these work environments are experienced as exposures by working people, and their ways of dealing with work tasks and job conditions, their coping efforts, and cognitive, affective and behavioural responses exert a substantial impact on health outcomes (see 1.1.2.2., Fig. 1.1. and Chapter 3). While the analysis of individual differences in outcomes is of considerable interest for disciplines such as psychology (Cunningham and Black 2021) and genetics (Conl ey and Fletcher 2017), it has been less extensively addressed in occupational epidemiology, sociology, demography, or economics, where downstream effects of macro- and meso-level
conditions on population health risks define the main focus.
A further difficulty of determining the impact of work and employment on health relates to the multi-faceted nature of work environments. Traditionally, their material dimensions received main attention in occupational medical research as well as in safety sciences. Material determinants of health are mainly transmitted via physical, chemical, and biological pathways (‘material work environment’). On one hand, the work environment or workplace contains toxic substances, such as asbestos, cadmium, benzene, and particulate matters. It produces gases or fumes, and workers are exposed to heat or cold temperature. Dangerous and risky work increases the occurrence of injuries. These hazards are analysed by toxicology and related basic sciences of occupational medicine. Experimental evidence, supported by epidemiological findings, shows that these hazards exert causal effects on workers’ health. Physical work environments additionally contribute to the burden of occupational diseases by job tasks that require repetitive movements or heavy lifting, stressing the musculoskeletal and cardiovascular systems. Large parts of today’s workforce are required to exert repetitive movements, and even with improved work settings (e.g. computer work) these demands increase the risk of musculoskeletal and cardiovascular complaints and disorders in the long run. The same holds true for excessive sedentary work with adverse consequences for cardiovascular functioning. On the other hand, there are occupational conditions with adverse effects on health whose direct causal pathways are either still under examination or act in concert with other work-related circumstances. Noise is one such hazard that affects health via excessive auditory stimulation, but also via psychological, autonomic nervous system-mediated factors of irritation or anger. Shift work is another example, where health effects are partly due to disturbed circadian biological rhythms, partly due to the impact of conflicts of adapting changed work time patterns to the individual living conditions (e.g. disturbances with family life) (for literature reviews on these work hazards for health, see Bültmann and Siegrist 2020; Theorell 2020). Equally so, long working hours, a main occupation health risk factors in todays’ world of work, can impair health by the length and intensity of time exposed to adverse working conditions as well as by an impact on reduced recovery and relaxation opportunities (World Health Organi zation and International Labour Organization 2021).
Importantly, exposure to occupational factors is not restricted to the material work environment, but it extends to the psychosocial work environment. Here, health is negatively affected via sensory input of signals emanating from work situations that are perceived and appraised as challenging or threatening, triggering negative emotions of irritation, anger, anxiety, or helplessness, and stimulating psychobiological stress responses. These psychosocial work environments and their non-material effects on health, mediated by psychobiological processes, are of central importance to our analysis and will be dealt with extensively throughout this book. The spectrum of psychosocial aspects at work is very broad. It includes features of job tasks that are positively evaluated by workers, given their importance, meaning, interest, and challenge, but that may overtax workers’ efforts due to their intensity and duration, or due to recurrent interruptions and adaptive changes. Healthcare work is an example where chronic work overload in a professional activity that is performed by workers who are strongly motivated and highly appreciated often results in
feelings of exhaustion and burnout. Monotonous jobs are another example where the task profile per se is not unhealthy, but where the working person’s awareness of lack of stimulation, control, and personal agency provokes feelings of powerlessness, frustration, and stressful tension. Yet, many work situations produce conflicts between superiors and subordinates, and between co-workers and colleagues. Competition, aggression, unfair behaviour, as well as lack of trust, support, and solidarity are just some of the many manifestations of conflicts at work causing tension, anger, disappointment, and stressful arousal. As will be detailed in later chapters, difficulties and failures of organizational and human resource management contribute to work overload, unbalanced work division, poor work performance, and job dissatisfaction. Another source of stressful experiences at work concerns contextual economic and labour market-related conditions, such as high risks of downsizing, redundancy, and job loss, or lack of promotion prospects. In all these cases, an adverse psychosocial work environment threatens basic psychological needs of the working person, such as the need for security, autonomy, and self-direction; the need for successful agency and self-esteem; the need for trust, belonging, and support; and the need for appreciation, respect, and fair treatment. Need frustration is associated with pronounced negative emotions and psychobiological stress responses (see Chapter 3). Despite the complexity of its manifestations the psychosocial work environment displays an essential common feature in all types of job: distinct from the material work environment that exerts its direct health effects on the working person’s organism, in all instances of a psychosocial work environment, it is the working person with his or her perceptions, appraisals, emotions, motivations, and behavioural responses that influences the final stress response that matters for health. This process is termed ‘coping’ (see 1.1.2.2 and Chapter 3). Therefore, despite an overriding impact of situational (‘extrinsic’) factors, person characteristics (as ‘intrinsic’ factors) contribute to the health effects at individual level.
