
By Your Side
Navigating Health Challenges with Care Management
11 Are Biosimilar Medications as Good as the
BACK COVER
• Do You Have a Child Turning 26?
• Approaching 65?


By Your Side
11 Are Biosimilar Medications as Good as the
BACK COVER
• Do You Have a Child Turning 26?
• Approaching 65?

Network Health takes health insurance fraud seriously. Insurance fraud costs millions of dollars each year, and it results in higher health care costs. Network Health investigates all reports we receive. Tips from our members are critical in helping us identify fraud, waste and abuse. We urge you to contact us if you feel you’ve been impacted.
• A health care provider bills for services you never received.
• A durable medical equipment (DME) supplier bills for equipment different than what was ordered and provided or was unsolicited.
• Someone uses another person’s member ID card to get medical care, supplies or equipment.
• Misrepresenting alternative medicine or cosmetic procedures as covered plan benefits.
If you suspect fraud, here’s what you can do.
• Call your health care provider to make sure the bill is correct.
• Call the member experience team at the number located on the back of your Network Health member ID card.
• Email us at paymentintegrity@networkhealth.com
Vice President David Sengkhammee Marketing
Strategic Marketing Julie Buchanan and Communications Laura Lopez Coordinators
Supervisor Debra Sutton Creative Design
Michael Jurmu, Jennifer Quadracci, Kristy Yarcho, Carisa Satorius, Romi Norton, Ted Regalia, Susan Wendt
Balance is published by Network Health. The health information contained in Balance is meant to supplement, not replace, the advice of health care professionals.
© 2025 Network Health. No portion of this newsletter may be reproduced without written permission from Network Health.
If you have questions, suggestions or a story about how Network Health has made a difference in your life, send us an email at marketing@networkhealth.com.
YOU CAN ALSO WRITE TO US AT:
Network Health
Attention: Julie Buchanan 16960 W. Greenfield Ave., Suite 5, Brookfield, WI 53005

At Network Health, we understand that navigating health care can be challenging, and we are here to make it easier for you. We take the extra steps to make health insurance understandable, so you are comfortable with your coverage. With your personalized, secure member portal, you can easily manage your plan by accessing important plan documents, benefits, claims updates and more.
Access your portal at the times most convenient to you. The portal works great on your mobile phone and is built to be viewed on any smart device. Either scan this QR code with your smart device or type login.networkhealth.com into your favorite internet browser.
Want less clutter and faster updates? You have the freedom to choose the way you’d like some items sent to you. Going paperless to receive information via email is fast, secure and does not clutter your mailbox. In fact, this newsletter is one of the items you can choose to receive electronically. If there are communications you’d still rather receive as hard copies through the mail, you can select that preference.
To select your preferences, simply log in to the portal, click your name in the upper right corner and select Change My Communication Preferences. From there, you can choose email for some or all the available categories. Make sure to click Next to save your choices.
The member portal is your one-stop shop for information specific to your health plan.
• Benefits and coverage overview
• Claims detail and status
• Access your mobile Network Health member ID card
• Out-of-pocket expenses tracker
• Monthly explanation of benefit (EOB) statements
• Select or update your personal doctor (or request replacement hard copies)
The member portal also provides seamless connections to other valuable resources.
• Pharmacy benefits and claims information*
• Your health questionnaire
• Virtual visits
• Wellness programs and tools*
To keep your information safe, we use multi-factor authentication. It’s easy to set up and gives you peace of mind when accessing your important information wherever you go – the pharmacy, doctor’s office or even on vacation. Just visit login.networkhealth.com
*Not all Network Health plans have a wellness program or pharmacy benefits. Check your plan documents for details.
by Katrina G., CSW, social work care manager special needs plan and Lexi F., BSVR, CSW, social work care manager special needs plan at Network Health
A POA is a legal document designating a person (your “agent”) to make decisions for you when you are no longer able. The document gives you the opportunity to express your wishes relating to end-of-life care.
