




















This handbook was created to orient you to the work we will do together as a committee over the next two years.

Section 1 Introduction to Patient Engagement in Family Medicine
Section 2 The PFAC Member Council
Section 3 DFCM Glossary Terms
Section 4 About DFCM
Section 5 DFCM Family
Section 6 Questions and Answers
Section 7 Resources



They are patients, families, and caregivers who are passionate about health care and want to share their experiences to improve health services for everyone. When we say “patient”, we are referring to individuals cared for at any one of our teaching clinics.


Patients know a surprising amount about healthcare: they know how it feels, whether systems work, and the impact of treatment on their lives. Patient engagement is about bringing the perspective of patients to the planning, delivery and evaluation of health care. The key part is WITH, not FOR patients.





I was born in 1973 in Mamou, a city located in West Africa’s Republic of Guinea Following the influx of refugees from Liberian and Sierra Leon; I migrated to Canada in 2010. I am a devoted volunteer for the causes of black immigrant communities, notably within the Association Amical Francophone des Guinéens et Guinéennes de l'Ontario (AFROGUI) and also the Fulani Cultural Association of Ontario (FUCA- Ontario)



I am a former child and family therapist which included certification as a play therapist. Teaching adults and children the importance of play was one of the best parts of the job. Being disabled for many, many years has taught me the ways in which patient care works and how it might be improved upon, which in turn can only help the health care provider, the patient and the system in the future. My guilty secret is watching British dramas, crime dramas and cozy mystery shows. I also read select cozy mysteries before bed too, but don’t tell anyone.

My name is Julie King. I have been a patient at the Southlake Family Health Team for 17 years. I am a mom of four and I work with students who are deaf and hard of hearing. I joined the Committee to give back to the medical community that has provided so much to my family. I bring a unique perspective to the team as I am American. I spend most of my free time cheering on my kids in ice rinks and volleyball courts.








My name is Gerald Crowell and I live in the East End of Toronto in Leslieville. I’ve been here almos t 30 years and have recently retired from a consulting career . I joined the Committee to contribute back to the amazing medical community. I’ve been a patient at St Lawrence Health Centre for more than 15 years. I joined the clinic to be able to have the same family physician as my husband who lives with a chronic condition. The clinic has always provided exceptional care. Fun fact: I’m an avid gardener, starting my Master Gardener Program and like to exotics like citrus and pineapple.

I live in Riverdale and have been a patient of Mt. Sinai Academic Family Health Team for over four years. Before retirement I was an elementary school teacher, potter and lawyer (not all at once).The focus of my law practice was health law where I acted for physicians. In addition, I was an adjunct professor teaching Health Law at the Faculty of Medicine. I have had a rich and rewarding volunteer life, most notably as the President of the YWCA of Canada and Vice President of Youthlink. I am looking forward to volunteering with the DCFM. My hobbies include taking care of my two grandchildren, gardening and various art projects.

I am a consultant by trade, avid traveller, and humanitarian based out of Toronto. With a M aster’s degree in International Humanitarian Action, I am passionate about contributing to initiatives that impact people’s day to day lives. Having worked on humanitarian healthcare initiatives throughout her career, I am excited to bring a unique and varied perspective to the Patient and Family Advisory Committee.



I recently moved to St Catharin es but I’m still a patient at Credit Valley Family Health Te am (CVFHT) in Mississauga due to the excellent care they’ve provided to me for over 12 years I’m excited to be joining this advisory committee and sharing a patient's perspective. I look forward to meaningful engagement with others from across the province Now that I’m fully retired, I enjoy giving back to my community through volunteer work





I live in East York with my familyand wehave been patients of the 80 Bond Clinic in downtown Toronto for over 15 years. I have a long history with St Michael’s Hospital (I was born there!) and am also a member of the SMH community advisory panel (CAP). I am a Social Worker working primarily with people experiencing homelessness and in the housing sector for the past 20 years.. I am a wife and mother of 2 young children. I enjoy travelling with my family and long hikes and my superpower is parallel parking.