Summing up the arguments, we can state that analysing the impact of work and employment on health is a challenging task, given the difficulty of separating the work environment from the broader environment, and given the multifaceted nature of work environments. The former challenge is addressed by applying a multilevel approach where conditions operating at the macro-, meso-, and micro-level are distinguished. To tackle the second challenge, an interdisciplinary perspective is required that enables a combined study of material (physical, chemical, biological) and psychosocial (psychological, social) aspects of work environments. As health is the central outcome of interest, this interdisciplinary perspective is best realized in the frame of a biopsychosocial model of health and disease (En gel 1977). In this model, the three spheres of organism (molecules, genes, receptors, organs), individual person (emotions, cognitions, motivations), and social environment (macro-, meso-, micro-level conditions) are assumed to be interconnected by bi-directional pathways, reflecting the systemic nature of dynamic interactions between person and environment. Importantly, a main pathway is assumed to lead from the social environment (work demands) to the individual person (coping with these demands), whose action affects the health of the organism (through duration and intensity of psychobiological stress responses). This pathway will be of main interest in this book (see Part III). Yet, an alternative pathway is of interest as well. Impaired health at the level of the organism (e.g. reduced physical functioning) can
affect the cognitions, emotions, and motivations of individual persons (e.g. depressed mood, reduced achievement motivation), and can impair the opportunities of working and being employed (e.g. inability to return to work). Obviously, this alternative pathway deserves primary attention as well, particularly in view of an aging workforce where chronic disorders are prevalent and exert huge effects on work performance and employability (see Part IV).
1.1.2 The psychosocial work
environment
1.1.2.1
Historical development
The term ‘psychosocial work environment’was proposed some fifty years ago as an umbrella concept representing the complexity of non-material working conditions with potential relevance for health (Levi 1971). It was not by chance that this occurred in Sweden as this country, and in particular Stockholm University and the Karolinska Institute, had been conducting pioneering occupational health research since the late 1960s. One aspect of research, led by psychiatrists and psychologists, focused on health effects of piecework and time pressure at work. Probably for the first time, effects of underload and overload on stress hormones and cardiovascular function were analysed in experimental studies (Frankenhaeuse r and Gardell 1976). Another aspect was concerned with the impact of low control and other organizational constraints on workers’ attitudes and behaviour, applying concepts from work and organizational psychology (Gardell 1971). In a third aspect, epidemiologists included questions on life events and working conditions in cohort studies on risk factors for coronary heart disease and demonstrated the first evidence on their association (Theorell et al. 1975). A couple of years later, Robert A. Karasek, an American sociologist, went to Stockholm to collaborate with this epidemiological research team, led by cardiologist Töres Theorell. This was the first opportunity to test a theoretical model of a stressful psychosocial work environment, termed ‘demand-control’, developed by Karasek, with regard to its ability to explain elevated health risks. This model assumes that job tasks characterized by high psychological demands in combination with low control and decision latitude generate health-adverse stress reactions (Karasek 1979; see Chapter 3). As a result of this collaboration, preliminary evidence of the model’s contribution towards explaining elevated risks of cardiovascular disease was obtained (Alfredsson et al. 1982; Karasek et al. 1981). These are prominent examples of early research on psychosocial work environments and health in Sweden and other Scandinavian countries that had a significant impact on the shape of this field of research, as will be documented in later chapters of the book.
Yet, this does not mean that Scandinavian researchers were the only pioneers in this domain. In fact, several far-reaching discoveries were made by scientists in the US and in the United Kingdom, even if the term ‘psychosocial work environment’ was not used. One of the first landmark studies was published as early as 1958 by cardiologists Meyer Friedman and Ray Rosenman as first authors. They documented a striking association between a period of excessive psycho-mental workload, called ‘occupational stress’, among tax accountants and increased levels of cholesterol as well as altered blood clotting (Friedman et al. 1958). Another study revealed changes in blood lipids among workers who lost their job (Kasl et al. 1968). It is of interest to note that the cardiovascular system was the main target of analysis
in these studies. In the 1960s, extensive animal experimental research laid scientific ground for the pathogenic role of chronic stress in the development of high blood pressure, atherogenic lipids, and other determinants of coronary atherosclerosis, the main risk factor of ischaemic heart disease (IHD) (Henry and Cassel 1969; Henry and Stephens 1977). At the same time, epidemiological studies documented elevated risks of IHD in population groups characterized by stressful circumstances, such as frequent occupational change (Syme et al. 1 964), occupational mobility (Kaplan et al. 1971), inconsistency of occupational and educational status (Shekelle et al. 1969), and low occupational position (Cassel et al. 1971). These pioneer studies preceded a stage of substantial scientific progress starting in the final decades of the twentieth century that will be documented in later parts of the book.