A POA for Health Care specifically addresses health care matters. The person you designate as your health care agent only has authority to act on your behalf if you are declared incapacitated by two health care providers. Incapacity means you are unable to receive or process information, or unable to communicate your medical decisions. It’s recommended that those 18 and older should have a POA for Health Care in place. In Wisconsin, a family member (“next of kin”) is not automatically authorized to make health care decisions for you. You must have a POA for Health Care document created.
A Durable POA is for financial matters. This POA becomes effective immediately unless you specify a future date or occurrence that will activate the powers expressed in this form.
You can access free advance directive forms, including the POA for Health Care and Durable POA, through the Wisconsin Department of Health Services website dhs.wisconsin.gov/forms/advdirectives/adformspoa.htm. Your personal doctor may also have forms available to you.
Guardianship is needed when someone is deemed incompetent, meaning the person’s impairment is likely permanent and prevents them from understanding information or expressing their wishes. Unlike a POA, the court system will appoint a guardian. An individual may require a court-appointed guardian of the person, a guardian of the estate, or both.
A PHI form allows you to designate someone to receive information on your behalf. Your designation can be a spouse, relative, friend, advocate, attorney, doctor, organization or another person you trust. The form gives permission to share your PHI with those you designate but does not authorize them to make decisions on your behalf.
You can submit this form to Network Health through your member portal. You can also contact the member experience team at the number located on the back of your member ID card, to request the form be mailed to you.
Establishing a POA can prevent the need for guardianship, which is a lengthy and costly process. A POA document ensures your wishes are honored and decision-making remains with your chosen person (agent). Take the time to
Advance Directives are legal documents that allow you to express your health care preferences in advance, in case you become unable to make your own decisions in the future. While navigating the various forms can seem complex, taking this simple step today can provide peace of mind for you and those closest to you.
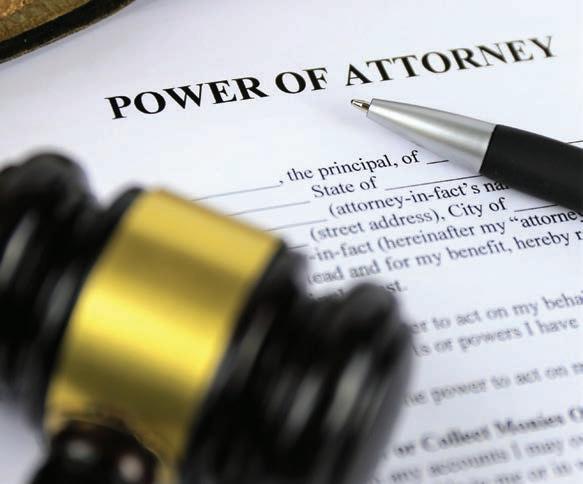
ensure that your voice will be heard when it matters most. Consider these steps when advance care planning.
1. Think about what is important to you.
2. Learn about options for end of life – what you want and don’t want.
3. Choose the agent you trust to make decisions on your behalf.
4. Engage in open communication with your agent and your doctor.
5. Document your wishes by completing your POA.
6 Ensure your POA is shared with your doctor, local hospital and agent. Keep a copy for yourself in a safe place.
7. Review your POA regularly to make sure it is up to date.
Don’t wait; start planning your future today to ensure your wishes are known and respected.
Your local Aging and Disability Resource Center (ADRC) Greater Wisconsin Agency on Aging Resources, Inc. at gwaar.org/guardianship-resources
Fox Valley Advance Care Planning Partnership at fvacpp.org Network Health Care Management team at 866-709-0019 (TTY 711), Monday-Friday from 8 a.m. to 5 p.m.
by Melissa Anderson, director provider operations and vendor contracting at Network Health
At Network Health we want to ensure you know where to seek urgent or emergency care services when they are needed, while in our service area to minimize additional out-of-pocket costs.