My name is Michelleand I wear many hats: I amawoman, a mother to three youngchildren, a wife and an educator. I have always been an advocate of social justice and enjoy taking on opportunities to improve the overall welfare of people in our community I currently live in York Region We are a very active family! My husband and I have three energetic kids and a big furball husky who is equally as active We recently enjoyed a beautiful summer with our family and relatives beach days, day trips, cottaging and endless birthday parties and gatherings We loved every minute of it but are now happily settling back into our slower-paced fall routines.


I was born and raised in Toronto, but havelived in both Montreal and London, UK. I now live in Midtown with my husband, son, and our 2 cats. I am really excited to be part of PFAC as a patient at the Sunnybrook Academic Family Health Team. I feel very passionately about everyone having equal access to fantastic primary care. I have worked in tech for the past 10 years in a variety of Operations roles. In my spare time I love to go on adventures around the city, read, and watch reality TV.



I live in EastYork and I am relatively a new patient affiliated with the Schulich Family Medicine Teaching Unit at the Wilson Site of Humber River Health, I am eager to participate in thoughtful discussions on ways of enhancing the patient experience throughout the healthcare system. I have a rather eclectic background spanning studies in psychology, biology, education, modern languages and music complemented by work experience as a teacher, researcher, writer, editor and translator. Culture as a force shaping how we are and who we are has long fascinated me, and my time living abroad in Europe,


I live in Barrie with my 14-year-oldson.Iattendthe Family Medicine Teaching Unit at the Royal VictoriaHospital in Barrie, and I've been a patient there for going on 7 years. I wanted to join the committee as I believe there is always room for improvement, and the way doctors are taught is no different. Sometimes a fresh set of eyes and different life experiences can bring about positive changes. It's a priceless but valuable opportunity. A fun fact about me... I have grand aspirations of making it on Jeopardy but I'm too chicken to audition! Maybe one day! :)


My name is Trudy Penny and I was born on the beautiful island of Grenada. Myfamily and I moved to Canada when I was 2 years old, so Canada has been my home for over 30 years! I am a wife, mother of two and a second-year midwifery student at Toronto Metropolitan University. In my free time, I enjoy trying new restaurants and travelling to different countries to learn about new cultures. A fun fact about me is that I enjoy playing boardgames with my husband and I am proud to say we have a collection of over 75 board games!


I currently live in the KingWest area of the city. I am an elementary school teacher. My most important job to date and one in which I am most proud o f is being a mother to my energetic five year old son. I have been a patient of the Toronto Western Family Medicine Clinic for approximately 15 years. As a Black woman of Afro-Caribbean ancestry, I am aware of the importance of representation in healthcare and the danger of policies and decisions made in the absence of consideration of the lived experience of marginalized communities. FunFact:My favourite TV show is called Call the Midwife, currently my go to music is Salsa and Afro-Beats.

My name is Niáll Johnston, and I represent the Summerville Family Health Team - Etobicoke location, although I live just ‘over the border’ in Mississauga. Being born and raised in the UK, and having lived and worked as a public educator in Canada for over 25 years, I am deeply committed to the maintenance and improvement of publicly-funded healthcare and enhancing how the system serves our ever-changing community. I joined the Patient and Family Advisory Committee as a son, father, husband and a frequent patient(!) to share my experiences and insights as to how we can advance family medicine for everyone involved.


TheOntario healthcare system and the Department of Family & Community Medicine (DFCM) at U of T consists of acronyms and other terms that may be hard to understand. As a patient or caregiver partner, it can be common to feel a bit lost in the many terms you will come across. It’s okay to ask healthcare staff to explain terms that my be unfamiliar to you.



College of Physicians and Surgeons of Ontario (CPSO)



An academic hospital combines the services of a hospital with the education and training of medical students and residents as well as medical research.
Ontario Health Teams are groups of healthcare professionals that aim to work together to provide coordinated care spread across Ontario based on geographic areas.
An association for Ontario Health team clinics in Ontario.