However, one of the most influential contributions to the development of psychosocial occupational health originates from Great Britain, and more specifically from the Whitehall II study inaugurated by epidemiologist Michael Marmot (Marmot et al. 1991). Based on data obtained from an earlier occupational cohort, the Whitehall I study of civil servants, Marmot and colleagues documented a consistent, steep social gradient of morbidity and mortality, most pronounced in case of IHD, according to the civil servants’ occupational position (Mar mot et al. 1978). The Whitehall II study was set up to explain this fundamental pattern of social inequality in health. In fact, over the past three decades, the research consortium of the Whitehall II study produced a unique wealth of outstanding innovative research that promoted evidence on the psychosocial work environment as an important determinant of health to the forefront of international science. Several parts of this book capitalize on this rich collection of new knowledge.
Taken together, these research findings from different disciplines contributed to the construction of a biopsychosocial model of cardiovascular disease, as they were able to link factors related to the social environment (and in particular the work environment) to the individual person experiencing stressful encounters, and to biomedical indicators of elevated risk of cardiovascular disease (see Chapters 3, 6, 7). For a long time, cardiovascular disease (and more specifically IHD) was the prototype of an evidence-based biopsychosocial human disorder, but more recently, metabolic disorders, mental disorders, and different physiological systems (inflammation, immune competence) contributing to these disorders were integrated into this analysis. Against this background, we now ask how the notion of ‘psychosocial work environment’can be elaborated in a more convincing way.
1.1.2.2
Proposed model
Proposing a model that specifies levels and pathways of analysis is one way of depicting the complex notion of ‘psychosocial work environment’. Figure 1.1 represents one such model. It integrates the core arguments mentioned above, and it adds precision using arrows indicating the direction of proposed effects. In detail, factors located at the macro-level are assumed to influence the work and employment contexts and settings located at the mesolevel. These contexts and settings contain the multifaceted material and psychosocial work environments, and they are considered the main exposures to workers’ health outcomes. As can be seen, at the individual level, effects on health are transduced to the organism by different channels, partly via physical, chemical, and biological hazards, and partly via
sensory input. This latter pathway is crucial in case of psychosocial work environments, where sensory input is cognitively appraised and emotionally evaluated, and where the individual worker’s coping activity impacts on the physiological and behavioural stress response. Two qualifying statements are important at this stage. Firstly, the way individual workers experience a psychosocial work environment varies according to their learning history, their coping capabilities, and their genetic and personality profile. Therefore, the cognitive and affective appraisal of an identical exposure by a group of workers is likely to reveal considerable individual differences. This means that individual appraisals of psychosocial work environments represent a mixture of ‘objective’, situation-related, and ‘subjective’, person-related information. This fact points to a central methodological challenge in view of a widely established research approach that assesses exposure to a psychosocial work environment via self-rated information reflecting workers’ experiences as subjective evaluations. A discussion will be devoted to this methodological problem in later parts of the book (see Chapters 4 and 5). A second argument concerns the question of whether sensory input of environmental information always reaches the level of consciousness, as proposed by cognitive stress theory (Lazarus and Folkman 1984), or whether this input bypasses conscious appraisal under certain conditions, by directly affecting limbic structures and the hypothalamus that transduces afferent neocortical input into signals of the autonomic nervous system. Neuroscientific evidence on the brain’s information processing supports this latter assumption (LeDoux 1996). Only a limited proportion of the total amount of information input reaching the brain every second is subjected to cognitive awareness, and this input is prioritized according to novelty and threat. Redundant information confirming previous experience more easily bypasses the threshold of conscious awareness. Thus, repeated, routinized experience of a psychosocial work environment is more likely to bypass this threshold than new, threatening sensory input that interrupts the stock of habituated previous knowledge (see Chapter 3).
The core link from stress responses to health functioning depicted in Figure 1.1 is hypothesized to involve a direct and an indirect pathway. The direct pathway from sensory input to an activated stress response matters most, and research has devoted its major interest to unravelling this crucial process. Importantly, the quality and intensity of a stress response is modified by the working person’s coping capability. Yet, extrinsic and intrinsic constraints often limit successful coping efforts. Under these latter circumstances, an indirect pathway is often mobilized. Here, people tend to reduce their emotional strain by the consumption of stress-relieving substances. This consumption may offer an instantaneous relief but, as it does not target the sources of stressful experience, there is a considerable risk of chronic use resulting in addictive health-damaging behaviour (smoking, alcohol or drug consumption; unhealthy food; physical inactivity; sedentary behaviour) (see Chapter 3). Ultimately, these direct and indirect pathways result in altered health functioning (see Chapter 6).