1. Seek services at participating, or “in-network,” urgent care facilities when in our service area. All out-of-network urgent care services will be denied if you have an HMO policy. Aurora, Aspirus and Marshfield are not participating providers, for example.
2. If you seek services from an in-network urgent care facility you may receive two bills, one for the doctor and one for the facility.
3. MDLIVE® can be used for certain conditions and you can seek care from the comfort of your home with little out-of-pocket expense.
If you are seeking emergency care services, please keep the following in mind.
1. Seek emergency care with our in-network facilities while in the service area.
2. If you are seeking out-of-network emergency care in our service area without an ambulance transfer and you are admitted, Network Health may not cover the inpatient stay as care is available in-network. Please contact Network Health immediately to seek transfer of services.
To find in-network urgent and emergency care facilities, visit networkhealth.com and select Find a Doctor at the top, or contact our member experience team at the number located on the back of your member ID card.
T here are several organizations that exist to help improve the quality of health care across the United States, including the National Committee for Quality Assurance (NCQA), the Wisconsin Office of the Commissioner of Insurance (OCI) and the Centers for Medicare & Medicaid Services (CMS). They use a variety of performance measurement tools and regulations to help ensure consumers are protected and receive quality health care services.
These organizations also require health plans to provide information to their members on these specific topics.
• Access to Network Health Care Management Employees and Services
• Evaluating New Technologies
• How Do Health Plans Make Decisions?
• Member Rights and Responsibilities
• Submitting a Claim for Reimbursement
• What’s the Difference Between Emergency Care, Urgent Care and Virtual Visits?
• Ensuring You Receive the Service You Deserve
• Falls/Osteoporosis
• Keep Yourself Safe from Medicare Fraud
• Network Health’s Focus on Quality
• The Importance of Exchanging Information
• What is Population Health Management?
You can find a downloadable PDF of this information at networkhealth.com/required-info. If you do not have access to the internet and need a hard copy, please call your member experience team at the number located on the back of your Network Health member ID card.

By Laura Lopez
TPhotography
wo days after Christmas in 2023, Network Health member Mark S. sent his wife Jeanne a text asking her to pick him up from work because he wasn’t feeling well.
Jeanne, a Network Health employee, left work to pick Mark up. When they arrived at home, he went to the bedroom to rest. Within a few minutes, Jeanne heard a noise and found Mark on the floor of the bedroom. She immediately called 911, and Mark was rushed to the hospital.
A CT scan revealed he was bleeding internally, and his spleen had ruptured. Emergency surgery was performed to remove his spleen. During the surgery, the surgical team found enlarged lymph nodes and took several biopsies. Mark spent a week recovering in the hospital. During this time, he underwent
additional blood work. The medical team raised concerns about the possibility that Mark might have chronic lymphocytic leukemia (CLL).
After Mark left the hospital, he and Jeanne were unsure what to do next.
“We went to Mark’s follow-up appointment at the surgeon’s office, but no one was able to give us any test results. They told us they didn’t have access and that it would take a couple of weeks.”
Without any clear guidance, Jeanne and Mark continued to wait for answers about Mark’s health.
That’s when Cheryl H., registered nurse and care manager at Network Health, contacted Mark. As a care manager, Cheryl routinely reaches out to members like Mark who are transitioning from the hospital to home.
After talking with Mark and Jeanne, Cheryl knew it was important for Mark to be seen quickly. She successfully secured an appointment with a local oncologist within a couple of days.
Cheryl was very strong and very supportive, and she told us ‘You don’t need to wait, this needs to be done right away’,” said Jeanne.
The oncologist’s office got the biopsy results and did additional testing to quickly arrive at the diagnosis – chronic lymphocytic leukemia (CLL).
While the diagnosis was difficult, Jeanne and Mark made informed decisions on how to proceed with treatment with the support and expertise of the oncologist and care manager guiding them.