An organization that regulates the practice of medicine in Ontario. All physicians in Ontario must be members of the College in order to practice medicine.

Employees of the clinic; some might answer phones, check patients in and out, handle themedical records, and assist with other office work.


Community Health Centre (CHC)

Non-profit, community-based organizations that provide primary health and health promotion programs for individuals, families and communities.
Electronic Medical Record (EMR)

Faculty

Family Health Team (FHT)

Fiscal Year (FY)

A digital (electronic) version of a person’s medical record.


Staff that are connected with the University of Toronto and could be a family physician or a non physician teaching and delivering education at the University of Toronto.

A team of family physicians, nurse practitioners, registered nurses, social workers, dietitians, and other professionals who work together to provide primary health care to individuals.

A timeframe used for accounting and performance management. In most health care organizations, the fiscal year runs from April 1st of one year to March 31st of the following year



Interprofessional Care (IPC)

Ontario College of Family Physicians (OCFP)

Ontario Health Teams (OHTs)

Ontario Medical Association (OMA)

Patient and Family Centred Care


When health care providers from different professions (doctors, nurses, pharmacists, social workers and others) work collaboratively to deliver care, based on a patient’s needs and goals.

An association that represents family physicians in Ontario.

Ontario Health Teams are groups of providers and organizations that aim to deliver coordinated care to a defined geographic population.

Represents Ontario’s physicians, residents and medical students in areas of economic interests, healthy policy and professional advocacy, and legal services.

A guiding approach where patients, families and health care providers collaborate as partners in the planning, delivery and evaluation of care.



Post Graduate Education


Personal Health Information Protection Act (PHIPPA)

After completing an M.D. degree program and becoming a licensed doctor; physician move on to postgraduate medical education or residency training. This is the final stage of medical education where doctors can specialize in their area of focus.

PHIPA provides a set of rules for the collection, use and disclosure of personal health information

Quality Improvement (QI)


Activities that lead to measurable improvement (making better) in health care services and health outcomes for patients

Quality Improvement Plan (QIP)



A Quality Improvement Plan is an organization’s plan outlining how they will improve the quality of care they provide to their patients, residents or clients in the coming year.



Resident



Staff Physician
Resident doctors are medical doctors training in Family Medicine. They can do the same things as your family doctor such as examine you, order tests, and prescribe medications


Teaching practice
Teaching Site


Family doctors who work as staff at our teaching sites. They may supervise residents in addition to their doctor duties.


Family doctors get 2 months of experience attending a teaching practice in a remote area. There are faculty in 40+ community practices ranging in location from rural southern Ontario to as far as Moose Factory.


Read

A clinic or hospital that provides medical education and training to future and current health care professionals. Teaching sites are almost always affiliated with one or more universities.


The Department of Family and Community Medicine (DFCM)
The University of Toronto’s DFCM is one of the largest family medicine departments in the world.




What we do
Our faculty, staff and learners are dedicated to train future family doctors.

DFCM in Numbers



























Complete 4 years of universit 1 y





2


Learn about family medicine through clinic placements and courses every year of the 4 year program




4



Acceptance to medical school and 34 years of study


Graduated doctors who want to specialize in family medicine apply for acceptance through a national application process to join as residents at the DFCM.
6 5



Pass an examthat demonstrates you know enough about medicine before treating patients





8

Family medicine residents work full-time and are supervised by staff doctors connected to the University of Toronto.
After two years of residency, the goal is for residents to learn more topics and to be able to practice without needing supervision.
3 7




Residents must pass a Canadian licensing exam before seeing patients without supervision.






How often did you receive care within a reasonable time? How would you rate your overall experience when booking your last appointment over the phone? How would you describe the length of time it took between making the urgent care appointment and receiving care?
Can I take part?
The survey is distributed and analyzed twice a year since June 2020.
How is the data being used?

If you have observed any changes or have suggestions, please share them with clinic staff. any ideas, please share with our clinic staff.

To learn more about the survey, click here


Family medicine is introduced as a topic when students are completing their 4 years of undergraduate training to become doctors. Doctors who want to become family doctors join our department and complete 2 years of training which is guided by the Post Graduate Family Medicine Education program.