The explanation of this notion of a psychosocial work environment with relevance for health deserves a further comment. In line with a biopsychosocial approach to health and disease, a reverse pathway from health to the social environment is operating as well. Impaired health can have a severe impact on a person’s coping capability, his or her healthrelated behaviour, cognitive appraisal, and emotional state (see reverse arrow in Fig. 1.1). For
instance, substantive research documented increased levels of depression following the manifestation of a variety of chronic diseases, where depressed mood in turn weakens cognitive and motivational coping capabilities. Moreover, these afflictions reduce the opportunities of returning to work after rehabilitation and to participate in productive activity (Bültmann and Siegrist 2020; see reverse arrow in Fig. 1.1). To demonstrate the importance of this reverse pathway in analysing relationships between psychosocial work environments and health, a special part of this book is devoted to its elaboration (Part IV).
So far, few attempts have been made to elaborate and visualize the different pathways linking the psychosocial work environment with health. A remarkable model depicted by Reiner Rugulies (2019) has inspired us to conceptualize these links in a slightly different way, as depicted in Figure 1.1. The figure indicates the main directions of assumed causes and effects of interest in this book, but it does not represent an empirically validated causal model.
Figure 1.1 Psychosocial work environment and health: A conceptual framework developed and extended based on a model proposed by Rugulies (2019).
Source: Adapted with permission from Rugulies, R. (2019), ‘What is a psychosocial work environment?’, Scand J Work Environ Health, 45 (1), 1–6 [Figure 1, p 2] (Creative Commons Attribution 4 0 International License, https://creativecommo ns.org/licenses/by/4.0/).
1.1.2.3
Dimensions of health
‘Health functioning’ is the outcome of central interest in our analysis of effects of psychosocial work environments. Although the term can be applied to places, geographical regions, or even the planet, it is conventionally limited to the individual person. Importantly, when discussing this notion, it is obvious that health can be improved or harmed, thus providing a positive and a negative dimension. Traditionally, for compelling reasons, its negative dimension has been investigated and tackled much more intensely than its positive
dimension. Absence of health is more visible and urges more attention than its presence. This absence of health is dealt with in three different systems of reference, termed ‘disease’, ‘illness’, and ‘sickness’. ‘Disease’ reflects the professional system of reference where signs of reduced health are analysed in a biomedical framework of pathophysiological developments of organs and organ systems. Based on scientific evidence and clinical knowledge, the International Classification of Diseases (ICD) (World Health Organization 20 22a) has identified and classified a large number of physical and mental disorders. Each disease is identified via a set of symptoms, biochemical and physiological data obtained through laboratory or functional tests, imaging techniques, and medical history information. Ideally, each disease is explained by one or several causal factors, and specific medical treatment approaches are available to restore health or to reduce disease severity. To a certain extent, due to insufficient knowledge, the causes of disease are not yet established. In these cases, at least distinct risk factors are known whose manifestations increase the probability of disease occurrence. As many diseases have multiple causes derived from socioenvironmental and personal (psychological, behavioural, genetic) factors, they are best analysed and tackled in a systemic, interdisciplinary, and inter-professional approach, as proposed by the biopsychosocial model. ‘Illness’ represents the system of reference of lay persons experiencing their personal health state. Due to the subjective interpretation and differential knowledge of symptoms and bodily signs, people’s definitions of illness vary widely according to socio-cultural, educational, ethnic, age- and gender-related circumstances. In view of the significance of illness behaviour (e.g. to seek medical aid, to comply with treatment obligations), these wide variations of defining illness and of responding to related needs can be problematic as they may diverge from the health needs induced by distinct diseases. For instance, symptoms of a severe disease (cancer, stroke, IHD) may remain unobserved or misinterpreted, causing delay of treatment or premature mortality. Alternatively, over-utilization of health services may occur due to inappropriate illness behaviour. ‘Sickness’ delineates the society’s system of reference. As many disorders largely prevent economically active people from participation in paid work and from contributing to economic productivity, and as the treatment and prevention of diseases induce substantial financial costs, every society is obliged to establish systems of cost control and compensation. Sickness funds, regulations of health-care utilization, and cash transfer systems are examples of how the reference system of sickness is working.
In today’s aging societies, physical and mental disabilities are of growing concern from a public health perspective, in addition to acute and chronic diseases mentioned above. Their main general feature is the restriction of functioning. Accordingly, to supplement the ICD, an International Classification of Functioning, Disability and Health (ICF) has been developed ( World Health Organization 2001). This classification contains the three dimensions of bodily functions and structures (impairment), activity (limitations), and participation in social life (restrictions), and these dimensions are influenced not only by type and extent of the disabling condition, but also by environmental and personal factors. Thus, compared to the ICD, the ICF has incorporated distinct personal and social factors into a biomedical paradigm of disease and disability.