“Cheryl helped us all along the way. She even mailed us a packet of paperwork for Mark’s PHI consent, POA and advance directive so that I could speak with her directly on Mark’s behalf.”
As Jeanne and Mark navigated his diagnosis over the next year, Cheryl continued to check in regularly by phone, or when it was more convenient, by email.
The first year, I reached out to her with a lot of questions. She was our cheerleader. Having her right there was really helpful,” said Jeanne.
As Mark’s treatment for CLL is ongoing, Cheryl continues to be a resource and a cheerleader. “I don’t know where we would be right now if we didn’t have Cheryl,” Jeanne shared.
When a member is facing a difficult diagnosis, complex medical condition or behavioral health condition, having an experienced and compassionate care manager like Cheryl by their side can ensure that the member gets the care they need, when they need it. Network Health care managers provide personalized care and advocate for members in the following ways.
• Review medications and treatment plans
• Identify signs that a health condition is worsening so the member understands when to act, including when to contact their health care provider
• Work with a member’s health care provider to ensure they are aware of changes in the member’s health
• Include the member and their caregivers in health care decisions
• Share helpful community resources

For Cheryl, care management is more than a job. “It’s who I am, and it’s a huge part of my life. You’re helping people and sometimes you’re actually changing their lives. It’s very rewarding.”
As for members, Cheryl shared they often tell her “It’s so nice to call and have an actual person to talk to.” She also explained that members are surprised to find out that their health plan offers care management services at no cost.

If you or a loved one are navigating complex health needs, Network Health’s care management team is here for you, whether you need help coordinating appointments, navigating treatment plans or finding someone to talk to.
Accessing these services is simple.
• Transition of Care. A Network Health care manager may contact you during a transition of care, such as returning home from the hospital.
• Referral. You can ask your personal doctor or health care provider for a referral to care management.
• Self-Initiation. You can contact the care management team at Network Health to explore your options. Call 866-709-0019 (TTY 711) Monday–Friday, 8 a.m. to 5 p.m. or visit networkhealth.com/ wellness/care-management.
Your health journey matters to us. Our dedicated RNs and social workers are here to listen with compassion and help you navigate the path that’s right for you.”
– Katie M., manager of care management




Network Health believes in building healthier communities—both through providing exceptional health plans and through giving back. In 2024, our dedication to making a positive impact reached new heights, and we couldn’t have done it without our members, clients and community partners.
Throughout 2024, we invested in our local Wisconsin communities by spending $917,155.82 with businesses that are also Network Health clients. We believe in supporting those who support us, and this significant investment reflects our commitment to keeping business local.
But it’s not just about dollars spent. Our employees showed their passion for community involvement by volunteering over 2,640 hours throughout the year. That’s 61.5% of our employees stepping up to make a difference, helping support 95 different organizations through their time and dedication.
Network Health also partnered with 138 Wisconsin organizations to host and support 473 community and member engagement events, drawing more than 196,000 attendees. From educational seminars and member events to fun, family-friendly gatherings … our goal is always to make every event meaningful and accessible.
As we move forward, we continue to build connections with our communities. Join us this year for more events and opportunities to come together. Some highlights include, Farmers Markets at the Fondy Market in Milwaukee
Appleton Noon Lions Club Senior Expo
Fox Cities Marathon in Appleton
Old Glory Pulling for Honor
Museum of Wisconsin Art (MOWA) in West Bend
For a full list of upcoming events and details, visit networkhealth.com/community.
Thank you for being a part of the Network Health community. Continuing to make 2025 another year of connection, support and health is our top priority.
At Network Health, our mission is to create healthy and strong Wisconsin communities and there are several ways we achieve this. We have voluntary, no cost programs that help empower you to take charge of your well-being to be the healthiest “you” possible. They are our health coaching, care management and condition management programs, designed to support you through your health journey.
Network Health members have access to health coaches. These health and wellness experts help members reach their personal health goals.