Our faculty can give up some of their time for research. to explore new topics and answer questions about family medicine.
The Quality and Innovation program exists to make primary care in Canada better. Teaching doctors to improve health outcomes and the patient experience. Patient partners will be working closely with this program.

Teaching staff in this program work on education, research, quality improvement, clinical innovation, leadership and advocacy in areas including social accountability, Indigenous health, climate change and more both in Canada and globally. Click the links to learn more about each program!


Faculty development is a term used to describe activities and programs designed to assist teaching staff to develop skills related to the role of teacher, researcher and leader.
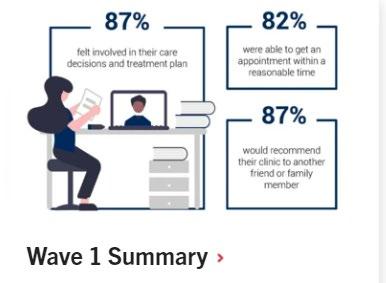

Learn about our patient experience survey and what we have learned so far

Meet some of the key leaders you will be working with as a DFCM patient partner.



Dr.DanielleMartin isChairof the Department of Family and Community Medicine (DFCM), University of Toronto. Dr. Martin is an active family physician and respected leader in Canadian medicine and well - recognized media spokesperson, regularly named on lists such as Medical Post’s Power List. Her 2014 presentation to a United States Senate Subcommittee about the Canadian health care system has been viewed by over 30 million people across the globe. Dr. Martin spent eight years as a senior hospital executive, most recently as Executive Vice President and Lead Medical Executive at Women’s College Hospital (WCH ).
Fun fact: Danielle drives a yellow vespa to work.
Ms. Brenda Chow is the Business Administration Director a key leadership position within DFCM that plays a vital role in the department’s operations and strategic direction. Brenda brings nearly a decade of experience in administrative leadership.
Fun fact:
Outside of work, Brenda loves short, slow runs and long, leisurely walks, preferably by the lake. She’s an animal lover and has two aloof cats and one rascally dog. She and her husband are science nerds and have a beautiful artistic daughter who is currently studying graphic design at OCADU.
Dr . Noor Ramji is currently an academic Family Physician and Faculty member at the St Michael's Hospital Academic Family Health Team (SMHAFHT) in the Department of Family & Community Medicine at the University of Toronto in Toronto, Ontario . Dr . Ramji has been SMHAFHT Quality Improvement (QI) Director since 2018 , with notable experience in quality improvement in preventative health, chronic disease management, access, patient experience and understanding and optimizing equity in Primary Care . She was recently appointed as Practice Improvement Director for the Dept of Family and Community Medicine for University of Toronto in Sept/ 2023 and serves as a Quality Improvement Coach with the College of Physicians and Surgeons of Ontario
Fun facts : Favourite TV show - Star Trek the Next Generation Can't live without - summer gelato! Favourite song - Lovely Day by Bill Wither

Meet some of the key leaders you will be working with as a DFCM patient partner



Dr. Henry is the Vice - Chair of Community and Partnerships in the Department of Family and Community Medicine, University of Toronto She is a staff physician at Oak Valley Health, Markham - Stouffville site, and a family physician at the community - based clinic of Health for All . In her community clinic, she previously held the positions of board chair, and director of the Global Health program through the teaching unit She currently works as a physician at Blue Door Shelter and provides physician support through the Community Paramedic Outreach Response Team (CPORT) program Fun fact : Melanie reads Jane Austen’s Pride and Prejudice at least once per year .
I am interested in joining DFMC’s PFAC because as a current medical resident training to become a Family Physician, I resonate deeply with the committee’s goal of engaging directly with patients and community members to improve family medicine teaching and promote patient care. I have received some of the best and most memorable feedback directly from my patients and would love to work with a diverse group of patients, community members, faculty, and researchers to further enhance the family medicine training program that I am fortunate to be a part of.
As a resident at Humber River Hospital, I am especially interested in joining the Patient and Family Advisory Committee because I see this role as an opportunity to strengthen the connection between patients, families, and residents in shaping primary care. Humber River’s family medicine residency program is new and was designed to fill an important need for comprehensive primary care in northwestern Toronto. I am committed to seeing this program succeed in addressing that gap, and I believe that working with the PFAC will provide invaluable insights into patient and family experiences that can inform both my own development and the growth of the program. The committee’s focus on collaboration, quality improvement, and education aligns with my goals as a resident to advocate for patientcentered care and contribute to the long - term success of primary care training and delivery in our region.