In conclusion, the negative dimension of health is addressed as a high priority and by
multiple activities of scientific research, medical and paramedical professional agency, health-care delivery, and structural measures of health and social policy. The terms ‘disease’, ‘disability’, ‘illness’, and ‘sickness’ illustrate this priority. In contrast, the positive dimension of health has received less prominence within the professional systems of medicine and health care, and within the priority agendas of governments. It is true that health promotion and prevention of disease have been recognized as relevant health policy goals more recently, not least by several initiatives from the World Health Organization (2008). Yet, there is still a huge imbalance in terms of investments and concerns between the two dimensions. Furthermore, from a scientific point of view, it seems difficult to find a consensual definition of ‘positive health’ other than ‘absence of disease or illness’. A variety of biological markers was proposed as indicators of positive health, but this debate is ongoing. Internationally, there is a strong emphasis on defining positive health in terms of subjective well-being (Dien er 1984). ‘Subjective well-being’ is considered a three-dimensional construct, incorporating an evaluative component of cognitive judgment about one’s personal situation (‘life satisfaction’, ‘purpose in life’), an experiential component of emotional state (‘positive and negative affect’), and a eudaemonic component of positive functioning (in terms of selfrealization, agency, and social relatedness) (Ryan and Deci 2018). These components are assessed by self-rated scales indicating the amount and comprehensiveness of subjective well-being. There is no doubt that subjective well-being promotes mental and physical health, thus being a relevant outcome criterion in research on work and health. However, mainstream occupational health research has largely focused on indicators of ‘disease’, ‘disability’, or ‘illness’ to measure work-related outcomes. This mainstream approach will be documented in later chapters dealing with empirical evidence in this field of research.
In summary, Figure 1.1 and the explanatory text may offer an instructive introduction into the complex, yet intriguing and relevant matter of this book. Research on psychosocial work environments and health represents a new, rapidly expanding field of knowledge accumulation that is still debated at theoretical, methodological, and empirical levels (for discussion, see Kivimäki et al. 2018). This book is one of the first attempts to synthesize this knowledge and to advance the state of art by critical discussions and proposed suggestions.
1.2 Scientific disciplines and challenges of psychosocial oc cupational health
We have seen that knowledge of psychosocial work environment and its relationship with health comes from different scientific disciplines. Here, a short description of the main disciplines, their specific contributions, and their relevance for the practice of occupational health is given. The focus on five core disciplines does not claim to be exhaustive, but it covers essential developments. This section will be followed by an introductory illustration of some prominent challenges of the world of modern work and employment for psychosocial occupational health, where the useful role of knowledge and competences evolving from the study of this new field becomes evident.
1.2.1 Main scientific disciplines
In very general terms, science is considered a controlled collective activity which searches for truth and new knowledge. The notion of control refers to common criteria of the quality of knowledge acquisition, and collective activity indicates that expertise from different people and different areas is required, and that findings from individual scientists require independent replication and collective approval. The development of scientific expertise follows a process of division of labour, where different disciplines are established, often resulting in sub-disciplines and innovative cross-disciplinary specializations. A scientific discipline is best characterized as a field of expertise that describes and explains a specific area, aspect, or phenomenon of the living or non-living world by a structured process of knowledge acquisition. To this end, a common language of description, common methods of information collection, and a common set of explanatory theoretical models are required. Scientific disciplines stand out by high levels of expertise, shared standards of training, and procedures of quality control, and by their impact on society through professional associations and organizations. The following scientific disciplines have contributed most significantly to the development of the field of occupational health in its current shape (see B ox 1.1).
Box 1.1 Main scientific disciplines
Occupational Medicine: As a specialty field of medicine, this discipline is concerned with the detection, surveillance, prevention, and rehabilitation of occupational hazards and occupational diseases Main activities are research, teaching, preventive, and consulting activities, and to some extent clinical work. Close links were developed with Environmental Medicine and Occupational Health Nursing
Epidemiology: A discipline concerned with the distribution and the determinants of health conditions in populations, using quantitative methods. Its descriptive, analytic, and interventional approaches enable the application of research results to prevention, public health, and health care Occupational epidemiology is a crosscutting interdisciplinary field, rather than a sub-discipline.
Psychology: The main discipline of behavioural sciences concerned with perceptions, cognitions, emotions, motivations, and behaviours of individual persons and of groups of individuals It offers a broad spectrum of methods, including tests and experiments, and a variety of theoretical models. Practical applications refer to individual counselling and therapy, and to monitoring and intervention activities.