Members receive one-on-one discussions with a coach, trained in behavior change and motivational encouragement, self-management tools to help with nutrition, weight management, stress, blood pressure, blood sugar, tobacco use and more and access to a Network Health pharmacist for prescription questions.
Our care management program is for members who are experiencing a shortterm illness or more complex diagnosis. Network Health’s care managers provide personalized support to help members and their caregivers manage current health conditions.
The program begins with a one-on-one connection with a care manager, who is a nurse or social worker. They ensure you feel included and put you in control of your health care decisions.
Our condition management program is for members with chronic conditions
such as asthma, diabetes, chronic obstructive pulmonary disease (COPD), heart disease, stroke or heart failure. Condition managers help members identify and understand existing conditions, connect with education and resources to manage their journey with confidence, promote emotional health and more. You can be referred to the condition management program by your personal doctor, caregiver, yourself or through claims, labs or information from Medicare.
Care and condition management will work with members to develop an individualized care plan and work with their personal doctor to coordinate and communicate the care plan. Together with the member, they review medications and treatments, inform if there are signs that conditions are worsening and share community resources.
There is a lot to consider when deciding which health plan is best for you. Network Health offers a variety of health insurance plans from which to choose. Often, the decision is between a High Deductible Health Plan (HDHP) and a traditional plan.
Generally speaking, HDHPs have low premiums and high deductibles. On the other hand, traditional health plans have higher premiums and lower deductibles. Deciding which plan is best for you comes down to your needs and budget.
Traditional health plans have lower deductibles, so they make a good option if you or members of your family go to the doctor often. It might also make sense if you expect major medical costs in the future, such as having a baby.
HDHPs have a high deductible that must be met before the plan starts paying its share. However, with its lower premiums, if you are healthy and do not go to the doctor often, an HDHP may save you money in the long run.
These are general examples and may not be true in every case. However, when you are comparing these two types of plans, it is a good place to start.
Regardless of what plan you choose, Network Health’s Member Experience Team will provide the same great customer service you expect. We’ll help you make the most of your coverage.
• May not have copayments; which means you could pay the full cost until your deductible is met
• Higher deductible
• Lower premiums
• Often combines with a health savings account (HSA)
• Has copayments until you meet your deductible; then you may pay coinsurance
• Lower deductible
• Higher premiums
• Health savings account (HSA) may not be as important
by Ted Regalia, RPh, vice president of pharmacy benefits and Beth Coopman, PharmD, pharmacist at Network Health
A nationwide effort to address the ongoing opioid crisis has made some progress, however, challenges still exist. The good news is, according to the Centers for Disease Control and Prevention (CDC), the national opioid dispensing rate declined from 46.8 opioid prescriptions per 100 people in 2019 to 37.5 opioid prescriptions per 100 people in 2023. Despite this progress, opioid-related deaths grew to over 105,000 in 2023.
Opioid use disorders can happen to anyone. These disorders include opioid addiction, which can interfere with a person’s health, well-being and quality of life, not to mention the hardship and strain it can cause loved ones.
The scale of this crisis underscores the need for comprehensive solutions. Here are the ways our members, providers and Network Health all play a role in keeping our communities safe.
The State of Wisconsin uses a monitoring program requiring doctors to consult a website every time they prescribe a controlled substance that includes opioids. This displays prescriptions from other doctors and pharmacies across the United States, so the prescriber has a full picture of the medications a patient is receiving. Additionally, Wisconsin doctors are required to take continuing education classes on safe opioid prescribing.
Naloxone is an opioid antidote and is a life saver in cases of opioid overdose. Wisconsin allows naloxone to be sold over the counter without a prescription and it can even be found in some specialized vending machines. We strongly recommend you discuss naloxone with your personal doctor or pharmacist.