Meet some of the key leaders you will be working with as a DFCM patient partner.



Erin Plenert istheQuality & Innovation Program Manager at the Department of Family &Community Medicine,Universityof Toronto. Erin brings a diverse set of skills after working in both clinical and community - based research for many years. Erin has extensive experience working with different stakeholder groups, including patients and community - members. She also brings a wealth of experience in growing and managing diverse yet cohesive teams. Overall, Erin is passionate about contributing to meaningful changes to our healthcare system to ensure that all people can access care that is safe, equitable, and of high quality. Fun fact: Erin can't live without her dog or pasta. Erin also has a secret love of Below Deck!
Dana joined as the department’s first patient engagement specialist. In her role, Dana supports patient engagement activities at the department and will be working closely with patient partners. Fun fact: Dana likes to paint and participates in number of sports including wheelchair tennis, adaptive climbing, rowing and sailing. She also rides a red e - trike everywhere which she named Ruby.
Marisa Schwartz is the Quality and Innovation Program Administrative Officer at the Department of Family & Community Medicine, University of Toronto. She is a mom of 2. Fun fact: Marisa and her husband are both identical twins!




Many of our clinics have patient family advisory committees that work with patient partners on different aspects of work at their clinic. For example, patient partners share perspectives on our patient experience survey, quality and safety issues and redesign of clinic spaces.

Residents are always supervised by the family doctor with whom they are working. This helps give the resident feedback on the visit and improves teaching. Supervision of patient care may take many forms, including: ·Video : The staff physician may watch a resident during your visit using a video camera. In Room: A supervising physician may join the resident in the examination room during your visit. ·Supervisor Consultation : Resident doctors may routinely step out of the room to discuss your case with their supervising staff doctor.


Can a resident doctor do the same things as my family doctor?


Residents can do the same things as your family doctor such as examine you, order tests, and prescribe medications. A resident doctor is supervised by a staff Family Doctor during your visit with them. You can ask to see the staff doctor at any time during your visit.



Resident may routinely step out of the room to discuss your case with their supervising staff doctor. Sometimes staff physicians are busy seeing a patient or helping another resident so it may take time. This process helps to make sure that that you receive the best care for your medical issue.

The College of Family Physicians of Canada (CFPC) is the professional organization that represents more than 42,000 members across the country. The College establishes the standards for and accredits postgraduate family medicine training in Canada's 17 medical schools. It reviews and certifies continuing professional development programs and materials that enable family physicians to meet certification and licensing requirements.

Why is my resident doctor sometimes not available?


Residents practice at the clinic and at a hospital. As part of learning, sometimes a resident is studying surgery and may be working at a hospital and just coming into the clinic once a week. You can ask to see a staff physician if your resident doctor is not available.



Patient Partnering Tools and Resources
Here are some of our favorites:
•Glossary of Health Care Terms
•What is Quality Improvement
•Getting involved in Quality
Improvement
•Quality improvement course
•Capturing the voice of healthcare customer

The college works with universities to review and certify programs.

Here are some of our favorites:
•Healthcare in Canada
•A guide to having a conversation about what matters
•How to communicate effectively on an advisory panel
•10 lessons learned from patient and family advisors



Learn more about:
•The Quality & Innovation program
•Our patient experience survey
•Patient partner important documents
•Residency program


•Tips for how to be an effective patient advisor
•Zoom instructions
•Check-in Checklist