Sociology: This discipline is concerned with the analysis of structures and processes of societies at macro-, meso-, and micro-level of social life, applying theories and methods developed in social sciences. With close links to social epidemiology and to the sub-discipline of medical or health sociology, it explores occupational determinants and consequences of health
Economics: A discipline applying the analysis of two important pathways between economy and health to the field of occupational research: the impact of economic conditions (e g unemployment) on people’s health, and the economic consequences (financial costs) of healthy or unhealthy work. Its advanced quantitative methods are considered a particular strength.
1.2.1.1 Occupational medicine
Occupational Medicine is the primary, most established, and oldest discipline dealing with our topic. As a specialty field of medicine, this discipline is concerned with the detection, surveillance, and prevention of occupational hazards and occupational diseases, and with
processes of rehabilitation and return to work of disabled workers. Its focus is on research, teaching, and on preventive and consulting activities, and with certified qualifications it also addresses clinical work. Close links exist with the discipline of Environmental Medicine (La nce 2019). Traditionally, occupational medicine was developed as a scientific discipline in the area of industrialization during the nineteenth century, when toxicology, physics, biochemistry, biology, and clinical medicine shaped its scientific profile. With its search for specific substances and conditions at work that cause certain diseases, occupational medicine combined two methodological approaches from the very beginning: experimental studies using basic science methods, and epidemiological investigations of working populations. More recently, with substantial changes of employment sectors, technologies, and work environments, the discipline was gradually enlarged to include environmental medicine, and, in part, ergonomics and industrial hygiene. In some countries, the academic institutionalization of occupational medicine includes preventive and social medicine. Moreover, on many sites, collaborative links were developed with the fields of industrialorganizational psychology and occupational health psychology (see 1.2.1.3). As a distinction, occupational physicians are an internationally established professional group with legally defined tasks, in addition to strong boundaries with research and teaching in tertiary institutions. Guidelines for training and practice strengthen the professionalization process, and beyond associations at local and national level, a strong international professional organization was developed, the International Commission on Occupational Health (ICOH). Founded in 1906, this worldwide non-governmental professional society exerts an influential role in occupational health policy, not least in collaboration with the World Health Organization and the International Labour Organization. Although significant research input to psychosocial occupational health comes now from social and behavioural sciences, occupational medicine contributes substantially to the biomedical foundation of analyses linking the psychosocial work environment with health. In addition, occupational medicine has an important role in translating scientific evidence into practice in terms of screening and surveillance, expert opinions, guidelines, and implementation of preventive measures at worksites. One important extension is Occupational Health Nursing, which is a specialty within the nursing discipline to train occupational health nurses. In the US, such training is mainly supported by the National Institute for Occupational Safety and Health (NIOSH) through the Education and Research Centres. Modern roles and responsibilities of occupational health nurses have expanded immensely to include case management, counselling and crisis intervention, health promotion and risk reduction, legal and regulatory compliance, worker and workplace hazard detection. Particularly, ‘psychosocial needs/concerns’ and ‘stress management’ are clearly highlighted by the American Association of Occupational Health Nurses (see ‘Useful websites’).
1.2.1.2 Epidemiology
Epidemiology represents the discipline with the major methodological impact on the field of occupational health. Epidemiology is commonly defined as the discipline concerned with the distribution and the determinants of health conditions (usually diseases) in populations, using quantitative methods. Its descriptive, analytic, and interventional approaches enable the
application of research results to prevention, public health, and health care (Lash et al. 2021).
Historically, several ground-breaking epidemiological investigations on the burden of work-related disease promoted the academic development of occupational medicine as well as the establishment of occupational safety and health legislation and occupational healthcare services. Most famous in this regard was the study by Louis-René Villermé, a French physician, who, among others, revealed and criticized the noxious working conditions in cotton, linen, and silk industry in 1840 (Julia and Valleron 2011). Rather than being a distinct sub-discipline, occupational epidemiology is a cross-cutting field of scientific inquiry, reaching from genetics, environmental sciences, clinical medicine, to social epidemiology. During the twentieth century, occupational epidemiologists made many relevant discoveries. To mention just two examples related to different diseases: In the 1960s, prospective evidence of a causal role of asbestos fibres for the development of lung cancer and a formerly unknown disease, mesothelioma, was obtained (Selikoff 1990). As a practical consequence, a range of countries banned the use of asbestos, but more developed than developing countries. Around the same time, a landmark study of London bus drivers showed a clear link between sedentary work and elevated risk of IHD (Morris et al. 1966). Although this study could not rule out all relevant confounding factors and although excessive physical activity at work can also increase this risk, findings had far-reaching implications for worksite health prevention programmes of compensating physical activity among sedentary jobs. It is, by the way, of interest to observe that leisure-time physical activity exerts beneficial effects on cardiovascular health (Holtermann et al. 2020).