We have implemented quantity limits on new prescriptions for members who have not had an opioid in the last six months. In other words, if you are not a routine opioid user, you will be limited in the number of pills you receive. This is to prevent unintentional intake, overdoses or the unused opioids getting into the wrong hands. We have also put a prior authorization in place for cases where high-dose opioids are medically necessary.
For patients experiencing opioid use disorders, specialized doctors have different medication therapies that may assist with recovery such as other medications, counseling and behavioral therapies. If you are concerned about your opioid use, please contact your personal doctor to discuss the options available. To find out more about medication assisted treatment plan coverage, call your Network Health member experience team at the number found on your member ID card.
You play the most important role. If you need pain control, use additional treatment options to help minimize your opioid use, including non-opioid medications, physical therapy and other interventions suggested by your doctor. Also, store your pain medication in a secure place, do not share your medications with others and dispose of unused medications either at your pharmacy or follow disposal instructions provided by the Food and Drug Administration (FDA) at fda.gov. Finally, teach those around you about naloxone and how to use it.
by Anna Peterson Sanders, PharmD, BCGP, pharmacist at Network Health
The advent of biosimilars has played an important role to contain medical costs as we continue to see rising prices on both existing drugs and new drugs coming to the market. These biosimilars have a reduced cost with some up to 90 percent less than the original, first-to-market product, or “reference product.” While some health plans may want to retain rebates by steering you to the reference product, Network Health chooses to pass those savings on to you by covering these lower cost biosimilar products.
A biosimilar can be compared to a generic medication. However, they differ from the term “generic” since the active ingredient in generics tend to be a smaller molecule that is easier to replicate. Biologics and their biosimilars are large and complex protein structures created through living organisms which could have slight variations. No dose or batch will be exactly the same. However, the slight variations that do exist occur outside the clinically active portion of the molecule and do not interfere with how the drug works in your body.
Yes. The Food and Drug Administration (FDA) requires that manufacturers of biosimilars demonstrate there are no differences in safety and effectiveness compared to the reference product. Biosimilar purity, molecular structure and activity in the body must also be comparable.
Below are examples of the biosimilar medications in your formulary. While these drugs are anti-inflammatories used to treat conditions such as rheumatoid arthritis, plaque psoriasis and Crohn’s disease, other biosimilars exist such as insulin products and some cancer drugs. Switching to a lower cost alternative can be a huge savings. Even if you have reached your maximum out-of-pocket, switching to a lower cost medication helps to contain medical costs which keeps your premiums stable each year.

*Pricing acquired from IPD Analytics on May 19, 2025.
If you, your child or someone you know is turning 26 soon and won’t be enrolling in an employer’s group plan, we invite you to review Network Health’s Individual and Family Plans. We offer a variety of plans to ensure excellent coverage, along with the high-quality service you’ve come to expect. And let’s not forget, we are Wisconsin-based and are here when you need us.
We understand that health insurance isn’t always the easiest item to shop for. This is true for those who have purchased and used it for years, and it can be even more complicated if you’re shopping for the first time.
That’s where Network Health can help. For over 40 years, we have been a trusted expert in health insurance, offering a different kind of health plan that puts members first. Our plans are easy to understand and affordable. We can provide the information needed to help you choose the plan that’s best for you. Making sure you keep up on your preventive medical tests, appointments and procedures, as well as dental care, is vital in maintaining a healthy "you".
If you or someone you know is turning 65, now is a perfect time to explore our Medicare Advantage plans.
We are Wisconsin. Just like you. You will receive the same exceptional one-on-one service you’ve experienced for years and we make enrolling in a Medicare Advantage plan easy.
As good as Original Medicare is, it will not cover all your health care expenses. Most people who are eligible for Medicare choose to get their benefits through private health insurance companies to help cover costs. With a Network Health Medicare Advantage Plan, you’ll get extra benefits that Original Medicare doesn’t cover. With plan options that give you the flexibility to choose the best Medicare Advantage plan that pairs a $0 monthly premium with the extra benefits that fit your lifestyle best. It’s your choice.