The sub-discipline of social epidemiology is concerned with the analysis of social determinants of health, where social inequalities of working and employment conditions are of major interest. This was most convincingly demonstrated in the classic British Whitehall study of civil servants mentioned above, documenting a social gradient of cardiovascular mortality according to occupational grade: the lower the grade, the higher the mortality risk ( Marmot et al. 1978). More recently, a further characteristic of this sub-discipline was suggested by the term ‘psychosocial epidemiology’, where the close links between social and psychological factors are at stake. Clearly, research on psychosocial work environments and health is one of the core areas in this regard (Kivimäki et al. 2018). Yet, when it comes to explanations of observed statistical associations, social and psychosocial epidemiologists often depend on input from other disciplines, and in particular from psychology and sociology, as will now be described.
1.2.1.3 Psychology
Psychology is the main discipline of behavioural sciences as it is concerned with perceptions, cognitions, emotions, motivations, and behaviours of individual persons and of groups of individuals. It uses systematic observations, tests, experiments, and surveys to explore these phenomena, and it applies theories to their explanation. Psychology has a strong connection with practical applications, either in terms of individual counselling and therapy, or in terms of monitoring and intervention activities. As a mature academic discipline with a long history, this field has developed a number of sub-disciplines where two specializations have put their main focus on work. Industrial-organizational psychology analyses the interface of
working persons with organizational contexts, with a broad spectrum of interest, including work motivation and performance, recruitment and training, leadership and teamwork, or organizational and personnel development. While many concepts in this research are useful when applied to relationships between work and health, health is not an explicit priority of this sub-discipline. Rather, this is the case for occupational health psychology. Evolving during the 1990s, this field has put its main emphasis ‘on the ways in which experiences at work, exposures to work tasks, and associated environmental factors impact worker health, safety, and well-being’, as defined in an excellent recent textbook (Cunningham and Black 20 21, p. 2). Occupational health psychology owes its rapid growth not least to the influential Journal of Occupational Health Psychology, to special training and promotion activities of the American Psychological Association, to innovative scientific associations, and to a series of handbooks under the leadership of British psychologist Cary L. Cooper (Cooper and Quic k 2017). Throughout this book, several chapters will draw quite substantially on research findings derived from this field. At the same time, it should be noted that essential theoretical input to this sub-discipline comes from the general field of psychology. To cite just two classic examples, one of the fundamentals of this research is provided by psychological stress theory (Lazarus 1966), and one of the core concepts of coping with work applied to occupational health psychology concerns Bandura’s theory of self-efficacy (Bandura 1977). Moreover, concept such as ‘conservation of resources’ (Hobfoll 1989), ‘equity’ (Adams 1965), and ‘organizational injustice’ (Greenberg and Cohen 1982) were integrated in respective investigations. Chapter 3 will discuss some leading current concepts of occupational health psychology in more detail. Last not least, the psychological notion and assessment of ‘burnout’ had a major impact on empirical research in this field (Maslach 1982).
1.2.1.4 Sociology
Sociology is the discipline concerned with the analysis of structures and processes of societies. Over the course of their evolution, humans evolved as social animals, developing groups, norms, social roles, social differentiations, and social institutions. The interplay of individual and society is at the core of sociological analysis, and this interaction is analysed at different levels, the macro-, meso-, and micro-level. The societal structure of work and employment and the organization of work with its impact on workers’ behaviour were main topics in the founding period of sociology, as documented by the seminal work on alienated labour by Karl Marx (Marx 1984). However, the application of leading sociological concepts to the analysis of work and health occurred much later, mainly during the second half of the twentieth century. Examples of relevant concepts are ‘social support’ (Durkheim 1897, 1951), ‘social status’ (Merton 1968), ‘control and self-direction’ (Kohn and Schooler 1973), and ‘social exchange and reciprocity’ (Gouldner 1960). Social support was shown to be a protective factor in associations of work stress with coronary heart disease (House 1981), while social (or occupational) status was identified as an important determinant of life expectancy and overall mortality (Antonovsky 1967). Social status was also linked to mental illness (Hollingshead and Redlich 1958) and, in combination with critical life events, to the onset of depression (Brown and Harris 1978). How leading sociological models of a
psychosocial work environment with relevance to health and disease were influenced by classical theoretical concepts in sociology will be discussed in Chapter 3. Of interest, among the sub-disciplines of sociology, medical (or health) sociology is a field of research with an extensive interest in relationships of work and health.
1.2.1.5 Economics
The discipline of economics enriched the field of occupational health in two different directions. One direction deals with the impact of economic conditions (unemployment, low income, income inequality) on people’s health, whereas the other direction is concerned with the analysis of economic consequences (financial costs) of healthy or unhealthy work. Based on large datasets from the USA that were subjected to ecological analysis, Harvey M. Brenner discovered a significant increase of indicators of mental pathology, including suicide and homicide, within a year of heightened unemployment rates (Brenner 1973). Subsequently, this approach was applied to chronic diseases, such as IHD, where a time lag of two to three years following job loss was observed, and it was extended to explore the impact of economic business cycles on morbidity, using time-series analyses (Brenner and M ooney 1982). Although innovative and intriguing, the validity of these results was restricted, given the methodological problem of ecological fallacy. Thus, individual-level cohort studies corroborated an association of unemployment with morbidity and mortality (e.g. Dupre et al. 2012; J. K. Morris et al. 1994; Moser et al. 1987). A further line of research investigated the links between income, income inequality, and health. Many studies documented higher morbidity and mortality among people with low income, but research identified a reciprocal association between these two factors, such that poor health also results in low income (Mack enbach 2019). In a similar way, the causality of a prominent role of augmented income inequality in explaining high morbidity and mortality across different countries is still debated (Wilkinson and Pickett 2009). The second direction of economic research with relevance to occupational health focuses on evaluating and estimating the costs of the burden of work-related diseases (Goetzel et al. 2004), and the benefits of health-promoting worksite interventions (Johanson and Aboagye 2020).
These remarks on relevant disciplines serve as an introductory orientation to readers, and they are by no means exhaustive. Yet, cumulative research conducted in the frame of these five scientific disciplines laid the ground for essential knowledge on psychosocial occupational health. How useful this knowledge can be in tackling dominant challenges to occupational health is illustrated in the next section. Three such challenges are selected as instructive examples.
1.2.2 Some current challenges
1.2.2.1
The COVID-19 pandemic
The outbreak of the COVID-19 pandemic early in 2020 with its subsequent worldwide surges of infection was an unpredicted and threatening event to humanity. According to the WHO Coronavirus (COVID-19) Dashboard, more than 6.8 million deaths and more than 700
million cases were recorded by March 2023 (World Health Organization 2023). In addition, evidence on adverse long-term effects of this infection became evident, with a syndrome of symptoms defined as ‘long COVID’. Thanks to rapid, successful development of vaccines, the deleterious effects of this pandemic could be substantially reduced, but large parts of populations in less developed countries had no or very limited access to these vaccines. Moreover, considerable parts of the population even in highly developed countries rejected vaccination, thus reinforcing the outbreak and expansion of new waves of infection.
The associations between the COVID-19 pandemic and the world of work are particularly worrying as they involve at least two different aspects of working people’s health. Firstly, specific occupational groups were and continue to be at high risk of infection due to the nature of their work. These occupations include medical and paramedical professions dealing with victims of infection, most often in the context of treatment in intensive care units of hospitals. Through this direct pathway, the demands of their work, further occupational groups were continuously exposed to the wider public, thus suffering from elevated rates of viral infection (e.g. delivery of services; taxi drivers; police, military service; teachers, social workers). Many factories and organizations failed to protect workers from infectious risks, in particular those with less developed occupational health services, and those with a less skilled or even precarious workforce (e.g. construction workers, cleaners; Mutambudzi et al. 2020). As a result, social inequalities of mortality due to the COVID-19 epidemic were reported from several national reports, with highest levels among those in lowest socioeconomic positions (as an early document, see Wise 2020).
What does the psychosocial dimension of occupational health add to these observations? Obviously, the recurrent threat of being infected in one’s daily work aggravated an already high burden of workload in these occupations. Signs of exhaustion, burnout, and physiological breakdown were observed to be more frequent, calling for measures of mitigation. Improving mental health among occupational and professional groups exposed to the pandemic has become an internationally acknowledged high priority for workplace intervention efforts (World Health Organization 2022b). During the COVID-19 pandemic, many workers were asked to work from home, which was one of the public health measures of prevention at macro-level. Indeed, research evidence indicated that working from home was associated with reduced risk of infection, in this unexpected natural experiment (Alipour et al. 2021). However, essential workers (including health-care workers) had to work onsite, and they suffered from high levels of stress and mental symptoms. An intervention study among health-care workers in Canada, using online cognitive-behavioural therapy techniques at micro-level, demonstrated significant improvements in symptoms of anxiety, depression, and post-traumatic stress disorder (Trottier et al. 2022).
The second aspect of how this pandemic affects workers’ health concerns indirect rather than direct pathways. Widespread and long-lasting ‘lockdown’ measures resulted in substantial reductions of employment. For instance, according to an estimate of the International Labour Organization, total hours worked globally in 2022 remained almost two per cent below the pre-pandemic level, resulting in a deficit of some fifty-two million fulltime equivalent jobs (International Labour Organization 2022). Thus, reduced working time resulting in income loss has become a major concern, specifically in the absence of national